Imiquimod 5% cream for the treatment of actinic
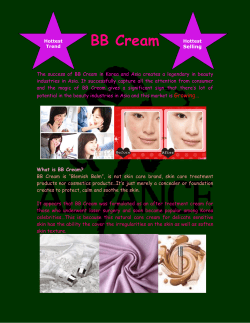
Imiquimod 5% cream for the treatment of actinic keratosis: Results from two phase III, randomized, double-blind, parallel group, vehicle-controlled trials Mark Lebwohl, MD,a Scott Dinehart, MD,b,c David Whiting, MD,d Peter K. Lee, MD, PhD,e Naji Tawfik, MD, PhD,f,g Joseph Jorizzo, MD,h James H. Lee, MD, PhD,i and Terry L. Fox, MSi New York, New York; Little Rock, Arkansas; Dallas, Texas; Minneapolis and St Paul, Minnesota; Indianapolis and Evansville, Indiana; and Winston-Salem, North Carolina Background: The immune system plays a critical role in the development and pathogenesis of actinic keratosis (AK). Imiquimod has been shown to stimulate the cutaneous immune response and be effective for the treatment of nonmelanoma skin cancers. Objective: Two phase III, randomized, double-blind, vehicle-controlled studies evaluated the efficacy of imiquimod 5% cream compared with vehicle in the treatment of AK lesions on the face and balding scalp. Methods: A total of 436 participants at 24 centers in the United States and Canada were randomized to either imiquimod 5% or vehicle cream. Study cream was applied one time per day, 2 days per week for 16 weeks. Clearance of AK lesions was clinically assessed at an 8-week posttreatment visit. Results: The complete clearance rate was 45.1% for the imiquimod group and 3.2% for the vehicle group. The difference in complete clearance rates (imiquimod minus vehicle) was 41.9% with a 95% confidence interval of 34.9% to 49%. The partial (ⱖ75%) clearance rate was 59.1% for the imiquimod group and 11.8% for the vehicle group. The difference in partial clearance rates (imiquimod minus vehicle) was 47.3% with a 95% confidence interval of 39.5% to 55.1%. The median percent reduction in AK lesions was 83.3% for the imiquimod group and 0% for the vehicle group. Local skin reactions were common. Severe erythema was reported by 17.7% of participants who received imiquimod and 2.3% of participants who received vehicle. Overall, imiquimod was very well tolerated. Conclusion: Imiquimod 5% cream used 2 times per week for 16 weeks is an effective and well-tolerated treatment for AK. (J Am Acad Dermatol 2004;50:714-21.) From the Department of Dermatology, Mount Sinai School of Medicine, New York, New Yorka; University of Arkansas for the Medical Sciences, Little Rock, Arkansasb; Bressinck, Gibson, Parker, Dinehart and Sangster Dermatology, Little Rock, Arkansasc; Dallas Associated Dermatologistsd; University of Minnesota Academic Health Center, Department of Dermatology, Division of Clinical Research, Minneapolis, Minnesotae; Indiana University School of Medicine, Indianapolis, Indianaf; Welborn Clinic Research Center, Evansville, Indianag; Wake Forest University School of Medicine, Department of Dermatology, Winston-Salem, North Carolinah; and 3M Pharmaceuticals, St Paul, Minnesota.i Supported by 3M Pharmaceuticals, St Paul, Minnesota. Disclosure: Drs Lebwohl, Dinehart, Whiting, P. Lee, Tawfik, and Jorizzo have received support from 3M Pharmaceuticals for performing clinical trials. Drs Jorizzo and P. Lee have served as consultants for 3M Pharmaceuticals. Drs Lebwohl and Tawfik have received speaking honoraria. Dr J. Lee and Mr Fox are employees of 3M Pharmaceuticals. 714 A ctinic keratoses (AK) are epidermal lesions consisting of dysplastic keratinocytes that generally occur in pale-skinned individuals chronically exposed to UV radiation.1,2 As the incidence of nonmelanoma skin cancer increases, the Portions of this information have been presented at the 62nd Annual Meeting of the American Academy of Dermatology, Washington, DC, February 6-11, 2004 and at ACADEMY 2003, Chicago, Ill, July 25-29, 2003. Accepted for publication December 1, 2003. Reprint requests: Mark Lebwohl, MD, Department of Dermatology, The Mount Sinai School of Medicine, 5 E 98 St, Box 1048, New York, NY 10029-6574. E-mail: Lebwohl@aol.com. 0190-9622/$30.00 © 2004 by the American Academy of Dermatology, Inc. doi:10.1016/j.jaad.2003.12.010 J AM ACAD DERMATOL VOLUME 50, NUMBER 5 incidence of AK is also expected to increase throughout the world.3 In the white-skinned population older than 40 years who live in the northern hemisphere, the incidence of AK is estimated to range from 11% to 25%, whereas in the whiteskinned population living in Australia, the incidence is estimated to range from 40% to 60%.4,5 Histologically and clinically, there is a continuum and a progression between AK and squamous cell carcinoma (SCC) that makes reliable clinical distinction between the diseases difficult to determine; an AK lesion that evolves into an invasive SCC lesion can do so without displaying any distinguishing clinical features.6,7 Because it is impossible to predict the point at which an individual AK lesion will evolve into invasive SCC, some clinicians advocate the treatment of all AK lesions. The most common current therapies for the treatment of AK include cryosurgery, curettage with or without electrosurgery, and topical 5-fluorouracil. Because the pathogenesis of AK involves suppression of the cutaneous immune response, a treatment that stimulates the immune response would also be a potentially effective therapy. Imiquimod 5% cream is currently available as Aldara (3M Pharmaceuticals, St Paul, Minn) and is indicated for the treatment of external genital warts. It has been shown to stimulate the immune system by activating antigen-presenting cells such as monocytes/macrophages and dendritic cells to produce interferon and other cytokines and chemokines. Because of this unique mechanism, imiquimod has been used for the treatment of AK. Published anecdotes and small pilot studies suggested imiquimod would be an effective and well-tolerated treatment option for AK.8-11 To confirm these preliminary findings, two large, randomized, double-blind, parallel group, vehiclecontrolled trials were conducted to evaluate the efficacy and safety of topically applied imiquimod 5% versus vehicle cream for the treatment of AK lesions on the face and balding scalp. The two studies were of the same size and design, and were carried out concurrently at different study centers across the United States and Canada to provide independent confirmatory evidence of safety and efficacy. METHODS Study population Eligible participants were otherwise healthy men and women at least 18 years of age with 4 to 8 clinically diagnosed AK lesions located within a contiguous 25-cm2 treatment area on the face or balding scalp, but not both. Participants were to be excluded from the study if they had any condition in the treatment area that could be exacerbated by treat- Lebwohl et al 715 ment with imiquimod 5% cream or that would impair the examination of the treatment area. If a participant had previously received treatment with imiquimod 5% cream in the treatment area or had any known allergies to any excipients in the study cream, they were excluded. Participants were also excluded from study participation if they had received any of the following treatments in the 6 months before treatment initiation: psoralen plus UVA therapy; UVB therapy; laser abrasion; dermabrasion; or chemical peel. The use of moisturizers, over-the-counter retinol products, or products containing ␣- or -hydroxy acids in the treatment area was prohibited. Throughout the study and in the 4 weeks before treatment initiation, the following treatments were not allowed: prescribed topical retinoids; 5-fluorouracil; masoprocol; cryodestruction; chemodestruction; surgical excision; photodynamic therapy; curettage; interferon/interferon inducers; cytotoxic drugs; drugs with major organ toxicity; immunomodulators; immunosuppressive therapies; oral corticosteroids; or topical steroids anywhere on the head. Enrollment for both studies began in September 2001, and all study procedures were completed by August 2002. All study procedures and informed consent documents received approval from an institutional review board or international ethics committee, and all enrolled participants signed informed consent forms. The studies were conducted in compliance with the Code of Federal Regulations (CFR) of the United States Food and Drug Administration (21 CFR Part 56, Institutional Review Boards, and 21 CFR Part 50, Protection of Human Subjects) and the International Conference on Harmonization guidelines. Study design Data from participants enrolled at 24 centers in the United States and Canada were analyzed in two phase III, randomized, double-blind, parallel group, vehicle-controlled studies. The studies consisted of a prestudy period, a 16-week treatment period, and an 8-week posttreatment period. Participants who discontinued from the treatment period were asked to return for an assessment of their AK lesions 8 weeks after their last dose of treatment. At the prestudy visit, participants were screened for eligibility; demographic information was collected; and clinical laboratory tests, vital sign measurements, and physical examinations were performed. Enrolled participants were randomized to either imiquimod 5% or vehicle cream in a 1:1 ratio. The randomization assignments were made according to a computer-generated randomization schedule and 716 Lebwohl et al were allocated at treatment initiation. Labels with hidden disclosure panels were used to conceal treatment assignments from participants, investigators, study staff, and the sponsor. Study cream was delivered as imiquimod 5% cream (Aldara, 3M Pharmaceuticals) or vehicle cream. The vehicle cream was similar in appearance to imiquimod 5% cream, and was of identical composition, with the exception of the active ingredient. Study cream was administered topically from a single-use sachet that contained 250 mg of cream. Participants applied study cream 1 time per day, 2 days per week for 16 weeks. Dosing days were a minimum of 3 days apart (eg, Monday and Thursday), and participants were instructed to dose on the same 2 days of the week for each week of treatment. The 16-week treatment period was followed by an 8-week treatment-free follow-up period. Throughout the treatment and posttreatment periods, participants returned to the study centers for safety and efficacy assessments at weeks 1, 2, 4, 6, 8, 10, 12, 16 (end of treatment), 20, and 24 (end of posttreatment). Efficacy evaluation The primary objective was to evaluate the efficacy of imiquimod 5% cream compared with vehicle in the treatment of AK lesions when the cream was applied 2 times per week for 16 weeks. Efficacy was evaluated by clinically counting and recording the number of AK lesions present in the treatment area at the treatment initiation; at weeks 4, 8, and 16; and at 8-week posttreatment visit. The primary efficacy variable was the complete clearance rate, defined as the proportion of participants at the 8-week posttreatment visit with a count of 0 clinically visible AK lesions in the treatment area. The secondary efficacy variable was the partial clearance rate, defined as the proportion of participants at the 8-week posttreatment visit with at least a 75% reduction in the number of AK lesions counted at baseline in the treatment area. Safety evaluation Safety was monitored at every study center visit by photographing the treatment area and by reviewing adverse events, local skin reactions, and concomitant medication use. All safety data were tabulated separately by treatment group. Adverse events. Spontaneous participant-reported adverse events were categorized as follows: mild, the participant was aware of the signs and symptoms, but the signs and symptoms were easily tolerated; moderate, the signs and symptoms were sufficient to restrict, but not prevent, usual daily J AM ACAD DERMATOL MAY 2004 activity for the participant; and severe, the participant was unable to perform usual daily activity. Local skin reactions. Local skin reactions are adverse events that commonly occur in the treatment area. Data regarding local skin reactions were collected independently of other adverse events. Before the studies began, 7 local skin reactions were identified for assessment by the investigator at each study visit. They were clinically categorized as erythema, edema, erosion/ulceration, scabbing/crusting, weeping/exudate, vesicles, or flaking/scaling/ dryness. The severity of each local skin reaction was rated by a study investigator on a scale of 0 to 3, where 0 ⫽ none, 1 ⫽ mild, 2 ⫽ moderate, and 3 ⫽ severe. Clinical laboratory tests. At the prestudy visit and the week-16 (end-of-treatment) visit, hematology (hemoglobin, hematocrit, red blood cell, white blood cell, and platelet counts) and serum chemistry (random glucose, blood urea nitrogen, creatinine, total bilirubin, serum glutamic oxaloacetic transaminase, serum glutamic pyruvic transaminase, lactate dehydrogenase, alkaline phosphatase, potassium, sodium, calcium, chloride, total protein, albumin, phosphorous, and cholesterol) laboratory parameters were assessed. In addition, urine specimens were analyzed for color/appearance, specific gravity, pH, protein, glucose, and ketones; a microscopic examination was also performed. Skin quality assessments. At the treatment initiation and 8-week posttreatment visits, the investigator performed a skin quality assessment of each participant’s treatment area. Described characteristics included skin surface, hyperpigmentation, hypopigmentation, mottled or irregular pigmentation (both hyperpigmentation and hypopigmentation), degree of scarring, and atrophy. After visual, clinical, and tactile examinations of the treatment area, the investigator coded the intensity of each characteristic on a scale of 0 to 3, where 0 ⫽ none, 1 ⫽ mild, 2 ⫽ moderate, and 3 ⫽ severe. If, for example, atrophy was coded as mild and then later coded as severe, that skin characteristic would have increased in intensity. Statistical analysis The primary data set analyzed was the intent-totreat data set, which was composed of combined data from 24 study centers and included all randomized participants. For each study, the sample size was based on having at least 90% power to detect a minimum clinically meaningful difference in complete clearance rates of 14% for the vehicle group versus 35% for the imiquimod group, with a type I Lebwohl et al 717 J AM ACAD DERMATOL VOLUME 50, NUMBER 5 Fig 1. Participant accountability for combined twice weekly application studies. error rate of 0.05. There were no interim analyses or stopping rules. Treatment groups were compared with respect to the complete clearance rate by means of the Cochran-Mantel-Haenszel test, which adjusted for the effects of multiple study centers. These efficacy analyses were also done for the partial clearance rate. Fisher’s exact tests were used to compare treatment groups with respect to the incidence of adverse events, and Wilcoxon’s rank sum tests were used to compare treatment groups with respect to the most intense local skin reactions experienced by the participants. The Cochran-Armitage test for trend examined the data for relationships between complete clearance and maximum intensity of local skin reactions. For laboratory parameters, Wilcoxon’s signed rank tests were used to assess the significance of within-treatment shifts and within-treatment changes from baseline and Wilcoxon’s rank sum tests were used to compare treatment groups with respect to change from baseline. For skin quality assessments, Wilcoxon’s signed rank tests were used to assess the significance of within-treatment changes from baseline. For participant demographics, Fisher’s exact tests were used to compare treatment groups with respect to sex, race, and skin type; analysis of variance was used to compare treatment groups with respect to age. All statistical analyses were performed using software (SAS, Version 8, SAS Institute, Inc, Cary, NC). RESULTS Study population Between the two studies, a total of 623 people were screened and 436 (217 in one study and 219 in the other) were enrolled. Violations of inclusion or exclusion criteria were the most common reasons for study ineligibility. Overall, 215 participants were randomized to treatment with imiquimod 5% cream, and 221 were randomized to treatment with vehicle cream. Participant accountability is shown in Fig 1. There were no significant differences between treatment groups for age, sex, race, or Fitzpatrick skin type (Table I). Efficacy Imiquimod 5% cream was statistically significantly better than vehicle with respect to the complete clearance rate (P ⬍ .001). A complete clearance rate of 45.1% (97 of 215) was achieved by the imiquimod group, whereas the vehicle group had a complete clearance rate of 3.2% (7 of 221). The difference in complete clearance rates (imiquimod minus vehicle) was 41.9% with a 95% confidence interval of 34.9% to 49%. When examined separately, the complete clearance rates were very similar between the two studies. One study showed 718 Lebwohl et al J AM ACAD DERMATOL MAY 2004 Table I. Summary of participant demographics Variable Sex Female Male Age (y) Mean [SD] Range Race White American Indian Skin type (Fitzpatrick) I-II III-VI No. of baseline lesions Median (range) Imiquimod 5% cream (n ⴝ 215) 28 (13%) 187 (87%) Vehicle cream (n ⴝ 221) P value 28 (12.7%) 193 (87.3%) 1.00 65.5 [9.8] 37-88 .26 215 (100%) 0 (0%) 220 (99.5%) 1 (0.5%) 1.00 125 (58.1%) 90 (41.9%) 113 (51.1%) 108 (48.9%) .15 6 (4, 10) 6 (3, 9) .53 66.6 [10.6] 39-88 complete clearance rates of 45.8% (49 of 107) and 2.7% (3 of 110) for the imiquimod and vehicle groups, respectively; whereas in the second study the complete clearance rates were 44.4% (48 of 108) and 3.6% (4 of 111) for the imiquimod group and the vehicle group, respectively. Partial clearance rates were also significantly better for the imiquimod group than the vehicle group (P ⬍ .001). The partial clearance rates for the imiquimod and vehicle groups were 59.1% (127 of 215) and 11.8% (26 of 221), respectively. The difference in partial clearance rates (imiquimod minus vehicle) was 47.3% with a 95% confidence interval of 39.5% to 55.1%. Like the complete clearance rates, the partial clearance rates were very similar between the two studies. One study showed partial clearance rates of 59.8% (64 of 107) and 10% (11 of 110) for the imiquimod and vehicle groups, respectively; whereas in the second study the partial clearance rates were 58.3% (63 of 108) and 13.5% (15 of 111) for the imiquimod group and the vehicle groups, respectively. Both efficacy and safety results were comparable between the two studies, and for this reason the remaining results will be presented as combined data. At the 8-week posttreatment visit, the median percent reduction in the number of AK lesions counted at baseline was 83.3% for the imiquimod group and 0% for the vehicle group. Therefore, half of the participants in the imiquimod group had at least an 83.3% reduction in the number of AK lesions counted at baseline. During the treatment period, 48% (103 of 215) of the imiquimod group and 33% (72 of 221) of the vehicle group had an increase in AK lesion count (above the baseline level) at one or more of the defined AK lesion count collection visits during the treatment period. In the imiquimod group, those with complete clearance had a slightly higher rate of increased AK lesion counts during the treatment period compared with those without clearance: 52% (50 of 97) of participants with complete clearance experienced an increase in AK lesion count compared with 45% (53 of 118) of participants without complete clearance. For the imiquimod treatment group, statistically significant (P ⬍ .05) trends were found for erythema, edema, erosion/ulceration, weeping/exudate, and scabbing/crusting; specifically, the complete clearance rate increased as the severity of these local skin reactions increased. No relationships were significant for the vehicle group. Safety Adverse events. Adverse events were reported by 77.2% (166 of 215) of participants who received imiquimod and 63.8% (141 of 221) of participants who received vehicle. During the study, 6% (13 of 215) of participants treated with imiquimod and 6.3% (14 of 221) of participants who received vehicle reported at least one severe adverse event. Application site reactions (adverse events in the treatment area that were not predefined) were the most frequently reported adverse events and were reported by 33% (71 of 215) of participants on imiquimod and 14.5% (32 of 221) of participants on vehicle. Adverse events that were probably or possibly related to study cream were reported by 34.4% (74 of 215) of participants on imiquimod and by 14.9% (33 of 221) of participants on vehicle. The most commonly reported application site reactions that were possibly or probably Lebwohl et al 719 J AM ACAD DERMATOL VOLUME 50, NUMBER 5 Table II. Application site reactions possibly or probably related to study drug that were reported by at least 1% of participants in the twice weekly studies Application site reaction* Itching at target site Burning at target site Bleeding at target site Stinging at target site Induration at target site Pain at target site Tenderness at target site Itching at remote site Burning at remote site Irritation at remote site Imiquimod 5% cream 2 d/wk (n ⴝ 215) Vehicle cream 2 d/wk (n ⴝ 221) P value 44 (20.5%) 12 (5.6%) 7 (3.3%) 6 (2.8%) 5 (2.3%) 5 (2.3%) 4 (1.9%) 7 (3.3%) 4 (1.9%) 3 (1.4%) 15 (6.8%) 4 (1.8%) 1 (0.5%) 2 (0.9%) 3 (1.4%) 2 (0.9%) 3 (1.4%) 3 (1.4%) 0 (0.0%) 0 (0.0%) ⬍.001 .04 .04 .17 .50 .28 .72 .22 .06 .12 *Target site refers to the treatment area; remote site refers to the area surrounding the treatment area and beyond. related to study cream are listed by type in Table II. A total of 30 serious adverse events, including one death, were reported by 10 participants who received imiquimod and 8 participants who received vehicle. None of the serious adverse events were judged as related to study cream. In addition, two participants randomized to treatment with imiquimod had local skin reactions or adverse events in the treatment or surrounding areas that were suggestive of bacterial infection. Skin culture results, coupled with the signs and symptoms that prompted the skin culture, led to a clinical diagnosis of bacterial infection for one participant (⬍1%). During the treatment period, 7 (3%) of the 215 participants who received imiquimod and 2 (1%) of the 221 participants who received vehicle discontinued because of adverse events. Of these adverse events, 4 were considered to be possibly or probably related to treatment (3 incidences of application site reactions, and 1 incident of flu-like symptoms). All 4 events considered possibly or probably related to treatment were experienced by participants who received imiquimod. No participants who received vehicle (0%) discontinued from the treatment period as a result of the adverse event of application site reaction, and no participants discontinued from the posttreatment period because of application site reactions. Local skin reactions. Local skin reactions were common and occurred in both treatment groups. Erythema was experienced by 97.2% (209 of 215) of participants in the imiquimod group and 93.6% (206 of 220) of participants in the vehicle group. Severe local skin reactions were experienced by participants randomized to treatment with imiquimod and by participants who received vehicle; the rate of severe local skin reactions was higher in the imi- Table III. Incidence of severe local skin reactions Type of local skin reaction Imiquimod 5% cream 2 d/wk (n ⴝ 215) Vehicle cream 2 d/wk (n ⴝ 220*) Erythema Scabbing/crusting Flaking/scaling/dryness Erosion/ulceration Edema Vesicles Weeping/exudate 38 (17.7%) 18 (8.4%) 16 (7.4%) 5 (2.3%) 0 (0%) 0 (0%) 0 (0%) 5 (2.3%) 4 (1.8%) 7 (3.2%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) *One participant in the vehicle group did not have an assessment of local skin reactions after treatment initiation; consequently the denominator is 220 rather than 221. quimod group. The most common investigator-assessed severe local skin reactions were erythema, flaking/scaling/dryness, and scabbing/crusting (Table III). The local skin reactions shown in Fig 2, B, represent typical responses to imiquimod 5% cream and were generally well tolerated. Two participants who received imiquimod (1%) and no participants on vehicle (0%) discontinued from the treatment period because of local skin reactions. No participants discontinued from the posttreatment period because of local skin reactions. Clinical laboratory tests. Changes in hematology parameters, particularly in platelet counts and hemoglobin, were observed that showed a significant difference within and between treatment groups. In addition, statistically significant withintreatment shifts in hemoglobin values from baseline to the end of treatment (relative to the reference range) were observed for the imiquimod group. The standard errors of these significance tests were small as a result of the large sample sizes, thus, making it 720 Lebwohl et al J AM ACAD DERMATOL MAY 2004 Fig 2. A, Baseline count of 4 actinic keratosis (AK) lesions in treatment area (an approximation of the treatment area is outlined). B, Treatment area with 6 AKs, mild flaking/scaling/dryness, and moderate erythema after 4 weeks of treatment. C, Complete clearance at 8 weeks posttreatment (0 lesions). possible to detect small differences as statistically significant. None of the changes were considered clinically meaningful as they were minor and without clinical sequelae. Skin quality assessments. In general, 2 times per week dosing with imiquimod 5% cream did not increase the intensity of skin quality characteristics. In particular, at the end of the study less intense assessments of the characteristic skin surface (ie, roughness/dryness/scaliness) were noted in participants who received imiquimod. Of the 205 participants randomized to treatment with imiquimod who had both initiation and 8-week posttreatment skin surface assessments, 114 (56%) had a decrease in roughness/dryness/scaliness at 8 weeks posttreatment compared with baseline, and 3 (1%) had an increase in roughness/dryness/scaliness (P ⬍ .001). For the 210 participants on vehicle, 46 (22%) had a decrease in roughness/dryness/scaliness at 8 weeks posttreatment compared with baseline and 30 (14%) had an increase (P ⫽.20). DISCUSSION Imiquimod 5% cream is an effective and welltolerated treatment option for AK lesions on the face and scalp. The results confirm earlier study results and published anecdotes that showed imiquimod 5% cream was an effective treatment for AK. The benefits of treatment with topical imiquimod 5% cream include complete clearance of AK lesions for 45.1% of participants and partial clearance (ⱖ75% reduction in the number of baseline lesions) for 59.1% of participants. According to this protocol, participants who experienced resolution of 7 out of 8 lesions were considered treatment failures because they did not achieve complete clearance; however, the partial clearance of most of their lesions would be considered clinically meaningful by both patients and physicians. Half of the participants treated with imiquimod experienced at least an 83% reduction in the number of AK lesions counted at baseline. An additional benefit of treatment with imiquimod was that it effectively uncovered and treated subclinical lesions. In fact, more than half of participants treated with imiquimod who experienced complete resolution of their AK lesions also experienced an increase in their AK lesion count during the study. This increase in lesion count was most likely a result of the appearance of subclinical lesions rather than the formation of new AK lesions. Most of the participants who received imiquimod had local skin reactions and one third of them reported application site reactions. The side effects were consistent with local stimulation of an immune response. Even though erythema was experienced by more than 97% of participants in the imiquimod group, most participants denied accompanying discomfort. In fact, only 2.3% and 5.6% of the participants in the imiquimod treatment group reported pain and burning at the treatment site, respectively. Imiquimod has been shown to stimulate the immune system by activating antigen-presenting cells such as monocytes/macrophages and dendritic cells to produce interferon and other cytokines and chemokines. The activation of Langerhans cells has been shown to increase the recognition of antigens expressed by actinically damaged cells.12 In addition, cytokines produced by various immune regulatory cells (eg, macrophages, monocytes, Langerhans cells) have been shown to result in an influx of lymphocytes into the epidermis, an up-regulation of tumor cell surface markers so they can be more readily recognized by these lymphocytes, and an up-regulation of the apoptotic signaling pathway leading to individual AK cell death.13 This immune response was evident in the local skin reactions experienced by participants treated with imiquimod. The cutaneous immune response has been shown to play an important role in the transformation of AK into invasive SCC.14 Therefore, the stim- J AM ACAD DERMATOL VOLUME 50, NUMBER 5 ulation of the immune response by imiquimod could potentially decrease the transformation rate of AK into invasive SCC. Similarly, induction of a cellmediated response could theoretically decrease the recurrence rate or the rate of new AK lesion formation in the treated areas. Although the results of this study provide important information on an additional treatment option in the management of AK, there are some limitations that need to be addressed. The patient population studied was selected to represent the typical patient who presents to a dermatologist for treatment of AK lesions. Patients with extensive disease were not evaluated in this study and, therefore, extrapolation of the complete and partial clearance rates may not be valid for this patient population. Although the study design was double blind, the pharmacodynamic effect of the imiquimod treatment likely increased the observation bias. However, this bias is inherent in studies where there is an observable pharmacodynamic response. Because the primary objective of this study was to evaluate the efficacy of imiquimod treatment, no long-term follow-up period was incorporated into this study. The long-term safety and recurrence rate need to be evaluated in a long-term follow-up study. Finally, patient-centered outcomes were not collected and need to be addressed in future studies. In conclusion, the results of this study demonstrate that imiquimod 5% cream is an effective and safe treatment for AK. Imiquimod 5% cream is a topical, patient-applied product that offers both the patient and clinician a unique therapeutic approach. We thank Nanda Gosala, MD, for medical monitoring; Mary Owens, MD, for editorial contributions; Scott McKane for statistical analyses support; and A´ ine Skow for manuscript preparation. The following are principal investigators who participated in the study: Scott Dinehart, MD (coordinating investigator); Mark Lebwohl, MD (coordinating investigator); Donald Belsito, MD; Robert Brown, MD; Charles Dugan, MD; Richard Fitzpatrick, MD; Scott Fosko, MD; Lebwohl et al 721 Glenn Goldman, MD; William Harwell, MD; Joseph Jorizzo, MD; Richard Langley, MD; Peter Lee, MD, PhD; Nicholas Lowe, MD; David McDaniel, MD; Ida Orengo, MD; Yves Poulin, MD; Ronald Rapini, MD; Leonard Swinyer, MD; David Tashjian, MD; Naji Tawfik, MD, PhD; John Toole, MD; Jeffrey Weinberg, MD; David Whiting, MD; and Paul Yamauchi, MD, PhD. REFERENCES 1. Frost CA, Green AC. Epidemiology of solar keratoses. Br J Dermatol 1994;131:455-64. 2. Heaphy MRJ, Ackerman AB. The nature of solar keratosis: a critical review in historical perspective. J Am Acad Dermatol 2000; 43:138-50. 3. Coldiron BM. Thinning of the ozone layer: facts and consequences. J Am Acad Dermatol 1992;27:653-62. 4. Engel A, Johnson M-L, Haynes SG. Health effects of sunlight exposure in the United States: results from the first national health and nutrition examination survey 1971-1974. Arch Dermatol 1988;124:72-9. 5. Frost CA, Green AC, Williams GM. The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia). Br J Dermatol 1998;139:1033-9. 6. Ponsford MW, Goodman G, Marks R. The prevalence and accuracy of diagnosis of non-melanotic skin cancer in Victoria. Australas J Dermatol 1983;24:79-82. 7. Moy RL. Clinical presentation of actinic keratoses and squamous cell carcinoma. J Am Acad Dermatol 2000;42(Suppl):S8-10. 8. Stockfleth E, Meyer T, Benninghoff B, Salasche S, Papadopoulos L, Ulrich C, et al. A randomized, double-blind, vehicle-controlled study to assess 5% imiquimod cream for the treatment of multiple actinic keratoses. Arch Dermatol 2002;138:1498-502. 9. Stockfleth E, Meyer T, Benninghoff B, Christophers E. Successful treatment of actinic keratosis with imiquimod cream 5%: a report of six cases. Br J Dermatol 2001;144:1050-3. 10. Persaud AN, Shamuelova E, Sherer D, Lou W, Singer G, Cervera C, et al. Clinical effect of imiquimod 5% cream in the treatment of actinic keratosis. J Am Acad Dermatol 2002;47:553-6. 11. Salasche S, Levine N, Morrison L. Cycle therapy of actinic keratoses of the face and scalp with 5% topical imiquimod cream: an open-label trial. J Am Acad Dermatol 2002;47:571-7. 12. Aberer W, Shuler G, Stingl G, Hunigsmann H, Wolff K. Ultraviolet light depletes surface markers of Langerhans cells. J Invest Dermatol 1981;76:202-7. 13. Strickland F, Kripke M. Immune response associated with nonmelanoma skin cancer. Clin Plast Surg 1997;24:637-47. 14. Tucci M, Offidani A, Lucarini G, Simonelli L, Amati S, Cellini A, et al. Advances in the understanding of malignant transformation of keratinocytes: an immunohistochemical study. J Eur Acad Dermatol Venereol 1998;10:118-24.
© Copyright 2025