continuing education for pharmacists Common Cold, Sinusitis, Influenza: The Diseases, Prevention, Treatment
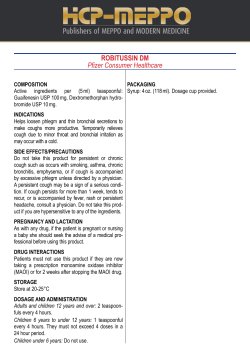
continuing education for pharmacists Volume XXX, No. 11 Common Cold, Sinusitis, Influenza: The Diseases, Prevention, Treatment Mona T. Thompson, R.Ph., PharmD Dr. Mona T. Thompson has no relevant financial relationships to disclose. Goal. The goal of this lesson is to provide disease state reviews of the common cold, sinusitis, and influenza. This lesson will also highlight key differences between each disease state, and review current treatment recommendations and prevention when applicable. Objectives. At the completion of this activity, the participant will be able to: 1. demonstrate an understanding of the basic pathophysiology of the common cold, sinusitis, and influenza; 2. compare the symptoms of these three disease states; 3. list the antibiotics used in the treatment of sinusitis; 4. recognize the appropriate use of antiviral agents in the prevention and/or treatment of influenza; and 5. list the recommendations for the appropriate use of the influenza vaccine. The Common Cold The term common cold refers to a collection of upper respiratory symptoms that are caused by an array of viral pathogens. Symptoms include nasal congestion, rhinorrhea, sneezing, sore throat, cough, low-grade fever, headache, and malaise. The average incidence of the common cold is six to eight episodes per year in preschool children, and two or three per year in adults. Adults who live with young children experience more colds than those who don’t. In infants and young children, symptoms usually peak on day two or day three of the illness and persist for 10 to 14 days. In some children, the cough may last up to three or four weeks. The duration of illness for adolescents and adults is usually seven to 10 days. While generally considered mild and self-limiting, the common cold is associated with a tremendous economic burden due to lost productivity and the cost of treatment. It is estimated that viral respiratory tract infections account for 21 million days of school absence and 20 million days of work absence per year in the U.S. alone. Annually, approximately three billion dollars are spent on over-thecounter cough and cold medications for symptomatic treatment. The pathogens most commonly associated with common cold symptoms are the rhinoviruses. There are over 100 different types that account for 40 to 50 percent of the cases. Other responsible pathogens include coronaviruses and respiratory syncytial virus (RSV). While influenza, parainfluenza, and adenoviruses may be associated with cold symptoms, they often cause lower respiratory and systemic symptoms, in addition to the upper respiratory symptoms characteristic of the common cold. These infections also present differently in younger children, versus older children and adults. For instance, RSV in older chidren and adults often presents the same as other colds, but in infants and toddlers, it can result in bronchiolitis and involve the lower respiratory tract. Similarly, parainfluenza may present as croup in younger children and as a typical cold in an older child. The cold season begins in late August/September and remains constant until the spring due to the number of viruses. Rhinovirus begins to increase in the early fall. Alternatively, parainfluenza peaks in the late fall and late spring, while RSV and influenza viruses are highest between December and April. Common cold symptoms are associated with each of these outbreaks. An effective vaccine for the common cold is unlikely for two reasons. First, some of these viruses do not cause lasting immunity such as RSV, parainfluenza viruses, and coronavirus which can result in recurrent infections. Second, even though other viruses do produce lasting immunity, there are so many serotypes that a vaccine would not produce a real impact on reducing the frequency of common cold infections. Transmission and Prevention. Colds may be spread through three mechanisms: (1) small-particle aerosols produced from coughing and inhaled by another person; (2) large particle droplets produced from saliva that is expelled during a sneeze and lands on the conjunctivae or nasal mucosa of another person; or (3) self-inoculation from touching one’s own nasal mucosa after touching a person or object contaminated with a cold virus. Hence, poor hygiene and curiosity may be factors that lead to children’s increased susceptibility to colds. Hand-washing removes the cold virus from the hands. Virucidal tissues have been shown to reduce secondary transmission. However, alcohol-based hand sanitizers have not been shown to reduce secondary transmission of colds, most likely because rhinovirus is not affected by these products. Treatment. While treatment options differ in adults and children, symptomatic and supportive treatment remains the mainstay for the common cold. The following treatment options do not reduce disease duration. Antibiotics are not indicated unless symptoms strongly suggest a secondary bacterial infection. Antiviral therapy is not available for viruses that cause the common cold. Treatment in Adults. Ipratropium bromide (Atrovent® Nasal Spray), an anticholinergic medication which is administered intranasally, may be helpful in improving symptoms of rhinorrhea and sneezing. Via application to the nasal mucosa, it inhibits mucous gland secretions. However, it does not improve nasal congestion. It is usually dosed as two sprays in each nostril, three to four times a day. Adverse effects include nosebleeds, nasal dryness, and dry mouth. First-generation antihistamines such as diphenhydramine may improve rhinorrhea and sneezing, but their use is limited due to bothersome side effects including sedation and drying of the eyes, nose, and mouth. A systematic review of available data concluded that first-generation antihistamines had a small clinical benefit for relief of rhinorrhea and sneezing, but that this was out- weighed by the frequency of side effects. Non-sedating antihistamines, such as loratadine and cetirizine, were not effective. Therefore, antihistamines have minimal benefit in treating the common cold. Cough associated with the common cold is often due to post-nasal drip or nasal obstruction. The American College of Chest Physicians guidelines do not recommend cough suppressants or antitussives, such as codeine or dextromethorphan, for relief of cough associated with upper respiratory infections. Several clinical trials, however, have concluded that dextromethorphan is superior to placebo for cough suppression. Trials examining patients with acute cough due to the common cold found no consistent benefit when codeine was compared with placebo, even though it may be helpful for chronic cough. Topical and oral adrenergic agents such as phenylephrine and pseudoephedrine may temporarily alleviate nasal congestion. Phenylephrine is less effective than pseudoephedrine for treating rhinitis symptoms, yet it is a common ingredient in many OTC cold preparations. Since pseudoephedrine is currently being used in the illegal manufacturing of methamphetamine, FDA has limited purchases and the availability to behind-the-counter in pharmacies. Topical decongestants should not be used for longer than two to three days, as they can result in rebound rhinitis. Adverse effects associated with these agents include increased blood pressure in those with preexisting hypertension, nosebleeds (topical), agitation, and insomnia. Expectorants are intended to increase mucous production. The most common commercial agent is guaifenesin. Studies show it may have a marginal effect in improving the thickness and quantity of sputum in adults. Sore throat may be treated with aspirin or acetaminophen, while non-steroidal anti-inflammatories (NSAIDs) may be used for headache, ear pain, muscle and joint pains, malaise, and sneezing associated with the common cold. While their effectiveness is questioned, saline nasal sprays or irrigations and inhaling warm vaporized air may ease some of these symptoms. Treatment in Children. Over the past few years, the use of OTC cough and cold medications for children and infants has been under investigation. Over the past 20 years, 123 deaths involving children younger than six years of age have resulted from the use of OTC cough and cold medications. The adverse events associated with their use, as well as accidental ingestion, are a common cause for emergency department visits. Poor labeling, use of multi-ingredient products, and multiple caregivers administering medications are factors that lead to inadvertent overdosing. In October 2007, the U.S. Food and Drug Administration (FDA) Advisory Committee voted to recommend against the use of OTC cough and cold medications in children younger than two years. Drug manufacturers voluntarily discontinued the marketing of these agents for children less than two years of age. Subsequently, the number of emergency department visits for adverse events involving these medications was cut in half for children in this age group. In 2011, the FDA advisory group voted again to further ban the use of these agents in children less than six years of age. The American Academy of Pediatrics (AAP) recommends against the use of OTC cough and cold medications in children younger than six years, due to safety concerns and the lack of efficacy data surrounding their use. Supportive therapy for children, as well as adults, includes increasing fluid intake to thin secretions; ingesting warm fluids such as tea which may soothe the respiratory mucosa, increase the flow of nasal mucus, and loosen mucus; the use of topical saline and nasal suction to remove nasal secretions; and the use of a humidi- Table 1 Comparison of the common cold and flu Symptoms Cold Flu Fever Rare Characteristic, high, lasting 3-4 days Headache Rare Prominent General Aches, Pains Rare Prominent Fatigue, Weakness Mild May last 2-3 weeks Extreme Exhaustion Never Early and prominent Stuffy Nose Common Sometimes Sneezing Usual Sometimes Sore Throat Usual Sometimes Chest Discomfort, Cough Mild to Common; can become severe moderate hacking cough Prevention Good hygiene Influenza vaccine Treatment Temporary symptom relief fier which helps loosen nasal secretions. While these interventions are not proven to be effective, they are safe and inexpensive. Symptomatic treatment is suggested only when symptoms are interfering with sleep or causing discomfort. Single ingredient products are recommended to avoid overdosing from multiple medications that contain the same ingredient. Fever and general discomfort from the common cold may be treated with acetaminophen for children older than three months or ibuprofen for children older than six months. The use of aspirin is not recommended in children due to the association with Reye’s Syndrome. Regarding the treatment of nasal congestion and rhinorrhea, ipratropium 0.06 percent nasal spray (Atrovent® Nasal Spray) is indicated for the relief of rhinorrhea due to the common cold for ages five to 11 years. There is no evidence supporting the effectiveness of either oral or topical decongestants in children. Antihistamines or combination antihistamine/decongestants are also not recommended for nasal symptoms. Antitussives are not recommended in children for several reasons. Coughing is a protective action that clears the airway; suppressing it may be harmful to chil- Antiviral drugs (Relenza® or Tamiflu®) within 24-48 hours dren, especially those with asthma. In addition, studies have failed to indicate improvement when dextromethorphan was used. Lastly, accidental overdose of antitussives can cause respiratory depression. One recent study suggested that the bedtime application of vapor rub containing menthol, camphor, and eucalyptus oils to the chest and neck of children aged two to 11 years resulted in relief of night-time cough, congestion, and difficulty in sleep compared to petrolatum or no treatment. It should not be applied to the nasal passages, as it may cause chemical irritation there. Gastrointestinal and central nervous system effects may result from accidental ingestion. Complications of the Common Cold. Wheezing or secondary bacterial infections such as otitis media, sinusitis, or pneumonia may complicate the common cold. Approximately 30 percent of colds in preschool-aged children may be complicated by otitis media, with the risk being highest in children six to 11 months of age. Sinusitis may occur in 5 to 10 percent of children with colds, and is considered when symptoms do not improve after 10 days. Infants and children with reactive airway disease or asthma are at a higher risk for complications, and may have increased severity and duration of respiratory symptoms. Fifty percent of asthma exacerbations are associated with viral infections, particularly rhinovirus. RSV is also associated with wheezing exacerbations. Table 1 includes comparison of symptoms, prevention and treatment for the common cold and influenza. Sinusitis Acute rhinosinusitis (ARS) is defined as symptomatic inflammation of the nasal cavity and paranasal sinuses lasting fewer than four weeks. The term rhinosinusitis is used since inflammation of the sinuses is almost always accompanied by inflammation of the nasal cavity, and is more commonly referred to as sinusitis. Viral etiology associated with an upper respiratory infection (URI) or the common cold is the most frequent cause of sinusitis. However, sinusitis can also be caused by allergens, environmental irritants, and bacterial or fungal infections. Acute viral rhinosinusitis (AVRS) is extremely common, while secondary bacterial infections of the paranasal sinuses following a viral URI are estimated to occur in 0.5 to 2 percent of adults and 5 percent of children. Even though viral infections account for 92 to 98 percent of the cases, acute rhinosinusitis is the fifth leading indication for antibiotic prescribing by healthcare professionals. Contrary to common belief, the presence of colored or green nasal discharge alone does not indicate that the infection has been complicated by bacteria. In an uncomplicated case of viral URI, the nasal discharge begins as clear and watery, and becomes thicker and more mucoid throughout the course of the disease. It may become thick, colored, and opaque for several days before reversing to mucoid and clear again or drying. Because differentiating between AVRS and bacterial infection is difficult, it is challenging to determine when antibiotics are indicated. Table 2 Outpatient antimicrobial regimens for acute bacterial rhinosinusitis in adults* Indication First-line Second-line Initial empiric therapy Amoxicillin-clavulanate Amoxicillin-clavulanate (500mg/125mg PO tid (2000mg/125mg PO bid) or 875mg/125mg PO bid) Doxycycline (100mg PO bid or 200mg qd) Beta-lactam allergy Doxycycline (100mg PO bid or 200mg qd) Levofloxacin (500mg PO qd) Moxifloxacin (400mg PO qd) Risk for antibiotic resistance or failed initial therapy Amoxicillin-clavulanate (2000mg/125mg PO bid) Levofloxacin (500mg PO qd) Moxifloxacin (400mg PO qd) *Adapted from IDSA Guidelines for ABRS 2012 Studies indicate that some patients with acute bacterial rhinosinusitis (ABRS) may clear the infection spontaneously without antibiotic treatment. Sinusitis rarely leads to severe complications. Several practice guidelines have been published by various professional organizations to aid practitioners in appropriate antimicrobial prescribing. The treatment recommendations discussed in this lesson are based on the Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults published by the Infectious Disease Society of America (IDSA) in 2012. Since sinus aspirate cultures are not readily available, it is not possible to distinguish between AVRS and ABRS in the first 10 days of illness based on history and examination. Therefore, ABRS should be considered when any of the following are present: (1) persistent signs and symptoms of ARS lasting 10 or more days with no clinical improvement; (2) severe symptoms or signs of high fever (>102°F) and purulent nasal discharge, or facial pain lasting for at least three to four consecutive days at the beginning of the illness; or (3) worsening signs or symptoms characterized by the new onset of fever, headache, or increase in nasal discharge, following a typical upper respiratory infection that lasted five to six days and were initially improving. The last symptoms are referred to as double-sickening. Treatment of Sinusitis. The following treatment recommendations are for patients with suspected ABRS. For the relief of pain associated with ARS, analgesics such as NSAIDs and acetaminophen may be used. Intranasal saline irrigation, with either normal saline or hypertonic saline, may be used in adults and children to relieve nasal symptoms. Although saline irrigation is safe and may make the patient more comfortable, it is associated with nasal burning, irritation, and nausea. Saline irrigation is less well tolerated in babies and young children. Intranasal corticosteroids may be used as an adjunct to antibiotics in patients with a history of allergic rhinitis. Neither decongestants (topical or oral) nor antihistamines is recommended for adjunct treatment in patients with ABRS. Empiric antimicrobial therapy should be initiated in patients with signs and symptoms suggestive of ABRS as soon as the clinical diagnosis is made. Based on IDSA’s clinical criteria previously outlined, patients with bacterial infection are more likely to be appropriately identified. The recommendation for “watchful waiting” is gener- ally no longer necessary. However, “watchful waiting” with follow-up still may be employed in patients where the diagnosis of a bacterial infection is uncertain and milder symptoms are present. Treatment in Adults. Amoxicillin was formerly recommended as a first-line agent due to its narrow spectrum of coverage and low cost. However, the pathogens for ABRS have changed since the introduction of routine conjugated pneumococcal vaccination in children. For both adults and children, the percentage of ABRS due to S. pneumoniae has decreased while the percentage due to H. influenzae has increased. Antimicrobial resistance to both respiratory pathogens continues to rise. Therefore, the IDSA guidelines now recommend amoxicillin-clavulanate (Augmentin®) over amoxicillin as a first-line agent for non-penicillin allergic adults. The dose for most adults is 500mg/125mg orally three times a day, or 875mg/125mg orally twice daily. High dose amoxillin-clavulanate of 2 grams orally twice daily is recommended for geographic regions with high endemic rates (>10 percent) of penicillin-nonsusceptible (PNS) S. pneumoniae, and for patients who are 65 years and older, recently hospitalized, treated with an antibiotic in the previous month, or immunocompromised. For patients who are allergic to penicillin, doxycycline may be used first line, or a respiratory fluoroquinolone such as levofloxacin or moxifloxacin. According to the IDSA, the duration of treatment in adults should be five to seven days. Second-line treatment options include amoxicillin-clavulanate 2000mg/125mg orally twice daily; levofloxacin 500mg orally once daily; or moxifloxacin 400mg orally once daily. (Table 2) Treatment in Children. Again, amoxicillin-clavulanate, rather than amoxicillin alone, is recommended as empiric firstline therapy in children. The addition of clavulanate improves Table 3 Outpatient antimicrobial regimens for acute bacterial rhinosinusitis in children* Indication First-line Second-line Initial empiric therapy Amoxicillin-clavulanate Amoxicillin-clavulanate (90mg/ (45mg/kg/day PO bid) kg/day PO bid) Beta-lactam allergy Type I hypersensitivity Non-type I hypersensitivity •Levofloxacin (10-20mg/kg/day PO every 12-24 hours) •Clindamycin (30-40mg/kg/day PO tid) plus cefixime (8mg/kg/ day PO bid) or cefpodoxime (10mg/kg/day PO bid) Risk for antibiotic resistance or failed initial therapy •Amoxicillin-clavulanate (90mg/ kg/day PO bid) •Clindamycin (30-40mg/kg/day PO tid) plus cefixime (8mg/kg/ day PO bid) or cefpodoxime (10mg/kg/day PO bid) •Levofloxacin (10-20mg/kg/day PO every 12-24 hours) coverage for ampicillin-resistant H.influenzae and M. catarrhalis in ABRS. However, it also increases the likelihood of diarrhea. If oral antibiotics cannot be given initially due to vomiting, a single dose of ceftriaxone, dosed at 50mg/kg/day, may be administered intramuscularly or intravenously, followed by oral antibiotics 24 hours later (once vomiting has been resolved). High dose amoxicillin-clavulanate, 90mg/kg/day orally twice daily, is recommended for children in geographic areas with PNS S. pneumoniae, as well as those with severe infection, attending daycare, less than 2 years of age, recently hospitalized, having used antibiotics within the past month, or those who are immunocompromised. Combination therapy with a third-generation oral cephalosporin (i.e., cefixime or cefpodoxime) plus clindamycin may be used as second-line therapy for children with non-type I penicillin allergy in regions with high rates of PNS S. pneumoniae. Children with a type I penicillin allergy may be treated with levofloxacin. (Table 3) In children, the recommended duration of antimicrobial therapy for ABRS is 10 to 14 days. This longer duration, in comparison to adults, is indicated based on the lack of randomized studies in children concluding efficacy in the shorter duration. Macrolides, such as clarithromycin and azithromycin, trimethoprim-sulfamethoxazole (TMP-SMX), and second- or thirdgeneration cephalosporins, are not recommended for empiric therapy due to high rates of resistance with S. pneumoniae. TMP-SMX also has high rates of resistance with H. influenzae. Response to empiric therapy should be seen after three to five days. Altering therapy is suggested for patients who do not show an improvement in that time frame, or when symptoms worsen after two to three days of therapy. *Adapted from IDSA Guidelines for ABRS 2012 Influenza Influenza virus infection is another common viral disease that is highly contagious among children and adults. The annual influenza cycle or season begins as early as October, with a peak in January or February, and ends as late as May. It causes an acute febrile illness and varying other systemic and upper respiratory symptoms which result in loss of workdays, school absences, as well as morbidity and mortality. Over the past three decades, the estimated annual influenza-related deaths have ranged from 3,000 to 49,000, with approximately 226,000 annual hospitalizations in the U.S. alone. Pediatric mortality from influenza is typically highest in the first year of life. The signs and symptoms of influenza overlap with other viral URIs and include: fever, myalgia, headache, malaise, non-productive cough, sore throat, and rhinitis. Additionally, otitis media, nausea, and vomiting are common in children. A typical uncomplicated course of illness begins after an incubation period of one to two days (up to four), and resolves in three to seven days for most persons, although cough and malaise can persist for greater than two weeks. Fever is the most important clinical finding. It rises rapidly to a peak of 100°F to 104°F (occasionally 106°F), and subsides after three days along with other systemic symptoms. However, the fever may last four to eight days. Complications can occur and lead to primary influenza viral pneumonia; exacerbate underlying medical conditions (i.e,. pulmonary or cardiac disease); lead to secondary bacterial pneumonia, otitis media, or sinusitis; and contribute to co-infections with other viral or bacterial pathogens. Adults shed the virus from the day before symptoms occur, through five to 10 days after illness onset, while the infectivity decreases rapidly by three to five days. Young children may shed the virus several days before illness onset, and can be infectious for 10 or more days after. While limited antivirals are available to treat influenza, vaccine prevention is the most effective strategy. Influenza viruses are encapsulated, single-stranded RNA viruses of the family Orthomyxoviridae. The core nucleotides are used to distinguish between types A, B, and C. In humans, influenza A is generally more pathogenic than influenza B. These viruses infect humans and a variety of animals; some of these strains may spread from animal species to humans as well. The influenza viruses are ever changing via antigenic drift and shift. Antigenic drift is a process by which the virus produces ongoing gene mutations resulting in new subtypes and altered virulence. Antigenic shift is less common, but creates virulent strains that are transmissible to a greater population of susceptible individuals which can cause a pandemic. The gene segments between two strains are re-assorted, presumably during a co-infection in a single host. The “Spanish flu” of 1918 was a result of an antigenic shift. This pandemic alone affected 20 to 50 million people globally and was responsible for 549,000 deaths in the U.S. The 2009 H1N1 influenza (also referred to as Swine Flu) pandemic was a recombinant influenza consisting of a mix of swine (pig), avian (bird), and human gene segments. Influenza Diagnosis. Respiratory illnesses caused by influenza virus infection are difficult to differentiate from other illnesses caused by respiratory pathogens based on signs and symptoms alone. Once the presence of influenza virus is confirmed in a region or community, healthy adults with acute influenza-like symptoms most likely have the infection. The accuracy of diagnosis in an influenza outbreak can be as high as 80 to 90 percent. Rapid diagnosis can also be made by testing respiratory secretions from nasopharyngeal samples and/or throat swabs. There are a variety of rapid tests with results available as quickly as 30 minutes. While some are useful in differentiating influenza A and influenza B, none of the current tests can distinguish between influenza A (H1N1) and influenza A (H3N2). The optimal use of rapid diagnostic tests in patient management is not yet defined. Transmission. Influenza viruses are spread primarily through large-particle respiratory droplet transmission via coughing or sneezing. Transmission requires close contact with a susceptible individual, since the large droplets do not remain suspended in the air and only travel a short distance. Transmission may also occur via contact with surfaces contaminated with respiratory droplets or through small particles suspended in the air. Influenza Vaccine. Each year in the U.S., a vaccine containing the antigens from the strains most likely to cause infection during the season is produced. At the time of writing this lesson, the vaccine contains three strains, two influenza A strains and one influenza B. The 20122013 vaccine contains the following: A/California/7/2009(H1N1) pdm09-like virus, A/Victoria/361/ 2011(H3N2)-like virus, and B/ Wisconsin/1/2010-like virus. The Centers for Disease Control and Prevention (CDC) recommends that everyone six months of age and older get a flu vaccine each year as soon as it is available. It is especially important for people who are at high risk of developing serious complications such as pneumonia. This includes individuals who have asthma, diabetes, chronic lung disease, are pregnant, or are 65 years of age and older. The vaccine is also important for those who live with, or care for, persons at high risk for developing serious complications. It takes about two weeks for antibodies to develop and provide protection against influenza. Despite the fact that immunity declines over time, most healthy adults and older children will remain protected throughout the season. There are two types of influenza vaccine: inactivated vaccine given by injection and live, attenuated influenza vaccine (LAIV) sprayed into the nostrils. The inactivated vaccine, referred to as the “flu shot,” may or may not contain thimerosal. The flu shot can be given to all persons aged six months and older. A high-dose inactivated vaccine is also available for persons 65 years of age and older. This product has four times the amount of antigen in the standard formulation, and has been shown to provide higher antibody responses in older adults when compared to the standard dose. Side effects are minor and include soreness, redness, or swelling at the injection site; hoarseness; sore, red, or itchy eyes; cough; fever, aches, headache, itching, and fatigue. Life threatening severe reactions to either vaccine formulation are very rare. LAIV is recommended for healthy persons two through 49 years of age who are not pregnant and do not have chronic health conditions (heart disease, lung disease, asthma, kidney or liver disease, diabetes, anemia, or other blood disorders). The vaccine should not be given if a severe allergy to a component of the vaccine exists or if the patient has an allergy to eggs. It does not contain thimerosal or other preservatives. LAIV is made from a weakened virus and does not cause influenza, but may cause mild symptoms such as runny nose, cough, congestion, fever, headache, muscle aches, cough, chills, tiredness/weakness, sore throat, wheezing, abdominal pain, vomiting, or diarrhea. Specific product labeling and CDC vaccine information statements (http://www.cdc.gov/vaccines/pubs/vis/) should be referred to for complete prescribing instructions and recommendations. Antiviral Treatment/Prophylaxis. Influenza antiviral treatment can shorten the duration of fever, lessen symptoms, reduce the risk of complications from influenza, and shorten hospitalization stays. It is recommended to begin antiviral treatment as soon as possible ― ideally within 48 hours of illness onset, for any patient (1) with confirmed or suspected influenza who is hospitalized; (2) who has severe, complicated, or progressive illness; or (3) at higher risk of complications. Treatment should not be withheld pending laboratory confirmation of influenza. Antiviral treatment can also be considered in previously healthy outpatients without risk of complications on the basis of clinical judgment, again, if it is begun within 48 hours. Antiviral medications for chemoprophylaxis should not be used indiscriminately as widespread use may lead to resistance. However, they are recommended to control outbreaks among high risk persons in institutional settings. In order to be effective as chemoprophylaxis, the medication must be taken each day for the duration of potential exposure to a person with influenza, and continued for seven days after the last known exposure. For persons taking antiviral medications following immunization, the duration of therapy is until immunity after vaccination develops (generally two weeks, but may be longer in children). It is generally not recommended if more than 48 hours have elapsed since the last exposure to an infectious person. While four antiviral drugs are currently available for the prevention and treatment of influenza, only two of them, oseltamivir (Tamiflu®) and zanamivir (Relenza®), which are neuraminidase inhibitors, are clinically useful against influenza A and B. Amantadine and rimantadine are part of a class of medications called adamantanes which were initially effective against influenza A. However, the current strains of influenza are resistant to both adamantane agents. Resistance to the neuraminidase inhibitors is currently low. Oseltamivir is approved for chemoprophylaxis and treatment in children greater than one year of age and in adults. Pediatric dosing is weight-based until the child reaches 40kg or 12 years of age. Then the child may be administered the adult dose of 75mg orally twice daily for treatment, or 75mg orally once daily for chemoprophylaxis. Oseltamivir is available as 30mg, 45mg, and 75mg capsules and 6mg/mL powder for suspen- sion. Directions for emergency compounding using the capsules to make a suspension can be found on the manufacturer’s website at: http://www.tamiflu.com/hcp/ resources/hcp_resources_pharmacists.jsp. Zanamivir is approved for chemoprophylaxis in children greater than five years of age, and for treatment in children greater than seven years as well as adults. The dose for both populations is 10mg (two inhalations) twice daily for treatment or 10mg (two inhalations) once daily for chemoprophylaxis. Zanamivir is available as a 5mg powder dose for oral inhalation using the Diskhaler® inhalation device. The recommended duration of therapy for treatment is five days, but can be extended for those who remain severely ill. The recommended duration is seven days for chemoprophylaxis following exposure. However, CDC recommends a minimum duration of two weeks when outbreaks occur in long term facilities and hospitals. Practitioners should consult the Advisory Committee on Immunization Practices’ (ACIP) recommendations for the appropriate use of antivirals for influenza treatment and prophylaxis at: http:// www.cdc.gov/mmwr/pdf/rr/rr6001. pdf. The author, the Ohio Pharmacists Foundation and the Ohio Pharmacists Association disclaim any liability to you or your patients resulting from reliance solely upon the information contained herein. Bibliography for additional reading and inquiry is available upon request. This lesson is a knowledge-based CE activity and is targeted to pharmacists in all practice settings. Program 0129-0000-12-011-H01-P Release date: 11-15-12 Expiration date: 11-15-15 CE Hours: 1.5 (0.15 CEU) The Ohio Pharmacists Foundation Inc. is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. continuing education quiz Please print. Program 0129-0000-12-011-H01-P 0.15 CEU Name________________________________________________ Address_____________________________________________ Common Cold, Sinusitis, Influenza: The Diseases, Prevention, Treatment City, State, Zip______________________________________ Email_______________________________________________ 1. The pathogens most commonly associated with symptoms of the common cold are: a. adenoviruses. c. respiratory syncytial virus. b. coronaviruses. d. rhinoviruses. 2. Alcohol-based hand sanitizers have been shown to reduce secondary transmission of colds. a. True b. False 3. The mainstay treatment for the common cold is: a. symptomatic. c. antibacterial agents. b. antiviral agents. d. vaccine prevention. 4. Which of the following common cold treatments in adults should not be used longer than two to three days because they can result in rebound rhinitis? a. First-generation antihistamines b. Non-sedating antihistamines c. Topical decongestants d. Cough suppressants 5. The American Academy of Pediatrics recommends against the use of OTC cough and cold agents in children: a. <6 years. b. <12 years. 6. The most frequent cause of sinusitis is: a. allergens. c. environmental irritants. b. bacterial infection. d. viral URI. 7. The presence of colored or green nasal discharge alone can indicate an acute bacterial rhinosinusitis infection. a. True b. False Completely fill in the lettered box corresponding to your answer. 1. 2. 3. 4. 5. [a] [a] [a] [a] [a] [b] [b] [b] [b] [b] [c] [d] 6. [a] 7. [a] [c] [d] 8. [a] [c] [d] 9. [a] 10. [a] [b] [b] [b] [b] [b] [c] [c] [c] [c] [d] [d] [d] [d] 11. [a] 12. [a] 13. [a] 14. [a] 15. [a] [b] [b] [b] [b] [b] [c] [d] [c] [d] [c] [d] [c] [d] I am enclosing $5 for this month’s quiz made payable to: Ohio Pharmacists Association. 1. Rate this lesson: (Excellent) 5 4 3 2 1 (Poor) 2. Did it meet each of its objectives? yes no If no, list any unmet_______________________________ 3. Was the content balanced and without commercial bias? yes no 4. Did the program meet your educational/practice needs? yes no 5. How long did it take you to read this lesson and complete the quiz? ________________ 6. Comments/future topics welcome. NABP e-Profile ID*__________________________________ *Obtain NABP e-Profile number at www.MyCPEmonitor.net. Birthdate____________ (MMDD) Return quiz and payment (check or money order) to Correspondence Course, OPA, 2674 Federated Blvd, Columbus, OH 43235-4990 8. Saline irrigation is less well tolerated in: a. adults. c. babies. b. teenagers. d. elderly. 9. In treating non-penicillin allergic adults with sinusitis, IDSA guidelines recommend the following as a first-line agent. a. Levofloxacin c. Doxycycline b. Amoxicillin d. Amoxicillin-clavulanate 10. In children, the recommended duration of antimicrobial therapy for ABRS is: a. 3 days. c. 10 to 14 days. b. 5 to 7 days. d. 21 days. 11. The most important clinical finding in diagnosing influenza is: a. fatigue. c. headache. b. cough. d. fever. 12. Antigenic drift creates virulent strains that are transmissable to a greater population. a. True b. False 13. CDC recommends flu vaccine administration to all the following persons EXCEPT: a. asthmatics. b. pregnant women. c. children three months of age and older. d. caregivers of persons at high risk. 14. Within what period of time of illness onset should antiviral treatment be started for influenza? a. 24 hours c. Three days b. 48 hours d.One week 15. Which two antiviral drugs are clinically useful against influenza A and B? a. Oseltamivir and zanamivir b. Oseltamivir and amantadine c. Amantadine and rimantidine d. Amantadine and zanamivir To receive CE credit, your quiz must be received no later than November 15, 2015. A passing grade of 80% must be attained. All quizzes received after July 1, 2012 will be uploaded to the CPE Monitor and a statement of credit will not be mailed. Send inquiries to opa@ohiopharmacists.org. november 2012
© Copyright 2025