Thrombotic thrombocytopenic purpura Review articles J Thachil
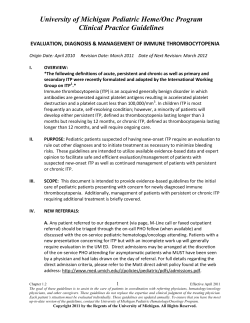
Review articles © The Intensive Care Society 2011 Thrombotic thrombocytopenic purpura J Thachil Thrombocytopenia is the most common coagulation problem in intensive care units with an incidence of up to 60% in some studies. It is often associated with multiple organ failure and high mortality. One of the life-threatening causes of thrombocytopenia in intensive care is thrombotic thrombocytopenic purpura (TTP). It is important that an early diagnosis of this condition is made in critically ill patients since early initiation of treatment can translate into a successful outcome. Patients who are diagnosed with TTP outside critical care units may very often require intensive care management due to the high rate of complications associated with this condition. This review summarises recent advances and outlines a practical approach to patients who are suspected to have TTP. Keywords: thrombocytopenia; thrombotic thrombocytopenic purpura; microangiopathy; ADAMTS-13 Introduction Thrombocytopenia is a well-known complication in intensive care unit (ICU) patients and is associated with increased mortality.1 A low platelet count develops, secondary to various factors including sepsis, drugs, disseminated intravascular coagulation and, rarely, the potentially life-threatening condition of thrombotic thrombocytopenic purpura (TTP). TTP is categorised as a microangiopathic haemolytic anaemia, which is a group of disorders characterised by haemolytic anaemia, thrombocytopenia and small vessel damage (microangiopathy).2 It is not easily distinguishable from conditions causing thrombotic microangiopathy, where haemolysis is not common (see Table 1). There has been tremendous progress in understanding of the pathogenesis and treatment of TTP in the last two decades, with its transformation from a universally fatal condition (greater than 90% mortality) to a treatable disease with less than 10% mortality with early treatment.3 Epidemiology Thrombotic thrombocytopenic purpura is a rare disease, with an incidence of 4 cases per million.4 However, an enhanced awareness of the condition and an increase in predisposing conditions such as bone marrow transplant, has led to more cases being diagnosed in recent years. TTP is more common in women in their third and fourth decades, reflecting its autoimmune nature and the triggering nature of pregnancy for this condition.4 It is also more common among black people.4 TTP occurs less frequently in children. However, TTP can be inherited or acquired and the inherited form of TTP usually presents in the neonatal period, with jaundice secondary to haemolytic anaemia, or in infancy where infections often precipitate its onset.5 Some cases of congenital TTP may be first diagnosed in adulthood (eg in pregnant females).6 In 1960, Schulman and colleagues described an 8-year-old girl who had repeated episodes of bleeding from the neonatal period with chronic thrombocytopenia and microangiopathic JICS Volume 12, Number 3, July 2011 Microangiopathic haemolytic anaemias • Thrombotic thrombocytopenic purpura • Haemolytic uremic syndrome • Disseminated intravascular coagulation • Disseminated cancer • Haemolysis elevated liver enzymes and low platelet (HELLP) syndrome Thrombotic microangiopathy (without overt haemolysis) • Catastrophic antiphospholipid syndrome • Macrophage activation syndrome • Malignant hypertension • Pre-eclampsia • HIV infection • Antibodies to vascular endothelial growth factor (VEGF) treatment • Allogeneic bone marrow transplant recipients • Renal allograft rejection Table 1 Causes of thrombotic microangiopathy. haemolytic anaemia.7 Two decades later, Upshaw described a 29-year-old woman who, since childhood, had had multiple episodes of thrombocytopenia and microangiopathic haemolytic anaemia, similar to Schulman’s case.8 These descriptions have led to recognition of inherited TTP, which is also termed Upshaw-Schulman syndrome. Clinical features The original description of TTP in 1924 by Moschowitz detailed the pentad of signs and symptoms:9 • anaemia • thrombocytopenia • fever 215 Review articles common cause of death especially if there has been a delay in initiation of plasma exchange. Pancreatitis can precipitate TTP and may be responsible for non-specific abdominal pain in the absence of intestinal ischaemia.14 In this context, it is useful to bear in mind that the presence of large ecchymotic patches, early lung involvement and large vessel thrombosis are all features leading away from the diagnosis of TTP. Pathogenesis Figure 1 Pathogenesis of thrombotic thrombocytopenic purpura (TTP). In the top figure, the normal physiological state is explained. Von Willebrand factor (red circles) is normally coiled in the subendothelium (yellow rectangles), but unfolds in ultra-large high molecular weight multimer forms with endothelial injury. These are normally cleaved by the protease, ADAMTS-13 (scissors), preventing platelets (purple circles) aggregating on to these multimers. TTP occurs when there is deficiency of this enzyme (congenitally or through antibody formation) allowing persistence of these multimers which cause platelet aggregation and thrombotic consequences. • neurological disturbance • renal impairment. However, these five classical features are often not evident in the majority of patients. The absence of the pentad should not discourage physicians from making the diagnosis of TTP, which requires only the presence of microangiopathic haemolysis and thrombocytopenia that cannot be explained otherwise.10 The most common presenting symptoms of TTP are nonspecific and can include abdominal pain, vomiting, and generalised weakness.2 Many patients may have these symptoms for many weeks before full-blown TTP develops.11 Fever is rare unless a septic illness triggers the onset of the condition, but a high temperature should raise the suspicion of a non-TTP cause of thrombotic microangiopathy. In a recent study, Escherichia coli infections predominantly, but also bacteria other than Enterobacteriaceae, were associated with thrombotic microangiopathy in intensive care patients, especially those patients who are immunocompromised (eg with human immunodeficiency virus infection or systemic lupus erythematosis).12 Neurological symptoms are seen in about half of the patients and can vary from minor symptoms like headache and transient confusion to hemiparesis and coma.2 It is important to remember that the neurological symptoms can be fluctuant in their presentation and severity and can develop during therapy. Renal impairment is unusual with very few patients having elevated serum creatinine although microscopic haematuria and proteinuria are common.11 Cardiac involvement with biochemical evidence of myocardial injury is frequent in TTP and an elevated troponin has been suggested to be a useful biomarker in some studies.13 This is also a very 216 The pathological basis of TTP is the widespread formation of platelet thrombi in the microcirculation of several organs, leading to thrombocytopenia (Figure 1). The accelerated platelet aggregation is secondary to the binding to ultra-large, high molecular weight multimers of von Willebrand factor (VWF) in the circulation.13 VWF unfolds under conditions of high shear stress, allowing proteolysis by a protease enzyme, ADAMTS-13 (a disintegrin and metalloprotease with thrombospondin repeats), into smaller fragments of VWF.15 In physiological states, ultra-large VWF multimers released by the endothelium induce platelet aggregation in areas of high shear stress, but this only occurs briefly as VWF is rapidly broken down by ADAMTS-13.15 However, in congenital deficiency or where there is failure of ADAMTS-13 to act because of an inhibitory antibody, there is excessive platelet aggregation. In acquired TTP, antibodies develop against this enzyme, while in the rare congenital type, enzyme deficiency occurs due to mutation in the ADAMTS-13 gene.16,17 The resulting ADAMTS13 deficiency allows the unusually large multimers of VWF to remain in the circulation, resulting in multiple platelet aggregates.18 It has also been suggested that activated endothelial cells can secrete large amounts of the ultra-large VWF, which can overwhelm the enzyme activity of the protease, leading to TTP in the absence of antibodies.14,19 Haemolysis in TTP is the result of platelet microthrombi in the circulation which shear the red cells. This results in schistocytes, which are fragmented red cells, easily observed on a peripheral blood smear examination. Detection of schistocytes is essential in the diagnosis of TTP because it means that thrombocytopenia is caused by thrombotic microangiopathy. This is especially important in intensive care patients where there are multiple causes for a low platelet count. Certain studies have suggested the possibility that the red cell damage is responsible for the development of platelet aggregates, especially in selected cases where the ADAMTS-13 enzyme is not severely depleted.20 Haemoglobin released from haemolysed red cells mops up the platelet anti-aggregatory agent nitric oxide, which also has vasodilatory properties.14,20 Uninhibited platelet aggregation and vasoconstriction can lead to the thrombotic complications of TTP. In addition, the release of adenosine diphosphate from inside the red cells can act as a strong platelet aggregating agent.14 Diagnosis The diagnosis of TTP is a clinical one, in the presence of haemolysis and thrombocytopenia with no alternate explanation (Figure 2).10 As it occurs frequently in previously healthy individuals and the acute presentation can be dramatic, Volume 12, Number 3, July 2011 JICS Review articles Involve haematologist lab lgy o t o em Ha Suspect TTP Coagulation lab n io us sf an Tr Bioc hem istr y la Vir b olo gy lab Request blood film, reticulocyte count Request clotting screen & ADAMTS-13 work-up Request LDH & haptoglobin b la Request hepatitis B, C & HIV status Ask for Coombs test Arrange for urgent plasma exchange Figure 2 Diagnosis of thrombotic thrombocytopenic purpura. the diagnosis should be suspected and treatment initiated on an urgent basis. The laboratory abnormalities associated with TTP include: • Full blood count – the platelet count is often very low in the acute phase, with a median value of 16 x109/L in the Oklahoma registry data.11 Severe bleeding secondary to thrombocytopenia is uncommon, as the basic pathogenic mechanism for TTP is platelet aggregation. Anaemia develops secondary to haemolysis, with haemoglobin about 8 g/dL.11 • Blood film – examination of the peripheral blood smear is critical in the diagnosis of TTP. The presence of schistocytes or red cell fragments in the peripheral blood smears should be confirmed or excluded by an experienced morphologist. TTP cannot be diagnosed in the absence of schistocytes. However, there may be a time lag of up to 24 hours before these fragments are noted under the microscope and hence serial examination by an experienced observer is necessary.10 • Signs of haemolysis – anaemia, increased reticulocyte count, elevated lactate dehydrogenase (LDH) and decreased haptoglobin with negative direct Coomb’s or antiglobin tests. LDH in TTP has been suggested to be also secondary to tissue ischaemia in addition to haemolysis and, as such, the normalisation of this parameter can take longer than the other haemolytic markers.21 • The coagulation screen is usually normal and can be helpful in differentiating TTP from other causes of microangiopathy, such as disseminated intravascular coagulation. • Abnormal renal function tests (abnormal in only a few patients with TTP) can be helpful in pointing towards a diagnosis of haemolytic uraemic syndrome. • Abnormal liver function tests can suggest HELLP syndrome JICS Volume 12, Number 3, July 2011 in pregnant women. • HIV tests –TTP can be triggered by the virus in some cases. The largest series reported so far included 30 episodes of HIV-associated TTP noted in 24 patients over 10 years.22 In this paper, a new diagnosis of HIV corresponded with the first presentation of TTP in eight patients. Strict adherence to once-daily highly active anti-retroviral therapy in combination with plasma exchange was associated with a good outcome in most cases with immunosuppression with rituximab needed in approximately 10% of cases. ADAMTS-13 assays The identification of the ADAMTS-13 enzyme has been a major advance in the understanding of TTP. Undetectable or very low plasma levels of enzymatic activity (less than 10%) establish a diagnosis of inherited or acquired TTP unequivocally. However, patients with normal levels of ADAMTS-13 activity may have the characteristic features of TTP, while low enzyme levels (10-40%) may also occur in disorders other than TTP, especially those secondary to other conditions such as HIV infection and allogeneic bone marrow transplantation.23 In congenital TTP, ADAMTS-13 assay is beneficial in diagnosing the deficiency, while in acquired TTP, inhibitory antibodies to the enzyme should be measured in specialised laboratories. Currently, the usefulness of measuring ADAMTS-13 is not in the initial diagnosis of TTP, which remains a clinical one, but in predicting future relapses.24 Both small-scale prospective and retrospective studies have shown that patients with severe ADAMTS-13 deficiency and antibodies to ADAMTS-13 protease had a much higher likelihood of relapse.25 The assay may also be helpful in cases where the diagnosis of TTP is not straightforward. In these cases, plasma exchange is started and ADAMTS-13 levels are awaited to confirm or refute the diagnosis. Differential diagnosis There are several other disorders that should be considered (Table 2): 1. Haemolytic uraemic syndrome (HUS) – HUS is classified into two categories, depending on whether it is associated with Shiga-like toxin. Toxin-associated HUS (D+HUS) is the classic or typical form seen in young children and is associated with diarrhoea and more severe and sometimes persistent renal impairment. The atypical form of HUS (DHUS) is much more difficult to differentiate from TTP, although neurological symptoms would suggest the diagnosis of TTP and moderate to severe renal failure, HUS.26 ADAMTS-13 deficiency is unusual with typical HUS although non-severe (>10%) deficiency may be noted in the atypical form. Atypical HUS is a disease of complement dysregulation, where genetic mutations of both complement regulators and activators, and autoantibodies against the complement regulator factor H occur. Identification of the underlying molecular abnormality can help in planning future management of these patients.27 2. Disseminated intravascular coagulation (DIC) – the main differentiating factors are abnormal coagulation screen, low fibrinogen and high D-dimers. Serial testing of these 217 Review articles TTP DIC CAPS MAPS Thrombocytopenia Sudden Gradual Sudden Gradual Coagulation abnormalities Rare Common Rare Rare Haemotology Anaemia Reticulocytosis Anaemia rare Cytopenias Cytopenias Biochemistry High LDH Low haptoglobin No change May show renal or liver abnormalities May show renal or liver abnormalities Table 2 Differential diagnosis of thrombotic thrombocytopenic purpura. Key: TTP: thrombotic thrombocytopenic purpura DIC: disseminated intravascular coagulation CAPS: catastrophic antiphospholipid syndrome MAS: macrophage activation syndrome LDH: lactate dehydrogenase. Begin plasma exchange Patient responding Patient not responding Add anti-platelets and start thromboprophylaxis once platelet count >50 Double plasma exchange Consider rituximab Platelet count & LDH normal with haemoglobin normal or near normal for 2 days Other immunosuppressives or experimental therapies Taper plasma exchange Figure 3 Treatment algorithm for thrombotic thrombocytopenic purpura. markers may be necessary to confirm DIC. 3. The HELLP syndrome (Haemolysis, Elevated Liver enzymes and Low Platelets) and pre-eclampsia – in pregnancy, both these diagnoses can mimic TTP, although in HELLP, there are abnormal liver tests and in both HELLP and preeclampsia, hypertension and proteinuria co-exist. 4. Catastrophic antiphospholipid syndrome (CAPS) and macrophage activation syndrome (MAPS) – in both these conditions, there may be a history of autoimmune disorders such as systemic lupus erythematosis or juvenile rheumatoid arthritis. CAPS (also known as Asherson’s syndrome) presents in a dramatic fashion, with multiorgan failure developing over a very short period of time, associated with histopathological evidence of multiple vessel occlusions.28 It is often preceded by a precipitating event, mainly infectious, and is associated with high mortality. Laboratory tests such as anti-cardiolipin antibodies and lupus anticoagulant tests will be positive in CAPS especially, in very high titres.29 MAPS is another potentially fatal condition associated with excessive activation of 218 macrophages and T-cells leading to an overwhelming inflammatory reaction.30 Patients with MAPS can have pancytopenia and hepatosplenomgaly. Ferritin is increased in these cases, along with triglycerides, which can aid the diagnosis.31 Clinically, both CAPS and MAPS affect major venous and arterial vessels rather than the microvasculature, as in the case of TTP. Management Plasma exchange is the most important component of therapy for all patients with suspected TTP. (Figure 3) In all cases of suspected TTP, plasma exchange should be initiated as a matter of urgency.10 Before the empirical use of plasma exchange therapy, TTP was associated with a fatal outcome in almost all patients. Following reports from trials of plasma exchange, survival of 80-90% is reported.3 This treatment modality may work by removing ADAMTS-13 antibodies, and/or replacing the deficient protease. However, it has been reported to be efficacious even in cases with normal plasma levels of ADAMTS-13 and no detectable autoantibody.11 The effectiveness of the plasma exchange procedure may also be that it ‘cleans up’ the haemolytic products, which in turn mop up beneficial nitric oxide.20 It is important to note that in hospitals with no access to plasma exchange that infusion of fresh frozen plasma (30 mL/kg) may be tried to ‘buy time,’ although volume overload can be a problem. The British Committee for Standards in Haematology suggest that singlevolume daily plasma exchange should be commenced ideally within 24 hours of TTP presentation, although reports of early deaths due to cardiac involvement suggest that the sooner the exchange is commenced, the better the outcome.10 Solvent detergent-treated plasma is preferred, to minimise the risk of viral transmission through blood products. Hepatitis B vaccination should be considered in patients who are negative for hepatitis B antibodies, to prevent transfusion-transmitted infection.10 Plasma exchange, once commenced, is continued until two days after remission is confirmed with the platelet count greater than 150 x109/L, normal LDH and schistocytes no longer present on blood films.10,11 Anaemia can worsen during therapy and renal dysfunction, if present, may not recover in all patients.11 The presence of antibodies to ADAMTS-13 in acquired TTP has led to the use of immunosuppressive therapies. Most commonly, steroids are prescribed at 1-2 mg/kg/day.10 In very ill Volume 12, Number 3, July 2011 JICS Review articles Plasma exchange Second and third trimester Steroids + plasma exchange TTP No tb et te r First trimester Aim to Deliver Be tte r HELLP Pre-eclampsia Postpartum Treat as TTP Figure 4 Management of thrombotic microangiopathy in pregnancy. The main distinction for a suspected case of TTP in pregnancy is from HELLP and PET. In the first trimester, delivery of a viable baby is not possible. So continuation of pregnancy is advisable since TTP is more likely and plasma exchange is administered. In the second and third trimesters, since both HELLP and PET are diagnostic considerations, glucocorticoids in combination with plasma exchange is a relevant option with the hope that the delivery of the fetus can be undertaken at a a safe period. If the delivery of the fetus makes the clinical and laboratory parameters better, PET or HELLP can be confirmed and TTP can be excluded with the discontinuation of plasma exchange. In the post-partum period, the female is treated as having TTP since PET and HELLP are less likely. patients, methyl prednisolone 1g IV for three days is recommended.11 In the past, vincristine, cyclophosphamide, azathioprine, intravenous immunoglobulins and splenectomy have been tried. All patients should receive folate supplementation for haemolytic anaemia. Adjunctive treatment for patients with TTP includes an antiplatelet agent, like aspirin, and an antithrombotic agent, like low-molecular-weight heparin, to retard the platelet aggregatory process and prevent the high incidence of thrombosis in these patients. A randomised trial reported a non-significant reduction in mortality when antiplatelet agents were added to plasma exchange, although it may be prudent to wait for the platelet count to be over 50 x109/L before staring aspirin.11,32 A study of 68 patients with TTP demonstrated seven cases of venous thromboembolism, with the authors recommending thromboprophylaxis with low-molecularweight-heparin once the platelet count is adequate.33 Platelet transfusions are considered to be relatively contraindicated in TTP as they may add ‘fuel to the fire’ by enhancing further platelet aggregation. However, if there is a need for central venous access for plasma exchange or urgent surgery, platelet transfusions may be considered. A recent systematic review did not show added risk from platelet infusions.34 Refractory and relapsed cases Despite the considerable success of plasma exchange, approximately 10-20% of patients are refractory or relapse early.35 In refractory cases of TTP, plasma exchange may be intensified to twice daily regimen.9 Recently, there has been JICS Volume 12, Number 3, July 2011 interest in the monoclonal antibody to CD20, rituximab, at doses of 375 mg/m2 weekly for four cycles, with good response noted in about three weeks.36,37 Over 100 TTP cases have been treated with rituximab, with about 88% of refractory cases and almost all relapsed cases achieving remission.38 Front-line therapy with rituximab has not been extensively studied in TTP, although there is interest in this regimen in combination with plasma exchange due to the immune-mediated nature of acquired TTP. While using rituximab and plasma exchange concurrently, an interval of 24-36 h after rituximab should be provided to prevent washout of the drug. Drugs on the horizon include recombinant ADAMTS-13 concentrates and an aptamer with the function of inhibiting the binding between platelets and ultra-large VWF multimers. A recent publication also noted N-acetyl cysteine to play a role in reducing the size and activity of VWF in vitro and animal experiments.39 TTP in pregnancy TTP in pregnant females can be a very difficult challenge. The main differential diagnosis includes other causes of thrombotic microangiopathy such as pre-eclampsia and HELLP syndrome. It is important to distinguish these conditions since both HELLP and preeclampsia are managed by delivery of the fetus, which is not effective for TTP.10 Although both HELLP and preeclampsia usually present in the third trimester and have classical clinical accompaniments, eg elevated liver enzymes (with HELLP) and proteinuria/hypertension (pre-eclampsia), the distinction can be difficult (Figure 4 for a practical algorithm).40 In these situations, multidisciplinary involvement with experienced obstetricians, haematologists and intensivists is essential. Once TTP has been diagnosed, the treatment is similar to that for a non-pregnant patient with TTP, with plasma exchange.10 This procedure has been successfully tried in many cases of TTP, although increased plasma requirement may be noted during gestation.10 Monitoring of ADAMTS-13 activity can guide the adequacy and frequency of plasma exchange.41 TTP can relapse in future pregnancies; those at risk are patients with idiopathic TTP compared to those who presented with TTP in association with pregnancy (25% vs 12%).41 Severe deficiency of ADAMTS-13 activity during pregnancy predicts a high risk of relapse.42 These patients may benefit from prophylactic therapy. Rituximab treatment is NOT safe during pregnancy. A recent literature review identified that out of 153 pregnancies with known outcomes, there were 90 live births, 22 premature births, one neonatal death, eleven neonates with haematological abnormalities and two with congenital malformations.43 References 1. Baughman RP, Lower EE, Flessa HC et al. Thrombocytopenia in the intensive care unit. Chest 1993;104:1243-47. 2. George JN. Thrombotic thrombocytopenic purpura. N Engl J Med 2006; 354:1927-35. 3. Rock GA, Shumak KH, Buskard NA et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic purpura. Canadian apheresis study group. N Engl J Med 1991;325:393-97. 4. Terrell DR, Williams LA, Vesely SK et al. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency. J Thromb Haemost 2005;3:1432-36. 219 Review articles 5. Loirat C, Girma JP, Desconclois C et al. Thrombotic thrombocytopenic purpura related to severe ADAMTS13 deficiency in children. Pediatr Nephrol 2009;24:19-29. 6. Fujimura Y, Matsumoto M, Kokame K et al. Pregnancy-induced thrombocytopenia and TTP, and the risk of fetal death, in UpshawSchulman syndrome: a series of 15 pregnancies in 9 genotyped patients. Br J Haematol 2009;144:742-54. 7. Schulman I, Pierce M, Likens A, Currimbhoy Z. Studies on thrombopoiesis. A factor in normal human plasma required for platelet production; chronic thrombocytopenia due to its deficiency. Blood 1960;14:943-57. 8. Upshaw JD. Congenital deficiency of a factor in normal plasma that reverses microangiopathic hemolysis and thrombocytopenia. N Engl J Med 1978;298:1350-52. 9. Moschcowitz E. An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries. Arch Intern Med 1925;36:89-93. 10.Allford SL, Hunt JB, Rose P, Machin SJ. Guidelines on the diagnosis and management of the thrombotic microangiopathic haemolytic anaemias. Br J Haematol 2003;120:556-73. 11.George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood 2010;116:4060-69. 12.Coppo P, Adrie C, Azoulay E et al. Infectious diseases as a trigger in thrombotic microangiopathies in intensive care unit (ICU) patients? Intensive Care Med 2003;29:564-69. 13.Hughes C, McEwan JR, Longair I et al. Cardiac involvement in acute thrombotic thrombocytopenic purpura: association with troponin T and IgG antibodies to ADAMTS-13. J Thromb Haemost 2009;7:529-36. 14.Thachil J. Lessons from acute pancreatitis-induced thrombotic thrombocytopenic purpura. Eur J Intern Med 2009;20:739-43. 15.Scully MA, Machin SJ. Berend Houwen Memorial Lecture: ISLH Las Vegas May 2009: the pathogenesis and management of thrombotic microangio-pathies. Int J Lab Hematol 2009;31:268-76. 16.Furlan M, Robles R, Galbusera M et al. Von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolyticuremic syndrome. N Engl J Med 1998;339:1578-84. 17.Tsai H-M, Lian ECY. Antibodies to von-Willebrand factor cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med 1998;339:1585-94. 18.Moake JL. Thrombotic microangiopathies. N Engl J Med 2002;347: 589-600. 19.Jimenez JJ, Jy W, Mauro LM et al. Elevated endothelial microparticles in thrombotic thrombocytopenic purpura: findings from brain and renal microvascular cell culture and patients with active disease. Br J Haematol 2001;112:81-90. 20.Thachil J. Thrombotic thrombocytopenic purpura: is there more than ADAMTS-13? J Thromb Haemost 2007;5:634-35. 21.Cohen JA, Brecher ME, Bandarenko N. Cellular source of serum lactate dehydrogenase elevation in patients with thrombotic thrombocytopenic purpura. J Clin Apher 1998;13:16-19. 22.Hart D, Sayer R, Miller R et al. Human immunodeficiency virus associated thrombotic thrombocytopenic purpura – favourable outcome with plasma exchange and prompt initiation of highly active antiretroviral therapy. Br J Haematol 2011 Mar 10 [Epub ahead of print]. 23.Vesely SK, George JN, Lammle B et al. ADAMTS-13 activity in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: relation to presenting features and clinical outcomes in a prospective cohort of 142 patients. Blood 2003;101:60-68. 24.Peyvandi F, Lavoretano S, Palla R et al. ADAMTS-13 and anti-ADAMTS13 antibodies as markers for recurrence of acquired thrombotic thrombocytopenic purpura during remission. Haematologica 2008;93: 232-39. 25.Mannucci PM, Peyvandi F. TTP and ADAMTS-13: When is testing appropriate? Hematology Am Soc Hematol Educ Program 2007:121-26. 220 26.Remuzzi G, Galbusera M, Noris M et al. von Willebrand factor cleaving protease (ADAMTS-13) is deficient in recurrent and familial thrombotic thrombocytopenic purpura and hemolytic uremic syndrome. Blood 2002;100:778-85. 27.Taylor CM, Machin S, Wigmore SJ, Goodship TH. Clinical practice guidelines for the management of atypical haemolytic uraemic syndrome in the United Kingdom. Br J Haematol 2010;148:37-47. 28.Cervera R, Bucciarelli S, Plasín MA et al. Catastrophic antiphospholipid syndrome (CAPS): descriptive analysis of a series of 280 patients from the “CAPS Registry”.J Autoimmun 2009;32:240-45. 29.Erkan D, Espinosa G, Cervera R. Catastrophic antiphospholipid syndrome: updated diagnostic algorithms. Autoimmun Rev 2010;10:74-79. 30.Grom AA, Mellins ED. Macrophage activation syndrome: advances towards understanding pathogenesis. Curr Opin Rheumatol 2010;22: 561-66. 31.Ravelli A. Macrophage activation syndrome. Curr Opin Rheumatol 2002;14:548-52. 32.Bobbio-Pallavicini E, Gugliotta L, Centurioni R et al. Antiplatelet agents in thrombotic thrombocytopenic purpura (TTP): results of a randomized multicenter trial by the Italian Cooperative Group for TTP. Haematologica 1997;82:429-35. 33.Yarranton H, Cohen H, Pavord SR et al. Venous thromboembolism associated with the management of acute thrombotic thrombocytopenic purpura. Br J Haematol 2003;121:778-85. 34.Swisher KK, Terrell DR, Vesely SK et al. Clinical outcomes after platelet transfusions in patients with thrombotic thrombocytopenic purpura. Transfusion 2009;49:873-87. 35.Rüfer A, Brodmann D, Gregor M et al. Rituximab for acute plasma refractory thrombotic thrombocytopenic purpura. A case report and concise review of the literature. Swiss Med Wkly 2007;137:518-24. 36.Scully MF, Cohen H, Cavenagh JD et al. Remission in acute refractory and relapsing thrombotic thrombocytopenic purpura following rituximab is associated with a reduction in IgG antibodies to ADAMTS-13. Br J Haematol 2006;136:451-61. 37.Ling HT, Field JJ, Blinder MA. Sustained response with rituximab in patients with thrombotic thrombocytopenic purpura: a report of 13 cases and review of the literature. Am J Hematol 2009;84:418-21. 38.Caramazza D, Quintini G, Abbene I et al. Relapsing or refractory idiopathic thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: the role of rituximab. Transfusion 2010;50:2753-60. 39.Chen J, Reheman A, Gushiken FC et al. N-acetylcysteine reduces the size and activity of von Willebrand factor in human plasma and mice. J Clin Invest 2011;121:593-603. 40.McMinn JR, George JN. Evaluation of women with clinically suspected thrombotic thrombocytopenic purpura-hemolytic uremic syndrome during pregnancy. J Clin Apher 2001;16:202-09. 41.Scully M, Starke R, Lee R et al. Successful management of pregnancy in women with a history of thrombotic thrombocytopenic purpura. Blood Coagul Fibrinolysis 2006;17:459-63. 42.Raman R, Yang S, Wu HM, Cataland SR. ADAMTS-13 activity and the risk of thrombotic thrombocytopenic purpura relapse in pregnancy. Br J Haematol 2011 Jan 31. doi: 10.1111/j.1365-2141.2010.08558.x E-Pub ahead of print. Accessed April 2011. 43.Chakravarty EF, Murray ER, Kelman A. Farmer P. Pregnancy outcomes after maternal exposure to rituximab. Blood 2011;117:1499-506. Jecko Thachil Consultant in Haemostasis and Thrombosis, Roald Dahl Haemostasis and Thrombosis Centre, Royal Liverpool University Hospital jeckothachil@yahoo.co.uk Volume 12, Number 3, July 2011 JICS
© Copyright 2025