Document 137708
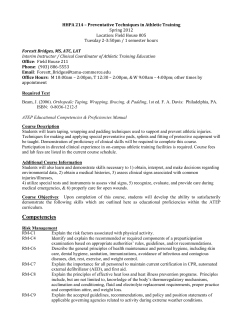
Athletic Pubalgia: Recognition, Treatment, and Prevention A Review of the Literature Sarah B. Rabe, MS, ATC, LAT; and Gretchen D. Oliver, PhD, ATC, LAT ABSTRACT Athletic pubalgia is a term grossly misunderstood throughout the sports medicine community. This syndrome is multifaceted and lacks true definition. Athletic pubalgia involves a wide variety of structures surrounding the pelvis and often results in cessation of physical activity. There are many factors contributing to athletic pubalgia, including sport, position, and gender, and it should be addressed through an initial physical examination. Athletic pubalgia is difficult to assess through diagnostic imaging and is often overlooked or misdiagnosed. To provide optimal health care for patients, athletic trainers and health care professionals must understand athletic pubalgia and distinguish it from other injuries. The purpose of this literature review is to aid in recognizing, treating, and preventing athletic pubalgia and to highlight surgical options. A thletic pubalgia is a multifaceted syndrome that lacks a true definition and confuses many health care professionals. Athletic pubalgia is referred to as a syndrome because it results from several different injuries.1 Athletic pubalgia is most commonly referred to as sport hernia, sportsman’s hernia, Gilmore’s groin, and groin disruption,2 but it currently lacks a universally accept- Ms Rabe is Assistant Athletic Trainer, Athletic Department, and Dr Oliver is from the Graduate Athletic Training Education Program and the Department of Health, Kinesiology, Recreation, and Dance, University of Arkansas, Fayetteville, Ark. Originally submitted January 8, 2009. Accepted for publication June 30, 2009. Posted online September 4, 2009. The authors have no financial or proprietary interest in the materials presented herein. Address correspondence to Gretchen D. Oliver, PhD, ATC, LAT, 309 HPER University of Arkansas, Fayetteville, AR 72701; e-mail: goliver@uark.edu. doi:10.3928/19425864-20090827-01 ed definition.1 Athletic pubalgia is difficult to ascertain; however, clinicians’ ability to recognize the syndrome has increased.3 Increased diagnosis could be attributed to the recent increase in literature and research about athletic pubalgia. Essentially, athletic pubalgia is caused by muscular imbalances and weaknesses that result in an uneven distribution of forces.4 Five percent of all sports injuries occur in the groin area and are caused by activities involving significant twisting and cutting in different directions.5 With a specific mechanism of injury, athletic pubalgia is viewed as sport and position specific. Athletic pubalgia has been found in 58% of football players,2 most commonly in highly skilled positional players, and soccer and ice hockey players.1 Athletic pubalgia primarily affects the pelvic region. The pelvis consists of four pelvic bones: the coccyx, sacrum, and the two hip bones, which join anteriorly at the pubic symphysis. The area of concern is the pubic symphysis and the forces acting on it from muscular attachments. As Meyers et al4 described, it is common to think of the forces acting on the pubic symphysis as being housed in three compartments: anterior, posterior, and medial. The muscle imbalance or weakness involves the anterior, posterior, and medial muscles that have attachment on the pubic symphysis. Muscles of interest include the abdominals, the hamstrings, the three adductors, the gracilis, and the obturator externus. Weak transverse and rectus abdominis often cause the pelvis to tilt, altering the function of the pelvis. If the function of the pelvis is altered, then other muscles (eg, the adductors) will also have altered function. Athletic pubalgia is often referred to as an 25 Rabe & Oliver exertional imbalance and temporary loss of postural control. It is evident that athletic pubalgia is a pelvis injury requiring a multidirectional approach of several medical disciplines. The key diagnostic method that distinguishes athletic pubalgia from other injuries is symptom relief during rest6 and reaggravation when activity resumes.7 It is speculated that athletic pubalgia is a symptom of an overuse injury. In a study of 21 athletes evaluated for chronic groin pain and athletic pubalgia, 19 had two or more injuries that contributed to the groin pain, further emphasizing athletic pubalgia as a syndrome.5 The onset of groin and lower abdominal pain usually leads to the discovery of a weak abdominal wall, with athletes’ chief complaint being a pulling sensation in the groin area.8 Often, athletic pubalgia is misdiagnosed as osteitis pubis, groin strain, or abdominal wall strain.8 The pubis symphysis is a pivot point for the transference of forces from the lumbopelvic joint to the femoroacetabular joint. This transfer of force is often shear in nature (ie, a shearing stress) and results in chronic stress.1 Athletic pubalgia’s mechanism of injury includes trunk hyperextension with simultaneous hip hyperadduction accompanied with changes in direction, twisting, turning, running, or kicking.2,4,7,9,10 Shear forces across the pubis symphysis can lead to separation of the internal oblique and transverse abdominis.5 Athletic pubalgia is a syndrome that encompasses a wide list of injuries involving attachment disruption and instability.4 Most cases include a relationship between the inguinal ring and the anterior lower abdomen wall; the attachment sites of the rectus abdominis and adductors on the pubis11; and an incompetent posterior wall of the inguinal canal12 with no palpable hernia.5 The athletic pubalgia syndrome commonly includes a lower abdominal and groin injury secondary to a rectus abdominis injury associated with adductor pathology.13 The syndrome often results from micro tears to the attachment of the rectus abdominis. These tears alter the force distribution on the femur, leading to dysfunction of the adductors.1 Nine out of 10 patients observed had laxity or tears of the transversalis fascia at its attachment near the internal ring.14 Other structures that can produce groin pain when injured are the adductor longus, iliopsoas, and rectus femoris.4 Meyers et al4 describes grade classifications for the severity of athletic pubalgia: 26 Grade I is defined as single or multiple tears of the rectus abdominis or adductor muscles. l Grade II is defined as a partial avulsion from the pubic symphysis. l Grade III is defined as a complete avulsion with associated micro tears. l FINDINGS Athletic pubalgia is most commonly found in male athletes.7 Almost 2% of female athletes who have been diagnosed with a hernia have been found to have athletic pubalgia.7 Originally, the discrepancy in athletic pubalgia reported in men versus women was based on the few numbers of women participating in high-performance sports.7 With increased research, the number of discrepancies between male and female athletes diagnosed with athletic pubalgia relates to anatomical differences rather than participation.2 Women have a wider pelvis, making it more stable, which results in more efficient distribution of forces to the lower body.4 Strength differences between the genders also contribute to the increased incidence in the male population. Men usually have a stronger muscular base than females, which leads to the muscular imbalances causing athletic pubalgia.10 There is usually chronic, nagging, unilateral, or bilateral groin pain associated with athletic pubalgia6,11; however, it is mostly reported as unilateral.3 The onset of groin pain is intensified with activity but subsides when the athlete is at rest and returns when activity resumes.1,2,6,9,12-15 The pain starts unilaterally and increases with exertional activity. If untreated, symptoms may affect daily living.6,16 Most pain is centered on the pubis symphysis and tubercle where the rectus abdominis attaches. The pain often radiates toward the midline of the body and into the adductors.3-5,7,9,10,12-14,16 Actions that reproduce this dull, chronic pain include resisted hip adduction, hip flexion and internal rotation, and resisted situp.3,6,7,10,12,14 Hip range of motion is also decreased due to painful movements.7 Patients will notice pain when sprinting, cutting, bending, and kicking.6,9,14,16 Patients are often weak on a resisted sit-up and resisted hip adduction. Reduction of hip internal rotation may be a result of increased shear force across the pubic symphysis, and thus cause for suspicion of athletic pubalgia. It is paramount that all other pathologies are excluded after physical examination. Common groin injuries atshc.com Athletic Pubalgia are due to adductor strains and other musculotendinous injuries, resulting in pain without compromised strength or motion. Pain can be found along the upper inner thigh, with tenderness around the origin of adductor muscles, and can be increased with activity and resisted hip adduction and extension,9,17 mimicking the mechanism of injury.10 Physical examination will not find an actual hernia, even though most of these signs and symptoms lead health care professionals to believe that one is present.1,2,5,6,9,16 The Valsalva maneuver, along with muscle testing of the hip adductors, rectus abdominis, rectus femoris, and iliopsoas, will produce some discomfort.9 Clinical findings can include a variety of conclusions, including inflammation of the pubic symphysis causing weakness and instability,11 dilated inguinal ring or conjoined tendon along the inguinal canal,5,9,10 and weakness of the posterior abdominal wall.15,16 The weak posterior abdominal wall often occurs from shear forces along the pubic symphysis, which can separate the transversalis fascia and the internal oblique aponeurosis, resulting in pain.1 Tab l e Sports Rehabilitation Program Lower Abdomen and Core Exercises Posterior pelvic tilt with complete exhalation Posterior pelvic tilt with complete exhalation while bridging Posterior pelvic tilt with complete exhalation with a crunch Front and side planks while maintaining pelvis neutral Proprioception Exercises Balance on unstable surface maintaining pelvic neutral (progressing from double-leg stance to a single-leg stance) Balance on unstable surface while throwing and catching a ball (progressing from double-leg stance to single-leg stance) Balance on unstable surface with BodyBlade (Hymanson Inc, Marina Del Rey, CA) (progressing from double-leg stance to single-leg stance) These pathologies mimic athletic pubalgia because they often have radicular pain in the groin area. Thus, diagnostic imaging is primarily used to rule out the susceptibility of other injuries and not necessarily as a tool to determine athletic pubalgia. DIFFERENTIAL DIAGNOSIS PREVENTION and TREATMENT Proper diagnosis requires a thorough evaluation. It is difficult to diagnose an injury or syndrome with unclear etiology and pathology. A large part of the treatment is to exclude all other injuries and narrow the diagnosis, which relies heavily on diagnostic imaging. Imaging, including magnetic resonance imaging (MRI), rarely indicates positive findings for athletic pubalgia and is mainly used to rule out other pathologies.6,7,9,11,13,16 Hip pathologies, which mimic the symptoms of athletic pubalgia, are lengthy and include: l Articular lesions. l Osteitis pubis. l Stress fracture. l Rectus abdominis tendinopathy. l Adductor pathology. l Hernias. l Sacroiliac joint pathology. l Intrinsic hip pathology.12 l Snapping hip syndrome.9 l Avulsions. l Nerve pain.2 l Bone edema.17 l Lumbar disc referred pain.18 Prevention is paramount in decreasing the number of patients who experience athletic pubalgia. Core and hip stability and flexibility should be emphasized.4 Preparticipation physical examinations should include clinical assessment of core stability and hip flexibility. Identification of weak and overcompensating muscles to treat the imbalance before athletic pubalgia presents itself should also occur.4 Strengthening and developing coordination of the hip adductors, flexors, internal rotators, core stabilizers, gluteals, and spinal musculature is important.10 The Table describes a rehabilitation program that focuses on these muscles. Typical rehabilitation should include isometric holds that target the lumbopelvic hip complex musculature. Difficulty of the rehabilitation exercises can be enhanced by increasing the number of repetitions and the length of holds. The hip adductors, hip flexors, and lumbopelvic stabilizers need to work in sync to functionally control the lumbar spine, pelvis, and femur.1 Any imbalance, strength deficit, or lack of flexibility will affect the forces exerted across the pubic symphysis, femoral acetabular joint, lumbar spine, Athletic Training & Sports Health Care | Vol. 2 No. 1 2010 27 Rabe & Oliver posterior or anterior abdominal wall, and pelvic floor.1 The goal of all prevention programs should be obtaining core control. In addition to making sure there are adequate strength balances, it is also important that a thorough history is obtained of lumbar, abdominal, pelvic, and femoral health. A functional movement screening test should also be included.16 By obtaining a solid history of any predisposing factors, the clinician can develop a rehabilitative program to address the areas of concern and hopefully prevent athletic pubalgia. It is important to note that there are several contributing factors to athletic pubalgia. Athletic pubalgia should be viewed as a multifaceted syndrome of several underlying conditions acting on the kinetic chain, resulting in a progression of events that eventually leads to inability to perform. Nonoperative treatment of athletic pubalgia includes rest, anti-inflammatory medications, strengthening of the core musculature, and regaining postural control.2,7 Along with these treatments, incorporating deep massage of the adductors and using hot and cold therapy has demonstrated success.9 The core stability program corrects the imbalance between the hip and the pelvis.9 At least 6 to 8 weeks of a sports-specific rehabilitation program should be performed before surgery.6,7,9,14,16 The sports-specific rehabilitation program should be as strenuous as possible to allow any imbalance to correct itself. Strengthening and stabilization of the abdominal wall, along with massage and stretching of the adductors, should be performed routinely.6 After a well-prescribed, sports-specific rehabilitation program has failed, surgery is then considered to correct the imbalance or the damage the imbalance has caused. SURGICAL OPTIONS Surgical options should be considered when 6 to 8 weeks of nonsurgical treatment fail and a thorough physical examination has dismissed other potential injuries. Typically, surgical repairs of the hip, groin, and lower abdominal injuries are divided into an open or laparoscopic approach. If the approach taken is an open technique, the surgeon evaluates the insertion of the rectus abdominis, external oblique aponeurosis, and the conjoint tendon for abnormalities. This cannot be performed if the approach were laparoscopic.15 28 A common open technique advocated by Meyers et al17 which involves stabilizing the pelvis by reattachment of the rectus abdominis and its fascia,15 has had a 97% return to previous activity level. An open approach can require 3 months to heal before return to full activity.18 Repair of the external oblique aponeurosis can require 6 weeks to heal along with a modified shouldice repair.18 Gilmore19 has reported that a successful repair requires the open approach. Other open repairs reported by Kumar et al20 indicated that of the 35 patients (34 men, 1 woman) who underwent an open repair of a tear in the external oblique aponeurosis and darn or mesh repair of the posterior inguinal canal, 93% returned to previous activity levels. In the laparoscopic repairs, it is assumed that all pain is caused from an incipient hernia.15 Inserting mesh will reinforce and strengthen the area. With the laparoscopic approach, there is better visualization of the defect, and if the individual has bilateral defects, both can be repaired through one incision.13 However, with laparoscopic repair, other areas of the external oblique aponeurosis, conjoint tendon, or insertion of the rectus cannot be examined. Meyers et al17 reported that laparoscopic repairs cannot address the causative pathology as well as open repairs. Success rates for the conventional or laparoscopic technique have shown results from 89% to 97% return to previous activity.9 It is evident that laparoscopic repair has the fastest return to activity and best success rate (approximately 95%.)15 Ingoldby21 compared open techniques to laparoscopic techniques and found that all patients were able to return to their preinjury activity levels with no severe pain. Return to play for laparoscopic repairs have been reported as early as 4 weeks or less.9 Typically, most patients return to play in 4 to 6 weeks for laparoscopic repairs and within 1 to 6 months for open repairs.9 After surgery, rehabilitation should focus on gradually rebuilding the core musculature. Rehabilitation starts soon after surgery, with gentle walking and light activities of daily living, and then progresses to more strenuous walking and stationary biking with light stretching.7 Strengthening of the core musculature, including lower back and adductors, should be performed, along with stretching and massage.7 The final stages of rehabilitation consist of functional activities (eg, jogging, sprinting, and cutting and pivoting), preceding return to activity.7 atshc.com Athletic Pubalgia CONCLUSION Athletic pubalgia is a complicated and multifactorial syndrome that should be approached with caution and attentiveness. The purpose of this literature review was to distinguish athletic pubalgia from other injuries. Clinicians should recognize this syndrome early to prevent further injury to their athletes. Early recognition through thorough evaluations of the injury, including palpation of the areas of concern and manual muscle testing in attempt to rule out all possible conditions, is paramount to injury diagnosis. Many times, patients will describe chronic lower abdominal, pelvic, and thigh pain that radiates into the groin.3 If a patient does describe these symptoms, clinicians should investigate the possibility of athletic pubalgia. However, one must be cognizant that these findings will not always lead to a diagnosis of athletic pubalgia. Athletic pubalgia may be caused by an acute injury through trunk hyperextension and hyperadduction of the thigh presenting with tenderness over the pubic tubercle and symphysis. More often, a patient will report activity-induced groin pain unresponsive to conservative treatment.15 Typically, the mechanism of injury is not the case. Clinicians must be knowledgeable of the condition and have a high index of suspicion when a patient reports unresolved groin pain. Most imaging studies will present as normal, and the patient will typically not respond to the nonoperative treatment. Surgical options should be explored when there is no response to nonoperative treatment after 6 weeks. Most patients can return to preinjury competition within 2 to 6 weeks after a laparoscopic repair and within 1 to 6 months after an open repair.5,7,8,20-24 Athletic pubalgia, being such a complicated syndrome, warrants further research to truly understand its components and requires a universal understanding by the medical profession to distinguish it from hernias, sports hernias, and other pathologies. REFERENCES Further RESEARCH Continual research, such as injury surveillance studies and reliability and sensibility studies of current evaluation methods dedicated to athletic pubalgia, are necessary for this syndrome to be universally accepted and to distinguish it from other injuries involving the hip and pelvis. Further research should Athletic Training & Sports Health Care | Vol. 2 strive to find a standard definition, a common mechanism of injury, and a universal statement defining athletic pubalgia and its symptoms. In addition, more imaging studies should be performed to improve our understanding of the pathology. Currently, athletic pubalgia’s definition is inconsistent and, therefore, the syndrome is misdiagnosed.4,6,13,15 Further research on appropriate evaluation, diagnosis, and rehabilitation to correctly acknowledge athletic pubalgia is crucial. n No. 1 2010 1. Geisler PR, Kelly E. Groin pains. Training and Conditioning. 2008; 18.07:31-35. 2. Diesen DL, Pappas TN. Sports hernias. Adv Surg. 2007;41:177-187. 3. Unverzagt CA, Schuemann T, Mathisen J. Differential diagnosis of a sports hernia in a high-school athlete. J Orthop Sports Phys Ther. 2008;38:63-70. 4. Meyers WC, Yoo E, Devon ON, et al. Understanding “sports hernia” (athletic pubalgia): The anatomic and pathophysiologic basis for abdominal and groin pain in athletes. Operative Techniques in Sports Medicine. 2007;15:165-177. 5. Schuricht A, Haut E, Wetzler M. Surgical options in the treatment of sports hernia. Operative Techniques in Sports Medicine. 2002;10: 224-227. 6. Ahumada LA, Ashruf A, Espinosa-de-los-Monteros A, et al. Athletic pubalgia definition and surgical treatment. Ann Plast Surg. 2005;55:393-396. 7. Larson CM, Lohnes JH. Surgical management of athletic pubalgia. Operative Techniques in Sports Medicine. 2002;10:228-232. 8. Srinivasan A, Schuricht A. Long-term follow-up of laparoscopic preperitoneal hernia repair in professional athletes. J Laparoendosc Adv Surg Tech A. 2002;12:101-106. 9. Farber AJ, Wilckens JH. Sports hernia: Diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15:507-514. 10. Scifers JR. A perplexing problem: Athletic pubalgia is poorly understood and misdiagnosed. Adv Dir in Rehab. 2003;12:53-55. 11. Shortt CP, Zoga AC, Kavanagh EC, Meyers WC. Anatomy, pathology, and MRI findings in the sports hernia. Semin Musculoskelet Radiol. 2008;12:54-61. 12. Swan KG, Wolcott M. The athletic hernia: A systematic review. Clin Orthop. 2007;455:78-87. 13. Diaco JF, Diaco DS, Lockhart L. Sports hernia. Operative Techniques in Sports Medicine. 2005;13:68-70. 14. Edelman DS, Selesnick H. “Sports” hernia: Treatment with biologic mesh (surgisis). Surg Endosc. 2006;20:971-973. 15. Harmon, KG. Evaluation of groin pain in athletes. Curr Sports Med Rep. 2007;6:354-361. 16. Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35:991-1014. 17. Meyers WC, Lanfranco A, Castellanos A. Surgical management of chronic lower abdominal and groin pain in high-performance athletes. Curr Sports Med Rep. 2002,1:301-305. 18. Nam A, Brody F. Management and therapy for sports hernia. J Am Coll Surg. 2008;206:154-164. 29 Rabe & Oliver 19. Gilmore J. Groin pain in the soccer athlete: Fact, fiction, and treatment. Clin Sports Med. 1998;17: 787-93. 20. Kumar A, Doran J, Batt ME, Nguyen-Van-Tam JS, Beckingham IJ. Results of inguinal canal repair in athletes with sports hernia. J R Coll Surg Edinb.2002;47:561-565. 21. Ingoldby CJH: Laparoscopic and conventional repair of groin disruption in sportsmen. Br J Surg. 1997;84:213-215. 22. Susmallian S, Ezri T, Elis M, Warters R, Charuzi I, Muggia-Sullam M. Laparoscopic repair of “sportsman’s hernia” in soccer players as 30 treatment of chronic inguinal pain. Med Sci Monit. 2004;10:CR52CR54. 23. Van Der Donckt K, Steenbrugge F, Van Den Abbeele K, Verdonk R, Verhelst M. Bassini’s hernial repair and adductor longus tenotomy in the treatment of chronic groin pain in athletes. Acta Orthop Belg. 2003;69:35-41. 24. Azurin DJ, Go LS, Schuricht A. McShane J, Bartolozzi A. Endoscopic and conventional repair of groin disruption in sportsmen. Br J Surg. 1997;7:7-12. atshc.com
© Copyright 2025