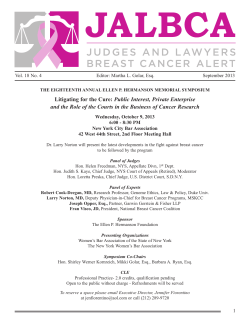
Breast Cancer Research and Treatment
Breast Cancer Research and Treatment CONTENTS VOL. 106, Supplement 1, December 2007 Special issue 30th Annual SAN ANTONIO BREAST CANCER SYMPOSIUM – December 13–16, 2007 Program iii–xlviii Invited Abstracts S1–S4 Abstracts General Sessions [#11-82] Poster Discussion Sessions [#101-511] Poster Session I [#1001-1119] Poster Session II [#2001-2121] Poster Session III [#3001-3113] Poster Session IV [#4001-4117] Poster Session V [#5001-5119 (excl. 5015)] Poster Session VI [#6001-6119 plus 5015] S5–S23 S24–S40 S41–S83 S84–S125 S126–S165 S166–S206 S207–S246 S247–S287 Author index for abstracts S288–S302 Breast Cancer Res Treat (2007) DOI 10.1007/s10549-007-9793-3 © Springer Science+Business Media, LLC. 2007 Photocopying. In the U.S.A.: This journal is registered at the Copyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923 [info@copyright.com]. Authorizations to photocopy items for internal or personal use, or the internal or personal use of specific clients, is granted by Springer for users registered with the Copyright Clearance Center (CCC). For those organizations that have been granted a photocopy licence, a separate system of payment has been arranged. Authorization does not extend to other kinds of copying, such as that for general distribution, for advertising or for promotional purposes, for creating new collective works, or for resale. The CCC’s services for users can be found on the internet at www.copyright.com. In the rest of the world: Permissions to photocopy must be obtained from the copyright owner. Please apply to Springer Rights & Permissions Department, P.O. Box 17, 3300 AA, Dordrecht, The Netherlands [permissions.dordrecht@springer.com]. Breast Cancer Research and Treatment is published monthly plus 1 additional issue in January, March, May, July, September and November (Volumes 101–106, 3 issues each, 2007). Periodicals postage paid at Rahway, N.J. USPS No. 663–130. U.S. Mailing Agent: Mercury Airfreight International Ltd., 365 Blair Road, Avenel, NJ 07001. Published by Springer, P.O. Box 17, 3300 AA Dordrecht, The Netherlands, and 101 Philip Drive, Norwell, MA 02061, U.S.A. Postmaster: Please send all address corrections to: Breast Cancer Research and Treatment c/o Mercury Airfreight International Ltd., 365 Blair Road, Avenel, NJ 07001, U.S.A. Printed on acid free paper 30t Annual December 13 – 16, 2007 Henry B. Gonzalez Convention Center 200 E. Market Street, San Antonio, Tx 78205 Sponsors and an NCI-designated Clinical Cancer Center a partnership of & Industry And Agency Support (at press time) Donors Angel Plus Adjuvant, Inc. Almac Diagnostics AlphaMed Press AmeriPath, Inc. Aptium Oncology Biocare Medical LLC Biogen Idec Breakthrough Breast Cancer Cambridge University Press Care Wise Medical Products Cianna Medical Clinical Oncology News Coalition of Cancer Cooperative Groups Congressional Directed Medical Research Programs(CDMRP) CURE Media Group Diplomat Specialty Pharmacy Elsevier, Inc. Faxitron X-Ray LLC Hem/Onc Today/SLACK Incorporated ImpediMed, Inc Informa Healthcare Jones and Bartlett Publishers KUBTEC X-Ray Lippincott Williams & Wilkins MedPage Today, LLC National Accreditation Program for Breast Centers The Oncology Group Oncology Nursing Society Springer TRIO (CIRG/TORI) Wiley-Blackwell Women’s Health Boutique, Inc. Abraxis Oncology AstraZeneca Bristol-Myers Squibb Eli Lilly and Company Genentech BioOncology Genomic Health, Inc. GlaxoSmithKline Novartis Oncology Pfizer Roche sanofi-aventis Patron Plus Amgen Patron Eisai, Inc. Major Supporter Plus Merck Oncology Veridex, A Johnson and Johnson Company Major Supporter Aperio Technologies, Inc. Bayer HealthCare PharmaceuticalsCarl Zeiss Surgical, Inc. Cytogen Corporation Cytyc CorporationGE Healthcare Monogram Biosciences Valeant Pharmaceuticals. Contributors Agendia B.V. CBCE CRI Cytori Therapeutics Exagen Diagnostics Gamma Medica-Ideas Molecular Profiling Institute Myriad Genetic Laboratories, Inc. Naviscan PET Systems NeoMatrix Nichols Institute for Oncology North American Scientific Ortho Biotech PhenoPath Laboratories Physicians’ Education Resource Projects in Knowledge, Inc. RadPharm, Inc. Research to Practice SenoRx, Inc. SiteSelect Medical SurgRx, Inc. Sysmex TopoTarget USA, Inc. University of Florida Jacksonville Healthcare, Inc. US Labs Ventana Medical Systems, Inc. Visual Med Clinical Solutions Corp. Conference Grants National Cancer Institute Future Symposium Meeting Dates 31st Annual SABCS December 11-14, 2008 (Thursday-Sunday) 32ⁿd Annual SABCS December 10-13, 2009 (Thursday-Sunday) 33rd Annual SABCS December 9-12, 2010 34t Annual SABCS December 7-10, 2011 30th Annual San Antonio Breast Cancer Symposium Program Schedule 10:15 10:30-12:00 Jenny Chang, MD, Co-Moderator Baylor College of Medicine, Houston, TX and Michael Lewis, PhD, Co-Moderator Baylor College of Medicine, Houston, TX Exhibit Halls A, B, C & D, Ballrooms A & B: Street Level Bridge Hall: Street Level 12:00-7:00 10:30 Introduction 10:30 Breast cancer stem cell: Targets for prevention & therapy Max Wicha, MD University of Michigan Comprehensive Cancer Center Ann Arbor, MI 11:00 Cancer stem cells in therapeutic resistance and as cellular targets Jeremy Rich, MD Duke University Medical Center Durham, NC 11:30 Epigenetic stem cell signatures in breast cancer Peter Laird, PhD USC/Norris Comprehensive Cancer Center Los Angeles, CA REGISTRATION – Bridge Hall Pre-registered attendees can obtain materials. Those who have not yet registered may do so. Thursday, December 9:00-9:10 WELCOME – Exhibit Hall D Opening Remarks C. Kent Osborne, MD Charles A. Coltman, Jr., MD 9:10-9:30 PLENARY LECTURE 1 – Exhibit Hall D The worldwide overview: new results for systemic adjuvant therapies 12:00-1:00 LUNCH [Ticket Required] – Exhibit Hall A 1:00-1:30 PLENARY LECTURE 2 – Exhibit Hall D Richard Peto, for the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) University of Oxford Oxford, UNITED KINGDOM 9:30-10:30 9:30 Radiation treatment planning for breast cancer: A journey through time Lori Pierce, MD University of Michigan Medical School Ann Arbor, MI GENERAL SESSION 1 – Exhibit Hall D 11. High-dose chemotherapy with autologous stem-cell support versus standard-dose chemotherapy: meta-analysis of individual patient data from 15 randomized adjuvant breast cancer trials. Berry DA, Ueno NT, Johnson MM, Lei X, Lopez V, Caputo J, Bregni M, Demirer T. MDACC-EBMT Meta-Analysis Group, Houston, TX. 9:45 12. Extended follow-up and analysis by age of the US Oncology Adjuvant trial 9735: docetaxel/cyclophosphamide is associated with an overall survival benefit compared to doxorubicin/cyclophosphamide and is well-tolerated in women 65 or older. Jones S, Holmes F, O’Shaughnessy J, Blum J, Vukelaj S, McIntyre K, Pippen J, Bordelon J, Kirby R, Sandbach J, Hyman W, Khandelwal P, Negron A, Richards D, Mennel R, Boehm K, Meyer W, Asmar L, Muss H, Savin M. US Oncology Research, Inc., Houston, TX; Vermont Cancer Center, Burlington, VT. 10:00 13. Role of anthracycline-based therapy in the adjuvant treatment of breast cancer: efficacy analyses determined by molecular subtypes of the disease. Slamon DJ, Mackey J, Robert N, Crown J, Martin M, Eiremann W, Pienkowski T, Bee V, Taupin H, Villalobos I, Lindsay M-A, Riva A, Hurvitz S, Glaspy J, Pauletti G, Sauter G, Press M. Cancer International Research Group (CIRG), Edmonton, AB, Canada. MINI-SYMPOSIUM 1 – Exhibit Hall D STEM CELLS IN BREAST CANCER Room Locations Wednesday, December , 14. Outcome of breast cancer therapies for adjuvant versus advanced disease: how much do they differ? Critical comments towards the present process of randomized trials as a pre-requisite for adjuvant therapy guidelines. Ragaz J, Spinelli JJ. McGill University Health Centre, Montreal, QC, Canada; British Columbia Cancer Agency, Vancouver, BC, Canada. 1:30-3:45 GENERAL SESSION 2 – Exhibit Hall D 1:30 21. Long-term results of a randomized trial of accelerated hypofractionated whole breast irradiation following breast conserving surgery in women with node negative breast cancer. Whelan T, Pignol JP, Julian J, Grimard L, Bowen J, Perera F, Schneider K, Fyles A, Gulavita S, Shelley W, Freeman C, Szechtman B, Levine M. Juravinski Cancer Centre, Hamilton, ON, Canada; McMaster University, Hamilton, ON, Canada; Toronto Sunnybrook Regional Cancer Centre, Toronto, ON, Canada; Ottawa Regional Cancer Centre, Ottawa, ON, Canada; Northeastern Ontario Regional Cancer Centre, Sudbury, ON, Canada; London Regional Cancer Centre, London, ON, Canada; Windsor Regional Cancer Centre, Windsor, ON, Canada; Princess Margaret Hospital, Toronto, ON, Canada; Northwestern Regional Cancer Centre, Thunder Bay, ON, Canada; Kingston Regional Cancer Centre, Kingston, ON, Canada; McGill University Health Centre, Montreal, QC, Canada. 1:45 22. dHER2 cancer immunotherapeutic: clinical response in breast cancer patients is associated with an induction of functional antibodies and the generation of specific T cells. Limentani SA, Curigliano G, Campone M, Dorval T, Romieu G, Vogel C, White S, de Boer R, Lehmann F, Cormont F, Louahed J. Blumenthal Cancer Center, Charlotte, NC; Ist Eur Oncol, Milan, Italy; Cent R Ganducheau, Nantes, France; Inst Curie, Paris, France; CRLCC, Montpellier, France; Cancer Res Network, Boca Raton, FL; Austin Hosp, Heidelberg, Australia; Royal Melbourne Hosp, Parkville Vic, Australia; GSK Bio, Rixensart, Belgium. 2:00 23. Fulvestrant 500 mg vs 250 mg: first results from NEWEST, a randomized, phase II neoadjuvant trial in postmenopausal women with locally advanced, estrogen receptor-positive breast cancer. Kuter I, Hegg R, Singer CF, Badwe R, Lowe E, on behalf of the NEWEST investigators. Massachusetts General Hospital, Boston, MA; University of Sao Paulo & Perola Bygton Hospital, Sao Paulo, Brazil; Medical University of Vienna, Vienna, Austria; Tata Memorial Hospital, Mumbai, India; AstraZeneca, Wilmington, DE. 5:00-7:00 101. Serial detection and characterization of circulating tumor cells in an animal model. Eliane JP, Luker KE, Brown M, Repollet M, Doyle GV, Hayes DF, Luker GD. University of Michigan Medical School, Huntingdon Valley, PA. 2:15 24. Anti-estrogens promote an invasive phenotype in intercellular adhesion deficient breast cancer cells. Borley AC, Barrett-Lee PJ, Gee JMW, Shaw VE, Nicholson RI, Hiscox SE. Velindre Cancer Centre, Cardiff, United Kingdom; Tenovus Centre for Cancer Research, Cardiff, United Kingdom. 102. 2:30 25. The VEGF-R inhibitor PTK787/ZK222584 (PTK/ZK) also inhibits aromatase: preclinical studies of PTK/ZK in combination with endocrine therapy. Banerjee SN, Thornhill A, Evans DB, Littlewood-Evans AJ, Dowsett M, Martin L-A. Institute of Cancer Research, London, United Kingdom; Novartis Institute for BioMedical Research-Basel, Basel, Switzerland. A new system for enrichment and detection of circulating tumor cells in the peripheral blood of patients with metastatic breast cancer. Deng G, Burgess D, Manna E, Krag D, Herrler M. Applied Imaging Corp., San Jose, CA; University of Vermont, College of Medicine, VT. 103. MagSweeper: an automated system for high efficiency and specificity capture of live circulating tumor cells. Powell AA, Talasaz AAH, Mindrinos M, Carlson R, Pease FW, Davis RW, Jeffrey SS. Stanford University, Stanford, CA. 104. 26. Bone mineral density (BMD) at 5 years after diagnosis in premenopausal patients with endocrine-responsive breast cancer, after 3 years of adjuvant endocrine treatment with goserelin and tamoxifen or anastrozole or both treatments in combination with zoledronic acid - new results from ABCSG-12. Gnant M, Mlineritsch B, Luschin-Ebengreuth G, Kainberger F, Kaessmann H, Piswanger-Soelkner C, Seifert M, Schippinger W, Menzel C, Dubsky P, Fitzal F, Steger G, Greil R, Marth C, Kubista E, Samonigg H, Jakesz R, on behalf of the ABCSG. Austrian Breast and Colorectal Cancer Study Group, Vienna, Austria. Circulating tumor cells as a reliable assessment of treatment efficacy in metastatic breast cancer. Liu MC, Shields P, Isaacs CJD, Warren R, Cohen P, Wilkinson M, Ottaviano Y, Zhang Y, Shen R, Jasti M, Gallagher A. Lombardi Cancer Center, Georgetown University Hospital, Washington, DC; Franklin Square Hospital, Baltimore, MD. 105. Disseminated tumor cells correlate with estrogen receptor positivity in operable breast cancer patients. Alvarado MD, Brissaud C, Scott J, Magbanua M, Moore D, Ewing CA, Hwang S, Esserman LJ, Park JW. University of California, San Francisco, CA. 106. 27. The effect of zoledronic acid on aromatase inhibitorassociated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: the Z-FAST study 36-month follow-up. Brufsky A, Bosserman L, Caradonna R, Haley B, Jones M, Moore H, Dong M, Warsi G, Lacerna L, Perez E. Z-FAST Study Group; Novartis Pharmaceuticals, East Hanover, NJ. Features of patients (pts) with metastatic breast cancer (mBC) and a circulating tumor cell count (CTCc) of 0. Bubis JA, Marsland TA, Justice KM, Edwards D. Integrated Community Oncology Network, Orange Park, FL. 107. Bone marrow micrometastasis and circulating tumor cells are respectively strong prognostic factors in early and metastatic breast cancer, a comparative study on 759 patients. Bidard F-C, Vincent-Salomon A, Sastre X, Sigal-Zafrani B, Nos C, Mignot L, Dieras V, Asselah J, Thiery JP, Pierga J-Y. Institut Curie, Paris, France; IMCB Biopolis, Singapore, Singapore. 108. Prognostic value of the detection of circulating tumor cells using a multimarker RT-PCR (CK19, mammaglobin A, HER2/ neu) in early breast cancer. Ignatiadis M, Kallergi G, Ntoulia M, Apostolaki S, Perraki M, Xenidis N, Stathopoulou A, Lianidou E, Georgoulias V, Mavroudis D. University General Hospital of Heraklion, Heraklion, Crete, Greece; School of Medicine, University of Crete, Heraklion, Crete, Greece; University of Athens, Athens, Greece. 109. Circulating CK-19 mRNA (+) cells in patients with stage I and II breast cancer after the completion of adjuvant chemotherapy: evaluation of their prognostic relevance. Xenidis N, Apostolaki S, Perraki M, Politaki E, Kalbakis K, Ignatiadis M, Kalykaki A, Agelaki S, Georgoulias V, Mavroudis D. University General Hospital of Heraklion, Heraklion, Crete, Greece; School of Medicine, University of Crete, Heraklion, Crete, Greece. 110. Circulating epithelial tumor cells a new tool for therapy monitoring in breast cancer: a more than tenfold increase in numbers during systemic therapy is highly predictive of relapse. Pachmann K, Camara O, Cavallaris A, Krauspe S, Malarski N, Gajda M, Kroll T, Runnebaum I, Hoeffken K. Friedrich SchillerUniversität Jena, Jena, Germany. 2:45 3:00 3:15 3:30 3:45-5:00 28. Effect of anastrozole on bone mineral density after one year of treatment: results from bone sub-study of the International Breast Cancer Intervention Study (IBIS-II). Singh S, Cuzick J, Edwards R, Blake G, Truscott J, Coleman J, Eastell R, Howell A. Wolfson Institute of Preventive Medicine, London, United Kingdom; Kings College School of Medicine, London, United Kingdom; University of Leeds, United Kingdom; University of Newcastle, Australia; Christie Hospital, Manchester, United Kingdom; Northern General Hospital, Sheffield, United Kingdom. 29. Risk stratification based on the CYP2D6 tamoxifen metabolizing gene within the Italian tamoxifen prevention trial. Bonanni B, Maisonneuve P, Johansson H, Macis D, Serrano D, Guerrieri-Gonzaga A, Basso D, Zambon C, Plebani M, Nicoloff M, Fontecha M, Hillman G, Wieczorek L, Rotmensz N, Decensi A. European Institute of Oncology (EIO); EIO, Milan, Italy; University-Hospital of Padova, Padova, Italy; Roche Molecular Diagnostics, Pleasanton, CA; E.O. Ospedali Galliera, Genova, Italy. SUSAN G. KOMEN FOR THE CURE BRINKER AWARDS FOR SCIENTIFIC DISTINCTION LECTURES – Exhibit Hall D POSTER DISCUSSION 1 & RECEPTION – Ballroom B Circulating Tumor Cells 101-110 1014 Are the MRI characteristics of malignant breast lesions different for African American women? Jansen SA, Abe H, Shimauchi A, Karczmar GS, Olopade O, Newstead GM. University of Chicago, Chicago, IL. 1015 Pushing the limits: very high spatial resolution spectroscopic MR imaging of human breast. Medved M, Newstead GM, Abe H, Wood AM, Olopade OI, Shimauchi A, Fischer S, Karczmar GS. University of Chicago, Chicago, IL; Philips Medical Systems, Cleveland, OH. 1016 The effect of computer-aided detection on the interpretation of screening mammograms at Intermountain Healthcare facilities. Parkinson B, Belnap T, Rowley B, Blaney S, Kerry A, Pinto K, Nkoy F. Intermountain Healthcare, Salt Lake City, UT. 1017 A new approach to studying the progression of mammary gland carcinoma in mice: high resolution MRI of early cancer and DCIS. Jansen SA, Conzen S, Zamora M, Krausz T, Newstead GM, Karczmar GS. University of Chicago. Telemammography in a rural community. Lopez AM, Deasy S, Carroll M, Krupinski E, Kreykes L, Weinstein R. University of Arizona, Tucson, AZ; Tuba City Reginal Health Care Corporation, Tuba City, AZ. 1018 Magnetic resonance imaging in predicting pathologic residual disease after primary induction chemotherapy. Anderson CM, Patrick RJ, Rybicki LA, Chellman-Jeffers M, Obi B, Crowe JP. Cleveland Clinic, Cleveland, OH. Mammography screening and other preventive care among African American and native American women with access to health care. Bachman SI, Shim V. Kaiser Permanente, Oakland, CA. 1019 Initial clinical evaluation of laser optoacoustic imaging system for diagnostic imaging of breast cancer. Oraevsky AA, Ermilov SA, Conjusteau A, Miller T, Gharieb RR, Lacewell R, Mehta K, Radulescu EG, Herzog D, Thompson S, Stein A, McCorvey M, Otto P, Khamapirad T. Fairway Medical Technologies, Houston, TX; Seno Medical Instruments, San Antonio, TX; University of Texas Medical Branch, Galveston, TX; University of Texas Health Science Center, San Antonio, TX. 1020 Sonobreast: a novel predictive model for the risk of malignancy in solid breast nodules with echographic expression. Paulinelli RR, Freitas-Junior R, Lucena CEM, Moreira MAR, Moraes VA, Ruiz AN, Bernardes-Junior JRM, Vidal CSR, Lucato MT, Costa NGS, Teixeira DA. Federal University of Goias, Goiania, Goias, Brazil; Santa Casa de Misericordia, Belo Horizonte, Minas Gerais, Brazil. 1021 High resolution positron emission mammography in breast cancer management. Schilling KJ. Boca Raton Community Hospital, Boca Raton, FL. 1022 A comparison study between multidetector-row CT and histopathological findings in terms of the extension diagnosis of breast cancer. Sumiyoshi K, Kani H, Nohara T, Iwamoto M, Harada T, Tanaka S, Kimura K, Takahashi Y, Shibayama Y, Tsuji M, Kurisu Y, Tanigawa N. Osaka Medical College, Takatsuki, Osaka, Japan. 1023 Correlation of Ki67 expression with FDG-PET positivity in triple negative breast cancer. Tchou J, John T, Basu S, Rosen M, Schnall M, Alavi A. University of Pennsylvania, Philadelphia, PA. 1024 Breast optical tomography: sensitivities and specificities for the detection of cancer. Sharma A, Enfield L, Gibson AP, Everdell NL, Schweiger M, Arridge S, Delpy DT, Hebden JC, Keshtgar M, Sainsbury RS, Douek M. University College London Hospital, London, United Kingdom; University College London, Malet Place, London, United Kingdom. 1025 Mammographic features of triple-negative versus HER2+ and ER+ breast cancers. Yang WT, Dryden M, Broglio K, Dawood S, Valero V, Hortobagyi G, Atchley D, Arun B. M. D. Anderson Cancer Center, Houston, TX. 5:00-7:00 POSTER SESSION 1 & RECEPTION Exhibit Hall B (#1001-1119) Detection and Diagnosis: Mammography / Imaging 1001-1033 1001 1002 1003 1004 Effect of magnetic resonance imaging on the clinical management of women with newly diagnosed breast cancer. Newstead GM, Abe H, Jansen SA, Shimauchi A, Sennett CA, Schmidt RA, Zak L, Olopade O, Jaskowiak N. University of Chicago, Chicago, IL. Deconvolution-based dynamic contrast enhanced MRI of breast cancer: correlation of tumor blood flow with pathologic and molecular markers. Makkat S, Fontaine C, Stadnik T, Luypaert R, Bourgain C, De Greve J, De Mey J. UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium. 1005 How does ER/PR and Her2/Neu status affect the MR characteristics of invasive ductal carcinoma? Jansen SA, Abe H, Shimauchi A, Karczmar GS, Newstead GM. University of Chicago, Chicago, IL. 1006 Breast density assessment using magnetic tesonance imaging and diffuse optical spectroscopy. Klifa CS, Shah NS, Watkins M, Li A, Hattangadi J, Tromberg B, Hylton N. University of California, San Francisco, CA; University of California, Irvine, CA. 1007 MR imaging of tumor response in breast cancer patients following neoadjuvant chemotherapy: correlated with pathological findings. Chen J-H, Agrawal G, Yu H, Carpenter P, Mehta R, Nalcioglu O, Su M-Y. University of California Irvine, Irvine, CA. 1008 The utility of MRI in preoperative planning for breastconserving therapy. Kaufman G, Guth AA, Singh B, Axelrod D, Moy L. NYU School of Medicine, New York, NY. 1009 Does MRI improve chances of obtaining negative surgical margins after localized excision? A retrospective study. Kulkarni K, Newstead GM, Jansen SA, Abe H, Shimauchi A, Schmidt RA, Jaskowiak N. University of Chicago, Chicago, IL. 1010 The role of breast MRI in the preoperative evaluation of patients with newly diagnosed breast cancer. Schell AM, Kaufman PA, Lewis PJ. Dartmouth-Hitchcock Medical Center, Lebanon, NH. 1011 Comparative accuracy of MRI and ultrasound for predicting breast cancer extent after neoadjuvant chemotherapy. Karuna ST, Wechter DG. Virginia Mason Medical Center, Seattle, WA. 1012 Accuracy of preoperative evaluation of the axilla with MRI in breast cancer. Kaufman G, Guth AA, Axelrod D, Moy L. NYU School of Medicine, New York, NY. 1013 Model selection for analysis of dynamic contrast enhanced MRI (DCE-MRI) data. Yankeelov T, Welch EB, Chakravarthy B, Lee R, Freehardt D, Mayer I, Meszoely I, Kelley M, Means-Powell J, Gore J. Vanderbilt University, Nashville, TN; Philips Medical Systems, Cleveland, OH. 1026 1027 Effects of the steroidal aromatase inhibitor exemestane on mammographic breast density and other end-organ functions. Cigler T, Fabian CF, Yaffe MJ, Johnston D, Ingle JN, Nassif E, Brunner R, Wadden N, Pater JL, Richardson H, Tu D, Shangle Q, Goss PE. Massachusetts General Hospital, Boston, MA; Sunnybrook Health Sciences Centre, Toronto, ON, Canada; Kansas University Medical Center, Kansas City, KS; Mayo Clinic, Rochester, MN; Notre Dame Hospital, Montreal, QC, Canada; University of Nevada School of Medicine, Reno, NV; Memorial University of Newfoundland, St. John’s, NL, Canada; National Cancer Institute of Canada Clinical Trials Group, Kingston, ON, Canada; (NCIC CTG) MAP.2. Influence of bilateral breast magnetic resonance imaging in treatment planning for patients with stage I/II breast cancer. Figueredo ND, Carruthers CL, Frazier TG. Lankenau Hospital, Wynnewood, PA; Comprehensive Breast Center, Bryn Mawr Hospital, Bryn Mawr, PA. 1028 Follow-up rather than excision for benign papillary lesions of the breast. Copit DS, Vaidynathan S, Chaudhri Y. Albert Einstein Medical Center, Philadelphia, PA. 1029 Using three-parameter empirical mathematical model to analyze breast DCEMRI data; comparison with conventional BI-RADS classification. Fan X, Arkani S, Karczmar GS, Abe H, Schmidt RA, Newstead GM. University of Chicago, Chicago, IL. 1030 A double-blind randomized controlled trial of paracetamol as a pre-medication for mammography. Freitas-Junior R, Nascente CM, Carvalho AA, Ximenes C, Silva MF, Leite Filho AR, Freitas PF. Goias Federal University, Goiania, GO, Brazil. 1032 Accuracy of clinical evaluation of locally advanced breast cancer in patients receiving neoadjuvant chemotherapy. Prati R, Minami CA, Gornbein JA, DeBruhl N, Chung D, Chang HR. University of California, Los Angeles, CA. 1033 Breast specific gamma imaging and managment of breast cancer. Stern L, Rosenberg AL, Brill KL. Methodist Hospital, Philadelphia, PA; Jefferson Medical College, Kimmel Cancer Center, Philadelphia, PA. 1038 Concordance of contralateral breast cancer for steroid receptor and tumour characteristics. Absar MS, Martin C, Howe M, Zeiton A, Cramer A, Morris J, Bundred NJ. University Hospital of South Manchester, Manchester, United Kingdom. 1039 Breast cancer in the elderly: benefits of screening mammography in the diagnosis. Hines NL, Leibman AJ. Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY. 1040 Utility of echocardiographic screening for late-onset cardiomyopathy in breast cancer survivors treated with cardiotoxic chemotherapy. Wazir S, Budd GT, Moore HCF, LeGrand S, Andresen S, Tang WH. Cleveland Clinic, Cleveland, OH. Prognosis and Response Predictions: Prognostic Factors I 1041-1074 1041 Does HER-2 status influence locoregional failure rates after mastectomy in patients with pT1-3pN0 early stage breast cancer? Kwan W, Al-Tourah AJ, Speers C, Kennecke H, Norris B, Olivotto I. BC Cancer Agency, Fraser Valley Centre, Surrey, BC, Canada; BC Cancer Agency, Vancouver Centre, Vancouver, BC, Canada; BC Cancer Agency, Vancouver Island Centre, Victoria, BC, Canada. 1042 Elevated JAG1 mRNA expression, associated with the basal phenotype, is a poor-prognosis indicator in lymph nodenegative breast cancer. Reedijk M, Dickson BC, Pinnaduwage D, Mulligan AM, Zhang H, Bull SB, O’Malley F, Egan SE, Andrulis IL. University Health Network, Toronto, ON, Canada; Mount Sinai Hospital, Toronto, ON, Canada; Hospital for Sick Children, The Toronto Medical Discovery Tower, Toronto, ON, Canada. 1043 Recurrence score by oncotype DX evaluated on the primary breast tumor predicts the 2-year survival after first relapse. Bianchini G, Zambetti M, Mariani P, Moliterni A, Bianchi G, Mariani G, Fasolo A, Carcangiu ML, Valagussa P, Gianni L. Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy. 1044 Intracystic papillary carcinoma: a review of 917 cases. Grabowski JE, Saltzstein SL, Sadler GR, Blair SL. UCSD, San Diego, CA; UCSD, La Jolla, CA. 1045 Short term prognostic index for breast cancer: NPI or Lpi. Decock J, Hendrickx W, Van Belle V, Brouckaert O, Pintens S, Van Huffel S, Paridaens R, Amant F, Leunen K, Smeets A, Berteloot P, Van Limbergen E, Weltens C, Van den Bogaert W, Vanden Bempt I, Drijkoningen M, Wildiers H, Vergote I, Christiaens M-R, Neven P. UZ Leuven, Leuven, Belgium. 1046 The microstaging of sentinel lymph node biopsies is not associated with disease-free survival in breast cancer. Pugliese MS, Arthurs ZM, Tickman RJ, Allison KH, Beatty JD. Swedish Cancer Institute, Seattle, WA. 1047 Meta-analysis of gene-expression profiles in breast cancer: towards a unified understanding of breast cancer sub-typing and prognosis signatures. Sotiriou C, Wirapati P, Kunkel S, Farmer P, Pradervand S, Haibe-Kains B, Desmedt C, Sengstag T, Schütz F, Goldstein DR, Delorenzi M, Piccart M. Institute Jules Bordet, Brussels, Belgium; Université Libre de Bruxelles, Brussels, Belgium; University of Lausanne, Lausanne, Switzerland. 1048 The presence of a fibrotic focus and expansive growth pattern in breast tumors is associated with gene expression profiles of aggressive tumor biology. Van den Eynden GG, Smid M, Van Laere SJ, Colpaert CG, Van Marck EA, Dirix LY, Vermeulen PB, Foekens JA. (Lab Pathology University of Antwerp/University Hospital Antwerp, Wilrijk; Oncology Center, GH St.-Augustinus, Wilrijk, Belgium), Antwerp, Belgium; Erasmus MC-Daniel den Hoed, Rotterdam, Netherlands. Detection and Diagnosis: Screening 1034-1040 1034 The missing exam in clinical breast exam. Goodson III WH, Moore II DH. California Pacific Medical Center Research Institute, San Francisco, CA; University of California, San Francisco, CA. 1035 Comparing performance measures in opportunistic and organized screening mammography for early breast cancer detection. Hofvind S, Vacek P, Skelly J, Geller BM. The Cancer Registry of Norway, Oslo, Norway; University of Vermont, Burlington, VT. 1036 Cost-effectiveness of breast cancer (BC) screening with contrast enhanced magnetic resonance imaging (MRI) as an adjunct to x-ray mammography (XM) in high-risk women. Taneja C, Edelsberg J, Weycker D, Guo A, Oster G, Weinreb J. Policy Analysis Inc. (PAI), Brookline, MA; Bayer HealthCare Pharmaceuticals, Wayne, NJ; Yale University School of Medicine, New Haven, CT. 1037 High incidence of brain metastases found in patients with HER2 positive metastatic breast cancer. Should these patients be followed by regular MR scans? Langkjer ST, Krøldrup L, Kristiansen C, Enevoldsen K, Edal AL, Ormstrup TE. Vejle Hospital, Vejle, Denmark. 1049 An inflammatory breast carcinoma signature is associated with reduced relapse free survival in patients with noninflammatory breast cancer. Van Laere SJ, Van den Eynden GG, Van der Auwera I, van Dam P, Van Marck EA, Dirix LY, Vermeulen PB. Lab Pathology University Antwerp and Oncology Center, General Hospital SintAugustinus, Wilrijk, Antwerp, Belgium. 1050 Plasma and serum levels of tissue inhibitor of metalloproteinases-1 are associated with prognosis in nodenegative breast cancer – a prospective study. Würtz SØ, Møller S, Mouridsen H, Hertel PB, Friis E, Brünner N. University of Copenhagen, Frederiksberg, Denmark; Rigshospitalet, Copenhagen, Denmark. 1051 Non-proportional breast cancer mortality patterns according to expression of the HER2 protein, using the residual tissue repository of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. Anderson WF, Luo S, Chatterjee N, Rosenberg PS, Goodman MT, Hernandez BY, Reichman M, Dolled-Filhart MM, O’Regan RM, Perou CM, Jatoi I, Cartun RW, Sherman ME. National Cancer Institute, Rockville, MD; University of Hawaii, Honolulu, HI; Hartford Hospital, Hartford, CT; Emory University, Atlanta, GA; University of North Carolina, Chapel Hill, NC; HistoRx, New Haven, CT; National Naval Medical Center, Bethesda, MD. 1052 Withdrawn 1053 Patterns of metastatic spread in triple negative breast cancer. Dent R, Trudeau M, Sun P, Narod S. Sunnybrook Health Sciences Center, Toronto, ON, Canada; Women’s College Hospital, University of Toronto, Toronto, ON, Canada. 1060 The prognostic significance of human epidermal growth factor receptor-2 over-expression for the development of local recurrence after newly diagnosed breast cancer. Gabos Z, Thoms J, Hanson J, Ghosh S, Deschenes J, Mackey J, Abdulkarim B. Cross Cancer Institute, Edmonton, AB, Canada; University of Alberta, Edmonton, AB, Canada. 1061 Do grade I breast cancers require follow-up after breast conserving treatment? Hamed H, Jones G, Allen D, Kontos M. Guy’s Hospital, London, United Kingdom. 1062 Prognostic factors for BRCA1/2-associated familial breast cancer from Russian population. Lyubchenko LN, Pospechova NI, Lushnikova AA, Portnoy SM, Bryuzgin VV, Karpukhin AV, Garkavtseva RPh. N.Blokhin Cancer Res., Center RAMS, Moscow, Russian Federation; Research Center for Medical Genetics, Moscow, Russian Federation. 1063 Restratification of the Nottingham prognostic index using carcinoembroinic antigen cell adhesion molecule 6. Maraqa L, Cummings M, Peter MB, Hanby AM, Shaaban AM, Horgan K, Speirs V. St James’s University Hospital, Leeds, West Yorkshire, United Kingdom; Leeds General Infirmary, Leeds, West Yorkshire, United Kingdom. 1064 The Amsterdam 70-gene signature predicts outcome in breast cancer patients with 1-3 positive axillary lymph nodes. Mook S, Rutgers EJT, Peterse JL, Nuyten DSA, Horlings H, van de Vijver MJ, van ‘t Veer LJ. Netherlands Cancer Institute, Amsterdam, Netherlands. 1065 Quantitative justification of the change from 10% to 30% for HER-2 scoring in the ASCO-CAP guidelines: tumor heterogeneity in breast cancer and its prognostic and predictive implications. Moeder CB, Giltnane JM, Harigopal M, Molinaro A, Robinson A, Gelmon K, Huntsman D, Camp RL, Rimm DL. Yale University School of Medicine, New Haven, CT; British Columbia Cancer Agency, Vancouver, BC, Canada. 1054 E-cadherin levels may predeict outcome in inflammatory breast cancer (IBC). Levine PH, Ganesan C, Young HA, Portera C, Yang S, Swain SM. The George Washington University Medical Center, Washington, DC; National Cancer Institute, Bethesda, MD; Washington Hospital Center, Washington, DC. 1055 Impact of hormone replacement therapy on breast cancer: Women’s Healthy Eating and Living (WHEL) study experience. Parker BA, Flatt SW, Mortimer JA, Natarajan L, Gold EB, Bardwell WA, Jones LA, Hollenbach KA, Pierce JP. University of California, La Jolla, CA; University of California, Davis, CA; The University of Texas, Houston, TX. 1066 HER2 status adds prognostic, but not tamoxifen treatment predictive, information in hormone receptor positive premenopausal primary breast cancer. Rydén L, Fernö M, Stål O, Landberg G, Bendahl P-O. Clinical Science, Lund, Sweden; Biomedicine and Surgery, Linköping, Sweden; Laboratory Medicine, Malmö University Hospital, Malmö, Sweden. 1056 Survival outcomes in pregnancy-associated breast cancer. Ali A, Wang Y, Kelly J, Falk J, Sehgal R, Vogel V. University of Pittsburgh Medical Centre, Pittsburgh, PA; University of Pittsburgh, Pittsburgh, PA. 1067 1057 Clinicopathological and prognostic relevance of uptake level revealed by 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18FFDG PET/CT) in primary breast cancer. Ueda S, Tsuda H, Asakawa H, Omata J, Fukatsu K. National Defense Medical College, Tokorozawa, Saitama, Japan. Prospective prognostic value of proliferation in small, lowgrade, lymph-node negative breast cancers. Baak JPA, Van Diest PJ, Janssen EAM, Voorhorst F, and Other MMMCP Collaborators. Stavanger University Hospital, Stavanger, Norway; The Gade Institute, University of Bergen, Bergen, Norway; University Medical Center, Utrecht, Netherlands; Free University Medical Center, Amsterdam, Netherlands. 1068 Identification of IGFBP4 as a marker of tamoxifen failure in primary breast cancer. Hadad SM, Robertson KE, Baker L, Bray SE, Purdie CA, Jordan L, Vendrell JA, Cohen PA, Thompson AM. Ninewells Hospital and Medical School, Dundee, United Kingdom; Universite Lyon, Lyon, France. 1069 Genomic copy number alterations as predictive markers of systemic recurrence in breast cancer. Hwang K-T, Han W, Lee JW, Cho J, Ko E, Kim EK, Jung S-Y, Jeong E-M, Kang JJ, Yang S-J, Kim S-W, Noh D-Y. Seoul National University Boramae Hospital, Seoul, Republic of Korea; College of Medicine, Seoul National University, Seoul, Republic of Korea; Cancer Research Institute, College of Medicine, Seoul National University, Seoul, Republic of Korea; Macrogen, Inc., Seoul, Republic of Korea. 1058 1059 Prognostic differences of WHO-assessed mitotic activity index (MAI) and mitotic impression by quick scanning in invasive ductal breast cancer patients under 55 years of age. Skaland I, van Diest PJ, Janssen EAM, Gudlaugsson E, Søiland H, Baak JPA. Stavanger University Hospital, Stavanger, Norway; University Medical Center, Utrecht, Netherlands; University of Bergen, Bergen, Norway; Free University, Amsterdam, Netherlands. Complementary and alternative therapies among long-term breast cancer survivors. Carpenter CL, Ganz PA, Bernstein L. Keck School of Medicine at USC, Los Angeles, CA; David Geffen School of Medicine at UCLA, Los Angeles, CA. 1070 Prognostic value of the shed antigen of HER-2/neu in premenopausal breast cancer patients in the TABLE-study. Lueftner DI, Pechlivanis K, Geppert R, Possinger K. Charite Campus Mitte, Berlin, Germany. 1071 Down regulation of EFEMP1 is associated with unfavourable prognosis in sporadic breast cancer patients. Ramser J, Harbeck N, Sadr-Nabavi A, Naehrig J, Busch R, KiechleBahat M, Meindl A. Tech. University, Munich, Germany. 1072 Cell cycle proteins add independent prognostic information to Nottingham Prognostic Index (NPI). Loddo M, Kingsbury S, Sainsbury R. University College London, United Kingdom. 1073 The prognostic significance of androgen receptor expression in breast cancer. Peter M, Maraqa L, Horgan K, Speirs V, Shaaban A. University of Leeds, Leeds, W Yorks, United Kingdom; Leeds General Infirmary, Leeds, W Yorks, United Kingdom. 1074 Comparative analysis of uPA/PAI-1 in core biopsies versus surgical breast cancer samples. Vetter M, Lantzsch T, Abraha-Späth RS, Olenik C, Thomssen C, Dittmer J. Martin-Luther University, Halle/Saale, Germany; St. Elisabeth & St. Barbara Hospital, Halle/Saale, Germany; University Hospital Eppendorf, Hamburg, Germany; American Diagnostica GmbH, Pfungstadt, Germany. Treatment: Chemotherapy – General 1075-1087 1075 Risk of dementia in older breast cancer survivors: a population-based cohort study of the effect of chemotherapy. Baxter NN, Durham SB, Phillips K-A, Virnig EA, Virnig BA. University of Toronto, Toronto, ON, Canada; University of Minnesota, Minneapolis, MN; Peter MacCallum Cancer Centre, Melbourne, Australia. 1076 Final results of the AGO breast cancer study group MAMMA-3 trial: first-line capecitabine + paclitaxel vs epirubicin + paclitaxel for high-risk metastatic breast cancer. Lück H-J, du Bois A, Schrader I, Huober J, Heilmann V, Fasching PA, Stähle A, Jackisch C, Marth C, Richter B, von Minckwitz G. HSK, Klinik für Gynäkologie und Gynäkologische Onkolgie, Wiesbaden, Germany; Henriettenstiftung, Frauenklinik, Hannover, Germany; Universitäts-Frauenklinik Tübingen, Tübingen, Germany; Universitäts-Frauenklinik and Poliklinik Ulm, Ulm, Germany; Universitätsklinikum Erlangen, Frauenklinik, Erlangen, Germany; St. Vincentius-Krankenhäuser, Frauenklinik, Karlsruhe, Germany; Klinik für Gynäkologie und Geburtshilfe Klinikum Offenbach, Offenbach, Germany; Universitätsklinik für Frauenheilkunde Innsbruck, Innsbruck, Austria; Elbland-Kliniken Meißen-Radebeul, Standort Radebeul, Frauenklinik, Radebeul, Germany; Zentrum Frauenheilkunde und Geburtshilfe, Frankfurt, Germany. 1077 Combined trastuzumab (HER)/docetaxel (TAX) versus sequential trastuzumab followed by docetaxel at progression as first line chemotherapy for Her2-positive metastatic breast cancer: preliminary results (multicenter BOOG-study; 2002-02). Hamberg P, Bontenbal M, Vernhout RM, Bos MM, Braun HJ, Erdkamp F, Stouthard JML, van Deijk GA, Schmitz PIM, Seynaeve C, Klijn JGM. Erasmus University Medical Center, Daniel den Hoed Cancer Center, Rotterdam, Netherlands; Reinier de Graaf Hospital, Delft, Netherlands; Vlietland Hospital, Vlaardingen, Netherlands; Maasland Hospital, Sittard, Netherlands; Haga Hospital, Den Haag, Netherlands; Medical Center Rijnmond-Zuid, Rotterdam, Netherlands; Erasmus University Medical Center, Rotterdam, Netherlands. 1078 Phase III study of gemcitabine plus docetaxel versus capecitabine plus docetaxel for anthracycline-pretreated metastatic breast cancer patients: survival results. Chan S, Romieu G, Huober J, Tubiana-Hulin M, Schneeweiss A, Lluch A, Llombart A, du Bois A, Carrasco E, Thareau Vaury A, Fumoleau P. Nottingham City Hospital, Nottingham, United Kingdom; CRLC Val d’Aurelle, Montpellier Cedex 5, France; University of Tuebingen, Tuebingen, Germany; Centre Rene Huguenin, Saint Cloud, France; University of Heidelberg, Heidelberg, Germany; Hospital Clinico de Valencia, Valencia, Spain; Hospital Arnau de Villanova, Lerida, Spain; Dr. HorstSchmidt-Klinik, Wiesbaden, Germany; Eli Lilly Spain, Madrid, Spain; Eli Lilly France, Suresnes Cedex, France; Centre GeorgesFrancois Leclerc, Dijon, France. 1079 Analysis of chemotherapy-induced amenorrhea by three different chemotherapy regimens in premenopausal women with early breast cancer. Han HS, Lee KS, Kim SY, Ro J. National Cancer Center, Goyang-si, Korea. 1080 A descriptive study of pharmacokinetic alterations of epirubicin as a function of body size. Madarnas Y, Clemons M, Walker S, McLean H, Nakatsu K, Sawka C. Queen’s University; University of Toronto; Cancer Centre of Southeastern Ontario; Toronto-Sunnybrook Regional Cancer Centre; Princess Margaret Hospital. 1081 A multicenter, randomized, double-blind, parallelgroup phase II study of gefitinib (IRESSA) or placebo in combination with docetaxel, as first-line treatment in patients with metastatic breast cancer. Tubiana-Hulin M, Spielmann M, Dieras V, Fumoleau P, Delaloge S, Mefti F, Girre V. Centre Rene Huguenin, Saint Cloud, France; Institut Gustave Roussy, Villejuif, France; Institut Curie, Paris, France; Centre G.F. Leclerc, Dijon, France. 1082 Vinflunine in combination with trastuzumab: an active combination in the treatment of HER2 positive metastatic breast cancer. Paridaens R, Wildiers H, Dalenc F, Rixe O, Roche H, Cadic V, Delgado F-M. UZ Gasthuisberg, Leuven, Belgium; Institut Claudius Regaud, Toulouse, France; Hopital Pitie-Salpetriere, Paris, France; Institut de Recherche Pierre Fabre, Boulogne-Billancourt, France. 1083 A phase III study on the efficacy and safety of docetaxel, every three weeks or as a weekly regimen in patients with metastatic breast cancer. Willemse PH, Munck L, Creemers GJ, Graaf H, Smit W, Erjavec Z, Stouthard JM, Deijk G, Bochove A, Vader W, Westermann AM. UMC, Groningen, Netherlands; Comprehensive Cancer Centre North-Netherlands, Groningen, Netherlands; Catharina Ziekenhuis, Eindhoven, Brabant, Netherlands; MCL Zuid, Leeuwarden, Friesland, Netherlands; Medisch Spectrum Twente, Enschede, Overijssel, Netherlands; Delfzigt Ziekenhuis, Delfzijl, Groningen, Netherlands; MCR-Zuid, Rotterdam, Zuid-Holland, Netherlands; HAGA Ziekenhuis-Rode Kruis, Den Haag, ZuidHolland, Netherlands; ZaansMC, Zaandam, Noord-Holland, Netherlands; Sanofi-Aventis, Gouda, Zuid-Holland, Netherlands; AMC, Amsterdam, Noord-Holland, Netherlands. 1084 Benchmarking quality oncology care in the community setting. Schwartzberg LS, Tauer K, Blakely J, Johnson R, Reed J, Somer B, Wheeler B, Walker MS, Stepanski EJ, Fortner BV. The West Clinic, Memphis, TN; Accelerated Community Oncology Research Network, Memphis, TN. 1085 Age and prognosis – how did adjuvant therapies influence the real prognosis? Morishita M, Thomas G, Leonard R. South West Wales Cancer Institute, Swansea, United Kingdom; Velindre Hospital, Cardiff, United Kingdom; Imperial College School of Medicine, London, United Kingdom. 1086 Dexamethasone, metoclopropamide and omperazole combination is simple, safe and effective for delayed nausea and vomiting control in adjuvant chemotheray for early breast cancer. Sanchetee SC. Sanchetee Hospital and Cancer Insitute, Jodhpur, Rajasthan, India. 1087 N0332 phase II trial of weekly irinotecan and docetaxel in refractory metastatic breast cancer: a North Central Cancer Treatment Group trial. Tan WW, Hillman D, Salim M, Northfelt DW, Anderseon DM, Stella PJ, Niedringhaus R, Bernath AM, Gamini SS, Frances P, Perez PA. Mayo Clinic, Jacksonville, FL; Mayo Clinic, Rochester, MN; Allan Blair Cancer Center, Saskatchewan, Canada; Mayo Clinic Scottsdale, Scottsdale, AZ; Abbott Northwestern Hospital, Minneapolis, MN; Michigan Cancer Research Consortium, Ann Arbor, MI; Duluth CCOP, Duluth, MN; Geisinger Clinic & Medical Center, Danville, PA; Missouri Valley Cancer Consortium, Omaha, NE. 1093 Predictors of weight gain in patients with early stage breast cancer. Mills JB, Gui J, Mulrooney TJ, Schwartz GN. DartmouthHitchcock Medical Center, Lebanon, NH; Dartmouth Medical School, Hanover, NH. 1094 Memory loss after adjuvant chemotherapy for breast cancer: a preliminary analysis of mediating variables utilizing crosssectional correlations and multilevel longitudinal analysis. Beadle G, Rolfe M, Vearncombe K, Andrew B, Mengersen K, Wright M. Queensland Institute of Medical Research, Brisbane, Queensland, Australia; Southern Cross University, Lismore, New South Wales, Australia; University of Queensland, Brisbane, Queensland, Australia; Queensland University of Technology, Brisbane, Queensland, Australia. 1095 Research on optimal recovery practices in breast cancer: the RESTORE trial. Kimmick GG, McCoy TP, Milhalko SL, Ribisl PM, Anderson RT. Wake Forest University School of Medicine, Winston-Salem, NC; Wake Forest University, Winston-Salem, NC; Duke University Medical Center, Durham, NC. 1096 Breaking bad news: experiences receiving breast cancer diagnosis in a specialty breast center versus community practice. Smith RL, Crawford BJ, Petersen LR, Johnson RE, Mandrekar J, Cha S, Rhodes DJ, Hartmann LC. Mayo Clinic, Rochester, MN. 1097 Appraisals, coping and distress among couples dealing with breast cancer. Hernandez AM, Bigatti SM. Indiana University Purdue University Indianapolis, Indianapolis, IN. 1098 The psychosocial issues for women diagnosed with breast cancer who have a concurrent pregnancy or want the option of a subsequent pregnancy. Ives A, Longman G, Saunders C, White K. The University of Western Australia, Perth, WA, Australia; University of Sydney, Sydney, NSW, Australia. 1099 Prevalence of cognitive complaints is not higher in postmenopausal breast cancer patients before adjuvant hormonal therapy compared to healthy controls. Schilder CM, van Dam F, Boogerd WS, Seynaeve C, van de Velde CJ, Nortier HW, Linn SC, Schagen SB. Netherlands Cancer Institute, Amsterdam; Erasmus Medical Center, Rotterdam; University Medical Center, Leiden, Netherlands. 1100 Unexpected effects of reassurance in women with low-risk breast cancer. Griggs JJ, Corbin K, Weiss M, Shields CG. University of Michigan, Ann Arbor, MI; University of Rochester School of Medicine and Dentistry, Rochester, NY; breastcancer.org, Narberth, PA. 1101 Breast reconstruction in a university-based public hospital. Levine SM, Vaksman A, Hiotis K, Levine JP. New York University Medical Center, New York, NY. Treatment: Chemotherapy – Support 1088-1090 1088 1089 1090 Reduced incidence of febrile neutropenia and related complications in elderly breast cancer patients receiving chemotherapy with pegfilgrastim primary prophylaxis versus current practice neutropenia management – results from an integrated analysis. Aapro M, Schwenkglenks M, Lyman G, Lopez Pousa A, Easton V, Skacel T, Bacon P, Von Minckwitz G. Clinique de Genolier, Genolier, Switzerland; University of Basel, Basel, Switzerland; University of Rochester, Rochester; Hospital Sant Pau, Barcelona, Spain; Amgen Ltd, Cambridge, United Kingdom; Amgen (Europe) GmbH, Zug, Switzerland; University of Frankfurt, Frankfurt, Germany. Pegfilgrastim promotes neutrophil recovery in elderly breast cancer patients following anthracycline-containing chemotherapy. Brugger W, Bacon P, Lawrinson S, Romieu G. Schwarzwald-Baar Clinic, University of Freiburg, Villingen-Schwenningen, Germany; Amgen (Europe) GmbH, Zug, Switzerland; Amgen Ltd, Uxbridge, United Kingdom; CRLC Val d’Aurelle, Montpellier, France. Pre-treatment differential white blood cell counts can be used to identify patients who are at increased risk of severe myelosuppression following adjuvant chemotherapy. Jenkins P, Benstead K, Owen R, Elyan S, Ingledew I, Bristol J, Chan C, Freeman S. Cheltenham General Hospital, Cheltenham, Gloucestershire, United Kingdom; University of Birmingham, Birmingham, Edgbaston, United Kingdom. Treatment: Psychosocial Aspects 1091-1101 Tumor Cell Biology: Angiogenesis 1102-1109 1091 Quality of life in the Intergroup Exemestane Study (IES) 5 years post-randomisation. Fallowfield LJ, Langridge CI, Kilburn LS, Jones SE, Snowdon CF, Bliss JM, Coombes C. Brighton & Sussex Medical School, Falmer, United Kingdom; Institute of Cancer Research, Sutton, United Kingdom; US Oncology Research, TX; Imperial College London, United Kingdom; on behalf of the IES Group. 1102 Anti-tumor activity of motesanib diphosphate alone and in combination with docetaxel or tamoxifen in xenograft models of human breast carcinoma. Coxon A, Bush T, Belmontes B, Saffran D, Ona V, Rex K, Caenepeel S, Hughes P, Kaufman S, Radinsky R, Kendall R, Price J, Polverino A. Amgen Inc, Thousand Oaks, CA; UT MD Anderson Cancer Center, Houston, TX. 1092 Prospective multi-center study of the impact of the 21-gene recurrence score assay on patient satisfaction, anxiety and decisional conflict for adjuvant breast cancer treatment selection. Mumby PB, Lo SS, Norton J, Smerage J, Joseph K, Chew HK, Hayes D, Albain KS. Loyola University Medical Center, Maywood, IL; University of Michigan, Ann Arbor, MI; Edward Hospital, Naperville, IL; University of California, Sacramento, CA. 1103 Non-invasive in vivo subcellular multicolor imaging of the tumor microenvironment and drug response in real time. Yang M, Jiang P, Al-Zaid M, Hoffman RM. AntiCancer, Inc., San Diego, CA; University of California, San Diego, CA. 1104 Anti-angiogenic potential of coenzyme Q10, riboflavin and niacin in breast cancer patients undergoing tamoxifen therapy. Panchanatham S. DR. A.L.M.P-G.I.B.M.S., University of Madras, Tarmani Campus, Chennai, Tamilnadu, India. 1105 Molecular imaging in the mouse model of breast cancer based on optical illumination and ultrasonic detection. Oraevsky AA, Ermilov SA, Eghtedari MA, Conjusteau A, Miller T, Radulescu EG, Herzog D, Gharieb RR, Lacewell R, Thompson S, Mehta K, Stein A, Motamedi M. Fairway Medical Technologies, Houston, TX; Seno Medical Instruments, Houston, TX; University of Texas Medical Branch, Galveston, TX. 1116 Combination therapy with tetramethoxystilbene and phosphatidylinositol 3-kinase inhibitor is effective for killing hormone-resistant breast cancer. Park H, Aiyar SE, Kim S, Lee Y, Fan P, Santen RJ. Kyungpook National University Hospital, Daegu, Republic of Korea; University of Virginia, Charlottesville, VA; Seoul National University, Seoul, Republic of Korea. 1106 Variation of circulating angiogenic factor level and its potential value during chemotherapy in patients with metastatic breast cancer. Tang J, Zhao J, Qin J, Pan L, Xu Z. Jiangsu Tumor Hospital, Nanjing, Jiangsu, China; Nanjing University of Traditional Chinese Medicine, Nanjing, Jiangsu, China. 1117 Inhibition of breast cancer growth with the combination of lapatinib and an ADAM protease inhibitor. Witters LM, Scherle PA, Friedman SM, Redman J, Fridman JS, Caulder E, Lipton A. Pennsylvania State University College of Medicine, Hershey, PA; Incyte Corporation, Wilmington, DE. 1118 1107 Association of genetic polymorphisms of VEGF and VEGFR-2 with outcome in E2100. Schneider B, Wang M, Radovich M, Sledge G, Badve S, Thor A, Flockhart D, Hancock B, Davidson N, Miller K. Indiana University School of Medicine, Indianapolis, IN; Harvard, Boston, MA; University of Colorado Health Sciences Center, Denver, CO; Johns Hopkins Sidney Kimmel Cancer Center, Baltimore, MD. uPAR gene amplification in breast cancer tissue: a rare event. Pintens S, Vanden Bempt I, Drijkoningen M, Van Belle V, Brouckaert O, Christiaens M-R, Neven P, Peeters C. UZ Leuven, Leuven, Belgium; ESAT KULeuven, Leuven, Belgium. 1119 Targeting of mTOR is associated with decreased VEGF expression and secretion in cancer cells. Lackner EM, Krauth MT, Kondo R, Rebuzzi L, Eigenberger K, Vales A, Kornek GV, Zielinski CC, Valent P. Medical University Vienna, Internal Medicine I, Division of Oncology, Vienna, Austria; Medical University Vienna, Internal Medicine I, Division of Hematology and Hemostaseology, Vienna, Austria; Clinic for Int. Medicine and Infectious Disease, Vienna, Austria; Hanusch Krankenhaus, Vienna, Austria. 1108 A novel assay to assess the antiangiogenic potential of cytotoxic drugs in human breast cancer. Lyons, III JM, Anthony CT, Woltering EA. Louisiana State University Health Science Center, New Orleans, LA. 1109 Comparing serum levels of vascular endothelial growth factor in premenopausic women with breast cancer according to menstrual cycle phase. Rios Zaragoza S, Martinez Chequer J, Mainero Ratchelous F. Hospital “Luis Castelazo Ayala” IMSS, Mexico, DF, Mexico. 7:00-10:00 Tumor Cell Biology: Antigens and Markers 1110-1112 1110 Labeling pattern of breast cancer stem phenotype in invasive breast carcinomas: an immunohistochemical analysis. Shaye AN, Sahin AA, Huo L, Woodward WA. UT M.D. Anderson Cancer Center, Houston, TX. 1112 Differential proteomic profiles observed in FFPE breast tissue specimens of several pathologic states. Izbicka E, Streeper R, West FB, Yeh I-T. CTRC, San Antonio, TX; UTHSCSA, San Antonio, TX. Tumor Cell Biology: Growth Factors / Inhibitors 1113-1119 1113 1114 1115 Susan G. Komen for the Cure proudly presents the 2007 Brinker Awards for Scientific Distinction featuring special guest and keynote speaker Ambassador Nancy G. Brinker. Nuclear FoxO3a expression is associated with lymph node negative, ER+ invasive ductal carcinomas. Turashvili G, Fridman E, Romanska H, Lam E, Skarda J, Murray P, Kolar Z, Lalani E-N. Institute of Pathology, University Olomouc, Palacky, Czech Republic; Tel Aviv University, Chaim Sheba Medical Center and Sackler School of Medicine, Tel Aviv, Israel; Division of Cancer Studies, University of Birmingham, Birmingham, United Kingdom; Imperial College, London, United Kingdom. 1111 Insulin-like growth factor I activates gene transcription programs strongly associated with ER – breast cancer and poor patient prognosis. Creighton CJ, Casa A, Lazard ZW, Tsimelzon A, Hilsenbeck SG, Lee AV. Baylor College of Medicine, Houston, TX. HER-1 overexpression is found only in oestrogen receptor negative breast cancer and is rarely associated with HER-1 gene amplification. Pintens S, Vanden Bempt I, Drijkoningen M, Van Belle V, Brouckaert O, Christiaens M-R, Neven P, De Wolf-Peeters C. UZ Leuven, Leuven, Belgium; ESAT, Leuven, Belgium. Effectiveness of RAD001 (everolimus) in combination with endocrine therapy varies with cell phenotype. Farmer I, Pancholi S, Thornhill A, Evans DB, Lane HA, Dowsett M, Martin L-A. Institute of Cancer Research, London, United Kingdom; Novartis Institute for BioMedical Research-Basel, Basel, Switzerland. SUSAN G. KOMEN FOR THE CURE BRINKER AWARDS FOR SCIENTIFIC DISTINCTION DINNER - Henry B. Gonzalez Convention Center Ballroom C “Towards a Culture of Discovery: Progress and Passion in the Search for the Cures” will be an evening to remember as we celebrate Susan G. Komen for the Cure’s 25th anniversary, congratulate the 2007 Brinker Award Recipients, Joe W. Gray, PhD and Leslie Bernstein, PhD and honor the great achievements of our past Brinker Laureates – Henry B. Gonzalez Convention Center – Ballroom C. Please purchase your tickets to the 2007 Brinker Dinner when registering at www.sabcs.org. You may also purchase your tickets onsite at the Susan G. Komen for the Cure booth. Tickets will be awarded on a first-come, first-served basis. If you have additional questions, please contact sdeland@komen. org. Friday, December 7:00-9:00 POSTER DISCUSSION 2 & CONTINENTAL BREAKFAST – Ballroom B Metastasis 201-210 201 A unique model of estrogen receptor (ER) Ĝ-positive breast cancer metastasis. Fuqua SA, Beyer A, Selever J, Hilsenbeck SG, Tsimelzon A, Cui Y. Baylor College of Medicine, Houston, TX. 202 Primary tumor heterogeneity and sentinel lymph node metastases: understanding molecular processes of breast cancer metastasis. Ellsworth DL, Ellsworth RE, Patney HL, Becker TE, Deyarmin B, Jordan RM, Hooke JA, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 203 Identification of genetic predisposition to development of lymph node metastasis in breast cancer patients. Callaghan KA, Weyandt JD, Ellsworth RE, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 204 Identification of new candidate breast cancer metastasis genes. Geradts J, Desouki MM, Liao S. Duke University Medical Center, Durham, NC; Medical University of South Carolina, Charleston, SC. 205 ALDH1 positive stem cells in inflammatory breast cancer mediate metastasis and are associated with a poor clinical outcome. Charafe-Jauffret E, Ginestier C, Tarpin C, Iovino F, Esterni B, Jacquemier J, Xerri L, Merajver S, Dontu G, Birnbaum D, Wicha M, Viens P. Institut Paoli-Calmettes, Marseille, France; Comprehensive Cancer Center, University of Michigan Medical Center, Ann Arbor, MI. 206 Programmed cell death 4, a novel inhibitor of breast cancer invasion. Nieves-Alicea R, Simeone AM, Colburn NH, Tari AM. The University of Texas M.D. Anderson Cancer Center, Houston, TX; National Cancer Institute, Frederick, MD. 207 TROP2 is a novel, major determinant in breast cancer growth and metastatization. Alberti S, Trerotola M, Vacca G, Zappacosta R, Rossi C, Guerra E, Bonasera V, Lasorda R, Lattanzio R, Piantelli M. Foundation University of Chieti, Chieti Scalo, Chieti, Italy. 208 Osteoblasts and their progenitors stimulate breast cancer cell migration through chemokine secretion. Molloy AP, Dwyer RM, Kerin MJ. National University of Ireland, Galway, Ireland. 209 Significance of PELP1/MNAR-mediated ER-nongenotropic actions in cytoskeleton signaling. Chakravarty D, Chandrasekharan Nair B, Rajhans R, Cortez V, Nair SS, Tekmal RR, deGraffenried LA, Sun LZ, Vadlamudi RK. UTHSCSA, San Antonio, TX. 210 2003 17ß-hydroxysteroid dehydrogenase type 1 is a predictive factor in premenopausal hormone receptor positive breast cancer treated with tamoxifen. Kallstrom A-C, Salme R, Ryden L, Gunnarsson C, Nordenskjold B, Stal O. Helsingborg Hospital, Helsingborg, Sweden; University Hospital, Linkoping, Sweden; University Hospital, Lund, Sweden. 2004 A high ratio of 17HSD1/17HSD2 protein expression predicts the outcome of tamoxifen treatment in postmenopausal breast cancer. Jansson A, Gunnarsson C, Persson L, Fornander T, Skoog L, Nordenskjöld B, Stål O. Linköping University, Linköping, Sweden; Karolinska University Hospital, Stockholm, Sweden. 2005 TOP2A gene amplification and response to adriamycin based therapy. Tubbs R, Barlow W, Budd GT, Swain E, Porter P, Yeh I-T, Sledge G, Shapiro C, Ingle J, Haskell C, Albain K, Livingston R, Hayes D. Cleveland Clinic, Cleveland, OH; Fred Hutchinson Cancer Research Center, Seattle, WA; University of Texas Health Science Center at San Antonio, San Antonio, TX; Indiana University Medical Center, Indianapolis, IN; Arthur James Cancer Center Hospital, Columbus, OH; Mayo Clinic, Rochester, MN; UCLA Medical Center, Santa Monica, CA; Loyola University Medical Center, Maywood, IL; Arizona Cancer Center, Tucson, AZ; University of Michigan Medical Center, Ann Arbor, MI. 2006 Double staining chromogenic in situ hybridization is a useful alternative to fluorescent in situ hybridization: first comparative study of HER2 and TOP2A gene amplification in breast cancer. Lacroix-Triki M, Mounie E, Charafe-Jauffret E, Jacquemier J. Institut Claudius Regaud, Toulouse, France; Institut PaoliCalmettes, Marseille, France. 2007 Quantitative measurements of HER2 expression and HER2:HER2 dimerization identify subgroups of HER2 positive metastatic breast cancer patients with different probabilities of response to trastuzumab treatment. Huang W, Lipton A, Leitzel K, Ali SM, Fuchs EM, Weidler J, Chappey C, Sperinde J, Tan Y, Jin X, Paquet A, Winslow J, Petropoulos C, Kostler WJ, Bates M. Monogram Biosciences, Inc., So San Francisco, CA; Penn State/Hershey Medical Center, Hershey, PA; Medical University of Vienna, Vienna, Austria. 2008 Inter-observer interpretative reproducibility of HER2 genotyping of a consecutive series of primary breast carcinomas by Silver In Situ Hybridization (SISH). Tubbs R, Myles J, Papouchado B, Lloyd R, Oliveira A, McElhinny A, Vladich F, Pestic-Dragovich L, Downs-Kelly E, Prescott N, Pettay J, Loftus M, Roberts C, Grogan T, Roche P. Cleveland Clinic and the Cleveland Clinic Lerner College of Medicine, Cleveland, OH; Mayo Clinic, Rochester, MN; Ventana Medical Systems International, Tucson, AZ. 2009 HER2 tumors are heterogeneous, clinically, molecularly, and in response to preoperative trastuzumab: pathway analysis of gene expression profiles from three breast cancer datasets. Harris LN, Eklund AC, Carter S, Li X, Winer EP, Hilsenbeck S, Esteva FJ, Symmans WF, Pusztai L, Szallasi Z, Chang J. Yale University, New Haven, CT; Childrens Informatics Program, Boston, MA; Dana Farber Cancer Institute, Boston, MA; Baylor University, Houston, TX; MD Anderson Cancer Center, Houston, TX. 2010 Comparison of ERBB2 evaluation by immuno-histochemistry and a quantitative RT-PCR method in primary breast cancers. Giacchetti S, Lehmann-Che J, De Roquancourt A, Cuvier C, Hocini H, Bertheau P, De The H, Espié M, Turpin E. Hopital Saint-Louis, Assistance Publique-Hopitaux de Paris, Paris, France; Hopital Saint-Louis, APHP, Paris, France. Lapatinib prevents the metastatic colonization of EGFR+ and Her-2+ breast cancer cells in the brain. Palmieri D, Gril BM, Herring J, Vega-Valle E, Hua EK, Leiwehr D, Steinberg SM, Gilmer TM, Rubin SD, Steeg PS. National Cancer Institute, Bethesda, MD; SAIC-NCI, Fredrick, MD; GlaxoSmithKline, Collegeville, PA. 7:00-9:00 POSTER SESSION 2 & CONTINENTAL BREAKFAST - Exhibit Hall B (#2001-2121) Prognosis and Response Predictions: Predictive Factors I 2001-2026 2001 2002 Elevated serum TIMP-1/HER-2 predicts decreased response and survival in metastatic breast cancer. Lipton A, Leitzel K, Chaudri-Ross HA, Evans DB, Ali SM, Demers L, Hamer P, Brown-Shimer S, Pierce K, Guar V, Carney W. Penn State University/Hershey Medical Center, Hershey, PA; Novartis Pharma AG, Basel, Switzerland; Novartis Institutes for BioMedical Research Basel, Basel, Switzerland; Penn State/Hershey Medical Center; Lebanon VAMC, Lebanon, PA; Oncogene Science Biomarker Group/Siemens Medical Solutions Diagnostics, Cambridge, MA. Plasminogen activator inhibitor-1 and tissue inhibitor of metalloproteinases-1 are additive in predicting response to chemotherapy in metastatic breast cancer. Schrohl Rasmussen A-S, Meijer-van Gelder ME, Holten-Andersen MN, Christensen IJ, Look MP, Mouridsen HT, Foekens JA, Brünner N. University of Copenhagen, Faculty of Life Sciences, Copenhagen, Denmark; Erasmus MC, Josephine Nefkens Institute, Rotterdam, Netherlands; Hvidovre Hospital, Hvidovre, Denmark; Rigshospitalet, Copenhagen, Denmark. 2011 Development of novel proximity-based immunoassays for the detection of HER heterodimerization in breast cancer cell line lysates and formalin-fixed, paraffin-embedded tissue. Eli* L, Shi* Y, Dao-Pick T, Bose J, Frankson K, Penuel E, Weston J, Pidaprthi S, Mukherjee A, Nguyen X-T, Williams S, Goodman L, Winslow J. Monogram Biosciences, South San Francisco, CA. 2019 Adding the estimation of cyclin D1 gene amplification to the standard panel of predictors in breast carcinoma can significantly improve identification of tumors resistant to tamoxifen. Petrakova K, Nenutil R, Vyskocil J, Fabian P, Palacova M, Hanzelkova Z, Knoflickova D. Masaryk Memorial Cancer Institute, Brno, Czech Republic. 2012 Characterization of a novel proximity immunoassay for the quantitative determination of HER2 protein expression and HER2 homodimerization in formalin-fixed, paraffinembedded breast cancer tissue. Winslow J, Shi Y, Tan Y, Jin X, Dua R, Penuel E, Mukherjee A, Sperinde J, Pannu H, Chenna A, DeFazio-Eli L, Pidiparthi S, Chen L, Williams S, Larson J, Goodman L, Whitcomb J, Petropoulos C, Huang W. Monogram Biosciences, Inc., South San Francisco, CA. 2020 Single agent in vitro drug sensitivity of molecular breast cancer subtypes defined by gene expression analysis. Brase J, Schmidt M, Hengstler J, von Törne C, Kölbl H, Gehrmann M. University of Luebeck, Luebeck, Germany; University of Mainz, Mainz, Germany; University of Dortmund, Dortmund, Germany. 2021 Tumour volume analysis. A better way than RECIST? Gordon AB, Stebbing J, Coombes C. Charing Cross Hospital, London, United Kingdom. 2022 Association of an extracellular matrix gene cluster with breast cancer prognosis and response to tamoxifen. Helleman J, Jansen MPHM, Sieuwerts AM, van Staveren IL, Ritstier K, Look MP, Meijer-van Gelder ME, Klijn JGM, Foekens JA, Berns EMJJ. Erasmus MC, Rotterdam, Netherlands. 2023 Increased b1 integrin expression is a predictor of trastuzumab resistance in HER-2 overexpressing metastatic breast cancer patients. Thoms J, Sabri S, Lesniak D, Lai R, Deschennes J, Mackey J, Murray D, Abdulkarim B. University of Alberta, Edmonton, AB, Canada. 2024 Preliminary results from I-SPY trial: tumor patterns on pre-treatment MRI predict breast conservation therapy eligibility. Gomez R, Hylton N, Madhavan S, Leung E, Broadwater G, Herman B, Esserman L, ISPY Radiology, Clinical & Pathology Investigators. UCSF, San Francisco, CA; NCI, Bethesda, MD; CALGB, Durham, NC; ACRIN, Providence, RI. 2025 Molecular markers as predictors of breast cancer response to adjuvant epirubicin-CMF chemotherapy in the BR9601 trial. Bartlett JM, Munro AF, Cameron DA, Thomas J, Prescott R, Twelves C. University of Edinburgh, Edinburgh, United Kingdom; Western General Hospital, Edinburgh, United Kingdom; University of Bradford, Bradford, United Kingdom. 2026 Identification of molecular predictors of response of advanced breast cancer patients to aromatase inhibition. Haynes B, Ghazoui Z, Anderson H, Dunbier A, Dexter T, Mackay A, Smith IE, Dowsett M. Royal Marsden Hospital, London, United Kingdom; The Breakthrough Toby Robins Breast Cancer Research Centre, London, United Kingdom. 2013 HER2 and SPARC status in tumors play an important role in the relative effectiveness of nanoparticle albumin-bound (nab) paclitaxel versus polysorbate-based docetaxel. Desai N, Trieu V, Hwang L, Wu R, Hawkins M, Soon-Shiong P, Gradishar W. Abraxis BioScience, Inc., Los Angeles, CA; Northwestern University, Chicago, IL. 2014 HER2 immunohistochemistry: comparison of image analysis based interpretation of CB11 and 4B5 clones using reference fluorescence in-situ hybridization. Fine JL, Bhargava R, Surti U, Dabbs DJ. Magee-Womens Hospital of UPMC, Pittsburgh, PA. 2015 Expression of the microtubule-associated protein, tau, predicts improved survival, but not response, to a combination of docetaxel and vinorelbine in HER-2 negative metastatic breast cancer. Gralow JR, Barlow WE, Gown AM, Goldstein LC, Porter PL, Yeh I-T, Livingston RB, Hayes DF. University of Washington, Seattle, WA; Fred Hutchinson Cancer Research Center, Seattle, WA; Phenopath, Seattle, WA; UT San Antonio, San Antonio, TX; Arizona Cancer Center, Tucson, AZ; University of Michigan, Ann Arbor, MI. 2016 2017 2018 Microtubule-associated protein tau is a marker of pathological complete response in Her-2/neu positive neoadjuvant treated breast cancer patients. Rueckert S, Wirtz R, Lenhard M, Hasmueller S, Ditsch N, Ruehl I, Kahlert S, Bauerfeind I, Untch M. LMU, Universtity of Munich, Munich, Germany; Siemens Medical Solutions Diagnostics GmbH, Leverkusen, Germany; Helios Klinikum Berlin-Buch, Berlin, Germany. Cyclin-dependent kinase 2 to 1 specific activity ratio predicts response to epirubicin and paclitaxel in human breast cancer. Kim SJ, Miyoshi Y, Taguchi T, Tamaki Y, Noguchi S, Tsukamoto F, Akazawa K, Nakayama S, Matsushima T, Torikoshi Y, Ishihara H. Graduate School of Medicine, Osaka University, Suita, Osaka, Japan; Osaka Koseinenkin Hospital, Osaka, Japan; Sysmex Corporation, Kobe, Hyogo, Japan. High pretreatment cyclin E levels may define a higher risk subset of basal-like breast cancers: in depth immunohistochemical analysis and clinical outcome of neoadjuvantly treated basal-like breast cancers. Osborne CR, Tripathy D, Allada N, Bian A, Xie X-J, Ashfaq R. UT Southwestern Medical Center, Dallas, TX; Baylor University Medical Center, Dallas, TX. Risk and Prevention: Diet and Nutrition 2027-2031 2027 Diet, lifestyle, and BRCA-related breast cancer risk among French-Canadian. Ghadirian P, Nkondjock A, Robidoux A, Narod S. University of Montreal, Epidemiology Research Unit, Research Centre CHUM, Hôtel-Dieu, Montreal, QC, Canada; CHUM, Hôtel-Dieu, Montreal, QC, Canada; Women’s College Hospital - University of Toronto, Toronto, ON, Canada. 2028 Milk products are a source of dietary progesterone. Goodson III WH, Handagama P, Moore II DH, Dairkee S. California Pacific Medical Center Research Institute, San Francisco, CA. 2029 Cardioprotective effects of oral dietary glutamine in tumorbearing rats treated with doxorubicin. Todorova VK, Kaufmann Y, Klimberg VS. University of Arkansas for Medical Sciences, Little Rock, AR; Central Arkansas Veterans Healthcare System, Little Rock, AR. 2030 Effects of Korean red ginseng on the concentration of blood estrogen, leptin and urinary excretion of estrogen metabolites in postmenopausal women. Kang SH, Lee SJ, Baek NW, Kim EM. Yeungnam University Medical Center, Daegu, Korea. 2031 Breast cancer survivors who use selected herbal supplements have lower circulating estradiol and free estradiol: the Health, Eating, Activity and Lifestyle study. Wayne SJ, Koprowski C, Neuhouser ML, Ulrich CM, Bernstein L, Gilliland F, Wiggins C, Baumgartner K, Baumgartner R, McTiernan A, Ballard-Barbash R. University of New Mexico, Albuquerque, NM; University of Southern California, Los Angeles, CA; Fred Hutchinson Cancer Research Center, Seattle, WA; National Cancer Institute, Bethesda, MD. Risk and Prevention: Familial Breast Cancer / Genetic Testing 2032-2051 2032 2033 2034 Toward individualized risk prediction: the clinical benefit of risk reduction mastectomy and oophorectomy in BRCA carriers with breast cancer. Burke HB, Hoang A, Metcalfe K, Culver JO, MacDonald DJ, Grant M, Thornton A, Robson M, Narod S, Weitzel JN. George Washington University, Washington, DC; University of Toronto, Toronto, ON, Canada; Memorial Sloan Kettering CA Ctr, New York, NY; City of Hope, Duarte, CA. A BRCA1 or BRCA2 mutation and young age predict fast breast cancer growth. Implications for screening? Tilanus-Linthorst MM, Obdeijn I-M, Hop WC, Causer P, Leach MO, Warner E, Pointon L, Hill K, Klijn JG, Warren RM, Gilbert FJ. Erasmus University MC, Rotterdam, Netherlands; Sunnnybrook & Women’s Health Sciences Centre, Toronto, Canada; Institute of Cancer Research and Royal Marsden NHS, Sutton, Surrey, United Kingdom; Addenbrooke’s Hospital and University, Cambridge, United Kingdom; University of Aberdeen, Aberdeen, United Kingdom. Breast carcinoma in situ and the prevalence of BRCA1 and BRCA2 mutations in a large commercial database. Hall MJ, Reid JE, Noll WW, Frye CA, Burbidge LA, Wenstrup RJ. Herbert Irving Comprehensive Cancer Center, New York, NY; Myriad Genetic Laboratories, Inc., Salt Lake City, UT. 2035 Lifetime risk for breast and ovarian cancer in postmenopausal BRCA carriers: cause for concern? Tice JA, Crawford B, Ziegler J, McLennan J, Beattie M. UCSF, San Francisco, CA. 2036 BRCA1- and BRCA2-associated breast cancer is more sensitive to standard chemotherapy for metastatic disease in comparison with sporadic breast cancer. Kriege M, Seynaeve C, Meijers-Heijboer H, Collee M, MenkePluymers MBE, Bartels CCM, van den Ouweland A, van Geel B, Hooning M, Brekelmans CTM, Klijn JGM. ErasmusMC-Daniel den Hoed Cancer Center, Rotterdam, Netherlands. 2037 BRCA mutation in Chinese population: preliminary results from the Hong Kong hereditary and high risk breast cancer programme. Kwong A, Wong CLP, Ma E, Ford JM. The University of Hong Kong; Hong Kong Santorium and Hospital, Hong Kong; Stanford University, CA. 2038 The CHEK2*1100delC variant: present in the west of Ireland breast cancer population. Colleran GC, Rowan A, Miller N, Sawyer E, Curran C, Kerin M, Tomlinson I. National University of Ireland Galway, Galway, Ireland; London Research Institute, Cancer Research UK, London, England, United Kingdom. 2039 Addressing the needs of men in BRCA1/2 families. Daly MB. Fox Chase Cancer Center, Philadelphia, PA. 2040 Identification of a recurring BRCA1 mutation in Bahamian women with breast cancer. Donenberg T, Turnquest T, Lunn J, Curling D, Krill-Jackson E, Hurley J. University of Miami/Jackson Memorial Hospital, Miami, FL; Doctor’s Hospital, Nassau, Bahamas; Princess Margaret Hospital, Nassau, Bahamas; Mount Sinai Comprehensive Cancer Center, Miami Beach, FL. 2041 BRCA1 and BRCA2 mutation carrier predictions using the BRCAPRO model in clinic-based minority families. Huo D, Senie RT, Terry MB, Daly MB, Buys SS, Ogutha J, Hope K, Olopade OI. University of Chicago, Chicago, IL; Columbia University, New York, NY; Fox Chase Cancer Center, Philadelphia, PA; University of Utah Health Sciences Center, Salt Lake City, UT. 2042 Outcome in BRCA2 mutation carriers is superior to that of high-risk women with sporadic breast cancer. McLennan JL, Hwang ES, Moore DH, Crawford BB, Esserman LJ, Ziegler JL. University of California, San Francisco, CA. 2043 BRCA mutations among women with bilateral breast cancer: mutation carrier rate and sensitivity of the BRCAPRO model based on age at first diagnosis. Ready K, Vogel K, Atchley D, Amos C, Solomon K, Lu K, Arun B. The University of Texas M.D. Anderson Cancer Center, Houston, TX. 2044 Large genomic alterations in BRCA1 in young women with breast cancer participating in the breast cancer family registry. Smith LD. Genetic Epidemiology Laboratory, The University of Melbourne, Parkville, VIC, Australia. 2045 Clinical characteristics and choices regarding prophylactic surgery in BRCA mutation carriers. Stuckey A, Dizon D, Legare R, Wilbur J, Kent J, Tejada-Berges T, Gass J. Women and Infants’ Hospital/Warren Alpert Medical School of Brown University, Providence, RI. 2046 Cancer-predictive methylation patterns in hereditary breast cancer. Suijkerbuijk KP, Fackler MJ, Sukumar S, van Gils CH, van Laar T, Vooijs M, van der Wall E, van Diest PJ. University Medical Center Utrecht, Utrecht, Netherlands; Johns Hopkins, Baltimore, MD. 2047 BRCA testing in underserved women: 5 years of follow-up. Wilcox C, Lee R, Chan S, Crawford B, Luce J, Ziegler J, Beattie MS. San Francisco General Hospital, San Francisco, CA; University of California, San Francisco, San Francisco, CA. 2048 Prophylactic surgeries among BRCA1/2 mutation carriers in the Netherlands. Hooning MJ. The Collaborative Group on Hereditary Breast and Ovarian Cancer in the Netherlands (HEBON). 2049 Breast cancer outcomes in an ethnically diverse clinic-based cohort of high-risk individuals. Nanda R, Spyrka S, Huo D, Cook M, Chen L, Hope K, Cummings S, Olopade O. University of Chicago, Chicago, IL. 2050 Different rate of BRCA1/BRCA2 predisposing mutations according to family history and clinical criteria of breast/ ovarian cancer risk. Sidoni T, De Marchis L, Midulla C, Capalbo C, Giusti R, Paris I, Assalone P, Rocchi A, Ronzino G, Di seri M, Scambia G, Ficorella C, Marchetti P, Cortesi E, Frati L, Gulino A, Giannini G, Ricevuto E. University of L’Aquila, Medical Oncology, L’Aquila, Italy; University “La Sapienza”, Service of Molecular and Ultrastructural Pathology, Rome, Italy; University “La Sapienza”, Medical Oncology, Rome, Italy; UCSC, Campobasso, Italy; S. Carlo Hospital, Rome, Italy; S. Andrea Hospital, Rome, Italy. 2051 Endogenous sex hormones and family history of breast cancer in Chinese women. Zhou L, Yin W, Lu J, Di G, Wu J. Cancer Hospital, Shanghai, China. 2061 A retrospective analysis of the impact of oncotype DX low recurrence score results on treatment decisions in a single academic breast cancer center. Liang H, Brufsky AM, Lembersky BB, Rastogi P, Vogel VG. University of Pittsburgh Cancer Institute, Pittsburgh, PA. 2062 A cohort study of the total health care costs for modern treatment of disseminated breast cancer. Dahlberg L, Lindman H, Lundkvist J. Uppsala University, Uppsala, Sweden; European Health Economics, Stockholm, Sweden. 2063 Halved pegfilgrastim doses in adjuvant breast cancer patients associated with similar efficacy but reduced toxicity. Bartelt ME, Harman S, Lower EE. University of Cincinnati, Cincinnati, OH. 2064 Cost-effectiveness analysis of trastuzumab therapy in patients with early HER-2 positive breast cancer in Brazil. Vernaglia PR, Cunha FM, Correa M, Perdicaris MR, Saggia MG, Santos EAV, Nasciben VD, Pelizon C. Brazilian Institute for Cancer Control, São Paulo, SP, Brazil; Campinas Medical Center, Campinas, SP, Brazil; A. C. Camargo Cancer Hospital, São Paulo, SP, Brazil; Beneficência Portuguesa Hospital, Santos, SP, Brazil; Roche Pharmaceuticals, São Paulo, SP, Brazil. 2065 Cost comparison of capecitabine in the treatment of patients with breast cancer: an analysis from a claims database. Rugo HS, Schulman KL, Zelt S. University of California San Francisco, San Francisco, CA; Thomson Healthcare, Cambridge, MA; Roche Labs Inc., Nutley, NJ. Treatment: Bone Metastases 2052-2057 2052 2053 Systemic treatment of transforming growth factor-beta (TGFĝ) antagonists inhibited osteolytic bone metastasis induced by human breast cancer cells. Bandyopadhyay A, Wang L, Agyin JJ, Lopez-Casillas F, Tang Y, Sun LZ. University of Texas Health Science Center, San Antonio, TX; Universidad Nacional Autónoma de México, Mexico DF, Mexico. Bone-derived IGF-1 enhances bone pain through activation of acid-sensing nociceptors in bone metastases of breast cancer. Sakurai T, Umemura T, Yono H, Williams P, Farias A, Yoneda T. Wakayama Medical University Kihoku Hospital, Ito, Wakayama, Japan; University of Texas Health Center San Antonio, San Antonio, TX. 2054 Patients’ disease and treatment parameters significantly affect survival in metastatic breast cancer. Major P, Cook R. Juravinski Cancer Centre, Hamilton, ON, Canada; University of Waterloo, Waterloo, ON, Canada. 2055 Natural history of skeletal complications in patients receiving chemotherapy for breast cancer metastatic to bone. Major P, Cook R. Juravinski Cancer Centre, Hamilton, ON, Canada; University of Waterloo, Waterloo, ON, Canada. 2056 Application of preventive measures minimizes the occurrence of the osteonecrosis of the jaw (ONJ) in solid tumors patients (pts) with bone metastases treated with bisphosphonates (BPs): a single Institution series. Ripamonti C, Maniezzo M, Cislaghi E, Campa T, Fagnoni E, Saibene G, Bareggi C, Ascani L, Pigni A, Brunelli C. National Cancer Institute, IRCCS Foundation, Milano, Italy. 2057 Treatment: Endocrine Therapy 2066-2106 2066 Phase II double-blind randomized trial of daily oral RAD001 (everolimus) plus letrozole (LET) or placebo (P) plus LET as neoadjuvant therapy for ER+ breast cancer. Baselga J, Semiglazov V, van Dam P, Manikhas A, Bellet M, Mayordomo J, Campone M, Kubista E, Greil R, Bianchi G, Steinseifer J, Molloy B, Tokaji E, Dixon JM, Jonat W, Rugo HS. Hospital Vall d’Hebron, Barcelona, Spain; NN Petrov Research Inst of Oncology, St. Petersburg, Russian Federation; Onc Centrum St Augustinus, Wilrijk, Belgium; City Oncological Dispensary, St. Petersburg, Russian Federation; Hospital Clinico Univ Lozana Blesa, Zaragoza, Spain; Centre Rene Gauducheau, Nantes, France; General Hospital, Vienna, Austria; Univ Hospital, Salzburg, Austria; Novartis Pharma AG, Basel, Switzerland; Istituto Nazionale Tumori, Milan, Italy; Western General Hospital, Edinburgh, United Kingdom; Univ-Frauenklinik, Kiel, Germany; Univ of CA SF, San Francisco, CA. 2067 Randomized Phase II study of gefitinib (IRESSA) or placebo in combination with tamoxifen in patients with hormone receptor positive metastatic breast cancer. Osborne K, Neven P, Dirix L, Mackey J, Robert J, Underhill C, Gutierrez C, Magill P, Hargreaves L. Baylor College of Medicine, Houston, TX; Gasthuisberg, Leuven, Belgium; Sint Augustinus Oncologisch, Wilrijk, Belgium; Cross Cancer Institute, Edmonton, Canada; CHAUQ Hospital du St-Sacrement, Quebec, Canada; Murray Valley Private Hospital, Wondonga, Australia; AstraZeneca, Macclesfield, United Kingdom. 2068 Withdrawn. Bone pain effectiveness and renal safety of ibandronate in breast cancer patients - are results of controlled clinical trials consistent with daily clinical practice? Interim analysis of a non-interventional post marketing surveillance trial in Germany. Meden H, Kuehnle H, Seraphin J, Soeling U, Luhn B. Diakoniekrankenhaus Rotenburg, Germany; Medizinische Hochschule Hannover, Hannover, Germany; Haematological and Oncological Practice, Northeim, Germany; Kassel, Germany; Hamburg, Germany. Treatment: Cost Effectiveness 2058-2065 2058 Cost-effectiveness of late extended adjuvant letrozole following a prolonged therapy break from tamoxifen MA-17 post-unblinding analysis. Karnon J, DiTrapani F, Kaura S. University of Sheffield, Sheffield, Yorkshire, United Kingdom; Novartis Pharmaceuticals, East Hanover, NJ. 2059 Comparison of cost of distant disease-free year gained of aromatase inhibitors letrozole, anastrozole or exemestane versus tamoxifen for early breast cancer in hormone receptor-positive postmenopausal women: Canadian perspective. El Ouagari K, Karnon J, Kaura S. Novartis, Dorval, QC, Canada; University of Sheffield, Sheffield, United Kingdom; Novartis, East Hanover, NJ. 2060 Surgical follow-up for low to average risk breast cancer patients: too much too soon? Khokhotva V, George RL, Khokhotva M. Kingston General Hospital, Queen’s University, Kingston, ON, Canada. 2069 Hot flushes and the risk of recurrence - retrospective, exploratory results from the ATAC trial. 2080 Increased prevalence of retinal hemorrhages among anastrozole users. Eisner A, Falardeau J, Toomey MD, Vetto JT. Oregon Health & Science University, Beaverton, OR; Oregon Health & Science University, Portland, OR. 2081 New treatment strategies using aromatase inhibitors: a preclinical study. Chen S, Phung S, Masri S. Beckman Research Institute of the City of Hope, Duarte, CA. 2082 A placebo-controlled trial examining the effects of letrozole on mammographic breast density and bone and lipid metabolism. Cigler T, Yaffe MJ, Johnston D, Verma S, Findlay B, Wadden N, Pater JL, Richardson H, Tu D, Shangle Q, Goss PE. Massachusetts General Hospital, Boston, MA; Sunnybrook Health Sciences Centre, Toronto, ON, Canada; The Ottawa Hospital, Ottawa, ON, Canada; Niagara Health System, St. Catharines, ON, Canada; Memorial University of Newfoundland, St. John’s, NL, Canada; National Cancer Institute of Canada Clinical Trials Group, Kingston, ON, Canada; (NCIC CTG) MAP.1. 2083 Survival analysis of first-line tamoxifen versus aromatase inhibitors for estrogen-positive metastatic breast cancer in postmenopausal women - a BC perspective. Kyritsis V, De Lemos M, Walker B, Kennecke H, Nakashima L. BC Cancer Agency, Vancouver, BC, Canada; Queens University Belfast, Belfast, Ireland. 2084 Impact of CYP2A6 genotype on pharmacokinetics, safety and efficacy of letrozole treatment in Japanese postmenopausal women with metastatic breast cancer. Minami H, Ohsumi S, Nakamura S, Inaji H, Takenoshita S, Fujiwara Y, Iino Y, Woo M, Tanii H, Tominaga T, Takashima S. CGS20267 Collaborate Study Group, Tokyo, Japan. 2085 Bone health and anastrozole adverse events in Japan. Sagara Y, Rai Y. Hakuaikai Sagara Hospital, Kagoshima City, Kagoshima Prefecture, Japan. 2086 The effects of exemestane, anastrozole and tamoxifen on bone mineral density and bone turnover markers in postmenopausal early breast cancer patients: preliminary results of N-SAS (national surgical adjuvant study) BC04, the TEAM Japan sub-study. Aihara T, Hozumi Y, Suemasu K, Takei H, Takehara M, Osumi S, Saito T, Masuda N, Ohashi Y. Aihara Hospital, Minoo, Osaka, Japan; Jichi Medical University, Shimono, Tochigi, Japan; Saitama Cancer Center, Kitaadachi, Saitama, Japan; Hokkaido Cancer Center, Sapporo, Hokkaido, Japan; Shikoku Cancer Center, Matsuyama, Ehime, Japan; Saitama Red Cross Hospital, Saitama, Saitama, Japan; Osaka National Hospital, Osaka, Japan; The University of Tokyo, Tokyo, Japan. 2087 LET-LOB: preoperative letrozole plus lapatinib or placebo in hormone-receptor positive HER2 negative operable breast cancer. Preliminary report of activity and cardiac tolerability. Frassoldati A, Guarneri V, Cagossi K, Bottini A, Cavanna L, Jovic G, Piacentini F, Oliva C, Conte P. University of Modena, Modena, Italy; Ramazzini Hospital, Carpi, Modena, Italy; Azienda Ospedaliera, Cremona, Italy; General Hospital, Piacenza, Italy; Glaxo SmithKline, Greenford, United Kingdom. Cuzick J. Wolfson Institute of Preventive Medicine, London, United Kingdom. 2070 Withdrawn. 2071 Risk factors for joint symptoms in the ATAC trial. Sestak I, on Behalf of the ATAC Trialists’ Group. Wolfson Institute of Preventive Medicine, London, United Kingdom. 2072 Comparison of joint problems as reported by patients in a randomised adjuvant trial of anastrozole and letrozole. Renshaw L, McHugh M, Williams L, Dixon OM, Fallowfield LJ, Evans DB, Dixon JM. Western General Hospital, Edinburgh, Scotland, United Kingdom; University of Edinburgh, Edinburgh, Scotland, United Kingdom; Brighton & Sussex Medical School, Falmer, Sussex, United Kingdom; Novartis Institutes for BioMedical Research Basel, Basel, Switzerland. 2073 The effect of anastrozole on bone mineral density: updated results from the bone subprotocol of the ATAC trial. Eastell R, Coleman R, Mansel R, Bianco A, Nagykalnai T, Cuzick J, on Behalf of the ATAC Trialists’ Group. Academic Unit of Bone Metabolism, Sheffield, United Kingdom; Cancer Research Centre, Sheffield, United Kingdom; University of Wales College of Medicine, Cardiff, United Kingdom; Universita Degli Studi De Napoli Federico II, Naples, Italy; Uzsoki H Hospital, Budapest, Hungary; Cancer Research UK, London, United Kingdom. 2074 A randomised study of the effects of letrozole and anastrozole on bone turnover. McCaig FM, Renshaw L, Williams L, Young O, Murray J, Macaskill EJ, McHugh M, Hannon R, Dixon JM. Western General Hospital, Edinburgh, Scotland, United Kingdom; Medical School, University of Edinburgh, Edinburgh, Scotland, United Kingdom; Northern General Hospital, Sheffield, England, United Kingdom. 2075 Increased efficacy and combination therapy: targeted letrozole/estrogen receptor-ĝ specific ligand nanoparticles homing to mammary tumors in HER-2/aromatase double transgenic mice. Nair HB, Santhamma B, Agyin JK, Perla RP, Rossini G, Kirma NB, Liu Y-G, Evans DB, Tekmal RR. University of Texas Health Science Center at San Antonio, San Antonio, TX; Southwest Research Institute, San Antonio, TX; Novartis Pharma AG, Basel, Switzerland. 2076 Molecular characterization of aromatase inhibitor resistance: a genome-based approach. Masri S, Phung S, Wang X, Wu X, Yuan Y-C, Chen S. Beckman Research Institute of the City of Hope, Duarte, CA. 2077 Therapeutic strategies using aromatase inhibitors and tamoxifen in a post-menopausal breast cancer model. Alami N, Li Z, Macedo LF, Brodie A, Leyland-Jones B. VM Institute of Research, Montreal, QC, Canada; U. of Maryland, Baltimore, MA; McGill University, Montreal, QC, Canada. 2078 Endometrial status in the Intergroup Exemestane Study (IES) up to 2 years post-treatment. Bertelli G, Hall E, Ireland E, Jassem J, Bliss JM, Snowdon CF, Coombes RC. Singleton Hospital, Swansea, United Kingdom; Institute of Cancer Research, Sutton, United Kingdom; Medical University of Gdansk, Poland; Imperial College London, United Kingdom; on behalf of the IES Group. 2079 Adjuvant aromatase inhibitors in early breast cancer toxicity and adherence. Important observations in clinical practice. Dent SF, Hopkins S, Di Valentin T, Verreault J, Vandermeer L, Verma S. The Ottawa Hospital Regional Cancer Centre (TOHRCC), Ottawa, ON, Canada. 2088 2089 Health-related quality of life and psychological distress in Japanese patients with breast cancer treated with tamoxifen, exemestane or anastrozole for adjuvant therapy: a phase III randomized study of National Surgical Adjuvant Study of Breast Cancer (N-SAS BC) 04. Takehara M, Ohsumi S, Takei H, Shimozuma K, Ohashi Y, Suemasu K, Hozumi Y. Jichi Medical University, Shimotsuke, Tochigi, Japan; National Hospital Organization Shikoku Cancer Center, Matsuyama, Ehime, Japan; Saitama Cancer Center, KitaAdachi, Saitama, Japan; Ritsumeikan University, Kusatsu, Shiga, Japan; University of Tokyo, Bunkyo, Tokyo, Japan; Arche Clinic Breast Center, Omiya, Saitama, Japan. The lipid metabolism of SERMs and AI with primary breast cancer: combined results of Multi 01 and 02 trial. Kusama M, Mitsuyama S, Yanagita Y, Doihara H, Komaki K, Ikeda T, Kimura M, Sano M, Miyauchi K, Anan K. Shinjuku Breast Center, Tokyo, Japan; Kitakyushu Municipal Medical Center, Fukuoka, Japan; Gunma Cancer Center, Gunma, Japan; Okayama University Medical School, Okayama, Japan; Breastopia NAMBA Hospital, Miyazaki, Japan; Teikyo University School of Medicine, Tokyo, Japan; Ota General Hospital, Gunma, Japan; Niigata Association of Occupational Health Inc., Niigata, Japan; Miyauchi Clinic, Hyogo, Japan. 2090 Estrogen deprivation is crucial for the antitumor effect of fulvestrant and adding the HER inhibitor gefitinib delays acquired resistance in a xenograft model of ER-positive breast cancer. Massarweh S, Osborne K, Heidi W, Schiff R. University of Kentucky and Markey Cancer Center, Lexington, KY; Baylor College of Medicine and Dan L. Duncan Cancer Center, Houston, TX. 2091 Fulvestrant vs exemestane following non-steroidal aromatase inhibitor failure: first overall survival data from the EFECT trial. Chia S, Piccart M, Gradishar W, on Behalf of the EFECT Writing Committee. British Columbia Cancer Agency, Vancouver, BC, Canada; Jules Bordet Institute, Brussels, Belgium; Robert H. Lurie Comprehensive Cancer Centre of Northwestern University, Chicago, IL. 2092 Pharmacokinetic profile of the fulvestrant (Fasolodex™) loading-dose regimen in postmenopausal women with hormone receptor-positive advanced breast cancer. McCormack PJ, Sapunar F. AstraZeneca, Macclesfield, Cheshire, United Kingdom. 2093 Fulvestrant does not stimulate endometrial growth in postmenopausal breast cancer patients. Morales L, Neven P, Timmerman D, Wildiers H, Konstantinovic ML, Tan PN, Christiaens M-R, Paridaens R. University Hospitals KULeuven; Faculty of Medicine, KULeuven, Belgium. 2094 Fulvestrant in pretreated postmenopausal patients with metastatic breast cancer: analysis from the French multicentre compassionate use programme. Gligorov J, Antoine EC, Dalenc F, Namer M, Chollet P, Spielmann M, Campone M, Zelek L, Debled M. APHP Tenon, Paris, France; Clinique Hartmann, Neuilly, France; APHP H Mondor, Creteil, France; Centre Antoine Lacassagne, Nice, France; Institut Gustave Roussy, Villejuif, France; Centre Claudius Regaud, Toulouse, France; Centre Bergonie, Bordeaux, France; Centre Rene Gauducheau, Nantes, France; Centre Jean Perrin, Clermont Ferrand, France. 2095 Plasma immunoreactive estradiol is increased during therapy with fulvestrant in menopausal breast cancer patients. Illarramendi JJ, Salgado E, Vera R, Rivero A, Tirapu B, Del Rio L, Lainez N, Martinez M. Hospital de Navarra, Pamplona, Spain. 2096 HDAC inhibitors sensitize ER negative breast cancer cells to AIs. Sabnis GJ, Gediya LK, Njar VCO, Brodie AMH. University of Maryland, School of Medicine, Baltimore, MD; University of Maryland Greenebaum Cancer Center, Baltimore, MD. 2097 Phase II trial of the HDAC inhibitor, vorinostat, in combination with tamoxifen for patients with advanced breast cancer who have failed prior anti-hormonal therapy. Lacevic M, Minton SE, Schmitt ML, Bicaku E, Marchion DC, Munster PN. H. Lee Moffitt Cancer Center & Research Institute, Tampa, FL. 2098 Tamoxifen resistance and tumor initiation mediated by Dicer overexpression in breast cancer progenitor cells - role of BCRP. Selever J, Lewis MT, Corona-Rodriguez A, Tsimelzon A, Fuqua SA. Baylor College of Medicine, Houston, TX. 2099 Co-prescription rates of tamoxifen and CYP2D6 inhibitors: are we compromising breast cancer outcome? Connolly RM, Barron TI, Feely J, Kennedy MJ. Mater Misericordiae Hospital, Dublin, Ireland; Trinity College Dublin, Dublin, Ireland; Trinity College Dublin & St James’s Hospital, Dublin, Ireland. 2100 Association of chemotherapy and estrogen receptor genotype with change in bone mineral density after one year of tamoxifen therapy. Henry NL, Nguyen A, Robarge J, Li L, Hayden J, Lemler S, Schott A, Skaar TC, Flockhart DA, Hayes DF, Stearns V, Consortium on Breast Cancer Pharmacogenomics (COBRA) Investigators. University of Michigan, Ann Arbor, MI; Indiana University, Indianapolis, IN; Johns Hopkins University, Baltimore, MD. 2101 Late tamoxifen treatment in patients previously operated for breast cancer without postoperative tamoxifen: interim analysis. La Mura N, Magri MD, Scalone S, Da Ronch L, Miolo G, Freschi A, Veronesi A. Centro di Riferimento Oncologico, Aviano, PN, Italy. 2102 Randomized phase III trial of exemestane or tamoxifen in first-line hormonal treatment of postmenopausal women with metastatic breast cancer. Chernozemsky I, Kalinov K, Tzekov H, Racheva M, Hristova S, Tomova A, Koynova T, Taskova V, Boideva L, Eniu A, Krasteva E. National Oncology Centre, Sofia, Bulgaria; New Bulgarian University, Sofia, Bulgaria; University Hospital “Sv. Marina”, Varna, Bulgaria; Dispensary of Oncological Diseases, Veliko Tarnovo, Bulgaria; Dispensary of Oncological Diseases, Plovdiv, Bulgaria; Dispensary of Oncological Diseases, Sofia, Bulgaria; Dispensary of Oncological Diseases, Varna, Bulgaria; Dispensary of Oncological Diseases, Haskovo, Bulgaria; Institute of Oncology, Cluj Napoca, Romania. 2103 Tamoxifen withdrawal syndrome. Sedlacek SM, Sedlacek JE. Rocky Mountain Cancer Centers, Denver, CO; Dartmouth College, Hanover, NH. 2104 Downregulated expression of SIAH2, an ubiquitin E3 ligase, is associated with endocrine therapy failure. Jansen MP, Ritstier K, Dorssers LC, van Staveren IL, Helleman J, Look MP, Meijer-van Gelder ME, Sieuwerts AM, Portengen H, Klijn JG, Foekens JA, Berns EM. Erasmus MC/Daniel den Hoed Cancer Center, Rotterdam, Netherlands. 2105 PET FES measures uterine and tumor in vivo pharmacodynamics of endocrine therapy. Linden HM, Peterson LM, Schubert EK, Sandarajan L, Mankoff DA. University of Washington, Seattle, WA. 2106 Adjuvant hormonal therapy choice in women with early stage breast cancer. Song X, Nicholas G, Dent S, Verma S. The Ottawa Hospital Regional Cancer Centre, Ottawa, ON, Canada. 2117 Lentivirus-mediated oncogene delivery to initiate tumors in mouse mammary epithelial cells. Siwko S, Lewis B, Gutierrez C, Li Y. Baylor College of Medicine, Houston, TX; University of Massachusetts Medical Center, Worcester, MA. 2118 FGFR1 amplification is a breast cancer treatment target and is associated with endocrine therapy resistance. Turner NC, Iorns E, Smith A, Lambros MB, Reis-Filho JS, Ashworth A. The Institute of Cancer Research, London, United Kingdom. 2119 Identification of proline-, glutamic acid-, leucine, rich protein (PELP1) as a novel CDK4 substrate and characterizing its role in breast cancer cell proliferation. Chandrasekharan Nair B, Nair SS, Chakravarty D, Rajhans R, Cortez V, Yew RP, Tekmal R, Vadlamudi RK. UTHSCSA, San Antonio, TX. 2120 The regulation of LKB1 by hormones and its implications for post-menopausal breast cancer. Brown KA, McInnes KJ, Simpson ER. Prince Henry’s Institute, Clayton, Victoria, Australia; Monash University, Clayton, Victoria, Australia. 2121 Androgen receptor CAG repeats, haplotypes, non-random X chromosome inactivation, and LOH at Xq25 in relation to breast cancer risk. Chien H-T, Tsai H-C, Chen S-T, Chien Y-C. National Changhua University, Changhua, Taiwan, Taiwan; Changhua Christian Hospital, Changhua, Taiwan, Taiwan. Tumor Cell Biology: Imunology / Immunotherapy 2107-2114 2107 A systematic review of the role of adjuvant ovarian ablation in the treatment of women with early stage breast cancer. Eisen A, Messersmith H, Trudeau M. Cancer Care Ontario, ON, Canada; McMaster University, Hamilton, ON, Canada. 2108 Trilostane (modrenal) as a hormonal treatment for postmenopausal women with breast cancer. Sabine VS, Speirs V, Macaskill JE, Shaaban AM, Campbell F, Renshaw L, Faratian D, Bartlett JM, Dixon MJ. University of Edinburgh, Edinburgh, United Kingdom; University of Leeds, Leeds, United Kingdom. 2109 Characterization of anti-MUC1 immune response in patients with in situ, early and locally-advanced breast cancer. Geller BA, Lepisto AJ, McKolanis JR, Ahrendt GM, Potter DM, Finn OJ, Brufsky AM. University of Pittsburgh Cancer Institute, Pittsburgh, PA; University of Pittsburgh School of Medicine, Pittsburgh, PA; University of Pittsburgh Cancer Institute; MageeWomens Hosptial of UPMC, Pittsburgh, PA. 2110 2111 Relation of intratumoral B-cells and response to neoadjuvant chemotherapy. Lenhard MS, Wirtz RM, Hasmueller S, Rueckert S, Ditsch N, Ruehl I, Kahlert S, Bauerfeind I, Untch M, on Behalf of the Participating Centers. Ludwig-Maximilians-University of Munich, Munich, Germany; Molecular Research, Leverkusen, Germany; Helios Hospital, Berlin-Buch, Germany. Decreased accumulation of CD163-positive macrophages is associated with nodal metastases in patients with breast cancer. Mansfield AS, Heikkila P, Vakkila J, von Smitten K, Leidenius M. Helsinki University Central Hospital, Helsinki, Finland; University of Helsinki, Helsinki, Finland. 2112 Immunological status of micrometastasis-positive sentinel nodes in breast cancer patients. Matsuura K, Osaki A, Saeki T, Ohara M, Murakami S, Arihiro K. International Medical Center, Saitama Medical University, Hidaka, Saitama, Japan; Research Institute for Radiation Biology and Medicine, Hiroshima, Japan; Hiroshima University, Hiroshima, Japan. 2113 Clinicopathological significance of regulatory T cells in breast cancer. Ohara M, Murakami S, Yamaguchi Y, Arihiro K. Radiation Biology and Medicine, Hiroshima University, Hiroshima, Japan; Kawasaki Medical School, Kurashiki, Okayama, Japan; Hiroshima University, Hiroshima, Japan. 2114 Alternatively activated macrophages promote the invasiveness of breast cancer cells. Gong C, Zhang X, Liu S, Yu F, Su F, Song E. Sun Yat-Sen Memorial Hospital, Guangzhou, Guangdong, China. 9:00-9:30 Energy balance, insulin, and breast cancer Michael Pollak, MD McGill University Montreal, CANADA 9:30-11:15 Mechanism of action of herceptin killing of HER-2+ breast cancer cells under “in vitro” and “in vivo” conditions. Kute TE, Savage L, Wood J, Vaughn J. Wake Forest University Medical Center, Winston-Salem, NC; Wake Forest University, Winston-Salem, NC. 2116 Clinical and immunologic responses of HLA-A3+ breast cancer patients vaccinated with the HER2/neu-derived peptide vaccine, E75, in a phase I clinical trial. Patil R, Holmes JP, Amin A, Carmichael M, Jama YH, McNeill A, Hueman MT, Craig D, Ponniah S, Peoples GE. Windber Medical Center, Windber, PA; National Naval Medical Center, Bethesda, MD; USUHS, Bethesda, MD; Brooke Army Medical Center, Ft. Sam Houston, TX. GENERAL SESSION 3 – Exhibit Hall D 9:30 31. Genomic approaches to breast cancer subset identification and treatment. Albertson D, Chin K, Devries S, Feiler H, Pinkel D, Spellman P, Waldman F, Wang N, Hennessy B, Mills G, Barcellos Hoff MH, Bissell M, Guan Y, Hu Z, Kuo W-L, McCormick F, Neve R, Stampfer M, Wooster R, Yaswen P, Das D, Fridlyand J, Correll E, Jin J, Nordmeyer B, Sudar D, Chew K, Dairkee S, Ljung BM, Hwang S, Esserman L, Arbushites M, Benz C, Koehler M, Marks JD, Zhou Y, Park J, Weber B, Gray J. University of California, San Francisco, CA; Lawrence Berkeley National Laboratory, Berkeley, CA; MD Anderson Cancer Center, Houston, TX; GlaxoSmithKline, King of Prussia, PA; California Pacific Medical Center, San Francisco, CA; Buck Institute for Age Research, Novato, CA; Genentech, South San Francisco, CA. 9:45 32. Genome-wide analysis of DNA copy number alterations in conjunction with gene expression profiling identifies DNA amplification loci that predict distant recurrence in lymph node-negative (LNN) primary breast cancer patients. Zhang Y, Klijn J, Yu J, Jiang J, Jatkoe T, Sieuwerts A, Martens J, Wang Y, Foekens J. Johnson & Johnson, San Diego, CA; Erasmus MC, Rotterdam, Netherlands. 10:00 33. Gene expression profiles of ER+/PR-breast cancer are associated with genomic instability and Akt/mTOR signaling, and predict poor patient outcome better than clinically assigned PR status. Creighton CJ, Osborne CK, van de Vijver M, Foekens JA, Wang Y, Zhang Y, Klijn JGM, Horlings HM, Hilsenbeck SG, Lee AV, Schiff R. Baylor College of Medicine, Houston, TX; Netherlands Cancer Institute, Amsterdam, Netherlands; Erasmus MC-Daniel den Hoed, Rotterdam, Netherlands; Veridex LLC, a Johnson & Johnson Company, San Diego, CA. Tumor Cell Biology: Oncogenes/Tumor Suppressor Genes 2115-2121 2115 PLENARY LECTURE 3 – Exhibit Hall D 10:15 10:30 10:45 11:00 34. Expression of alphavbeta6 supersedes Her2 and triplenegative/basal classification of breast cancer and defines novel subgroups with poor survival: implications for breast cancer classification and treatment. Jones JL, Thomas GJ, Duffy SW, Chou P, Gabe R, Ellis I, Green A, Saha A, Mulligan KT, Ryder K, Gillet C, Violette S, Weinreb P, Hart IR, Marshall JF. Bart’s and the London, Queen Mary’s School of Medicine and Dentistry, London, United Kingdom; Nottingham City Hospital, Nottingham, United Kingdom; Guy’s Hospital, London, United Kingdom; Biogen Idec, Cambridge, MA. 35. A stroma-related gene signature predicts resistance to epirubicin-containing neoadjuvant chemotherapy in breast cancer. Farmer P, Bonnefoi H, Anderle P, Cameron D, Wirapati P, Becette V, André S, Piccart M, Campone M, Tubiana-Hulin M, MacGrogan G, Petit T, Jassem J, Rouanet P, Blot E, Bogaerts J, Bergh J, Iggo R, Delorenzi M. National Centre of Competence in Research (NCCR) Molecular Oncology, Swiss Institute for Experimental Cancer Research (ISREC), Epalinges, Switzerland; Swiss Institute of Bioinformatics (SIB), Lausanne, Switzerland; European Organisation for Research and Treatment of Cancer (EORTC), Breast Cancer Group, Brussels, Belgium; The Swiss Group for Clinical Cancer Research (SAKK), Bern, Switzerland; The Anglo-Celtic Cooperative Oncology Group (ACCOG), Edinburgh University, Edinburgh, United Kingdom; The Swedish Breast Cancer Group (SweBCG), Karolinska Institute, Stockholm, Sweden. 36. The clinical significance of polysomy 17 in the HER2+ N9831 intergroup adjuvant trastuzumab trial. Reinholz MM, Jenkins RB, Hillman D, Lingle WL, Davidson N, Martino S, Kaufman P, Kutteh L, Perez EA. Mayo Clinic College of Medicine, Rochester, MN; John Hopkins, Baltimore, MD; The Angeles Clinic and Research Institute, Santa Monica, CA; Dartmouth Hitchcock Medical Center, Lebanon, NH; Oncology Associates of Cedar Rapids, Cedar Rapids, IA; Mayo Clinic College of Medicine, Jacksonville, FL. 2:00 The women’s health initiative randomized trials of menopausal hormone therapy: Results and impact on clinical practice Rowan Chlebowski, MD, PhD LA Biomedical Research Institute Torrance, CA 2:30 A review of HRT and breast cancer in other epidemiologic studies Jack Cuzick, PhD Wolfson Institute of Preventive Medicine London, UNITED KINGDOM 3:00 Understanding changes in breast cancer incidence. Interactions between epidemiological and clinical trial evidence. Peter Ravdin, MD, PhD MD Anderson Cancer Center Houston, TX 3:30-5:00 3:30 41. ATAC: 100 month median follow-up (FU) shows continued superior efficacy and no excess fracture risk for anastrozole (A) compared with tamoxifen (T) after treatment completion. Forbes JF, Cuzick J, Buzdar A, Howell A, Baum M on behalf of the ATAC Trialists’ Group. University of Newcastle, Calgary Mater Hospital, NSW, Australia; Cancer Research UK, UK; M.D. Anderson Cancer Center, USA; Christie Hospital, UK; Portland Hospital, UK. 3:45 42. Mid-term efficacy of a breast cancer screening program for women with a familial or genetic susceptibility: update of the Dutch MRI screening study (MRISC). Rijnsburger AJ, Obdeijn I-M, Kriege M, Boetes C, Oosterwijk JC, Tollenaar RAEM, Peterse H, Bergers E, Tilanus-Linthorst MMA, de Koning HJ, Rutgers EJT, Klijn JGM, on behalf of the MRISC Study Group. Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands; University Medical Center Nijmegen, Nijmegen, Netherlands; Groningen University Medical Center, Groningen, Netherlands; Leiden University Medical Center, Leiden, Netherlands; Netherlands Cancer Institute, Amsterdam, Netherlands; Free University Medical Center, Amsterdam, Netherlands. 4:00 43. Detection of enhancing lesions on contrast-enhanced MRI of the breast using real-time virtual sonography: fusion of MRI and sonography data. Nakano S, Yorozuya K, Takasugi M, Mouri Y, Fukutomi T, Arai O, Mitake T. Aichi Medical University, Aichi-gun, Aichi, Japan; Hitachi Medical Corporation, Kashiwa-city, Chiba, Japan. 4:15 44. MRI for diagnosing pure ductal carcinoma in-situ. Kuhl CK, Schrading S, Wardelmann E, Braun M, Kuhn W, Schild HH. University of Bonn, Bonn, Germany. 4:30 45. Noninvasive monitoring of neoadjuvant chemotherapy using optical tomography with ultrasound localization: initial experience. Tannenbaum S, Hegde P, Kane M, Xu C, Kurtzman S, Baccaro N, Iyer M, Wilson L, Deckers P, Zhu Q. University of Connecticut, Farmington, CT; University of Connecticut, Storrs, CT. 4:45 46. Tomosynthesis for the detection of breast cancer in a clinical setting. Ikeda DM, Ruschin M, Timberg P, Svahn T, Zackrisson S, Andersson I. Radiology, Lund University, Malmoe University Hospital, Malmoe, Sweden; Radiology, Stanford University School of Medicine, Stanford, CA. 37. Multidrug resistance and breast cancer: a meta-analysis of MDR1 and its clinical significance. Trock B, Leonessa F, Clarke R. Johns Hopkins, Baltimore, MD; Uniformed Services University of Health Sciences, Bethesda, MD; Georgetown University, Washington, DC. 11:15-12:00 WILLIAM L. MCGUIRE MEMORIAL LECTURE – Exhibit Hall D Sponsored by GlaxoSmithKline. Biomarking the oestrogen dependence of breast cancer Mitchell Dowsett, PhD Institute of Cancer Research/Royal Marsden NHS Trust London, UNITED KINGDOM 12:00-1:00 LUNCH [Ticket Required] – Exhibit Hall A 12:30-1:45 CASE DISCUSSION 1 – Ballroom A 2:00-3:30 MINI-SYMPOSIUM 2 – Exhibit Hall D WOMEN’S HEALTH INITIATIVE: HRT AND OTHER ISSUES Peter Ravdin, MD, PhD, Moderator MD Anderson Cancer Center Houston, TX 2:00 Introduction GENERAL SESSION 4 – Exhibit Hall D 5:00-7:00 POSTER DISCUSSION 3 & RECEPTION – Ballroom B 309 Evaluation of trastuzumab, docetaxel and capecitabine as first-line therapy for HER2-positive locally advanced or metastatic breast cancer. Wardley A, Antón-Torres A, Pivot X, Morales-Vasquez F, Zetina L, Dias Gaui M, Otero Reyes D, Jassem J, Button P, Bell R. Christie Hospital NHS Foundation Trust, Manchester, United Kingdom; Hospital Universitario Miguel Servet, Zaragoza, Spain; CHU Jean Minjoz, Besançon, France; Instituto Nacional de Cancerología, Mexico City, Mexico; Hospital Roosevelt, Guatemala City, Guatemala; Instituto Nacional do Câncer, Rio de Janeiro, Brazil; Hospital CIMA, San José, Costa Rica; Akademia Medyczna, Gdansk, Poland; Roche Products Pty Ltd, Dee Why, New South Wales, Australia; Andrew Love Cancer Centre, Geelong Hospital, Geelong, Victoria, Australia. 310 A phase I study of trastuzumab-DM1, a first-in-class HER2 antibody-drug conjugate, in patients with advanced HER2+ breast cancer. Krop IE, Beeram M, Modi S, Rabbee N, Girish S, Tibbitts J, Holden SN, Lutzker SG, Burris HA. Dana-Farber Cancer Institute, Boston, MA; Institute for Drug Development, San Antonio, TX; Memorial Sloan-Kettering Cancer Center, New York, NY; Genentech, South San Francisco, CA; Sarah Cannon Research Institute, Nashville, TN. Antibodies and Immunotherapy 301-310 301 Optimal dose and schedule of a HER2/neu peptide (E75) vaccine in disease-free breast cancer patients: results from two phase I/II clinical trials. Holmes JP, Patil R, Amin A, Jama YH, McNeill A, Hueman MT, Craig D, Ponniah S, Peoples GE. National Naval Medical Center, Bethesda, MD; Windber Medical Center, Windber, PA; USUHS, Bethesda, MD; Brooke Army Medical Center, Ft. Sam Houston, TX. 302 Clinical results of a phase I trial of a HER2/neu-derived peptide (GP2) vaccine in disease-free, node-negative breast cancer patients. Carmichael M, Holmes JP, Mittendorf EA, Amin A, Hueman MT, Ponniah S, Peoples GE. USUHS, Bethesda, MD; National Naval Medical Center, Bethesda, MD; UTMD Anderson Cancer Center, Houston, TX; Brooke Army Medical Center, Ft. Sam Houston, TX. 303 Immunotherapy against metastatic breast cancer with a twist. Demaria S, Wang B, Yang AM, Santori F, Kawashima N, Matsumura S. New York University School of Medicine, New York, NY. 304 10 years follow up of pilot phase III immunotherapy study in early stage breast cancer patients using oxidized mannanMUC1. Vassilaros S, Tsibanis A, Tsikkinhs A, McKenzie IF, Apostolopoulos V. PROLIPSIS – Diagnostic Breast Center, Athens, Greece; Burnet Institute at Austin, Heidelberg, Victoria, Australia. POSTER SESSION 3 & RECEPTION – Exhibit Hall B (#3001-3120) Detection and Diagnosis: Axillary/Sentinel Nodes 3001-3027 3001 Is intraoperative cytology of sentinel nodes useful and predictive for non-sentinel axillary nodes? NSABP B-32. Julian TB, Anderson SJ, Fourchotte V, Brown AM, Boudros E, Mamounas EP, Costantino JP, Wolmark N. NSABP Medical Affairs, NSABP Investigators & NSABP Operation & Biostatistical Centers, Pittsburgh, PA. Targeting of the chemokine receptor CXCR4 in acquired trastuzumab resistance. Tripathy D, Mukhopadhyay P, Verma U, Mukhopadhyay C, Shelton J, Story M, Ding L. University of Texas Southwestern Medical Center, Dallas, TX. 3002 First clinical results on the potential of intraoperative imaging for sentinel lymph node biopsy in breast cancer. Barranger E, Kerrou K, Pitre S, Duval M-A, Charon Y, Uzan S. Tenon Hospital, Paris, France; Lariboisiere Hospital, Paris, France; CNRS Paris 7- Paris 11, Orsay, France. TBCRC 001: EGFR inhibition with cetuximab in metastatic triple negative (basal-like) breast cancer. Carey LA, Mayer E, Marcom PK, Rugo H, Liu M, Ma C, Rimawi M, Storniolo A, Forero A, Esteva F, Wolff A, Ingle J, Ferraro M, Sawyer L, Davidson N, Perou CM, Winer EP. University of North Carolina; Dana Farber; Duke; UCSF; Georgetown; Washington University; Baylor; Indiana University; University of Alabama-Birmingham; M.D. Anderson; Johns Hopkins; Mayo. 3003 Optical biopsy scanner utilising elastic scattering spectroscopy for rapid intra-operative diagnosis of sentinel node metastases in breast cancer. Somasundaram SK, Chicken DW, Austwick MR, Bown SG, Keshtgar MR. University College London, London, United Kingdom. 3004 Sentinel lymph node biopsy for advanced breast cancer after neoadjuvant chemotherapy: results of the French multicenter prospective trial GANEA. Classe J-M, Giard S, Mignotte H, Rodier J-F, Leveque J, Ferron G, Marchal F, Alran S, Ladonne J-M, Cuisenier J, Dupre P-F, Body G, Andrieux N, Campion L. Cancer Center, Nantes, France; Cancer Center, Lille, France; Cancer Center, Lyon, France; Cancer Center, Strasbourg, France; University Hospital, Rennes, France; Cancer Center, Toulouse, France; Cancer Center, Nancy, France; Cancer Center, Paris, France; Cancer Center, Rouen, France; Cancer Center, Dijon, France; University Hospital, Brest, France; University Hospital, Tours, France. 3005 The basal breast cancer molecular subtype predicts for a lower incidence of axillary lymph node involvement in primary breast cancer. Crabb SJ, Immonen T, Bajdik CD, Cheang MC, Leung S, Speers CH, Huntsman D, Nielsen TO, Chia SK. BC Cancer Agency, Vancouver, BC, Canada. 305 Circulating immature myeloid cells in breast cancer patients correlate with clinical cancer stage and cyclophosphamide treatment: implications for cancer immunotherapy. Montero AJ, Dewaay DJ, Salem M, Cole DJ, Diaz-Montero CM. Medical University of South Carolina, Charleston, SC. 306 307 308 5:00-7:00 Preliminary results of a randomized phase II study of weekly irinotecan/carboplatin with or without cetuximab in patients with metastatic breast cancer. O’Shaughnessy J, Weckstein DJ, Vukelja SJ, McIntyre K, Krekow L, Holmes FA, Asmar L, Blum JL. US Oncology Research, Inc., Houston, TX; Baylor-Charles A. Sammons Cancer Center, Dallas, TX; Texas Oncology, P.A. – Dallas Presbyterian, Dallas, TX; New Hampshire Oncology-Hematology, Hookset, NH; Tyler Cancer Center, Tyler, TX; The Breast Care Center of North Texas, Bedford, TX; Texas Oncology, P.A., Houston, TX. 3006 Axillary staging is more accurate today than ever before: no increase in the false negative rate with wide-spread adoption of sentinel node technique. Helyer LK, Coburn NG, Law CH, McCready DR. Princess Margaret Hospital, Toronto, ON, Canada; Sunnybrook Health Sciences Centre, Toronto, ON, Canada. 3007 Rapid detection of lymph node metastasis in breast cancer patients by “One-step Nucleic Acid Amplification (OSNA)”: results from a multi-institutional clinical study. Kaneko T, Akiyama F, Tsujimoto M, Noguchi S, Inaji H, Nakamura S, Otomo Y, Kato Y, Matsuura N. The Cancer Institute Ariake Hospital of the Japanese Foundation for Cancer Research, Tokyo, Japan; Osaka Police Hospital, Osaka, Japan; Osaka University, Osaka, Japan; Osaka Medical Center of Cancer and Cardiovascular Diseases, Osaka, Japan; St Luke’s International Hospital, Tokyo, Japan; SYSMEX Corp, Kobe, Japan. 3008 Clinical significance of occult axillary lymph node metastases in breast cancer patients without adjuvant systemic therapy: a long-term retrospective study. Kelten C, Mittendorf EA, Broglio K, Vo T, Middleton LP, Ueno N, Hunt KK, Sahin AA. UT M.D. Anderson Cancer Center, Houston, TX. 3009 Dual-labeled trastuzumab-based imaging agent for the detection of human epidermal growth factor receptor-2 (HER2) overexpression in breast cancer. Sevick-Muraca EM, Sampath L, Kwon S, Ke S, Schiff R, Mawad ME. Baylor College of Medicine, Houston, TX. 3010 Peripheral blood microarray data may aid in predicting lymph node status of breast cancer patients. Jordan RM, Hu H, Heckman CM, Kvecher L, Shriver CD, Mural R, Yang Y-C. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 3011 Magnetic nanoparticles for detecting cancer spread. Joshi T, Pankhurst QA, Hattersley S, Brazdeikis A, Hall-Craggs M, De Vita E, Bainbridge A, Sainsbury R, Sharma A, Douek M. Royal Free and University College Medical School, London, United Kingdom; London Centre for Nanotechnology, London, United Kingdom; Texas Center for Superconductivity, Houston, TX; University College London Hospital, London, United Kingdom. 3012 Intra-operative assessment of sentinel lymph node using real time quantitative PCR versus delayed assessment of sentinel lymph node: a cost-effectiveness model. Goyal A, Douglas-Jones A, Woods V, Jasani B, Mansel RE. School of Medicine, Cardiff University, Cardiff, United Kingdom. 3013 Discriminating between sentinel node micrometastases and sub micrometastases is not contributive to omit axillary lymph node dissection. Gilles HG, Sylvia GS, Herve MH, Max BM, Jean Marc CJM, Monique CM, Claude NC, GCFCC. Institut Paoli Calmettes, Marseille, Bouches du Rhone, France; Centre Oscar Lambret, Lille, France; Centre Leon Berard, Lyon, France; Centre Rene Gauducheau, Nantes, France; Casamance, Marseille, France; Hopital G Pompidou, Paris, France; Groupe des Chirurgiens de Federation des CLCC, France. 3014 3015 Scoring system to predict non-sentinel lymph node status in breast cancer patients with metastatic sentinel lymph nodes: comparison with other scoring systems and nomogram. Cho J, Han W, Ko E, Lee JW, Chung SY, Kim E-K, Hwang K-T, Kim S-W, Noh D-Y. Seoul National University College of Medicine, Seoul, Korea. Detailed pathologic evaluation of non-sentinel axillary lymph nodes following identification of sentinel lymph node metastases by cytokeratin immunohistochemistry and/or permanent section H&E levels. Lillemoe TJ, Dunn D, Bretzke M, Johnson E, O’Leary J, Stoller D, Fraki S, Pearson S, Diaz LK. Abbott Northwestern Hospital, Minneapolis, MN. 3016 “One Step Nucleic Acid Amplification” for rapid molecular analysis of breast cancer lymph nodes: the way towards one stop sentinel node surgery? Snook KL, Kissin MW, Layer GT, Jackson P, de Vries CS, Shousha S, Sinnett HD, Nigar E, Singhal H, Chia Y, Cunnick G. Royal Surrey Hospital, Guildford, Surrey, United Kingdom; The University of Surrey, Guildford, Surrey, United Kingdom; Charing Cross Hospital & Imperial College, London, United Kingdom; Northwick Park Hospital, Harrow, Middlesex, United Kingdom; Wycombe General Hospital, High Wycombe, Buckinghamshire, United Kingdom. 3017 Rapid detection of sentinel lymph node metastasis in breast cancer by OSNA assay. Beitsch P, Taylor W, Jordan J, Garcia M, Kocian L. Dallas Surgical Group, Dallas, TX. 3018 Preoperative axillary ultrasound and fine needle aspiration cytology of the axillary nodes in the diagnosis of axillary nodal involvement in breast cancer. Swinson C, Ravichandran D, Nayagam M, McLaggan S, Wilkie J, Wright D, Yanny L, Allen S. Luton & Dunstable NHS Foundation Trust, Luton, United Kingdom. 3019 Metastatic pattern of axillary lymph nodes after sentinel lymph node on 3D-CT lymphography. Yamashita K, Shimizu K. Musashikosugi Hospital, Nippon Medical School, Kawasaki, Kanagawa, Japan; Nippon Medical School, Bunkyo-ku, Tokyo, Japan. 3020 The necessity of two gene markers for accurate detection of lymph node micrometastasis using an investigational real time RT-PCR assay confirmed by 0.2 mm interval frozen section analysis in breast cancer. Kurosumi M, Kobayashi Y, Takei H, Kitsugi K, Ueno M, Green G, Vargo J. Saitama Cancer Center, Saitama, Japan; Veridex LLC, Japan; Veridex LLC, NJ. 3021 Navigation surgery using a dye and fluorescence for detecting sentinel lymph nodes in breast cancer. Hojo T, Kinoshita T, Yoshida M, Shien T, Iwamoto E, AkashiTakana S. National Canver Center Hospital, Tokyo, Japan. 3022 Real time reverse transcriptase-polymerase chain reaction assay as an adjuvant tool in evaluation of breast cancer sentinel lymph nodes. Tafe LJ, Schwab MC, Rizzo EJ, Joel LA, Wells WA, Tsongalis GJ. Dartmouth Medical School, Dartmouth Hitchcock Medical Center and Norris Cotton Cancer Center, Lebanon, NH. 3023 Sentinel node excision after neoadjuvant chemotherapy - a multicentric analysis. Bauerfeind IGP, Kuehn T, Himsl I, Ruehl IM, Kahlert S, Lebeau A, Untch M, Hoess C. Ludwig-Maximilians-University of Munich, Grosshadern, Munich, Germany; Klinikum Esslingen, Esslingen, Germany; University Eppendorf, Hamburg, Germany; Klinikum Berlin Buch, Berlin, Germany; Krankenhaus, Ebersberg, Germany. 3024 Clinicopathologic factors associated with microinvasion in ductal carcinoma in situ: possible utility in planning sentinel lymph node biopsy. Mahtani R, Ying B, Rescigno J, Aziz M, Bernik S, Klein P. St. Vincents Cancer Care Center, New York, NY. 3025 Utility of internal mammary lymph node biopsy in breast cancer. Ozmen V, Cabioglu N, Ozcinar B, Ozgen G, Tihan D, Mudun A, Ozmen T, Igci A, Muslumanoglu M, Kecer M, Dagoglu T. Istanbul Medical Faculty, University of Istanbul, Istanbul, Capa Fatih, Turkey. 3026 3027 Long term follow up after 664 sentinel node biopsies: local axillary failure and overall survival. Soler C, Bouteille C, Chol R, Reynaud R, Gremillet E, Bousserolles AM. Centre Hospitalier Privé de la Loire, Saint-Etienne, France; Centre Hospitalier Universitaire, Saint-Etienne, France; Centre Hospitalier General, Firminy, France; Centre Hospitalier General, Le Puy en Velay, France. Patterns of cellular distribution within the sentinel node positive for breast cancer. Tsiapali E, Dizon D, Steinhoff M, Gass J. Women and Infants Hospital, Providence, RI; Brown University Medical School, Providence, RI. 3037 Fine needle aspiration cytology material is highly suitable for mRNA extraction and subsequent molecular analysis of breast cancer. Uzan C, Andre F, Veronique S, Suzette D, Philippe V. Institut Gustave Roussy, Villejuif, France; UPRESS EA 3535, France. 3038 The borderline amplified HER2 FISH result on breast core biopsy: indications for further sampling do affect patient management. Striebel JM, Bhargava R, Surti U, Brufsky A, Dabbs DJ. Magee Womens Hospital, University of Pittsburgh Medical Center, Pittsburgh, PA. 3039 Core biopsy following neoadjuvant chemotherapy in breast cancer - a tool to predict both residual disease and plan axillary treatment. Balasubramanian R, Aref F, Sivagurunathan S, Riddle P, Ahmad R, Vashisht R. West Middlesex University Hospital, London, United Kingdom. 3040 Medico-economic evaluation of the rapid diagnosis of breast lesions using fine-needle aspiration in a one stop breast clinic. Delaloge S, Noel E, Andre F, Benhamou E, Larue C, Balleyguier C, Vielh P, de Pouvourville G. Institut Gustave Roussy, Villejuif, France; ESSEC Business School, Cergy Pontoise, France. 3041 Equivocal triple assessment summary scores - do they mean anything? Parmeshwar R, Harland RN. Royal Albert Edward Infirmary, Wigan, Lancashire, United Kingdom. Detection and Diagnosis: Diagnostic Pathology 3028-3041 3028 3029 3030 Gene expression by standardized quantitative RT-PCR in the special histologic subtypes of estrogen receptor positive invasive breast cancer. Baehner FL, Watson D, Ballard JT, Palmer G, Shak S. Genomic Health, Inc., Redwood City, CA. One-step nucleic acid amplification for intra-operative detection of lymph node metastases in breast cancer patients. Schem C, Maass N, Bauerschlag DO, Jonat W, Carstensen M, Löning T, Tiemann K. University Clinic of Schleswig-Holstein, Campus Kiel, Kiel, Germany; Albertinen Krankenhaus, Hamburg, Germany; University Clinic of Hamburg Eppendorf, Hamburg, Germany. Discrepancy between triple negative phenotype and basallike tumor: an immunohistochemical analysis based on 150 “triple-negative” breast cancers. Conforti R, Bidard F-C, Michiels S, Boulet T, Tomasic G, Mathieu M-C, Delaloge S, Andre F. Institut Gustave Roussy; Breast Cancer Business Unit; Institut Gustave Roussy, Villejuif, France. 3031 Prophylactic mastectomy - trends in pathology findings. Wen YH, Roses DF, Axelrod DM, Guth AA, Shapiro RL, Cangiarella J, Ziguridis N, Darvishian F, Singh B. New York University School of Medicine, New York, NY. 3032 Multiplexed immunohistochemical quantitative molecular phenotyping via multispectral imaging and automated segmentation. Hoyt CC, Gossage K, Levenson RM, Bandaru R, Gardner H. Cambridge Research and Instrumentation, Inc., Woburn, MA; Novartis Institutes for BioMedical Research Inc., Cambridge, MA. 3033 3034 3035 3036 Assessment of ErbB2 gene amplification with quantitative real time PCR. Gunnarsson C, Olsson H, Nilsson J, Holmlund B, Jansson A. Linkoping University Hospital, Linkoping, Sweden; Faculty of Health Science Linkoping, Linkoping, Sweden. Scoring system to predict malignancy in patients diagnosed as atypical ductal or lobular hyperplasia on ultrasoundguided core needle biopsy. Ko E, Han W, Lee JW, Cho J, Kim E, Jung S-Y, Moon WK, Park IAe, Kim S-W, Lee ES, Noh D-Y. Seoul National University Hospital, Seoul, Korea; Bundang Seoul National University Hospital, Sungnam-si, Korea; National Cancer Center, Goyang-si, Korea. Identification of commonly aberrant genomic regions using high-resolution array CGH on paraffin-embedded breast cancer samples. Davis R, Poirier B, De Witte A, Lin E, Borowsky A, Gosh J, Gao J, Giles S, LeProust E, Amorese D, Roberts D, Shams S, Carmack C, Gregg JP. UC Davis, Sacramento, CA; Agilent Technologies, Santa Clara, CA; BioDisovery, Manhattan Beach, CA. Correlation between breast core biopsies of uncertain malignant potential and subsequent excision biopsies. Fazel MZ, Rothnie ND, Payne S. Southend University Hospital, Southend-on-Sea, Essex, United Kingdom. Detection and Diagnosis: Biopsy Techniques 3042-3044 3042 Is diathermy excision of gynaecomastia superior to saline adrenaline and sharp dissection technique? Parmeshwar R, Harland RNL, Prasad R. Royal Albert Edward Infirmary, Wigan, Lancashire, United Kingdom. 3043 The accuracy of preoperative core biopsy in patients with ductal carcinoma in situ. Halliday M, Bruce E, Marshall, Thompson C, Shokuhi S, Jones L, Harries S, Clarke D. Warwick Hospital, Warwick, Warwickshire, United Kingdom. 3044 Breast biopsy for mammographically detected nonpalpable lesions using a vacuum-assisted biopsy device (Mammotome) and an upright-type stereotactic mammography unit. Ohsumi S, Taira N, Aogi K, Takashima S, Nishimura R. National Hospital Organization Shikoku Cancer Center, Matsuyama, Ehime, Japan. Epidemiology and Outreach: Racial Aspects 3045-3052 3045 Racial differences in frequency and spectrum of BRCA1/2 mutations in young women with breast cancer. Haffty BG, Choi DH, Moran MS, Silber A, Matloff E, Lee MH, Ranieri K, Toppmeyer D. UMDNJ-RWJMS and Cancer Institute of New Jersey, New Brunswick, NJ; Soonchunhyang Hospital, Seoul, Korea; Yale University, New Haven, CT. 3046 A transcription factor-centric computational analysis of genes differentially expressed in healthy breast tissues from African American and Caucasian women. Hu H, Stegmaier P, Field LA, Kel A, Shriver CD, Liebman MN, Mural RJ. Windber Research Institute, Windber, PA; BIOBASE GmbH, Wolfenbüttel, Germany; Walter Reed Army Medical Center, Washington, DC. 3047 Identification of protein expression differences in invasive breast tumors from African American compared to Caucasian women. Ellsworth RE, Seeley EH, Ellsworth DL, Sanders M, Hooke JA, Caprioli RM, Shriver CD. Windber Research Institute, Windber, PA; Vanderbilt University, Nashville, TN; Walter Reed Army Medical Center, Washington, DC. 3048 NCIC CTG MAP.3: enrollment and study drug adherence of ethnic minority women in a breast cancer prevention trial. Moy B, Richardson H, Johnston D, Pater JL, Chlebowski R, AlésMartínez JE, Ingle J, Goss PE. Massachusetts General Hospital, Boston, MA; Queen’s University, Kingston, ON, Canada; HarborUCLA, Torrance, CA; Hospital Ruber Internacional, Madrid, Spain; Mayo Clinic, Rochester, MN. 3049 Ethnicity and breast cancer: risk and predictors in a pre-paid health plan. Shim VC, Li Y, Baer D, Udaltsova N, Klatsky AL. Kaiser Permanente Medical Center, Oakland, CA; Kaiser Permanente Medical Care Program, Oakland, CA. 3050 Identification of trends in large breast cancers in an ethnically diverse population. Bailey L, Mendelsohn MA, Bishop S. Alta Bates Summit Medical Center, Berkeley-Oakland, CA. 3051 Patterns of therapy and adherence to established treatment guidelines in caucasian versus African-American newepisode breast cancer patients. Short L, Fisher M, Wahl P, White S, Rodriguez N, Kelly M. HealthCore, Inc., Wilmington, DE; Blue Cross Blue Shield of Georgia, Atlanta, GA; University of Pittsburgh School of Medicine, Pittsburgh, PA. 3052 Multiethnic comparisons of genome-wide alterations in breast cancer using paraffin embedded samples. Baumbach LL, Ahearn ME, Jorda M, Gomez C, Halsey TA, Ellison K, Farragher SM, Jellema GL, Gluck S. Miller School of Medicine, Univ of Miami, Miami, FL; Almac Diagnostics, Durham, NC. 3056 Multicenter phase II randomized trial evaluating toxicities of concurrent and sequential radiotherapy and letrozole (COHORT) as adjuvant therapy after conservative surgery in postmenopausal women with hormone receptor positive tumors: preliminary results. Azria D, Ozsahin M, Rosenstein B, Romieu G, Gutowski M, Zaman K, Llacer Moscardo C, Lemanski C, Jeanneret-Sozzi W, Gligorov J, Gourgou S, Larbouret C, Pelegrin A, Dubois J-B, Belkacemi Y. CRLC Val d’Aurelle, Montpellier, France; Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; NYU School of Medicine, New York, NY; AP-HP CancerEst Tenon, Paris, France; CLCC Oscar Lambret, Lille, France. 3057 Distant metastasis: the most common type of early recurrence with adjuvant tamoxifen therapy. Doughty JC, Wilson CR, Monypenny IJ, Skene AI, Abram P, Gattuso J, Carpenter R, Angerson WJ, Mansell J. Western Infirmary, Glasgow, Scotland, United Kingdom; University of Wales College of Medicine, Cardiff, United Kingdom; Royal Bournemouth Hospital, Bournemouth, United Kingdom; Northern Ireland Cancer Centre, Ulster, United Kingdom; St. Bartholomew’s Hospital, London, United Kingdom. 3058 Acceptance of extended hormonal therapy with letrozole after 5 years of adjuvant tamoxifen in post menopausal breast cancer patients in Calgary, Alberta. Trotter T, Railton C, Webster M, Paterson AHG. Tom Baker Cancer Centre, Calgary, AB, Canada. 3059 Chronological changes of side effect profile of anastrozole compared with tamoxifen in Japanese women: findings from N-SAS BC03 trial every 3 months after one year of the randomization. Hozumi Y, Aihara T, Takatsuka Y, Osumi S, Aogi K, Imoto S, Iwata H, Watanabe T, Nakagami K, Ohashi Y. Jichi Medical University, Shimotsuke, Tochigi, Japan; Kansai Rosai Hospital, Amagasaki, Hyogo, Japan; Shikoku Cancer Center, Matsuyama, Ehime, Japan; National Cancer Center East, Kashiwa, Chiba, Japan; Aichi Cancer Center Central, Nagoya, Aichi, Japan; Hamamatsu Oncology Center, Hamamatsu, Shizuoka, Japan; Shizuoka General Hospital, Shizuoka, Japan; Tokyo University, Bunkyo-ku, Tokyo, Japan. 3060 First results of the prospective Hospital del Mar Bone Health Breast Cancer study (HMBHBC) in postmenopausal women receiving adjuvant aromatase inhibitors for early breast cancer. Nogues X, Servitja S, Velat M, Nadal R, Garces JM, Pena MJ, Albanell J, Diez-Perez A, Tusquets I. Hospital del Mar, Autonomous University Barcelona, Barcelona, Spain. 3061 Compliance with tamoxifen and arimidex in the adjuvant treatment of women with breast cancer. Hadji P, Ziller V, Holzhauer W, Ziller M, Kalder M, Wagner U. Philipps-University of Marburg, Marburg, Germany. 3062 Risk of contralateral breast cancer in patients receiving adjuvant aromatase inhibitor - the rate of positive biopsies for cancer. Castaner MC, Elledge R, Tham YL. Baylor College of Medicine, Houston, TX. 3063 Phase II feasibility trial incorporating bevacizumab into dose dense doxorubicin and cyclophosphamide followed by paclitaxel in patients with lymph node positive breast cancer: a trial of the Eastern Cooperative Oncology Group (E2104). Miller KD, O’Neill A, Perez EA, Seidman AD, Sledge GW. Indiana University Cancer Center, Indianapolis, IN; Dana Farber Cancer Institute; Mayo Clinic; Memorial Sloan Kettering Cancer Center. Treatment: Adjuvant Therapy 3053-3082 3053 A prospective study comparing clinical rheumatological findings and tenosynovial and synovial changes on magnetic resonance imaging of breast cancer patients receiving adjuvant aromatase inhibitors or tamoxifen. Morales L, Pans S, Verschueren K, Paridaens R, Westhovens R, Timmerman D, Desmet L, Marie-Rose C, Neven P. University Hospitals KULeuven, Belgium. 3054 A study of associations between estrogen and tamoxifen metabolism, cytochrome 2D6 and sulfotransferase 1A1 polymorphisms, and sulfotransferase 1A1 gene copy number during steady state tamoxifen treatment. Gjerde J, Geisler J, Lundgren S, Ekse D, Breilid H, Hauglid M, Varhaug JE, Mellgren G, Steen VM, Lonning PE, Lien EA. Section for Endocrinology, Institute of Medicine, University of Bergen, Norway; Section of Oncology, University of Bergen, Norway; Norwegian University of Science and Technology, Department of Cancer Research and Molecular Medicine, Norway; Haukeland University Hospital, Norway; Center for Medical Genetics and Molecular Medicine, Haukeland University Hospital, Norway; Institute of Medicine, University of Bergen, Norway; University of Bergen, Norway; Section of Oncology, University of Bergen, Bergen, Norway; Section for Endocrinology, University of Bergen, Norway. 3055 How compliant are patients with oral hormonal therapies? Data from a randomized, placebo controlled study of tamoxifen after adjuvant chemotherapy in premenopausal women with early breast cancer (NCIC CTG MA.12). Bramwell VHC, Pritchard KI, Tu D, Tonkin K, Vachhrajani H, Robert J, Arnold A, Vandenberg TA, O’Reilly SE, Graham B, Shepeherd LE. National Cancer Institute of Canada Clinical Trials Group, Queen’s University, Kingston, ON, Canada. 3064 BCIRG 006: quality of life (QoL) of patients (pts) treated with docetaxel and trastuzumab-based regimens in node positive and high risk node negative HER2 positive early breast cancer. Au H-J, Robert N, Eiermann W, Pienkowski T, Crown J, Martin M, Pawlicki M, Chan A, Bee V, Slamon D. Breast Cancer International Research Group (BCIRG), Edmonton, AB, Canada. 3065 Cardiac safety of adjuvant bevacizumab plus dose-dense doxorubicin/cyclophosphamide followed by nanoparticle albumin-bound paclitaxel in patients with early stage breast cancer. McArthur HL, Rugo H, Paulson M, Rourke M, Traina T, Panageas K, Steingart R, Dang C, Fornier M, Park J, Moasser M, Melisko M, Sugarman S, Norton L, Hudis CA, Dickler MN. Memorial SloanKettering Cancer Center, New York, NY; UCSF Comprehensive Cancer Center, San Francisco, CA. 3066 3067 Preliminary results of a multicenter study of bevacizumab with 3 docetaxel-based adjuvant breast cancer regimens. Yardley DA, Hart L, Badarinath S, Waterhouse DM, Daniel B, Childs BH, Burris III HA. Tennessee Oncology, Nashville, TN; Florida Cancer Specialists, Fort Meyers, FL; Integrated Community Oncology Network, Jacksonville, FL; Oncology Hematology Care, Cincinnati, OH; Chattanooga Oncology & Hematology Associates, Chattanooga, TN; Sanofi-Aventis, Bridgewater, NJ. Pre-anthracycline and herceptin cardiac scanning for adjuvant breast carcinoma: a retrospective analysis of results in Scotland’s biggest cancer centre. Lindsay CR, McIlroy P, Stirling L, Canney PA. Gartnavel General Hospital, Glasgow, Scotland, United Kingdom. 3068 Adjuvant trastuzumab uptake outside of clinical trials. Snow SL, Rayson D, Barnes PJ, Sellon M, Skedgel C, Dewar R, Weber A, Younis T. Queen Elizabeth II Health Sciences Centre, Halifax, NS, Canada; Cancer Care Nova Scotia, Halifax, NS, Canada. 3069 Final toxicity analysis of the ADEBAR phase III study evaluating the role of docetaxel in the adjuvant therapy of breast cancer patients with extensive lymph node involvement. Janni W, Harbeck N, Sommer H, Rack B, Augustin D, Simon W, Jueckstock J, Wischnik A, Annecke K, Friese K, Kiechle-Bahat M. LMU, Munich, Germany; Frauenklinik, Deggendorf, Germany; Frauenklinik, Stuttgart, Germany; Frauenklinik, Augsburg, Germany; Klinikum Rechts der Isar TU, Munich, Germany. 3070 T1N0 triple negative breast cancer: adjuvant chemotherapy treatment and risk of recurrence. Kaplan HG, Malmgren JA, Atwood MK. Swedish Cancer Institute, Seattle, WA; HealthSTAT Consulting, Inc, Seattle, WA. 3071 The incidence of thromboembolism in patients receiving adjuvant anthracycline based chemotherapy for early stage breast cancer. Nolan L, Boleti E, Darby A, Simmonds PD. Southampton University Hospitals NHS Trust, Southampton, United Kingdom. 3072 Chemotherapy dose delays and dose reductions in breast cancer patients receiving dose-dense FEC and docetaxel results of a randomized, open-label phase II study. Wildiers H, Dirix L, Neven P, Prové A, Clement P, Amant F, Skacel T, Paridaens R. University Hospital Gasthuisberg, Leuven, Belgium; St-Augustinus Hospital, Wilrijk, Belgium; Amgen (Europe) GmbH, Zug, Switzerland. 3073 A feasibility study of capecitabine monotherapy for elderly patients with high risk early breast cancer. Bernard-Marty C, Widakowich C, Demonty G, Personeni N, Lebrun F, Paesmans M, Veys I, Lieutenant F, Kabanga E, Biganzoli L, Nogaret J-M, Piccart MJ, Cardoso F. Jules Bordet Institute, Brussels, Belgium; Prato Hospital, Prato, Italy. 3074 Delivery of adjuvant dose dense doxorubicin+cyclophosph amide¢paclitaxel to early stage breast cancer patients with pegfilgrastim and darbepoetin alfa support - interim results from an Australian phase II study. De Boer RH, Patterson W, Beith J, Rocchi L, Beer F, Lewis C. Royal Melbourne Hospital, Melbourne, Victoria, Australia; Queen Elizabeth Hospital, Woodville, South Australia, Australia; Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia; Amgen Australia Pty Ltd, Hawthorn, Victoria, Australia; Prince of Wales Hospital, Randwick, New South Wales, Australia. 3075 A pilot study to investigate the feasibility and cardiac effects of pegylated liposomal doxorubicin (PL-DOX) as adjuvant therapy in elderly breast cancer patients. Wildiers H, Jurcut R, Denys H, de Backer J, Ganame J, Herbots L, Neven P, Cocquyt V, Rademakers F, Voigt J-u, Paridaens R. University Hospital Gasthuisberg, Leuven, Belgium; University Hospital Gent, Gent, Belgium. 3076 Adjuvant chemotherapy in breast cancer patients older than 70 years. Garg P, Rana F, Guthrie TH. University of Florida, Jacksonville, FL; Baptist Cancer Center, Jacksonville, FL. 3077 Annual hazard rates of recurrence for early breast cancer. What has changed in the last 10 years? Results from the NORA study. Cazzaniga ME, Mustacchi G, Pronzato P, De Matteis A, Di Costanzo F, Nardi M, Barberis G, D’Aprile M, Rulli E, Floriani I. Az Osp Treviglio-Caravaggio, Treviglio, Bergamo, Italy. 3078 Do patients with infiltrating lobular carcinoma (ILC) have an increased risk of contralateral, local, or distant recurrences compared with patients with infiltrating ductal carcinoma (IDC)? Pestalozzi BC, Zahrieh D, Mallon E, Gusterson B, Gelber R, Price K, Castiglione-Gertsch M, Coates A, Goldhirsch A. International Breast Cancer Study Group, Berne, Switzerland. 3079 Prognostic effect of amenorrhea and return of menses after adjuvant treatment of premenopausal patients with nodepositive breast cancer. Jonat W, Sauerbrei W, Kaufmann M, Schumacher M. UKSH Schleswig Holstein, Kiel, Germany; Universitätsklinikum Freiburg, Freiburg, Germany; University of Frankfurt, Frankfurt, Germany. 3080 Detection of minimal residual disease (MRD) in peripheral blood of primary breast cancer patients - translational research in the SUCCESS-study. Jueckstock JK, Rack B, Thurner-Hermanns E, Forstbauer H, Pantel K, Ulmer H-U, Beckmann MW, Lichtenegger W, Janni WJ, Friese K, Sommer HL. Frauenklinik, Klinikum Innenstadt, Munich University, Munich, Bavaria, Germany; Klinikum Rosenheim, Rosenheim, Bavaria, Germany; Oncologic Practice Dr. Forstbauer/ Dr. Ziske, Troisdorf, Nordrhein-Westfalen, Germany; University Hamburg-Eppendorf, Hamburg, Germany; Klinikum Karlsruhe, Karlsruhe, Baden-Wuerttemberg, Germany; Frauenklinik, University of Erlangen, Erlangen, Bavaria, Germany; Charite Universitaetsmedizin, Berlin, Germany. 3081 Biological risk assessment based on snap frozen tissue samples. Feasibility, qualitiy assuance and study progress of the multicenter trial NNBC 3-Europe. Thomssen C, Vetter M, Geurts-Moespot A, Persing M, Paepke D, Schmidt M, Meisner C, von Minckwitz G, Sweep F, Harbeck N. Martin-Luther Universitaet, Halle/Saale, Germany; Radboud Universiteit, Nijmegen, Netherlands; Technische Universitaet Muenchen, Muenchen, Germany; Johannes-Gutenberg Universitaet, Mainz, Germany; Eberhard-Karls Universitaet, Tuebingen, Germany; German Breast Group, Neu-Isenburg, Germany. 3082 Evaluation of practice patterns in the treatment of nodenegative, hormone-receptor positive breast cancer patients with the use of the oncotype DX assay at the University of Pennsylvania. Erb C, Fox KR, Patel M, Hook K, DeMichele A, Kaplan C, Domchek S. University of Pennsylvania, Philadelphia, PA. 3094 Targeting up-regulated notch signaling in the CD133+ stem cells within the protected niche of the lymphovascular embolus of inflammatory breast cancer. Barsky SH, Xiao Y, Ye Y. The Ohio State University College of Medicine, Columbus, OH. 3095 The overexpression of ERBB receptor tyrosine kinases and ABC transporters is associated with an increased side population in hormone resistant breast cancer cells. Chumsri S, Nakanishi T, Phatak P, Macedo LF, Sabnis G, Hamburger AW, Brodie AH, Burger AM. University of Maryland Greenebaum Cancer Center, Baltimore, MD; University of Maryland School of Medicine, Baltimore, MD. 3096 CTEN and LKB1: novel tumor biomarkers for breast cancer implications of resistance and response to tyrosine kinase inhibitor (TKI)-based therapies in breast cancer. Yarden Y, Shell SA, Spector NL, Bacus SS. Targeted Molecular Diagnostics, Westmont, IL; Duke University Medical Center, Durham, NC; Weizmann Institute of Science, Rehovot, Israel. 3097 HER2 increases the translational rates of acetyl-CoA carboxylase alpha and fatty acid synthase in breast cancer cells. Lee MJ, Park B-W, Yoon S, Lee M-Y, Kim K-S, Kim J-H, Park S-H. Yonsei University, College of Medicine, Seoul, Korea; Yonsei University, College of Medicine, Korea. 3098 The identification of proteins associated with radiotherapy resistance in breast cancer cells: screening 725 antibodies simultaneously using novel microarray technology. Smith L, Qutob O, Watson MB, Beavis AW, Lind MJ, Drew PJ, Cawkwell L. University of Hull, Hull, East Yorkshire, United Kingdom. 3099 A combined proteomic and microarray screening approach for the identification of proteins associated with radiotherapy resistance in breast cancer cells. Smith L, Qutob O, Watson MB, Beavis AW, Jameel JK, Welham KJ, Drew PJ, Lind MJ, Cawkwell L. University of Hull, Hull, East Yorkshire, United Kingdom. 3100 Genomic signature of invasive lobular cancer by DNA array hybridization. Hwang ES, Devries S, Roydasgupta R, Fridlyand J, Chin K, Chen Y-Y, Korkola J, Waldman FM. University of California, San Francisco, CA; Memorial Sloan Kettering Cancer Center, New York, NY. 3101 The genomic relationship between breast carcinomas and their paired lymph node metastases. Desouki MM, Gaile DP, Conroy J, McQuaid D, Nowak NJ, Shepherd L, Liao S, Geradts J. Medical University of South Carolina (MUSC), Charleston, SC; State University of New York, Buffalo, NY; Roswell Park Cancer Institute, Buffalo, NY; Duke University Medical Center, Durham, NC. 3102 A Q-RT PCR profile for the cytological diagnosis of early breast lesions. Delaloge S, Laurent I, Scott V, Dessen P, Andre F, Suciu V, Saghatchian M, Lazar V, Lidereau R, Michiels S, Vielh P. Institut Gustave Roussy, Villejuif, France; Centre Rene Huguenin, Saint Cloud, France. 3103 Breast cancer classication according to “stem cell-like” features and its relevance for systemic adjuvant treatment decision. Rody A, Holtrich U, Gätje R, Engels K, von Minckwitz G, Loibl S, Gehrmann M, Ruckhäberle E, Ahr A, Solbach C, Karn T, Kaufmann M. J.W. Goethe-University, Frankfurt, Germany; German Breast Group, Neu-Isenburg, Germany; Siemens Medical Solutions Diagnostics GmbH, Leverkusen, Germany. Treatment: Hormone Replacement Therapy 3083-3087 3083 Reduced use of HRT by women in Victoria Australia in 2002 was not followed by a fall in breast cancer incidence. Bell R, Chappell G, Stagoll O, Maljevac S, Wilkinson J, Giles GG. The Geelong Hospital, Barwon Health, Geelong, Victoria, Australia; BreastScreen Victoria, Melbourne, Victoria, Australia; Victorian Cancer Registry, Melbourne, Victoria, Australia. 3085 The effects of vaginal estrogens on plasma estradiol levels in women taking aromatase inhibitors. Howard G, Wills S, Kresge C, McConnell D, Balasubramaniam M, Decker D. William Beaumont Hospital, Royal Oak, MI; School of Public Health, University of Michigan, Ann Arbor, MI. 3086 Use of hormonal therapies before and after diagnosis of a high risk breast lesion among 1,198 women in the community setting. Habel LA, Puligandla B, Jiang SF, Callahan ME, Kutner S, Shim V. Kaiser Permanente, Oakland, CA; Kaiser Permanente, Santa Teresa, CA. 3087 The multidisciplinary management of menopause symptoms after breast cancer. Saunders CM, Hickey M, Stuckey B. University of Western Australia, Perth, WA, Australia; Sir Charles Gairdner Hospital, Perth, WA, Australia. Tumor Cell Biology: Apoptosis 3088-3089 3088 Protein kinase C-epsilon and -eta confers TRAIL resistance in breast cancer cells via distinct mechanisms. Persaud SD, Jain K, Shankar E, Basu A. University of North Texas Health Science Center, Fort Worth, TX. 3089 Naphthaquinones - Promising anticancer agents against breast and ovarian cancers. Thasni AK, Nair RS, Rojini G, Ratheeshkumar T, Gopal S, Banergji A, Srinivas P. Rajiv Gandhi Centre for Biotechnology, Trivandrum, Kerala, India. Tumor Cell Biology: Carcinogenesis 3090-3092 3090 Contribution of chromosomal alterations to the development of poorly-differentiated invasive breast carcinomas. Ellsworth RE, Hooke JA, Ellsworth DL, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 3091 Mouse mammary tumor virus-related sequence expression in the patients with breast phyllodes tumors. Luschnikova AA, Parokonnaya AA, Lyubchenko LN, Polevaya EB, Peredereeva EV, Smirnova EG. N.Blochin Cancer Research Center RAMS, Moscow, Russian Federation. 3092 Interactions between breast cancer cells and their stromal component: an analysis of alterations in gene expression. Sotiriou C, El Ouriaghli F, Majjaj S, Haibe-Kains B, Desmedt C, Lallemand F, Larsimont D, Piccart M. Institut Jules Bordet, Brussels, Belgium; Université Libre de Bruxelles (U.L.B.), Brussels, Belgium. Tumor Cell Biology: Tumor Biology 3093-3112 3093 Insulin sensitivity gene expression and efficacy of systemic adjuvant therapy in women with early breast cancer. Gennari A, Sormani M, Bruzzi P, Pronzato P, Mirisola V, Ravera G, Pfeffer U. National Cancer Rsearch Institute, Genoa, Italy; University of Genoa, Genoa, Italy. 3104 DNA hypermethylation profile of inflammatory breast cancer. Van der Auwera I, Van den Bosch S, Van Laere SJ, Van den Eynden GG, van Dam P, Colpaert CC, van Engeland M, Van Marck EA, Vermeulen PB, Dirix LY. Translational Cancer Research Group (Laboratory of Pathology University of Antwerp/ University Hospital Antwerp, Edegem; Oncology Centre, General Hospital St-Augustinus, Wilrijk), Wilrijk, Antwerp, Belgium; Research Institute GROW, Maastricht, Netherlands. 3105 Changes of stromal protein expression after preoperative systemic therapy in breast cancer. Szasz AM, Tokes A-M, Toth AI, Farkas A, Dank M, Molnar IA, Harsanyi L, Kulka J. Semmelweis University, Budapest, Hungary. 3106 3107 Vitronectin in the tumor microenvironment promotes breast cancer cell proliferation and elevated protein synthesis despite hypoxia by integrin Ĝvĝ3 activation of the mTOR/4E-BP1 pathway. Pola C, Formenti SC, Schneider RJ. New York University School of Medicine, New York, NY. Caveolin-1 enhances the growth inhibitory effects of gefitinib in MCF-7 breast cancer cell line. Agelaki S, Spiliotaki M, Markomanolaki Ch, Kallergi G, Stournaras Ch, Georgoulias V. University General Hospital of Heraklion, Heraklion, Crete, Greece; School of Medicine, University of Crete, Heraklion, Crete, Greece. 6054 The breast cancer surveillance consortium: a platform for collaborative research stemming from breast cancer risk through survivorship research. Geller BM, Ballard-Barbash R, Buist DSM, Carney PA, Kerlikowske K, Miglioretti DL, Rosenberg RD, Taplin SH, Yankaskas B, Weaver DL. University of Vermont, Burlington, VT; National Cancer Institute, Bethesda, MD; Group Health Cooperative Center for Health Studies, Seattle, WA; Dartmouth College, Lebanon, NH; UCSF, San Francisco, CA; University of New Mexico, Albuquerque, NM; University of North Carolina, Chapel Hill, NC. 6093 Second nonbreast malignancies following breast cancer in the Japanese female population. Sato N, Kanbayashi C, Sano M. Niigata Cancer Center Hospital, Niigata, Japan; Niigata Breast Examination Center, Niigata, Japan. Saturday, December 7:00-9:00 POSTER DISCUSSION 4 & CONTINENTAL BREAKFAST – Ballroom B Estrogen Receptors 401-409 401 Patterns of estrogen receptor alpha (ER) protein expression and ESR1 gene amplification in primary and metastatic breast cancer. Holst F, Haas H, Nottbohm AK, Sauter G, Simon R. University Medical Center Hamburg-Eppendorf, Hamburg, Germany. 402 Amplification of ESR1 may predict resistance to adjuvant tamoxifen in postmenopausal patients with hormone receptor positive breast cancer. Ejlertsen B, Nielsen KV, Rasmussen BB, Balslev E, Müller S, Møller S, Mouridsen HT. Rigshospitalet, Copenhagen, Denmark; Dako A/S, Glostrup, Denmark. 403 Relationship between ESR1 copy number and ER expression in the DBCG 89D trial. Ejlertsen B, Nielsen KV, Rasmussen BB, Jensen M-B, Møller S, Balslev E, Müller S, Mouridsen HT. Rigshospitalet, Copenhagen, Denmark; Dako A/S, Glostrup, Denmark. 404 Gene copy number variability of oestrogen receptor-Ĝ in breast cancer. Drury S, Lambros, Marchio, Johnson, Salter J, Levey, Fletcher, Peto, Reis-Filho J, Dowsett M. The Breakthrough Breast Cancer Research Centre, London, United Kingdom; CR-UK Epidemiology & Genetics, LSHTM, London, United Kingdom. 405 Serine118 phosphorylation of estrogen receptor: correlation with kinase pathways and evolution after preoperative endocrine therapy. Zoubir M, Mathieu M-C, Simmans F, Bouaziz J, Geha S, Drusch F, Liedtke C, Spielmann M, Delaloge S, Andre F. Institut Gustave Roussy, Paris, France; MD Anderson Cancer Center, Houston, TX. 406 Induction of a novel estrogen receptor (ERĜ) phosphoserine (S154) in human breast cancer cells identified by mass spectrometry. Britton D, Scott G, Schilling B, Held J, Atsriku C, Baldwin M, Gibson B, Benz C. Buck Institute for Age Research, Novato, CA. Rescheduled Posters 407 Withdrawn 1031 408 Mitogen activated protein kinase (MAPK) regulation of estrogen receptor (ER) Ĝ and tamoxifen resistance. Cui Y, Fuqua SAW. Baylor College of Medicine, Houston, TX. 3108 3109 The downregulation of cyclin B1 sensitizes the antiproliferative effect of chemotherapeutics in breast cancer cells. Yuan J, Androic I, Kramer A, Kaufmann M, Strebhardt K. Medical School, J.W. Goethe-University, Frankfurt, Hessen, Germany. ER dependent regulation of sphingolipid metabolism in the context of apoptosis and proliferation in breast cancer. Ruckhäberle E, Karn T, Schiffmann S, Grösch S, Geisslinger G, Gätje R, Holtrich U, Rody A, Kaufmann M. J.W. Goethe University, Frankfurt, Germany. 3110 Studies on the role of nicotinic receptors-mediated cell proliferative effects in human breast cancer cells. Wu C-H, Ho Y-S. Taipei Medical University, Taipei, Taiwan. 3111 Osteocalcin as a prognostic indicator in ductal mammary carcinoma. Davies SR, Mansel RE, Jiang WG. College of Medicine, Caridiff University, Cardiff, South Glamorgan, United Kingdom. 3112 Expression and activity of core binding factor (CBF) in human breast cancer cells. Yong T, Fowler M, Davis N, Meyers S, Sun A. Louisiana State University Health Sciences Center, Shreveport, LA. Prognosis and Response Predictions: Prognostic Factors I 3113 3113 Immunohistochemical expression of YKL-40 is not a prognostic marker in patients with high-risk primary breast cancer. Roslind A, Knoop AS, Jensen M-B, Johansen JS, Nielsen DL, Price PA, Balslev E. Herlev University Hospital, Copenhagen, Denmark; Odense University Hospital, Odense, Denmark; Copenhagen, Denmark; University of California San Diego, La Jolla, CA. Why women with breast cancer do not return for surveillance mammography. Geller B, Skelly J, Muss H. University of Vermont, Burlington, VT; Vermont Cancer Center, Burlington, VT. 409 Single nucleotide polymorphism 3814 C>T (P1272S) in steroid receptor coactivator-1 alters its coactivation activity. Richter AS, Hartmaier RJ, Lee AV, Skaar T, Rae J, Li L, Flockhart D, Tchatchou S, Hemminki K, Schmutzler RK, Meindl A, Bartram CR, Burwinkel B, Oesterreich S. Baylor College of Medicine, Houston, TX; Indiana University, Indianapolis, IN; University of Michigan, Ann Arbor, MI; DKFZ, Heidelberg, Germany; University of Cologne, Cologne, Germany; Klinikum Rechts der Isar TU, Munich, Germany; University of Heidelberg, Heidelberg, Germany. 7:00-9:00 4007 Risk categorisation of node positive tamoxifen treated breast cancer patients based on genetically defined subtypes. Schmidt M, Span P, Müller V, Rody A, von Törne C, Sweep F, Gehrmann M. University of Mainz, Mainz, Germany; Radboud University Nijmegen, Nijmegen, Netherlands; University of Hamburg-Eppendorf, Hamburg, Germany; Goethe-University Frankfurt, Frankfurt, Germany; Siemens Medical Solutions, Leverkusen, Germany. 4008 ABCB1 MDR1) inherited polymorphisms in relation to doxorubicin and docetaxel pharmacokinetics in patients with breast cancer. Gligorov J, Selle F, Lévy E, Beerblock K, Saintigny P, Avenin D, Rezai K, Bernaudin J-F, Uzan S, Antoine M, Lévy P, Lokiec F, Fajac A. Hôpital Tenon, Paris, France; HEGP, Paris, France; Hôpital Avicenne, Bobigny, France; Centre René Huguenin, Saint-Cloud, France. 4009 Breast cancer proteomic profiles of tumor susceptibility to neoadjuvant chemotherapy. He J, Shen D, Chung D, Saxton R, Faull KF, Whitelegge JP, Chang HR. School of Medicine, UCLA, Los Angeles, CA. 4010 47% pathologic complete response rate to anthracyclinesbased associated with high cyclophosphamide doses neoadjuvant chemotherapy in basal-like and triple negative breast cancer patients. Le Tourneau C, Dettwiler S, Laurence V, Alran S, Beuzeboc P, Pierga J-Y, Frenaux P, Sigal-Zafrani B, Dieras V, Vincent-Salomon A. Institut Curie, Paris, France. 4011 Pharmacogenetic influences on outcome from AC chemotherapy in the treatment of breast cancer. Lee JS, Verrill MW, Sludden J, Griffin MJ, Erb S, Sumpter KA, Cole M, Calvert AH, Boddy AV. Newcastle University, Newcastle upon Tyne, Tyne & Wear, United Kingdom; Newcastle General Hospital, Newcastle upon Tyne, Tyne & Wear, United Kingdom. 4012 COX-2 over-expression and sensitivity to celecoxib and capecitabine in metastatic breast cancer patients. Metro G, Melucci E, Sperduti I, Mottolese M, Papaldo P, Milella M, Carlini P, Ferretti G, Cognetti F, Fabi A. Regina Elena National Cancer Institute, Rome, Italy. 4013 Thymidine phosphorylase expression is associated with time to progression in patients receiving docetaxel-modulated capecitabine for metastatic breast cancer. Puglisi F, Cardellino GG, Di Loreto C, Lombardi D, Perin T, Puppin C, Andreetta C, Russo S, Minisini AM, Mansutti M, Pizzolitto S, Adami G, Dipasquale M, Veronesi A. Azienda OspedalieroUniversitaria, Udine, Italy; CRO di Aviano, Aviano (PN), Italy; General Hospital, San Daniele del Friuli, Italy. 4014 The presence of the FRA12E/SMRT fragile site in the genome of breast cancer (BC) patients is a predictor of metastatic development. O’Connor T, Houde C, Dolce J, Bundy B, Nesline M, Davis W, Ambrosone C, Levine E, Edge SB, Coignet LJ. Roswell Park Cancer Institute, Buffalo, NY. 4015 Correlation of IGF1R gene expression and mutations with the risk of local recurrence in early breast carcinoma treated with conservative surgery and radiation therapy. Adrover E, Peiró G, Benlloch S, Sánchez-Tejada L, Lerma E, Peiró FM, Aranda FI. Universitary General Hospital, Alicante, Spain; Sant Paús Hospital, Barcelona, Spain. 4016 A retrospective clinical correlation study of the breast cancer patients’ responses to anticancer drugs with the expression level of drug response indicators (DRI) measured in patient’s archival tumor tissue. Rak Tkaczuk KH, Tait NS, Rogers WH, Tan M, Ioffe O, Lesko SA, Deamond S, Lum Z-P, Ts’o PO. University of Maryland Greenebaum Cancer Center, Baltimore, MD; CCC Diagnostics LLC, Baltimore, MD. POSTER SESSION 4 & CONTINENTAL BREAKFAST– Exhibit Hall B (#4001-4117) Prognosis and Response Prediction: Predictive Factors II 4001-4025 4001 4002 4003 4004 4005 4006 Early changes in expression of oestrogen-regulated and proliferation genes illustrate heterogeneity in primary resistance to letrozole. Miller WR, Larionov A, Evans DB, Dixon M. University of Edinburgh, Edinburgh, United Kingdom; Novartis Institutes for BioMedical Research, Basel, Switzerland. Radiation-induced CD8 T-lymphocyte apoptosis yield predicts toxicities after adjuvant treatment with concurrent and sequential radiotherapy and letrozole in postmenopausal women with hormone receptor positive breast cancers: preliminary results of the multicenter phase II randomized trial (COHORT). Ozsahin M, Belkacemi Y, Rosenstein B, Llacer Moscardo C, Lemanski C, Romieu G, Gutowski M, Zaman K, Jeannerat-Sozzi W, Gourgou S, Gligorov J, Larbouret C, Pèlegrin A, Dubois J-B, Azria D. Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; Centre Oscar Lambret, Lille, France; Mount Sinai School of Medicine and NYU School of Medicine, NY, NY; CRLC Val d’Aurelle, Montpellier, France; AP-HP CancerEst Tenon, Paris, France; Centre de Recherche en Cancérologie de Montpellier, Montpellier, France. Signal pathway profiling of primary breast tumors identifies potential phosphoprotein biomarkers that are predictive for tamoxifen response following recurrence. Wulfkuhle J, Umar A, Deng J, Timmermans M, Liotta L, Foekens J, Petricoin E. George Mason University, Manassas, VA; Erasmus Medical Center, Rotterdam, Netherlands. Selective serotonin reuptake inhibitors and modification of tamoxifen effectiveness in Danish breast cancer patients. Lash T, Cronin-Fenton D, Pedersen L, Ahern T, Sorensen HT, Lunetta K, Rosenberg C, Silliman R, Hamilton-Dutoit S, Garner JP, Ewertz M. Boston University, Boston, MA; Aarhus University Hospital, Aarhus, Denmark; Aalborg Hospital, Aalborg, Denmark. Predictive gene expression profile of breast cancer patients treated with tamoxifen. Lyng MB, Laenkholm AV, Vach W, Pallisgaard N, Knoop A, Ditzel HJ. Odense University Hospital (OUH); University of Southern Denmark (SDU); SDU; OUH, Odense, Denmark. Biomarker analysis of a phase II double-blind randomized trial of daily oral RAD001 (everolimus) plus letrozole or placebo plus letrozole as neoadjuvant therapy for patients with estrogen receptor positive breast cancer. Gardner H, Bandaru R, Barrett C, Calcaterra M, Crowell T, Decker J, Dixon M, Fisch R, Fuchs M, Gelb A, Hanoteau N, Jonat W, Lane H, Lebwohl D, Liu W-H, Molloy B, Pena C, Phillips P, Rheinhardt J, Rugo H, Salesky S, Steinseifer J, Stumm M, Tokaji E, Voelker F, Yarbrough G, Yateman N, Yu Y, Zuber E, Baselga J. Novartis Institutes for Biomedical Research, Cambridge, MA; Novartis Pharmaceuticals, East Hanover, NJ; Hospital Vall d’Hebron, Barcelona, Spain; Novartis Pharma AG, Basel, Switzerland; UnivFrauenklinik, Kiel, Germany; UCSF, San Francisco; Western General Hospital, Edinburgh, United Kingdom. 4017 4028 Withdrawn 4029 Traditional breast cancer risk factors and common breast pathologies in post-menopausal women. Maskery SM, Hu H, Liebman M, Hooke J, Shriver CD, Taioli E. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC; University of Pittsburgh, Pittsburgh, PA. 4030 Validation of the Gail model for breast cancer risk in postmenopausal women with osteoporosis. Goldstein S, Yeo A, Qu Y, Wong M, Mitchell B, Mershon J. NYU, New York, NY; Eli Lilly and Company, Indianapolis, IN. 4031 A pilot study of known or controversial breast cancer risk factors using the Clinical Breast Care Project database as a research environment. Bekash A, Maskery SM, Kvecher L, Hooke J, Liebman MN, Shriver CD, Mural RJ, Hu H. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 4032 Prognostic determinants in patients with breast cancer who are staged using sentinel lymph node biopsy. Rosman M, Cheng Z, Sawyer K, Verbanac K, Tafra L. Anne Arundel Medical Center, Annapolis, MD; East Carolina University, Greenville, NC. Absolute breast fibroglandular volume strongly associated with breast cancer risk. Shepherd JA, Kerlikowske K, Malkov S, Ma L, Margolin F, Cummings S. University of California at San Francisco, San Francisco, CA; California Pacific Medical Center, San Francisco, CA. 4033 Significance of Akt activation and compartmentalization for prediction of outcome in Her-2 positive breast cancer patients treated with trastuzumab. Svoboda M, Grell P, Fabian P, Radova L, Palacova M, Nenutil R, Vyzula R. Masaryk Memorial Cancer Institute, Brno, Czech Republic; Tomas Bata University in Zlin, Zlin, Czech Republic. Large errors in volumetric fibroglandular density occur if breast thickness and paddle tilt are not measured. Shepherd JA, Malkov S, Cummings S. University of California at San Francisco, San Francisco, CA; California Pacific Medical Center, San Francisco, CA. 4034 The ratio of the estradiol metabolites 2-hydroxyestrone (2OHE1) and 16a-hydroxyestrone (16aOHE1) predicts breast cancer risk in postmenopausal but not in premenopausal women - a case-control study. Huober J, Zimmermann B, Brunner S, Mueck AO, Wallwiener D, Seeger H. Kantonsspital St. Gallen, St. Gallen, Switzerland; University Womens Hospital, Tuebingen, Germany. 4035 Type II diabetes and breast cancer; a potentially modifiable risk factor? Jones K, George RL. Kingston General Hospital, Queen’s University, Kingston, ON, Canada. 4036 Reproductive risk factors and breast tumor characteristics in African American and non-Hispanic White women with early onset breast cancer. Ogutha J, Huo D, Olopade OI. The University of Chicago Medical Center, Chicago, IL. 4037 Sub epithelial impedance: a new biomarker of breast cancer risk. Greene T, Brumfield MK, Pierce M, Davies RJ. Hackensack University Medical Center, Hackensack, NJ. 4038 The OncoVue® model for predicting breast cancer risk. Jupe ER, Ralph DA, Manjeshwar S, Knowlton NS, Pugh TW, DeFreese DC, Gramling BA, Shimasaki CD. InterGenetics Incorporated, Oklahoma City, OK; NSK Statistical Solutions, LLC, Choctaw, OK. Estrogen receptor status: a prognostic predictor of outcome in HER-2 positive breast cancer with brain metastases. Vallow L, Hines S, Jain A, Tan W, Buskirk S, Perez EA. Mayo Clinic, Jacksonville, FL. 4018 The potential prognostic value of osteoprotegrin in ductal carcinoma of the breast. Davies SR, Mansel RE, Jiang WG. College of Medicine, Cardiff University, Cardiff, South Glamorgan, United Kingdom. 4019 The initial response of circulating epithelial tumor cells to primary systemic chemotherapy in breast cancer is highly predictive for final tumor reduction and outcome. Camara O, Kavallaris A, Rengsberger M, Koch A, Schneider U, Egbe A, Untch M, Pachmann K. Friedrich Schiller-Universität Jena, Jena, Germany; Helios Klinikum Berlin-Buch, Berlin, Germany; Transfusionsmedizinisches Zentrum Bayreuth, Bayreuth, Germany. 4020 4021 4022 Predictors of response to neoadjuvant chemotherapy in women with locally advanced breast cancer. Parmar V, Nadkarni MS, Hawaldar R, Shet T, Nair R, Gupta S, Chinoy R, Badwe R. Tata Memorial Hospital, Mumbai, Maharashtra, India. 4023 Use of flow cytometry to identify breast cancer patients likely to benefit from specific targeted therapies. Visram H, Sangrar W, George R, Greer P. Queen’s University, Kingston, ON, Canada. 4024 Is pathologic complete response related to level of hormonal receptor positivity in hormonal-sensitive breast cancer treated with anthracycline-based neo-adjuvant chemotherapy? Petit T, Wilt M, Velten M, Rodier J-F, Fricker J-P, Dufour P, Ghnassia J-P. CLCC Paul Strauss, Strasbourg, France. 4025 Serum markers predictive of chemotherapy-induced premature ovarian failure among premenopausal women with early stage breast cancer. Anders CK, Snyder SA, Gu L, Unruhe SP, Welch RA, Lyons PS, Kimmick GG, Marcom KP, Shaw HS, Antenos M, Woodruff TK, Blackwell KL. Duke University, Durham, NC; Northwestern University, Chicago, IL. Risk and Prevention: Risk Factors 4026-4038 4026 4027 Women with elevated body mass index at increased risk of breast cancer with a poor prognosis. Kerlikowske K, Desai A, Miglioretti DL, Walker R, Ballard-Barbash RSM, Buist DSM. UCSF, San Francisco, CA; John Hopkins, Baltimore, MD; Group Health, Seattle, WA; National Cancer Institute, Bethesda, MD. Risk factors for developing breast cancer following benign breast disease: a 25-year follow-up of a nationwide cohort. Papa MZ, Chetrit A, Oberman B, Feldman D, Lubin F, Sadetzki S. Chaim Sheba Medical Center, Ramat-Gan, Israel; Gertner Institute for Epidemiology and Health Policy Research, RamatGan, Israel; Tel-Aviv University, Tel-Aviv, Israel. Risk and Prevention: Prevention 4039-4055 4039 A study of relationship between lipophilic statin use and estrogen receptor negative breast cancers. Gupta S, Desai A. Albert Einstein Medical Center, Philadelphia, PA. 4040 4041 4042 Phase II tissue-based biomarker prevention trial of celecoxib in premenopausal women at high risk for development of breast cancer. Fabian CJ, Kimler BF, Mayo MS, Zalles CM, Khan SA, Dooley WC, Krontiras H, Browne D. University of Kansas Medical Center, Kansas City, KS; Yale University, New Haven, CT; Northwestern University Medical Center, Chicago, IL; University of Oklahoma Health Science Center, Oklahoma City, OK; University of Alabama Birmingham, Birmingham, AL; National Cancer Institute, Bethesda, MD. Immunomodulatory effects of celecoxib in patients at increased risk for breast cancer. Arun B, Vuskovic M, Vasiliu D, Xu HY, Atchley D, Chambers J, Bovin N, Sneige N, Hortobagyi GN, Huflejt M. The University of Texas M.D. Anderson Cancer Center, Houston, TX; Cellexicon, Inc, La Jolla, CA; Shemyakin Institute of Bioorganic Chemistry RAS, Moscow, Russian Federation. Cumulative effects of raloxifene on the incidence of breast cancer over 8 years in postmenopausal women with osteoporosis. Mershon J, Yeo A, Qu Y, Wong M, Mitchell B, Vogel V. Eli Lilly and Company, Indianapolis, IN; University of Pittsburgh, Pittsburgh, PA. 4043 Incidence of breast cancer in postmenopausal women after discontinuation of long-term raloxifene use. Vogel V, Qu Y, Wong M, Mitchell B, Mershon J. University of Pittsburgh, Pittsburgh, PA; Eli Lilly and Company, Indianapolis, IN. 4044 Relative cost-effectiveness of raloxifene and tamoxifen in chemo-prevention of breast cancer with less thromboembolic events than no chemoprevention. Bishop JF, Glass P, Taylor PS, Pezzullo ML, Moore PT, Parkinson BT, Cotter TF, Tracey EA. Cancer Institute NSW, Sydney, Australia; Access Economics Pty Ltd, Canberra, Australia. 4045 Tamoxifen for the prevention of breast cancer development: an updated meta-analysis. Dahabreh IJ, Economopoulos KP. National University of Athens, Medical School, Athens, Greece. 4046 Prevention of breast cancer using rexinoids: results of a phase II biomarker modulation trial using bexarotene in women at high risk of breast cancer. Brown P, Arun B, Miller A, Isaacs C, Gutierrez C, Huang J, Mohsin S, Sneige N, Kim H, Sexton K, Weiss H, Hilsenbeck S, Lamph W, Negro-Vilar A, Johnson K, Elledge R. Baylor College of Medicine, Houston, TX; MD Anderson Cancer Center, Houston, TX; Cancer Therapy and Research Center, San Antonio, TX; Georgetown University, Washington, DC; Ligand Pharmaceuticals, San Diego, CA; National Cancer Institute, Bethesda, MD. 4047 Chemoprevention in a mouse model for ductal carcinoma in situ: targeting the mTOR pathway. Liu SY, Namba R, Enriquez RJ, Tepper CG, Young LJT, Abbey CK, Borowsky AD, Cardiff RD, Gregg JP. University of California, Davis, Sacramento, CA; University of California, Davis, CA; University of California, Santa Barbara, CA. 4048 A strong association between body fat mass and proteomes of nipple aspirate fluids. Huang Y, Nagamani M, Anderson KE, Kurosky A, Haag AM, Lu L-JW. University of Texas Medical Branch, Galveston, TX. 4049 Prophylactic mastectomy: pathological findings in high risk women. Sedlacek SM, Sedlacek JE. Rocky Mountain Cancer Centers, Denver, CO; Dartmouth College, Hanover, NH. 4050 A pilot study to increase physical activity in sedentary women at risk for breast cancer. Korde L, Venzon D, Smith AW, Nehrebecky M, Calhoun T, Sebring N, Drinkard B, Smith M, Prindiville S, Zujewski J, EngWong J. NCI; NIH Clinical Center. 4051 Improving informed consent in clinical trials: a randomised controlled trial of a decision aid for women invited to participate in a breast cancer prevention trial (IBIS-II). Juraskova I, Butow P, Lopez A-L, Seccombe M, Smith B, Coates A, Boyle F, McCarthy N, Reaby L, Forbes JF. University of Sydney, NSW, Australia; University of Newcastle, NSW, Australia; Royal Brisbane Hospital, QLD, Australia. 4052 Effect of green tea extract and tamoxifen on mammary carcinogenesis of C3H/OuJ mouse. Sakata M, Ikeda T, Imoto S, Jinno H, Kitagawa Y. Keio University School of Medicine, Shinjuku, Tokyo, Japan; Teikyo University School of Medicine, Itabashi, Tokyo, Japan; Kyorin University School of Medicine, Mitaka, Tokyo, Japan. 4053 Lyophilized aqueous extract of American ginseng (AG) abrogates induced COX-2 expression in human breast cancer cells. Minnis J, Louis S, Peralta E. Southern Illinois University School of Medicine, Springfield, IL. 4054 Conjugated linoleic acid synergizes with the CYP1B1 inhibitor 2,3’,4,5’-tetramethoxystilbene in suppressing breast cancer cell growth. Kirma NB, Nair HB, Liu Y-g, Tekmal RR. University of Texas Health Science Center @ San Antonio, San Antonio, TX. 4055 Serving the high risk patient in community practice: development and managment of a high risk clinic. Prill SJ, Vogel W. Blue Ridge Medical Specialists, Bristol, TN. Treatment: Antibody-Based Regimens 4056-4064 4056 Trastuzumab treatment beyond progression in patients with HER-2 positive metastatic breast cancer - the TBP study (GBG 26/BIG 3-05). von Minckwitz G, Vogel P, Schmidt M, Eidtmann H, Cufer T, de Jongh F, Maartense E, Zielinski C, Andersson M, Stein R, Nekljudova V, Loibl S. University Hospital Frankfurt, Frankfurt, Germany; German Breast Group, Neu-Isenburg, Germany; Klinik für Gynäkologie und Gynäkologische Onkologie, Wiesbaden, Germany; University Hospital Mainz, Mainz, Germany; Studienzentrale Gynäkologische Onkologie (SGO) Kiel, Kiel, Germany; Institute of Oncology Ljubljana, Ljubljana, Slovenia; Ikazia Zickenhuis, Rotterdam, Netherlands; Reinier de Graaf Gasthuies, Delft, Netherlands; University Hospital and Cancer Centre, Wien, Austria; Rigshospitalet University Hospital, Kopenhagen, Denmark; University College London Hospital, London, United Kingdom. 4057 Retrospective evaluation of clinical outcomes in HER2positive advanced breast cancer patients progressing on trastuzumab-based therapy in the pre-lapatinib era. Montemurro F, Viale G, Donadio M, Bottini A, Sanna G, Botti G, dei Tos AP, Marchiò C, Danese S, Clavarezza M, Del Curto B, Sapino A, Aglietta M. Institute for Cancer Research and Treatment, Candiolo, Italy; European Institute of Oncology, Milano, Italy; Centro Onco Ematologico Subalpino, Torino, Italy; Breast Unit Istituti Ospitalieri, Cremona, Italy; Istituto Nazionale Tumori (IST) Fondazione Senatore Pascale, Napoli, Italy; Ospedale Regionale, Trevisio, Italy; Ospedale S. Anna, Torino, Italy; Istituto Nazionale per la Ricerca sul Cancro (IST), Genova, Italy; Ospedale San Giovanni Battista- Molinette, Torino, Italy. 4058 4059 4060 4061 Evaluation of first-line trastuzumab in combination with epirubicin/cyclophosphamide for patients with HER2positive metastatic breast cancer. Untch M, Tjulandin S, Jonat W, Meerpohl H, Lichinitser M, Manikhas GM, Jänicke F, Muscholl M, Pauschinger M, Thomssen C, Lehle M. Frauenheilkunde mit Geburtshilfe, Berlin, Germany; Russian Cancer Research Center, Moscow, Russian Federation; Christian-Albrechts-Universität, Kiel, Germany; Frauenklinik der St-Vincentius-Krankenhäuser, Karlsruhe, Germany; St Petersburg City Oncology Hospital, Russian Federation; Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany; Ludwig-MaximiliansUniversität, Munich, Germany; Charité - Universitätsmedizin Benjamin Franklin, Berlin, Germany; Martin-Luther-Universität Halle-Wittenberg, Halle, Germany; F Hoffmann-La Roche, Basel, Switzerland. Clinical use of trastuzumab (Herceptin®) in metastatic breast cancer (MBC) in Germany from 2001 to 2006. Jackisch C, Eustermann H, Schoenegg W, Soelling U, Stauch M, Goehler T, Kuehn W, Krieger G, Reichert D. Klinikum Offenbach, Offenbach, Germany; Research Institute, Langen, Germany; Gynaekologische Praxis, Berlin, Germany; Gynaekologische Praxis, Kassel, Germany; Praxis, Kronach, Germany; Praxis, Dresden, Germany; Charité, Berlin, Germany; Hegau Klinikum, Singen, Germany; Klinikum Oldenburg, Germany. HER-2 positive inflammatory breast cancer: high pathological response rate with trastuzumab-based neoadjuvant therapy. Dawood S, Gonzalez-Angulo AM, Broglio K, Gong Y, Resetkova E, Yang WT, Barnett CM, Islam R, Ueno NT, Hortobagyi GN, Cristofanilli M. UT M.D. Anderson Cancer Center, Houston, TX. Survival gain by trastuzumab therapy after the onset of intracranial metastasis in metastatic breast cancer. Nam BH, Kim SY, Han HS, Lee KS, Ro J. National Cancer Center, Goyang, Korea. 4062 A phase II trial of docetaxel with bevacizumab as first line therapy for Her2/neu negative metastatic breast carcinoma. Hurvitz SA, Kabbinavar FF, Allen HJ, Moroose RL, Chan D, Hagenstad C, Applebaum SH, Patel G, Hu EH, Reese D, Slamon DJ. UCLA, Los Angeles, CA; Translational Oncology Research International, Los Angeles, CA. 4063 Bevacizumab combined with chemo-endocrine preoperative therapy in locally advanced operable breast cancers. Ferrari B, Scarano E, Pietri E, Dellapasqua S, Colleoni M. European Institute of Oncology, Milan, Italy. 4064 Capecitabine + docetaxel + bevacizumab as neoadjuvant therapy for invasive breast cancer: results of a phase II pilot study. Greil R, Moik M, Reitsamer R, Ressler S, Stoll M, Namberger K, Menzel C, Mlineritsch B. Private Medical University Hospital Salzburg, Salzburg, Austria. 4067 Breast-conserving therapy: balancing surgery and radiation. Indelicato D, Galloway T, Morris CG, Mendenhall NP. University of Florida, Gainesville, FL. 4068 Cosmetic effect of breast radiotherapy in older women. Kunkler IH, Prescott RJ, Williams L, King CC, Jack WJL, Dixon MJ, van der Pol M. Edinburgh University, Edinburgh, United Kingdom; Aberdeen University. 4069 Breast conservative therapy results of triple negative breast cancer. Tulusan AH, Popovich M, Bühner M, Keilholz L, Volkholz H, Lex B. Klinikum Bayreuth GmbH, Bayreuth, Germany. 4070 Does surgical closure technique affect early mammographic detection of tumor recurrence following breast-conserving therapy? Newlin HE, Indelicato DJ, Abbitt P, Marshall J, Wymer D, Grobmyer S, Haigh L, Copeland E, Morris CG, Mendenhall NP. University of Florida, Gainesville, FL. 4071 Stem cell augmented reconstruction: a new hope for reconstruction after breast conservation therapy. Kitamura K, Kajitani K, Hedrick M, Sugimachi K. Kyushu Central Hospital, Fukuoka, Japan; Cytori Therapeutics, San Diego, CA. 4072 Co-transplantation of adipose tissue-derived regenerative cells improves long-term retention of fat graft. Zhu M, Zhou Z, Chen Y, Schreiber R, Fraser JK, Hedrick MH, Ransom JT, Kuo H-C. Cytori Therapeutics Inc, San Diego, CA; UCLA, Los Angeles, CA. 4073 Radiofrequency ablation therapy for breast cancer. Oura S, Tamaki T, Yoshimasu T, Ohta F. Wakayama Medical University, Wakayama, Japan. Treatment: Radiation Therapy 4074-4097 4074 Concurrent chemoradiation with capecitabine achieves meritable response and local control for inoperable and recurrent neoadjuvant chemotherapy refractory breast cancer. Perkins GH, Middleton LP, Tran R, Garcia SM, Cristofanilli M, Pusztai L, Singletary SE, Strom EA, Woodward WA, Yu T-K, Oh JL, Tereffe W, Whitman GJ, Huang E, Allen PK, Buchholz TA. The University of Texas M. D. Anderson Cancer Center, Houston, TX. 4075 The late radiotherapy normal tissue phenotypes of telangiectasia, fibrosis and atrophy in breast cancer patients have distinct genotype-dependant causes. Symonds P, Giotopoulos G, Peat I, Foweraker K, Plumb M. University of Leicester, Leicester, Leicestershire, United Kingdom; University Hospitals of Leicester NHS Trust, Leicester, Leicestershire, United Kingdom. 4076 Increased use of regional radiotherapy is associated with improved outcome in a population-based cohort of women with breast cancer and 1-3 positive nodes. Wai ES, Tyldesley S, Speers CH, Truong PT, Kyle K, Olivotto IA. BC Cancer Agency - Vancouver Island Centre, Victoria, BC, Canada; BC Cancer Agency - Vancouver Centre, Vancouver, BC, Canada; BC Cancer Agency - Vancouver, Vancouver, BC, Canada. 4077 Roles of radiotherapy and chemotherapy in the development of contralateral breast cancer. Hooning MJ, Aleman BMP, Hauptmann M, Klijn JGM, Noyon R, Stovall M, van Leeuwen FE. Netherlands Cancer Institute, Amsterdam, Netherlands; Erasmus MC, Daniel den Hoed Cancer Center, Rotterdam, Netherlands; University of Texas, M.D. Anderson Cancer Center, Houston, TX. Treatment: Breast Conservation 4065-4073 4065 4066 Increased use of breast-conserving surgery: preferred treatment or failure to provide adequate local therapy? Virnig B, Habermann E, Al-Refaie W, Jensen E, Tuttle T. University of Minnesota, Minneapolis, MN. Impact of the interval between breast conserving surgery and adjuvant radiotherapy on clinical outcomes in early stage breast cancer. Campbell SAM, Kerr GR, Kunkler IH. Edinburgh Cancer Centre on Behalf of the Edinburgh Breast Group, Edinburgh, United Kingdom. 4078 4079 4080 4081 4082 4083 4084 4085 4086 Toxicity and cosmesis from RTOG 95-17: a phase I/II trial to evaluate brachytherapy as the sole method of radiation therapy for stage I and II breast carcinoma. Rabinovitch R, Winter K, Taylor M, Kuske R, Bolton J, Arthur D, White J, Hanson W, Wilenzick R, McCormick B. U of CO, Aurora, CO; RTOG, Philadelphia, PA; Washington U, Saint Louis, MO; AZ Onc Services, Scottsdale, AZ; Ochsner Clinic, New Orleans, LA; Med Coll VA, Richmond, VA; Med Coll WI, Milwaukee, WI; MDACC, Houston, TX; MSKCC, New York, NY. Update of the phase II MammoSite® brachytherapy trial for DCIS. Streeter, Jr OE, Benitez P, Vicini F, Mehta V, Quiet C, Kuske R, Hayes M, Arthur D, Kuerer H, Strom E, Freedman G, Keisch M, DiPetrillo T, Khan D, Hudes R, Groshen S, Silverstein MJ. USC/Norris Cancer Center, Los Angeles, CA; William Beaumont Hospital, Royal Oak, MI; Swedish Cancer Institute, Seattle, WA; Arizona Oncology Services, Scottsdale, AZ; New York Presbyterian Hospital, NY, NY; Virgnia Commenwealth University, Richmond, VA; M.D. Anderson Cancer Center, Houston, TX; Fox Chase Cancer Center, Philadelphia, PA; Cedars Medical Center, Miami, FL; Rhode Island Hospital, Providence, RI; Centinela Freeman Medical Center, Inglewood, CA; St. Agnes Healthcare, Baltimore, MD. Partial breast irradiation using the MammoSite® device for low risk breast carcinoma in patients aged ≥ 60 years: toxicity, cosmesis and quality of life results of a phase II study. Belkacemi Y, Chauvet MP, Giard S, Lacornerie T, Bonodeau F, Baranzelli MC, Bonneterre J, Lartigau E. Centre Oscar Lambret, Lille, France. Intra-fraction motion during tangential treatment of the left breast: how consistently is the heart actually blocked? Wang Z, Yin F-F, Maurer J, Wu QJ, Hubbs J, Marks LB. Duke University Medical Center, Durham, NC. Prospective trial of individual optimal positioning (prone versus supine) for whole breast radiotherapy: results of 194 patients. Formenti SC, Guth AA, Axelrod DM, Goldberg JD, DeWyngaert JK. New York University School of Medicine, New York, NY. Relative importance of posterior and upper borders of tangential radiation portals in axillary lymph node coverage after breast conserving surgery. Gross E, Padovani L, Badinand D, George L, Muracciole X, Cowen D. Hôpital Timone, Marseille, France. Post-operative radiotherapy does not adversely affect the outcome of autologous free abdominal flap breast reconstruction. Chatterjee J, Lee A, Baker L, Anderson W, Dewar JA, Stevenson JH, Thompson AM. University of Dundee, Ninewells Hospital and Medical School, Dundee, Scotland, United Kingdom. Linear accelerator-based intraoperative radiotherapy in limited stage breast cancer - results of an ISIORT pooled analysis in 1131 patients. Reitsamer R, Fastner G, Merz F, Menzel C, Kopp M, Hager E, Ciabattoni A, Willich N, Orecchia R, Valentini V, Sedlmayer F. Paracelsus Private Medical School Salzburg, Salzburg, Austria; General Hospital Klagenfurt, Klagenfurt, Austria; San Francisco Neri Hospital, Rome, Italy; University Hospital Münster, Münster, Germany; European Institute of Oncology, Milan, Italy; Gemelli University Clinic, Rome, Italy; on behalf of the ISIORT. The Cambridge breast intensity modulated radiotherapy trial: dosimetry results for 1089 patients. Coles CE, Wilkinson JS, Moody AM, Wilson CB, Twyman N, Hoole ACF, Burnet NG. Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom. 4087 Utilization of fiducial markers in accelerated partial breast irradiation with intensity modulated radiotherapy (IMRT). Page BR, Gibbons SK. Albany Medical College, Albany, NY; Albany Medical Center, Albany, NY. 4088 Intervals longer than 20 weeks from breast conserving surgery to radiation therapy are associated with inferior outcome for women with early stage breast cancer not receiving chemotherapy. Olivotto I, Lesperance M, Berrang T, Speers C, Nichol A, Tyldesley S, Germain F, Wai E, Holloway C, Kwan W, Truong P. BC Cancer Agency, Victoria, Vancouver, Kelowna, Surrey, BC, Canada; University of Victoria, Victoria, BC, Canada; BC Cancer Agency, Vancouver, BC, Canada. 4089 Are patients with T1-2 breast cancer with 1-3 positive nodes suitable candidates for partial breast radiotherapy trial enrolment? Truong PT, Jones S, Alexander A, Speers C, Kader H, Wai E, Olivotto IA. BC Cancer Agency, Vancouver Island Centre, Victoria, BC, Canada. 4090 Lumpectomy and accelerated partial breast irradiation as an alternative to mastectomy following prior mantle field radiation or breast irradiation. Adkison JB, Palazzi-Churas K, Kuske RR, Patel RR. University of Wisconsin Hospital and Clinics, Madison, WI; Arizona Oncology Services, Phoenix, AZ. 4091 Surgeon characteristics and receipt of adjuvant radiotherapy following breast conservation surgery in elderly women with breast cancer. Hershman DL, Buono D, Jacobson JS, Tsai WY, Joseph KA, Grann VR, Neugut AI. Columbia University Medical Center, New York, NY; Mailman School of Public Health, New York, NY. 4092 Non-invasive imaging techniques quantify radiation induced vascular changes in the breast. Klifa CS, Hattangadi J, Hwang J, Watkins M, Sakata T, Tromberg B, Hylton N, Park C. University of California, San Francisco, CA; University of California, Irvine, CA. 4093 The identification of patients for postmastectomy radiotherapy using the Cambridge index: audit of a prospective series. Wilson CB, Haba Y, Wishart GC. Addenbrookes Hospital, Cambridge, United Kingdom. 4094 Postmastectomy locoregional recurrence in Hong Kong: low risk patients without radiotherapy have more failures than intermediate risk patients with radiotherapy. Yau TK, Chang TY, Soong S, Chan K, Sze H, Yeung MW, Lee WM. Pamela Youde Nethersole Eastern Hospital, Hong Kong, China. 4095 Thyroid dysfunction following modern three-dimensional conformal radiation therapy to low neck in women with breast cancer — a dosimetric, volumetric, and biochemical assessment. Albuquerque K, Beall N, Bova D. Loyola University Medical Center, Maywood, IL. 4096 Oesophageal carcinoma as second malignancy after irradiation for breast cancer. From meta-analysis and large epidemiological studies to patients’ records and dosimetric questions: where is the truth? Large scale single institutional experience. Kirova YM, Asselain B, Fourquet A. Institut Curie, Paris, France. 4097 Patient rated breast symptoms and body image in early breast cancer: first results of the UK standardisation of breast radiotherapy (START) trials. Hopwood P, Haviland J, Sumo G, Mills J, Bliss JM, Yarnold J. Christie Hospital NHS Foundation Trust, Manchester, United Kingdom; The Institute of Cancer Research, Sutton, United Kingdom; Royal Marsden NHS Foundation Trust, Sutton, United Kingdom; on behalf of the START Trial Management Group. 4108 Profiling HER-family receptor dimerization in HER2 overexpressing cells that coexpress mutated EGFR receptors. Dua R, Nhonthachit P, Petropoulos C. Monogram Biosciences, Inc, South San Francisco, CA. 4109 ERBB2 influences the subcellular localization of the estrogen receptor in tamoxifen resistant MCF-7 cells leading to the activation of AKT and p90RSK. Pancholi S, Lykkesfeldt A, Dowsett M, Martin L-A. Institute of Cancer Research, London, United Kingdom; Danish Institute of Cancer Research, Copenhagen, Denmark. 4110 Reverse phase protein array analysis of an ER-positive/ HER2-positive breast cancer xenograft model reveals distinct resistance mechanisms to HER2 targeted therapy. Wang Y-C, Hennessy B, Huang C, Wiechmann LS, Rimawi M, Mills GB, Osborne CK, Schiff R. Baylor College of Medicine; M.D. Anderson, Houston, TX. 4111 Carcinoembryonic antigen cell adhesion molecule 6 has a functional role in endocrine resistance. Cummings M, Maraqa L, Speirs V. University of Leeds, Leeds, West Yorks, United Kingdom. 4112 Distinct chemokines mediate tumourigenicity of breast cancer cells. Potter SM, Dwyer RM, Kerin MJ. National University of Ireland, Galway, Ireland. The role of amphiregulin in exemestane-resistant breast cancer cells: evidence of an autocrine loop. Wang X, Masri S, Phung S, Chen S. City of Hope/Beckman Research Institute, Duarte, CA. 4113 BRCA1 transcriptionally regulates the genes associated with the basal phenotype in breast cancer. James CR, Quinn JE, Gorski JJ, Stewart G, Harkin P. Queen’s University Belfast, Belfast, Northern Ireland, United Kingdom. Ĝ6ĝ1 and Ĝ6ĝ4 integrins and their critical role in promoting resistance to multiple treatment strategies for breast cancer. Huang C, Osborne CK, Schiff R. Baylor College of Medicine, Houston, TX. 4114 Kinome survey of molecular pathways lead to tamoxifenresistant breast cancer cell growth. Gonzalez LG, Park J, Geistlinger TR, Pearlberg J, Endege W, Degot S, Sawyer J, Hu Y, Harlow E, Labaer J. Harvard Institute of Proteomics, Cambridge, MA; Dana-Farber Cancer Institute, Boston, MA. 4115 On the role of calpain in regulation of HER2 and resistance to trastuzumab in breast cancer cells. Kulkarni S, Reddy KB, Esteva FJ, Budd TG, Moore HCF, Tubbs RR. Cleveland Clinic, Cleveland, OH; M.D. Anderson Cancer Center, Houston, TX. 4116 P450 aromatase regulation by autocrine human growth hormone confers resistance to aromatase inhibitors in a human mammary carcinoma cell line. Perry JK, Yang W-S, Grandison P, Lobie PE. University of Auckland, Auckland, New Zealand. 4117 Tissue inhibitor of metalloproteinases-1 influences sensitivity to etoposide in MCF-7 S1 breast cancer cells. Schrohl Rasmussen A-S, Würtz SØ, Brünner N, Lademann U. University of Copenhagen, Faculty of Life Sciences, Copenhagen, Denmark. Tumor Cell Biology: Cell Biology 4098-4105 4098 4099 4100 4101 4102 4103 4104 4105 Distinct cancer stem cells may mediate heterogeneity among the human breast premalignant lesions. Behbod F, Kittrell FS, Allred DC, Eaves C, Kuperwasser C, Perou CM, Rosen JM, Medina D. Baylor College of Medicine, Houston, TX; Washington University School of Medicine, St. Louis, MO; BC Breast Cancer Research Center, Vancouver, Canada; Tufts Univeristy School of Medicine, Boston, MA; University of North Carolina at Chapel Hill, Chapel Hill, NC. Preliminary characterization and in vitro propagation of putative stem/progenitor cells from human inflammatory breast cancer. Woodward WA, Reuben J, Gao H, Krishnamurthy S, Lucci A, Singh B, Li L, Cristofanilli M. The University of Texas M.D. Anderson Cancer Center, Houston, TX. Tumour-associated tenascin-C isoforms promote breast cancer cell invasion and proliferation through MMPdependant and -independant mechanisms. Alcock RA, Allen MD, Holliday DL, Edwards DR, Pennington CL, Shaw JA, Walker RA, Pringle JH, Jones JL. University of Leicester, Leicester, United Kingdom; Bart’s and the London, Queen Mary’s School of Medicine and Dentistry, London, United Kingdom; University of East Anglia, Norwich, United Kingdom. Development of in vitro models to study microenvironmental influences on breast cancer progression. Holliday DL, Mulligan KT, Jones JL. Barts and the London, Queen Marys School of Medicine and Dentistry, London, United Kingdom. MCF7 and MDA-MB-231 cells cultured on Poly-HEMAcoated dish are more invasive, yet show less tumourigenicity, than cells cultured on the tissue culture dish. Kim JB, Lee K-M, Ko E, Han W, Lee JE, Shin I, Lee JW, Cho J, Noh D-Y. Seoul National University College of Medicine, Seoul, Korea; College of Natural Sciences, Hanyang University, Seoul, Korea. The anti-aromatase effect of the natural metabolites of progesterone: 20Ĝ-dihydroprogesterone and 5Ĝ dihydroprogesterone in MCF-7aro breast cancer cells. Pasqualini JR, Chetrite GS. Hormones and Cancer Research Unit, Paris, France. Tumor Cell Biology: Drug Resistance 4106-4117 4106 4107 Development of resistance to targeted therapy strategies transforms the clinically-defined molecular profile subtype of breast tumors. Creighton CJ, Massarweh S, Tsimelzon A, Huang S, Hilsenbeck SG, Osborne CK, Schiff R. Baylor College of Medicine, Houston, TX; University of Kentucky, Lexington, KY. The farnesyltransferase inhibitor R115777 (tipifarnib) in combination with tamoxifen acts synergistically to inhibit MCF-7 breast cancer cell proliferation and cell-cycle progression in-vitro and in-vivo. Martin L-A, Head JE, Pancholi S, Salter J, Quin E, Detre S, Kaye S, Howes A, Dowsett M, Johnston SR. Institute of Cancer Research, London, United Kingdom; Johnson & Johnson PRD, High Wycombe, United Kingdom; Royal Marsden Hospital, London, United Kingdom. 9:00-9:30 PLENARY LECTURE 4 – Exhibit Hall D Multidisciplinary guidelines across the continuum of care: the NCCN experience Robert Carlson, MD Stanford University Stanford, CAS 9:30-10:00 PLENARY LECTURE 5 – Exhibit Hall D Symptom management in breast cancer survivors Charles Loprinzi, MD Mayo Clinic Rochester, MN 10:00-11:00 10:00 10:15 10:30 10:45 GENERAL SESSION 5– Exhibit Hall D 2:00-3:30 51. Is completion axillary dissection always required after a positive sentinel node biopsy? NSABP B-32. Julian TB, Anderson SJ, Fourchotte V, Brown AM, Boudros E, Mamounas EP, Bear H, Costantino JP, Wolmark N. NSABP Medical Affairs, NSABP Investigators & NSABP Operation & Biostatistical Centers, Pittsburgh, PA. 52. The impact of micrometastases in the sentinel nodes of patients with invasive breast cancer. Hansen NM, Grube BL, Ye C, Turner R, Brennan M, Brenner J, Giuliano AE. John Wayne Cancer Institute, Santa Monica, CA; Saint John’s Hospital and Health Center, Santa Monica, CA. 53. High sensitivity of a molecular assay for breast metastases in sentinel lymph nodes that are difficult to detect by frozen section. Blumencranz P, Deck KB, Whitworth PW, McCue P, Reintgen DS, Chagpar AS, Beitsch P, Julian TB, Mamounas M, Saha S, Giuliano A, Simmons R. Morton Plant Mease Healthcare, Clearwater, FL; Saddleback Memorial Hospital, Laguna Hills, CA; Nashville Breast Center, Nashville, TN; Jefferson Medical College, Philadelphia, PA; Lakeland Regional Medical Center, Lakeland, FL; James Brown Cancer Center, Louisville, KY; Dallas Surgical Group, Dallas, TX; Allegheny General Hospital, Pittsburgh, PA; Aultman Hospital, Canton, OH; McLaren Regional Medical Center, Flint, MI; John Wayne Cancer Institute, Santa Monica, CA; Weill-Cornell Breast Center, New York, NY. 54. Increased sentinel lymph node lymphangiogenesis predicts non-sentinel axillary lymph node involvement in breast cancer patients with a positive sentinel node. Van den Eynden GG, Vandenberghe MK, van Dam P-JH, Colpaert CG, van Dam P, van Marck EA, Vermeulen PB, Dirix LY. (Lab Pathology University of Antwerp/University Hospital Antwerp, Wilrijk; Oncology Center, GH St-Augustinus, Wilrijk, Belgium), Antwerp, Belgium. SYSTEMS BIOLOGY AND TARGETING THE HER NETWORK IN THE TREATMENT OF BREAST CANCER C. Kent Osborne, MD, Co-Moderator Baylor College of Medicine, Houston, TX and Rachel Schiff, PhD, Co-Moderator Baylor College of Medicine, Houston, TX 2:00 Introduction 2:00 HER pathways in the context of systems biology and integrating networks Yosef Yarden, PhD The Weizmann Institute of Science Rehovat, ISRAEL 2:30 3:00 3:30-5:00 Development of non-invasive optical methods for breast cancer detection and clinical management Bruce J. Tromberg, PhD Beckman Laser Institute Irvine, CA 11:30 61. The influence of a very high vegetable-fruit-fiber, lowfat diet on prognosis following treatment for breast cancer: results from the Women’s Healthy Eating and Living (WHEL) randomized trial. Pierce JP, Natarajan L, Cann BJ, Parker BA, Greenberg ER, Flatt SW, Rock CL, Kealey S, Al-Delaimy WK, Bardwell WA, Carlson R, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Madlensky L, Marshall J, Newman VA, Ritenbaugh C, Thomson CA, Wasserman L, Stefanick ML. Moores UCSD Cancer Center, University of California, San Diego, La Jolla, CA; Kaiser Permanente Northern California, Oakland, CA; Fred Hutchinson Cancer Research Center, Seattle, WA; Stanford Comprehensive Cancer Center, Stanford University, Stanford, CA; University of California, San Diego; University of California, Davis, CA; M.D. Anderson Cancer Center, The University of Texas, Houston, TX; Center for Health Research, Portland, OR; Roswell Park Cancer Institute, Buffalo, NY; University of Arizona, Tucson, AZ; Arizona Cancer Center, Arizona Prevention Center, University of Arizona, Tucson, AZ; Stanford Prevention Research Center, Stanford University, Stanford, CA. 3:45 62. Outcome prediction for Clinical Stage II and III ER+ breast cancer based on treatment response, pathological stage, tumor grade, Ki67 proliferation index, and estrogen receptor status after neoadjuvant endocrine therapy. Ellis MJ, Tao Y, Luo, Evans DB, Bhatnagar, Chaudri-Ross HA, von Kameke, Miller WR, Eiermann W. Washington University, St Louis, MO; Novartis Pharma AG, Basel, Switzerland; Edinburgh University, Scotland; Red Cross Women’s Hospital, Munich, Germany. 4:00 63. Prognostic utility of the 21-gene assay compared with Adjuvant! in hormone receptor (HR) positive operable breast cancer with 0-3 positive axillary nodes treated with adjuvant chemohormonal therapy (CHT): an analysis of intergroup trial E2197. Goldstein L, Ravdin P, Gray R, Yoshizawa C, Childs B, Rowley S, Shak S, Badve S, Baehner FL, Davidson N, Sledge GW, Sparano JA. Eastern Cooperative Oncology Group, Brookline, MA; MD Anderson Cancer Center, Houston, TX; Genomic Health, Inc., Redwood City, CA; sanofi aventis, Bridgewater, NJ. Functional breast imaging: State of the PET Eric L. Rosen, MD Seattle Cancer Care Alliance Seattle, WA 12:00-1:00 LUNCH [Ticket Required] – Exhibit Hall A 12:30-1:45 CASE DISCUSSION 2 – Ballroom A GENERAL SESSION 6 – Exhibit Hall D 3:30 Susan Hilsenbeck, PhD, Co-Moderator Baylor College of Medicine, Houston, TX and Eva Sevick-Muraca, PhD, Co-Moderator Baylor College of Medicine, Houston, TX Introduction Novel experimental global approaches in studies of signaling networks and therapy resistance René Bernards, PhD The Netherlands Cancer Institute Amsterdam, NETHERLANDS MOLECULAR IMAGING FOR BREAST CANCER DIAGNOSTICS 11:00 Novel strategies for HER-targeted therapy and mechanisms of resistance C. Kent Osborne, MD Baylor College of Medicine Houston, TX 11:00-12:00 MINI-SYMPOSIUM 3 – Exhibit Hall D 11:00 MINI-SYMPOSIUM 4 – Exhibit Hall D 4:15 64. Value of centrally-assessed Ki-67 labeling index as a marker of prognosis and predictor of response to adjuvant endocrine therapy in the BIG 1-98 trial of postmenopausal women with estrogen receptor-positive breast cancer. Viale G, Giobbie-Hurder A. BIG 1-98 Collaborative Group and International Breast Cancer Study Group (IBCSG), Bern, Switzerland. 4:30 65. Erythropoietin receptor expression in breast cancer and correlation to tamoxifen response. Larsson A-M, Jirstrom K, Rydén L, Landberg G, Pahlman S. Lund University, University Hospital MAS, Malmo, Sweden. 4:45 66. Inflammatory breast cancer pathogenesis is mediated in significant part by translation initiation factor eIF4G amplification and unorthodox protein synthesis. Silvera D, Arju R, Darvishian F, Levine PH, Formenti SC, Schneider RJ. New York University School of Medicine, New York, NY; The George Washington University School of Public Health and Health Services, Washington, DC. 5:00-7:00 507 Differential effects of doxorubicin and zoledronic acid on intra-osseous vs extra-osseous breast tumour growth in vivo. Ottewell PD, Deux B, Monkkonen H, Cross SS, Coleman RE, Clezardin P, Holen I. University of Sheffield, Sheffield, Yorkshire, United Kingdom; Faculte de Medicine Laennec, Lyon, France. 508 Survival in breast cancer patients with bone metastases and reductions in markers of bone resorption during zoledronic acid treatment. Lipton A, Cook R, Major P, Smith M, Coleman R. Milton S. Hershey Medical Center, Hershey, PA; University of Waterloo, Waterloo, ON, Canada; Juravinski Cancer Centre, Hamilton, ON, Canada; Massachusetts General Hospital Cancer Center, Boston, MA; University of Sheffield, Sheffield, United Kingdom. 509 Effects of zoledronic acid on wnt inhibition by dickkopf1 and frizzled-related protein in patients with bone metastases. Helsten TL, Mortimer JE, Corr M. Moores UCSD Cancer Center, La Jolla, CA; University of California, San Diego, CA. 510 Zoledronic acid as adjuvant therapy for women with early stage breast cancer and occult tumor cells in bone marrow. Lin A, Park J, Melisko M, Goga A, Moasser M, Moore D, Brissaud C, Rugo H. University of California-San Francisco, Comprehensive Cancer Center, San Francisco, CA. 511 Effect of zoledronate on persisting isolated tumor cells in the bone marrow of patients without recurrence of early breast cancer. Rack BK, Jueckstock J, Genss E-M, Schoberth A, Schindlbeck C, Strobl B, Heinrigs M, Rammel G, Zwingers T, Sommer H, Friese K, Janni W. Ludwig-Maximilians-University, Munich, Germany; Laboratory Drs. Tiller and Partners, Munich, Germany; Estimate GmbH, Augsburg, Germany. POSTER DISCUSSION 5 & RECEPTION Ballroom B Bisphosphonates for Bone Loss and Bone Metastases 501-511 501 502 503 504 505 506 The ZO-FAST trial: zoledronic acid effectively inhibits aromatase inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: 24 month BMD results. De Boer R, Eidtmann H, Lluch A, Pinotti G, Miller J, Schenk N, Dias R, Coleman R. Royal Melbourne Hospital, Parkville, Victoria, Australia; Universitaetsklinikum, Kiel, Germany; Hospital Clinico Universitario de Valencia, Valcenia, Spain; Ospedale di Circolo Fondazione Macchi, Varese, Italy; Novartis, East Hanover, NJ; Weston Park Hospital, Sheffield, United Kingdom. The SABRE (Study of Anastrozole with the Bisphosphonate RisedronatE) study: 12-month analysis. Van Poznak C, Hannon RA, Clack G, Campone M, Mackey JR, Apffelstaedt J, Eastell R. University of Michigan, Ann Arbor, MI; University of Sheffield, Sheffield, United Kingdom; AstraZeneca, Macclesfield, Cheshire, United Kingdom; Site Hospitalier Nord de Nantes, Nantes, France; University of Alberta, Edmonton, AB, Canada; University of Stellenbosch, Tygerberg, South Africa. The effect of risedronate on hip structural geometry in chemotherapy-induced postmenopausal women on SERMS versus aromatase inhibitors: a 2 year trial. van Londen G, Perera S, Vujevich K, Sereika S, Bhattacharya R, Vogel V, Brufsky A, Lembersky B, Greenspan S. University of Pittsburgh, Pittsburgh, PA; University of Kansas, Kansas City, KS. Practical guidance for the prevention of aromatase inhibitor-associated bone loss in women with breast cancer. Hadji P, Appro M, Brufsky A, Tubiana-Hulin M, Guise T, Body JJ. Philipps-University of Marburg, Marburg, Germany; Institut Multidisciplinaire d’Oncology, Genolier, Switzerland; University of Pittsburgh, Pittsburgh, PA; Centre René Huguenin, St. Cloud, France; University of Virginia, Charlottesville, Virginia; Université Libre de Bruxelles, Brussels, Belgium. Effect of zoledronic acid on bone loss in women undergoing chemotherapy for breast cancer. Aft R, Chavez-MacGregor M, Trinkaus K, Naughton M, Weilbaecher K. Washington University, Siteman Cancer Center, St. Louis, MO; John Cochran Veterans Administration Hospital, St. Louis, MO. Zoledronic acid prevents bone loss in premenopausal women undergoing adjuvant chemotherapy for early stage breast cancer. Hershman DL, McMahon D, Crew K, Cremers S, Irani D, Cucchiara G, Brafman L, Siarra A, Shane E. Columbia University Medical Center, New York, NY. 5:00-7:00 POSTER SESSION 5 & RECEPTION Exhibit Hall B (#5001-5119) Detection and Diagnosis: Detection 5001-5012 5001 Molecular etiology of breast cancer: potential biomarkers of risk and for use in prevention. Cavalieri E, Gaikwad N, Rogan E, Pruthi S, Ingle J. University of Nebraska Medical Center, Omaha, NE; Mayo Clinic College of Medicine, Rochester, MN. 5002 Increased detection of breast cancer markers human epidermal growth factor receptor dimer and downstream signaling proteins utilizing the VeraTag technology with dextran modified antibodies. Wallweber J, Dang T, Gupta S, Winslow J, Petropoulos C. Monogram Biosciences, Inc., South San Francisco, CA. 5003 Changing pattern of the detection of loco-regional relapse in breast cancer: the Edinburgh experience. Montgomery DA, Krupa K, Kerr G, Jack W, Dixon M. Royal Infirmary, Glasgow, United Kingdom; Royal Alexandra Hospital, Paisley, United Kingdom; Western General Hospital, Edinburgh, United Kingdom. 5004 Value of clinical follow-up following breast conserving treatment for breast cancer. Hamed H, Kontos M, Jones G, Allen D. Guy’s Hospital, London, United Kingdom. 5005 Estrogen plus progestin and breast cancer detection with mammography and breast biopsy. Chlebowski RT, Anderson G, Pettinger M, Lane D, Langer RD, Gillian MA, Walsh BW, Chen C, McTiernan A. Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, CA; Fred Hutchinson Cancer Research Center, Seattle, WA; The State University of New York, Stony Brook, NY; Geisinger Healthcare, Danville, PA; Medical College of Wisconsin, Milwaukee, WI; Bringham & Womens Hospital, Boston, MA. 5006 Galactose oxidase Schiff’s reactivity is higher in nipple aspirate fluid from cancerous breasts than from healthy patients. Chagpar AB, Evelegh M. University of Louisville, Louisville, KY; McMaster University, Hamilton, ON, Canada. 5007 Hormonal attributes of breast ductal lavage fluid in pre- and post-menopausal women. Effect of tamoxifen. Chatterton RT, Avram MJ, Helenowski IB, Khan SA. Northwestern University, Chicago, IL. 5008 Novel impedance device to detect breast cancer in younger women. Boolbol SK, Ironstone JS, Feldman SM. Beth Israel Medical Center, New York, NY. 5009 Intraoperative in vivo reflectance spectroscopy for discrimination of normal, benign, and malignant breast tissues. Brown JQ, Wilke LG, Kennedy S, Palmer GM, Geradts J, Ramanujam N. Duke University, Durham, NC; Duke University Medical Center, Durham, NC. 5010 5011 5012 Water state changes in malignant and benign breast tumors measured by diffuse optical spectroscopy in vivo. Chung SH, Cerussi AE, Merritt SI, Hsiang D, Mehta R, Tromberg BJ. University of California, Irvine, CA; Masimo Corporation, Irvine, CA; UCI Medical Center, Orange. Sonopheresis and ductal epithelial impedance spectroscopy as a non-invasive technique for breast cancer diagnosis. Davies RJ, Brumfield MK, Pierce M, Greene T. Hackensack University Medical Center, Hackensack, NJ; UMD-New Jersey Medical School, Newark, NJ. Combination of mammogram BI-RADS data and serum mass spectrometry proteomic profiles in improving breast cancer diagnosis. Sun M, Sun M, Lokshin AE, Modugno FM, Bigbee WL. University of Pittsburgh Cancer Institute, Pittsburgh, PA; University of Pittsburgh, Pittsburgh, PA. 5019 Serum HER2 compared with CA153 for the monitoring of advanced breast cancer. Briscoe T, Thompson D, Bosomworth M, Dodwell DJ, Adlard JW. St James’s University Hospital, Leeds, United Kingdom. 5020 Liquid FISH-like assay for detection of HER-2 gene amplification in the serum of patients with breast cancer. Yeh C-H, Whitmire III WA, Albitar M. Quest Diagnostics Nichols Institute, San Juan Capistrano, CA. 5021 CA 15-3 level at time of metastatic relapse of breast cancer strongly correlates with hormone receptor but not with Her2 expression. Bensouda Y, Andre F, Boulet T, Mathieu MC, Conforti R, Ponzio-Prion A, de la Motte Rouge T, Zoubir M, El Masmoudi Y, Spielmann M, Delaloge S. Institut Gustave Roussy, Villejuif, France. 5022 Differential gene expression in circulating tumor cells between primary and metastatic breast cancer patients. Reinholz MM, Kitzmann KK, Hillman D, Lingle WL, Hobday T, Moreno A, Vivek R, Perez EA. Mayo Clinic College of Medicine, Rochester, MN; Mayo Clinic College of Medicine, Jacksonville, FL. 5023 Metastasis in blood of breast cancer patients. Lu J, Zeng W, Zhao Q, Zaslavsky E, Fan T, O’Hea B, Burk M, Merriam L, Pameijer C, Chen W-T. Stony Brook University Medical Center, Stony Brook, NY; Vitatex, Inc., Stony Brook, NY. Detection and Diagnosis: Marrow and Blood Micrometastases 5024-5025 5024 RASSF1A DNA methylation in bone marrow (mRASSF1ABM) or peripheral blood plasma (mRASSF1APB) of primary breast cancer (BC) patients. Braun S, Auer D, Vogl FD, Schneitter A, Egle D, Taucher S, Daxenbichler G, Marth C. Innsbruck Medical University, Innsbruck, Austria; Medical Services, Meran, Italy. 5025 Incidence and kinetics of circulating tumor cells in breast cancer patients treated with primary systemic therapy including trastuzumab for patients with HER2positive tumors - a translational project within the study “GeparQuattro”. Riethdorf S, Loibl S, Komor M, Huober J, Schrader I, Conrad U, Untch M, von Minckwitz G, Pantel K, Mueller V. University Medical Center Hamburg-Eppendorf, Hamburg, Germany; Goethe University Frankfurt, Frankfurt, Germany; German Breast Group, Neu Isenburg, Germany; University Medical Center Tuebingen, Tuebingen, Germany; Henriettenstiftung Hannover, Hannover, Germany; St. Barbara Klinik Hamm Heessen, Hamm Heessen, Germany; Heliosklinik Berlin-Buch, Berlin, Germany. Detection and Diagnosis: Circulating Markers 5013-5023 5013 Identification of a metabolic fingerprinting for metastatic breast cancer by proton nuclear magnetic resonance spectroscopy-metabolomic analysis. Claudino WM, Colangiuli D, Biganzoli L, Nepi S, Cappadona S, Ciarlo A, Luchinat C, Vinci E, Bertini I, Di Leo A. Hospital of Prato; Istituto Toscano Tumori-Prato, Prato, Italy; Scientific Pole, University of Florence, Sesto Fiorentino, Florence, Italy; Sesto Fiorentino, Florence, Italy. 5014 Identification of blood-based biomarkers for the detection of breast cancer and lymph node status. Field LA, Love BJ, Hadix JA, Ellsworth RE, Shriver CD. Windber Research Institute, Windber, PA; Invitrogen Informatics, Carlsbad, CA; Walter Reed Army Medical Center, Washington, DC. 5016 Discovery of serum biomarkers for breast cancer detection. Sheta EA, Bryson JK, Meyers GL, Hollingsworth A. Power3 Medical Products, Inc., The Woodlands, TX; Mercy Women’s Center, Oklahoma City, OK. 5017 Protein markers for the stratification of breast cancer patients. Quong JN, Rosenberg AL, Farooqi S, Yeow W-S, Brill KL, Minkeau A, Sabherwal Y, Quong AA. Thomas Jefferson University and Hospital, Philadelphia, PA. 5018 Detection of oligometastases in breast cancer by using tumor markers. Ertl I, Heinemann V, Bauerfeind I, Laessig D, Nagel D, Seidel D, Stieber P. Institute of Clinical Chemistry, Munich, Germany; Medical Department III, Munich, Germany; Gynecological Department, Munich, Germany. Prognosis and Response Predictions: Prognostic Factors – Methods 5026-5040 5026 Web calculators for estimating the risk of breast cancer death and the impact of adjuvant treatment on that risk. Michaelson JS, Chen L, Martei Y, Smith B, Younger J. Massachusetts General Hospital, Boston, MA. 5027 Nodal ratios as an alternative to pN-staging in node-positive breast cancer: a validation study. Vinh-Hung V, Vlastos G, Fioretta G, Usel M, Neyroud-Caspar I, Rapiti E, Verkooijen L, Bouchardy C. Institute for Social and Preventive Medicine, Geneva University, Geneva, Switzerland; UZ Brussel, Jette, Brussels, Belgium; International Nodal Ratio Working Group; Geneva University Hospitals, Geneva, Switzerland. 5028 Automated image analysis for high-throughput quantitative detection of ER and PgR expression levels in large-scale clinical studies: the TEAM trial experience. Faratian D, Kay C, Campbell F, Robson T, Grant M, Rea D, Bartlett J. Edinburgh Cancer Research Centre, Edinburgh, Scotland, United Kingdom; University of Birmingham, Birmingham, United Kingdom. 5029 Estrogen receptor and breast cancer survival in a Kaiser permanente population-based study: comparison of quantitative reverse transcriptase polymerase chain reaction and immunohistochemistry. Habel LA, Achacoso N, Maddala T, Alexander C, Baehner FL, Shak S, Quesenberry C, Gown AM, Goldstein LC. Kaiser Permanente, Oakland, CA; Genomic Health Inc, Redwood City, CA; PhenoPath Laboratories, Seattle, CA. 5030 Androgen receptor determination in breast cancer: a comparison of the dextran-coated charcoal method and quantitative immunohistochemical analysis. Søiland H, Skaland I, Van Diermen B, Janssen EAM, Kørner H, Varhaug JE, Søreide JA, Baak JPA. Stavanger University Hospital, Stavanger, Norway; Haukeland University Hospital, Bergen, Norway; University of Bergen, Bergen, Norway; Free University, Amsterdam, Netherlands. 5031 Human epidermal growth factor receptor 2 (Her-2/Neu), immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) testing at McGill University Health Centre: a comparison of absolute FISH copies (FISH-ABS abs) with Her-2 COPY/chromosome 17 ratio (FISH-17 RATIO) in 198 consecutive early breast cancer cases. Sade S, Momta P, Quenneville L, Mihalcioiu C, Omeroglu A, Ragaz J. McGill University Health Centre, Montreal, QC, Canada; McGill University, Montreal, QC, Canada; Jewish General Hospital, Montreal, QC, Canada. 5032 Quality control procedures are essential in accurate HER2 FISH testing using automated morphometric image analysis. Barry TS, Tse C, Goldstein LC, Kim PM, Kussick SJ, Kandalaft P, Gown AM. Phenopath Labs, Seattle, WA. 5033 Impact of ERBB2 on prognosis and microarray data. Koscielny S. Institut Gustave Roussy, Villejuif, France. 5034 Reproducibility of HER2-analysis in a national survey performed at 24 routine pathology departments in Sweden. Ferno M, Haglund M, Bendahl P-O, Hatschek T, Kolaric A, Kovacs A, Olsson A, Olsson H, Ryden L, Strand C. University Hospital, Lund, Sweden; University Hospital, Malmo, Sweden; Karolinska University Hospital, Stockholm, Sweden; University Hospital, Orebro, Sweden; University Hospital, Gothenburg, Sweden; University Hospital, Linkoping, Sweden. 5035 Assessing HER-2 status via virtual microscopy. Bloom KJ, Kyshtoobayeva A, Chen S, Hii A. CLARiENT, Aliso Viejo, CA. 5036 Intrinsic near-infrared spectroscopic biomarkers applied for evaluation of final pathological response to neaoadjuvant chemotherapy. Kukreti S, Cerussi AE, Tanamai VW, Tromberg BJ, Rita M, David H, Gratton E. University of California, Irvine, CA; University of Illinois, Urbana-Champaign, IL. 5037 Prognosis-prediction model using multimarker in lymph node negative breast cancer by decision tree analysis. Jung S-Y, Han W, Han M-R, Park IA, Ko E, Kim E, Lee JW, Cho J, Kim S-W, Hwang K-T, Noh D-Y. Seoul National University Hospital, Seoul, Republic of Korea. 5038 Bayesian analysis of recurrence in lymph node positive and lymph node negative breast cancer patients. Maskery S, Hu H, Liebman M, Shriver C, Verbanac K, Tafra L, Rosman M. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC; East Carolina University, Greenville, NC; Ann Arundel Medical Center, Annapolis, MD. 5039 Stage migration of breast cancer using two techniques of tumor size assessment and its impact on projection for survival and treatment decision making. Phillips J, Staszewski H, Schuss A, Buyuk A. Winthrop University Hospital, Mineola, NY. 5040 Withdrawn Treatment: DCIS 5041-5047 5041 Sentinel node biopsy in ductal carcinoma in situ of breast - a meta-analysis. Ansari B, Ogston SSA, Purdie CCA, Adamson DJA, Brown DC, Thompson AM. Dundee University, Dundee, Scotland, United Kingdom. 5042 Pathologic and radiographic response of ER-positive DCIS to neoadjuvant letrozole therapy. Hwang ES, Chen Y-Y, Wolverton DE, Lessing JN, Shim V, Devries S, Anderson J, Johnson LR, Hylton NM, Esserman LJ, Waldman FM. University of California, San Francisco, CA; Kaiser Permanente Oakland Medical Center, Oakland, CA; California Pacific Medical Center, St. Luke’s Hospital, San Francisco, CA; Emory University School of Medicine, Atlanta, GA; University of California, San Francisco, CA. 5043 ERISAC trial: evidence exemestane effects oestrogen receptor (ER) positive ductal carcinoma in situ (DCIS) proliferation. Bundred NJ, Cramer A, Cheung KL, Johnson RL, Flint P, Young O, Grassby S, Turner L, Baildam A, Barr L, Byrne GJ, Dixon JM. University Hospital of South Manchester, Manchester, United Kingdom; University of Nottingham, Nottingham, United Kingdom; Western General Hospital, Edinburgh, United Kingdom. 5044 Genetic and phenotypic characteristics in pleomorphic lobular carcinoma in situ. Chen Y-Y, Roydasgupta R, DeVries S, Anderson J, Wa C, Fitzgibbons P, Jacobs T, MacGrogan G, Peterse H, VincentSalomon A, Tokuyasu T, Hwang ES, Schnitt S, Waldman FM. University of California, San Francisco, CA; St Jude Med Ctr, Fullerton, CA; Virginia Mason Med Ctr, Seattle, WA; Institute Bergonie, Bordeaux, France; Netherlands Cancer Institute, Amsterdam, Netherlands; Insititute Curie, Paris, France; Beth Israel Deaconess Med Ctr, Boston, MA. 5045 Molecular profiling of DCIS: identification of distinct subgroups of potential prognostic importance. Clark SE, Marshall JF, Hart IR, Carpenter R, Jones JL. St. Bartholomew’s Hospital, London, United Kingdom; Institute of Cancer, QMUL, London, United Kingdom. 5046 Suboptimal local control of ductal carcinoma in situ of the breast is associated with inferior 10-year breast cancer specific survival in a population-based cohort of women treated with breast conserving surgery. Wai ES, Alexander CS, Culp M, Moccia P, Mackinnon M, Moore S, Olivotto IA. BC Cancer Agency - Vancouver Island Centre, Victoria, BC, Canada; University of British Columbia, Victoria, BC, Canada. 5047 Can subcutaneous mastectomy be considered an alternative for ductal carcinoma in situ treatment, when breast conservation is not possible? Giménez Climent MJ, Merck B, LLopis Martínez F, Sancho Merle F, Vázquez Albaladejo C. Fundación Instituto Valenciano de Oncología, Valencia, Spain. Treatment: Male Breast Cancer 5048-5051 5048 Male breast cancer (MBC): impact of early diagnosis and adjuvant treatments. Analysis of 983 cases. Cutuli B, Cohen-Solal-Le-Nir C, Serin D, Kirova Y, Belkacemi Y, Gaci Z, Lemanski C, De Lafontan B, Zoubir M, Maingon P, Mignotte H, Tunon de Lara C, Edeline J, Penault-Llorca F, Romestaing P, Delva C. Polyclinique de Courlancy, Reims, France; Sylia-Stat, Bourg La Reine, France. 5049 Survivin and COX-2 expression in male breast cancer. Younis T, Dakin-Hache KA, Rayson D, Dewar R, Gray S, Barnes PJ. Queen Elizabeth II Health Sciences Centre, Halifax, NS, Canada; Cancer Care Nova Scotia, Halifax, NS, Canada; Dalhousie Medical School, Halifax, NS, Canada. 5050 Patterns of body size in male breast cancer and impact of obesity on disease outcome. Kulkarni S, Franssen E, Madarnas Y. Queen’s University, Kingston, ON, Canada. 5051 Expression of basal-like markers in male breast cancers. Flanagan MB, Bhargava R, Dabbs DJ, Thull D, Chivukula M. Magee-Womens Hospital, Pittsburgh, PA. 5056 Randomized placebo-controlled phase l l trial with preoperative epirubicin and cyclophosphamide +/- gefitinib in patients with operable and estrogen receptor negative breast cancer. Ejlertsen B, Bentzon N, Jacobsen E, Kromann N, Ottestad L, Ingvar C. University Hospital of Copenhagen, Copenhagen, Denmark; Herlev Hospital, Herlev, Denmark; Vejle Hospital, Vejle, Denmark; University Hosp. of Copenhagen Rigshospitalet, Copenhagen, Denmark; Norske Radiumhospital, Oslo, Norway; University Hospital Lund, Lund, Sweden. 5057 Efficacy and safety results from a randomized, phase II trial of neoadjuvant capecitabine + epirubicin + cyclophosphamide vs 5-FU + epirubicin + cyclophosphamide in operable breast cancer. Roché H, Penault-Llorca F, Berton Rigaud D, Tubiana Mathieu N, Ferrero J-M, Coudert B, Mousseau M, Monnier A, Orfeuvre H, Audhuy B, Rotarski M, Homokos H, Fumoleau P. Inst Claudius Régaud, Toulouse, France; Centre Jean Perrin, Clermont-Ferrand, France; Centre René Gauducheau, St. Herblain, France; Hôpital Dupuytren, Limoges, France; Centre Antoine Lacassagne, Nice, France; Centre Georges François Leclerc, Dijon, France; CHU de Grenoble, La Tronche, France; CH de Montbeliard, Montbeliard, France; CH de Fleyriat, Bourg en Bresse, France; Hôpital Pasteur, Colmar, France; Centre Oncologie Du Pays Basque, Bayonne, France; Roche, Neuilly sur Seine, France. Treatment: Neoadjuvant Therapy 5052-5076 5052 Significant improvement in disease free and overall survival with neoadjuvant, dose intensified two weekly treatment with anthracycline and taxane in primary breast cancer, including inflammatory disease. Fifty five months median follow up results of a multicenter prospective randomised phase III AGO-trial. Untch M, Konecny G, Moebus V, Bauerfeind I, Thomssen Ch, Harbeck N, Kuhn W, Bothmann G, Wallwiener D, Kreienberg R, Lueck HJ. Helios Klinikum Berlin Buch, Berlin, Germany; Mayo Clinic, Rochester, MN; Klinikum Frankfurt Hoechst, Frankfurt, Germany; University of Munich Grosshadern, Munich, Germany; University of Halle, Halle, Germany; Technical University of Munich, Munich, Germany; University of Bonn, Bonn, Germany; Städtisches Klinikum, Wolfsburg, Germany; University of Tuebingen, Tuebingen, Germany; University of Ulm, Ulm, Germany; Horst Schmitt Kliniken, Wiesbaden, Germany. 5053 Evaluating the efficacy and safety of trastuzumab given concomitantly to epirubicin/cyclophosphamide ¢ docetaxel±capecitabine as neoadjuvant treatment of HER2 overexpressing primary breast cancer. First analysis of the GBG/AGO intergroup-study “GeparQuattro”. Untch M, Rezai M, Loibl S, Fasching P, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Mehta K, von Minckwitz G. Frauenklinik, Berlin, Germany; Senologie, Brustzentrum, Düsseldorf, Germany; University Hospital Frankfurt, Frankfurt, Germany; Neu-Isenburg, Germany; Frauenklinik mit Poliklinik, Erlangen, Germany; Senologiezentrum Ostschweiz SENZO, St. Gallen, Switzerland; Onkologie Bethanien, Frankfurt, Germany; Frauenklinik, München, Germany; Frauenklinik, Hannover, Germany. 5058 Sequential epirubicin/cyclophosphamide followed by docetaxel with or without celecoxib or trastuzumab according to HER2 status, as primary chemotherapy for localized invasive breast cancer patients: results of the planned interim analysis and analysis of predictive parameters. Supported by PHRC AOM/2OO2/02117, Pfizer inc., Roche, sanofi-aventis. Marty M, Guinebretiere J-M, Mathieu M-C, Sigal-Zafrani B, de Roquancourt A, Spielmann M, Giacchetti S, Extra J-M, Spyratos F, de The H, Pierga J-y, Salmon R, Mefti-Lacheraf F, Asselain B. Saint Louis University Hospital, Paris, France; Centre Rene Huguenin, Saint Cloud, France; Institut Gustave Roussy, Villejuif, France; Institut Curie, Paris, France. 5054 Development of a genomic tool to predict pathologic complete remission in a community-based, preoperative, phase II trial of 5-fluorouracil, epirubicin, cyclophosphamide followed by docetaxel-capecitabine for stage II, III breast cancer. Holmes FA, Hellerstedt B, Pippen J, Vukelja SJ, Kocs D, Collea R, Blum JL, McIntyre K, Ward FT, Pusztai L, Boehm KA, Asmar L, O’Shaughnessy J. US Oncology Research, Houston, TX; Texas Oncology, P.A., Houston, TX; Baylor-Charles A. Sammons Cancer Center, Dallas, TX; Texas Oncology Cancer Centers, Austin, TX; Tyler Cancer Center, Tyler, TX; Texas Cancer Center, Round Rock, TX; New York Hematology and Oncology, Albany, NY; Texas Oncology, P.A., Dallas, TX; M.D. Anderson Cancer Center, Houston, TX. 5059 Neoadjuvant capecitabine plus docetaxel ± trastuzumab therapy for recently diagnosed breast cancer: phase II results. Tripathy D, Moisa C, Gluck S. University of Texas Southwestern Medical Center, Dallas, TX; Roche Laboratories, Inc, Nutley, NJ; University of Miami, Miami, FL. 5060 Dose-dense docetaxel, carboplatinum and trastuzumab as neoadjuvant therapy for human epidermal growth factor receptor-2 - positive stage II and III breast cancer. Han HS, Doliny P, Blaya M, Gluck S, Slingerland J, Silva O, Welsh C, Hurley J. Sylvester Comprehensive Cancer Center, University of Miami, Miami, FL. 5061 High pathologic complete response rate effectively predicted by proliferation index in HER2-positive localized breast cancer treated with weekly paclitaxel followed by FEC with concurrent trastuzumab. Pernas S, Urruticoechea A, Falo C, Pardo B, Villanueva R, Ortega R, Garcia A, Moreno A, Perez J, Gil M. Institut Català d’OncologiaH.U. de Bellvitge. IDIBELL, L’Hospitalet-Barcelona, Spain. 5062 The influence of T-cells on the response to a neodjuvant therapy with docetaxel/epirubicin/cyclophosphamide (TEC). Kemming D, Bosse U, Vogt U, Schlotter CM, Tidow N, Brandt BH. University Medical Center Hamburg Eppendorf, Hamburg, Germany; Institute of Pathology, Osnabrueck, Germany; European Laboratory Association, Ibbenbueren, Germany; Clinic Center Ibbenbueren, Ibbenbueren, Germany; Uiniversity of Muenster, Muenster, Germany. 5055 Primary systemic therapy using docetaxel/ cyclophosphamide/bevacizumab (TCB) followed by doxorubicin (A) in operable or locally advanced breast cancer (BC). Makhoul I, Klimberg S, Henri-Tillmen R, Westbrook K, Hutchins L. University of Arkansas for Medical Sciences, Little Rock, AR. 5063 Preliminary recurrence and survival analysis of patients (pts) receiving neoadjuvant q4week carboplatin and weekly paclitaxel ± weekly trastuzumab in resectable and locally advanced breast cancer: update of BrUOG BR-95. Sikov WM, Fenton MA, Strenger R, Dizon DS, Legare RD, Graves TA, Brown University Oncology Group. Rhode Island Hospital, Providence, RI; Women and Infants Hospital, Providence, RI; The Miriam Hospital, Providence, RI. 5064 Pharmacokinetic and pharmacodynamic analysis of cyclophosphamide, epirubicin and capecitabine vs 5-FU, epirubicin and cyclophosphamide as neoadjuvant therapy in breast cancer patients. Milano G, Deporte R, René N, Etienne-Grimaldi M-C, Berton Rigaud D, Ferrero J-M, Dalenc F, Piutti M, Homokos H, Fumoleau P. Centre Antoine Lacassagne, Nice, France; Centre René Gauducheau, Saint Herblain, France; Institut Claudius Regaud, Toulouse, France; Roche, Neuilly sur Seine, France; Centre Georges François Leclerc, Dijon, France. 5071 The farnesyl transferase (FT ase) inhibitor (FTI) tipifarnib inhibits FT ase in vivo and enhances the efficacy of neoadjuvant dose-dense doxorubicin-cyclophosphamide (AC) in patients with locally advanced breast cancer (LABC). Sparano JA, Coppola D, Kazi A, Merajver S, Vahdat L, Li T, Pellegrino C, Munster P, Hoschander S, Hopkins U, Hershman D, Wright JJ, Kleer C, Sebti S. Montefiore-Einstein Cancer Center, Bronx, NY; H. Lee Moffitt Cancer Center, Tampa, FL; University of Michigan, Ann Arbor, MI; Weill Medical College of Cornelly University, NY, NY; Columbia University, NY, NY; National Cancer Institute, Bethesda, MD. 5072 A phase 2 trial of neoadjuvant letrozole for postmenopausal patients with stage 2 and 3 ER and/or PgR+ breast cancer endpoint comparisons. Ellis M, Luo R, Tao Y, Crowder R, Hoog J, Guintoli T, Commean P, Carey L, Harris L, Fleming G, Esserman L, Budd T, Iversen E, Olson J. Siteman Cancer Center, MO; UNC-CH, NC; DFCI, MA; U Chicago, IL; UCSF, CA; Cleveland Clinic, OH; Duke, NC. 5065 Does combination of neoadjuvant and adjuvant chemotherapy improve outcome in operable breast cancer patients? Knauer M, Haid A, de Vries A, Schneider Y, Lang A, Winder T, Alton R, Wenzl E. University Teaching Hospital, Feldkirch, Austria. 5073 A randomized phase II neoadjuvant trial in patients with stage II-III and inflammatory breast cancer. Somlo G, Paz B, Shen J, Garberoglio C, Luu T, Chung C, Hurria A, Frankel P, Baker N, Wilczynski S, Arnold K, Yeb Y. City of Hope Comprehensive Cancer Center, Duarte, CA. 5066 Pathologic complete response following paclitaxel (cremophor or albumin bound) + carboplatin ± trastuzumab ± bevacizumab sequenced after in vivo chemosensitivity-adapted dose-dense doxorubicincyclophophamide in inflammatory breast cancer. Mehta RS, Schubbert T, Jackson D, Hsiang D, John B. University of California, Irvine, Orange, CA. 5074 Clinical relevance of neoadjuvant chemotherapy in invasive lobular carcinoma of the breast. Vrancken Peeters M-JTFD, Linn SC, Loo CE, Peterse HL, Rutgers EJTh, Rodenhuis S. Netherlands Cancer Institute, Amsterdam, Netherlands. 5075 Tumor and normal interstitial fluid proteomic characterization in breast cancer patients receiving neoadjuvant chemotherapy. Cortesi L, Barchetti A, De Matteis E, Ruscelli S, Della Casa L, Tazzioli G, Lazzaretti MG, Iannone AC, Federico MR. University of Modena and Reggio Emilia, Modena, Italy; Carpi Hospital, Carpi, Modena, Italy. 5076 Pathological and clinical outcomes in response to neoadjuvant chemotherapy: a comparison of basal-like, hormone receptor-positive and HER2-positive breast cancers. Allada N, Osborne CR, Xie X-J, Ashfaq R, Bian A, Tripathy D. UT Southwestern Medical Center, Dallas, TX; Baylor Sammons Cancer Center, Dallas, TX. 5067 Epirubicin and docetaxel as neoadjuvant treatment of locally advanced breast cancer: a phase II study. Lombardi D, Scalone S, Crivellari D, La Mura N, Miolo G, Murrone A, Perin T, Coran F, Candiani E, Massarut S, Veronesi A. Centro di Riferimento Oncologico, Aviano, PN, Italy. 5068 Neoadjuvant biweekly chemotherapy with liposomal doxorubicin and docetaxel in patients with stage II-III breast cancer. Alvarez I, Modolell A, Mayordomo JI, Heras L, Villadiego K, Rolfo CD, Garcia-Bueno JM, Pica P, Murillo L, Morales S, Valero P, Florian J. H San Jorge, Huesca; Inst Oncologia Corachan, Barcelona; H Clinico, Zaragoza; Cruz Roja, Hospitalet; H Sagrat Cor, Barcelona; Clin Roger, Palma de Mallorca; Clin Serosa, Palma de Mallorca; Hosp Infanta Cristina, Badajoz; H Reina Sofia, Tudela; Clin Perpetuo Socorro, Lerida; Clin Infanta Luisa, Sevilla; H Barbastro, Barbastro, Spain. 5069 Phase II study of a 3-weekly liposome-encapsulated doxorubicin/docetaxel/pegfilgrastrim in combination with weekly trastuzumab as primary treatment in HER2 positive (HER2+) early stage breast cancer patients (II-IIIa). Intermediate analysis of 26 patients. GEICAM 2003-03 study. Antón A, Ruiz-Simon A, Plazaola A, Segui MA, Muñoz M, Calvo L, Puértolas T, Guerrero A, Alfaro J. Spanish Breast Cancer Research Group (GEICAM), Spain. 5070 A phase IV study of neo-adjuvant combination chemotherapy with pegylated liposomal doxorubicin (CAELYX®) and vinorelbine for locally advanced breast cancer. Shen ZZ, Shao MZ, Xu HB, Wang L, Wang SY, Liu J, He QP, Su XF, Jiang FZ, Zhang B. Fudan Univ. Affiliated Tumor Hospital, Shanghai, China; Cancer Institute & Hospital Chinese Academy of Medical Sciences, Beijing, China; The Fourth Military Medical Univ. Affiliated No1. Hospital, Xi’an, Shanxi, China; Shandong Tumor Hospital, Jinan, Shandong, China; Fujian Provincial Tumor Hospital, Fuzhou, Fujian, China; Shanghai 6th People Hospital, Shanghai, China; Sun Yat-Sen Memorial Hospital, Guangzhou, Guangdong, China; 307 Hospital of PLA, Beijing, China; Liaoning Cancer Hospital & Institute, Shenyang, Liaoning, China. Treatment: Surgery 5077-5101 5077 Optimal loco-regional treatment of the primary tumor in metastatic breast cancer patients is associated with a significant survival advantage. Vlastos G, Rapiti E, Bouchardy C, Fioretta G, Verkooijen HM, Storme G, Vinh Hung V. Geneva University Hospitals, Geneva, Switzerland; Institute for Social and Preventive Medicine, University of Geneva, Geneva, Switzerland; National University of Singapore, Singapore, Singapore; Oncology Center UZ, Brussels, Belgium. 5078 NEW START: the United Kingdom sentinel lymph biopsy training programme. A model of how multi-professional training can achieve competent national performance whilst maintaining patient safety. MacNeill F, Mansel R, Horgan K, Keshtgar M, Kissin M, Wishart G, Brown D, NEW START Steering Group and Trainers. Royal College of Surgeons (England), London, United Kingdom. 5079 The effect of dedicated breast surgeons on the short term outcomes in breast cancer. Zork NM, Komenaka IK, Bowling MW, Norton LE, Pennington RE, Clare SE, Goulet RJ. Indiana University School of Medicine, Indianapolis, IN. 5080 Shared decision-making in routine clinical practice: the example of breast cancer in a regional cancer centre in France. Hervé M, Nora M-F, Christelle F, Anne M, Marie Odile C. Centre Léon Bérard, Lyon, France. 5091 Staged sentinel node biopsy to guide timing of breast reconstruction. Ahrendt G, Johnson R, Horton F, Bonaventura M, Falk J, Keenan D, Soran A. Magee-Womens Hospital of University of Pittsburgh Medical Center, Pittsburgh, PA. 5081 Paget’s disease of the nipple in a population based cohort. Dalberg K. Danderyds University Hospital, Stockholm, Sweden. 5092 5082 Infiltration of ropivacaine efficacy on acute breast pain after surgery for breast cancer. Preliminary results of a multicentric study. Emmanuelle F, Aline A-F, Catherine B, Alain B, Smail H, Max B, Cyrus M, Jean-Remi G, Sameh Y, Serge L, Jean-Louis B, Louis B, Catherine N, Christian J. Rene Huguenin Cancer Centre, Saint-Cloud, France; Institut Paoli Calmettes, Marseille, France; Institut Gustave Roussy, Villejuif, France; Ambroise Pare Hospital, Boulogne, France. Rib fractures: a complication of radiation therapy and tissue expansion for breast reconstruction. Huang AH, Wong MS, Whetzel TP, Stevenson TR. University of California-Davis Medical Center, Sacramento, CA. 5093 Does quality of life after breast reconstruction change with time? Thomson HJ, Fallowfield LJ, Winters ZE. University of Bristol, Bristol, United Kingdom; Psychosocial Oncology Group, Brighton, United Kingdom. 5094 Three-dimensional imaging provides valuable clinical data to aid in unilateral tissue expander-implant breast reconstruction. Tepper OM, Karp NS, Small K, Unger J, Pritchard A, Roses D, Shapiro R, Guth A, Axelrod D, Choi M. New York University School of Medicine, New York, NY. 5095 Postoperative analgesia and flap perfusion after pedicled TRAM flap reconstruction - continuous wound instillation with ropivacaine 0.2% - a pilot study. Dagtekin O, Thomas A, Hotz A, Kampe S, Auweiler M, Warm M. University of Cologne, Cologne, Germany; University of Medicine, Charité, Berlin, Germany. 5096 Optimizing surgical technique for total skin-sparing mastectomy. Chattopadhyay R, Radzio A, Kumar A, Foster R, Ewing C, Shelley H, Michael A, Esserman LJ. University of California, San Francisco, San Francisco, CA. 5097 Quality of life and morbidity at medium term follow up after sentinel lymph node, and immediate or delayed axillary disssection. Maryam ANM, Max BM, Laeticia HL, Carole TC, Jean Marc EJM, Agnes TA, Gilles HG. Institut Paoli Calmettes, Marseille, Bouches du Rhone, France. 5098 Radiation after axillary lymph node dissection: impact of neoadjuvant chemotherapy. Kirstein LJ, MacDonald S, Abi Raad R, Taghian AG, Smith BL, Specht MC. Massachusetts General Hospital, Boston, MA. 5099 Intraoperative ultrasound localization of nonpalpable breast cancers. Salmon RJ, Petitperrin F, Ngo C, Fourchotte V, Pollet AG. Institut Curie, Paris, French Polynesia. 5100 Tumor stage of the primary breast cancer is a predictor of the size of local recurrence. Kahlert SD, Roth J, Mayr D, Bauerfeind I, Friese K. Klinikum Grosshadern, LMU, Munich, Germany. 5101 Minimally invasive excision of gynaecomastia - a novel and effective surgical technique. Qutob O, Garimella V, Ihsan N, Drew PJ. University of Hull, Hull, United Kingdom; Hull and East Yorkshire Hospitals NHS Trust, Hull, United Kingdom. 5083 Surgical follow up and clinical presentation of 142 of breast papillary lesions diagnosed by ultrasound guided breast biopsy. Rizzo M, Lund MJ, Oprea G, Schniederjan M, Mosunjac M. Emory University, School of Medicine, Atlanta, GA; Emory University, Rollins School of Public Health, Atlanta, GA. 5084 Oncologic safety of nipple areola complex preservation for breast cancer; 5 year follow-up result. Lee SJ, Kang SH, Baek NW, Kim EM. Yeungnam University of Medical Center, Daegu, Republic of Korea. 5085 Breast surgery for women presenting with stage IV breast cancer. Barkley CR, Bafford AC, Burstein HJ, Winer EP, Lipsitz SR, Smith BL, Iglehart JD, Golshan M. Brigham and Women’s Hospital, Boston, MA; Dana Farber Cancer Institute, Boston, MA; Massachusetts General Hospital, Boston, MA. 5086 Can the resection of primary breast cancer improve survival of patients with stage IV breast cancer? Shien T, Kinoshita T, Shimizu C, Yonemori K, Kohno T, Hojo T, Ando M, Akashi-Tanaka S, Katsumata N, Fujiwara Y. National Cancer Center Hospital, Tokyo, Japan. 5087 Cosmetic outcome after latissimus dorsi based breast reconstruction: comparing the effects of radiotherapy and time. Thomson HJ, Greenwood RJ, Bahl A, Cawthorn S, Winters ZE. University of Bristol, Bristol, United Kingdom; United Bristol Healthcare Trust, Bristol, United Kingdom; Bristol Haematology and Oncology Centre, Bristol, United Kingdom; Frenchay Hospital, Bristol, United Kingdom. 5088 Interval inset of TRAM flaps in immediate breast reconstruction: a technical refinement. Comizio R, Yurkewich K, Collins D. Darmouth Hitchcock Medical Center, Lebanon, NH; Dartmouth Medical School, Hanover, NH; Norris Cotton Cancer Center, Lebanon, NH. 5089 Immediate two-stage breast reconstruction and irradiation with a tissue expander and an implant: results, risk factors for failure and self-evaluation. Gurriet B, Padovani L, Tallet A, Letrosne E, VAINI V, Boyer A, Houvenaeghel G, Cowen D. Hop Timone, Marseille, France; IPC Cancer Center, Marseille, France; Axium Clinic, Aix en Provence, France; Etoile Clinic, Puyricard, France. 5090 Skin-sparing mastectomy and immediate ‘mini-flap’ reconstruction - a novel technique. Vestey SB, Court FG, Bristol JB, Ghilchick M, Chan CY. Cheltenham General Hospital, Cheltenham, Gloucestershire, United Kingdom. Tumor Cell Biology: Estrogen and Progestin Receptors 5102-5109 5102 Evidences that progesterone receptor b decreases estrogen receptor gene expression through its interaction to a halfPRE site at estrogen receptor gene promoter. De Amicis F, Zupo S, Malivindi R, Andò S. University of Calabria, Arcavacata di Rende, Italy. 5103 Influence of estrogen receptor expression on HER2 mRNA levels in HER2-gene amplified breast cancer tumors as measured using FISH and the novel DASL assay. Abramovitz M, Audet R, Catzavelos C, Li Z, Provencher C, Ponton A, Leyland-Jones B. VM Institute of Research, Montreal, QC, Canada; McGIll University, Montreal, QC, Canada; Emory University, Atlanta, GA. 5104 Detection of elevated HER2/neu levels in breast cancer cell lines overexpressing estrogen receptor ĝ. Lattrich C, Juhasz-Böss I, Ortmann O, Treeck O. University of Regensburg, Regensburg, Germany. 5105 5106 5107 5108 5109 5114 Biomarker analyses in Japanese refractory advanced breast cancer patients treated with lapatinib monotherapy. Toi M, Iwata H, Fujiwara Y, Wakamatsu T, Kanezaki M, Katsura K, Koehler M, Ellis C, Gagnon R, Allen K, Martin AM, Sasaki Y, Takashima S. Tokyo Metropolitan Komagome Hosp, Japan; Aichi Cancer Ctr Hosp, Japan; Nat. Cancer Ctr, Tokyo, Japan; GSK, Japan; GSK, PA; Saitama Med Univ, Japan; Shikoku Cancer Ctr, Ehime, Japan. 5115 EGFR, pAkt and pPI-3 kinase are co-expressed in circulating tumor cells of breast cancer patients. Kallergi G, Kalykaki A, Agelaki S, Mavroudis D, Georgoulias V. School of Medicine, University of Crete, Heraklion, Crete, Greece; University General Hospital of Heraklion, Heraklion, Crete, Greece. 5116 Expression of estrogen receptors ĝ in triple negative breast cancer. Litwiniuk M, Filas V, Breborowicz J. Poznan University of Medical Sciences, Poznan, Poland. CD146-downstream signaling mediating breast tumour invasion/metastasis. Yousief ZA, Abdraboh ME, Masood HM, Ouhtit A. Louisiana State University Health Sciences Center; Stanley S Scott Cancer Center, New Orleans, LA. 5117 Immunohistochemical expression of CK5/6, CK17, ERß in triple negative breast cancer patients. Liu Z, Wu J, Ping B, Shao Z, Shen Z. Cancer Hospital, Shanghai, China. Xenograft model for the evaluation of breast cancer metastatic progression. Zang XP, Lerner MR, Brackett DJ, Pento JT. University of Oklahoma, HSC, Oklahoma City, OK. 5118 High phosphorylation of estrogen receptor Ĝ serine 167 and low p53 protein accumulation improve survival in estrogen receptor-positive breast cancer patients treated with tamoxifen. Sugiura H, Toyama T, Kondo N, Kobayashi S, Fujii Y, Yamashita H. Nagoya City University Graduate School of Medical Science, Nagoya, Aichi, Japan. Rhodiola crenulata decreases invasion and regulates cyclooxygenase-2 expression in a highly metastatic ER-negative breast cancer cell line. Doerner JL, Smith-Schneider S, Arenas RB. University of Massachusetts, Amherst, MA; Pioneer Valley Life Sciences Institute, Springfield, MA; Baystate Medical Center, Springfield, MA. 5119 Lymphangiogenesis in breast cancer: correlation with lymphatic microvessel density and clinicopathologic parameters. Lee I-k, Park Y, Kim D, Jo B-h, Lee W, Yoon S, Kim H, Park S-y. MizMedi Hospital, Seoul, Korea. Mammary fibroblasts express ERĝ1 and ERĝ2 and can modulate breast cancer behaviour in a co-culture model. Green CA, Scott DJ, Hughes TA, Cummings M, Hanby AM, Shaaban AA, Speirs V. University of Leeds, Leeds, W Yorks, United Kingdom. Characterization of estrogen receptor positive breast cancers: gene expression analysis of archived tumours. Thorat M, Morimiya A, Sledge G, Badve S. Indiana University, Indianapolis, IN. Tumor Cell Biology: Metastasis / Invasion 5110-5119 5110 5111 5112 5113 7:00-9:30 Controversies in Adjuvant Endocrine Therapy for Breast Cancer Identification of gene expression differences in primary breast tumors from node-negative and node-positive women. Field LA, Seebach JF, Love BJ, Deyarmin B, Kane J, Hooke JA, Ellsworth RE, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC; Invitrogen Informatics, Carlsbad, CA. Sponsored by Physicians Education Resource Register on line at: www.adjuvantai.cancerconferences.com For information, contact: Kathryn Wallace 214-367-3329 Fax: 214-367-3303 kathryn.wallace@pergrouplp.com Identification of a gene expression breast cancer metastasis profile. Seebach J, Field LA, Love B, Hollern K, Hooke JA, Ellsworth RE, Shriver CD. Walter Reed Army Medical Center, Washington, DC; Windber Research Institute, Windber, PA; Invitrogen Informatics, Carlsbad, CA. Genomic discrimination of metastatic from non-metastatic primary breast tumors. Ellsworth RE, Patney HL, Ellsworth DL, Love B, Hooke JA, Shriver CD. Windber Research Institute, Windber, PA; Invitrogen Informatics, Carlsbad, CA; Walter Reed Army Medical Center, Washington, DC. Tumor microenvironment in breast cancer metastasis: direct tissue protein profiling of tumor-associated stroma from invasive breast cancer patients with versus without axillary lymph node metastasis. Ellsworth DL, Seeley EH, Ellsworth RE, Deyarmin B, Sanders ME, Hooke JA, Caprioli RM, Shriver CD. Windber Research Institute, Windber, PA; Vanderbilt University, Nashville, TN; Walter Reed Army Medical Center, Washington, DC. SATELLITE SYMPOSIUM - Ballroom A Supported by an educational grant from Novartis Pharmaceuticals Corporation Sunday, December 7:00-9:00 POSTER SESSION 6 & CONTINENTAL BREAKFAST – Exhibit Hall B (#6001-6119, 5015) Prognosis and Response Predictions: Prognostic Factors II 6001-6034 6001 Loss of nuclear p27 is independently associated with young age at breast cancer diagnosis. DeMichele A, Mick R, Beaver J, Ruddy K, Sherman L, McNally S, Acs G, Wang Y, Feldman M, Norman S, Rebbeck T, Lee W, Weber B. University of Pennsylvania, Philadelphia, PA. 6002 Stratifying primary operable breast cancers by steroid and HER-2 expression status predicts short term disease free survival. Brouckaert O, Pintens S, Van Belle V, Van Huffel S, Amant F, Leunen K, Smeets A, Berteloot P, Van Limbergen E, Decock J, Hendrickx W, Weltens C, Van den Bogaert W, Vanden Bempt I, Drijkoningen M, Paridaens R, Wildiers H, Vergote I, Christiaens M-R, Neven P. UZ Leuven, Leuven, Belgium; ESAT; UZ Leuven. 6003 Comparison of prognostic value of hormonal receptors (HR) and HER-2 overexpression on overall survival (OS) in breast cancer. Tacca O, Abrial C, Penault-Llorca F, Mouret-Reynier M-A, Raoelfils I, Ferrière J-P, Gimbergues P, Curé H, Chollet P, Durando X. Centre Jean Perrin, Clermont Ferrand, France; INSERM U484, Clermont Ferrand, France; Université d’Auvergne, Clermont Ferrand, France; Institut Jean Godinot, Reims, France. 6004 6005 6006 6007 6008 Correlation of ER/PR status and HER-2 status in invasive breast carcinoma. Bloom KJ, Kyshtoobayeva A, Chen S, Hii A. CLARiENT, Aliso Viejo, CA. Prognostic significance of HER2 status in women with inflammatory breast cancer. Dawood S, Broglio K, Yang W-T, Cristofanilli M, Kau S-W, Hortobagyi GN, Gonzalez-Angulo AM. MD Anderson Cancer Center, Houston, TX. Validation of an immunohistochemical biomarker for identifying Her2+ patients at high risk of recurrence. Seitz RS, Ross DT, Ring BZ, Beck RA, Khoury T, Vardarajan R, Iqbal J, Kulkarni S, Janarthanan BR, Hicks DG. Applied Genomics, Inc, Huntsville, AL; Applied Genomics, Inc, Burlingame, CA; Roswell Park Cancer Institute, Buffalo, NY. Prognostic value of both HER-2 and VEGF-A mRNA overexpression in primary tumors of high-risk breast cancer patients. Fountzilas G, Skarlos D, Wirtz RM, Dafni U, Stropp U, Pectasides D, Papakostas P, Markopoulos C, Karapanagiotis K, Polichronis A, Timotheadou E, Grimani I, Samantas E, Kosmidis P, Kalogeras KT. Hellenic Cooperative Oncology Group (HeCOG), Athens, Greece; Siemens Medical Solutions Diagnostics GmbH, Leverkusen, Germany. The pathological characteristics of gestational breast cancer. What is different? Ives A, Harvey J, Sterrett G, Saunders C, Semmens J. The University of Western Australia, Perth, WA, Australia; PathWest, Perth, WA, Australia; Curtin University of Technology, Perth, WA, Australia. 6009 The mitotic activity index is able to separate two prognostic subgroups in grade II estrogen receptor (ER)-positive nodenegative breast carcinomas. Geha S, Mazouni C, Spielmann M, Garbay J-R, Bourgier C, Delaloge S, Andre F, Mathieu M-C. Institut Gustave-Roussy, Villejuif, France; Hopital La Timone, Marseille, France. 6010 Assessing final pathological response to neoadjuvant chemotherapy using diffuse optical spectroscopy. Tanamai VW, Cerussi AE, Hsiang D, Mehta R, Tromberg BJ. University of California, Irvine, CA. 6011 The ProEx Br immunohistochemical assay has prognostic utility in early stage breast cancer using a manual scoring method. Chatterjee A, He Q, Nelson R, Gore M, Hudson R, Murphy PG, Malinoski D, Fisher TJ, Bigras G, Hugh J, Whitehead CM. BD Diagnostics Tripath, Durham, NC; Dynacare Kasper Medical Laboratories, Edmonton, AB, Canada. 6012 CXCR4 coexpression with EGFR/HER2 positivity in breast cancer is a poor prognostic factor in patients with isolated tumor cells in bone marrow. Cabioglu N, Igci A, Ozmen V, Muslumanoglu M, Dagoglu T, Sahin AA, Yildirim EO, Aktas E, Bilgic S, Price JE, Deniz G, Kecer M. University of Istanbul, Istanbul Medical Faculty, Istanbul, Turkey; UT MD Anderson Cancer Institute, Houston, TX; University of Istanbul, Institute of Experimental Medical Research, Istanbul, Turkey; UT MD Anderson Cancer Center, Houston, TX. 6013 Characterization of a good prognosis set of genes in breast cancer patients with at least 5 involved lymph nodes. Sevenet N, Badel A, Marquand E, Cuvier C, de Roquancourt A, Geneix C, Janin A, Launay J-M, Cottu PH, Camproux A-C, Marc E. Hospital Lariboisiere, Paris, France; Universite Denis Diderot, Paris, France; Hospital Saint Louis, Paris, France; Institut Curie, Paris, France. 6014 Cytogenetic heterogeneity within breast tumor specimens is revealed by the eXagenBC test. Davis LM, Tang L, Carpio C, Garcia N, Bauer R, Perrine M, Sanchez L, Chakraborty S, Zhou F, Flejter W, Tepperberg J, Alsobrook J. Exagen Diagnostics, Albuquerque, NM; LabCorp America, Brentwood, TN; LabCorp America, Research Triangle Park, NC. 6015 An alternatively spliced variant of cyclin D1 is present in human breast carcinoma. Gupta-Abramson V, Feldman M, Troxel A, Wang Y, Sherman L, McNally S, Lee W, Diehl A, DeMichele A. University of Pennsylvania, Philadelphia, PA. 6016 Evaluation of prognostic factors influencing the therapeutic management of post-treatment metastatic breast cancer. A retrospective study on 1096 patients who have been treated between 1980 to 2005 at the Centre Antoine Lacassagne. Largillier R, Chamorey E, Doyen J, Courdi A, Ettore F, Maestro C, Raoust I, Lallement M, Namer M, Ferrero JM. Centre Antoine Lacassagne, Nice, France. 6017 Brain metastases in HER2+ metastatic breast cancer patients: analysis of prognostic factors. Henry S, Pierga J-Y, Asselah J, Cottu P, Mignot L, Sigal-Zafrani B, Bollet M, Diéras V. Institut Curie, Paris, France. 6018 Clinical outcome of patients with triple negative breast cancer who develop brain metastasis. Hines SL, Vallow L, Tan W, Jain A, Perez E. Mayo Clinic, Jacksonville, FL. 6019 Characteristics of breast cancer patients with central nervous system metastases and factors associated with survival after development of central nervous system metastasis. Harputluoglu H, Dizdar O, Aksoy S, Kilickap S, Dede DS, Ozisik Y, Guler N, Barista I, Gullu I, Selek U, Cengiz M, Zorlu F, Tekuzman G, Altundag K. Hacettepe University Institute of Oncology, Ankara, Turkey. 6020 Brain metastases in breast cancer: a retrospective cohort study of 187 patients and prognostic markers determination. Svoboda M, Fabian P, Ondrova B, Palacova M, Grell P, Gombosova J, Princ D, Slaby O, Slampa P, Vyzula R. Masaryk Memorial Cancer Institute, Brno, Czech Republic. 6022 Topoisomerase 2 Ĝ gene amplification and protein expression in fresh and recurrent breast cancers. Tseng LM, Liu JM, Lan C, Lin LC, Hsu DH, Chang CP, Kao HL. Taipei-Veterans General Hospital and National Yang Ming University Medical School, Taipei, Taiwan; National Health Research Institutes, Taipei, Taiwan; Roch Products Ltd., Taipei, Taiwan. 6023 6024 6025 6026 6027 Cyclin-dependent kinase 1 and 2 activity as prognostic markers in early breast cancer. van Nes JGH, Smit VTHBM, Putter H, Kuppen PJ, Kim SJ, Masuda N, Inaji H, Yoshidome K, Tsujimoto M, Akiyama F, Tsukamoto F, Ishihara H, Noguchi S, van de Velde CJH. Leiden University Medical Centre (LUMC), Leiden, Netherlands; LUMC, Leiden, Netherlands; Graduate School of Medicine, Osaka Univ., Suita, Japan; Sysmex Corporation, Kobe, Japan; Osaka National Hospital, Osaka, Japan; Osaka Medical Center for Cancer & Cardiovascular Diseases, Osaka, Japan; Osaka Police Hospital, Osaka, Japan; Cancer Institute Hospital, Koto-ku, Japan; Osaka Kosei-Nenkin Hospital, Osaka, Japan. Prognosis and clinical outcome of patients with node negative ≤ 1cm breast cancer. Amar S, Ann ME, Geiger XJ, Rebecca MB, Winston T, Kyle CE, Beiyun C, Boughey JC, Edith PA. Mayo Clinic Jacksonville, Jacksonville, FL; Mayo Clinic Scottsdale, Scottsdale, AZ; Mayo Clinic Rochester, Rochester, MN. MAPK expression is associated with poor outcome in patients with hormone receptor negative breast cancer. Eralp Y, Derin D, Ozluk Y, Yavuz E, Guney N, Saip P, Muslumanoglu M, Igci A, Kucucuk S, Dincer M, Aydiner A, Topuz E. Istanbul University Institute of Oncology, Istanbul, Turkey; Istanbul University, Istanbul Medical Faculty, Istanbul, Turkey. The role of the stromal immune response in breast cancer recurrence. Hall JA, Bertos N, Finak G, Pepin F, Zhao H, Sadekova S, Meterissian S, Hallett M, Park M. McGill University, Montreal, QC, Canada. Comparison of patients with “triple negative” breast cancer (ER-, PR-, HER2-) in a cohort of 1052 patients treated in a single institution between 1999 and 2007. Kantelhardt EJ, Pauli N, Grosse R, Vetter M, Holzhausen HJ, Strauss HG, Thomssen C. Martin Luther University, Halle, Germany. 6028 Obesity at diagnosis increases relapse rate and shortens disease free interval in breast cancer patients. Quispe D, Hussain S, Leveau MQ, Mansour R, Burton GV, Shi R, Sun A. Louisiana State University Health Sciences Center, Shreveport, LA. 6029 Elevated MIB-1(%) and c-myc amplification are relevant prognosticators of ER positive/HER2 negative (“luminal A”) primary breast cancers. Schlotter CM, Wassmann K, Vogt U. Klinikum Ibbenbueren, Ibbenbueren, NRW, Germany; European Laboratory Association, Ibbenbueren, NRW, Germany. 6030 Allelic imbalance and predictors of outcome in ipsilateral breast tumor recurrences after systemic therapy for early stage breast cancer. Zekman R, Jaiyesimi I, Nadeau L, Mitchell C, Wallace M, McGrath S, Wills S, Goldstein N, Vicini F. Division of Hematology/ Oncology; William Beaumont Hospital, Royal Oak, MI. 6031 Impact of progesterone receptor (PR) status on survival of estrogen receptor (ER) positive women with invasive breast cancer (IBC). Ingle AM, Kumar P, Dagen T, Day K, Baney B, Galley AS. Children’s Oncology Group, Arcadia, CA; Mount Nittany Medical Center, State College, PA. 6032 Tumor biology of breast carcinoma in elderly women: comparison between elderly and young postmenopausal women. Okanami Y, Iwase T, Kimura K, Morizono H, IIjima K, Miyagi Y, Nishimura S, Tada K, Makita M, Horii R, Akiyama F. Cancer Institute, Koto-ku, Ariake 3-10-6, Tokyo, Japan. 6033 A community-based single institution registry study of treatment outcomes in breast cancer patients with 4 or more positive lymph nodes. Rivkin SE, Moon J, Atwood M, Tennent N. Swedish Medical Center, Seattle, WA. 6034 HMGA2 with uPAI/PAI-1 as prognostic factors in node negative breast cancer patients. Wischnewsky M, Boecker W, Meyer A, Milde-Langosch K, Bullerdiek J. University of Bremen, Bremen, Germany; University of Muenster, Muenster, Germany; University Hospital HamburgEppendorf, Hamburg, Germany. Epidemiology and Outreach: Advocacy/Education 6035-6046 6035 Defining endpoints for recurrence in randomized controlled trials of systemic therapy for early breast cancer: a call for standardization. Kilburn LS, Peckitt C, Ireland E, Bliss JM. The Institute of Cancer Research, Sutton, Surrey, United Kingdom. 6036 Has the quality of early breast cancer randomized controlled trials publications improved since CONSORT? A systematic review. Peckitt C, Ireland E, Kilburn LS, Bliss JM. The Institute of Cancer Research, Sutton, Surrey, United Kingdom. 6037 Moving from informed consent to informed choice: an ethical imperative. Devine P, Perlmutter J, Carbine N, Chingos D, Brady C. Cancer Information & Support Network (CISN), Auburn, CA. 6038 BreastCancerTrials.org: from regional pilot to nation-wide clinical trial matching service. Cohen EJ, Bechtold T, Laird J, Anand A, Ernest ML, Pederson, Melisko M, Park J, Hogarth M, Esserman LJ. UCSF, San Francisco, CA; UC Davis, Davis, CA. 6039 Inflammatory breast cancer biorepository: research collaboration. Mason G, Johnson O. Inflammatory Breast Cancer Research Foundation, Bainbridge Island, WA. 6040 Community-based outreach is an effective strategy for linking underserved women to breast cancer screening: data from the Avon Foundation Breast Care Fund. Opdyke KM, Gujrati ML, McCulloch A, Gates-Ferris K, Hurlbert M. Cicatelli Associates Inc., New York, NY; Avon Foundation Breast Cancer Crusade, New York, NY. 6041 Improving access to care in an AVON Foundation Comprehensive Breast Center (AFCBC) serving a predominantly urban African American (AA) patient population. Gabram S, Lund MJ, Lamson P, Harrison C, Koenig E, Bates S, Bumpers H, Green V, Gundry K, Okoli J, Rizzo M, Roberson S, Brawley O. Winship Cancer Institute, Emory University; Georgia Cancer Center for Excellence at Grady; Rollins School of Public Health, Emory University; Morehouse School of Medicine, Atlanta, GA. 6042 A comprehensive diagnostic program for medically underserved women with abnormal breast screening evaluations in an urban population. Palmieri FM, DePeri ER, Mincey BA, Smith JA, Wen LK, Chewar DM, Perez EA. Mayo Clinic, Jacksonville, FL; First Coast Dermatology and Internal Medicine, Jacksonville Beach, FL; Pfizer Oncology, New York, NY. 6043 Enhancing communication between oncologists and breast cancer patients. Kirk MC, Parker B. Y-ME National Breast Cancer Organization, Chicago, IL. 6044 Upfront: new perspectives on breast cancer – report by the Canadian Breast Cancer Foundation-Ontario Chapter (CBCF-OC). Easton B, Trussler T, Wood S, Verma S. Canadian Breast Cancer Foundation, Ontario Chapter, Toronto, ON, Canada; Ottawa Regional Cancer Center, Ottawa, ON, Canada. 6055 Incidence and tumor characteristics of breast cancer diagnosed before and after implementation of a population-based screening-program. Hofvind S, Sørum R, Thoresen S. The Cancer Registry of Norway, Oslo, Norway; University of Vermont, Burlington, VT; GlaxoSmithKline Norway, Oslo, Norway. 6045 Counselling women with breast cancer - whose line is it anyway? Court FG, Scarrott S, Cassidy-Gray M, Thomas A, Vestey S, Bristol J, Ghilchik M, Chan HY. Cheltenham General Hospital, Cheltenham, United Kingdom. 6056 6046 Identification and prioritization of unmet medical, educational and psychosocial needs in patients with metastatic breast cancer: results of a patient survey. Kirk M. Y-ME National Breast Cancer Organization, Chicago, IL. The wish for pregnancy after breast cancer, results of a French survey on 269 youngs breast cancer survivors. Dupré P-FPF, Menez-Orieux CC, Dravet FF, Barrière PP, Classe J-MJM. University Hospital of Brest, Brest, Finistère, France; University Hospital of Nantes, Nantes, Loire Atlantique, France; Anti Cancer Center, Saint Herblain, Loire-Atlantique, France. 6057 Survival of breast cancer over the last 30 years in a cohort of 7651 women and up-to-date estimates for patients recently diagnosed. Huiart L, Bardou V-J, Jacquemier J, Puig B, Tallet A, Reyrat E, Tarpin C, Buttarelli M, Extra J-M, Houvenaeghel G. Institut Paoli-Calmettes; FNCLCC, Paris; Institut Paoli-Calmettes, Marseille, France. 6058 Ethnicity, multiparity and the risk of premenopausal breast cancer. A population-based, multi-ethnic study from Singapore. Verkooijen HM, Yap K, Bhalla V, Chow KY, Chia KS. National University of Singapore, Singapore, Singapore; Geneva University, Geneva, Switzerland; Health Promotion Board, Singapore, Singapore. 6059 Time distribution of the recurrence risk for Chinese breast cancer patients undergoing surgery. Yin W, Lu J, Liu G, Di G, Wu J, Shen K, Shen Z, Shao Z. Cancer Hospital/Cancer Institute, Fudan University, Shanghai, China. 6060 The rates of chemotherapy-induced amenorrhea in patients treated with different regimen at different ages in Chinese breast cancer paients. Zhou L, Yin W, Lu J, Di G, Wu J, Shen K, Han Q, Shen Z, Shao Z. Cancer Hospital, Shanghai, China. Epidemiology and Outreach: Epidemiology 6047-6060 6047 6048 6049 A family history of breast or ovarian cancer further increases the risk of secondary leukemia, especially chronic leukemia, in breast cancer patients. Verkooijen HM, Fioretta G, Rapiti E, Vlastos G, Neyroud-Caspar I, Chappuis PO, Bouchardy C. Geneva Unversity, Geneva, Switzerland; National University of Singapore, Singapore, Singapore; Geneva University Hospitals, Geneva, Switzerland. HER2 status in a US population-based cohort: results from a tissue microarray-based analysis of 2,898 breast cancers from women enrolled in the nurses’ health study. Tamimi RM, Deitz AC, Schnitt SJ, Colditz GA, Collins LC. Brigham and Women’s Hospital and Harvard School of Public Health, Boston, MA; GlaxoSmithKline, Philadelphia, PA; Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA; Washington University School of Medicine, St. Louis, MO. registHER: patient characteristics and time course of CNS metastases in patients with HER2-positive metastatic breast cancer. Yardley DA, Kaufman PA, Mayer M, Ulcickas Yood M, Tan-Chiu E, Brufsky AM, Rugo HS, Tripathy D, Brammer MG, Paik S. Sarah Cannon Research Institute, Nashville, TN; Dartmouth-Hitchcock Medical Center, Lebanon, NH; Patient Advocate, New York, NY; EpiSource LLC, Yale University School of Medicine, New Haven, CT; Florida Cancer Care, Tamarac, FL; University of Pittsburgh Cancer Center, Pittsburgh, PA; UCSF Comprehensive Cancer Center, San Francisco, CA; University of Texas Southwestern Medical Center, Dallas, TX; Genentech, Inc., South San Francisco, CA; National Surgical Breast and Bowel Project, Pittsburgh, PA. 6050 Short-term cancer risk in a cohort of 2,353 women with high-risk breast lesions. Shim V, Puliganda B, Collins L, Jiang SF, Callahan ME, Kutner S, Habel LA. Kaiser Permanente, Oakland, CA; Beth Israel Deaconess Medical Center, Boston, CA; Kaiser Permanente, Santa Teresa, CA. 6051 Carcinoma and atypical hyperplasia are frequent findings in women with macromastia undergoing reduction mammoplasty: a prospective study. Ambaye AB, Goodwin A, MacLennan SE, Suppan T, Naud S, Weaver DL. Pathology; University of Vermont, Burlington, VT. 6052 Osteoporosis and breast cancer treatment. Quispe D, Shi R, Leveau MQ, Burton G, Sun A. Louisiana State University Health Sciences Center, Shreveport, LA. 6053 Prevalence of anemia in hospitalized French cancer patients: results of a one-day cross-sectional survey. Delaloge S, Hennequin C, Lemarie E, Zureik M, Castaigne S, Tourani J-M. Institut Gustave Roussy, Villejuif Cedex, France; Hopital Saint Louis, Paris, France; CHU - Hopital Bretonneau, Tours Cedex, France; Faculte de Medecine Bichat, Paris, France; Hopital Andre Mignot, Le Chesnay, France; CHU - Hopital La Miletrie, Poitier Cedex, France. Treatment: Chemotherapy - New Drugs and Formulations 6061-6074 6061 HKI-272, an irreversible pan erbB receptor tyrosine kinase inhibitor: preliminary phase 2 results in patients with advanced breast cancer. Burstein H, Awada A, Badwe R, Dirix L, Tan A, Jacod S, Lustgarten S, Vermette J, Zacharchuk C. Dana Farber Cancer Institute, Boston, MA; Medical Oncology Clinic, Brussels, Belgium; Tata Memorial Hospital, Mumbai, India; Medische Oncologie, Wilrijk, Belgium; Cancer Institute of New Jersey, New Brunswick, NJ; Wyeth Research, Paris, France; Wyeth Research, Cambridge, MA. 6062 Preliminary results of a phase 2 study of bosutinib (SKI606), a dual Src/Abl kinase inhibitor, in patients with advanced breast cancer. Campone M, Bondarenko I, Brincat S, Epstein RJ, Munster PN, Dubois E, Martin EC, Turnbull K, Zacharchuk C. Centre René Gauducheau, St. Herblain, France; Dnepropetrovsk State Medical Academy, Dnepropetrovsk, Ukraine; Sir Paul Boffa Hospital, Floriana, Malta; Queen Mary Hospital, Pokfulam, Hong Kong; H. Lee Moffitt Cancer Center, Tampa, FL; Wyeth Research, Paris, France; Wyeth Research, Cambridge, MA. 6063 mTOR inhibitor nanoparticle albumin-bound (nab) rapamycin is effective in a breast cancer xenograft model. Trieu V, De T, Yim Z, Cordia J, Yang A, Beals B, Ci S, Nguyen P, Louie L, Desai N. Abraxis BioScience, Inc., Los Angeles, CA. 6064 6065 6066 A multicenter phase Ib study of the safety, pharmacokinetics, biological activity and clinical efficacy of INCB7839, a potent and selective inhibitor of ADAM10 and ADAM17. Infante J, Burris HA, Lewis N, Donehower R, Redman J, Friedman S, Scherle P, Fridman J, Li J, Emm T, Troy S, Eckhardt SG. Sarah Cannon Research Institute, Nashville, TN; Fox Chase Cancer Center, Philadelphia, PA; Johns Hopkins Cancer Center, Baltimore, MD; Incyte Corporation, Wilmington, DE; University of Colorado Health Sciences Center, Denver, CO. Preclinical characterization of INCB7839, a potent and selective inhibitor of ErbB ligand and HER2 receptor shedding: inhibition of ADAM10 and ADAM17 for the treatment of breast cancer. Fridman JS, Scherle PA, Liu X, Caulder E, Hansbury M, Yang G, Wang Q, Lo Y, Zhou J, Yao W, Newton RC, Yeleswaram S, Friedman SM, Vaddi K. Incyte Corporation, Wilmington, DE. Tanespimycin (an Hsp90 inhibitor) and trastuzumab is an active combination in patients (pts) with Her2-positive trastuzumab-refractory metastatic breast cancer (MBC): phase 2 trial. Modi S, Stopeck A, Kinden H, Sugarman S, Ma W, Solit D, Kersey K, Johnson R, Hannah AL, Hudis C. Memorial Sloan-Kettering Cancer Center, New York, NY; Arizona Cancer Center, Tucson, AZ; Seattle Cancer Care Alliance, Seattle, WA; Kosan Biosciences, Hayward, CA. 6067 Withdrawn. 6068 CTEP-sponsored phase I/II trial of paclitaxel and low dose suramin in metastatic breast cancer. Shapiro CL, Sheils D, Barton L, Young D, Shen T, Chen L, Wei Y, Au J. The Ohio State University Medical Center and James Cancer Hospital, Columbus, OH; The Ohio State University Medical Center and Comprehensive Cancer Center, Columbus, OH; The Ohio State University, Columbus, OH. 6069 Combination therapy with the novel epothilone B analog, ixabepilone, plus capecitabine has efficacy in ER/PR/HER2negative breast cancer resistant to anthracyclines and taxanes. Rugo HS, Thomas ES, Lee RK, Fein LE, Peck R, Verrill M. UCSF Comprehensive Cancer Center, San Francisco, CA; Kaiser Permanente, Oakland, CA; The St. Luke’s Medical Center, Quezon City, Philippines; The Centro de Oncologia Rosario, Sante Fe, Argentina; Bristol-Myers Squibb, Wallingford, CT; Northern Institute for Cancer Research, Newcastle upon Tyne, United Kingdom. 6070 A phase II trial of trastuzumab, weekly ixabepilone (BMS247550) and carboplatin (TIC) in patients with HER2/neupositive (HER2+) metastatic breast cancer (MBC): a trial coordinated by the Eastern Cooperative Oncology Group (E2103). Moulder S, Wang M, Gradishar W, Perez EA, Sparano J, Pins M, Sledge G. University of Texas, M.D. Anderson Cancer Center, Houston, TX. 6071 A phase 1 study of ARRY-543, a potent, selective, reversible inhibitor of ErbB receptors. Gelmon K, Kane K, Kollmannsberger C, Maloney L, Gordon G, D’Aloisio S, W C, Litwiler K, Berlin J, Rothenberg M. BC Cancer Agency, Vancouver, BC, Canada; Vanderbilt-Ingram Cancer Center, Nashville, TN; Array Biopharma, Boulder, CO. 6072 Identification of a small molecule estrogen related receptor Ĝ specific antagonist that inhibits cell growth in MCF-7 and T47D breast cancer cells. Chisamore MJ, Cai S-J, Birzin ET, O’Donnell GT, Mosley RT, Zuck PD, Flores OA, Schaeffer JM, Rohrer SP, Wilkinson HA. Merck Research Laboratories, West Point, PA; Merck Research Laboratories, Rahway, NJ; Merck Research Laboratories, North Wales, PA. 6073 Exogenous histone H2A induces senescence and differentiation in breast cancer cells. Hadnagy A, Kaouass M, Mansour S, Beaulieu R, Balicki D. HôtelDieu du CHUM, Montréal, QC, Canada; Université de Montréal, Montréal, QC, Canada. 6074 Safety and pharmacokinetics of motesanib diphosphate (AMG 706) with paclitaxel or docetaxel for the treatment of locally recurrent, unresectable or metastatic breast cancer. de Boer R, White S, Mainwaring P, Koczwara B, Ye Y, Sun Y-N, Parson M, Braun A, Kotasek D. Western Hospital, Footscray, VIC, Australia; Austin Health, Heidelberg, VIC, Australia; Mater Hospital, South Brisbane, QLD, Australia; Flinders Medical Centre, Bedford Park, SA, Australia; Amgen Inc., Thousand Oaks, CA; Ashford Cancer Centre, Ashford, SA, Australia. Treatment: Other Therapies 6075-6086 6075 A prospective study to determine the prevalence of hypovitaminosis D in women with early stage breast cancer treated with an aromatase inhibitor and the benefit of vitamin D supplementation on musculoskeletal symptoms and overall QOL. Khan QJ, Reddy PS, Kimler BF, Baxa SE, Sharma P, Fabian CJ. University of Kansas Medical Center, Kansas City, KS; Cancer Center of Kansas, Wichita, KS. 6076 Lapatinib and capecitabine for the treatment of brain metastases in patients with HER2+ breast cancer - an updated analysis from EGF105084. Lin NU, Paul D, Dieras V, Liu M, Greil R, Roche H, Rubin SD, Zembryki D, Oliva C, Jayawardene D, Winer EP. Dana-Farber Cancer Institute, Boston, MA; Institut Jules Bordet, Brussels, Belgium; Institut Curie, Paris, France; Lombardi Comprehensive Cancer Center, Georgetown University Hospital; LKH, Salzburg, Austria; Centre Claudius Regaud, Toulouse, France; GlaxoSmithKline, Collegeville, PA; GlaxoSmithKline, Greenford, United Kingdom. 6077 Lapatinib Expanded Access Program (LEAP): design, operation and initial safety data. De Placido S, Link J, Conte PF, Tosi D, Kaufmann B, Byrne J, Rosenlund J, Gress M, Zembryki D, Oliva C. Universita degli Studi di Napoli Federico II, Italy; Breast Link Med Group, CA; Universita degli Studi di Modena e Regio Emilia, Italy; Instituto Nazionale per lo Studio e la Cura dei Tumori, Italy; Sheba Medical Centre, Israel; GSK, PA; GSK, United Kingdom. 6078 A phase I study of sunitinib plus paclitaxel for first-line treatment of advanced breast cancer: preliminary results. Kozloff MF, Chuang E, Roy J, Starr A, Gowland PA, Tarpey MJ, Collier M, Verk L, Kern K, Miller K. Ingalls Memorial Hospital, Harvey, IL; Cornell University, New York, NY; Indiana University Cancer Center, Indianapolis, IN; Pfizer Global Research and Development, San Diego, CA. 6079 Exploratory evaluation of a sequential administration of docetaxel and sunitinib in women with advanced breast cancer. Gianni L, Cardoso F, Mariani G, Isaksson-Friman E, BesseHammer T, Vigano L, Verk L, Rossi C, Giorgetti C, Bergh J. Istituto Nazionale per lo Studio e la Cura dei Tumori, Milano, Italy; Institut Jules Bordet, Brussels, Belgium; Karolinska Institute and University Hospital, Stockholm, Sweden; Pfizer Global Research and Development, San Diego, CA; Pfizer Italia S.r.l., Milano, Italy. 6080 AZD2171 for refractory breast cancer: a phase 2 trial. Mayer EL, Hamel S, Savoie J, Parker LM, Lin NU, Anderson K, Heymach JV, Gelman R, Ivy SP, Winer EP, Burstein HJ. DanaFarber Cancer Institute, Boston, MA; The University of Texas M. D. Anderson Cancer Center, Houston, TX; National Cancer Institute, Rockville, MD. 6081 Vandetanib with docetaxel as second-line treatment for advanced breast cancer: a double-blind, placebo controlled, randomized phase II study. Boer K, Lang I, Llombart-Cussac A, Andreasson I, Vivanco GL, Sanders N, Pover GM, Murray E. St Margit Hospital, Budapest, Hungary; National Institute of Oncology, Budapest, Hungary; Hospital Universitario Arnau de Vilanova, Lleida, Spain; Centrallasarettet, Vasteras, Sweden; Plaza de Cruces, Bizkaia, Spain; AstraZeneca, Loughborough, United Kingdom; AstraZeneca, Macclesfield, United Kingdom; New Groote Schuur Hospital, Cape Town, South Africa. 6082 Preclinical efficacy in breast cancer xenografts and phase 1 results of PTC299, a novel VEGF expression inhibitor. Hirawat S, Davis T, Weetall M, Elfring GL, Miller LL. PTC Therapeutics Inc, South Plainfield, NJ. 6083 Radiofrequency ablation versus cryoablation of small breast cancer with dedicated probes. Initial clinical experience. Manenti G, Perretta T, Cossu E, Contino G, Gioia A, Bonanno E, Masala S, Buonomo OC, Simonetti G. University Tor Vergata, Roma, RM, Italy. 6084 Role of differing estrogen receptor status on the proliferative effects of genistein. Rajah TT, Du N, Drews N, Cohn R. DePaul University, Chicago, IL. 6094 Triple negative, “basal-like” breast cancer: an institutional review. Herms BT, Jain D, Chagpar AB. University of Louisville Health Sciences Center, Louisville, KY. 6095 Assessment of efficacy and health related quality of life of proprioceptive neuromuscular facilitation (PNF) arm rehabilitation after surgical treatment of breast carcinoma. Bonanni V, Contino G, Lezzerini S, Buonomo OC. University Tor Vergata, Roma, RM, Italy. 6096 The physical therapist’s role in minimising impaired shoulder movement after axillary dissection. Tass DM. Capio Rivers Hospital, Sawbridgeworth, Hertfordshire, United Kingdom. 6097 Management and outcome of elderly patients (70 and over) with early stage breast cancer in rural community setting. McCoy JA, McCoy MM, Tezcan AZ, Tezcan H. North Idaho Cancer Center, Coeur d Alene, ID. 6098 High prevalence of vitamin D deficiency or insufficiency in breast cancer patients. Presant CA, Bosserman L, Ampudia M. Wilshire Oncology Medical Group, West Covina, CA. Tumor Cell Biology: Molecular Biology 6099-6111 6085 Maintenance hormonal and immunotherapy in metastatic breast cancer with a clinical benefit from anthracyclinepaclitaxel based induction chemotherapy. Recchia F, Candeloro G, Necozione S, Rea S. Civilian Hospital, Avezzano, AQ, Italy; Università degli Studi, L’Aquila, AQ, Italy. 6099 Changes in cyclins’ and CDKs’ mRNA expression during neoadjuvant treatment with letrozole. Larionov A, Murray E, Evans DB, Miller WR, Dixon JM. Western General Hospital, Edinburgh, United Kingdom; Novartis Institutes for BioMedical Research, Basel, Switzerland. 6086 Efficacy and safety of vaginal testosterone for atrophic vaginitis in breast cancer patients on aromatase inhibitors: a pilot study. Witherby SM, Johnson JV, O’Brien P, Demers LM, Mount SL, Muss HB. Fletcher Allen Health Care (FAHC)/University of Vermont College of Medicine (UVM), Burlington, VT; FAHC/ UVM, Burlington, VT; The Pennsylvania State University, Hershey, PA. 6100 Differences in recurrent genomic alterations between the molecular subtypes of breast cancer. Han W, Hwang K-T, Cho J, Jung E-M, Bae J-Y, Kang JJ, Yang S-J, Ko E, Lee JW, Kim S-W, Park I-A, Noh D-Y. Seoul National University College of Medicine, Seoul, Korea; Macrogen, Inc., Seoul, Korea. 6101 The corepressor SAFB in breast cancer - identification of target genes. Kaipparettu BA, Hille S, Tsimelzon A, Lee AV, Meyer R, Polo JM, Melnick A, Steffi O. Baylor College of Medicine, Houston, TX; Albert Einstein College of Medicine, Bronx, NY. 6102 The efficacy of sertraline for controlling menopausal symptoms in women with breast cancer. Wu M-F, Hilsenbeck SG, Tham Y-L, Kramer RM, Elledge RM, Chang JC, Friedman LC. Baylor College of Medicine, Houston, TX; University Hospitals Case Medical Center, Cleveland, OH. Potential role of dopamine and cAMP-regulated phosphoprotein, Mr 32000 (DARPP-32) in trastuzumab response in breast cancer. Narayan M, Kumar A, Lezon-Geyda K, Nairn AC, Harris LN. Yale University, New Haven, CT. 6103 Persistent peripheral neuropathy in breast cancer survivors treated with taxane chemotherapy. Crew KD, Adelson K, Weimer LH, Raptis G, Brafman L, Fuentes D, Ortiz Y, Hershman DL. Columbia University Medical Center, New York, NY; Mailman School of Public Health, New York, NY. Dysregulation of cofactor of BRCA1 expression in breast cancers. Sun J, Watkins G, Amleh A, Jiang WG, Li R. University of Texas Health Science Center at San Antonio, San Antonio, TX; School of Medicine Cardiff University, Cardiff, United Kingdom. 6104 Regulation of BRCA1 protein stability and its impact on estrogen biosynthesis in ovarian granulosa cells. Lu Y, Amleh A, Sun J, Li R, Hu Y. Institute of Biotechnology, UTHSCSA, San Antonio, TX. 6105 A novel anti-Patched1 antibody can suppress hedgehog signaling pathway in human breast carcinoma cells. Kubo M, Nakamura M, Kameda C, Tanaka H, Koga K, Mikami Y, Ikebe M, Tanaka M, Katano M. Graduate School of Medical Sciences, Kyushu University, 3-1-1 Maidashi, Higashi-Ku, Fukuoka, Japan. 6106 MicroRNA expression in primary breast tumors. Lowery AJ, Miller N, McNeill RE, Kerin MJ. National University of Ireland Galway, Galway, Ireland. 6107 MicroRNAs in triple negative breast cancer. Weidhaas J, Slack F. Yale University. Treatment: Patient Management 6087-6098 6087 6088 6089 6090 6091 6092 Influence of chemotherapy on bone in premenopausal women with breast cancer. Hadji P, Maskow C, Kalder M, Ziller V, Wagner U. PhilippsUniversity of Marburg, Marburg, Germany. Standardized evaluation of regional and institutional breast cancer outcomes. Beatty JD, Rees J, Atwood M, Pugliese M, Bolejack V. Swedish Cancer Institute, Seattle, WA. Challenges in metastatic breast cancer: optimistic vs realistic goals for treatment. Sepucha K, Ozanne E, Partridge A, Moy B. Massachusetts General Hospital, Boston, MA; Dana Farber Cancer Institute, Boston, MA. Differences in care of breast cancer patients in an underinsured population. Norton LE, Komenaka IK, Zork NM, Pennington, Jr RE, Clare SE, Bowling MW, Goulet, Jr RJ. Indiana University, Indianapolis, IN. 6108 6109 The expression of gene transcripts of telomere-associated genes in human breast cancer: correlation with clinicopathological parameters and clinical outcome. Salhab M, Jiang WG, Newbold RF, Mokbel K. St George’s University of London, London, United Kingdom; Cardiff University School of Medicine, Cardiff, United Kingdom; Brunel University, Uxbridge, Middlesex, United Kingdom. Expression of the putative breast cancer gene “breast cancer and salivary gland expression”; relationship with microRNA 154* and estrogen receptor status. Lowery AJ, Miller N, Kerin MJ. National University of Ireland Galway, Galway, Ireland. 6110 In vivo imaging of breast cancer using genetically engineered light-emitting bacteria. Park M, Yoon J, Jegal Y. Chonnam National University Hwasun Hospital, Hwasun-eup, Jeollanam-do, Republic of Korea. 6111 The four and a half LIM-only protein 2 mediates repression of Plk1 in breast cancer cells. Martin BT, Kleiber K, Kaufmann M, Strebhardt K. Medical School, University Frankfurt, Frankfurt/Main, Hessen, Germany. 6119 Rescheduled Poster Detection and Diagnosis: Circulating Markers 5015 9:00-12:00 HER-2 gene amplification is a marker for global genomic instability. Ellsworth RE, Deyarmin B, Patney HL, Hooke JA, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC. 6113 Array-CGH identifies CCNE1 amplification in ER/HER2 negative breast cancers. Natrajan R, Rodriguez-Pinilla SM, Marchio C, Moreno-Bueno G, Vatcheva R, Mahler-Araujo B, Lambros MBK, Mackay A, Palacios J, Ashworth A, Reis-Filho JS. ICR, London, United Kingdom; CNIO, Madrid, Spain; Instituto de Investigaciones Biomedicas Alberto Sols, Madrid, Spain; HHUU Virgen del Rocio, Seville, Spain. 6114 Novel Mdm2 intron 1 single nucleotide polymorphisms and their role in breast cancer. Paulin FE, O’Neill M, McGregor G, Cassidy A, Ashfield A, Ali CW, Baker L, Munro AJ, Lane DP, Thompson AM. Ninewells Hospital, University of Dundee, Dundee, United Kingdom. 6115 HER2/TOP2A amplicon in breast cancer: a microarray-based and chromogenic in situ hybridisation analysis. Arriola E, Lambros MBK, Marchio C, Tan D, Natrajan R, Rodriguez-Pinilla SM, Tamber N, Fenwick K, Mackay A, Jones C, Dowsett, Ashworth A, Reis-Filho JS. Institute of Cancer Research, London, United Kingdom; ICR, Sutton, United Kingdom. 6116 Genetic polymorphisms in the vascular endothelial growth factor (VEGF) gene and breast cancer risk. Langsenlehner T, Gerger A, Hofmann G, Kapp KS, Langsenlehner U. Medical University of Graz, Graz, Austria. 6117 Molecular genetics and immunophenotypical characterisation of micropapillary carcinomas of the breast. Marchio C, Iravani M, Natrajan R, Lambros MBK, James M, Savage K, Mackay A, Fenwick K, Tamber N, Schmitt FC, Ellis I, Bussolati G, Sapino A, Ashworth A, Reis-Filho JS. Institute of Cancer Research, London, United Kingdom; IPATIMUP, Porto, Portugal; University of Nottingham, Nottingham, United Kingdom; University of Torino, Torino, Italy. 6118 Impact of deleterious BRCA mutations and unclassified BRCA variants upon breast cancer characteristics at presentation. Miolo G, La Mura N, Lombardi D, Scalone S, Della Puppa L, Magri MD, De Giacomi C, Dolcetti R, Veronesi A, Viel A. Centro di Riferimento Oncologico, Aviano, PN, Italy. Heparanase expression in circulating lymphocytes of breast cancer patients is induced by the primary tumor and/or by distant metastasis. Theodoro TR, de Matos LL, Lambiasi AVL, Pinhal MAS, del Giglio A. Faculdade de Medicina da Fundação ABC, Santo André, Sãoi Paulo, Brazil. GENERAL SESSION 7 – Exhibit Hall D 9:00 71. Disease-free survival according to local immunohistochemistry for HER2 and central fluorescence in situ hydridization for patients treated with adjuvant chemotherapy with and without trastuzumab in the HERA (BIG 01-01) trial. McCaskill-Stevens W, Procter M, Goodbrand J, Azambuja E, Leyland-Jones B, Ruschoff J, Dowsett M, Wermuth P, Dolci S, Gelber RD, Piccart-Gebhart M. National Cancer Institute, Bethesda, MD; Frontier Science, Kingussie, United Kingdom; Jules Bordet Institute, Brussels, Belgium; Emory University, Atlanta, GA; Klinikum Kasseland TARGOS Molecular Pathology Gmbh, Kassel, Germany; Hoffmann-La Roche, Basel, Switzerland; Royal Marsden National Health Service Trust, London, United Kingdom; DanaFarber Cancer Institute, Boston, MA. 9:15 72. 3-year follow-up of trastuzumab following adjuvant chemotherapy in node positive HER2-positive breast cancer patients: results of the PACS-04 trial. Spielmann M, Roché H, Humblet Y, Delozier T, Bourgeois H, Serin D, Romieu G, Canon JL, Monnier A, Piot G, Maerevoet M, Orfeuvre H, Extra JM, Hardy AC, Martin AL, Kramar A, Genève J. Inst Gustave Roussy, France; Inst Claudius Régaud, France; UCL St-Luc, Belgium; Centre François Baclesse, France; CHU Poitiers, France; Inst Ste Catherine, Avignon, France; Centre Val d’Aurelle, France; CH ND Reine Fabiola, Belgium; CHG Montbelliard, France; CMC les Ormeaux, Le Havre, France; Clinique St Pierre, Ottignies, Belgium; CH Bourg en Bresse, France; Inst Curie, France; Cl Armoricaine St Brieuc, France; FNCLCC, France 9:30 73. Safety of pertuzumab plus trastuzumab in a Phase II trial of patients with HER2-overexpressing metastatic breast cancer which had progressed during trastuzumab therapy. Fumoleau P, Wardley A, Miles D, Verma S, Gelmon K, Cameron D, Gianni L, Conte PF, Ross G, McNally V, Baselga J. Centre Georges-François-Leclerc, Dijon, France; Christie Hospital, Manchester, UK; Mount Vernon Cancer Centre, Middlesex, UK; Ottawa Regional Cancer Center, Ottawa, ON, Canada; British Columbia Cancer Agency, Vancouver, BC, Canada; Western General Hospital, Edinburgh, UK; Oncologia Medica, Milano, Italy; Divisione di Oncologia Medica, Modena, Italy; *Roche products limited, Welwyn, UK; Vall d’Hebron University Hospital, Barcelona, Spain. 9:45 74. Combination of nab-paclitaxel and bevacizumab eradicates well-established tumors as well as lymphatic and pulmonary metastases in a MDA-MB-231 model of a highly metastatic human breast cancer. Ran S, Volk L, Bivens C, Trieu V, Desai N. Southern Illinois University, Springfield, IL; Abraxis BioScience, Inc., Los Angeles, CA. Tumor Cell Biology: Genetics 6112-6119 6112 Premature thelarche variant and estrogen receptor-Ĝ coregulator single nucleotide polymorphisms. Hartmaier RJ, Richter AS, Wit JM, Walenkamp MJE, Oesterreich S. Baylor College of Medicine, Houston, TX; Leiden University Medical Center, Leiden, Netherlands. 10:00 75. ErbB-2 inhibition activates notch-1 and sensitizes breast cancer cells to a gamma-secretase inhibitor: opportunity for a novel therapeutic combination. Osipo I, Patel P, Hao L, Whitehouse L, Strack P, Golde T, Albain K, Miele L. Loyola University Medical Center, Maywood, IL; Merck Research Laboratories, Boston, MA; The Mayo Clinic College of Medicine, Jacksonville, FL. 10:15 76. Parity regulates activation of p53 in human breast tissue. Crisi GM, Mathews L, Bentley B, Stueber K, Jerry DJ, SmithSchneider S. Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; Pioneer Valley Life Sciences Institute, Springfield, MA; Baystate Medical Center/Baystate Plastic Surgery Associates, Springfield, MA. 10:30 77. Cytrochrome P450 2D6 activity predicts adherence to Tamoxifen therapy. Rae JM, Sikora MJ, Henry NL, Li L, Kim S, Oesterreich S, Skaar T, Nguyen A, Desta Z, Storniolo AM, Flockhart DA, Hayes DF, Stearns V for the COBRA investigators. University of Michigan Comprehensive Cancer Center; University of Michigan School of Medicine; Indiana University; Baylor College of Medicine; Johns Hopkins University School of Medicine. COBRA is the Consortium on Breast Cancer Pharmacogenomics, an NIH supported Consortium of investigators at these institutions studying pharmacogenomics in the treatment of breast cancer. 10:45 78. Preliminary results of the UK Taxotere as Adjuvant Chemotherapy (TACT) Trial. Ellis PA, Barrett-Lee PJ, Bloomfield D, Cameron DA, Hall E, Johnson L, Johnston SRD, Bliss JM. Guys, Kings & St Thomas’s Hospital, London, United Kingdom; Velindre Hospital, Cardiff, Wales, United Kingdom; Royal Sussex County Hospital, Brighton, Sussex, United Kingdom; University of Leeds, Leeds, United Kingdom; Institute of Cancer Research, Sutton, Surrey, United Kingdom; Royal Marsden NHS Foundation Trust, London, United Kingdom. 11:00 79. Evaluating the efficacy of capecitabine given concomitantly or in sequence to epirubicin/ cyclophosphamide « docetaxel as neoadjuvant treatment for primary breast cancer. First efficacy analysis of the GBG/ AGO intergroup-study “GeparQuattro”. von Minckwitz G, Rezai M, Loibl S, Fasching P, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Mehta K, Untch M. University Hospital Frankfurt, Frankfurt, Germany; German Breast Group, Neu-Isenburg, Germany; Senologie, Brustzentrum, Düsseldorf, Germany; Frauenklinik mit Poliklinik, Erlangen, Germany; Senologiezentrum Ostschweiz SENZO, St. Gallen, Switzerland; Onkologie Bethanien, Frankfurt, Germany; Frauenklinik, München, Germany; Frauenklinik, Hannover, Germany; Frauenklinik, Berlin, Germany. 11:15 80. Characterizing the biology and response of locally advanced breast cancer in women undergoing neoadjuvant therapy: preliminary results from the I-SPY trial. Hylton N, Carey L, DeMichele A, Blume J, Broadwater G, Madhavan S, Rosen M, George S, Esserman L, ISPY Clinical, Research, Pathology and Radiology Investigators. Univ of California San Francisco, San Francisco, CA; Univ of North Carolina, Chapel Hill, NC; Univ of Pennsylvania, Philadelphia, PA; ACRIN, Philadelphia, PA; CALGB, Chapel Hill, NC; NCI-SPORE, Bethesda, MD. 11:30 81. Elucidating the stem and progenitor cell hierarchy in breast development and cancer - an essential role for GATA-3. Lindeman GJ, Asselin-Labat M-L, Sutherland KD, Barker H, Thomas R, Shackleton M, Hartley L, Robb L, Grosveld FG, van der Wees J, Visvader JE. The Walter and Eliza Hall Institute of Medical Research, Melbourne, Australia; The Royal Melbourne Hospital, Melbourne, Australia; Erasmus University, Rotterdam, Netherlands. 11:45 82. Decrease in tumorigenic breast cancer stem cells in primary breast cancers with neoadjuvant lapatinib. Li X, Creighton C, Wong H, Hilsenbeck SG, Osborne CK, Rosen JM, Lewis MT, Chang JC. Dan L Duncan Cancer Center at Baylor College of Medicine, Houston, TX. 12:00 ADJOURNMENT, 30th Annual San Antonio Breast Cancer Symposium Abstracts – Invited Speakers ML-1 Biomarking the estrogen responsiveness of breast cancer. Dowsett M. Royal Marsden Hospital Bene¿t from endocrine treatment of breast cancer is con¿ned to patients with estrogen receptor positive (ER+) disease. Development of modern endocrine treatments has been guided by the application of hormonal analyses, particularly of plasma estrogens, that can be used as pharmacodynamic markers. However, while these analyses may also be useful in de¿ning patients at risk of breast cancer they do not differentiate breast cancer patients that bene¿t from therapy from those that do not. Recent studies suggest that the differential bene¿t from tamoxifen and possibly other endocrine therapies may be partly determined by genetic host factors but molecular features of tumors are the major determinant of clinical heterogeneity. The degree of variability in responsiveness can be demonstrated and putative determinants evaluated in presurgical studies of endocrine therapy. The validity of changes in the proliferation marker Ki67 as an intermediate end-point of treatment bene¿t was demonstrated in the IMPACT trial. Reduced Ki67 occurs in over 90% of patients treated with third-generation aromatase inhibitors indicating that the large majority of ER+ patients bene¿t from a slowing of tumour growth even if this does not translate to an objective response to therapy. Similarly a global index of dependence on estrogen (GIDE) which integrates the transcriptional changes that occur with estrogen deprivation varies more than 30-fold among ER+ tumors. Unexpectedly, measures of apoptosis indicate that this is reduced during endocrine therapy. These reductions in cell death are markedly outweighed by the profound suppression of proliferation but may contribute to the relatively slow regressions seen with endocrine therapy. Despite compelling preclinical data, markers such as PgR and HER2 do not appear to de¿ne patients with a particularly high relative bene¿t of an aromatase inhibitor over tamoxifen. Further study of the molecular changes that occur with estrogen deprivation and association of these with clinical outcome may be expected to identify the hallmarks of breast cancer that are supported by estrogen stimulation and allow improved rationalisation of endocrine therapy ± other therapeutic agents. P-1 Management of symptoms in breast cancer survivors. Loprinzi CL. Mayo Clinic, Rochester, MN Given improved screening and early diagnosis of breast cancer, and also improved treatment for localized breast cancer, there is an increase in the number of breast cancer survivors, many destined to live for decades after their diagnosis. Breast cancer survivors can have many untoward symptoms related to their treatment and/or requiring different therapies than other women. Such symptoms include cognitive dysfunction, fatigue, chemotherapy induced neuropathy, weight gain, sexuality issues, vaginal dryness, and hot Àashes. For some of these symptoms, there are treatments which have been shown to be useful. For fatigue and weight gain, exercise and calorie restriction are helpful, while pharmacologic means of treating these symptoms have not delineated any helpful therapies. For hot Àashes, centrally acting agents, like newer antidepressants and gabapentin, have been identi¿ed as being valuable for some patients. For many of these symptoms, however, there are no good, identi¿ed therapeutic options for management. Neither the etiologies of cognitive dysfunction associated with cancer, or its treatment, nor helpful pharmacologic agents for this problem have been identi¿ed. For decreased libido, while testosterone combined with available estrogen appears to be helpful in women in general, testosterone without concomitant estrogen does not appear to be useful in female cancer survivors. While vaginal estrogen effectively treats vaginal atrophy in many women, new data demonstrating the bene¿ts of aromatase inhibitors raise concerns about the use of any treatment that could impact systemic estrogen in women with hormone sensitive cancers. At this time there are no pharmacologic therapies to recommend for preventing or treating chemotherapy-induced neuropathy. Continued research attention to the above noted issues is necessary to ¿nd improved therapies for control of these symptoms. S1 P-2 Multidisciplinary treatment guidelines across the continuum of care: the NCCN experience. Carlson RW, for the NCCN Breast Cancer Treatment Guidelines Panel. Stanford Cancer Center, Stanford, CA The National Comprehensive Cancer Network (NCCN) Breast Cancer Treatment Guidelines provide multidisciplinary, comprehensive, state-of- the-art treatment recommendations and strategies across the continuum of cancer care. The Guidelines are developed by a multidisciplinary expert panel using an evidence-based consensus process and are updated at least annually. Panel members represent the specialties of surgical oncology, medical oncology, radiation oncology, pathology, reconstructive surgery, and patient advocacy. Guideline modi¿cations are considered based upon recommendations or requests from breast cancer providers within the NCCN institutions, Panel members, patient advocacy organizations, industry, third party payors or individuals. Panel members are required to disclose ¿nancial conÀicts of interest verbally and in writing, must absent themselves from discussions where meaningful conÀicts exist, and conÀicts are published in the aggregate with the guidelines. Panel meetings over two - three days include a series of formal, issue focused presentations followed by an open discussion of any proposed guideline change. The ¿nal document is generated by an iterative process involving all panel members. All recommendations made by the guideline are associated with a corresponding category of evidence. The recommendations are presented in graphical, algorithmic form that is designed to follow the reasoning process of the expert clinician providing care. The guidelines are inclusive of treatment options, and an accompanying referenced manuscript provides the rationale and justi¿cation for the algorithmic recommendations. The guidelines are published in updated form annually on the NCCN web site (www.nccn.org) and in the Journal of the NCCN on a biennial basis. The American Cancer Society and NCCN publish a patient oriented version of the guideline updated on an annual basis. Over 250,000 copies of the guidelines are distributed or accessed annually. Separate, focused task forces are used to address in depth especially controversial issues in breast cancer treatment such as selection of adjuvant chemotherapy regimen, PET scanning, bisphosphonate use, methods of HER2 testing, and treatment of the older adult. The guidelines are complemented by an NCCN Outcomes Database that monitors the actual treatment delivered at NCCN institutions and allows for the identi¿cation of rates of compliance with guideline recommendations. A compendium is also published that allows third party payors to ef¿ciently identify the pharmaceutical agents recommended for speci¿c medical situations within the guidelines. The NCCN collaborates with breast cancer care providers in Latin America, Japan, and China to provide economically, socially, and culturely appropriate international, non-English versions of the NCCN Breast Cancer Guideline. P-3 Energy balance, insulin, and breast cancer. Pollak M. McGill University, Montreal, QC, Canada We will review (1) evidence for an adverse inÀuence of high body mass index (BMI) or high caloric intake on breast cancer prognosis (2) research regarding the underlying mechanisms and (3) implications for breast cancer prevention and treatment. While there is evidence that BMI inÀuences breast cancer risk, the relationship is modest and varies with menopausal status and other factors. BMI is more consistently identi¿ed as an important adverse prognostic factor. Women with higher BMI have higher circulating insulin levels associated with “insulin resistance” of classic insulin target tissues such as muscle and fat -- the extent to which cancer cells of a patient with insulin resistance and hyperinsulinism are sensitive to insulin stimulation is an important unanswered question, but insulin signaling is a candidate mediator of the effect of BMI on breast cancer prognosis. It has been recognized for decades that restriction of energy intake reduces carcinogenesis and attenuates aggressive cancer behavior in laboratory models. More recent experimental data provide early S2 Abstracts – Invited Speakers evidence that the growth of some cancers is increased when caloric intake of the host is increased. Increasing energy intake in these models is associated with increased insulin levels, but this does not demonstrate causality because circulating levels of many factors that might impact tumor growth are also changed. Clinical research provides further circumstantial evidence for a role of insulin or factors inÀuenced by or correlated with insulin levels in determining breast cancer prognosis: higher fasting insulin levels or c-peptide levels (a marker of insulin production) at time of diagnosis are associated with worse outcome. Furthermore, it is now recognized that breast cancers commonly express insulin receptors, IGF-I receptors, and hybrid insulin/IGF-I receptors, and that these can activate key downstream growth regulatory signaling pathways. All this has led to renewed interest in the clinical relevance of work carried out decades ago which provided evidence that insulin acts as a potent growth factor for breast cancer in vitro. Since obesity and hyperinsulinism are common (and increasing) in afÀuent societies, the public health impact of the adverse impact of these factors on breast cancer prognosis may be considerable. Furthermore, the population also includes women who are described as “metabolically obese, normal weight” individuals, and these may also have a relatively poor prognosis if diagnosed with cancer. Importantly, the metabolic abnormalities associated with obesity represent potentially modi¿able adverse prognostic factors. Lifestyle (diet and exercise) as well as pharmacologic (eg metformin) strategies are known to improve hyperinsulinism and the other metabolic abnormalities associated with obesity. Inhibitors of insulin/IGF signaling are also under study. There are important opportunites to use the post-operative adjuvant treatment setting to advance knowledge in this area. We hypothesize that any bene¿t of lifestyle or pharmacologic strategies that lower insulin levels will not be be homogeneously distributed in the breast cancer population, but rather will be of most bene¿t to those who are hyperinsulinemic at baseline. P-4 Radiation treatment planning for breast cancer: a journey through time. Pierce L. Recent improvements in breast cancer-speci¿c and overall survival shown best in the Overview are attributed, in part, to signi¿cant improvements in loco-regional control following comprehensive radiotherapy. The gains in survival, however, have been tempered by costly rates of excess mortality from causes other than breast cancer, primarily heart disease. Therefore treatment planning approaches which minimize treatment to uninvolved tissues are critical to the ultimate success achieved with radiation. Radiation treatment planning for breast cancer has changed dramatically through the years with modi¿cations in clinical target volumes, treatment delivery systems, and techniques. Early target volumes reÀected a Halstedian philosophy in which extensive (loco-) regional ¿elds were felt to be necessary for cure but through successive studies, volumes have been re¿ned that maintain high rates of loco-regional control while minimizing toxicity. Treatment delivery systems and techniques have evolved from clinically placed ¿elds treated with the limited depth dose characteristics of orthovoltage to two- and three-dimensional forward planned ¿elds and now, in some cases, to complex inversely planned ¿elds delivered with intensity modulated radiotherapy. The clinical bene¿t of these changes has been demonstrated in recent outcome studies. Optimization of each of these components of treatment planning has resulted in a convergence of treatment goals with the intent to optimize survival while decreasing toxicity. However, no one approach can be applied to all patients; thus, treatment planning must be individualized in each case. Trade-offs of treatment planning directives will be presented. MS1-1 Systems approach to growth factor signaling and to therapeutic intervention in breast cancer. Yarden Y. Weizmann Institute of Science, Rehovot, Israel Growth factors and their transmembrane receptors contribute to all steps of tumor progression, from the initial phase of clonal expansion, through angiogenesis and tmetastasis. Hence, the information relay system involved in growth factor signaling provides potential site for signal interception and tumor inhibition. A relevant example comprises the epidermal growth factor (EGF) and the respective receptor tyrosine kinase, namely ErbB-1/EGFR, which belongs to a prototype signaling module that drives carcinoma development. The extended module includes two autonomous receptor, EGFR and ErbB-4, and two nonautonomous receptors, namely: a ligand-less oncogenic receptor, HER2/ ErbB-2, and a kinase-dead receptor (ErbB-3). This signaling module is richly involved in human cancer and already serves as a target for several cancer drugs. Due to inherent complexity and a large amount of experimental data, we propose a systems approach to understanding ErbB signaling. EGF - to - ErbB signaling is envisioned as a bow-tie con¿gured, evolvable network, sharing modularity, redundancy and control circuits with robust biological and engineered systems. My presentation will concentrate on system controls, a plethora of negative feedback loops, which include E3 ubiquitin ligases, receptor endocytosis and newly transcribed genes. Because network fragility is an inevitable tradeoff of robustness, systems level understanding is expected to identify therapeutic opportunities for targeting aberrant activation of the network in human pathologies. Speci¿c examples will be discussed with an emphasis on gene expression and the control of metastsis. MS1-2 Targeting the HER network in breast cancer: therapeutic successes and failures. Osborne CK, Schiff R. Baylor College of Medicine, Houston, TX The HER network is a robust, complex, and redundant network providing important proliferation and survival signals to a subset of human breast cancer. It is a layered system consisting of an input layer of four receptors and their eleven ligands, a core processing unit or signaling pathway from the membrane to the nucleus, and an output layer consisting of transcription factors and the genes they regulate. The network is also controlled by a system of positive and negative regulatory circuits to ¿nely tune the system. Gene ampli¿cation of HER2, a critical player in the input layer, in 25% of breast cancer led to development of drugs targeting the pathway. In breast cancer, drugs that are currently in use target the receptor input layer to block the pathway. Trastuzumab binds to the external domain of HER2 and, thereby, inhibits signaling through the network. In metastatic breast cancer, the drug used alone induces responses in 30% of patients while the majority demonstrate de novo resistance. In the adjuvant setting about 50% of patients with HER2 expressing tumors bene¿t from trastuzumab with a sizable improvement in time to progression and survival. Still many patients demonstrate either de novo or acquired resistance to the drug. Considering the complexity of the network, resistance to trastuzumab could develop at several levels. One potential mechanism is incomplete blockade of signals generated by the various dimer pairs formed by this family of receptors. However, other drugs have been developed that target the pathway in slightly different ways including the tyrosine kinase inhibitors lapatinib, ge¿tinib, or erlotinib or the dimerization inhibitor pertuzumab. In preclinical models these drugs used in various combinations to more completely block signals from all heterodimers pairs is a more effective strategy than any of the agents used alone and is capable of completely eradicating some xenograft models of human breast cancer. Other xenograft models are resistant to combination therapy suggesting alternative mechanisms of resistance. The strategy of combining more than one HER pathway inhibitor in patients is now being studied in metastatic disease as well as the neoadjuvant and adjuvant settings. Strategies to identify and then circumvent other mechanism of resistance are an active area of research. Abstracts – Invited Speakers MS1-3 Identi¿cation of biomarkers of resistance to HER2 targeted therapy using loss of function genetic screens. Bernards R. The Netherlands Cancer Institute, Amsterdam, Netherlands Unresponsiveness to therapy is remains a signi¿cant problem in the treatment of cancer, also with the new classes of targeted therapeutics. In my laboratory, we use functional genetic approached identify biomarkers that can be used to predict responsiveness to clinicallyrelevant cancer therapeutics. We focus on the well-established targeted cancer drugs such as Trastuzumab. This drug targets a speci¿c molecule (HER2) that is over-expressed or in breast cancer. Nevertheless, it remains poorly explained why a signi¿cant number of tumors, which express the drug target, do not respond to the therapy. We aim to elucidate the molecular pathways that contribute to unresponsiveness to targeted cancer therapeutics using a functional genetic approach. This will yield biomarkers that can be used to predict how individual patients will respond to speci¿c drugs. Furthermore, this work may allow the development of drugs that act in synergy with the established drug in the treatment of cancer. To identify biomarkers that control tumor cell responsiveness to cancer therapeutics, we use both genome-wide gain-of-function genetic screens (with cDNA expression libraries) and genome wide loss-of-function genetic screens (with RNA interference libraries) in cancer cells that are sensitive to the drug-of-interest. We search for genes whose overexpression or down-regulation in cultured cancer cells confers resistance to the drug-of-interest. Once we have identi¿ed such genes, we ask if their expression is correlated with clinical resistance to the drug-ofinterest using tumor samples of cancer patients treated with the drug in question, whose response to therapy is documented. In this presentation, I will discuss how loss-of-function genetic screens can be used to identify mechanisms of resistance to Trastuzumab in breast cancer. MS2-1 The Women’s Health Initiative randomized trials of menopausal hormone therapy: results and impact on clinical practice. Chlebowski RT. Los Angeles Biomed Res Institute, Torrance, CA The Women’s Health Initiative (WHI) trial of combined conjugated equine estrogens (CEE) plus medroxyprogesterone acetate (MPA) was stopped early and reported in 2002 when overall health risks including coronary heart disease, stroke, pulmonary embolism and invasive breast cancer exceeded bene¿ts. Invasive breast cancers were diagnosed more frequently in the CEE + MPA group; hazard ratio (HR), 1.24 p=0.003 and were diagnosed at more advanced stage (p=0.04) compared with those in the placebo group. In the combined hormone group mammograms with abnormalities were increased by 74% after one year (p<0.001) and, in a sub-study, mammographic breast density was also signi¿cantly increased. The WHI trial of CEE alone for women with prior hysterectomy continued until 2006 and the global index of chronic disease events was equivalent in the hormone and placebo groups with no overall bene¿t seen for CEE alone use. Fewer invasive breast cancers were diagnosed in the CEE alone group (HR 0.80, p=0.09) and the frequency of mammograms requiring short interval follow-up was signi¿cantly increased, but not those with more serious abnormalities, in the CEE compared to placebo group (p<0.001). The risk bene¿t ratio for both the global index of chronic diseases and invasive breast cancer differed for CEE + MPA use in women with an intact uterus compared to results with CEE alone use in women with prior hysterectomy. As the clinical characteristic of the two study populations differ in several aspects, cautious interpretation is required. Subsequent to the WHI report of the CEE+MPA trial, a nearly 50% reduction in menopausal hormone therapy use occurred in the US, followed by a sharp decrease in breast cancer incidence S3 especially in postmenopausal women for receptor positive breast cancer beginning in 2003 and sustained through 2004. Potential associated factors inÀuencing this decrease will be discussed. WHI Investigators. JAMA 288:321, 2002; Chlebowski RT, Hendrix S, Langer R et al. JAMA 289:3243, 2003; Anderson GL, Limacher M, Assaf AR, et al. JAMA 292:1701, 2004; Stefanick M, Chlebowski RT. JAMA 242:1048, 2006; Anderson GL, Chlebowski RT, Rossouw J, et al. Maturitas 54:478, 2006. MS2-2 Hormone replacement therapy and breast cancer – a summary of results from other studies. Cuzick J. Wolfson Institute of Preventive Medicine The Women’s Health InitiativeWHI) has produced a wealth of interesting and provocative ¿ndings on the the risk of breast cancer and heart disease in relation to the use of hormone replacement therapy. For breast cancer, WHI found an increased risk associated with combined estrogen and progesterone therapy, but no increase and even a suggestion of a decreased risk with estrogen only therapy. While the ¿rst of these ¿ndings has generally been supported by most of the other studies, the second has not, where increased risks, which are generally smaller than those with combined therapy are the consensus ¿nding. While WHI has the undeniable strength of being a randomised study and so is not subject to the potential biases of obsevational studies, it does have limitations, primarily related to the late age at which women were randomised ( mean age 63y). The results of this study are compared and constrasted to those of the Oxford case-control overview, Harvard Nurse’s study, Million women study and other recent relevant ¿ndings with regard to these issues. Other points including the risks associated with use of progestin only preparations and tibolone, the potential interaction with other risk factors for breast cancer, duration of use and duration of risk after stopping treatment and the type/prognosis of the excess cancers are also examined. MS3-1 Learning from the brain: cancer stem cells in therapeutic resistance and as molecular targets. Rich JN. Duke University Medical Center Cancer biologists increasingly recognize that tumors are complex organs formed not only by neoplastic cells but also by supporting vasculature, immune cells, and ¿broblasts. This complexity of cellular heterogeneity of cancers has also extended to the neoplastic cells themselves. In an increasing number of cancers (most clearly in hematopoietic, central nervous system, and breast cancers), a restricted subset of tumor cells share have been de¿ned functionally as cancer stem cells through maintained self-renewal and in vivo tumorigenesis. Cancer stem cells may contribute to tumor growth, progression, and spread. In a recently published study (Bao, Nature, 2006), we demonstrated that radiation enriches for brain cancer stem cells and that cancer stem cells survive radiation treatment at a greater rate than the majority of tumor cells. Cancer stem cells form tumors after standard radiation doses with essentially no loss of potency. As radiation induces cell death primarily through DNA damage, we examined the role of the DNA damage checkpoint in cancer stem cell radioresistance. Cancer stem cells preferentially activate ATM and the checkpoint kinases, and a checkpoint kinase inhibitor sensitizes cancer stem cells to radiation. Studies from other groups investigating breast cancer cell line models con¿rmed that cells expressing cancer stem cell markers are resistant to radiation but also demonstrated that ectopic expression of Wnt or beta-catenin augmented the radioresistance of cancer stem cells (Phillips et al., 2006; Chen et al., 2007; Woodward et al., 2007). In additional unpublished studies, we have found that the development of chemotherapy resistance selects for speci¿c subpopulations of cancer stem cells. In summary, we have demonstrated that cancer stem cells are highly resistant to cytotoxic therapies through speci¿c molecular mechanisms that may be targeted with novel therapies. In another recent study (Bao, Cancer Research, 2006), we demonstrated that brain cancer stem cells promote tumor angiogenesis through S4 Abstracts – Invited Speakers expression of VEGF. Further, a novel anti-angiogenic therapy in clinical use for glioblastomas (bevacizumab, Avastin) speci¿cally blocks the impact of cancer stem cells on endothelial cells and potently attenuates tumor growth of cancer stem cells but not other tumor cells. In unpublished studies, we have found that cancer stem cells exhibit differential responses to a key regulator of tumor angiogenesis, hypoxia, than the majority of cancer stem cells. We have also determined that cancer stem cells display a highly invasive phenotype. Therapy directed against cancer stem cells may be more effective in controlling tumor growth but these therapies may have increased toxicities against somatic stem cells. We have initiated research efforts to identify molecular targeted therapies that may be effective against cancer stem cells and have identi¿ed gene products speci¿cally expressed by cancer stem cells that contribute to tumor malignancy suggesting that anti-cancer stem cell therapies can be developed to improve tumor control. Abstracts – General Sessions 11 High-dose chemotherapy with autologous stem-cell support versus standard-dose chemotherapy: meta-analysis of individual patient data from 15 randomized adjuvant breast cancer trials. Berry DA, Ueno NT, Johnson MM, Lei X, Lopez V, Caputo J, Bregni M, Demirer T. MDACC-EBMT Meta-Analysis Group, Houston, TX Background: The role of adjuvant high-dose chemotherapy (HDC) with autologous hematopoietic stem-cell transplantation for primary breast cancer at high risk of recurrence (at least 4 involved axillary lymph nodes) has not been well de¿ned. Individually, the available trials have limited power to determine whether HDC has any bene¿t for this indication, or for any subgroup of patients. Methods: Individual patient data from 15 known randomized trials were merged into a single database. Disease-free survival (DFS) was de¿ned as time from surgery to recurrence or death. Breast cancer speci¿c survival (BCSS) was de¿ned as time from surgery to death resulting from breast cancer or treatment-related toxicity. Overall survival (OS) was de¿ned as time from surgery to death. Cox proportional hazards regression compared the effect of HDC vs standard-dose chemotherapy (SDC) on DFS, BCSS and OS adjusted for age, trial and hormone receptor (HmR) status (positive if either estrogen (ER) and/or progesterone (PgR) receptor positive). Subgroup analyses were by age and HmR status. Results: A total of 6210 patients (3118 HDC, 3092 SDC) had median follow-up of 6 years (range 0 to 15.3). Median age was 46 years (range 20 to 67). HmR was positive in 46.8%, negative in 23.7% and missing in 29.5%. After adjusting for age and trial, HDC signi¿cantly prolonged DFS (hazard ratio (HR) 0.87; 95%CI 0.81-0.94; p=0.0001) but not BCSS (HR 0.93; CI 0.85-1.02; p=0.10) or OS (HR 0.95; CI 0.87-1.02; p=0.16). After adjusting as well for HmR in the subset for which it was available, HDC signi¿cantly prolonged DFS (HR 0.83; CI 0.77-0.90; p<0.0001) and had a modest and marginally signi¿cant bene¿t on BCSS (HR 0.88; CI 0.79-0.97; p=0.013) and OS (HR 0.89; CI 0.82-0.98; p=0.016). For BCSS and OS, neither age nor HmR had a statistically signi¿cant interaction with treatment yet there was a signi¿cant interaction between age and treatment for DFS. Conclusions: HDC as used in our 15 randomized trials prolongs DFS in adjuvant breast cancer. HDC has at most a modest bene¿t on BCSS and OS. Any bene¿ts of HDC in the context of contemporary regimens such as taxanes and targeted therapies are unknown. S5 12 Extended follow-up and analysis by age of the US Oncology Adjuvant trial 9735: docetaxel/cyclophosphamide is associated with an overall survival bene¿t compared to doxorubicin/cyclophosphamide and is well-tolerated in women 65 or older. Jones S, Holmes F, O’Shaughnessy J, Blum J, Vukelaj S, McIntyre K, Pippen J, Bordelon J, Kirby R, Sandbach J, Hyman W, Khandelwal P, Negron A, Richards D, Mennel R, Boehm K, Meyer W, Asmar L, Muss H, Savin M. US Oncology Research, Inc., Houston, TX; Vermont Cancer Center, Burlington, VT Background: At SABCS 2005 we reported 5-year results of a randomized trial of 4 cycles of docetaxel/cyclophosphamide (TC) compared to 4 cycles of standard (doxorubicin/cyclophosphamide (AC) in women with node(-) (∼50%) and node(+) early breast cancer (BC). A signi¿cant improvement in disease-free survival (DFS), but not overall survival (OS), was observed. (Jones, et al. JCO. 2006;24:5381) Older women are not commonly enrolled on adjuvant chemotherapy (CT) trials. Muss, et al reported that only 8% of women on CALBG trials were >65. (Muss, et al. JAMA. 2005;293:1073) In the AC/TC trial 16% (160 pts) were >65 years (yrs) of age. With 2 more yrs of follow-up, we now report on OS as well as the effect of treatment by age (using 65 as the cutoff) on outcome and toxicity. Patients and Methods: Pts were eligible if they had Stage I-III operable invasive BC with complete surgical excision of the primary tumor. Between June 1997 and December 1999, 1016 pts were assigned to 4 cycles of either standard-dose AC (60/600/mg/m2) [n=510], or TC (75/600mg/m2) [n=506], by intravenous infusion every 3 weeks as adjuvant CT. Radiation therapy (as indicated) and tamoxifen, for pts with hormone receptor positive disease, were given after completion of CT. Results: Baseline characteristics of all pts and those in the 2 age subgroups were well-matched. The median age in women <65 was 50 (range, 27-64) and for women >65 was 72 (range, 65-77). Median follow-up is now 6.9 yrs and the difference in OS between TC and AC is signi¿cant. Results are summarized in the table below: In the TC group, there were 75 DFS events (15%) and 57 deaths (11%); the AC group had 108 DFS events (21%) and 83 deaths (16%). Younger women in both the TC and AC groups had less febrile neutropenia (4.4% and 2.3%, respectively) compared with older women (7.7% and 3.7%, respectively [not signi¿cant]). Toxicity, by treatment, was similar in both age groups to the groups as a whole, and will be presented. Conclusions: With longer follow-up, TC was associated with improved DFS as well as OS compared to standard AC. TC should now be a standard non-anthracycline combination for early BC. In addition, TC was well-tolerated in older women without excessive toxicity compared to their younger counterparts, and may be preferable due to its lack of cardiotoxicity. Supported by a research grant from sano¿-aventis, Bridgewater, NJ. 6-year Results (%) by Regimen TC (# of pts) Overall DFS 85% 506 OS 88% 506 DFS <65 88% 428 DFS 65 82% 78 AC 79% 84% 82% 75% (# of pts) 510 510 428 82 P value 0.018 0.045 (HR) (0.69) (0.73) (0.64) (0.69) 13 Role of anthracycline-based therapy in the adjuvant treatment of breast cancer: ef¿cacy analyses determined by molecular subtypes of the disease. Slamon DJ, Mackey J, Robert N, Crown J, Martin M, Eiremann W, Pienkowski T, Bee V, Taupin H, Villalobos I, Lindsay M-A, Riva A, Hurvitz S, Glaspy J, Pauletti G, Sauter G, Press M. Cancer International Research Group (CIRG), Edmonton, AB, Canada Background: The use of anthracycline-based therapies for the adjuvant treatment of high-risk breast cancer has now become a common standard part of clinical practice. The evidence supporting this approach was initially controversial but ¿nally thought to be resolved when the Oxford overview demonstrated a 4-5 % survival advantage in favor of anthracycline-based therapies over those that did not contain an anthracycline. S6 Abstracts – General Sessions Materials and Methods: We performed a systematic review of published data from randomized, controlled adjuvant chemotherapy trials reporting HER2 subtype, i.e. HER2 positive vs. HER2 normal breast cancers. In addition, the analysis of two recent and separately conducted adjuvant trials of HER2 positive and HER2 normal breast cancers respectively, that were further sub-classi¿ed by whether or not they contained co-ampli¿cation of the topoisomerase II alpha (topo IIa) gene were included. Results: The published data demonstrate a remarkably consistent ¿nding. Speci¿cally, the incremental ef¿cacy bene¿t attributed to anthracyclinebased therapies is restricted to the HER2 positive subgroup. A recent analysis of the BCIRG 006 (HER2+) and 005 (HER2-) studies reveals that topo IIa ampli¿cation is con¿ned to cancers that contain the HER2 amplicon. In >1,600 HER2 FISH negative samples there is not a single topo IIa ampli¿ed case. Conversely, deletion of topo IIa was found in 5% of HER2+ and 3% of HER2– tumors respectively. An analysis of the impact of topo IIa co-ampli¿cation demonstrates that the improved ef¿cacy imparted by an anthracycline vs. a non anthracycline-based regimen is restricted to the HER2/topo IIa co-ampli¿ed cancers. These constitute 35% of the HER2+ cancers. In these cancers the ef¿cacy resulting from an anthracycline-based regimen alone was similar in magnitude to the addition of trastuzumab to adjuvant therapy. Conclusion: The use of anthracyclines in the adjuvant treatment of all breast cancer is not supported by the existing data. Given the known long-term cardiac and leukemogenic/MDS toxicities of anthracyclines and the lack of an incremental bene¿t in non HER2/topoIIa co-ampli¿ed cancers (which is ∼92% of the overall breast cancer population), other approaches to the adjuvant treatment of breast cancer should now be adopted. 14 Outcome of breast cancer therapies for adjuvant versus advanced disease: how much do they differ? Critical comments towards the present process of randomized trials as a pre-requisite for adjuvant therapy guidelines. Ragaz J, Spinelli JJ. McGill University Health Centre, Montreal, QC, Canada; British Columbia Cancer Agency, Vancouver, BC, Canada INTRODUCTION Thanks to technological advances, an accelerated rate of development of “targeted therapy” is seen – with advent of new drugs with curative potential for human cancer. Their development from early clinical trials into guidelines requires more swiftness, speed and ef¿ciency than seen presently. This study will review if results generated in stage IV (advanced, metastatic) breast cancer con¿rming with evidence level I and / or with statistical signi¿cance a) safety b) ef¿cacy c) superiority over placebo & standard therapy could be applicable to adjuvant setting, with a possibility of avoiding sizable number of breast cancer deaths much earlier than presently seen. OBJECTIVES AND METHODOLOGY Relative Risk rates (RR) or Hazard rates (HR) obtained from recent pivotal randomized studies, conducted ¿UVW in stage IV advanced disease, and WKHQ in the adjuvant setting, were compared, focusing on Aromatase Inhibitors (e.g. letrozole) versus Tamoxifen trials (AIs vs. TAM); and trastuzumab versus placebo (trastuz vs Plac) trials. Relative Risk rates (or HR) of classical stage IV outcomes (response rates, duration of response / median survival) were compared with the HR of disease free survival (DFS) in adjuvant setting. CONCLUSION This study con¿rms the constancy of RR rates between stage IV and adjuvant trials of Breast Cancer. Additional analogous observations will be discussed from the 1980’s trials involving Tamoxifen and or adjuvant CMF-based chemotherapy regimens, where documented responses / clinical bene¿t in stage IV disease led consistently to improve DFS and reduced mortality in adjuvant setting. These data con¿rm that if agents & regimens are documented to be safe and more effective than standard therapy LQVWDJH,9GLVHDVH, they will be effective LQDGMXYDQWVHWWLQJ with a great potential for affecting mortality. In those instances, placebo-control randomized adjuvant trials may not be indicated in majority of these instances. Instead, biomarker studies selecting optimum cohorts for new therapies, duration studies or other comparators not including placebo, ought to be considered. These recommendations, if adopted, will lead to a substantially more rapid materialization of signi¿cant survival gains, with great dollar cost and number of lives saved. RESULTS RR rates (HR - Hazard Rates) Stage IV (Reference) Adjuvant (Reference) Als (Letrozole) vs TAM: 0.70 Mouridsen JCO May 01 0.57 MA-17 NEJM Nov 03 0.82 BIG 1-98 JCO Feb 07 Trast. vs Plac: 0.58 Slamon NEJM 01 0.48 N9831 Ҝ B31 NEJM Oct 05 0.54 HERA NEJM Oct 05 0.42 FinHER NEJM Feb 06 0.48 BCIRG ASCO 06 21 Long-term results of a randomized trial of accelerated hypofractionated whole breast irradiation following breast conserving surgery in women with node negative breast cancer. Whelan T, Pignol JP, Julian J, Grimard L, Bowen J, Perera F, Schneider K, Fyles A, Gulavita S, Shelley W, Freeman C, Szechtman B, Levine M. Juravinski Cancer Centre, Hamilton, ON, Canada; McMaster University, Hamilton, ON, Canada; Toronto Sunnybrook Regional Cancer Centre, Toronto, ON, Canada; Ottawa Regional Cancer Centre, Ottawa, ON, Canada; Northeastern Ontario Regional Cancer Centre, Sudbury, ON, Canada; London Regional Cancer Centre, London, ON, Canada; Windsor Regional Cancer Centre, Windsor, ON, Canada; Princess Margaret Hospital, Toronto, ON, Canada; Northwestern Regional Cancer Centre, Thunder Bay, ON, Canada; Kingston Regional Cancer Centre, Kingston, ON, Canada; McGill University Health Centre, Montreal, QC, Canada BACKGROUND: Breast irradiation after lumpectomy is an integral component of breast conserving therapy. The optimal fractionation for whole breast irradiation is unknown. 50 Gy in 25 fractions in 5 weeks has been widely used but recently there has been renewed interest in hypofractionation due to potential radiobiological advantages, convenience and lower cost. However, long-term effects are a concern. The purpose of this study was to determine if an accelerated hypofractionated 3-week fractionation schedule was equally effective to a more traditional 5-week schedule of whole breast irradiation. METHODS: Women with invasive breast cancer treated by lumpectomy with pathologically clear resection margins and negative axillary nodes were randomly assigned to receive whole breast irradiation of 42.5 Gy in 16 fractions over 22 days (arm A) or 50 Gy in 25 fractions over 35 days (arm B). The primary outcome was local recurrence of invasive cancer in the treated breast. The secondary outcomes included disease free survival, overall survival, and radiation morbidity. RESULTS: From April 1993 through September 1996 1,234 women were randomly assigned to treatment (622 in arm A and 612 in arm B). Results previously reported (JNCI 2002; 94:1143-50) at a median follow-up of 69 months showed similar rates of local recurrence, disease free survival, overall survival and radiation morbidity. Long-term results of this trial with a median follow-up now of over 140 months will be updated for presentation. This will include both ef¿cacy and long-term radiation morbidity data. CONCLUSIONS: Initial results of trials of hypofractionation in early breast cancer have been quite promising, but there continues to be reluctance to adopt this approach until long-term results are available. Results of this study should have important implications for the use of hypofractionation in early breast cancer. Abstracts – General Sessions 22 dHER2 cancer immunotherapeutic: clinical response in breast cancer patients is associated with an induction of functional antibodies and the generation of speci¿c T cells. Limentani SA, Curigliano G, Campone M, Dorval T, Romieu G, Vogel C, White S, de Boer R, Lehmann F, Cormont F, Louahed J. Blumenthal Cancer Center, Charlotte; Ist. Eur. Oncol., Milan, Italy; Cent. R. Ganducheau, Nantes, France; Inst. Curie, Paris, France; CRLCC, Montpellier, France; Cancer Res. Network, Boca Raton; Austin Hosp., Heidelberg, Australia; Royal Melbourne Hosp., Parkville Vic., Australia; GSK Bio, Rixensart, Belgium Background We designed an Antigen-Speci¿c Cancer Immunotherapeutic ASCI to induce T cells able to recognize HER2 protein epitopes and a polyclonal antibody reponse Methods The dHER2 ASCI is a recombinant HER2 protein, including a truncated intra-cellular sequence ICD and the complete extracellular sequence ECD, combined with immunological adjuvant AS15 (GSK proprietary). Dose escalation from 20 to 500 µg of HER2 protein was evaluated in a Ph I study in adjuvant breast cancer setting. In another ongoing Ph II study in metastatic breast cancer patients, 500 µg dHER2 ASCI is given in the 1st or 2nd line metastatic setting, before or after Herceptin™ therapy. The immunization schedule comprised 2 cycles of q2w x 6, followed by 1 cycle of q3w x 6. Clinical and immunological evaluation was assessed after each immunization cycle. Results In both studies, dHER2 ASCI treatment was well tolerated, no symptomatic cardiotoxicity was recorded. In the Ph I study (61 patients) a dose response for antibody titer was observed, but poor maintenance of anti-ECD Ab titer associated with a lower IgG switch has been observed in about ½ of the patients. The dHER2 ASCI treatment induces speci¿c CD4+ and CD8+ T cells. Incubation of serum from 2 patients with breast cancer cell lines showed that the impact on molecular pathways resembled that of Herceptin™. In the metastatic trial, in contrast to the adjuvant trial, anti-ECD Ab responses demonstrated rapid IgG switch with sustained Ab-titer during immunization schedule. 1 complete clinical response (1st line setting) on skin lesions (3 cm) and 2 patients with stable diseases ≥ 6 months were recorded. Signs of minor clinical activity have also been recorded in other patients. Clinical activity is associated with high anti ECD antibody titers and T cell response magnitude. These titers are higher than these obtained in the adjuvant setting or non-responder patients, suggesting that overcoming immunotolerance may be key to achieve clinical ef¿cacy. In vitro, the anti ECD abs. of clinical responders bound HER2 overexpressing breast-cancer cell lines and were able to induce abdependent cellular cytotoxicity and growth inhibition of these cell lines. Preliminary assays show that speci¿c T cells were obtained in patients presenting clinical activity. Conclusions Overall, dHER2 ASCI treatment is well tolerated. In the metastatic setting, a complete response and 2 stabilizations of disease have been obtained. Clinical activity is associated with speci¿c T cell response and high anti ECD ab titer against HER2. In contrast to the adjuvant setting, the antibody response was maintained over time of immunizations with a rapid IgG switch. 23 Fulvestrant 500 mg vs 250 mg: ¿rst results from NEWEST, a randomized, phase II neoadjuvant trial in postmenopausal women with locally advanced, estrogen receptor-positive breast cancer. Kuter I, Hegg R, Singer CF, Badwe R, Lowe E, on Behalf of the NEWEST Investigators. Massachusetts General Hospital, Boston; University of Sao Paulo & Perola Bygton Hospital, Sao Paulo, Brazil; Medical University of Vienna, Vienna, Austria; Tata Memorial Hospital, Mumbai, India; AstraZeneca, Wilmington Background: The neoadjuvant setting represents a unique opportunity to assess the relationship between pharmacological dose/exposure, response, and effect on biomarkers in breast cancer therapy. Fulvestrant (Faslodex®) is an estrogen receptor (ER) antagonist licensed for the S7 treatment of postmenopausal women with advanced breast cancer progressing or recurring on an antiestrogen. Two studies have assessed the activity of fulvestrant in a presurgical setting, demonstrating a dosedependent downregulation of ER and the proliferation marker Ki67 with doses up to 250mg; however, clinical response was not assessed, nor was it established whether fulvestrant 250 mg is the optimal dose for use in the neoadjuvant setting. Methods: NEWEST (Neoadjuvant Endocrine Therapy for Women with Estrogen-Sensitive Tumors) is a randomized, open-label, multicenter, phase II study comparing fulvestrant at the approved dose (AD; 250 mg/month) and at a high dose (HD; 500 mg/month plus 500 mg on day 14 of month 1) as neoadjuvant therapy for postmenopausal women with newly diagnosed, ER-positive, locally advanced (T2,3,4b, N0-3, M0) breast cancer. No prior breast cancer treatment was permitted. Patients received treatment for 16 weeks immediately prior to de¿nitive surgery. Tumor biopsies were taken at baseline, week 4 and at surgery (week 16), and assessed for changes in ER, progesterone receptor (PgR), HER1, HER2 and Ki67 labeling index (LI), and for exploratory biomarker/gene array analysis. The primary objective was to compare the effect of fulvestrant AD and HD on Ki67 LI after 4 weeks of treatment. Secondary objectives included: assessment of tolerability; correlation between Ki67 LI changes and changes in ER and PgR expression; tumor response (assessed by ultrasound); correlation of response at 16 weeks to changes in biological endpoints (ER, PgR, HER1 and HER2) at weeks 4 and 16; and extent of breast surgery performed. Other secondary objectives included a comparison of the effects of fulvestrant AD and HD on endometrial thickness/uterine dimensions and serum bone markers. Results: A total of 212 women were recruited to this trial between February 9 2005 and January 22 2007. These patients were recruited from 36 centers across 6 different countries (Brazil, Austria, India, Germany, USA, and UK). The last patient is expected to complete this study on July 9 2007. Discussion: NEWEST is the ¿rst study to compare the fulvestrant AD and HD regimens in the neoadjuvant setting and to assess directly the relationship between fulvestrant dose, duration of treatment, magnitude of Ki67 LI and ER downregulation, and clinical activity of the drug. Activity and tolerability data from the NEWEST trial will be reported. 24 Anti-estrogens promote an invasive phenotype in intercellular adhesion de¿cient breast cancer cells. Borley AC, Barrett-Lee PJ, Gee JMW, Shaw VE, Nicholson RI, Hiscox SE. Velindre Cancer Centre, Cardiff, United Kingdom; Tenovus Centre for Cancer Research, Cardiff, United Kingdom Background: Anti-estrogens classically exert gene inhibitory effects during the drug responsive phase in estrogen receptor positive (ER+) breast cancer cells. Paradoxically, however, these drugs are also able to induce the expression of genes which, in the appropriate cell context, may contribute to an adverse cell phenotype. Here we have investigated the effects of anti-estrogen treatment on invasive signalling. Methods: The effect of estrogen (E2, 10-12 M), 4-hydroxy tamoxifen (TAM, 10-7M) or fulvestrant (FAS, 10-7M) on the invasive capacity of endocrine-sensitive MCF cells, in the presence or absence of functional E-cadherin, was determined by Matrigel invasion assays. Western Blotting using phospho-speci¿c antibodies was performed to ascertain changes in invasive signalling whilst Affymetrix microarray analysis with PCR veri¿cation was used to explore gene changes in response to anti-estrogen versus E2 treatment. Results: TAM or FAS alone did not signi¿cantly alter MCF-7 cell invasion versus E2 treatment. Disruption of intercellular adhesion promoted a modest increase in invasive capacity, which was reduced by inclusion of E2 (p<0.05); in contrast to this, both TAM and FAS promoted a striking increase in cell invasion in the absence of intercellular adhesions (p<0.02), with an accompanying increase in Src kinase activity. Subsequently, anti-estrogen-induced cellular invasion in these cells was reduced by inclusion of the Src kinase inhibitor SU6656 (1µM; p<0.05). Affymetrix analysis and subsequent PCR validation revealed that TAM and FAS induced the expression of several genes (RhoE, δ-catenin, LYN, PAK2) which have been linked to invasive behaviour and whose protein products may be regulated by Src kinase. S8 Abstracts – General Sessions Discussion: These data demonstrate that anti-estrogens can promote an invasive phenotype in ER+ breast cancer cells under conditions of poor cell-cell contact and suggest a role for Src kinase and associated pro-invasive genes in this process. This invasion-promoting ability of anti-estrogens may have major clinical implications for those patients whose tumours display inherently poor intercellular adhesion. In such cases, combination treatment with anti-Src agents may prove therapeutically valuable. 25 The VEGF-R inhibitor PTK787/ZK222584 (PTK/ZK) also inhibits aromatase: preclinical studies of PTK/ZK in combination with endocrine therapy. Banerjee SN, Thornhill A, Evans DB, Littlewood-Evans AJ, Dowsett M, Martin L-A. Institute of Cancer Research, London, United Kingdom; Novartis Institute for BioMedical Research-Basel, Basel, Switzerland Background: Angiogenesis and Vascular Endothelial Growth Factor (VEGF) are key components of breast cancer growth, invasion and metastasis. Clinical studies provide support for targeting VEGF in breast cancer. Estrogen Receptor (ER) and VEGF signalling pathways may be linked and increased VEGF levels have been associated with endocrine-resistance. Targeting both signalling pathways concomitantly may provide enhanced therapeutic bene¿t. We report the ¿rst studies of the oral, VEGF-R tyrosine kinase inhibitor, PTK/ZK, in in-vitro and in-vivo models of endocrine-resistant and -sensitive disease. Methods: The effects of PTK/ZK and endocrine therapy were investigated in human breast cancer cell lines engineered to express aromatase: MCF7-AROM1 (ER+HER2-; endocrine-sensitive) and BT474-AROM3 (ER+, HER2++; endocrine-resistant). The effect of PTK/ZK ± tamoxifen or letrozole was assessed in proliferation and ER alpha-mediated transcription assays. The effect of PTK/ZK on aromatase activity was measured in the tritiated water assay. Xenograft studies with MCF7-AROM1 cells were carried out to compare the effect of escalating doses of PTK/ZK on tumor growth over 28 days. Dynamic changes in the tumor neovasculature were monitored by confocal microscopy using lectin perfusion and CD31 staining. Results: Escalating doses of both E2 and androstenedione (AND) induced a proliferative response and increased ER-mediated transcription which were inhibited by 4OH-T or LET in both MCF7-AROM1 and BT474AROM3 cells in vitro. PTK/ZK alone and in the presence of E2 had no effect on proliferation or ER/ERE-mediated transcription. However, in the presence of AND, PTK/ZK suppressed both AND-stimulated proliferation and ER-transactivation in a concentration-dependent manner suggesting PTK/ZK has angiogenic-independent effects. Combinations of PTK/ZK with 4OH-T or LET enhanced the antiproliferative and ER-mediated transcriptional effects of these agents. Further analysis using tritiated water assays showed PTK/ZK possessed unexpected anti-aromatase activity. Early data from MCF7-AROM1 xenografts showed that PTK/ZK (50mg/kg) reduced tumor volumes together with an associated decrease in tumor vasculature assessed by lectin perfusion and concomitant CD31 staining. Conclusion: PTK/ZK has novel anti-aromatase activity in addition to its anti-angiogenic effects. Since this represents a previously unknown action and potential facet of its clinical activity, studies are ongoing to assess the degree to which the anti-aromatase activity of PTK/ZK may contribute to its anti-tumor activity. 26 Bone mineral density (BMD) at 5 years after diagnosis in premenopausal patients with endocrine-responsive breast cancer, after 3 years of adjuvant endocrine treatment with goserelin and tamoxifen or anastrozole or both treatments in combination with zoledronic acid – new results from ABCSG-12. Gnant M, Mlineritsch B, Luschin-Ebengreuth G, Kainberger F, Kaessmann H, Piswanger-Soelkner C, Seifert M, Schippinger W, Menzel C, Dubsky P, Fitzal F, Steger G, Greil R, Marth C, Kubista E, Samonigg H, Jakesz R, on Behalf of the ABCSG. Austrian Breast and Colorectal Cancer Study Group, Vienna, Austria Background: Cancer treatment-induced bone loss (CTIBL) is now generally accepted as a major side effect of modern endocrine therapies. Long-term adjuvant ovarian function suppression plus tamoxifen or aromatase inhibitors in premenopausal patients with endocrineresponsive breast cancer can lead to signi¿cant CTIBL (Gnant et al, JCO 2007; 25: 820-8). This randomized study investigates the use of the bisphosphonate zoledronic acid (ZA) in order to prevent CTIBL and reports on late BMD results 2 years after completion of adjuvant treatment. Patients and Methods: ABCSG-12 is a randomized, open-label, phase III, four-arm trial comparing tamoxifen (20 mg/d orally) and goserelin (3.6 mg every 28 days subcutaneously) ± zoledronic acid (4 mg intravenously every 6 months) versus anastrozole (1 mg/d orally) and goserelin ± zoledronic acid for 3 years in premenopausal women with endocrine-responsive breast cancer. In a BMD subprotocol, patients underwent serial BMD measurements at 0, 6, 12, 24, 36, and 60 months. Results: Of 1,801 patients in the trial, 404 were prospectively included in a bone substudy using standardized quality-controlled DEXA at prede¿ned time points. 201 patients received adjuvant ZA together with their endocrine treatment whereas 203 patients did not. Median patient age at diagnosis was 44 years. After 3 years of treatment, patients who did not receive ZA showed a BMD loss of 11.3 per cent as compared to baseline (p<0.0001). CTIBL was more pronounced if anastrozole was used in combination with goserelin as compared to tamoxifen (-13.6% vs. -9%). At 60 months of follow-up, i.e. two years after the completion of treatment, patients without ZA still showed impaired BMD as compared to baseline (-6.8%, p=0.0005). In contrast, patients who received ZA showed unchanged BMD at 36 months (+.3%, p=0.85) and increased BMD at 60 months (+3.9%, p=0.02). Discussion: Adjuvant endocrine therapy using goserelin plus tamoxifen or anastrozole for three years causes signi¿cant CTIBL in premenopausal women with breast cancer. While there is some recovery after completion of treatment, patients show still compromised BMD after 5 years, particularly those who received goserelin plus anastrozole. Zoledronic acid 4 mg every 6 months for three years completely inhibits CTIBL, and leads to improved BMD at 5 years. 27 The effect of zoledronic acid on aromatase inhibitorassociated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: the Z-FAST study 36-month follow-up. Brufsky A, Bosserman L, Caradonna R, Haley B, Jones M, Moore H, Dong M, Warsi G, Lacerna L, Perez E. Z-FAST Study Group; Novartis Pharmaceuticals, East Hanover, NJ Background: Aromatase inhibitor (AI) therapy effectively increases disease-free survival in postmenopausal women (PMW) with ER+ and/ or PR+ BCa. However, the use of AIs in this patient population results in nearly complete ablation of estrogen production which can lead to accelerated bone loss and increased fracture risk. The Z-FAST study evaluates the ef¿cacy and safety of Zoledronic acid (ZA) in preventing AI associated bone loss in PMW with early breast cancer (EBC) who are receiving adjuvant Letrozole (LET) therapy. Material and Methods: 602 PMW with stage I-IIIa ER+ and/or PR+ BCa starting LET (2.5 mg qd x 5 yrs) were randomized to upfront ZA (4 mg IV q 6 mos) vs delayed ZA in 94 centers in the US and Canada. The delayed group receives ZA when either the post-baseline Abstracts – General Sessions T-score decreases to <-2 or a clinical fracture occurs. All patients (pts) are treated with calcium and vitamin D. The primary endpoint, the percent change in lumbar spine (LS) bone mineral density (BMD) at 12 mos, was reported at ASCO 2005. The results of 36 mos follow-up are reported here. Results: Baseline characteristics were similar between groups. At 36 mos, the upfront ZA group (n=189) showed a mean increase of 3.72% in LS BMD while the delayed group (n=188) showed a mean decrease of 2.95%, resulting in an absolute difference of 6.7% (p<0.001). The upfront group (n=189) showed a mean increase of 1.66% in total hip (TH) BMD while the delayed group (n=187) showed a mean decrease of 3.51%, resulting in an absolute difference of 5.2% (p<0.001). The overall difference in LS and TH BMD between the two groups was 8.2% and 6.7%, respectively, when BMD data in the delayed group was excluded after pts started ZA. Among pts with baseline T score between -1 and -2, 40.4% of upfront pts (7.6% of delayed pts) returned to normal T score (T score >-1) and 13.4% of delayed pts (2.1% of upfront pts) became severely osteopenic (T <-2). 15% of delayed pts had a decrease in BMD that required initiation of ZA. Fractures occurred in 5.6% of upfront pts and 6.3% of delayed pts. 199 upfront pts and 191 delayed pts had baseline and 36 mos spinal x-rays. 0.5% upfront pts and 0.52% delayed pts had a radiological fracture detected at 36 mos. The study was not designed to detect a signi¿cant difference in the fracture rate between treatment arms. Administration of ZA q 6 mos for up to 36 mos was safe and well tolerated. No serious renal adverse events and no con¿rmed osteonecrosis of the jaw cases were reported. Disease recurrence was reported in 9 (3.0%) pts in the upfront group, and 14 (4.7%) pts in the delayed group (p=0.24). Discussion: The 36 mos follow-up of the Z-FAST trial show that the overall difference in the percentage change in BMD between the upfront and delayed ZA treatment groups, at both LS and TH, progressively increased from baseline through 36 mos. These data demonstrate that ZA 4mg IV q 6 mos is effective in preventing bone loss associated with adjuvant AI therapy in PMW with EBC. 28 Effect of anastrozole on bone mineral density after one year of treatment: results from bone sub-study of the International Breast Cancer Intervention Study (IBIS-II). Singh S, Cuzick J, Edwards R, Blake G, Truscott J, Coleman R, Eastell R, Howell A. Wolfson Institute of Preventive Medicine, London; Kings College School of Medicine, London; University of Leeds, United Kingdom; University of Newcastle, Australia; Christie Hospital, Manchester, United Kingdom; Northern General Hospital, Shef¿eld, United Kingdom Background: The third generation aromatase inhibitors have been shown to reduce bone mineral density when compared with tamoxifen in the advanced, adjuvant and neoadjuvant settings in women with early breast cancer. No trial to date has compared the effect of anastrozole treatment versus placebo on bone mineral density in the prevention setting. Materials and Methods: The bone sub-protocol of IBIS-II assessed changes in the bone mineral density in postmenopausal women aged 40-70 years with a high risk of breast cancer receiving anastrozole 1 mg/day versus placebo for 5 years. Out of 1540 women recruited to date in the prevention study, 613 women have taken part in the bone sub-protocol of the study. Lumbar spine and femoral neck BMD have been assessed at baseline and 1 year by DXA scans for 250 women at the time of analysis. Results are expressed as mean percentage change. Out of 250 women, 162 with normal BMD joined stratum-I of the study and received only monitoring without bisphosphonate treatment, 59 osteopenic women joined stratum-II and were further randomised to receive either risedronate or placebo, 29 osteoporotic women joined stratum-III of the study and all received treatment with risedronate. Results: In stratum-I, a greater BMD loss was observed in the anastrozole vs placebo group at both the lumbar spine (-2.5% vs. 0.97%; P= .002), and total hip (-1.34 vs. -0.37%; P= .02). In stratum-II, women randomised to risedronate had higher BMD scores both in the anastrozole and in the placebo arm. The BMD changes were (risedronate vs. non-risedronate group; Spine 0.32% vs. -0.17%, P=0.75, Hip 0.67% vs. -2.27%, P= .01) in the anastrozole arm, and (Spine 0.84% vs. S9 -0.25%, P=.36; Hip -0.35% vs. -1.2%, P=.23) in the placebo arm. In stratum-III, the BMD changes observed were (Spine 1.8% vs. 4.17%, P= .03; Hip -0.13% vs. 1.5%, P=.06) in the anastrozole and placebo group, respectively. Discussion: Women with normal BMD at baseline had a signi¿cant BMD loss with anastrozole treatment. However, women on anastrozole, who joined the trial with an osteopenic or osteoporotic T-score, gained BMD after receiving risedronate treatment for a year. This data con¿rms the BMD losses observed with third generation AIs on breast cancer patients, but it is also reassuring that BMD loss can be controlled if women receive DXA scans at baseline and bisphosphonate treatment as needed along with AIs. Longer-term follow-up and analysis on more BMD data is required to con¿rm the above results. These data will be further updated at the time of meeting. 29 Risk stratification based on the CYP2D6 tamoxifen metabolizing gene within the Italian tamoxifen prevention trial. Bonanni B, Maisonneuve P, Johansson H, Macis D, Serrano D, Guerrieri-Gonzaga A, Basso D, Zambon C, Plebani M, Nicoloff M, Fontecha M, Hillman G, Wieczorek L, Rotmensz N, Decensi A. European Institute of Oncology (EIO); EIO, Milan, Italy; University-Hospital of Padova, Padova, Italy; Roche Molecular Diagnostics, Pleasanton, CA; E.O. Ospedali Galliera, Genova, Italy Background: Plasma levels of the active tamoxifen (TAM) metabolites are associated with the cytochrome CYP2D6 genotype. We recently published results (JCO 24:3708-9, 2006) indicating that women with the CYP2D6*4/*4 genotype had a reduced likelihood to bene¿t from TAM as a chemopreventive agent for breast cancer (BC) using real-time TaqMan CYP2D6*4 Allelic Discrimination Assay (Applied Biosystems). These ¿ndings warranted an expanded genotyping study to gain a deeper understanding of the role of CYP2D6 variation in predicting response to TAM. Objectives: The aim of this research was to screen participants in the case-control study of the Italian TAM Prevention Trial for additional CYP2D6 polymorphisms. We used the AmpliChip® CYP450 Test (Roche Molecular Diagnostics) to investigate whether Poor and Intermediate Metabolizers (PM, IM) receiving TAM are less likely to bene¿t from treatment and how Ultra-rapid Metabolizers (UM) respond to TAM treatment. Methods: The study included 182 subjects (135 controls and 47 BC cases). The AmpliChip® CYP450 Test queries 32 CYP2D6 alleles and classi¿es subjects into 4 phenotypes: PM (no activity), IM (reduced activity), Extensive Metabolizers (EM, normal activity) and UM (excess activity). Results: The clinical effect of CYP2D6 phenotype (poor vs other metabolizers) on BC risk was con¿rmed. Among women in the tamoxifen arm, PM had higher risk of BC (p=0.035) (Table 1). We found no correlation between IM and BC risk. In addition, 3 UMs were identi¿ed in the placebo arm. Interestingly, having at least one CYP2D6*2A allele was strongly associated with lower risk for BC (p=0.0008) in the TAM arm. Of the women with a CYP2D6*2A allele (n=58), 10 developed BC (9 placebo, 1 TAM). This statistically signi¿cant effect was not seen with other functioning alleles (CYP2D6*1, CYP2D6*35), nor those with reduced activity (CYP2D6*9, *10, *41) or null alleles (CYP2D6*3, *4, *5, *6, *7). Conclusions: Our results con¿rm the utility of CYP2D6 genotyping in predicting response to TAM as a chemopreventive agent. PMs are less likely to bene¿t from TAM. In addition, we report a novel ¿nding that women on TAM carrying a CYP2D6*2A allele appear more likely to bene¿t from treatment, although these data need to be independently con¿rmed. These ¿ndings provide new perspectives on the clinical application of pharmacogenetics in tailoring patient care in oncology. Table 1: CYP2D6 Predicted Phenotype in the Tamoxifen Arm Phenotype Total Control Breast cancer P-value TOTAL 85 65 20 (23.5%) UM EM 73 59 14 (19.2%) IM 7 5 2 (28.6%) PM 4 1 3 (75.0%) P=0.035 (poor vs other metabolizers) NO CALL 1 1 S10 Abstracts – General Sessions 31 Genomic approaches to breast cancer subset identi¿cation and treatment. Albertson D, Chin K, Devries S, Feiler H, Pinkel D, Spellman P, Waldman F, Wang N, Hennessy B, Mills G, Barcellos Hoff MH, Bissell M, Guan Y, Hu Z, Kuo W-L, McCormick F, Neve R, Stampfer M, Wooster R, Yaswen P, Das D, Fridlyand J, Correll E, Jin J, Nordmeyer B, Sudar D, Chew K, Dairkee S, Ljung BM, Hwang S, Esserman L, Arbushites M, Benz C, Koehler M, Marks JD, Zhou Y, Park J, Weber B, Gray J. University of California, San Francisco, CA; Lawrence Berkeley National Laboratory, Berkeley, CA; MD Anderson Cancer Center, Houston, TX; GlaxoSmithKline, King of Prussia, PA; California Paci¿c Medical Center, San Francisco, CA; Buck Institute for Age Research, Novato, CA; Genentech, South San Francisco, CA Genome-wide analyses of the epigenome, genome and transcriptome in human breast cancers have revealed a wide range of molecular defects that likely contribute to cancer pathophysiology. Moreover, these analyses have revealed subsets of breast cancers carrying speci¿c recurrent aberration signatures that progress and respond differently to speci¿c therapies. Two of these subtypes – designated as basal and luminal/ampli¿er – often do not respond well to current chemotherapy and tend to recur or progress so that new treatment strategies are needed. Hundreds of candidate therapeutic agents are under development in academia and industry that can be considered for subtype speci¿c therapy. We have developed an in vitro system comprised of 50 wellcharacterized breast cancer cell lines that we are using to identify therapeutics that will be effective against the basal and luminal/ampli¿er breast cancer subtypes, develop assays that will predict individual responses within subtypes and identify mechanisms of response that may guide selection of complementary therapeutic agents. We have applied this approach to assess responses to 26 approved or experimental anticancer drugs. Drug induced changes in viable cell number were assessed for each cell line at 9 different drug concentrations and each analysis was performed in triplicates. Three general results emerge from these studies. (a) Many approved and experimental drugs show strong breast cancer subtype speci¿city. (b) Correlative analyses of associations between biological response and pretreatment molecular features yield multivariate predictors of individual response. The magnitude of biological response varies considerably between drugs and predictors of individual response are most accurate for drugs showing high variability of response between cell lines. (c) Drugs designed to target speci¿c genomic defects are most effective in cell lines with those defects thereby validating the overall correlative approach. For example, Lapatinib and Herceptin are most effective against tumors over expressing ERBB2. An assessment of the utility of markers developed using the in vitro cell line collection that predict cell line responses to Lapatinib to predict results in the EGF30001 trial of Paclitaxel-placebo vs Paclitaxel-Lapatinib will be presented. 32 Genome-wide analysis of DNA copy number alterations in conjunction with gene expression pro¿ling identi¿es DNA ampli¿cation loci that predict distant recurrence in lymph node-negative (LNN) primary breast cancer patients. Zhang Y, Klijn J, Yu J, Jiang J, Jatkoe T, Sieuwerts A, Martens J, Wang Y, Foekens J. Johnson & Johnson, San Diego, CA; Erasmus MC, Rotterdam, Netherlands Background: In our previous gene expression study of lymph nodenegative (LNN) breast cancer patients, we have identi¿ed a 76-gene signature that stratifies patients to provide better means of risk assessment on an individual basis for breast cancer patients (The Lancet 365:671-679, 2005). The aim of this study was to identify DNA copy number alterations from the same cohort of patients to provide alternative/complementary means for risk assessment of recurrence. Material and Methods: The genomic DNA of frozen tumor tissue specimens from 314 LNN breast cancer patients samples was extracted and hybridized using Affymetrix GeneChips@ Human Mapping 100K Array Set. All the patient samples were collected between 1980-1995 and none of the patients received systemic adjuvant endocrine- or chemotherapy. The mean age is 54 years old and the median follow-up is 102 months. 199 patients are ER positive and 114 patients had distant recurrences. The DNA copy numbers of the genes were determined using Affymetrix CNAT software. We analyzed the DNA copy numbers and the gene expression levels of the samples to identify genomic loci that showed high correlation to distant recurrence in LNN breast cancer. The patients were randomly divided into a 200-patient training set and 114-patient testing set. The candidate loci were identi¿ed from the training set and validated on the testing set. First, the loci where the DNA copy number alterations correlated with patient’s prognosis were identi¿ed by the Cox proportional hazards regression. Then these alterations at the DNA level were con¿rmed using the concordant changes in gene expression regulation on the mRNA level. Results: From the training set, we identi¿ed a panel of 6 genomic loci that showed high DNA ampli¿cation in patients who developed distant recurrence, and these gene ampli¿cations were supported by the concordant up-regulation of these genes at the mRNA level. When tested on the independent 114 patients of the testing set, the genomic ampli¿cations of these loci identi¿ed a subset of breast cancer patients that had high probability of recurrences (hazard ratio of 3.2, C.I. 1.56.9, P=0.002). Discussion: Our study highlights the feasibility of identifying prognostic markers on the genomic DNA level. The clinical implication for such prognostic assays is to signi¿cantly reduce the number of patients that receive unnecessary treatment. Our result suggests that DNA copy number alterations, together with gene expression pro¿les, provide a strategy to combine several molecular markers and build mathematical models of risk assessment. 33 Gene expression pro¿les of ER+/PR-breast cancer are associated with genomic instability and Akt/mTOR signaling, and predict poor patient outcome better than clinically assigned PR status. Creighton CJ, Osborne CK, van de Vijver M, Foekens JA, Wang Y, Zhang Y, Klijn JGM, Horlings HM, Hilsenbeck SG, Lee AV, Schiff R. Baylor College of Medicine, Houston, TX; Netherlands Cancer Institute, Amsterdam, Netherlands; Erasmus MC-Daniel den Hoed, Rotterdam, Netherlands; Veridex LLC, a Johnson & Johnson Company, San Diego, CA Background: Patient prognosis and response to endocrine therapy in breast cancer correlate with protein expression of both estrogen receptor (ER) and progesterone receptor (PR), with poorer outcome in patients with ER+/PR- compared to ER+/PR+ tumors. Materials and Methods: To better understand the underlying biology of ER+/PR- tumors, we examined RNA expression (n>1000 tumors) and DNA copy number pro¿les (n= total 89 tumors) from ¿ve previously published studies of human breast cancers with clinically assigned hormone receptor status (ER+/PR+, ER+/PR-, and ER-/PR-). Results: We identi¿ed an expression “signature” of genes with either elevated or diminished RNA levels speci¿cally in ER+/PR+ compared to ER-/PR- and most ER+/PR- tumors. We similarly identi¿ed a gene signature speci¿c to ER-/PR- tumors. ER+/PR- tumors, on the other hand, were a mixture of three different subtypes: tumors manifesting the ER+/PR+ signature, tumors manifesting the ER-/PR- signature, and tumors not associating entirely with ER+/PR+ nor with ER-/PRtumors but sharing patterns with both. Tumors in this third group were considered to be distinctive ER+/PR- tumors at the transcriptome level and showed gene expression patterns that were intermediate between ER+/PR+ and ER-/PR-; these ER+/PR- tumors shared similarities with ER+/PR+ tumors, in that they did not manifest the signature speci¿c to ER-/PR- tumors, and with ER-/PR- tumors, in that they did not manifest the ER+/PR+ signature. In analyses of patients treated with tamoxifen (263 patients in the dataset from Loi et al.) and of those who received no adjuvant therapy (155 patients in the dataset from van de Vijver et al.), ER+/PR- breast cancers de¿ned by gene expression pro¿ling (i.e. tumors neither truly ER+/PR+ nor ER-/PR- but sharing expression patterns with both) tended to have poor outcome as compared to those with pure ER+/PR+ or ER-/PR- patterns (Loi P=0.02, van de Vijver P=0.0006, log-rank statistic); these differences were not observed when using the LBA and IHC clinical assays to assign ER and PR status (P>0.1). ER+/PR- tumors showed approximately twice as much DNA Abstracts – General Sessions copy gain or loss compared to ER+/PR+ and ER-/PR- tumors (78 with fold change >1.5 compared to 32 for ER+/PR+, and 38 for ER-/PR-, based on analysis of 89 CGH pro¿les consisting of 2149 DNA probes). Targets of transcriptional up-regulation by speci¿c oncogenic pathways, including PI3K/Akt/mTOR, were enriched in both ER+/PR- and ER/PR- compared to ER+/PR+ tumors. Discussion: Gene expression pro¿les may provide a better assay over current clinical methods for inferring PR status for diagnostic and therapeutic purposes. 34 Expression of alphavbeta6 supersedes Her2 and triplenegative/basal classi¿cation of breast cancer and de¿nes novel subgroups with poor survival: implications for breast cancer classi¿cation and treatment. Jones JL, Thomas GJ, Duffy SW, Chou P, Gabe R, Ellis I, Green A, Saha A, Mulligan KT, Ryder K, Gillet C, Violette S, Weinreb P, Hart IR, Marshall JF. Bart’s and the London, Queen Mary’s School of Medicine and Dentistry, London, United Kingdom; Nottingham City Hospital, Nottingham, United Kingdom; Guy’s Hospital, London, United Kingdom; Biogen Idec, Cambridge, MA Background: Molecular characterization permits a more functional classi¿cation of breast cancer. The epithelial-speci¿c integrin alphavbeta6 shows negligible expression on normal tissues but may be upregulated by many types of carcinoma. This study examined the functional and prognostic importance of expression of this integrin in breast cancer. Method: Involvement of alphavbeta6 expression in breast cancer cell invasion in vitro was assessed and alphavbeta6 levels were analyzed in 1800 breast cancers relative to conventional prognostic indices, molecular subtypes and survival. Results: alphavbeta6 contributed signi¿cantly to the invasive behavior of breast cancer cell lines and, in patient samples, was associated with high tumor grade, negative ER and PR status, and distant metastasis (p<0.001). Strong alphavbeta6 expression superseded ER negative tumor categorization into triple-negative/basal or Her2 -positive subgroups as a predictor of reduced survival, even when adjusted for tumor grade, size and lymph node status [HR 1.70; CI 1.19-2.44]. Thus alphavbeta6 expression correlated with both the triple-negative/basal subtype (p=<0.007) and Her2-positive status (p<0.001) but was of greater prognostic importance than either, de¿ning poor prognosis subsets within these groups. In Cox proportional hazards regression analysis alphavbeta6 was associated with a signi¿cant reduction in survival (10 year survival for Her2+ve/alphavbeta6+ve cases 34% vs Her2+ve/alphavbeta6-ve (52%) or Her2-ve/alphavbeta6-ve (79%) subgroups; p=0.006). Conclusions: alphavbeta6, possibly through promotion of cancer cell invasion, identi¿es a novel sub-group of poor prognosis breast cancers. We suggest that determining alphavbeta6 expression should precede classi¿cation into Her2-positive and triple-negative/basal subtypes. Such an algorithm identi¿es alphavbeta6 as a promising new target in aggressive breast disease. S11 35 A stroma-related gene signature predicts resistance to epirubicin-containing neoadjuvant chemotherapy in breast cancer. Farmer P, Bonnefoi H, Anderle P, Cameron D, Wirapati P, Becette V, André S, Piccart M, Campone M, Tubiana-Hulin M, MacGrogan G, Petit T, Jassem J, Rouanet P, Blot E, Bogaerts J, Bergh J, Iggo R, Delorenzi M. National Centre of Competence in Research (NCCR) Molecular Oncology, Swiss Institute for Experimental Cancer Research (ISREC), Epalinges, Switzerland; Swiss Institute of Bioinformatics (SIB), Lausanne, Switzerland; European Organisation for Research and Treatment of Cancer (EORTC), Breast Cancer Group, Brussels, Belgium; The Swiss Group for Clinical Cancer Research (SAKK), Bern, Switzerland; The Anglo-Celtic Cooperative Oncology Group (ACCOG), Edinburgh University, Edinburgh, United Kingdom; The Swedish Breast Cancer Group (SweBCG), Karolinska Institute, Stockholm, Sweden Background: Biological markers predicting sensitivity of breast tumours to speci¿c chemotherapies would allow selection of the optimal therapy for individual patients. The goal of this study was to identify a gene expression signature predicting for a pathological complete response to neo-adjuvant Àuorouracil, epirubicin and cyclophosphamide (FEC) therapy in patients with large operable breast cancer. Material and Methods: A total of 63 samples from ER negative tumors enrolled in EORTC 10994/BIG 00-01 study (28 pCR) were hybridized to Affymetrix X3P arrays. Results: Using linear models to ¿nd groups of genes highly correlated to a speci¿c biological process, we found that activated stroma was significantly associated with resistance to FEC treatment (AUC 0.70; p < 0.01). In a multivariate analysis that included pre-treatment classic- clinico-pathological variables (clinical size & node status, grade and ERBB2), the stroma signature was the only covariate that remained signi¿cant. Using data from an independent experiment for which epithelial and stromal tumor tissues were separated with laser dissection microscopy prior hybridization on microarrays, we could show that genes included in this signature are speci¿cally expressed in the reactive-stroma. The association of stroma with resistance to chemotherapy was validated in an external cohort of 53 ER negative patients treated with T-FAC (Hess et al. J. Clin. Oncol. 2006): AUC 0.70 [0.52-0.85] (CI 95%), odds ratio 3.41, p < 0.05. A Gene Set Enrichment Analysis showed a signi¿cant association for both Wnt and TGFβ targets genes and the stroma expression module. Discussion: These ¿ndings identify a novel resistance mechanism of ER negative breast carcinoma to FEC treatment which is stroma activation. 36 The clinical signi¿cance of polysomy 17 in the HER2+ N9831 intergroup adjuvant trastuzumab trial. Reinholz MM, Jenkins RB, Hillman D, Lingle WL, Davidson N, Martino S, Kaufman P, Kutteh L, Perez EA. Mayo Clinic College of Medicine, Rochester, MN; John Hopkins, Baltimore, MD; The Angeles Clinic and Research Institute, Santa Monica, CA; Dartmouth Hitchcock Medical Center, Lebanon, NH; Oncology Associates of Cedar Rapids, Cedar Rapids, IA; Mayo Clinic College of Medicine, Jacksonville, FL Background: Recent preliminary ¿ndings suggest an association between chromosome 17 number anomalies and trastuzumab bene¿t in metastatic breast cancer patients. Purpose: The objective of this study is to determine the correlation between HER2 gene copy and chromosome 17 number anomalies with outcome (disease free survival-DFS) of patients treated with or without trastuzumab. Patients/Methods: This analysis included 1888 patients from the HER2+ N9831 intergroup adjuvant trastuzumab phase III clinical trial who were not or concurrently treated with trastuzumab. Disease free survival was the primary endpoint of the study. Fluorescent in situ hybridization (FISH) was centrally performed in the Mayo Clinic Clinical Cytogenesis Laboratory using a dual probe mixture for HER2 (17q11.2-12/ centromere 17) from Vysis (Downers Grove, IL). Sixty non-overlapping interphase nuclei were counted using an Axioplan-2 microscope (Zeiss) with a triple-pass ¿lter. Results: Interestingly, patients who did not receive trastuzumab and had p17 had a 34% lower DFS rate (p = 0.04) than the non-trastuzumab-treated patients S12 Abstracts – General Sessions who had n17. Patients whose tumors were ampli¿ed with polysomy 17 (p17) and with normal 17 number (n17) and treated with trastuzumab had improved DFS with hazard ratios of 0.52 (p = 0.006) and 0.37 (p = 0.0004), respectively. We had an insuf¿cient number of events to address the ef¿cacy of trastuzumab in patients with monosomy 17 (m17), small clone ampli¿cation or duplication FISH results (see Table and Figure). Conclusions: Patients treated only with standard chemotherapy and who had p17 bene¿ted more than those who had n17, whereas both groups of p17 and n17 patients bene¿ted from trastuzumab as compared to standard therapy with similar 3 and 5 year DFS rates. These results suggest that chromosome 17 number status is not predictive of trastuzumab response. with progression or survival: only 7 of 16 studies showed signi¿cant associations, but follow-up was short. Of 11 sestamibi imaging studies, 10 showed a signi¿cant association between shorter retention and higher levels of MDR1/gp170, suggesting active protein pumping of contrast agent. For the ¿rst time, a large number of studies (11) of multidrug reversing agents could be reviewed. None of these agents produced even a partial clinical response in >25% of previously refractory patients. However, studies included patients who did not express MDR1/gp170, who would not be expected to respond to reversing agents. Conclusion. This meta-analysis includes nearly 3 times as many studies as our 1997 analysis. MDR1 is expressed in approximately half of breast cancer patients, and is induced by chemotherapy. 56% of patients who express MDR1 after chemotherapy fail to achieve a clinical response. Sestamibi gives the strongest support that MDR1/gp170 is associated with active efÀux of agent from cells. Further follow-up is needed to determine the impact on survival, and multidrug reversing agents must be tested in more rigorously designed studies. Given the major role of anthracyclines and taxanes in breast cancer therapy, the MDR1 pathway may be an important contributor to modern chemotherapy resistance. 41 ATAC: 100 month median follow-up (FU) shows continued superior ef¿cacy and no excess fracture risk for anastrozole (A) compared with tamoxifen (T) after treatment completion. 37 Multidrug resistance and breast cancer: a meta-analysis of MDR1 and its clinical signi¿cance. Trock B, Leonessa F, Clarke R. Johns Hopkins, Baltimore, MD; Uniformed Services University of Health Sciences, Bethesda, MD; Georgetown University, Washington, DC Background. The clinical signi¿cance of MDR1/gp170 as a mechanism of multidrug resistance in breast cancer has not been established, despite the 2 leading classes of breast cancer drugs, anthracyclines and taxanes, both being substrates for this gene. Ten years ago we published a meta-analysis examining MDR1/gp170 in breast cancer, based on a relatively small number of studies with clinical endpoints, and prior to widespread use of taxanes. We now report an updated meta-analysis with signi¿cantly more clinical data. Methods. Published papers on MDR1/gp170 and breast cancer were identi¿ed by searching literature databases and bibliographies of published papers. Standard methods for pooling data in meta-analysis were applied. Results. 84 studies with >2000 patients were included in analysis: 63 measured MDR1/gp170 expression, 21 measured response to chemotherapy, 11 measured sestamibi efflux, and 11 evaluated multidrug resistance reversing agents. MDR1/gp170 expression was induced by chemotherapy: it was detected in 46% of breast tumors prior to treatment vs. 67% after treatment (p<0.0001). gp170 expression did not differ by antibody type (p=0.57). Failure to respond to chemotherapy with MDR1 substrates, such as anthracyclines or taxanes, was nearly three times as frequent when tumors measured after chemotherapy were positive for MDR1: 56% (128/228) vs patients with negative tumors: 18% (32/176), p<0.0001. When weighted by study variance, the pooled relative risk of nonresponse was 1.9 (95% CI 1.5-2.5). However, if MDR1 was measured prior to induction by chemotherapy it was no longer signi¿cantly associated with response, p=0.27. There was no clear association Forbes JF, Cuzick J, Buzdar A, Howell A, Baum M, on Behalf of the ATAC Trialists’ Group. University of Newcastle, Calgary Mater Hospital, NSW, Australia; Cancer Research UK, United Kingdom; M.D. Anderson Cancer Center; Christie Hospital, United Kingdom; Portland Hospital, United Kingdom Background: ATAC has shown that A (N = 3125) is signi¿cantly more effective than T (N = 3116) in preventing recurrences and is better tolerated, but associated with a higher risk of fractures on treatment.1,2 Little data exist on whether ef¿cacy bene¿ts or side effects persist after AI treatment is completed. New data comparing A with T at a median FU of 100 months are presented. Methods: The primary endpoint, disease-free survival (DFS), and secondary endpoints of time to recurrence (TTR), incidence of new contralateral breast cancer (CLBC), time to distant recurrence (TTDR), overall survival (OS) and death after recurrence, were assessed in both the total (ITT) and hormone receptor-positive (HR+ve) populations (84% of ITT). After treatment completion, fractures and serious adverse events continued to be collected in a blinded fashion. Results: Signi¿cant improvements were seen for A compared with T for DFS, TTR, TTDR and CLBC. In the HR+ve population: DFS (hazard ratio (HR) 0.85; 95% CI 0.76, 0.94; p=0.003), TTR (HR 0.77; 95% CI 0.67, 0.88; p=0.0001) TTDR (HR 0.84; 95% CI 0.72 – 0.98; p=0.027), and CLBC (OR 0.6; 95% CI 0.42, 0.85; p=0.004). Absolute differences for A and T increased over time (TTR 2.7% at 5 yrs and 4% at 9 yrs) and hazard rates remained lower on A compared with T after treatment completion. Breast cancer deaths were non-signi¿cantly(ns) fewer with A than T (351 vs 380 ITT; 246 vs 268 HR+ve), but there was no difference in OS (HR= 0.97 HR +ve). After treatment completion fracture rates for A and T were similar and safety bene¿ts were maintained. No new safety concerns were seen. Myocardial infarction rates on A were identical to T, on or off-treatment, and endometrial cancer rates remained lower for A than T off-treatment (Table 1). Conclusion: After a median FU of 100 months, the significant advantage for A over T for TTR, CLBC and DFS has been maintained. TTDR was also signi¿cantly superior with A compared to T. Deaths after recurrence remain ns lower on A than T. After treatment completion fracture rates on A were not different to T and no new side-effects were Abstracts – General Sessions seen. These data con¿rm the long-term superior ef¿cacy and safety of A over T as initial adjuvant therapy for post-menopausal women with hormone sensitive early breast cancer. References 1. ATAC Trialists Group Lancet 2005; 365: 60-62 2. The ATAC Trialists GroupLancet Oncol 2006; 7: 633-43 42 Mid-term ef¿cacy of a breast cancer screening program for women with a familial or genetic susceptibility: update of the Dutch MRI screening study (MRISC). Rijnsburger AJ, Obdeijn I-M, Kriege M, Boetes C, Oosterwijk JC, Tollenaar RAEM, Peterse H, Bergers E, Tilanus-Linthorst MMA, de Koning HJ, Rutgers EJT, Klijn JGM, on Behalf of the MRISC Study Group. Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands; University Medical Center Nijmegen, Nijmegen, Netherlands; Groningen University Medical Center, Groningen, Netherlands; Leiden University Medical Center, Leiden, Netherlands; Netherlands Cancer Institute, Amsterdam, Netherlands; Free University Medical Center, Amsterdam, Netherlands Introduction First results of prospective studies have shown that magnetic resonance imaging (MRI) appears to be more sensitive than mammography in detecting tumors in women with a familial or genetic susceptibility to breast cancer. We evaluated the mid-term ef¿cacy of MRI and mammography for screening in this group of women with increased breast cancer risk. Methods In the Dutch MRISC study, a non-randomized prospective multicenter study, women with >15% cumulative lifetime risk (CLTR) of developing breast cancer were screened every six months with a clinical breast examination (CBE) and once a year by mammography and MRI. Participants were divided into three subgroups according to their estimated CLTR of developing breast cancer: BRCA1/2 mutation carriers (50-85% CLTR), a high-risk group (30-50% CLTR) and a moderate risk-group (15-30% CLTR). The imaging modalities were assessed according to the BI-RADS classi¿cation, with independent readings. Results From November 1999 to March 2006, 2283 women were included in the study, including 600 proven carriers of a BRCA1 (n=427) or BRCA2 mutation (n=173) and 1080 women in the high-risk group. The mean age at entry was 40 years (range 19-75); the median follow-up time 5.3 years. Ninety-four malignant breast tumors were detected, including 19 DCIS (20%); 78 breast cancers were detected by screening. The overall rate of detection was 43.2 per 1000 women, with the highest rate in BRCA2 mutation carriers (92.5 per 1000 women). Ten of the 13 interval cancers were found in BRCA1 mutation carriers. The relative sensitivity of CBE was 21%, of mammography 44% and of MRI 69%. For DCIS these numbers were 13%, 67% and 33% respectively. The speci¿city of CBE was 98%, of mammography 95% and of MRI 90%. In BRCA1 and BRCA2 mutation carriers, 7% resp. 37% of the tumors was DCIS. In BRCA1 mutation carriers, 31% of the tumors was > 2 cm, compared to 10% in BRCA2 mutation carriers and 20% in the total group of women. The distribution of nodal status did not show much difference between BRCA1 and BRCA2 mutation carriers. Conclusions Mid-term results still show a higher sensitivity and lower speci¿city of MRI compared to mammography. Based on the results of this update, ¿rstly the high incidence of DCIS is striking, especially in BRCA2 mutation carriers. Secondly, in BRCA1 mutation carriers, the high number of interval cancers, a low incidence of DCIS and an unfavorable tumor size at diagnosis is clinically very relevant; adaptation of the screening schedule may be necessary for this speci¿c subgroup. S13 43 Detection of enhancing lesions on contrast-enhanced MRI of the breast using real-time virtual sonography: fusion of MRI and sonography data. Nakano S, Yorozuya K, Takasugi M, Mouri Y, Fukutomi T, Arai O, Mitake T. Aichi Medical University, Aichi-gun, Aichi, Japan; Hitachi Medical Corporation, Kashiwa-city, Chiba, Japan Purpose Contrast-enhanced MR imaging (MRI) is the most sensitive imaging method for detecting invasive breast cancer. Due to the limited speci¿city of MRI, attempts have been made to re-identify enhancing incidental lesions on sonography in order to more rapidly assess lesions. We recently developed a real-time virtual sonography (RVS) system, enabling both breast sonography and contrast-enhanced MRI cutaway images of the same site to be displayed in real time. The objective of this study was to assess the accuracy, reproducibility and clinical value of the RVS system for breast imaging. Materials and Methods Between May 2006 and May 2007, a total of 85 women with newly diagnosed breast cancer underwent breast surgery in our hospital. Of these, 35 women with histologically proven invasive ductal carcinoma underwent RVS. All patients were examined using mammography, sonography, and dynamic breast MRI before core needle biopsy or surgical resection. Results were correlated with histopathological ¿ndings. MR images were obtained on a Magnetom 1.5-T imager using a Àexible body surface coil. All patients were examined in the supine position as near as possible to the sonography/surgical position. Both non-enhanced and contrast-enhanced images were acquired using coronal T1-weighted 3-D FLASH sequences. Results Of 35 women with invasive ductal carcinoma, 3 patients displayed 1 additional malignant lesion. A total of 17 foci of 38 lesions were palpable (median size, 14 mm; range, 7-54 mm). Lumpectomy was performed for 18 women, and 17 women underwent mastectomy. Sensitivity was 89% (34/38) for sonography, 94% (36/38) for MRI, and 94% (36/38) for the RVS system. As 2 lesions were not visualized on MRI, RVS was performed in 36 enhancing lesions. A virtual MPR image of the target tumor was displayed under good condition correspondence with the sonography image in all patients(Fig.1). Furthermore, RVS was largely unaffected by respiratory movements. Enhancing incidental lesions present in 5 lesions were not seen using conventional techniques. Of these, 3 lesions (60%) could be identi¿ed only on repeated sonography, but all 5 incidental lesions could be identi¿ed easily using the RVS system. Of the 2 lesions (40%) not initially seen on sonography, one was a benign hemangioma, and the other was a small breast cancer. Conclusions The RVS system could project enhanced MRI information onto a body surface correctly while checking sonography form images without large-scale equipment or radiation exposure. The present results suggest that the RVS system offers excellent accuracy for identi¿cation of enhancing incidental lesions. S14 Abstracts – General Sessions 44 MRI for diagnosing pure ductal carcinoma in-situ. Kuhl CK, Schrading S, Wardelmann E, Braun M, Kuhn W, Schild HH. University of Bonn, Bonn, Germany Background: Diagnosing breast cancer in its intraductal stage may be helpful to prevent the development of invasive cancer. We investigated the detection rates of ductal carcinoma in situ (DCIS) by mammography and breast MRI, and compared the biologic pro¿le of mammographydetected versus MRI-detected DCIS. Methods: During a 5-year study period, women who were referred to an academic national breast center were offered MRI in addition to mammography for diagnostic assessment and screening. Mammograms and breast MRI studies were interpreted independently by two radiologists. A total 193 women received the ¿nal surgical pathology diagnosis of pure DCIS, without associated invasive breast cancer or micro-invasion. Of those, 167 had undergone both imaging tests preoperatively. We investigated the mode of detection (diagnosed with both modalities, diagnosed with neither modality, diagnosed only by mammography or diagnosed only by MRI) and compared the biologic pro¿le (nuclear grading, receptor status, size) of mammographydiagnosed DCIS with MRI-only detected DCIS. In addition, we investigated the risk profile of women with DCIS diagnosed by mammography versus those who were diagnosed by MRI. Results: Overall, 93 of the 167 DCIS (56%) were diagnosed by mammography, and 153 (92%) by MRI (p < 0.001). With increasing nuclear grade, sensitivity of mammography decreased; it was highest in low grade DCIS and lowest in high grade DCIS. It even dropped further (to 35%) in high grade DCIS without necroses. The sensitivity of MRI was superior to that of mammography across all DCIS subtypes. In addition, sensitivity increased with nuclear grade of DCIS; it was lowest in low grade DCIS (80%) and highest in high grade DCIS (98%), independent of presence of absence of necroses. The risk pro¿le of women with MRI-only diagnosed DCIS did not differ signi¿cantly from women with mammography diagnosed DCIS. In particular, women with mammography-negative (only MRI-detected) DCIS had the same personal or familial risk pro¿le, the same age and age range, and the same mammographic breast density as those whose DCIS was diagnosed by mammography. Discussion: Mammographic sensitivity for DCIS is indeed limited. This holds especially true for high grade DCIS: Half of all high grade DCIS that came to diagnosis during the study period was only MRI detected. Thus, MRI improves our ability to diagnose DCIS overall, but in particular regarding high grade DCIS. Thus, MRI may help avoid potentially aggressive invasive breast cancer. 45 Noninvasive monitoring of neoadjuvant chemotherapy using optical tomography with ultrasound localization: initial experience. Tannenbaum S, Hegde P, Kane M, Xu C, Kurtzman S, Baccaro N, Iyer M, Wilson L, Deckers P, Zhu Q. University of Connecticut, Farmington, CT; University of Connecticut, Storrs, CT PURPOSE: To investigate the feasibility of using optical tomography using near infrared light (NIR) combined with ultrasound (US) localization (NIR/US) to monitor tumor vascular changes during chemotherapy and assessing tumor pathological response. We were also interested in a comparison of NIR/US with contrast-enhanced Magnetic Resonance Imaging (MRI) in predicting residual cancer following neo-adjuvant chemotherapy. PATIENTS AND METHODS: 11 female patients who underwent neoadjuvant chemotherapy were studied at intervals during their treatments with a combined imager consisting of a commercially available US system coupled to a near infrared imager constructed by our group. A centrally located US transducer and NIR sensors surrounding it (NIR/US) was used to simultaneously acquire coregistered US images and optical data. Tumor vascular content was assessed based on calculated total hemoglobin (tHb) concentration and volume. Percentage blood volume index (PBVI) was calculated as the product of tHb concentration and volume using the pretreatment image as baseline. Based on the pathological assessment of the specimen, patients were classi¿ed into three response groups: complete or near complete responders A, partial responders B, and non-responders C. Student’s t distribution was used to calculate statistical signi¿cance on the PBVI between three groups. RESULTS: The mean PBVI of groups of A, B and C were 23.6%4.2%, 42.6%5.5%, 86.8% 30.1%, respectively. The PBVI in A is signi¿cantly lower than B (p<0.01) and C (p<0.02); while the PBVI in B is signi¿cantly lower than non-responder group C (p<0.05). The PBVI results from responders (A+B) obtained at the end of cycles two, four and prior to surgery were also evaluated. Reduction in PBVI was noted in most responders at the ¿rst response assessment compared to pre-treatment levels. At the end of cycle four, the PBVI of the responder group is signi¿cantly lower than non-responders (p<0.01); the signi¿cance increases prior to surgery (p<0.001). NIR/US images revealed different patterns of response in all patient groups emphasizing the heterogeneity of these large tumors. NIR/US was comparable to MRI in distinguishing non-responders (C) from the responding groups (Aand B). Conclusion: Our ¿ndings indicate that NIR/US using volumetric tHb concentration as de¿ned by PBVI has great potential to repeatedly monitor tumor vascular changes during chemotherapy. The PBVI correlates well with the pathologic response in this pilot study. In this study, NIR/US appears comparable to MRI in distinguishing responding from non-responding tumors. Additionally, it distinguished the degree of response between complete (A) and partial (B) responders. 46 Tomosynthesis for the detection of breast cancer in a clinical setting. Ikeda DM, Ruschin M, Timberg P, Svahn T, Zackrisson S, Andersson I. Lund University, Malmoe University Hospital, Malmoe, Sweden; Stanford University School of Medicine, Stanford, CA Purpose: To compare the performance of tomosynthesis to digital mammography for cancer detection in a clinical setting Material and Methods: Patients were selected from a digital mamographic screening (14) or clinical (15) series for subtle signs of breast carcinoma. Tomosynthesis (TS) was performed in the projection in which the ¿nding was least visible or not visible. The digital mammograms (DM) were obtained on Siemens Mammomat Novation, the TS on a prototype adapted from the Mammomat Novation. For the TS 25 projection images were aquired over an angular range of 50 degrees at a dose that was approximately double that of one DM image and using the same beam quality as determined by the automatic exposure control of the DM unit (W/Rh). All patients had a complete work-up including in addition to DM, US, and needle biopsy followed by surgery. DM and TS images were reviewed for signs of breast cancer by 2 expert breast imagers who classi¿ed ¿ndings for lelsion visibility and probability of breast carcinoma using BIRADS categories. Findings: Twenty-nine women (average age 59 years, range 34 – 84) with 33 breast cancers in 30 breasts were eligible for the study. Average tumor size was 1.4 cm. The histologic types included 17 invasive ductal cancers (IDC), 9 invasive lobular cancers, 3 IDC with ductal carcinoma in situ (DCIS), 1 DCIS alone and 1 intracystic papillary carcinoma. On TS 15 spiculated masses were found (including 2 found by TS alone), 6 masses combined with calci¿cations, 5 cases of architectural distortion and 2 cases with clustered calci¿cations. In 5 cases no lesion was visible, Findings were more conspicuous on TS compared to DM in 22 cases, equally visible in 10 and not visible in one. Two cancers were seen on tomosynthesis alone, both were unexpected second spiculated masses in dense breast tissue in breasts with one known spiculated cancer. The BIRADS classi¿cation was upgraded from BIRADS 1-3 on DM to 4 - 5 on TS in 17 patients. Conclusion: These results suggest that the sensitivity of TS is superior to DM for the detection of breast cancer in this clinical setting. Abstracts – General Sessions 51 Is completion axillary dissection always required after a positive sentinel node biopsy? NSABP B-32. Julian TB, Anderson SJ, Fourchotte V, Brown AM, Boudros E, Mamounas EP, Bear H, Costantino JP, Wolmark N. NSABP Medical Affairs, NSABP Investigators & NSABP Operation & Biostatistical Centers, Pittsburgh, PA Background: A positive sentinel node biopsy (SNB) is usually followed by an axillary dissection (AD). In the majority of clinically node negative patients the risk for positive non-sentinel axillary nodes (NSN) is low. Factors affecting the positive NSN rate and the necessity of AD following a positive SNB are evaluated in NSABP B-32. Materials and Methods: After strati¿cation, women with operable invasive breast cancer and clinically negative nodes were randomized to Sentinel Node Resection (SNR) with immediate conventional Axillary Disection (AD) [Group 1] or to SNR without AD [Group 2]. Group 2 patients with positive SNs underwent AD. A multivariate analysis of SN positive patients for whom both a SNR and an AD had been performed was used to assess the need for AD following SNB. Their nodes were classi¿ed as either SNs or NSNs, de¿ned as all axillary dissection nodes plus any intramammary or other nodes that were not resected as SNs Results: Between May 1999 and February 2004, 5,611 patients were entered into NSABP Protocol B-32. 2,807 were assigned to Group 1 and 2,804 were assigned to Group 2. There was a total of 1,361 SN positive patients with AD from Groups 1 and 2. Data from 1,166 patients were available for multivariate analysis (595 from Group 1; 571 from Group 2). Results from the multivariate analysis indicated that a signi¿cantly higher percentage of Group 2 patients had positive NSN compared to Group 1 (41.5% vs. 35.5%, p=0.032). Clinical tumor size was a signi¿cant predictor for positive NSN (p=0.0010). Percentages of patients having positive NSN were signi¿cantly increased by the number of positive SNs (p<0.0001). Lymphovascular invasion was a signi¿cant predictor for positive NSN (p<0.0001). The percentages of patients with positive NSN signi¿cantly decreased as the number of hot spots identi¿ed increased (p=0.0047), and as the number of SNs removed increased (p<0.0001). Age at study entry, type of biopsy performed, histologic grade, HER-2 status, location of tumor and ER/PR status were not signi¿cant multivariate predictors of having positive NSN. Predictive modeling for positive NSN probability will be presented. Conclusion: Completion AD following a positive SNB, although helpful in prognosis and treatment planning, may not be required in patients with small tumors and in the absence of lymphovascular invasion. 52 The impact of micrometastases in the sentinel nodes of patients with invasive breast cancer. Hansen NM, Grube BL, Ye C, Turner R, Brennan M, Brenner J, Giuliano AE. John Wayne Cancer Institute, Santa Monica, CA; Saint John’s Hospital and Health Center, Santa Monica, CA Background: Lymph node metastases ar the most signi¿cant prognostic indicator for patients with breast cancer. With the emergence of sentinel node biopsy (SNB) and the ability to evaluate multiple levels of a sentinel node (SN), there has been an increase in the detection of metastases in the SN (s) both with routine hemoxylin and eosin stains (H&E) as well as with the addition of immunohistochemical stains (IHC). Most of the increase is due to the identi¿cation of micrometastases. This prospective study was designed to determine the survival impact of micrometastases in SN(s) of patients with invasive breast cancer. The study is based on the new 6th ed AJCC staging criteria which de¿nes a negative lymph node N0 if it is negative on H&E, pN0(i+) if there is a tumor deposit<0.2mm detected by IHC alone, a micrometastases as pN1mic as a tumor deposit measuring between 0.2mm and 2mm and a macrometastases as pN1 with a tumor deposit >2mm. Any case done prior to the new 6th ed AJCC staging criteria was re-evaluated and classi¿ed according the most current staging critieria. Results: Between 1/92 and 4/30/99, 790 paitents underwent SNB at our institution. The SN was examined by H&E and if the SN was negative S15 on H&E, then IHC stains were added. The patients were divided into 4 groups based on the size of the SN metastases as follows: Group I: pN0 (n=486), Group II: pN0(i+) (n=84), Group III: pN1mic (n=54) and Group IV: pN1 (n=166). The majority of patients in all 4 groups chose a breast conserving procedure. 76.5% of patients received some form of adjuvant therapy. Of the patients treated with adjuvant therapy, 43.9% received hormonal therapy alone, 21.2% received chemotherapy alone and 34.9% received a combination of chemotherapy and hormonal therapy. At a median follow up of 72.5 months, the size of SN metastases was a signi¿cant predictor of disease free survival (DFS) and overall survival (OS) only for patients in Group IV. There was no signi¿cant difference in 8-yr DFS or OS among patients in Groups I, II and III. Conclusions: Patients with micrometastastic tumor deposits in the SN de¿ned as pN0(i+) or pN1mic do not appear to have a worse 8-yr DFS or OS compared to SN negative patients. There was a signi¿cant decrease in 8-yr DFS and OS in patients with pN1 disease in the SN. The true signi¿cance of these micrometastatic depositis is still unclear but may help to eventually better de¿ne which patients should receive maximum adjuvant therapy, medical or surgical and in which patients additional therapy could be avoided. DFS and OS by Group Group I II III IV 8-yr DFS (%) 92.9 92.8 89.6 77.5 8-yr OS (%) 94.6 100 94.1 79.6 53 High sensitivity of a molecular assay for breast metastases in sentinel lymph nodes that are dif¿cult to detect by frozen section. Blumencranz P, Deck KB, Whitworth PW, McCue P, Reintgen DS, Chagpar AS, Beitsch P, Julian TB, Mamounas M, Saha S, Giuliano A, Simmons R. Morton Plant Mease Healthcare, Clearwater, FL; Saddleback Memorial Hospital, Laguna Hills, CA; Nashville Breast Center, Nashville, TN; Jefferson Medical College, Philadelphia, PA; Lakeland Regional Medical Center, Lakeland, FL; James Brown Cancer Center, Louisville, KY; Dallas Surgical Group, Dallas, TX; Allegheny General Hospital, Pittsburgh, PA; Aultman Hospital, Canton, OH; McLaren Regional Medical Center, Flint, MI; John Wayne Cancer Institute, Santa Monica, CA; Weill-Cornell Brest Center, New York, NY Background: Metastases in the lymph nodes of patients with grade I tumors, stage I tumors, invasive lobular carcinomas, or post neoadjuvant treatment are dif¿cult to identify due to being smaller or dif¿cult to assess. An accurate diagnosis requires a highly skilled pathologist with extensive experience. RT-PCR may offer a more accurate intra-operative method for diagnosing nodal metastases. Methods: A prospective study was conducted at 12 clinical sites with a rapid RT-PCR assay (GeneSearchTM Breast Lymph Node (BLN) Assay; Veridex, LLC) for the detection of nodal metastases in invasive breast cancer patients. The RT-PCR assay includes genetic markers cytokeratin 19 and mammaglobin to detect metastases > 0.2 mm and evaluates half of the node. Performance calculations used permanent section H&E as the comparator. Results: 319 patients had intra-operative frozen section H&E (FS) results and RT-PCR assay results. 45 patients (14.1%) were diagnosed with invasive lobular carcinoma only. 187 patients (58.6%) were stage I; 176 patients (55.2%) were grade I; 9 patients (2.8%) had neoadjuvant therapy. Results for BLN Assay and FS performance against permanent section histology are shown in the table below. Conclusions: The data indicate the rapid RT-PCR assay has high sensitivity to detect nodal metastases as compared to frozen section in patients with invasive lobular breast cancer, tumor grade I, tumor stage I and neo-adjuvant therapy. Comparable speci¿city is seen with both tests. These data indicate that the RT-PCR assay that allows intra-operative evaluation of 50% of the node, rather than the <5% by frozen section S16 Abstracts – General Sessions histology, may offer a better opportunity for avoiding second surgeries for complete axillary dissection in these dif¿cult-to-detect cases. BLN Assay and FS Performance Characteristics Patient Category N Performance Measure BLN Assay (95% CI) Lobular 45 Sensitivity 100% (76.8 – 100) Speci¿city 93.5% (78.6 – 99.2) Stage I 187 Sensitivity 96.2% (80.4 – 99.9) Speci¿city 96.3% (92.1 – 98.6) Grade I 176 Sensitivity 97.3% (85.8 – 99.9) Speci¿city 92.8% (87.2 – 96.5) Neo-adjuvant 9 Sensitivity 66.6% (9.4 – 99.2) Speci¿city 100% (54.1 – 100) FS (95% CI) 64.3% (35.1 – 87.2) 96.8% (83.3 – 99.9) 84.6% (65.1 – 95.6) 98.1% (94.7 – 99.6) 83.8% (68.0 – 93.8) 98.0% (93.8 – 99.6) 33.3% (0.84 – 90.6) 83.3% (35.9 – 99.6) 54 Increased sentinel lymph node lymphangiogenesis predicts non-sentinel axillary lymph node involvement in breast cancer patients with a positive sentinel node. Van den Eynden GG, Vandenberghe MK, van Dam P-JH, Colpaert CG, van Dam P, van Marck EA, Vermeulen PB, Dirix LY. (Lab Pathology University of Antwerp/University Hospital Antwerp, Wilrijk; Oncology Center, GH St-Augustinus, Wilrijk, Belgium), Antwerp, Belgium Background: Lymph node (LN) lymphangiogenesis has recently been shown to be important in the premetastatic niche of sentinel LNs. To study its role in the further metastatic spread of human breast cancer, we investigated the association of angiogenesis and lymphangiogenesis in sentinel LN metastases with the presence of non-sentinel LN metastases in breast cancer patients with a positive sentinel LN. Methods: Angiogenesis and lymphangiogenesis -quantified as endothelial cell proliferation fraction (ECP%) and lymphatic endothelial cell proliferation fraction (LECP%)- were assessed in sentinel LN metastases of 65 T1/T2 breast cancer patients using respectively CD34/Ki67 and D2-40/Ki67 immunohistochemical doublestains. Correlations were analysed between non-sentinel LN status, ECP%, LECP% and previously established factors predicting non-sentinel LN status (number of metastatically involved sentinel LNs, size of the primary tumour and LN metastasis, presence of lymphovascular invasion in the primary tumour and of extracapsular growth in the sentinel LN metastasis). Results: Metastatical involvement of 1, 2, 3 or 4 sentinel LNs was found in respectively 45 (69.2%), 11 (16.9%), 8 (12.3%) and 1 (1.5%) patient. Thirty seven out of 65 patients (56.9%) had at least one metastatically involved non-sentinel LN (median = 3). Size of the sentinel LN metastasis (p = 0.001), lymphovascular invasion (p = 0.02), extracapsular growth (p = 0.02) and LECP% (p = 0.01) were correlated with a positive non-sentinel LN status. Nor the size of the primary tumour, nor Nottingham grade, nor ER, PR or Her2 status, nor the metastatical involvement of more than one sentinel LN, nor ECP% in the lymph node metastases were correlated with the presence of non-sentinel LN metastases. The multivariate logistic regression model retained high LECP% (OR = 4.2, p = 0.01) and the presence of extracapsular growth (OR = 3.38, p = 0.04) as independent predictive factors for the presence of non-sentinel LN metastases. Conclusions: Increased sentinel LN metastasis lymphangiogenesis predicts metastatical involvement of non-sentinel axillary LNs. These are the ¿rst data in human samples supporting the hypothesis that lymphangiogenesis in sentinel LN metastases is involved in further metastatic spread of human breast cancer. Our data furthermore suggest that including sentinel LN lymphangiogenesis might improve instruments to predict the likelihood of additional LN metastases in breast cancer patients with a positive sentinel LN biopsy, such as the Memorial Sloan Kettering Cancer Center nomogram. 61 The inÀuence of a very high vegetable-fruit-¿ber, low-fat diet on prognosis following treatment for breast cancer: results from the Women’s Healthy Eating and Living (WHEL) randomized trial. Pierce JP, Natarajan L, Cann BJ, Parker BA, Greenberg ER, Flatt SW, Rock CL, Kealey S, Al-Delaimy WK, Bardwell WA, Carlson R, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Madlensky L, Marshall J, Newman VA, Ritenbaugh C, Thomson CA, Wasserman L, Stefanick ML. Moores UCSD Cancer Center, University of California, San Diego, La Jolla, CA; Kaiser Permanente Northern California, Oakland, CA; Fred Hutchinson Cancer Research Center, Seattle, WA; Stanford Comprehensive Cancer Center, Stanford University, Stanford, CA; University of California, San Diego; University of California, Davis, Davis, CA; M.D. Anderson Cancer Center, The University of Texas, Houston, TX; Center for Health Research, Portland, OR; Roswell Park Cancer Institute, Buffalo, NY; University of Arizona, Tucson, AZ; Arizona Cancer Center, Arizona Prevention Center, University of Arizona, Tucson, AZ; Stanford Prevention Research Center, Stanford University, Stanford, CA Context: Evidence is lacking that a dietary pattern high in vegetables, fruit, and ¿ber and low in total fat can inÀuence breast cancer recurrence or survival. Objective. To assess whether a major increase in vegetable, fruit, and ¿ber intake and a decrease in dietary fat affects risk for recurrent and new primary breast cancer or mortality in breast cancer survivors. Design, Setting, and Participants. A multi-institutional randomized controlled trial of dietary change in 3088 women previously treated for early stage breast cancer, aged 18-70 years at diagnosis. Women were enrolled between 1995 and 2000, and followed through June 1, 2006. Intervention. A telephone counseling program supplemented with cooking classes and newsletters promoted daily targets of 5 vegetable servings, 16-oz vegetable juice or vegetable equivalents, 3 fruit servings, 30 g ¿ber, and 15-20% energy intake from fat. The comparison group was provided national dietary guidelines. Main Outcome Measures. Invasive breast cancer event (recurrence or new primary) or death from any cause. Results. From comparable dietary patterns at baseline, a conservative imputation analysis showed that the intervention group (N=1537) achieved and maintained the following statistically significant differences from the comparison group (N=1551) through 4 years: servings of vegetables, +65%; fruit, +25%; ¿ber, +30% and energy intake from fat, -13%. Large differences in plasma carotenoid concentrations validated changes in fruit and vegetable intake. Throughout the study, women in both groups received similar clinical care. We will report breast cancer endpoints and overall mortality on over 95% of both study groups through the 7.3-year average followup period. We will discuss the differences between our results and the previously published WINS. Trial Registration: http://www.clinicaltrials.gov/ct/show/ NCT00003787?order=1 Identi¿er: NCT 00003787. 62 Outcome prediction for clinical stage II and III ER+ breast cancer based on treatment response, pathological stage, tumor grade, Ki67 proliferation index, and estrogen receptor status after neoadjuvant endocrine therapy. Ellis MJ, Tao Y, Luo J, Evans DB, Bhatnagar AS, Chaudri Ross H, von Kameke A, Miller WR, Eiermann W. Washington University, St. Louis, MO; Novartis Pharma AG, Basel, Switzerland; WWS Group Ltd, Muttenz, Switzerland; Edinburgh University, Scotland; Red Cross Women’s Hospital, Munich, Germany Introduction: Long-term follow up of postmenopausal women with estrogen receptor positive (ER+) Stage II and III breast cancer too large for breast conservation enrolled into a randomized neoadjuvant endocrine therapy study facilitated the development of a model for risk of relapse based on the short-term anti-tumor effects of letrozole or tamoxifen. Abstracts – General Sessions Methodology: Post-treatment ER status, Ki67 proliferation index, histological grade, pathological tumor size, node stage, and treatment response were analyzed by Cox proportional hazards modeling to identify independent predictors for relapse free and overall survival. Since there was no difference between neoadjuvant letrozole and tamoxifen in terms of RFS and OS and almost all patients received adjuvant tamoxifen, the two groups were pooled for analysis. Results: Median follow-up was 61.2 months from the initiation of endocrine therapy. Patients with con¿rmed baseline ER+ tumors that were down-staged to Stage 1 at surgery had 100% relapse free survival (RFS) (P=0.0006). Multivariate testing of post-treatment tumor characteristics revealed that pathological tumor stage, node status, Ki67 level, tumor grade, ER status, and clinical response were signi¿cant independent factors. A predictive model incorporating this information differentiated among four groups of patients with RFS within the observation period of 100%, 82%, 52%, and 0% with a Harrell’s optimism-corrected c discrimination index of 0.73 (95% CI: 0.70-0.84). Conclusions: Clinical stage II or III patients down-staged to Stage 1 or 0 with endocrine therapy are at very low risk of relapse at ¿ve years of follow up. A multivariate predictive model provides additional information to discriminate between patients with the extremes of breast cancer outcomes. Four months of neoadjuvant endocrine therapy followed by a response assessment is a promising approach for predicting the course of ER+ breast cancer in postmenopausal women. 63 Prognostic utility of the 21-gene assay compared with Adjuvant! in hormone receptor (HR) positive operable breast cancer with 0-3 positive axillary nodes treated with adjuvant chemohormonal therapy (CHT): an analysis of intergroup trial E2197. Goldstein L, Ravdin P, Gray R, Yoshizawa C, Childs B, Rowley S, Shak S, Badve S, Baehner FL, Davidson N, Sledge GW, Sparano JA. Eastern Cooperative Oncology Group, Brookline, MA; MD Anderson Cancer Center, Houston, TX; Genomic Health, Inc., Redwood City, CA; Sano¿ Aventis, Bridgewater, NJ Background: Although previous reports have compared multigene markers to clinical features in multivariate models, there is little information about the utility of such markers in the context of validated instruments incorporating clinical features and treatment interventions such as Adjuvant!. Methods: A sample of 465 patients (pts) with HR-positive disease from E2197 who did (N=99) or did not have a recurrence after CHT and had available tissue had an Oncotype DX Recurrence Score (RS) assay, and also had recurrence risk estimated by Adjuvant! E2197 included 2885 evaluable pts with 0-3 positive nodes treated with four 3-week cycles of doxorubicin (60 mg/m2) plus cyclophosphamide 600 mg/m2 (AC) or docetaxel 60 mg/m2 (AT) and tamoxifen. Median follow-up was 76 months. Tumor grade, HR expression, and Her2 expression were determined centrally. Five-year recurrence estimates were computed by Adjuvant! with a batch processor (using central grade), and pts were classi¿ed as “low”, “intermediate”, or “high” Adjuvant! risk similar in proportion to the standard RS risk groups. The prognostic utility of RS was evaluated in each Adjuvant! risk group. Results: Similar to node-negative disease, 46% had low (< 18), 30% had intermediate(18–30), and 24% had a high RS (≥ 31). RS was a highly signi¿cant predictor of recurrence (local and distant), including node-negative (P = 0.0007) and positive (P=0.0004) disease. Low RS predicted low recurrence (< 5%) irrespective of nodal status. RS provided additional information to Adjuvant! (see table); more detailed analyses comparing the prognostic utililty of Adjvuant! and RS will be presented. Conclusions: Oncotype DX RS provides additional prognostic information in HR-positive operable breast cancer treated with adjuvant CHT when outcome is modeled by Adjuvant!, particularly in those projected by Adjuvant! to have better outcomes. Although both Adjuvant! and Oncotype DX have been prospectively validated for 10 year outcomes (including only node-negative tam-treated pts S17 for the latter), this analysis demonstrates that multigene signatures provide additional prognostic information to clinical variables in this population treated with CHT. Odds Ratio for Recurrence by Oncotype DX RS in Adjuvant ! Risk Groups Adjuvant! Low (N=202) Adjuvant! Int. (N=138) Adjuvant! High (N=125) RS Ratio: 2.55 (1.11,5.85) P=0.03 9.37 (3.01,2.92) P<0.001 0.89 (0.3,2.63) P=0.83 Inter/Low RS Ratio: 4.00 (1.73, 9.25) P=0.001 5.78 (1.7,19.6) P=0.004 2.62 (1.05,6.51) P=0.04 High/Low Odds ratio for recurrence (95% con¿dence intervals) 64 Value of centrally-assessed Ki-67 labeling index as a marker of prognosis and predictor of response to adjuvant endocrine therapy in the BIG 1-98 trial of postmenopausal women with estrogen receptor-positive breast cancer. Viale G, Giobbie-Hurder A. BIG 1-98 Collaborative Group and International Breast Cancer Study Group (IBCSG), Bern, Switzerland Background: Ki-67 protein has been shown to have prognostic value; however, as a marker of response to endocrine therapy, the results are less clear. We explore Ki-67 labeling index (Ki-67 LI) as a predictive marker using data from the BIG-1-98 trial, a randomized, double-blind, phase III trial which showed that letrozole (L) improved disease-free survival (DFS) as compared with tamoxifen (T) for postmenopausal women with hormone receptor-positive disease. Methods: Between March 1998 and May 2003, 8,010 postmenopausal women with hormone receptor-positive breast cancer were enrolled in the BIG 1-98 trial, of whom 4,922 were randomly assigned to the two monotherapy arms (L or T for 5 years; 51 months median followup). 2,685 of 4,922 women had ER+ (> 1% immunoreactive cells by central review) tumors and also had tumor material assessed by the IBCSG Central Pathology Laboratory for Ki-67 LI using the Mib-1 monoclonal antibody (Dako). Ki-67 LI data were analyzed divided at the median of the distribution of values. Cox modeling estimated hazard ratios comparing L vs T on DFS and assessed treatment-bycovariate interactions. Results: Ki-67 showed prognostic value: DFS was signi¿cantly worse in the cohort with higher Ki-67 LI (log-rank p=0.0001). A differential treatment effect of L vs. T was observed (p= 0.07 interaction) suggesting greater bene¿t in the L arm for the cohort with higher Ki-67 LI. 4-Yr DFS % (S.E.) Overall 2,685 89.1 (0.68) Ki-67 N 0%-11% 1,433 92.2 (0.80) > 11% 1,252 85.6 (1.12) Treatment L T L T L T 4-Yr DFS % (S.E.) 91.8 (0.85) 86.5 (1.06) 93.4 (1.01) 90.9 (1.27) 89.6 (1.41) 81.5 (1.73) Hazard Ratio 95% CI (L:T) 0.64 (0.51, 0.80) 0.82 (0.58, 1.16) 0.54 (0.40, 0.72) Conclusion: The value of Ki-67 as a marker of prognosis in postmenopausal women with ER+ tumors is clear. A possible predictive role for response to adjuvant endocrine therapies is suggested and will be further explored. 65 Erythropoietin receptor expression in breast cancer and correlation to tamoxifen response. Larsson A-M, Jirstrom K, Rydén L, Landberg G, Pahlman S. Lund University, University Hospital MAS, Malmo, Sweden Background: Erythropoietin (EPO) stimulates erythropoiesis in response to hypoxia. The biological effects of EPO in erythropoiesis are mediated through its receptor (EPOR), which initiates intracellular signalling cascades that lead to increased proliferation, differentiation and survival. In recent years EPO and EPOR have also been detected in various cancer forms, but it is still not fully elucidated in what way this expression affects tumours. Recombinant EPO is also used for treating anaemia in cancer patients and there are contradicting results regarding direct effects on tumour growth and behaviour. The aim with this study was to evaluate the expression of EPOR in a clinical breast tumour material and to investigate if this expression could add predictive or prognostic information in relation to Tamoxifen treatment in premenopausal breast cancer patients. S18 Abstracts – General Sessions Material and methods: A tissue microarray based on 500 tumours from a clinical trial with premenopausal women randomized to receive two years of either Tamoxifen or no adjuvant treatment was evaluated for EPOR expression using immunohistochemistry (IHC) (anti-EPOR antibody, C-20, Santa Cruz). The speci¿city of the antibody was veri¿ed by Western blot and IHC analyses in MCF-7 breast carcinoma cells with EPOR expression knocked down by EPOR siRNA. The staining intensity was scored semi-quantitatively as weak, moderate or strong. Results: EPOR expression was significantly associated with age (p=0.001), and inversely associated with tumour size (p=0.011). There was also a strong positive correlation between EPOR and VEGFR2 expression (p=0.005). Tamoxifen signi¿cantly increased recurrence free survival (RFS) in patients with ER and/or PR positive (ER/PR+) tumours and low expression of EPOR (p=0.001). In tumours with a high expression of EPOR, no statistically signi¿cant effect was detected in the Tamoxifen-treated patients compared to controls (p=0.98), indicating that EPOR might be a negative predictive marker, associated with Tamoxifen resistance. In the untreated cohort, RFS was signi¿cantly improved for patients with ER+ tumours with a high EPOR expression. In ER- tumours there was no difference in RFS in relation to EPOR expression. This indicates that EPOR might add prognostic information in patients with ER+ breast cancer not treated with Tamoxifen. Discussion: EPOR is expressed in breast cancer cells but its function there is not fully known. Here we show that high expression of EPOR is related to Tamoxifen resistance. The biological signi¿cance behind this observation is not known. However, EPOR and VEGFR2 expression covariate in the studied material and one hypothesis is that the intracellular signalling pathways downstream of EPOR and VEGFR2 might interfere with ER pathways independent of Tamoxifen. Our ¿ndings suggest that EPOR expression in breast carcinoma affects tumour behaviour, and it is of great importance to further unravel the functions of EPOR in tumour cells and how tumours are affected by EPO stimulation. 66 Inflammatory breast cancer pathogenesis is mediated in signi¿cant part by translation initiation factor eIF4G ampli¿cation and unorthodox protein synthesis. Silvera D, Arju R, Darvishian F, Levine PH, Formenti SC, Schneider RJ. New York University School of Medicine, New York, NY; The George Washington University School of Public Health and Health Services, Washington, DC Background: The molecular mechanisms that drive development of inÀammatory breast cancer (IBC) are unknown. IBC is unusual in generation of tumor emboli, which are highly metastatic cell clusters that strongly over-express VEGF-A, which in turn permeabilizes the vasculature and sustains emboli proliferation. IBC also uniquely over-expresses the adhesion molecule E-cadherin, which promotes metastasis by blocking adherence of IBC emboli to stroma. Using patient IBC specimens and development of modi¿ed IBC cell lines and animal models, we show that many of the extreme pathological disease characteristics of IBC, including VEGF-A and E-cadherin overexpression, result in large part from overexpression of a single gene encoding translation initiation factor eIF4G. eIF4G overexpression reprograms the protein synthetic machinery of IBC cells for increased translation of a small group of mRNAs that promote IBC tumor cell survival, vascular permeabilization/angiogenesis, and emboli formation. Materials and Methods: Protein factor levels expressed in IBC tissues were determined by immunohistochemistry (IHC), and in IBC cell lines by immunoblot analysis. eIF4G expression was silenced by shRNA adenoviruses. To analyze tumor growth and vasculogenesis we used the chicken chorioallantoic membrane (CAM) model, and xenograft cell subcutaneous implantation in nude mice. Maintenance of silencing of eIF4G protein, expression of VEGF and E-cadherin levels, as well as angiogenesis, were monitored by immuno-staining techniques. Results & Discussion: Gene expression and IHC studies revealed that the SUM149 IBC cell line, as well as 70% of IBC specimens (n= 42; p<0.01) strongly over-expressed eIF4G compared to normal tissue, with no alteration in other translation factors. In animal models, shRNA silencing of eIF4G by ∼90% only slightly reduced global protein synthesis, but selectively inhibited IBC tumor growth, VEGF, and p120 catenin mRNA translation, as well as cell surface retention of Ecadherin, vasculature permeabilization and angiogenesis– key hallmarks of IBC. E-cadherin is retained on the cell surface by interaction with p120 catenin. Engineered overexpression of p120 restored E-cadherin to the cell surface and IBC tumor formation. Surprisingly, analysis of VEGF-A and p120 catenin mRNAs showed they contain capindependent translation elements known as an Internal Ribosome Entry Sites (IRES), which required high levels of eIF4G for translation. These and other data demonstrate that high levels of eIF4G are singularly responsible for many of the unique properties of IBC. Inhibition of eIF4G might constitute an attractive target for development of new therapeutics for IBC. 71 Disease-free survival according to local immunohistochemistry for HER2 and central Àuorescence in situ hydridization for patients treated with adjuvant chemotherapy with and without trastuzumab in the HERA (BIG 01-01) trial. McCaskill-Stevens W, Procter M, Goodbrand J, Azambuja E, LeylandJones B, Ruschoff J, Dowsett M, Wermuth P, Dolci S, Gelber RD, Piccart-Gebhart M. National Cancer Institute, Bethesda, MD; Frontier Science, Kingussie, United Kingdom; Jules Bordet Institute, Brussels, Belgium; Emory University, Atlanta, GA; Klinikum Kasseland TARGOS Molecular Pathology Gmbh, Kassel, Germany; Hoffmann-La Roche, Basel, Switzerland; Royal Marsden National Health Service Trust, London, United Kingdom; Dana-Farber Cancer Institute, Boston, MA Background: Recent American Society of Clincal Oncology guidelines for the use of immunohistochemistry (IHC) and Àuorescence in situ hydridization (FISH) to determine which patients have HER-2 gene ampli¿cation or protein overexpression for treatment of breast cancer with trastuzumab have been published (Wolff, et al., JCO 2007). Evidence-based data are required to determine the best assay to use and to ¿ne tune criteria for positivity. Methods: In the HERA trial, tissue for patients with local IHC 3+ and 2+ were submitted for central assessment prior to randomization. Patients with central IHC 3+ or centeral FISH + were eligible for enrollment. We analyzed data from women in the HERA trial randomized to 1 year of trastuzumab or observation. Disease-free survival (DFS) was the primary endpoint and treatment differences were assessed using KaplanMeier estimates and hazard ratios. At 23.5 months median follow-up, the 3-year DFS percent was 80.4% for the trastuzumab group (n=1703) compared with 74.4% for the observation group (n=1698) (HR 0.64, 95% CI [0.54, 0.76]) (Smith, et al., Lancet 2007). Conclusion: Local IHC assessment and central FISH assessment of HER2-positivity in the HERA trial did not indicate substantial heterogeneity in the relative treatment effect of 1-year trastuzumab compared with observation following completion of all adjuvant chemotherapy; this appears to be in contrast with a subset analysis of the NCCTG 9831 trial suggesting a lack of bene¿t in the IHC 2+/FISH + subpopulation. No. of No. (%) of 3-year DFS % Hazard ratio patients* DFS events (95% CI) (95% CI) Local IHC 3+/no central FISH assessment 1 year Trastuzumab 1075 144 (13.3%) 78.7 (74.4, 82.8) 0.64 (0.52, 0.79) Observation 1112 221 (19.9%) 74.6 (71.4, 77.8) Local IHC 3+/central FISH + 1 year Trastuzumab 376 48 (12.8%) 82.2 (77.3, 87.1) 0.78 (0.53, 1.14) Observation 358 56 (15.6%) 74.5 (67.5, 81.5) Local IHC 2+/central FISH + 1 year Trastuzumab 179 19 (10.6%) 83.0 (73.4, 92.7) 0.51 (0.29, 0.92) Observation 145 29 (89.4%) 74.0 (65.1, 82.9) * Not including 156 patients (73 trastuzumab, 83 observation) who do not meet the criteria for any of the above categories. Population/Treatment Abstracts – General Sessions 72 3-year follow-up of trastuzumab following adjuvant chemotherapy in node positive HER2-positive breast cancer patients: results of the PACS-04 trial. Spielmann M, Roché H, Humblet Y, Delozier T, Bourgeois H, Serin D, Romieu G, Canon JL, Monnier A, Piot G, Maerevoet M, Orfeuvre H, Extra JM, Hardy AC, Martin AL, Kramar A, Genève J. Inst Gustave Roussy, France; Inst Claudius Régaud, France; UCL St-Luc, Belgium; Centre François Baclesse, France; CHU Poitiers, France; Inst Ste Catherine, Avignon, France; Centre Val d’Aurelle, France; CH ND Reine Fabiola, Belgium; CHG Montbelliard, France; CMC les Ormeaux, Le Havre, France; Clinique St Pierre, Ottignies, Belgium; CH Bourg en Bresse, France; Inst Curie, France; Cl Armoricaine St Brieuc, France; FNCLCC, France Background: Following the PACS 01 trial, this randomised, multicentre, phase III trial was designed to evaluate the bene¿t of concomitant docetaxel (D) and epirubicin (E) versus anthracyclines, and the sequential use of Trastuzumab (T) in the adjuvant treatment of node-positive (N+) early breast cancer (EBC). Method: Women aged ≤65 years (yr) with N+ EBC were randomised initially to receive Arm A: 6 cycles (cy) of adjuvant 5-Àuorouracilepirubicin-cyclophosphamide (FEC100: F and C 500 mg/m2, E 100 mg/m2), or Arm B: 6 cy of concomitant ED (E and D 75 mg/m2) every 3 weeks. Radiotherapy (RT) was performed after chemotherapy and Hormonal therapy was prescribed to patients (pts) with hormonereceptor-positive tumours. As soon as HER2 status was available, pts with HER2+ (IHC3+ or IHC2+/FISH+) tumours were randomised to Arm C: observation only, or Arm D: 1 yr of T (8 mg/kg loading dose, 6 mg/kg 3qw). T was started after completion of RT for pts with normal cardiac function. The primary endpoint was 3-yr DFS for C and D arms. All survival times were calculated from ¿rst randomisation. To ensure a minimal power of 80% with a one sided α=5% (HR=0.625), 520 pts were to be randomized to Arm C or D and 118 events were to be observed. Assuming a 20% HER2+ sub-population and a 10% drop-out rate before ¿rst T administration, it was estimated that a whole population of 3000 pts were to be recruited. Results: 3010 pts (Arm A: n=1515, Arm B: n=1495), were randomized between 02/2001 and 08/2004. 528 HER2+ pts (18%) were randomised to Arm C (n=268) or Arm D (n=260). Baseline demographic and disease characteristics were well balanced between arms A and B as well as between C and D. 96% pts received 6 chemotherapy cy in arms A and B. 10% of pts in arm D did not receive T and 82% of the 233 pts in this Arm received T for more than 9 m, with a median cumulative dose of 109 mg/kg. Overall, 400 ¿rst events have been observed after a median follow-up of 36 months(m), but data are not mature for a comparative analysis between arms A and B. As of 30 April 2007, after a median follow-up of 40.5 m, 115 ¿rst events have been observed in HER2+ pts (18 locoregional relapses, 88 metastasis, 7 controlateral breast cancers, and 2 deaths) and the overall 3-yr DFS rate was 78%. Final ef¿cacy and safety analysis will be presented for HER2+ pts. Conclusion: This study will determine the potential benefit of combining ED in pts with N+ EBC and adding sequential T to FEC100 or ED75 in pts with HER2+ disease. 73 Safety of pertuzumab plus trastuzumab in a phase II trial of patients with HER2-overexpressing metastatic breast cancer which had progressed during trastuzumab therapy. Fumoleau P, Wardley A, Miles D, Verma S, Gelmon K, Cameron D, Gianni L, Conte PF, Ross G, McNally V, Baselga J. Centre GeorgesFrancois-Leclerc, Dijon, France; Christie Hospital, Manchester, United Kingdom; Mount Vernon Cancer Centre, Middlesex, United Kingdom; Ottawa Regional Cancer Center, Ottawa, ON, Canada; British Columbia Cancer Agency, Vancouver, BC, Canada; Western General Hospital, Edinburgh, United Kingdom; Oncologia Medica, Milano, Italy; Divisione di Oncologia Medica, Modena, Italy; Roche Products Limited, Welwyn, United Kingdom; Vall d’Hebron University Hospital, Barcelona, Spain Background: Pertuzumab (P) is a humanized MAb, the ¿rst of a new class of HER dimerization inhibitors (HDI), that binds to HER2 S19 blocking HER2 homodimerization as well as heterodimerization between HER2 and other HER receptors, targeting multiple HER pathways. In contrast, trastuzumab (Herceptin®, H) binds to the juxta-membrane epitope preventing both HER2 signal transduction and shedding of the extracellular domain of the receptor. Xenograft studies suggest that the complementary mechanisms of action of P&T could lead to increased ef¿cacy when combined. An understanding of the adverse event (AE) pro¿le of this combination, particularly cardiac, is of importance. Methods: Pts with measurable, centrally tested HER2-overexpressing metastatic breast cancer (MBC) who had received 3 prior lines of therapy (including adjuvant therapy), who had progressed during H as most recent treatment, with a baseline left ventricular ejection fraction (LVEF) 55% without decline to <50% during prior H treatment, were eligible for this single-arm, two-stage trial. Consenting patients receive H at 2 mg/kg qw (4 mg/kg loading dose [LD]) or 6 mg/kg q3w (8 mg/kg LD) plus P at 420 mg q3w (840 mg LD) starting within 9 weeks of the last dose of H. LVEF is assessed regularly in all pts. Results: By end-April 2007, 42 pts had received 1 dose of therapy and 33 had 1 tumor evaluation while on treatment. Activity in these 33 pts was: CR 1 (3%); PR 5 (15%); SD 6 months 7 (21%); SD <6 months 10 (30%); PD 10 (30%). Of 42 pts evaluable for safety, 34 had 1 AE. Frequent AEs (>10%) included: diarrhea (57%), nausea/vomiting (33%), fatigue (31%), rash (28%), muscle spasms (17%), cough (14%), headache (12%), dyspnea (12%), nasopharyngitis (12%). Over 80% of these AEs were grade 1 or 2. Five pts had an AE grade 3, including diarrhea (n=1), rash (n=1), and deep vein thrombosis (n=1); only diarrhea was considered treatment related (the rash was attributed to CT contrast medium). 64.3% of pts had received prior anthracycline. One pt experienced the protocol-de¿ned AE of fall in LVEF of 10% to <50%; this pt remained asymptomatic and was withdrawn from the study for PD. Discussion: The combination of P&H is active and well tolerated in HER2-positive MBC patients who had progressed during prior H therapy. AEs have been generally grade 1 or 2 and no patient has been withdrawn because of treatment-related AEs. Updated safety data will be presented at the meeting. Further studies on pts with either MBC or early breast cancer are planned. 74 Combination of QDE-paclitaxel and bevacizumab eradicates well-established tumors as well as lymphatic and pulmonary metastases in a MDA-MB-231 model of a highly metastatic human breast cancer. Ran S, Volk L, Bivens C, Trieu V, Desai N. Southern Illinois University, Spring¿eld, IL; Abraxis BioScience, Inc., Los Angeles, CA Background: Nab-paclitaxel (Abraxane®, ABX) is a 130-nm, albumin-bound paclitaxel that has shown greater anti-tumor ef¿cacy and a better safety pro¿le than solvent-based paclitaxel (Taxol®) and docetaxel (Taxotere®) in xenograft models and clinical trials. The goal of the present study was to determine the effects of nab-paclitaxel and bevacizumab (Avastin®, AVA), as a single or combined therapy, on the rate and metastasis of the large orthotopic tumors of MDA-MB-231 modeling a highly metastatic human breast cancer. Material and Methods: Luciferase-tagged MDA-MB-231 cells were implanted orthotopically into the mammary fatpad of female SCID mice and allowed to reach 460 mm3 in size before treatment. A group of 6-8 mice were treated with two cycles of ABX (30 mg/kg, qdx5, MTD) followed by injection of AVA(4 mg/kg) twice a week for 10 weeks. Additional groups received ABX or AVA alone or saline. Mice were monitored for tumor growth and signs of toxicity, and sacri¿ced when the tumor volume reached 2000 mm3. Luciferase activity was measured in extracts from proximal and contralateral lymph nodes and both lobes of lungs. Results: ABX-treated mice did not gain weight for the duration of the treatment (3 weeks) but no additional signs of toxicity were observed in that or other experimental groups. AVA-treated mice had nearly identical tumor growth rate as the controls indicating lack of the effect of this drug given alone. On day 37 after last treatment the tumor volume in the ABX-treated group showed a TGI of 84% (P<0.0001 vs. saline). However, all tumors regrew and reached the same volume as controls S20 Abstracts – General Sessions 45 days after reaching their minimal size. In contrast, 100% mice treated with ABX plus AVA therapy had signi¿cant tumor inhibition (TGI 94% on day 37, P<0.0001 vs. saline and ABX alone) and complete regression of tumors (TGI 100%, P<0.0001 vs. saline and ABX alone) by day 48 after last injection. Tumors did not regrow for the combination treatment and the study was terminated on day 75. Neither ABX nor AVA alone inhibited metastasis as compared with control mice with 100% mice (7/7 for ABX and 6/6 for AVA alone) being positive for lymph node and pulmonary metastasis. In contrast, 100% mice (6/6) treated with the combination were metastasis-free in either proximal or contralateral lymph nodes as well as in lungs. Discussion: Bevacizumab alone did not suppress well-established tumors or metastasis. Nab-paclitaxel alone showed a TGI of 84%; however, tumors re-grew in 100% of the mice. Neither drug alone was able to reduce the incidence or total metastatic burden in lymph nodes or lungs. In contrast, nab-paclitaxel plus bevacizumab successfully eradicated the primary tumors (TGI 100%) as well as lymph node and pulmonary metastasis in 100% of the treated mice for the duration of experiment. Nab-paclitaxel and bevacizumab combination is highly effective in treatment of primary tumors as well as distant metastases in an aggressive breast cancer model. 75 ErbB-2 inhibition activates notch-1 and sensitizes breast cancer cells to a gamma-secretase inhibitor: opportunity for a novel therapeutic combination. Osipo C, Patel P, Hao L, Whitehouse L, Strack P, Golde T, Albain K, Miele L. Loyola University Medical Center, Maywood, IL; Merck Research Laboratories, Boston, MA; Mayo Clinic, The Mayo Clinic College of Medicine, Jacksonville, FL BACKGROUND: ErbB-2 is ampli¿ed or overexpressed in aggressive breast tumors-associated with the poorest overall survival. Notch-1 is a potent cell fate determinant and oncogene that is also overexpressed with its ligand Jagged-1 in aggressive breast cancers. Notch signaling is important for survival and proliferation of breast tumor initiating cells. ErbB-2 positive tumors are treated with trastuzumab plus chemotherapy. Unfortunately, trastuzumab resistance is common and recurrence inevitable. Therefore, we investigated whether a novel crosstalk between ErbB-2 and Notch-1 contributes to resistance. MATERIALS AND METHODS: SKBr3, BT474, and stably transfected lines, MCF-7/Neo and MCF-7/HER2-18, cells were used in the studies. Notch transcriptional activity was measured using a pGL2CBF-1-Luc reporter construct. Expression of PY-ErbB-2, total ErbB-2, Notch-1, Notch-1 targets: Hes5, Hey1, Hes1 was detected by Western blotting. Cellular localization of Notch-1, Jagged-1, and Dynamin 2 was measured using confocal microscopy. Cell surface localization of Notch-1 and Jagged-1 was measured by biotinylating surface proteins at 4oC, immunoprecipitation and Western blotting. Activity of gammasecretase was measured using a ligand-independent cleavage assay. Cell proliferation was measured using DNA content. Early apoptosis was detected by Annexin V staining. RESULTS: MCF-7/HER2-18 cells have 5-fold lower Notch transcriptional activity than MCF-7/Neo cells. Conversely, either trastuzumab or a dual EGFR/ErbB-2 tyrosine kinase inhibitor (TKI) increased Notch transcriptional activity by 2-6-fold in ErbB-2 positive breast cancer cells. Trastuzumab increased amount and nuclear accumulation of active intracellular Notch-1 (Notch1IC) and Notch target proteins, Hes5, Hey1, and Hes1. Trastuzumab polarized the localization of both Notch-1 and ligand Jagged-1 near the cell surface. This surface accumulation was abrogated by inhibiting endosomal transport with a dominant negative Dynamin 2 (K44A). In addition, trastuzumab increased the interaction between Notch-1 and presenilin-1 and increased the proteolytic activity of g-secretase, which was inhibited by a inhibitor (GSI). Cell proliferation of SKBr3 or MCF-7/HER2-18 cells was inhibited more effectively in response to trastuzumab plus a GSI than by either agent alone. Similar results were observed with a dual EGFR/ErbB-2 TKI. CONCLUSIONS: Inhibition of ErbB-2 by trastuzumab or a TKI reactivates Notch-1, a potent breast oncogene, by at least two mechanisms: 1) Increasing the availability of Notch-1 and Jagged-1 at the cell surface through a Dynamin 2-dependent process and 2) Increasing g-secretase activity. These results suggest that trastuzumab- or TKI-GSI combinations may be effective in ErbB-2 positive tumors and may delay or prevent the onset of resistance. 76 Parity regulates activation of p53 in human breast tissue. Crisi GM, Mathews L, Bentley B, Stueber K, Jerry DJ, Smith-Schneider S. Baystate Medical Center/Tufts University School of Medicine, Spring¿eld, MA; Pioneer Valley Life Sciences Institute, Spring¿eld, MA; Baystate Medical Center/Baystate Plastic Surgery Associates, Spring¿eld, MA Early parity (≤ age 24) is associated with a signi¿cant reduction in breast cancer risk. Studies in rodents have suggested that p53 becomes more sensitive to DNA damage after pregnancy. Furthermore, mice lacking p53 are unable to mount a protective response to chemical carcinogens after undergoing parity, proving that p53 actively participates in this response. We hypothesized that women who had an early full term pregnancy (EP) would have increased levels of p53 as compared to nulliparous women (NU), or from women who had a later pregnancy (LP). Materials and Methods: Women undergoing elective breast reduction surgery were asked to voluntarily enroll in an IRB sanctioned study. A pre-operative questionnaire was administered to obtain pertinent information: onset of menses, last menses, parity, age at ¿rst pregnancy, family history of breast cancer. Two 500 mg portions of tissue were cultured on gelatin sponges for 24 hours in a 37º incubator. Cultures were then exposed to ionizing radiation (5 Gy), and re-incubated for 6 hours. Duplicate control cultures remained unirradiated. The tissues were formalin ¿xed and paraf¿n-embedded. Immunohistochemical (IHC) staining was performed using a polyclonal antibody to p53 (DO7) (1:400). Semiquantitative immunoreactivity for p53 in epithelial cells was scored as follows: percentage of cells staining: none (N), 1 = less than 10%, 2 = 10-50%, 3 = greater than 50%; intensity of cell staining: 0 = none, 1+ = weak, 2+ = moderate, 3+ = strong. Differences in p53 scores between each patient’s non-irradiated and irradiated tissue, were calculated and reported. Results: A total of 42 patients have been enrolled, 11 nulliparous (NU), 24 with a ¿rst pregnancy before age of 25 years (early parity - EP), 7 with a ¿rst pregnancy at age greater than 26 years (late parity –LP). A signi¿cant increase in percentage of cells staining positive for p53 was observed in EP patients (50%) when compared to NU patients (23%) (p-value = 0.004). LP patients demonstrated 37% of cells staining positive for p53; this was not statistically signi¿cant when compared to either NU or EP. Conclusion: We demonstrate for the first time that, as in rodent models, an increase in responsiveness of p53 is seen in cultured human mammary tissue from women who had a full term pregnancy at an early age. Our ¿ndings demonstrate that, like in mice, parity enhances the responsiveness of p53, implying that p53 confers protection to women who have an early full term pregnancy, and thus puts them at a lesser risk for the development of breast cancer. Abstracts – General Sessions 77 Cytochrome P450 2D6 activity predicts adherence to tamoxifen therapy. Rae JM, Sikora MJ, Henry NL, Li L, Kim S, Oesterreich S, Skaar T, Nguyen AT, Desta Z, for the COBRA Investigators. University of Michigan Comprehensive Cancer Center, University of Michigan School of Medicine, Indiana University, Baylor College of Medicine, Johns Hopkins University School of Medicine, COBRA is the Consortium on Breast Cancer Pharmacogenomics, an NIH supported Consortium of investigators at these institutions studying pharmacogenomics in the treatment of breast cancer Background: The selective estrogen receptor modulator tamoxifen has been shown to reduce mortality in estrogen receptor positive breast cancer and to reduce the incidence of the disease in high-risk women. The metabolism of tamoxifen to its active metabolite, endoxifen, by cytochrome P450 2D6 (CYP2D6) is believed to be required for antitumor activity. Previously, we showed that patients with CYP2D6 polymorphisms had lower response rates and less hot Àashes while on tamoxifen than patients with wild-type CYP2D6 genotype. Studies of adherence to tamoxifen therapy suggest that nearly one third of breast cancer patients stop taking their medication before the recommended 5 years. Side effects including hot Àashes are the main causes of treatment discontinuation. In the current study, we tested the hypothesis that CYP2D6 genotype is predictive of non-adherence to tamoxifen. Methods: Women with breast cancer (n=297) enrolled in a prospective clinical trial testing associations between genetic polymorphisms and clinical response were genotyped for CYP2D6, CYP2C19, CYP3A5 and estrogen receptor (ESR) variants. Using genotype information, patients were assigned a CYP2D6 “score” based on known speci¿c allele activities from 0 (no activity) to 2 (high activity). Results: Twenty eight patients (10.5%) stopped taking tamoxifen during the ¿rst year of treatment due to side effects. All women with a CYP2D6 score of 0 completed tamoxifen treatment, while increasing scores correlated with increasing rates of drop out. Linear regression and a nonlinear Michaelis-Menten Model both describe a strong correlation between increasing CYP2D6 score and drop out rates (R2 = 0.75, p = 0.057 and R2 = 0.935, p = 0.018, respectively). Polymorphisms in other CYP450s or ERs did not correlate with adherence. Conclusions: The presence of active CYP2D6 alleles predicts a higher likelihood of tamoxifen discontinuation due to treatment related side effects. These data may explain part of the current controversy over CYP2D6 genotype predicting response to tamoxifen and suggest that patients most likely to bene¿t from tamoxifen are paradoxically most likely to stop their tamoxifen therapy prematurely. Genetic testing to identify patients likely not to comply with tamoxifen therapy could help identify patients a priori who will bene¿t most from the effective use of co-medications that ameliorate the side effects of tamoxifen and could signi¿cantly impact response to therapy. This knowledge may provide an ef¿cient means of improving tamoxifen ef¿cacy relative to other treatments. 78 Preliminary results of the UK Taxotere as Adjuvant Chemotherapy (TACT) Trial. Ellis PA, Barrett-Lee PJ, Bloom¿eld D, Cameron DA, Hall E, Johnson L, Johnston SRD, Bliss JM. Guys, Kings & St Thomas’s Hospital, London, United Kingdom; Velindre Hospital, Cardiff, Wales, United Kingdom; Royal Sussex County Hospital, Brigton, Sussex, United Kingdom; University of Leeds, Leeds, United Kingdom; Institute of Cancer Research, Sutton, Surrey, United Kingdom; Royal Marsden NHS Foundation Trust, London, United Kingdom Introduction: Previously reported phase III adjuvant chemotherapy trials suggest a modest survival bene¿t favoring taxane containing regimens over anthracycline regimens. However, uncertainty remains with regard to the bene¿t of taxanes compared with anthracycline regimens of similar duration. The UK TACT Trial, a large multicentre phase III randomised trial comparing sequential FEC-Taxotere to standard UK anthracycline chemotherapy, will provide further evidence with regard to overall bene¿t, as well as which sub-groups, if any, have more or less to gain from this intervention. S21 Patients & Methods: Between Feb 2001 and July 2003 4162 women with operable histologically con¿rmed completely resected early invasive breast cancer were recruited from 104 centres in the UK (103) and Belgium (1). Centres chose FEC (600/60/600 mg/m2 q3wk x 8) or E-CMF (Epirubicin 100mg/m2 q3wk x 4 → CMF 100mg/m2 PO d1-14 or 600mg/m2 IV d1&8 /40/600 mg/m2 q4wk x 4) as their control arm, reÀecting standard UK practice. Pts were randomised to FEC-T (FEC q3wk x 4 → T 100 mg/m2 q3wk x 4) or control. 2523 patients were from centres using FEC (FEC=1265: FEC-T=1258) and 1639 from centres using E-CMF (E-CMF=824; FEC-T=815) as their chosen control arm. Tumor blocks were collected prospectively for central HER2 testing and creation of tumor microarrays. The primary endpoint was diseasefree survival (DFS) de¿ned as time to loco-regional or distant relapse, contralateral invasive breast cancer or death prior to relapse. Secondary endpoints included overall survival (OS), tolerability of regimens and quality of life. TACT has 80% power to detect a clinically meaningful 4% difference in DFS (from 71% to 75% at 5 yrs). Survival estimates will be compared using strati¿ed log-rank tests and Cox regression. Results: At May 1 2007, median follow up is 50 mths (interquartile range: 45-59). 954 DFS events were reported, exceeding the threshold set by the independent Data Monitoring & Ethics Committee for analysis for presentation. Centrally con¿rmed HER2 status is available for 3565 (83%) pts; assessment of other biomarkers for taxane responsiveness is ongoing. Data to be presented, by treatment group, are DFS, OS and planned subgroup analyses by ER and HER2 status. Discussion: TACT will provide further data to inform the use of adjuvant taxanes in early breast cancer. Subgroup analyses will allow further exploration of the potential interaction with ER and HER2. 79 Evaluating the ef¿cacy of capecitabine given concomitantly or in sequence to epirubicin/cyclophosphamide → docetaxel as neoadjuvant treatment for primary breast cancer. First ef¿cacy analysis of the GBG/AGO intergroup-study “GeparQuattro”. von Minckwitz G, Rezai M, Loibl S, Fasching P, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Mehta K, Untch M. University Hospital Frankfurt, Frankfurt, Germany; German Breast Group, NeuIsenburg, Germany; Senologie, Brustzentrum, Düsseldorf, Germany; Frauenklinik mit Poliklinik, Erlangen, Germany; Senologiezentrum Ostschweiz SENZO, St. Gallen, Switzerland; Onkologie Bethanien, Frankfurt, Germany; Frauenklinik, München, Germany; Frauenklinik, Hannover, Germany; Frauenklinik, Berlin, Germany Background: Integration of new cytotoxic agents is possible by either simultaneous or sequential addition to established regimens. Direct comparison of these strategies is usually biased by differences in treatment duration. A three-arm neoadjuvant study was designed to address this question by adding capecitabine (X) to docetaxel (D) after pretreatment with epirubicin/cyclophosphamide (EC). Patients (Pts) and methods: Pts were eligible in whom adjuvant chemotherapy would be considered otherwise. Therefore, either large operable (T3) and locally advanced (T4), or estrogen (ER) and progesterone (PR) negative receptor status, or ER/PR positive tumors but clinically node-positive disease were recruited in 115 German centers to receive 4 cycles of EC (90mg/m2 / 600mg/m2) and to be than randomized to either 4 cycles of D (100mg/m2) or 4 cycles of DX (75mg/m2 / 1800mg/m2) or 4 cycles of D (75mg/m2) followed by 4 cycles of X (1800mg/m2) (D→X). Pts with HER-2 positive tumors received trastuzumab concomitantly with all regimens. The primary endpoint was pathologic complete response (pCR) at surgery. The coprimary objectives were to assess the effect of X by comparing EC→ D vs. EC→DX + EC→D→X (effect of X) and to assess the effect of time (24 vs 36 weeks) by comparing EC→D + EC→DX vs EC→Doc→ X. The trial was designed to detect an increase in pCR from 17% to 23.5% (OR 1.5) for each comparison. Results: Between 08/05 and 12/06 1512 pts entered and after receiving 4 cycles EC, 1421 pts were randomized to D (N=471), DX (N=471), and D→X (N=479). Complete response (N=102, 7.2%), partial response (N=917; 64.5%), and no change (N=402; 28.3%) after 4xEC was used to stratify randomization. Further strati¿cation factors were extent of disease (1202 [84.6%] operable, 219 [15.4%] locally advanced), ER/ S22 Abstracts – General Sessions PR status (523 [36.8%] ER and PR negative, 898 [63.2%] ER and/or PR positive), and HER2 status (434 [30.5%] positive, 979 [68.9%] negative, 8 not measurable). Surgery is planned for the last pt at the end of August 2007. Conclusions: Results of the primary endpoint from this ¿rst mature, randomized trial evaluating capecitabine as treatment for primary breast cancer will elucidate which strategy appears to be superior. 80 Characterizing the biology and response of locally advanced breast cancer in women undergoing neoadjuvant therapy: preliminary results from the I-SPY trial. Hylton N, Carey L, DeMichele A, Blume J, Broadwater G, Madhavan S, Rosen M, George S, Esserman L, ISPY Clinical, Research, Pathology and Radiology Investigators. Univ of California San Francisco, San Francisco, CA; Univ of North Carolina, Chapel Hill, Chapel Hill, NC; Univ of Pennsylvania, Philadelphia, PA; ACRIN, Philadelphia, PA; CALGB, Chapel Hill, NC; NCI-SPORE, Bethesda, MD Background: The I-SPY Trial is a multi-institutional study of locally advanced breast cancer integrating serial biopsy and MRI to measure response of tumors to neoadjuvant chemotherapy. The primary objective is to identify surrogate markers of response to neoadjuvant chemotherapy that are predictive of pathologic remission and survival in women with stage II/III breast cancer. Methods: Eligible patients had histologically-con¿rmed primary breast cancer measuring at least 3 cm within the breast following diagnostic biopsy. Required initial treatment was an anthracycline (AC)-based neoadjuvant chemotherapy regimen: AC followed by T (91%); ACbased regimen without T (6%);chemotherapy beyond AC +/- T (2%). Surgical treatment was individualized based upon response, surgeon, and patient preference. Serial MRI and core biopsies were performed at baseline (T1), after one cycle of AC (T2), intra-regimen (T3) and pre-surgery (T4) to identify markers of tumor response. Patients were accrued at nine institutions from 2002-2006. Results: 222 patients were available for analysis as of 4/17/07. The median patient age was 49 years, with a range of 27-69. The distribution by age was 20%, 35%, 36%, and 10% for women < 40, 41-50, 51-60, 61-70. The racial distribution was 74% Caucasian, 19% African-American, 4% Asian, and 3% other. Median tumor size was 6 cm (0-25 cm); 70% had clinically positive nodes. Distribution by grade was 22% low, 38% intermediate, and 39% high. 54% were ER positive and 28% had Her-2/neu overexpression. Clinical complete response (CR) rates (46%) were higher than pathologic CR (35%). pCR rate in Her2/neu+ patients was double that of Her2/neu- (51% vs. 25%). MRI demonstrated residual disease in 27% compared to 15% with clinical residual disease. Prede¿ned morphologic MRI patterns have been assessed in 219 patients. More patients had mutlinodular or diffuse disease (54%) than solitary masses (46%). Distribution by phenotype showed: single unicentric mass with well-de¿ned margins (16%), multilobulated but well-de¿ned mass (30%); multifocal (30%); diffuse(14%), and septal pattern (8%). As we continue to explore and dissect the heterogeneity of this disease, we will be aided by the analysis of baseline biomarkers collected, including 120 Agilent expression arrays; 159 cDNA microarrays, 59 BAC CGH arrays, 126 MIP arrays, 195 reverse phase protein lysate arrays and 195 IHC assays to date. Conclusion: The I SPY Trial is a rich repository to study breast cancer biology and therapeutic response that will enable more effective therapy for non-responders in the future. 81 Elucidating the stem and progenitor cell hierarchy in breast development and cancer – an essential role for GATA-3. Lindeman GJ, Asselin-Labat M-L, Sutherland KD, Barker H, Thomas R, Shackleton M, Hartley L, Robb L, Grosveld FG, van der Wees J, Visvader JE. The Walter and Eliza Hall Institute of Medical Research, Melbourne, Australia; The Royal Melbourne Hospital, Melbourne, Australia; Erasmus University, Rotterdam, Netherlands Background: We have previously isolated discrete populations of mouse mammary cells on the basis of cell-surface markers and de¿ned a population that expresses ‘basal’ markers and is highly enriched for mammary stem cells. Expanded stem cell numbers were noted in the pre-neoplastic phase in the MMTV-wnt-1 mammary tumor model, consistent with tumors originating in stem cells in this model. Interestingly, the stem cell-enriched basal population was ‘triple negative’ for ER, PR and ErbB2. This phenotype is reminiscent of human basal tumors, suggesting that the mammary stem cell is the ‘cell of origin’ for this poor prognosis subset. Methods & Results: We now report that the luminal cell population can be further subdivided on the basis of CD61 (β3-integrin) expression. The CD61-positive subset contained luminal progenitors, as de¿ned by 2D and 3D colony formation assays. Intriguingly, the CD61+ luminal progenitor was the earliest cell-type to express ER, with approximately 5% of progenitor cells expressing ER compared to 40% of mature luminal (CD61-) cells. Since the GATA-3 transcription factor is a key marker of ‘luminal’ breast tumors, we next studied its role in normal mammary gland development. A gradient of expression was noted within the epithelial hierarchy, with low levels in the stem cell-enriched population and high levels in differentiated luminal cells. Utilising knockout mice, Gata-3 was found to be essential for mammary gland morphogenesis in both the embryo and adult. Gata-3 de¿ciency resulted in an expansion of CD61+ luminal progenitors and a concomitant block in differentiation in both nulliparous and pregnant mice. Remarkably, introduction of Gata-3 into the stem cell-enriched population was suf¿cient to induce maturation along the alveolar luminal lineage. Discussion: Our studies provide evidence for the existence of an epithelial hierarchy within the mammary gland and establish GATA-3 as a critical regulator of luminal cell differentiation. These ¿ndings suggest that high expression of GATA-3 in luminal breast tumors confer a favorable prognosis due to the promotion of differentiation, while GATA-3 loss likely results in a more clinically aggressive phenotype. 82 Decrease in tumorigenic breast cancer stem cells in primary breast cancers with neoadjuvant lapatinib. Li X, Creighton C, Wong H, Hilsenbeck SG, Osborne CK, Rosen JM, Lewis MT, Chang JC. Dan L Duncan Cancer Center at Baylor College of Medicine, Houston, TX Background: Previously, we have shown that tumorigenic breast cancer cells (CD44+/CD24-/low) were resistant to conventional chemotherapy. Residual cancers showed an increase in tumorigenic CD44+/CD24-/low cells, enhanced tumor-initiation by mammosphere (MS) formation, and increased new tumor formation by xenograft transplantation assays. Molecular pathways like EGFR/HER2 have been shown to be aberrant in CSCs. Methods: We performed a neoadjuvant clinical trial in 30 patients with locally advanced HER-2 overexpressing breast cancers who received lapatinib (EGFR/HER2 tyrosine kinase inhibitor) given initially as a single agent for the ¿rst 6 weeks, followed by a combination of weekly trastuzumab and 3-weekly docetaxel for 12 weeks before primary surgery. Pathologic response in the surgical specimens after neoadjuvant therapy was assessed. Sequential core biopsies of the primary cancers were taken in patients at time of diagnosis and after week 6 of lapatinib, and assessed for tumorigenic CD44+/CD24-/low cells by Àow cytometry, and MS formation. Global gene expression differences between cancer cells bearing CD44+/ CD24-/low cells and all other sorted cells, and between cancer MS and the primary bulk invasive cancers were analyzed. Results Signi¿cant tumor regression in the product of bidimensional tumor measurements with a median decrease of –60.8% (range 0, -86.5%, p=0.001) was observed in primary tumors after only 6 weeks of single agent lapatinib. Unlike with chemotherapy, lapatinib treatment decreased tumorigenic CD44+/CD24-/low breast cancer cells from 10.6% to 4.7%, and also reduced self-renewal capacity measured by MS assays (30 to 15 MS/10,000 cells, p=0.01). The pathologic complete response rate after lapatinib and trastuzumab/docetaxel was much higher than expected, at 63%(16/25). The gene transcription pathways that underlie chemoresistant, MS-forming CD44+/CD24-/low cells involve genes belonging to stem cell self-renewal, Notch (Jagged-2, Hes1, Lunatic fringe, mastermind-like 2), Hedghog (Cyclin B1, CDC2), and Wnt pathways, FOXP1, growth factor/PI3K/AKT signaling (AKT3, BCL2, CTNNB1, FGFR2, FOXO1A, FOXO3A, PIK3R1, PTEN), and early development pathways (JARID2, JMJD2C, and MBNL1), regardless of HER2 expression in the primary tumor. Conclusion Contrary to Abstracts – General Sessions conventional chemotherapy, human breast cancer specimens obtained from this prospective in vivo study has demonstrated for the ¿rst time, that lapatinib decreases tumorigenic breast cancer stem cells in the primary breast cancers of women receiving neoadjuvant treatment. This data suggests that speci¿c signaling inhibitors of the pathways responsible for stem cell self-renewal could provide a therapeutic strategy for eliminating tumorigenic cells in order to achieve long-term eradication of cancer. S23 S24 Abstracts – Poster Discussion Sessions 101 Serial detection and characterization of circulating tumor cells in an animal model. Eliane JP, Luker KE, Brown M, Repollet M, Doyle GV, Hayes DF, Luker GD. University of Michigan Medical School; Immunicon Corporation, Huntingdon Valley, PA Introduction: The ability to serially monitor tumor response in animal models in the preclinical phase of drug development could substantially advance translational studies. Recent publications have shown that circulating tumor cells (CTC) measured at any point during treatment of metastatic breast, colorectal, or prostate cancer patients indicate therapeutic bene¿t. Patients with elevated CTC have shorter progression free survival and overall survival than those with low levels. The objectives of this project were to ¿rst adapt an existing automated human CTC assay system for use in mice and then to optimize the performance of the murine / CTC model as a tool for drug development. Materials and methods: Spike-in models: using ∼170 µL of normal mouse blood spiked with 100-5000 cultured breast cancer cells were used to establish assay precision. 0.5 - 1 x 106 tumor cells from breast cancer cell lines (MDA-MB-231, MCF7-FGF, SUM-159) or primary cells from clinical breast cancer biopsies were used to established an orthotopic xenograft in SCID NOD mice. The FDA cleared immunomagnetic/immunoÀuorescence based automated CellTracks™ system (Immunicon Corporation) was used to isolate and enumerate CTC in 75-100 µl blood samples from serial direct cardiac puncture (26 gauge needle) of living mice. Normal SCID NOD mice functioned as controls GFP transfected cell lines used to inoculate mice functioned as an independent identi¿er for CTC in addition to the cytokeratin cocktail used in the standard assay. Post-mortems were performed when possible and results were correlated with site of mets, extent of disease and CTC levels. Results: Blood from controls as well as xenograft animals contained background epithelial cells when blood was drawn from the retroorbital site. No contaminating epithelial cells were found in specimens when tail vein, direct cardiac or jugular venepuncture methods were performed. As anticipated, GFP was visible in enriched stably transduced MDA-MB-231 cells con¿rming that CTC were derived from human tumor xenografts. Mice bearing MDA-MB-231 or MCF-7-FGF xenografts had detectable CTC as early as 7 days after implanting cells, approximately 5 weeks before tumors became palpable. All animals with detectable orthotopic tumors had CTC (n = 11). Conclusion: Using an automated system, CTC can be accurately and reproducible isolated and enumerated from volumes as low as 50 µl of mouse blood. CTC represent a non-invasive real-time method of serially monitoring tumor activity in animal systems. They are also an effective means of optimizing a murine model of metastasis by identifying the most effective cell line, inoculum site, timing and method of phlebotomy. Most importantly, this system can be used in pre-clinical and clinical studies and ultimately translated into actual use in the clinical setting as currently cleared by the FDA. 102 A new system for enrichment and detection of circulating tumor cells in the peripheral blood of patients with metastatic breast cancer. Deng G, Burgess D, Manna E, Krag D, Herrler M. Applied Imaging Corp., San Jose, CA; University of Vermont, College of Medicine, VT Background: Circulating tumor cells (CTCs) may offer to meet an existing medical need to monitor cancer patients during a course of treatment and for helping to determine recurrent disease. Currently, neither imaging nor blood tests meet the needs of the oncologist treating the cancer patient in respect of sensitivity, speci¿city and time to results. Beside the importance to understand the role of CTCs in the metastatic process, CTCs might also be useful as biomarkers in the design of clinical trials and to evaluate new potential drug candidates. Relatively successful approaches for CTC enrichment and detection are based on binding to anti-EpCAM antibodies. However, some tumor cells are lacking or have low expression of EpCAM. Materials and Methods: Here we report a new, highly sensitive and reproducible method for CTC enrichment and detection and have successfully applied it to metastatic breast cancer patient’s blood samples. Anti-cytokeratin alone or in combination with anti-EpCAM antibodies linked to microbeads is used for CTC enrichment. Fluorescence labeled anti-cytokeratin (CK), anti-CD45 and DAPI are used for CTC identi¿cation. Applied Imaging’s ARIOL® SL-50 was used for image capture and analysis of CTCs on standard microscope glass slides. Results: In a method comparison, 37 blood samples from metastatic breast cancer patients were processed with the CellSearch system and in parallel by our method. Our method recovered equivalent numbers of CTCs in the prognostically relevant range (≥5 CTCs) relative to the CellSearch™ assay; however, our method showed a signi¿cantly (p=0.04) higher detection rate in the low range (≥1 and ≤4 CTCs). The Ariol® system achieved an overall higher CTC detection rate (51% vs. 30%) and a wider dynamic range (1-571 vs. 1-270) than the CellSearch™ system. No CTCs were detected in blood samples from healthy individuals. Conclusion: Our assay is detecting anti-CK enriched tumor cells from breast cancer patient’s blood samples. Preliminary data indicate that enrichment with anti-EpCAM and anti-CK may enhance assay sensitivity. The ARIOL® system provides superior imaging quality by combining fluorescent and brightfield images. This allows discriminating between intact cells and cell fragments. 103 MagSweeper: an automated system for high ef¿ciency and speci¿city capture of live circulating tumor cells. Powell AA, Talasaz AAH, Mindrinos M, Carlson R, Pease FW, Davis RW, Jeffrey SS. Stanford University, Stanford, CA Our group has developed a novel automated robotic device that ef¿ciently isolates circulating tumor cells (CTCs) while removing all contaminating blood cells. Our device, the MagSweeper, uses powerful magnetic rods covered in removable plastic sleeves. These rods sweep through blood samples, capturing cancer cells labeled with antibodies linked to magnetic nanoparticles. Upon completion of the capturing protocol, the magnetic rods undergo several rounds of washing, thereby removing all contaminating blood cells. Finally, the cancer cells are released by removing the magnetic rods from the sleeves, causing the captured cells to be gently dislodged. We have tested our prototype using a buffered solution on patient blood spiked with MCF7 breast cancer cells labeled with Epithelial Cell Adhesion Molecule (EpCAM) antibodies and nanoparticles. In preliminary tests using buffer, our capture rates averaged 96%. Using patient blood we achieved capture rates up to 100%, without any contamination by blood cells. Additionally, cells captured by our device show no reduced viability when cultured after capture. The exceedingly high purity and capturing ef¿ciency of CTCs isolated by the MagSweeper will allow for a variety of genetic and growth assays to be preformed on these important and poorly understood cells. 104 Circulating tumor cells as a reliable assessment of treatment ef¿cacy in metastatic breast cancer. Liu MC, Shields P, Isaacs CJD, Warren R, Cohen P, Wilkinson M, Ottaviano Y, Zhang Y, Shen R, Jasti M, Gallagher A. Lombardi Cancer Center, Georgetown University Hospital, Washington, DC; Franklin Square Hospital, Baltimore, MD BackgroundThe enumeration of >5 CTC/7.5 mL (CTC, circulating tumor cells) has been associated with worse progression free survival (PFS) and overall survival (OS) in metastatic breast cancer (MBC), and the persistence of >5 CTC/7.5 mL appears to predict for treatment failure (NEJM 2004; 351:781. Clin Cancer Res 2006; 12:4218.). We are conducting a prospective clinical trial to validate the prognostic and predictive signi¿cance of this serum biomarker in MBC. Methods Serial CTC levels are obtained in patients starting a new systemic treatment regimen for progressive, radiographically measurable MBC. 10 mL of peripheral blood are collected before the start of treatment and then at 3-4 week intervals. All subjects are followed for OS and offered the opportunity to continue CTC testing upon disease progression. CTC enumeration is performed on a 7.5 mL blood volume using the Abstracts – Poster Discussion Sessions CellSearch™ technology (Veridex, LLC; Warren, NJ). Epithelial cells are immunomagnetically separated and Àuorescently labeled, and nucleated (DAPI+) cells with the EpCAM+, cytokeratin 8/18/19+, and CD45- phenotype are counted as CTC. Clinical outcomes are based on radiographic studies and physical examination in accordance with RECIST criteria. Results 54/100 subjects have been accrued to date with a median follow-up of 28 weeks. 41 subjects have completed at least one radiographic staging evaluation, with 120 pairs of concurrent CTC values and imaging assessments. Treatment at study entry for the 41 evaluable patients includes chemotherapy (34%), endocrine therapy (36%), and combination therapy with a biologic agent (30%). 98% of subjects (40/41) had >1 CTC/7.5 mL (range 1-311), and 89% (36/41) had >2 CTC/7.5 mL. Focusing on the pairs of CTC values and radiographic assessments (irrespective of subject), disease progression occurred in 33% of cases with <5 CTC/7.5 mL and 71% of cases with >5 CTC/7.5 mL (p<0.0001). When considering the correlation between CTC values and radiographic assessments from the same patient, >5 CTC/7.5 mL is associated with a 4.9-fold higher risk of disease progression (p=0.0003). Median PFS was 2.7 months and 4.9 months for subjects with >5 vs <5 CTC/7.5 mL at baseline, respectively (p=0.10). Discussion Reporting PFS on the basis of CTC assessments at baseline and/or ¿rst-follow-up is complex, as PFS estimates are arti¿cially bound by timing of the imaging studies. Correlating CTC levels with concurrent radiographic determinations of disease response should therefore provide a clearer determination of the signi¿cance of CTC relative to treatment ef¿cacy. Our preliminary analysis indicates that the odds of disease progression are 4.9 fold higher for patients with >5 vs <5 CTC/7.5 mL (p=0.0003). CTC levels may be useful as a surrogate marker for treatment ef¿cacy, and therefore provide a reliable means of assessing treatment response in the setting of radiographically nonmeasurable disease. 105 Disseminated tumor cells correlate with estrogen receptor positivity in operable breast cancer patients. Alvarado MD, Brissaud C, Scott J, Magbanua M, Moore D, Ewing CA, Hwang S, Esserman LJ, Park JW. University of California, San Francisco, San Francisco, CA Background: Disseminated tumor cells (DTC) in bone marrow (BM) and circulating tumor cells (CTC) in peripheral blood have both shown prognostic and/or predictive signi¿cance in early and advanced breast cancer, respectively. However, in early breast cancer DTC have typically been detected by nonquantitative IHC assays and CTC have been more dif¿cult to detect. We hypothesize that quantitative analysis of these cells may provide advantages in assessing impact on outcome. Methods: Patients (pts) with operable breast cancer had BM and blood sampled at the time of surgery. DTC/CTC were subjected to antiEpCAM immunomagnetic enrichment, followed by multiparameter Àow cytometry (FC). Primary tumor characteristics included tumor size, lymph node status, ER and Her-2-neu receptor status. Statistical analysis was performed using Cox proportional hazard models and chi square analysis. Results: 220 pts have been prospectively accrued with a median followup of 58 months. There have been only 22(10%) recurrences and 9(4%) deaths, a lower than predicted event rate in this contemporary treatment population. BM was sampled in 202 pts and blood in 208. A positive result for DTC was identi¿ed in 65% of pts. A positive result for CTC was identi¿ed in 39% of pts. For death, only LN status is signi¿cantly prognostic (p=0.043) to date. For recurrence, only tumor size is prognostic (p=0.019) to date. DTC or CTC are not yet signi¿cantly prognostic for outcome. DTC showed correlation with ER positivity (p=0.02). Conclusion: Simultaneous analysis of DTC and CTC is feasible in early breast cancer. These have not shown signi¿cant impact on outcome in this patient population and may be related to the unexpectedly low number of events to date. The presence of DTC appears to correlate with ER positivity, suggesting the delineation of a subgroup of ER+ pts at an increased risk of recurrence. However, longer follow-up is needed to ascertain this possibility, given the prolonged time for recurrence in the ER+ breast cancer patient. Relationship Between Tumor Characterisitcs and DTC All pts (n=202) BM+ pts (n=132) Tumor size cm (p=0.66) 0 to <1 62 37 1 to <2 94 61 2 to <4 46 27 >4 11 7 ER (p=0.002) pos 183 118 neg 18 14 Her2 (p=0.42) pos 41 26 neg 169 103 Grade (p=0.83) 1 82 49 2 79 49 3 56 34 Node status (p=0.68) pos 82 47 neg 120 85 Relationship Between Tumor Characteristics and CTC Total pts (n=208) CTC+ pts (n=81) Tumor size cm (p=0.26) 0 to <1 64 21 1 to <2 36 2 to <4 18 >=4 6 ER (p=0.13) pos 72 neg 9 Her2 (p=0.55) pos 13 neg 66 Grade (p=0.44) 1 36 2 24 3 21 Node status (p=0.56) pos 28 neg 53 S25 BM- pts (n=70) 25 27 15 3 50 19 10 55 29 24 17 27 43 CTC- pts (n=127) 43 54 27 3 102 24 24 97 46 47 34 49 78 106 Features of patients (pts) with metastatic breast cancer (mBC) and a circulating tumor cell count (CTCc) of 0. Bubis JA, Marsland TA, Justice KM, Edwards D. Integrated Community Oncology Network, Orange Park, FL Background: Circulating tumor cells (CTCs) can be measured in the peripheral blood of pts with breast cancer (BC). These cells likely play a role in the dissemination of disease and may be present prior to radiologic or clinical ¿ndings of metastatic disease. The Veridex CellSearch assay is the only FDA approved method for detecting these cells. A CTCc of 5 or greater per 7.5 mL of blood is predictive of a decreased progression free survival and decreased overall survival in pts with mBC. In pts receiving therapy, an increasing CTCc or a persistent CTCc of 5 or greater may indicate the need to consider changing therapies. While a CTCc of 0 is reassuring, some patients with a CTCc of 0 have clearly measurable and/or progressive disease. We have endeavored to review the characteristics of these patients. Materials & Methods: This is a single institution, IRB-approved, retrospective chart review. All CTCs were measuring in our laboratory using the Veridex CellSearch assay. Results: 24 pts were found to have a CTCc of 0 at various stages of therapy. Including repeat studies, the total number of time points studied with a CTCc of 0 = 48. CA27.29 correlates were obtained for 29/48. Average CA27.29 = 112.3 (range 15.0-807.2). Average age = 67 (range 34-89). 17 pts were postmenopausal. ER+ =14/24. HER2+=13/24. ER-/HER2- = 2. Stage IV at diagnosis = 3. Bone-only metastases = 4. Lung-only metastases = 1. Liver-only metastases = 3. Other sites (includes pleural effusion, chest wall, thyroid, mediastinum, pelvis, brain)= 9. Bone and visceral metastases = 5. 2 pts had CTCc of >5 and subsequently went to zero with continued evidence of persistent disease and rising CA27.29s. Discussion: CTCs can be a helpful test in predicting prognosis and response to ongoing therapy. However, we have demonstrated that a CTCc of 0 does not always correlate with the behavior of mBC. Our data indicates that pts with a CTCc of 0 may still have active, progressive disease; although the small number of patients prevents us from drawing statistical conclusions. This study is ongoing; further investigation of this patient population is indicated. Updated data will be available for presentation. S26 Abstracts – Poster Discussion Sessions 107 Bone marrow micrometastasis and circulating tumor cells are respectively strong prognostic factors in early and metastatic breast cancer, a comparative study on 759 patients. Bidard F-C, Vincent-Salomon A, Sastre X, Sigal-Zafrani B, Nos C, Mignot L, Dieras V, Asselah J, Thiery JP, Pierga J-Y. Institut Curie, Paris, France; IMCB Biopolis, Singapore, Singapore Background: Disseminated cancer cells are bone marrow micrometastasis (MM) and circulating tumor cells (CTC). Bone marrow MM has been reported to be a pronostic factor for both early and metastatic breast cancers. CTC have also a prognostic impact in the metastatic setting. With a highly speci¿c method for MM and CTC detection, we analyzed the pronostic impact of these disseminated tumors cells in stage I to III and in stage IV breast cancers. Material and Methods: From 11/98 to 11/04, cytospun Ficoll fractions of bone marrow aspirates from 759 breast cancer patients (621 stage I to III and 138 stage IV) were screened by immunocytochemical (ICC) with the pancytokeratin monoclonal antibody A45-B/B3. Morphologic criteria were used to distinguish isolated cancer cells from other cytokeratin-positive cells in BM. CTC were simultaneously in peripheral blood were screened by ICC in 77 stage I to III and 37 stage IV patients. Bone marrow status was correlated with clinical outcome after a median follow-up of 51 months. Results: Bone marrow MM with tumoral morphologic features were detected in 15% of the patients with stage I to III. On multivariate analysis, MM in BM was the strongest prognostic factor for overall survival (RR= 2.43, p<0.0001). Other prognostic factors were clinical stage (p=0.004), tumor grade (p=0.011) and tumor emboli (p=0.02). MM detection was also associated with a poorer distant metastasis-free survival (DMFS, RR=2.03 p=0.002) with a trend for more liver than bone metastasis. Surprisingly MM were also associated with a poorer local relapse free survival (RR= 3.92, p=0.0001). In 138 stage IV patients, MM detection (65%) in BM was highly associated with clinical or radiological bone metastasis (p=0.0001) and lobular histology (p=0.05). Presence of MM in BM was not associated with a poorer survival rate. Adverse prognostic factors for overall survival were hormonal receptor negativity (p <0.001), more than one line of chemotherapy (p=0.004), and liver involvement. CTC detection in a subgroup of 37 metastatic patients was associated with a shorter survival (p=0,01). Conclusion For early stage of breast cancer, MM detection in bone marrow is a strong independent prognostic factor. MM in BM in stage IV breast cancer patients did not have a prognostic signi¿cance. This study ¿nally suggest that CTC are a usefull marker of the tumor aggressivity in metastatic patients, whereas bone marrow MM are a marker of the primary tumor ability to metastasize. 108 Prognostic value of the detection of circulating tumor cells using a multimarker RT-PCR (CK19, mammaglobin A, HER2/neu) in early breast cancer. Ignatiadis M, Kallergi G, Ntoulia M, Apostolaki S, Perraki M, Xenidis N, Stathopoulou A, Lianidou E, Georgoulias V, Mavroudis D. University General Hospital of Heraklion, Heraklion, Crete, Greece; School of Medicine, University of Crete, Heraklion, Crete, Greece; University of Athens, Athens, Greece Objective: To investigate the prognostic value of the molecular detection of Circulating Tumor Cells using 3 markers (CK19, MammaglobinA and Her2/neu) in early breast cancer Patients and methods: CK19 mRNA-, MammaglobinA mRNA-, and HER2 mRNA- positive cells, were detected using real-time (CK19) and nested (MammaglobinA and HER2) RT-PCR, in 140 women with stage I-III breast cancer before the initiation of adjuvant chemotherapy. Their detection was correlated with clinical outcome. In 10 breast cancer patients, double immunofluoresence staining experiments were performed to investigate the co-expression of Cytokeratin (CK), MammaglobinA and HER2 in CTCs. Results: Among the 140 patients, 32.9% were premenopausal, 75.7% had tumors > 2cm, 49.3% were histological grade III, 38.6% were ER negative and 70.7% had in¿ltrated axillary lymph nodes. CK19 mRNA, MammaglobinA mRNA- and HER2 mRNA-positive cells were detected in 42.8%, 9.3% and 22.1% of patients, respectively. Patients had one of the following molecular pro¿les: CK19+/MammaglobinA+/ HER2+ (n=6), CK19+/MammaglobinA+/HER2- (n=2), CK19+/ MammaglobinA-/HER2+ (n=25), CK19+/MammaglobinA-/ HER2- (n=27), CK19-/MammaglobinA+/HER2- (n=5), CK19/MammaglobinA-/HER2- (n=75). Immunofluorence experiments con¿rmed the following CTC phenotypes: CK+/MammaglobinA+, CK+/MammaglobinA-, CK-/MammaglobinA+, CK+/HER2+, CK+/ HER2-, MammaglobinA+/HER2- and MammaglobinA+/HER2+. In univariate analysis, the molecular detection of CK19-, MammaglobinAand HER2-positive cells were all significantly associated with shorter disease-free survival (DFS), (p<0.001, p=0.004 and p=0.017, respectively), whereas only the detection of CK19-positive cells was associated with worse overall survival (p=0.001). In multivariate analysis, histological grade III tumors and the detection of CK19 mRNA- and mammaglobinA mRNA-positive cells were independently associated with worse DFS. Conclusion: This multimarker RT-PCR provides significant and independent prognostic information regarding DFS in women with early breast cancer. 109 Circulating CK-19 mRNA (+) cells in patients with stage I and II breast cancer after the completion of adjuvant chemotherapy: evaluation of their prognostic relevance. Xenidis N, Apostolaki S, Perraki M, Politaki E, Kalbakis K, Ignatiadis M, Kalykaki A, Agelaki S, Georgoulias V, Mavroudis D. University General Hospital of Heraklion, Heraklion, Crete, Greece; School of Medicine, University of Crete, Heraklion, Crete, Greece Purpose: To evaluate the prognostic value of circulating CK-19 mRNA (+) cells in patients with early stage breast cancer after the completion of adjuvant chemotherapy. Patients and Methods: 450 patients with early (stage I/II) breast cancer were included in the present study. All patients received adjuvant chemotherapy (CMF= 43; FEC= 210; T/EC= 197). Peripheral blood (20ml in EDTA) was obtained before the initiation and after the completion of adjuvant chemotherapy. Circulating CK19 mRNA (+) cells were evaluated by real time RT-PCR. Results: One hundred and forty-seven (32.7%) patients had detectable CK-19 mRNA (+) cells post-chemotherapy. Only the presence of >3 involved axillary lymph nodes was associated with a higher incidence of CK-19 mRNA (+) cells post-chemotherapy. Detection of circulating CK-19 mRNA (+) cells post-chemotherapy was signi¿cantly associated with either a clinical relapse (p= 0.002) or disease-related death (p= 0.001). Multivariate analysis demonstrated that the detection of CK-19 mRNA (+) cells after chemotherapy was an independent factor for early relapse (H.R 1.726; 95% CI 1.146-2.598; p= 0.009) and overall survival (H.R 2.034; 95% CI 1.079-3.836; p= 0.028). Conclusions: These results further support that the detection of circulating CK-19 mRNA (+) cells after adjuvant chemotherapy is a prognostic factor associated with poor clinical outcome. 110 Circulating epithelial tumor cells a new tool for therapy monitoring in breast cancer: a more than tenfold increase in numbers during systemic therapy is highly predictive of relapse. Pachmann K, Camara O, Cavallaris A, Krauspe S, Malarski N, Gajda M, Kroll T, Runnebaum I, Hoeffken K. Friedrich Schiller-Universität Jena, Jena, Germany Background: To demonstrate the feasibility of the analysis of circulating epithelial tumor cells (CETC) to monitor the response to adjuvant therapy and to early detect patients at risk of relapse. Abstracts – Poster Discussion Sessions Patients and Methods: In 91 non-metastatic primary breast cancer patients CETC were quanti¿ed using Laser Scanning cytometry of antiEpCAM stained epithelial cells from whole unseparated blood before and during adjuvant chemotherapy consisting of adjuvant Epirubicin/ Cyclophosphamid, Fluorouracil/Epirubicin/Cyclophosphamid with or without subsequent taxane, or Cyclophosphamid/ Methotrexate/ Fluorouracil therapy. Results: Numbers of CETC were analyzed before each new cycle and at the end of chemotherapy. 3 typical patterns of response were observed: 1. a decline, 2. minor changes in cell numbers, 3. a (sometimes saw-toothed) increase (more than tenfold), or an initial decline with subsequent reincrease more than tenfold in numbers of CETC. 20 (22%) relapses were observed within the accrual time of 40 months, 1 among the 28 patients from response group 1; 5 among the 30 patients from response group 2 and 14 among the 33 patients from response group 3. Mean relapse free survival time was 537 days for patients without increase of CETC and 479 days for patients with increase of CETC. The difference in relapse free survival was highly signi¿cant (p < 0.0001). Conclusion: These results show that cell numbers are inÀuenced differently by the different agents and even after initial response to therapy, an increase at the end of therapy is a strong predictor of relapse (hazard ratio = 250) and is a surrogate marker for the aggressiveness of the tumor cells. 201 A unique model of estrogen receptor (ER) α-positive breast cancer metastasis. Fuqua SA, Beyer A, Selever J, Hilsenbeck SG, Tsimelzon A, Cui Y. Baylor College of Medicine, Houston, TX Background: Mortality from breast cancer results from the ability of some tumors to metastasize to distant sites. Unfortunately, we only have a few preclinical breast cancer cell lines which metastasize to distant sites. But these models are from ERα-negative cell lines, and are thus not representative of the majority of patients, since two-thirds of patients have ERα-positive tumors. Material and Methods: To identify genes whose expression was associated with the development of treatment resistance and metastasis, we employed expression microarray analyses comparing primary tumors from patients treated with the antiestrogen tamoxifen (Tam) who did not recur, vs. metastatic tumors from patients that progressed during adjuvant Tam treatment. We identi¿ed Rho guanine disassociation inhibitor (GDI) α as being signi¿cantly under expressed in the Tamresistant group. We engineered ERα-positive MCF-7 breast cancer cells by stable transfection with a plasmid encoding a short hairpin (sh) RNA to Rho GDIα. We used growth assays in vitro and in vivo to examine the effects of Rho GDIα blockade on hormone responsiveness and metastatic behavior. Results: Rho GDIα knockdown cells exhibited hormone-independent growth in soft agar. Vector control and knockdown cells were injected into athymic nude mice supplemented with estrogen and were randomized to estrogen treatment, or to have the estrogen withdrawn and remain untreated, or to begin Tam treatment. The Rho GDIα knockdown tumors were resistant to Tam treatment. Remarkably 3050% of the Rho GDIα knockdown Tam and estrogen-treated tumors metastasized to the lung within three months. These metastases were ERα and progesterone receptor positive using immunohistochemistry. We found that knockdown of Rho GDIα with shRNA enhanced estrogen-induced activity in vitro. Since p21 activated kinase (PAK1) is an effector of Rho GDIα, and we and others have shown that protein kinase A and PAK1 can signal to and phosphorylate ERα at serine (S) 305, we performed an in vitro immune complex kinase assay and found that knockdown of Rho GDIα led to PAK-1 phosphorylation of S305. Discussion: We have established for the ¿rst time an ef¿cient metastatic model of ERα-positive breast cancer cells which will be useful for preclinical testing of inhibitors to intervene in the distant metastatic cascade in vivo. Furthermore, our preliminary data suggests that ERα phosphorylation at S305 may be downstream of Rho GDIα’s effects. S27 We hypothesize that loss of Rho GDIα function promotes distant metastatic spread of hormone-resistant ERα-positive breast tumors via crosstalk with ERα and/or by triggering downstream molecules with metastasis-promoting activities. 202 Primary tumor heterogeneity and sentinel lymph node metastases: understanding molecular processes of breast cancer metastasis. Ellsworth DL, Ellsworth RE, Patney HL, Becker TE, Deyarmin B, Jordan RM, Hooke JA, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC Background: Sentinel lymph node (SLN) status is a key prognostic factor for breast cancer patients. Sentinel nodes are believed to receive early disseminating cells from the primary tumor, but it is unclear whether the timing of metastatic dissemination or heterogeneity among cell lineages in the primary tumor de¿nes the genetic makeup and ultimately the clinical behavior of lymph node metastases. This study used allelic imbalance (AI) to examine genomic relationships among metastases in the sentinel and non-sentinel axillary lymph nodes and multiple microdissected areas of the primary carcinoma in 20 patients with lymph node positive breast cancer. Methods: Heterogeneity was assessed in three dimensions by laser microdissection of 6-15 areas (each ∼2.86 sq mm in size) from multiple sections of the primary tumor. Sentinel nodes were localized by standard scintigraphic and gamma probe techniques using 1.0 mCi technetium-99m sulfur colloid (Tc-99). Pathologically positive nodes were identi¿ed by H&E histology/IHC and metastases were isolated by microdissection. AI was assessed at 26 chromosomal regions and used to examine molecular mechanisms and infer timing of metastatic spread to the sentinel and axillary nodes. Results: A high level of discordance was observed in patterns and frequencies of AI events between metastases in the sentinel versus the nonsentinel axillary nodes. Hierarchical clustering and phylogenetic analyses suggest that (1) multiple genetically-divergent metastatic cells independently colonize the lymph nodes with vastly different patterns of genomic alterations; (2) genomic heterogeneity in the primary tumor at the time of diagnosis may not fully explain patterns of molecular changes in the corresponding metastases; and (3) the genomic composition of sentinel node metastases varies considerably and may reÀect timing of metastatic dissemination rather than primary tumor heterogeneity. Conclusions: Genomic diversity and timing of metastatic nodal spread may be important factors in determining outcomes of breast cancer patients. Metastases successfully colonizing the sentinel nodes have different patterns of molecular alterations not completely explained by primary tumor heterogeneity, suggesting that these metastases arise at different times during disease progression. Early growth of metastases in the sentinel nodes thus may be a consequence of stimulating factors that affect proliferation of previously disseminated cells rather than the timing of metastatic spread. 203 Identi¿cation of genetic predisposition to development of lymph node metastasis in breast cancer patients. Callaghan KA, Weyandt JD, Ellsworth RE, Shriver CD. Windber Research Institute, Windber, PA; Walter Reed Army Medical Center, Washington, DC Background: Breast cancer metastasis to ipsilateral axillary nodes is one of the most important predictors of poor outcome in breast cancer cases, and signi¿cantly inÀuences the recommendations for adjuvant treatment such as chemotherapy. There is currently no way to predict which patients will develop lymph node metastases despite multiple studies examining the potential impact of primary tumor characteristics on this phenomenon. Here we attempt to identify DNA variants that potentially predispose individuals with breast cancer to the development of lymph node metastases. Methods: Genomic DNA was obtained from blood samples from node-positive (n=37) and node-negative (n=40) Caucasian female S28 Abstracts – Poster Discussion Sessions breast cancer patients under 50 years of age. Following digestion, ligation, and PCR, the biotin-labeled DNA product was fragmented and hybridized to GeneChip Human Mapping 100K single nucleotide polymorphism (SNP) arrays (Affymetrix). Data was analyzed using Exemplar software and signi¿cance was evaluated using a P value of <0.001. Results were compared between node-positive and nodenegative samples to identify signi¿cant differences in polymorphisms between the two groups. Results: Association studies using Fisher’s exact test revealed that allele frequencies from 39 SNP markers representing 31 chromosomal regions were signi¿cantly different between the two groups (P<0.001). Additional model building analysis supported 36 of these markers, with each of these regions demonstrating a difference in two or more statistical tests when comparing node-negative to node-positive samples. Of note, there were six chromosomal regions (5p13.2, 6q22.31, 8q13.3, 9p24.1, 14q32.2, and Xq23) in which multiple SNP markers exhibited signi¿cance in both association analysis and model building algorithms. Conclusions: Identi¿cation of SNPs within six chromosomal regions with signi¿cant differences between node-negative and node-positive breast cancer patients suggests that the propensity to develop metastases may be inÀuenced by genetic factors. Of the potential candidate genes that have been discovered in these regions, several have been found to function in immuno-modulation, cell growth regulation, and lipid metabolism, thus polymorphisms within these genes may either confer a protective effect by enhancing the host’s immuno-surveillance or render individuals susceptible to metastatic spread by creating a host tissue environment favorable to metastatic colonization. 204 Identi¿cation of new candidate breast cancer metastasis genes. Geradts J, Desouki MM, Liao S. Duke University Medical Center, Durham, NC; Medical University of South Carolina, Charleston, SC Background: We recently reported our results of a study identifying a number of DNA copy number changes that distinguished small, high grade, ER-positive breast carcinomas with and without associated nodal metastases, as well as primary breast carcinomas and their paired nodal deposits. We now describe a series of validation experiments that support the role of six genes in breast cancer progression, most of which were not previously implicated in mammary neoplasia. Materials and Methods: DNA was extracted from macrodissected paraf¿n sections (tumor cellularity >50%) of formalin ¿xed invasive ductal carcinomas and their paired lymph node deposits (n=29), as well as matched primary breast carcinomas without associated nodal metastases within at least 5 years (n=24). The DNA was used for comparative PCR, and the frequency of copy number gains and losses was determined for each candidate gene. Additional validation studies employed immunohistochemistry and quantitative RT-PCR using RNA extracted from another cohort of frozen breast carcinomas and from cell lines. Results: We con¿rmed that 5 genes were more commonly deleted in primary carcinomas compaired to their nodal metastases: DNCLI1, SOX6, BCL2-L10, DDX6, and TIAM1. DDX6 and TIAM1 were further remarkable for amplification in 25-30% of lymph node metastases, suggesting a possible role of these genes in breast cancer progression. The novel tetraspanin TSPAN1 was ampli¿ed in almost half of tumors without nodal deposits, but deleted in almost half of breast cancers with metastases, suggesting a possible role of this gene as a metastasis suppressor (similar to other tetraspanins). At the mRNA expression level, TSPAN1 was markedly downregulated in HER2-negative versus HER2-positive breast cancer cell lines. Expression was also signi¿cantly lower in HER2-negative and ERnegative breast carcinomas. Interestingly, by far the lowest levels were observed in ER-/HER2- (basal-like) tumors. Although we could not con¿rm their differential ampli¿cation or deletion, we identi¿ed a number of additional candidate metastasis genes including Claudin 10 that showed copy number losses in a signi¿cant subset of primary breast carcinomas. Discussion: Our validation experiments have provided additional evidence for the role of several novel genes in breast cancer metastasis. Of these, TSPAN1, DDX6 and TIAM1 may be particularly relevant. 205 ALDH1 positive stem cells in inÀammatory breast cancer mediate metastasis and are associated with a poor clinical outcome. Charafe-Jauffret E, Ginestier C, Tarpin C, Iovino F, Esterni B, Jacquemier J, Xerri L, Merajver S, Dontu G, Birnbaum D, Wicha M, Viens P. Institut Paoli-Calmettes, Marseille, France; Comprehensive Cancer Center, University of Michigan Medical Center, Ann Arbor, MI, France Inflammatory breast cancer (IBC) is a relatively rare aggressive form of breast cancer with a poor prognosis associated with a high propensity to develop systemic metastasis. The molecular mechanisms which mediate metastasis in this cancer and markers to predict its occurrence remain unde¿ned. There is accumulating evidence that breast cancers may contain a small «cancer stem cell» population which drives tumorogenesis and contributes to therapeutic resistance. In order to determine whether inÀammatory breast carcinoma contains cancer stem cell populations which mediate metastasis, we utilize a cell line SUM 149, derived from a primary IBC. Cells expressing the stem cell maker aldehyde dehydrogenase were isolated from this cell line utilizing the ALDEFLOUR assay. Utilizing Àow cytometry, we isolated an ALDEFLUOR-positive component composing 3-5% of the total population which displayed stem cell properties. ALDEFLUORpositive but not ALDEFLUOR-negative cells were tumorigenic in NOD/SCID mice and were able to reconstitute the global heterogeneity of the initial cell line upon serial passage in mice. In order to examine the metastatic capacity of these cells they were labeled with a luciferase containing lentivirus and introduced via intracardiac injection into NOD/SCID mice. Only the ALDEFLUOR-positive cells were able to form metastasis. In order to investigate the clinical relevance of ALDH1 expression in IBC, we examined the expression of ALDH1 utilizing a monoclonal antibody in a series of 109 IBC specimens. ALDH1 was found to be expressed in 31% of these tumors, ALDH1 expression did not correlate with other clinical pathologic markers including estrogen and progesterone receptor, BCL2, ERBB2, MUC1, or E-cadherin. However, ALDH1 expression was found to be a strong predictor of patient outcome and was associated with poor overall survival p=0.0337, as well as metastasis-free survival p=0.0152. Metastasis-free survival was 49 months in patients with ALDH1-negative tumors as compared to 20 months in patients with ALDH-positive tumors. Multi-variant analysis using Cox proportional hazard models showed that ALDH1 is the most powerful marker of speci¿c survival (p=0.0012 and the only marker of metastasis-free survival HR=2.81, 95% CI [1.355-5.815], p=0.0055). These studies suggest that a subset of IBC contain ALDH1 positive «cancer stem cells» which are responsible for tumor metastasis. In addition, the expression of ALDH1 in patient specimens is a strong predictor of metastasis and poor clinical outcome. The measurement of ALDH1 in pretreatment biopsies may help to de¿ne those patients needing particularly aggressive therapy. Furthermore, successful treatment of these patients may require development of strategies which selectively target this cell population. 206 Programmed cell death 4, a novel inhibitor of breast cancer invasion. Nieves-Alicea R, Simeone AM, Colburn NH, Tari AM. The University of Texas M.D. Anderson Cancer Center, Houston, TX; National Cancer Institute, Frederick, MD High expression of the cyclooxygenase-2 (COX-2) protein is found in 36-63% of human breast tumors, and is associated with tumor invasion and metastasis. Previously we demonstrated that COX-2 increases the invasion of breast cancer cells by increasing the production of prostaglandin E2 (PGE2), which results in increased protein kinase C (PKC) activity and increased interleukin-8 (IL-8) production. Here we expand our studies to determine speci¿cally what downstream factors are inhibited by the COX-2/PGE2/PKC/IL-8 pathway for breast cancer invasion. Microarray analysis revealed that the mRNA expression of Programmed Cell Death 4 (PDCD4) is 2-fold lower in MCF-7 breast cancer cells stably transfected with COX-2 (MCF-7/COX-2) than Abstracts – Poster Discussion Sessions parental MCF-7 cells. PDCD4 is a tumor suppressor protein whose expression is decreased in many tumor types, including breast tumors. Western blot analysis of MCF-7/COX-2 cells showed decreased PDCD4 expression, in comparison to the parental MCF-7 cells, thus corroborating our microarray results. In addition, PDCD4 protein levels were decreased when MCF-7 cells were treated with PGE2, the PKC activator phorbol-12-myristate-13-acetate (PMA), or IL-8. We hypothesized that COX-2 utilizes the PGE2/PKC/IL-8 pathway to suppress PDCD4 expression to induce breast cancer invasion, and that overexpression of PDCD4 would reverse the invasive activity of COX-2. Plasmids encoding the human PDCD4 cDNA were stably transfected into MCF-7 cells (MCF-7/PDCD4). Matrigel invasion assay was used to investigate the invasiveness of MCF-7/PDCD4 cells. PGE2, PMA, and IL-8 all failed to induce the invasion of MCF-7/PDCD4 cells, indicating that high levels of PDCD4 suppress breast cancer invasion. Furthermore, MCF-7/PDCD4 cells were found to produce 4-fold higher levels of the Tissue Inhibitor of Metalloproteinases-2 (TIMP-2) than the parental MCF-7 cells. To determine whether TIMP-2 is essential for PDCD4 to inhibit invasion, we used siRNA to knock down TIMP-2 expression in MCF-7/PDCD4 cells. Pretreatment of MCF-7/PDCD4 cells with TIMP-2 siRNA allowed PGE2, PMA, and IL-8 to induce the invasion of MCF-7/PDCD4 cells, indicating that knocking down the expression of TIMP-2 reversed the anti-invasive effects of PDCD4. Here we report the novel ¿ndings that COX-2 decreases PDCD4 expression via the PGE2/PKC/IL-8 pathway, and that PDCD4 increases TIMP-2 production to inhibit breast cancer cell invasion. Bone metastasis occurs in 3 out of 4 patients with advanced breast cancer. COX-2 has been indicated as a determinant of breast cancer bone metastasis. We are currently conducting experiments to determine whether PDCD4 overexpression could block COX-2 driven breast cancer bone metastasis. 207 TROP2 is a novel, major determinant in breast cancer growth and metastatization. Alberti S, Trerotola M, Vacca G, Zappacosta R, Rossi C, Guerra E, Bonasera V, Lasorda R, Lattanzio R, Piantelli M. Foundation University of Chieti, Chieti Scalo, Chieti, Italy Background: TROP2 is an intronless gene that encodes a transmembrane calcium signal transducer, that contains an EGF-like and a thyroglobulin domain in its extracellular portion and a HIKE motif / PKC phosphorylation site in its cytoplasmic region. Material and Methods: A relationship between expression patterns of TROP2 and differentiation / tumor progression stages was explored with DNA array, SAGE, Northern and Western blotting, Àow cytometry, confocal microscopy and IHC analysis of normal and transformed tissues. The functional role of Trop-2 in breast cancer was analysed in vitro and in vivo by transfection of the gene or down-regulation of endogenous expresssion. Mutagenesis of the Trop-2 cytoplasmic tail was used to identify signaling pathways in tumor growth and metastatization in vivo. Results: The TROP2 gene was found upregulated in most breast cancers by DNA microarray, EST, SAGE, RT-PCR and Northern blot analysis. IHC analysis of 1231 breast cancer cases demonstrated a dramatic overexpression of the Trop-2 protein. Trop-2 potently stimulated the growth of tumor cells, whereas TROP2 siRNA inhibited the growth of breast cancer cell lines. Trop-2 transfectants demonstrated a reduced cell-cell and cell-substrate adhesion, that correlated with changes in cell shape and cell aggregate geometry and orientation. Deletion of the cytoplasmic region of Trop-2 abolished its growth stimulatory capacity, as did mutagenesis of the S303 PKC phosphorylation site. Proteomic and phosphoproteomic analysis indicated PKCα as a downstream effector of Trop-2. In vivo imaging showed dynamic colocalization of PKCα and Trop-2 in vivo in membrane rufÀes and podosomes. DN PKCα and PKCα siRNA abolished the Trop-2-induced growth. The increase in cell growth correlated with cell surface levels of Trop-2, and IHC analysis revealed up-regulation of Trop-2 in breast cancer metastases compared with primary tumors. To assess if Trop-2 played a direct role in metastatic spreading, TROP2-transfected KM12SM cells were orthotopically injected in nude mice. TROP2-overexpressing transfectants demonstrated increased metastatic potential to the liver. Deletion of the HIKE domain of Trop-2 severely diminished, whereas S29 that of the whole cytoplasmic region vastly increased metastatic diffusion, indicating the existence of both metastatic enhancers and silencers in the Trop-2 cytoplasmic tail. Discussion: Our findings candidate Trop-2 as a novel, critical determinant of breast tumor growth, as well as of metastatic cancer. Novel diagnostic and therapeutic procedures are being targeted to Trop-2. 208 Osteoblasts and their progenitors stimulate breast cancer cell migration through chemokine secretion. Molloy AP, Dwyer RM, Kerin MJ. National University of Ireland, Galway, Ireland Introduction Although breast cancer mortality is decreasing, in patients with advanced disease over 80% will develop bone metastases for which there is no cure. Bone is a very dynamic environment with continuous cell turnover, which may play an important role in directing the homing and engraftment of circulating breast cancer cells. Mesenchymal Stem Cells (MSCs) and osteoblasts are two subpopulations of cells that exist within bone. MSCs have the potential to differentiate into a range of cell types, and when cultured under appropriate conditions will develop into osteoblasts. Chemokines secreted from bone derived cells are believed to create a favourable microenvironment for development of metastases. Aim The aim of this project was to investigate chemokine secretion by bone derived cells and elucidate the potential role of MSCs and NHOst (osteoblast progenitor) cells in breast cancer cell migration. Methods Migration of breast cancer cells (BT-474 and MDA-MB-231) in response to MSCs and NHOst cells was investigated using Transwell™ migration inserts. Chemokines secreted by the bone derived cells were detected using ChemiArray™ & ELISA®. The potential role of Monocyte Chemotactic Protein -1 (MCP-1) in breast cancer cell migration was investigated using a monoclonal antibody to the chemokine. Differentiation of cells into mature osteoblasts was induced in the presence of appropriate media supplements and con¿rmed using Von Kossa staining. The level of MCP-1 secreted was quanti¿ed at various stages of differentiation. Results There was a signi¿cant increase in migration of both breast cancer cell lines in response to factors secreted by the bone derived cells (5-10 fold increase). MSCs and NHOst cells were shown to secrete a range of chemokines including IL-6 & 8, TIMP 1 & 2 and MCP-1. A monoclonal antibody to MCP-1 resulted in inhibition of MDA-MB-231 (20% reduction) and BT-474 (30% reduction) migration in response to bone derived cells. Differentiation of cells into mature osteoblasts was con¿rmed by the presence of calcium deposits following Von Kossa staining. When cultured in differentiating conditions the levels of MCP-1 rose signi¿cantly from 319 pg/ml on day 3 to 12,280 pg/ml on Day 21, which was signi¿cantly higher than that seen in control cells (p<0.05). Conclusion Bone derived MSCs and NHOst cells secrete varying levels of chemokines, including MCP-1, that play a potentially important role in mediating breast cancer cell migration. This variation in both type and level of chemokines detected during differentiation may aid the development of a favourable premetastatic niche, and inÀuence subsequent homing and engraftment of circulating cancer cells. 209 Signi¿cance of PELP1/MNAR-mediated ER-nongenotropic actions in cytoskeleton signaling. Chakravarty D, Chandrasekharan Nair B, Rajhans R, Cortez V, Nair SS, Tekmal RR, deGraffenried LA, Sun LZ, Vadlamudi RK. UTHSCSA, San Antonio, TX Background: Emerging evidence suggests that in addition to wellstudied nuclear functions, the estrogen receptor (ER) also participates in nongenotropic (cytoplasmic and membrane-mediated) signaling via S30 Abstracts – Poster Discussion Sessions formation of a multiprotein complex collectively called as “signalsome”. The role of ER-nongenotopic signaling in the progression and metastasis of breast cancer is not known and the identity of the molecular targets in the ER-signalsome is elusive. Recent studies identi¿ed Proline, glutamic acid, and leucine-rich protein-1 (PELP1) as one of the component of ER signalsome. PELP1 participates in ER nongenotropic signaling and its expression is deregulated in breast tumors. In this study we examined the signi¿cance of PELP1-mediated nongenotropic signals in the cytoskeleton signaling. Methods: To mimic ER nongenotropic signaling seen in tumors, we created breast cancer cells that express PELP1 exclusively in cytoplasm and that excessively activates ER-nongenotropic signaling via ER sequestration. We have used ligands and shRNA that activate or block nongenotropic signaling. Yeast 2-hybrid screen was performed to identify other components of signalsome. Using confocal microscopy, migration, wound healing and western analysis, we studied the significance of PELP1-mediated nongenotropic signaling in ER mediated cytoskeleton signaling. Results: Activation of nongenotropic signaling uniquely enhanced E2mediated rufÀes and ¿lopodia-like structures. Our results indicate that PELP1 play a key role in facilitating ER nongenotropic signaling in the cytoskeleton remodeling. MCF7 cells stably expressing PELP1-shRNA showed diminished ER-nongenotropic signaling and exhibited defects in cytoskeletal reorganization. Yeast 2-hybrid screen identi¿ed ILK as a binding protein of PELP1. We have con¿rmed PELP1 interactions with ILK using invitro and in vivo assays. ILK functions as down stream effector of ER- nongenotropic signaling leading to cytoskeletal reorganization and PELP1 mediates ER interactions with ILK. PELP1 interaction with ILK enhances its activity and ER-PELP1-ILK signaling appears to contribute to activation of AKT pathway in part in nongenomic manner. Conclusions: Our results suggest that ER-nongenotropic actions play a role in cell motility/metastasis and establishes that PELP1/MNAR as a critical component of ER-nongenotropic actions leading to cell motility. The findings of this study suggest that ER-PELP1-ILK pathway represent a novel target for preventing the emergence of ER+ve metastatic cells via blockage of ER-nongenotropic signals in combination with endocrine therapy. 210 Lapatinib prevents the metastatic colonization of EGFR+ and Her-2+ breast cancer cells in the brain. Palmieri D, Gril BM, Herring J, Vega-Valle E, Hua EK, Leiwehr D, Steinberg SM, Gilmer TM, Rubin SD, Steeg PS. National Cancer Institute, Bethesda, MD; SAIC-NCI, Fredrick, MD; GlaxoSmithKline, Collegeville, PA Central nervous system or brain metastases occur in approximately 20% of metastatic breast cancer patients and are associated with a dire prognosis. The incidence of brain metastases appears to be higher in metastatic patients with Her-2 ampli¿ed tumors. The ef¿cacy of the dual EGFR/Her-2 tyrosine kinase inhibitor, lapatinib, on brain metastatic colonization of a human breast carcinoma cell line was determined. An EGFP labeled brain-seeking derivative of the human MDA-MB231 cell line (231-BR) endogenously overexpressed EGFR. When 231-BR cells were transfected with a control vector or Her-2 cDNA, the Her-2 over expressing clones produced 2.5-3-fold greater large (>50 µm²) metastases in the brains of Balb/c nude mice following intracardiac injection (p=0.0001). In vitro, using siRNA knockdown of endogeneous EGFR, lapatinib equally inhibited the growth of 231-BR cells that overexpressed either Her-2 or EGFR. However, when both receptors were overexpressed lapatinib increased growth inhibition approximately 30% compared to cells that overexpressed either Her2 or EGFR. To determine the effect of lapatinib on brain metastatic colonization in vivo, mice received intracardiac injections of either the control or the Her-2 transfected 231-BR cells. Five days later mice were randomized to vehicle, 30 or 100 mg/kg lapatinib by twice daily oral gavage. Histologic analysis was conducted to quantify both micrometastases and large metastases from 10 step sagittal sections in one hemisphere of the brain. For the control transfectant mean (95% CI) large metastases were 3.36 (2.73-3.98) per section in the vehicle controls, were unaffected by 30 mg/kg lapatinib but declined 54% to 1.56 (0.94-2.17) when treated with 100 mg/kg lapatinib (p=0.0001). The Her-2 transfectant produced 6.83 (5.86-7.79) large metastases per section. Treatment with 30 mg/kg resulted in a 53% decline to 3.21 (2.31-4.11) large metastases (p<0.0001), while treatment with 100 mg/kg resulted in a 50% decline to 3.44 (2.55-4.32) large metastases (P<0.0001). The data indicate that lapatinib can inhibit the brain colonization of dual EGFR-Her-2+ breast cancer cells. 301 Optimal dose and schedule of a HER2/QHX peptide (E75) vaccine in disease-free breast cancer patients: results from two phase I/II clinical trials. Holmes JP, Patil R, Amin A, Jama YH, McNeill A, Hueman MT, Craig D, Ponniah S, Peoples GE. National Naval Medical Center, Bethesda, MD; Windber Medical Center, Windber, PA; USUHS, Bethesda, MD; Brooke Army Medical Center, Ft. Sam Houston, TX Background: We have administered the HER2/neu-derived peptide E75 as a preventive vaccine in disease-free breast cancer (BrCa) patients. The combined results of two clinical trials showed the vaccine is safe, immunogenic and may reduce recurrences. In this study, we have assessed the clinical results based on the different doses and schedules of the vaccine to to determine the optimal biologic dose (OBD). Materials and Methods: Disease-free node-positive (NP) and nodenegative (NN) BrCa patients were vaccinated over six months either 3, 4 or 6 times with E75 + GM-CSF in different dose/schedule groups. Toxicities were graded per NCI Common Terminology Criteria. GMCSF was reduced for signi¿cant toxicity. Immunologic response was measured by local reactions, delayed type hypersensitivity test (DTH) and E75-speci¿c CD8+ T-cells quanti¿ed with HLA-A2:IgG dimer and Àow cytometry. Results: 96 patients (45 NP and 51 NN) were vaccinated over 6 months in one of seven dose groups [peptide(µg).GM-CSF(µg).#doses]: 100.250.6, 500.125.3, 500.125.4, 500.250.4, 1000.250.4, 500.250.6, 1000.250.6. Twenty patients required GM-CSF dose reduction. Patients receiving GM-CSF 250µg for six doses were more frequently reduced than patients on <250µg or <6 doses (33% vs 8%, p<0.01). The majority of dose reductions were due to local toxicity (75%). The OBD was was found to be 1000.250.6. Patients in the OBD dose group (n=27) experienced similar toxicities to the 69 sub-optimally dosed patients (SUB). Mean E75-speci¿c CD8+ T-cells were similar in the OBD and SUB groups at all time points post-vaccination (OBD±SE vs SUB±SE): post-vaccination average (0.89±0.1% vs 0.71±0.1%); maximum (1.8±0.3% vs 1.99±0.2%); and long-term response (0.79±0.2% vs 0.79±0.1%). Despite similar quantitative T-cell responses, the OBD patients had signi¿cantly larger post-vaccination DTH responses to E75 compared to SUB patients (22±2.7mm vs 11±1.3mm, p=0.0008). OBD patients had worse prognostic factors than SUB patients with larger tumors (≥T2 52% vs 22%, p=0.006), more NP patients (NP 74% vs 36%, p=0.001) and higher grade tumors (grade 3 48% vs 29%, p=0.1). Recurrence rates in the OBD patients were lower (3.7%) than SUB patients (10.1%, p=0.4) although the OBD has a shorter median follow-up time. Discussion: In our trials, the OBD of E75 in disease-free BrCa patients is 1000.250.6. However, some patients required dose reduction of the GM-CSF. Using this dosing strategy, a robust local reaction to successive inoculations was maintained, while limiting cumulative toxicity, and resulted in the best in vivo immune response (DTH). Of the 8 recurrences in all of the E75-vaccinated patients, only one occurred in the optimally dosed group. 302 Clinical results of a phase I trial of a HER2/QHX-derived peptide (GP2) vaccine in disease-free, node-negative breast cancer patients. Carmichael M, Holmes JP, Mittendorf EA, Amin A, Hueman MT, Ponniah S, Peoples GE. USUHS, Bethesda, MD; National Naval Medical Center, Bethesda, MD; UTMD Anderson Cancer Center, Houston, TX; Brooke Army Medical Center, Ft. Sam Houston, TX Background: E75 and GP2 are HER2/neu-derived immunogenic peptides. Pre-clinical studies demonstrated epitope spreading to GP2 in disease-free breast cancer (BrCa) patients receiving E75 as a Abstracts – Poster Discussion Sessions preventive vaccine, and GP2-stimulated CD8+ T-cells lyse HER2/neuexpressing cancer cells in vitro. Here, we describe the results of a phase I dose escalation study of GP2 used as a vaccine in disease-free BrCa patients. Materials and Methods: Disease-free node-negative HLA-A2+ BrCa patients were vaccinated in a dose escalation study of GP2 + GM-CSF. Vaccinations were given monthly for 6 months. Dose groups consisted of 3 patients each and were as follows [GP2(µg). GM-CSF(µg)]: 100.250, 500.250, 1000.250, 500.125. Toxicities were graded per NCI Common Terminology Criteria. GM-CSF was reduced 50% for signi¿cant toxicity and large local reactions. Immune response was measured with pre- and post-vaccination delayed-type hypersensitivity test (DTH). GP2-speci¿c CD8+ T-cells were measured by Àow cytometry utilizing HLA-A2:IgG dimer. Results: Twelve patients have been enrolled. Maximum local toxicities were grade 1 (33%) and grade 2 (67%). Maximum systemic toxicities were grade 1 (67%) and grade 2 (33%). All of the patients (n=9) vaccinated with 250µg GM-CSF required dose reduction for large local reactions. Median post-vaccination DTH response to GP2 (34mm, range 18-115mm) was signi¿cantly larger than pre-vaccination DTH (0mm, 019mm; p<0.0001). Maximum levels of post-vaccine GP2 speci¿c CD8+ T-cells (median 0.81%, range 0.44-2.35%) were higher than pre-vaccine (0.12%, range 0-0.98%, p=0.001). Median long-term (6 month postvaccine) levels of GP2-speci¿c CD8+ T-cells in 5 patients was 0.44% (0.04-0.65%) suggesting durable though waning immunity. Discussion: GP2 can be safely and effectively administered to BrCa patients in combination with GM-CSF with minimal toxicity. The GP2 peptide appears to be very immunogenic requiring lower doses and less GM-CSF than the E75 vaccine. A randomized study of GP2 + GM-CSF vs GM-CSF is underway in node-positive breast cancer patients to further delineate the clinical effects of this immunogenic peptide. The views expressed herein are those of the authors and do not represent the policy of the Department of Army, Department of Navy, Department of Defense or the US Government. 303 Immunotherapy against metastatic breast cancer with a twist. Demaria S, Wang B, Yang AM, Santori F, Kawashima N, Matsumura S. New York University School of Medicine, New York, NY Background: Effective loco-regional treatments are available for breast cancer, but metastatic disease remains a therapeutic challenge. The effectiveness of immunotherapy (IT) will depend on the ability to target antigens that are essential for the metastatic process. Expression of the transcriptional regulator Twist is required for the metastatic behavior of 4T1 cells, an experimental mouse model of metastatic breast cancer (Yang, et al., Cell 2004, 117: 927-939). Here we show that Twist behaves as a tumor associated antigen (TAA) that can be recognized by tumor-speci¿c CD8+ T cells. Methods: H2 d haplotype-restricted CD8+ T cell epitopes were identified within Twist protein using the SYFPEITHI Epitope Prediction computer-based algorithm. The top scoring peptides were tested for binding to H2-Ld or H2-Kd in a major histocompatibility complex (MHC) stabilization assay using RMA-S cells expressing the appropriate MHC class I allele. Next, the stability of peptideMHC complexes was measured by determining the time required for loss of 50% (DC50) of peptide-H2-Kd or H2-Ld complexes at 37°C. Binders were further tested for the ability to sensitize P815 cells to lysis by 4T1 tumor-speci¿c cytolytic T cells (CTL) in a standard 51Cr release assay. γ-interferon production was determined by intracellular cytokine staining. Results: One out of ¿ve candidate peptides bound to H2-Ld, and four out of ¿ve candidate peptides bound to H2-Kd. Among them, only peptide #9 (pTw9) formed stable complexes with H2-Kd with a half live of >6 hours on the cell surface. pTw9-speci¿c CTL precursors were expanded in vitro from mice previously cured of metastatic 4T1 tumors with a combination of local radiation and IT (Demaria et al., Clin. Cancer Res. 2005, 11:728-34). pTw9-speci¿c CTL showed peptide-speci¿c anti-tumor effector functions such as killing and γinterferon production in vitro. Vaccination experiments indicated that S31 pTw9 peptide is immunogenic in naïve mice. Discussion: These data indicate that Twist, a gene normally expressed during embryonic development, and playing a critical role in metastasis of breast cancer cells, can be a target of the anti-tumor immune response. IT approaches targeting Twist could be effective for the treatment of cancers with high expression of Twist such as human lobular carcinoma of the breast. Supported, in part, by Department of Defense grant W81XWH-051-0436. 304 10 years follow up of pilot phase III immunotherapy study in early stage breast cancer patients using oxidized mannan-MUC1. Vassilaros S, Tsibanis A, Tsikkinhs A, McKenzie IF, Apostolopoulos V. PROLIPSIS – Diagnostic Breast Center, Athens, Greece; Burnet Institute at Austin, Heidelberg, Victoria, Australia Introduction. We report the 10 year follow up of a pilot phase III immunotherapy study, in stage II adenocarcinoma of the breast, by injecting subcutaneously oxidated Mannan-MUC1. MUC1 is a high molecular weight glycoprotein overexpressed on adenocarcinoma cells and is the target of this immunotherapy protocol. Method. The study is a randomized double blind. 31 (16 in the study group and 15 in the placebo group) patients, operated for stage II adenocarcinoma of the breast, were enrolled and followed from December 1997 to May 2007, in order to evaluate any difference in the length of the disease free period. Disease free period, survival and immunological assays, were assessed. Results. From December 1997 to May 2007 in the study group of 16 patients who were injected with oxidated MUC1, only one developed metastatic disease, 96 months after the initial surgery. In the placebo group of 15 patients, the disease was relapsed in 6 patients at 8, 18, 34, 78, 89 and 102 months after the initial surgery. These ¿nding was statistically signi¿cant (p=0,0247). Nine out of 13 patients had measurable antibodies to MUC1 and 4 out of 10 had MUC1-speci¿c Tcell response; None of the placebo group exhibited any immune response to MUC1. Ten years passed after the ¿rst enrolment in the study and the mean period of follow up is 8,5 years. Conclusion. The results suggest that in early breast cancer MUC1 immunotherapy is bene¿cial and that a larger phase III study should be undertaken. 305 Circulating immature myeloid cells in breast cancer patients correlate with clinical cancer stage and cyclophosphamide treatment: implications for cancer immunotherapy. Montero AJ, Dewaay DJ, Salem M, Cole DJ, Diaz-Montero CM. Medical University of South Carolina, Charleston, SC Background: Tumor-associated immune suppression is known to be an important contributor to cancer progression. One important mechanism is the abnormal accumulation of immune suppressive immature myeloid cells (ImC) in the peripheral blood. Although both tumor burden and cyclophosphamide (CTX) induced accumulation of ImC are well described in animal studies, human studies have been limited. Thus, the goal of our study was to determine whether levels of ImC in whole blood correlate with clinical cancer stage in patients (pts) with breast cancer and determine whether standard dose dense (dd) chemotherapy with doxorubicin and cyclophosphamide (ddAC) results in greater increases in ImC than paclitaxel (ddT). Methods: Flow cytometry analyses were performed on whole peripheral blood from 14 normal healthy volunteers and 57 newly diagnosed cancer pts including 27 patients with breast cancer (stages: I/II n=15; III, n=11; IV, n=31) prior to therapy. ImC population was de¿ned as lineage-, CD33+, HLA-DR-, CD11b+. In 16 pts with stage II-III breast cancer receiving (ddAC→ddT) blood was collected on day 1 of each cycle of chemotherapy prior to receiving the subsequent cycle. Results: Greater circulating levels of ImC in cancer pts vs. normal were noted (4.02% vs. 1.46%; P=6.37x10-5). Stage IV pts had the highest percentage and absolute number of ImC (Table 1). Moreover, ddAC was S32 Abstracts – Poster Discussion Sessions associated with signi¿cant increases in circulating ImC compared with pretreatment levels (2.51% vs. 13.17%; P=1.6x10-12), and also when compared to ddT (4.6%; P=2.76x10 –9). This increase was sustained throughout ddAC chemotherapy. Conclusions: Overall elevated levels of ImC correlated with advanced clinical breast cancer stage. ddAC chemotherapy was associated with signi¿cant and sustained increases in ImC in breast cancer pts. This has important implications for breast cancer vaccine therapy because vaccine-elicited anti-tumor responses can be signi¿cantly dampened by this cell type. Novel pharmacologic means to decrease levels of circulating ImC or to modify them to acquire an immunoenhancing rather than an immunosuppressive phenotype have the potential to signi¿cantly enhance the effectiveness of immunotherapy in breast cancer and other solid tumors. Finally, although CTX is currently used in adoptive immunotherapy protocols in part because it can decrease numbers of regulatory T-cells, our study shows that CTX is also associated with signi¿cant rises in ImC which could antagonize development of tumor speci¿c immunity. Table 1. Circulating Levels of ImC by Clinical Cancer Tumor Stage Clinical Cancer Stage % ImC Total ImC (cells/microliter) Normal Volunteers 1.46* I/II 2.46* 163.74* III 2.89* 205.72* IV 5.17* 414.21* *P<0.04 306 Targeting of the chemokine receptor CXCR4 in acquired trastuzumab resistance. Tripathy D, Mukhopadhyay P, Verma U, Mukhopadhyay C, Shelton J, Story M, Ding L. University of Texas Southwestern Medical Center, Dallas, TX Background: The anti-HER2 antibody trastuzumab is effective in HER2-expressing breast cancer, yet clinical resistance develops in almost all cases of advanced disease. Acquired trastuzumab resistance is not well understood, although it has been shown that expression of the HER2 target is preserved, suggesting alterations in downstream or interacting signaling pathways. We describe a novel speci¿c alteration in a cell line model of acquired trastuzumab resistance, the targeting of which reverses resistance. The chemokine receptor CXCR4 has been implicated in increased metastatic potential in breast and colon cancer and as a scaffolding protein required for optimal HER2 function. Methods: A trastuzumab-resistant subclone (BT 474HR) of the HER2positive breast cancer line BT 474 was developed by serial passage in trastuzumab for about 1 year. Gene expression pro¿les before and after trastuzumab exposure were assessed using Affymetrix HG-U133A/B human gene arrays. siRNA mediated knockdown of CXCR4 in BT 474 and BT 474HR cells was performed and con¿rmed by real timePCR and Western blotting (fusin antibody, Santa Cruz), and effects on cell viability were assessed using the CellTiter-Glo luminescent cell viability assay (Promega). Subcellular localization of CXCR4 was assessed by immunoÀuorescence and gradient centrifugation. The effect of the CXCR4 inhibitor AMD3100 (Sigma) on sensitive and resistant cells was measured. Effects of CXCR4 ligand SDF-1 (R&D Systems) on HER2 phosphorylation was assessed using anti-pHER2 antibody (2247 Cell Signaling). Results: BT 474HR cells exhibited upregulation of several genes including CXCR4 (con¿rmed by real-time PCR), CSTA (cysteine protease inhibitor) and mitotic checkpoint regulators. Gene-speci¿c knock down of CXCR4 was con¿rmed by real-time PCR and Western blotting, and led to re-sensitization of BT 474HR to trastuzumab, with a >60% reduction in cell number in both resistant and sensitive cells. CXCR4 inhibitor AMD3100 treatment led to partial reversal of trastuzumab resistance in resistant cells. BT474HR cells demonstrated nuclear compared to membrane distribution of CXCR4. Treatment of both cell lines with SDF-1 led to rapid HER2 phosphorylation. Conclusions: In this cell line model, acquired resistance to trastuzumab is associated with CXCR4 is upregulation and nuclear redistribution. Stimulation of CXCR4 leads to HER2 phosphorylation and may represent a bypass pathway for the activation of the HER2 signaling pathway that is augmented with trastuzumab resistance. Inhibition of CXCR4 reverses acquired trastuzumab resistance. This phenomenon needs to be validated in other cell line and in xenograft models as well as in breast tumor tissue from patients prior to and after clinical trastuzumab resistance. CXCR4 antagonists may be useful in preventing or reversing trastuzumab resistance. 307 TBCRC 001: EGFR inhibition with cetuximab in metastatic triple negative (basal-like) breast cancer. Carey LA, Mayer E, Marcom PK, Rugo H, Liu M, Ma C, Rimawi M, Storniolo A, Forero A, Esteva F, Wolff A, Ingle J, Ferraro M, Sawyer L, Davidson N, Perou CM, Winer EP. University of North Carolina; Dana Farber; Duke; UCSF; Georgetown; Washington University; Baylor; Indiana University; University of Alabama-Birmingham; M.D. Anderson; Johns Hopkins; Mayo Background: Basal-like breast cancer (BBC) has low expression of ER, PR, and HER2, and is thus often called “triple negative” (TN) BrCa. Preclinical studies suggest that BBC may be EGFR (HER1)dependent for proliferation. TBCRC 001 is a multicenter randomized phase II study of cetuximab with carboplatin in TN BrCa. In 3/07, Arm 1 (cetuximab alone) was closed according to prespeci¿ed response criteria. This report summarizes the interim analysis of cetuximab alone in stage IV TN BrCa. Methods: Eligible patients (pts) had measurable TN metastatic BrCa, </= 3 prior chemotherapies, no prior platinum or EGFR inhibitor. Pts randomized to Arm 1 received cetuximab alone (400 mg/m2, then 250 mg/m2 weekly) with carboplatin (AUC 2 weekly, 3 of 4 weeks) added upon progression (PD). Pts on Arm 2 receive cetuximab + carboplatin throughout. The primary endpoint is objective response (RR, CR+PR). Results: Of 21 evaluable pts in Arm 1: mean age 48.6 (range 33-67), 33% African-American, 10% Hispanic, 62% PS=0. 86% had received prior (neo)adjuvant chemotherapy, usually anthracycline/taxane-based; 62% had also received at least 1 regimen for metastatic disease. Single agent cetuximab was well-tolerated; grade 3 drug-related AEs: rash (4 pts), fatigue (1), cellulitis (1), back pain (1), irregular menses (1), and elevated LFTs (1). One grade 4 anaphylaxis occurred. There is 1 PR (4%) that has lasted over 40 weeks, 4 SD (19%), and 16 PD (76%) in Arm 1. Most progressed quickly; 5 (24%) PD 4 weeks into therapy, and 10 (48%) by 8 weeks. 19 pts had carboplatin added to cetuximab after PD; 14 are currently evaluable, 4 (28%) have uncon¿rmed PR and 4 (28%) have SD. Molecular subtyping on 10 tumors from the overall study con¿rmed BBC in 9 (1 claudin subtype). Further subtyping and preliminary studies of the biologic effects of EGFR inhibition will be presented. Conclusion: Cetuximab alone was well-tolerated but had a low single agent response rate so failed criteria for ongoing study. Rapid progression in this population may have limited evaluation of ef¿cacy. Cetuximab + carboplatin Arm 2 is ongoing, expecting completion in mid-2007. Translational studies con¿rming molecular subtype, identifying biologic effects of EGFR inhibition and platinum, evaluating circulating tumor cells, and studying the BRCA1 pathway are ongoing. Support: Translational Breast Cancer Research Consortium; AVON PFP award; NCI Breast Cancer SPOREs at UNC (CA58223) and other sites; NIH (M01RR00046, LAC). 308 Preliminary results of a randomized phase II study of weekly irinotecan/carboplatin with or without cetuximab in patients with metastatic breast cancer. O’Shaughnessy J, Weckstein DJ, Vukelja SJ, McIntyre K, Krekow L, Holmes FA, Asmar L, Blum JL. US Oncology Research, Inc., Houston, TX; Baylor-Charles A. Sammons Cancer Center, Dallas, TX; Texas Oncology, P.A. – Dallas Presbyterian, Dallas, TX; New Hampshire Oncology-Hematology, Hookset, NH; Tyler Cancer Center, Tyler, TX; The Breast Care Center of North Texas, Bedford, TX; Texas Oncology, P.A., Houston, TX Background: Irinotecan and carboplatin (ICb) is a synergistic antineoplastic combination in several cancers. Weekly irinotecan is active in metastatic breast cancer (MBC) and has proven activity in combination with cetuximab in colorectal cancer. The primary objective of this study was to determine the objective response rates produced by Abstracts – Poster Discussion Sessions irinotecan and carboplatin therapy ± cetuximab; secondary objectives were progression-free survival (PFS), overall survival, and safety. Subjects and Methods: 163 pts with measurable disease were randomly assigned to either (Arm 1) irinotecan (I) 90 mg/m2 followed by carboplatin (Cb) area AUC=2 Days 1 and 8 of each 21-day cycle or (Arm 2) same as Arm 1 except C 400 mg/m2 IV dose 1, then 250 mg/m2 weekly thereafter. Pts who progressed on Arm 1 could cross-over to single-agent cetuximab (Arm 1b). Results: Enrollment to this study has been completed. In this preliminary analysis reporting on 103 patients who have been on study >4 months, 49 pts and 54 pts were enrolled in Arms 1 and 2, with a median age of 54 years. 76 pts had received prior adjuvant chemotherapy and 33 pts had received 1 prior chemotherapy for metastatic disease. Of 36 pts on Arm 1 currently evaluable for response, 19% had an objective response compared with 39% of the 31 pts evaluable for response on Arm 2. Grade 3-4 toxicities for Arm 1/Arm2 were: fatigue 6%/18.5%, diarrhea 18%/50%, vomiting 12%/17%, neutropenia 50%/91%, and thrombocytopenia 12%/20%. Conclusions: This preliminary assessment suggests that the addition of cetuximab to ICb may improve antitumor activity but is associated with greater toxicity. A complete analysis of all patients and all study endpoints will be available for SABCS 2007. This research was supported, in part, by research grants from BristolMyers Squibb, Plainsboro, NJ, and P¿zer, Inc., New York, NY. FINAL ABSTRACT WITH FINAL RESPONSE DATA WILL BE SUBMITTED NO LATER THAN NOVEMBER 12, 2007. 309 Evaluation of trastuzumab, docetaxel and capecitabine as ¿rst-line therapy for HER2-positive locally advanced or metastatic breast cancer. Wardley A, Antón-Torres A, Pivot X, Morales-Vasquez F, Zetina L, Dias Gaui M, Otero Reyes D, Jassem J, Button P, Bell R. Christie Hospital NHS Foundation Trust, Manchester, United Kingdom; Hospital Universitario Miguel Servet, Zaragoza, Spain; CHU Jean Minjoz, Besançon, France; Instituto Nacional de Cancerología, Mexico City, Mexico; Hospital Roosevelt, Guatemala City, Guatemala; Instituto Nacional do Câncer, Rio de Janeiro, Brazil; Hospital CIMA, San José, Costa Rica; Akademia Medyczna, Gdansk, Poland; Roche Products Pty Ltd, Dee Why, New South Wales, Australia; Andrew Love Cancer Centre, Geelong Hospital, Geelong, Victoria, Australia Background: Trastuzumab (Herceptin®; H) in combination with docetaxel (T) is standard ¿rst-line therapy for HER2-positive metastatic breast cancer (MBC). The Phase II international, open-label CHAT (Capecitabine, Herceptin And Taxotere) study evaluated the addition of capecitabine (X) to the HT combination as ¿rst-line therapy for HER2positive locally advanced breast cancer (LABC)/MBC. Materials and Methods: Patients with HER2-positive (IHC 3+ and/or FISH+) LABC/MBC were randomised to receive H (8 mg/kg loading dose, then 6 mg/kg q3w) + T (75 mg/m2 in HTX arm and 100 mg/m2 in HT arm, q3w) +/- X (950 mg/m2 bid on Days 1-14 q3w). Primary end point was overall response rate (ORR); secondary end points included duration of response (DoR), progression-free survival (PFS), time to progression (TTP), overall survival (OS) and safety. Results: In total, 222 patients were randomised and received study medication. Baseline characteristics were reasonably well balanced. Median follow-up for the 2 arms was 25.5 (HTX) and 23.5 (HT) months. Key ef¿cacy and safety results are shown in the tables. Discussion: High response rates were displayed by both regimens, with HTX achieving signi¿cant improvement in TTP and PFS compared with HT in HER2-positive LABC/MBC. Both regimens were generally well tolerated and cardiac safety was consistent with other H-based trials. ORR, % Complete response, % Partial response, % Stable disease, % Progressive disease, % Missing, % Median DoR, months Median PFS, months Median TTP, months Median OS, months HTX (n=112) 71 23 47 25 4 1 15.9 17.9 18.6 43.5 HT (n=110) 73 16 56 16 9 2 13.4 12.8 13.6 47.3 p value 0.717 0.0402 0.029 0.485 S33 HTX (n=112) HT (n=110) Grade 3/4 neutropenia, % 27 24 Grade 3/4 febrile neutropenia, % 15 27 Grade 3/4 neutropenic sepsis, % 4 <1 LVEF absolute drop, 15%, % 19 17 LVEF decline to <40%, % 2 2 Symptomatic congestive heart failure,a % <1 <1 Grade 3 hand-foot syndrome, % 17 <1 Grade 3/4 diarrhoea, % 11 4 Treatment-related deaths, % <1 3 a New York Heart Association class II; LVEF, left ventricular ejection fraction. 310 A phase I study of trastuzumab-DM1, a ¿rst-in-class HER2 antibody-drug conjugate, in patients with advanced HER2+ breast cancer. Krop IE, Beeram M, Modi S, Rabbee N, Girish S, Tibbitts J, Holden SN, Lutzker SG, Burris HA. Dana-Farber Cancer Institute, Boston, MA; Institute for Drug Development, San Antonio, TX; Memorial Sloan-Kettering Cancer Center, New York, NY; Genentech, South San Francisco, CA; Sarah Cannon Research Institute, Nashville, TN Rationale Trastuzumab-DM1 (T-DM1) is a ¿rst-in-class HER2 antibody-drug conjugate (ADC) in development for HER2-positive breast cancer (BC). T-DM1 is designed to combine the biological activity of trastuzumab (T) with the targeted delivery of a highly potent antimicrotubule agent (DM1) to HER2-expressing cells. Focusing such chemotherapeutic agents on tumor cells via high-speci¿city monoclonal antibodies that bind unique and/or over-expressed cell-surface tumor antigens is intended to improve the therapeutic window for such agents, allowing their potential to be applied to the clinic. DM1 binds to tubulin competitively with vinca alkaloids, but 20-100 times more potently than vincristine. Its parent molecule, maytansine, has induced responses in patients (pts) with breast and lung cancer, with principal adverse events (AEs) of nausea, vomiting, diarrhea, and sensory neuropathy. The stable MCC linker molecule was engineered to potentially enhance the therapeutic window of DM1 by improving exposure to T-DM1 and minimizing exposure to free DM1. T-DM1 is the ¿rst ADC with an MCC linker in clinical trials. T-DM1 binds to HER2 with affinity similar to that of T and is internalized via the normal ongoing HER2 internalization process. T-DM1 has activity in both T-sensitive and T-insensitive HER2+ BC xenografts; its principal preclinical AEs were reversible transaminase (TA) elevations, reversible decreases in platelets, and neuropathy. Objectives This ongoing ¿rst-in-human phase I study is evaluating the safety and pharmacokinetics (PK) of T-DM1 given IV to pts with advanced HER2+ BC who have progressed on a T-containing regimen. Results Nineteen pts (median age 50 (range 35-70); all PS 0-1); median number prior chemo regimens 8 (range 2-18) have received 83 doses of T-DM1 at 6 dose levels (0.3-4.8 mg/kg) on a q3 wk schedule. Related mildmoderate AEs include TA elevations (grade (gr) 1, 4 pts; gr 2, 1 pt), thrombocytopenia (TCP; gr 1, 5 pts), fatigue (gr 1, 5 pts; gr 2, 1 pt), anemia (gr 2, 2 pts), and peripheral neuropathy (gr 1; 1 pt). Related gr 3-4 AEs have been limited to rapidly reversible TCP (gr 3, 1 pt; gr 4, 2 pts). There has been no cardiac toxicity. T-DM1 clearance decreased with increasing dose as predicted by preclinical modeling. Four of 16 pts treated at or below the MTD have had partial responses; three are con¿rmed and ongoing after 1.7-5.5 months. Conclusions The MTD of T-DM1 given IV q3 wks is 3.6 mg/kg; TCP was doselimiting at 4.8 mg/kg. At the MTD, gr ≥2 AEs related to T-DM1 have been infrequent and manageable. T-DM1 PK is consistent with q3-week dosing. Objective tumor responses have been observed at doses at or below the MTD. Phase II trials in advanced HER2+ BC are being initiated; weekly dosing is also being explored. S34 Abstracts – Poster Discussion Sessions 401 Patterns of estrogen receptor alpha (ER) protein expression and ESR1 gene ampli¿cation in primary and metastatic breast cancer. Holst F, Haas H, Nottbohm AK, Sauter G, Simon R. University Medical Center Hamburg-Eppendorf, Hamburg, Germany Background: Estrogen receptor alpha (ESR1) gene ampli¿cations belong to the most frequent genetic alterations in breast cancer. In a recent study we found ESR1 alterations in more than 30% of tumors. Ampli¿cation was linked to low grade and early stage cancers, and predicted response to tamoxifen therapy. These ¿ndings raise the question whether possible differences of the ESR1 ampli¿cation status between primary tumors and metastases might contrubute to failure of, or resistence to hormone therapy in breast cancer. Materials and Methods: Two sets of primary and metastatic breast cancer tissues were analyzed by means of immunohistochemistry (IHC) and Àuorescence in-situ hybridization (FISH) to compare patterns of ER expression and ESR1 ampli¿cation. The ¿rst set of samles included 192 primary tumors, each with three matched lymph node metastases. The second set consisted of 59 primary tumors with multiple (range 1-15) matched distant metastases from the lungs, liver, brain, and bone marrow. To study possible intratumoral heterogenetity, three punches were compared from every individual tissue sample. Results: As expected, strong ER expression was signi¿cantly linked to ESR1 gene ampli¿cation in all samples (p<0.0001). Comparison of three punch cores from the same tissue sample showed a high degree of concordance with respect to both ER expression (1341/1525, 88%) as well as ESR1ampli¿cation (810/933, 87%), strongly arguing against presence of signi¿cant intratumoral heterogeneity. Comparison between primary tumors and matched metastases yielded identical results in the majority of cases. In ER positive primary cancers, 92% (92/100) of the nodal metastases and 94% (27/29) of the distant metastases were also ER positive. For ESR1 ampli¿cation, the concordance was 86% (12/14) for nodal metastases and 75% (3/4) for distant metastases. Discussion: Intratumoral heterogeneity is infrequent for both ER expression and ESR1 ampli¿cation in breast cancer, and might be ¿rst of all related to technical issues. Our data do also not suggest major differences of ER/ESR1 between primary cancers and both nodal or distant metastases. It is therefore unlike that heterogeneity of ER/ESR1 has major contribution to failure of hormone therapy in breast cancer. 402 Ampli¿cation of (65 may predict resistance to adjuvant tamoxifen in postmenopausal patients with hormone receptor positive breast cancer. Ejlertsen B, Nielsen KV, Rasmussen BB, Balslev E, Müller S, Møller S, Mouridsen HT. Rigshospitalet, Copenhagen, Denmark; Dako A/S, Glostrup, Denmark Background: The estrogen receptor (ER) is the target of tamoxifen, and patients with ER negative breast cancer are unlikely to bene¿t from tamoxifen. Unfortunately, endocrine therapies do not bene¿t all patients with ER positive tumors and we therefore hypothesized that copy number changes in the ESR1 gene, encoding the estrogen receptor, confer resistance. Material and Methods: Within a consecutive series of postmenopausal patients allocated to tamoxifen 20 mg daily for 5 years following radical surgery for early hormone receptor positive breast cancer, we identi¿ed 61 patients with recurrence less than 4 years and 48 patients with recurrence more than 7 years after initiation of adjuvant tamoxifen. Archival tissue from the primary tumor was collected from 100 of the 109 patients (92%). The tumor samples were analyzed for ESR1 copy number changes using FISH with a probe covering the ESR1 gene at 6q25 and a reference probe covering the centromere of chromosome 6. FISH was performed with Dako Histology FISH accessory kit. Results: The FISH analysis for ESR1 was successful in 94 of the 100 patients (94%). Ampli¿cation (ratio ESR1/CEN-6 > 2) was observed in 11 of 52 (21%) with an early recurrence (< 4 years), compared to 2 of 42 (5%) patients who still were recurrence free after more than 7 years (p=0.03). In both groups 2 patients with ESR1 deletion (ratio ESR1/CEN-6 <0.8) were identi¿ed. Discussion: In accordance with our hypothesis, this pilot study supports that ampli¿cation of ESR1 might be a marker for tamoxifen resistance in patients with operable and ER positive breast cancer. This study also revealed the existence of ESR1 deletions. The prognostic and predictive impact of ESR1 copy number changes is being further analyzed in clinical trials. 403 Relationship between (65 copy number and ER expression in the DBCG 89D trial. Ejlertsen B, Nielsen KV, Rasmussen BB, Jensen M-B, Møller S, Balslev E, Müller S, Mouridsen HT. Rigshospitalet, Copenhagen, Denmark; Dako A/S, Glostrup, Denmark Background: The ESR1 gene located on chromosome 6q25 encodes the estrogen receptor alpha (ER). The present study explores the prognostic impact and relationship between ESR1 and ER in the DBCG 89-D trial. Material and Methods: The DBCG 89-D trial randomized 980 high-risk Danish breast cancer patients to nine series of CMF or CEF, without endocrine therapy. Overall CEF was superior to CMF in terms of DFS and OS. TMA’s were constructed and analyzed centrally for ER expression and ESR1 copy number changes using FISH (Dako Histology FISH accessory kit) with a probe covering the ESR1 gene at 6q25 and a reference probe covering the centromere of chromosome 6. Relationships between DFS, OS and biomarkers were analyzed using uni- and multivariate statistics. Results: Cut sections from 41 TMA blocks with 707 patient samples (72% of total eligible) were available and the ESR1 test was successful in 607 (86%). Eight patients (1%) had ESR1 ampli¿cation (ratio ESR1/ CEN-6 > 2) and 162 (27%) had ESR1 deletion (ratio ESR1/CEN-6 < 0.8). Central ER was successful in 633 (90%) and 427 patients (67%) had ER negative (< 10% positive stained cells) tumors. ER expression was associated with (p=0.02) ESR1 aberrations. In this material of predominantly ER negative patients the proportion of patients with ESR1 ampli¿cation was too small to enable a statistical analysis. ESR1 deletion was not signi¿cantly associated with other established prognostic factors including positive nodes, tumor size, grade, ER, HER2 or TOP2A. ESR1 deletion was not a signi¿cant independent prognostic factor for DFS (p=0.13) or OS (p=0.26). Discussion: Deletions in ESR1 were demonstrated in a high proportion of predominantly ER negative patients in the DBCG 89D trial, but an independent prognostic value of ESR1 deletion could not be demonstrated. 404 Gene copy number variability of oestrogen receptor-α in breast cancer. Drury S, Lambros M, Marchio C, Johnson N, Salter J, Levey P, Fletcher O, Peto J, Reis-Filho JS, Dowsett M. The Breakthrough Breast Cancer Research Centre, London, United Kingdom; CR-UK Epidemiology & Genetics, LSHTM, London, United Kingdom Background: Approaching 80% of breast cancers (br ca) are ER+ and ER status provides a guide to therapy. It has recently been reported (Nat. Gen. 19:655-660) that the ER-α (ESR1) gene is ampli¿ed in approximately 20% of ER+ br ca. However, c.20% of normal subjects are reported to have ESR1 copy number polymorphisms, usually as copy number gains. We have sought to con¿rm the reports of ESR1 ampli¿cation using quantitative real-time PCR (qRT-PCR) and in situ hybridisation, using two sets of invasive primary br ca and germline gDNA from br ca patients. Methods: DNA was extracted from 35 microdissected, formalin-¿xed and paraf¿n-embedded, invasive br ca (91% ER+; grade 2 46%, grade 3 40%) using the DNeasy Blood and Tissue kit. DNA was isolated from circulating lymphocytes of 30 patients with synchronous, bilateral breast cancer using the QIAamp DNA Blood Kit. ESR1 (exon 2 and 8) and the reference genes FAM38B and ASXL2 were detected using qRT-PCR. Reference genes were selected based on not being affected by copy number polymorphisms (http://projects.tcag.ca/variation/) Abstracts – Poster Discussion Sessions and not being targeted by copy number aberrations in br ca. ESR2 was measured in the tumours. Ampli¿cations and gains were de¿ned as normalised values between >2 and 1.5-2, respectively. ESR1-speci¿c CISH was performed using biotin-labelled, in-house generated probes on 13/35 of the invasive tumours analysed by qPCR, in addition to a further 148 invasive breast cancers, 85.1% of which were ERα-positive. CISH was analysed by JSR-F and CM. Ampli¿cation was de¿ned as >50% of neoplastic cells harbouring > 5 ESR1 gene signals/ nucleus or large ESR1 gene clusters. Results: Using qRT-PCR on the cohort of 35 invasive breast cancers, when ESR1 was normalised to ESR2, 2/35 samples (5.7%) showed gain and 2/35 samples (5.7%) showed ampli¿cation of ESR1. When normalised to both reference genes (ASXL2 and FAM38B), 0/35 samples showed gain and 1/35 (2.8%) showed ampli¿cation. This ampli¿ed sample had the highest EIA score (500fmol/mg versus a mean of 82fmol/mg) and second highest H-score (248.6 versus a mean of 138). CISH did not con¿rm the single ampli¿cation detected by comparison to the combined reference genes, but in conjunction with Àuorescent in situ hybridisation (FISH) con¿rmed one gain and one ampli¿cation as judged by normalisation to FAM38B alone. CISH analysis of an independent 148 samples of invasive breast cancers con¿rmed that the frequency of ESR1 ampli¿cation is uncommon; only 2 tumours (1.6%) harboured ESR1 gene ampli¿cation as de¿ned by the presence of large gene clusters. All ampli¿cations were con¿rmed with FISH. To assess whether the high prevalence of ESR1 ampli¿cation observed in previous studies could be due to a copy number polymorphic gain in germline DNA, germline DNA from br ca patients was assessed by qRT-PCR as described above. No increase in ESR1 copy numbers could be identi¿ed. Conclusion: The notion of copy number gain of ESR1 in breast cancer is an important route of investigation given the applicability and wide use of this marker in guiding br ca therapy. However, in our hands, de¿nite ESR1 ampli¿cation in ERα-positive invasive br ca and ESR1 gene copy number variation in germline DNA was uncommon. 405 Serine118 phosphorylation of estrogen receptor: correlation with kinase pathways and evolution after preoperative endocrine therapy. Zoubir M, Mathieu M-C, Simmans F, Bouaziz J, Geha S, Drusch F, Liedtke C, Spielmann M, Delaloge S, Andre F. Institut Gustave Roussy, Paris, France; MD Anderson Cancer Center, Houston, TX Background: Serine (ser) 118 phosphorylation has been reported to be involved in the activation of Estrogen Receptor (ER). In the present study, we evaluated whether kinase pathways correlated with the level of ER phosphorylation on ser118 and assessed the evolution of ER phosphorylation under endocrine therapy. Patients and Methods: We constructed a tissue microarray that included 68 localized primary breast tumors before the administration of endocrine therapy. A second tissue microarray was performed that included 38 tumors obtained after endocrine therapy from the same patients. Immunostainings for ER (anti-ER 6F11antibody), phosphoSer118-ER (P-Ser118 antibody), Her2, IGFR, PAK1, pMAPK were performed. The level expression of pER was determined as a composite score that include percentage of stained cells and intensity. Results: 68 patients received endocrine therapy for a median duration of 211 days. The median age at diagnosis was 79 years (64-93). Median tumor size was 53 mm (15-90). 27 patients received tamoxifen while 41 received aromatase inhibitors. A clinical objective tumor response was observed in 36 patients (54%). Immunostaining for PhosphoSer118-ER was higher in Her2-, IGFR- and pMAPK-expressing tumors (p<0.0001 for all markers, t-test), but did not correlate with ER expression (p=0.16, t-test), nor PAK1 expression (p=0.15, t-test). ER phosphorylation at baseline did not signi¿cantly correlate with the occurrence of a clinical tumor response (p=0.16). PhosphoSer118 ER expression was signi¿cantly reduced by endocrine therapy (n=38 paired samples). The mean score was 160 (range:0-300) and 80 (range:0-300) in pre- and post-endocrine therapy samples respectively (p<0.0001, t-test). At the opposite, ER expression was not signi¿cantly modulated by endocrine therapy (p=0.18, t-test). Interestingly, the occurrence of a phospho- S35 ER downregulation after endocrine therapy was associated with the occurrence of clinical response. The clinical response rates were 36% (7 out of 19 patients) and 63% (12 out of 19 patients) in patients with stable or downregulated phosphoSer118 ER expression respectively (p=0.10, Khi-square test). Conclusion: Phosphorylation of ER on ser118 correlated with Her2, IGFR and pMAK expressions and was downregulated by endocrine therapy. The decrease of ER phosphorylation on ser118 was associated with ef¿cacy of endocrine therapy. 406 Induction of a novel estrogen receptor (ERα) phosphoserine (S154) in human breast cancer cells identi¿ed by mass spectrometry. Britton D, Scott G, Schilling B, Held J, Atsriku C, Baldwin M, Gibson B, Benz C. Buck Institute for Age Research, Novato, CA While crystallographic and nuclear magnetic resonance structures have provided critical understanding of the C-terminal ligand-binding domain of ERα, lack of structural information about the N-terminal region of ERα and limited availability of suf¿ciently powerful analytical tools to catalog ERα post-translational modi¿cations have hampered our understanding of ligand-dependent and ligand-independent ERα activation. In particular, the N-terminal 184 amino acids of ERα, predicted to be highly disordered, encompass its critical AF1 activation function domain (aa 38-149) and contain 14 serine (S) residues of which only ¿ve are known to be phosphorylated (S102, S104, S106, S118, S167) in response to ligands (e.g. E2) or growth factors (e.g. EGF, IGF-1, TGF-α) and their receptor-activated downstream serine/ threonine kinases. We employed high precision mass spectrometry (MS), including HPLC-ESI-MS/MS (Q-STAR) and vMALDI-MSn (vMALDI-LTQ), to look for novel N-terminal phospho-serine modi¿cations in ERα immunoprecipitated from E2 (vs. serum-stripped control) or EGF (vs. serum-free control) stimulated MCF7 cells. Commercially obtained recombinant human ERα (expressed in insect cells) was used to optimize immunoaf¿nity puri¿cation, in-gel protease digestions, and MSn procedures; immunoaf¿nity enriched extracts were also immunoblotted for ERα phospho-S118 and phospho-S167 to assure preservation of phosphorylation status. MS analysis of peptides from the N-terminal region resulting from ERα trypsin digestion revealed a 5-fold increase in phospho-S154 content following E2 (30 min) stimulation of MCF7 cells, with no detectable phospho-S173 or phospho-S178. Immunoblotting with a newly produced rabbit antiserum generated against a synthetic ERα phospho-S154 peptide con¿rmed this MS observation. Unlike ERα phospho-S118 and phospho-S167 induction, phospho-S154 was equally stimulated by either E2 (30 min) or EGF (10 min) treatment of MCF7 cells. Following E2 exposure, phospho-S154 induction exceeded that of phospho-S167 but not that of phospho-S118. Following EGF exposure, phospho-S167 induction exceeded that of both phospho-S118 and phospho-S154. This ¿nding of phospho-S154 illustrates the analytical power and potential biological impact of applying comprehensive proteomic and MS strategies for unbiased interrogation of endogenous ERα to identify novel posttranslational modi¿cations. Hopefully, these ¿ndings will also shed new light on breast cancer serine/threonine kinase pathways thought to modify receptor function and the clinical behavior of ERα-positive breast cancers. 407 Withdrawn by author 408 Mitogen activated protein kinase (MAPK) regulation of estrogen receptor (ER) α and tamoxifen resistance. Cui Y, Fuqua SAW. Baylor College of Medicine, Houston, TX Background: Tamoxifen (Tam) has been the most widely prescribed antiestrogen for the treatment of women with ERα-positive breast cancer. While Tam is initially useful for many patients, acquired tamoxifen resistance can develop. Increasing evidence from both the laboratory and the clinic suggest that crosstalk between the MAPK and S36 Abstracts – Poster Discussion Sessions ERα pathways may play a role in the development of resistance. We have previously demonstrated that MAPK phosphatase 3 (MKP3) levels were signi¿cantly higher in tamoxifen-resistant breast tumors, and that its overexpression conferred resistance both in vivo and in vitro1. Materials and Methods: In an effort to explore the potential mechanisms underlying MKP3-mediated tamoxifen resistance, we utilized gene reporter transactivation assays, and performed binding studies between ERα, MAPK, and MKP3. Results: We discovered that MKP3 overexpression augmented estrogeninduced ERα activity in a number of breast cancer cell lines, and that MKP3 phosphatase activity was not essential for this coactivator effect because a phosphatase dead MKP3 mutant exerted a similar effect as wild-type MKP3 on ERα activity. We found that MKP3 enhanced the activity of a number of other steroid receptors, including the receptors for androgen, progesterone, and retinoic acid. ERα activity could also be increased by MKP5 which belongs to the same MAPK phosphatses family as MKP3, but not by the unrelated phosphatase, pp2B. This result suggests that MAPK phosphatases might regulate ERα through their target MAPK. Overexpression of ERK2 MAPK or a dominant negative mutant of ERK2 dramatically repressed both ligand-independent and estrogen-induced ERα activity. This suggests that repression of ERα activity by MAPK might not be dependent on its activation. Overexpression of MKP3 relieved ERK2 repression of ERα activity. Using GST-pulldown assays, we demonstrated that ERα directly interacts with ERK2 MAPK in a ligand-independent manner. All of the ERα functional domains bound to ERK2, except for the amino-terminal, ligand-independent AF1 domain which harbors the MAPK phosphorylation site within ERα (serine 118). This was unexpected since it has been generally considered that S118 was the structural determinant for MAPK and ERα cross-talk. Conlusion: Our data suggests a novel mechanism underlying MAPK modulation of ERα and tamoxifen resistance in breast cancer cells. 1 Cui,Y. et al. Cancer Res, 66:5959, 2006. 409 Single nucleotide polymorphism 3814 C>T (P1272S) in steroid receptor coactivator-1 alters its coactivation activity. Richter AS, Hartmaier RJ, Lee AV, Skaar T, Rae J, Li L, Flockhart D, Tchatchou S, Hemminki K, Schmutzler RK, Meindl A, Bartram CR, Burwinkel B, Oesterreich S. Baylor College of Medicine, Houston, TX; Indiana University, Indianapolis, IN; University of Michigan, Ann Arbor, MI; DKFZ, Heidelberg, Germany; University of Cologne, Cologne, Germany; Klinikum Rechts der Isar TU, Munich, Germany; University of Heidelberg, Heidelberg, Germany Introduction: Genetic alterations as single nucleotide polymorphisms (SNPs) can contribute to alterations in breast cancer risk, outcome, and treatment ef¿ciency. Since the steroid receptor coactivator (SRC) family, speci¿cally SRC1, has been implicated in disease recurrence/ progression as well as response to hormonal therapy, we hypothesize that SNPs in SRC1 alter the transcriptional activity of estrogen and progesterone receptor, and could impact breast cancer risk and Tamoxifen response. Methods: ERE-LUC-Reporter and DBD-Gal4-tethering assays were conducted in MCF7, T47D, Ishikawa, or HEK293 cells, and PRE-LUCReporter assays in Ishikawa cells. To determine changes in protein half live, pulse-chase experiments were performed. The genotype effect on bone mineral density (BMD) change was tested by Wilcoxon-signed rank test. Results: To con¿rm SNPs from databases we sequenced the SRC1 gene from 48 African American and 48 Caucasian healthy subjects from the Coriell DNA diversity panel. We found the 3814C>T SNP causing a P1272S amino acid change located in the activation domain-2 (AD2) of SRC1. We observed a signi¿cant loss of coactivation due to this SNP compared to WT in ERE- as well as PRE-LUC assays. A similar loss of activity was also seen using the AD2 in DBD-Gal4-tethering assay suggesting that causative changes are inherent to the domain between amino acids 1241 and 1385. Further, we compared turnover rates of SRC1 WT and SNP. Treatment with cycloheximide followed by immunoblotting as well as pulse chase experiments revealed that SRC1 SNP is degraded faster than WT. To determine whether these in vitro ¿ndings may play a role in breast cancer etiology and response to endocrine therapy, clinical samples were genotyped. In a case-control study with 759 healthy controls and 857 familiar breast cancer patients (negative for BRCA1/2 mutations), the SNP was not associated with breast cancer risk. We genotyped 258 samples from patients treated only with Tamoxifen after tumor resection. BMD change at 12 months after treatment was used as a surrogate endpoint. Lumbar and hip BMD were found to be signi¿cantly lower in patients carrying the SNP compared to WT. According to these preliminary results, the SRC1 3814C>T genotype is associated with a detrimental effect on BMD change after Tamoxifen treatment. Summary: We have, for the ¿rst time, identi¿ed a SNP in a coactivator that alters ERα activity. The mechanism includes increased turnover rate. There was no significant association with risk, however, preliminary results suggests that the SNP alters tamoxifen effects in bone. Studies are ongoing to con¿rm these results, and further understand the mechanism. 501 The ZO-FAST trial: zoledronic acid effectively inhibits aromatase inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: 24 month BMD results. De Boer R, Eidtmann H, Lluch A, Pinotti G, Miller J, Schenk N, Dias R, Coleman R. Royal Melbourne Hospital, Parkville, Victoria, Australia; Universitaetsklinikum, Kiel, Germany; Hospital Clinico Universitario de Valencia, Valcenia, Spain; Ospedale di Circolo Fondazione Macchi, Varese, Italy; Novartis, East Hanover, NJ; Weston Park Hospital, Shef¿eld, United Kingdom Background: Letrozole is safe and effective in the treatment of receptor positive early breast cancer (EBC) in postmenopausal women (PMW). But like other aromatase inhibitors, long-term letrozole is associated with loss of bone mineral density (BMD) and a higher incidence of fractures. This multicenter open-label randomized study evaluates an immediate or delayed strategy of bone protection therapy with zoledronic acid (ZA) in preventing aromatase inhibitor induced bone loss (AIBL) in PMW with EBC who are receiving adjuvant Letrozole (Let) therapy. Material and Methods: 1065 PMW with stage I-IIIa ER+/PR+ EBC starting Let (2.5 mg qd x 5 yrs) were randomized to immediate ZA (4 mg IV infusion q 6 mos) vs delayed ZA in 112 centers in 28 countries. The delayed group will receive ZA when either post-baseline T-score decreases to less than -2.0 SD or if a non-trauma fracture occurs. The primary endpoint, the percent change in lumbar spine (LS) BMD at 12 mos was reported at the 2006 European Breast Cancer Conference. The results of longer term (24 mos) follow up are reported here. Results: Baseline characteristics were similar between the two groups. 730 of 1065 pts are evaluable for 24 mos LS BMD. Immediate ZA group shows a mean increase of 3.7%, the delayed group shows a mean decrease of 4.5%, resulting in a signi¿cant difference of 8.2% between groups (p<0.0001). 718 of 1065 pts were evaluable for 24 mos total hip (TH) BMD. Immediate ZA group shows a mean increase of 1.7%, the delayed group shows a mean decrease of 3%, resulting in a signi¿cant difference of 4.7% between groups (p<0.0001). The median duration of Let therapy was similar in both arms (31.7 vs 31.5 mos). Patients on the immediate arm received a median of 5 doses of ZA. 100 patients on the delayed arm had started ZA at the time of the 24 month analysis. 21 patients in the immediate arm had a breast cancer recurrence versus 32 in the delayed arm. At month 24, the most common adverse event was arthralgia with a similar incidence (40.2% vs 37.2%). 30 patients had a clinical fracture (13-immediate, 17-delayed). Two patients on the delayed arm had reported episodes of renal failure. Neither patient had received ZA. There were two cases of suspected osteonecrosis of the jaw. These cases will be independently adjudicated. Conclusion: These results show the continuing ef¿cacy of Zometa in preventing AIBL. The 24 mos data shows an even greater difference in the LS and TH BMD between the immediate and the delayed arms than was seen at 12 mos. Overall, the incidence of adverse events was not different between the two arms, con¿rming the safety of Zometa in this setting. Abstracts – Poster Discussion Sessions 502 The SABRE (Study of Anastrozole with the Bisphosphonate RisedronatE) study: 12-month analysis. Van Poznak C, Hannon RA, Clack G, Campone M, Mackey JR, Apffelstaedt J, Eastell R. University of Michigan, Ann Arbor, MI; University of Shef¿eld, Shef¿eld, United Kingdom; AstraZeneca, Maccles¿eld, Cheshire, United Kingdom; Site Hospitalier Nord de Nantes, Nantes, France; University of Alberta, Edmonton, AB, Canada; University of Stellenbosch, Tygerberg, South Africa Background: The SABRE trial (NCT00082277) evaluated the effects of the bisphosphonate risedronate on bone mineral density (BMD) and bone turnover in postmenopausal women with hormone receptorpositive early breast cancer treated with anastrozole. Materials and methods: Lumbar spine and hip T-scores were used to assess baseline risk of fracture, and pts were strati¿ed into treatment groups accordingly. Pts with a T-score <-2.0 for either spine or hip, or those pts deemed by the investigator to be at increased risk of fracture, were designated higher-risk (H), and received anastrozole 1 mg/day plus risedronate 35 mg/week orally. Moderate-risk (M) pts (T-score <-1.0 for spine or hip but ≥-2.0 at both sites) were randomized in a double-blind manner to receive anastrozole plus risedronate (A+R) or anastrozole plus placebo (A+P). Pts with T-scores ≥-1.0 at both spine and hip were designated lower-risk (L), and received anastrozole alone. All pts received calcium and vitamin D. Levels of serum C-terminal crosslinking telopeptide of type I collagen (sCTX), serum procollagen type I amino terminal peptide (PINP) and bone alkaline phosphatase (bALP) were used to assess bone turnover. Lipid pro¿les were also assessed before and during treatment. Results of the 12-month analysis are now available. Results: The table shows percentage change in BMD. In H, BMD increased signi¿cantly, while in L, a numeric decrease was observed. A signi¿cant difference was seen between M treatment groups for total hip (p=0.002) and lumbar spine (p<0.0001, analysis of covariance) in favor of A+R. In M, percentage changes in bone markers were signi¿cantly different between the A+R and A+P treatment groups (sCTX -43.73 vs 5.18, PINP -47.56 vs -7.65, bALP -23.91 vs 1.61, respectively; p<0.0001 for all). Incidences of adverse events (AEs) and serious AEs were comparable between M treatment groups (A+R 88%; A+P 86%), as were serious AEs (A+R 5%; A+P 5%). Discussion: In postmenopausal women with breast cancer who are scheduled for treatment with adjuvant anastrozole and are already at moderate to high risk of fragility fracture, BMD can be managed with risedronate at the licensed dose and bone health can be managed according to established guidelines. Stratum/treatment Lumbar spine L / A only M / A+P Total hip N 35 65 Estimated % change in BMD from baseline to 12 months (95% CI) -0.62 (-1.93, 0.71) -0.41 (-1.11, 0.29) M / A+R 73 +1.71 (0.85, 2.58) H / A+R L / A only M / A+P 36 35 65 +3.36 (2.05, 4.69) -0.35 (-1.37, 0.68) -0.09 (-0.66, 0.47) M / A+R 73 +1.29 (0.69, 1.90) H / A+R 37 +1.53 (0.37, 2.71) A, anastrozole; CI, con¿dence intervals; P, placebo; R, risedronate 503 The effect of risedronate on hip structural geometry in chemotherapy-induced postmenopausal women on SERMS versus aromatase inhibitors: a 2 year trial. van Londen G, Perera S, Vujevich K, Sereika S, Bhattacharya R, Vogel V, Brufsky A, Lembersky B, Greenspan S. University of Pittsburgh, Pittsburgh, PA; University of Kansas, Kansas City, Kansas Background: Although aromatase inhibitors (AIs) cause signi¿cant loss of bone mineral density (BMD), little is known about their effect on bone structure, a signi¿cant contributor to fracture risk. Our objectives were 1) to examine the impact of AIs versus Selective Estrogen Receptor Modulators (SERMs) and no hormone therapy on hip structural geometry, and 2) to determine if bisphosphonates could affect these changes. Methods: This sub-analysis of a 2 year, double-blind trial of 72 chemotherapy-induced postmenopausal women with nonmetastatic S37 breast cancer who were randomized to risedronate, 35 mg once weekly (RIS), or placebo (PBO). Outcomes included changes in Beck’s hip structure analysis (HSA) derived BMD and structural indices measured at the intertrochanteric region, femoral neck, and proximal shaft [i.e. cross sectional area (CSA), section modulus (SM: measure of bending strength), and buckling ratio (BR: index of cortical bone stability)]. Results: Twenty women did not receive adjuvant hormone therapy, while 28 women received SERMs and 24 received AIs (distributed similarly between RIS and PBO). Compared to PBO, RIS improved BMD and several HSA indices in women on no hormonal therapy or AIs at the intertrochanteric site. In the RIS group, BMD and indices were poorer in women on AIs than those on no hormonal treatment. Changes at the narrow neck and femoral shaft revealed similar ¿ndings. Discussion: In addition to decreases of BMD, AIs cause a deterioration of hip structural indices. Weekly RIS was able to attenuate these effects. These ¿ndings provide an important insight into AI-induced changes in bone geometry, which deserve further exploration to allow individualized management. Absolute changes over 24 months for HSA-derived BMD and structural parameters at the intertrochanteric site [Mean (SE)] RIS PBO BMD (g/cm2) §‡ None † 0.059 (0.026)* -0.000 (0.013) SERMs 0.030 (0.019) 0.018 (0.014) CSA (cm2) § SM (cm3) § ¨ BR §‡ AIs 0.006 (0.013) -0.034 (0.013)* None † SERMs 0.311 (0.127)* 0.180 (0.083)* 0.022 (0.054) 0.111 (0.061) AIs 0.018 (0.058) -0.085 (0.053) None † SERMs 0.305 (0.115)* 0.166 (0.076)* 0.013 (0.046) 0.138 (0.052)* AIs 0.004 (0.057) 0.029 (0.059) None † SERMs -0.660 (0.278)* -0.218 (0.223) 0.175 (0.145) -0.128 (0.146) AIs † -0.006 (0.174) 0.503 (0.181)* * P < 0.05 Difference from baseline. † P < 0.05 RIS vs. PBO. § P < 0.05 AIs vs. none in RIS. ¨ P < 0.05 AIs vs. SERMs in RIS. ‡ P < 0.05 AIs vs. SERMs in PBO. 504 Practical guidance for the prevention of aromatase inhibitorassociated bone loss in women with breast cancer. Hadji P, Appro M, Brufsky A, Tubiana-Hulin M, Guise T, Body JJ. Philipps-University of Marburg, Marburg, Germany; Institut Multidisciplinaire d’Oncology, Genolier, Switzerland; University of Pittsburgh, Pittsburgh, PA; Centre René Huguenin, St. Cloud, France; University of Virginia, Charlottesville, Virginia; Université Libre de Bruxelles, Brussels, Belgium Background: American Society of Clinical Oncology guidelines on bone health issues in women with breast cancer recommend that women with osteoporosis (T-score <–2.5) receive bisphosphonate therapy to increase bone mineral density (BMD) and reduce the risk of fracture and that osteopenic women (T-score –1 to –2.5) receive individualized therapy. Because the majority of fractures occur in osteopenic women, this threshold appears inadequate for averting fractures in patients with breast cancer, particularly those receiving aromatase inhibitor (AI) therapy. Given that BMD testing is not readily available to all patients, our goal was to provide additional evidence-based guidance to assess fracture risk and direct treatment with or without BMD scores. Material and Methods: A systematic literature review was performed to identify factors that contribute to the increased fracture risk observed in women with breast cancer. Risk factors were evaluated using an evidence-based medicine approach to identify patients at high risk, to determine when to initiate bisphosphonate treatment, and to identify the appropriate bisphosphonate for treatment. Results: With the exception of AI treatment, fracture risk factors were chosen based on their validation in large, prospective, population-based studies. Risk factors in patients with breast cancer were AI therapy, Tscore <–1.5, age >65, family history of hip fracture, history of personal fragility fracture after age 50, oral corticosteroid use >6 months, or low body mass index (<20). Additional risk factors were identi¿ed for which S38 Abstracts – Poster Discussion Sessions guidance could not be provided because available data were insuf¿cient: a diagnosis of breast cancer, chemotherapy, radiotherapy, low weight, and smoking. Available data clearly suggest that combined risk factors contribute to fracture risk independent of BMD and that some women receiving AIs do not become osteoporotic before experiencing a fracture; therefore, BMD measurement should not be the sole criterion to assess fracture risk in this patient population. Randomized clinical trials support zoledronic acid 4 mg every 6 months for prevention of AI-associated bone loss when a patient is identi¿ed to be at risk, and data with other bisphosphonates are emerging. Discussion: Our recommendations for treatment and prevention of AI-associated bone loss are as follows: In addition to calcium and vitamin D, any patient initiating AI therapy with a T-score <–2.0 should receive zoledronic acid 4 mg twice yearly. Any patient receiving AI therapy with any 2 of the following risk factors, T-score <–1.5, age >65 years, family history of hip fracture, personal history of fragility fracture after age 50, or oral corticosteroid use >6 months, should receive zoledronic acid. 505 Effect of zoledronic acid on bone loss in women undergoing chemotherapy for breast cancer. Aft R, Chavez-MacGregor M, Trinkaus K, Naughton M, Weilbaecher K. Washington University, Siteman Cancer Center, St. Louis, MO; John Cochran Veterans Administration Hospital, St. Louis, MO Background: Ovarian failure secondary to adjuvant chemotherapy is known to have an adverse effect on bone mineral density and to increase bone turnover markers. The effect of chemotherapy with growth factor support in the absence of hormonal changes on bone loss has not been described. We conducted a randomized Phase II study to determine the effect of zoledronic acid on bone loss related to breast cancer therapy. Methods: 120 women with localized stage II/III breast cancer were randomized to either zoledronic acid 4 mg IV every 3 weeks for 1 year starting with the first cycle of chemotherapy or no bisphosphonate therapy. All women received chemotherapy with epirubicin (75 mg/m2) and docetaxel (75 mg/m2). Four cycles were given prior to surgical resection and 2 cycles in the adjuvant setting. Prophylactic dexamethasone and G-CSF was given during all cycles of chemotherapy. Bone turnover markers (urinary N-telopeptide, serum speci¿c alkaline phosphatase, and osteocalcin) were measured at baseline, 3 months, and 1 year after initiation of chemotherapy. Bone mineral density (BMD) was measured by dual-x-ray absorptiometry (DEXA) of the hip, lumbar spine, and wrist at baseline and at 1 year. Eligible patients received aromatase inhibitors or tamoxifen after chemotherapy. Data was analyzed using Wilcoxon Signed rank tests or Mann-Whitney tests. Results: Between March 2003 and March 2006 120 patients were enrolled in the trial. The groups were well balanced for stage, grade, menopausal status, ER positivity, baseline BMD and bone turnover markers. Baseline and 1 year DEXA results are available for 62 women. The percentage change in the bone turnover markers were signi¿cantly less in the zoledronic treated group for all markers (p<.001). Both pre- and post-menopausal women in the control group experienced a signi¿cant decrease in BMD (p<0.001); whereas women receiving zoledronic acid experienced a statistically signi¿cant increase in BMD from baseline (p=0.001). More women with normal BMD at baseline developed osteopenia and osteoporosis in the no treatment group compared to the zoledronic acid group (p=0.025). Discussion: Our study evaluated the effect of zoledronic acid on bone loss in women undergoing chemotherapy for breast cancer. This is the ¿rst demonstration that anthracycline-taxane chemotherapy with growth factor support increased bone resorption markers in both pre- and post-menopausal women independent of endocrine therapy, radiation therapy, and surgery. We found that both pre- and post-menopausal women experienced signi¿cant decreases in bone mineral density related to breast cancer therapy. A signi¿cant proportion (42%) of these women with normal BMD at baseline developed osteopenia or osteoporosis at 1 year. The addition of zoledronic acid to systemic chemotherapy resulted in signi¿cant improvement in bone mass at 1 year following the initiation of systemic chemotherapy. 506 Zoledronic acid prevents bone loss in premenopausal women undergoing adjuvant chemotherapy for early stage breast cancer. Hershman DL, McMahon D, Crew K, Cremers S, Irani D, Cucchiara G, Brafman L, Siarra A, Shane E. Columbia University Medical Center, New York, NY Background: Adjuvant therapy for breast cancer may be associated with increased rates of bone loss and decreased bone mineral density (BMD) that may contribute to early onset osteoporosis and increased risk of fracture. This study examined whether zoledronic acid can prevent bone loss associated with adjuvant chemotherapy in premenopausal women with early stage breast cancer. Methods: This study is a randomized, double-blind, multi-center, phase III trial comparing zoledronic acid (4 mg intravenously every 3 months) versus placebo for 1 year in premenopausal women with invasive breast cancer undergoing adjuvant chemotherapy. Patients underwent serial BMD measurements at 0 (after surgery and before initiating therapy), 6 and 12 months. Patients were strati¿ed by presence or absence of hormone sensitive tumors. Fasting morning blood was analyzed at week 0, 6, 12, 18, 26, 36 and 52. Serum was archived, stored at -70o and analyzed in batches in a research laboratory for markers of bone turnover. Information on demographic, clinical and tumor characteristics, and quality of life were collected. The primary outcome variable was lumbar spine (LS) BMD at 6 months. Secondary outcomes were LS spine BMD at 12 months, other BMD sites, markers of bone resorption and formation, and predictors of bone loss. A linear mixed model analysis was performed with SAS version 9. Results: Of 122 women randomized, 104 completed the 6 month and 94 the 12 month evaluations (retention 85% and 77%, respectively). The remaining women withdrew before completion, but none due to toxicity. Baseline characteristics were evenly distributed between groups. Mean age was 42 years. No renal or other toxicities were observed in either group. Chemotherapy without zoledronic acid was associated with signi¿cant decline in LS BMD after both 6 (2.4%) and 12 (4.1%) months. Similarly total hip (TH) BMD declined by 0.8% at 6 months and 2.6% by 12 months.in In contrast, BMD remained stable in zoledronic acid-treated patients (P<.0001 compared with chemotherapy alone). Markers of bone turnover are being analyzed and will be presented. Conclusions: Chemotherapy was associated with signi¿cant bone loss in the lumbar spine and total hip in premenopausal women with breast cancer. Zoledronic acid 4 mg every 3 months effectively prevented bone loss. Additional analyses are planned to determine whether the onset of chemotherapy-induced menopause inÀuences which patients bene¿t the most from early initiation of concomitant bisphosphonate therapy for prevention of bone loss. Regular BMD measurements should be considered for premenopausal women undergoing chemotherapy for invasive early stage breast cancer. Abstracts – Poster Discussion Sessions 507 Differential effects of doxorubicin and zoledronic acid on intra-osseous vs extra-osseous breast tumour growth LQ YLYR. Ottewell PD, Deux B, Monkkonen H, Cross SS, Coleman RE, Clezardin P, Holen I. University of Shef¿eld, Shef¿eld, Yorkshire, United Kingdom; Faculte de Medicine Laennec, Lyon, France Introduction: Breast cancer patients with bone metastases are commonly treated with chemotherapeutic agents such as doxorubicin (dox), as well as zoledronic acid (zol) to control their bone disease. Sequential administration of dox followed by zol has been shown to increase tumour cell apoptosis in vitro . We have, therefore, investigated the antitumour effects of clinically relevant doses of these drugs in a mouse model of breast cancer bone metastasis. Methods: MDA-MB-231/BO2 (BO2) cells were injected via the tail vein into athymic mice. Tumour-induced osteolytic lesions were detected in all animals following x-ray analysis 18 days after tumour cell inoculation (day 18). Mice were then administered saline, 100?g/kg zol, 2mg/kg dox, dox and zol simultaneously, or dox followed 24h later by zol. Dox treated animals received a second injection on day 25, and all animals were sacri¿ced on day 32. Tumour growth in the marrow cavity and on the outside surface of the bone was measured on 4 non-serial histological sections. Apoptosis and proliferation were assessed at both sites following immunohistochemistry for caspase 3 and BrdUrd, respectively. Effects of treatments on bone were evaluated following X-ray and µCT analysis. Results: Animals treated with zol, alone or in combination with dox, had signi¿cantly smaller tumour-induced osteolytic lesions compared with control (saline) or dox treated animals. In addition, sequential treatment with dox then zol caused a signi¿cant inhibition of intraosseous tumour growth compared with control, either drug alone, or simultaneous treatment with dox and zol. The reduced intra-osseous tumour volume was associated with an increase in tumour cell apoptosis, and a decrease in tumour cell proliferation. Extra-osseous tumour growth was unaffected in all treatment groups. Conclusions: Sequential treatment with clinically relevant doses of dox followed by zol reduces intra-osseous but not extra-osseous growth of BO2 breast tumours in long bones of immunocompromised mice. 508 Survival in breast cancer patients with bone metastases and reductions in markers of bone resorption during zoledronic acid treatment. Lipton A, Cook R, Major P, Smith M, Coleman R. Milton S. Hershey Medical Center, Hershey, PA; University of Waterloo, Waterloo, ON, Canada; Juravinski Cancer Centre, Hamilton, ON, Canada; Massachusetts General Hospital Cancer Center, Boston, MA; University of Shef¿eld, Shef¿eld, United Kingdom Background: Most breast cancer patients (pts) with bone metastases receive bisphosphonates, which can lower their levels of biochemical markers of bone metabolism. Pts with bone metastases and high levels of N-telopeptide of type I collagen (NTX) are likely to experience skeletalrelated events (SREs) and reduced survival. The purpose of this study was to assess whether zoledronic acid (ZOL)-mediated reductions in NTX levels correlate with long-term bene¿ts. This post hoc analysis investigated whether early (3-mo) suppression of NTX levels during ZOL therapy correlate with prolonged survival and a reduced risk of SREs in pts with breast cancer. Material and Methods: This was a subset analysis of breast cancer pts enrolled in a phase III randomized trial comparing intravenous ZOL with pamidronate in pts with bone lesions from breast cancer or multiple myeloma. Urine was obtained as a morning second-void sample, and NTX levels were corrected according to creatinine (CRE) levels. NTX levels ≥64 nmol/mmol CRE were considered elevated. Pts with breast cancer who received ZOL and had NTX assessments at baseline and mo 1 and 3 (n=328) were included in this analysis. The correlation between changes from baseline NTX level at 3 mo and the following time-dependent variables were modeled: bone lesion progression, skeletal-related events (SRE), and survival. Results: Median NTX level at baseline was 77 nmol/mmol CRE (25th S39 percentile = 50 nmol/mmol CRE and 75th percentile = 127 nmol/mmol CRE). Baseline NTX was elevated in 196 (60%) pts. Of these pts, 149 (76%) normalized NTX after 3 mo of ZOL, and 31 (16%) pts still had elevated NTX at 3 mo. Median survival was approximately 50% longer and the risk of SREs approximately 50% lower for pts whose NTX normalized compared with pts whose NTX remained elevated (P=.0004 and P=.0034, respectively). In all pts, the percentage reduction in NTX level versus baseline corresponded with continuous decreases in the risk of SREs, death, and bone lesion progression. ZOL decreased NTX levels by ≥40% versus baseline at the 3-mo assessment in 80% of pts. In models correlating NTX reductions with bone lesion progression for patients with different baseline NTX levels, a ≥40% reduction was associated with a signi¿cant 32% (25th percentile baseline NTX), 34% (median baseline NTX), or 39% (75th percentile baseline NTX) decrease in risk of bone lesion progression compared with similar pts without a 40% reduction (P<.05 for each). Discussion: These results suggest that early normalization or reduction of elevated baseline NTX while receiving ZOL is associated with improved SRE-free and overall survival compared with persistently elevated NTX. Further analyses of NTX kinetics in patients with breast cancer are warranted. 509 Effects of zoledronic acid on wnt inhibition by dickkopf1 and frizzled-related protein in patients with bone metastases. Helsten TL, Mortimer JE, Corr M. Moores UCSD Cancer Center, La Jolla, CA; University of California, San Diego, CA Background: Data from mice and humans suggest that wnt/frizzled signaling is important for skeletal development and regulation of adult bone mass. There are two types of soluble inhibitors of wnt signaling: dickkopf1 (DKK1) and frizzled-related proteins (FRP). In multiple myeloma, serum DKK1 levels correlate with the burden of lytic bone lesions, but no such data are known for solid tumors. Breast cancer is primarily osteolytic, but may be osteoblastic or mixed, while prostate cancer is osteoblastic. We explored the wnt antagonists DKK1 and FRP as potential biomarkers in patients with bone metastasis from breast or prostate cancer and their response to treatment with zoledronic acid (ZA). Methods: This is a cohort study of bisphosphonate naïve breast and prostate cancer patients with bone metastases. Anti-cancer therapy was not speci¿ed. Sera were collected at baseline and at day 60 after treatment with 2 monthly doses of ZA (4 mg IV) for measurement of DKK1, FRP, and bone-speci¿c alkaline phosphatase (BAP, a standard marker of bone turnover and osteoblast activity) using standard ELISA protocols. Primary endpoints: mean changes in serum DKK1 and FRP. Secondary endpoints: correlation of markers with each other and comparison of breast vs. prostate cancer patients. Statistics: two-tailed student t-tests and Pearson correlation coef¿cients. Results: The cohort included 20 patients: 11 with breast and 9 with prostate cancer. Mean age = 61 years (range 42-79). Three breast cancer patients were premenopausal. Four breast and 4 prostate cancer patients received chemotherapy; all others were treated hormonally. Pretreatment BAP was higher in prostate than breast cancer patients (mean 107.0 mg/dl vs. 35.5 mg/dl). As expected, ZA decreased BAP in all but one patient (mean decrease 24.83 mg/dl, 95%CI -3.71 to 53.37). There was no clear trend in DKK1 (mean change -0.08 mg/dl, 95%CI -8.38 to 8.21) or FRP (mean change -6.31 mg/dl, 95%CI -14.85 to 2.23), nor any apparent difference between breast and prostate cancer. DKK1 and FRP tended to change in the same direction (15/20 patients), but not linearly (p = 0.1). Pretreatment DKK1 and FRP correlated with each other (r2 = 0.26, p = 0.02), but not with BAP. Post-treatment DKK1 correlated with BAP (r2 = 0.41, p = 0.002), while FRP did not (r2 = 0.01, p = 0.7). ZA treatment abrogated the correlation between DKK1 and FRP (r2 = 0.19, p = 0.06). Conclusions: Both DKK1 and FRP are present in the sera of patients with bone metastases and treatment with ZA has measurable effects on their levels. While DKK1 and FRP correlated with each other moderately well at baseline and tended to change in the same direction after ZA, DKK1 more than FRP seems to correlate with bone turnover S40 Abstracts – Poster Discussion Sessions after ZA treatment (as measured by BAP). These pilot data suggest that bisphosphonates may have an effect on wnt inhibition, though the effects of concurrent anti-cancer treatment and disease response are not known. Further studies are needed. 510 Zoledronic acid as adjuvant therapy for women with early stage breast cancer and occult tumor cells in bone marrow. Lin A, Park J, Melisko M, Goga A, Moasser M, Moore D, Brissaud C, Rugo H. University of California-San Francisco, Comprehensive Cancer Center, San Francisco, CA Background: The presence of occult tumor cells (OTC) in the bone marrow (BM) is associated with an increased risk of distant recurrence and death from cancer in women with early stage breast cancer (BC), particularly when these cells are detected after completion of adjuvant systemic therapy. Bisphosphonates have the potential to act as antitumor agents by a variety of mechanisms including induction of tumor cell apoptosis. Adjuvant clodronate in women with OTC at BC diagnosis reduced the incidence of osseous and non-osseous metastasis and improved survival. Zoledronic acid is signi¿cantly more potent that clodronate in inhibiting bone resorption. We are conducting a pilot study to evaluate the effects of zoledronic acid in women with early stage BC with OTC following systemic chemotherapy (CTX). We hypothesize that treatment with zoledronic acid will result in decrease in OTC which could serve as a surrogate marker of anti-tumor effect. Methods: OTCs are detected by immunomagnetic enrichment + Àow cytometry (FC) as follows: 4 ml of BM aspirate was subjected to anti-EpCAM-conjugated iron particles, followed by FC for EpCAM, CD45, and nucleic acid content for quantitative analysis of OTC per ml. Patients (pts) with stage I-III BC are evaluated for OTC with a unilateral BM aspiration following neoadjuvant or adjuvant CTX; eligibility was de¿ned as >4 OTC/ml within 12 weeks of study entry. This cutoff is de¿ned as > 2.5 standard deviations above that found in 50 normal BM samples (Park, Proc ASCO 2002). Pts receive 4 mg of zoledronic acid IV monthly for 2 years. Concomitant hormone therapy was allowed. Serum creatinine and toxicity are evaluated monthly and urinary n-telopeptide is measured at 0, 2, 4, 6, 12, and 24 months (mos). Repeat BM aspirations are performed at 1 and 2 years. Results: 44 pts are enrolled in this study. We report an interim analysis of baseline and one year BM results. The mean OTC at baseline is 25.6 OTC/ml (range 5-332 OTC/ml), and the mean follow-up period is 16.2 mos (range: 1 to 31 mos). Baseline OTC >30 OTC/ml predicts for distant recurrence (p=0.007). 26 pts have received more than 12 mos of zoledronic acid and 22 have had BM aspirations at 1 year. 16/22 pts (73%) had a decrease in OTC from baseline to 1 year (p=0.013). To date, only 9 pts have had BM aspirations at 2 years. Five breast cancer recurrences occurred during the ¿rst year of study enrollment (average time to recurrence 5.2 mos); all pts were node positive, and negative for ER, PR, Her2/neu. Zoledronic acid was well tolerated with only 1 pt discontinuing study treatment due to side effects. Discussion: Serial detection of OTC in BM is feasible in women with early stage BC. High baseline BM OTCs predicted for early recurrence in women with high risk disease. This preliminary data suggests that zoledronic acid may decrease the number of OTC at one year, and this treatment was well tolerated. The study is ongoing, updated data will be presented. 511 Effect of zoledronate on persisting isolated tumor cells in the bone marrow of patients without recurrence of early breast cancer. Rack BK, Jueckstock J, Genss E-M, Schoberth A, Schindlbeck C, Strobl B, Heinrigs M, Rammel G, Zwingers T, Sommer H, Friese K, Janni W. Ludwig-Maximilians-University, Munich, Germany; Laboratory Drs. Tiller and Partners, Munich, Germany; Estimate GmbH, Augsburg, Germany 3XUSRVH Recently, the highest level of evidence was reached for the prognostic impact of isolated tumor cells (ITC) in bone marrow of breast cancer pts both at primary diagnosis and during recurrence-free follow-up. Chemotherapy seems to have only limited effect on ITC in dormant state. The goal of the present study is to investigate the therapeutic ef¿cacy of zoledronate on the persistence of ITC in the bone marrow of breast cancer pts after completion of primary therapy. 0HWKRG We followed 172 breast cancer pts without evidence for distant recurrence but detection of ITC in bone marrow. As part of an interventional pilot study, zoledronate was applied at 4mg q4wx6mon (loading dose 8mg) to 31 pts who had completed surgery, leading to R0 resection of their tumor, and adjuvant chemotherapy for at least 6 months. In a matched pair analysis, these pts were compared to those 141 pts, who were treated according to standard guidelines but did not receive additional zoledronate treatment. The bone marrow was re-examined after a median of 7.9 months (std .89) in the treatment group and 11.5 months (std 12.41; P=.11) in the control group. ITC were detected by immunocytochemical staining using the monoclonal pan-cytokeratin antibody A45-B/B3 and the APAAP technique. Pts were followed prospectively for a median of 39 months following the ¿rst aspiration. 5HVXOWV Primary tumor characteristics, i.e. tumor size (P=.09), axillary nodal status (P=.85), hormone receptor status (P=.67) and grading (P=.35), as well as surgical (P=.22), adjuvant systemic (P=.18) and irradiation treatment (P=.51) were well balanced between both pt groups. While ITC were detected in all 172 pts at the time of ¿rst bone marrow aspiration, four pts (13%) showed ITC following 6 months of zoledronate therapy. In contrast, persisting ITC were detected in 38 pts (27%) of the control group without zoledronate treatment (P=.099). The reduction in cell numbers between ¿rst and second aspiration reached statistical signi¿cance in the zoledronate group (P=.02) in contrast to control pts (P=.14). Persistent ITC at the follow-up aspiration were associated with reduced RFS (P=.05). Among 12 pts without detection of ITC in bone marrow after treatment who underwent additional aspirations, 10 pts showed a persistently negative bone marrow status after a median of 19 months (range 4.7-38.7 mon) following treatment. Zoledronate treatment was well tolerated with mild bone pain as the most common side effect in 45% of pts (n=14). &RQFOXVLRQ These results indicate a potential antineoplastic effect of the cell-cycle independent agent zoledronate on persisting ITC in dormant state. Our data provide a hypothesis generating basis to investigate the therapeutic ef¿cacy of zoledronate on ITC in the secondary adjuvant setting by prospectively randomized trials. Abstracts – Poster Session I 1001 Effect of magnetic resonance imaging on the clinical management of women with newly diagnosed breast cancer. Newstead GM, Abe H, Jansen SA, Shimauchi A, Sennett CA, Schmidt RA, Zak L, Olopade O, Jaskowiak N. University of Chicago; University of Chicago, Chicago, IL Background: Magnetic resonance imaging (MRI) has been shown to identify multifocal, multicentric and contralateral breast cancer, not identi¿ed by clinical examination, mammography and ultrasound. Although the biological importance of additional areas of disease identi¿ed by histopathology has been questioned, we sought to evaluate the contribution of MRI to the initial staging of newly diagnosed breast cancer patients, and to document the effect of MRI assessment on patient management. Materials and Methods: MRI has been routinely and non-selectively used for breast cancer staging at our institution since 2002. We identi¿ed 459 consecutive patients with 465 newly diagnosed breast cancers who underwent MRI between July 1 2002 and December 31 2006. Excluded were patients with clinical ¿ndings of inÀammatory cancer. All patients were assessed by clinical examination, bilateral mammography (MG) and ultrasound (US) of the affected breast. Location, number and size of the cancers were documented. Mean patient age was 56.5 yrs (range 26-82). Histology of the index lesion: invasive duct carcinoma (IDC) n=201 (43.2%), invasive lobular carcinoma (ILC) n=40 (8.6%), ductal carcinoma-in-situ (DCIS) n=69 (14.8%) and IDC with DCIS n=155 (33.3%). Dynamic bilateral MR contrast-enhanced protocol:1 pre and 4-6 post-contrast images acquired in the coronal or axial plane, with 60-75 s timing. Analysis of lesion morphology and kinetic curve shape was classi¿ed according to the BIRADS lexicon. Location, number and size of unsuspected areas of additional tumor were documented, and classi¿ed according to their location: within the same quadrant (multifocal), within a different quadrant and at least 3 cms away (multicentric), and in the contralateral breast. Patients with positive MR for additional lesions underwent “second look” directed MG and US to search for additional tumor, and selected patients underwent biopsy and/or localization of additional tumor under US or MR guidance. All imaging and histologic ¿ndings were discussed at an interdisciplinary treatment conference. Results: Analysis of the MRI staging data with pathology review, demonstrated secondary disease to be present in 106 (23.1%) patients, mean age 51.2 years (5 years younger than mean age of all). Distribution of additional disease: multifocal n=58 (12.6%), multicentric n=27 (5.9%), contralateral breast n=21(4.5%). Additional cancer histology: IDC n=36 (33.9%), IDC + DCIS n=26 (24.5%), DCIS n=29 (27.4%), ILC n=15 (14.2%). Management change: More extensive cancer surgery with breast conservation n= 86 (81.1%), mastectomy rather than conservation n=10 (9.4%) and Neoadjuvant chemotherapy n=5 (4.7%). Conclusion: MR imaging offers more precise assessment of tumor extent than mammography or ultrasound imaging. Therapeutic management was changed in 23.1% patients (n=106), resulting in a change from breast conservation to mastectomy in 9.4% patients. 1002 Deconvolution-based dynamic contrast enhanced MRI of breast cancer: correlation of tumor blood Àow with pathologic and molecular markers. Makkat S, Fontaine C, Stadnik T, Luypaert R, Bourgain C, De Greve J, De Mey J. UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium Purpose: Characterization of angiogenesis has been performed mostly by in-vitro immunohistochemical evaluation of angiogenic tumor markers. Non-invasive measurement of blood Àow in tumors has potential for assessing changes in angiogenic vasculature because the blood Àow in tumors is usually abnormal. The aim of our study was to test whether breast carcinomas possess characteristic values of tumor blood Àow that correlate with pathologic and molecular prognostic markers. Materials and Methods: 57 patients with carcinoma of the breast (31–80 years; mean 51 years) who underwent mastectomy or wide excision after MR imaging were studied by in-vivo perfusion S41 measurements on a 1.5 T scanner (Philips Intera). The routine MR protocol was ¿rst applied, which included whole breast dynamic contrast enhanced (DCE MR) sequence. The slice in which the lesion enhanced maximally was located by visual inspection of the subtracted DCE MR images. A second bolus of 0.1 mmol/kg Gd-DTPA was injected and a dynamic single slice inversion prepared FLASH acquisition (400 dynamics with a temporal resolution of 0.3s) was performed at that slice position. The relative enhancement time courses of this second bolus sequence were deconvolved pixel wise, to generate the impulse response function, the maximum of which corresponds to tumor blood Àow (TBF). Quantitative value for each patient was derived as the median value of all the pixels in the ROI covering the lesion. Formalin-¿xed, paraf¿n-embedded slides were evaluated for histological size and grade. Tumor samples were stained for estrogen receptor (ER), progesterone receptor (PR) and HER-2 protein by IHC. For an HER-2 protein score of 2+ and 3+, HER-2 gene status was assessed by FISH. For ER, PR and HER-2 gene status, median TBF was compared between positive and negative groups. Results: Signi¿cantly higher TBF was observed in tumors larger than 2 cm in size and in PR negative tumors (p <0.05). In addition, the median TBF values were signi¿cantly higher in the HER-2 positive group (98 ± 37 ml/100ml/min) compared with the HER-2 negative group (71 ± 43 ml/100ml/min) (p <0.05). In both the HER-2 positive and the negative groups, the ER+/PR+ had a lower median TBF compared to the ER-&PR-. This difference was statistically signi¿cant in the HER-2 positive group (p <0.05). Conclusion: Our preliminary results support the hypothesis that there is increased blood Àow in poor prognostic (HER-2 positive and hormone receptor negative) tumors. Moreover, our results also show that a pixel wise deconvolution analysis of DCE MR data in malignant breast tumors can provide pre-operative information regarding the angiogenic status as assessed by the blood Àow. Further validation of perfusion data against clinical and biological parameters could enable TBF to become a noninvasive angiogenic marker that could also be explored in the context of anti-angiogenic therapies for which in vivo biomarkers are currently lacking. 1003 A new approach to studying the progression of mammary gland carcinoma in mice: high resolution MRI of early cancer and DCIS. Jansen SA, Conzen S, Zamora M, Krausz T, Newstead GM, Karczmar GS. University of Chicago Background: Longitudinal studies of the progression of mammary gland carcinoma in mice usually involve large, palpable tumors. For example, in many preclinical evaluations of therapies, a drug is administered to mice with palpable tumors, and subsequent changes in tumor size are measured using calipers. However, these xenografted or transgenic tumors are not necessarily realistic models of human breast carcinoma presentation: 64% of breast cancer patients present with localized cancer, and 15-25% have preinvasive ductal carcinoma in situ (DCIS). Improved imaging is needed to study the full progression from hyperplasia to DCIS to invasive cancerin animals. Thus, the purpose of this study was to develop techniques to study very early breast cancer and its progression in vivo with histopathologic correlation. Materials and Methods: Twelve C3(1) SV40 TAg transgenic mice between 10-18 weeks of age were used. A pair of inguinal mammary glands in each mouse was imaged using a T1-weighted gradient echo (GE) sequence, with and without fat suppression, with 117 micron in plane resolution. H&E sections of the glands were obtained. We used a polyethylene grid embedded in partially deuterated agar to register tissue sections and MR images. On one representative H&E section from each mouse, the tumors and ducts distended with DCIS were identi¿ed by an experienced pathologist. The MR images were examined to see if correlative structures were discernable. Results: GE images were able to detect 1/1 large (∼5mm) tumor, 17/18 small (∼1mm) tumors, and 13/16 ducts distended with DCIS greater than 300 microns (please see ¿gure below). There were no false positives—a clear MR ¿nding corresponded to cancer in all glands. The morphology of DCIS lesions was either linear ductal or stippled, while small invasive tumors appeared as round masses with smooth margins. Discussion: This is the ¿rst report demonstrating in vivo, high resolution S42 Abstracts – Poster Session I imaging of early cancers in mice, including DCIS, with high sensitivity and speci¿city. With these techniques, MRI could be used to study the natural history of experimental breast cancer, and evaluate effects of therapies on localized, non-palpable and spontaneous cancers. These cancers are more realistic models of clinical disease than the larger, often palpable tumors measurable and imaged in pre-clinical studies. Use of MRI to assess the in vivo ef¿cacy of therapies on earlier cancers may in turn lead to more clinically effective therapies. Advances in non-invasive imaging methods, such as those described here, will shift the paradigm for pre-clinical research to detecting and preventing early cancer from progressing. -0.05 to 0.96). A moderate positive linear relationship between MRI and pathologic size was identi¿ed (r=0.665, p<0.001, Figure 1). Discussion: A moderate correlation between post-PIC MRI and pathologic size was identi¿ed, with a trend for MRI to over-estimate pathologic size. 1005 How does ER/PR and Her2/Neu status affect the MR characteristics of invasive ductal carcinoma? 1004 Magnetic resonance imaging in predicting pathologic residual disease after primary induction chemotherapy. Anderson CM, Patrick RJ, Rybicki LA, Chellman-Jeffers M, Obi B, Crowe JP. Cleveland Clinic, Cleveland, OH Background: Magnetic resonance imaging (MRI) is useful to assess response to primary induction chemotherapy (PIC) and to assist in surgical planning. This report assesses the ability of MRI to predict pathologic residual disease after PIC. Materials and Methods: Data were available in our institutional review board approved registry for patients who underwent MRI before and after PIC between April 2004 and December 2006. MRI were performed using the same scanner (HARMONY, Siemens Medical Systems; Erlangen, Germany) with a dedicated breast coil, operating at 1.0 Tesla. Breast radiologists interpreted all MRI using computer-aided detection (Cadstream, Con¿rma, Inc, Kirkland, WA, USA). Radiographic tumor response was assessed using Response Evaluation Criteria in Solid Tumors (RECIST). Longest diameter of the largest lesion on postPIC MRI was compared to subsequent pathologic size of the largest remaining tumor. Data were analyzed using Spearmans correlation (r) and Wilcoxon signed-rank test; a p-value of <0.05 was signi¿cant. Results: Data were available for 30 patients. A majority of patients were premenopausal (67%), TNM Stage IIB-IIIA (70%), and diagnosed with in¿ltrating ductal histology (90%). Most patients (97%) received four cycles of either doxorubicin/cyclophosphamide or epirubicin, either with or without a taxane. Median diameter of largest tumor on pre-PIC MRI was 4.4 cm (range 2.4-14.0). Median diameter of largest tumor on post-PIC MRI was 1.9 cm (range 0-7.4). Evaluation of tumor response on post-PIC MRI showed complete response (rCR) for ¿ve (17%) patients, partial response (PR) for 16 (53%) and stable disease (SD) for nine (30%). Of the ¿ve patients achieving rCR, one had pathologic CR (pCR), three had residual microscopic nests of tumor (near pCR), and one had 0.4 cm residual tumor. Surgery was completed a median of 23 days (range 2-50) after post-PIC MRI. Eighteen (60%) patients underwent modi¿ed radical mastectomy and 12 underwent lumpectomy. Median diameter of largest tumor pathologically was 1.0 cm (range 09.5). Six patients achieved pCR, of whom one had rCR, four had PR, and one had SD on post-PIC MRI. Four patients achieved near pCR, of whom three had rCR and one had SD on post-PIC MRI. Post-PIC MRI measurement over-estimated pathologic size for 57% of tumors; median over-estimation was 0.2 cm (95% con¿dence interval Jansen SA, Abe H, Shimauchi A, Karczmar GS, Newstead GM. University of Chicago, Chicago, IL Background: Dynamic contrast enhanced MRI (DCEMRI) is being used increasingly due to its high sensitivity to breast cancer. DCEMRI provides both morphologic and functional characterization of lesions via contrast media uptake and washout (or ‘kinetic’) curves. Prior reports have linked kinetic curves to underlying lesion vasculature and biology. Molecular markers, such as estrogen receptor (ER), progesterone receptor (PR) and Her2/Neu gene ampli¿cation status, are important for selection of appropriate therapy. They are also related to tumor biology, with Her2/Neu positive and ER negative lesions showing less favorable prognosis. The purpose of our study was to perform a systematic evaluation of the kinetic characteristics of 145 invasive ductal carcinoma (IDC) lesions classi¿ed by ER, PR, and Her2/Neu status. Materials and Methods: 138 patients with 145 histologically proven IDC lesions with known ER, PR and Her2/Neu status were selected for IRB approved review. These lesions were classi¿ed as: ER positive (n=101), ER negative (n=44), PR positive (n=76), PR negative (n=69), Her2/Neu positive (n=25) and Her2/Neu negative (n=120). Dynamic MR protocol: 1 pre and 3-5 post-contrast T1-weighted SPGR sequence with 68 s timing. Analysis of kinetic curve shape was made according to the BiRads lexicon: initial rise (rapid, medium, slow) and delayed phase (persistent, plateau, washout). In addition, several quantitative parameters were derived from the kinetic curves: initial enhancement percentage (E1), the signal enhancement ratio (SER), and the time to peak enhancement (Tpeak). Results: Overall, 92% of lesions showed rapid initial enhancement, and 74% exhibited washout curves. ER negative lesions had a stronger initial enhancement, stronger washout and a shorter time to peak enhancement (E1=351%, SER=1.36, Tpeak=94 seconds) compared with ER positive lesions (E1=286%, SER=1.02, Tpeak=142 seconds), with p values < 0.03 for all parameters. PR negative lesions exhibited a stronger washout (SER=1.25) compared with PR positive lesions (SER=1.01), with p value < 0.01. Kinetic parameters did not differ for Her2/Neu negative and positive lesions. Discussion: The kinetic characteristics of ER and PR positive and negative lesions showed some statistically signi¿cant differences (p <0.03), with ER negative lesions showing the strongest initial enhancement, shortest time to peak enhancement and strongest washout. This suggests that PR and in particular ER status may be related vasculature in a way that Her2/Neu status is not. Abstracts – Poster Session I 1006 Breast density assessment using magnetic tesonance imaging and diffuse optical spectroscopy. Klifa CS, Shah NS, Watkins M, Li A, Hattangadi J, Tromberg B, Hylton N. University of California, San Francisco, CA; University of California, Irvine, CA Background: We studied breast density using Magnetic Resonance Imaging (MRI) and Near Infra-Red Broadband Diffuse Optical Spectroscopy (DOS) to obtain unique information about breast tissue structure and function that may be complementary to mammographic breast density. Breast MRI provides high tissue contrast and three-dimensional characterization of tissue structures. Near-infrared Broadband Diffuse Optical Spectroscopy is a new non-invasive modality that characterizes breast tissue composition and function. The DOS probe is a handheld device that is applied on the breast at several locations. Light absorption and scattering are quanti¿ed at each measurement, at a maximum depth of 2cm. DOS parameters including concentrations of breast total hemoglobin, water, lipid, as well as scatter power (related to the distribution of scatter particle size in tissue) are extracted at each location. The overall goal of our research is to provide a reproducible quantitative technique that could lead to a better understanding of the biological basis of the relation between breast density and cancer risk. If we can explain what biological components in the breast are linked to breast density, using our combination of MRI and DOS, then we may be able to better monitor breast cancer risk by monitoring these components. Method: Twenty nine normal female volunteers were recruited and underwent one DOS scan immediately before or after a non-contrast enhanced breast MRI exam. All volunteers were scanned in the prone position for all scans, in order to facilitate coregistration of both modalities. MR parameters such as Apparent Diffusion Coef¿cient (ADC) and measures of breast density and breast tissue patterns were extracted from all volunteers MRI data. DOS measures were obtained at 8 locations on the surface of the breast, for all volunteers. Results: We evaluated MRI/DOS parameters that may contribute to radiological breast density in the 29 volunteers’ data and found that 1) MR apparent diffusion coef¿cient, 2) MR morphology components related to fat involvement in breast tissue and 3) DOS measures such as Total Hemoglobin and Water contents were very closely correlated with MR breast density, suggesting an association between underlying physiological tissue properties and breast density. Conclusion: The MR quantitative index of tissue patterns strongly translated differences in fat/tissue composition in women with similar MR breast densities, providing a potentially powerful strati¿cation tool. This novel MR index and the combined DOS/MRI measures translating breast density will be further evaluated on larger populations of patients, in particular women taking breast density changing treatments. 1007 MR imaging of tumor response in breast cancer patients following neoadjuvant chemotherapy: correlated with pathological ¿ndings. Chen J-H, Agrawal G, Yu H, Carpenter P, Mehta R, Nalcioglu O, Su M-Y. University of California Irvine, Irvine, CA Background: This study aimed to evaluate the role of MRI in evaluating tumor response of breast cancer following neoadjuvant chemotherapy (NAC) and correlate with ¿nal pathological ¿ndings. Materials and Methods: In a period of three years, ¿fty nine breast cancer patients, including 28 HER-2 positive and 31 HER-2 negative patients, were studied. For 25 HER-2 positive cancer patients , the NAC protocol consisted of 2-4 cycles of bi-weekly AC (Anthracycline (doxorubicin)-Cyclophosphamide), followed by Taxane regimen (TCa ± H), including paclitaxel or Nab-paclitaxel (Abraxane) and Carboplatin, with Trastuzumab (Herceptin), then surgery. For 26 HER-2 negative cancer, the protocol consisted of 2-4 cycles AC (Anthracycline (doxorubicin)-Cyclophosphamide) followed by 3-4 cycles of TCa. Five patients received AC followed by Taxane and three patients received S43 AC regimen only. The clinical stages were stage II (N = 25), stage III (N = 20), and stage IV (N = 14). The tumor size ranged from 0.9 cm to 8.5 cm (median 2.4 cm). The tumor morphologies, divided into four categories, in the baseline MRI and the imaging ¿ndings in the ¿nal MRI after completion of NAC were studied and correlated with the pathological ¿ndings after surgery. Results: Complete clinical response on MRI was identi¿ed in 36 patients (61%). Pathological complete response (pCR) was achieved in 28 patients (47%) and MRI correctly diagnosed 27 pCR (27/36, 75%), including 19 of 20 patients (95%) in HER-2 positive group and 8 of 16 patients (50%) in HER-2 negative group (P < 0.01). High correlation of residual lesion size between ¿nal MRI and pathology was found for the 23 patients showing partial response on MRI (r = 0.986). For comparison of baseline tumor morphologies vs. pCR and non-pCR, and baseline tumor morphologies vs. pathologically positive axillary lymph nodes, they all showed non-signi¿cant difference (P = 0.44 – 1.0). When comparing the pathologically positive axillary lymph nodes versus pCR and non-pCR, a statistically signi¿cant difference was found in the whole patient cohort (P < 0.01) and in Her-2 positive group (P < 0.05) but not in HER-2 negative group (P = 0.401). Conclusion: MRI was an excellent imaging modality in predicting pCR especially with a high accuracy in HER-2 positive patients. The high correlation of lesion size between ¿nal MRI and pathology might help breast surgeons in determining the breast conservation surgery. The tumor morphology in the baseline MRI did not correlate with pathological response after NAC. 1008 The utility of MRI in preoperative planning for breastconserving therapy. Kaufman G, Guth AA, Singh B, Axelrod D, Moy L. NYU School of Medicine, New York, NY Introduction: The use of preoperative MRI is increasing for patients with breast cancer to determine extent of disease and the appropriate surgical approach. However, the impact of MRI on improving surgical outcome is unknown. The goal of this study was to compare the re-excision rates for patients with breast cancer in those who underwent MRI, compared to a matched control group who did not undergo preoperative MRI. The conversion rate from BCT to mastectomy has been used as a surrogate marker for ptient outcome. Objective criteria such as re-excision rates and margin width have not been widely investigated. Methods: Retrospective study of patients undergoing preoperative MRI with initial plan for BCT, from 2002-2006. Re-excision rates were compared to a control group selected from the same time period undergoing evaluation for BCT. Results: 70 patients underwent preoperative MRI. The re-excision rates were similar for both groups (Table 1). The conversion rate from BCT to mastectomy was higher in the control group: 14% vs. 9%. Negative margin rates were similar between the two groups, however the MRI group had a lower incidence of close surgical margins. The percentage of patients who ultimately underwent mastectomy was the same in both groups. Conclusions: Women undergoing preoperative MRI in this study had an increased rate of successful BCT, and a decreased incidence of multiple re-excisions followed by mastectomy. Pre-operative MRI in planned breast-conserving therapy Characteristic MRI Group Study group(# patients) 70 Initial # patients undergoing BCT/mastectomy 52(74%)/18(26%) No. undergoing re-excision 14(30%) Re-excision/DCIS 5(35%) Re-excision/invasive cancer 1(8%) Re-excision/mix DCIS-invasive cancer 8(57%) Conversion BCT to mastectomy 4(9%) Total # mastecomies 22(30%) Control Group 57 48(84%)/9(16%) 21(37%) 6(31%) 3(16%) 11(52%) 8(14%) 17(30%) S44 Abstracts – Poster Session I 1009 Does MRI improve chances of obtaining negative surgical margins after localized excision? A retrospective study. Kulkarni K, Newstead GM, Jansen SA, Abe H, Shimauchi A, Schmidt RA, Jaskowiak N. University of Chicago, Chicago, IL Background: Dynamic contrast enhanced MR imaging (DCE-MRI) of the breast has been shown to have high sensitivity to breast cancer, with lower speci¿city. The role of DCE-MRI in patient management is not well-established. Some advocate DCE-MRI for every cancer patient, while others favor use of breast MRI in more restricted circumstances, such as evaluation of treatment response. Here, the purpose was to determine the role of DCE-MRI in achieving negative surgical margins. The study was designed to compare positive surgical margin rate in patients who underwent DCE- MRI in conjunction with conventional mammography and ultrasound to the positive surgical margin rate published in the surgical literature using conventional imaging alone. Materials and Methods: A retrospective analysis of 168 women (mean age 60.3 yrs, range 35-92) with breast cancer presenting to evaluate for extent of malignant disease from September 2002 to June 2006 was performed. A total of 64 women that underwent modi¿ed radical mastectomy were excluded from the study. The remaining 104 women underwent localized excision of breast cancer following DCE-MRI evaluation. Surgical margins were assessed by dedicated pathologists and were categorized using the same criteria as in the literature: free (>2mm), very close (>0≤1mm), close (>1≤2mm) and positive. These cases were further classi¿ed based on their histological subtypes as: 33% in¿ltrating ductal carcinoma (IDC), 46% IDC with ductal carcinoma in situ (DCIS), 12% DCIS, 8% in¿ltrating lobular carcinoma (ILC) and 1% ILC with DCIS. The size of the index lesion obtained from mammogram and breast MRI were compared to assess the total extent of disease. Results: The surgical margins were positive in 5% (n=5), very close (>0≤1mm) in 13.4% (n=14), close (>1≤2mm) in 9% (n=9) and free in 73% (n=76) of cases. Out of the 5 cases with positive margins, the histological subtypes were: 1 ILC only, 3 IDC with DCIS and 1 ILC with DCIS. Out of the14 cases with very close (>0≤1mm) margins, 7% (n=1) were DCIS only, 43% (n=6) were IDC with DCIS, 36% (n=5) were IDC, 14% were (n=2) ILC. At our institution, one of the criteria for re-excision in cases of DCIS alone is distance from the tumor margin ≤1mm, and thereby the true re-excision rate is 6% (5 with positive margins + 1 with very close margin with DCIS alone, out of 104). The extent of disease was larger on the MRI than the mammogram in 61%, comparable in 9%, and smaller on MRI in 23% of cases. Conclusion: The true re-excision rate was 6% which is signi¿cantly less than previously published values that range from to 15 to 63% in the surgical literature. These results demonstrate a pivotal role of DCE-MRI in effective patient management by signi¿cantly reducing re-excision surgeries for residual disease. An effort to compare the current re-excision rate at University of Chicago with the re-excision rate before the advent of routine preoperative DCE-MRI at the same institution will be made in near future. 1010 The role of breast MRI in the preoperative evaluation of patients with newly diagnosed breast cancer. Schell AM, Kaufman PA, Lewis PJ. Dartmouth-Hitchcock Medical Center, Lebanon, NH Introduction: MRI is being increasingly used in the preoperative evaluation of patients with biopsy-proven breast cancer. We performed a prospective study of the diagnostic utility of breast MRI in a rural tertiary referral setting. Methods: All patients between September 2005 and December 2006 with a new diagnosis of invasive breast cancer who underwent bilateral breast MRI preoperatively at a single institution were enrolled in the study. All gadolinium-enhanced breast MRI scans were performed on a 1.5T magnet; during the initial six months of the study contralateral and ipsilateral breasts were scanned on separate days, in the remaining patients both breasts were scanned on one occasion. All studies were interpreted by 4 experienced mammographers and image data entered into a Filemaker Pro® database at the time of the scan. Patients were managed according to imaging and clinical data. Analyzed data included additional imaging and biopsies performed based on the MRI scan ¿ndings, ¿nal surgical management, and pathological correlation on a lesion by lesion basis. Results:Two hundred and thirteen patients had ipsilateral breast MRI, 206 of these also had contralateral scans. Ipsilateral breast: One hundred and ¿ve BIRADS category 3,4 or 5 lesions were found in addition to the known malignancy in 83 patients (39%). Thirteen percent of patients required an additional ipsilateral biopsy as a result of the MRI, some additional lesions were excised at the time of the primary lesion excision. Fifty-eight lesions in 46 (22%) patients were found to be malignant. An additional two lesions were isolated high risk. Twenty percent of lesions were not biopsied or follow up is not available. Contralateral breast: Fifty-two BIRADS category 3,4 or 5 lesions were found in 41 (21%) patients. Twenty-nine (15%) patients had 33 contralateral lesions biopsied, and of these, 11 lesions in 9 (5%) patients were malignant and 5 lesions were high risk. No pathology is available on 29 lesions. In total, 20% of patients needed additional (mammographic/ultrasound) imaging as a result of the MRI. MRI detected 69 additional cancers in 53 (23%) patients. 80% of these malignancies were invasive. The false negative rate is not currently known, only one BIRADS 3 lesion was found at a biopsy after the six- month follow up to be DCIS. Conclusion: Breast MRI clearly detects unsuspected malignant lesions in both the ipsilateral and contralateral breasts in patients with a new diagnosis of breast cancer in this single instutional study. How this, and how the signi¿cant false positive rate impacts the ¿nal surgical and medical management, is currently being investigated. 1011 Comparative accuracy of MRI and ultrasound for predicting breast cancer extent after neoadjuvant chemotherapy. Karuna ST, Wechter DG. Virginia Mason Medical Center, Seattle, WA Background: Neoadjuvant chemotherapy is utilized to reduce breast cancer size and allow a patient to undergo a lesser procedure, either partial mastectomy instead of mastectomy, or a smaller excision with partial mastectomy. There is little consensus regarding the best imaging modality to predict the post-treatment extent of breast cancer. Various imaging techniques such as MRI, mammography, and ultrasound have been used. Although MRI sensitivity and speci¿city compare favorably with clinical breast exam and mammography, its accuracy compared to ultrasound is less clear. Operative planning depends upon the residual tumor size, so accurate measurement with imaging is crucial. Material and methods: A retrospective review from January 2001 to October 2006 included 44 patients with invasive breast cancer treated with neoadjuvant chemotherapy and imaged with post-treatment MRI, ultrasound, or both. Most patients received four cycles of doxorubicin and cyclophosphamide and four cycles of taxane-based therapy. Operation was performed less than eight weeks after imaging. Results: Thirty-nine tumors were evaluated with ultrasound, and 24 with MRI. For all tumors, correlation between tumor size on imaging and pathology showed an r-value of +0.65 (p<0.005) for ultrasound and +0.47 for MRI (p<0.005). For patients with invasive ductal carcinoma only, r= +0.79 and +0.75 for MRI and ultrasound, respectively (p<0.005 for both). Though the sample size was small, for patients with invasive breast cancer with lobular features, MRI and ultrasound both demonstrated poor correlation, r= -0.23 (p=0.5517) and r= +0.31 (p=0.3537) respectively. Conclusion: Ultrasound may be more accurate than MRI in prediction of residual tumor size after neoadjuvant chemotherapy. Although the data cannot support eliminating the use of post-treatment MRI, in cases of discrepancy between MRI and ultrasound, perhaps more attention should be paid to the ultrasound prediction in surgical planning. Further study of a larger group of patients is needed to better assess the comparative accuracy of ultrasound and MRI in patients who have received neoadjuvant chemotherapy, especially those with lobular features. Abstracts – Poster Session I Assessment of Breast Cancer Extent Post-Neoadjuvant Chemotherapy: Correlation Between Breast Imaging and Final Pathology PATIENT POPULATION IMAGING MODALITY R-VALUE All study patients MRI +0.47 All study patients Ultrasound +0.65 Study patients with invasive MRI +0.79 ductal carcinoma only Study patients with invasive ductal carcinoma only Study patients with invasive breast cancer with lobular features Study patients with invasive breast cancer with lobular features P-VALUE <0.005 <0.005 <0.005 Ultrasound +0.75 <0.005 MRI -0.23 0.5517 Ultrasound +0.31 0.3537 1012 Accuracy of preoperative evaluation of the axilla with MRI in breast cancer. Kaufman G, Guth AA, Axelrod D, Moy L. NYU School of Medicine, New York, NY Background The ability to assess axillary lymph node involvement in patients undergoing surgery for invasive breast cancer can lead to changes in their surgical management. Traditional imaging modalities such as ultrasound have been used with increasing success in the preoperative evaluation of the axilla. The increasing use of MRI in the preoperative evaluation of patients undergoing surgery for breast cancer may impact axillary evaluation and inÀuence surgical decision making. The ef¿cacy of conventional MRI for this evaluation has not been fully evaluated. The goal of this retrospective analysis was to determine the sensitivity of breast MRI in the detection of metastatic lymph node involvement and to determine if surgical management is altered. Methodology Patients undergoing preoperative MRI were identi¿ed from a radiology/ pathology database from 2002-2006. The rates of sentinel lymph node and axillary dissection and conversion to axillary dissection in the MRI group were compared to a control group selected from patients undergoing breast conserving therapy during a similar time period. Statistical analysis used Chi-square test. Results A total of 63 patients had preoperative MRI and underwent lymph node dissection. The sensitivity and speci¿city of MRI for detecting metastatic disease involving the lymph nodes was 33% and 94% respectively. MRI had a positive predictive value of 80% and a negative predictive value of 68%. A fewer number of patients in the MRI cohort (6%) had initial axillary dissection compared to the control group (13%). However, a greater percentage of patients in the MRI cohort (28%) compared to control group (20%) converted from sentinel lymph node biopsy to completion axillary dissection. Therefore the rates of axillary dissection were similar in both groups. The rate of micrometastatic disease approached 10%. Conclusions The evolving applications of MRI in the evaluation of patients with breast cancer are increasing. The ability of MRI to accurately predict size and detect synchronous lesions in patients with known invasive cancer has been sufficiently demonstrated. The efficacy of MRI to stage the axilla of patients with breast cancer has not yet been demonstrated. Continued research involving speci¿c protocols for axillary evaluation and the use of speci¿cally designed MRI breast coils for this purpose may enhance its overall ef¿cacy. Although breast MRI has a high speci¿city for the evaluation of axillary lymph nodes, the poor sensitivity makes this modality unreliable for screening the axilla for metastatic involvement prior to surgery. The lack of sensitivity may be due to the subset of patients that present with micrometastatic disease. 1013 Model selection for analysis of dynamic contrast enhanced MRI (DCE-MRI) data. Yankeelov T, Welch EB, Chakravarthy B, Lee R, Freehardt D, Mayer I, Meszoely I, Kelley M, Means-Powell J, Gore J. Vanderbilt University, Nashville, TN; Philips Medical Systems, Cleveland, OH Background: DCE-MRI is the acquisition of MR images before and after an intravenous injection of contrast agent (CA). By ¿tting S45 DCE-MRI data to a model, physiological parameters such as vessel perfusion (Ktrans) and extracellular volume fraction (ve) are extracted [1]. In diagnosing breast cancer, DCE-MRI is shown high sensitivity (77-100%), but moderate speci¿city (26-97%) [1]. A possible reason is that the standard model used to analyze such data may not describe the relevant physiology. The standard model relies on a linear dependence between the MRI signal intensity and the concentration of CA in tissue [2]. This model assumes that tissue is effectively one compartment; in MRI, this assumption is referred to as the fast exchange limit (FXL). Studies have shown this assumption is violated in vivo [2]. By accounting for the effect of the intra- and extracellular compartments a “fast exchange regime” (FXR) model is obtained which has revealed errors of up to 200% in the FXL [2]. Through two common statistical tests, we show that the FXR is the preferred model. As DCE-MRI ultimately aims to positively impact clinical decisions, model choice is important. Methods: 10 patients with locally advanced breast cancer underwent DCE-MRI (at 3.0T) prior to neoadjuvant chemotherapy. DCE-MRI data were analyzed on a voxel basis by the (standard) FXL and (new) FXR models to return estimates of Ktrans and ve. The Durbin-Watson statistic (a well-known test for detecting serial correlation) was computed for the residuals returned from both models for each voxel. Percentage of voxels showing serial correlation by each method was tabulated. Additionally, the Akaike Information Criteria (AIC) was computed for each voxel. Given a set of models, the AIC determines the model that best balances complexity with goodness of ¿t. Results: The FXR analyses of the DCE-MRI data resulted in a signi¿cant reduction in percentage of voxels showing serial correlation of residuals: 42.6% +/- 12.6% and 21.5% +/- 7.7% for the FXL and FXR, respectively (P=0.0002). In 99% of voxels, the AIC indicated that the FXR model was superior. This translated into signi¿cant differences in parameters extracted: 0.43 min-1 +/- 0.22 min-1 (FXR) versus for 0.25 min-1 +/- 0.10 min-1 (FXL) for Ktrans (P<0.04), and 0.33 +/- 0.08 (FXR) versus 0.12 +/- 0.05 (FXL) for ve (P<0.00001). Discussion: The parameters Ktrans and ve are studied to both diagnose and assess treatment response in breast cancer. The values extracted are determined by which model is selected. We have shown here that the FXR model is statistically superior as quanti¿ed by both the DurbinWatson statistic and the Akaike Information Criteria. An ongoing clinical trial is examining whether the FXR is superior to the FXL in predicting pathologic outcome in patients undergoing neoadjuvant chemotherapy. References: 1. Beatty et al, AJS2007:193;600-5. Yankeelov et al, MRM2003:50;1151-69, 3. Li et al, ISMRM2007;141. 1014 Are the MRI characteristics of malignant breast lesions different for African American women? Jansen SA, Abe H, Shimauchi A, Karczmar GS, Olopade O, Newstead GM. University of Chicago, Chicago, IL Background: Disparities in breast cancer mortality and stage at diagnosis between African American and Caucasian women has been a topic of recent interest, with evidence to suggest earlier onset of more aggressive cancer in African American women. This disparity has been attributed to differences in quality of medical care and genetic background. Dynamic contrast enhanced MRI (DCEMRI) of breast cancers is being used increasingly due to its high sensitivity and accuracy in determining extent of disease. DCEMRI provides both morphologic and functional lesion characterization via contrast media uptake and washout (or ‘kinetic’) curves, which are related to tumor blood Àow. The purpose of this study was to compare the MR presentation of malignant breast lesions in African American and Caucasian women. Materials and Methods: 108 patients with 122 histologically proven malignant lesions were selected for review:51 African American patients with 59 lesions (average age 58 yrs) and 57 Caucasian women with 63 lesions (average age 55 yrs). The malignant lesions were classi¿ed as ductal carcinoma in situ (DCIS), invasive ductal carcinoma (IDC), invasive lobular carcinoma (ILC) and ‘other’. The number of IDC lesions positive for Her2/Neu overexpression was determined. Dynamic MR protocol: 1 pre and 5 post-contrast images using a T1weighted SPGR with 68 sec timing. Analysis of kinetic curve shape and morphology was made by an experienced radiologist, and several S46 Abstracts – Poster Session I quantitative parameters were derived from the kinetic curves. Results: Overall, there were 62 IDC, 38 DCIS, 12 ILC and 10 ‘other’ malignant lesions. The predominant MR morphology was homogeneous or heterogeneous mass-like enhancement, in a round or irregular shape. The mean lesion size was 2.1 cm. There was no difference in the morphology, size or kinetics of malignant lesions by race. When considering only IDC lesions, again no signi¿cant differences in morphology, size or kinetics by race were demonstrated. Her2/Neu was overexpressed in 19% (6/31) of IDC lesions in African American women, and 16% (5/31) of Caucasians. Discussion: Despite recent evidence of racial disparities in breast cancer stage at diagnosis, in our study, we found no difference in the lesion size, MR morphologic or kinetic presentation of malignant lesions between African American and Caucasian women. In addition, similar numbers of African American and Caucasian women demonstrated overexpression of Her2/Neu. At our institution, comparable numbers of African American and Caucasian women present for diagnostic breast evaluation, implying a similar level of care upon which biological differences can be explored. Our results indicate that newly diagnosed breast cancers in African American and Caucasian women share many similarities. This points to future work on follow-up of the ef¿cacy of treatment and survival in these patients. 1015 Pushing the limits: very high spatial resolution spectroscopic MR imaging of human breast. Medved M, Newstead GM, Abe H, Wood AM, Olopade OI, Shimauchi A, Fischer S, Karczmar GS. University of Chicago, Chicago, IL; Philips Medical Systems, Cleveland, OH Background: MRI is increasingly used for breast cancer screening. However, further improvements in specificity are needed. This laboratory has proposed use of high spectral and spatial resolution (HiSS) imaging of water and fat proton resonances at the spatial resolution of conventional anatomic MR images. HiSS images offer complete fat suppression across the entire breast and excellent image contrast for maximum sensitivity and speci¿city for small breast lesions. In addition, analysis of the spectral line shapes of water and fat signal provides new sources of image contrast that may increase speci¿city. Previously reported HiSS images were produced in 2 mm thick slices with 1 mm in-plane resolution. Here we report HiSS images with halfmillimeter spatial resolution in 1 mm thick planes. The images show increased anatomic detail with adequate signal-to-noise ratio. Materials and Methods: Four women were scanned with informed consent on a Philips Achieva 1.5T scanner, using an echo-planar spectroscopic imaging-based sequence. The water and fat spectra in each 0.5 x 0.5 mm voxel in 1 thick mm slices, were obtained at the spectral resolution of approximately 5 Hz. This allowed post-processing of spectral data through ¿tting the water and fat peaks, complete separation of water and fat signal, and generation of water resonance peak height images with a combination of T1 and T2 weighting. Three to four slices were acquired in 8 minutes for each patient. Results: Figure 1 shows a typical spectroscopic water peak height image obtained with our technique. Water peak height images were produced with acceptable signal-to-noise ratio, high dynamic range, and complete separation of water and fat signal. The data may allow high-resolution B0 mapping - possibly sensitive to calci¿cations. The water peak height images show parenchyma clearly against a dark background of highly-suppressed fat signal. Discussion: These results demonstrate that HiSS imaging is feasible with 0.5 x 0.5 mm in-plane resolution, 1 mm thick slices, and clinically reasonable run-times. Predictable improvements in technology (e.g. higher ¿eld strength, improved detectors) will result in even better SNR, faster acquisition times, and/or higher spectral resolution. The spectroscopic information can in principle be used to obtain highresolution B0 maps, and to visualize micro-calci¿cations via distortions in the B0 ¿eld. This is a novel approach to MRI of the breast that is likely to increase the diagnostic utility of MRI breast scans. 1016 The effect of computer-aided detection on the interpretation of screening mammograms at Intermountain Healthcare facilities. Parkinson B, Belnap T, Rowley B, Blaney S, Kerry A, Pinto K, Nkoy F. Intermountain Healthcare, Salt Lake City, UT Background: Over the last ¿ve years, computer aided detection (CAD) in mammography has been widely implemented throughout the United States. CAD employs an electronic algorithm to mark suspicious lesions on mammograms. These marks are designed to assist radiologists in improving diagnostic accuracy. Several published studies have assessed the effectiveness of CAD with respect to cancer detection rate, percentage of patients called back for additional imaging evaluation (callback rate) and percentage of patients recommended for biopsy. These studies have evaluated the effectiveness of CAD, but with conÀicting results. Although it is generally agreed that CAD may ¿nd more cancers, whether or not it results in an unacceptable callback rate is still controversial. This prospective study is designed to determine the effect of CAD on callback and cancer detection rates at four Intermountain Healthcare facilities. Method: During a 12-month period (1 January 2005 to 31 December 2005) researchers at Intermountain Healthcare prospectively tracked mammographic ¿ndings of 43,175 patients who were screened at four breast cancer screening centers. Each mammogram was initially interpreted without the aid of CAD, followed by an immediate reevaluation with CAD. All four facilities used the same equipment and software; the infrastructure remaining constant throughout the study. Each recalled case was classi¿ed into one of three categories: radiologist and CAD both perceived ¿nding, only radiologist perceived ¿nding, or CAD prompted radiologist to perceive ¿nding and recall patient. Results: The recall rate in 2005 did not show a statistically signi¿cant increase over the previous year (p<0.505, 10.85% vs 10.71%). 4,685 patients were recalled for additional imaging, resulting in a recommendation for biopsy in 750 patients (16.0%). 701 biopsies were actually performed and 190 cancers were diagnosed. Of the recalled patients, 153 were found only by CAD. This resulted in a diagnosis of seven additional cancers which would have been missed without CAD (PPV1 = 4.58%). In other words, 22 patients were recalled by CAD for each additional cancer detected. Overall this increased the cancer detection rate by 3.7%. Conclusion: The implementation of CAD at Intermountain Healthcare resulted in the detection of seven additional cancers which would have otherwise been missed. Given the discovery of these malignant lesions attributed speci¿cally to the use of CAD with no signi¿cant increase in recall rate, the use of this technology did not impose an undue burden to the system. Abstracts – Poster Session I 1017 Telemammography in a rural community. Lopez AM, Deasy S, Carroll M, Krupinski E, Kreykes L, Weinstein R. University of Arizona, Tucson, AZ; Tuba City Reginal Health Care Corporation, Tuba City, AZ Women in the U.S. have a 1 in 7 lifetime risk for developing breast cancer. Despite many advances in screening, mammography remains the gold standard for detection of breast cancer. In this study, participants included women presenting to a remote community in northern Arizona for mammography. One problem with rural medicine is women getting mammograms. Many times a traveling mammographer or couriers for the ¿lms are the only options. Due to this situation, rural women experience longer time periods to get ¿nal mammogram results. When results become available, it is often that the woman can’t be reached or is unable to return to receive the results. This loss to follow-up can be devastating. When the woman returns later, their disease can be more advanced. In working with the rural community, a telemammography service was established. Mammograms are performed at a ‘mobile’ clinic and are transmitted for reads at a mammography center, over the Arizona Telemedicine Program’s telecommunications network. The project, which was intended to enhance timeliness of service to the rural community, has far exceeded expectations and has had a major impact on women’s health care in that community. By introducing an effective turnaround time of approximately one hour, women willingly wait for their mammography results. This enhances cancer detection capacity by eradicating the need to track down patients who may have moved, who may not have a phone or who do not have an address but who now have an abnormal mammogram result. Since the conception of this service, nearly 20,000 mammograms have been performed for rural women. In this presentation we will discuss the clinical outcomes of this service. 1018 Mammography screening and other preventive care among African American and native American women with access to health care. Bachman SI, Shim V. Kaiser Permanente, Oakland, CA Background: Studies show that African American and Native American women are less likely to get screening mammograms than white women, possibly due to lack of access or to using services only when sick. This study looks at race differences in screening and other preventive care in two age groups (40-49, 50-69) in an HMO population with equal access to health care services. Methods: We calculated two-year screening compliance rates for 188,234 women aged 52-69 and 102,652 women aged 42-51 in Kaiser Permanente Northern California. Logistic regression models were used to compare African Americans and Native Americans to whites: (1) control age and tenure; (2) add utilization, primary visits and linkage to a personal care provider (PCP); (3) add gynecology visits and linkage only. Using administrative data, we tested group differences in routine gynecology visits, pap smears, and breast exams and their relationship with screening mammography. Results: For both age groups and three models, African Americans and Native Americans have lower compliance rates than whites. The differences are larger in the older group. (See Table 1 for the adjusted odds ratios). Among both age groups, both African Americans and Native Americans have more visits and more primary care visits than whites, but they are less likely to have a routine gynecological exam, a pap smear, or a routine breast exam. The older women are also less likely to have a gynecology visit or a gynecology personal care provider. In the younger group, the minority women have more gynecology visits than whites, but are more likely to have non-routine visits without a routine exam. Routine gynecological care measures show moderate relationships with mammography compliance (r ranges from .14 to .41). Discussion: Even with equal access to health care, African Americans and Native Americans are less likely than whites to comply with mammography guidelines. Although younger minority women readily use gynecology services, they are less likely to get routine and preventive care. Older minority women continue to use primary care S47 services but are less likely to use gynecology services or get preventive care. This provides some support for the theory that African American and Native American women tend to seek health care only when in need of treatment. Table 1. Odds Ratios for Mammography Compliance, African Americans and Native Americans Compared to Whites MODEL 1 2 3 AGE 42-51 Nat Amer .84 .75 .87 Afric Amer .93 .86 .87 AGE 52-69 Nat Amer .79 .72 .87 Afric Amer .88 .86 .93 1019 Initial clinical evaluation of laser optoacoustic imaging system for diagnostic imaging of breast cancer. Oraevsky AA, Ermilov SA, Conjusteau A, Miller T, Gharieb RR, Lacewell R, Mehta K, Radulescu EG, Herzog D, Thompson S, Stein A, McCorvey M, Otto P, Khamapirad T. Fairway Medical Technologies, Houston, TX; Seno Medical Instruments, San Antonio, TX; University of Texas Medical Branch, Galveston, TX; University of Texas Health Science Center, San Antonio, TX BACKGROUND This study was performed in order to provide preliminary clinical feasibility testing of the Laser Optoacoustic Imaging System, a novel imaging system that uses pulsed optical illumination of the breast in the near-infrared spectral range (which provide high tissue contrast and suf¿cient depth of penetration) and detection of the resulting ultrasonic signals (which provides enhanced resolution relative to pure optical tomography). MATERIALS and METHODS LOIS employs short pulses of near-infrared light to illuminate the breast volume and generate transient pressure in blood-rich tumors and blood vessels. These resultant acoustic signals are detected by ultrawide-band ultrasonic transducers placed along a 180-deg concave arc. After back-projection reconstruction, tumor location, shape and dimensions are determined with a spatial resolution of better than 1 mm in the image plane. RESULTS Initial studies on 50 patients demonstrated that the optoacoustic system can detect across varying tissue densities with maximum contrast in younger women. Illumination at 757 nm provides contrast based mainly on the hypoxic blood of breast carcinomas, while a wavelength of 1064 nm produces contrast dominated by enhanced water content and normally oxygenated blood in benign ¿broadenomas. Comparison of signal amplitudes provided tumor brightness proportional to optical absorption. Information obtained at two different wavelengths, one preferentially absorbed by hemoglobin (757 nm) and the other preferentially absorbed by oxyhemoglobin and water (1064 nm) allowed detection of breast carcinomas and their differentiation from normal and benign tissues. DISCUSSION The combination of optically-induced functional contrast and acoustically received high resolution imaging in a novel breast cancer imaging modality demonstrated clinical feasibility and the potential for a noninvasive diagnostics. The new modality is envisioned as an adjuvant to X-ray mammography as an ultrasonic imaging enhanced by the optical contrast. 1020 Sonobreast: a novel predictive model for the risk of malignancy in solid breast nodules with echographic expression. Paulinelli RR, Freitas-Junior R, Lucena CEM, Moreira MAR, Moraes VA, Ruiz AN, Bernardes-Junior JRM, Vidal CSR, Lucato MT, Costa NGS, Teixeira DA. Federal University of Goias, Goiania, Goias, Brazil; Santa Casa de Misericordia, Belo Horizonte, Minas Gerais, Brazil OBJECTIVE: To create a predictive model for the risk of malignancy in solid breast nodules, with echogra¿c expression. METHODS: This study performed at the Federal University of Goias and at the Santa S48 Abstracts – Poster Session I Casa de Misericordia of Belo Horizonte, included prospectively 1,403 patients with solid breast nodules. The ultrasound features were recorded in a formulary, and compared with the de¿nitive results of the anatomopathology or considered benign after a minimum follow up of two years. The age of the women and the familial history of breast cancer were also included in the model. RESULTS: 1,390 (99.1%) nodules had a conclusive diagnosis. Among them, there were 343 (24.7%) malign tumors, and 1,047 (75.3%) benign nodules. The odds ratio (and con¿dence interval) of breast malignancy for each variable included in the model, as calculated by multivariate analysis, are presented in Table 1. There were no advantage to include the presence of internal vascularity and the presence of thickened Cooper’s ligaments in the model. The area under the ROC curve for the model was 0.94 (0.92-0.96) (Figure 1). The predictive model was named “Sonobreast” and it is freely available for medical purposes in the internet site: http://www.hc.ufg.br/sonobreast/page.php. CONCLUSION: The probability of malignancy in breast tumors can be stipulated based on their ultrasound features, the age of the woman and the family history of breast cancer. Table 1. Predictive multivariate model for the risk of malignancy in solid breast nodules based on the sonographic features, age and family history of a ¿rst-degree relative with breast cancer (Sonobreast). Features B SE Wald p OR 95% CI (lower, upper) Irregular / not circumscribed 2.77 0.37 56.15 < 0.01 16.02 7.75 33.09 Heterogeneous echo texture 1.50 0.31 22.82 < 0.01 4.50 2.42 8.23 Posterior shadowing 0.87 0.34 6.63 0.01 2.38 1.23 4.62 Thick echogenic rim 0.96 0.45 4.63 0.03 2.62 1.09 6.31 Vertical orientation 0.80 0.39 4.27 0.04 2.23 1.04 4.75 Age > 40 years old 0.78 0.28 7.62 < 0.01 2.19 1.26 3.81 Positive family history 2.01 0.53 14.45 < 0.01 7.50 2.65 21.18 B: estimated coef¿cient, SE: standard error, OR: odds ratio, CI: con¿dence interval. Constant (B = -4.71, SE = 0.37, Wald = 160.40, p<0.01, OR <0.01). 1021 High resolution positron emission mammography in breast cancer management. Schilling KJ. Boca Raton Community Hospital, Boca Raton, FL Background: Whole body positron emission mammography (WBPET) has been found to be helpful in the identi¿cation of multiple malignancies but it offers less than optimum sensitivity in breast cancer detection and assistance in the surgical management of early disease. Magnetic resonance imaging (MRI) is highly sensitive in the detection of early breast cancer but has signi¿cant speci¿city issues, often resulting in unnecessary biopsy. Positron emission mammography (PEM) is a new high resolution metabolic imaging approach that claims increased sensitivity and speci¿city in the evaluation of primary breast cancer. The current pilot study was undertaken to determine the value of PEM in comparison to conventional modalities, breast MRI and WB-PET. Materials and Methods: 32 patients to date have been enrolled in this ongoing prospective IRB approved pilot study. Results from each imaging modality were compared to each other and to the gold standard, surgical pathology, to determine the accuracy of cancer detection. Kinetic curves and morphology were utilized with MRI, SUV was utilized with WB-PET while lesion to background ration was used to assist in discriminating malignant from benign lesions with PEM. Results: A total of 28 patients successfully completed all imaging studies and surgery. The age range of patients was 33-85 years with a mean of 60 years. Eight were pre-menopausal, 1 perimenopausal and 19 postmenopausal. The sensitivity in the detection of the index lesion was 46% for WB-PET, 93% for PEM and 96% for MRI. 2 lesions were outside the ¿eld of view for the PEM device. Lesions found in the surgical specimen (index plus incidental) were compared to the lesions detected with imaging. Lesion sensitivity for WB-PET was 39%, MRI 90% and PEM 92%. Discussion: PEM provides functional information and has been found to be superior to WB-PET in the identi¿cation of early breast cancer and providing information useful for surgical planning. PEM appears equivalent to MRI with regards to superior cancer detection but also results in fewer false positive ¿ndings. Lesion to background ratio may provide quantitative information which may be shown useful in suggesting the severity of pathology.Continued evaluation will be necessary to identify the eventual, most effective role of PEM in the breast imager’s tool box. 1022 A comparison study between multidetector-row CT and histopathological ¿ndings in terms of the extension diagnosis of breast cancer. Sumiyoshi K, Kani H, Nohara T, Iwamoto M, Harada T, Tanaka S, Kimura K, Takahashi Y, Shibayama Y, Tsuji M, Kurisu Y, Tanigawa N. Osaka Medical College, Takatsuki, Osaka, Japan Background: With a recent widespread use of Breast-conserving therapy (BCT), it has increasingly become important to assess the degree of extension of breast cancer. This study was made to examine the diagnosis of extension of breast cancer, especially for extensive intraductal component (EIC), by multidetector-row CT (MD-CT). Material and Methods: One-hundred and forty-eight resected lesions of invasive breast carcinoma in which MD-CT was peformed were subjected to this study. Seventy three cases (49.3%) were operated by BCT. Histological preparations were made of the resected material at interval of 5 mm, the presence of EIC was determined, and then the results were compared to CT ¿ndings. Results: Extending morphologies of tumors on CT were classi¿ed into six categories, and abnormal (linear, spotty, or cord-like) stains continuing from the main lesion were designated EIC positive. There were 63 cases (42.6%) with histological EIC, and 85 cases (57.5%) without histological EIC. The direction of histological EIC were, nipple side,48.7%; opposite side of nipple,28.9%; lateral side,40.8%. For detecting EIC by MD-CT, the sensitivity was 74.6%, the speci¿city was 80.0%, and, and the accuracy was 77.7%. The underestimation (detachment of more than 10mm) was noted in 18 cases and the overestimation, in 24 cases. Sporadic EIC was apt to be underestimated. Dif¿cult cases in evaluation were considered to be of : 1) scirrhous carcinoma (or including scirrhous component) or lobular carcinoma; 2) intraductal component dominant tumor (mainly DCIS); 3) mastopathy; 4) breast cancer including cystic lesion such as mucinous carcinoma; and 5) including necrotic component such as comedo type. Discussion: This study was to compare the accuracy of MD-CT and MRI for evaluating EIC of 67 cases among all 148 cases. The sensitivity, speci¿city, and accuracy in detecting EIC were 68.0%, 83.3%, and 77.6%, respectively, using MD-CT; and 72.0%, 83.3%, and 79.1%, respectively, using MRI. There was no difference between MD-CT and MRI in the evaluation of EIC. MD-CT is a useful modality for preoperative examination of breast cancer, especially for assessing, not only localized evaluation but axillary lymph node status, lung metastasis, liver metastasis. Abstracts – Poster Session I 1023 Correlation of Ki67 expression with FDG-PET positivity in triple negative breast cancer. Tchou J, John T, Basu S, Rosen M, Schnall M, Alavi A. University of Pennsylvania, Philadelphia, PA Background: Breast cancer is a heterogeneous disease. Current targeted therapy for breast cancer is guided by the expression of estrogen, progesterone and Her2-neu receptors in tumors. A distinct group of women who will bene¿t from novel targeted therapy are those with triple negative cancer since these women do not respond to conventional targeted therapy. Clinical trials of new agents prior to de¿nitive surgery are perfect setting to test ef¿cacy of novel agents. We explore here the potential use of FDG-PET imaging as a non-invasive means to measure proliferation index of triple negative cancer by correlating Ki67 expression with FDG-PET positivity. Materials and Methods: Between March 2002 and July 2006, 307 women with a diagnosis of invasive breast cancer participated in our institutional breast imaging study using a combination of digital mammography, ultrasound, MRI, to image the affected and contralateral breasts. Whole body FDG-PET imaging was also performed. We excluded women who had excision biopsy of their primary cancer for diagnosis purposes and those who had their de¿nitive surgery performed elsewhere (n=158). Of the 149 eligible patients, 31 had triple negative cancer (21%). We were able to perform Ki67 immunostaining on 21 of 31 triple negative cancers. FDG-PET standard uptake values (SUV) were compared with % Ki67 nuclei stain (scale 0 – 5, 0% to > 50%). Results: Of the 21 women with triple negative cancer, 20 had a positive PET scan of the index cancer (95%). Ki67 nuclear stain scores were compared to SUV of the index lesion as shown in Table. We noted that as Ki67 score increases, the median SUV also increases although the rise is not statistically signi¿cant. Discussion: This is a pilot study to investigate whether the glucose uptake FDG-PET SUVs correlate with a proliferation marker, Ki67, in triple-negative breast cancers. Work is underway to explore the role of FDG-PET in monitoring treatment response in the neoadjuvant chemotherapy setting. Ki67 nuclear stain correlation with FDG-PET Standard uptake values of 21 women with triple negative breast cancer % Ki67 nuclear stain score number Median SUV 1 (0%) 2 1.7 2 (0-2%) 1 not detected 3 (11 - 25%) 0 not applicable 4 (26 - 50%) 10 3.9 5 (>50%) 8 9.0 1024 Breast optical tomography: sensitivities and speci¿cities for the detection of cancer. Sharma A, En¿eld L, Gibson AP, Everdell NL, Schweiger M, Arridge S, Delpy DT, Hebden JC, Keshtgar M, Sainsbury RS, Douek M. University College London Hospital, London, United Kingdom; University College London, Malet Place, London, United Kingdom Background: Mammography is the standard breast imaging modality. It involves exposure to ionizing radiation and breast compression which causes discomfort. Optical tomography is a functional imaging technique that uses near-infrared (NIR) light to produce threedimensional (3D) images of the breast. We assessed the feasibility of using optical tomography to characterise breast lumps. Materials and Methods: Women presenting with discrete palpable breast lumps were prospectively recruited from the breast clinic, prior to any imaging. Ethical approval was granted and informed consent obtained. A 32-channel time resolved imaging device, developed at UCL, was used to scan the participants. Both variations in tissue scatter and absorption were measured and from these, spatial maps of blood volume and oxygenation were derived. Two assessors, blinded to other imaging ¿ndings, were trained to interpret optical images using scans of 8 patients with known diagnoses, con¿rmed histologically. After training, the assessors then independently analysed scans from subsequent patients. Scans were presented in the same con¿guration S49 as training images. Any images that could not be obtained in the same way were excluded. Images were graded from 1 to 5 were 1 = hardly perceivable inhomogeneity of the scan, 2 = weak contrast scan, 3 = contrast inferior to other homogeneities, 4 = contrast comparable to other homogeneities and 5 = contrast of lesion dominates. For any disagreements between assessors, scans were reviewed to reach an agreed conclusion. Results: A total of 80 individual breast images were obtained from 49 patients. Of the 49 patients standard imaging detected 23 breast cancers (1 bilaterally), 12 ¿broadenomas, 6 cysts, 6 with post-operative scar tissue and 3 patients with implants. 29 women were imaged using an older format of the device and these images were excluded. Of the training images, there were 4 tumours, 3 ¿broadenomas and 1 normal image following presentation with mastalgia. Of 12 assessed images, 7 tumours, 4 ¿broadenomas and 1 example of ¿brocystic change were presented. The assessors independently correctly assessed 9 out of the 12 images for both diagnosis and location of lesion. For the detection of breast cancer optical tomography had a sensitivity of 100%, speci¿city of 75% and a positive predictive value for cancer of 80%. Discussion: Optical tomography is feasible for the characterisation of breast lumps. Further work should focus on its potential role alongside existing imaging modalities. 1025 Mammographic features of triple-negative versus HER2+ and ER+ breast cancers. Yang WT, Dryden M, Broglio K, Dawood S, Valero V, Hortobagyi G, Atchley D, Arun B. M. D. Anderson Cancer Center, Houston, TX Background. Triple receptor negative (TRN) cancers are high grade ER, PR, and HER2 negative cancers that represent a distinct tumor subtype with a poor prognosis and characteristic gene expression pro¿le (basal-like breast cancer, BLC). Tumors arising in women with a BRCA/germline mutation share many similarities to sporadic BLC including a TRN immunophenotype and a basal-like gene expression pro¿le. The aim of this study was to compare mammographic breast density, mammographic visibility, and mammographic tumor features between cancers of different immunophenotypes. Materials and Methods. Between January 2003 and November 2005, 204 premenopausal patients (pts) diagnosed with breast cancer from a single institution who had mammography performed at initial diagnosis were identi¿ed, of whom87 (43%) underwent genetic testing. HER2- disease was de¿ned as negative expression by IHC or gene ampli¿cation by FISH. HER2+ disease was de¿ned as 3+ on IHC or gene ampli¿cation by FISH. Variables recorded included clinical, histological, and mammographic features of cancers which were strati¿ed into three groups by IHC: TRN, HER2+, and ER+. Results. Thirty-eight (19%) pts had TRN, 67 (33%) pts had HER2+, and 99 (49%) pts had ER+ cancers. Of the 67 pts with HER2+ cancers, 28 (42%) were also ER+. Thirteen (15%) of 87 pts who underwent genetic testing had TRN disease. Thirteen (15%) pts showed a BRCA1/2 mutation, of whom four (31%) had TRN disease. Median age was 32, 33, and 32yrs respectively for pts with TRN, HER2+, and ER+ disease (p=0.475). Median tumor size was 3.0, 2.2, and 2.2 cm respectively for pts with TRN, HER2+, and ER+ disease (p=0.06). Greater than 50% breast density was observed in 84%, 90%, and 82% respectively of the TRN, HER2+, and ER+ cancers (p=0.39). Mammographic visibility of the TRN, HER2+, and ER+ cancers was 86.6% (33/38), 95.5% (64/67), and 92.9% (92/99) respectively (p=0.26). Visible cancers presented as a mass in 86.6% (33/38), 71.6% (48/67), and 42.4% (42/99) respectively (p < 0.00001), and as calci¿cations in 13.2% (5/38), 64.2% (43/67), and 54.4% (56/99) respectively, of the TRN, HER2+, and ER+ cancers (p < 0.00001). The 13 BRCA/germline cancers were associated with greater than 50% breast density in 85% (11/13), were mammographically visible in 92% (12/13), and were associated with a mass in 62% (8/13), and calci¿cations in 31% (5/13). Conclusion. The mammographic features of TRN breast cancers are signi¿cantly different from HER2+ and ER+ cancers, presenting primarily as a mass with a striking absence of calci¿cations and support the biological concept of a distinct tumor subtype that has similarities to tumors with a BRCA/germline mutation. S50 Abstracts – Poster Session I 1026 Effects of the steroidal aromatase inhibitor exemestane on mammographic breast density and other end-organ functions. Cigler T, Fabian CF, Yaffe MJ, Johnston D, Ingle JN, Nassif E, Brunner R, Wadden N, Pater JL, Richardson H, Tu D, Shangle Q, Goss PE. Massachusetts General Hospital, Boston, MA; Sunnybrook Health Sciences Centre, Toronto, ON, Canada; Kansas University Medical Center, Kansas City, KS; Mayo Clinic, Rochester, MN; Notre Dame Hospital, Montreal, QC, Canada; University of Nevada School of Medicine, Reno, NV; Memorial University of Newfoundland, St. John’s, NL, Canada; National Cancer Institute of Canada Clinical Trials Group, Kingston, ON, Canada; (NCIC CTG) MAP.2 Background: Exemestane (EXE) is a potent aromatase inhibitor with unique androgenicity secondary to its steroidal structure. Breast density is a biomarker of risk that is sensitive to hormonal inÀuences: increased by hormone replacement therapy and reduced by tamoxifen. Thus the effects of exemestane on both mammographic density as well as on bone and lipid metabolism were examined. Methods: NCIC CTG MAP.2 was an international, double-blind, placebo-controlled trial in healthy postmenopausal women without a prior history of breast cancer and baseline mammographic density (Boyd Grade 2-6). Women were randomized to EXE (25mg daily) or placebo (PLAC) for 12 months and followed for a total of 24 months. Endpoints included changes in breast density between baseline and 12 month as estimated by a computer-assisted thresholding program and changes in plasma lipids, bone biomarkers and bone mineral density (BMD). Results: Ninety-eight women were randomized (49 to EXE; 49 to PLAC). Results of breast density with attention to intra- and inter observer variation will be presented. The percent change in the bone resorption marker N-telopeptide was signi¿cantly higher in the EXE arm at 12 months (29.7% EXE vs. –5.7% PLAC, p value 0.04). No statistically signi¿cant differences in percent change in BMD (lumbar spine and femoral neck) were observed between the two treatment arms at either 12 or 24 months. Treatment groups differed signi¿cantly in percent changes in total cholesterol at 6 months (-5.2% EXE vs. 0.8% PLAC, p value 0.02), HDL at 6, and 12 months (-6.3% EXE vs. 2.0% PLAC, p value 0.009; -6.6% EXE vs. 0.7% PLAC, p value 0.013), and lipoprotein a at 6 and 12 months (-7.2% EXE vs. 13.3% PLAC, p value 0.006; -0.9% EXE vs. 4.2% PLAC, p value 0.034). However, changes in total cholesterol were not apparent between treatment arms at 12 or 24 months. Changes in HDL and lipoprotein a were also not apparent between treatment arms at 24 months. No signi¿cant differences in percent change in LDL or triglycerides were noted at any time point. Discussion: EXE administered for one year to healthy postmenopausal women resulted in an increase in the bone resorption marker Ntelopeptide without signi¿cant change in BMD during and after the treatment period. Changes in lipid parameters on this trial were mild and reversible and of uncertain clinical signi¿cance. In light of powerful estrogen suppression and potential androgenicity from EXE, its effects on mammographic density are awaited with interest. 1027 InÀuence of bilateral breast magnetic resonance imaging in treatment planning for patients with stage I/II breast cancer. Figueredo ND, Carruthers CL, Frazier TG. Lankenau Hospital, Wynnewood, PA; Comprehensive Breast Center, Bryn Mawr Hospital, Bryn Mawr, PA Background: Traditional screening methods including physical exam, ultrasound, and mammography may not detect the extent of disease in newly diagnosed breast cancer patients. Prior studies have shown that magnetic resonance imaging (MRI) changes surgical management of breast cancer in approximately 9-30% of patients. We evaluated the inÀuence of preoperative breast MRI in the surgical management of patients in our community breast center. Methods: 100 consecutively diagnosed patients with stage I/II breast cancer treated by a single breast surgeon, in a community breast center were evaluated. All patients had bilateral breast MRI prior to de¿nitive surgical treatment. Results: Prior to MRI the proposed treatment plan for these 100 patients was breast conservation. 26 of these patients (26%) had their treatment plan altered by the MRI result. 14 of these 26 patients (53.8%) underwent unilateral mastectomy for presumed multi-focal disease. All 14 had more extensive disease or actual multi-focal disease on ¿nal pathology. 11 of 26 patients (42.3%) chose bilateral mastectomy based on MRI ¿ndings. 7 of these 11 patients (63.6%) had bilateral disease on ¿nal pathology. 1 patient of the 26 (3.84%) had bilateral unifocal disease and chose bilateral wide segmental resection with primary radiation treatment. Conclusion: Bilateral breast MRI utilized as part of the staging workup for newly diagnosed breast cancer has changed our surgical management in 26% of cases. We conclude that breast MRI is appropriate and an important complement to mammography and ultrasound in a signi¿cant number of patients with presumed unifocal breast cancer. 1028 Follow-up rather than excision for benign papillary lesions of the breast. Copit DS, Vaidynathan S, Chaudhri Y. Albert Einstein Medical Center, Philadelphia, PA PURPOSE Management of papillary lesions of the breast diagnosed at percutaneous biopsy has been controversial. Based on several studies, at our institution we have traditionally recommended follow up rather than excision for these patients, assuming there are no other associated highrisk lesions. Because of the controversy that remains today, we decided to perform a retrospective review of our data to study the safety of our practice. We decided to include data from patients for whom we have at least two year potential follow up. METHOD AND MATERIALS We performed a retrospective review of all percutaneous biopsies performed from January 2003 through February 2005. Out of a total of 661 procedures, 28 revealed benign papillary lesions (solitary papilloma or papillomatosis). We excluded any patients with atypia (whether or not associated with the papillary lesion) or any other lesions that have well-established recommendations for excision. RESULTS All biopsies were performed with an 11 gauge vacuum-assisted device. A total of 23 patients had ultrasound guidance and 5 had stereotactic guidance for their biopsy. The average length of follow up was 30.8 months (range 14-43 months). Three patients were lost to follow up. One patient developed DCIS at her biopsy site at 1 year follow up. Seven lesions were excised because of patient preference (n=1), surgeon’s or pathologists’ recommendation (n=5) or radiologic-histologic discordance (n=1). The remaining 17 have not developed cancer in either breast. CONCLUSION Patients who have a percutaneous biopsy with an 11 gauge vacuumassisted device that reveal benign papillary lesions can be safely followed with mammography rather than undergoing surgical excision. 1029 Using three-parameter empirical mathematical model to analyze breast DCEMRI data; comparison with conventional BI-RADS classi¿cation. Fan X, Arkani S, Karczmar GS, Abe H, Schmidt RA, Newstead GM. University of Chicago, Chicago, IL Background: Dynamic contrast enhanced MRI (DCEMRI) is becoming increasingly important for early detection of breast cancer. Optimal use of DCEMRI data for cancer diagnosis requires objective, quantitative analysis of rates of contrast media uptake and washout. Most DCEMRI studies have relied on pharmacokinetic compartment modeling to relate contrast media kinetics to tumor blood Àow. However, 3D DCEMRI data acquired in routine clinical practice has very low time resolution (∼60 s). Under these conditions, the accuracy of physiological parameters obtained from compartmental models is questionable. In addition, these models require an arterial input function, which is dif¿cult to estimate accurately. Alternatively, empirical mathematical equations can be used to ¿t the kinetic curves. In this study, a simple Abstracts – Poster Session I empirical mathematical model (EMM) with only three parameters was used to analyze 3D bilateral DCEMRI breast data. Sensitivity and speci¿city obtained with this approach was compared to that of the BIRADS® lexicon. Material and Methods: 3D DCEMRI data with time resolution of 68 s, from 34 benign and 79 malignant lesions were selected for review. Plots of signal intensity vs. time (6 time points) were produced from a manually selected region of interest that contained the most rapidly enhancing contiguous pixels in a suspicious lesion. The EMM was used to ¿t the raw data. Formulas for commonly used diagnostic parameters,such as initial area under curve, initial slope of enhancement, the time to peak enhancement, signal enhancement ratio, and enhancement curvature at peak, were derived in terms of the three EMM parameters. Finally, the sensitivity and speci¿city for malignant lesions using these parameters were evaluated by using receiver operating characteristic analysis, and was compared to the kinetic curve classi¿cation according to the BI-RADS. Results: The results demonstrate that the EMM was able to accurately ¿t all the signal enhanced kinetic curves with only 6 points. There was a statistically signi¿cant difference between benign and malignant lesions for several diagnostic parameters: the uptake rate, initial slope, signal enhancement ratio, and curvature at the peak enhancement (p ≤ 0.04). EMM analysis provided at least the diagnostic accuracy of the kinetic classi¿ers described in the BI-RADS lexicon with the sensitivity and speci¿city of 91% and 18%, respectively. Discussion: Although the sensitivity and speci¿city of the EMM approach vs. Bi-RADS were not signi¿cantly different, the EMM offered key advantages. Unlike the BI-RADS classification, the EMM can be used to achieve a continuous spectrum of sensitivity and speci¿city, from which Radiologists can choose the optimal combination, depending on other clinical factors. The EMM can be used to standardize data from different institutions with different dynamic protocols, so that the diagnostic parameters obtained with different protocols can be interpreted using uniform criteria. This suggests that the EMM may be useful for analysis of routine clinical data. 1030 A double-blind randomized controlled trial of paracetamol as a pre-medication for mammography. Freitas-Junior R, Nascente CM, Carvalho AA, Ximenes C, Silva MF, Leite Filho AR, Freitas PF. Goias Federal University, Goiania, GO, Brazil; Goiania, GO, Brazil INTRODUCTION: Mammography represents an important method of detection of breast cancer. However, the pain caused by this exam is one of the principal factors why some women abandon the exam routine, or do not follow the chronogram. The analgesic intervention is a possible solution for minimizing pain and discomfort that are felt during the mammography. OBJECTIVE: Verify the possibility of diminishing pain and discomfort during the mammography procedure trough analgesic administration. METHODOLOGY: randomized, double-blinded, placebo controlled trial, testing paracetamol to diminish the pain and discomfort during mammography. 300 patients that came to the Radiology Service of HC/UFG were randomized for this study. A questionnaire with two parts was used: the ¿rst had questions that concerned the patient identi¿cation and factors related to the pain during mammography; and the second asked about the scale of discomfort (without discomfort; uncomfortable, but tolerable; extremely uncomfortable; unbearable) and the pain (analogical linear scale) during the mammography. Each patient received 1000 mg of paracetamol or placebo. Afterwards each patient ¿lled out the second part of the questionnaire. Three patients were excluded from the analysis; this resulted in 149 in the paracetamol group, and 148 in the placebo group. RESULTS: The two groups were homogenous concerning the mean of the ages, weight, height and breast size. The mean of the pain was 3.5 in the paracetamol and 2.9 in the placebo group (p=0.12). Concerning the scale of discomfort, in the paracetamol group, 92% of the patients said that they did not fell any discomfort or that the exam was uncomfortable, but tolerable, meanwhile in the placebo group, this value was 93.8% (NS). The exam was extremely uncomfortable or that the exam was unbearable counted for 8.1% of the patients in group 1 and 6.2% of the patients in group 2 (NS). CONCLUSION: The usage of paracetamol before the mammography did not reduce the discomfort S51 and pain generated by the radiological exam. 1031 Why women with breast cancer do not return for surveillance mammography. Geller B, Skelly J, Muss H. University of Vermont, Burlington, VT; Vermont Cancer Center, Burlington, VT Background: Studies using health claims databases or registries have reported between 15 – 22% of women with recently diagnosed breast cancer (BC) did not have surveillance mammography (SM). Because these women are at high risk for recurrence or second primary tumors and SM is the recommended test for BC detection it is important to understand why they do not return. Methods: We identi¿ed women diagnosed with BC between 19982001 in the Vermont Breast Cancer Surveillance System, a member of the NCI’s Breast Cancer Surveillance Consortium. After excluding women with a bilateral mastectomy, stage 4 cancer, or a prior breast cancer there were 1223 who did (controls) and 241 who did not (cases) have SM 7-30 months after the BC diagnosis. Sampling was strati¿ed by age groups and stage. Through telephone interviews in 2006 we collected data on treatment and surveillance history, psychological measures and demographics. Cases and controls were compared for each explanatory factor. Results: We found that 16% did not have SM during the follow up period. After a National Death Index search and a search for current address and telephone number, and applying matching criteria for each sampling cell we invited 107 cases and 109 controls to be interviewed. See Table 1 for participation rates. Of the 53 cases interviewed 49 reported having SM. We con¿rmed SM for 16 cases and converted these to controls and 6 out of state cases were dropped from the analyses. Thus the analyses were conducted with 31 cases and 68 controls. Of the 4 cases reporting no SM, 3 reported having a bilateral mastectomy and one stated she did not think she needed it. Three explanatory factors were signi¿cantly different between cases and controls. Women who received hormonal therapy were 2.4 times more likely to have SM during the follow up period compared to women who did not. For each unit increase in co-morbidity a woman’s odds of having SM was reduce by .89. Women in the two middle income ranges had an increased odds of having SM during the follow up period (OR=4.00 and 3.67 respectively), compared to women in the <$25,000 income range, and although not signi¿cant, women in the highest income range were more likely than women in the lowest range to return for SM. Conclusion: Women using hormonal therapy and who had little or no comorbidity were more likely to have SM. Income also appeared to play a role in not returning for SM. Database research has inherent limitations. All but 4 of 53 cases reported SM and we were able to con¿rm 27. Our database was missing data from out of state mammography, death records and data on women who had moved. Although our study showed that SM is usually obtained, it is still important for health care providers to encourage BC survivors to participate in mammography after treatment is completed. Supported by a grant from the Susan G. Komen Foundation and NCI. Table 1. Reasons for not participating Invited Deceased Unable to reach or locate Declined participation Not inverviewed, other reason Interviewed Cases 107 10 26 16 2 53 (49.5%) Controls 109 8 23 22 4 52 (46.8%) 1032 Accuracy of clinical evaluation of locally advanced breast cancer in patients receiving neoadjuvant chemotherapy. Prati R, Minami CA, Gornbein JA, DeBruhl N, Chung D, Chang HR. University of California, Los Angeles, Los Angeles, CA Background: Physical examination (PE), mammography (MG), breast MRI, FDG-PET and pathologic evaluation are the standard assessments of primary breast cancer. The accuracy of each of these methods has not been well studied in patients receiving neoadjuvant chemotherapy. We compared the accuracy of each of them in tumor and nodal assessment in patients with T3-T4 tumors receiving neoadjuvant chemotherapy. S52 Abstracts – Poster Session I Materials and methods: We analyzed 45 patients with T3-T4 tumors from an ongoing trial. All patients had 4 cycles of docetaxel/carboplatin with or without trastuzumab before surgery. Tumor assessments by PE, MG, and MRI as well as nodal status by PE and PET were obtained before and after chemotherapy. Final tumor and nodal staging by pathology were also obtained. Spearman corr (r) and root mean square error (RMSE) measured accuracy. Results: At baseline, when compared to the tumor size measured by PE, MRI was more accurate than MG (r=0.559, RMSE=35.4%, vs. r=0.046, RMSE=66.1%). After 4 cycles of chemotherapy, PE tumor assessment correlated better with pathological evaluation than MG or MRI (r=0.656, RMSE=90% vs. r=0.126, RMSE=152% and r=0.364, RMSE=93%, respectively). Nodal assessment after neoadjuvant chemotherapy showed high speci¿city but low sensitivity by both PET and PE. Conclusion: Accurate tumor assessment of locally advanced breast cancer (T3-T4) by PE is clinically accurate both before and after neoadjuvant chemotherapy. Our study suggested that breast cancer size determined by PE was more accurate when compared with imaging to the pathology ¿ndings. Both PET and PE predicted pathologically positive nodes but not negative nodes. Pathological nodal staging is still the standard of care regardless of the PE and PET results. 1033 Breast speci¿c gamma imaging and managment of breast cancer. Stern L, Rosenberg AL, Brill KL. Methodist Hospital, Philadelphia, PA; Jefferson Medical College, Kimmel Cancer Center, Philadelphia, PA Intro:Scintimammography (SM), a functional breast imaging technique, has produced high speci¿city for breast lesions of 86 - 89% and shown to be as effective or better than breast MRI. In spite of these promising results, SM has not been widely utilized due to its lack in sensitivity for sub-centimeter lesions (around 55%). To address these issues, several breast-speci¿c gamma imaging (BSGI) systems have been introduced. The sensitivity and speci¿city for BSGI are both upwards of 90%. Additionally, such designs allow the breast to be imaged from several angles including those which mimic the cranialcaudal (CC) and medial-lateral-oblique (MLO) mammographic views. MRI had also continued to develop with improving technology and clinical experience. The ACRIN Study on breast MRI utilized both 3-D and dynamic MRI and demonstrated a sensitivity of 88% and speci¿city of 68%. The sensitivity and speci¿city of BSGI were analyzed and the role and impact on management assessed. Methods: BSGI was performed on 524 patients during the time period from 5/1/06 through 5/1/07. We reviewed and compared the results of ¿ndings on BSGI, MRI, mammography and ultrasound for these patients. Results: Indications for BSGI included: 1) Patients with recently diagnosed breast cancer to look for multifocality and multicentricity. 2) Patients with BRCA mutations. 3) Patients with past history of breast cancer and possible recurrence, 3) Patients with multiple masses on mammography and/or ultrasound, 4) Patients with unexplained pain or palpable abnormalities, 5) Patients with extremely dense breasts, and 6) Patients with indeterminate calci¿cations. Of the 84 patients with BIRADS 4 or 5, 11 had a new diagnosis of cancer and 8 were evaluated for recurrence. Mass or abnormal mammography was the indication for 63% of patients and 13% had suspicious calci¿cations. There were 8 patients classi¿ed as BIRADS 4 or 5 on BSGI who also had an MRI. All 7 of the patients that had a positive BSGI and MRI had a positive biopsy for cancer. The one patient negative on MRI was also negative on biopsy. This would indicate a sensitivity of 87.5% and a speci¿city of 87.5% for BIRADS 4 and 5. BSGI documented evidence of multicentricity and contralateral disease in 16 cases. It identi¿ed recurrent disease in 6 cases. Conclusion: While BSGI has been directly compared to MRI only in a few small studies, it has demonstrated comparable sensitivity but higher speci¿city. This limited data is not suf¿cient for conclusions. Additionally, findings on BSGI altered the subsequent surgical management of breast cancer patients in 4% of cases due to discovery of multicentric and contralateral disease or the presence of recurrent disease. There are approximately 40 sites in the US performing BSGI and around 20,000 procedures have been completed to date. The authors of this work propose a multi-center retrospective comparative analysis of BSGI and MRI in patients who routinely received both imaging modalities to allow comparison of the performance of these techniques in the detection of breast carcinoma in these patients. 1034 The missing exam in clinical breast exam. Goodson III WH, Moore II DH. California Paci¿c Medical Center Research Institute, San Francisco, CA; University of California, San Francisco, CA Background: Clinical breast exam (CBE) is necessary during diagnosis of the 15% of breast cancers missed by mammograms (JNCI 2005; 97:1476). Inadequate application of CBE is a problem, however, because clinicians as a group fail to make a timely diagnosis of 5 percent of breast cancers because they allow negative mammogram results to override CBE ¿ndings (Arch Int Med 2002; 162:1343). CBE application will not improve unless clinicians practice CBE frequently enough to become facile with the procedure, but surveys suggest that fewer clinicians perform routine CBE. To guide efforts to improve CBE, we surveyed women to determine the percent that receive even a basic CBE by asking them to compare their experience of CBE with a minimal standard CBE. Methods: We posted a real-time video of a minimal, 2-minute CBE on the internet at www.2minutebreastexam.com and asked women to compare their own experience to the CBE video. The choice of responses was: 1) “My annual breast exam is like the exam in the video.” 2) “My annual breast exam is not as thorough as the exam in the video.” 3) “My doctor doesn’t do any breast exam.” We used the internet because respondents needed proximate access to the video to make their comparisons and, logistically, it was most feasible to make the video accessible via the internet. We illustrated 2-minute supine palpation suggested by Mahoney and Csima (CMA Journal 1982; 127: 729) as the minimal acceptable CBE because: a) a CBE shorter than 2 minutes is also shorter than any longer CBE method (3); and b) from discussion at community groups, most women receive less than 2 minutes anyway. With IRB approval, we tabulated a convenience sample of the ¿rst 320 respondents. Results: Only 70 (21%; 95% CI 15-26%) reported that they received a CBE comparable to the 2-minute CBE illustrated on the site. Seventynine percent (95% CI 74-85%) received either a CBE that was not as thorough (n=237) or no CBE (n=13). Responses were from all ten zip code regions of the United States. Discussion: A CBE that does not allow time to examine the breasts is not a CBE; and, although one might debate the minimal acceptable time for CBE, the acceptable minimum is unlikely to be less than 2 minutes. From our survey, we conclude that clinicians are abandoning an essential clinical skill and with it the opportunity to improve diagnosis of the 15 percent of breast cancers that are invisible to mammograms. Based on the response to our survey, we believe that, in addition to informing choices for cancer treatment, the internet should be used to inform women of what they should be able to expect in breast cancer screening, especially for their periodic clinical breast exam. 1035 Comparing performance measures in opportunistic and organized screening mammography for early breast cancer detection. Hofvind S, Vacek P, Skelly J, Geller BM. The Cancer Registry of Norway, Oslo, Norway; University of Vermont, Burlington, VT Background: In the U.S. screening mammography is initiated by women themselves, usually in response to a recommendation by a health care provider. In contrast to this opportunistic screening, Norway and most other European counties have organized screening programs in which women are invited to attend scheduled mammography examinations at regular intervals. In Norway women are screened every two years while in Vermont most women are screened annually. Another difference between Vermont’s delivery of screening mammography and Norway’s program is the way that examinations are read with Norway routinely using independent double reading with consensus by radiologists who Abstracts – Poster Session I are specialists in breast imaging. The performance measures of these two systems for delivering screening mammography have not been previously compared. Methods: We compared recall and detection rates, positive predictive value, sensitivity and speci¿city in women aged 50-69 years old, undergoing opportunistic screening mammography in Vermont (n=45,050) and organized screening in Norway (n=194,294) during 1997-2003. The results are given for the subsequent screening examinations. Results: The recall rate in Vermont was more than three times higher than in Norway (9.8% vs. 2.7%, p<0.001), while the screening detection rate per 1,000 screens for one year follow-up was signi¿cantly lower (3.9 vs. 5.1, p<0.001). The interval cancer rate for two year follow-up was signi¿cantly higher in Vermont, both per 1,000 screens (1.84) and per 1,000 women years (1.23), compared to Norway (1.73 and 0.87 respectively). Positive Predictive Values (PPV) for two-year follow-up was 4.6% in Vermont and 19.2% for Norway for initial assessment, 19.4% and 49.4% for ¿nal assessment. The sensitivity was 77.6% for initial assessment and 68.6% for ¿nal assessment in Vermont, and 75.9% and 74.8% for Norway after two years of follow up. The speci¿city was lower for Vermont compared to Norway, both for initial and ¿nal assessment. Conclusion: Our study suggests that screening mammography in the organized screening program in Norway is more accurate. Lower recall and biennial screening makes it also more ef¿cient than the opportunistic screening in Vermont. Independent double reading with consensus and the longer screening intervals are probably the major reasons for the greater accuracy. Radiologists in the United States should be encouraged to routinely use independent double reading with consensus. 1036 Cost-effectiveness of breast cancer (BC) screening with contrast enhanced magnetic resonance imaging (MRI) as an adjunct to x-ray mammography (XM) in high-risk women. Taneja C, Edelsberg J, Weycker D, Guo A, Oster G, Weinreb J. Policy Analysis Inc. (PAI), Brookline, MA; Bayer HealthCare Pharmaceuticals, Wayne, NJ; Yale University School of Medicine, New Haven, CT Background: Screening for BC with MRI plus XM is now recommended for high-risk women; its cost-effectiveness (vs XM) is largely unknown. Methods: We developed a model to depict outcomes and costs of MRI+XM vs XM screening in a cohort of 10,000 women with BRCA1/2 mutations or high lifetime risk of BC (collectively, “high risk”). Patients were assumed to be 40 years of age, and to be screened once at model entry. Prevalence of undetected BC (invasive and DCIS) was assumed to be 2.3%. Sensitivity and speci¿city of MRI+XM (90.2% and 84.1%) and XM (40.0% and 94.7%) were estimated based on published prospective studies employing both modalities. The model predicts the number of women correctly and incorrectly diagnosed with each strategy, and consequences in terms of additional care (further diagnostic evaluation, BC treatment), patient utilities, and life expectancy. Women with BC not detected at screening were assumed to be correctly diagnosed (often at a more advanced stage) in the next 12 months. Costs included those of initial screening, further diagnostic work-up, and BC treatment. Cost-effectiveness was calculated as cost per quality-adjusted life-year (QALY) gained; costs (2005US$) and effectiveness were discounted at 3% annually. Results: Among 230 (out of 10,000) women with undetected BC, 208 cases would be detected by MRI+XM screening and 92 by XM. MRI+XM would yield more false-positives (37 vs 12). Cost of screening would be $1,887 per patient for MRI+XM vs $936 for XM. MRI+XM screening would produce an expected gain in (undiscounted) life-years (39.50 vs 39.44). Cost per QALY gained is $27,634 for women with BRCA mutations, and $59,639 for other high-risk women; overall, cost per QALY gained is $53,878. Discussion: MRI+XM screening would improve detection of BC and thereby life expectancy in high-risk women, and is cost-effective by current standards. S53 1037 High incidence of brain metastases found in patients with HER2 positive metastatic breast cancer. Should these patients be followed by regular MR scans? Langkjer ST, Krøldrup L, Kristiansen C, Enevoldsen K, Edal AL, Ormstrup TE. Vejle Hospital, Vejle, Denmark Background: A high incidence of brain metastases has been found in studies of patients with HER2 over-expression (HER2 positive patients). Prophylactic cerebral irradiation to this patient group has been considered. It has been claimed that irradiation of asymptomatic brain metastases can prevent them from becoming symptomatic. Our aim was to study the incidence, pattern, and timing of cerebral metastases in patients with relapse of breast cancer with HER2 over-expression in order to evaluate weather regular MR scans should be offered to ¿nd the brain metastases earlier when they are still asymptomatic. Patients and Methods: Patient data from a phase II study of patients with relapse of HER2 positive breast cancer was examined retrospectively. It consisted of 36 patients diagnosed with disseminated breast cancer and over-expression of HER2 status either proven by immunhistochemistry (IHC) 3+ and or Àuorescence in situ hybridization (FISH). The patients were treated with trastuzumab and paclitaxel either as ¿rst or second line chemotherapy. Patients were included between November 2001 and October 2005. Results: Approximately half a year after inclusion in the protocol the ¿rst patients developed symptomatic brain metastases. Within a few years 18 of the 36 patients in the study were diagnosed with cerebral metastases (50%). Especially patients with more than 2 systemic metastatic sites seemed to be at risk. All patients with cerebral metastases had multiple cerebral metastases and received radiotherapy (full-dose whole brain radiotherapy, 20Gy/4 fractions). The disease status at the time of brain metastases showed that 12 of the 18 patients had regression or stable systemic disease. Discussion: Our study shows that patients with HER2 over-expression have a very high risk of developing brain metastases. Trastuzumap and chemotherapy is effective to control the patients systemic disease but seems to be less effective for treatment of brain metastases, because of poor penetration of the blood-brain barrier. The median survival time for patients with cerebral metastases is poor. Since half of HER2 over-expressing patients developed brain-metastases close surveillance for brain metastases (clinical and/or imaging) is necessary even during effective systemic treatment. We therefore recommend that this patient group should be followed with regular MR scans of the brain. 1038 Concordance of contralateral breast cancer for steroid receptor and tumour characteristics. Absar MS, Martin C, Howe M, Zeiton A, Cramer A, Morris J, Bundred NJ. University Hospital of South Manchester, Manchester, United Kingdom Contralateral breast cancers affect 5%-10% of patients. The aim of the study was to determine whether the ¿rst cancer predicted the tumour characteristics of the second cancer. Materials and methods: Women who developed Bilateral breast cancer between 1976 and 2005 were retrieved from the breast unit database. Variables compared included mode of detection, pathological size, histological type and grade, oestrogen receptor(ER) status, epithelial proliferation (Ki67) and lymph node status. Results: The mean age of diagnosis of the ¿rst cancer was 53 years. Twenty six percent ( 66/254) of the index cases and 53% (135/254) of the contra lateral cases were screen detected. Mammographically detected (screen) cancer had a higher likelihood of 85% (56/66) of having screen detected contralateral cancer (p=0.001). Symptomatic cancers were higher grade than screen detected (p=0.005). SDCBC tended to be smaller with 72% being <20 mm and mainly lymph node negative (75%).whereas 50% of symptomatic cancers were > 20mm and 47% were node positive. Mode of detection, grade of tumour, Oestrogen receptor status and epithelial proliferation correlated between the tumours in both groups. S54 Abstracts – Poster Session I Conclusion: An individuals genetic makeup determines the tumour characteristics of both primary and contralateral breast cancer. Mammographic follow up should be tailored to mode of presentation and ER status of the initial primary cancer. Tumour Concordance Metachronous (n=197) Concordance Spearman correlation Synchronous (n=76) Concordance Spearman correlation Detection mode 85% 0.001 85% 0.0001 Nodal status 48% 52% 0.006 0.005 Size group 53% 0.107 Oestrogen receptor 77% 0.001 Ki67 group 72% 0.001 57% 57% 0.001 0.180 53% 0.092 95% 0.001 59% 0.001 Grade 1039 Breast cancer in the elderly: benefits of screening mammography in the diagnosis. Hines NL, Leibman AJ. Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY Introduction: Recently, the American Cancer Society revised its recommendations which stated that women should continue screening mammography as long as they are in good health. As life expectancy increases, a greater percentage of our population is becoming elderly. At the same time, their risk for developing breast cancer increases. In the 2006 National Vital Statistics Report by the CDC, the average life expectancy for a female of any race at the age of 70 was reported to be 15.9 years. Therefore, we believe that the continuation of annual screening mammography beyond the age of 70 years will identify clinically occult and earlier stage cancers that can be successfully treated, and possibly prolong survival. Materials and Methods: We retrospectively reviewed breast cancer patients age 70 years and older presenting to our institution during an 8 year period (1999-2007). We reviewed clinical history as well as mammographic, pathologic and surgical data. Analysis of several mammographic factors was performed, including screening versus diagnostic mammography, presence of prior mammograms, length of time since the prior mammogram as well as mammographic ¿ndings. The type of surgery was noted. Pathology data was reviewed to determine type and extent of tumor. Results: 37 patients with an average age of 73.4 years (range 70 - 86 years) presented with 41 cancers. 29 of the 41 (71%) cancers were identi¿ed on screening mammograms and 12 (29%) presented for diagnostic mammograms. 23 (62%) patients had prior mammograms, the average time since the prior mammogram was 1.2 years. Suspicious calci¿cations were identi¿ed in 5 (12%), a mass was identi¿ed in 21 (51%) and a mass with calci¿cation was identi¿ed in 15 (37%). Pathology in 11 of the 41 (27%) cancers was DCIS. In 28 (68%) pathology demonstated in¿ltrating ductal carcinoma and in 2 (5%) invasive lobular carcinoma. The average tumor size was 2.0 cm on pathologic. 34 cancers were managed surgically at our institution by either lumpectomy (n=21) or mastectomy (n=14). In the subgroup of DCIS, 8 of 11 patients with DCIS were diagnosed based on screening mammography ¿ndings. 7 (64%) of the DCIS patients had prior mammograms with an average time interval of 1.5 years. Of the 11 patients with DCIS, 8 (73%) were identi¿ed on screening examinations. Suspicious calci¿cations were identi¿ed in 3 (27%), a mass in 4 (36%) and a mass with calci¿cation in 4 (36%). Discussion: The population of elderly women in the US is increasing. At the same time, the elderly have an increased rate of breast cancer. With the enlarging group of women in this age group at increased risk, the bene¿ts of screening mammography continue to be debated. We reviewed the clinical history, mammography and pathology ¿ndings as well as surgical history of 37 elderly patients. Our results suggest that screening mammography continues to be very bene¿cial in the elderly. Screening mammography should continue to be requested in elderly. 1040 Utility of echocardiographic screening for late-onset cardiomyopathy in breast cancer survivors treated with cardiotoxic chemotherapy. Wazir S, Budd GT, Moore HCF, LeGrand S, Andresen S, Tang WH. Cleveland Clinic, Cleveland, OH Background: The diagnostic utility of routine surveillance echocardiographic screening to identify late-onset cardiomyopathy in breast cancer survivors treated with cardiotoxic chemotherapy has not been examined. Methods: We prospectively evaluated 157 consecutive breast cancer survivors (>2 years in remission) who had received standard anthracycline-based chemotherapy and who were without known history of heart failure, ischemic heart diseases, or cardiac dysfunction. All subjects had pre-chemotherapy documentation of preserved LV ejection fraction. Limited echocardiography using MicroMaxx (Sonosite Inc) were performed by a designated trained individual. Results: In our study cohort of breast cancer survivors (mean age 57 ± 10 years, 93% Caucasian, 74% received radiation therapy), none of the subjects had impaired LV ejection fraction (all ≥50%), 2 patients had LV dilatation (LV internal diameter >5.7cm), and 16 (10%) had left ventricular hypertrophy, and 58 (37%) had evidence of diastolic dysfunction by mitral inÀow patterns (E/A <1). This represented <0.5% prevalence of screen-detected cardiomyopathy, which was even below the expected prevalence in the general population. Conclusion: Our data do not support routine surveillance echocardiographic screening for late-onset cardiomyopathy in breast cancer survivors despite prior exposure to cardiotoxic chemotherapy. 1041 Does HER-2 status inÀuence locoregional failure rates after mastectomy in patients with pT1-3pN0 early stage breast cancer? Kwan W, Al-Tourah AJ, Speers C, Kennecke H, Norris B, Olivotto I. BC Cancer Agency, Fraser Valley Centre, Surrey, BC, Canada; BC Cancer Agency, Vancouver Centre, Vancouver, BC, Canada; BC Cancer Agency, Vancouver Island Centre, Victoria, BC, Canada Purpose: To determine if HER-2 positivity inÀuences locoregional failure rates among patients with pT1-3pN0 breast cancer treated with mastectomy and no adjuvant radiotherapy. Methods: Nine hundred and thirty women with known HER-2 receptor status and treated with a modi¿ed radical mastectomy without adjuvant radiotherapy for pT1-3pN0 breast cancer diagnosed between 1986 and 1992 were analyzed for local, regional and distant relapse free survival (LRFS, RRFS & DRFS, respectively). HER-2 positivity was de¿ned as 2+ immunohistochemistry (IHC) stain with a positive FISH, or a 3+ IHC stain. The use of adjuvant systemic therapy (Tamoxifen, chemotherapy or both) was documented. Trastuzumab was not available in the period these patients were treated. Log rank statistics were used to compare 10-year Kaplan-Meier curves of LRFS, RRFS & DRFS. Results: Median follow up was 123 months. 107 (11.5%) patients were HER-2 positive. Equivalent proportion of patients received adjuvant systemic therapy in the HER-2 positive vs. HER-2 negative cohorts (32% vs 27%, respectively, p= 0.3 by Chi-Square test). 10-year LRFS among HER-2 positive patients was 91.5% compared to 86.6% for HER-2 negative patients (p= 0.27). 10-year RRFS for HER-2 positive patients was 88.2% compared to 93.1% for HER-2 negative patients (p= 0.23). 10-year DFRS among HER-2 positive patients was 62.4% compared to 74.7% for HER-2 negative patients (p= 0.03). Conclusions: HER-2 positivity did not signi¿cantly impact locoregional control in pT1-3pN0 breast cancer patients treated with mastectomy. HER-2 positivity on its own is not an indication for radiotherapy after mastectomy. Abstracts – Poster Session I 1042 Elevated JAG1 mRNA expression, associated with the basal phenotype, is a poor-prognosis indicator in lymph nodenegative breast cancer. Reedijk M, Dickson BC, Pinnaduwage D, Mulligan AM, Zhang H, Bull SB, O’Malley F, Egan SE, Andrulis IL. University Health Network, Toronto, ON, Canada; Mount Sinai Hospital, Toronto, ON, Canada; Hospital for Sick Children, The Toronto Medical Discovery Tower, Toronto, ON, Canada Background: While most women with lymph node negative (LNN) breast cancer are cured of their disease, approximately 20% experience a relapse. We have previously shown that expression of the JAG1 gene, which codes for a Notch ligand, correlates with poor overall survival in women with advanced breast cancer. We therefore undertook to test whether expression of JAG1 is associated with reduced disease free survival in LNN breast cancer. Methods: For analysis of JAG1 expression in LNN breast cancer we performed in situ hybridization and immunohistochemistry on approximately 887 samples on tissue microarrays. Results: Moderate to high JAG1 mRNA expression was associated with reduced disease free survival (DFS) in univariate analysis (hazard ratio of 1.58; 95% con¿dence interval, 1.04 to 2.40; p=0.034) and correlated with large tumor size, ER and PgR negativity, high tumor grade, and p53 antibody reactivity. JAG1 mRNA was positively associated with expression of basal breast cancer markers, however, in contrast to the ¿nding that basal gene expression is most strongly associated with reduced DFS in the ¿rst 36 months of followup, JAG1 mRNA expression continued to be associated with reduced DFS through the full follow-up period. Tumors expressing high levels of both mRNA and protein showed reduced disease free survival as compared to all other groups (hazard ratio of 1.73; 95% con¿dence interval, 1.09 to 2.74; p=0.020) in univariate analysis. Conclusions: These data reveal that JAG1 mRNA expression is associated with poor disease free survival in LNN breast cancer over median follow-up greater than 8 years, and con¿rm a synergistic association of elevated JAG1 mRNA and protein with poor outcome in this disease. As JAG1 is a target of several oncogenic signaling pathways, and is a ligand for the Notch pathway, these data provide novel insights into signaling that may contribute to the progression of early stage breast cancer. 1043 Recurrence score by oncotype DX evaluated on the primary breast tumor predicts the 2-year survival after ¿rst relapse. Bianchini G, Zambetti M, Mariani P, Moliterni A, Bianchi G, Mariani G, Fasolo A, Carcangiu ML, Valagussa P, Gianni L. Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy Background: Gene expression pro¿les of the primary breast tumors are most often similar to those in distant metastases eventually developing in the same patient (pt). The aim of the present study was to determine whether the Recurrence Score (RS) assay based on 21-gene expression also predicted prognosis after metastatic relapse. Patients and Methods: Thirty-nine pts at ¿rst relapse after receiving the same neoadjuvant chemotherapy for locally advanced breast cancer in a single institution were evaluated (Gianni et al, JCO 2005). All pts with positive estrogen receptor (ER) received adjuvant tamoxifen. Therapy at distant relapse was not mandated, but was reasonably homogeneous. Oncotype DX™ on paraf¿n-embedded core biopsies was performed at diagnosis of breast cancer and it was not repeated at relapse. Two risk groups were de¿ned using the Recurrence Score cut-off value of 25 used in the TAILORx study. Results: All pts but one were followed for a minimum of 2 years. Of the 39 pts, 11 had a RS≤25 (28%) and 28 a RS>25 (72%). The overall 2-year survival for the 39 pts was 48% and was signi¿cantly different in pts with RS≤25 vs RS>25 (90% vs 32%; log-rank test P<0.01). Univariate analysis showed that RS>25 (HR 11.2; 1.5-84 95% CI; P<0.05), short relapse-free interval (RFI) from surgery (HR 2.79; 1.23-6.31 95% CI; P<0.05, less than 12 vs more than 24 months), and negative ER status (HR 2.6; 1.06-6.41 95% CI; P<0.05) had a signi¿cant association with S55 poorer overall survival. Number of metastatic sites (3 or more) only had a marginal association (HR 2.76; 0.99-7.66 95%CI; P=0.05) and visceral involvement was not signi¿cant. Multivariate analysis of the same variables showed that short RFI (HR 2.85; 1.09-7.47 95% CI; P<.05) and RS>25 (HR 7.18; 0.9-57.7 95% CI; P=0.06) were the only variables inÀuencing survival after relapse. The comparison of the multivariate models with and without the RS by likelihood-ratio test was signi¿cant (p<0.05). Conclusion: The RS assessed on the primary breast cancer by Oncotype DX is also associated with different trends of survival in the ¿rst 2 years after recurrence. 1044 Intracystic papillary carcinoma: a review of 917 cases. Grabowski JE, Saltzstein SL, Sadler GR, Blair SL. UCSD, San Diego, CA; UCSD, La Jolla, CA Background: Intracystic papillary carcinoma (IPC) is an uncommon breast neoplasm. There is limited data about its epidemiology and no clear consensus regarding the optimal management of the disease. Using a large case series, this study aimed to identify speci¿c characteristics of patients with IPC, investigate its natural history, especially as compared to other breast neoplasms, and determine its prognosis in an effort to help develop evidence-based management recommendations for clinicians. Materials and Methods: The California Cancer Registry (CCR), a population-based registry, was reviewed from the years 1988 to 2005. The data were analyzed with relation to patient gender, age at presentation, tumor stage, and overall survival. Relative survival was determined using Berkson-Gage life table analysis and was compared to the relative survival of patients with all other types of invasive and in-situ breast cancers. The CCR classi¿es isolated IPC as either in-situ (CIS) or invasive, as determined by the local pathologist. Results: A total of 917 cases of IPC were identi¿ed in the CCR. While the majority of IPC cases occurred in women (96.5%), 3.5% of cases occurred in men, which is signi¿cantly higher than the rate of all other breast cancers in men (0.6%, p<.001). The median age of IPC patients was 69.5 years old (range 27-99 years). Forty-seven percent of cases (n=427) were CIS while 53% of cases had invasion (n=490). The vast majority of these invasive cases were localized at the time of diagnosis (89.6%, n=439), while 7.8% (n=39) of these cases had regional disease, with either lymph node involvement or direct extension in adjacent tissues. Only 2 of the cases had distant metastasis (0.4%). At 10 years, patients with CIS and invasive disease had a similar relative cumulative survival (96.8% and 94.4% respectively, P=0.18). The overall 10-year relative survival from IPC, whether CIS or invasive was 95.6%, which is similar to the 10-year relative cumulative survival of patients with all other in-situ breast neoplasms (98.1%, p=1), but signi¿cantly better than that of patients with all other types of invasive breast cancer (74.6%, p<.001). Discussion: Intracystic papillary carcinoma is a rare disease, occurring in an older population and in a higher percentage of men than other breast neoplasms. There is no signi¿cant difference in the long-term survival of patients in the two histologically-derived subgroups of IPC. The relative cumulative survival from IPC, whether CIS or invasive, is similar to that of patients with other in-situ breast neoplasms, but signi¿cantly better than patients with other types of invasive breast cancer. 1045 Short term prognostic index for breast cancer: NPI or Lpi. Decock J, Hendrickx W, Van Belle V, Brouckaert O, Pintens S, Van Huffel S, Paridaens R, Amant F, Leunen K, Smeets A, Berteloot P, Van Limbergen E, Weltens C, Van den Bogaert W, Vanden Bempt I, Drijkoningen M, Wildiers H, Vergote I, Christiaens M-R, Neven P. UZ Leuven; ; UZ Leuven, Leuven, Belgium Background: Lymph node involvement is the most important prognostic factor for breast cancer survival, but is confounded by the number of examined nodes. We investigated whether the empirical log odds of nodal involvement (Lpi) is a better predictor of survival than the S56 Abstracts – Poster Session I Nottingham Prognostic Indicator (NPI). Methods: We included 2021 operable breast cancer patients treated in UZ Leuven (2000-2006). NPI de¿nition: 0,2 x tumor size (cm) + grade (1-3) + nodal score (1 if npos = 0; 2 if npos 3; 3 if npos > 3). Lpi de¿nition: tumor size (cm) + 1 if grade 3 or 4 (0 otherwise) + Log ((npos+0,5)/(nneg+0,5)), where npos and nneg are the number of positive and negative nodes (Vinh-Hung et al, SABCS 2006 Poster #5023). NPI and Lpi were categorized in 3 risk levels: low (NPI 3,4; Lpi 0), intermediate (3,4 NPI 5,4; 0< Lpi 5) and high (NPI > 5,4; Lpi > 5). Disease-free survival (DFS) was analysed by Kaplan-Meier. Results: Of 2021 patients, 188 relapsed and 37% had positive lymph nodes. The maximum difference in DFS between the low and high; and the low and intermediate risk group as de¿ned by Lpi is marginally larger than between the corresponding NPI groups, respectively 34% (Lpi) vs 32% (NPI) and 10% (Lpi) vs 9% (NPI). This slight trend could not be found at median follow-up time (42 months), with 15% (Lpi) vs 19% (NPI) for the low and high risk groups and 5% (Lpi) vs 10% (NPI) for the low and moderate risk groups. Node positive patients categorized as moderate risk by the Lpi had a worse DFS than those with a NPI-moderate risk; a tendency which was also found for the low risk group. Interestingly, a signi¿cant proportion of Lpi-moderate (60%) and -low (83%) node positive patients was differentially classi¿ed by NPI into the high and moderate risk group, respectively. Moreover, the survival curve of these patients ¿ts perfectly with the curves of the corresponding NPI risk groups, indicating that the Lpi in fact misclassi¿ed them. This may explain the higher risk of recurrence of the node positive low and moderate Lpi-de¿ned risk groups (table 1). In addition, we were not able to show that the Lpi adds signi¿cant value to the NPI in node positive patients. Discussion: This study does not support the hypothesis that the Lpi is a better prognostic index than the NPI. Moreover, we did not ¿nd an added value of the Lpi to the NPI. Conclusions: SLN biopsy allows a more sensitive evaluation of lymph nodes for the presence of metastatic cells. However, to date, the new microstaging categories are not associated with signi¿cant changes in DFS. Short term recurrence rate for node positive cases comparing NPI with Lpi Low % (r/n)* Moderate % (r/n)* High % (r/n)* NPI 0% (0/24) 9% (27/299) 20% (83/426) Lpi 7% (8/123) 15% (71/484) 22% (31/142) * r/n de¿nes the number of reccurrences in a speci¿c risk group in relation to the number of patients in this group 1046 The microstaging of sentinel lymph node biopsies is not associated with disease-free survival in breast cancer. Pugliese MS, Arthurs ZM, Tickman RJ, Allison KH, Beatty JD. Swedish Cancer Institute, Seattle, WA Introduction: In 2003, the American Joint Committee on Cancer (AJCC) initiated the 6th edition staging criteria, including new pN0i(+) and pN1mic categories for breast cancer. This study examines the signi¿cance of microstaging, which to date is largely uncharacterized. Methods: A single institution’s prospectively collected breast cancer registry was queried to identify patients staged with sentinel lymph node (SLN) biopsy. SLN evaluation included serial sectioning and immunohistochemical stains. SLN biopsies performed before January 2003 were reviewed and re-staged according to 6th edition criteria. Results: During the study period, 954 SLN biopsies [N0i(-)=579, N0i(+)=96, N1mic=76, N1a=157, N2a=34, N3a=12] were identi¿ed with a mean follow-up of 41(±22) months. Compared to a 99% 5-year DFS for pN0i(-), there was no difference in pN0i(+) or pN1mic (DFS = 93% & 98%, respectively; P = 0.231), whereas there was a signi¿cant difference between N1a, N2a, and N3a (DFS = 89%, 81%, & 78%, P<0.01). Cox regression analysis identi¿ed the following variables to negatively impact DFS: Bloom-Richardson Score (hazard ratio [HR] = 1.45; 95% CI, 1.06 to 1.99; P<0.01), pN1a (HR = 7.86; 95% CI, 2.72 to 22.67; P<0.01), pN2a (HR = 8.31; 95% CI, 2.06 to 33.51; P<0.01), pN3a (HR = 17.88; 95% CI, 2.06 to 155; P<0.01). Both ER+ staining (HR = 0.08; 95% CI, 0.2 to 0.40; P<0.01) and hormonal therapy (HR = 0.21; 95% CI, 0.09 to 0.48; P<0.01) improved DFS. Age, tumor size, multifocal disease, lymphovascular invasion, pN0(i+), pN1mic, adjuvant therapy, and type of surgical therapy did not independently impact DFS. 1047 Meta-analysis of gene-expression pro¿les in breast cancer: towards a uni¿ed understanding of breast cancer sub-typing and prognosis signatures. Sotiriou C, Wirapati P, Kunkel S, Farmer P, Pradervand S, HaibeKains B, Desmedt C, Sengstag T, Schütz F, Goldstein DR, Delorenzi M, Piccart M. Institute Jules Bordet, Brussels, Belgium; Université Libre de Bruxelles, Brussels, Belgium; University of Lausanne, Lausanne, Switzerland Background: Breast cancer sub-typing and prognosis have been extensively studied by gene expression pro¿ling, resulting in disparate signatures with little overlap in their constituent genes. The biological roles of individual genes in a signature, the equivalence of several signatures and their relation to conventional prognostic factors are still unclear. Methods: Here we undertook a comprehensive meta-analysis of publicly available gene-expression and clinical data from 18 studies totaling 2833 breast tumor samples. The concept of “co-expression modules” (comprehensive lists of genes with highly correlated expression) was used extensively to reveal the common thread connecting molecular sub-typing and several prognostic signatures, as well as conventional clinico-pathological prognostic factors. Results: The disparity of the gene lists reported by several investigators can be attributed to sampling variation due to small sample size relative to the number of genes examined. Breast tumors were consistently grouped into three main subtypes corresponding roughly to ER- Abstracts – Poster Session I /ERBB2- (basal), ERBB2+ and ER+ (luminal) tumors. ERBB2+ tumors showed an intermediate estrogen receptor module score which is not obvious from the traditional ER and ERBB2 marker status combination. Both, ER-/ERBB2- and ERBB2+ subtypes were characterized by high proliferation, whereas the ER+ subtype appeared to be more heterogeneous. Using our meta-analytical approach we were able to identify 524 genes which were signi¿cantly associated with survival. Of the 524 prognostic genes, 65% were strongly co-expressed with proliferation, 14% with ER, 0.6% with ERBB2, 2.7% with tumor invasion, 1.5% with immune response and 16% with none of our coexpression modules. All previously reported prognostics signatures examined in this meta-analysis (N=9) , despite the disparity in their gene lists, carried similar information with regard to prognostication, with proliferation genes being the common driving force. They were all very useful for determining the risk of recurrence in the ER+ subgroup and much less informative for ER- and ERBB2+ disease. Combining the signatures did not improve their performances. Finally, in multivariate analysis nodal status and tumor size still retained independent prognostic information. Conclusions: This meta-analysis uni¿es various results of previous gene-expression studies in breast cancer. It reveals connections between traditional prognostic factors, expression-based subtyping and prognostic signatures, highlighting the important role of proliferation in breast cancer prognosis. 1048 The presence of a ¿brotic focus and expansive growth pattern in breast tumors is associated with gene expression pro¿les of aggressive tumor biology. Van den Eynden GG, Smid M, Van Laere SJ, Colpaert CG, Van Marck EA, Dirix LY, Vermeulen PB, Foekens JA. (Lab Pathology University of Antwerp/University Hospital Antwerp, Wilrijk; Oncology Center, GH St.-Augustinus, Wilrijk, Belgium), Antwerp, Belgium; Erasmus MC-Daniel den Hoed, Rotterdam, Netherlands ,QWURGXFWLRQ A ¿brotic focus (FF) is a scar-like area of exaggerated reactive stroma formation in the centre of an invasive breast tumor. FF is a practical, easily assessable and reproducible integrative histological prognostic parameter in breast cancer. Furthermore, its presence is associated with an expansive growth pattern (GP), the presence of hypoxia and (lymph)angiogenesis. Little is known about gene expression differences between breast tumors with and without a FF. 0DWHULDOV DQG PHWKRGV: One hundred and three patients were selected of whom microarray data of the tumor and HE slides for histological analysis were available. The GP (in¿ltrative, expansive or mixed) and the presence and size of a FF (no FF, FF<1/3th or FF>1/3th tumor diameter) were assessed. Differential gene expression between tumors with different GPs and sizes of FF was studied using SAM, PAM, GO and KEGG-analysis. Furthermore, the correlation of GP and FF with other molecular breast cancer signatures and with clinico-pathological variables and survival was investigated. 5HVXOWV The presence (p=0.002) and size (p=0.002) of an FF were correlated with an expansive GP. The presence of a FF was associated with the basal-like cell-of-origin subtype (Perou et al. p=0.02), a poor prognosis 76-gene signature (Wang et al. p=0.004), an activated woundhealing signature (Chang et al. p=0.04) and a desmoid-type fibromatosis signature (West et al. p=0.06). The presence of an expansive growth pattern was associated with the basal-like and erbB2-overexpressing subtype (p=0.003), an activated woundhealing signature (p=0.06) and the presence of an invasiveness gene signature (Liu et al. p=0.005). Furthermore, the presence of a FF (p=0.02) and especially of a large FF (p=0.004) was associated with shorter metastasis free survival. Differential gene expression analysis of tumors with different sizes of FF showed an overrepresentation of genes involved in chemotaxis, antigen presentation and processing, humoral immune response and response to external stimuli. Genes overrepresented in tumors with an expansive and in¿ltrative GP belonged to amino acid metabolism, organogenesis and Wnt signaling pathways, and to lipid and phosphorus metabolism, respectively. &RQFOXVLRQ The presence of a FF or expansive GP is associated with gene expression signatures indicative of aggressive tumor behaviour. This is in line with the association of the presence of a FF with shorter S57 survival. Our results furthermore suggest that immune responses and chemotaxis are different between tumors with and without a FF or with different GPs. The Wnt-signaling pathway plays an important role in immune reactions. Whether these differences are also involved in the formation of a FF and their role in tumor progression remains to be elucidated. 1049 An inÀammatory breast carcinoma signature is associated with reduced relapse free survival in patients with noninÀammatory breast cancer. Van Laere SJ, Van den Eynden GG, Van der Auwera I, van Dam P, Van Marck EA, Dirix LY, Vermeulen PB. Lab Pathology University Antwerp and Oncology Center, General Hospital Sint-Augustinus, Wilrijk, Antwerp, Belgium Introduction. InÀammatory Breast Carcinoma (IBC) is an aggressive and highly metastatic form of locally advanced breast cancer, characterized by poor patient survival. We investigated if genes, predictive of the IBC phenotype, can be used to stratify patients with non-InÀammatory Breast Cancer (nIBC) with respect to prognosis. Materials and Methods. RNA was extracted from 19 IBC samples and 40 non-stage matched nIBC samples and hybridized onto Affymetrix HGU133 Plus 2.0 chips. Using the nearest shrunken centroid algorithm, a gene signature predictive of IBC, comprising 281 genes, was identi¿ed. Using a centroid mediated classi¿cation algorithm, this signature was applied onto publicly available gene expression data from 522 nIBC samples (GSE2290, GSE3744 and GSE2034) with survival data of 475 nIBC samples. Samples were classi¿ed as “IBC-like” or “nIBC-like”. Relapse free survival in these groups was compared by the Kaplan-Meier method. In addition, we classi¿ed the same 522 nIBC breast cancer samples according to the Cell-of-Origin Subtypes (Perou et al, Nature, 2000), the Wound Healing Response (WHR) signature (Chang et al, Plos Biol, 2004) and the Invasiveness Gene Signature (IGS) (Liu et al, N Engl J Med, 2007) and compared this to the classi¿cation according to the IBC signature. Cox regression analysis was performed to identify the most predictive signature with respect to relapse free survival. Results. Kaplan-Meier analysis revealed a significant difference between nIBC breast tumours classi¿ed as “IBC-like” and “nIBC-like” (p=0.0044) with respect to relapse free survival. Breast tumours with an “IBC-like” phenotype demonstrate a shorter relapse free survival interval. Classi¿cation according to the IBC signature is signi¿cantly associated with classi¿cation according to the cell-of-origin subtypes (p<0.0001), the WHR signature (p<0.0001) and the IGS (p<0.0001). Breast tumours having an “IBC-like” phenotype generally belong to the Basal-like, ErbB2-Overexpressing or Luminal B cell-of-origin subtypes, are characterized by an activated WHR signature and express the IGS. In addition, a signi¿cant association was found between the IBC signature and the Nottingham Prognostic Grade (p<0.0001). Using a conditional backward Cox regression analysis, the IBC signature was identi¿ed as the most predictive signature with respect to relapse free survival (Exp(B)=1.539, C.I. = 1.140 – 2.077, p=0.005). Discussion. Our data demonstrate that nIBC breast tumours having an “IBC-like” phenotype have a signi¿cantly reduced relapse free survival interval. Remarkably, within this data set, our IBC signature seems to outperform other known classi¿ers with prognostic relevance. Nevertheless, it is important to stress that all signatures are strongly associated, with respect to prognosis. Hence, it can be argued that each signature reÀects a common set of phenotypic traits, associated with poor patient prognosis. 1050 Plasma and serum levels of tissue inhibitor of metalloproteinases-1 are associated with prognosis in nodenegative breast cancer – a prospective study. Würtz SØ, Møller S, Mouridsen H, Hertel PB, Friis E, Brünner N. University of Copenhagen, Frederiksberg, Denmark; Rigshospitalet, Copenhagen, Denmark The tumor tissue level of TIMP-1 has recently been suggested to be a new prognostic marker in breast cancer. The purpose of this study S58 Abstracts – Poster Session I was to investigate whether TIMP-1 also carries prognostic information when measured in blood as this is a much more preferable material compared with tumor tissue extracts. Therefore, using ELISA, TIMP1 was measured in prospectively collected pre-operative plasma and serum samples from 519 patients with primary breast cancer and the measurements were related to patient outcome. The median age of the patients was 58 years (range 38-80 years) and the median follow up time was 1043 days (range 300-1630 days). The results showed that plasma and serum measurements correlated signi¿cantly with each other with a Pearson correlation coef¿cient of 0.75 (p <0.0001). For univariate survival analysis, patients were divided into four groups according to increasing TIMP-1 levels (Q1-Q4) where Q1 was the group with the lowest levels. Analysis of all patients showed that high TIMP-1 plasma levels were signi¿cantly associated with a shorter disease free survival (p = 0.0159). Sub-group analysis showed that plasma TIMP-1 signi¿cantly predicted prognosis in the node-negative group of patients (p = 0.0181) but not in node-positive patients. Importantly, plasma TIMP-1 was even able to further stratify low-risk node negative patients (p = 0.0019). High serum TIMP-1 levels were associated with a shorter disease free survival however the association was not statistically signi¿cant. In contrast, serum TIMP-1 signi¿cantly predicted the prognosis in the group of node-negative (p = 0.0347) and low-risk (p = 0.0204) patients. In multivariate survival analysis of node negative patients including all the classical prognostic parameters, plasma TIMP-1 remained signi¿cantly associated with prognosis when comparing Q1 with Q2 (Hazard ratio = 5.671, p = 0.026) and Q4 (Hazard ratio = 7.054, p = 0.012). Serum TIMP-1 only remained signi¿cant when comparing Q1 with Q4 (Hazard ratio = 4.757, p = 0.0200). Taken together, this study is to our knowledge the ¿rst large prospective study suggesting that TIMP-1 carries independent prognostic information when measured in blood, especially plasma. This was especially true in the node-negative group of patients and even in patients already de¿ned as low-risk patients using the currently available prognostic parameters. 1051 1RQSURSRUWLRQDOEUHDVWFDQFHUPRUWDOLW\SDWWHUQVDFFRUGLQJ WRH[SUHVVLRQRIWKH+(5SURWHLQ using the residual tissue repository of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. Anderson WF, Luo S, Chatterjee N, Rosenberg PS, Goodman MT, Hernandez BY, Reichman M, Dolled-Filhart MM, O’Regan RM, Perou CM, Jatoi I, Cartun RW, Sherman ME. National Cancer Institute, Rockville, MD; University of Hawaii, Honolulu, HI; Hartford Hospital, Hartford, CT; Emory University, Atlanta, GA; University of North Carolina, Chapel Hill, NC; HistoRx, New Haven, CT; National Naval Medical Center, Bethesda, MD %DFNJURXQG Overexpression of the HER2 protein is evident in approximately 20% of all breast cancers. Although generally associated with excess recurrence and death, the time-dependent prognosis according to HER2 expression has never been fully elucidated. 0DWHULDOV: In 2001, the NCI’s Surveillance, Epidemiology, and End Results program supplemented Tumor Registries in Hawaii, Iowa, and Los Angeles to collect tissue blocks from pathology laboratories within their catchment areas, linked to SEER’s main database. We performed immunostains for HER2 (Dako polyclonal, 1:1000) using tissue microarrays (TMAs) of incident invasive breast cancers prepared from cases in the Hawaii Tumor Registry (HTR), diagnosed in 1995 and followed through 2006. HER2+ was de¿ned as 3+ intensity staining in >20-30% of tumor cells. 5HVXOWV: The TMAs contained 354 breast cancer cases, representing 51% of corresponding cases in the 1995 HTR. TMAs and HTR cases were similar with respect to age-at-diagnosis, size, grade, histology, stage, and estrogen receptor. HER2+ was detected in 12% of 350 cases with evaluable tissue cores. HER2+ was associated with younger agesat-diagnosis, positive nodes (39%), and negative estrogen receptors (68%). HER2+ actuarial survival declined rapidly for 38 months then plateaued near 75%, with no subsequent breast cancer deaths. HER2+ hazard rates peaked near 8% per year, 2 years following diagnosis then declined. &RQFOXVLRQ: We assessed the time-dependent risk of breast cancer death in patients who were diagnosed with HER2+ tumors, prior to the availability of adjuvant trastuzumab. Trastuzumab naïve HER2+ breast cancer mortality was non-proportional, showing short-term excess hazard and long-term event free survival. 1052 Reassigned to 3113 1053 Patterns of metastatic spread in triple negative breast cancer. Dent R, Trudeau M, Sun P, Narod S. Sunnybrook Health Sciences Center, Toronto, ON, Canada; Women’s College Hospital, University of Toronto, Toronto, ON, Canada Background and Purpose: It is widely recognized that triple-negative breast cancers (de¿ned as those that are estrogen receptor-negative, progesterone receptor-negative and HER2neu-negative) have a poorer prognosis than other subtypes of breast cancer. However, the pattern of disease spread is not well established. Methods: We studied a cohort of 1601 patients with breast cancer, diagnosed between January 1987 and December 1997 at Women’s College Hospital in Toronto. Triple-negative breast cancers were de¿ned as those that were estrogen receptor-negative, progesterone receptornegative and HER2neu-negative. We set out to determine the temporal distribution and pattern of metastatic spread in triple negative breast cancers versus other breast cancers. Results: The median follow-up time of the 1601 women was 8.1 years. 180 of 1601 patients (11.2%) had triple-negative breast cancer. Compared to other women with breast cancer, those with triple-negative breast cancer had an increased likelihood of distant recurrence (hazard ratio (HR) 2.6; 95 % CI: 2.0 - 3.5, p<0.0001) and death (HR 3.2; 95 % CI: 2.3 - 4.5; p<0.001) within ¿ve years of diagnosis. The probability of developing visceral metastases was signi¿cantly higher among women with triple-negative breast cancers compared to other women with breast cancer (p< 0.0001; see ¿gure 1). However, there was no difference in developing bone metastases between the two groups (p= 0.6). Visceral metastases occurred early in the follow-up of women with triple-negative breast cancer with no visceral metastases occurring after eight years of follow-up. Compared to other women with breast cancer, those with triple-negative breast cancer were also more likely to present with visceral metastases (vs. bone metastases) as their ¿rst site of metastatic spread (81 vs. 50%, p = 0.0003). Conclusions: There is a predominance towards visceral metastases in women with triple-negative breast cancer suggesting that these tumors possess a distinct mechanism of metastatic spread. The pathways driving these tumors are still poorly understood; however the development of targeted therapies could result in better outcomes for these patients. Abstracts – Poster Session I S59 1055 Impact of hormone replacement therapy on breast cancer: Women’s Healthy Eating and Living (WHEL) study experience. 1054 E-cadherin levels may predeict outcome in inÀammatory breast cancer (IBC). Levine PH, Ganesan C, Young HA, Portera C, Yang S, Swain SM. The George Washington University Medical Center, Washington, DC; National Cancer Institute, Bethesda, MD; Washington Hospital Center, Washington, DC Background: IBC is the most aggressive and lethal form of breast cancer. One of the most common biomarkers implicated in IBC is e-cadherin overexpression in the tumor cells. In our earlier study of tumor markers in IBC (Portera et al, SABCS 2006) mean e-cadherin expression was higher in IBC patients than controls but there was wide individual variation. In this report we describe the relationship of clinical parameters to e-cadherin levels. Materials and Methods: The e-cadherin in all 48 IBC Registry patients with pathologic con¿rmation (involvement of the dermal lymphatics) that were part of our earlier study were analyzed by our earlier criteria as high (>/=1.03, n=29) or low (n=19) levels. Their responsiveness to chemotherapy was assessed based on the presence of pathological evidence of residual tumor at mastectomy and both patient’s and the oncologist’s assessment of the clinical response to chemotherapy. The responses were broadly divided into excellent/good, partial, and none/ poor responses. Comparative analysis also included Her2neu, ER, PR status, progression-free survival (PFS) and overall survival (OS), stage at diagnosis and presence of metastasis. Results: All patients in the low e-cadherin expression category had either an excellent /good response to chemotherapy or a partial response. In the high level category 3 had no response and none had an excellent response to chemotherapy. Patients with higher levels were more likely to present with metastatic disease (62% vs 31%) and be Her2/neu positive (72% vs 21%, p=.0002). 17% of the patients in the high category presented with Stage 4 disease vs. 5% in the low category. No difference was seen regarding ER/PR receptors. Mean PFS was 842 for the high and 1424 for the low group (p=0.93, NS).but there was no apparent difference in OS. Discussion: The results of this study suggest that e-cadherin overexpression is associated with increased aggressiveness of pathologically con¿rmed IBC. It is speculated that the increased adhesiveness of the cells facilitates the establishment of microemboli. Parker BA, Flatt SW, Mortimer JA, Natarajan L, Gold EB, Bardwell WA, Jones LA, Hollenbach KA, Pierce JP. University of California, San Diego, La Jolla, CA; University of California, Davis, Davis, CA; The University of Texas, Houston, TX Prior hormone replacement therapy (HRT) has been associated with an increased incidence of breast cancer. Conflicting information exists regarding the impact of prior HRT on subsequent breast cancer development. We utilized data from the Women’s Healthy Eating and Living (WHEL) Study to determine the natural history of breast cancer in women who reported HRT prior to their diagnosis of breast cancer. Our aim was to determine the features of breast cancer, the severity of vasomotor symptoms, and the disease-free survival in women with breast cancer and reported prior HRT as compared with no reported prior HRT. The WHEL Study is a multi-institutional randomized trial of dietary change to a diet high in vegetables and fruits in Stage IIIIA breast cancer patients within 4 years of diagnosis. Baseline data regarding tumor characteristics, demographics, and the Thoughts and Feelings questionnaire regarding vasomotor symptoms were analyzed. A total of 1544 patients randomized to the non-intervention group were included in this analysis. We used bivariate statistics to assess the association of reported prior HRT with covariates, logistic regression to analyze tumor histology, and a proportional hazards model for diseasefree survival. A total of 706 patients reported prior HRT including 453 who received combined estrogen and progesterone HRT for a mean of 6.8 years and 216 women with estrogen alone HRT for a mean of 9.3 years. The results of our analysis indicate that patients reporting prior HRT as compared with no prior HRT were older (mean 57 versus 48 years), had a higher incidence of lobular cancer (10.2 % versus 6.2%), had lower grade tumors (18.4% Grade 1 versus 13.6%), were more likely to report hot Àashes (74.9% versus 60.6%), were more likely to report night sweats (58.3% versus 48.0%), were more likely have ER+PR+ tumors (63.6% versus 59.3%), and had a greater likelihood of being disease-free at 7.3 years follow-up (84.7% versus 81.3% as of June 1, 2006). In multivariate models, reported prior HRT weakly predicted lobular histology of the original primary tumor (OR = 1.53, 95% CI = 0.99 – 2.36) but did not predict disease-free survival (HR 0.78, 95% CI = 0.58-1.06). However, the signi¿cant predictive effect on disease-free survival of low tumor stage, low tumor grade and presence of hot Àashes remained. These results add to reports suggesting that prior HRT is associated with an increased incidence of lobular histology at diagnosis. In our study, prognosis was similar regardless of prior reported HRT. 1056 Survival outcomes in pregnancy-associated breast cancer. Ali A, Wang Y, Kelly J, Falk J, Sehgal R, Vogel V. University of Pittsburgh Medical Centre, Pittsburgh, PA; University of Pittsburgh, Pittsburgh, PA Introduction: Pregnancy-associated breast cancer (PABC) has been de¿ned as breast cancer diagnosed during pregnancy or within one year of delivery. It is currently believed that after adjusting for age and stage, the 5-year survival rates are the same in both pregnant and non-pregnant women. Methods: We conducted a retrospective casecontrol study among patients treated at our institution between 1990 and 2005 to compare the ¿ve-year survival outcomes for PABC with women treated for breast cancer but not pregnant. Women were matched for age and stage of breast cancer at diagnosis. Overall survival (OS) and disease-free survival (DFS) were estimated by the Kaplan-Meier method, and log rank tests were used to assess the associations between OS, DFS and pregnancy status, HER2 status, ER/PR status and family history. Multivariate Cox regression was used to assess the association between OS, DFS and pregnancy status after adjusting for age, stage, family history, ER/PR status, radiotherapy and chemotherapy. Results: Forty women treated for PABC were compared with forty age- and stage–matched, non-pregnant controls. The median age was 33 yrs (range 24-42) for both PABC and non-pregnant groups. Five had stage S60 Abstracts – Poster Session I I, 27 had stage II, 6 had stage III and 2 had stage IV disease in the PABC group, while 5 had stage I, 27 had stage II, 7 had stage III and 1 had stage IV disease for non-pregnant group. Twenty- three (57.5%) patients in the PABC group had a family history of breast cancer in a ¿rst-degree relative compared to 17 (42.5 %) in the non-pregnant group. Twentytwo (55%) patients with PABC were ER/PR receptor positive compared with 20 (50%) for the controls. Of the 11 women with known positive HER2/neu status, 4 belonged to the PABC group while 7 were not pregnant. 90% of patients with PABC received chemotherapy compared with 87.5% in the non-pregnant group. 91.5% of patients with PABC had breast-conserving surgery and 8.5% had mastectomies compared to 86 % and 14%, respectively, for the non-pregnant group. The median overall survival was 4.9 years in the PABC group compared to 6 years for the controls (p = 0.02). The median disease-free survival was 2.7 years for the PABC group compared with 5.1 years for the controls (p = 0.01). The most common site of relapse was bone for the PABC group (27%) and local recurrence (33%) for the controls. In the univariate analysis, OS and DFS were signi¿cantly associated with pregnancy status, family history, ER/PR status, age and stage. After adjusting for age and disease stage, PABC patients had higher risk of both death (p = 0.01) and recurrence (p = 0.02) compared to non-pregnant controls. Conclusion: Women with PABC had signi¿cantly shorter overall survival and shorter disease-free survival compared with non-pregnant age- and stage-matched controls. 1057 Clinicopathological and prognostic relevance of uptake level revealed by 18F-Àuorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18FFDG PET/CT) in primary breast cancer. Ueda S, Tsuda H, Asakawa H, Omata J, Fukatsu K. National Defense Medical College, Tokorozawa, Saitama, Japan 385326( Integrated 18F-Àuorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/ CT) can visualize anatomical localizations of hypermetabolic cancer lesions more accurately than 18F-FDG PET alone. In this study, the clinicopathological and prognostic signi¿cance of 18F-FDG PET/CT was evaluated in patients with primary breast cancer. 0(7+2'6 Clinicopathological correlation with the maximum Standard Uptake Value in 60 min (SUV) obtained by preoperative 18FFDG PET/CT was examined in 162 patients with primary breast cancer. The prognostic implications of the SUV were simulated by means of the software program Adjuvant! in 146 (90%) patients with invasive ductal carcinoma (IDC). RESULTS: High SUV detected by 18F-FDG PET/CT was signi¿cantly correlated with the size of the invasive component (2 cm<) (p<0.0001), higher nuclear grade (p<0.0001), nuclear atypia (p<0.0001), mitosis count (p<0.0001), negative hormone receptor status (p=0.001), high c-erbB-2 expression (p=0.006), lymph node metastasis (p=0.002), and IDC in comparision with invasive lobular carcinoma (p=0.004). The prognostic impact of SUV in 146 IDCs was explored for six tentative SUV thresholds: 2.0, 3.0, 3.5, 4.0, 4.5, and 5.0. Tumors with high SUV showed poorer relapse and mortality rates than those with low SUV, and SUV 4.0 was the most discriminable cut-off value (t=-5.99 and p<0.0001). &21&/86,216 High uptake of 18F-FDG is predictive of aggressive features of cancer cells and poor prognosis in patients with primary breast cancer. 18F-FDG PET/CT could be a useful tool for pretreatment prediction of the biological characteristics and baseline risk of breast cancer. 1058 Prognostic differences of WHO-assessed mitotic activity index (MAI) and mitotic impression by quick scanning in invasive ductal breast cancer patients under 55 years of age. Skaland I, van Diest PJ, Janssen EAM, Gudlaugsson E, Søiland H, Baak JPA. Stavanger University Hospital, Stavanger, Norway; University Medical Center, Utrecht, Netherlands; University of Bergen, Bergen, Norway; Free University, Amsterdam, Netherlands Background: The proliferation marker mitotic activity index (MAI) is the strongest prognostic/predictive indicator in node-negative (LN-) breast cancer (1, 2). The World Health Organization (WHO) 2003 de¿ned procedure for determining MAI (WHO-MAI) is often replaced by a quick-scan mitotic impression (MIMP). Material and Methods: We evaluated the prognostic consequences of this practice in 433 LN- invasive ductal type breast cancers with longterm follow up (median 112 months, range 12-187 months). Results: Twenty-seven percent of the studied cases developed distant metastases, and 25% died of disease. Agreement between WHO-MAI (0-5=1, 6-10=2, >10=3) and MIMP (1, 2, 3) categories was 66% (kappa=0.41), including 85% for category 1, 26% for category 2, and 52% for category 3. The WHO-MAI was a much stronger prognosticator than the MIMP (Figure 1), and the 10-year survival rates of the same categories (e.g., MAI and MIMP category both 2) differed greatly (Table 1). When grade was assessed by combining WHO-MAI or MIMP with the same values for tubular formation and nuclear atypia, grades disagreed in 18% of the cases. Discussion: Deviation from the formal WHO-MAI assessment guidelines in breast cancer often results in erroneous prognosis estimations with therapeutic consequences and may explain why the prognostic value of proliferative activity in breast cancer is not always con¿rmed. References 1. Baak JP, van Diest PJ, Voorhorst FJ, et al: Prospective multicenter validation of the independent prognostic value of the mitotic activity index in lymph node-negative breast cancer patients younger than 55 years. J Clin Oncol 2005; 23(25):5993-6001. 2. Janssen EA, van Diest PJ, Soiland H et al. Success predictors of adjuvant chemotherapy in node-negative breast cancer patients under 55 years. Cell Oncol. 2006;28(5-6):295-303. Figure 1. Comparison of the signi¿cance of no probability in predicting recurrence free survival by the MAI, the grade based on MAI, the quick-scan derived MIMP, and the grade based on MIMP. MAI, mitotic activity index; MIMP, mitotic impression. Abstracts – Poster Session I S61 1060 The prognostic signi¿cance of human epidermal growth factor receptor-2 over-expression for the development of local recurrence after newly diagnosed breast cancer. 1059 Complementary and alternative therapies among long-term breast cancer survivors. Carpenter CL, Ganz PA, Bernstein L. Keck School of Medicine at USC, Los Angeles, CA; David Geffen School of Medicine at UCLA, Los Angeles, CA Background: Increasing numbers of healthy adults are using complementary and alternative medicine (CAM), in conjunction with or instead of usual medical care. Breast cancer patients may be more or less likely to use CAM than healthy adults. That is, breast cancer patients may be more compliant with conventional treatment and less likely to use CAM if they fear their cancer is worsening. On the other hand, breast cancer patients may turn to CAM because conventional therapies are not working. We conducted a descriptive study that examined the qualityof-life (QOL) of long-term breast cancer survivors, in relationship to potential associations with CAM and other psychosocial, lifestyle, behavioral and medical characteristics, to determine whether CAM users had different patterns of association than non-CAM users. Materials and Methods: We conducted a follow-up telephone interview with breast cancer case patients from a population-based epidemiological case-control study of breast cancer in young women in Los Angeles County, California, that had survived at least 10 years. Three hundred seventy four (374) were interviewed about surgical and reconstructive history, disease-related and lifestyle factors, weight and exercise history. CAM usage was measured by summarizing a list of 28 commonly used herbal or alternative remedies. QOL was measured using the Medical Outcomes Study Short Form 36 questionnaire (SF-36). Results: CAM users in our study population were over-represented (59%) in comparison to nationwide population estimates for women using a similar CAM de¿nition (39%). Age, MET-hours of exercise after diagnosis, extent of original disease, prevalence of smoking, body-mass index, alcohol consumption, and fear of recurrence were similar, on the average, for CAM users compared to non-CAM users. Evaluating SF-36 sub-scores, CAM users had signi¿cantly lower scores on emotional well-being (p = 0.01), and had signi¿cant emotional role limitations (p = 0.06) compared to non-CAM users. Physical functioning sub-scale scores did not differ. Discussion: Moderate differences in emotional functioning among breast cancer survivors may exist between CAM users and non-CAM users. Gabos Z, Thoms J, Hanson J, Ghosh S, Deschenes J, Mackey J, Abdulkarim B. Cross Cancer Institute, Edmonton, AB, Canada; University of Alberta, Edmonton, AB, Canada Background: Human epidermal growth factor receptor-2 (Her-2) overexpression occurs in 20-30% of invasive breast cancer and results in aggressive disease and high-risk of recurrence. The impact of Her-2 over-expression on the risk of local recurrence is unclear. Objectives: In this population-based study, we have investigated the incidence of local recurrence in newly diagnosed breast cancer patients with Her-2 over-expression. Methods: Newly diagnosed breast cancer patients between 01/1998 and 12/2003 with uniform Her-2 testing were identi¿ed from a cancer registry. A total of 460 Her-2 over-expressing patients were reviewed. A random sample of 500 patients with Her-2 negative disease was also reviewed. Patients were excluded if there was a breast cancer diagnosed before 01/ 1998 or other cancer. A total of 266 Her-2 positive and 338 Her-2 negative patients were included for this analysis. The groups were strati¿ed based on surgical treatment, lumpectomy versus mastectomy. The association between histological features and local recurrence was evaluated with univariate and multivariate analyses. Results: In patients treated by lumpectomy, Her-2 over-expression was the only factor to be associated with increased risk of local recurrence, on both univariate and multivariate analysis, hazard ratio 7.4 (95% CI, 1.6-33.9, p=0.01). In patients treated by mastectomy it was not associated with increased risk of local recurrence. Conclusions: In our population-based study, Her-2/neu over-expression is signi¿cantly associated with increased risk of local recurrence in newly diagnosed breast cancer patients treated by lumpectomy. In patients treated by mastectomy, Her-2 over-expression is not associated with an increased risk of local recurrence. 1061 Do grade I breast cancers require follow-up after breast conserving treatment? Hamed H, Jones G, Allen D, Kontos M. Guy’s Hospital, London, United Kingdom INTRODUCTION An increasing number of institutions are abandoning routine follow up after breast conserving treatment (BCT) for early breast cancer. However there is growing body of evidence indicating that breast cancer is not a single disease with some types having a more “benign” course present minor clinical problems following treatment. The discontinuation of follow up of all breast cancer patients regardless of cancer subtypes could potentially lead to delayed in diagnosis of recurrence especially among the cases with the more “aggressive” tumors. The aim of this study is to investigate the rate of the recurrences of grade I breast cancers, which conventionally are regarded as the more “benign” ones and to compare it to the other grades’ in an attempt to customize follow-up strategies. PATIENTS AND METHODS Breast cancer patients who had Breast conserving treatment (BCT) between the years 1990 and 1997 and followed up at Guy’s Hospital, Breast Unit formed the basis for this study. Cases were identi¿ed from the Patient Electronic Database. They were divided into 3 groups based on the histological grade (I, II or III). Patients that presented with a loco-regional relapse and contralateral disease for each group were identi¿ed. Recurrence rates were calculated and statistically compared. Correlation between the exact location of recurrence (ipsilateral or contralateral breast, axilla, supraclavicular fossa or skin), the mammographic positivity, method of detection (recurrence detected by the patient, the doctor or the mammogram) and node positivity were studied for each group. RESULTS Six hundred and ¿fty patients received BCT during the study period. Of those 115 were grade I, 279 grade II and 256 grade III. Median follow S62 Abstracts – Poster Session I up was 115 months (range 2-196 months). Loco-regional recurrences were diagnosed in 3 cases (2.6%), 45 cases (16.1%) and 41 cases (16%) in grade I, II, III respectively. The difference between grades I and II and between grades I and III was statistically signi¿cant (p=0.000191 and 0,000221 respectively). The location (ipsi, contra, axilla etc) of the recurrence, the mammographic positivity, the method of detection of recurrence were analyzed. In multivariate analysis tumor grade was an independent risk factor. The 3 relapses in the grade I group occurred at year 9 (2 of the 3 had one axillary node involved in metastatic disease at the time of primary diagnosis and treatment) and were n the breast parenchyma and were seen on mammography. CONCLUSION Patients treated with BCT for grade I breast cancer present very low risk of loco-regional recurrence or contralateral disease. Relapses were con¿ned to breast parenchymal with no evidence of local regional disease. The data from this study suggest that patients who presented with grade I breast cancer and treated with BCT can be safely discharged after completion of their treatment to The national mammographic screening program. 1062 Prognostic factors for BRCA1/2-associated familial breast cancer from Russian population. Lyubchenko LN, Pospechova NI, Lushnikova AA, Portnoy SM, Bryuzgin VV, Karpukhin AV, Garkavtseva RPh. N.Blokhin Cancer Res., Center RAMS, Moscow, Russian Federation; Research Center for Medical Genetics, Moscow, Russian Federation Background: It has been demonstrated that cancer arising in carriers of mutation in BRCA1/2 genes differs from sporadic breast cancer (BC) of age-matched control. We have screened the patients from cancer genetics registry of N.Blokhin Cancer Res.Center, Moscow for germline mutations in BRCA1/2 genes to prove this observation. Materials and Methods: DNA samples from 250 breast and/or ovarian cancer patients with strong cancer history were studied using PCR, CSGE and direct sequencing. Mouse mammary tumor virus (MMTV)-homologous sequences were analyzed by lymphocyte and BC tissue DNA sample PCR using primers for gp52- coding area of the env MMTV gene, Sagcoding area of 3’LTR and sequencing. Multivariant analysis includes 64 cases of BRCA1-linked BC. Control group consisted of 117 patients with sporadic BC selected on the basis of age and disease stage. A mean age was 39 years old in cancer patients group and 41 years old – in control group. A mean menarche age was 13.3 years old in BRCA carriers and 13.7 years old in sporadic cancer patients. Results: 94(33.2%) BRCA1/2 mutations carriers have been detected. High frequency of the mutation 5382insC (76.4% of all revealed mutations) was shown. In 8 (12.2%) BC patients with pathological BRCA genotype BC developed during pregnancy. Histopathological characteristics of BRCA-associated BC were the following: (1) in¿ltrated ductal carcinoma - 89.8%/87.7%; (2) high grade – 58.2%/29.2%; (3) prominent lymphocyte in¿ltrate – 60.2%/34.5%; (4) negative estrogen receptors – 77.6%/38.8%; (5) complete clinical response to primary chemotherapy (anthracyclinbased treatment) followed by surgical treatment – 98.1%/38.2%, compared with the control group (p<0.05). MMTV-related sequences with 92-95% homology with MMTV (C3H, GR strains) were revealed by speci¿c PCR in 38% of sporadic BC patients (n=180), in 52% of familial BC patients (n=84) and in 57-60% BC patients during pregnancy and lactation (n=65). MMTV- related exogenous retroviral infection might be considered as BC risk factor, especially in familial BC and BC during pregnancy or lactation. 1063 Restrati¿cation of the Nottingham prognostic index using carcinoembroinic antigen cell adhesion molecule 6. Maraqa L, Cummings M, Peter MB, Hanby AM, Shaaban AM, Horgan K, Speirs V. St James’s University Hospital, Leeds, West Yorkshire, United Kingdom; Leeds General In¿rmary, Leeds, West Yorkshire, United Kingdom Introduction: Carcinoembryonic Antigen Cell Adhesion Molecule (CEACAM) 6 is a marker of aggressive disease in colonic, pancreatic and other carcinomas. Its role in human breast cancer, however, remains poorly understood. Previous work in our laboratory indicated that CEACAM 6 was signi¿cantly up-regulated in tamoxifen-resistant MCF-7 derivatives compared to sensitive controls. The aim of this study was to retrospectively test its prognostic signi¿cance in a cohort of breast cancers with long term follow up. Methods: CEACAM 6 immunohistochemistry was performed on tissue microarrays comprising 108 primary breast cancers which subsequently relapsed following adjuvant endocrine therapy and 243 non-relapsed controls. Mean age at diagnosis was 58.1 years (SD 13.9) with follow up time of 81.5 months (range 1 – 229 months, SD 43.1). CEACAM 6 staining was scored based on the proportion of positive cells and intensity of membranous, cytoplasmic and combined global staining. A maximum score of 3 indicated strong staining in ≥10% of cells. After case dichotomisation using ROC curves, CEACAM 6 was incorporated into an outcome predictor model using Cox regression analysis. Results: Of patients who subsequently developed a recurrence, 35/108 (33.3%) demonstrated moderate to strong membranous CEACAM staining. This was signi¿cantly higher than the control group, 32/243 (13.2%), OR = 3.16 (95% CI 1.83 to 5.47, p < 0.0001). Although tumour size, grade, lymph node positivity, HER-2 expression and cytoplasmic and global CEACAM expression were signi¿cant on univariate analysis, only the Nottingham Prognostic Index (NPI), PR and membranous CEACAM 6 remained sigini¿cant on multivariate analysis. Using our outcome predictor model, patients were strati¿ed into either low or high risk groups with no intermediate categories. This performed better than NPI alone. Moreover, it successfully restrati¿ed the NPI intermediate risk group into higher or lower risk categories. Using this model, 10-year Disease Free Survival was 39% for higher risk patients versus 73% if lower risk, log rank p < 0.001. Conclusion: Our ¿ndings strongly support the importance of CEACAM 6 as a prognostic model. Its signi¿cance lies in re-categorisation of patients in the intermediate NPI group, potentially facilitating chemotherapy decisions. Abstracts – Poster Session I S63 Conclusion Our results show that the 70-gene signature outperforms other prognostic factors in selecting a low risk group that has a 10-year survival of > 90%. After validation in an independent sample series the prognostic value of the 70-gene signature in patients with 1-3 positive nodes will be prospectively validated in the MINDACT trial. Incorporation of the 70-gene signature in clinical decision-making for patients with 1-3 positive nodes may lead to reconsider the need of adjuvant chemotherapy. 1065 Quantitative justi¿cation of the change from 10% to 30% for HER-2 scoring in the ASCO-CAP guidelines: tumor heterogeneity in breast cancer and its prognostic and predictive implications. 1064 The Amsterdam 70-gene signature predicts outcome in breast cancer patients with 1-3 positive axillary lymph nodes. Mook S, Rutgers EJT, Peterse JL, Nuyten DSA, Horlings H, van de Vijver MJ, van ‘t Veer LJ. Netherlands Cancer Institute, Amsterdam, Netherlands Introduction The axillary lymph node status is considered to be the most powerful prognostic factor for operable breast cancer, with a direct relationship between number of positive nodes and disease outcome. However, approximately 30% of lymph node-positive patients will remain free of distant metastases without adjuvant chemotherapy. Identifying patients with lymph node-positive disease who are at low risk of recurrence might lead to changes in guidelines for adjuvant chemotherapy. The aim of this study was to identify a low risk group with an excellent disease outcome in breast cancer patients with 1-3 positive lymph nodes, using the 70-gene signature (MammaPrint®). Methods One-hundred-six patients with 1-3 positive lymph nodes were separately selected from the previous described series of 295 patients (Van de Vijver et al. NEJM 2002). Patients were diagnosed between 1984 and 1995 at the Netherlands Cancer Institute, and under the age of 53 at diagnosis. Tumors were primary invasive breast carcinomas less than 5 cm, treated by modi¿ed radical mastectomy or breast-conserving therapy, including dissection of the axillary lymph nodes. Eightytwo percent received adjuvant systemic treatment, consisting of chemotherapy (59,4%), hormonal therapy (12,3%) or a combination (10,4%). Gene expression signatures had been obtained previously; clinical follow-up data were updated. Results Of the 106 patients 18 developed distant metastasis, and 88 were free of disease at a median follow-up of 10.3 years. The median time to distant metastasis was 2.8 years. Using the 70-gene signature 43 patients were classi¿ed as having a good-prognosis signature, while 63 patients were classi¿ed as having a poor-prognosis signature. At 10 years, the probability of remaining free of distant metastases and overall survival was 94% (SE 4%) and 97% (SE 3%) in patients with a good-prognosis signature versus 66% (SE 7%) and 62% (SE 7%) in those with a poorprognosis signature, respectively. The estimated hazard ratio (HR) for overall survival in the poor-prognosis signature group as compared with the good-prognosis signature group was 7.0 (95% CI 2.1-23.3). When adjusted for clinicopathological prognostic factors, the 70-gene signature was the strongest predictor with an estimated HR for overall survival of 4.2 (95% CI 1.0-17.7). Other independent prognostic factors were angioinvasion and adjuvant systemic therapy with hazard ratios of 2.7 (95% CI 1.1-6.7) and 0.3 (95% CI 0.1-0.8) respectively. Moeder CB, Giltnane JM, Harigopal M, Molinaro A, Robinson A, Gelmon K, Huntsman D, Camp RL, Rimm DL. Yale University School of Medicine, New Haven, CT; British Columbia Cancer Agency, Vancouver, BC, Canada Purpose: The variability in scoring of immunohistochemistry(IHC), whether due to true heterogeneity or artifacts in preparation, has led to decreased reliability in companion diagnostics and the recommendation for new standards (eg the ASCO-CAP guidelines for HER-2 testing). The basis of this problem is the amount of tissue required to be representative of an entire tumor. Since protein expression on tissue microarrays(TMAs) can be rigorously measured, and one 0.6mm spot is equivalent to 2-3 high power ¿elds, we used TMAs assess levels of heterogeneity and to determine optimal representation as a function of outcome. Patients and Methods: We analyzed estrogen receptor (ER), progesterone receptor (PR) and HER-2 expression quantitatively using AQUA® on a series of 5 separate tissue microarrays made from a retrospective cohort from Yale New Haven Hospital of nearly 700 breast cancer cases with known outcome. We assessed heterogeneity for each of the markers by comparing the unique array spots using linear regression analysis. A minimum, average, and maximum score was generated for each set that was then assessed for prognostic value. A similar analysis was done on a 152 case retrospective trastuzumab treated cohort (metastatic breast cancer) collected at the British Columbia Cancer Agency with RESIST-based outcome. Results: Each marker shows some heterogeneity, but average r values between 0.7 and 0.8 are seen between TMA spots. Analysis for prognostic value shows that a high maximum score (of 5 spots) is the most prognostic for ER, while a high minimum score is most prognostic for poor outcome for HER-2. A high minimum HER-2 score was also most predictive of response in the trastuzumab treated cohort. Conclusions: These results suggest that representivity required for each biomarker may be a function of its role in tumorigenesis. Furthermore, these results provide scienti¿c basis for the ASCO-CAP guidelines for assessment of HER-2 expression, but perhaps suggest that the 30% ¿gure is still too conservative. 1066 HER2 status adds prognostic, but not tamoxifen treatment predictive, information in hormone receptor positive premenopausal primary breast cancer. Rydén L, Fernö M, Stål O, Landberg G, Bendahl P-O. Clinical Science, Lund, Lund, Sweden; Biomedicine and Surgery, Linköping, Sweden; Laboratory Medicin, Malmö University Hospital, Malmö, Sweden Background: Overexpression of human epidermal growth factor (HER2) or ampli¿cation of its gene is a prognostic tumour marker in primary breast cancer considered a predictor for tamoxifen treatment ef¿ciency in oestrogen receptor (ER) positive disease. In the present study we used a de¿ned cohort of breast cancer patients in order to assess prognostic and tamoxifen treatment information yielded by S64 Abstracts – Poster Session I HER2 status. Methods: Premenopausal breast cancer patients with stage II tumours (n=564) randomised to two years of adjuvant tamoxifen treatment versus no treatment with long-term follow-up data were included. ER and progesterone receptor (PR) status and HER2 status was determined by immunohistochemistry using a tissue microarray. HER2 ampli¿cation was analysed by Àuorescense in situ hybrydisation (FISH) and tumours being ampli¿ed and/ or HER2 3+ were considered HER2 positive. Result: HER2 status was evaluable in 83% of the patients and 12.6% were HER2 positive. In the control arm, HER2 positivity was a prognostic factor in ER+ patients, HR 2.95; 95% CI 1.61-5.38, p<0.001, but not in ER- patients, HR 0.67; 0.28-1.61, p=0.4, and a prognostic interaction between the two markers p=0.008 was found. Two years of adjuvant tamoxifen was bene¿cial in the ER + and HER2- cohort (n=275), (HR 0.64; 95% CI 0.44-0.93, p=0.02), whereas no signi¿cant effect by tamoxifen was seen in the ER+ and HER2+ cohort (n=24), (HR 0.71; 95%CI 0.23-2.20, p=0.6). However, when the treatment effect was explored using a multivariate interaction model including HER2-status and treatment, there was no statistically difference in tamoxifen treatment ef¿ciency according to HER2 status (term of interaction, p=0.95). Discussion: HER2 positive and hormone receptor positive breast cancer constitutes a small subgroup of tumours with poor prognosis in premenopausal breast cancer deserving to be identi¿ed in the clinical setting in order to optimise adjuvant treatment options. In this study, no tamoxifen treatment interaction was found for HER2 status in ER+ tumours. The strong prognostic interaction between HER2 and ER should be taken into account when interpreting HER2 data in nonrandomised trials of adjuvant tamoxifen. Figure 1. Comparison of the overall long follow-up survival associated with MAI in patients with (a) tumours <1 cm diameter (all grades), (b) 1–2 cm, grades 1+2 1067 Prospective prognostic value of proliferation in small, lowgrade, lymph-node negative breast cancers. Baak JPA, Van Diest PJ, Janssen EAM, Voorhorst F, and Other MMMCP Collaborators. Stavanger University Hospital, Stavanger, Norway; The Gade Institute, University of Bergen, Bergen, Norway; University Medical Center, Utrecht, Netherlands; Free University Medical Center, Amsterdam, Netherlands Background: The proliferation factor Mitotic Activity Index (MAI) is the strongest prognosticator in lymph-node negative invasive breast cancer patients under age 71, and predictor of successfulness of systemic adjuvant chemotherapy in node negative women under 55 years1,2. The question remains, however, whether this also holds for tumors <1 cm in diameter, in tumors ≥1 and <2 cm and grades 1+2, and tumors ≥2 and <3 cm) < 3 cm and, grades 1+2. Materials and methods: Multicenter prospective survival analysis of the prognostic value in a cohort of 853 long-term follow-up patients under 71 years of MAI and other prognosticators for distant recurrence-free survival (RFS) and overall cancer-related survival (OS) of grade, MAI The median follow-up was 116 (8-187) months. Results: In all tumors <1 cm, all grades (n=84), and in tumors 1 to 3 cm and grades 1+2 (n=300), multivariate comparison revealed the prognostic superiority of MAI for RFS and OS in all tumors <2cm (Figure 1). Other features (grade, ER, diameter, age) did not enhance its prognostic value. In tumors 2-3cm diameter, ER has additional prognostic value but only if MAI<10. Discussion: In patients <71 years with node negative invasive breast cancer, the proliferation factor MAI ≥10 is the strongest prognosticator in identifying high-risk patients in all small, grade 1+2 tumors (survival 53-57%) which should be considered for adjuvant systemic therapy, even for tumors <1 cm in diameter. References: 1. Baak JP, van Diest PJ, Voorhorst FJ, et al: Prospective multicenter validation of the independent prognostic value of the mitotic activity index in lymph node-negative breast cancer patients younger than 55 years. J Clin Oncol 2005; 23(25):5993-6001. 2. Janssen EA, van Diest PJ, Soiland H, Gudlaugson E, Nysted A, Voorhorst FJ, Vermorken JB, Soreide JA, Baak JP. Success predictors of adjuvant chemotherapy in node-negative breast cancer patients under 55 years. Cell Oncol. 2006;28(5-6):295-303. 1068 Identi¿cation of IGFBP4 as a marker of tamoxifen failure in primary breast cancer. Hadad SM, Robertson KE, Baker L, Bray SE, Purdie CA, Jordan L, Vendrell JA, Cohen PA, Thompson AM. Ninewells Hospital and Medical School, Dundee, United Kingdom; Universite Lyon, Lyon, France Background: Insulin-like growth factor binding protein 4 (IGFBP4) is an insulin-like growth factor (IGF) inhibitor. It is down-regulated in tamoxifen-resistant cell lines and it may have a role in protecting cells from over stimulation by IGFs. Using cDNA microarray, RTQ-PCR and Immunohistochemistry (IHC) on tissue microarrays (TMA), ERα and IGFBP4 were among the genes down-regulated and were associated with clinical development of tamoxifen resistance. The aim of this study was to test this hypothesis on a larger scale of patients. Materials and Methods: IHC performed on TMAs of 117 tamoxifentreated breast cancer patients (104 ductal cancers) from a single recruiting centre of the National Cancer Research Institute (NCRI) Adjuvant Breast Cancer (ABC) clinical trial. Patients aged 34-76 years (mean 51). Antibodies to ERα, IGFBP4, BCL2, c-Fos, and c-MET were used and scored using quick-score method (scores 0-3). Patterns of protein expression were compared with previously tested Ki67, Her2 and clinical data including minimum 5 years follow up. Results: ERα and IGFBP4 found under-expressed in 43/115 (37.4%) and 38/102 (37.2%) of the cases respectively. As expected, 5-year disease-free survival was 68.9% for ER- patients compared to 91.7% for ER+ patients (Log Rank Test; p=0.001; DF=1). Under-expression of IGFBP4 (scores 0-1) was strongly associated with ER- tumours (Fisher’s exact test; p=0.000) and was associated with earlier death (Wilcoxon method; p=0.015; DF=1). We have also demonstrated a negative correlation between IGFBP4 and Ki67 (Fisher’s exact test; p=0.002), Her2 (Fisher’s exact test; p=0.026), axillary node status (Fisher’s exact test; p=0.038) and histological grade (Fisher’s exact test; p=0.002). Conclusion: IGFBP4 under-expression is a marker of poor prognosis and tamoxifen failure in patients receiving adjuvant tamoxifen. Abstracts – Poster Session I 1069 Genomic copy number alterations as predictive markers of systemic recurrence in breast cancer. Hwang K-T, Han W, Lee JW, Cho J, Ko E, Kim EK, Jung S-Y, Jeong E-M, Kang JJ, Yang S-J, Kim S-W, Noh D-Y. Seoul National University Boramae Hospital, Seoul, Republic of Korea; College of Medicine, Seoul National University, Seoul, Republic of Korea; Cancer Research Institute, College of Medicine, Seoul National University, Seoul, Republic of Korea; Macrogen, Inc., Seoul, Republic of Korea We tried to ¿nd novel predictive markers of systemic breast cancer recurrence by array comparative genomic hybridization (CGH). We performed array CGH with 4,044 human bacterial artificial chromosome clones to assess copy number changes in 31 pairs of clinicohistologically well matched recurred / nonrecurred fresh-frozen breast cancer tissues. We selected those clones that hit the conditions of frequency criteria (more than 10%), consecutive clones (more than 2 clones), chi square test (p<0.05), multiple comparison test (adjusted p<0.05), and Kaplan-Meier test (p<0.05). Eleven clones in gain and 3 clones in loss were selected to be the candidate clones. The most signi¿cant chromosomal alterations were found in the region of 5p15.33, 11q13.3, 15q26.3, 17q25.3, 18q23, 21q22.3 in gain, and 9p12, 11q24.1, 14q32.33 in loss. Especially, the loss of 14q32.33 region was associated with good disease free survival (p=.022) and overall survival (p=.019). We selected 4 candidate genes in gain and 6 candidate genes in loss. Our array CGH analysis could detect novel candidate clones and genes for predictive markers of systemic breast cancer recurrence. Table 1. Clinicopathological characteristics Recurrence Characteristics group (31) N (%) Age (range) 44 (32-67) T stage T1 4 (12.9) T2 24 (77.4) T3 2 (6.5) T4 1 (3.2) N stage N0 9 (32.2) N1 7 (19.4) N2 4 (12.9) N3 11 (35.5) Hormonal receptor Positive 19 (61.3) Negative 12 (38.7) c-erbB2 Positive 16 (51.6) Negative 15 (48.4) S65 relapse free survival after 2 years. sHER-2/neu was measured using a standardized ELISA (upper limit of normal 15ng/ml). As the baseline sHER-2/neu concentrations ranged from 3.8 ng/ml to 14.0 ng/ml, results were grouped in terciles. Data were analyzed using Kaplan-Meier and Cox Proportional Hazards survival analysis. Results: Material was available from 80 patients in leuprorelin arm and 53 patients in CMF arm. 65 of 133 patients had relapsed during the follow-up time of up 7 years after treatment. The median RFS was 62.9 mo. The RFS time depended on the concentrations of sHER-2/neu at baseline: RFS was signi¿cantly shorter in patients of the third tercile with sHER-2/neu levels >8.8 ng/ml than in patients of the ¿rst tercile with levels <7.2 ng/ml (p=0.0232). Five years after initial therapy, we found that 73% of patients in the ¿rst tercile group of baseline sHER2/neu had no relapse. In the second tercile, 63.3% of patients were relapse-free, while in the third tercile only 47.2% of patients had not suffered a relapse. Conclusions: Increased sHER-2/neu concentrations at the beginning of adjuvant therapy in the TABLE-Study have a prognostic importance for RFS. This observation was evaluated irrespective of the HER-2/neu tissue status and could be of clinically importance for adjuvant therapy with the monoclonal anti-HER-2/neu antibody trastuzumab or other anti-HER-2/neu targeted therapies. Non-recurrence group (31) N (%) 46 (31-65) 4 (12.9) 23 (74.2) 3 (9.6) 1 (3.2) 9 (32.2) 7 (19.4) 4 (12.9) 11 (35.5) 19 (61.3) 12 (38.7) 16 (51.6) 15 (48.4) Table 2. Candidate clones and chromosomal alteration regions Clone Cytoband X2 test FDR* DFS† 5262 5p15.33 0.011 0.003 0.0108 2312 5p15.33 0.022 0.006 0.0256 124 11q13.3 0.034 0.007 0.0141 2776 15q26.3 0.009 0.010 0.0300 2547 17q25.3 0.034 0.012 0.0402 5883 18q23 0.003 0.015 0.0101 5877 18q23 0.013 0.022 0.0178 5516 18q23 0.005 0.022 0.0091 641 21q22.3 0.006 0.032 0.0159 2806 21q22.3 0.005 0.034 0.0156 5856 21q22.3 0.020 0.043 0.0325 1000 11q24.1 0.010 0.011 0.020 710 14q32.33 0.021 0.024 0.022 4688 9p12 0.023 0.026 0.039 *False Discovery Rate; †Disease Free Survival 1070 Prognostic value of the shed antigen of HER-2/neu in premenopausal breast cancer patients in the TABLEstudy. Lueftner DI, Pechlivanis K, Geppert R, Possinger K. Charite Campus Mitte, Berlin, Germany Background: Increased serum HER-2/neu (sHER-2/neu) concentrations at the beginning of adjuvant breast cancer therapy have been shown to be of prognostic importance. Using the sera from the Takeda® Adjuvant Breast Cancer Study with Leuprorelin (TABLE), we tested for the prognostic value of sHER-2/neu. Material and Methods: A total of 133 premenopausal, node-positive, hormone-receptor positive patients received either 11.25 mg of leuprorelin s.c. every 3 months over 2 years or CMF chemotherapy for 6 cycles. Blood samples were collected at baseline and at 3, 6, 12, 18, 24 and 30 mo. The primary endpoint of the study was to determine the 1071 Down regulation of ()(03 is associated with unfavourable prognosis in sporadic breast cancer patients. Ramser J, Harbeck N, Sadr-Nabavi A, Naehrig J, Busch R, KiechleBahat M, Meindl A. Tech. University, Munich, Germany Background: EFEMP1 belongs to the ¿bulin gene family, a newly characterized family of extracellular matrix proteins that are localized at basement membranes, stroma and ECM ¿bres. Recently, EFEMP1 was described to be an angiogenesis antagonist and to act as a suppressor of formation and progression of human malignancies. Materials and Methods: Immunohistochemistry on tissue microarrays of 203 clinically well characterized primary breast carcinomas, was used to assess the potential clinical relevance of reduced EFEMP1 protein expression regarding patient outcome. Cox regression for multivariate survival modelling as well as univariate analyses were performed. Next to immune reactivity score for EFEMP1 expression, tumor grade, hormone receptor-, lymph node- and Her-2 status, tumor size, and type of adjuvant systemic therapy were included into analysis. Results: Analysis of the total cohort (n=203: 17 N0, 186 N+) revealed no signi¿cant impact of EFEMP1 expression on patient outcome. However, in the 186 node-positive cases, multivariate regression analysis revealed that next to tumor size and grade, EFEMP1 expression remained in the survival model as a relevant factor inÀuencing disease free and overall survival at borderline signi¿cance (DFS: p=0.14; OS: p=0.077). We further investigated the relevance of EFEMP1 expression in subgroups with homogeneous adjuvant systemic therapy. Signi¿cant correlations of low EFEMP1 expression with poor DFS (p=0.037) and OS (p=0.032) were only seen in those node-positive patients with adjuvant anthracycline-containing chemotherapy (n=31) but not in those treated by either CMF (n=49) (DFS: p=0.605; OS: p=0.934) or S66 Abstracts – Poster Session I adjuvant endocrine therapy (tamoxifen) alone (n=106) (DFS: p=0.735; OS: p=0.275). Median DFS in anthracycline-treated patients was > 10 years if tumors showed high EFEMP1 expression, compared to only 3.1 years with low EFEMP1 expression. Similarly, median OS was > 10 years when tumors had high EFEMP1 expression in contrast to 4.5 years associated with low EFEMP1 expression. Discussion: In a substantial cohort of 203 primary breast cancer cases we found that next to tumor size and grade, low EFEMP1 expression was associated with poor patient outcome in node-positive patients. Univariate analysis displayed signi¿cant correlations only in nodepositive patients with anthracycline-containing chemotherapy. In our retrospective cohort, patients with anthracycline-containing chemotherapy were also those patients with a clinically perceived high risk of relapse. Thus, at present we cannot distinguish a potential predictive impact of EFEMP1 expression with regard to response to anthracycline chemotherapy from a merely prognostic impact with regard to survival of high risk breast cancer patients. However, keeping the biological role of EFEMP1 in mind, it is not unreasonable to assume that its anti-angiogenic properties may enhance an anti-angiogenic chemotherapy effect of anthracyclines. 1072 Cell cycle proteins add independent prognostic information to Nottingham Prognostic Index (NPI). Loddo M, Kingsbury S, Sainsbury R. University College London, United Kingdom INTRODUCTION: Mitogenic growth signaling leads to passage through the restriction point, initiation of DNA replication and ultimately cell division. Proteins critical for progression through the G1-S and G2-M transitions include the DNA replication licensing factors (RLFs) which render chromosomal replication origins competent for DNA synthesis and mitotic kinases which orchestrate passage through mitosis. Both RLFs and mitotic kinases have been highlighted as targets for therapeutic intervention, with mitotic kinase inhibitors already in phase I/II trials. The aim of this study was to investigate the prognostic value of these cell cycle proteins in the management of breast cancer patients. MATERIALS AND METHODS: 182 cases of primary breast cancer were sectioned and immunohistochemically stained for ER, PR, HER2, the proliferation marker Ki67, and a selected set of RLFs and mitotic kinases. Antibodies were either commercially obtained or raised in house. Follow up data for all patients was available for recurrence (632 years; 3.8 per subject) and survival (684 years; 4.1 per subject) and the NPI was calculated (0.2x size + grade + nodes). RESULTS: NPI was signi¿cantly related to both recurrence (HR [95% CI]: 1.79 [1.46 to 2.20]; P<0.001) and survival (HR: 2.18 [1.63 to 2.93]; P<0.001) in this series. There was a signi¿cant association between the studied biomarkers and grade and NPI, but not between the markers and DNA ploidy, nodal status or size. HER2 and ploidy were not correlated, although increased staining of HER2 was associated with increasing NPI scores (P=0.014). Importantly, several of the biomarkers individually added additional information to NPI score (up to an additional HR of 3.31 [1.57 to 6.97]; P=0.002), allowing wide separation of the NPI survival curves. Inclusion of one signi¿cant biomarker is enough to add to the prognostic value of NPI; no further markers are necessary in adding further prognostic capability. DISCUSSION: The G1-S and G2-M transitions of the cell cycle act as relay stations for growth regulatory signaling pathways. NPI is one prognostic tool in common use but is relatively crude. A variety of additional parameters to render it more sensitive have been proposed, but few have stood the test of time. Several of the studied cell cycle biomarkers are strongly associated with recurrence and remain statistically signi¿cant after adjusting for NPI, so that they are predictive independent of NPI. This type of biomarker analysis could also be used as a predictive test for mitotic kinase inhibitors and may help decide which patients would bene¿t most from this new treatment option. 1073 The prognostic signi¿cance of androgen receptor expression in breast cancer. Peter M, Maraqa L, Horgan K, Speirs V, Shaaban A. University of Leeds, Leeds, W Yorks, United Kingdom; Leeds General In¿rmary, Leeds, W Yorks, United Kingdom Androgens have been hypothesised to inÀuence risk of breast cancer but the precise role of the androgen receptor (AR) as a prognostic factor in breast cancer is still unclear. The aim of this study was to determine the prognostic signi¿cance of AR in a large cohort of breast carcinomas with long term follow up. Four hundred and eight cases of invasive breast cancer were incorporated into tissue microarrays (TMAs) retrospectively selected from 1993-1997. Mean age at diagnosis was 58.4 (± 14.5) with an average follow-up period of 91.9 months (± 42.21). Two hundred and sixty patients had Tamoxifen therapy and 60 patients relapsed after endocrine treatment. TMA sections were stained with a speci¿c monoclonal antibody for AR and scored as continuous variables and using the Allred score. Results were then correlated with patient and histopathological variables including overall survival (OS), disease free survival (DFS), relapse on Tamoxifen, Nottingham Prognostic Index (NPI), estrogen receptor α (ERα) and progesterone receptor (PR). Nuclear expression of AR signi¿cantly correlated with age, grade, recurrence, distant metastasis, death, ERα and PR. AR expression, calculated using the Allred Score or as a continuous variable respectively correlated with better OS (p=0.0098, p=0.04), DFS (p=0.0096, p=0.0028) using cut off values of 3(Allred) and 10% positive cells (continuous). In the cohort of patients on Tamoxifen therapy, AR expression was additionally associated with a reduced risk of recurrence after endocrine therapy (Allred: p=0.0021, continuous: p=0.0017). This study suggests that AR expression may have a role in stratifying patients for treatment alongside the conventional prognostic variables of NPI, node positivity, ERα and PR. Measurement of AR in clinical practice could also be used to predict the likelihood of recurrence whilst on adjuvant endocrine therapy. 1074 Comparative analysis of uPA/PAI-1 in core biopsies versus surgical breast cancer samples. Vetter M, Lantzsch T, Abraha-Späth RS, Olenik C, Thomssen C, Dittmer J. Martin-Luther University, Halle/Saale, Germany; St. Elisabeth & St. Barbara Hospital, Halle/Saale, Germany; University Hospital Eppendorf, Hamburg, Germany; American Diagnostica GmbH, Pfungstadt, Germany Background: It has been estimated that 70% of the patients with breast cancer without axillary node involvement would survive 10 years after surgery without additional systemic adjuvant therapy. Nevertheless, all of these patients usually get chemotherapy. To avoid this unnecessary therapy, additional biological markers can be assessed. The invasion protein uPA (urokinase-type plasminogen activator) and its inhibitor PAI-1 are well established markers for this purpose. Originally, 300 mg of surgically removed tissue was used to determine the level of these proteins by ELISA. Nowadays, patients are often core needle biopsied which may remove much of the tumor tissue leaving little for uPA/PAI-1 measurement. In addition, these presurgical manipulations may change gene expression pattern in the remaining tissue. Hence, we explored the possibility to use core biopsies as a alternative source for uPA/PAI-1 measurement. Design: Fresh frozen material of 2-3 core needle biopsies and the corresponding surgically removed tumor material were collected, snap frozen on liquid nitrogen and analyzed for the uPA/PAI-1 status by ELISA. Only those areas in the remaining tumor were selected that were not close to the side of a core needle insertion. In three different sets, each with tumors from 30 patients, uPA/PAI-1 values in core biopsies were compared to values in remaining tumor. In the ¿rst set, core biopsies were taken ex vivo, in the second set, core biopsies were taken in vivo, but not examined by pathologist for tumor content and in a third set in vivo core biopsies were examined by a pathologist and only parts of the biopsies that were proven to contain tumor cells were used. Abstracts – Poster Session I Results and Conclusion: In all sets of experiments, uPA and PAI1 levels in core biopsies signi¿cantly correlated with those in the corresponding surgical samples. The calculated negative predictive values for uPA were as followed: 1.00 for set 1; 0.84 for set 2 and 0.85 for set 3. The appropriate npv for PAI-1 are 0.83, 0.74 und 0.77. Hence, core biopsies can be suggested as an alternative source to measure uPA/PAI-1 levels. 1075 Risk of dementia in older breast cancer survivors: a population-based cohort study of the effect of chemotherapy. Baxter NN, Durham SB, Phillips K-A, Virnig EA, Virnig BA. University of Toronto, Toronto, ON, Canada; University of Minnesota, Minneapolis, MN; Peter MacCallum Cancer Centre, Melbourne, Australia Background: An association between adjuvant chemotherapy for breast cancer and cognitive impairment in young women has been found in some studies; however these studies included few older women and the effect of chemotherapy on development of dementia in older survivors has not been evaluated. Methods: We conducted a retrospective cohort study using Surveillance, Epidemiology, and End Results cancer registry data linked to Medicare claims data to determine if there is a signi¿cant association between adjuvant chemotherapy and development of dementia in women over age 66 with breast cancer in the United States who did not have a previous dementia diagnosis. Women age 66 to 80 diagnosed with non-metastatic invasive breast cancer from 1991 through 1999 were included. We determined whether patients had undergone chemotherapy within 6 months of diagnosis using standard ICD-9 and CPT codes. We evaluated the effect of chemotherapy on the diagnosis of dementia, adjusting for potential confounders using a proportional hazards model. We strati¿ed our analysis for age at diagnosis (66-70, 71-75, 76-80) Results: 18931 women met our study selection criteria, 2823 were exposed to chemotherapy, 16108 were not. Women in the exposed group were younger than in the unexposed group (mean = 70 vs. 73 years) (p<0.001) justifying a strati¿ed analysis. Mean follow-up time for the entire cohort was 62.4 months. Dementia developed in 4.9% (936) women - 2.7% of exposed women (n=76) and 5.3% of unexposed women (n=860). Within the ¿rst 5 years of our study period, the cumulative incidence of dementia was as follows: of women age 66-70, 2.1% in the exposed group vs. 1.6% in the unexposed group; of women age 71-75, 2.6% vs. 4.4%; and of women age 76-80, 6.8% vs. 9.3% (Figure). In our proportional hazards model, after controlling for other factors, we did not ¿nd a signi¿cant association between receipt of chemotherapy and development of dementia. In fact, while not statistically signi¿cant, all models suggest that women receiving chemotherapy were less likely to develop dementia. Only an elevated comorbidity index was consistently associated with development of dementia across age strata. Conclusions: Receipt of chemotherapy in older women with breast cancer is not associated with an increased risk of diagnosis of dementia over time; however in this age group, women who undergo chemotherapy may be at lower baseline risk of cognitive impairment. S67 1076 Final results of the AGO breast cancer study group MAMMA-3 trial: ¿rst-line capecitabine + paclitaxel vs epirubicin + paclitaxel for high-risk metastatic breast cancer. Lück H-J, du Bois A, Schrader I, Huober J, Heilmann V, Fasching PA, Stähle A, Jackisch C, Marth C, Richter B, von Minckwitz G. HSK, Klinik für Gynäkologie und Gynäkologische Onkolgie, Wiesbaden, Germany; Henriettenstiftung, Frauenklinik, Hannover, Germany; Universitäts-Frauenklinik Tübingen, Tübingen, Germany; Universitäts-Frauenklinik and Poliklinik Ulm, Ulm, Germany; Universitätsklinikum Erlangen, Frauenklinik, Erlangen, Germany; St. Vincentius-Krankenhäuser, Frauenklinik, Karlsruhe, Germany; Klinik für Gynäkologie und Geburtshilfe Klinikum Offenbach, Offenbach, Germany; Universitätsklinik für Frauenheilkunde Innsbruck, Innsbruck, Austria; Elbland-Kliniken Meiβen-Radebeul, Standort Radebeul, Frauenklinik, Radebeul, Germany; Zentrum Frauenheilkunde und Geburtshilfe, Frankfurt, Germany Background: Anthracycline/taxane combinations are now standard adjuvant chemotherapy for early breast cancer, and are highly effective for high-risk metastatic breast cancer (MBC). Addition of capecitabine (X) to docetaxel signi¿cantly improves overall survival (OS) in MBC. Phase II studies of X + paclitaxel (XP) show high ef¿cacy and good tolerability. Therefore we performed a randomized, phase III trial of XP vs epirubicin + paclitaxel (EP). Methods: The primary objective was to demonstrate non-inferior progression-free survival (PFS) with XP vs EP. Secondary endpoints were OS, response rate (RR; RECIST), safety (NCI CTC v2.0) and QoL (EORTC C30 and BR23). Female MBC patients (pts) aged 18-75 years with no prior chemotherapy for MBC were randomized to six 21-day cycles of either XP (X 1,000 mg/m2 bid, d1-14; P 175 mg/m2 d1) or EP (E 60 mg/m2; P 175 mg/m2, both on d1). Results: Accrual of 340 pts (170 per arm) completed in April 2005. Median age was 55 years (XP) and 56 years (EP). Most patients were anthracycline-naive (81% and 80%, respectively). Visceral metastases were present in 56% and 47%, respectively. In both arms, a median of 6 cycles were delivered. Median doses delivered per cycle were: P 175 mg/m2 (both arms), E 60 mg/m2, X 926 mg/m2 bid. After 9.9 months’ median follow-up, PFS and OS were not signi¿cantly different (Table). The most frequent grade 3/4 toxicities were neutropenia (XP: 38% of pts; EP: 52%) and leukopenia (XP: 12%; EP: 41%). Grade 3 hand-foot syndrome occurred in 12% of XP pts (absent with EP) and grade 3/4 diarrhea in 5% vs <1%, respectively. Rates of grade 3/4 cardiotoxicity were 1% with XP vs 2% with EP. Conclusions: The primary endpoint, to show that XP is non-inferior to EP, was met. XP is well tolerated compared with other nonanthracycline-containing combination regimens, and is a valid and active ¿rst-line treatment option for patients with high-risk MBC. Final ef¿cacy results (due July 2007) and QoL data will be presented. Median PFS, months (95% CI) Median OS, months (95% CI) Overall RR Complete response Partial response Stable disease XP 12.0 (10.2-13.9) 25.6 (20.1-28.0) 52% 7% 45% 35% EP 11.1 (7.7-14.4) 24.0 (18.0-30.1) 51% 8% 43% 37% S68 Abstracts – Poster Session I 1077 Combined trastuzumab (HER)/docetaxel (TAX) versus sequential trastuzumab followed by docetaxel at progression as ¿rst line chemotherapy for Her2-positive metastatic breast cancer: preliminary results (multicenter BOOGstudy; 2002-02). Hamberg P, Bontenbal M, Vernhout RM, Bos MM, Braun HJ, Erdkamp F, Stouthard JML, van Deijk GA, Schmitz PIM, Seynaeve C, Klijn JGM. Erasmus University Medical Center, Daniel den Hoed Cancer Center, Rotterdam, Netherlands; Reinier de Graaf Hospital, Delft, Netherlands; Vlietland Hospital, Vlaardingen, Netherlands; Maasland Hospital, Sittard, Netherlands; Haga Hospital, Den Haag, Netherlands; Medical Center Rijnmond-Zuid, Rotterdam, Netherlands; Erasmus University Medical Center, Rotterdam, Netherlands Background Trastuzumab (HER) in combination with chemotherapy (CT) is superior over CT alone in Her2 positive metastatic breast cancer (MBC). At this moment, it is not yet clear what the outcome is of sequential treatment with HER followed by CT. The HERTAX study is a randomized multicenter phase II study designed to determine progression free survival (PFS) of the combination of HER and docetaxel (TAX) (arm A) versus sequential therapy of HER followed by TAX at progression (arm B). Methods Patients with HER2-positive MBC, eligible for ¿rst line CT, were randomized in a 1:1 fashion. Adjuvant non-taxane containing CT was allowed, previous HER therapy not. Treatment A consisted of: weekly HER (2 mg/kg, after a loading dose of 4 mg/kg), combined with TAX 100 mg/m2 every three weeks until progression. Patients in arm B were treated with HER monotherapy at the same schedule, and upon progression with TAX (100mg/m2, q 3 weeks). Current analysis is performed on the time from date of ¿rst administration until date of ¿rst progression, by using the log-rank test. Results A total of 98 patients were randomized, ef¿cacy data are currently available on 89 patients. Patient characteristics are: median age 51 years (range 32-74 years), prior adjuvant CT administered in 58%, and adjuvant endocrine treatment in 30% without major differences between treatment arms. The median PFS signi¿cantly differed between the combination regimen and monotherapy HER, being 9.1 months and 4.0 months, respectively (p = 0.004). Data regarding the complete sequential treatment are in the process of analysis. Two deaths occurred during study treatment both in arm A, caused by pneumonia and neutropenic fever/diarrhea. In arm A, 25 serious adverse events (SAE’s) occurred (including the two deaths), mainly consisting of neutropenic fever (n=14) and fever/infection without neutropenia (n=7). 4 SAE’s were noticed in arm B, being allergic reactions (n=2), pulmonary embolism (n=1) and syncope (n=1). No statistical difference in cardiac toxicity (measured by a LVEF decline below 50%) was observed between the treatment arms (13% and 7% in arm A and B, respectively; p=0.34). Conclusion Combination therapy with HER/TAX results in a signi¿cantly longer PFS as compared to HER monotherapy, at the cost of more severe toxicity. Whether the shorter PFS during monotherapy HER will extend beyond the PFS on combined HER/TAX after complete sequential therapy (accompanied by less toxicity) is being analyzed. These data will be available at the meeting. 1078 Phase III study of gemcitabine plus docetaxel versus capecitabine plus docetaxel for anthracycline-pretreated metastatic breast cancer patients: survival results. Chan S, Romieu G, Huober J, Tubiana-Hulin M, Schneeweiss A, Lluch A, Llombart A, du Bois A, Carrasco E, Thareau Vaury A, Fumoleau P. Nottingham City Hospital, Nottingham, United Kingdom; CRLC Val d’Aurelle, Montpellier Cedex 5, France; University of Tuebingen, Tuebingen, Germany; Centre Rene Huguenin, Saint Cloud, France; University of Heidelberg, Heidelberg, Germany; Hospital Clinico de Valencia, Valencia, Spain; Hospital Arnau de Villanova, Lerida, Spain; Dr. Horst-Schmidt-Klinik, Wiesbaden, Germany; Eli Lilly Spain, Madrid, Spain; Eli Lilly France, Suresnes Cedex, France; Centre Georges-Francois Leclerc, Dijon, France Background: Patients (Pts) pre-treated with anthracyclines frequently receive combination chemotherapy with a taxane and an antimetabolite like gemcitabine or capecitabine in metastatic setting. This phase III study directly compared gemcitabine plus docetaxel (GD) combination with capecitabine plus docetaxel (CD), in pts with metastatic breast cancer (MBC). Primary objective was progression-free survival (PFS), and secondary objectives included overall response rate (ORR), time to treatment failure (TtTF), overall survival (OS), and toxicity assessments. In a previous analysis GD demonstrated similar ef¿cacy to CD but with a better non-hematological toxicity pro¿le [Chan et al, ASCO-2005]. This report presents the ¿nal OS analysis Patients and Methods: Pts with histologically/cytologically con¿rmed MBC who had received anthracycline-based regimen either in neoadjuvant, adjuvant, or ¿rstline metastatic setting, were randomized to GD (G=1000 mg/m2 d1,8; D=75 mg/m2 d1) or CD (C=2500 mg/m2 d1-14; D=75 mg/m2 d1) q21 days. Results: Characteristics of the 305 included patients (GD=153; CD= 152) were previously reported. A median of 6 cycles was delivered on both arms. CTC grade 3/4 hematologic toxicity was similar in both arms, except for grade 3/4 thrombocytopenia GD=11%; CD=3%; p=0.014). Nonhematologic toxicities were low in both arms, but signi¿cantly different grade 3/4 toxicities were more pronounced in CD arm; diarrhea (GD=8%; CD=18%; p=0.0088), mucositis (GD=4%; CD=15%; p=0.0008), and hand-foot syndrome (GD=0%; CD=26%; p<0.0001). 13% of pts stopped therapy due to adverse event on GD vs 30% on CD. Best overall response rates in both arms were 32% (p=0.93). Median PFS (with 1% of patients censored in GD and 7% in CD) was 8.05 months (95% CI 6.60-8.71) on GD arm, and 7.98 (95% CI 6.93-8.77) on CD arm (log-rank p=0.121). Of notice when interpreting this data, 11% in GD arm vs 26% in CD arm received additional chemotherapy before progression. With a median follow-up of 19.2 months, and 23% of patients censored, the median overall survival was 19.29 months (95% CI 15.57-23.59) on GD arm, and 21. 45 (95% CI 17.12-24.94) on CD arm (log-rank p=0.983). Conclusion: These data suggest that the two regimens are also comparable in OS; however a more favorable toxicity pro¿le on GD arm may be a determining factor in selecting a better treatment option. Exploratory sub-group ef¿cacy analysis results will be presented at the meeting. 1079 Analysis of chemotherapy-induced amenorrhea by three different chemotherapy regimens in premenopausal women with early breast cancer. Han HS, Lee KS, Kim SY, Ro J. National Cancer Center, Goyang-si, Korea Background: Although the incidence or implication of chemotherapyinduced amenorrhea (CIA) have been studied more recently, the data on CIA are inadequate with newer regimens. The objective of this analysis was to evaluate CIA in premenopausal women with early breast cancer on three different preoperative or adjuvant chemotherapy regimens. Methods: We conducted a retrospective cohort study on a phase III trial at the National Cancer Center, Korea involving node positive Abstracts – Poster Session I S69 breast cancer patients who were randomized to receive preoperative doxorubicin⁄cyclophosphamide (AC) versus docetaxel/capecitabine (TX), then postoperatively crossed over to the other therapy (n = 96). For the comparison, we reviewed the medical records of premenopausal early breast cancer patients receiving adjuvant AC followed by paclitaxel (T) (n = 26) or 5-Àuorouracil/doxorubicin/cyclophosphamide (FAC) (n = 96). Results: Between 3/2002 and 7/2005, total 218 patients who took one of above three regimens were analyzed for the data. There were 115 patients ≥ 40 years and 103 patients <40 years with a median age of 41 years (range, 21 to 49) and a median follow-up of 40 months (range, 8 to 60). The distribution of age, body mass index, use of tamoxifen were well balanced in each chemotherapy regimen. CIA rates were 97%, 96% and 91% by AC/TX, AC followed by T and FAC, respectively at the 6th month (p=0.169) and 94%, 89% and 81% by AC/TX, AC followed by T and FAC, respectively at the 12th month (p=0.035), which decreased to 70%, 65% and 72% by AC/TX, AC followed by T and FAC, respectively by the 24th month (p=0.789). More than 60% of patients were still amenorrheic at the end of 3 years. Age (p<0.0001), tamoxifen (p=0.011) and chemotherapy regimen (p=0.007) were signi¿cant factors for CIA by multivariate analysis after the initial ¿rst year. Age and tamoxifen remained signi¿cant variables for CIA after 2 years. Discussion: The type of chemotherapeutic regimen is a signi¿cant factor affecting CIA rates by the end of ¿rst year, which however, becomes insigni¿cant after the second year. More than half of patients continue to be amenorrheic even after 3-4 years by these chemotherapeutic regimens. The persistent signi¿cant predictors of CIA are age and tamoxifen. Supported by NCC Grant 0610240-2. 1080 A descriptive study of pharmacokinetic alterations of epirubicin as a function of body size. Madarnas Y, Clemons M, Walker S, McLean H, Nakatsu K, Sawka C. Queen’s University; ; University of Toronto; Cancer Centre of Southeastern Ontario; Toronto-Sunnybrook Regional Cancer Centre; Princess Margaret Hospital Background: Obesity (Ob) prevalent among women with breast cancer (BC) and is known to adversely affect BC outcomes. We postulate that Ob contributes to suboptimal chemotherapy (CT) dosing as a result of associated physiologic changes affecting the pharmacokinetics (PK) and pharmacodynamics (PD) of antineoplastic drugs. Alterations in the disposition of many drugs in Ob have been described, but few publications speci¿cally address PK alterations of antineoplastic agents in the setting of Ob. Methods: This is a descriptive PK study in women with BC spanning a broad range of body size who received BSA-dosed epirubicin (E)-based CT at two institutions. A total of 56 women were enrolled providing 8 samples each (pre/post infusion, at 1, 2, 4, 24, 48 and 72 hrs post E infusion). Serum concentrations of E were determined and for each patient and standard PK parameters were derived. Body mass index (BMI) and body surface area (BSA) were derived from recorded height and weight. The relationship between the different pharmacokinetic parameters and body size was then examined. Results: Median BMI was 25.15kg/m2 and median BSA was 1.72m2. We observed substantial interpatient variability in E concentration at each timepoint. Most women had no measurable E by 24hrs post infusion, and all but one by 48hrs. Observed E half life (t1/2) was signi¿cantly shorter than that reported in the literature, suggesting extremely rapid drug elimination. Volume of distribution (Vd) could not be accurately estimated, but was very large. Body size displayed a signi¿cant positive linear correlation with area under the concentration vs time curve (AUC), which was attenuated when E concentration at 1hr was omitted. Graphic relationship of AUC with BMI and BSA is displayed below. Further analyses with other modeling techniques are underway to better understand our data and will be presented. Conclusion: In this group of women, E PK parameters displayed signi¿cant interpatient variability despite E being dosed on the basis of BSA; observed t1/2 and Vd differed signi¿cantly from what is reported in the literature; and AUC increased with increasing body size. 1081 A multicenter, randomized, double-blind, parallelgroup phase II study of ge¿tinib (IRESSA) or placebo in combination with docetaxel, as ¿rst-line treatment in patients with metastatic breast cancer. Tubiana-Hulin M, Spielmann M, Dieras V, Fumoleau P, Delaloge S, Mefti F, Girre V. Centre Rene Huguenin, Saint Cloud, France; Institut Gustave Roussy, Villejuif, France; Institut Curie, Paris, France; Centre G.F. Leclerc, Dijon, France Background: This double-blind, placebo-controlled, parallel-group, Phase II study (1839IL/0148) evaluated docetaxel alone or combined with ge¿tinib (IRESSA) in patients with untreated metastatic breast cancer. Methods: Women (18-70 years) eligible for ¿rst-line chemotherapy were randomized 2:1 to receive continuous ge¿tinib 250 mg or placebo orally once daily, plus docetaxel 100 mg/m2 iv every 21 days for up to 8 cycles. Maintenance ge¿tinib/placebo therapy was allowed, concurrent with hormonal therapy if indicated. Treatment was continued until disease progression, unacceptable toxicity or withdrawal of consent. Primary endpoint was objective response rate (ORR, RECIST criteria). Secondary endpoints were time to progression (TTP), response duration, overall survival (OS), time-to-treatment failure (TTF), and pharmacokinetic evaluations. Adverse events (AEs) were assessed by CTC version 3.0. Results: 76 patients (median age 56 years [30-70]; PS 0-2; prior adjuvant anthracycline n=75) received combination therapy (n=50) or docetaxel monotherapy (n=26). At median time on trial of 172.5 days, ORR was 46.0% (95% CI 31.8, 60.7) and 53.8% (95% CI 33.4, 73.4), median TTP was 215 (95% CI 129, 263) and 328 (95% CI 238, 363) days, response duration was 188 (95% CI 147, 364) and 213 (95% CI 185, 297) days, and TTF was 129 (95% CI 84-188) and 238 (95% CI 180-270) days, for combination and monotherapy, respectively. Median OS was not reached for combination therapy. Addition of ge¿tinib to docetaxel had no effect on steady state exposure of docetaxel. No statistically signi¿cant difference was observed in ge¿tinib responders in correlation with hormonal status. Grade 3/4 AEs were reported by 88.0% of combination and 96.2% of monotherapy patients. The incidence of the following AEs tended to be higher in the combination arm than in the monotherapy arm: febrile neutropenia (42.0% and 26.9%), diarrhea (66.0% and 38.5%), nausea (54.0% and 34.6%), S70 Abstracts – Poster Session I vomiting (26.0% and 19.2%), stomatitis (24.0% and 11.5%), rash (32.0% and 15.4%) and anorexia (18.0% and 3.8%). Conclusions: In this parallel-group study in metastatic breast cancer, there appeared to be no bene¿t of adding ge¿tinib to docetaxel. IRESSA is a trademark of the AstraZeneca group of companies. 1082 VinÀunine in combination with trastuzumab: an active combination in the treatment of HER2 positive metastatic breast cancer. Paridaens R, Wildiers H, Dalenc F, Rixe O, Roche H, Cadic V, Delgado F-M. UZ Gasthuisberg, Leuven, Belgium; Institut Claudius Regaud, Toulouse, France; Hopital Pitie-Salpetriere, Paris, France; Institut de Recherche Pierre Fabre, Boulogne-Billancourt, France Background VinÀunine (VFL, JAVLOR®) is a microtubule inhibitor of the vinca alkaloid class with high activity in several tumour types especially in second line treatment of metastatic breast cancer (MBC). Overexpression of HER2 is observed in 20-25% of all breast cancers and is associated with a poor prognosis. Anti-HER2 therapy with trastuzumab (T) signi¿cantly increases survival in HER2 positive MBC. Both compounds have single agent activity in MBC, therefore a combination regimen study was warranted. Methods This phase I was designed to determine the recommended dose (RD) of VFL in combination with T for treatment of ¿rst or second line MBC patients (pts). Subsequently safety pro¿le (NCI CTC version 2.0) of the combination together with its antitumour activity were explored. Results Thirty pts, median age 55 [33-74] years, WHO performance status 0/1: 18/12 pts, respectively were given VFL 280 mg/m² (9 pts) or 320 mg/m² (21 pts) day 1 every 3 weeks (w) in combination with T (loading dose 4 mg/kg and subsequently 2 mg/kg/w). Six pts were chemonaive and ¿ve pts received this combination in second line for advanced metastatic disease. In the ¿rst step of the study 6 pts were given VFL 280 mg/m² and none of them experienced dose-limiting toxicity. The RD was then established at the second VFL dose explored of 320 mg/m² in the following six pts. Nine pts were given 280 mg/m² while 21 received 320 mg/m². In both groups, the median number of VFL administrations per pt was 8. All pts were evaluable for safety. Grades (G) 3 and 4 haematological toxicities were with VFL 280 and 320 mg/m², respectively: anaemia 0 and 1 pt; neutropenia 4/18 pts, febrile neutropenia 0/1 pt. Among the 9 pts treated at 280 mg/m², for a total of 83 cycles, one single G 3 non-haematological adverse event (AE), sensory neuropathy, was recorded in one pt. Among the 21 pts who received 320 mg/m², for a total of 204 cycles, G 3 AE (no G 4 recorded) were: constipation, fatigue, myalgia in 5 pts; infection with neutropenia, abdominal pain in 2 pts; arthralgia, hyponatraemia, ileus in 1 pt. No signi¿cant cardiac events were observed (based on MUGA scans done on a regular basis). An external radiologist reviewed all ¿les and response rates were 66.7% [95% con¿dence interval (CI): 29.9-92.5] and 76.2% [95% CI: 52.891.8] in pts receiving VFL at 280 mg/m² and 320 mg/m² respectively. As of today, median progression free survival and duration of response are not mature. Conclusions In MBC, the combination of vinÀunine/trastuzumab resulted in a very encouraging response rate with an acceptable safety pro¿le. Updated results of this ongoing trial will be presented at the meeting. A phase III study comparing VFL + T versus paclitaxel + T has been initiated. 1083 A phase III study on the ef¿cacy and safety of docetaxel, every three weeks or as a weekly regimen in patients with metastatic breast cancer. Willemse PH, Munck L, Creemers GJ, Graaf H, Smit W, Erjavec Z, Stouthard JM, Deijk G, Bochove A, Vader W, Westermann AM. UMC, Groningen, Groningen, Netherlands; Comprehensive Cancer Centre North-Netherlands, Groningen, Groningen, Netherlands; Catharina Ziekenhuis, Eindhoven, Brabant, Netherlands; MCL Zuid, Leeuwarden, Friesland, Netherlands; Medisch Spectrum Twente, Enschede, Overijssel, Netherlands; Delfzigt Ziekenhuis, Delfzijl, Groningen, Netherlands; MCR-Zuid, Rotterdam, Zuid-Holland, Netherlands; HAGA Ziekenhuis-Rode Kruis, Den Haag, Zuid-Holland, Netherlands; ZaansMC, Zaandam, Noord-Holland, Netherlands; Sano¿-Aventis, Gouda, Zuid-Holland, Netherlands; AMC, Amsterdam, Noord-Holland, Netherlands Introduction. The standard schedule of docetaxel is effective but weekly administration of docetaxel might have a favourable safety pro¿le. This randomised phase III study compared two schedules of docetaxel for anthracycline-resistant metastatic breast cancer (MBC) for safety pro¿le, ef¿cacy and quality of life. Methods 162 patients with MBC previously treated with anthracyclins were randomised to receive either docetaxel 36 mg/m2 weekly for 6 weeks followed by 2 weeks rest (arm A; 3 cycles) or docetaxel 100 mg/m2 every three weeks (arm B 6 cycles). Primary end point: safety pro¿le. Secondary end points: time to progression (TTP), response rate (RR), overall survival (OS) and Quality of Life (QoL) Results. 81/79 patients received treatment: 81 in arm A and 79 in arm B. In this analysis median follow-up was 15 months. 72/70 patients were evaluable for safety and QoL, whereas 51/63 patients for response. More grade 3/4 hematological toxicities were reported for arm B versus A: 3 % vs. 5% cycles with neutropenia, and 1 vs. 11 admissions for febrile neutropenia (FN p<.05). Grade 3/4 non- hematological toxicities were different in cycles of arm A vs. arm B: 2% vs. 5% for gastro-intestinal toxicities, 15% vs 10% for fatigue, 8% vs. 0% for Àuid retention (p<.05), 1% vs. 4% for peripheral sensory neuropathy, 0% vs. 5% for stomatits and 12% vs. 2% for skin- and/or nailtoxicity (p<.05). Treatment was discontinued due to toxicity in 26 (27%) vs. 12 (13%) patients and completed in 15% vs. 36% of patients treated in arm A and B respectively (p<.05). QoL scores were not different for patients in arm A and B at treatment start or after 12 or 24 weeks. There were no differences between arm A and B in RR, with PD in 63% vs 51% and median TTP 21.2 vs 21.9 wks. Clinical bene¿t was apparent in 37% vs. 49% of patients while the median duration of 32 and 30 wks for patients in arm A and B resp. Conclusion: Although more pts had PD on Arm A, the ef¿cacy of both docetaxel regimens was comparable in terms of clinical bene¿t, TTP and OS. Against expectations there was more fatigue, skin + nail toxicity and Àuid retention in Arm A, but more FN in arm B. Patients in either arm had comparable QoL scores. 1084 Benchmarking quality oncology care in the community setting. Schwartzberg LS, Tauer K, Blakely J, Johnson R, Reed J, Somer B, Wheeler B, Walker MS, Stepanski EJ, Fortner BV. The West Clinic, Memphis, TN; Accelerated Community Oncology Research Network, Memphis, TN Background: The cancer death rate has been falling since 1991 in part due to wider access to quality care. Continuing this trend will require provision of state-of-the-art treatment regimens, and the establishment of benchmarks of quality cancer care. This preliminary report presents ¿ndings from a pilot project for benchmarking standards of oncology care among patients (pts) being treated in the community setting. Method: Retrospective review of electronic or paper medical records assessed demographic characteristics, and quality indicators selected for concordance with previous research. These included general indicators, and guideline-speci¿c use of supportive care, treatment and surveillance. Eligible pts had stage I – IIIC breast cancer (BrCa), had ≥ one cycle of chemotherapy between July 2004 and 2005, and had ≥ 12 weeks of documented follow-up after ¿rst treatment visit. Results: The sample comprised 102 BrCa pts treated by 10 medical oncologists across four practice sites. The sample was 54% Caucasian, 35% African American, and 11% other ethnicity. The mean age was 54.6 (range: 34 - 81), and 67% had private insurance. The Table shows the percentage compliance with key quality indicators. Abstracts – Poster Session I Quality indicator General --Pathology report present in chart --Stage of disease documented in chart Treatment Speci¿c --First-line chemotherapy regimen identi¿ed --Chemotherapy education provided before treatment --Anti-emetics used with chemotherapy --Pain assessed at each visit --Nausea and vomiting assessed at each visit --Fatigue assessed at each visit --Documentation of hospitalization --Guideline-speci¿c use of chemotherapy induced anemia treatment Breast Cancer Speci¿c --Taxane-based therapy for node+ disease --Yearly mammogram after treatment --Hormone therapy for hormone receptor positive tumors --Radiation therapy post surgery for T3-T4 or N2-N3 disease Mean Compliance Compliance 99.0% 95.1% 100.0% 92.2% 100.0% 86.8% 91.2% 86.3% 100.0% 83.3% 95.8% 74.5% 98.2% 94.4% 92.6% Compliance across 14 areas of care averaged 92.6%, and was < 80% for only one survey item—documentation of yearly mammogram following treatment. There were no signi¿cant differences in the rate of compliance across pt age, ethnicity, or insurance status. Documentation of follow-up mammogram varied by treatment location (p = .004). Assessment of pain and fatigue, and chemotherapy education tended to vary by treatment location (p < .10). Conclusions: Establishing meaningful benchmarks of quality care is feasible in the community oncology setting. Preliminary evidence suggests compliance is intrinsically high. Benchmarks should encompass disease site-speci¿c aspects of cancer care, as well as patient-oriented processes related to education and symptom assessment. Ongoing research will include documentation of the administrative burden associated with routine assessment of the quality of care, and inter-rater reliability for these measures. 1085 Age and prognosis – how did adjuvant therapies inÀuence the real prognosis? Morishita M, Thomas G, Leonard R. South West Wales Cancer Institute, Swansea, United Kingdom; Velindre Hospital, Cardiff, United Kingdom; Imperial College School of Medicine, London, United Kingdom Background: Adjuvant chemotherapies for breast cancer have been regarded as major contributor to improve the prognosis. This effect was examined by comparing different age groups. Material and methods: We reviewed 918 breast cancer patients operated during 1996-2000 and followed their outcome against prognosis as determined by the Nottingham prognostic index (NPI). Categorization of NPI score, expected good prognosis (G=NPI ≤3.4), moderate prognosis (M=NPI 3.41-5.4), poor prognosis (P=NPI >5.4). Age groups are divided as 3544 years old (yo) (n=93), 45-54yo (n=277), 55-64yo (n=251), 65-74yo (n=196) and over 75yo (n=101), prognostic groups were distributed as G 31%, M 50%, P 19% in 35-44yo group, G 36%, M 49%, P 15% in 45-54yo group, G 51%, M 30%, P 19% in 55-64yo group, G 38%, M 46%, P 16% in 65-74yo group and G 32%,M 48%, P 20% in over 75yo group. Results: Median follow up time was 5.5 years. Most of patients had received adjuvant hormonal therapy in all age groups (94.6-96.4%) regardless ER status. Neo-adjuvant and/or adjuvant chemotherapy was used in 81% in 35-44yo group, 66% in 45-54yo group, 34% in 55-64yo group, 16% in 65-74yo group and 1% in over 75yo group patients (regimens consisted of CMF(84%), Anthracycline based (11%) and others (5%). Percentages of death from breast cancer were similarly seen in each age group, 22%, 17%, 16%, 20% and 21%. Most of those cases (>60%) were seen in poor prognostic groups (NPI>5.4) in older age groups (>55yo) while 15% in younger age group (35-44yo). Discussion: Neo-/adjuvant chemotherapies were used in most of cases in younger age group (>80% in 35-44yo patients), this may contributed to lower mortality (17%) in high risk group (NPI>5.4) in those young patients, however, 33% of patients in moderate risk group (NPI 3.415.4) died. Many cases, 66% in 45-54yo and 34% in 55-64yo groups received neo-/adjuvant chemotherapy, the actual mortality was not signi¿cantly different with those of older groups (> 65yo), majority of those did not have adjuvant chemotherapy (only 16% in 65-74yo and 1% in over 75yo group). However, elderly patients among high risk group (NPI>5.4) may have had bene¿t from adjuvant chemotherapy. S71 The lack of overall differences in survival between the different age groups may be due to a segregation of better biology in the older age groups (eg. Grade 3 tumor rate was 46% in 35-44yo, 35% in 45-54yo, 27% in 55-64yo, 28% in 65-74yo and 26% in over 75yo group). Further study is necessary to improve prognosis. Number of patients (%) and mortality [%] in different age groups NPI 35-44yo 45-54yo 55-64yo 65-74yo 3.4 29 (31) [7] 99 (36) [0] 129 (51) [2] 74 (38) [1] 3.41-5.4 46 (50) [33] 135 (49) [18] 75 (30) [13] 90 (46) [18] >5.4 18 (19) [17] 43 (16) [56] 48 (19) [56] 32 (16) [69] >75yo 32 (32) [1] 48 (48) [15] 21 (20) [62] 1086 Dexamethasone, metoclopropamide and omperazole combination is simple, safe and effective for delayed nausea and vomiting control in adjuvant chemotheray for early breast cancer. Sanchetee SC. Sanchetee Hospital and Cancer Insitute, Jodhpur, Rajasthan, India BACKGROUND: Delayed nausea and vomitting in chemotherapy are the most frequently of side effect. Our study aimed to determine the effectiveness of Dexa+omeprazol versus Dexa+omeprazol+met oclopramide in the prophylaxis of dealyed emesis after emetogenic chemotheray. METHODS: Patients after treated with FAC regimen-adjuvant chemotherapy for early stage breast cancer, receive dexamethasone 4mg oral, twice time daily and omeprazol 20mg oral, twice time daily, all for ¿ve days (Daxo) or dexamethoasone 4mg oral, twice time daily, omeprazol 20mg oral, twice time daily and metoclopramide 20mg oral, thrice time daily, all for ¿ve days (DexoPrim). Patient diary with nausea and vomiting module and toxicity criteria were used to monitor and evaluate patient outcomes. RESULTS: From Jan 2004 to Dec 2005, 122 (mean=45,7years) outpatients were randomized with 60 Dexo and 62 DexoPrim con¿rmed eligible. Patient characteristics were similar between the two groups. No drug related serious adverse evetns were reported. During ¿rst cycle fo chemotherapy, DexoPrim was complete protection against vomiting better Dexo(78vs.52%;p=0.05). For the entire study period, there was better DexoPrim (69vs, 48%;p=0.02), lower average nausea score (0.02 vs. 0.39, p=0.04) and no cases must entry hospital for recuing anti eetic. Global QoL declined in both groups during chemotherapy but DexoPrim was less than Dexo (p=0.03). Appetite was the same in both groups. There were no signi¿cant differences in toxicity. CONCLUSION: The use of combination DexoPrim oral daily for ¿ve day after chemotherapy is simple, cheap cost, safe, and effective in preventing vomiting, reducing nausea and preserving QoL. 1087 N0332 phase II trial of weekly irinotecan and docetaxel in refractory metastatic breast cancer: a North Central Cancer Treatment Group trial. Tan WW, Hillman D, Salim M, Northfelt DW, Anderseon DM, Stella PJ, Niedringhaus R, Bernath AM, Gamini SS, Frances P, Perez PA. Mayo Clinic, Jacksonville, FL; Mayo Clinic, Rochester, MN; Allan Blair Cancer Center, Saskatchewan, Canada; Mayo Clinic Scottsdale, Scottsdale, AZ; Abbott Northwestern Hospital, Minneapolis, MN; Michigan Cancer Research Consortium, Ann Arbor, MI; Duluth CCOP, Duluth, MN; Geisinger Clinic & Medical Center, Danville, PA; Missouri Valley Cancer Consortium, Omaha, NE Background: Capecitabine is approved to treat patients with refractory metastatic breast cancer (MBC) after anthracycline and taxane treatment, with response rates of 20-25% and median survival of less than a year. There is a need to test other approaches to improve tumor response and potentially survival in this population. Weekly irinotecan had been found to lead to a response rate of 23% in a similar patient population treated in a previous NCCTG trial (Perez EA,et al. JCO 2004). Several studies in other tumor types have documented the ef¿cacy of irinotecan and docetaxel in the clinical setting ( breast, lung, esophageal, gastric) with partial non-cross resistance and tolerability. Patients & Methods: A single stage phase II study with an interim analysis of irinotecan and docetaxel was conducted with these objectives: tumor response, toxicity, time to progression and overall survival. Regimen: docetaxel S72 Abstracts – Poster Session I 25 mg/m2 and irinotecan 70 mg/m2 days 1 and 8 of each of 3- week cycle. Results: 70 patients were enrolled from May 2004-October 2006; 64 patients were evaluable. Number of prior metastatic regimens:0 in 14 patients, 1 in 34 patients and 2 in 16 patients.A median of 4 cycles were administered. Overall 16 patients (25%) (95% CI:15-31%) had a tumor response ( 1 CR and 15 PR. Additionally, four patients had stable disease for greater than 6 months, for a clinical bene¿t rate of 31%. Median duration of tumor response was 5.6 months (95% CI:2.8-16.4 months). Median follow up of 10.6 months range (1.7-30.4 months). Median progression-free survival was 5.1 months (95% CI:3.1-7.2 months). The 6 months overall survival was 84% (95% CI:76-94%) and 6-month progression free survival was 44% (95% CI: 33-59%). The median dose level administered was 25 mg/m2 for docetaxel and 70 mg/m2 for irinotecan for cycles 1-9. The range of cycles given was 0-22.The most common severe (grade 3/4) adverse events were fatigue 14 (22%), neutropenia 13 (20%), diarrhea 9 (14%), dyspnea 6(9%) and nausea 6 (9%). 61% (39/64) of patients experienced a grade 3+ adverse event (AE) and 17% experienced a grade 4+ AE.Conclusion: Weekly irinotecan and docetaxel combination is active in heavily pretreated MBC. The combination under study showed fairly similar ¿ndings to historical data of other chemotherapy regimens, and is an option to consider for patient treatment. 1088 Reduced incidence of febrile neutropenia and related complications in elderly breast cancer patients receiving chemotherapy with peg¿lgrastim primary prophylaxis versus current practice neutropenia management – results from an integrated analysis. Aapro M, Schwenkglenks M, Lyman G, Lopez Pousa A, Easton V, Skacel T, Bacon P, Von Minckwitz G. Clinique de Genolier, Genolier, Switzerland; University of Basel, Basel, Switzerland; University of Rochester, Rochester; Hospital Sant Pau, Barcelona, Spain; Amgen Ltd, Cambridge, United Kingdom; Amgen (Europe) GmbH, Zug, Switzerland; University of Frankfurt, Frankfurt, Germany Background Recent EORTC/ASCO guidelines recommend granulocyte colony stimulating factor (G-CSF) primary prophylaxis (PP) for cancer patients at overall ≥20% risk of febrile neutropenia (FN) during chemotherapy (CT). Patient-related FN risk factors (particularly age ≥65 years) should be considered as well as the mean risk from a given CT regimen. In this subgroup analysis from the NeuCuP project, the incidence of FN and related complications is compared for elderly breast cancer patients receiving CT supported by PP peg¿lgrastim or any G-CSF according to current practice (CP). Methods Studies involving breast cancer CT regimens with moderate (15–20%)/high (≥20%) FN risk were identi¿ed by literature review. For this integrated analysis, individual patient data were available from 8 clinical trials and 3 observational studies (conducted 1998–2005) involving these regimens and PP peg¿lgrastim (6 mg dose, all cycles) or CP neutropenia management (no G-CSF or peg¿lgrastim/daily GCSF in any cycle). The primary outcome measure was the incidence of FN over all cycles. Descriptive data are reported for the subgroup of patients aged ≥65 years. Results 254/2282 patients were aged ≥65 years and included in this analysis. Patients’ mean age (±SD, years) was 69±4 for PP vs 68±3 for CP; 37% vs 31% had Stage IV disease, 95% vs 79% were ECOG 0–1 (1% vs 15% missing) and 32% vs 30% had prior chemo/radiotherapy. Docetaxel was the most common regimen (41% vs 47%), followed by TAC (24% vs 27%), and ADoc (28% vs 7%). In cycle 1, 73% of CP patients received no G-CSF, 13% received peg¿lgrastim only, and 14% received various G-CSF regimens. FN, FN-related hospitalization and CT delivery parameters are shown (table). Conclusions In elderly breast cancer patients receiving CT with moderate/high FN risk, PP peg¿lgrastim was associated with a lower overall incidence of FN vs CP neutropenia management (including cycle 1, when most FN occurs). PP peg¿lgrastim also resulted in fewer dose delays and dose reductions. Peg¿lgrastim provided effective PP in elderly patients, who are particularly vulnerable to FN and its complications. FN FN-related hospitalization Dose delay >3 days Dose reduction 15% All cycles % patients (95% CI) PP (n=150) CP (n=104) 6 (2, 10) 24 (16, 32) 5 (2, 9) 15 (8, 22) 14 (8, 20) 21 (13, 29) 15 (9, 20) 29 (20, 38) Cycle 1 % patients (95% CI) PP (n=150) CP (n=104) 3 (0, 6) 15 (8, 22) 4 (1, 7) 13 (6, 19) N/A N/A N/A N/A 1089 Pegfilgrastim promotes neutrophil recovery in elderly breast cancer patients following anthracycline-containing chemotherapy. Brugger W, Bacon P, Lawrinson S, Romieu G. Schwarzwald-Baar Clinic, University of Freiburg, Villingen-Schwenningen, Germany; Amgen (Europe) GmbH, Zug, Switzerland; Amgen Ltd, Uxbridge, United Kingdom; CRLC Val d’Aurelle, Montpellier, France Background: Myelosuppressive chemotherapy (CT) is associated with risk of febrile neutropenia (FN), particularly in elderly patients. FN frequently leads to CT dose delays and dose reductions that may compromise treatment outcome, while FN itself has an inhospital mortality rate up to 10%. Prophylactic granulocyte colony stimulating factors (G-CSFs) aid neutrophil recovery following CT, reducing duration of neutropenia and risk of FN, and facilitating delivery of subsequent CT cycles. In a phase II study of neutropenic events in elderly patients receiving pegfilgrastim as primary or secondary prophylaxis (PP or SP) after Àurouracil/epirubicin/cyclophosphamide (FEC) CT (Romieu et al. Crit Rev Onc Haem 2007), the pro¿le of neutrophil recovery in cycle 1 was assessed. Methods: Elderly patients ≥65 years with stage II–III breast cancer were included in the study and treated with up to 6 cycles of adjuvant F 500 mg/m2 / E 100 mg/m2 / C 500 mg/m2 (FEC100). Patients were prospectively randomized to receive open-label peg¿lgrastim PP (6 mg sc) on Day 2 after CT from cycle 1, or peg¿lgrastim SP (on Day 2 of all cycles subsequent to a neutropenic event). In this analysis, the mean absolute neutrophil count (ANC) pro¿le in cycle 1 (during which no SP patient received peg¿lgrastim) was reviewed. Results: Sixty patients were randomized to PP (n=31) or SP (n=29) peg¿lgrastim. The mean (±SD, years) age in the PP group was 67.5±3.6 vs 69.0±3.2 in the SP group; 71% vs 62% had ductal breast carcinoma, 68% vs 83% were ER positive and 68% vs 72% had ≥4 positive lymph nodes. The mean ANC at baseline was 4.3±1.0 vs 4.0±1.2 x109/L, respectively. The ANC pro¿le in cycle 1 for patients (n=59) receiving prophylactic peg¿lgrastim or no growth factor support is shown. Mean ANC was ≥1.0 x 109/L from Day 9 in patients receiving peg¿lgrastim compared with Day 18 in those receiving no growth factor. All cycles were delivered at planned dose and schedule in 26/30 (87%) of PP patients compared with 20/29 (69%) of the SP group. Conclusions: In cycle 1, pegfilgrastim promoted ANC recovery compared with no growth factor support in elderly patients. On average, the depth and duration of ANC nadir was reduced in patients receiving peg¿lgrastim compared with those receiving no growth factor, therefore reducing the period of risk for FN and complications due to grade 3/4 neutropenia. PP may therefore reduce CT dose delays and dose reductions in subsequent cycles compared with SP. Abstracts – Poster Session I 1090 Pre-treatment differential white blood cell counts can be used to identify patients who are at increased risk of severe myelosuppression following adjuvant chemotherapy. Jenkins P, Benstead K, Owen R, Elyan S, Ingledew I, Bristol J, Chan C, Freeman S. Cheltenham General Hospital, Cheltenham, Gloucestershire, United Kingdom; University of Birmingham, Birmingham, Edgbaston, United Kingdom Introduction Maintaining the dose intensity of adjuvant breast cancer chemotherapy is important to maximise the results of treatment. The identi¿cation of factors that predict for severe myelosuppression would enable clinicians to better target growth factor support. We have previously demonstrated that obesity does not predispose to excess haematological toxicity (EJC 43 544). Here we report our observations on the predictive value of pre-treatment full blood count parameters. Methods 360 patients (pts) receiving 6 cycles of adjuvant FEC chemotherapy were studied. The regimen employed comprised 5-Àuorouracil 600mg/ m2, epirubicin 60mg/m2 and cyclophosphamide 600mg/m2, cycled at 3 weekly intervals. Chemotherapy was delayed for one week if the neutrophil count on the date of treatment was <1.5x109/l. Following 2 delays, or an episode of neutropaenic sepsis, a 20% dose reduction was made. Chemotherapy dose intensity (DI) was considered suboptimal of it fell below 85% of that planned (DI<85). 55 pts in whom the schedule was modi¿ed due to non-haematological toxicity were excluded from the analysis. Haematological growth factors were not employed in the period of this audit. Parameters from the pre-treatment full blood count were analysed for there ability to predict for a DI<85. Results In total 108 (35%) pts had a schedule modi¿cation due to haematological toxicity. 26 (9%) pts had an episode of neutropaenic sepsis and 88 (29%) had one or more treatment delays. The mean dose intensity was 93.8%. 64 pts (21%) received a DI<85%. On univariate analysis (t-test) only the absolute neutrophil count (ANC), the absolute lymphocyte count (ALC) and the total white cell count (WCC) were associated with the DI<85 (p<0.005). On multivariate analysis (logistic regression) ALC and WCC remained signi¿cant (p<0.01). Using the median values of ANC (4.1x109/l) and ALC (2x109/l) we developed a simple model which categorised pts into four risk groups with a 8%, 18%, 25% and 36% chance of receiving suboptimal DI (see ¿gure). Conclusions Differential white blood cell counts can be used to de¿ne groups at increased risk of receiving suboptimal DI. This will aid clinicians in targeting cytokine growth factors and prophylactic antibiotics to the groups that most need it. We are currently developing a validation sample. S73 1091 Quality of life in the Intergroup Exemestane Study (IES) 5 years post-randomisation. Fallow¿eld LJ, Langridge CI, Kilburn LS, Jones SE, Snowdon CF, Bliss JM, Coombes C. Brighton & Sussex Medical School, Falmer, United Kingdom; Institute of Cancer Research, Sutton, United Kingdom; US Oncology Research, TX; Imperial College London, United Kingdom; on behalf of the IES Group Background: IES has shown switching to exemestane (E) following 2-3 years of tamoxifen (T) improves disease outcome in hormone sensitive postmenopausal breast cancer patients compared to 5 years of T alone1; and without detriment to QoL up to 24m post-randomisation2. Few adjuvant hormonal trials have reported long-term QoL. Here we report QoL through to 60m including post treatment follow-up. Methods: 582 women entered the QoL substudy, with FACT-B-ES questionnaires at baseline (BL) 3, 6, 9, 12, 18, 24, 30, 36, 48 and 60m. Primary endpoint was trial outcome index (TOI), a summation of the physical, functional and breast cancer concerns subscales. Secondary outcomes were overall endocrine symptom (ES) scores plus severity of individual symptoms. Most patients ¿nished trial treatment by 30-36m. Results: Questionnaire completion was good with 84.4% available for analysis. Overall QoL did not differ signi¿cantly between groups; both showed a gradual improvement over time. There were no signi¿cant differences between groups for ES; both groups reported a lessening of symptoms over time and post treatment. Severe vasomotor complaints, especially hot Àushes and night sweats, remained problematic for both groups on treatment. Reports of severe vaginal discharge were signi¿cantly higher (p<0.01) with T at 6, 9, 12, 18 and 24m. Libido never recovered to BL levels for either group, even post treatment. At 60m 32.5% (22.6%-43.7%) reported a considerable loss of libido in both groups. Discussion: Mature IES data suggest that the benefits of E are accompanied by good overall QoL. Further research is needed to ameliorate the sexual and gynecological symptoms associated with hormonal treatment. 1. Coombes RC et al. Lancet 2007; 369: 55970 2. Fallow¿eld LJ et al. JCO 2006; 24; 6: 910-916. N TOI 24m 60m ES 24m 60m E T E T E T E T 224 212 102 103 225 213 101 107 Change from BL within groups (mean (95%CI)) -0.46 (-1.65, 0.73) 0.52 (-0.62, 1.66) -0.46 (-2.39, 1.47) 0.11 (-1.85, 2.06) 1.91 (0.96, 2.86) 1.49 (0.56, 2.42) 3.11 (1.44, 4.78) 3.36 (1.98, 4.74) p= 0.45 0.37 0.64 0.91 <0.001 0.002 <0.001 <0.001 Change between p= groups (mean (95%CI)) -0.98 (-2.62, 0.67) 0.24 -0.57 (-3.30, 2.16) 0.68 0.42 (-0.91, 1.74) 0.54 -0.25 (-2.40, 1.89) 0.82 1092 Prospective multi-center study of the impact of the 21-gene recurrence score assay on patient satisfaction, anxiety and decisional conÀict for adjuvant breast cancer treatment selection. Mumby PB, Lo SS, Norton J, Smerage J, Joseph K, Chew HK, Hayes D, Albain KS. Loyola University Medical Center, Maywood, IL; University of Michigan, Ann Arbor, MI; Edward Hospital, Naperville, IL; University of California, Sacramento, CA Background: Use of the Oncotype DX Recurrence Score assay (RS) in a prospective, multi-institutional study resulted in a change in medical oncologist (MO) adjuvant treatment recommendation in 31.5% (n=28) of cases; the most common change was from chemo/hormonal therapy (CHT) to hormone therapy (HT) (Lo et al., ASCO 2007). This new report analyzes the patient (pt) portion of the study, with objectives to determine the impact of the RS on pt’s treatment decision-making and anxiety level before and after the test. Material and Methods: Patients at 1 community and 3 academic centers completed 3 questionnaires pre- and post-RS: 1) the Patient Treatment Decision Making Questionnaire; 2) the Decisional ConÀict Scale (DCS); and 3) the State-Trait Anxiety Inventory. Frequency distributions, means and standard deviations were used to summarize data. Paired samples t-tests assessed anxiety, satisfaction, and decisional conÀict pre- and post-RS. S74 Abstracts – Poster Session I Results: Accrual goal was met with 89 evaluable pts. 95% (n=81) of pts were glad they took the test, and 83% (n=89) reported the assay inÀuenced their treatment choice. 26.8% (n=24) of pts had a change in treatment plan post-RS, with 10.1% (n=9) changing from pre-test CHT to post-test HT. Results from the DCS indicate reduced conÀict over treatment decision post-RS (p <.0001), greater pt satisfaction, and increased con¿dence with choice of adjuvant therapy (p <.0001). State anxiety was also reduced post-RS (p. = 001). Discussion: Results of the RS changed both MO’s and pt’s decisions regarding adjuvant therapy. Use of the assay resulted in less chemotherapy use, decreased pt anxiety and increased pt con¿dence regarding adjuvant treatment decisions. 1093 Predictors of weight gain in patients with early stage breast cancer. Mills JB, Gui J, Mulrooney TJ, Schwartz GN. Dartmouth-Hitchcock Medical Center, Lebanon, NH; Dartmouth Medical School, Hanover, NH Background: Weight gain after the diagnosis of breast cancer occurs frequently in women who receive adjuvant chemotherapy, and it can be a distressing and hazardous burden for breast cancer survivors. Prior series have found up to a 5 kg median weight gain associated with chemotherapy, but it is not known what effect newer adjuvant therapies containing taxanes or aromatase inhibitors may have on weight gain. Material and Methods: A retrospective cohort of 90 women who were diagnosed with Stage I-II breast cancer between July 2001 and June 2004 and treated with adjuvant therapy had weight and BMI, chemotherapy and endocrine therapy treatment, age, baseline menopausal status and change in menopausal status, the use of antidepressants, thyroid function, hemoglobin, and fatigue assessed at baseline, and at 6, 12, and 24 mo after diagnosis. Correlates of weight gain were identi¿ed by univariate analysis, and joint associations were identi¿ed by combining predictors in a multiple regression model. Results: The median age at diagnosis was 55 and 25% of the subjects were <50 at diagnosis. The median BMI was 26.2 at baseline, 36% had a BMI <25, and 26% had a BMI>30. 50% of patients received chemotherapy and 32% received a taxane-based regimen. 74% were given tamoxifen and 12% received an AI. 20% were treated with an SSRI. The median weight gain was 0.8 kg at 24 mo. Median weight gain at 24 mo was 2 kg in premenopausal women and 0.4 kg in postmenopausal women. Baseline weight, age at diagnosis, menopausal status, anemia, a change in menopausal status, the use of an SSRI, baseline TSH, fatigue score, chemotherapy, and endocrine therapy were not signi¿cantly associated on univariate or multivariate regression with weight gain at any time point. Only a lower baseline BMI was predictive of subsequent weight gain (p<0.05). Discussion: Our experience ¿nds no association of weight gain with breast cancer therapy, including the newer systemic regimens. The only predictor for weight gain following diagnosis of early stage breast cancer was a lower BMI at baseline. Women who are not overweight at baseline are at risk for weight gain following a breast cancer diagnosis and could be targeted with interventions to prevent weight gain, such as exercise to reduce therapy-related changes in body composition. 1094 Memory loss after adjuvant chemotherapy for breast cancer: a preliminary analysis of mediating variables utilizing cross-sectional correlations and multilevel longitudinal analysis. Beadle G, Rolfe M, Vearncombe K, Andrew B, Mengersen K, Wright M. Queensland Institute of Medical Research, Brisbane, Queensland, Australia; Southern Cross University, Lismore, New South Wales, Australia; University of Queensland, Brisbane, Queensland, Australia; Queensland University of Technology, Brisbane, Queensland, Australia BACKGROUND Cognitive impairment is a well recognized complication of adjuvant chemotherapy but further research is required to identify factors that mediate cognitive change in breast cancer survivors. METHODS This study investigated cognitive change in verbal memory in 119 women aged less than 70 years before, at completion of, and 6 months after adjuvant chemotherapy. Verbal memory was assessed with the auditory verbal learning test trials 1-5 (AVLT1-5) and executive processing of immediate and delayed recall with the AVLT7 and the AVLT8 respectively. Cross-sectional correlations were performed with time invariant variables of age, years of education and general cognitive ability utilizing the national adult reading test (NART). Correlations with time varying variables included quality of life measures (HADS, FACT-B and FACT-F) and changing hormonal phenotype (cessation of hormone replacement therapy after diagnosis of breast cancer and changing menstrual function after chemotherapy). Unconditional random intercept quadratic regression models were ¿tted to AVLT1-5, AVLT7 and AVLT8, with temporal and subject level variances estimated by restricted maximum likelihood. RESULTS In this exploratory analysis, age, NART and years of education were signi¿cantly correlated with AVLT1-5, AVLT7 and AVLT8 at all time points (all p values <0.05). Quality of life correlates were inconsistent at most time points but statistically signi¿cant when all time points were combined (HADS depression <0.05 and FACT fatigue <0.05 for AVLT8; FACT-B <0.05 for AVLT1-5, and <0.01 for AVLT7 and AVLT8). Age, NART and years of education were signi¿cant predictors of these changes (p <0.01). In particular, a high NART predicted a less steep decline of memory over time. There was no evidence of a statistically signi¿cant association between AVLT and self-report measures of quality of life or changing hormonal phenotype after adjustment for age and NART. CONCLUSION A signi¿cant decline of the AVLT occurred during and after treatment with adjuvant chemotherapy. Age, NART and years of education were strongly associated with AVLT at all time points but not quality of life or changing hormonal phenotype. Further investigation of memory and executive functioning is currently underway in a larger sample of patients followed over a longer time. Multilevel longitudinal analysis is a promising tool for investigating longitudinal data that contain multiple changing covariates. 1095 Research on optimal recovery practices in breast cancer: the RESTORE trial. Kimmick GG, McCoy TP, Milhalko SL, Ribisl PM, Anderson RT. Wake Forest University School of Medicine, Winston-Salem, NC; Wake Forest University, Winston-Salem, NC; Duke University Medical Center, Durham, NC Background: Post-treatment behavioral interventions, designed to prevent disability and improve quality of life in breast cancer survivors, are needed. Emotional distress, fatigue and psychosocial issues may be signi¿cant and persist over time. The RESTORE study is a randomized, controlled, clinical trial designed to test and compare the effectiveness of a moderate, tailored exercise program on improving quality of life (FACT-B)and physical function (six-minute walk) of women treated for stage I to III breast cancer at 18-months post-enrollment, versus usual care. Objectives: Women, with stage I-III breast cancer treated at one of two large medical centers, were recruited within 6-12 weeks of surgery and randomized to treatment or control. Those in the treatment group began a center-based exercise and a lymphedema education program 2 to 3 days per week gradually shifting to the home. Controls received patient education. Study participants were assessed at 3-month intervals through 18-months. Distributions over time were examined using box plots and smoothed curves. Repeated measures analysis of covariance was used to model the total meters walked over time and FACT-B scores. Models were adjusted for baseline measurement, baseline affected arm volume, number of nodes removed during surgery, age at randomization, # of self-reported symptoms, baseline SF-12 mental and physical components scores, visit and treatment group. Signi¿cance was considered to be a 2-sided p-value < 0.05. Results: There were 105 women in the study, 82 of whom completed all 18 months of the study. Mean age (range) was 53.6 (32-82) years; 88% were Caucasian; 45% were employed full-time; 44% and 27% were Abstracts – Poster Session I overweight and obese. At baseline 46% had breast conserving surgery; 79% had axillary node dissection; 59% received chemotherapy and 64% received radiation. Patients in the treatment group had increased total meters walked compared to controls: adjusted means (SE) were 606.5 (10.7) and 577.1 (6.8) respectively (p=0.025). There was no difference in the adjusted means for FACT-B scores: 117.2 (2.0) for the treatment group and 114.7 (1.5) for the control group (p=0.33). Conclusions: With this early exercise intervention after breast cancer diagnosis, signi¿cant improvement was achieved in physical ¿tness over time with no decline in health-related quality of life, as measured by FACT-B. 1096 Breaking bad news: experiences receiving breast cancer diagnosis in a specialty breast center versus community practice. Smith RL, Crawford BJ, Petersen LR, Johnson RE, Mandrekar J, Cha S, Rhodes DJ, Hartmann LC. Mayo Clinic, Rochester, MN Context: Recommendations for “breaking bad news” and disclosure of cancer diagnosis have been promoted for many years. In view of the rise in specialty breast centers and less invasive biopsy techniques, current experiences of women receiving breast cancer (BC) diagnosis are not well characterized. Methods: A total of 177 subjects responded to a questionnaire regarding the experience receiving BC diagnosis: 121 women (68%) received BC diagnosis then were referred to a specialty breast center (community, CP) and 56 (32%) received BC diagnosis within the specialty center (SC). Speci¿c items included recent stress levels; context factors (i.e. location, duration, privacy), clinician behaviors (i.e. providing educational materials, using touch to comfort, approach to discussing diagnosis) and patient-clinician relationship. Satisfaction was also rated on a 5 point scale. Results: Patients were enrolled 1 to 54 days following BC diagnosis. Mean age of SC patients was higher (63 vs. 56 yrs, p=0.005). Context factors differed between groups, with mode of delivery shown in Table 1. In decreasing frequency, CP patients received diagnosis from generalists, surgeons, radiologists, nurses, NP/PAs, gynecologists, specialists, family members and secretaries. CP patients described relationship with person who disclosed diagnosis as excellent (21%), good (25%), satisfactory (26%), inadequate (7%), poor (5%) and did not know well enough (15%). Almost all SC patients received diagnosis from a breast specialist. Selected differences in clinician behavior and content are shown in Table 2. BC stage did not differ between CP and SC patients. Patient satisfaction was favorable, but differed between groups, (CP 3.50 vs SC 4.60, p <.0001). Conclusions: Patient experiences receiving BC diagnosis are variable and may be associated with patient satisfaction. Differences in the experience provide an opportunity to identify factors with potential to inÀuence satisfaction with medical care and psychological outcomes. Table 1: Mode of Delivery Community (N=121) 71 (59%) 48 (40%) 1 (1%) Specialty Center (N=56) 19 (34%) 35 (63%) 0 (0%) Table 2: Clinician Behavior and Content Community Clinician Behaviors + Content (N=121) Information found helpful 58 (48%) Educational materials provided 23 (21%) Opportunity to ask questions 89 (74%) Touch used to comfort 27 (22%) Specialty Center (N=56) 42 (75%) 34 (67%) 53 (96%) 27 (51%) Mode of Delivery Telephone Face to Face Letter Signi¿cance p = 0.0003 p = 0.006 p = 1.00 Signi¿cance p = 0.010 p < 0.0001 p = 0.0001 p = 0.0003 1097 Appraisals, coping and distress among couples dealing with breast cancer. Hernandez AM, Bigatti SM. Indiana University Purdue University Indianapolis, Indianapolis, IN This study aimed to investigate the cognitive appraisals, coping styles and levels of distress of couples dealing with breast cancer. Cognitive S75 appraisals are evaluations individuals make of stressful situations in order to categorize them as benign/irrelevant, challenge, threat, or harm. These cognitive appraisals predict coping mechanisms, which in turn impact levels of distress. Studying couples, or dyads, is important because the coping style of one individual in the dyad is associated with outcomes in the other. One adaptive form of coping is emotional approach coping, which consists of emotional processing and emotional expression. Breast cancer patients currently undergoing chemotherapy treatment (n = 22) and their spouses (n = 22) were recruited from a breast cancer clinic. Both the patient and spouse completed surveys at home and returned them by mail. Stanton’s Emotional Approach Coping Scale, Kessler’s Cognitive Appraisal of Health Scale, and the Pro¿le of Mood States (POMS) were included in the questionnaire packages. Most of the patients had stage IV breast cancer (68.2%). The average age for patients was 53.55 (SD = 11.571) and for husbands was 54.49 (SD = 11.784). Participants were married an average of 27.28 years (13.99). Most reported a yearly income above $70,000. Husbands scored higher in the anxiety subscale of the POMS and were more likely to appraise the cancer as a threat than the patients themselves. We grouped couples into those who matched on appraisals and those who did not and examined the groups’ level of distress and coping. We found no differences by group for husbands on either variable, or for wives on the POMS. However, wives who did not match on appraisals with their husbands engaged in more emotional approach coping F(1,20)= 6.474, p=.019), and more speci¿cally emotional expression F(1,20) = 4.969, p = .037) and emotional processing coping F (1,20) = 6.089, p = .023). These ¿ndings suggest that patients who have a different view of the cancer than their partners may need to engage in more coping efforts than those who have the same view. Possibly agreement, regardless of the appraisal agreed upon, relieves the patient from reappraising. On the other hand disagreement may require both processing and expression to determine whether the appraisal is in fact correct or should be reconsidered. Because appraisals change throughout the cancer experience, it may be that one impetus for reappraisals is disagreement with a spouse and subsequent emotional work. 1098 The psychosocial issues for women diagnosed with breast cancer who have a concurrent pregnancy or want the option of a subsequent pregnancy. Ives A, Longman G, Saunders C, White K. The University of Western Australia, Perth, WA, Australia; University of Sydney, Sydney, NSW, Australia Objectives: To identify psychosocial issues for women diagnosed with breast cancer when pregnant or who become pregnant after their diagnosis and develop strategies to assist others who go through this experience in the future. Methods: Women were randomly invited to participate in this study via the Western Australian Department of Health. Interviewees were from one of three groups of women less than 45 years of age when diagnosed with breast cancer; either with gestational breast cancer, or who subsequently conceived or with breast cancer unrelated to pregnancy. Semi-structured interviews were recorded and transcribed verbatim. During the interviews, the researcher sought to identify any psychological and social issues related to the decisions made by women diagnosed with breast cancer and relating to their concurrent or subsequent pregnancy. Areas of interest included: coping mechanisms used; formal and informal support structures; breast cancer treatment and outcome issues; fertility and contraception issues; pregnancy events; dealing with illness and a young child. The data was analysed by four researchers using thematic analysis consistent with this explorative qualitative research design. Results: Motherhood was identi¿ed as of key importance to these women. For example, protecting their young children or an unborn child – for some of them this was foregoing treatment but for others it was terminating their pregnancy to ensure they could have the necessary cancer treatment to spend time with their other children. Three unmet needs were highlighted: isolation, lack of support and lack of information. The feelings of isolation came from believing that they were the only person who had ever been through such an experience; S76 Abstracts – Poster Session I a feeling that was not dispelled by their health professionals. These women needed to make dif¿cult decisions about their breast cancer management and/or pregnancy and they felt that that they were being judged and not supported in the decisions. There was also a lack of information on available breast cancer and pregnancy management options for these women and treating clinicians did not appear to have access to the small but relevant knowledge base available. Conclusions: The study highlighted the high priority women place on doing the best or the right thing by their child or children. Every woman behaved differently based on her life experiences but simple steps such as a telephone support network and unbiased support could reduce the stresses of such life changing events. There is also a growing need for better evidence based information to be readily available to this group of women and their treating clinicians. 1099 Prevalence of cognitive complaints is not higher in postmenopausal breast cancer patients before adjuvant hormonal therapy compared to healthy controls. Schilder CM, van Dam F, Boogerd WS, Seynaeve C, van de Velde CJ, Nortier HW, Linn SC, Schagen SB. Netherlands Cancer Institute, Amsterdam; Erasmus Medical Center, Rotterdam; University Medical Center, Leiden, Netherlands Background Breast cancer (BC) patients (pts) treated with adjuvant therapy often report cognitive changes such as memory or concentration problems. Up till now, it is insuf¿ciently investigated whether cognitive complaints are already present after BC surgery and before subsequent adjuvant treatment. The aim of this study was to assess the prevalence of cognitive complaints before adjuvant Hormonal Therapy (HT) in postmenopausal BC pts. In addition, relationships with time since diagnosis and surgery, and symptoms of anxiety/depression and fatigue were studied. This information will provide more insight into the association between cognitive complaints, speci¿c treatments and disease- and treatment related factors. Methods Occurrence of cognitive complaints was studied in 1) BC pts not quali¿ed to receive chemotherapy (n=205, mean age 68.9 yrs; range 5084) participating in the TEAM-trial, a randomized study investigating tamoxifen and exemestane as adjuvant HT, and 2) a control group of healthy female friends/relatives of the TEAM pts (n=124, mean age 66.5 yrs; range 49-87). Participants were interviewed about memory, concentration, thinking and language problems, after surgery (mean nr. of days since surgery 42, range 9-140) but before adjuvant HT. 15% of the pts underwent radiotherapy at the moment of the interview. Anxiety/depression was measured with the Hopkins Symptom Check List (HSCL), fatigue with the Multidimensional Fatigue Scale (MFI; scales general and physical fatigue). Group differences were analyzed with χ 2-tests, correlations with Spearman correlation coef¿cients. Results BC pts did not report a higher frequency of memory, thinking and language problems than controls. A lower frequency of concentration problems even was observed in BC pts versus controls (6% versus 13%, p=.04). The occurrence of cognitive complaints did not correlate with age or IQ. Time since diagnosis and surgery, and current radiotherapy (y/n) were not related to presence of cognitive problems. In both groups, a signi¿cant higher proportion of persons that scored in the ‘possibly depressive case’-range (HSCL ≥ 1.55; BC pts 23%; controls 14%, p=.045) reported concentration problems compared to nondepressed persons (BC pts: 15% versus 3%, p=.007; controls: 41% versus 9%, p= .002). For memory, thinking and language complaints no relationships with anxiety/depression were found. General and physical fatigue were not related to cognitive complaints. Conclusion Shortly after BC surgery and before adjuvant HT, the prevalence of cognitive complaints is not higher in postmenopausal BC pts than in a healthy age-matched population. In both pts and controls, higher anxiety/depression scores were associated with a higher frequency of concentration complaints, but not with memory, thinking and language complaints. Neither general and physical fatigue, nor treatment related factors were associated with cognitive complaints. 1100 Unexpected effects of reassurance in women with low-risk breast cancer. Griggs JJ, Corbin K, Weiss M, Shields CG. University of Michigan, Ann Arbor, MI; University of Rochester School of Medicine and Dentistry, Rochester, NY; breastcancer.org, Narberth, PA Objective: Patients with low-risk breast cancer are often told they have a “good cancer.” The purpose of this study was to investigate the impact of this form of reassurance on distress and concerns about recurrence in women with ductal carcinoma in situ (DCIS) and early stage invasive breast cancer. Methods: We conducted an anonymous survey on the website of breastcancer.org, a non-pro¿t organization. The survey inquired about disease and treatment characteristics and contained the Positive and Negative Affect Scale (PANAS) and the Concerns about Recurrence Scale (Vickberg, Ann Behav Med 2003). Participants were also asked if they had been told by any of their medical providers that they had a “good cancer” or “favorable cancer” Analyses were performed to investigate the impact that being told one has or had a “good cancer” and feelings of reassurance, isolation, distress, guilt, and concerns about recurrence. Results: A total of 646 participants with localized or regional breast cancer (n = 323) or DCIS (n = 323) breast cancer completed the survey. Being told that she had had a “good cancer” was reported by 62% of women with DCIS and 32% of women with invasive disease. Among those told they had a good cancer, 59% reported that being told this led to their feeling moderately-to-extremely “reassured.” A high percentage of respondents (29%) reported feeling minimally reassured by this phrase. Many respondents also reported moderate-to-severe negative responses to being told that they had a good or favorable cancer—feeling moderately-to-extremely “isolated” (21%), “distressed” (40%), “scared” (45%), or “guilty” (20%). In addition, among women with DCIS, the good cancer message was associated with greater level of concern about recurrence, controlling for age, time since diagnosis, surgical treatment, and mental health (p < .005) Conclusions: Although telling patients they have a “good” or “favorable” cancer leads to feelings of being reassured in many women, such terms may also contribute to distress, feelings of isolation, and guilt among many patients who otherwise might enjoy a good prognosis quality of life. Providing reassurance is a complex process. Further research into effective ways of communicating reassurance is warranted in order to minimize distress and enhance quality of life. 1101 Breast reconstruction in a university-based public hospital. Levine SM, Vaksman A, Hiotis K, Levine JP. New York University Medical Center, New York, NY Breast reconstruction rates continue to rise in large part due to patients and communities becoming more knowledgeable about postmastectomy options. Overall satisfaction with breast reconstruction is traditionally high only adding to the popularity of the choice. Prior research has demonstrated that race, age, and socioeconomic status, are important determinants in whether a patient undergoes breast reconstruction; speci¿cally, indigent women have only an 8% rate of breast reconstruction compared with a national average of 42 %. Our study retrospectively examined the breast reconstruction choices made by patients at a large public hospital in New York City where resources for reconstruction are fully available, within a multidisciplinary clinic environment. Between January 2001 and December 2006, 179 patients underwent mastectomy, and 73 (41 %) elected reconstruction. Patients in age ranges 20-39 and 40-59, were both signi¿cantly more likely to undergo reconstruction than patients greater than 60 years of age. Disease stage was not signi¿cantly related to rates of breast reconstruction. Reconstruction rates by race and ethnicity were analyzed and demonstrated a signi¿cantly lower rate of breast reconstruction in Asian women (32 %) compared with Hispanic women (47 %), despite the same access to available services. Our data demonstrate breast reconstruction rates signi¿cantly higher than prior studies for women in this public hospital demographic, while at the same time maintaining other trends with regard to breast reconstruction. These data suggest that indigent patients are more likely to have breast reconstruction when their Abstracts – Poster Session I care is delivered at a university based public hospital where consistent patient education is practiced, in a multidisciplinary fashion. 1102 Anti-tumor activity of motesanib diphosphate alone and in combination with docetaxel or tamoxifen in xenograft models of human breast carcinoma. Coxon A, Bush T, Belmontes B, Saffran D, Ona V, Rex K, Caenepeel S, Hughes P, Kaufman S, Radinsky R, Kendall R, Price J, Polverino A. Amgen Inc, Thousand Oaks, CA; UT MD Anderson Cancer Center, Houston, TX Background: Angiogenesis is necessary for tumor growth and vascular endothelial cell growth factor (VEGF) and its receptors play a pivotal role in the neovascularization process. Motesanib diphosphate (AMG 706) is a highly selective, oral agent that is being evaluated for its ability to inhibit angiogenesis and lymphangiogenesis by targeting vascular endothelial growth factor receptors 1, 2, and 3 (VEGFR1-3). It is also under investigation for its potential direct anti-tumor activity by targeting platelet-derived growth factor receptor (PDGFR), and stem cell factor receptor (c-kit) signaling. In this study, we examined the effects of motesanib diphosphate in preclinical models of human breast carcinoma, both as a single agent and in combination with docetaxel or tamoxifen. Materials and Methods: The ability of motesanib diphosphate to inhibit the growth of MDA-MB-231 (mesenchymal), MCF-7 (luminal), Cal-51 (basal) and GILM2 (basal) breast carcinoma cells cultured in vitro was determined using the ATPlite cell viability assay. To determine in vivo ef¿cacy, nude mice bearing established (∼100-200 mm3) MCF-7, MDA-MB-231, Cal-51 or GILM2 xenografts were treated orally with motesanib diphosphate BID at 7.5, 25 and 75 mg/kg. For combination experiments, docetaxel and tamoxifen were administered IP at 20 mg/kg once weekly and 30 mg/kg ¿ve times per week, respectively. At the end of treatment, tumors were collected for blood vessel area (anti-CD31 staining) and viable tumor area (hematoxylin) assessment. Results: Motesanib diphosphate had no effect on the in vitro growth of any of the breast cancer cell lines. In contrast, treatment with motesanib diphosphate in vivo resulted in a dose-dependent inhibition of tumor growth in all four breast cancer models. Signi¿cant inhibition (p <0.05) was observed with all three doses of motesanib in the Cal-51 and GILM2 basal models. In the MCF-7 model, signi¿cant inhibition (p <0.0005) was achieved at the 25 and 75 mg/kg doses, whereas only the 75 mg/kg dose was signi¿cant (p <0.0001) in the MDA-MB-231 model. Histological analysis of the MDA-MB-231, Cal51 and MCF-7 tumors revealed a signi¿cant decrease in viable tumor fraction and a reduction in blood vessel area after motesanib treatment. In combination studies, treatment with motesanib diphosphate in the MDA-MB-231 and MCF-7 models signi¿cantly enhanced the anti-tumor activity of docetaxel and tamoxifen respectively (p <0.05). Together, these data suggest that motesanib diphosphate inhibited tumor growth via an inhibition of angiogenesis, and that this was enhanced when combined with standard chemotherapy. Conclusion: The preclinical anti-tumor activity of motesanib diphosphate in multiple models of breast carcinoma supports the development of this anti-angiogenic agent in the broad management of breast cancers, in combination with other current breast cancer therapies. 1103 Non-invasive LQYLYR subcellular multicolor imaging of the tumor microenvironment and drug response in real time. Yang M, Jiang P, Al-Zaid M, Hoffman RM. AntiCancer, Inc., San Diego, CA; University of California, San Diego, San Diego, CA Background: In order to non-invasively image cancer-cell—stromalcell interaction in the tumor micro-environment and drug response at the cellular level in live animals in real time, we developed a new imageable three-color animal model. Materials and Methods: The model consists of GFP-expressing mice transplanted with dual-color breast cancer cells labeled with GFP in the nucleus and RFP in the cytoplasm. The Olympus IV100 Laser Scanning Microscope, with ultra-narrow microscope objectives (“stick S77 objectives”), is used for three-color whole-body imaging of the twocolor cancer cells interacting with the GFP-expressing stromal cells. In this model, drug response of both cancer and stromal cells in the intact live animal is also imaged in real time. Results: Various in vivo phenomena of tumor-host interaction and cellular dynamics were imaged including mitotic and apoptotic tumor cells, stromal cells interacting with the tumor cells, tumor vasculature, and tumor blood Àow. This new model system enables the ¿rst cellular and subcellular images of unperturbed tumors in the live intact animal at the subcellular level. Discussion: New visible real-time targets for novel anticancer agents are provided in this model including the color-coded interacting cancer and stromal cells, tumor vasculature, and blood Àow. This imageable model should lead to many new insights of in vivo cancer cell biology and to novel drug discovery. 1104 Anti-angiogenic potential of coenzyme Q10, riboÀavin and niacin in breast cancer patients undergoing tamoxifen therapy. Panchanatham S. DR. A.L.M.P-G.I.B.M.S., University of Madras, Tarmani Campus, Chennai, Tamilnadu, India Background: To evaluate the anti-angiogenesis effect of CoenzymeQ10, riboÀavin and niacin (CoRN) in breast cancer patients undergoing tamoxifen therapy. Efficacy of the combinatorial (CT) drug was correlated with serum angiogenic marker levels. Methods: Eighty four women with breast cancer undergoing tamoxifen therapy were treated with 100 mg CoenzymeQ10, 10 mg RiboÀavin and 30 mg Niacin for 90 days. Blood samples were collected at the start of the study, at 45 days and 90 days of the treatment regimen. Circulating markers such as Vascular endothelial growth factor (VEGF), Matrix metalloproteinase (MMP) - 2, MMP-9, Tissue Inhibitor of metalloproteinase (TIMP) - 1, TIMP-2, Interleukin (IL) -1β, IL-6, IL-8, Tumour necrosis factor (TNF) -α, Extracellular domain (ECD) Her2/neu, c-myc, Epidermal growth factor (EGFR), VCAM-1, E-selectin, Tumour growth factor (TGF) –β, Angiogenin, Carcinoembryonic antigen (CEA) and Carbohydrate antigen (CA) 15-3 were evaluated to determine the anti-angiogenic of this CT drug. Results and Discussion: We found a statistically signi¿cant correlation between CoRN supplementation and reduction in angiogenesis markers. There was a reduction in the levels of serum IL-1β, IL-6, IL-8, TNF-α, MMP-2, MMP-9, Angiogenin, E-selectin, VCAM-1 EGFR, TGF-β and VEGF levels, which are stimulators of angiogenesis as well as factors for cancer cell proliferation and growth. There was a signi¿cant reduction in tumour marker levels of CEA, CA15-3, ECD Her-2/neu and c-myc. In conclusion, this study suggests that supplementation of CoRN to tamoxifen therapy may provide good treatment prognosis by reducing the risk of cancer recurrence and metastases by decreasing the levels of angiogenic and tumour markers and importantly, the relation between dietary supplementation and cancer treatment may also have therapeutic implications in the future. 1105 Molecular imaging in the mouse model of breast cancer based on optical illumination and ultrasonic detection. Oraevsky AA, Ermilov SA, Eghtedari MA, Conjusteau A, Miller T, Radulescu EG, Herzog D, Gharieb RR, Lacewell R, Thompson S, Mehta K, Stein A, Motamedi M. Fairway Medical Technologies, Houston, TX; Seno Medical Instruments, Houston, TX; University of Texas Medical Branch, Galveston, TX BACKGROUND A three-dimensional laser optoacoustic imaging system was developed, which combines the advantages of optical spectroscopy and high resolution ultrasonic detection to produce high contrast maps of optical absorbance in tissues. The images were based on spatial distribution of desoxyhemoglobin and oxyhemoglobin, which are the main endogenous tissue chromophores in the red and near-infrared spectral ranges. Visualization of these chromophores provides structural information on tissue vasculature and functional information on blood concentration and oxygen saturation. S78 Abstracts – Poster Session I MATERIALS and METHODS The system was tested in a nude mouse model of breast cancer and produced deep tissue images with sub-millimeter resolution. Optoacoustic imaging using two or more illumination wavelengths permits a quantitative assessment of the angiogenesis-related microvasculature, and thereby, an evaluation of the tumor stage and its metastatic potential. The optoacoustic system was also used to generate molecular images of the malignancy-related receptors induced by the xenografts of BT474 mammary adenocarcinoma cells in nude mice. The acquisition of the latter images was facilitated by the use of an optoacoustic contrast agent that utilizes gold nanorods conjugated to monoclonal antibody raised against HER2/neu antigens. These nanorods possess a very strong optical absorption peak that can be tuned in the near-infrared by changing their aspect ratio. The effective conversion of the optical energy into heat by the gold nanorods followed by the thermal expansion of the surrounding water makes these nanoparticles an effective optoacoustic contrast agent. RESULTS Three-dimensional images of mouse circulation as well as breast tumors grown from xenografts of BT474 cells were obtained. Administration of the gold nanorod bioconjugates to mice resulted in an enhanced contrast of breast tumors relative the background of normal tissues in the nude mouse model. DISCUSSION In the presence of advanced tumor angiogenesis, the developed system can provide functional information on blood concentration and its oxygen saturation in the tumor microvasculature. In the absence of a suf¿cient endogenous contrast in certain types of tumors, the combination of the nanoparticulate contrast agent and the optoacoustic imaging has the potential to become a useful imaging modality for preclinical research in murine models of cancer. 1106 Variation of circulating angiogenic factor level and its potential value during chemotherapy in patients with metastatic breast cancer. Tang J, Zhao J, Qin J, Pan L, Xu Z. Jiangsu Tumor Hospital, Nanjing, Jiangsu, China; Nanjing University of Traditional Chinese Medicine, Nanjing, Jiangsu, China Background: Systemic chemotherapy is crucial for advanced or metastatic breast cancer. However, that is not well understood whether angiogenic factors from tumor and/or other tissue cells are inÀuenced by chemotherapy and whether the changes of their circulating levels add useful information to conventional tumor markers in monitoring breast cancer. This study aimed to investigate the changes in circulating vascular endothelial growth factor (VEGF) and endostatin (ES) levels during chemotherapy and to discuss their correlations with conventional tumor markers, therapeutic response and survival. Materials and Methods: 120 series serum samples form 40 patients with metastatic breast cancer were collected before chemotherapy (B0), at the end of 1 cycle (B1) and 5-6 cycle chemotherapy (B2). Serum VEGF or ES level was measured by ELISA, and serum CA153 or CEA level was determined by electrochemiluminescence immunoassay. The positive predictive values (PPV) of each marker and of marker combinations for different types of clinical response were calculated. Results: (1)The median levels of 496.6 (range, 62.5-1106.7), 524.8 (range, 69.0-1463.5) and 306.5 (range, 62.5-1004) pg/ml serum VEGF with the positive rates of 57.5%, 52.5% and 35.0% in B0, B1 and B2 samples were obtained, respectively. There was statistically signi¿cant difference between B1 and B0 (P=0.047) and between B2 and B0 or B1 (P<0.001). (2)ES medians in B0, B1 and B2 samples were 95.5 (range, 48.0-164.7), 110.5 (range, 52.0-179.9) and 113.3 (range, 62-208.0) ng/ml, respectively. Although there was an upward trend from B0 to B2, but no statistical difference was observed between different groups (P>0.05). (3)The changes in serum VEGF levels after 5 or 6 cycles of chemotherapy correlated with clinical response. VEGF level in 27 patients with partial response (PR) and stable disease (SD) showed a signi¿cant decrease (287.4 vs 501.2pg/ml; P<0.001), neither but in 13 patients with progressive disease (PD; 568.9 vs 493.9pg/ml;P=0.312). VEGF showed the highest PPV for SD (61.9%), and CA153 showed the highest PPV for both PR (42.9%) and PD (70.0%). Moreover, a combination of CA153 and VEGF could signi¿cantly increase the PPV for PD to 100% and the PPV for PR+SD to 81.3%. (4)Before treatment, serum VEGF levels correlated with increasing clinical stages and visceral involvement. After treatment, three of the 4 patients with both persistently high VEGF and CEA levels died of carcinoma within 2-year follow-up, which showed a worse outcome than that with VEGF or CEA elevated alone (75% vs 44.4% or 60%). Conclusion: Systemic chemotherapy for breast cancer results in a signi¿cant decrease of serum VEGF level, but has only minor effect on ES without statistical signi¿cance. The change in VEGF level may provide additional information to that obtained from CA153 or CEA in estimating the clinical response and predicting the prognosis. 1107 Association of genetic polymorphisms of VEGF and VEGFR-2 with outcome in E2100. Schneider B, Wang M, Radovich M, Sledge G, Badve S, Thor A, Flockhart D, Hancock B, Davidson N, Miller K. Indiana University School of Medicine, Indianapolis, IN; Harvard, Boston, MA; University of Colorado Health Sciences Center, Denver, CO; Johns Hopkins Sidney Kimmel Cancer Center, Baltimore, MD Background: E2100 was a phase III, Intergroup trial that demonstrated an improvement in progression free survival (PFS) and response rate (RR) when adding bevacizumab to paclitaxel for women with previously untreated metastatic breast cancer. There was also signi¿cantly more hypertension in women who received bevacizumab. To date no biomarkers have been identi¿ed to predict outcome with use of an anti-angiogenic agent. Genetic variability has the potential to predict differences in incidence of malignancy, prognosis, and altered metabolism of certain drugs. Several polymorphisms within the angiogenesis pathway have demonstrated capacity to discriminate biologic phenotypes for processes that rely on angiogenesis. The Vascular Endothelial Growth Factor (VEGF) -1498C allele has previously been associated with increased promoter activity and an increased risk of breast cancer. Methods: DNA was extracted from tumor blocks of 363 patients from E2100. Approximately 50% were from the control arm (paclitaxel) and 50% from the experimental arm (paclitaxel + bevacizumab). Genotyping was performed on VEGF (-2578C/A, -1498C/T, -1154 G/A, -634G/C, & 936C/T) and VEGF-Receptor 2 (VEGFR-2) (889G/A & 1416A/T) genes. Testing for correlations between each polymorphism with ef¿cacy (PFS and RR) and toxicity (grade 3/4 hypertension) was performed. Cox’s proportional hazards method and Fisher’s exact test were used to assess association. P-values were two sided. Testing for associations of polymorphisms with overall survival and expression (immunohistochemical assessment of VEGF and VEGFR2) is planned. Results: The -1498C and -634G alleles were associated with grade 3/4 hypertension in the experimental arm. Percentage of grade 3/4 hypertension for women who received bevacizumab by -1498 C/T genotype was: CC=33% (n=24), CT=27% (n=63), TT=10% (n=48) (p=0.03). Percentage in the -634G/C genotype was: GG=26% (n=51), GC=27% (n=64), CC=0% (n=19); (p=0.02). -1498 C/T and -634 G/C are in linkage disequilibrium. Signi¿cantly higher response rates were seen for patients with the VEGFR-2 889A allele: AA=100% (n=2), GA=57% (n=30), GG=37% (n=121) (p=0.02). No difference, however, was observed for PFS for this allele. A trend for inferior PFS for patients with VEGF 936TT genotype was observed (TT v.s CC+CT; HR=2.30(95% CI=0.93, 5.68), p=0.07) but there were only ¿ve patients with this genotype. Conclusion: Our data support an association between increased risk of grade 3/4 hypertension with the VEGF -1498C and the -634G alleles. Findings of an inferior PFS for those with the VEFG 936TT genotype are provocative but there were too few numbers to draw de¿nitive conclusions. These results should be re-evaluated in an independent data set. Abstracts – Poster Session I 1108 A novel assay to assess the antiangiogenic potential of cytotoxic drugs in human breast cancer. Lyons, III JM, Anthony CT, Woltering EA. Louisiana State University Health Science Center, New Orleans, LA Background: Trends in breast cancer management advocate individualizing therapy. Investigators often use tumors’ cellular proliferation or growth factor expression as a measure of drug ef¿cacy; however, there are no human, tumor-based assays available which evaluate a drug’s antiangiogenic potential. To develop such an assay, we hypothesized that fresh, surgically-harvested, human, malignant breast tumors would develop an angiogenic response in a ¿brin-thrombin clot, sprouting neovessels in a time-dependent fashion. We further speculated that treatment of tumors with standard antineoplastic drugs would inhibit the percent of tumor explants that developed invasion of neovessels into the ¿brin-thrombin clot. Materials and Methods: Fragments of freshly harvested human breast tumors were embedded in ¿brin-thrombin clots and treated with ¿ve cytotoxic agents commonly used in breast cancer: Adriamycin, Taxol, 5-FU, Methotrexate, and Vincristine (n=30 explants per treatment group). Tumor fragments were tested with a single dose of each reagent at or above its clinically achievable in vivo concentration. These experiments were repeated using four separate breast cancer specimens. The angiogenic response was visually assessed noting the angiogenic invasion into the clot (% I) and the extent of angiogenic growth (AI) using a previously validated scale. These data were then combined to give a mean overall angiogenic effect for each treatment group. Results: All four breast cancer specimens tested developed an angiogenic response sprouting neovessels in vitro in a time-dependent fashion (r = .81, p =.0008). Taxol statistically inhibited angiogenesis in all 4 tissues with a decrease in the mean angiogenic initiation, neovessel growth, and overall effect that were 76%, 66%, and 94% of control values, respectively. Vincristine also inhibited the overall angiogenic effect in all 4 tumors (mean decrease compared to control = 90%). Methotrexate increased mean angiogenic initiation, neovessel growth, and overall effect by 8%, 8%, and 14%, respectively. These results were not statistically signi¿cant. 5-FU inhibited angiogenesis in 3 of 4 breast cancers (mean decrease in overall effect compared to control = 78%), while Adriamycin inhibited angiogenesis in 2 of 4 tissues (mean decrease in overall effect compared to control = 60%). Discussion: Freshly harvested breast cancer specimens develop an angiogenic response in our assay system, and they respond to treatment with antineoplastic /antiangiogenic drugs. The antiangiogenic potential of commonly used breast cancer drugs varied among individual human breast malignancies. Data obtained from this model is unique and could potentially be used to further enhance the ef¿cacy of cytoxic regimens and further individualize patient therapy. 1109 Comparing serum levels of vascular endothelial growth factor in premenopausic women with breast cancer according to menstrual cycle phase. Rios Zaragoza S, Martinez Chequer J, Mainero Ratchelous F. Hospital “Luis Castelazo Ayala” IMSS, Mexico, DF, Mexico Background. Breast cancer (BC) is a serious and increasing health problem in Mexico. There are no available assays that compare serum levels of vascular endothelial growth factor (VEGF) in premenopausic women with BC undergoing surgical treatment. Hypoxia and steroid hormones (specially progesterone) among other factors, stimulate angiogenesis. This can be measured by determining serum levels of VEGF. Premenopausic women have hormonal level variations by effect of the ovulation process throughout their menstrual cycle (MC). Hence we considered the next question: what’s the effect of menstrual cycle phases on angiogenesis in breast cancer patients? Our objective was to evaluate serum concentrations of VEGF in premenopausic women with BC according to the phase of their MC. Material and methods. Two groups of patients were considered. The ¿rst group was for premenopausic women with BC in the proliferative phase (PP) of their MC prior to the surgery date. The second group was for those in the secretory phase (SP). They were ¿rst divided by means of their last menstrual period date (LMP) obtained by direct questioning S79 and afterwards hormonal levels for each patient were compared with the LMP in order to con¿rm that each patient belonged to the correct group. Blood samples were drawn from all patients and processed the day before and the day after the surgery. Luteinizing hormone, follicle-stimulating hormone, estrogen, progesterone and VEGF serum levels were measured to these samples via quimioluminiscence and ELISA (using Quantikine© human VEGF immunoassay). Results were compared between both groups. Once the statistical analysis was completed it resulted as follows. Results. After comparing hormonal status and LMP for each patient, both groups of study were established: the PP group (n=24) and the SP group (n=42) Mean age was 40.6 years. The mean concentration of VEGF for patients in PP was of 239,16 pg/ml (SD 107,05 pg/ml) whereas for the group of patients in SP was of 600,72 pg/ml (SD 297,06 pg/ml) the variance analysis revealed that VEGF concentrations were signi¿cantly higher for the group of patients in secretory phase that in those of the group in proliferative phase (p = 0.001) A subgroup variance analysis of histological type, number of axillary lymph nodes and clinical stage showed similar results. Conclusions & discussion. With these results, a precedent is set concerning the impact of hormonal status in premenopausic patients with BC as an angiogenesis-stimulating inÀuence particularly during the SP of the MC. This study continues in order to gather additional information on the inÀuence of surgical timing; surgical and hormonal impact of these results combined and follow-up along with survival rates in these patients. 1110 Nuclear FoxO3a expression is associated with lymph node negative, ER+ invasive ductal carcinomas. Turashvili G, Fridman E, Romanska H, Lam E, Skarda J, Murray P, Kolar Z, Lalani E-N. Institute of Pathology, University Olomouc, Palacky, Czech Republic; Tel Aviv University, Chaim Sheba Medical Center and Sackler School of Medicine, Tel Aviv, Israel; Division of Cancer Studies, University of Birmingham, Birmingham, United Kingdom; Imperial College, London, United Kingdom INTRODUCTION. The FoxO (Forkhead bOX-containing protein, O subfamily) family of transcription factors have been implicated in a number of processes including tumour suppression, promoting apoptotic cell death and protecting cells from DNA damage and oxidative stress. The activity of FoxOs is primarily controlled via the phosphoinositide3-kinase-protein-kinase-B (PI3K-PKB/c-Akt) pathway. Recent evidence suggests that deregulation of FoxOs may occur in a variety of tumors including breast cancers. AIM: The aims of our study were to: a. assess the pattern of protein expression of FoxO3a; and b. determine if there was any association between pattern of FoxO3a expression with grade, stage, oestrogen (ER), progesterone (ER) and c-erbB2 receptor expression, in invasive ductal breast carcinomas (IDCs). MATERIAL AND METHODS. We constructed a tissue microarray from 80 IDCs. TMA sections were stained using standard immunohistochemical methods and expression analysis of FoxO3a, ER, PR and c-erbB-2 was undertaken utilizing commercially available monoclonal and polyclonal antibodies. RESULTS. 78.8% (63/80) of the IDCs expressed FoxO3a. Two predominant subcellular localisation patterns of FoxO3a were observed: a. Cytoplasmic in 24/63 (38%) samples and b. nuclear-cytoplasmic in 39/63 (62%) samples The majority of cases with nuclear-cytoplasmic pattern 87% (34/39) were lymph node negative. The converse (only 37.5%, 9/24) was observed in cases with the cytoplasmic expression only. c-erb2 was ampli¿ed in 50% of the cases in which cytoplasmic FoxO3a expression was seen but in none of the cases with nuclearcytoplasmic expression. The pattern of FoxO3a expression was associated with ER+ status but not histological grade or PR status. CONCLUSION. The in vivo FoxO3a pattern of expression appears to relate to its function and biological behaviour of IDC. The functional link with c-erbB2 ampli¿cation remains to be elucidated. S80 Abstracts – Poster Session I 1111 Labeling pattern of breast cancer stem phenotype in invasive breast carcinomas: an immunohistochemical analysis. Shaye AN, Sahin AA, Huo L, Woodward WA. UT M.D. Anderson Cancer Center, Houston, TX Background: The epithelial component of breast parenchyma is thought to arise from a stem cell which is capable of pluripotent differentiation and self-renewal. Breast carcinomas are thought to originate from these stem cells or their immediate progeny. The identi¿cation of these stem cells and their further characterization have important implications for the understanding of carcinogenesis and may suggest new approaches for the treatment and prevention of breast cancer. Results of Àow cytometric studies suggest that breast cancer stem cells are characterized by a CD44+/CD24- phenotype. The purpose of this study was to evaluate the distribution of CD44+/CD24- phenotype cells in invasive breast carcinoma and adjacent non-neoplastic breast parenchyma using immunohistochemistry (IHC). Materials and Methods: Serial sections from archival paraf¿n-embedded tissue blocks from 33 invasive primary breast carcinomas were analyzed using IHC for CD44 (Novocastra; Boston, MA) and CD24 (Neomarkers; Freemont, CA). Positive tumor cell staining was de¿ned as circumferential membrane labeling for CD44 and as cytoplasmic labeling for CD24. The number of tumor cells expressing CD44 and CD24 was assessed by light microscopy and grouped into the following categories for both invasive carcinoma and carcinoma in-situ: <5%, 5-50% and >50% labeling. Results: Both invasive and in situ carcinomas showed varying expression and distribution patterns of CD44 and CD24 labeling. Labeling percentages for both markers in invasive and in situ carcinoma components are shown in Table 1. Benign stromal cells and myoepithelial cells also stained positively for CD44 in >80% of cases where it was present in the tissue section. CD24 positivity was identi¿ed in a similar proportion of cases, and was con¿ned to luminal cells. Discussion: In the majority of the invasive carcinomas, <50% of cells showed immunohistochemical labeling for CD44; whereas, CD24 labeling was more diffuse. There was no consistent pattern of distribution of CD44 positive cells in invasive carcinoma. Similarly, the staining pattern of invasive and in-situ carcinoma components were not always concordant. There was no pronounced difference in labeling of invasive or in-situ carcinoma for CD24. The higher proportion of positive labeling tumor cells for CD44 using immunohistochemistry compared to previously reported Àow cytometric studies suggests that immunohistochemistry may lack speci¿city in the identi¿cation of breast cancer stem cells. Further studies are required in order to evaluate the utility of immunohistochemistry in the identi¿cation of tumor cells which express the breast cancer stem cell phenotype, CD44+/CD24-. Additional markers need to be investigated. Labeling Percentages Invasive Carcinoma (n=33) <5% 5-50% >50% CD 44 13 13 7 CD 24 9 10 14 In-situ Carcinoma (n=13) <5% 5-50% >50% 4 2 7 2 2 9 1112 Differential proteomic pro¿les observed in FFPE breast tissue specimens of several pathologic states. Izbicka E, Streeper R, West FB, Yeh I-T. CTRC, San Antonio, TX; UTHSCSA, San Antonio, TX Background: Proteomic analysis of tissue specimens allows for the characterization of protein expression pro¿les that reÀect the altered physiologic state of cells present in pathology tissue specimens. The differences observed may serve to guide the identi¿cation of pathognomonic protein expression patterns that will facilitate the early detection of pathologic transformations with high speci¿city and sensitivity. Formalin ¿xed paraf¿n embedding is the storage method of choice for diagnostic specimens in pathology departments. We undertook this study determine the identities of differentially expressed protein species in FFPE specimens from various pathological states of breast tissue Materials and Methods: We examined FFPE archival breast tissue specimens including normal (n = 23), ¿broadenomas (n = 21), node negative (n = 25) and node positive (n = 22) breast cancers. Ten micron sections were microdissected, de-paraf¿nized and digested with trypsin. Digests were then analyzed by liquid chromatography electrospray ionization mass spectrometry (LC-ESIMSMS) Differential analysis of the resulting mass spectral data allowed for the identi¿cation of differentially expressed mass/time signals which were then subjected to both on line and off line mass spectrometry-mass spectrometry (MSMS) analysis for the determination of peptide sequence. The data were analyzed and putative protein identi¿cations were made using the Mascot protein mass spectral database search software. Clinical data including histological subtype, estrogen and progesterone receptor status, HER2 status, p53 and Ki-67 status were also evaluated in the breast cancer specimens. Results: MS analyses of FFPE tissue digests allowed the identi¿cation of a number of proteins and classes of proteins that are differentially expressed in the examined pathologic states relative to the levels observed in the analyses of normal tissue samples. We have observed that a number of proteins are either over or under expressed in the examined specimens. Notable is the relative dearth of peptide signals observed in the breast cancer specimens, both node negative and node positive. Identi¿ed classes include types of intra-cellular structural proteins, proteins involved in energy metabolism, transcriptional regulation and intra and inter cellular signaling pathway related species. Discussion: These results of our examination of the proteomic pro¿les of FFPE breast tissues show a number of signi¿cant differences between normal and tumor tissues. The physiological implications of the observed differences suggest a number of lines of inquiry for future studies. The results are to a degree confounded by factors including variability in tryptic digestion ef¿ciency due to gross structural differences, differing degrees of formalin mediated crosslinking within the specimens or basic proteomic changes characteristic of malignant tissues. 1113 Insulin-like growth factor I activates gene transcription programs strongly associated with ER – breast cancer and poor patient prognosis. Creighton CJ, Casa A, Lazard ZW, Tsimelzon A, Hilsenbeck SG, Lee AV. Baylor College of Medicine, Houston, TX Background: Substantial evidence implicates insulin-like growth factor I (IGF-I) signaling in the development and progression of breast cancer. To identify transcriptional targets of IGF action, we performed gene expression pro¿ling (>22,000 RNA transcripts) of IGF-I-stimulated MCF-7 cells, a well characterized breast cancer cell line highly responsive to IGFs. Materials and Methods: We de¿ned an IGF-I gene signature pattern of hundreds of genes either up- or down-regulated at both 3 and 24 hrs in vitro. After removing genes considered generic to cell proliferation, the signature was examined in various public pro¿le datasets of human breast tumors, as well as in pro¿le datasets of experimental models for various oncogenic signaling pathways. Results: Genes with early and sustained regulation by IGF-I were highly enriched for transcriptional targets of the estrogen, Ras, and PI3K/Akt/ mTOR pathways. The IGF-I signature appeared activated in most ERhuman breast tumors and in a substantial subset (∼25%) of ER+ breast tumors. Patients with tumors showing activation of the IGF-I signature tended to have a shorter time to disease recurrence (including patients not receiving adjuvant therapy), both when considering all patients and the subset of ER+ patients. Discussion: We found evidence for cross-talk and common transcriptional endpoints between the IGF-I and estrogen systems. Our results support the idea that the IGF-I pathway is one mechanism by which breast tumors may acquire hormone independence and a more aggressive phenotype. Abstracts – Poster Session I Multivariate Cox analysis of tumor characteristics and IGF gene signature in relation to the likelihood of distant recurrence. van de Vijver dataset Wang dataset Miller dataset Variable P-value 95% CI HR P-value 95% CI HR P-value 95% CI HR Age 0.37 0.43-1.38 --0.38 0.36-1.50 Tumor size 0.05 1.00-2.38 --0.004 1.38-5.78 Grade 0.26 0.86-1.72 --0.76 0.54-1.58 LN 0.19 0.50-1.15 --<0.001 1.66-5.54 ER status 0.31 0.61-4.47 0.62 0.60-2.34 0.32 0.57-5.46 ER mRNA 0.78 0.68-1.65 0.04 1.01-1.89 0.24 0.83-2.01 PR mRNA 0.02 0.58-0.96 <0.001 0.56-0.87 0.54 0.64-1.27 HER2 mRNA 0.21 0.93-1.35 0.69 0.79-1.17 0.08 0.97-1.65 IGF signature <0.001 1.36-2.53 0.004 1.12-1.82 0.006 1.17-2.79 Age, size, LN, and ER-status were binary variables (0 for age<50y and 1 for age>=50, 0 for dia<=2cm and 1 for dia>2cm, 0 for LN- and 1 for LN+, and 0 for ER- and 1 for ER+, respectively). Grade was binned as 1, 2, and 3, for low, medium, and high, respectively. ER mRNA, PR mRNA, HER2 mRNA, and the IGF gene signature coef¿cient were each transformed to SD from the mean. 1114 HER-1 overexpression is found only in oestrogen receptor negative breast cancer and is rarely associated with +(5 gene ampli¿cation. Pintens S, Vanden Bempt I, Drijkoningen M, Van Belle V, Brouckaert O, Christiaens M-R, Neven P, De Wolf-Peeters C. UZ Leuven, Leuven, Belgium; ESAT, Leuven, Belgium Background and Aims: Recently, it has been hypothesized that HER-1 overexpression plays a role in triple ER-/PR-/HER-2- negative breast carcinomas. As HER-1 might be a target for therapy, we investigated the HER-1 status in triple negative compared to grade-matched nontriple negative breast carcinomas. Materials and methods: In total, 57 high-grade breast carcinomas were studied: 25 triple negative cases and 32 grade-matched controls with variable ER/PR/HER-2 phenotypes. For all cases, formalin-¿xed paraf¿n-embedded material was available. HER-1 expression was examined by immunohistochemistry (IHC) using the standardized PharmDx kit (Dakocytomation). Cases with membrane staining in more than 10% of invasive tumour cells were regarded as showing HER-1 overexpression. HER-1 gene copy number was determined by Fluorescence in situ Hybridisation (FISH) using a probe for HER-1 and a control probe for chromosome 7, on which HER-1 is located (Vysis). A mean ratio of HER-1 gene to chromosome 7 copy number greater than 2 was considered to be HER-1 gene ampli¿cation. Results: Overall, HER-1 overexpression was found in 20 out of 57 (35.1%) high-grade breast carcinomas, all of them being ER negative. Out of the 25 triple negative cases, 13 showed HER-1 overexpression (52.0%). HER-1 gene ampli¿cation was found in 5 cases (8,8 %) and was always associated with HER-1 overexpression. Of note, HER-1 gene ampli¿cation was a generalized event, as it was found in more than 90% of the tumours cells in all 5 cases. By contrast, HER-1 expression was more variable throughout the tumour. Still, 3 out of 5 HER-1 ampli¿ed cases also showed generalized HER-1 overexpression. Interpretation and Conclusion: HER-1 overexpression was restricted to ER-negative breast carcinomas, half of which were triple negative. HER-1 overexpression was accompanied by HER-1 gene ampli¿cation in only a minority of the cases. Therefore, HER-1 gene ampli¿cation is unlikely to be a driving mechanism for HER-1 overexpression. Nevertheless, it might delineate a particular subgroup of ER-negative breast carcinomas that might benefit from therapy with HER-1 inhibitors. 1115 Effectiveness of RAD001 (everolimus) in combination with endocrine therapy varies with cell phenotype. Farmer I, Pancholi S, Thornhill A, Evans DB, Lane HA, Dowsett M, Martin L-A. Institute of Cancer Research, London, United Kingdom; Novartis Institute for BioMedical Research-Basel, Basel, Switzerland Background: Cross-talk between Receptor Tyrosine Kinase (RTK) and ER signal transduction pathways appears to contribute to endocrineresistance leading to elevations in phosphorylated ERK1/2 and AKT. Based on this evidence, one strategy to improve the ef¿cacy of current endocrine agents as well as delaying the onset of resistance is to target the ER and pertinent signal transduction pathways concomitantly. An S81 obvious choice is mTOR (a down-stream member of the PI kinase family), which regulates cell cycle progression, by enhancing translation initiation and/or the stability of cell cycle regulatory proteins such as D-type cyclins. In the following study we investigated the use of RAD001 (everolimus), a speci¿c inhibitor of mTOR in combination with tamoxifen or letrozole on a panel of human breast cancer cell lines modelling endocrine-sensitive and -resistant disease. Materials and Methods: Human breast cancer cell lines with varying expression levels of ER and HER2 [MCF7 (ER+HER2-), BT474 (ER+, HER2++) and SKBR3 (ER-, HER2++)] were engineered to express aromatase. The effect of RAD001 ± tamoxifen or letrozole was assessed in proliferation and ER alpha-mediated transcription assays. Immunoblotting was used to monitor the effect of RAD001 on mTOR signalling and cell cycle. Xenograft studies with MCF7-AROM1 cells and BT474-AROM3 were carried out to compare RAD001 in combination with endocrine therapy. Results: Treatment of the target cell lines with increasing concentrations of RAD001 resulted in a concentration-dependent decrease in proliferation regardless of the cells ER/HER2 status. A concomitant reduction in phosphorylated p70 S6 kinase and S6 coupled with an increase in phosphorylated AKT was also noted. RAD001 in combination with either tamoxifen or letrozole enhanced the antiproliferative effect compared to either monotherapy in the ER+ cell lines. This was associated with an increase in the number of cells in G1 phase compared to the monotherapies. Of note the combination of RAD001 with letrozole or tamoxifen enhanced nuclear accumulation of p27 and increased p27 phosphorylated at Ser10. There was also a marked decrease in cyclin D1 and enhanced phosphorylation of Rb compared to cells treated with the endocrine agents alone. MCF7AROM1 xenografts were growth-suppressed with letrozole, tamoxifen or RAD001 when used alone as compared to the vehicle-treated control. However, whilst tamoxifen in combination with RAD001 provided no added bene¿t compared with either agent alone, letrozole plus RAD001 resulted in the greatest reduction in tumor volume. Strikingly, treatment of BT474-AROM3 xenografts, showed that RAD001 alone was equally effective at reducing tumor volume as the combination therapies. Conclusion: These data suggest that the tumor phenotype markedly affects the response to the combination of RAD001 with endocrine therapy, and may predict the effectiveness of the combination clinically for the treatment of breast cancer. 1116 Combination therapy with tetramethoxystilbene and phosphatidylinositol 3-kinase inhibitor is effective for killing hormone-resistant breast cancer. Park H, Aiyar SE, Kim S, Lee Y, Fan P, Santen RJ. Kyungpook National University Hospital, Daegu, Republic of Korea; University of Virginia, Charlottesville, VA; Seoul National University, Seoul, Republic of Korea Background: Treatment of hormone-dependent breast cancer with tamoxifen, faslodex and aromatase inhibitors can initially lead to tumor regression but relapses usually occur after 12-18 months on average. Resistance to these inhibitors occurs in part because of up-regulation of growth factor pathways. Abrogation of these pathways with inhibitors of MAP kinase, PI-3-kinase, mTOR EGF-R, IGF-R and HER-2 have been used, but are not completely effective for preventing and treating resistance. Targeted therapies also are not suf¿cient to control metastatic breast cancer. Therefore, combination therapy has been suggested as an alternative strategy. We have discovered that TMS (2,3’,4, 5’tetramethoxystilbene), a derivative of an herbal compound, modulates microtubule polymerization and results in death of breast cancer cell lines. TMS inhibited phosphorylation of focal adhesion kinase (FAK), Akt, and mammalian target of rapamycin (mTOR), while stimulating c-Jun N-terminal kinase (JNK) activity. We propose that TMS can be used in combination with other inhibitors to induce potent cell death while minimizing toxicity. Methods: The following MCF7 ER (+) cell lines were used: parental, tamoxifen resistant (TamR), long term estrogen deprived (LTED) and ICI resistant (ICI-R). We examined TMS in the absence and presence of the following inhibitors (PI3K, mTOR, MAPK, AKT, EGFR and IGFR) S82 Abstracts – Poster Session I for both cell growth analysis and apoptosis measurements Results: Treatment of MCF7 cells with TMS alone reduced MCF7 cell counts by 70%. When used in combination with the PI3K inhibitor, the cell counts were further reduced by 80% over PI3K inhibitor alone (p=.00000117). Combination treatment increased apoptosis 1.7 fold over TMS alone (p=.000218). In addition, E2 does not change the apoptotic effect of TMS. The PI3K inhibitor was also the most effective compound ( i.e 60% reduction in cell number ) in the hormone-resistant cell line TamR. The combination of the PI3K inhibitor and TMS is highly effective for decreasing the TMA R cell number. LTED cells were most effectively killed by either a combination of TMS + Estradiol or a combination of TMS + PI3K inhibitor. Immunoblot analysis demonstrated that PARP is cleaved by single treatment with either TMS or PI3K, while the combination of the two resulted in increased cleavage. PARP cleavage can be blocked in the presence of zVAD. Conclusion: TMS, when used in combination with another inhibitor, reduced cell counts and increased apoptosis. Therefore, we suggest that combination therapy with TMS may be an effective way to control ER(+) hormone-resistant breast cancer. 1117 Inhibition of breast cancer growth with the combination of lapatinib and an ADAM protease inhibitor. Witters LM, Scherle PA, Friedman SM, Redman J, Fridman JS, Caulder E, Lipton A. Pennsylvania State University College of Medicine, Hershey, PA; Incyte Corporation, Wilmington, DE The ErbB family of receptors, ErbB1 (EGFR) and ErbB2 (HER-2/ neu), has been shown to play a signi¿cant role in the proliferation of human tumors. Many breast tumors overexpress these receptors and this correlates with poor prognosis and resistance to therapy. These receptors, when triggered by the binding of appropriate ligands, activate multiple cellular downstream pathways that in turn lead to tumor growth and survival. Although inhibitors of the ErbB family of receptors, e.g., Herceptin, have demonstrated clinical ef¿cacy in several solid tumors, not all HER-2/neu positive tumors respond and many that respond initially develop resistance, presenting the need for alternative therapies. Proteolytic cleavage of both ErbB ligands and receptors has been shown to be a critical event resulting in pathway activation. This cleavage is necessary for the generation of soluble, functionally active forms of the ligands and in the case of HER-2/neu, results in a shed extracellular domain (ECD) and a membrane bound fragment (p95) containing a kinase domain with signi¿cant constitutive activity. Importantly, the presence of elevated HER-2/neu ECD in the sera of cancer patients has been linked to poor response rates. Both ErbB ligand and HER2/neu cleavage have been shown to be mediated by the ADAM (a distintegrin and metalloproteinase) family of zinc-dependent proteases. We ¿rst examined the effect of combining a dual kinase inhibitor of EGFR and HER-2/neu similar to lapatinib (GW2974) with an ADAM protease inhibitor (INCB3619: Incyte Corp.) on the growth of MCF-7 and HER-2/neu-transfected MCF-7 cells. Exposure to INCB3619 (10 - 40 µM) produced minimal growth inhibition as a single agent in the HER-2/neu-transfected MCF-7 cells (0-14% inhibition) and MCF-7 cells (22-38% inhibition). Addition of the EGFR/HER-2/neu inhibitor (GW2974) resulted in a synergistic inhibitory effect in both cell lines. Lower concentrations of INCB3619 (0.25 – 1 µM) (doses found to be clinically achievable with the equipotent ADAM inhibitor, INCB7839, currently in clinical trials) were also tested in the HER-2/neu-transfected cells and produced synergistic growth inhibition when combined with GW2974. Three days exposure to 10 µM INCB3619 signi¿cantly reduced the amount of shed HER-2/neu ectodomain into the supernatant of treated cells as measured by a HER-2/neu ectodomain speci¿c ELISA (Oncogene Science). Combination of the clinical candidate ADAM inhibitor, INCB7839, with lapatinib prevented tumor growth in the BT474-SC1 human breast cancer xenograft model. These results suggest that combining an ADAM inhibitor with kinase inhibitors of the ErbB family may provide an improved result in the treatment of metastatic breast cancer. 1118 X3$5 gene ampli¿cation in breast cancer tissue: a rare event. Pintens S, Vanden Bempt I, Drijkoningen M, Van Belle V, Brouckaert O, Christiaens M-R, Neven P, Peeters C. UZ Leuven, Leuven, Belgium; ESAT KULeuven, Leuven, Belgium Introduction: Overexpression of the urokinase Plasminogen Activator Receptor (uPAR) has been associated with increased metastatic potential and adverse prognosis in breast cancer. Recently, uPAR overexpression has been associated with uPAR gene ampli¿cation on chromosome 19q13 and was frequently found together with HER-2 gene ampli¿cation in isolated breast cancer cells. Aims: We aimed to investigate the uPAR gene status in tissue sections of breast cancer and to study its relation to the HER-2 gene status. Materials and Methods: In total, we studied 57 high-grade primary invasive breast carcinomas for which formalin-¿xed paraf¿n-embedded material was available. The HER-2 and uPAR gene status were determined by Fluorescence in situ Hybridisation (FISH) analysis. For HER-2, a dual-probe kit was used including a probe for HER-2 and a control probe for chromosome 17 (PathVysion, Vysis): a HER-2/ chromosome 17 ratio greater than 2 was considered ampli¿ed for HER2. For uPAR, we used a dual-probe kit including a probe for uPAR and a control probe for the opposite arm of chromosome 19 (19p13). A ratio of uPAR/19p13 greater than 2 was considered ampli¿ed for uPAR. Results: Out of 57 cases, 25 were ampli¿ed for HER-2. Only 1 of these cases showed concurrent ampli¿cation of the uPAR gene (1/25, 4.0%). Thereby, the mean uPAR gene copy number was 10 compared to 20 for HER-2. No uPAR gene ampli¿cation was found in non-HER-2 ampli¿ed breast carcinomas. While uPAR gene ampli¿cation was rare, we frequently observed aneuploidy of chromosome 19 (35/57, 61.40%): 34 cases showed polysomy 19 and one case monosomy 19. Interpretation and Conclusion: FISH analysis on tissue sections indicates that uPAR gene ampli¿cation is extremely rare in breast cancer. Whereas related to HER-2 gene ampli¿cation, it is unlikely to play an important role in the pathogenesis of breast cancer. 1119 Targeting of mTOR is associated with decreased VEGF expression and secretion in cancer cells. Lackner EM, Krauth MT, Kondo R, Rebuzzi L, Eigenberger K, Vales A, Kornek GV, Zielinski CC, Valent P. Medical University Vienna, Internal Medicine I, Division of Oncology, Vienna, Vienna, Austria; Medical University Vienna, Internal Medicine I, Division of Hematology and Hemostaseology, Vienna, Vienna, Austria; Clinic for Int. Medicine and Infectious Disease, Vienna, Vienna, Austria; Hanusch Krankenhaus, Vienna, Vienna, Austria Background: Cancer progression and metastasis are often associated with increased angiogenesis and with the formation of malignant effusions. Vascular endothelial growth factor (VEGF) is a major regulator of angiogenesis, vascular permeability, and cell survival. We examined the production and secretion of VEGF in various cancer cell lines and primary tumor cells, and examined the regulation of synthesis/secretion of VEGF in tumor cells. Methods&Results: As assessed by ELISA, the VEGF protein was detected in supernatants of cell lines derived from breast cancer (MDA-MB231), pancreatic carcinoma (BxPC-3), lung cancer (A-427), colon carcinoma (HCT8), and cholangiocellular carcinoma (EGI-1). In addition, VEGF was detected in supernatants of primary tumor cells obtained from malignant effusions in various malignancies (breast cancer, n=5; pancreatic cancer, n=1; ovarial cancer, n=1; parotic carcinoma, n=1; esophageal carcinoma n=1). In each case, the VEGF protein was detectable in neoplastic cells by immunocytochemistry, and was found to accumulate in supernatants of cultured tumor cells over time, suggesting constant production and secretion. Correspondingly, as assessed by RT-PCR, primary tumor cells as well as the cell lines tested were found to express VEGF mRNA in a constitutive manner. Since mTOR is a well known regulator of VEGF synthesis, we applied rapamycin on neoplastic cells. Rapamycin (20-200 nM) was found to counteract the production and secretion of VEGF in all tumor cells tested (VEGF in supernatants in cultures supplemented with rapamycin at 100 Abstracts – Poster Session I nM on day 6: MDA-MB231: 11.8±0.2%; BxPC-3: 23.6±18.8%; A-427: 30.1±3.4%; HCT8 17.2±0.5%; EGI-1 28.4±1.1%; p<0.05). Neither rapamycin nor VEGF were found to modulate growth of primary tumor cells or tumor cell lines. Conclusions: Various human tumor cells express and secrete VEGF. The production of VEGF in tumor cells is mediated through mTOR. These observations may have implications for the design of new treatment approaches attempting to counteract VEGF production/ secretion and effusion-formation in solid tumors. S83 S84 Abstracts – Poster Session II 2001 Elevated serum TIMP-1/HER-2 predicts decreased response and survival in metastatic breast cancer. Lipton A, Leitzel K, Chaudri-Ross HA, Evans DB, Ali SM, Demers L, Hamer P, Brown-Shimer S, Pierce K, Guar V, Carney W. Penn State University/Hershey Medical Center, Hershey, PA; Novartis Pharma AG, Basel, Switzerland; Novartis Institutes for BioMedical Research Basel, Basel, Switzerland; Penn State/Hershey Medical Center; Lebanon VAMC, Lebanon, PA; Oncogene Science Biomarker Group/Siemens Medical Solutions Diagnostics, Cambridge, MA Background: Tissue inhibitor of metalloproteinase-1 (TIMP-1) has been shown to have diverse multifunctional roles in tumorigenesis such as inhibition of the catalytic activity of MMPs, growth promotion, inhibition of apoptosis and regulation of angiogenesis. Increased TIMP1 has been associated with an unfavorable prognosis in many cancers including lymphomas, colorectal, gastric, head and neck, and lung cancer. We have previously reported in separate analyses that elevated pre-treatment serum TIMP-1 or HER-2 individually predict decreased response to 1st-line hormone therapy and reduced survival in patients receiving 1st-line hormone therapy. Materials and Methods: Pre-treatment serum TIMP-1 and HER-2 levels were determined from 522 patients enrolled in a phase III 1st-line hormone therapy trial comparing letrozole vs. tamoxifen (H Mouridsen et al, J Clin Oncol; 19(10):2596-2606, 2001) and from post-menopausal control females using the TIMP-1 and HER-2 ELISAs from Oncogene Science Biomarker Group/Siemens Medical Solutions Diagnostics, Cambridge, MA. Results: The serum TIMP-1 levels from the post-menopausal control group (n = 49) had a mean + SD of 315 + 117 ng/ml (range 175940 ng/ml). The upper limit of normal (ULN) was de¿ned as the 95 percentile (non-parametric method) of the control group (454 ng/ml). Serum TIMP-1 values were elevated above this ULN in 120/522 patients (23 %). Serum HER-2 values were elevated above the ULN of the control group (15 ng/ml, mean + 2SD) in 152/522 patients (29.1 %). In combined analysis for time to progression (TTP), patients with elevated TIMP-1/normal HER-2 levels had signi¿cantly decreased TTP (median 5.7 mo.) compared to patients with normal TIMP-1 and HER-2 levels (median 11.6 mo., p<0.0001). Within treatment arms, TTP was signi¿cantly longer for letrozole compared to tamoxifen in biomarker subgroups with normal HER-2 expression regardless of TIMP-1 levels, but there was no signi¿cant difference between treatments in subgroups with elevated HER-2. For overall survival, elevated vs. normal TIMP1 levels identi¿ed patients with signi¿cantly shorter survival in both normal HER-2 (median 26 vs. 42 mo., p= 0.0006) and elevated HER-2 (15 vs. 25 mo., p= 0.012) patient subgroups. Conclusion: Combined serum biomarker analysis of both TIMP-1 and HER-2/neu confers additional ability to predict subgroups of patients with signi¿cantly different clinical outcomes to hormone therapy as compared to using either biomarker alone. These data suggest that patients with elevated pre-treatment serum TIMP-1 and/or HER-2/neu levels may require additional targeted therapies together with endocrine therapy. 2002 Plasminogen activator inhibitor-1 and tissue inhibitor of metalloproteinases-1 are additive in predicting response to chemotherapy in metastatic breast cancer. Schrohl Rasmussen A-S, Meijer-van Gelder ME, Holten-Andersen MN, Christensen IJ, Look MP, Mouridsen HT, Foekens JA, Brünner N. University of Copenhagen, Faculty of Life Sciences, Copenhagen, Denmark; Erasmus MC, Josephine Nefkens Institute, Rotterdam, Netherlands; Hvidovre Hospital, Hvidovre, Denmark; Rigshospitalet, Copenhagen, Denmark Background: Predictive markers are urgently needed in breast cancer. Here, we analyzed the predictive value of tumor tissue levels of Plasminogen Activator Inhibitor-1 (PAI-1), which is an established strong prognostic marker in breast cancer patients. Tumor levels of Tissue Inhibitor of Metalloproteinases-1 (TIMP-1) has previously been determined in this patient group (Schrohl et al. 2006) and we combined the present ¿ndings on PAI-1 with data showing that high tumor tissue levels of TIMP-1 are associated with a poor response to chemotherapy. Materials and methods: The concentration of PAI-1 was measured by ELISA in cytosolic extracts of primary tumors from 174 patients who all developed metastatic breast cancer. Response to chemotherapy for metastatic disease (cyclophosphamide-adriamycin/epirubicin-5Àuorouracil (CAF/CEF) or single-agent adriamycin) was evaluated and it was analyzed whether this was related to tumor tissue PAI-1 levels. In addition, we investigated whether PAI-1 and TIMP-1 could be combined for prediction of response to chemotherapy. Results: In a test for trend, PAI-1 was not signi¿cantly associated with response rate. However, it was possible to identify a cut point that when used allowed us to identify two groups with signi¿cantly different response rates. The group with high tumor tissue PAI-1 levels consisted of 25 patients of which only two responded to chemotherapy (8%). In the remaining group (149 patients), having low tumor tissue PAI-1 levels, 62 patients responded to chemotherapy (42%). Combining these results with our previous ¿ndings on TIMP-1 we divided patients into a group having low tumor tissue levels of both markers and a group having high levels of one or both markers. This resulted in two patient groups; one group with low marker levels (142 patients) with a response rate of 44% and one group (32 patients) with a high level of one or both markers and with a response rate of 6% (p<0.001). In total, 110 patients were non-responders and by using PAI-1 and TIMP1 we were able to identify 30 of these (27%), at the same time only misclassifying 2 patients. Conclusions: In the present study, by measuring tumor tissue PAI-1 and TIMP-1, we were able to identify 27% of all non-responders. In the group having high levels of tumor tissue TIMP-1 and PAI-1 or both markers, the response rate was 6% compared with a response rate of 44% in the remaining patient group (low levels of both markers). Thus, this study generates the hypothesis that patients having high tumor tissue levels of PAI-1, TIMP-1 or both markers should not be offered chemotherapy with CMF and/or anthracycline-containing regimens but should rather be offered an alternative treatment. 2003 17ß-hydroxysteroid dehydrogenase type 1 is a predictive factor in premenopausal hormone receptor positive breast cancer treated with tamoxifen. Kallstrom A-C, Salme R, Ryden L, Gunnarsson C, Nordenskjold B, Stal O. Helsingborg Hospital, Helsingborg, Sweden; University Hospital, Linkoping, Sweden; University Hospital, Lund, Sweden Background: 17ß-hydroxysteroid dehydrogenase (17HSD) are enzymes involved in the local regulation of sex steroids. 17HSD type 1 enzyme converts the weak estrone (E1) to the more potent estradiol (E2) and 17HSD type 2 carries out the reverse reaction (E2 to E1). The expression of these enzymes in breast cancer differs from that in the normal mammary glad. Altered expression levels of these enzymes can be responsible for the modulation of growth as well as responsiveness to endocrine treatment. The aim was to investigate the levels of these enzymes in premenopausal breast cancers and to determine if they have any prognostic or predictive value. Material and Methods: 564 premenopausal patients with invasive breast cancer, stage II (UICC) were randomized to receive either 2 years of adjuvant tamoxifen (n=276) or no tamoxifen (n=288). Only nine patients received adjuvant chemotherapy. The median period of follow-up was 16 years and data were available for all patients. 396 of the 564 tumors were available for analysis of 17HSD-1 and 373 tumors for 17HSD-2. The analysis was done with immunohistochemistry using tissue micro array from paraf¿n-embedded breast cancer. The enzyme expression level was determined on a scale ranging from low (-/+/++) to high (+++). Estrogen and progesterone receptors content were measured in cytosols and with immunohistochemistry. Results: Patients with hormone receptor positive tumors with lower levels (-/+/++) of 17HSD type 1 showed a 43% reduced risk of recurrence when treated with tamoxifen, HR=0.57 (CI 0.37-0.87). This was statistically signi¿cant (p =0.0075). On the other hand patients with high (+++) expression of 17HSD type 1 showed no signi¿cant difference between the two treatment arms (HR=0.91, CI 0.43-1.95). Discussion: It has been suggested that 17HSD type 1 predominates in malignant cells and gives a higher conversion of E1 to E2, which results in higher intratumoral E2 levels and increased tumor growth. Abstracts – Poster Session II Our results suggest that tamoxifen may be unable to block the higher levels of E2 in these tumors. Tamoxifen showed to signi¿cantly reduce the risk of recurrence in tumors with low expression of 17HSD type 1. Our data suggest that 17HSD type 1 may be used as a predictive factor in hormone receptor positive breast cancer treated with tamoxifen but this needs to be con¿rmed in further studies. 2004 A high ratio of 17HSD1/17HSD2 protein expression predicts the outcome of tamoxifen treatment in postmenopausal breast cancer. Jansson A, Gunnarsson C, Persson L, Fornander T, Skoog L, Nordenskjöld B, Stål O. Linköping University, Linköping, Sweden; Karolinska University Hospital, Stockholm, Sweden Background: After menopaus estrogen biosynthesis in peripheral tissue has a major role. An enzyme group that affects the availability of active estrogens is the 17b-hydroxysteroid dehydrogenase family (17HSD). It is well known that 17HSD activity is responsible for the balance between estrone and estradiol in breast tissue. There are multiple family members expressed in breast tissue even though 17HSD1 and 17HSD2 seem to be the principal 17HSD enzymes involved in breast cancer this far. 17HSD1 catalyzes reduction of estrone to estradiol with NADP(H) as a cofactor, and 17HSD2 catalyzes oxidation from estradiol to estrone with NAD(H) as a cofactor. In breast cancer high expression of 17HSD1 and low expression of 17HSD2 is associated to decreased survival in estrogen receptor (ER) positive breast cancer. However, it remains unclear if 17HSD-enzymes can predict the outcome of tamoxifen treatment. The aim of this study was to investigate the prognostic and predictive value of 17HSD1 and 17HSD2 expression in a group of breast cancer patients randomized to tamoxifen treatment. Material and Methods: A randomized tamoxifen trial comprising 1,780 low risk breast cancer patients was conducted in Stockholm, Sweden, 1976-1990. All patients had lymph node negative primary breast cancer and were postmenopausal at the time of diagnosis. We analyzed the protein expression of 17HSD1 and 17HSD2 with immunohistochemistry using tissue microarrays, which were constructed from paraf¿n blocks originating from 912 patients. 17HSD1 and 17HSD2 could be scored in 871 (95.5%) and 858 (94%), respectively. Results: Low expression of 17HSD1 was associated with signi¿cant bene¿t of tamoxifen treatment (P=0.00045), whereas high expression was not (p=0.15). For ER+ patients with a 17HSD1 score not exceeding that of 17HSD2, tamoxifen decreased the risk of distant recurrencefree survival (DRFS) (RR=0.37, 95% C.I. 0.23-0.60) and breast cancer survival (BCS) (RR 0.30 (0.16-0.54)), whereas no apparent effect was observed when the score of 17HSD1 was higher that that of 17HSD2. The interaction was signi¿cant for both DRFS and BCS (p=0.036, p=0.014). In the cohort of systemically untreated patients no prognostic importance for 17HSD1 or 17HSD2 could be found. Discussion: In this study we could not con¿rm that high 17HSD1 expression is associated to shorter recurrence free survival among systemically untreated patients. More interestingly, in this unique series of breast cancer patients randomized to tamoxifen we found that if the expression of 17HSD1 exceeded that of 17HSD2, there was no bene¿t from tamoxifen treatment. This implicates that tamoxifen does not completely block the estrogen receptor in these tumors and that the cells respond to high estradiol levels. S85 2005 723$ gene ampli¿cation and response to adriamycin based therapy. Tubbs R, Barlow W, Budd GT, Swain E, Porter P, Yeh I-T, Sledge G, Shapiro C, Ingle J, Haskell C, Albain K, Livingston R, Hayes D. Cleveland Clinic, Cleveland, OH; Seattle, WA; Fred Hutchinson Cancer Research Center, Seattle, WA; University of Texas Health Science Center at San Antonio, San Antonio, TX; Indiana University Medical Center, Indianapolis, IN; Arthur James Cancer Center Hospital, Columbus, OH; Mayo Clinic, Rochester, MN; UCLA Medical Center, Santa Monica, CA; Loyola University Medical Center, Maywood, IL; Arizona Cancer Center, Tucson, AZ; University of Michigan Medical Center, Ann Arbor, MI Introduction: Reports have suggested that ampli¿cation and/or deletion of the TOP2A gene are positive predictive markers of response to anthracycline-based therapy. Using Àuorescence in situ hybridization (FISH), we determined the status of the HER2 and TOP2A genes in a large cohort of breast cancer patients treated with two regimens of doxorubicin (A) and cyclophosphamide (C). Patients and Methods: Tissue microarrays (TMA) were constructed from paraf¿n blocks collected from SWOG study S9313/Intergroup0137. Survival was similar in 3122 women with moderate-risk primary breast cancer who received equivalent doses of either concurrent adjuvant highdose chemotherapy with A plus C (n = 1595) or high-dose, sequential chemotherapy with A followed by C (n = 1527) (Linden, JCO. 25:656, 2007). FISH for TOP2A/CEP17 and HER2/CEP17 (Abbott Molecular) were performed for 1637 and 1493 cases respectively, using automated TMA core tracking and FISH tiling quanti¿cation (Metasystems). Results: An abnormal TOP2A genotype was identi¿ed for 150/1637 (9.1%) of cases (3.7% ampli¿ed, 5.4% deleted). An abnormal HER2 genotype was identi¿ed for 294/1493 (19.7%) of cases (18.1% ampli¿ed, 1.6% deleted). All but one TOP2A ampli¿ed case were co-ampli¿ed for HER2. Survival was marginally associated with HER2 ampli¿cation (ratio>2) (OS hazard ratio (HR) = 1.32; p=.07; DFS HR=1.22; p=.12), but was strongly associated for a ratio>4 (OS hazard ratio (HR) = 1.78; p=.001; DFS HR=1.65; p=.001). No signi¿cant differences in either overall or disease free survival were identi¿ed for TOP2A ampli¿cation and deletion. Conclusions: TOP2A genotypic abnormalities were not associated with outcome in this large prospective trial of patients treated with AC, consistent with TOP2A abnormalities being associated with an adverse prognosis, but balanced by greater responsiveness to anthracycline-based chemotherapy. HER2 ampli¿cation remains a prognostic marker in anthracycline-treated patients. 2006 Double staining chromogenic in situ hybridization is a useful alternative to Àuorescent in situ hybridization: ¿rst comparative study of HER2 and TOP2A gene ampli¿cation in breast cancer. Lacroix-Triki M, Mounie E, Charafe-Jauffret E, Jacquemier J. Institut Claudius Regaud, Toulouse, France; Institut Paoli-Calmettes, Marseille, France Background : Analysis of gene ampli¿cation such as HER2 and TOP2A in invasive breast cancer has now become a critical issue. Chromogenic in situ hybridization (CISH), which uses the easier bright¿eld microscopy, is an attractive alternative to Àuorescent in situ hybridization (FISH), particularly since the recent development of a dual-color CISH technique converting FISH signals to chromogenic stainings. In comparison with FISH, we analyzed not only HER2 but also TOP2A gene ampli¿cation using a new CISH conversion kit allowing a two-probe co-hybridization. Material and Methods: We selected 30 breast cancer samples with a known HER2 status as determined by immunohistochemistry (IHC). Cases were distributed in HER2-IHC score 1+ (n=2), score 2+ (n=16) and score 3+ (n=12). For each case, we performed a double-staining S86 Abstracts – Poster Session II CISH for HER2 and TOP2A genes, and a standard FISH for the same genes. The CISH conversion kit (Dako Denmark A/S) allowed the cohybridization of two probes on the same slide with a two-color detection, thus enabling centromere 17 (CEN17) analysis (blue signal) in addition to HER2 or TOP2A detection (red signal). The two techniques were performed in different institutions, and interpreted without knowing the results of the alternative technique. Results: The HER2 and TOP2A CISH slides showed contrasted and well-balanced blue and red signals, which were clearly identi¿ed at low magni¿cation and easily counted at high magni¿cation. Tumor morphology was fully preserved, without any signal-fading overtime, thus providing excellent reading conditions for the pathologist. Preliminary statistical analysis for HER2 gene showed a high concordance (95.6%) between double-staining CISH and FISH. Ongoing studies are evaluating TOP2A concordance and detailed correlations between HER2 and TOP2A gene copy numbers, HER2:CEN17 and TOP2A:CEN17 ratios, as obtained by the two techniques. Discussion: In addition to supporting the fact that dual-color HER2 CISH is a promising alternative to FISH, we described here the ¿rst CISH conversion kit enabling extension of this innovating technique to other genes such as TOP2A. Without the disadvantage of signal-fading, double-staining CISH improves the ease and time needed for signal enumeration and should be particularly valuable for routine practice and high-throughput tissue microarray studies. 2007 Quantitative measurements of HER2 expression and HER2: HER2 dimerization identify subgroups of HER2 positive metastatic breast cancer patients with different probabilities of response to trastuzumab treatment. Huang W, Lipton A, Leitzel K, Ali SM, Fuchs EM, Weidler J, Chappey C, Sperinde J, Tan Y, Jin X, Paquet A, Winslow J, Petropoulos C, Kostler WJ, Bates M. Monogram Biosciences, Inc., So San Francisco, CA; Penn State/Hershey Medical Center, Hershey, PA; Medical University of Vienna, Vienna, Austria Background: Immunohistochemistry (IHC) and Àuorescence in situ hybridization (FISH) are currently used to determine patient eligibility for trastuzumab therapy. However, not all HER2+ patients bene¿t from trastuzumab. Reliable measures that indicate which HER2+ patients will respond to trastuzumab have not been ¿rmly established. Here we describe the correlation of quantitative measurements of total HER2 expression (H2T) and HER2:HER2 dimerization (H22D) using a novel assay technology, VeraTagTM, with objective response rate (ORR), time-to-progression (TTP) and overall survival (OS) in a cohort of metastatic breast cancer (MBC) patients treated with trastuzumabbased regimens. Methods: MBC patients received ¿rst-line trastuzumab alone or combined with chemotherapy regimens. Selection of HER2+ patients for trastuzumab treatment was based on IHC performed by a central lab (Med Univ of Vienna). Formalin-¿xed paraf¿n-embedded (FFPE) tissues from 58 patients were retrospectively measured for H2T and H22D using VeraTag (Monogram), blinded to the outcome data. Patients were categorized as high (> median) or low (< median) H2T or H22D. Correlation of H2T and H22D with clinical outcome was analyzed using the Kaplan-Meier method and Cox Proportional Hazards regression analysis. Results: Patients with high H2T showed signi¿cantly higher ORR than those with low H2T (59.3% vs. 17.9%, p < 0.001). Similarly, patients with high H22D had higher ORR than those with low H22D (55.6% vs. 21.4%, p < 0.01). Kaplan-Meier analysis revealed signi¿cantly longer TTP for patients with high H2T as compared to those with low H2T (median TTP 12.8 mo vs. 4.0 mo), and a relative risk of progression nearly half for patients in the high H2T group compared with the low group (HR=0.52, log-rank test p=0.013). A similar trend was observed for H22D (median TTP 12.8 mo vs. 4.0 mo for high H22D vs. low H22D, respectively), but did not reach statistical signi¿cance (HR=0.65 p=0.11). In separate multivariate Cox models where patients were strati¿ed by age and number of distal metastatic sites, high H2T and high H22D were independent correlates of TTP (H2T, p=0.007, and H22D, p=0.009). The high H2T group showed a trend toward better OS in a univariate Cox model (p=0.17). Further validation of H2T and H22D using overall survival as an endpoint may require larger datasets. Conclusion: In a population of MBC patients selected to receive trastuzumab based on HER2+ IHC, higher HER2 expression and HER2: HER2 dimerization were independently correlated with better objective response and longer time to progression. The results suggest that more precise methods of quantitating HER2 expression or measuring HER2 functionality (dimerization) will allow for improved strati¿cation of MBC patients for trastuzumab treatment. 2008 Inter-observer interpretative reproducibility of HER2 genotyping of a consecutive series of primary breast carcinomas by Silver In Situ Hybridization (SISH). Tubbs R, Myles J, Papouchado B, Lloyd R, Oliveira A, McElhinny A, Vladich F, Pestic-Dragovich L, Downs-Kelly E, Prescott N, Pettay J, Loftus M, Roberts C, Grogan T, Roche P. Cleveland Clinic and the Cleveland Clinic Lerner College of Medicine, Cleveland, OH; Mayo Clinic, Rochester, MN; Ventana Medical Systems International, Tucson, AZ Introduction Determination of HER2 status in breast carcinoma may be established by Àuorescence in situ hybridization (FISH) as the primary method of testing or for con¿rmation of equivocal immunohistochemistry results. Requirements for specialized instrumentation and training, overnight hybridization, manual rather than automated methods, and workÀow issues may restrict routine implementation of FISH in many pathology laboratories. Fully automated silver in situ hybridization (SISH) provides permanently stained slides for determination of a HER2 genotype in six hours and may reduce overall laboratory costs. Preliminary studies have shown excellent performance against FISH as the reference standard. We evaluated the inter-observer interpretative reproducibility of HER2 SISH in a consecutive series of primary breast carcinomas previously genotyped by FISH. Patients and Methods SISH HER2 was done using unstained paraffin sections of 292 consecutive primary breast carcinomas genotyped by FISH in the year 2006. The SISH procedure was fully automated and completed within six hours, including on line deparaf¿nization, cell conditioning, target denaturation, probe/target hybridization, and enzyme metallographic signal detection. Interpretation was performed by standard bright ¿eld manual signal enumeration of two representative ¿elds of invasive carcinoma. Each observer was pre-trained using a standardized tutorial and representative SISH preparations. Pathologists reviewed an H and E slide, a SISH slide stained for HER2 using a repeat depleted DNP labeled probe, and a SISH slide stained for chromosome 17 (CHR17) using a DNP labeled centromeric oligonucleotide probe. The HER2 and CHR17 signal counts were enumerated and the HER2/CHR17 ratio was calculated. Overall agreement and kappa statistics were calculated for each observer versus the consensus SISH score for all observers and versus the reference HER2 status established by FISH. Results Overall agreement of HER2 amplification status among the five pathologists interpreting the SISH preparations was excellent. Overall agreement among observers ranged from 94.9 - 96.6%. The kappa statistic correcting for chance agreement among observers ranged from 0.760 - 0.869; the agreement between consensus SISH and FISH was 94.2% and the kappa statistic was 0.775 Conclusions Silver in situ hybridization (SISH) is a robust and rapid automated method for determination of HER2 genotypic status. Interpretation of SISH preparations by pathologists is reproducible and represents a promising alternative to FISH testing for determination of HER2 status in breast carcinoma. Abstracts – Poster Session II 2009 HER2 tumors are heterogeneous, clinically, molecularly, and in response to preoperative trastuzumab: pathway analysis of gene expression pro¿les from three breast cancer datasets. Harris LN, Eklund AC, Carter S, Li X, Winer EP, Hilsenbeck S, Esteva FJ, Symmans WF, Pusztai L, Szallasi Z, Chang J. Yale University, New Haven, CT; Childrens Informatics Program, Boston, MA; Dana Farber Cancer Institute, Boston, MA; Baylor University, Houston, TX; MD Anderson Cancer Center, Houston, TX HER2 ampli¿ed tumors cluster on transcriptional pro¿ling largely driven by genes on the 17q12-21 amplicon, however this molecular subtype is heterogeneous. We analyzed the inÀuence of pathways signatures on response to preoperative trastuzumab-containing (trz) therapy in HER2 ampli¿ed breast cancer. Methods Three cohorts of patients with HER2 3+/FISH+, stage II-III breast cancer were included, summarized in Table. Extremes of response were used to compare with gene expression signatures: resistance was de¿ned as stable or progressive disease (SD+PD) using RECIST. Pathologic complete response (pCR) was de¿ned as lack of invasive disease in the breast and lymph nodes at the time of surgery. Raw data from each of the three data sets were modeled separately with the RMA algorithm. The relative expression of each signature in each sample was estimated by taking the mean expression of all genes in the signature. We used 14 published signatures said to characterize activity of e2f, myc, ras, src, bcat, PI3K, hypoxia, chromosomal instability (CIN), spindle checkpoint/assembly, genomic grade, DNA repair, BM1-1 and basal gene signatures. The association between signature and outcome was evaluated with Student’s t test. Results DFCI and Baylor cohorts were quite different with the majority of tumors from the Baylor study being ER/PR- and T4. The DFCI and MDACC cohorts were similar in T stage and ER status. Baylor and DFCI cohorts had similar rates of pCR of 19% and 14% respectively, compared to MDACC with 71% pCR, perhaps due in part to differences in treatment duration. We evaluated the ability of fourteen published signatures to predict response to therapy. While some of the signatures were of signi¿cance in a particular cohort, no signature showed a consistent correlation with pCR or resistance at a p>0.05. In fact, the majority of the signatures correlated associated with resistance in the opposite direction in the DFCI and Baylor cohorts. Higher levels of basal signature was associated with resistance to trz in the Baylor dataset (p=0.03) whereas the other two cohorts were not, although basal genes were signi¿cantly associated with resistance in the DFCI cohort in a separate analysis (p=0.03). Conclusions HER2 ampli¿ed tumors represent a heterogeneous group by lineage, pathway activation and treatment response. HER2 tumors of basal lineage may be less likely to respond to trz-containing therapy. Larger studies are required to understand the variability in this breast cancer subtype. Trial 1 2 3 Site Baylor DFCI MDACC Subjects 38 48 30 Treatment trz+docetaxel 12 wks trz+vinorelbine 12 wks trz+T>FEC 24 wks Tissue Core Bx Core Bx FNA Platform U133A U133+2 U133A Genechips 21 20 21 2010 Comparison of ERBB2 evaluation by immuno-histochemistry and a quantitative RT-PCR method in primary breast cancers. Giacchetti S, Lehmann-Che J, De Roquancourt A, Cuvier C, Hocini H, Bertheau P, De The H, Espié M, Turpin E. Hopital Saint-Louis, Assistance Publique-Hopitaux de Paris, Paris, France; Hopital SaintLouis, APHP, Paris, France Background: Immunohistochemistry (IHC) and Àuorescent in situ hybridization (FISH) are currently the most commonly used methods to assess ERBB2 status. They are semiquantitative methods. PCR-based assays are sensitive, speci¿c and quantitative approaches to determine ERBB2 ampli¿cation (DNA, Q-PCR) or over-expression (RNA, QRTPCR), but they mix tumor and stromal cells. Here, we performed S87 a large study comparing IHC and Q-RTPCR. Discordant cases were explored by Q-PCR and FISH. Material and Methods: We analyzed 442 primary breast tumors patients treated in St Louis Hospital from 2002 to 2007. Tissue samples were formalin-¿xed paraf¿n-embedded for IHC (CB11 antibody) and FISH. Tissues were frozen for Q-RTPCR and QPCR. IHC was positive 3+ if strong complete membrane staining was seen in ≥ 60% tumor cells. Relative quanti¿cation (RQ) by Q-RTPCR was performed (with a pathological control to ensure tumor cell density and the absence of in situ carcinoma) for ERBB2 detection and TBP as endogen control. Final results was expressed as a normalized ratio considered as low over-expressed if ≥ 5 and high over-expressed if >10. DNA analysis was performed with the LightCycler-HER-2/neu DNA Quanti¿cation KIT (Roche) in a subgroup of discordant patients. Results: High RNA positive samples were all IHC positive. In IHC negative cases, IHC / QRTPCR correlation was very high (97.5 %). In IHC3+ patients there are 16 discordant cases (14%). DNA analyses con¿rmed the absence of ampli¿cation in 13 cases. In IHC2+, 14/16 were RNA negative, 2 were low RNA positive. 1 out of these 2 was DNA positive. FISH analyses are on going. Conclusion: The exact determination of ERBB2 status is crucial because of the potential toxicity and the coast of Trastuzumab treatment. A quantitative method as PCR-based assays could be more reliable and could allow treatment according to the level of ERBB2 surexpression. This is a way to optimize ERBB2 + breast cancer treatment. 2011 Development of novel proximity-based immunoassays for the detection of HER heterodimerization in breast cancer cell line lysates and formalin-¿xed, paraf¿n-embedded tissue. Eli* L, Shi* Y, Dao-Pick T, Bose J, Frankson K, Penuel E, Weston J, Pidaprthi S, Mukherjee A, Nguyen X-T, Williams S, Goodman L, Winslow J. Monogram Biosciences, South San Francisco, CA Background: Trastuzumab, in combination with a chemotherapy regimen, is the primary treatment for metastatic breast cancer patients with tumors exhibiting HER2 protein over-expression. Of these patients, approximately 30% initially respond to treatment, and subsets of these patients demonstrate inherent or acquired resistance. Multiple mechanisms of Trastuzumab resistance have been proposed, including several that implicate HER receptor homo- and heterodimers as potential escape pathways. Assays identifying such signaling pathways could have clinical utility toward predicting response to Trastuzumab as well as other emerging drugs that speci¿cally target HER signaling pathways. Materials and Methods: We have developed a set of novel proximitybased immunoassays (VeraTag) that measure proteins and functional protein-protein interactions using two different formats: cell line/ tumor lysates and FFPE sections. To evaluate the importance of HER heterodimer formation as a potential escape pathway, lysateformat assays were applied to measure levels of EGFR/HER1-HER2 heterodimers in cell lines derived from breast and ovarian tumors. A matrix of positive and negative control cell lines, and HER antibodies, were identi¿ed by several cross-validating technologies and evaluated further by FFPE-format proximity immunoassays. Results: Using our lysate-format proximity assay, we demonstrate two-, three-, and ten-fold increases in EGFR/HER2 heterodimers in SKBR3, AU565, and SKOV3 cell lines, respectively, following ten minutes of stimulation with 100nM epidermal growth factor (EGF). Control experiments indicate no signi¿cant change in the total amounts of EGFR and HER2. These increases are further supported by the EGF-dependent co-immunoprecipitation of HER1 and HER2 in these cells. Additionally, we have generated stably transfected HEK-293 cell S88 Abstracts – Poster Session II lines that over-express varying levels of EGFR and HER2, and we are currently exploring the relationship between expression levels and heterodimer formation. To initiate evaluation of HER1-HER2 cell lines in the FFPE-format proximity assay, HER1 and HER2 antibodies were identi¿ed and an assay format tested on EGF-stimulated SKBR-3 cells, resulting in an increase in EGF-dependent heterodimer formation. Discussion: We have established a HER2 total and a HER2 homodimer assay (VeraTag) in FFPE breast tumors that is currently being validated and is predictive of Trastuzumab response. We are also developing VeraTag assays for other HER family members (for example, HER2HER3) and our preliminary evidence suggests that the use of this novel technology to make these quantitative measurements in tumor biopsies will be useful towards prediction of alternative or combination therapies for the treatment of Trastuzumab-resistant tumors. *Contributed equally. 2012 Characterization of a novel proximity immunoassay for the quantitative determination of HER2 protein expression and HER2 homodimerization in formalin-¿xed, paraf¿nembedded breast cancer tissue. Winslow J, Shi Y, Tan Y, Jin X, Dua R, Penuel E, Mukherjee A, Sperinde J, Pannu H, Chenna A, DeFazio-Eli L, Pidiparthi S, Chen L, Williams S, Larson J, Goodman L, Whitcomb J, Petropoulos C, Huang W. Monogram Biosciences, Inc., South San Francisco, CA Background: Although present methods such as HER2 immunohistochemistry (IHC) and Àuorescence in situ hybridization (FISH) are valuable for preliminary patient selection, both tests are limited in that they fail to fully discriminate responding and nonresponding populations. There is a need to develop 2nd generation diagnostic tests that will more effectively predict responses to HER2targeted drugs. We have utilized dual antibodies in a novel proximity format, termed the VeraTag assay, to develop sensitive and quantitative immunoassays measuring HER2 total and homodimerization levels in FFPE breast cancer cell lines and tumor tissues for application to predictive testing. Methods. The characterized assay detects HER2 total protein and HER2 homodimer protein-protein complexes by the release of novel fluorescent electrophoretic tags conjugated to an analyte-bound antibody. The release of Àuorescent tags requires proximity to a second HER2 “scissors” antibody which is activated upon illumination. The collected Àuorescent tags are separated and quantitated by capillary electrophoresis, and normalized to tumor area. Results. A HER2 monoclonal antibody proximity pair was selected based on assay signals that parallel the relative HER2 expression levels of human breast cancer cell lines (<103 to >106 receptors/cell). The HER2 total eTag assay signal was linear with antigen concentration over a 10-20-fold range of cell line section size and breast tumor area. A comparison of HER2 total levels in 174 breast cancers demonstrated a continuum over a wide dynamic range (>2 logs), in contrast with conventional IHC categories. The correlation between HER2 total levels and IHC categories was signi¿cant (p<0.0001). The VeraTag assay signal correlates well with IHC Histoscore at lower HER2 total levels, however, at high HER2 total levels the VeraTag assay provides extended dynamic range. HER2 gene ampli¿cation measured by FISH correlates loosely with IHC categories and HER2 total values. An algorithm was developed to normalize for systematic assay variation, generally <20-30%, allowing large scale processing of FFPE tumor samples.Conclusions. The results demonstrate that the VeraTag assay reliably measures HER2 total and HER2 homodimer levels quantitatively in FFPE tissues. The continuum of HER2 total levels over a wider dynamic range compared to conventional IHC and FISH HER2 tests, the novel HER2 homodimerization measure, and studies correlating HER2 levels with clinical responses to trastuzumab, suggest that the VeraTag assay technology may provide better predictive tests for targeted HER2 therapy. 2013 HER2 and SPARC status in tumors play an important role in the relative effectiveness of nanoparticle albumin-bound (QDE) paclitaxel versus polysorbate-based docetaxel. Desai N, Trieu V, Hwang L, Wu R, Hawkins M, Soon-Shiong P, Gradishar W. Abraxis BioScience, Inc., Los Angeles, CA; Northwestern University, Chicago, IL Background: HER2 overexpression in tumors is associated with a more aggressive phenotype with increased disease recurrence and poor prognosis. HER2 is overexpressed in about 25-30% of breast cancers, as well as in other cancers such as ovarian (15-30%) and stomach cancer (15-34%). The albumin-binding protein SPARC (Secreted Protein Acidic and Rich in Cysteine), which is overexpressed in about 50% of breast cancers, is associated with increased tumor invasion and metastasis and known to be a poor prognostic factor in breast cancer (Watkins 2005). This has also been demonstrated in a number of other cancers such as prostate, gastric, liver, lung, kidney, head and neck, and brain tumors. Nab-paclitaxel (Abraxane®) is an albumin-bound 130-nm particle form of paclitaxel that shows enhanced tumoral accumulation by targeting SPARC in tumors through a SPARC-albumin interaction (Trieu 2007). The goal of this study was to evaluate the importance of HER2 and SPARC status in determining the relative ef¿cacy of nabpaclitaxel with polysorbate 80/ethanol-based docetaxel (Taxotere®). Material and Methods: Maximum tolerated dose (MTD) of nabpaclitaxel and docetaxel were previously determined as >120mg/kg and 15 mg/kg respectively on a q4dx3 schedule (Desai 2006). HER2 and SPARC status in tumors was analyzed by RT-PCR and immunohistochemistry (IHC). The antitumor activity of docetaxel (15 mg/kg) was compared to nab-paclitaxel in breast tumor xenografts MX-1 (equidose level of 15 mg/kg, qwkx3), MDA-MB-231 (120 and 180 mg/kg, q4dx3) and MDA-MB-231/HER2+ (50 and 120 mg/kg, q4dx3). Additional tumor xenografts (LX-1 lung, PC3 prostate, and HT29 colon) were also studied. Tumor volume and body weights were monitored. Results: Two of three breast cancer lines (MDA-MB-231 and MX1) were HER2 negative. Amongst the non-breast tumors, only LX-1 was HER2 negative. Two HER2 positive tumors HT29 and PC3 were strongly SPARC positive with SPARC expression HT29>PC3>MB231/HER2+=MX1. MDA-MB-231 and LX-1 tumors had little to no SPARC expression. Nab-paclitaxel, even at doses less than its MTD, was a signi¿cantly more effective antitumor agent than polysorbatebased docetaxel administered at its MTD in the three HER2-negative tumors (MX-1, MDA-MB-231, and LX-1) and relative ef¿cacy was independent of SPARC expression. In HER2-positive tumors, the antitumor activity of nab-paclitaxel was equal to or better than docetaxel in two of the three tumors types (PC3, HT29, but not MB-231/HER2+) and increased with increasing levels of SPARC expression. Discussion: HER2 and SPARC expression may be of importance in determining antitumor activity of taxanes and potentially serve as useful as biomarkers for nab-paclitaxel effectiveness. The relative ef¿cacy of nab-paclitaxel vs. polysorbate-based docetaxel was signi¿cantly higher in HER2-negative than in HER2-positive tumors. In HER2 positive tumors, the relative ef¿cacy of nab-paclitaxel increased with increasing SPARC expression. 2014 HER2 immunohistochemistry: comparison of image analysis based interpretation of CB11 and 4B5 clones using reference Àuorescence in-situ hybridization. Fine JL, Bhargava R, Surti U, Dabbs DJ. Magee-Womens Hospital of UPMC, Pittsburgh, PA Background: Immunohistochemistry (IHC) testing for HER2/neu is under increased scrutiny in terms of laboratory accreditation, to ensure accurate and reproducible assessment of breast cancer patients for potential trastuzumab therapy. Image analysis systems can help pathologists provide improved HER2/neu IHC testing by: 1) reducing inter-observer scoring variability; 2) reducing time required to score IHC stains; and 3) increasing automation of both technical and interpretation components of IHC testing. This study details validation of image analysis for interpretation of HER2/neu IHC. Abstracts – Poster Session II Methods: Breast cancer cases were stained for HER2/neu utilizing CB11 and 4B5 antibody clones (Ventana Medical Systems, Tucson, AZ), according to the vendor’s instructions, on a Benchmark XT automated IHC platform (Ventana). Fluorescent in-situ hybridization (FISH) was performed to assess for HER2/neu ampli¿cation (Vysis, Downers Grove, IL). Image analysis of the IHC stained slides was carried out using a commercially available image analysis system (VIAS, Ventana). Using classi¿ers speci¿cally designed for each antibody, the system assigned a numerical score (0 to 3.50), which was then automatically rounded to the nearest whole number as a score (0, 1+, 2+, or 3+). These scores are intended to be directly analogous to scores that would be assigned by a pathologist: 0 or 1+ is negative; 2+ is weakly positive (FISH required); and 3+ is positive. Results: The image analysis system was able to differentiate tumor cells from non-tumor cells in a given ¿eld of view; it could not differentiate DCIS from invasive disease nor could it ¿nd a ¿eld automatically (i.e. a pathologist had to “show” the system which ¿elds to analyze). All CB11 analyses were 100% concordant with HER2/neu FISH results (n=52). There was 95% concordance between 4B5 analyses and FISH results; discrepancies were all weakly positive stains (i.e. over calls) that were not HER2/neu ampli¿ed by FISH (3 discrepancies, n=56). If a higher threshold for assigning a 3+ score was used instead of the rounded score (i.e. the system maximum numerical score 3.50), then 100% concordance was obtained for 4B5 analyses. Conclusion: There is excellent agreement between image analysis and FISH, provided an appropriate reference range (i.e. 4B5 3+ cut-off) is utilized. This validation study showed that this system can reliably analyze HER2/neu IHC stains, thus assisting pathologists in scoring these tests. This should reduce inter-observer variability in HER2/ neu IHC scoring, and future enhancements should seek to increase automation by: 1) communicating with other laboratory information systems; 2) improving ability to automatically ¿nd areas of invasive disease without pathologist intervention; and 3) increasing accuracy such that 2+ cases are reduced in number. Subsequent studies should examine other impacts that image analysis have on HER2/neu testing, such as number of required FISH tests, turn-around time, and error rates related to slide misidenti¿cation. 2015 Expression of the microtubule-associated protein, tau, predicts improved survival, but not response, to a combination of docetaxel and vinorelbine in HER-2 negative metastatic breast cancer. Gralow JR, Barlow WE, Gown AM, Goldstein LC, Porter PL, Yeh I-T, Livingston RB, Hayes DF. University of Washington, Seattle, WA; Fred Hutchinson Cancer Research Center, Seattle, WA; Phenopath, Seattle, WA; UT San Antonio, San Antonio, TX; Arizona Cancer Center, Tucson, AZ; University of Michigan, Ann Arbor, MI Background Drugs that poison the mitotic spindle, including taxanes and vinca alkaloids, are active agents against breast cancer. Tumor expression of beta-tubulin isoforms and microtubule-associated proteins (MAPs) may predict outcomes of anti-tubulin therapy. In breast cancer, high tau expression predicts for resistance to paclitaxel and sensitivity to endocrine agents. SWOG conducted a phase II study of the combination of docetaxel, vinorelbine plus ¿lgrastim as 1st or 2nd-line chemotherapy in HER-2 negative metastatic breast cancer (S0102). This study evaluates the predictive value of the MAP tau and class III beta-tubulin in breast cancer patients receiving two anti-tubulin agents. Methods Immunohostochemistry using antibodies to tau, class III beta-tubulin, ER, PR, p53, and Ki-67 was performed on a tissue microarray (TMA) constructed from S0102 paraf¿n blocks. All markers were scored from 0 to 3. Results Of the 95 patients registered, 92 were eligible and received treatment. There have been 69 deaths and 83 progressions. Median overall survival (OS) is 1.69 years with median progression-free survival (PFS) of 0.6 years. A total of 62 patents (67.4%) had a TMA constructed. There was no difference in outcome for those with or without a TMA. Tau was positively correlated with ER and PR, but not with class III beta-tubulin, S89 KI-67, or age. Class III beta-tubulin was not signi¿cantly correlated with any other marker. There was a signi¿cant effect of tau on OS (HR=0.62, p=0.0002) and PFS (HR=0.67, p=0.0007), with higher tau associated with longer survival. Higher tau was still associated with improved OS and PFS when adjusted for age and ER/PR. Expression of class III beta-tubulin was not associated with OS (HR=0.97, p=0.85) or PFS (HR=0.86, p=0.29). We also analyzed the 42 tumor responses among the 92 patients. There was no relationship of tau with tumor response adjusting for age (p=0.33). There was also no relationship of response with class III beta-tubulin (p=0.56), ER (p=0.32), PR (p=0.07), or KI-67 (p=0.14). For the 29 patients who had tau values of 0-1, the response rate was 38%, compared to 47% for those who had tau values of 2 or 3. Discussion High expression of tau was associated with improved survival in patients with HER-2 negative breast cancer treated with docetaxel and vinorelbine. Unlike previous studies with paclitaxel alone, increased tau expression did not predict resistance to the combination of docetaxel and vinorelbine. Further evaluation of the relationship between tau expression and response to anti-tubulin agents is warranted. This work was supported by a grant from the Breast Cancer Research Foundation. 2016 Microtubule-associated protein tau is a marker of pathological complete response in Her-2/neu positive neoadjuvant treated breast cancer patients. Rueckert S, Wirtz R, Lenhard M, Hasmueller S, Ditsch N, Ruehl I, Kahlert S, Bauerfeind I, Untch M. LMU, Universtity of Munich, Munich, Germany; Siemens Medical Solutions Diagnostics GmbH, Leverkusen, Germany; Helios Klinikum Berlin-Buch, Berlin, Germany Background: Microtubule-associated protein tau (MAPT) promotes tubulin polymerization and stabilizes microtubules. Microarray analysis of fresh breast cancer tissues revealed, that low expression of MAPT is a predictive marker for response to anthracycline and taxane based chemotherapy. In contrast, it has recently been shown, that high expression of MAPT may indicate response to endocrine therapies. Here, we have analyzed the RNA expression of MAPT in formalin ¿xed paraf¿n embedded breast cancer tumour tissues of patients treated within two neoadjuvant chemotherapy trials to evaluate the prognostic value in this setting. Patients and methods: Breast cancer patients (≥cT2, N0-N3, M0) received neoadjuvant chemotherapy of 4 cycles of epirubicin and cyclophosphamide followed by 4 cycles paclitaxel (PREPARE trial). In Her-2/neu positive breast cancer patients trastuzumab was administered parallel to paclitaxel therapy and continued after surgery (TECHNO trial). Samples of paraf¿n embedded core needle biopsies obtained at diagnosis of an initial group of 57 patients (34 TECHNO / 23 PREPARE) were prepared for ¿rst analysis. RNA was successfully isolated from the tissue samples by an automated system based on magnetic beads (Siemens Medical Solutions Diagnostics GmbH). RNA expression of ESR1, Her-2/neu and MAPT expression was determined by quantitative RT- PCR. MAPT expression was correlated to histopathological ¿ndings. Results: RNA expression of MAPT signi¿cantly correlated with ESR1 expression (Spearman r=0,677; p<0,0001), but not with Her2/neu expression. Median expression of MAPT was 4 fold higher ESR1 positive tumors. Of the 57 patients included in the ¿rst analysis, 10 patients showed a pathological complete response, 4 in the PREPARE and 6 in the Her-2/neu positive TECHNO group. There was a signi¿cant difference of MAPT-RNA expression between those patients with histopathologically complete response after neoadjuvant chemotherapy and those with no or partial response in the ¿rst cohort (Mann-Whitney-U, p=0.019). Patients with a complete response showed signi¿cantly lower levels of MAPT-RNA. Interestingly, this difference was prominent in the group of Her-2/neu positive tumors (TECHNO trial) with all responding tumors exhibiting a 4 fold lower median MAPT expression (Mann-Whitney-U, p=0.009). In contrast, no statistically difference was seen in the PREPARE group with only half of the tumors being below the median MAPT expression. S90 Abstracts – Poster Session II Conclusion: These results validated the initial hypothesis that low expression of MAPT indicates sensitivity to chemotherapy on RNA level in clinical routine paraf¿n tissue. Moreover, low MAPT-expression was particularly informative in Her-2/neu positive breast cancer patients treated with anthracyclin-based chemotherapy containing paclitaxel and trastuzumab. 2017 Cyclin-dependent kinase 2 to 1 specific activity ratio predicts response to epirubicin and paclitaxel in human breast cancer. Kim SJ, Miyoshi Y, Taguchi T, Tamaki Y, Noguchi S, Tsukamoto F, Akazawa K, Nakayama S, Matsushima T, Torikoshi Y, Ishihara H. Graduate School of Medicine, Osaka University, Suita, Osaka, Japan; Osaka Koseinenkin Hospital, Osaka, Japan; Sysmex Corporation, Kobe, Hyogo, Japan Background: We have reported that breast tumors with a high ratio of cyclin-dependent kinase (CDK) 2 speci¿c activity (SA) to CDK1SA (CDK2/1 ratio) are associated with high tumor cell proliferation and poor clinical outcome. The aim of the present study is to evaluate the correlation of CDK2/1 ratio with response to chemotherapy in breast cancer. Material and Methods: Of 76 primary breast cancer patients (pts) (age: 25-71y, mean: 49.2y), 33 were treated with cyclophosphamide + epirubicin (CE) (600/60 mg/m2, q3w) for three or four cycles and 43 with paclitaxel (80 mg/m2, q1w) for 12 cycles in the neoadjuvant setting. Frozen tumor tissues were obtained from core needle biopsy before chemotherapy, and CDK2/1 ratio was examined by the Cell Cycle Pro¿ling (C2P) assay as previously reported (Ishihara, et al: Biochim Biophys Acta 1741: 226, 2005). Clinical response was evaluated by MRI and patients were classi¿ed into responders (CR+PR) and non-responders (NC+PD). Cut-off values of CDK2/1 ratio were determined to best separate the responders and non-responders to CE and paclitaxel, respectively. Results: Pts characteristics were as follows: menopausal status: pre54%, post- 46%; Stage: II 41%, III 49%, IV 11%; Tumor size (cm): 2-5 cm 54%, > 5 cm 46%; histologic grade (HG): I 18%, II 41%, III 28%; ER: (+) 58%, (-) 42%; PR: (+) 41%, (-) 59%; HER2: (+) 29%, (-) 68%. In a CE treatment group, all 13 tumors with high CDK2/1 ratio responded to CE while only 7 of 20 tumors with low CDK2/1 ratio responded (positive prediction value (PPV): 100%, negative prediction value (NPV): 65%, accuracy: 79%, p < 0.001). In a paclitaxel treatment group, of 32 tumors with high CDK2/1 ratio, 29 responded to paclitaxel while only 4 of 11 tumor with low CDK2/1 ratio responded (PPV: 91%, NPV: 64%, accuracy: 84%, p = 0.0002). Discussion: The CDK2/1 ratio is signi¿cantly associated with response to CE and paclitaxel. The CDK2/1 ratio seems to have a potential to be used as a new predictive factor for epirubicin and paclitaxel in breast cancer. 2018 High pretreatment cyclin E levels may de¿ne a higher risk subset of basal-like breast cancers: in depth immunohistochemical analysis and clinical outcome of neoadjuvantly treated basal-like breast cancers. Osborne CR, Tripathy D, Allada N, Bian A, Xie X-J, Ashfaq R. UT Southwestern Medical Center, Dallas, TX; Baylor University Medical Center, Dallas, TX Background: Gene expression pro¿ling has revealed several subsets of breast cancer with distinct clinical outcomes. The basal-like subtype is in part characterized as HER2 and hormone receptor (HR) negative. We previously described a number of basal-like cases treated with neoadjuvant chemotherapy. In this cohort, relapsing patients were noted to have increasing Ki-67 values in their de¿nitive resection specimens compared to their baseline biopsy. Here we present further IHC characterization of neoadjuvantly treated basal-like cases. Methods: 35 basal-like cases treated with neoadjuvant chemotherapy were identi¿ed. Pre-chemotherapy and post-chemotherapy in depth breast tumor IHC characterizations including; cyclin E, androgen receptor (AR), survivin, EGFR, CK 5/6, CK 7, SPARC and Ki-67 expression were evaluated in relationship to relapse status. Wilcoxon rank sum, Chi-square and Fisher’s exact tests were performed as indicated. Results: Of the 22 patients who relapsed, 18 are deceased, 1 has progressive disease, 1 remains NED after surgery and 2 are lost to follow-up. CK 5/6 was expressed in 61.1% of relapsed pretreatment specimens but only 33.3% of non relapsed specimens, though this was not statistically signi¿cant (p=0.83). Table 1 demonstrates IHC results for the pre-chemotherapy specimens in relationship to relapsed vs. non relapsed status. Of interest, cyclin E, survivin and Ki-67 were more elevated in the relapsed cases compared with the non relapsed, though only cyclin E was found to be statistically signi¿cant (p=0.013). Post chemotherapy cases showed a signi¿cantly higher expression of Ki67 in the relapsed group as compared to the non relapsed group (65% vs. 51% p=0.042). Cyclin E and survivin expression remained high in the relapsed group (60% vs. 42% and 62% vs. 66% ) though these values were not statistically signi¿cant. There was a trend for higher AR expression in non-relapsing cases. Conclusions: Basal-like breast cancers have more aggressive disease and worse outcomes compared to other de¿ned subsets. Basal tumors demonstrate rapid cell cycling as evidenced by high cyclin E and Ki67 and may have augmented anti-apoptotic mechanisms manifest by elevated survivin levels which may allow for escape from cytotoxic effect. Additionally, high pretreatment cyclin E levels may in particular identify an even higher risk subset. Table 1 Variable AR CK7 Cylin E EGFR Ki-67 SPARC Survivn Relapsed NO Yes No Yes No Yes No Yes No Yes No Yes No Yes N 12 20 12 20 12 20 11 20 13 22 11 20 12 20 Mean 0.10 0.16 3.54 3.56 0.34 0.66 0.54 0.38 0.53 0.58 1.30 1.11 0.54 0.60 p Value 0.98 0.88 0.013 0.56 0.33 0.58 0.78 2019 Adding the estimation of cyclin D1 gene ampli¿cation to the standard panel of predictors in breast carcinoma can signi¿cantly improve identi¿cation of tumors resistant to tamoxifen. Petrakova K, Nenutil R, Vyskocil J, Fabian P, Palacova M, Hanzelkova Z, KnoÀickova D. Masaryk Memorial Cancer Institute, Brno, Czech Republic Background: Despite of many recently published predictors of resistance to tamoxifen, clinical practice lacks a simple, reproducible and commercially widely available tool, routinely applicable to identify patients, quali¿ed for adjuvant hormonal therapy, in which no bene¿t of tamoxifen treatment can be expected. Here we attempted to ¿nd a simple combination of predictors, recognizing most of tumors recurring during the course of tamoxifen treatment, while exhibiting reasonably low incidence in chronological series of unselected ER-alpha (ER) positive carcinomas. Material and Methods: Cases of ER positive breast carcinoma of clinical stage I+II at the time of diagnosis exhibiting a documented locoregional and/or distant tumor relapse during the adjuvant tamoxifen treatment were retrieved from medical records. Tissue microarrays (TMAs) were built from the archived paraf¿n blocks of primary (n=37) and secondary , (if available, n=27), tumors of above patients. TMAs from unselected cases of ER positive breast carcinomas (n=85) served as a control. Her-2 and cyclin D1 ampli¿cation were analyzed using Àuorescence in-situ hybridization (FISH) with Abbott probes. ER, progesterone receptor A+B (PR), Bcl2, estrogen receptor beta (ER-beta), cyclin A and cyclin D1 were estimated using immunohistochemistry with commercially available antibodies (Labvision, Novocastra). Clinical data, such as pT-stage, pN-stage, grade, patient’s age, and others, were available for analysis. Abstracts – Poster Session II Results: None of clinical parameters, neither Bcl2, ER-beta, cyclin D1 and cyclin A immunohistochemistry proved acceptably sensitive and speci¿c. On the contrary, the combination of Her-2 and/or cyclin D1 ampli¿cation and/or PR negativity, was found in 92% of secondary tumors growing during the tamoxifen treatment and in 66% of corresponding primary tumors. The incidence of this combination in consecutive cases was 28% only. Her-2 and/or Her-2 Cyclin D1 PR below 5% cyclin D1 ampli¿ed ampli¿cation ampli¿cation p<0,0001* and/or PR below p=0,008* p=0,006* 5% p<0,0001* Secondary tumors 26% n=23 Primary tumors with 36% relapse n=37 Control ER positive 12% primary tumors n=85 * Pearson Chi-square probability 36% 68% 92% 23% 26% 66% 12% 8% 28% Discussion: Cyclin D1 and Her-2 amplifications, as well as PR negativity, are already recognized to predict resistance to tamoxifen. FISH is in general better standardized and reproducible when compared to immunohistochemistry. For this reason we suggest to add FISH assessment of cyclin D1 gene status to the routine evaluation of breast carcinomas, normally including ER, PR and Her-2 estimation. The patients with ER positive tumors exhibiting Her-2 and/or cyclin D1 ampli¿cation and/or PR negativity may then be considered for adjuvant hormonotherapy other than tamoxifen. The study was supported from Czech Ministry of Health, No. NR 8270-3. 2020 Single agent in vitro drug sensitivity of molecular breast cancer subtypes de¿ned by gene expression analysis. Brase J, Schmidt M, Hengstler J, von Törne C, Kölbl H, Gehrmann M. University of Luebeck, Luebeck, Germany; University of Mainz, Mainz, Germany; University of Dortmund, Dortmund, Germany Background: Breast cancer is a heterogeneous disease for which a multitude of chemotherapeutic agents with different mechanisms of action are available. In neo-adjuvant studies gene signatures predictive for drug cocktails have been described. However, prediction with high accuracy remains a major challenge. In order to unravel response differences of individual drugs we combined gene expression pro¿ling of primary tumor tissues with an in vitro drug sensitivity model. Materials and Methods: Paclitaxel, Epirubicin, 5-Fluorouracil and Carboplatin were tested as single agents in a clinically relevant range of concentrations in an in vitro chemosensitivity assay (TCA-100; DCS, Innovative Diagnostic System, Hamburg, Germany) on cells isolated from 43 primary breast carcinomas. In addition, RNA was isolated from the primary tumor and gene expression pro¿ling was performed with Affymetrix HG-U133A microarrays. Unsupervised hierarchical clustering and prinicipal component analysis were applied to identify four molecular breast cancer subtypes. Drug sensitivity measured as area under the dose response curve was compared between subtypes by Kruskal-Wallis and Mann-Whitney tests. Results: Unsupervised hierarchical clustering and principal component analysis identi¿ed four major molecular subtypes, similar to the previously described luminal A, luminal B, stromal like and basal like subtype. We found that these subtypes could be classi¿ed with a small set of characteristic genes. ANOVA analysis revealed signi¿cant differences in drug sensitivity between the four molecular subtypes for Epirubicin (p = 0.002), Paclitaxel (p = 0.002), 5-Fluorouracil (p = 0.039) and Carboplatin (p = 0,025). The most striking difference was observed between basal and luminal A subtype for Epirubicin (p = 0.002) and Paclitaxel (p = 0.003). In contrast, these subtypes did not differ in sensitivity for 5-Fluorouracil and Carboplatin. Luminal B was more sensitive towards 5-Fluorouracil (p = 0.004) and slightly more sensitive for Paclitaxel (p = 0.053) and Carboplatin (p = 0,076) compared to the stromal like subtype. The inverse relation was seen for Epirubicin (p = 0.011). Discussion: Striking differences in drug sensitivity were seen between four major molecular breast cancer subclasses. The basal subtype was most sensitive towards Epirubicin and Paclitaxel but not 5-Fluorouracil, which was more active in the luminal B subtype. A larger study is needed to identify more subtle genetic differences and to elucidate the optimal combination of drugs for a given tumor. S91 2021 Tumour volume analysis. A better way than RECIST? Gordon AB, Stebbing J, Coombes C. Charing Cross Hospital, London, United Kingdom Background: RECIST – Response evaluation and criteria in solid tumours is the standard method of measuring complete response CR, partial response PR, stable disease SD and progressive disease PD. It utilises a single measurement as the longest diameter. Analysis of a true sphere may be calculated as volume = 4/3 Π r3. Many tumours are not truly spherical (one dimensional) but ellipsoid (two dimensional) or have three known dimensions. In a one diameter sphere the volume increases eight times when the diameter is doubled. This allows small increases in tumour diameter to become large changes in tumour volume. Volume becomes a more sensitive and accurate parameter to assess tumour response to treatment. Method: In partial response PR the RECIST guidelines are a 30% decrease in tumour diameter to be signi¿cant. In the case of a 2.0 cm diameter tumour (volume = 4.19 cm3) a 30% decrease is 6mm making a 1.4 cm tumour (volume 1.44 cm3). In fact a diameter reduction of 6mm (30%) becomes a volume decrease of 2.75 cm3 (74%). We are therefore underestimating the bene¿t of therapy. In the case of stable disease SD many patients will be in this group because a diameter change does not reach the RECIST 30%, although the volume would decrease by 30%. These cases would not be eligible as a response in Phase 2 clinical trials and the therapy discarded. In progressive disease PD the RECIST guidelines are 20% increase in diameter, in the case of a 2.0 cm tumour increases to become 2.4 cm. In fact the tumour volume has greatly increased from 4.19 cm3 to 7.25 cm3 (42%). New Material: A volume calculator is described for immediate assessment of a mass in cubic centimetres following measurement of diameter in centimetres. Tumour volume may be calculated in one, two or three dimensions UK Patent Application No. 0618342.0. This corrects for the clinical situation where few tumours are truly spherical. Discussion: RECIST and the WHO guidelines that preceded it both used diameter measurements in centimetres to assess response to therapy. It is demonstrated that volume analysis in cubic centimetres underestimates the bene¿t of therapy in partial response cases. Our treatments are more bene¿cial than we realised. It is proposed we express data as volume in cubic centimetres. Diameter and volume ¿gures. Diameter cm Volume cm3 Diameter cm Volume cm3 .4 .03 2.8 11.49 .6 .11 3.0 14.14 .8 .27 3.2 17.16 1.0 .52 3.4 20.58 1.2 .90 3.6 24.43 1.4 1.44 3.8 28.73 1.6 2.14 4.0 33.51 1.8 3.05 4.2 38.79 2.0 4.19 4.4 44.60 2.2 5.58 4.6 50.97 2.4 7.24 4.8 57.91 2.6 9.20 5.0 65.45 The volume has been calculated as: Vol = 4/3 r3 2022 Association of an extracellular matrix gene cluster with breast cancer prognosis and response to tamoxifen. Helleman J, Jansen MPHM, Sieuwerts AM, van Staveren IL, Ritstier K, Look MP, Meijer-van Gelder ME, Klijn JGM, Foekens JA, Berns EMJJ. Erasmus MC, Rotterdam, Netherlands Background: The expression of an extracellular matrix (ECM) gene cluster was previously found to be associated with response to ¿rstline tamoxifen therapy in metastatic breast cancer patients (Jansen et al J Clin Oncol 2006). This ECM gene cluster comprises six genes, collagen 1A1 (COL1A1), ¿bronectin (FN1), lysyl oxidase (LOX), secreted protein acidic cysteine-rich (SPARC), tissue inhibitor of metalloproteinase 3 (TIMP3) and tenascin C (TNC). In this study S92 Abstracts – Poster Session II we determined if these ECM genes are associated with response to tamoxifen monotherapy, metastatic potential, or both. Material and Methods: We have measured the ECM gene expression levels by real-time polymerase chain reaction in 1,286 primary breast tumor specimens. Expression levels were normalized to housekeeper gene levels and were analyzed as continuous variables in relation to clinicopathologic factors for all patients. In addition, in a multivariate analysis the expression levels were compared to traditional prognostic and predictive factors (age, menopausal status, tumor size, grade, LN status, ER, PgR, dominant site of relapse and disease-free interval). Results: TIMP3, FN1, LOX and SPARC expression was signi¿cantly associated with distant metastasis-free survival (MFS) in 680 lymph node negative untreated patients (p<0.03) indicating a relation of these ECM genes with metastatic potential, i.e. prognosis. The association of FN1, LOX and SPARC with MFS remained signi¿cant in multivariate analysis. Increased expression of TNC and FN1 was signi¿cantly associated with a shorter MFS in 145 lymph node and hormone receptor (ER and PgR) positive patients adjuvant treated with tamoxifen (FN1: HR=1.21, p=0.048, TNC: HR=1.42, p=0.004). For both genes multivariate analysis showed that the association with MFS was independent of prognostic factors. Interestingly, increased expression of TNC was also signi¿cantly associated with a shorter progression-free survival (PFS) in 298 patients who developed recurrent disease which was treated with tamoxifen monotherapy (HR=1.20, p=0.000). Multivariate analysis showed that the association of TNC with PFS was independent of predictive factors. Conclusion: High FN1, LOX and SPARC expression is associated with a worse prognosis for lymph node negative patients which is independent of traditional prognostic factors. Interestingly, TNC expression was not associated with prognosis while high expression did associate with resistance to tamoxifen treatment in the adjuvant as well as the advanced setting. Moreover, this association is independent of traditional prognostic and predictive factors. Additional studies are needed to con¿rm this outcome. 2023 Increased b1 integrin expression is a predictor of trastuzumab resistance in HER-2 overexpressing metastatic breast cancer patients. Thoms J, Sabri S, Lesniak D, Lai R, Deschennes J, Mackey J, Murray D, Abdulkarim B. University of Alberta, Edmonton, AB, Canada %DFNJURXQG: Trastuzumab (Herceptin) based chemotherapy, is standard of care in HER-2 (human epidermal growth factor receptor2) overexpressing metastatic breast cancer (MBC) patients. More than 50 % of HER-2 ampli¿ed MBC patients exhibit primary resistance to trastuzumab. Thus, the identi¿cation of new predictive markers of response to trastuzumab is crucial for appropriate patient selection for trastuzumab-based therapy. b1 integrin plays a major role in the proliferation, survival and invasion of carcinoma cells and its overexpression has been reported in JIMT-1, a breast cancer cell line established from a primary Trastuzumab resistant patient. To date, the predictive value of β1 integrin expression in trastuzumab resistance has not been investigated. 2EMHFWLYHV To investigate the value of β1 integrin expression in a population-based study of HER-2 overexpressing MBC patients treated with Trastuzumab-based therapy. 0HWKRGV We examined the expression of β1 integrin in a cohort of 85 MBC patients, treated in our institution with Trastuzumab-based therapy in the setting of metastatic disease during the period of 1998 – 2005 (December2005) Formalin-¿xed, paraf¿n-embedded breast tumors from these, specimens were analyzed by immunohistochemistry and scored for membranous and cytoplasmic β1 integrin staining (percentage of positive cells and intensity of staining) by two independent pathologists blinded to clinical outcome). The association between b1 integrin staining, conventional histological features (tumor size and grade, nodal status, hormone receptors, and lymphovascular invasion), overall survival (OS) and the time to tumor progression (TTP) was evaluated with univariate and multivariate analyses. 5HVXOWV The median OS is 17.8 months (14.6 - 20.3) and TTP is 6.7 months (5.6 - 8.5). High membranous β1 integrin staining (≥ 40% cells) was associated with signi¿cant decrease in OS and TTP. The median OS and TTP was 12.8 and 4.8 months in patients with high membranous β1 integrin staining versus 19.3 and 8.2 months, respectively in patients with low membranous β1 integrin staining (P < 0.0015). In a multivariate Cox proportional hazards model, membranous β1 integrin staining and tumor size (> 2.0cm) were independent prognostic factors for time to tumor progression (P = 0.0011). Strikingly, β1 integrin membranous staining alone was an independent predictor for survival in HER-2 overexpressing MBC patients treated with Trastuzumab therapy (P=0.001). &RQFOXVLRQ Our results show that β1 integrin overexpression has a powerful prognostic value to predict Trastuzumab response in HER-2 overexpressing breast cancer patients. This may be of a great signi¿cance, as HER-2 ampli¿cation/overexpression is currently the only clinical marker used to select patients for trastuzumab-based therapy. 2024 Preliminary results from I-SPY trial: tumor patterns on pre-treatment MRI predict breast conservation therapy eligibility. Gomez R, Hylton N, Madhavan S, Leung E, Broadwater G, Herman B, Esserman L, ISPY Radiology, Clinical & Pathology Investigators. UCSF, San Francisco, CA; NCI, Bethesda, MD; CALGB, Durham, NC; ACRIN, Providence, RI MRI patterns have been described which characterize tumor containment in women with locally advanced breast cancer (LABC). Previously, these patterns were shown to predict eligibility for breast conservation therapy (BCT) following neoadjuvant chemotherapy (NACT). Tumors that were more contained at diagnosis tended to achieve BCT eligibility more often. We sought to determine if MRI data from the I-SPY Trial, a correlative science trial in which LABC patients underwent NACT with serial MRI and biopsies, predicted BCT eligibility. Methods: Eligible patients with new primary breast cancer >3 cm were enrolled. All patients received anthracycline (AC)-based chemotherapy. Some received further treatment with taxane (T) or other agents. All patients had serial MRI at baseline (T1), after 1 cycle AC (T2), intraregimen (T3), and pre-surgery (T4). MRI patterns were de¿ned by a 5-point loss of containment (LOC) scale using the T1 MRI. Tumor patterns were de¿ned as follows: 1) single, unicentric, 2) multilobular, circumscribed 3) multinodular, 4) diffuse and 5) setpal. Eligibility for BCT following NACT was determined by a longest diameter (LD) <4 cm on the T4 MRI. Actual surgical treatment was individualized based on surgeon and patient preference. Results: 237 patients were enrolled at 9 institutions between 6/02-3/06. 15 patients withdrew or failed to complete the study. 18 patients had insuf¿cient data at the time of analysis on 5/14/07. 15 patients with tumors <4 cm in LD on baseline clinical exam and on T1 MRI were determined to be candidates for BCT prior to NACT and were not included in the analysis. 189 patients had tumors >4 cm in LD on either clinical exam or on T1 MRI (deeming them ineligible for BCT prior to NACT) and were included in the analysis. Patients were assigned MRI patterns according to the T1 MR. For patterns 1, 2, 3, 4, and 5 there were 28, 54, 60, 28, and 19 patients. After NACT, 65% patients were eligible to undergo BCT based on a T4 MR LD <4 cm. For patterns 1, 2, 3, 4, and 5, BCT eligibility was 21/28 (75%), 44/54 (81%), 34/60 (57%), 15/28 (54%), and 9/19 (47%). Only 61/189 (32%) eligible patients underwent BCT. Actual BCT rates by MR pattern were 12/28 (43%), 27/54 (50%), 14/60 (23%), 8/28 (28%), and 0/19 (0%) for patterns 1, 2, 3, 4, and 5. The majority of eligible patients (52%) and those that underwent BCT (61%) were patterns 1 or 2. Conclusions: 65% of patients with tumors >4 cm at diagnosis became eligible for BCT after NACT. MRI patterns were helpful in predicting who would achieve BCT eligibility. Well-contained lesions (types 1 and 2) tend to undergo a concentric size reduction, thus making these lesions more amenable to BCT. The lesser contained a tumor is on baseline MRI, the lower the likelihood that the tumor will respond so as to allow for BCT. This will help to set patient treatment expectations. Abstracts – Poster Session II 2025 Molecular markers as predictors of breast cancer response to adjuvant epirubicin-CMF chemotherapy in the BR9601 trial. Bartlett JM, Munro AF, Cameron DA, Thomas J, Prescott R, Twelves C. University of Edinburgh, Edinburgh, United Kingdom; Western General Hospital, Edinburgh, United Kingdom; University of Bradford, Bradford, United Kingdom Background: A number of studies have sought to identify which patients gain most from the clear additional bene¿t seen with the adjuvant use of anthracyclines. We tested the hypothesis that HER2, EGFr and HER3, Ki67 (proliferation) or topoisomerase (TIIa) expression are predictive of outcome on anthracycline-based chemotherapy in breast cancer. Methods: Tissue microarrays from 322 patients recruited to the BR9601 trial which compared ECMF with CMF were analysed for protein expression & HER2 ampli¿cation. Relapse free (RFS) and overall survival (OS) was performed by Kaplan Meier and Cox’s multiple regression tests identi¿ed treatment by marker interactions. Results: HER2 normal cases exhibited improved RFS when treated with ECMF vs CMF (HR = 0.49; p<0.01) vs. CMF. Tumors with normal HER1, HER2 (FISH) or HER3 levels exhibited signi¿cantly improved RFS (HR 0.37, p =0.005) & OS (HR 0.31, p<0.005) on ECMF vs. CMF treatment. No difference in RFS or OS was seen in HER1-3 overexpressing cases treated with ECMF vs. CMF. Cox’s regression established signi¿cant treatment by marker effects for RFS & OS (p<0.05). Neither Ki67 nor TIIa showed predictive value. Conclusion: Although these data con¿rm an interaction between HER2 (and HER1-3) status and anthracycline bene¿t, the results contrasts with the DBCSG and MA5 studies. Differences in treatment regimens, total anthracycline exposure and scheduling might be responsible, but what these results do suggest is that caution is required before combining different studies for meta-analyses and in interpreting results from individual studies across different treatment regimens. 2026 Identification of molecular predictors of response of advanced breast cancer patients to aromatase inhibition. Haynes B, Ghazoui Z, Anderson H, Dunbier A, Dexter T, Mackay A, Smith IE, Dowsett M. Royal Marsden Hospital, London, United Kingdom; The Breakthrough Toby Robins Breast Cancer Research Centre, London, United Kingdom Background: Aromatase inhibitors (AI) have greater ef¿cacy than tamoxifen in all stages of ER+ breast cancer in postmenopausal women. However, whilst several gene expression studies have identi¿ed markers of prognosis and response to tamoxifen, very few studies have investigated gene expression in relation to the clinical response of breast cancer patients to an AI. Our aim was to identify genes and gene pathways that are differentially expressed in the primary tumours of responders and non-responders to AI therapy for advanced disease. Methods: Tumours were selected from our liquid nitrogen bank if they were ER+ and the patient had received no neo-adjuvant therapy before surgery and was treated with letrozole or anastrozole for advanced disease. RNA was extracted and gene expression pro¿ling performed on Breakthrough 20K cDNA microarrays. Patients were categorised as responders (CR, PR or SD > 6 months) or non-responders. Genes that were differentially expressed between the two groups were identi¿ed by class comparison analysis. Proportional hazards models identi¿ed genes whose expression was signi¿cantly related to time-to-treatment failure. Gene ontology and pathway analysis was performed to identify functional groups of genes that correlated with response. Quantitative real-time PCR (QPCR) was used to con¿rm microarray ¿ndings for selected genes. Results: 58 tumours were analyzed (mean patient age at diagnosis 56 years, mean tumour size 2.6cm). Class comparison analysis identi¿ed 693 genes (at p < 0.01) that were differentially expressed between responders and non-responders. The most signi¿cantly differentially expressed gene was HSD17B7 which was con¿rmed by QPCR to be 1.97-fold higher in responders. This gene encodes one of the two isoforms of the 17β-hydroxysteroid dehydrogenase enzyme (17βHSD) that is primarily responsible for the formation of estradiol from estrone within the breast. AKR1C3 (aldo-keto reductase family 1, member S93 C3), a gene which possesses 17βHSD activity and correlates with aromatase expression, was also signi¿cantly up-regulated in responders. Pathway analysis showed the androgen-estrogen metabolic pathway to be signi¿cantly different between responders and non-responders (p < 0.0001). Other genes and pathways/molecular processes that showed signi¿cance included antigen processing and presentation (PSMB5, HLA-B), a lymphocytic signature (HPS5, ITGAL) and polyamine metabolism (ASS1, SAT1). Discussion: We have used an integrative approach to identify candidate genes and gene pathways predicting response to AI in advanced breast cancer and are subjecting these to further study in complementary sample sets. The presence of multiple pathway members among the signi¿cant genes suggests that global measures of activity of the androgen-estrogen pathway may provide stronger predictors than the individual genes. Supported by the Breast Cancer Research Foundation and Breakthrough Breast Cancer. 2027 Diet, lifestyle, and BRCA-related breast cancer risk among French-Canadian. Ghadirian P, Nkondjock A, Robidoux A, Narod S. University of Montreal, Epidemiology Research Unit, Research Centre CHUM, Hôtel-Dieu, Montreal, QC, Canada; CHUM, Hôtel-Dieu, Montreal, QC, Canada; Women’s College Hospital – University of Toronto, Toronto, ON, Canada Background: Although the connection between diet, lifestyle and hormones suggests that nutritional and lifestyle factors may exert an inÀuence in the etiology of breast cancer (BC), it is not clear whether these factors operate in the same way in women with BRCA1 and BRCA2 (BRCA) gene mutations who already have an elevated BC risk. Methods: A case–control study was conducted within a cohort of 80 French-Canadian families with 250 members involving 89 carriers of mutated BRCA gene affected with BC and 48 non-affected carriers. A validated semi-quantitative food frequency questionnaire was used to ascertain dietary intake, and a lifestyle core questionnaire, to gather information on physical activity and other lifestyle risk factors. Odds ratios (ORs) and 95% con¿dence intervals (CIs) were calculated in unconditional logistic regression models. Results: After adjustment for age, maximum lifetime body mass index (BMI) and physical activity, a positive association was found between total energy intake and BRCA-related BC risk. OR was 2.76 (95%CI: 1.10–7.02; p=0.026 for trend), when comparing the highest tertile of intake with the lowest. The intake of other nutrients and dietary components was not signi¿cantly associated with the risk of BC. Age at the time the subjects reached maximum BMI was signi¿cantly related to an elevated BC risk (OR=2.90; 95%CI: 1.01–8.36; p=0.046 for trend). In addition, a direct and signi¿cant relationship was noted between maximum weight gain since both age 18 and 30 years and BC risk. The ORs were 4.64 (95%CI: 1.52–14.12; p=0.011 for trend) for weight gain since age 18 years and 4.11 (95%CI: 1.46–11.56; p=0.013 for trend) for weight gain since age 30 years, respectively. No overall association was apparent between BRCA-related BC risk and BMI, smoking, and physical activity. Conclusion: The results of this preliminary study suggest that weight control in adulthood through dietary energy intake restriction is an important factor for the prevention of BRCA-related BC risk. 2028 Milk products are a source of dietary progesterone. Goodson III WH, Handagama P, Moore II DH, Dairkee S. California Paci¿c Medical Center Research Institute, San Francisco, CA Much of the increase in breast cancer over the last 30 years is thought to be hormone related. Menopause hormone replacement therapy (HRT) explains some of the increase, but HRT does not explain other hormone-related events associated with breast cancer risk, e.g. earlier menarche. Thus, other causes of early or life-long feminization are relevant to understanding breast cancer risk. We reasoned that hormones in dairy products might be a lifelong S94 Abstracts – Poster Session II source of feminizing hormones: in current dairy practice, milk cows are maintained in the pregnant state; and elevated progesterone levels in milk can be used to identify pregnant dairy cows (J Dairy Sci 1976;59:1528). To test whether progesterone absorbed from dairy products might influence biological outcome, we measured bioavailable progesterone levels after short-term consumption of high-fat dairy products. Methods: With IRB approval, salivary progesterone levels were measured in ¿ve healthy males (BMI 21.6 to 26.2, age 27 to 61 years) before and after 24 hours of a high-fat dairy diet. We tested saliva because a.) saliva progesterone levels reÀect bio-available hormone not bound to serum proteins, and b.) repeated sample collection is free from discomfort. We studied males because their baseline progesterone levels are low and relatively constant. We focused on common highfat dairy products since milk hormones are known to partition into the fatty components. After an evening saliva sample, subjects were asked to consume similar amounts of butter with breakfast the next day, cheese with lunch, and ice cream after lunch, prior to an afternoon saliva collection. Sampling was repeated one week later. Samples were collected in duplicate. Salivary progesterone was measured by radioimmunoassay in a commercial laboratory. Results: Salivary progesterone increased 22 to 116 percent in all subjects both times after 24 hours of a high-fat dairy product diet (p=0.043). Salivary progesterone decreased 48 hours after the end of the high-fat dairy diet (p=0.22) and returned to baseline levels in most subjects by one week (¿gure 1). superoxide dismutase (SOD), catalase and lipid peroxidation of cardiac tissue and plasma were determined using speci¿c assays. Caspase-3 activation and expression of alpha-actin, and HSP70 were determined by western bloting Results: GLN supplemented rats lost signi¿cantly less weight and had reduced tumor weight and volume vs. water gavaged rats. The pathohistological alterations increased with the increase of DOX dose but were signi¿cantly less severe in GLN-supplemented rats. GLN supplementation resulted in enhanced plasma antioxidant capacity, increased GPx and higher GSH regardless of DOX dose. At the same time GLN lowered cardiac lipid peroxidation and had no effect on on SOD and catalase. Conclusion: These results indicate that dietary GLN stimulates the antioxidant property of both plasma and cardiomyocytes of a tumor-bearing host treated with DOX. This effect of GLN is a result mainly from the increased GSH synthesis and not by the other natural antioxidants (such as SOD and catalase), supporting our hypothesis that the bene¿cial effect of GLN supplementation during conditions of oxidative stress is mainly through modulation of GSH metabolism. The increased antioxidant capacity of cardiomyocytes is able to counteract cardiac lipid peroxidation caused by DOX and thus can protect the heart from the oxidative damages. This data further con¿rmed the safety of GLN supplementation in a tumor-bearing host and its cardioprotective effects during chemotherapeutic treatment with DOX. Acknowledgements: This work was supported by a grant from Susan G. Komen to VKT. 2030 Effects of Korean red ginseng on the concentration of blood estrogen, leptin and urinary excretion of estrogen metabolites in postmenopausal women. Discussion: Early breeding of dairy cows was instituted in the mid 20th Century to increase production. We demonstrate that the resulting progesterone in high-fat dairy products is rapidly absorbed leading to a detectable increase in bio-available progesterone in individuals consuming such products. Given the magnitude of milk use, we must consider the possibility that a single change in food production technology might have a major inÀuence on the health of young persons who, with the best of intentions, are encouraged to drink milk. 2029 Cardioprotective effects of oral dietary glutamine in tumorbearing rats treated with doxorubicin. Todorova VK, Kaufmann Y, Klimberg VS. University of Arkansas for Medical Sciences, Little Rock, AR; Central Arkansas Veterans Healthcare System, Little Rock, AR Background: Previous data indicated that dietary glutamine (GLN) could prevent cardiac lipid peroxidation of rats treated with doxorubicin (DOX). The present study aimed to further examine the effect of oral GLN on cardiotoxicity of DOX in rats with mammary carcinoma. Materials and Methods: Female Fisher 344 rats (n=85) randomized into 5 groups: (i)MatBIII implantation + DOX + GLN gavage (n=20), ii)MatBIII implantation + DOX + water gavage (n=20), iii)DOX + GLN gavage (n=20); iv)DOX + water gavage (n=20); v)naive control (n=5), gavaged with GLN (1g/kg) or water were implanted with rat mammary adenocarcinoma cells (MatBIII). After tumor development the rats were treated i.p. with 4, 9, 12, 16 and 20 mg/kg DOX. Cardiac histological damage was determined in H&E stained paraf¿n slides. Total antioxidant capacity, GSH, glutathione peroxidase (GPx), Kang SH, Lee SJ, Baek NW, Kim EM. Yeungnam University Medical Center, Daegu, Korea Purpose: To evaluate the effect of ginseng administration on the endogenous hormonal environment, we measured blood estrogens, hormones and urinary estrogen metabolites which proven to be linked to breast cancer risk, in postmenopausal Korean women before and after Korean red ginseng supplemental administrations. Material and method: A randomized, blind, placebo-controlled crossover study was used. Forty three healthy postmenopausal women of average age 56.9 year were recruited and 25 of these women completed the study. The participants were randomly assigned to either ginseng supplemental group or placebo control group. Ginseng group were administered 1.2 gm of Korean red ginseng extracts per day and placebo group were administered a placebo without ginseng daily for 8 weeks. After a one month washout period with no medications, participants were crossed over (into either the ginseng or placebo group), and experimental procedure were repeated for 8 weeks. Serum and urine samples were obtained at immediate before and after each 8 week treatment period. Each samples were send to laboratory to measure serum E1, E2, LH (leuteinizing hormone), FSH (follicular stimulating hormone), SHBG (sex hormone binding globulin), TG (triglyceride), insulin, leptin and urinary 2OHE1 (2-hydroxyestrone) and 16αOHE1 (16α-hydroxyestrone). The effects of Korean red ginseng extract on blood estrogen and on urinary excretion of estrogen metabolites were compared with placebo. Results: There was no signi¿cant group difference for any demographic parameter (age, height, body weight, body mass index, fat content) and baseline level of serum E1, E2, LH, FSH, SHBG, TG, insulin, leptin and urinary 2OHE1/16αOHE1. And there were no signi¿cant changes in demographic parameters after both placebo and red ginseng treatment periods. Compared with placebo condition, the concentration changes of serum E1, E2, LH, FSH, SHBG, TG, insulin, leptin and urinary metabolites are not signi¿cantly different in Korean red ginseng extracts treatment group (p>0.05). Conclusion: We found that supplemental administration of daily dose of 1.2 gm of Korean red ginseng extract for 2 months did not change the endogenous hormonal levels proven to be linked to breast cancer risk signi¿cantly. Abstracts – Poster Session II 2031 Breast cancer survivors who use selected herbal supplements have lower circulating estradiol and free estradiol: the Health, Eating, Activity and Lifestyle study. Wayne SJ, Koprowski C, Neuhouser ML, Ulrich CM, Bernstein L, Gilliland F, Wiggins C, Baumgartner K, Baumgartner R, McTiernan A, Ballard-Barbash R. University of New Mexico, Albuquerque, NM; University of Southern California, Los Angeles, CA; Fred Hutchinson Cancer Research Center, Seattle, WA; National Cancer Institute, Bethesda, MD A high proportion of breast cancer survivors use herbal supplements. A number of these supplements have estrogenic properties that may inÀuence serum hormone levels, although conÀicting evidence exists about the magnitude and direction of this inÀuence. The estrogenic nature of these herbs may increase serum levels of estrogen or, conversely, may reduce circulating estrogen levels by inhibiting enzymes involved in estrogen biosynthesis and metabolism. We evaluated the relationship between estrogenic supplements and serum hormone levels among participants in the Health, Eating, Activity and Lifestyle (HEAL) study, a population-based, multi-center, prospective cohort study of breast cancer prognosis. Questionnaire data from 541 postmenopausal breast cancer survivors were obtained, on average, 31 months after diagnosis of breast cancer. The questionnaire asked for information on use of dietary supplements, including herbal preparations. Concurrently a fasting blood sample was drawn. Serum hormone data were logtransformed, and women taking hormone replacement therapy were excluded from these analyses. Seventeen supplements were identi¿ed as having estrogenic properties: astragalus, alfalfa, black cohosh, burdock root, cat’s claw, chaste berry, dehydroepiandrosterone, Àax, fo ti tieng, ginseng, licorice, nettles, red clover, saw palmetto, soy, turmeric, and yam. Thirty-¿ve percent of study participants reported use of at least one estrogenic supplement. Use of estrogenic supplements was signi¿cantly associated with younger age, higher education, increased physical activity, and Hispanic or Black race/ethnic classi¿cation. After controlling for these factors plus adjustments for tamoxifen use, body mass index and number of ovaries, participants taking any estrogenic supplement had signi¿cantly lower levels of estradiol (13.4 pg/mL v 15.4, p = 0.04) and free estradiol (0.30 pg/mL v 0.36, p = 0.01) than participants not taking estrogenic supplements. Estrone, testosterone, free testosterone, and dehydroepiandrosterone sulfate were lower and sex hormone-binding globulin higher in participants taking estrogenic supplements, but these differences were not statistically signi¿cant. It is possible that women who took estrogenic supplements did so because they had a lower level of some sex steroids and consequently had more estrogen withdrawal symptoms. However, these data suggest that use of estrogenic supplements may alter some sex hormone concentrations in breast cancer survivors. Considering the high use of these supplements among breast cancer patients, further research is needed to clarify the relative estrogenicity/antiestrogenicity of these compounds and their relation with prognosis. 2032 Toward individualized risk prediction: the clinical bene¿t of risk reduction mastectomy and oophorectomy in %5&$ carriers with breast cancer. Burke HB, Hoang A, Metcalfe K, Culver JO, MacDonald DJ, Grant M, Thornton A, Robson M, Narod S, Weitzel JN. George Washington University, Washington, DC; University of Toronto, Toronto, ON, Canada; Memorial Sloan Kettering CA Ctr, New York, NY; City of Hope, Duarte, CA Background:Breast cancer patients with a BRCA mutation have a markedly elevated risk for new cancers. Health care providers must communicate complex information about risk-reducing surgeries. We created models that provide individualized 5-year breast cancer survival and contralateral breast cancer predictions and the bene¿t of risk reduction mastectomy (RRM) and oophorectomy (RRSO). Method: The study population was 491 women treated for stage I or II breast cancer between 1975 and 2000 and who had a known mutation or were from a family with a documented mutation (BRCA1, n = 327; BRCA2, n = 152; both BRCA1 and BRCA2, n = 12). The independent variables S95 were age (less than 50 years old vs. 50 years old or older), tumor size (continuous variable), ER status (present vs. absent), and lymph node status (present vs. absent). Logistic regression was used to create the model. The output of one model was the probability of each outcome for RRM, and the output of the other model was the probability of each outcome for RRSO. Accuracy is assessed by the ROC. Results: See Table Below. Conclusion: In this population of women who had breast cancer and were BRCA positive, we found that, with the exception of RRSO and risk of contralateral breast cancer, the models were highly accurate predictors of the two outcomes. An unexpected ¿nding was the bene¿cial effect of RRSO on breast cancer survival. These are preliminary results and await validation on an independent dataset. The individualized output of the predictive models will then be incorporated into a decision support tool for use in cancer risk counseling. Results Risk reduction Risk reduction mastectomy (RRM) salpingo-oophorectomy (RRSO) 5-year breast Model ROC = 0.707 RRM Model ROC = 0.804 RRSO cancer-speci¿c survival was not signi¿cant was signi¿cant 5-year contralateral Model ROC = 0.749 RRSO Model ROC = 0.611 RRSO breast cancer was signi¿cant was not signi¿cant The 5-year breast and ovary cancer-speci¿c survival model did not differ signi¿cantly from the 5-year breast cancer-speci¿c survival model and is not reported here. 2033 A BRCA1 or BRCA2 mutation and young age predict fast breast cancer growth. Implications for screening? Tilanus-Linthorst MM, Obdeijn I-M, Hop WC, Causer P, Leach MO, Warner E, Pointon L, Hill K, Klijn JG, Warren RM, Gilbert FJ. Erasmus University MC, Rotterdam, Netherlands; Sunnnybrook & Women’s Health Sciences Centre, Toronto, Canada; Institute of Cancer Research and Royal Marsden NHS, Sutton, Surrey, United Kingdom; Addenbrooke’s Hospital and University, Cambridge, United Kingdom; University of Aberdeen, Aberdeen, United Kingdom Purpose Breast cancers of young women with an inherited predisposition can be detected at an early stage by MRI screening. Interval cancers were described in BRCA1 mutation carriers, possibly because their tumours grow fast. We investigated the inÀuence of a BRCA1 or BRCA2 mutation and age on the growth rate of breast cancers, as this inÀuences the optimal screening frequency. Methods To assess tumour growth rate, we reviewed 100 invasive cancers from the UK, Dutch and Canadian MRI screening trials for women at hereditary risk, measuring tumour size at diagnosis and on preceding MRI and/or mammography. Results In 43 BRCA1, 16 BRCA2 mutation carriers, and 41 women with high familial risk we calculated tumour volume doubling time. Growth was twice as fast in BRCA1 (p 0.003) and BRCA2 (p 0.03) mutation carriers than in high risk patients of the same age. Growth slowed down with increasing age (p 0.004) by a factor of 1.6 with each 10 years (range 27-67 yrs). With yearly imaging, pathological tumour size decreased with increasing age (p 0.001). Median tumour size was 15 mm at or below 40 years compared to 9 mm in older patients (p 0.003). In young BRCA1 patients tumour size was largest Conclusion Tumours grow more quickly in younger women and in BRCA1 and BRCA2 mutation carriers than in high risk women. With yearly screening tumours were largest in young BRCA1 mutation carriers, S96 Abstracts – Poster Session II therefore age and risk group should be taken into account when recommending screening frequency and for follow-up imaging. Numbers, geometric mean DT, average breast density and tumor pathology size of the 100 invasive cancers per age and risk group 40 years 41-50 years > 50 years p-value n=31 n=42 n=27 Nr. BRCA1/2 23 24 12 Nr. High Risk 8 18 15 28 83 2.6 68 121 2.5 81 173 2.0 0.039 0.014 0.03 15 (4-40) 15 (4-40) 11.5 (4-20) 10 (4-42) 9.5 (4-35) 10 (6-42) 9 (4-27) 8.5 (4-25) 9 (5-27) 0.009 0.016 0.45 Mean DT BRCA1/2 High Risk Mean Density total group Median Pathology size Total group BRCA1/2 High Risk * p for the difference in geometric mean DT between the three age groups adjusted for study center ** Mean density at a 4 point scale. Mean value would be 2.5 with equal numbers 50% and > 50% density. 2034 Breast carcinoma LQVLWX and the prevalence of %5&$ and %5&$ mutations in a large commercial database. Hall MJ, Reid JE, Noll WW, Frye CA, Burbidge LA, Wenstrup RJ. Herbert Irving Comprehensive Cancer Center, New York, NY; Myriad Genetic Laboratories, Inc., Salt Lake City, UT Background: The prevalence of BRCA1/2 mutations in women with breast carcinoma in situ remains controversial. The aim of this study was to assess the prevalence of BRCA1 and BRCA2 mutations in women with a diagnosis of breast carcinoma in situ who have undergone genetic testing by a large commercial laboratory. Methods: Between March 1996 and December 2006, full sequence DNA analysis of BRCA1 and BRCA2 and, since August 2002, break point analysis for five large genomic rearrangements in BRCA1 (exon13del3835bp, exon13ins6kb, exon14-20del26kb, exon22del510bp and exon8-9del7.1kb) was performed on individuals referred to our laboratory for genetic testing. For the current study, only individuals who indicated a personal history of breast cancer in situ and no history of breast or ovarian cancer were analyzed. Demographic, personal, and family cancer histories were requested from each tested individual and collected by way of a test requisition form (TRF) included in each testing kit. Individuals were also required to have a de¿nitively positive or negative familial cancer history in a ¿rst- or second-degree relative (those with missing family history data were not included). Odds ratios were calculated by Fisher’s Exact Test. Results: In total, 4,452 individuals reported a personal cancer history of only breast cancer in situ (3,435 Non-Ashkenazi, and 1,017 Ashkenazi(AJ)). Of these, 279/3435 (8.1%) women of non-AJ ancestry had a deleterious BRCA1/2 mutation. In AJ, 65/1017 (6.4%) carried a BRCA1/2 mutation. Non-AJ with in situ breast cancer <50 had an increased risk of a BRCA1/2 mutation compared to those women without breast or ovarian cancer [OR = 1.4, 95% CI 1.21-1.64, p<0.0001], but this was not the case for women ≥50 [OR = 0.58, 95% CI 0.41-0.79, p=0.0004]. Interestingly, BRCA2 mutations were seen more commonly than BRCA1 (ratio 41% to 59% BRCA1 to BRCA2 for AJ and non-AJ women combined). This is in contrast to the 67% to 33% ratio (AJ) and 56% to 44% ratio (non-AJ) seen associated with invasive breast cancer. Conclusions: Breast carcinoma in situ is a manifestation of the BRCA1/2-associated hereditary breast and ovarian cancer syndrome. Women with breast cancer in situ referred for genetic testing are at high risk for carrying a germline BRCA1/2 mutation. In light of these ¿ndings and a recent population-based study (Claus et al, JAMA 2005), women <50 with breast cancer in situ and a family history of breast or ovarian cancer should consider BRCA1/2 genetic testing. 2035 Lifetime risk for breast and ovarian cancer in postmenopausal BRCA carriers: cause for concern? Tice JA, Crawford B, Ziegler J, McLennan J, Beattie M. UCSF, San Francisco, CA Background: Older women who test for BRCA mutations commonly are motivated by their concern for their children. Data regarding cancer risk and uptake of risk-reducing surgeries in BRCA carriers who undergo testing at age 55 and older is scant. Methods: Participants in the UCSF Cancer Risk Program are recruited from UCSF, satellite clinics, and from family members who attend these clinics. All participants agree to a unique 20 year IRB approved follow-up protocol. To investigate cancer risk, we preformed KaplanMeyer analyses for incidence of breast and ovarian cancer among known BRCA carriers who are unaffected at age 55. Women were censored at the time of mastectomy, oophorectomy, or death. The analysis presents results to age 80, although the life expectancy of a 55 year old woman in 2007 is greater than 25 years. To investigate uptake of risk-reducing mastectomy and risk-reducing oophrectomy, we used Cox proportional hazard analyses. Results: Our cohort includes 152 BRCA carriers (97 BRCA1 and 56 BRCA2). The risk to age 80 for breast cancer was 35% for BRCA1 carriers and 48% for BRCA 2 carriers who were unaffected at age 55. Similarly the lifetime risk for ovarian cancer was 65% in BRCA1 carriers and 35% in BRCA2 carriers. Uptake of risk reducing mastectomy was 10% in women 55 and over, while uptake of risk reducing salpingo-oophorectomy was 17% in women 55 and over. Compared to women under 55, the relative hazard of RRM was 0.3 (0.1-.5) and the relative hazard to RRSO was 0.6 (.2-.9). Conclusion: BRCA1 and 2 carriers who are unaffected at age 55 are at very high lifetime risk for both breast and ovarian cancer. Intensive screening and consideration of prophylactic surgeries are as relevant for these women as they are for women at age 35. 2036 BRCA1- and BRCA2-associated breast cancer is more sensitive to standard chemotherapy for metastatic disease in comparison with sporadic breast cancer. Kriege M, Seynaeve C, Meijers-Heijboer H, Collee M, Menke-Pluymers MBE, Bartels CCM, van den Ouweland A, van Geel B, Hooning M, Brekelmans CTM, Klijn JGM. ErasmusMC-Daniel den Hoed Cancer Center, Rotterdam, Netherlands Background: Preclinical as well as small, retrospective, neo-adjuvant studies suggest that ovarian and breast cancer (BC) (cells) without functional BRCA1- or BRCA2-protein are particularly sensitive to DNA-damage based chemotherapy, such as anthracyclin- and platinum-containing regimens. In this study we assessed the response to chemotherapy of BRCA1- and BRCA2-associated patients with metastatic breast cancer (MBC). Data hereon are not yet available. Materials and methods: We selected 82 consecutive BRCA1- and 24 BRCA2-associated BC patients with MBC (treated between 1973 and 2006). Cases were matched for year of birth, year of BC diagnosis and Abstracts – Poster Session II year of diagnosis of MBC (within 5-years periods) with sporadic BC patients. Response rate (RR) and progression free survival (PFS) after ¿rst line chemotherapy for MBC in BRCA1- and BRCA2-associated patients versus sporadic BC patients were assessed. Results: Mean age at BC diagnosis was 40.4 years (range 23.8-65.7), and at diagnosis of MBC 44.8 years (range 25.9-79.8), not being signi¿cantly different between the three patient groups. Chemotherapy for MBC was thus far administered to 64/82 BRCA1-associated (78%), to 23/24 BRCA2-associated (96%), and to 91/106 sporadic patients (86%). The mainly used chemotherapy regimens were CMF /CMF-like (n=50), anthracyclin-based (n=108), taxane-based (n=12), platinumbased (n=4), and other regimens (n=4). RR and PFS were not evaluable in 9 patients (5 BRCA1, 1 BRCA2, 3 sporadic), because of early stop of treatment. The RRs to ¿rst line chemotherapy (see Table 1) were higher in both the BRCA1- (71%; p=0.07) and the BRCA2-associated group (86%, p=0.03) than in the sporadic group (51%). Table 1. Response rate to chemotherapy BRCA1 N % Response Rate 42 71 Stable Disease 10 17 Progressive Disease 7 12 Mixed Response Unknown BRCA2 N 19 2 1 % 86 9 5 Sporadic N 43 18 21 2 4 % 51 22 25 2 PFS was better for BRCA1- and BRCA2-associated as compared to sporadic breast cancer. Hazard Ratio (HR) for the risk of progressive disease was 0.70 (95% con¿dence interval (CI) 0.49-0.99) for BRCA1-, and 0.49 (95% CI 0.30-0.78) for BRCA2-associated, as compared to sporadic MBC. Conclusion: BRCA1- and BRCA2-associated BC patients have a higher response rate to and a longer PFS on ¿rst line standard chemotherapy modalities for MBC as compared to sporadic patients. Whether this may result in a prolonged post-relapse overall survival is under analysis. Further analysis will also stratify for different regimens and taking administration to hormonal therapy in account. 2037 BRCA mutation in Chinese population: preliminary results from the Hong Kong hereditary and high risk breast cancer programme. Kwong A, Wong CLP, Ma E, Ford JM. The University of Hong Kong; Hong Kong Santorium and Hospital, Hong Kong; Stanford University, CA Background: Little is known about the frequency and spectrum of BRCA 1/2 mutations among Chinese population. Previous research suggests possible differences in the prevalence and penetrance of these mutations among Asians versus Caucasians. Reports have suggested earlier presentation of breast cancer in Asian population may have more relevance to genetic causes. The Hong Kong Hereditary and High Risk Breast Cancer Programme was established in January 2007. This provides clinical testing, genetic counseling and research on the prevalence and spectrum of the mutation in Chinese population. The data will be entered in a newly established The Hong Kong Hereditary Breast Cancer Family Registry. Methods: Probands diagnosed to have breast cancer age 50 or below, have a family/personal history of breast and/or ovarian cancer, bilateral breast cancer, male breast cancer, and triple negative breast carcinoma were recruited. Genetic counseling was given and consent were obtained. Blood samples were collected and processed for DNA and RNA extraction. The entire coding regions and Àanking introns of BRCA1/2 were screened for germline mutations using full gene sequencing and Multiplex Ligation –dependent Probe Ampli¿cation (MLPA). RNA analysis was performed on suspicious variant to con¿rm pathogenicity. Results: 110 blood samples have been collected of which 29 has been sequenced and analysed to date. 10 deleterious mutations were identi¿ed. 2 were novel mutations. 7 of the 10 mutations found were BRCA 2 mutations. 8 other variant of unknown signi¿cicance (VUS) were also identi¿ed. Conclusions: Approximately 1/3 of tested Chinese women carry a deleterious mutation in BRCA1/2. In contrast to Caucasian data, a majority (70%) were BRCA 2 mutations. 28% of the tested women S97 carried VUS. With a highly selective inclusion criteria, a high yield of BRCA mutations were found. Further research on these variants and spectrum of the mutations in Chinese population has important implications on clinical management. Table1: BRCA1 and BRCA 2 deleterious mutation and VUS identi¿ed in Hong Kong Chinese FH of breast /ovarian FH of other BRCA1/2 Age BRCA1/2 VUS cancer cancers /type Mutation Carriers 60 Breast 38 Breast 39* Ovarian 50* Breast 50 Breast BRCA2 Exon 11, c.3109C>T BRCA2 Exon 11, 5164_5delAG BRCA2 Exon 18, Stomach, tongue, 8047-8054 dup larynx GCAAAAAAC BRCA2 Intron Stomach c.7806-9T>G BRCA 2 Exon11, c.3109C>T BRCA2 Exon 11, c.5851_5854delAGTT 57 Breast 45 Unknown - 65 Unknown - 48 No - 39 No - 52 Breast 26 No 54 Ovary 33 Breast 26 No 36 No 37 No - Laryngeal BRCA1 Exon 11, c.2635G>T BRCA2, c.3337 C>T BRCA1, c.589delCT BRCA1, c.4491C>T - Liver, Cervix - BRCA1 Exon 18, c.5271+66G>A BRCA1 Exon 18, c.5271+66G>A BRCA1 Exon 18, c.5271+66G>A BRCA1 Exon 18, c.5271+66G>A BRCA1 Exon 11 c.2726A>T BRCA2 Exon 5, c.440A>G BRCA2 Exon 5, c.440A>G *=Novel Mutation 2038 The CHEK2*1100delC variant: present in the west of Ireland breast cancer population. Colleran GC, Rowan A, Miller N, Sawyer E, Curran C, Kerin M, Tomlinson I. National University of Ireland Galway, Galway, Ireland; London Research Institute, Cancer Research UK, London, England, United Kingdom Background: As part of a population-based approach to breast cancer genetics, a West of Ireland cohort is under study to elucidate inherited variation which predisposes women to developing breast cancer. Due to the West of Ireland’s geographical location on the western edge of Europe the genetics of this population has been relatively undisturbed by the demographic movements that have shaped variation on mainland Europe and the USA.[1] Consequently, the West of Ireland population is relatively homogenous and amenable to case-control analysis. It is thought that several common low penetrance genes account for the non-BRCA associated genetic susceptibility to breast cancer.[7] These genes are likely to be inherited in a polygenic model whereby genes interact with each other and/or with the environment to induce their carcinogenic effects. CHEK2 has been identi¿ed as a low-penetrance breast cancer susceptibility gene conferring a two fold elevated risk of breast cancer in women and ten fold in men.[8] In addition, case-control studies have identi¿ed that germline mutations in CHEK2 (*1100delC) are associated with increased risk of breast, prostate and colorectal cancer in Dutch [9] and Finnish [10] populations. Its prevalence varies within ethnic groups and populations and its potential role in breast cancer aetiology in Irish patients has yet to be elucidated. Materials and Methods: To evaluate the prevalence of the CHEK2*1100delC variant, DNA collected from 591 breast cancer cases and 572 healthy controls was analysed. Patients were recruited from 2 af¿liated hospitals in the west of Ireland. Female controls had no personal history cancer, no family history of breast cancer and were over 60 years of age. Male controls had no personal history cancer, no family history of breast cancer. FAM (carboxyÀuorescein) labelled PCR products were capillary separated on the ABI 3700 and fragment analysis carried out using Genotyper v2.5. Normal PCR fragments measures 168bp and the CHEK2*1100delC could be clearly seen at S98 Abstracts – Poster Session II 167bp. A sequenced control CHEK2*1100delC patient DNA was PCR ampli¿ed for each test reaction. Results: The CHEK2 *1100delC mutation was found in three cases. The mutation was not found in any of the control samples. Of the three mutation carriers, one had a sibling who was affected with colorectal cancer. Discussion: We have established that the CHEK2*1100 delC variant is present in the Irish population and is in excess in cases over controls. CHEK2 mutations confer a two fold elevated risk of breast cancer in women and ten fold in men.[8] Our data are consistent with effect on risk. Given the emergence of other low penetrance genes including BRIP1[11] and ATM[12] their role in the clinical setting of screening and risk assessment and the public awareness of these developments necessitates revised guidelines in this area to assist clinicians managing breast cancer patients. References available on request. 2039 Addressing the needs of men in BRCA1/2 families. Daly MB. Fox Chase Cancer Center, Philadelphia, PA Male carriers of deleterious BRCA1/2 mutations have a 6% lifetime risk of male breast cancer, and a 6%-14% lifetime risk of prostate cancer. Despite these health implications, we have found a lack of understanding of genetic test results among the men in these families. As part of a larger study to explore family communication patterns of genetic risk, we identi¿ed 24 male ¿rst-degree relatives whose proband received a true positieve test result and reported telling the result to her male relatives. Six (25%) of these male relatives reported that they hadn’t received the results or had forgotten them. Of the remaining 18 (75%) who did report receiving the results, two (11%) reported tht it was a negative result. Only two (11%) reported any level of dif¿culty in understanding the test results, or indicated that they would like more information. However, only ¿ve (28%) could correctly identify their chance of being a mutation carrier. Seven (40%) did not believe that the test results increased their own risk for cancer, reÀected in a relatively low level (33%) of interest in genetic testing. Of the six men who did express interest, half expressed interest primarily for their children’s sake. And ¿nally, of the 14 men who expressed any level of concern about the meaning of the test result, 11 directed their concern toward other family members, primarily daughters and sisters. This limited experience tends to con¿rm a level of cognitive and emotional distance that men experience from the genetic testing process as it applies to them. 2040 Identi¿cation of a recurring BRCA1 mutation in Bahamian women with breast cancer. Donenberg T, Turnquest T, Lunn J, Curling D, Krill-Jackson E, Hurley J. University of Miami/Jackson Memorial Hospital, Miami, FL; Doctor’s Hospital, Nassau, Bahamas; Princess Margaret Hospital, Nassau, Bahamas; Mount Sinai Comprehensive Cancer Center, Miami Beach, FL Background: As previously reported by our group, the age distribution of women with breast cancer in the Bahamas is unusually early with 48% being under age 50 in an unselected group of 266 newly diagnosed cases. The Bahamian population is a unique and culturally distinct group originating in part from the African continent and likely harbors a low level of genetic heterogeneity. These observations prompted investigation into a common genetic etiology. The identi¿cation of a founder mutation in this relatively isolated geographic population may contribute to more ef¿cient cancer risk screening and prevention. Methods: Sixteen women of Bahamian background underwent full sequence analysis and limited large gene rearrangement testing for BRCA1 and BRCA2 genes at Myriad Genetic Labs. Study criteria included at least one parent born in the Bahamas, ovarian cancer or breast cancer under age 50 in the proband or breast cancer at any age and a ¿rst or second degree relative with breast or ovarian cancer. Results: Four seemingly unrelated patients were found to carry the same mutation (4730insG) in the BRCA1 gene. Two patients were found to have the IVS13+1G>A mutation in BRCA1, a suspected founder mutation reported in the African American population. Three patients were found to have unclassi¿ed variants in the BRCA2 gene. Discussion: Recurrent mutations in the BRCA1 gene may explain the high prevalence of early onset breast cancer observed in the Bahamian population. We aim to further characterize the mutational spectrum in the Bahamas by testing additional patients with the above criteria. In addition, haplotype analysis of those carrying the 4730insG mutation may help identify a common ancestor that populated these islands. The identi¿cation of a founder mutation can lead to simpli¿ed and less costly genetic testing with increased accuracy and may allow clinicians to serve this population better. Further investigation is needed to more fully de¿ne the prevalence of founder mutations and the underlying causes of early onset breast cancer in this population. 2041 %5&$ and %5&$ mutation carrier predictions using the BRCAPRO model in clinic-based minority families. Huo D, Senie RT, Terry MB, Daly MB, Buys SS, Ogutha J, Hope K, Olopade OI. University of Chicago, Chicago, IL; Columbia University, New York, NY; Fox Chase Cancer Center, Philadelphia, PA; University of Utah Health Sciences Center, Salt Lake City, UT Background: BRCA mutation prediction models, such as BRCAPRO, are used in cancer risk clinics, but they were developed based on mutation rates and penetrance observed in individuals of Ashkenazi Jewish and European ancestry. Furthermore, in clinical counseling it is not always clear whether to test additional family members for BRCA mutations after the proband tests negative. The aim of this study is to evaluate the performance of the BRCAPRO model among clinic-based minority families and to evaluate the clinical utility of testing additional family members in high risk families. Methods: A total of 398 families with at least one member having been tested for BRCA mutations were enrolled through the Breast Cancer Family Registry and University of Chicago. Families of Ashkenazi Jewish ancestry were excluded. Using the BRCAPRO model with default penetrance and allele frequency for non-Ashkenazi Jewish populations, the predicted likelihood of carrying either a BRCA1 or BRCA2 mutations was generated. Sensitivity, speci¿city, and area under the receiver operating characteristic curves (AUC) were calculated. Results: There were 113 African American, 195 Hispanic, 54 Asian American and 36 other minority families. The AUC was 0.808 (95% con¿dence interval, CI: 0.767-0.847) for all minorities combined. At a predicted probability of 10%, the sensitivity for identifying mutation carriers was 72% and the speci¿city was 73%. The performance was similar across the racial/ethnic groups (p=0.18). After taking into account the mutation status of family members, the performance of the BRCAPRO model was improved (p<0.001): the AUC increased to 0.883 (95% CI: 0.846-0.912) and the speci¿city at the 10% threshold increased to 79%, while the sensitivity increased to 76%. Discussion: The data support the use of BRCAPRO in pretest prediction of BRCA1/2 mutations for minority families in high risk clinic settings. Mutation status of family members provides additional predictive value, which may help counselors decide whether to offer other family members the test when one member has already tested negative, given a positive family history of breast and ovarian cancer. 2042 Outcome in BRCA2 mutation carriers is superior to that of high-risk women with sporadic breast cancer. McLennan JL, Hwang ES, Moore DH, Crawford BB, Esserman LJ, Ziegler JL. University of California, San Francisco, CA Background: Breast cancer histology does not differ signi¿cantly between BRCA mutation carriers and those with sporadic breast cancer. We conducted this study to determine whether there existed a difference in outcome between these two groups following a diagnosis of invasive breast cancer (IBC). Methods: We performed a review of data collected from a prospectively recruited cohort of BRCA2 mutation carriers and high-risk mutationnegative patients. All women in the cohort underwent genetic testing for a BRCA mutation between 1996 and 2006 and had a diagnosis Abstracts – Poster Session II of invasive breast cancer. Overall survival was compared using the Kaplan-Meier survival method. Median survival was compared using a log-rank test. A Cox proportional hazard model was used to compare adjusted risk of mortality among BRCA2 mutation carriers and subjects without BRCA mutations. Results: 57 BRCA2 mutation carriers and 406 high risk, mutationnegative women were diagnosed with invasive cancer between 1954 and 2005. Median follow-up time was 49 months. BRCA2 mutation carriers were slightly younger at diagnosis than those with sporadic cancer (42.8 years and 45.7 years respectively, p=0.03), but less likely to have node-positive disease (p=0.04) and more likely to have riskreducing salpingo-oophorectomy (RRSO) (67% versus 8.4%, p<0.001). Mutation carriers had a signi¿cantly longer median survival after diagnosis of IBC than non-carriers (median survival 90 months (95% CI 49-122) vs. 49 months (95% CI 42-56), p=0.01). In a multivariate model including age, BRCA mutation status and RRSO, only RRSO was associated with improved survival (HR 0.72, p=0.02). Conclusion: BRCA mutation carriers have longer median survival following a diagnosis of IBC than similarly high-risk, mutation-negative women. This observation may in large part be due to the higher use of RRSO among mutation-carriers. S99 breast cancer (AUROC=0.85). However, when the performance of the BRCAPRO model was evaluated for women with bilateral breast cancer strati¿ed by age at ¿rst diagnosis, it appeared that the BRCAPRO model performed better in cases where the age at ¿rst diagnosis was ≤40 years (AUROC=0.90), compared to women whose age at ¿rst diagnosis was >40 years (AUROC=0.76). Additionally, the carrier rate of BRCA mutations was signi¿cantly higher (p=0.002, Fisher’s exact test) in women with bilateral breast cancer whose age at ¿rst diagnosis was ≤40 years (58%; 14/24), compared to women whose age at ¿rst diagnosis was >40 years (18%; 8/42). When the same comparisons were made for women with unilateral breast cancer, no statistically signi¿cant differences were observed in either the performance of the BRCAPRO model or in the carrier rate of BRCA mutations when strati¿ed by age. Conclusion: The BRCAPRO model appears to perform better in cases of bilateral breast cancer where the ¿rst breast cancer is diagnosed ≤40 years. Furthermore, the carrier rate of BRCA mutations among women with bilateral breast cancer is higher among those whose ¿rst breast cancer is diagnosed ≤40 years. These results suggest that we may be overestimating the relative contribution bilateral breast cancer has on the likelihood of detecting a BRCA mutation. However, these results should be validated in larger studies. 2044 Large genomic alterations in %5&$ in young women with breast cancer participating in the breast cancer family registry. 2043 BRCA mutations among women with bilateral breast cancer: mutation carrier rate and sensitivity of the BRCAPRO model based on age at ¿rst diagnosis. Ready K, Vogel K, Atchley D, Amos C, Solomon K, Lu K, Arun B. The University of Texas M.D. Anderson Cancer Center, Houston, TX Background: Risk estimates for the likelihood of identifying a BRCA mutation are calculated using the BRCAPRO risk assessment program. However, the sensitivity of this program in patients with bilateral cancer has not been determined. Furthermore, population based studies suggest that there is a low proportion of mutation carriers among patients with bilateral breast cancer whose age at ¿rst diagnosis was >40 years. Therefore, our objectives were to determine the sensitivity of the BRCAPRO model among women with bilateral breast cancer, to determine the rate of BRCA1 and BRCA2 mutations among women with bilateral breast cancer, and to determine if their mutation status is dependent on their ¿rst age of diagnosis of breast cancer. Methods: A retrospective chart review was performed. Women who were diagnosed with either unilateral or bilateral breast cancer and who had undergone comprehensive BRCA genetic testing were included. The CancerGene program, version 4.3.1, was used to calculate the BRCAPRO scores. Results: Sixty-six women with bilateral breast cancer and 66 women with unilateral breast cancer were identi¿ed. Of the bilateral cases, 33% (n=22), and of the unilateral cases 14% (n=9) were carriers of a BRCA mutation. The average BRCAPRO score among the bilateral cases was 52%, and the average BRCAPRO score among the unilateral controls was 15%. Overall, there was no statistically signi¿cant difference between the performance of the BRCAPRO model among women with bilateral breast cancer (AUROC=0.86) compared to unilateral Smith LD. Genetic Epidemiology Laboratory, The University of Melbourne, Parkville, VIC, Australia Large genomic alterations of BRCA1 represent a signi¿cant proportion of clinically relevant BRCA1 mutations. Early studies of genomic alterations used methods that were laborious, technically challenging and usually required a large amount of DNA. Recently, tests to identify large genomic alterations in BRCA1 have been successfully applied to small amounts of DNA and larger scale screens for these alterations have become possible. The proportion of women with breast cancer, especially young women, whose cancers are attributable to large alterations within BRCA1 is currently unknown in many populations and clinical settings. We selected 450 women from The Breast Cancer Family Registry (BreastCFR) diagnosed with: 1) breast cancer before age 40 years with a strong family history (2 or more ¿rst- or second-degree relatives affected with breast or ovarian cancer) and/or 2) tumour morphology consistent with having a BRCA1 mutation (at least 5 of the following: presence of necrosis, a marked lymphocytic in¿ltrate, pushing margins, mitotic index >50 per 10 hpf, nuclear grade III/III, trabecular growth pattern, syncytial pattern and/or poor tubule formation). These women had undergone extensive testing for BRCA1 mutations via various methods. Women participating in the population-based group of the BreastCFR were selected regardless of mutation status. Women recruited via clinics were only selected for this study if prior testing failed to identify a BRCA1 mutation. We screened the germline DNA via Multiplex Ligation-dependent Probe Ampli¿cation and found a variety of large alterations involving the coding regions of BRCA1 and/or the promoter region that represent ∼25% of all BRCA1 mutations identi¿ed in this group. The prevalence, penetrance and molecular nature of these changes, as well as the relevance of this type of mutation screening in clinical genetics services will be discussed. 2045 Clinical characteristics and choices regarding prophylactic surgery in BRCA mutation carriers. Stuckey A, Dizon D, Legare R, Wilbur J, Kent J, Tejada-Berges T, Gass J. Women and Infants’ Hospital/Warren Alpert Medical School of Brown University, Providence, RI Background: BRCA mutation carriers are known to have a high lifetime risk of developing breast and ovarian malignancies. As genetic testing S100 Abstracts – Poster Session II becomes widely available, preventative measures are a choice for many of these women. The purpose of this study is to evaluate the characteristics of BRCA mutation carriers who chose prophylactic surgery (PS) compared to those who did not. Methods: Eligible patients had a mutation in the BRCA1 or BRCA2 genes identi¿ed in our genetics program. Demographic data as well as family history was collected by retrospective review. Patients who opted for and those who chose not to proceed with prophylactic surgery were compared. Results: A total of 90 patients were included in this study. Forty-six (51%) underwent PS and 44 (49%) did not. Prophylactic surgery included 39 bilateral salpingo-oophorectomies (PBSO) and 13 mastectomies (PM). Of those undergoing PS, eighty-nine percent of the pathology was benign. Among those undergoing PM, there were two cases of DCIS (15.4%) and one case of in¿ltrating ductal carcinoma (7.7%). Among those undergoing PBSO, there was one case of adenocarcinoma of the fallopian tube (2.6%) and one case of adenocarcinoma of the ovary (2.6%). Comparing the two groups, PS was more often chosen among BRCA2 carriers versus those with BRCA1 mutations (60.8% vs. 38.5%, p=0.06). In addition, being married (62% vs. 40%, p<0.10), and employed (56% vs. 31%, p>0.1) was associated with PS. However, a prior history of cancer was not associated with PS in our cohort. Discussion: Our study suggests a group of women who are more likely to undergo prophylactic surgery—those who are BRCA2 mutation carriers, employed, and married. Con¿rmation of the pro¿le of women most interested in proceeding with preventative surgery as cancer prophylaxis requires a larger data set. Furthermore, long-term follow-up is required to describe the potential side effects of prophylactic surgery on health-related quality of life. Clinical characteristics of BRCA mutation carriers Surgery BRCA mutation BRCA1 15 (38.5%) BRCA2 31 (60.8%) Employed Yes 33 (56.0%) No 5 (31.3%) Married Yes 31 (62%) No 12 (40%) Prior Cancer Diagnosis Yes 29 (50%) No 17 (53%) No Surgery P-value 0.059 24 (61.5%) 20 (39.2%) 0.21 26 (44.1%) 11 (68.8%) 0.09 19 (38%) 18 (60%) 0.9 29 (50%) 15 (46.9%) 2046 Cancer-predictive methylation patterns in hereditary breast cancer. Suijkerbuijk KP, Fackler MJ, Sukumar S, van Gils CH, van Laar T, Vooijs M, van der Wall E, van Diest PJ. University Medical Center Utrecht, Utrecht, Netherlands; Johns Hopkins, Baltimore, MD Background: Promoter methylation is a common epigenetic mechanism to silence tumor suppressor genes during breast cancer development. Methylation of a selected set of genes was detected in ductal Àuids of sporadic breast cancer patients. We investigated whether BRCAassociated breast tumors show cancer-predictive methylation patterns similar to sporadic tumors. Material and Methods: Quantitative Multiplex Methylation-Speci¿c PCR (QM-MSP) of eleven genes involved in breast carcinogenesis (APC, BRCA1, BRCA2, CYCLIN D2, CDH1, ERa, SCGB3A1, p16, RARβ, RASSF1A, TWIST1) was performed on 40 BRCA1/2associated and 46 sporadic breast carcinomas, and on normal breast tissue from 9 BRCA1/2 mutation carriers and 13 non-carriers. Results: The median cumulative methylation index (CMI) of all studied genes was signi¿cantly higher in tumors than in normal tissue. The median CMI was signi¿cantly lower in hereditary than in sporadic breast tumors and in lymph node negative compared to lymph node positive tumors. Frequency of a positive methylation test was signi¿cantly higher in tumors versus normals and in lymph node positive versus negative tumors. The extent of cumulative methylation increased with age. Malignancy was predicted with high accuracy using a panel of genes in sporadic cases as well in hereditary cases. Discussion: BRCA1/2-associated breast cancers show a lower extent of promoter methylation compared to sporadic breast carcinomas. Nevertheless, methylation status of a panel of breast cancer genes is still highly associated with hereditary breast cancer, and should be useful for early detection of cancer in nipple Àuids of genetically predisposed patients. 2047 BRCA testing in underserved women: 5 years of followup. Wilcox C, Lee R, Chan S, Crawford B, Luce J, Ziegler J, Beattie MS. San Francisco General Hospital, San Francisco, CA; University of California, San Francisco, San Francisco, CA BACKGROUND: BRCA testing, to date, has not been widely available to underserved populations. In 2002, San Francisco General Hospital (SFGH) became the ¿rst public hospital in the US to provide BRCA testing and follow-up, free of charge, to appropriate women, via an Avon Foundation grant. The purpose of this research is to describe the ¿rst 5 years of experience of BRCA testing at SFGH and to compare the SFGH satellite Cancer Risk Program to the UCSF/Mt. Zion Cancer Risk Program. METHODS: Patients at SFGH were referred through 3 main routes: a family history questionnaire administered during mammography (50%), hospital based clinics (34%) and community health centers (16%). 627 patients at SFGH have received “intake and education” visits for risk assessment in the last 5 years. Of these, 122 have been offered BRCA testing (2 declined). Using a similar testing threshold at UCSF/Mt. Zion, 1114 patients have been offered BRCA testing (77 declined). RESULTS: Table 1 compares all patients at SFGH and UCSF/Mt. Zion who have received BRCA testing. The ethnicity, employment, and educational backgrounds of patients at SFGH differ considerably from those at UCSF/Mt. Zion. The percent of patients from both sites, however, who test BRCA positive is not clinically different. Table 2 compares patients at SFGH and UCSF/Mt. Zion who test positive. Interestingly, SFGH has a higher ratio of BRCA2 positives than UCSF/Mt. Zion. Choices for risk reducing surgeries at SFGH and at UCSF/Mt. Zion do not differ clinically. CONCLUSIONS: Although the demographics between SFGH and UCSF/Mt. Zion populations are signi¿cantly different, the proportion of positive results is not clinically different among these 2 populations. The ratio of BRCA2:BRCA1 carriers is higher at SFGH compared to UCSF/ Mt. Zion, which may reÀect the more diverse ethnic population seen at SFGH. Underserved and diverse women who carry BRCA mutations appear as likely to choose risk reducing surgeries as frequently as women who carry BRCA mutations from tertiary care centers. Comparison of BRCA Testing Populations at SFGH and UCSF/Mt. Zion SFGH UCSF/Mt. Zion Number Tested 121 1037 % Women 96% 97% median age (range) 45 (30-84) 51 (20-82) BRCA+ 17% 22% VUS 10% 7% % Caucasian 49% 85% % Black 15% 5% %Asian 13% 6% % Latina 23% 4% % Ashkenazi Jewish 20% 26% % with post high school education 66% 97% % employed/spouse employed 50% 100% Comparison of BRCA Carriers at SFGH and UCSF/Mt. Zion SFGH UCSF/Mt. Zion BRCA2:BRCA1 ratio 1.5 0.8 % of eligible carriers choosing RRSO* 50% 51% % of eligible carriers choosing RRM* 36% 23% RRSO = Risk Reducing Salpingo-Oophrectomy, RRM = Risk Reducing Mastectomy, “eligible carriers” must have tissue at risk and be free of metastatic disease 2048 Prophylactic surgeries among BRCA1/2 mutation carriers in the Netherlands. Hooning MJ. The Collaborative Group on Hereditary Breast and Ovarian Cancer in the Netherlands (HEBON) The purpose of this study was to estimate the uptake of prophylactic surgeries in Dutch BRCA1/2 mutation carriers. Within the framework of Abstracts – Poster Session II S101 a nationwide study (GEO-HEBON) on gene-environment interactions, we invited 211 carriers for a survey on various preventive strategies, to which 175 (83%) carriers responded (3% refused, 14% non-response). Carriers were approached 7.7 ± 2.2 years after the DNA test. After exclusion of carriers without intact ovaries at DNA test result, 150 carriers remained for analysis (123 BRCA1 and 27 BRCA2), of whom 67 had had breast cancer. The median age at DNA testing was 39.7 ± 11.0 years. 104 carriers (69%) underwent bilateral prophylactic oopho
© Copyright 2025