The Widening Challenge: How to Learning
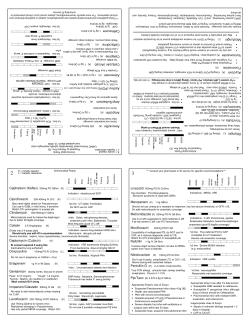
n ng io ui at in uc nt Ed Co ical ed M The Widening Challenge: How to Manage MRSA This once-limited organism is now thriving outside the hospital. Learning Objectives Upon completion of this article, the reader will 1) Have an appreciation for the increasing prevalence of communityacquired and hospitalacquired MRSA. 2) Be able to identify community-acquired and hospital-acquired MRSA on a culture and sensitivity report. 3) Have a basic understanding of the mechanism of resistance and the rationale for antibiotic selection for MRSA. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Continuing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $17.50 per topic) or 2) per year, for the special introductory rate of $109 (you save $66). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. In the near future, you may be able to submit via the Internet. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 192. Other than those entities currently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity. PM will, however, use its best efforts to ensure the widest acceptance of this program possible. This instructional CME program is designed to supplement, NOT replace, existing CME seminars. The goal of this program is to advance the knowledge of practicing podiatrists. We will endeavor to publish high quality manuscripts by noted authors and researchers. If you have any questions or comments about this program, you can write or call us at: Podiatry Management, P.O. Box 490, East Islip, NY 11730, (631) 563-1604 or e-mail us at bblock@juno.com. An answer sheet and full set of instructions are provided on pages 192-194.—Editor Photodisc By Warren S. Joseph, DPM and Mark Kosinski, DPM S taphylococcus aureus is one of the most common organisms encounteredin podiatric practice. For decades, beta-lactam www.podiatrym.com antibiotics have been the mainstay of therapy. Unfortunately, this treatment paradigm is changing. Staphylococcus Aureus, an Evolving Pathogen Staphylococcus aureus is one of the most common organisms encountered in podiatric practice. For decades, beta-lactam antibiotics have been the mainstay of therapy. Unfortunately, this treatment paradigm is changing. Methicillin-resistant Continued on page 140 NOVEMBER/DECEMBER 2005 • PODIATRY MANAGEMENT 139 M C ed on ica tin l E ui du ng ca tio n MRSA... Staphylococcus aureus (MRSA) has been isolated with increasing frequency from lower extremity infections. In some settings, MRSA has become the predominant form of S.aureus isolated from uncomplicated skin infections in the community. Some strains of MRSA produce cytotoxic virulence factors, resulting in severe necrotizing infections. In the era of resistance, the importance of taking a culture has taken on new meaning. MRSA: Thriving Outside the Hospital Since the introduction of penicillin in 1941, S. aureus has undergone a slow but steady metamorphosis. Methicillin was first introduced for clinical use in 1960 to combat the growing incidence of beta-lactamase production among S. aureus. Within a year of its introduction, the first strains of S. aureus resistant to methicillin began to emerge in the United Kingdom. Shortly afterwards, in 1963, MRSA appeared among staphylococci causing blood stream infections in Danish hospitals. Originally a nosocomial pathogen, MRSA has become endemic in the United States and many parts of the world and has become increasingly common in the community, occurring in patients with and without established risk factors. Mechanism of Resistance To understand why some drugs are active against MRSA and others are not, it is helpful to look at Since the introduction of penicillin in 1941, S. aureus has undergone a slow but steady metamorphosis. the mechanism of resistance. Methicillin resistance is associated with the presence of penicillin binding protein 2a (PBP2a). PBP2a, encoded by the mec A gene, has a low affinity for Betalactam antibiotics, resulting in resistance to all currently available Beta-lactam drugs. By definition, penicillins, cephalosporins, carbapenems and monobactams have no activity against MRSA. Horizontal transfer of the mec A gene Why is oxacillin tested instead of methicillin? A useful drug in its day, methicillin has fallen out of use in favor of safer, more active antibiotics. When reviewing a culture and sensitivity report, we now look to oxacillin as a surrogate marker for methicillin resistance. Oxacillin is more resistant to degradation in storage and is more likely to detect heteroresistant strains than methicillin. The acronym MRSA is still used to describe these isolates because of its historic role. For all practical purposes, resistance to oxacillin (ORSA) is synonymous with resistance to methicillin (MRSA). MRSA is defined as having an oxacillin MIC90>/= 4ug/ml. All MRSA is Not Created Equal MRSA can be divided into two main types: community-acquired MRSA (CA-MRSA) and hospital-acquired MRSA (HA-MRSA). The distinction between the two has become more difficult over the years as HAMRSA strains move into the community and CA-MRSA strains move into the hospital. Each, however, has important distinguishing features. Continued on page 141 FIGURE 1 FIGURE 2 Community-acquired MRSA (CA-MRSA) Hospital-acquired MRSA (HA-MRSA) Antibiotic Sensitivity Antibiotic Sensitivity Cefazolin Amoxicillin Oxacillin Erythromycin Tetracycline Clindamycin TMP/SMX Vancomycin Linezolid Resistant Resistant Resistant Resistant Sensitive Sensitive Sensitive Sensitive Sensitive Cefazolin Amoxicillin Oxacillin Erythromycin Tetracycline Clindamycin TMP/SMX Vancomycin Linezolid Resistant Resistant Resistant Resistant Resistant Resistant Resistant Sensitive Sensitive Multi-drug susceptible, community-acquired MRSA. Note susceptibility to all beta-lactam antibiotics. 140 into known MSSA strains converts the strains into MRSA in all cases. Multi-drug resistant, hospital-acquired MRSA. PODIATRY MANAGEMENT • NOVEMBER/DECEMBER 2005 www.podiatrym.com n ng io ui at in uc nt Ed Co ical ed M MRSA... beta-lactam antibiotics. This explains why HA-MRSA strains are multi-drug resistant. Type II is the most prevalent of these HA-MRSA strains found in the United States. SCC mec elements IV and V found in CA-MRSA strains lack an- tential to be more tissue destructive than its hospital counterpart. This is in part due to the production of cytotoxic virulence factors known as Panton Valentine Leukocidins (PVL’s). CA-MRSA isolates containing PVL genes have been linked to recurrent, severe necrotizing skin infections similar to those seen in Group A Streptococcal disease2. PVL’s create pores in the leukoCA-MRSA cyte membrane causing cell death and are Type IV, V thought to be in part responsible for the rapid More spread of infection. PVL More Common genes are less commonly found in HA-MRSA or Sensitive except MSSA community isoBeta-lactams lates. Strict definitions for CA-MRSA vary. The Centers for Disease Control and Prevention have defined CA-MRSA as an isolate obtained from a patient in an outpatient setting or in the first 48 hours of hospitalization in the absence of identified risk factors for acquisition. Others have relied on the antibiotic resistance Feature HA-MRSA profile, usually referring to clindamycin suscepMec-A Type I, II,II tibility to define CAMRSA isolates1. Toxins Fewer What all strains of PVL Rare MRSA have in common is the presence of the Abx Resistant Multiply mec-A gene and resisresistant tance to all antibiotics containing a Beta-lactam Inducible Clindamycin ring. Where CA-MRSA Community-acquired MRSA produce more toxins and virulence Resistance: MLS and HA-MRSA differ is in factors than its hospital counterpart. Clindamycin contintheir susceptibility to ues to be a commonly-prescribed non-beta lactam antibiotics. CAtibiotic resistance genes other than antibiotic for the treatment of meMRSA can be considered multi-drug mecA, thereby explaining resisthicillin-susceptible Staphylococcal susceptible (Figure 1), whereas HAtance only toward beta-lactam infections, and has even shown to MRSA can be considered multi-drug drugs. CA-MRSA can be considhave activity against some strains resistant (Figure 2). The reason for ered, by comparison, to be a multiof CA-MRSA. It is likely, however, this apparent paradox lies in their drug susceptible type of MRSA. that the true incidence of clingenetic makeup. damycin resistance has been underThe mec-A gene is contained CA-MRSA: Multi-Drug estimated. within a mobile genetic element Susceptible, But More Virulent It is standard practice to rely on called the staphylococcal chromoAlthough originally thought to some cassette mec or SCCmec. be a less virulent organism, MRSA Continued on page 142 has recently been shown to be more virulent MRSA can be than MSSA. In a study by Engedivided into two mann in 2003, main types: patients with MRSA skin and community-acquired skin structure inAntibiotic Sensitivity MRSA (CA-MRSA) fections had a Ampicillin-sulbactam Resistant greater 90-day and hospital-acquired mortality, a Cefazolin Resistant MRSA (HA-MRSA). longer duration Penicillin Resistant of infection and incurred twice Oxacillin Resistant the amount of There are currently five known alErythromycin Resistant hospital charges lotypes, designated SCCmec types Clindamycin Sensitive versus those paI-IV. HA-MRSA strains contain SCtients with MSSA Cmec types I, II and III. Whereas Tetracycline Sensitive infections5. CA-MRSA strains contain SCC mec TMP/SMX Sensitive types IV and V (Figure 3). Paradoxically, Vancomycin Sensitive The genetic sequence of type although more SCCmec found in HA-MRSA resusceptible to anveals plasmids and transposons tibiotics, CAthat mediate resistance to nonMRSA has the po- CA-MRSA with Inducible Clindamycin Resistance FIGURE 3 MRSA Differences FIGURE 4 Inducible Clindamycin Resistance www.podiatrym.com NOVEMBER/DECEMBER 2005 • PODIATRY MANAGEMENT 141 M C ed on ica tin l E ui du ng ca tio n MRSA... a culture and sensitivity report to choose an antibiotic for directed therapy. In the case of clindamycin, however, culture and sensitivity results may not always be reliable. A phenomenon known as inducible clindamycin resistance (ICR) may mislead the clinician into thinking that a particular strain of S. aureus is susceptible to clindamycin, when in fact it is not. During laboratory testing, S. aureus appears to be resistant to erythromycin and susceptible to clindamycin, however, once the patient is exposed to clindamycin, he or she may quickly develop resis- Although originally thought to be a less virulent organism, MRSA has recently been shown to be more virulent than MSSA. tance (Figure 4). Staphylococcal strains which possess the erm gene prevent macrolides and lincosamides (erythromycin and clindamycin) from binding to their target site. Clindamycin is a poor inducer of the erm gene compared to erythromycin. The isolate may appear sensitive on laboratory testing but the patient may fail to respond clinically. Inducible clindamycin resistance is seen in both MRSA and MSSA isolates. It has also been found that this inducible resistance extends to streptogramin b antibiotics, giving rise to the acronym MLS (macrolide, lincosamide, streptogramin) resistance. In some regions of the United States, a high proportion of CAMRSA isolates are clindamycin resistant. If the proportion of clindamycin resistant MRSA isolates exceeds 10-15 percent, it is recommended that cindamycin not be used as empiric treatment of suspected S. aureus infections3. Although clindamycin should be used with caution if erythromycin re- 142 recognition of two distinct genotypes. Although, with the exception of clindamycin as mentioned previously, just about any drug that is shown on the C&S report to be effective against the particular organism which has been isolated, can be selected. Some of the most freThe “D” Test quently mentioned and prescribed The “D” test is a double-disc antibiotics include the later generdiffusion test in which an eryation tetracyclines and trimethothromycin disc is placed 15 mm. prim/sulfamethoxazole. It should away from a clindamycin disc on be noted that few of these drugs an agar plate inoculated with S. auhave much medical evidence bereus. If inducible resistance is prehind their efficacy as the studies sent, a flattening of the zone of inhave not been performed on these hibition around the clindamycin older compounds. Furthermore, disc will be seen (Figure 5). This the FDA has not approved any of flattened zone of inhibition resemthese older agents as being specifibles the letter “D,” hence the name cally effective against MRSA. FDA “D” test. In one study, D tests of risk categories will help the physi91 clindamcin-susceptible, erycian choose the safest agent for thromycin resistant, S. aureus isotreatment of MRSA infections in lates showed that 68% of MSSA pregnant patients (Figure 6). and 12.3% of MRSA cultures were Probably the largest study to date D test positive4. It is recommended dealing with this issue was recently that the clinician contact a micropublished by Ruhe. In his study of biology laboratory to see if the “D” 24 patients with serious tetracycline test is routinely performed. sensitive MRSA infections (67% had complicated skin and skin structure Treatment Options infections) both doxycycline and Because of the increasing inciminocycline were used. Clinical cure dence of MRSA and the realization was achieved in 83% of these pathat there are, in fact, two distinct tients. Both drugs were well-toleratgenetic strains causing human ined. The conclufection, there has sion of this study been a correwas that long-actsponding interest The “D” test is a ing tetracyclines in finding new may be a reasontherapies against double-disc diffusion able treatment althese organisms. test in which an ternative6. The reAs discussed in detail above, not mainder of this erythromycin disc is all MRSA has the section will deal placed 15mm away same susceptibiliwith those drugs ty patterns. While that are specificalfrom a clindamycin disc HA-MRSA is usuly designed and on an agar plate ally only treated approved for use with non-beta against MRSA. inoculated with S. aureus. lactam antibiotics specifically deVancomycin signed to be used First approved against MRSA, CA-MRSA is usually in 1958, vancomycin has long been susceptible to a wide range of both the mainstay in the treatment of paold and new drugs. tients with serious MRSA infections. Some of these would never Despite recognized issues with inadhave been considered appropriate equate tissue penetration, the ability therapy for MRSA before this Continued on page 143 sistance is present, it is possible to have resistance to erythromycin without it signifying inducible clindamycin resistance. To determine if this is the case, the microbiology laboratory must Figure 5: The “D” test. Note the perform the “D” flattening of the zone of inhibitest. tion around the clindamycin disc. PODIATRY MANAGEMENT • NOVEMBER/DECEMBER 2005 www.podiatrym.com n ng io ui at in uc nt Ed Co ical ed M MRSA... oxazolidinone antibiotic has been pancytopenia in pashown in a number of randomized, tients receiving this drug to only dose it IV and concerns controlled clinical trials to be a for longer than 10 days. This about toxicity, it has established itvery effective drug for the treatis something that does need to self as an overall effective and safe ment of MRSA in complicated SSSI, be monitored if the patient will be drug for most MRSA infections. Its including diabetic foot infections. on a prolonged course of therapy. acceptance was further bolstered by In fact, it is one of a very few anInterestingly, at least two studies the perception that, quite frankly, it tibiotics that is specifically FDA-inhave looked at the potential to was “all there is.” In fact, it was; dicated for the treatment of diabetcause hematologic adverse events however, despite ic foot infections. versus that for vancomycin. In a the development It has the further study of 686 patients with nosocoof newer agents advantage of mial pneumonia, linezolid-induced First approved that have shown being 100% thrombocytopenia was found 6.4% remarkably higher bioavailable in of the time. With vancomycin, the in 1958, vancomycin efficacy rates and the oral formulasame was found 7.7% of the time10. has long been the rather staggering tion so its efficaRao looked at patients given long vancomycin failcy would be comterm therapy for orthopedic infecmainstay in the ure rates against parable whether tions and likewise found that there treatment of patients MRSA for skin and given IV or PO. were similar hematologic effects with serious MRSA skin structure inLooking at with a trend towards greater effect fections (SSSI), the the data, in a with vancomycin. Also, patients infections. drug remains the comparative trial placed on vancomycin first, folmainstay of treatof infected foot lowed by linezolid actually did ment in many ulcerations in dihave a higher rate of thrombocyhospitals and in the minds of many abetic patients, linezolid was comtopenia. All cases were reversible. physicians. Much of this may be atpared to ampicillin-sulbactam and tributed to a “comfort zone” situaamoxicillin-clavulanate, and found Daptomycin tion where docs have used the drug to be statistically more effective8. The second of the newer antifor almost half a century and they MRSA antibiotics to have data speAgainst vancomycin for complicatare comfortable with it, shortcomcific for SSSI is the cyclic lipopeped SSSI, Weigelt found that microings and all. biological cures Furthermore, the cost of some against MRSA of the new drugs is quite offwere found with putting to many physicians, palinezolid 87% of tients and pharmacies that need to the time versus stock the newer, expensive drugs. only 48% of the There is also a widely held theory time with vanthat all new antibiotics should be c o m y c i n “reserved” or restricted only to (p=0.0022)9. Antibiotic Category cases in which “Old Faithful” fails. Given the suThe problem with this approach is periority of this Clindamycin B that by the time the new drug is drug against Daptomycin B started, the patient may have lost commonly used Trimethoprim/sulfamethoxazole C limb or life. antibiotics in More recently there have been podiatric mediLinezolid C concerns about the development cine, where does Vancomycin C of tolerance and frank resistance of this fit? CertainMinocycline D staphylococcus to vancomycin. ly, in patients Vancomycin Intermediate Staphywith diabetes lococcus aureus (VISA) was first rewho have MSSA ported in Japan in 1997. As of infections, you Antibiotics with activity against MRSA and their FDA risk 2004, there are at least nine reportwould not use categories for pregnancy. ed cases in the US. Furthermore, linezolid. Stanthe first reports of vancomycin-retide drug daptomycin. This drug is dard therapy with a cephalosporin sistant Staphylococcus aureus effective against Staphylococcus auor other beta-lactam agent would (VRSA) was found in patients with reus-resistant to methicillin, vanbe most appropriate. In patients diabetic foot ulcerations7. comycin and linezolid. In its cliniwith diabetes who have a concal trials, daptomycin was tested firmed MRSA infection, however, against vancomycin for MRSA isothis drug, even given orally, could Linezolid lates and a penicillinase-resistant very well be statistically more efLinezolid was the first of the penicillin for MSSA. Of the 902 fective than vancomycin. newer generation of anti-MRSA anavailable patients, only about 10% Much has been made about the tibiotics to have clinical relevance potential for thrombocytopenia or to podiatric medicine. This novel Continued on page 144 FIGURE 6 FDA Risk Categories for Pregnancy www.podiatrym.com NOVEMBER/DECEMBER 2005 • PODIATRY MANAGEMENT 143 M C ed on ica tin l E ui du ng ca tio n MRSA... had MRSA. Clinical success rates were 81.1% for daptomycin vs. 73.8% for vancomycin12. This is most interesting to again demonstrate the rather significant vancomycin failure rates that have been found across a range of trials for different antibiotics. If between one-quarter to one-half of patients do not respond on vancomycin can it still be considered first line therapy? Data specifically against diabetic infections is somewhat sparse in that only about 12% of this population had a diabetic foot infection. Daptomycin can only be given parentally as no PO formulation exists. It does have the theoretical advantage of being considered a bactericidal agent but the validity of that advantage has been called into question13. At this point, its use in podiatric medicine remains to be elucidated. It could be effective in more resistant organisms, even those found resistant to linezolid. Also, the theoretical advantage of its bactericidal activity may be useful in osteomyelitis but no studies yet exist to demonstrate its efficacy. without the use of specific anticomycin-aztreonam combination in MRSA antibiotics15. treating patients with complicated SSSI. Looking at CA-MRSA in a more At least on the surface this general group of 453 patients, Fridlooks to be an ideal drug for podkin found that initial antibiotic iatric infections, especially in therapy that was inactive against those with severe diabetic foot CA-MRSA did not increase the infections. chance for an adverse outcome Monotherapy would be usable versus those that received antibecause combination drug therapy MRSA antibiotics. to cover MRSA, This last secgram negatives tion emphasizes and anaerobes one of the oldest The latest would be elimiaxioms of clinical nated. It may be infectious disdrug to receive FDA a bit too early to eases: It is imporapproval for get overly enthutant to treat your siastic, however. patient and not the treatment Careful analysis the culture reof MRSA SSSI is the of this data port. If the patetracycline derivative shows that in the tient is improvtigecycline group ing despite a cultigecycline. of 422 patients, ture report showonly 83 (<20%) ing MRSA resishad diabetes and tant to the preonly 7.1% had infected ulcers. Of scribed antibiotic, do not change greatest concern is the incredibly therapy—monitor the patient. high rate of gastrointestinal adYes, MRSA is an increasing verse events. Nausea occurred in problem. It has become much 34.5% of the patients, vs. 8.2% for more common than ever before. the comparator, and vomiting ocFurthermore, we now have the curred in almost 20% of patients added challenge of determining vs. 3.6% for the comparator. It will whether or not the patient prebe interesting to see how this drug sents with CA or HA-MRSA. Fortuis positioned and whether or not nately, new therapies are arriving more clinical experience bears out to treat those who really need the problem with the GI events. them. ■ Tigecycline The latest drug to receive FDA approval for the treatment of MRSA SSSI is the tetracycline derivative tigecycline. This drug is particularly The No Treatment Option exciting because up to this point all Although an anathema to other anti-MRSA drugs have been many podiatric physicians, there specifically targeted against gram comes a time positive organisms when no treatonly. Tigecycline ment may be the is a broad specLinezolid was best treatment. trum agent effecThis is particulartive against a wide the first of the newer ly true of MRSA. range of both sengeneration of Studies are startsitive and multiing to show that resistant gram anti-MRSA antibiotics just because positives, gram to have clinical MRSA is cultured negatives and from a wound, it even anaerobic orrelevance to podiatric may not be necganisms. In the medicine. essary to utilize pivotal phase 3 trispecific antials tigecycline was MRSA therapy. compared to vanLooking specifically at diabetic comycin with aztreonam for SSSI14. foot infections, Dang found that 1,116 patients were enrolled and although the overall number of 833 were clinically available. Clinipatients growing MRSA doubled cal response rates were found to be over a three year period, MRSA similar between the two arms. The was eradicated with debridement, conclusion was that tigecycline was topical treatment and isolation as safe and efficacious as the van- 144 PODIATRY MANAGEMENT • NOVEMBER/DECEMBER 2005 References 1 Crawford S, Daum R. Epidemic community-asociated methicillin resistant staphylococcus aureus:modern times for an ancient pathogen. The Pediatric Infectious Disease Journal. 24(5) May 2005 459-460. 2 Chambers H. community associated MRSA-resistance and virulence coverage. New England Journal of Medicine. 352:1485-1487 April 2005. 3 Kaplan S Treatment of community-associated methicillin resistant staphylococcus aureus infections. The Pediatric Infectious Disease Journal. 24(5) May 2005 457-458. 4 Levin T, Suh B, Axelrod T et.al. Potential Clindamycin Resistance in Clindamycin-Susceptible, Erythromycin-Resistant Staphylococcus aureus: Report of a Clinical Failure Antimicrobial Agents and Chemotherapy, March 2005, p. 1222-1224, Vol. 49, No. 3. 5 Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, Briggs JP, Sexton DJ, Kaye KS. Ad- Continued on page 145 www.podiatrym.com E X A M I N A T I O N verse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003 Mar 1;36(5):592-8. 6 Ruhe JJ, Monson T, Bradsher RW, Menon A. Use of longacting tetracyclines for methicillin resistant staphylococcus aureus infections: Case series and review of the literature. Clin Infect Dis. 2005 May 1: 40:1429-30. 7 Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004 Aug 15;39(4):539-45. 8 Lipsky Ba, Itani K, Norden C, et al. Treating foot infections in diabetic patients : A randomized, multicenter, open label tiral of linezolid vs. ampicillin sulbactam/amoxicillin clavulanate. Clin Infect Dis 2004 January 38:17-24. 9 Weigelt J, Kaafarani HMA, Itani KMF, Swanson RN. Linezolid eradicates MRSA better than vancomycin from surgical site infections. American Journ Surg. 2004 118:760-766 10 Nasraway ST, Shorr AF, Kuter DJ, et al. Linezolid does not increase the rist of thrombocytopenia in patients with nosocomial pneumonia: Comparative analysis of linezolid and vancomycin use. Clin Infect Dis. 2003 Dec 11:1609-16 11 Rao N, Ziran BH, Wagener MM, Santa ER, Yu VL. Similar hematologic effects of long term linezolid and vancomycin therapy in a prospective observational study of patients with orthopedic infections. Clin Infect Dis. 2004. 38:1058-64. 1 2 Arbeit RD, Maki D, Tally FP, et al. The safety and efficacy of daptomycin for the treatment of complicated skin and skin structure infections. Clin Infect Dis 2004 June 38:1673-81. 13 Pankey GA, Sabath LD. Clinical Relevance of bactierostatic versus bactericidal mechanisms of action in the treatment of Dr. Joseph is edigram positive bacteri- tor of the Journal al infections. Clin In- of the American fect Dis 2004 March Podiatric Medical Association and is 38:864-70. 14 Ellis-Grosse EJ, a podiatrist at Babinchak T, Dartois the Coatesville N, et al. The efficacy VA Medical CenPA. Dr. and safety of tigecy- ter, cline in the treatment Joseph is author of skin and skin struc- of Handbook of Lower Extremity Inture infections: Re- fectious Diseases (2nd Ed.). sults of two doubleblind phase 3 comparison studies with vancomycin-aztreonam. Clin Infect Dis 2005 Suppl 5. 41:S341-53. 15 Dang CN, Prasad YDM, Boulton AJM, Jude EB. Methicillin resistant Staphylococcus aureus in the diabetic foot clinic: a worsening problem. Diabetic Medicine. 20:159-161 2003. 16 Fridkin SK, Hageman JC, Morrison MHS, et al. Methicillin resistant Staphylococcus aureus disease in three communities. NEJM 352:1436-44, 2005. www.podiatrym.com Dr. Kosinski is a professor in the Department of Medicine and Chairperson of the Institutional Review Board at the New York College of Podiatric Medicine. He is an Instructor in the Department of Surgery at New York Medical College and a contributing editor to the Journal of the American Podiatric Medical Association. Dr. Kosinski has lectured and written extensively on lower extremity infections and is actively involved in clinical research. He completed a fellowship in Podiatric Infectious Diseases at St. Michael’s Medical Center in Newark, NJ, and is a member of the Infectious Diseases Society of America. See instructions and answer sheet on pages 194-196. n ng io ui at in uc nt Ed Co ical ed M MRSA... 1) Which of the following antibiotics is active against CA-MRSA? A) cephalexin B) minocycline C) amoxicillin/clavulanate D) dicloxacillin 2) You are treating an uncomplicated skin infection in a pregnant patient. Which of the following antibiotics is the least safe to use? A) linezolid B) vancomycin C) minocycline D) daptomycin 3) Which of the following has 100% bioavailable after oral administration? A) vancomycin B) linezolid C) minocycline D) clindamycin 4) Which of the following antibiotics cannot be used to treat an MRSA infection? A) imipenem/cilistatin B) daptomycin C) vancomycin D) linezolid 5) Penicillin binding protein 2a (PBP2a) is encoded by the A) erm gene B) mec A gene C) MLS gene D) PVL gene 6) Which of the following antibiotics cannot be used in a patient with a history of sulfa allergy? A) minocycline Continued on page 146 NOVEMBER/DECEMBER 2005 • PODIATRY MANAGEMENT 145 M C ed on ica tin l E ui du ng ca tio n E X A M I N A T I O N B) linezolid C) trimthoprim/sulfamethoxazole D) vancomycin 7) CA-MRSA strains contain which SCCmec types? A) I B) II C) III D) IV 8) Which drug is active against MRSA, gram negative organisms and anaerobes? A) vancomycin B) linezolid C) daptomycin D) tigecycline 9) Which anti-MRSA drug is considered bactericidal? A) vancomycin B) linezolid C) daptomycin D) tigecycline 10) In which site was the first reported case of VRSA found? A) Urinary tract B) Blood stream infection C) Diabetic foot ulcer D) Sacral decubitus 11) Methicillin was first introduced in 1960. The first strains of MRSA appeared within A) One year B) Five years C) Ten years D) Fifteen years 146 (cont’d) 12) Vancomycin intermediate S. sureus (VISA) was first reported in A) 1961 B) 1985 C) 1997 D) 2005 13) Which of the following has shown activity against S. aureus resistant to methicillin, vancomycin and linezolid? A) minocycline B) TMP/SMX C) Daptomycin D) Clindamycin 14) Which of the following is available in oral form for treatment of MRSA? A) linezolid B) daptomycin C) vancomycin D) tigecycline 15) Which of the following is safest to use in a pregnant patient? A) linezolid B) clindamycin C) trimethoprim/sulfamethoxazole D) vancomycin 16) The “D” test is used to detect A) inducible clindamycin resistance B) resistance to methicillin C) susceptibility to erythromycin D) susceptibility to daptomycin PODIATRY MANAGEMENT • NOVEMBER/DECEMBER 2005 17) Which of the following has shown reliable activity against hospital acquired MRSA (HA-MRSA)? A) Clindamycin B) TMP/SMX C) Tetracycline D) Vancomycin 18) Which is true about community-acquired MRSA (CAMRSA)? A) It is sensitive to antibiotics except beta-lactams B) It produces fewer toxins than HA-MRSA C) It rarely produces panton valentine leukocidins (PVL) D) It is associated with mec A type I, II, III 19) Resistance to which of the following antibiotics implies resistance to methicillin? A) oxacillin B) erythromycin C) clindamycin D) cephaolthin 20) Penicillin was introduced for clinical use in A) 1938 B) 1941 C) 1952 D) 1956 SEE INSTRUCTIONS AND ANSWER SHEET ON PAGES 194-196 www.podiatrym.com
© Copyright 2025