Prevention And Treatment of Critical Care Delirium Catherine Dudick MD FACS
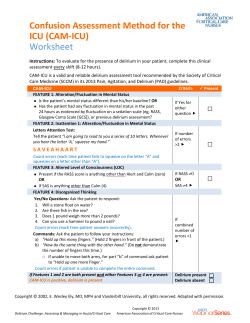
Prevention And Treatment of Critical Care Delirium Catherine Dudick MD FACS AtlantiCare Trauma Symposium May 20 2013 Disclosures icudelirium.org Morandi et al Int Care Med 2008;34:1907- Critical Care Delirium What is it? Why is it important? How can it be prevented/treated? Delirium Defined Morandi et al Int Care Med 2008;34:1907-15 What is delerium? Disturbance of consciousness (inattention) Acute in onset Accompanied by change in perception Generally reversible NOT dementia Generalized cognitive impairment Deterioration of previously acquired intellectual abilities Gradual in onset No clouding of consciousness Arousal AND Content Delirium Subtypes Combative Agitated Restless Hyperactive Delirium Mixed Delirium Alert & Calm Lethargic Sedated Stupor Hypoactive Delirium Prevalence in the ICU Occurs in up to 80% MICU/TICU/SICU ventilated patients 20-50% of lower severity ICU patients 65-70% goes undiagnosed if routine monitoring not done 10% remain delirious at hospital discharge Eli et al JAMA 2004;291:1753-62 Pathophysiology of Delirium Flacker, et al J Gerontol Bio Scien 1999; p47 Pathophysiology of Delirium Flacker, et al J Gerontol Bio Scien 1999; p47 Risk Factors of Delirium Medical conditions Preexisting dementia Substance intoxication or h/o HTN and/or alcholism withdrawl Toxin exposure Preexisting cognitive dysfunction severity of illness at admission Coma (independent risk factor) Benzodiazepines Age>70 years ? Propofol AAA surgery Sleep deprivation Poor functional status Combination Psychoactive medication Flynn et al JACS 2009;209:261-268 Panharepande, Anesthesiology 2006;104:21-26 Panharepande, Anesthesiology 2006;104:21-26 Panharepande, Anesthesiology 2006;104 Delirium in Pneumonia “altered mental status” strongest independent predictor of mortality in CAP (p<0.001) Relationship stronger with increasing age Waterer et al AJRCCM 2004;169:910-914 Delirium post op in SICU 100 non elective Surgical ICU patients Delirium prevalence 69% Average 4 days longer in ICU (p=0.03) Fewer days alive and vent-free (p=0.001) Midazolam was strongest modifiable predictor Pandharepande et al, SCCM 2006 ICU Delirium Increased ICU length of stay (8 vs 5 days) Increased hospital length of stay (21 vs 11 days) Increased time on ventilator (9 vs 4 days) Higher ICU costs ($22,000 vs $13,000) Higher ICU mortality (19.7% vs 10.3%) Higher hospital mortality (26.7% vs 21.4%) 3-fold increased risk of death at 6 months Ely, et al. ICM2001; 27, 1892-1900 Ely, et al, JAMA 2004; 291: 1753-1762 Lin, SM CCM 2004; 32: 2254-2259 Milbrandt E, et al, Crit Care Med 2004; 32:955-962. Ouimet, et al, ICM 2007: 33: 66-73. P<0.00 1 Ely et al JAMA 2004;291:1753-176 Ely et al JAMA 2004;291:1753-17 P<0.008 Ely et al JAMA 2004;291:1753- Ely et al JAMA 2004;291:1753-1762 Pisani et al Am J RCCM 2009;180:1092-1097 Cost of Delirium Milbrandt et al Crit Care Med 2004;32:955-62 Importance of Delirium ICU delirium is a predictor of: Mortality LOS Ventilator time Cost Reintubation Long term cognitive impairment Discharge to LTC facility Diagnosis and Management Occurs in up to 80% of MICU/SICU/TICU ventilated patients Occurs in 20-50% of lower severity ICU patients Hypoactive & mixed forms most common 65-70% goes undiagnosed if routine monitoring not done Delirium Management 1. Screen 2. Identify risk factors/etiology 3. Consider NON pharmacologic & pharmacologic treatment Jacobi J, et al. Crit Care Med 2002;30:119-141 Delirium Risk Factors Pneumonics icudelirium.org Assess and treat pain Assess and adjust sedation Screen for delirium and its treatable causes Crit Care Med 2013;41:263-306 Assess and treat pain Assess and adjust sedation Screen for delirium and its treatable causes Crit Care Med Arousal AND Content Delirium monitoring Screening recommended (B) 75% of delirium missed if screening not done The Confusion Assessment Method for the ICU(CAM-ICU) & Intensive Care Delirium Screening Checklist (ISDSC) most reliable Routine monitoring is feasible in clinical practice SCCM Guidelines, Crit Care Med 2013;41:263-306 CAM-ICU ICDSC Assess and treat pain Assess and adjust sedation Screen for delirium and its treatable causes SCCM Guidelines, Crit Care Med Sedation Light levels of sedation associated with improved clinical outcome (B) Light sedations causes increased physiologic stress but no increased myocardial ischemia (B) RASS (Richmond Agitation-Sedation Scale) or SAS (Sedation Agitation Scale) most reliable (B) SCCM Guidelines, Crit Care Med 2013;41:26 Sedation “Non benzodiazepine sedatives (either propofol or dexmedeomidine) may be preferred over sedation with benzodiazepines (either midazolam or lorazepam) to improve clinical outcomes in mechanically ventilated ICU patients” (+2B) Change from 2002 guidelines (midazolam, short term sedation; lorazepam, long term sedaiton; propofol for intermittent awakening) SCCM Guidelines, Crit Care Med 2013;41:263-306 Benzodiazepines Activate γ-aminobutyric acid A (GABA) neuronal receptors in brain Anxiolytic, sedating, hypnotic, anticonvulsant properties NO analgesia Amnestic effects extend beyond sedative effects Tolerance with long term administration Metabolized in liver Benzodiazepines Cause respiratory depression Systemic hypotension Elderly more sensitive Lorazepam cleared slower Studies suggest longer awakening with midazolam versus lorazepam Diazepam has prolonged duration of action Panharepande, Anesthesiology 2006;104 Propofol Binds to multiple CNS receptors (GABAA, glycine, nicotinic, M1 muscarinic) Sedative, hypnotic, anxiolytic, amnestic, antiemetic, anticonvulsant NO analgesia Dose dependent respiratory depression and hypotension PRIS (propofol infusion syndrome dexmedetomidine Selective α2 receptor agonist Sedative, analgesic/opiod sparing sympathomimetic properties Side effects of hypotension and bradycardia No significant effect on respiratory drive SCCM Guidelines, Crit Care Med 2013;41:263-306 SCCM Guidelines, Crit Care Med 2013;41:263-306 Sedation Strategy Analgesia first sedation Propofol or dexmedetomidate before benzodiazepines? SCCM Guidelines, Crit Care Med 2013;41:263-306 Assess and treat pain Assess and adjust sedation Screen for delirium and its treatable causes SCCM Guidelines, Crit Care Med 2013;41:263-306 Acute Pain Unrelieved pain has significant and long term consequences Majority(82%) of non-ICU hospitalized patients remember ETT discomfort and ICU pain Increased catecholamines Arteriolar vasoconstriction, impaired tissue perfusion, decreased tissue paO2 Hypermetabolism (lipolysis, slow healing, catabolism) Risk factor for developing chronic, often neuropathic pain SCCM Guidelines, Crit Care Med 2013;41:263-306 Acute Pain IV opiods are the first line drug of choice for non neuropathic pain in ICU patients(+1C) All equally effective when titrated to similar pain intensity endpoints(C) Enteral gabapentin or carbamazepine should be added for neuropathic pain(+1A) Use non opiod meds to decrease opiod load(+2C) Thoracic epidural considered for rib fractures (+2B) SCCM Guidelines, Crit Care Med 2013;41:263-306 It’s a Balance Analgesia, amnesia, sedation vs. delirium risk Seek goal but don’t overshoot Arousal and content Pharmacologic treatment 11. Milbrandt et al. Critical care medicine 2005 Jan;33(1):2269 Pharmacologic management www.surgicalcriticalcare.net/Guidelines/delirium_2011 Prevention Early mobilization (+1B) NO recommendation for pharmacologic, non- pharmacologic or combined prevention protocol No recommendation for use of Haldol No recommendation for use of Dexmedetomidate SCCM Guidelines, Crit Care Med 2013;41:26 Early Mobilization Early Mobilization Safe Decreases ICU LOS Improves skin integrity Saves money Bailey et al, Crit Care Med 2007;35:1 “Wake up and Breathe” Awakening and Breathing Controlled (ABC)Trial \ Paired daily interruption of sedation with spontaneous breathing trials 3 less days on vent (p=0.02) 3 less days in ICU (p=0.03) 5 less days in hosp (p=0.03) Improved mortality (p=0.01) For every 7 patients treated, one life saved Girard et al, Lancet 2008;371:126-134 www.icudelirium.org Girard et al, Lancet 2008;371:126-134 Girard et al, Lancet 2008;371:126-134 Sleep Sleep loss associated with irritability, memory loss, inattention, delusions, slurred speech, blurred vision, uncoordination Sleep loss and delirium Sleep in the ICU Long sleep onset Sleep fragmentation/frequent arousals Predominance of stage 1 &2 non REM sleep Decreased or absent stage 3 NREM sleep and REM sleep Melatonin production decrease in critically ill patients Mistraletti et al, Minerva Anestesiol 2008;74:329-33 Sleep and Hypnotics Increase total sleep time Alter physiological progression of sleep phases Decrease time in restorative phases Mistraletti et al, Minerva Anestesiol 2008;74:329-33 Melatonin Nocturnal sleep quality severely compromised Melatonin use associated with increased nocturnal sleep efficiency 1-2mg Bournel et al, Critical Care 2008;12:R52 14 subjects in simulated ICU environment poorer perceived sleep quality more light sleep (P < longer rapid eye movement (REM) latency 0.05) less REM sleep decreased nocturnal melatonin (P = 0.007) increased cortisol secretion levels (P = 0.004) anxiety levels similar (P = 0.06). Use of earplugs and eye masks more REM time shorter REM latency less arousal (P < 0.05) elevated melatonin levels (P = 0.002). ABCDE Protocol ICU Delirium and Cognitive Impairment Study Group www.icudelirium.org delirium@vanderbilt.edu Stop and THINK Do any meds need to be stopped or lowered? Especially consider sedatives Is patient on minimal amount necessary? Daily sedation cessation Targeted sedation plan Assess target daily Do sedatives need to be changed? Remember to assess for pain! Toxic Situations • CHF, shock, dehydration • New organ failure (liver/kidney) Hypoxemia Infection/sepsis (nosocomial), Immobilization Nonpharmacologic interventions • Hearing aids, glasses, reorient, sleep protocols, music, noise control, ambulation K+ or electrolyte problems Consider antipsychotics after evaluating etiology & risk factors E Early Exercise and Mobility Early Exercise and Mobility Eligibility = All patients are eligible for Early Exercise and Mobility Early Exercise in the ICU Early exercise = progressive mobility Study design: paired SAT/SBT protocol with PT/OT from earliest days of mechanical ventilation Wake Up, Breathe, and Move Schweickert WD, et al. Lancet. 2009;373:1874-1882. Early Exercise Study Results Intervention (n=49) Control (n=50) P 29 (59%) 19 (35%) 0.02 2.0 (0.0-6.0) 4.0 (2.0-7.0) 0.03 33 (0-58) 57 (33-69) 0.02 2.0 (0.0-6.0) 4.0 (2.0-8.0) 0.02 28 (26) 41 (27) 0.01 75 (7.5-95) 55 (0-85) 0.05 15 (31%) 27 (49%) 0.09 Ventilator-free days 23.5 (7.4-25.6) 21.1 (0.0-23.8) 0.05 Length of stay in ICU (days) 5.9 (4.5-13.2) 7.9 (6.1-12.9) 0.08 Length of stay in hospital (days) 13.5 (8.0-23.1) 12.9 (8.9-19.8) 0.93 9 (18%) 14 (25%) 0.53 Outcome Functionally independent at discharge ICU delirium (days) Time in ICU with delirium (%) Hospital delirium (days) Hospital days with delirium (%) Barthel index score at discharge ICU-acquired paresis at discharge Hospital mortality Schweickert WD, et al. Lancet. 2009;373:1874-1882. Perform Safety Screen First Safety Screen Patient responds to verbal stimulation (i.e., RASS > -3) FIO2 <0.6 PEEP <10 cmH2O No dose of any vasopressor infusion for at least 2 hours No evidence of active myocardial ischemia (24 hrs) No arrhythmia requiring the administration of new antiarrhythmic agent (24hrs) If patient passes Exercise/Mobility Safety Screen, move on to Exercise and Mobility Therapy If patient fails, s/he is too critically ill to tolerate exercise/mobility Early Exercise & Mobility Levels of Therapy* 1. Active range of motion in bed and sitting position in bed 2. Dangling 3. Transfer to chair (active), includes standing without marching in place 4. Ambulation (marching in place, walking in room or hall) *All may be done with assistance. Benefits of ABCDE Protocol Morandi A et al. Curr Opin Crit Care,2011;17:43-9 Questions???? Resources and References www.icudelirium.org www.sccm.org www.surgicalcriticalcare.net icusteps.org journals.lww.com/ccmjournal Delirium per CMS 2008 “Never Event”: errors in medical care that are clearly identifiable, preventable, and serious I consequences and indicate a problem in the safety of a healthcare facility. 2009 discussion: The next “never” event? Delirium has gained publicity Prevalence in the News
© Copyright 2025