Prescriptions of Chinese Herbal Medicine for Constipation Under the National Health
ORIGINAL
ARTICLE
Prescriptions of Chinese Herbal Medicine for
Constipation Under the National Health
Insurance in Taiwan
Maw-Shiou Jong1,5, Shinn-Jang Hwang2,4, Yu-Chun Chen2,4, Tzeng-Ji Chen2,4,
Fun-Jou Chen3, Fang-Pey Chen1,5*
1
Center for Traditional Medicine, 2Department of Family Medicine, Taipei Veterans General Hospital, Taipei;
3
Graduate Institute of Integrated Chinese and Western Medicine, Chinese Medical University, Taichung;
4
Division of Family Medicine, Department of Medicine, and 5Institute of Traditional Medicine,
National Yang-Ming University School of Medicine, Taipei, Taiwan, R.O.C.
Background: Constipation is a common gastrointestinal problem worldwide. The aim of this study was to determine the
frequency of use and prescriptive patterns of Chinese herbal medicine (CHM) in treating constipation by analyzing the
claims data of traditional Chinese medicine (TCM) from the National Health Insurance (NHI) in Taiwan.
Methods: The computerized claims dataset of the TCM office visits and the corresponding prescription files in 2004
compiled by the NHI Research Institute in Taiwan were linked and processed. Visit files with the single diagnostic coding
of constipation (ICD-9-CM code 564.0) were extracted to analyze the frequency and pattern of corresponding CHM prescriptions. The association rule was applied to analyze the co-prescription of CHM in treating constipation.
Results: There were 152,564 subjects who visited TCM clinics only for constipation in Taiwan during 2004 and received
a total of 387,268 CHM prescriptions. Subjects between 20 and 29 years of age comprised the largest number of those
treated (25.5%). Female subjects used CHM for constipation more frequently than male subjects (female:male = 3.31:1).
There was an average of 4.6 items of single Chinese herbs or formula in a single prescription for constipation. Ma-zi-renwan was the most commonly prescribed herbal formula, while Da-huang (Rheum palmatum) was the most commonly
used single Chinese herb. According to the association rule, the most common prescribed pattern of 2-drug combination
of CHM for treating constipation was Ban-xia-xie-xin-tang plus Ma-zi-ren-wan, while the 3-drug combination of CHM was
Fang-feng-tong-sheng-san, Rheum palmatum and Ma-zi-ren-wan.
Conclusion: This study showed the pattern of single Chinese herbs or herbal formulae used in treating constipation
in Taiwan. Further clinical trials are needed to evaluate the efficacy and safety of these CHMs in treating constipation.
[J Chin Med Assoc 2010;73(7):375–383]
Key Words: Chinese herbal medicine, constipation, pharmacoepidemiology, traditional Chinese medicine
Introduction
Constipation is a condition in which bowel movements
are infrequent, irregular, or difficult.1 It is a disorder
resulting from different causes such as insufficient
intake of dietary fiber, emotional influence, dysfunction
of the nervous system, structural abnormality, systemic
disease, or drug effects.1 Constipation is a common
gastrointestinal problem worldwide, and it affects at
least 8.5% of individuals in Taiwan, based on Rome II
diagnostic criteria.2 It often occurs in females, with
advanced age, low socioeconomic class and low educational position.2,3
The aim of treating constipation is to treat the underlying causes, improve symptoms, and resume the
normal physiological function of the bowel. Treating
constipation can be a comprehensive therapy tailored to
the individual.4 Drugs commonly used include bulk laxatives, osmotic laxatives, non-absorbable sugar, stimulant laxatives, cholinergic agents and other prokinetic
*Correspondence to: Dr Fang-Pey Chen, Center for Traditional Medicine, Taipei Veterans General
Hospital, 201, Section 2, Shih-Pai Road, Taipei 112, Taiwan, R.O.C.
E-mail: fpchen@vghtpe.gov.tw
Received: December 9, 2009
Accepted: June 22, 2010
●
J Chin Med Assoc • July 2010 • Vol 73 • No 7
© 2010 Elsevier Taiwan LLC and the Chinese Medical Association. All rights reserved.
●
375
M.S. Jong, et al
agents. Selective chloride channel activators, which can
increase intestinal water secretion, thereby increasing
intestinal motility and facilitating the bowel movement,
are also used.4,5
After excluding secondary constipation caused by
other problems, primary (idiopathic) constipation can
be classified into 3 categories: normal transit or irritable bowel syndrome, pelvic floor dysfunction, and slow
transit constipation. These 3 types of constipation overlap frequently. Normal and slow transit constipation are
usually treated by the drugs mentioned above.5 In
Eastern countries, traditional Chinese medicine (TCM)
is another option in addition to Western medicine for
treating constipation.6 The principles of diagnosis and
treatment of constipation in TCM are primarily based
on the manifestations of the syndrome Therefore, the
principal signs and symptoms of patients from which
a corresponding prescription of Chinese herbal medicine (CHM) is provided, is largely dependent on the
experience of the Chinese herbal doctors or from the
records of ancient Chinese books. The optimal choice
of CHM prescription for constipation is unknown.
Furthermore, whether these Chinese herbs or formulae
have modern pharmacological effects in the treatment
of constipation remains to be elucidated.
In Taiwan, the National Health Insurance (NHI)
has reimbursed medical expenses for Western medicine
for nearly all inhabitants since 1995 (22,134,270 beneficiaries at the end of 2004, covering nearly 98% of the
total population in Taiwan).7,8 The use of TCM has
been reimbursed by the NHI since 1996. People in
Taiwan are free to choose Western medicine or TCM,
and are allowed to visit primary care clinics or hospitals
without referral. Because all claims data are available to
researchers in electronic form, a large-scale survey of
pharmacoepidemiological issues can be easily conducted. The aim of the current study was to explore the
frequency and pattern of CHM use for subjects with
constipation by analyzing the NHI database in 2004 in
Taiwan.
(CM_CD2004.DAT and CM_OO2004.DAT), for
2004 from the NHIRD in Taiwan. The visit files recorded the dates of encounters, the medical care facilities and specialties, patients’ sex, birth date, and up to 3
diagnoses according to the International Classification
of Diseases, 9th Revision, Clinical Modification (ICD-9CM). For privacy protection, the identification data of
patients and institutions was scrambled cryptographically to ensure anonymity. The prescription files contained the prescription records of CHM corresponding
to the office visits. A CHM prescription contains 1 to
several single Chinese herbs or herbal formulae. The
Chinese herbal formulae or single herbs are made in
powder or fine granules in Taiwan, and can be easily
mixed and dispensed into small packages so that 1 prescription can be taken at a time.
All TCMs are provided only in ambulatory clinics
under the coverage of NHI in Taiwan and there is no
inpatient care. In addition, only licensed TCM physicians are qualified for reimbursement. The insurance
benefits of TCM in Taiwan include CHM, acupuncture
and traumatology manipulative therapy, especially for
joint dislocation.
Study design
Methods
Although the concept of disease entities in TCM is
quite different from that in Western medicine, the
TCM physicians in Taiwan are requested to make the
diagnosis based on ICD-9-CM coding for visiting
claims. In this study, we utilized the data of subjects
with the single diagnostic code for constipation (i.e.
ICD-9 code 564.0) among TCM visits.
According to the theory of TCM, a single prescription from a TCM physician may contain a single Chinese herb or multiple herbs of various dosages, namely
a compound (Fu-Fang) or a classical formula (regimen,
remedy or Fang-Ji). These are a combination of compatible Chinese herbs in fixed dosages ascribed to classical or well-known Chinese textbooks of medicine, or
a classical formula plus some Chinese herbs called ChiaChien-Fang. In addition, several formulae can be put
together with or without 1 or several Chinese herbs for
different symptoms and signs manifested by a patient.
Data sources
Data analysis
The NHI program in Taiwan was initiated in 1995, and
the Bureau of the NHI began to release all claims data
in electronic form to the public under the National
Health Insurance Research Database (NHIRD) project
since 1999. The structure of the claims files is described
in detail on the NHIRD website and in our previous
report.6 Briefly, we obtained the database of TCM
claims, including the visit files and prescription files
The database software, IBM DB2 version 8.1 (IBM,
Armonk, NY, USA), was used for data linkage and processing. Regular statistics (mean and percentage) were
displayed for the frequency of use and pattern of CHM
prescriptions for constipation. Association rule mining, originally developed in the 1990s to identify which
groups or sets of items were likely to be purchased
together in the market, was applied to calculate the
376
J Chin Med Assoc • July 2010 • Vol 73 • No 7
Chinese herb use for constipation in Taiwan
prescription of the Chinese herbs for constipation.9,10
An association rule was applied to prescriptions as follows: when a physician prescribes drug A (or drugs
{A1,A2}, drugs {A1,A2,A3}, etc.), he/she will also prescribe drug B in X% of cases, and this co-prescribing is
present in Y% of all prescriptions. The support factor
is the ratio of co-prescriptions of all prescriptions (i.e.
Y% in the above example). The confidence factor is the
ratio of co-prescriptions to prescriptions for drug A
(i.e. X% in the above example). For executing the program to identify association rules in our dataset, we
chose 0.5% as the minimum support factor and 30%
as the minimum confidence level.11
Mu-xiang-bin-lang-wan (4.8%), San-huang-xie-xin-tang
(4.7%), Tao-ren-cheng-qi-tang (4.6%), and Gan-luyin (4.5%; Table 2).
Single Chinese herbs
The most common single Chinese herb prescribed
for constipation was Rheum palmatum (Da-huang)
(18.4%), followed by Magnolia officinalis (Hou-pu)
(6.6%), Scrophularia ningpoensis (Xuan-shen) (6.3%),
Citrus aurantium (fruit; Zhi-shi) (6.1%), Rehmannia
glutinosa (Sheng-di-huang) (6.0%), Ophiopogon japonicus (Mai-dong) (6.0%), Crataegus pinnatifida (Shanzha) (5.7%), Cannabis sativa (Huo-ma-zen) (5.1%),
Glycyrrhiza uralensis (Gan-cao) (5.0%), and Citrus
aurantium (peel; Zhi-ke) (4.5%; Table 3).
Results
Combination of CHM
Epidemiology
Among the 22,134,270 valid beneficiaries of the NHI
at the end of 2004 in Taiwan, 6,224,436 (28.1%) subjects had used TCM during that year, and 152,564
(2.5%) subjects visited the TCM clinics and used CHM
only for constipation. Among these constipation subjects, there were a total of 387,268 CHM prescriptions.
The peak age of subjects with constipation treated by
TCM was between 20 and 29 years of age (25.5%), followed by 30–39 years of age (19.4%), and 40–49 years
of age (15.7%; Table 1). Female subjects used CHM
for constipation more frequently than male subjects
(female:male = 3.31:1).
Chinese herbal formulae
Ma-zi-ren-wan (34.4%) was the most commonly prescribed Chinese herbal formula for subjects with
constipation, followed by Fang-feng-tong-sheng-san
(17.6%), Run-chang-wan (12.4%), Run-chang-tang
(7.7%), Da-chai-hu-tang (6.6%), Ping-wei-san (4.9%),
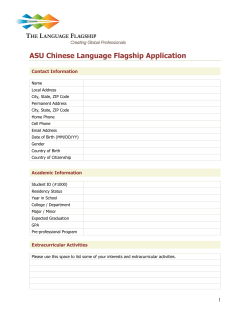
There was an average of 4.6 Chinese herbal items in a
single prescription for subjects with constipation. The
most common number of items in the prescription of
Chinese herbal formulae or single Chinese herbs for
subjects with constipation in Taiwan is 5 (16.6%), followed by 4 (16.5%), and 3 (15.3%; Figure 1). According to the association rule, the most commonly
prescribed pattern of a 2-drug combination of CHM
for treating constipation was Ban-xia-xie-xin-tang plus
Ma-zi-ren-wan (Table 4), while the 3-drug combination of CHM was Fang-feng-tong-sheng-san, Rheum
palmatum and Ma-zi-ren-wan (Table 5). The most
common 4-drug combination of CHM for constipation was Ophiopogon japonicus, Rehmannia glutinosa,
Scrophularia ningpoensis and Run-chang-wan, which
accounted for 0.3% of all prescriptions. The most common 5-drug combination of CHM was An-zhong-san,
Mu-xiang-bin-lang-wan, Run-chang-tang, Fang-fengtong-sheng-san and Ma-zi-ren-wan, which accounted
for 0.2% of all prescriptions.
Table 1. Age-specific frequency of the use of TCM in patients with constipation in Taiwan during 2004*
Subjects with constipation using TCM
Age (yr)
0–9
10–19
20–29
30–39
40–49
50–59
60–69
70–79
≥ 80
Total
Total patients
Males†
Females†
11,013 (7.2)
16,713 (11.0)
38,961 (25.5)
29,969 (19.6)
23,938 (15.7)
11,607 (7.6)
7,621 (5.0)
8,968 (5.9)
3,774 (2.5)
152,564 (100)
4,997 (3.3)
3,716 (2.4)
4,203 (2.8)
4,279 (2.8)
4,480 (2.9)
3,311 (2.2)
3,275 (2.1)
5,131 (3.4)
1,978 (1.3)
35,370 (34.05)
6,016 (3.9)
12,997 (8.6)
34,758 (22.7)
25,690 (16.8)
19,458 (12.8)
8,296 (5.4)
4,346 (2.9)
3,837 (2.5)
1,796 (1.2)
117,194 (65.95)
*Data presented as n (%); †male:female ratio is 1:3.31. TCM = traditional Chinese medicine.
J Chin Med Assoc • July 2010 • Vol 73 • No 7
377
M.S. Jong, et al
Table 2. Top 10 Chinese herbal formulae prescribed for constipation in Taiwan during 2004*
Chinese herbal formulae
(Chinese name)
Ma-zi-ren-wan
Fang-feng-tong-sheng-san
Run-chang-wan
Run-chang-tang
Da-chai-hu-tang
Ping-wei-san
Mu-xiang-bin-lang-wan
San-huang-xie-xin-tang
Tao-ren-cheng-qi-tang
Gan-lu-yin
Ingredients
Prescriptions, n (%)
Cannabis sativa, Paeonia lactiflora, Citrus aurantium, Rheum palmatum,
Magnolia officinalis, Prunus armeniaca
Saposhnikovia divaricata, Forsythia suspenae, Gardenia jasminoides,
Schizonepeta tenuifolia, Ephedra sinica, Ligusticum chuanxiong, Angelica
sinensis, Paeonia lactiflora, Atractylodes macrocephala, Rheum palmatum,
Mirabilite, Scutellaria baicalensis, Talcum, Gypsum Fibrosum, Mentha
haplocalyx, Platycodon grandiflorum, Glycyrrhiza uralensis, Zingiber officinale
Angelica sinensis, Notopterygium incisum, Rheum palmatum, Prunus persica,
Cannabis sativa
Rheum palmatum, Angelica sinensis, Rehmannia glutinosa, Cannabis sativa,
Prunus persica, Prunus armeniaca, Citrus aurantium, Scutellaria baicalensis,
Magnolia officinalis, Glycyrrhiza uralensis
Bupleurum chinense, Scutellaria baicalensis, Paeonia lactiflora, Pinellia ternate,
Citrus aurantium, Rheum palmatum, Ziziphus jujuba, Zingiber officinale
Atractylodes lancea, Magnolia officinalis, Citrus reticulate, Glycyrrhiza uralensis,
Zingiber officinale, Ziziphus jujuba
Saussurea lappa, Areca cathechu, Rheum palmatum, Coptis chinensis,
Phellodendron amurense, Cyperus rotundus, Ipomoea nil, Citrus reticulate,
Citrus reticulate (unripe), Curcuma phaeocaulis, Citrus aurantium, Sparganium
stoloniferum, Mirabilite
Rheum palmatum, Coptis chinensis, Scutellaria baicalensis
Prunus persica, Rheum palmatum, Cinnamomum cassia, Glycyrrhiza
uralensis, Mirabilite
Rehmannia gultinosa, Asparagus cochinchinensis, Ophiopogon japonicus,
Dendrobium nobile, Artemisia scoparia, Eriobotrya japonica, Scutellaria
baicalensis, Citrus aurantium, Glycyrrhiza uralensis
133,288 (34.4)
68,264 (17.6)
47,870 (12.4)
29,927 (7.7)
25,504 (6.6)
18,885 (4.9)
18,689 (4.8)
18,081 (4.7)
17,935 (4.6)
17,482 (4.5)
*Total number of prescriptions = 387,268.
Table 3. Top 10 single Chinese herbs prescribed for constipation in Taiwan during 2004*
Single Chinese herb (Chinese name)
Generic name
Da-huang
Hou-pu
Xuan-shen
Zhi-shi (fruit)
Sheng-di-huang
Mai-dong
Shan-zha
Huo-ma-zen
Gan-cao
Zhi-ke (peel)
Rheum palmatum
Magnolia officinalis
Scrophularia ningpoensis
Citrus aurantium
Rehmannia glutinosa
Ophiopogon japonicus
Crataegus pinnatifida
Cannabis sativa
Glycyrrhiza uralensis
Citrus aurantium
Prescriptions, n (%)
71,133 (18.4)
25,379 (6.6)
24,528 (6.3)
23,443 (6.1)
23,212 (6.0)
23.052 (6.0)
22,055 (5.7)
19,708 (5.1)
19,273 (5.0)
17,501 (4.5)
*Total number of prescriptions = 387,268.
Discussion
The current study, the first large-scale survey of the
use of CHM in the treatment of constipation in a
Chinese population, analyzed the claims dataset of
TCM office visits covered by the NHI in Taiwan. Our
results showed that females were dominant among
TCM users, which is in agreement with the results of
378
a systematic review by Peppas et al,3 who reported that
for those aged between 20 and 29 years, the femaleto-male ratio was 8.1. Chiarelli et al12 proposed that
hormonal factors may contribute to constipation in
women. Progesterone secreted during the luteal phase
of the menstrual cycle or during gestation is thought to
decrease the intestinal transit time, leading to constipation.12 In addition, we also found that most people
J Chin Med Assoc • July 2010 • Vol 73 • No 7
Chinese herb use for constipation in Taiwan
80,000
70,000
63,853 64,227
59,172
60,000
Number of prescriptions
54,187
49,405
50,000
40,000
33,968
30,000
26,663
18,926
20,000
8,553
10,000
4,105
0
1
2
3
4
5
6
7
8
9
≥10
Number of Chinese herbal formulae or
single herbs in a single prescription
Figure 1. The number of combinations of Chinese herbal medicine related to the number of prescriptions. The most common combination of Chinese herbal medicine used for treating constipation was 5, followed by 4 and then 3 items of Chinese herbal formulae or single herbs. There was a mean of 4.6 Chinese herbal items in a single prescription for subjects with constipation.
Table 4. Most common prescription patterns of a 2-drug combination of Chinese herbs in a single prescription for constipation in
Taiwan during 2004*
Chinese herbal formulae or single herbs
Ban-xia-xie-xin-tang plus Ma-zi-ren-wan
Shao-yao-gan-cao-tang plus Ma-zi-ren-wan
Yi-zi-tang plus Ma-zi-ren-wan
Platycladus orientalis plus Ma-zi-ren-wan
San-huang-xie-xin-tang plus Ma-zi-ren-wan
Xie-fu-zhu-yu-tang plus Ma-zi-ren-wan
Liu-wei-di-huang-wan plus Ma-zi-ren-wan
Gan-lu-yin plus Run-chang-wan
Da-huang-mu-dan-pi-tang plus Ma-zi-ren-wan
Cyperus rotundus plus Ma-zi-ren-wan
Support (%)
Prescription number
0.7
0.7
0.6
0.6
0.6
0.6
0.6
0.6
0.5
0.5
2,855
2,781
2,441
2,301
2,297
2,209
2,203
2,150
2,097
2,087
*Total number of prescriptions = 387,268.
using TCM for constipation were between 20 and
29 years of age (25.5%), followed by those between
30 and 39 years of age (19.6%), with the majority being
females. This result is different from the findings
reported by Higgins and Johanson,13 who showed an
increase in the prevalence of constipation with age.
Further studies are needed to clarify this issue and reveal
other causes.
J Chin Med Assoc • July 2010 • Vol 73 • No 7
Rheum palmatum, the most common single Chinese
herb for constipation, is also a component of 8 of the 10
most commonly used herbal formulae for constipation.
Rheum palmatum was first recorded in the classical
Chinese medical tome “Shennongbencaojing”, the earliest Materia Medica in China, before 25–225 AD. At
that time, Rheum palmatum was used as a type of purgative agent. The major bioactive constituents of Rheum
379
M.S. Jong, et al
Table 5. Most common prescription patterns of a 3-drug combination of Chinese herbs in a single prescription for constipation in
Taiwan during 2004*
Chinese herbal formulae or single herbs
Fang-feng-tong-sheng-sa, Rheum palmatum and Ma-zi-ren-wan
Angelica sinensis, Cistanche tubulosa and Ma-zi-ren-wan
Citrus aurantium, Magnolia officinalis and Ma-zi-ren-wan
Rehmannia glutinosa, Fang-feng-tong-sheng-san and Rheum palmatum
Areca catechu, Saussurea lappa and Ma-zi-ren-wan
Da-chai-hu-tang, Fang-feng-tong-sheng-san and Rheum palmatum
Crataegus pinnatifida, Fang-feng-tong-sheng-san and Ma-zi-ren-wan
Run-chang-tang, Rheum palmatum and Ma-zi-ren-wan
Citrus aurantium, Rheum palmatum and Ma-zi-ren-wan
Run-chang-wan, Rheum palmatum and Ma-zi-ren-wan
Support (%)
Prescription number
0.6
0.5
0.4
0.3
0.3
0.3
0.3
0.3
0.3
0.3
2,462
1,817
1,405
1,280
1,223
1,177
1,164
1,083
1,074
1,060
*Total number of prescriptions = 387,268.
palmatum are phenolic compounds, among which sennosides and anthraquinone glycosides are considered to
be the main purgative components.14 This stimulant laxative or its metabolites in the human body can stimulate the intestinal wall, enhance intestinal peristalsis, or
change the transport of liquid and electrolytes, thereby
enhancing gastrointestinal secretion and leading to
purgation.15 Besides Rheum palmatum, other Chinese
herbs also have the ability to modulate gastrointestinal
function. Mirabilite (sodium sulfate decahydrate) has
been reported to have osmotic laxative activity through
poor absorption of sulfate, which increases osmotic pressure and results in water and electrolytes being retained
in the intestinal cavity.16 Ipomoea nil extracts may affect
the ion transport of rat intestinal epithelia, leading to
water movement.17 The aqueous crude extract of
Prunus persica possesses spasmogenic activity in isolated
guinea pig ileum, which may be partially through the
cholinergic pathway.18 In animal experiments, the constituent arecoline in Areca catechu can stimulate colonic
motility through muscarinic acetylcholine receptors.19
Angelica sinensis may possess the ability to react with
serotonin receptors and then promote serotonergic
activity, thereby stimulating intestinal motility.20,21
The active ingredient in Rehmannia glutinosa,
catalpol, is an iridoid glycoside,22,23 and Gardenia jasminoides, which contains iridoid, may also possess purgative activity.24 In ritonavir-treated rats with slower
gastric emptying capability, gastrointestinal dysfunction
is improved after administration of a Scutellaria baicalensis extract.25 Zingiber officinale can speed up gastrointestinal transit in mice fed with a charcoal meal.26
The water-soluble components of Zizyphus jujuba can
reduce gastrointestinal transit time, thus enhancing
water retention in feces.27
The components of commonly used herbal formulae for treating constipation mostly have a purgation
380
effect, as described above by modern pharmacology.
However, there are some Chinese herbs that have an
opposite pharmacological function. For example, cannabidiol is a Cannabis sativa-derived compound that
can selectively inhibit croton oil-induced intestinal
hypermotility in mice,28 and decrease gastrointestinal
movement.29 Cyperus rotundus possesses antidiarrheal
activity.30 These Chinese herbs, which decrease gastrointestinal movement, have been used for the treatment
of constipation. Different pharmacological functions
may be due to the difference between a pure compound
and a crude extract of the herb, or the combined effects
of multi-component formulations, or through different
pathological mechanisms. How 1 Chinese herb can
exert effects that are diametrically opposed is still not
fully understood and deserves further investigation.
Glycycoumarin is 1 active component in Glycyrrhiza
uralensis. It has an antispasmodic effect on the contraction of mouse jejunum through inhibition of the
phosphodiesterase 3 mechanism.31 Other Chinese
medicines such as Magnolia officinalis,32 Mentha sp.,33
and Paeonia lactiflora34 have a spasmolytic effect, which
could possibly be beneficial for spasmodic constipation.35 In isolated animal tissue, the aqueous-methanol
crude extract of Saussurea lappa possesses a spasmogenic
effect through the cholinergic pathway. However,
under conditions such as a higher drug concentration
or intestinal hypermotility, the spasmolytic effect appears through a calcium channel blocker mechanism.36
Therefore, even for the same Chinese herb, there may
be different pharmacological functions with different
dosages or physical conditions.
Among the top 10 single Chinese herbs prescribed
for constipation, Scrophularia ningpoensis contains a
bioactive compound, iridoid, which possibly possesses
a purgative effect,23 and Crataegus pinnatifida was
once reported to have an antispasmodic effect.37 In the
J Chin Med Assoc • July 2010 • Vol 73 • No 7
Chinese herb use for constipation in Taiwan
classification of Chinese medicine, Ophiopogon japonicus is categorized as a Yin-tonifying medicinal, capable of nourishing Yin fluid and therefore moistening
the intestine.
In the top 10 Chinese herbal formulae prescribed
for constipation, Fang-feng-tong-sheng-san (Bofutsusho-san in Japanese) is usually used to combat
obesity.38 Da-chai-hu-tang extracts and San-huangxie-xin-tang extracts relax smooth muscle tone in the
gastrointestinal tract through phosphodiesterase inhibition, and are therefore capable of treating spasmodic
constipation.39 Ping-wei-san is usually applied for the
treatment of heartburn and gastritis.40 It is worth noting that Fang-feng-tong-sheng-san and Da-chai-hu-tang
have been reported to cause interstitial pneumonia or
hepatitis during clinical practice.41,42 It is often difficult
to completely understand the underlying mechanisms.
Therefore, it is necessary to conduct randomized,
double-blinded, placebo-controlled trials to assess the
efficacy and safety of these Chinese medicines in patients
with constipation. Additionally, Cistanche tubulosa contains iridoid glycosides, and thus possibly has purgative effects.43 Ban-xia-xie-xin-tang is reported to have
antidiarrheal activity,44 and Shao-yao-gan-cao-tang has
an antispasmodic effect.45
In our study, an average of 4.6 items, either Chinese
herbal formulae or single herbs, were contained in each
prescription for constipation. According to our results,
the most commonly prescribed CHM drug combination for treating constipation was mainly an herbal
formula and single herb.
This study was a retrospective analysis of the use of
CHM to treat constipation. Unlike clinical trials, which
can provide direct evidence of efficacy, many herbs in
the herbal formulae or single herbs frequently prescribed have been found to contain ingredients that assist defecation via varied mechanisms as discussed above.
In fact, the principle of TCM treatment is different
from that of Western medicine, as TCM involves the
patient’s constitutional needs, e.g. Bianzheng Lunzhi
(ᙃᢞᓵए, syndrome differentiation and treatment),46
and therefore, it is difficult to create a constitutionallymatched control group. With regard to the treatment
of constipation, although Chinese and Western medicine view the causes of the disease differently, both are
in agreement that constipation is a symptom rather than
a diagnosis. TCM treatment for constipation is based
on the syndrome of its subclassification; for example, if
the symptoms include a dry mouth, yellow urine, a red
tongue and surging pulse, it is subclassified as excess
syndrome (ኔᢞ) for which a formula such as Ma-zi-renwan can be prescribed, as it can discharge excessive
heat.47 On the other hand, if the symptoms include
J Chin Med Assoc • July 2010 • Vol 73 • No 7
fatigue, a pale complexion, pale tongue and a thready,
weak pulse, it is subclassified as deficient syndrome
(ဠᢞ). Therefore, a formula or single herb that can nourish Qi and Yin will be administered; in this case, Runchang-tang or Ophiopogon japonicus is a good choice.
In young people, constipation is mostly subclassified
as excess syndrome, which may explain why this study
found Ma-zi-ren-wan to be the formula most commonly prescribed for the treatment of constipation.
In conclusion, based on the availability of electronic
health care claims data in Taiwan, a population-based
survey of Chinese herbal pharmacoepidemiology on
constipation determined the frequency of use and patterns of prescriptions in a Chinese population. Nevertheless, the therapeutic effects and safety of those herbal
formulae or single herbs used requires further elucidation through efficiency-based clinical studies or
well-designed randomized, double-blinded, placebocontrolled trials.
Acknowledgments
This study was based on a portion of data from the
NHI Research Database provided by the Bureau of
NHI, Department of Health, and was managed by
the NHI Research Institutes in Taiwan. The interpretation and conclusions contained herein do not represent
those of the Bureau of NHI, Department of Health, or
National Health Research Institutes.
References
1. Longstreth GF, Thompson WG, Chey WD, Houghton LA,
Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology 2006;130:1480–91.
2. Lu CL, Chang FY, Chen CY, Luo JC, Lee SD. Significance of
Rome II-defined functional constipation in Taiwan and comparison with constipation-predominant irritable bowel syndrome.
Aliment Pharmacol Ther 2006;24:429–38.
3. Peppas G, Alexiou VG, Mourtzoukou E, Falagas ME. Epidemiology of constipation in Europe and Oceania: a systematic
review. BMC Gastroenterol 2008;8:5.
4. Johanson JF. Review of the treatment options for chronic constipation. Medgenmed [Computer file]. MedGenMed 2007;9:25.
5. Bharucha AE. Constipation. Best Pract Res Clin Gastroenterol
2007;21:709–31.
6. Chen FP, Chen TJ, Kung YY, Chen YC, Chou LF, Chen FJ,
Hwang SJ. Use frequency of traditional Chinese medicine in
Taiwan. BMC Health Serv Res 2007;7:26.
7. Cheng SH, Chiang TL. The effect of universal health insurance
on health care utilization in Taiwan: results from a natural experiment. JAMA 1997;278:89–93.
8. Bureau of National Health Insurance, Department of Health,
Executive Yuan, R.O.C. Available at: http://www.nhi.gov.tw/
webdata/webdata.asp?menu=1&menu_id=4&webdata_id=
1399&WD_ID= [Date accessed: August 10, 2005]
381
M.S. Jong, et al
9. Berry MJ, Linoff G. Data Mining Techniques: For Marketing
Sales, and Customer Support. New York: Welly Press, 1997.
10. Han J, Kamber M. Data Mining: Concepts and Techniques. San
Francisco: Morgan Kaufmann Press, 2001.
11. Chen TJ, Chou LF, Hwang SJ. Application of a data-mining
technique to analyze coprescription patterns for antacids in
Taiwan. Clin Ther 2003;25:2453–63.
12. Chiarelli P, Brown W, McElduff P. Constipation in Australian
women: prevalence and associated factors. Int Urogynecol J 2000;
11:71–8.
13. Higgins PD, Johanson JF. Epidemiology of constipation in
North America: a systematic review. Am J Gastroenterol 2004;
99:750–9.
14. Xiao P, He L, Wang L. Ethnopharmacologic study of Chinese
rhubarb. J Ethnopharmacol 1984;10:275–93.
15. Ewe K. The physiological basis of laxative action. Pharmacology
1980;20(Suppl):2–20.
16. Heizer WD, Sandler RS, Seal E Jr, Murray SC, Busby MG,
Schliebe BG, Pusek SN. Intestinal effects of sulfate in drinking
water on normal human subjects. Dig Dis Sci 1997;42:
1055–61.
17. Tsai JC, Tsai S, Chang WC. Comparison of two Chinese medical
herbs, Huangbai and Qianniuzi, on influence of short circuit
current across the rat intestinal epithelia. J Ethnopharmacol 2004;
93:21–5.
18. Gilani AH, Aziz N, Ali SM, Saeed M. Pharmacological basis
for the use of peach leaves in constipation. J Ethnopharmacol
2000;73:87–93.
19. Xie DP, Chen LB, Liu CY, Zhang CL, Liu KJ, Wang PS.
Arecoline excites the colonic smooth muscle motility via M3
receptor in rabbits. Chin J Physiol 2004;47:89–94.
20. Deng S, Chen SN, Yao P, Nikolic D, van Breemen RB, Bolton
JL, Fong HH, et al. Serotonergic activity-guided phytochemical investigation of the roots of Angelica sinensis. J Nat Prod
2006;69:536–41.
21. Galligan JJ, Vanner S. Basic and clinical pharmacology of new
motility promoting agents. Neurogastroenterol Motil 2005;17:
643–53.
22. Tian YY, An LJ, Jiang L, Duan YL, Chen J, Jiang B. Catalpol
protects dopaminergic neurons from LPS-induced neurotoxicity
in mesencephalic neuron-glia cultures. Life Sci 2006;80:193–9.
23. Tundis R, Loizzo MR, Menichini F, Statti GA, Menichini F.
Biological and pharmacological activities of iridoids: recent
developments. Mini Rev Med Chem 2008;8:399–420.
24. Yamauchi K, Fujimoto N, Kuwano S, Inouye H, Inoue K. The
mechanism of purgative action of geniposide, an iridoid glucoside of the fruit of Gardenia, in mice. Planta Med 1976;30:
39–47.
25. Mehendale S, Aung H, Wang CZ, Tong R, Foo A, Xie JT, Yuan
CS. Scutellaria baicalensis and a constituent flavonoid, baicalein,
attenuate ritonavir-induced gastrointestinal side-effects. J Pharm
Pharmacol 2007;59:1567–72.
26. Yamahara J, Huang QR, Li YH, Xu L, Fujimura H.
Gastrointestinal motility enhancing effect of ginger and its active
constituents. Chem Pharm Bull 1990;38:430–1.
27. Huang YL, Yen GC, Sheu F, Chau CF. Effects of water-soluble
carbohydrate concentrate from Chinese jujube on different intestinal and fecal indices. J Agric Food Chem 2008;56:1734–9.
28. Capasso R, Borrelli F, Aviello G, Romano B, Scalisi C, Capasso F,
Izzo AA. Cannabidiol, extracted from Cannabis sativa, selectively
inhibits inflammatory hypermotility in mice. Br J Pharmacol
2008;154:1001–8.
29. De Filippis D, Iuvone T, D’Amico A, Esposito G, Steardo L,
Herman AG, Pelckmans PA, et al. Effect of cannabidiol on
382
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
sepsis-induced motility disturbances in mice: involvement of
CB(1) receptors and fatty acid amide hydrolase. Neurogastroenterol Motil 2008;20:919–27.
Uddin SJ, Mondal K, Shilpi JA, Rahman MT. Antidiarrhoeal
activity of Cyperus rotundus. Fitoterapia 2006;77:134–6.
Sato Y, Akao T, He JX, Nojima H, Kuraishi Y, Morota T, Asano
T, et al. Glycycoumarin from Glycyrrhizae Radix acts as a potent
antispasmodic through inhibition of phosphodiesterase 3.
J Ethnopharmacol 2006;105:409–14.
Chan SS, Zhao M, Lao L, Fong HH, Che CT. Magnolol and
honokiol account for the anti-spasmodic effect of Magnolia officinalis in isolated guinea pig ileum. Planta Med 2008;74:381–4.
Grigoleit HG, Grigoleit P. Gastrointestinal clinical pharmacology
of peppermint oil. Phytomedicine 2005;12:607–11.
Yang HO, Ko WK, Kim JY, Ro HS. Paeoniflorin: an antihyperlipidemic agent from Paeonia lactiflora. Fitoterapia 2004;75:45–9.
Quartero AO, Meineche-Schmidt V, Muris J, Rubin G, de Wit
N. Bulking agents, antispasmodic and antidepressant medication
for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2005;2:CD003460.
Gilani AH, Shah AJ, Yaeesh S. Presence of cholinergic and calcium antagonist constituents in Saussurea lappa explains its use
in constipation and spasm. Phytother Res 2007;21:541–4.
Chang Q, Zuo Z, Harrison F, Chow MS. Hawthorn. J Clin
Pharmacol 2002;42:605–12.
Akagiri S, Naito Y, Ichikawa H, Mizushima K, Takagi T, Handa
O, Kokura S, et al. Bofutsushosan, an oriental herbal medicine,
attenuates the weight gain of white adipose tissue and the
increased size of adipocytes associated with the increase in their
expression of uncoupling protein 1 in high-fat diet-fed male
KK/Ta mice. J Clin Biochem Nutr 2008;42:158–66.
Saegusa Y, Sugiyama A, Takahara A, Nagasawa Y, Hashimoto K.
Relationship between phosphodiesterase inhibition induced by
several Kampo medicines and smooth muscle relaxation of gastrointestinal tract tissues of rats. J Pharmacol Sci 2003;93:62–8.
Riedlinger JE, Tan PW, Lu W. Ping wei san, a Chinese medicine for gastrointestinal disorders. Ann Pharmacother 2001;
35:228–35.
Hatanaka N, Yamagishi T, Kamemura H, Nakazawa I, Hirano
Y, Hosaka K, Sanno K, et al. A case of hepatitis and pneumonitis caused by Bofutsusyo-san herbal medicine. Nihon Kokyuki
Gakkai Zasshi 2006;44:335–9. [In Japanese]
Ikegami F, Sumino M, Fujii Y, Akiba T, Satoh T. Pharmacology
and toxicology of Bupleurum root-containing Kampo medicines
in clinical use. Hum Exp Toxicol 2006;25:481–94.
Xie H, Morikawa T, Matsuda H, Nakamura S, Muraoka O,
Yoshikawa M. Monoterpene constituents from Cistanche tubulosa: chemical structures of kankanosides A-E and kankanol.
Chem Pharm Bull 2006;54:669–75.
Kase Y, Hayakawa T, Ishige A, Aburada M, Komatsu Y. The
effects of Hange-shashin-to on the content of prostaglandin E2
and water absorption in the large intestine of rats. Biol Pharm
Bull 1997;20:954–7.
Ai M, Yamaguchi T, Odaka T, Mitsuhashi K, Shishido T, Yan J,
Seza A, et al. Objective assessment of the antispasmodic effect
of shakuyaku-kanzo-to (TJ-68), a Chinese herbal medicine, on
the colonic wall by direct spraying during colonoscopy. World J
Gastroenterol 2006;12:760–4.
Chen FP, Chen FJ, Jong MS, Tsai HL, Wang JR, Hwang SJ.
Modern use of Chinese herbal formulae from Shang-Han Lun.
Chin Med J 2009;122:1889–94.
Cheng CW, Bian ZX, Wu TX. Systematic review of Chinese
herbal medicine for functional constipation. World J Gastroenterol
2009;15:4886–95.
J Chin Med Assoc • July 2010 • Vol 73 • No 7
Chinese herb use for constipation in Taiwan
Appendix I. Summary of the scientific and Chinese equivalents of herbs and names appearing in this article
Angelica sinensis
Areca catechu
Artemisia scoparia
Asparagus cochinchinensis
Atractylodes lancea
Atractylodes macrocephala
Bupleurum chinense
Cannabis sativa
Cinnamomum cassia
Citrus aurantium
Citrus reticulate
Cistanche tubulosa
Coptis chinensis
Crataegus pinnatifida
Curcuma phaeocaulis
Cyperus rotundus
Dendrobium nobile
Ephedra sinica
Eriobotrya japonica
Forsythia suspense
Gardenia jasminoides
Glycyrrhiza uralensis
Gypsum Fibrosum
Ipomoea nil
ᅝូ
ឳᄏ
౼ຫ
֚॰מ
፧ؠ
ؠػ
־ո
ெࣤ
᷾ኔʻླྀʼ
ॹʻຫʼؼ
ۚⳠፚ
႓ຑ
՞⛹
⌇ؠ
ଉॵ
فක
႓
ࣣᆺ
ຑ
՞ඹ
ز౻
فፏ
ׄ
Ligusticum chuanxiong
Magnolia officinalis
Mentha haplocalyx
Mirabilite (sodium sulfate decahydrate)
Notopterygium incisum
Ophiopogon japonicus
Paeonia lactiflora
Phellodendron amurense
Pinellia ternate
Platycladus orientalis
Platycodon grandiflorum
Prunus armeniaca
Prunus persica
Rehmannia glutinosa
Rheum palmatum
Saposhnikovia divaricata
Saussurea lappa
Schizonepeta tenuifolia
Scrophularia ningpoensis
Scutellaria baicalensis
Sparganium stoloniferum
Talcum
Zingiber officinale
Ziziphus jujuba
՟ᮺ
দڸ
ᜳ๛ᆺ
ߝ࿎
ु
ຽ॰מ
ߟᢐ
႓ਹ
ת
ਹո
ே
ޖո
ո
چ႓
Օ႓
ଅ
ֵଉ
౸ग़
خ
႓ᴗ
Կᆆ
ᄶف
س᜶
Օའ
Appendix II. Summary of the English (Hanyu Pinyin) and Chinese equivalents of formulae and names appearing in this article
An-zhong-san
Ban-xia-xie-xin-tang
Da-chai-hu-tang
Da-huang-mu-dan-pi-tang
Fang-feng-tong-sheng-san
Gan-lu-yin
Liu-wei-di-huang-wan
Ma-zi-ren-wan
Mu-xiang-bin-lang-wan
ڜխཋ
תើ֨ྏ
Օྏ
Օ႓߃կྏؼ
ଅຏᆣཋ
زႏ
ք࠺چ႓Մ
ոՄ
Ping-wei-san
Run-chang-tang
Run-chang-wan
San-huang-xie-xin-tang
Shao-yao-gan-cao-tang
Tao-ren-cheng-qi-tang
Xie-fu-zhu-yu-tang
Yi-zi-tang
ؓષཋ
ᑮᆩྏ
ᑮᆩՄ
Կ႓ើ֨ྏ
ߟᢐز౻ྏ
ոʻுʼࢭྏ
ۨࢌດᅟྏ
Ԭྏڗ
ֵଉឳᄏՄ
J Chin Med Assoc • July 2010 • Vol 73 • No 7
383
© Copyright 2025