Methicillin-Resistant
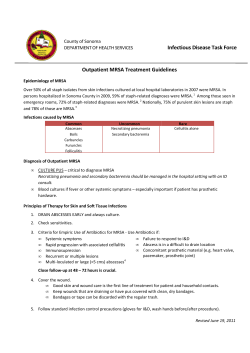
632SRBtoBCompPRNT 2/9/07 2:18 PM Page 1 Distributed by the publishers of Supported and approved by CRITICAL CARE SPECIAL EDITION A ll THE SCIENCE BEHIND PATIENT OUTCOMES ri py ts Co gh ri re gh se t rv © .R 20 ed 09 du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep Methicillin-Resistant Staphylococcus aureus Authors Donald E. Fry, MD, FACS Professor Emeritus Department of Surgery University of New Mexico School of Medicine Albuquerque, New Mexico Marin H. Kollef, MD Professor of Medicine Washington University School of Medicine Director, Medical Critical Care Director, Respiratory Care Services Barnes-Jewish Hospital St. Louis, Missouri Section I: The Pathophysiology of Skin Infections By Donald E. Fry, MD, FACS Section II: Pharmacoeconomic Considerations in the Treatment of Hospital-Associated Methicillin-Resistant Staphylococcus aureus By Alan D. Tice, MD te Section III: Toxin Inhibition and Gram-Positive Infection: Focus on Methicillin-Resistant Staphylococcus aureus Expressing the Panton-Valentine Leukocidin Gene Associate Professor John A. Burns School of Medicine University of Hawaii Honolulu, Hawaii By Marin H. Kollef, MD d. Alan D. Tice, MD 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 2 THE SCIENCE BEHIND PATIENT OUTCOMES A ll Section I: The Pathophysiology of Skin Infections ri Co gh Donald E. Fry, MD, FACS py ts Professor Emeritus Department of Surgery University of New Mexico School of Medicine Albuquerque, New Mexico ri re gh se t rv © ep 09 .R 20 ed Introduction du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M Infections of the skin and adjacent subcutaneous tissues are among the most common bacterial infections at major medical centers.1 The spectrum of these infections may vary from a simple, self-contained cellulitis to a severe, lifethreatening, and rapidly evolving necrotizing fasciitis. Many types of infections are seen between these 2 extremes. Erysipelas, furuncle, carbuncle, impetigo, and hidradenitis suppurativa are a few of the names that are used for the variable expressions of skin and soft tissue infections. Clinical infection is the activation of the local inflammatory response secondary to the proliferation of microbial pathogens within human tissue. An understanding of the pathophysiology of this complex process in the skin and soft tissues requires an understanding of the anatomy of the skin, knowledge of the potential pathogens that cause the infections, and insight into the human inflammatory response that attempts to contain and eradicate the microbes. Pathophysiology The Pathogen Infection arising from the skin is caused either by bacterial colonists that normally reside on the skin or by exogenous microbes that are carried into the skin and soft tissues as colonization that pre-existed on the wounding device. For example, gas gangrene from Clostridium perfringens is colonization that existed on the device causing the puncture, rather than being a normal colonist of the skin by the mechanism of wounding. Human skin normally has a diverse and rather large population of bacterial colonists (Table 1).2,3 They colonize the skin surface and transiently colonize the follicles and glandular openings before being expelled by normal secretions. Infection of the skin is most commonly the result of normal skin colonization that breaches the barrier with the wounding process. Of the many different bacterial strains that colonize skin, only a limited number are actually pathogenic. Staphylococcus aureus and Streptococcus pyogenes are the specific bacteria that are most likely to cause infection from skin colonization. The gram-positive cocci of normal skin colonization have particular virulence factors that make them aggressive pathogens in the injury site or within the obstructed glandular drainage systems of the skin. S. aureus is most noted for the production of coagulase, a potent enzyme that activates the coagulation cascade of the host.4 The precipitation of fibrin from the coagulation cascade creates an environment that protects the staphylococci from the phagocytic mechanisms of the host. Coagulase also te d. The anatomic structure of the skin provides a barrier to infection but also opportunities for infection to occur. The squamous epithelium of the epidermis provides a waterimpervious and resilient barrier against bacteria. This barrier function is the most basic and effective of the nonspecific host defenses. The surface of the skin is always colonized, but infection only occurs when a breach of the barrier occurs. Infection occurs in the skin by 2 mechanisms. The most common mechanism of infection occurs when there is a violation of the barrier from mechanical injury in the form of cuts, abrasions, punctures, or thermal injury. The microbe is introduced into the soft tissues with injury, and begins to multiply and invade the soft tissues. This multiplication and invasion results in activation of the human 2 inflammatory cascade, which then results in the erythema, induration, and pus that characterizes infection. However, the skin also has openings that are potential microbial havens. These openings in the skin communicate with hair follicles, sweat glands, and sebaceous glands. Normal surface bacteria are constantly gaining access to these openings, but the normal flow of sweat and sebaceous products keeps colonists from proliferating and invading the adjacent soft tissues. Any obstruction to the flow of sweat, oils, and sebaceous secretions can lead to infection. Exfoliated cells and hyperviscous secretions may occlude the flow of the normal secretions. Skin edema from contusions, abrasions, congestive heart failure, hypoalbuminemia, and radiation can all increase the hydrostatic pressure within the skin and obstruct the flow of normal secretions. With retention of bacteria in the ductal systems of the skin, proliferation of the pathogen occurs, the invasive and digestive enzymes of the pathogen degrade the epithelial barrier, and invasive infection occurs. 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 3 Supported and approved by Pfizer Table 1. Bacteria That Normally Colonize the Skin of Humans A Brevibacter species ll Corynebacterium species ri Co gh Micrococcus species py ts Propionibacter species ri re Staphylococcus albus gh se Staphylococcus aureus t rv 09 ep Streptococcus pyogenes 20 .R Staphylococcus hominis © ed Staphylococcus epidermidis du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M Note: Some authors have noted that the human skin has more bacterial colonists than the human body has cells. Adapted from references 2 through 4. heparinase, which allow the extracellular matrix of the host tissues to be digested, with enhanced invasiveness of the pathogen being the consequence.5 Staphylococcal infections that occur from skin injuries (eg, an infected cut) or spontaneous events from the glandular elements of the skin (eg, folliculitis or impetigo) have traditionally been viewed as methicillin-sensitive organisms. In recent years, new strains of community-associated methicillin-resistant S. aureus (CA-MRSA) have developed. Infections with CA-MRSA are predominantly skin and soft tissue infections.6 The resistance of CA-MRSA to β-lactam antibiotics is carried by a gene cassette (mec-type IV) that does not mediate resistance to certain non–β-lactam drugs but does carry the gene for the Panton-Valentine leukocidin.7 This particular virulence factor is toxic to human leukocytes but also results in a tissue toxicity that gives an exaggerated local inflammatory response characterized by necrosis and eschar formation. S. pyogenes has virulence factors that relate both to cell structure and to exotoxin production.8 M-proteins on the cell wall surface of streptococci retard phagocytosis and are fundamental to the virulence of these bacteria. Streptococci without M-protein are without virulence.9 A variety of very potent exotoxins are produced, including gives the particularly pyogenic character to staphylococcal infections. S. aureus may also produce hemolysins and leukocidins. They in turn produce collagenase, hyaluronidase, and Activation Event Cut, scrape, burn Folliculitis Initiatior Events Coagulation activation Platelet degranulation Mast cell degranulation Bradykinin synthesis Complement activation Phagocytic Phase Vasodilation Increased permeability Edema formation Neutrophil infiltration Monocyte infiltration Phagocytosis Cytokine regulation te Vasoactive Phase d. Figure 1. the sequential events in the activation of human inflammation. An activator event occurs with skin injury or the development of infection within a glandular element of the skin. Tissue injury activates the Initiator events, which in turn lead to the vasoactive phase of inflammation. The phagocytic phase follows. 3 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 4 THE SCIENCE BEHIND PATIENT OUTCOMES Inoculum of bacteria + Virulence of bacteria Adjuvant effects + = A Intrinsic host defense ll + ri py ts Co gh Acquired host defense impairments Probability/ severity of infection ri re Figure 2. A hypothetical equation of the interaction of the complex entities that are involved in determining whether infection will occur after skin injury or will be controlled or aggressively advance. gh se t rv © 20 ed du cytic response. The efficiency and robustness of the response dictate whether contamination is eradicated before infection occurs, or whether the evolving infection can be contained and minimized. The vasoactive response of inflammation has numerous components. Relaxation of the vascular smooth muscle and modification of the vascular endothelial cell results in vasodilatation of the microcirculation, increased bulk flow, increased vascular permeability, and tissue edema in the local area of inflammatory activation.11 The increase in bulk flow increases the delivery of phagocytic cells (and also oxygen, opsonins, antibodies, etc) to the area, but reduces flow velocity and shear on the endothelial surface to facilitate subsequent leukocyte margination. Increased permeability provides routes for phagocytic cells to exit the microcirculation, and edema formation creates aqueous conduits to permit phagocytic migration through the extracellular ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R hemolysins and enzymes that digest the extracellular matrix. The array of exotoxins produced by the group A streptococcus can be so toxic that the infection has a potent necrotizing character. Multitoxin-producing S. pyogenes is the pathogen associated with the “flesh-eating” bacterial infections of soft tissues. These are better known as necrotizing soft tissue infections. External bacteria can be introduced into the host and be the pathogen(s) of skin and soft tissue infection. Most commonly, bacteria introduced from farming accidents or soft tissue infections after operations or traumatic injury of the human intestinal tract will be polymicrobial, with gramnegative rods and potentially enteric anaerobic bacteria.10 Much less frequently, one may see Clostridium perfringens associated with the introduction of spores into the tissues from puncture wounds, Pasteurella species with cat bites, or Vibrio species with cutaneous injuries sustained in salt water. Depending on the mechanism of injury, the immune status of the patient (or if there is underlying illness), and the external microbial environment, any bacterial species introduced into the wounded area that results in a critical inoculation of contaminants can cause skin and soft tissue infection. Table 2. Adjuvant Factors That Enhance the Virulence of Bacterial Contamination Within a Soft Tissue Wound Variable The Inflammatory Response Debris from injury or suture material placed into the wound can enhance infection; neutrophils ingest bacteria on nonbiologic surfaces very poorly. Necrotic tissue Dead tissue does not swell with edema; neutrophils cannot penetrate tissue without the benefit of edema. d. 4 Foreign bodies te Whether infection originates within a cutaneous wound or from within a glandular structure, activation of the inflammatory response within the skin and soft tissues is the first line of the innate host response. Disrupted tissue, the release of tissue factor, exposed collagen, and released ADP activate the initiator events of human inflammation. The initiator events include the activation of the coagulation cascade, aggregation and degranulation of platelets, activation of the mast cells, activation of the bradykinin pathway, and activation of the complement cascade (Figure 1).10 These redundant and interactive responses result in an immediate vasoactive response and a secondary phago- Pathophysiologic Effect Hemoglobin Iron is a critical trace metal for the growth of bacteria; hemoglobin in a wound is a rich source of iron and protein. Dead space Dead space in a large wound or after surgical repair accumulates serum; neutrophils cannot phagocytose bacteria in suspended media. 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 5 Supported and approved by Pfizer A matrix. The vigor of this tissue level response is regulated by the intensity of the inflammatory signaling (ie, chemoattractant molecules, tumor necrosis factor, interleukin-1, and other soluble messengers that enhance inflammation) that arises from the 5 initiators identified above. In addition to the vasoactive consequences of activation of the initiator events, cleavage products and secreted proteins serve as chemoattractants. Chemoattractants are molecules that bind to specific receptor sites on the surface of leukocytes and provide a chemical gradient and direction for phagocytic migration into the area of injury or infection. The phagocytic response occurs with the actual infiltration of the injured or infected tissue with neutrophils followed by monocytes. The activation of endothelial selectin and integrin receptors allows them to serve as adhesion molecules that initially cause slowing on the surface tissue, and then result in adherence of the phagocytic cell to the endothelial cell.12 Diapedesis is then directed by the chemoattractant gradient from the epicenter of injury or infection. Phagocytosis of bacteria is initiated and then amplified by the release of tumor necrosis factor–α, interleukin-1, and other pro-inflammatory cytokines.13 Successful mobilization of the innate response to a skin injury results in eradication of the would-be pathogens. An effective response is one in which the infection is limited to a localized cellulitis or soft tissue abscess. Invasion of tissue with spreading cellulitis, lymphangitis, and lymphadenitis represents the summed virulence of the pathogen in excess of the efficiency of the mobilized host response. Aggressive tissue destruction, progressive tissue necrosis, vertical extension of the infection to the fascial level, and bacteremia reflect either virulence beyond the control of the host or host defenses that are inadequate to meet the challenge of the pathogen. In the latter scenario, systemic dissemination of the microbe, dissemination of its toxins, or dissemination of pathophysiologic quantities of the proinflammatory signals results in the systemic inflammatory response syndrome (SIRS).14 ll ri py ts Co gh ri re gh se t rv © References du 1. Centers for Disease Control and Prevention. Soft tissue infections among injection drug users—San Francisco, California, 1996-2000. MMWR Morb Mortal Wkly Rep. 2001;50: 381-384. 2. De Pauw BE, Donnelly JP. Infections in the immunocompromised host: general principles. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Disease., 5th ed. New York, NY: Churchill Livingstone; 2000:3079-3090. 3. Kok M, Pechere J-C. Nature and pathogenicity of micro-organisms. In: Armstrong D, Cohen J, eds. Infectious Diseases. London, England: Mosby; 1999:1.1.1-1.1.26. 4. Harrington DJ. Bacterial collagenases and collagen-degrading enzymes and their potential role in human disease. Infect Immun. 1996;64:1885-1891. 5. Printzen G. Relevance, pathogenicity and virulence of microorganisms in implant related infections. Injury. 1996;27(suppl 3):SC9-SC15. 6. Said-Salim B, Mathema B, Kreiswirth BN. Community-acquired methicillin-resistant Staphylococcus aureus: an emerging pathogen. Infect Control Hosp Epidemiol. 2003;24:392-396. 7. Lina G, Piemont Y, Godail-Gamot F, et al. Involvement of PantonValentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999;29:1128-1132. 8. Stevens DL. The toxins of group A streptococcus, the flesh-eating bacteria. Immunol Invest. 1997;26:129-150. 9. Fischetti VA, Gotschlich EC, Siviglia G, Zabriskie JB. Streptococcal M protein: an antiphagocytic molecule assembled on the cell wall. J Infect Dis. 1977;136(suppl):S222-S233. ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R 20 ed efficiency of responsiveness. Clinical variables that are thought to impair the host include blood transfusion, hypoalbuminemia, corticosteroid therapy, hypoxemia, tissue ischemia, hypothermia, hyperglycemia, malnutrition, and coexistent diseases associated with immunosuppression (eg, renal failure). Whether the contaminant is eliminated before infection occurs, whether mild cellulitis or a small tissue abscess remains as a localized and relatively innocent event, or whether an aggressive and life-threatening infection is the consequence is determined by this complex interaction. Understanding this relationship between the pathogen and the host sets the stage for a pathophysiologic approach to treating the patient with infections such as a soft tissue infection. Determinants of Infection 11. Fry DE. Microcirculatory arrest theory of SIRS and MODS. In: Baue AE, Faist E, Fry DE, eds. Multiple Organ Failure: Pathophysiology, Prevention, and Therapy. New York, NY: Springer; 2000:92-100. 12. Brown EJ, Lindberg FP. Leukocyte adhesion molecules in host defense against infection. Ann Med. 1996;28:210-218. 13. Klebanoff SJ, Vedes MA, Harlan JM, et al. Stimulation of neutrophils by tumor necrosis factor. J Immunol. 1986;136:4220-4225. te 14. Fry DE. Multiple organ dysfunction syndrome: past, present and future. Surg Infect. 2000;1:155-163. d. Thus, either the development of infection after skin injury or enhanced severity of the infection, once it occurs, is the consequence of multiple complex events illustrated in the hypothetical equation form in Figure 2.15 The forces favoring infection are the inoculum of bacteria in the tissue, the virulence characteristics of the bacterial contaminant, and the local environment that enhances microbial aggressiveness (Table 2).15 The forces of pro-infection are then pitted against the intrinsic capacity of the host, which is then modulated by acquired clinical conditions that impair the 10. Solomkin JS, Mazuski JE, Baron EJ, et al. Guidelines for the selection of anti-infective agents for complicated intra-abdominal infections. Clin Infect Dis. 2003;37:997-1005. 15. Fry DE. Surgical site infection: pathogenesis and prevention. Medscape Surgery, February 2003. Available at: www.medscape.com/clinicalupdate/ssi. Accessed: June 16, 2006. 5 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 6 THE SCIENCE BEHIND PATIENT OUTCOMES A ll ri Section II: Pharmacoeconomic Considerations In the Treatment of Hospital-Associated Methicillin-Resistant Staphylococcus aureus py ts Co gh ri re gh se t rv © du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro Associate Professor John A. Burns School of Medicine University of Hawaii Honolulu, Hawaii M ep 09 .R 20 ed Alan D. Tice, MD Economic analyses of the evaluation and therapy of methicillin-resistant Staphylococcus aureus (MRSA) infections are difficult but increasingly important, as issues regarding resistance to antibacterial agents continue to emerge and outbreaks with new and more virulent strains continue. An understanding of the factors involved in the significant financial costs of MRSA must consider a variety of perspectives as well as the value of a careful clinical assessment of every person infected. There are a number of economic perspectives that should be considered and reconsidered when therapeutic decisions are made. When Is Antibiotic Therapy Warranted? The Cost of Treatment If antibiotic treatment is necessary, choosing a drug based on its cost is one way to reduce the overall financial burden of treatment. However, there are other important considerations involved in antimicrobial selection, including: • the underlying disease(s) • clinical efficacy of the drug • adverse effects of treatment (including likelihood of allergic reaction) • the likelihood of patient compliance with treatment • the status of available healthcare resources • patients’ health insurance coverage • patients’ ability to care for themselves • costs associated with I.V. administation (including home infusion costs) • availability of oral formulations • the cost of therapeutic failure. Indeed, the price of an effective oral therapy for MRSA may well be worthwhile when other potential costs are factored into the equation.6 In a study of patients with community-acquired pneumonia, Davis et al demonstrated that conversion from I.V. to oral therapy can reduce associated treatment costs, without compromising efficacy.7 Table 1 summarizes the potential costs associated with antibiotic therapy and offers potential cost-saving strategies. Certain options may initially be more expensive, but they may save money in the long run through reductions in hospital stays, for which costs start at $1,000 per day.8 Table 2 illustrates the additional mortality, hospital costs, etc, associated with MRSA in the surgical setting. Perspectives on “cost effectiveness” vary greatly with the observer. Some hospitals, for instance, may see te d. The recovery of S. aureus on a culture is not, in and of itself, an indication for antibiotic therapy. Reports of MRSA strike fear into many healthcare workers and nursing home managers. In fact, roughly one third of otherwise healthy individuals carry S. aureus (usually in and around their nasal area), with no apparent symptoms.1 Some of these bacteria are MRSA. On the other hand, many infections are not treated aggressively, causing severe disease and other complications that could have been avoided. The challenge facing clinicians is distinguishing those patients who are truly infected from those who are not (ie, those who need aggressive treatment from those who do not). Indeed, clinical acumen is becoming increasingly important, and it has significant financial implications when it comes to MRSA. While a quick and inexpensive assessment for MRSA 6 can be done with on-site Gram stain testing, this procedure is typically done in an outside laboratory; results may not be available in a timely manner. Waiting for results can lead to costly delays in treatment decisions.2 For example, delays in initiating adequate antibiotic therapy have been associated with greater mortality in ventilator-associated pneumonia.3 They can also increase patient anxiety. A rapid means of detecting S. aureus and determining whether or not it is MRSA would be extremely useful. New and more expensive techniques for rapid identification of S. aureus and even MRSA markers are in development, but they are not yet available for bedside use.4 These newer tests, while costly in and of themselves, may prove cost-effective in the long run, especially given the increasing number of hospitalizations for MRSA and the need for prolonged courses of therapy.5 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 7 Supported and approved by Pfizer Table 1. Antibiotic Cost Factors in Hospitalized Patients, With Potential Strategies for Cost-Efficiency Cost-saving Strategies Price of acquisition (cost per dose or per day) Purchase bulk through groups or consortia. A Obvious Cost ll ri Hidden Costs Co gh Cost of I.V. administration py ts Selectively use antibiotics with long half-lives that may be given q12h or q24h. Use I.V.-to-PO switch programs. Consider treating more infections with oral antibiotics in both outpatient and hospital settings. ri re gh se t rv Consider avoiding drugs that require serum drug level monitoring. © 09 .R 20 ed Cost of monitoring du ct Cost of adverse reactions Cost of therapeutic failure (ie, prolonged treatment or need for retreatment with different antibiotic) Adapted from references 4 through 7. Minimize or avoid use of antibiotics associated with emergence of resistant organisms. i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep Cost of increased antibiotic resistance and outbreaks due to resistant organisms (includes cost of infection control of isolating patients) MRSA infections as a great expense involving prolonged, complex, and expensive stays when nosocomial infections occur. For these institutions, the objective is to get patients out of the hospital as soon as possible. This can Consider avoiding poorly tolerated antibiotics. Consider avoiding antibiotics likely to fail because of improper spectrum. Consider avoiding antibiotics with poor tissue penetration. be accomplished with some oral antibiotics or outpatient parenteral antibiotic therapy (OPAT), if resources and local expertise are available. From a pharmacy perspective, however, the acquisition Table 2. Adjusted Clinical Outcomes and Hospital Charges For Patients With MRSA in the Surgical Setting Outcome Uninfected Control Subjects (n=193) MRSA SSI (n=121) Death, n (%) 4 (2.1) 25 (20.7) After surgery 5 (3-8) 23 (12-38) After infection NA 15 (7-30) Total duration of hospitalization, median days (IQR) te 29,455 (15,637-41,764) 92,363 (40,198-136,479) d. Hospital charges, median $ (IQR) IQR, interquartile range; MRSA, methicillin-resistant Staphylococcus aureus; SSI, skin and soft tissue infection Adapted from reference 4. 7 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 8 THE SCIENCE BEHIND PATIENT OUTCOMES References A ll ri cost of an antibiotic may be a critical factor in antibiotic selection. Many hospital pharmacies operate on a fixed budget, and staff performance may be measured based on the ability to control expenses. Despite the common and frequent use of antibiotic therapy for S. aureus infections, there may be a lack of information about the agents’ adverse effects. Older oral agents have not been approved by the US Food and Drug Administration for the treatment of infections due to MRSA, and there have been few comparative studies.9 Nevertheless, the older antimicrobials are often used as first-line therapy for suspected or documented MRSA. Clinicians must not only consider drug costs but overall treatment costs and, of course, patient outcomes when selecting therapy. py ts Mainous AG 3rd, Hueston WJ, Everett CJ, Diaz VA. Nasal carriage of Staphylococcus aureus and methicillin-resistant S. aureus in the United States, 2001-2002. Ann Fam Med. 2006;4:132-137. 2. Lode H. Management of serious nosocomial bacterial infections: do current therapeutic options meet the need? Clin Microbiol Infect. 2005;11:778-787. 3. Kollef MH, Ward S. The influence of mini-BAL cultures on patient outcomes: implications for the antibiotic management of ventilator-associated pneumonia. Chest. 1998;113:412-420. 4. Paule SM, Pasquariello AC, Thomson RB Jr, Kaul KL, Peterson LR. Real-time PCR can rapidly detect methicillin-susceptible and methicillin-resistant Staphylococcus aureus directly from positive blood culture bottles. Am J Clin Pathol. 2005;124:404-407. 5. Lodise TP, McKinnon PS. Clinical and economic impact of methicillin resistance in patients with Staphylococcus aureus bacteremia. Diagn Microbiol Infect Dis. 2005;52:113-122. 6. Tice AD, Hoaglund PA, Nolet B, McKinnon PS, Mozaffari E. Cost perspectives for outpatient intravenous antimicrobial therapy. Pharmacotherapy. 2002;22:63S-70S. Co gh ri re gh se t rv © du i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R 20 ed ct Cost-Effective Treatment Approaches Cost-effective antimicrobial therapy starts with an initial, thorough evaluation and the initiation of therapy with an antibiotic. Possible treatment approaches might also include wound debridement, incision and drainage, a culture, parenteral therapy, and hospitalization. A daily clinical evaluation as well as a review of the culture results can quickly provide useful answers about whether more expensive care is needed or a switch to an oral or less expensive antibiotic is possible.10 Daily outpatient assessments for clinical response, adverse effects, and related medical problems also may be quite cost-effective compared with hospitalization. Conclusion 7. Davis SL, Delgado G Jr, McKinnon PS. Pharmacoeconomic considerations associated with the use of intravenous-to-oral moxifloxacin for community-acquired pneumonia. Clin Infect Dis. 2005;41(suppl2):S136-S143. 8. Engemann JJ, Carmeli Y, Cosgrove SE, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36:592-598. 9. Khawcharoenporn T, Tice A. HMJ. In press. 10. Parodi S, Rhew DC, Goetz MB. Early switch and early discharge opportunities in intravenous vancomycin treatment of suspected methicillin-resistant staphylococcal species infections. J Manag Care Pharm. 2003;9:317-326. te d. The bottom line in the evaluation of antimicrobial agents should be the patient. However, economic issues are a major consideration in antibiotic selection and use. The factors involved are multiple, complex, interrelated, and changing. The best approach is to conduct a comprehensive evaluation when a patient presents with a possible infection; if warranted, initiate aggressive intervention at the start and moderate it as clinical and laboratory information accumulates. Given the increasing incidence of MRSA, more clinical input, laboratory cultures, economic studies, clinical research, and clinician teamwork are urgently needed. 8 1. 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 9 Supported and approved by Pfizer Section III:Toxin Inhibition And Gram-Positive Infection: A Focus on Methicillin-Resistant Staphylococcus aureus Expressing the Panton-Valentine Leukocidin Gene ll ri Co gh py ts Marin H. Kollef, MD ri re Professor of Medicine Washington University School of Medicine Director, Medical Critical Care Director, Respiratory Care Services Barnes-Jewish Hospital St. Louis, Missouri Introduction gh se t rv © du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R 20 ed Over the past 20 years, methicillin-resistant Staphylococcus aureus (MRSA) has been isolated with increased frequency in hospitalized patients as well as in the community. MRSA infections have been associated with greater morbidity, mortality, and hospital costs than their methicillin-sensitive S. aureus (MSSA) counterparts. Until recently, treatment options for serious infections caused by MRSA have been limited to a few agents, most notably vancomycin. However, with the introduction of new antimicrobial agents, it has become possible to develop new treatment strategies for MRSA, including toxinproducing strains of MRSA that have been identified. Cell Wall Chromosome SCCmec Cell Membrane PVL Wall teichoic acid Surface protein adhesins Octameric pore IL- 8 LTB4 Ca2+ channel opening Mitochondrial injury Necrosis Apoptosis Neutrophil te Figure. CA-MRSA interacts with a neutrophil. d. Illustration of CA-MRSA interaction with a neutrophil resulting in cell death by either necrosis or apoptosis. Surface proteins and wall teichoic acid expression facilitate bacterial adherence to cell surfaces. Release of PVL facilitates octameric pore formation within the membranes of neutrophils. Low concentrations of PVL result in fewer octameric pores forming which allow further entry of PVL into the cytoplasm resulting in mitcochondial injury and apoptosis. Greater concentrations of PVL lead to more octameric pores forming with Ca2+ channel opening and necrosis. Additionally, formation of the octameric pores by PVL induces release of neutrophil chemotactic factors including IL-8 and leukotriene B4. Ca2+, calcium; CA-MRSA, community-associated methicillin-resistant Staphylococcus aureus; IL-8, Interleukin-8; LTB4, leukotriene B4; PVL, Panton-Valentine leukocidin; SCC, staphylococcal chromosomal cassette 9 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 10 THE SCIENCE BEHIND PATIENT OUTCOMES Table. Comparison of HA-MRSA and CA-MRSA CA-MRSA Setting Hospital, nursing home, dialysis clinic Community, entering hospitals Ethnic predominance White Non-white (African-American, Asian, Hispanic) Yes (hospital, nursing home) Yes (family, day care, military barracks, locker room, prison) Diabetes, head trauma, renal failure None None Skin and soft tissue Uncommon Common in skin and lung Uncommon Common with pneumonia Absent Can occur ll HA-MRSA ts A Characteristic ri Co gh py Horizontal transmission ri re gh se t rv Predisposing underlying illnesses © ed Preceding influenza illness Panton-Valentine leukocidin Susceptible to non– β-lactam antibiotics ct mecA gene du Waterhouse-Friderichsen syndrome i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R Tissue necrosis 20 Predominant site of infection Present Present Historically not found Usually present Usually not Often yes CA-MRSA, community-associated methicillin-resistant Staphylococcus aureus; HA-MRSA, healthcare-associated methicillin-resistant Staphylococcus aureus Adapted from reference 5. Epidemiology S. aureus strains can express many potential virulence factors, including surface proteins that promote colonization of host tissues, exotoxins and superantigens that cause tissue damage and the symptoms of septic shock, and invasins that promote bacterial spread in tissues (eg, leukocidin, kinases, hyaluronidase).6 Panton-Valentine leukocidin (PVL) is a cytotoxin produced by fewer than 5% of S. aureus strains, and it has been associated with primary skin infections and severe necrotizing pneumonia. In a study in which investigators screened 172 strains of S. aureus, PVL genes were detected in 93% of strains associated with furunculosis and in 85% d. 10 Virulence te Gram-positive cocci, in particular S. aureus, account for 20% to 30% of all cases of hospital-acquired pneumonia (HAP).1 Nosocomial strains of MRSA are found worldwide,2 and data from the US National Nosocomial Infections Surveillance System show that MRSA now accounts for more than 55% of S. aureus–related infections in the intensive care setting.3 Traditionally, MRSA has been considered a healthcareassociated organism if it is isolated from a patient at least 72 hours after admission in a healthcare facility (acutecare hospital or long-term care facility) and communityacquired if isolated from a patient at the time of admission or within 48 to 72 hours of hospital admission. However, without the use of sophisticated laboratory techniques, it is often difficult to know if the MRSA was actually acquired in the community or from previous contact with the healthcare system; therefore, some prefer to categorize different types of MRSA as “healthcare-associated” (HAMRSA), “community-associated (CA-MRSA) with risk factors for healthcare acquisition,” or “community-associated without risk factors for healthcare acquisition.”4 In comparing CA-MRSA with HA-MRSA, Naimi et al found that among MRSA infections, 12% were classified as CA-MRSA; CA-MRSA patients were younger than HAMRSA patients (average age, 23 years vs 68 years; P<0.001); more CA-MRSA patients than HA-MRSA patients were non-white (32% vs 11%; P<0.001); and CA-MRSA patients generally had a lower median income level than HA-MRSA patients ($25,395 vs $28,290; P=0.02) (Table).5 632SRBtoBCompPRNT 2/9/07 2:18 PM Page 11 Supported and approved by Pfizer A of strains associated with severe necrotic hemorrhagic pneumonia, both of which were community-acquired. PVL genes were not detected in strains associated with other types of infections, such as HAP, toxic shock syndrome, infective endocarditis, or mediastinitis.7,8 Conclusion ll The optimal management strategy for toxin-producing strains of S. aureus is still unknown. Pending further clinical investigations, clinicians should consider the use of antibiotics that can inhibit specific toxin production in patients with serious infection. ri ts Co gh Toxin Production py PVL is a synergohymenotropic toxin assembled from 2 component proteins.9 PVL creates lytic pores in the cell membranes of neutrophils and induces release of neutrophil chemotactic factors including interleukin-8 and leukotriene B4 (Figure).10 In a study of 422 patients with acute, purulent skin and soft tissue infections in 11 university-affiliated emergency departments, S. aureus was isolated in 320 patients (76%).11 Overall, the prevalence of MRSA was 59% on average, with a high of 74% at one participating institution. Staphylococcal chromosomal cassette mec (SCCmec) type IV and the PVL toxin gene were detected in 98% of all MRSA isolates. Antibiotic susceptibility among all strains isolated varied significantly. However, the study found that antibiotic therapy was not concordant with the results of susceptibility testing in 57% patients with MRSA infection who received antibiotics. As a result, the authors recommended that when antimicrobial therapy is indicated for the treatment of complicated skin and soft tissue infections, clinicians should consider obtaining cultures and modifying empiric therapy to provide MRSA coverage. In addition, Katayama et al noted that MRSA strains produce a cell wall penicillin-binding protein with a low affinity for β-lactam antibiotics.12 The authors added that a notable difference between MRSA and MSSA is that a higher percentage of MRSA strains possess toxins such as PVL. Indeed, when selecting antimicrobial therapy, minimum inhibitory concentrations (MICs) and coverage of the infection and the host are typically considered.11 Based on findings such as these, however, clinicians may also want to consider the issue of toxin penetration during the selection process. In addition to antibiotic therapy, alternative treatments may become available for toxin-producing strains of S. aureus. Polyclonal immunoglobulin has been proposed as a therapy for patients with serious CA-MRSA infections.13,14 Potential mechanisms of action include neutralization of circulating cytokines and downregulation of their expression. References ri re gh se t rv Lynch JP. Hospital-acquired pneumonia: risk factors, microbiology, and treatment. Chest. 2001;119:373S-384S. 2. Diekema DJ, Pfaller MA, Schmitz FJ, et al. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis. 2001;32:S114-S132. 3. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2003, issued August 2003. Am J Infect Control. 2003;31:481-498. © du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R 20 ed 1. 4. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillinresistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003;36:131-139. 5. Naimi TS, LeDell KH, Como-Sabetti K, et al. Comparison of community- and healthcare-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003;290:2976-2984. 6. Baba T, Takeuchi F, Kuroda M, et al. Genome and virulence determinants of high virulence community-acquired MRSA. Lancet. 2002;359:1819-1827. 7. Foster TJ. The Staphylococcus aureus “superbug.” J Clin Invest. 2004;114:1693-1696. 8. Lina G, Piemont Y, Godail-Gamot F, et al. Involvement of PantonValentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999;29:1128-1132. 9. Boussaud V, Parrot A, Mayaud C, et al. Life-threatening hemoptysis in adults with community-acquired pneumonia due to PantonValentine leukocidin-secreting Staphylococcus aureus. Intensive Care Med. 2003;29:1840-1843. 10. Konig B, Prevost G, Piemon Y, Konig W. Effects of Staphylococcus aureus leukocidins on inflammatory mediator release from human granulocytes. J Infect Dis. 1995;171:607-613. 11. Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666-674. 12. Katayama Y, Zhang HZ, Chambers HF. PBP 2a mutations producing very-high-level resistance to beta-lactams. Antimicrob Agents Chemother. 2004;48:453-459. te 13. Genestier A-L, Michallet M-C, Prevost G, et al. Staphylococcus aureus Panton-Valentine leukocidin directly targets mitochondria and induces Bax-independent apoptosis of human neutrophils. J Clin Invest. 2005;115:3117-3127. d. 14. Hampson FG, Hancock SW, Primhak RA. Disseminated sepsis due to a Panton-Valentine leukocidin producing strain of community acquired methicillin resistant Staphylococcus aureus and use of intravenous immunoglobulin therapy. Arch Dis Child. 2006;91:201. 11 Page 12 2:18 PM 2/9/07 632SRBtoBCompPRNT A ll ri py ts Co gh ri se gh re t du ct i ib d. t e ro h no s p e i is n rw sio is he ot rm ss pe le ut un ho up wit ro G art ng n p i hi r is bl e o Pu ol h on w ah in cM on i ro M ep 09 .R 20 ed © rv Methicillin-Resistant Staphylococcus aureus te d. SR06023/ZV274595
© Copyright 2025