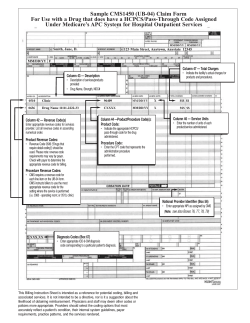
April - OptumCoding
Chargemaster Corner
Joe Martinez, CPC
Joe.martinez@optum360.com
April 2015 Quarterly Edition
We have completed the first quarter for 2015.
Chargemaster have been updated and everything
seems to be running smoothly. We now have new
changes to contend with in the second quarter of
2015. This edition of Chargemaster Corner explores
a few of the new changes and impact on the
Chargemaster process.
The following information was derived from
Transmittal 3217 and is intended for providers and
suppliers who submit claims to Medicare
Administrative Contractors (MACs), including Home
Health & Hospice (HH&H) MACs for services
provided to Medicare beneficiaries and are changes
to Current Procedural Terminology (CPT) and
Healthcare Common Procedure Coding System
(HCPCS) codes relating to the hospital Chargemaster
for the Quarter starting April 1, 2015.
New Service Effective April 1, 2015
C2623, Cath, translumin, drug-coat Catheter,
transluminal angioplasty, drug-coated, non-laser.
CMS has determined that a portion of the APC
payment amount associated with the cost of C2623 is
reflected in procedures assigned to various peripheral
transluminal balloon angioplasty codes in APC 0083,
APC 0229, and APC 0319. The C2623 device may be
billed with various peripheral transluminal balloon
angioplasty codes that are assigned to these three
APCs for CY 2015
We have received questions as to whether the code
should be reported, since it is packaged and no
separate reimbursement is received.
CMS indicates packaging encourages hospitals to
negotiate carefully with manufacturers and suppliers
to reduce the purchase price of items and services
or to explore alternative group purchasing
arrangements, thereby encouraging the most
economical health care.
“We encourage hospitals to report all HCPCS codes
that describe packaged services that were provided,
unless CPT or CMS provide other guidance. If a
HCPCS code is not reported when a packaged
service is provided, it can be challenging to track
utilization patterns and resource costs”
Reference: 2009 Proposed Rule page 155
Drugs and Biologicals with Payments Based on
Average Sales Price plus 6 Percent
In CY 2015, a single payment of ASP+6 percent for
pass-through
drugs,
biologicals
and
radiopharmaceuticals is made to provide payment
for both the acquisition cost and pharmacy overhead
costs of these pass-through items.
Payments for drugs and biologicals based on ASPs
will be updated on a quarterly basis as later quarter
ASP submissions become available.
Updated payment rates effective April 1, 2015 and
drug price restatements can be found in the April
2015 update of the OPPS Addendum A and
Addendum B on the CMS Web site at
http://www.cms.gov/HospitalOutpatientPPS/
Inpatient Only Services Update
CMS is revising their billing instructions to allow
payment for inpatient only procedures that are
provided to a patient in the outpatient setting on the
date of the inpatient admission or during the 3
calendar days (or 1 calendar day for a nonsubsection (d) hospital) preceding the date of the
inpatient admission that would otherwise be deemed
related to the admission to be bundled into billing of
Proprietary & Confidential
Page 1 of 3
Chargemaster Corner
Joe Martinez, CPC
Joe.martinez@optum360.com
the inpatient admission, according to our policy for
the payment window for outpatient services treated
as inpatient services.
Effective April 1, 2015, inpatient only procedures that
are provided to a patient in the outpatient setting on
the date of the inpatient admission or during the 3
calendar days (or 1 calendar day for a nonsubsection (d) hospital) preceding the date of the
inpatient admission that would otherwise be deemed
related to the admission, according to our policy for
the payment window for outpatient services treated
as inpatient services will be covered by CMS and are
eligible to be bundled into the billing of the inpatient
admission.
CMS is updating Pub. 100-04, Medicare Claims
Processing Manual, chapter 4, sections 10.12 and
180.7 to reflect the revised impatient only payment
policy.
Reporting of the “PO” Modifier
As stated in the CY 2015 OPPS Final Rule, we
finalized our instructions related to the reporting of the
“PO” modifier (the short descriptor ‘‘Serv/proc offcampus pbd,’’ and the long descriptor ‘‘Services,
procedures and/or surgeries furnished at off-campus
provider-based outpatient departments.’’).
Reporting the Modifier -59
Please note that providers may continue to use the 59 modifier after January 1, 2015, in any instance in
which it was correctly used prior to January 1, 2015.
The initial CR establishing the modifiers was
designed to inform system developers that
healthcare systems would need to accommodate
the new modifiers.
Additional guidance and education as to the
appropriate use of the new –X {EPSU} modifiers will
be forthcoming as CMS continues to introduce the
modifiers in a gradual and controlled fashion.
That guidance will include additional descriptive
information about the new modifiers. CMS will
identify situations in which a specific –X {EPSU}
modifier will be required and will publish specific
guidance before implementing edits or audits.
CR 8863 states that providers who wish to use the
new modifiers may use them in accordance with
their published definitions and the X modifiers will
function within CMS systems in the same manner as
the 59 modifier.
The “PO” HCPCS modifiers to be reported with every
code for outpatient hospital services furnished in an
off-campus PBD of a hospital. Reporting of this new
modifier will be voluntary for 1 year (CY 2015), with
reporting required beginning on January 1, 2016.
The modifier should not be reported for remote
locations of a hospital, Satellite facilities of a hospital,
or for services furnished in an emergency
department.
CMS is updating Pub. 100-04, Medicare Claims
Processing Manual, Chapter 4, sections 20.6.11 to
include the use of the “PO” HCPCS modifier.
Proprietary & Confidential
Page 2 of 3
Chargemaster Corner
Joe Martinez, CPC
Joe.martinez@optum360.com
We hope you enjoy receiving the Chargemaster
Corner from Optum360. Each quarter Optum360
will circulate this newsletter via e-mail to those
interested parties who have provided contact
information either via e-mail request or who have
completed an informational form when attending a
number of educational seminars conducted
nationwide. Contact information will not be shared
with any other organization and used only for
means of distributing this monthly newsletter.
Also please remember Optum360 can assist you
in the preparation of ICD-10-CM/ICD-10-PCS.
Whether doing a gap analysis, assessing financial
risk, chart audits or coder and physician
education, Optum360 is prepared to meet your
needs.
For direct contact concerning receipt of this
newsletter, please e-mail your comments to the
above noted e-mail address. Thank you for your
interest in this monthly Chargemaster newsletter
and hope you find it helpful.
Optum360 Consulting offers a variety of services
to assist hospitals in the inpatient and outpatient
coding and Chargemaster functions including:
1.
● Comprehensive Chargemaster review;
2.● Chargemaster maintenance Support;
3.● CPT® Coding Audits;
4.● Chart-to-claim audit;
● MS-DRG audits;
● Physician Coding audits,
● ICD-10-CM/PCS Preparation and Education,
● HIM/Revenue Cycle Operations, and
● Denials Management
If you wish to receive information about any of the
consulting services Optum360 offers, please
forward
your
inquiry
to
Joe.Martinez@Optum360.com.
Optum360
–
bringing your insight and expertise to your
Chargemaster reporting challenges.
Proprietary & Confidential
Page 3 of 3
© Copyright 2025