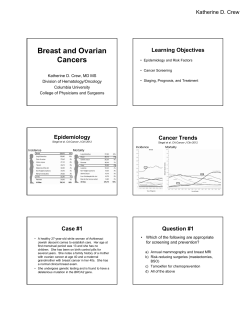
START Patient hdbk cover 2B1009.indd 1 TM
TM START Patient hdbk cover 2B1009.indd 1 6/30/09 3:54:38 PM Dear Patients, Family Members and Friends, Welcome to The START Center for Cancer Care where you will find health care teams dedicated to providing you with the highest quality of care. At START our concept is one of comprehensive patient care. We offer expertise and experience in the following areas: Medical Oncology, Radiation Oncology, Research, Hematology, Gynecologic Oncology and Integrative Oncology Services. In keeping with our commitment to treat the whole person we have dedicated 4,100 square feet to the Spa and Wellness Center which will deliver our Integrative Oncology Services. The Spa and Wellness Center, which opens the end of 2009, will offer acupuncture, massage, nutrition classes, guided imagery, counseling and other spa and wellness treatments. Our philosophy is to treat cancer patients with an inclusive, personalized coordination of care. This comprehensive approach may include any of the services mentioned above. In START’s Phase I clinic, while the same concept exists, our research physicians and their highly trained staff have also accomplished tremendous advances that have lead to an improved understanding and treatment of cancer. Their mission is to accelerate the development of new anti-cancer drugs with the purpose of improving quality of life and survival for patients with cancer. Through this program we are bringing you access to cutting edge therapy. We are committed to providing the highest quality of medical care in a personal and caring environment. You are the fundamental ingredient of your health care team and our goal is to work with you to treat your disease while making you feel informed, reassured and regarded with compassion. Soon after your initial registration you will be met by one of our Patient Advocates who will assist you, alleviate some of your concerns and help to reduce the stress of your experience. We hope you will call upon any member of your healthcare team with any questions or concerns because our promise is to provide you with the assistance, quality of care and kindness that you deserve. If you have questions or suggestions, which we welcome, please call our Patient Advocate department at 210-593-2652 or send an email to patient.advocacy@stoh.com. Sincerely, Your START Physicians 1 Queridos Pacientes, Familia y Amigos, Bienvenidos a The START Center for Cancer Care (El Centro START Para El Cuidado del Cáncer – mejor conocido como “START”) en donde encontrarán un equipo médico dedicado a proveerles el mejor cuidado posible. En START tenemos el concepto del cuidado total del paciente. Ofrecemos experiencia médica en las siguientes áreas: Oncología y Radiación Oncológica, Investigación, Hematología, Ginecología-Oncológica y otros servicios complementarios. De acuerdo con nuestro compromiso de tratar a la persona completa, hemos dedicado 4,100 pies cuadrados al Spa and Wellness Center (Spa y Centro de Bienestar), el cual abrirá sus puertas a finales del 2009, y ofrecerá acupuntura, masajes, clases de nutrición, imaginación guiada, consejería y otros tratamientos de spa y bienestar. Nuestra filosofía es tratar pacientes con cáncer con un cuidado coordinado que es inclusivo y personalizado. Este enfoque comprensivo podría incluir cualquiera de los servicios mencionados antes. En la Clínica Fase I de START, aunque existe el mismo concepto, nuestro equipo de investigación junto con su personal altamente entrenado también han logrado un tremendo avance en cuanto al entendimiento y tratamiento del cáncer. La misión en este centro es acelerar el desarrollo de nuevos medicamentos contra el cáncer con el propósito de mejorar la calidad de vida y supervivencia de los pacientes con esta enfermedad. A través de este programa estamos brindandoles acceso a una terapia de vanguardia. Nos comprometemos a proveer la mas alta calidad de cuidado médico dentro de un ambiente personal y humanitario. Ustedes son el ingrediente fundamental de nuestro equipo médico y nuestra meta es poder trabajar con ustedes para tratar su enfermedad y al mismo tiempo mantenerlos informados, hacerlos sentir tranquilos y siempre tratarlos con compasión. Luego de la inscripción inicial, uno de nuestros intercesores lo asistirá para aminorar sus preocupaciones y lo ayudara a reducir el estrés de esta experiencia. Esperamos que contacte a cualquier miembro de su equipo de cuidado médico con cualquier pregunta o inquietud, ya que nuestra promesa es proveerle la asistencia, cuidado y amabilidad que usted se merece. Actualmente estamos diseñando una guía para nuevos pacientes y esperamos poder ponerla a su disposición a la brevedad posible. Mientras tanto, si usted tiene alguna pregunta o sugerencias, por favor comuníquese a nuestro Departamento de Intercesores al (210) 593-2652 o a nuestro correo electrónico patient.advocacy@stoh.com. Atentamente Su Equipo Médico de START 3 GENERAL INFORMATION / REGISTRATION GENERAL INFORMATION/ REGISTRATION EMERGENCIES & PHONE CALLS If you are experiencing a true, life-threatening emergency, call 911. Call our office only after you have made arrangements to get to the Emergency Room. Our nurses return calls during business hours as time permits. If the matter is urgent, please tell our phone operator so that the nurse can confer with you in the timeliest manner possible. Please understand that calls for test results and prescription refills will be returned after urgent patient needs are met. We ask that you remember that physicians’ schedules are long and demanding. It may be late in the afternoon after all patients are seen, or sometimes the following day before non-emergency phone calls are returned. If you feel you need us, we want to hear from you. Please use this guide as to when you should make your phone call: Call anytime (210) 593-5700 – day or night – if: • • • • • • • • • • • Fever 100.5 F. degrees or greater. Uncontrollable nausea or diarrhea. Pain medication is not working. Chest pains or shortness of breath. Severe shaking or chills. Bleeding from the nose or gums. Blood in the urine. Black, tarry bowel movement. Constipation with intense abdominal cramping. Changes in your vision or hearing. Increased bruising or pinpoint red or purple spots anywhere on the body. Call During Regular Office Hours (8:00 a.m. - 4:30 p.m. Monday-Friday): • • • • • • • If you have questions about your medication, treatment or side effects. If you’re having nutrition problems. If you need a prescription refilled. Please call by 3 p.m. and have your pharmacy’s phone number. For narcotics such as Percocet, MS Contin or Oxycontin, plan to either come into the office for a written prescription or allow 5 days for the written prescription to be mailed. By law, your pharmacy must have a written prescription. No narcotic prescriptions can be written on weekends. If you’ve heard about a new treatment. If you notice new numbness or tingling of fingers or toes. For lab tests or scans, please know that results usually take: • • • • Scans: 48-72 hours Tumor markers: 72 hours Bone marrow: 7-10 days Pathology Reports: 3-5 days Never hesitate to call us for any problem that is important to you. There is no need to be miserable. If a certain medication is not working, call and let us know. Chances are, we can prescribe or suggest something to make you more comfortable. 5 LOCATIONS 1. The START Center 210-593-5700 4383 Medical Drive San Antoino, TX 78229 4. North Central Radiation Center 6. Boerne 210-593-5800 134 Menger Springs Rd, Ste 1120 Boerne, TX 78006 The Atrium at NC Baptist 502 Madison Oak, Ste 120 & 160 San Antoino, TX 78258 2. Downtown 210-593-5900 7. Bandera 210-593-5200 5. Northeast Santa Rosa Pavilion 315 N San Saba, Ste 1160 San Antoino, TX 78207 210-593-5600 Northease Baptist MOB 8715 Village Drive, Ste 116 San Antoino, TX 78217 3. Sonterra 210-593-5700 1300 Cedar Street Bandera, TX 78003 8. Westover Hills 210-593-2503 210-593-5700 155 E Sonterra, Ste 200 San Antoino, TX 78258 11212 Hwy 151, Ste 290 San Antoino, TX 78251 PARKING AT THE START CENTER For the convenience of the patients we have a parking garage located behind The Start Center for Cancer Care location at 4383 Medical Drive. The parking rates are: 00 – 30 minutes: 31 – 60 minutes; 61 – 90 minutes 91 – 120 minutes 121 – 150 minutes 151 – 180 minutes 181+ minutes Free $1.00 $2.00 $3.00 $4.00 $5.00 $6.00 We also have a $6.00 day pass for patients or family members who must come and go throughout the day. 6 PRIVACY POLICY Each time you visit our office, a record of your visit is made. Typically, this record contains your symptoms, examination and test results, diagnosis, treatment, and a plan for future care or treatment. This information, often referred to as your medical record, serves as a: • • • • • • • • • basis for planning your care and treatment means of communication among the many health professionals who contribute to your care legal document describing the care you received means by which you or a third-party payer can verify that services billed were actually provided a tool in educating health professionals a source of data for medical research a source of information for public health officials charged with improving the health of the nation a source of data for facility planning and marketing a tool with which we can assess and continually work to improve the care we render and the outcomes we achieve Understanding what is in your record and how your health information is used helps you to: • • • ensure its accuracy better understand who, what, when, where, and why others may access your health information make more informed decisions when authorizing the disclosure of your health information to others Your Health Information Rights Although your health record compiled by The START Center for Cancer Care is our physical property, the information belongs to you. And under state and federal laws, you have certain rights regarding that information. Specifically, you have the right to: • Request restrictions on certain uses and disclosures of your health information. Your request for restriction(s) must be submitted in writing to START Health Information Services. (45 CFR 164.522) Review of the restriction request will be completed within 30 days and will conclude with a written determination to you. START is not required to agree to the requested restriction(s). • Obtain a paper copy of the Notice of Information Practices upon request. • Inspect and/or obtain a copy of your medical record. (45 CFR 164.524) Requests to inspect or for copies of your health record must be submitted in writing to the Health Services Department and must contain the following information: ° The signature of the patient or the patient’s legally authorized representative, along with the date it was signed ° The identity of the information to be disclosed ° The dates of service to be disclosed ° The reason or purpose for the disclosure ° The identity of the person or entity to whom the information is to be disclosed An appointment to inspect your records or to pick up your copies will be made. Records will be inspected during START normal business hours. State law allows START 30 days to 7 P R I VA C Y P O L I C Y, c o n t i n u e d • • • • provide you with copies of your record, and allows START to charge you for those copies. You will be provided with an estimate of any charges before we make any copies for you. Request information in your health record be amended or changed. (45 CFR 164.528) Requests for changes or amendments to be made to your health information must be submitted in writing to the Health Information Management Department. Review of the change or amendment request will be completed within 30 days and will conclude with a written determination to you. START is not required to agree to the requested change or amendment. Obtain an accounting of disclosures of your health information for purposes other than Treatment, Payment, or Operations. (45 CFR 164.528) Requests for accounting disclosures of your health information must be submitted in writing to the Health Information Management Department. Request communication of your health information by alternative means or at alternative locations. (45 CFR 164.522) Revoke your authorization to use or disclose health information except to the extent that action has already been taken. The START Center for Cancer Care Information Responsibilities • START is required by law to: ° maintain the privacy of your health information ° provide you with a notice as to our legal duties and privacy practices with respect to information we collect and maintain about you abide by the terms of this notice ° notify you if we are unable to agree to a requested restriction ° accommodate reasonable request you may have to communicate health information by ° alternative means or at alternative locations 8 FINANCIAL & INSURANCE ISSUES The START Center for Cancer Care Billing Department is located at 4383 Medical Drive, on the fourth floor. The business office is open from 8:00 - 5:00 p.m. or by appointment and can be reached by calling 593-5711. To offer you the highest level of service the business office has assigned specific insurance companies to specific reimbursement specialists; thus maximizing the knowledge and understanding required to navigate the insurance industry. We believe that your active involvement with your Insurance Carrier is the key to ensuring you receive all benefits afforded to you under your policy. Please call the business office (210-593-5711) today to discuss your insurance benefits. Financial and Insurance Issues Financial and insurance issues can be stressful and confusing for you and your caregivers. It is important to create an organized system for managing this aspect of cancer care. By educating yourself about insurance benefits and keeping organized financial records, you may prevent financial dilemmas, thereby preventing unnecessary stress. Here are some general tips on insurance, a glossary of common insurance terms and information about medical costs and tax returns. Consider using a binder as your filing system to organize your healthcare records and financial information. Keep a record of all phone conversations with your insurance provider. In addition, some patients find it helpful to designate a caregiver or family member to keep track of all insurance/financial information. Insurance Tips Medical insurance and bill management can be one of the most frustrating aspects of cancer care for you and your caregivers. Importantly, most hospitals and clinics will provide a patient services representative to assist you. You should identify these individuals and seek help from them whenever necessary. Get the maximum benefit from your insurance policy! • • • • Get a copy of your policy and find out exactly what your coverage includes. Your employer or insurance company can help you with this. Call your health insurance provider to clarify any questions that you may have. Also, make sure you are aware of any possible coverage issues before you start treatment. Talk to your healthcare team to request that insurance coverage of any procedure, test or treatment be verified prior to you receiving them. If you healthcare team is unable to provide this service, they should be able to identify an alternative resource to assist you. Keep careful records of all your covered expenses, claims, denials and appeals throughout the claims process. Do not throw any correspondence away. Copyright©2008 CancerConsultants.com. All Rights Reserved. 9 FINANCIAL & INSURANCE ISSUES, continued • • Take notes during your conversations with insurance representatives. Include their names and job titles. Keep these notes with your records. If you think the representative is wrong, ask to speak with his or her supervisor. If you have a claim that has been denied, talk to your health insurance provider to find out what steps you can take to appeal. Understanding Insurance Terms accreditation - An evaluative process in which a healthcare organization undergoes an examination of its operating procedures to determine whether the procedures meet designated criteria as defined by the accrediting body, and to ensure that the organization meets a specified level of quality. ancillary services - Auxiliary or supplemental services, such as diagnostic services, home health services, physical therapy, and occupational therapy, used to support diagnosis and treatment of a patient’s condition. annual maximum benefit amount - The maximum dollar amount set by an MCO that limits the total amount the plan must pay for all healthcare services provided to a subscriber in a year. appropriateness review - An analysis of healthcare services with the goal of reviewing the extent to which necessary care was provided and unnecessary care was avoided. case management - A process of identifying plan members with special healthcare needs, developing a health-care strategy that meets those needs, and coordinating and monitoring the care, with the ultimate goal of achieving the optimum healthcare outcome in an efficient and cost-effective manner. Also known as large case management (LCM). claim - An itemized statement of healthcare services and their costs provided by a hospital, physician’s office, or other provider facility. Claims are submitted to the insurer or managed care plan by either the plan member or the provider for payment of the costs incurred. claim form - An application for payment of benefits under a health plan. claimant - The person or entity submitting a claim. claims administration - The process of receiving, reviewing, adjudicating, and processing claims. clinical practice guideline - A utilization and quality management mechanism designed to aid providers in making decisions about the most appropriate course of treatment for a specific clinical case. coinsurance - A method of cost-sharing in a health insurance policy that requires a group member to pay a stated percentage of all remaining eligible medical expenses after the deductible amount has been paid. Consolidated Omnibus Budget Reconciliation Act (COBRA) - A federal act which requires each group health plan to allow employees and certain dependents to continue their group coverage for a stated period of time following a qualifying event that causes the loss of group health coverage. Qualifying events include reduced work hours, death or divorce of a covered employee, and termination of employment. copayment - A specified dollar amount that a member must pay out-of-pocket for a specified service at the time the service is rendered. credentialing - The process of obtaining, reviewing, and verifying a provider’s credentials—the documentation related to licenses, certifications, training, and other qualifications—for the purpose of determining whether the provider meets the MCO’s preestablished criteria for participation in the network. deductible - A flat amount a group member must pay before the insurer will make any benefit payments. diagnostic and treatment codes - Special codes that consist of a brief, specific description of each diagnosis or treatment and a number used to identify each diagnosis and treatment. Copyright©2008 CancerConsultants.com. All Rights Reserved. 10 FINANCIAL & INSURANCE ISSUES, continued disease management (DM) - A coordinated system of preventive, diagnostic, and therapeutic measures intended to provide cost-effective, quality healthcare for a patient population who have or are at risk for a specific chronic illness or medical condition. Also known as disease state management. Employee Retirement Income Security Act (ERISA) - A broad-reaching law that establishes the rights of pension plan participants, standards for the investment of pension plan assets, and requirements for the disclosure of plan provisions and funding. fee-for-service (FFS) payment system - A system in which the insurer will either reimburse the group member or pay the provider directly for each covered medical expense after the expense has been incurred. fee schedule -The fee determined by an MCO to be acceptable for a procedure or service, which the physician agrees to accept as payment in full. Also known as a fee allowance, fee maximum, or capped fee. formulary - A listing of drugs, classified by therapeutic category or disease class, that are considered preferred therapy for a given managed population and that are to be used by an MCO’s providers in prescribing medications. generic substitution -The dispensing of a drug that is the generic equivalent of a drug listed on a pharmacy benefit management plan’s formulary. In most cases, generic substitution can be performed without physician approval. Health Insurance Portability and Accountability Act (HIPAA) - A federal act that protects people who change jobs, are self-employed, or who have pre-existing medical conditions. HIPAA standardizes an approach to the continuation of healthcare benefits for individuals and members of small group health plans and establishes parity between the benefits extended to these individuals and those benefits offered to employees in large group plans. The act also contains provisions designed to ensure that prospective or current enrollees in a group health plan are not discriminated against based on health status. Health Maintenance Organization (HMO) - A healthcare system that assumes or shares both the financial risks and the delivery risks associated with providing comprehensive medical services to a voluntarily enrolled population in a particular geographic area, usually in return for a fixed, prepaid fee. Indemnity Insurance - Traditional indemnity insurance is sometimes referred to as “fee for service.” This type of insurance plan allows patients to go to any doctor or hospital that they select, anywhere in the United States or abroad. Although insurance plans will vary, patients will generally be responsible for a deductible and copayments. lifetime maximum benefit amount - The maximum dollar amount set by an MCO that limits the total amount the plan must pay for all healthcare services provided to a subscriber in the sub-scriber’s lifetime. managed care - The integration of both the financing and delivery of healthcare within a system that seeks to manage the accessibility, cost, and quality of that care. managed care organization (MCO) - Any entity that utilizes certain concepts or techniques to manage the accessibility, cost, and quality of healthcare. Also known as a managed care plan. Medicaid - A jointly funded federal and state program that provides hospital expense and medical expense coverage to the low-income population and certain aged and disabled individuals. medical advisory committee - Committee whose purpose is to review general medical management issues brought to it by the medical director. medical director - Manager in a healthcare organization responsible for provider relations, provider recruiting, quality and utilization management, and medical policy. Medicare - A federal government hospital expense and medical expense insurance plan primarily for elderly and disabled persons. See also Medicare Part A, Medicare Part B, and Medicare Part C. Medicare Part A - The part of Medicare that provides basic hospital insurance coverage automatically for most eligible persons. See also Medicare. Copyright©2008 CancerConsultants.com. All Rights Reserved. 11 FINANCIAL & INSURANCE ISSUES, continued Medicare Part B - A voluntary program that is part of Medicare and provides benefits to cover the costs of physicians’ services. See also Medicare. Medicare Part C - The part of Medicare that expands the list of different types of entities allowed to offer health plans to Medicare beneficiaries. Also known as Medicare+Choice. See also Medicare. Medicare supplement - A private medical expense insurance plan that supplements Medicare coverage. Also known as a Medigap policy. Omnibus Budget Reconciliation Act (OBRA) of 1990 - A federal act which established the Medicare SELECT program, a Medicare supplement that uses a preferred provider organization to supplement Medicare Part B coverage. outcomes measures -Healthcare quality indicators that gauge the extent to which healthcare services succeed in improving patient health. Patient Bill of Rights - Refers to the Consumer Bill of Rights and Responsibilities, a report prepared by the President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry in an effort to ensure the security of patient information, promote healthcare quality, and improve the availability of healthcare treatment and services. The report lists a number “rights,” subdivided into eight general areas, that all healthcare consumers should be guaranteed and describes responsibilities that consumers need to accept for the sake of their own health. peer review -The analysis of a clinician’s care by a group of that clinician’s professional colleagues. The provider’s care is generally compared to applicable standards of care, and the group’s analysis is used as a learning tool for the members of the group. pharmacy and therapeutics committee - Committee charged with developing a formulary, reviewing changes to that formulary, and reviewing abnormal prescription utilization patterns by providers. pharmacy benefit management (PBM) plan - A type of managed care specialty service organization that seeks to contain the costs, while promoting safer and more efficient use, of prescription drugs or pharmaceuticals. Also known as a prescription benefit management plan. Preferred Provider Organization (PPO) - A PPO allows patients to see a doctor from the plan’s network of physicians for a small copayment fee. Patients who choose to see a doctor out of the network must pay the balance between the PPO’s scheduled fee and the billed amount. premium - A prepaid payment or series of payments made to a health plan by purchasers, and often plan members, for medical benefits. prior authorization - In the context of a pharmacy benefit management (PBM) plan, a program that requires physicians to obtain certification of medical necessity prior to drug dispensing. Also known as a medical-necessity review. therapeutic substitution - The dispensing of a different chemical entity within the same drug class of a drug listed on a pharmacy benefit management plan’s formulary. Therapeutic substitution always requires physician approval. usual, customary, and reasonable (UCR) fee - The amount commonly charged for a particular medical service by physicians within a particular geographic region. UCR fees are used by traditional health insurance companies as the basis for physician reimbursement. utilization management (UM) - Managing the use of medical services to ensure that a patient receives necessary, appropriate, high-quality care in a cost-effective manner. utilization review (UR) - The evaluation of the medical necessity, efficiency, and/or appropriateness of healthcare services and treatment plans. utilization review committee - Committee that reviews utilization issues brought to it by the medical director, often approving or reviewing policy regarding coverage, reviewing utilization patterns of providers, and approving or reviewing the sanctioning process against providers. Copyright©2008 CancerConsultants.com. All Rights Reserved. 12 FINANCIAL & INSURANCE ISSUES, continued Expensing Medical Costs on Your Tax Return Even with good insurance, treatment and follow-up care for cancer can incur many outof-pocket expenses. One way to recoup some of these expenses is to do an itemized deduction for your medical and dental expenses on your tax return. Note that you are only allowed to deduct the amount of your medical and dental expenses that is greater than a percentage of your income, currently 7.5% of your adjusted gross income (this is subject to change). If your income is high or your expenses are low, you might not benefit from an itemized deduction of medical expenses. The obvious deductible expenses include any medical or dental care costs for you, your spouse (if filing jointly), your child or dependent that were not covered by insurance. Any out-of-pocket medical expense that was reimbursed by insurance is not deductible. Other obscure expenses that are deductible include acupuncture, therapeutic massage, chiropractic medicine, contact lenses, eye glasses and laser eye surgery. Cosmetic or illegal surgeries are not deductible. If your treatment requires travel, transportation costs for travel by bus, taxi, train or plane are deductible. If traveling by car, you can expense the actual cost for oil and gas or allot 12 cents per mile. In either case, include parking fees and tolls. Lodging, but not meals, can also be deducted while traveling for the explicit purpose of medical treatment. Allowable lodging expenses may not exceed $50 per night per person. Other miscellaneous expenses you should keep track of and are allowed to deduct include medical conferences, prescription medication (including birth control pills), artificial limbs, wigs and nursing services. Nutritional supplements and household help other than nursing are not currently deductible. By keeping track of expenses and deducting them on your tax returns, you may be able to partially recover some of the out-of-pocket medical expenses not covered by your insurance. For more information on deducting medical and dental expenses look at Publication 502 and the instructions for Schedule A of form 1040 at www.irs.gov or see your accountant. Copyright©2008 CancerConsultants.com. All Rights Reserved. 13 ADMISSIONS The START Center for Cancer Care’s Admissions Department is responsible for obtaining complete and accurate demographic and personal information necessary for billing purposes. It is our goal to obtain as much of this information in advance to ensure a timely and expeditious check in and check out process. Patients may contact the admissions department for any questions regarding their insurance benefits, payment options, referrals, financial concerns they may have, or to report any changes in insurance coverage or mailing address by contacting 210-593-5700 and requesting to speak with any point of service representative at the appropriate site. PATIENT ADVOCACY Patient Advocacy Through our Patient Advocacy department we hope to create a better environment for our patients. A Patient Advocate will greet your during your first appointment, whenever possible. The Advocate will provide information about resources and services available to you and your representatives. This Advocate will also provide a confidential site for you to voice a complaint, concern or request and assist you in resolving the issue. It is our policy to resolve patient concerns and grievances in a timely, reasonable and consistent manner. Our goal is to learn from patients and whenever possible and appropriate we will take steps to improve the overall quality of patient care. We also welcome your compliments when appropriate, and pledge to notify the staff member responsible for assisting you. We encourage patients and their representatives to communicate with the Patient Advocacy office regarding any compliments, complaints, problems or concerns which have not been resolved directly with the parties involved. Contact Patient Advocacy at (210) 593-2652 or patient.advocacy@stoh.com, MondayFriday 8:00 a.m. - 5:00 p.m. ELECTRONIC MEDICAL RECORDS The START Center for Cancer Care utilizes an electronic medical record system designed specifically for oncologists. Physicians no longer flip through a patient’s chart page by page. Instead, the physician’s use the computer to scroll through the chart. Each exam room is equipped with a computer, so the patient’s information can be entered directly into the computer during the patient’s visit. This may include information such as vital signs, medications, allergies, past medical history, laboratory test results, and the patient’s exam. The physician and patient may review labs, scans, etc. through the computer. Electronic medical records improve accuracy in treatment, improve efficiency, and streamline communication among the medical team treating the patient. The records provide a continuity of care from doctor to doctor and a faster response time, as physicians can access patient records from wherever they are. 14 CLINICAL RESEARCH CLINICAL RESEARCH CLINICAL RESEARCH Introduction Clinical trials are studies that evaluate the effectiveness of new drugs or treatment strategies. The development of more effective cancer treatments requires that new and innovative therapies be evaluated with cancer patients. Each clinical trial is designed to find new or better ways to treat cancer patients. In oncology, clinical trials are especially important because, in the absence of high cure rates, nearly all therapeutic approaches are developmental in nature. Currently, there are hundreds of ongoing clinical trials in the United States. Although clinical trials are an important component of cancer care and are crucial for improving cancer treatment, fewer than 5% of cancer patients currently participate in clinical trials because they are uninterested or unaware that they exist, have difficulty finding an appropriate clinical trial that may be of benefit to them, or are ineligible to participate in a clinical trial because of prior treatment interventions. It is extremely important to decide whether or not to participate in a clinical trial before receiving any treatment from a physician. What are Clinical Trials? A clinical trial is a research study designed to evaluate potential new treatment options. These studies are the result of a long and deliberate cancer research process that often takes years. Clinical trials test the safety and effectiveness of new or modified cancer drugs, new drug doses, unique approaches to surgery or radiation therapy, and varied combinations of treatments. Clinical trials are an integral component for improving the treatment of medical conditions because they lead to higher standards of care. In the United States all new cancer treatment products must proceed through an orderly clinical trials evaluation process to ensure that they have an acceptable level of safety and demonstrate benefit to helping patients with a specific cancer before they become commercially available to other patients. Clinical trials essentially fall into two general categories. � The first general category of clinical trials are designed to evaluate new drugs, compounds, or biologic agents that have not yet been approved by the Food and Drug Administration (FDA) for administration to patients. All substances must go through several phases of clinical trials to document their safety and effectiveness before the FDA approves them for routine use to treat cancer patients. Prior to FDA approval, these substances are only available through clinical trials; however, after FDA approval, they are commercially available. � Clinical trials may also evaluate drugs, compounds, or biologic agents already approved by the FDA for the treatment of one type of cancer. These substances have already been determined to be safe by the FDA and they are now being evaluated in different doses, schedules, and combinations to determine how to optimally use them for the treatment of a variety of cancers. Copyright©2008 CancerConsultants.com. All Rights Reserved. 15 CLINICAL RESEARCH, continued Phases of Clinical Trials Development of new anticancer agents and treatment strategies occurs in four phases. Each phase is designed to determine specific information about the potential new treatment such as its risks, safety and effectiveness compared to standard therapy. The hope is that the new therapy will be an improvement over the previous standard therapy. Phase I Trials: This phase is probably the most important step in the development of a new drug or therapy. These trials usually involve a small number of patients for whom other standard therapies have failed or no known alternative therapy is available. Phase I therapy may produce anticancer effects and a small number of patients may benefit. However, the primary goals of this phase are to determine anticancer activity in humans, the maximum tolerated dose of the treatment, the manner in which the drug works in the body, the toxic side effects related to different doses and whether toxic side effects are reversible. Upon completion of phase I trials, the information that has been gathered is used to begin phase II trials. Phase II Trials: Once the information is gathered and analyzed from phase I trials, phase II trials are designed to determine the effectiveness of the treatment in a specific patient population at the dose and schedules determined in phase I. These trials usually require a slightly higher number of patients than phase I trials. This number may increase depending on the number of responses as the phase II trial progresses. Drugs or therapies that are shown to be active in phase II trials may become standard treatment or be further evaluated for effectiveness in phase III trials. Phase III Trials: Phase III trials compare a new drug or therapy with a standard therapy in a randomized and controlled manner in order to determine proof of effectiveness. Phase III trials require a large number of patients to measure the statistical validity of the results because patient age, sex, race, and other unknown factors could affect the results. To obtain an adequate number of patients, several physicians (investigators) from different institutions typically participate in phase III clinical trials. Phase IV Trials: Once the drug or treatment becomes part of standard therapy, the manufacturer of the drug may elect to initiate phase IV trials. This phase includes continued evaluation of the treatment effectiveness and monitoring of side effects as well as implementing studies to evaluate usefulness in different types of cancers. Copyright©2008 CancerConsultants.com. All Rights Reserved. 16 CLINICAL RESEARCH, continued How are Clinical Trials Conducted? Clinical trials are designed to test treatments under very specific scientific and ethical guidelines. Clinical trials use written protocols to define the purpose, design and conduct of a specific clinical trial. All of the research centers participating in a particular study use the same research protocol. The protocol is written by the sponsor of the study and explains what the trial will do, how it will be conducted, where it will be conducted, who may participate and how and when the participants will be evaluated. Sponsors of clinical trials include, but are not limited to, the National Cancer Institute, groups or networks of physicians, individuals within a single cancer institution and manufacturers of biopharmaceutical products. In order to protect patients participating in clinical trials, the sponsor reviews the protocol for safety and appropriateness and then the protocol must undergo a second neutral review by an Institutional Review Board (IRB). The Institutional Review Board is responsible for overseeing any clinical trials that are performed in the specific healthcare institution where the clinical trial is offered/conducted. An Institutional Review Board includes physicians, healthcare providers and individuals not involved in healthcare, including the clergy or ordinary citizens/consumers. Institutional Review Board members do not have any personal interest in the results of the trial and, therefore, can ensure that the study is conducted fairly and safely. Committee members serving on Institutional Review Boards address the following questions in reviewing protocols: • • • • • • • • • • Does this protocol have scientific value? Does the protocol have scientific validity? Does the study have a valid scientific design and yet pose an inappropriate risk for subjects? Are risks to subjects minimized? Are the risks to subjects reasonable in relation to anticipated benefits, if any, to subjects and the importance of the knowledge that may reasonably be expected to result? Is the selection of subjects equitable? Are additional safeguards in place for subjects likely to be vulnerable to coercion or undue influence? Will informed consent be obtained from research subjects or their legally authorized representatives? Is there adequate provision for monitoring the data collected to ensure the safety of subjects? Are there adequate provisions to protect the privacy of subjects and to maintain the confidentiality of data? The Institutional Review Board also reviews all informed consent documents to make sure that they provide clear and complete information for those evaluating the merits of enrolling in a specific clinical trial. Clinical trials evaluating cancer treatments or strategies may be offered in large university hospitals, local community hospitals and/or physician practices. The location where a clinical trial is conducted depends on the specific resources required to conduct the trial, the number of patients needed for enrollment in the trial to answer the question and the individual or institution’s interest in performing clinical trials in general. Copyright©2008 CancerConsultants.com. All Rights Reserved. 17 CLINICAL RESEARCH, continued Clinical Trials Safeguards Both standard care and clinical trials have risks, side effects and benefits that vary depending on the individual. However, there are rigorous guidelines in place to protect the well-being and safety of clinical trial participants. The physician and research nurse conducting the study will explain any known or anticipated risks ahead of time. Once a patient’s eligibility for a specific trial is established, the research nurse will explain the informed consent process. Informed consent is one of the patient’s most important rights in the research process, as it outlines the purpose of the study, the exact treatments that will be administered, all possible side effects, and the patient’s right to withdraw from the study at any point. Signing the consent form acknowledges that the trial was explained and is understood. Also, clinical trial participants are constantly monitored to identify any changes in their condition. Participating in Clinical Trials Clinical trials are designed to evaluate the effectiveness of new treatment interventions. The objective of these clinical trials is to test new therapies in patients who have cancer. Patients participate in clinical trials for several reasons, including: • • • The potential to benefit from a new drug or treatment procedure Improved management of symptoms resulting from treatment or cancer The opportunity to directly contribute to improving the understanding of how to treat a cancer and ultimately, benefit other patients Patients who participate in clinical trials receive either a promising new treatment or the best available conventional treatment. If a new treatment option is proven to work, patients who are participating in the clinical trial will be among the first to benefit. While there is no guarantee that any treatment will be successful, clinical trials have been proven to offer some of the most effective cancer treatments currently available today. Copyright©2008 CancerConsultants.com. All Rights Reserved. 18 CLINICAL RESEARCH, continued The Cost of Clinical Trials There are two types of costs associated with a trial: • • Patient care costs; and Research costs Patient care costs: These are costs associated with providing medical goods and services to each patient. Usual care costs include doctor visits, hospital stays, clinical laboratory tests, x-rays, and any other medical costs that occur regardless of whether a patient is participating in a clinical trial or receiving standard treatment. These costs are usually covered by a third-party health plan, such as Medicare or private insurance. Research costs: Research costs are costs that are associated with clinical trial participation, such as data collection and management, research physician and nurse time, analysis of results, and tests performed purely for research purposes. Such costs are usually covered by the sponsoring organization, such as a pharmaceutical company. Be sure to consult with your physician about the financial aspects of any trial you are evaluating. Health insurance companies and managed care companies decide which health care services they will pay for by developing coverage policies regarding the specific services. In general, the most important factor determining whether something is covered is a health plan’s judgment as to whether the service is established or investigational. Health plans usually designate a service as established if there is a certain amount of scientific data to show that it is safe and effective. If the health plan does not think that such data exists in sufficient quantity, the plan may label the service as investigational. Health care services delivered within the setting of a clinical trial are very often categorized as investigational and are not covered. This is because the health plan thinks that the major reason to perform the clinical trial is that there is not enough data to establish the safety and effectiveness of the service being studied. Thus, for some health plans, any mention of the fact that the patient is involved in a clinical trial results in a denial of payment. Health plans may define specific criteria that a trial must meet before extending coverage. Some plans, especially smaller ones, will not cover any costs associated with a clinical trial, while other, larger managed care plans have recently announced at least partial coverage of costs associated with clinical research. Policies vary widely, but in most cases the best strategy is to have a doctor initiate discussions with the health plans. Medicare Coverage For up-to-date information about Medicare coverage of clinical trials, visit the Web site http://www.hcfa.gov/medlearn/refctmed.htm to view the Medicare Clinical Trials Quick Reference Guide. Copyright©2008 CancerConsultants.com. All Rights Reserved. 19 20 SUPPORT SERVICES SUPPORT SERVICES SPA & WELLNESS CENTER Located just inside our lobby on the first floor is the beautiful Spa and Wellness Center which is due to open the end of 2009. The Start Center created the Spa and Wellness Center in keeping with our mission to deliver comprehensive cancer care. We believe that an integral part of comprehensive cancer care is addressing the needs of the whole person. We recognize that a cancer diagnosis can be challenging and can threaten your sense of well being and quality of life. The Spa and Wellness Center will offer complementary modalities in an effort to support you in your treatment and recovery process. Complementary modalities are evidence -based and are designed to complement your existing traditional medical regimen. Our treatments and services help manage chemotherapy side effects, pain, anxiety, stress, and depression. The spa services are designed to promote relaxation, rejuvenation and stress relief. Each service and modality is created with the special needs of a cancer patient in mind. The goal of the Spa and Wellness Center is to offer supportive services that optimize wellness by addressing the needs of body, mind, and spirit. The Spa and Wellness center will offer the following: • • • • • • • • • • • Acupuncture Massage Facials Nutritional Counseling Energy Therapy Reflexology Aromatherapy Psychological Counseling Spiritual Counseling Meditation Guided Imagery In addition to our treatments and services, the Spa and Wellness Center will have a specialty shop that will offer cancer specific products. Skin care, oral care, wigs, and mastectomy products are some of the items that will be found in our specialty shop. Our Spa and Wellness Center is available to patients, family members, or anyone touched by cancer seeking integrative oncology services. A full menu describing the services, prices, and items offered can be found in the center when we open. For further information, please contact the Director, Ginger Kemmy, RN, 593-5975. 21 VOLUNTEER AUXILIARY By becoming a member of the Care Today, Cure Tomorrow Volunteer Auxiliary… You will… Share the moments Share the benefits Share the caring, and Share the future. Whatever your background may be, your talents and skills can improve the lives of our patients. Membership is open to anyone interested in giving of themselves to help others. There are many areas in need of assistance…some including patient contact, while others consist of clerical assignments or helping nurses with preparing patient handouts. Before you volunteer, you will either need to attend a training class or agree to accompany a “buddy” for one shift. The requirements to become a Care Today, Cure Tomorrow Volunteer Auxiliary member are… � � � � � � � � Complete an application Meet with the Volunteer Coordinator Pay the one-time auxiliary membership dues ($10.00) Choose a specific day (Monday-Friday) Choose a shift (9:00 AM-12:00 PM or 12:00 PM-3:00 PM) Attend training session or choose a time to accompany a “buddy” Get a TB test (there is no charge…test can be given any day except Thursday) In order to remain an active volunteer, you must commit to a minimum of fifty (50) hours annually. In conjunction with the support of the START Center for Cancer Care administration, any funds acquired by the Auxiliary will be granted to the ThriveWell Cancer Foundation for patient assistance. The START Center for Cancer Care Patient Advocacy 4383 Medical Drive San Antonio, Texas 78229 Phone: 210-593-2652 Fax: 210-593-5992 Email: patient.advocacy@stoh.com 22 CANCER SUPPORT GROUPS LISTING Coping with Cancer A support group designed to educate and provide support for patients and their families. FOR USAA EMPLOYEES. Sponsored by American Cancer Society. 3rd Wed. from 12:30-1:00 USAA, Conference Room F-Fitness Area-Dugout Contact Charlotte Hickman or Susan McEreath 210-498-1385 A program designed to help patients, their families and friends better understand and learn to live with cancer. Several locations/times; see below. Sponsored by American Cancer Society. University Health Center - Downtown (formerly Brady Green) 1st and last Thursday of the month at 11:00 a.m. Bilingual Support Group 527 N. Leona, San Antonio, TX 78207 Contact Carmen Boudreau, LMSW 210-358-3620 St. Mathew’s Catholic Church 4th Monday at 7:30 p.m. except December 10703 Wurzbach Rd., San Antonio, TX 78230 Contact Norma Willet 210-561-0581 St. Philip of Jesus/UIW Health Ministry 3rd Sunday of every month, 10:30 - 11:30 Contact Jean Deliganis 210-224-7122 130 Bank Street , San Antonio, TX 78204 Northeast Baptist Hospital First floor - Cancer Resource room next to Oncology Area 3rd Tuesday of every month, 6:00 - 7:30 p.m. 8811 Village Dr., San Antonio, TX 78217 Contact Irene Henry 210-297-2419 St. Thomas Catholic Church Meet 4th Monday of the Month at 7:00PM Contact Eleanor Freeman 830-899-3211 or 210-382-5889 180 St. Thomas Dr, Canyon Lake, TX 78133 I Can Cope Support group for cancer survivors, family members or loved ones who are coping with cancer. 1st Tuesday of every month except public holidays Northeast Baptist Hospital–Classroom 2, 1st Floor (East Wing) Contact Northeast Baptist Hospital 210-297-7005 23 CANCER SUPPORT GROUPS LISTING, continued Women With Cancer-Support Group An educational program for women with cancer, their families and friends. This program includes doctors, nurses, social workers, and other health professionals who discuss issues related to cancer. Sponsored by American Cancer Society. 2nd Tuesday of every month, 6:30 p.m. - 7:30 p.m. First Baptist Church 1401 Pat Booker Rd., Universal City, TX 78148 Contact Nancy Anthony 210-422-6880 Life After Loss A bereavement support program for anyone who has experienced the loss of a loved one within the past two years. Sponsored by American Cancer Society. Please call the American Cancer Society for dates and locations. Contact the American Cancer Society Patient Services Dept 210-614-4212 Look Good… Feel Better… Provides information to women undergoing cancer treatments to help them look and feel more their appearance. This program is offered in a group setting by licensed cosmetologists. Sponsored by American Cancer Society. Last Monday of every month, 9:00 - 11:00 a.m. American Cancer Society office 8114 Datapoint Dr., San Antonio, TX 78229 Please contact the American Cancer Society to register or for information on other dates and locations. 210-614-4212 Lost Chord Club The American Cancer Society in cooperation with the International Association of Laryngectomees, provides visitation and support to laryngectomees and their families. Sponsored by American Cancer Society. 3rd Sunday of the month, 2:00 p.m. American Cancer Society office 8115 Datapoint Dr., San Antonio, TX 78229 Contact Patient Services Dept or Robert VanWinkle Volunteer 210-614-4212 or 210-403-2659 Reach to Recovery Volunteers who have been treated for breast cancer visit patients before and after surgery. Patients receive gift items including literature and a temporary breast form. Exercises are demonstrated at the request of the patient’s physician. Sponsored by American Cancer Society. A physician referral is required. Please call the American Cancer Society Patient Services Dept. for further details. www.cancer.org 1-877-227-1618 or 210-614-4213 24 CANCER SUPPORT GROUPS LISTING, continued United Ostomy Association of San Antonio Volunteers provide one-on-one visitation and support for colostomy, ileostomy and urostomy patients. This program is sponsored by American Cancer Society in partnership with the UOA. Meetings are last Monday of the month except May and December, 7:00 p.m. American Cancer Society Office 8114 Datapoint Dr., San Antonio, TX 78229 Contact Patient Services Dept–Diane Armstead 210-614-4212 or 210-684-2775 Brain Tumor Support Group Sponsored by Bexar County Brain Tumor Support Group Meet 2nd Tuesday of every month, 7:00 - 8:30 p.m. Warm Springs, 1st Floor, Resource Room 5101 Medical Center Drive, San Antonio, TX Contact Teresa Zdansky 830-779-3059 / cell: 210-386-5608 / sodagal@lavernia.net Cancer Support Group Sponsored by Boerne Cancer Support Group 2nd and 4th Monday of each month, 7:00 p.m. - 8:30 p.m. St. Mark Presbyterian Church 208 W. Bandera St., Boerne, TX 78006 Contact St. Mark Presbyterian Church for more information–Larry Warren, PhD 830-816-3000 Make Today Count Sponsored by Cancer Therapy & Research Center (CTRC) 2nd and 4th Thursdays, 6:00 p.m. Cancer Therapy & Research Center 7979 Wurzbach Rd., San Antonio, TX 78229 Contact Patient & Family Services @ 210-616-5570 or Jenny Gonzalez @ 210-450-1565 Cancer Support Counselors Available. Sponsored by Harvest Fellowship Community Church. Harvest Fellowship Community Church 1270 North Loop 1604, San Antonio, TX 78232 Contact Maxine Klein 210-249-2400 Kathy’s Angels Breast Cancer Support Group for Holy Trinity/St. Marks Church or anyone else who’d like to attend. Sponsored by Holy Trinity Catholic Church. Sonterra Country Club Please contact Sherry Drury for more information and details 210-497-4200, Ext. 305 25 CANCER SUPPORT GROUPS LISTING, continued Breast Cancer Support Group Sponsored by Keep Abreast. 1st Monday of the month; 6:00-7:00 p.m. Metastatic; 7:00-9:00 p.m. All Breast Cancer Cancer Therapy & Research Center Grossman Library 1st Floor 7979 Wurzbach Rd, San Antonio, TX 78229 Contact Suzi Emanuel for more information 210-593-5748 Kerrville Cancer Support Group Open to any patient receiving treatment, their caregiver or cancer survivor. Sponsored by Kerrville Cancer Support Group. 2nd Wednesday of the month, 5:00 p.m. in Reception Area Kerrville Cancer Center 218 Sidney Baker North, Kerrville, TX Contact Patrice Doerries 830-257-7088 or 1-888-621-0047 Multiple Myeloma Sponsored by Leukemia & Lymphoma Society 2nd Wed. of the month, 6:30-8:00 p.m. Contact Nicole Bell for more information 210-377-1775, ext. 111 Children Cancer Support Group For children with all types of cancer. Sponsored by Leukemia & Lymphoma Society Of America Various locations–contact Nicole Bell for more information 210-377-1775, Ext. 111 Medina Area Cancer Support Group For all types of cancers. Sponsored by Medina Area Cancer Support Group. 1st Monday of every month October through June, 7:00 p.m. Medina Community Library 13948 St. HWY 16 N, Medina TX 78055 Contact Robert Gladden 830-589-7664 Survivors Offering Support Breast cancer support group for the patient and family. Sponsored by Methodist Healthcare. 1st Tuesday of every month at 7:00 p.m. Northeast Methodist Hospital 12412 Judson Rd. at the Community Center Contact Libby Fleming 210-575-0355 26 CANCER SUPPORT GROUPS LISTING, continued General Cancer Support Group Support group for friends and families only of cancer patients. Program sponsored by Methodist Hospital. Thursdays, 2:00-3:00 pm Methodist Hospital– 8th floor-Family Waiting Room 7700 Floyd Curl Drive, San Antonio, TX 78229 Contact Nikki Yuill 210-575-4558 Prayer Meeting Service/Support Group. Program sponsored by Methodist Hospital. Tuesdays, 6:00 p.m. Methodist Hospital– 8th floor-Family Waiting Room 7700 Floyd Curl Drive, San Antonio, TX 78229 Contact Nikki Yuill 210-575-4558 Gynecologic Cancer Support Group Cervical, Ovarian and Uterine cancer. Sponsored by National Ovarian Cancer Coalition La Madeline Contact Linda Tarver for more information 210-824-3496 or 830-227-5778 Gynecologic Cancer Support Group Ovarian or other types of gynecologic cancer. Peer-to Peer Support through the NOCC. Sponsored by National Ovarian Cancer Coalition. Please contact Diedre J. Steele for more information 210-497-5259 / dierdresteele_nocc@sbcglobal.net The Harbor GYN Center Support Group Sponsored by Northwest Counseling Center. Meetings: 2nd Tuesday of January, April, July and October Sea Island Restaurant 1604 & Bandera, San Antonio, TX Contact Barbara Fry @ 210-736-5053 or Ann Cavett @ 830-981-4676 New Braunfels Area Breast Cancer Support Group Sponsored by St. Paul Lutheran Church New Braunfels 3rd Monday of the month, 9:30 a.m. St. Paul Lutheran Church 181 South Santa Clara Ave., New Braunfels, TX 78130 Contact Becky Voges for more information 830-625-9191 Help and Hope for the Journey Sponsored by University United Methodist Church. 2nd and 4th Wednesday of the month, 7:00 p.m. - 8:00 p.m. 5084 DeZavala #205 Contact Dorothy Phillips 210-292-3795 27 CANCER SUPPORT GROUPS LISTING, continued Prostate Cancer Support Group San Antonio Alamo Chapter Meetings. Sponsored by Us Too Partners. 1st Monday of the month at 5:30 p.m. 8310 Ewing Halsell Drive, San Antonio, TX 78229 For more information contact John Staha 24/7 Home 830-569-5516 or 830-570-7012 Prostate Cancer Survivor Support Group Support group provides information by specialist in the various fields related to prostate cancer, such as surgery, radiation and medicine. Sponsored by Us Too Partners. Normally scheduled for the 1st Thursday of each month at 7:00 p.m. South Texas Regional Medical Ctr. Chapter of Us Too 1905 Hwy. 97 East, Jourdanton, TX 78026 For more information contact John Staha 24/7 Home 830-569-5516 or 830-570-7012 Wilford Hall Medical Center General Cancer Support Group for the patient and the family. Military and civilian. Every Thursday of the month at 1:00-2:00 p.m. Wilford Hall Medical Center 2200 Bergquist, Family Room 6 A35, San Antonio, TX 78236 Call Cindy Burke @ 210-292-6914 or Dorothy Phillips @ 210-292-3795 for information 28 RESOURCES National Cancer Institute 1-800-4-CANCER or www.cancernet.com American Cancer Society (local offices throughout the U.S.) 1-800-ACS-2345 or www.cancer.org www.cancerfatigue.org www.chemocare.com www.cancersymptoms.org www.acor.org www.oncochat.org www.plwc.org www.utmb.edu www.cancerpatientcare.org www.cancer.gov www.planetcancer.org www.activesurvivor.org www.utmb.edu/nsights/18ways.htm www.aapainmanage.org www.patientcenters.com www.webmd.com www.preventcancer.org www.painfoundation.org www.texascancercouncil.org 29 AREA BUSINESSES Hotels Oak Hills Medical Center Inn & Suites 7401 Wurzbach 210-614-9900 Homegate Studios & Suites 10950 Laureate Drive 210-691-1103 Hampton Inn 4803 Manitou Drive 210-684-9966 Country Hearth Inn 7500 Louis Pasteur 210-616-0030 Staybridge Suites 4320 Spectrum One 210-558-9009 Courtyard at Marriott 8585 Medical Drive (off Fredericksburg @ Wurzbach) 210-614-7100 Residence Inn by Marriott 4041 Bluemel 210-561-9660 Omni San Antonio 9821 Colonnade Drive 210-691-8888 Motel 6 9400 Wurzbach 210-593-0013 Embassy Suites Hotel 7750 Briaridge (IH-10 @ Callaghan) 210-340-5421 Studio 6 7719 Louis Pasteur Court 210-349-3100 Hampton Inn (Six Flags) 11010 IH-10 @ Huebner 210-561-9058 Super 8 Motel 5319 Casa Bella (IH-10 @ DeZavala) 210-696-6916 Springhill Suites by Marriott 3636 NW Loop 410 @ Fredericksburg 210-737-6086 Drury Inn Northwest 9806 IH-10 West @ Wurzbach 210-561-2510 Hyatt Place 4325 Amerisuites Drive 210-561-0099 Homewood Suites 4323 Spectrum One 210-696-5400 Candlewood Suites 9350 IH-10 West 210-615-0550 Comfort Inn 1-877-727-8483 Complimentary Shuttle Ronald McDonald House 4803 Sid Katz 210-614-2554 Drury Inn 9806 IH 10 West 210-561-2510 30 AREA BUSINESSES, continued Grocery Stores HEB 5803 Babcock @ Huebner 210-641-6403 HEB 9900 Wurbach @ IH-10 210-696-0794 Pharmacies HEB 5803 Babcock @ Huebner 210-641-6405 Pill Box Pharmacy 7718 Louis Pasteur 210-614-3360 CVS Drugs 4805 Medical 210-616-0482 Oak Hills Pharmacy 7711 Louis Pasteur 210-614-4100 Walgreens 6393 Babcock 210-690-0825 Walgreens 5282 Medical Drive 210-614-3588 Long-Term Housing CWS Corporate Housing 210-479-7231 Banks Broadway National Bank Fredericksburg @ Datapoint 210-283-6500 Bank of America 7333 Wurzbach 210-614-9910 McMullen County State Bank 8800 Huebner @ Floyd Curl 210-641-7000 Washington Mutual 4703 Medical Drive 210-614-3754 Frost Bank Loop 410 @ Fredericksburg 210-220-6914 210-856-3315 Wells Fargo 4351 Medical Drive 210-856-5000 Compass Bank 7940 Floyd Curl @ Tower II Bldg. 210-592-5700 Wachovia 4727 Medical Drive 210-616-9486 Bank One 7954 Fredericksburg 210-617-6380 Compass Bank 7575 Wurzbach 210-592-5750 31 AREA BUSINESSES, continued Restaurants Chick-fil-A 4715 Medical Drive 210-615-5293 Black Eyed Pea 7959 Fredericksburg 210-614-3825 Big Apple Bagels 8434 Fredericksburg 210-614-3095 Quizno’s Italian Subs 8124 Fredericksburg 210-614-5577 Picnikins 8038 Wurzbach Road, Suite 140 210-616-0954 Dry Dock Oyster Bar 8522 Fredericksburg 210-692-3959 Jack In The Box 2465 Babcock 210-615-7328 Wendy’s 7727 Wurzbach 210-614-0540 Aldo’s Italian Restaurant Fredericksburg @ Wurzbach 210-696-2536 Luby’s Cafeteria 9251 Floyd Curl @ Huebner 210-699-6652 Druthers Café 8637 Fredericksburg 210-691-2777 Jim’s 410 @ Fredericksburg 210-732-5491 Applebee’s 8224 Fredericksburg 210-614-3131 Jim’s IH-10 @ Huebner 210-691-0665 Le Madeleine Huebner Oaks Shopping Center IH-10 access road @ Huebner 210-691-1227 Cha Cha’s Mexican Restaurant 2026 Babcock 210-681-2066 Sarika’s Thai Food 4319 Medical Drive 210-692-3200 California Pizza Kitchen Huebner Oaks Shopping Center IH-10 access road @ Huebner 210-699-4275 Cracker Barrel 11030 W. IH 10 (between Huebner & De Zavala) 210-690-3808 Mencius Chinese Medical Drive @ Fredericksburg 210-615-1288 Bei Fang Chinese Restaurant 8637 Fredericksburg Road 210-697-8895 32 QUESTIONS & ANSWERS CHEMOTHERAPY & RADIATION CHEMOTHERAPY & RADIATION QUESTIONS & ANSWERS QUESTIONS TO ASK Questions to Ask My Doctor about My Cancer Before Treatment Being diagnosed with cancer can be overwhelming. Learning on your own about the disease, how it is treated, and how to apply this information to your situation is a daunting task and you may feel you need some help. While we can give you general information about your disease and its treatment, your doctor is the best source of information about your particular situation. It is important to have frank, open discussions with your cancer care team. They want to answer all of your questions, no matter how trivial they might seem. But you need to know what to ask. Getting answers to the questions below can help you understand your cancer and your options, so that you can be an active participant in your cancer treatment. • • • • • • • • • • What kind of cancer do I have and where is it located? Has my cancer spread beyond the primary site? What is the stage of my cancer and what does that mean in my case? What treatment choices do I have? What do you recommend and why? What risks or side effects are there to the treatments you suggest? What are the chances my cancer will come back with these treatment plans? What is my prognosis with these treatments? What should I do to be ready for treatment? Should I follow a special diet? Will the treatment be painful? Will I have any scars? During and After Treatment Once you have decided on a course of treatment, you will need to know what to expect and what to look out for. While all of the following questions may not apply to you, asking the ones that do apply may be helpful. • • • • • • • • • • How will you know if the treatment is working? Is there anything more that I can do to manage side effects? Are there any symptoms that I should notify you about immediately? Will I need to be on a special diet during and after treatment? Are there any limitations on my activities or amount of exercise? How often will I need to have follow up exams? How will I know if the cancer has returned? What symptoms should I watch for? Will I have to have more imaging tests in the future such as CT scans or MRI scans? What blood tests will be needed? What are my options if the cancer comes back? ©2002 American Cancer Society 33 QUESTIONS TO ASK, continued Other questions I need answered In addition to the sample questions on the previous page, be sure to write down some of your own. For instance, you might want more information about recovery times so you can plan your work schedule. Or, you may want to ask about second opinions or about clinical trials for which you may qualify. Write your questions below. • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ • _______________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ 34 CHEMOTHERAPY QUESTIONS & ANSWERS Chemotherapy Chemotherapy is any treatment involving the use of drugs to kill cancer cells. Cancer chemotherapy may consist of single drugs or combinations of drugs, and can be administered through a vein, injected into a body cavity, or delivered orally in the form of a pill. Chemotherapy is different from surgery or radiation therapy in that the cancerfighting drugs circulate in the blood to parts of the body where the cancer may have spread and can kill or eliminate cancers cells at sites great distances from the original cancer. As a result, chemotherapy is considered a systemic treatment. More than half of all people diagnosed with cancer receive chemotherapy. For millions of people who have cancers that respond well to chemotherapy, this approach helps treat their cancer effectively, enabling them to enjoy full, productive lives. Furthermore, many side effects once associated with chemotherapy are now easily prevented or controlled, allowing many people to work, travel, and participate in many of their other normal activities while receiving chemotherapy. Being informed about chemotherapy and its potential side effects can help you to proactively manage your own care and optimize your treatment and outcome. Things you may need to know include the following topics: • • • • • • How is chemotherapy delivered? Managing Chemotherapy Side Effects Understanding and Monitoring Your Blood Count When to Call Your Doctor Frequently Asked Questions How is chemotherapy delivered? Overview There are a variety of schedules and techniques used to deliver chemotherapy and yours will depend on which treatment your doctor prescribes. Cancer chemotherapy may consist of a single drug or combinations of drugs that are delivered in cycles. A cycle consists of treatment with one or more drugs followed by a period of rest. Chemotherapy can be administered orally in the form of a pill, into a vein (intravenous), injected into a body cavity (such as the bladder), into a muscle (intramuscular), or into the spinal fluid (intrathecal). Currently, most chemotherapy is administered intravenously; however, oral chemotherapy drugs are gaining wider use. In some cases, it may be beneficial to administer IV chemotherapy through a venous access device (VAD), which is inserted into a major vein in the body and can remain in place for a long period of time. Not every chemotherapy patient requires a VAD. However, for those that are undergoing frequent treatment, blood tests, and nutritional support, a VAD is beneficial by reducing the number of needle sticks and associated discomfort. Copyright©2008 CancerConsultants.com. All Rights Reserved. 35 CHEMOTHERAPY QUESTIONS & ANSWERS, continued How often will I receive chemotherapy? Chemotherapy drugs are typically given in cycles. The cycle consists of the day(s) the drug is administered followed by a rest and recovery period. A cycle usually lasts one to four weeks and is then repeated, which means a treatment is administered every one to four weeks. Each course of chemotherapy is different, but generally consists of four to six cycles. The actual administration of some chemotherapy drugs may take only seconds or minutes, while others may take hours or even days. What are the advantages and disadvantages of oral chemotherapy drugs? In the past, chemotherapy drugs were mainly administered into a vein (intravenous). Recently, oral chemotherapy drugs are being developed. Oral drugs may provide greater ease of administration since patients can take them at home rather than going to a clinic or hospital for treatments. Not all chemotherapy drugs are available in oral form. Furthermore, intravenous (IV) administration is sometimes preferable because the doctor can be more certain that the patient received the appropriate dose as scheduled and they can monitor the patient during administration. What is a venous access device (VAD) and what types are used for cancer patients? A VAD is a surgically implanted device that provides long-term access to a major vein. Although there are several different types of VADs, the two most commonly used for cancer treatment and taking blood samples are: • • Tunneled external catheters (Hickman® catheter), or Subcutaneous implanted ports (port-a-cath). Both a Hickman® catheter and a port-a-cath are surgically implanted into a major vein. For the Hickman® catheter, the plastic tube or catheter is attached to a major vein and then comes out of the body for external access. A port-a-cath is implanted completely beneath the skin into a major vein under the collarbone. The port may then be accessed by a special needle through the skin to deliver chemotherapy, hydration, transfusions, and for taking blood samples. The following are some key features that distinguish these two types of VADs: Hickman® catheter • • Easier insertion, removal, and access Higher flow capacity due to single, double, or triple lumen (channel) Port-a-cath • • • • Fewer device-related infections Fewer activity restrictions Less day-to-day maintenance Lower flow capacity due to only single or double lumen (channel) Patients undergoing very demanding therapies that require frequent treatment, blood transfusions, and nutritional support—such as a stem cell transplant—may be required a Hickman® catheter instead of a port. Copyright©2008 CancerConsultants.com. All Rights Reserved. 36 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Who needs a VAD? Not every chemotherapy patient requires a VAD. For some chemotherapy treatment plans, the inconvenience of implanting and accessing a VAD may outweigh the benefits. You may wish to ask your doctor if a VAD is an appropriate option for you, especially if you experience any of the following: • • • • • • • • • You are extremely anxious about having needles inserted. Your veins are difficult to access or become inaccessible. You must have alternative veins in your foot or hand accessed, which may be associated with more discomfort. You are undergoing continuous infusion chemotherapy (over an hour). You anticipate many months of chemotherapy treatments. You are receiving intravenous chemotherapy that requires multiple needle sticks. Your treatment requires frequent drawing of blood samples. Your treatment strategy involves chemotherapy agents that may cause “vein pain” when administered through the arm. You have a physician or nurse who recommend a vascular access device. What special precautions are necessary with a VAD? Your VAD must be flushed in order for it to work properly. Flushing your VAD requires placing a needle in your port and flushing it out with heparin. Heparin is a blood thinner prevents the catheter (plastic tube) from becoming occluded (clogged). While you are on treatment, your VAD will be flushed after each treatment. When you are no longer on treatment you must still remember to have your VAD flushed regularly. This procedure needs to be done every 4-6 weeks. It is your responsibility to make the appointment to have your VAD flushed. Copyright©2008 CancerConsultants.com. All Rights Reserved. 37 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Managing Chemotherapy Side Effects The treatment of cancer may include the use of chemotherapy, radiation therapy, biological therapy, surgery or some combination of all of these therapeutic options. All of these treatment options are directed at killing or eradicating the cancer that exists in the patient’s body. Unfortunately, the delivery of cancer therapy, including chemotherapy, often affects the body’s normal organs and tissues not affected by cancer. The undesired consequence of damaging healthy cells is a complication of treatment, or a side effect. Side effects may be acute (short-term), chronic (longer-term), or permanent. When cancer treatments are evaluated, side effects are measured and reported as part of the treatment evaluation. Examples of acute side effects include nausea and vomiting, and mouth sores (mucositis). Why do side effects occur? Unfortunately, most chemotherapy drugs cannot tell the difference between a cancer cell and a healthy cell. Therefore, chemotherapy often affects the body’s normal tissues and organs which results in complication of treatments, or side effects. Side effects cause inconvenience, discomfort, and may occasionally be fatal. Additionally and perhaps more importantly, side effects may prevent doctors from delivering the prescribed dose of therapy at the specific time and schedule of the treatment plan. Because the expected outcome from therapy is based on delivering treatment at the dose and schedule prescribed in the treatment plan, a change from the treatment plan may reduce your chance of achieving an optimal outcome. This is extremely important to understand. In other words, side effects not only cause discomfort and unpleasantness, but may also compromise your chance of cure by preventing the delivery of therapy at its optimal dose and time. What are the most common side effects? All chemotherapy is associated with a wide variety of side effects. However, some side effects occur more frequently than others. Whether you will experience side effects, which ones, and their severity depends on a variety of factors, including your type of cancer, the type of chemotherapy drug or regimen you are taking, your physical condition, your age, and others. However, the following side effects are typically associated with chemotherapy: • • • • • • • • • • • • Anemia Depression Fatigue Hair Loss Infection/Fever Low Blood Counts Mouth Sores Nausea and Vomiting Neutropenia Pain Reproduction/Sexuality Thrombocytopenia Copyright©2008 CancerConsultants.com. All Rights Reserved. 38 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Can anything be done about side effects? Fortunately, in the last 20 years there has been a great deal of progress in the development of treatments to help prevent and control the side effects of cancer therapy. These developments have: • • • Led to vast improvements in the management of symptoms associated with cancer treatment Allowed chemotherapy to be delivered with greater accuracy and consistency, Made many cancer treatments more widely available. For example, modern anti-vomiting drugs, called antiemetics, have reduced the severity of nausea and vomiting with chemotherapy. In addition, blood cell growth factors are now available to protect patients from infection, to reduce the fatigue associated with anemia, and to ensure that treatment can be delivered at the planned dose and schedule for optimal outcomes. Understanding and Monitoring Your Blood Counts Overview A reduced number of blood cells in circulation is a common side effect of chemotherapy. Blood is composed of three basic blood cell types: red blood cells, white blood cells, and platelets. Blood cells are produced in the bone marrow and regularly released into circulation. Chemotherapy destroys rapidly dividing cells, a characteristic of cancer cells. However, bone marrow cells also divide rapidly and are frequently damaged by chemotherapy. Blood counts are monitored with a laboratory test called a Complete Blood Count (CBC). The best way to treat low blood counts is to prevent them before they occur. This can be accomplished with the administration of blood cell growth factors. In some circumstances, blood transfusions may also be necessary. • • • • • • What are low blood counts? What causes low blood counts? What are the symptoms of low blood counts? Why is it important to monitor low blood counts? How are low blood counts diagnosed? What are the treatments for low blood counts? What are low blood counts? A blood count is a measurement of the number of blood cells an individual has in circulation based on laboratory evaluation of a blood sample. Blood is composed of three basic blood cell types: red blood cells, white blood cells, and platelets. You should have billions of these blood cells circulating throughout your body. However, certain circumstances may cause you to have fewer cells than is considered normal, a condition which is called “low blood counts”. The laboratory test that is conducted to measure the number of blood cells is called a complete blood count, or CBC. Copyright©2008 CancerConsultants.com. All Rights Reserved. 39 CHEMOTHERAPY QUESTIONS & ANSWERS, continued What causes low blood counts? The most common reason cancer patients experience low blood counts is as a side effect of chemotherapy. Chemotherapy involves the use of drugs to destroy cancer cells. Chemotherapy works by destroying cells that grow rapidly, a characteristic of cancer cells. Unfortunately, chemotherapy also affects normal cells that grow rapidly, such as cells in the bone marrow that produce red blood cells, white blood cells, and platelets. What are the symptoms of low blood counts? Your symptoms will depend on which types of blood cells are low. Common symptoms of the different types of low blood cell counts are listed in table 1. Table 1: Common symptoms of low blood counts Low red blood cell Fatigue or tiredness Trouble breathing Rapid heartrate Difficulty staying warm Pale skin Dizziness Lightheaded Low white blood cell Infection Fever Low platelets Excessive bruising Excessive bleeding Nosebleeds Why is it important to monitor blood counts? It is important to monitor for low blood cell count because this condition may: • • Increase your risk of unpleasant and sometimes life-threatening side effects, such as fatigue, infection, and/or bleeding. Disrupt delivery of your cancer treatment, resulting in a change to the planned dose and time. How are low blood counts diagnosed? A test called the complete blood count (CBC) is used to determine whether your blood counts are low. The CBC measures the levels of the three basic blood cells: red, white, and platelets. In the United States, the CBC is typically reported in the format shown below. If your blood counts fall outside of the normal range, which is shown in the “Reference interval” column, their values will be reported in the “Flag” column with an ‘L’ for low and an ‘H’ for high. The example CBC on the next page shows that white blood cells, red blood cells, and platelets are all low. Copyright©2008 CancerConsultants.com. All Rights Reserved. 40 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Table 2: CBC with Differential Test White Blood Count Red Blood Count Hemoglobin Hematocrit Platelets Polys Lymphs Monocytes Eos Basos Polys (absolute) Lymphs (absolute) Monocytes (absolute) Eos (absolute) Basos (absolute) Result Flag 1.5 L 3.50 L 10.8 L 31.1 L 302 23 L 68 H 7 2 > .34 L 1.0 0.1 0.1 0.0 Units x 10-3/mL x 10-6/mL g/dL % x 10-3/mL % % % % % x 10-3/mL x 10-3/mL x 10-3/mL x 10-3/mL x 10-3/mL Reference Interval 4.0-10.5 4.70-6.10 14.0-18.0 42.0-52.0 140-415 45-76 17-44 3-10 0-4 0.2 1.8-7.8 0.7-4.5 0.1-1.0 0.0-0.4 0.0-0.2 Result column: The result column shows counts that fall within the normal range. Flag column: The flag column shows counts that are lower (“L”) or higher (“H”) than the normal range. Reference interval (or reference range) column: The reference interval shows the normal range for each measurement for the lab performing the test. Different labs may use different reference intervals. White blood cells: White blood cells help protect individuals from infections. The above CBC report shows that the patient’s total white cell count is 1.5, which is lower than the normal range of 4.0-10.5. The low white cell count increases the risk of infection. Differential: This portion of the CBC shows the counts for the 5 main kinds of white cells, either as percentages (the first 5 counts), or as the absolute number of cells (the second 5 counts). Absolute neutrophil count: Neutrophils are the main white blood cell for fighting or preventing bacterial or fungal infections. In the CBC report, neutrophils may be referred to as polymorphonuclear cells (polys or PMNs) or neutrophils. The absolute neutrophil count (ANC) is a measure of the total number of neutrophils present in the blood. When the ANC is less than 1,000, the risk of infection increases. The ANC can be calculated by multiplying the total WBC by the percent of polymorphonuclear cells. For example, this patient’s ANC is 0.34, which equals (WBC) 1.5 x 23%. Copyright©2008 CancerConsultants.com. All Rights Reserved. 41 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Red blood cells: Red blood cells carry oxygen from the lungs to the rest of the body. The above CBC report indicates that the patient has a red cell count of 3.5, which is lower than the normal range of 4.70-6.10, and therefore, shown in the flag column. Hemoglobin (Hb or Hgb): Hemoglobin is a protein in the red cell that carries oxygen. The above CBC report indicates that the patient’s Hb count is 10.8, which is below the normal range of 14.0-18.0. The hematocrit (HCT), another way of measuring the amount of Hb, is also low. This means that the patient has mild anemia and may be starting to notice symptoms. These three ranges will vary depending on age and gender. For women, they will be lower than those shown here. For example, the Hb reference interval for a woman is 12.0-16.0. Platelets: Platelets are the cells that form blood clots that stop bleeding. The above CBC report indicates that the platelet count for this patient is normal. What are the treatments for low blood counts? The best treatment for low blood counts is to prevent them before they occur. This can be accomplished with the administration of blood cell growth factors. Blood cell growth factors are substances produced by the body that stimulate the cells in the bone marrow to produce more red blood cells, white blood cells, or platelets. These factors have also been produced in a laboratory and are approved by the Food and Drug Administration (FDA) for the treatment of cancer patients with low blood counts. Low red blood cell counts: Erythropoietin is a blood cell growth factor that selectively increases production of red blood cells. Clinical trials have demonstrated that erythropoietin is safe and effective in reversing anemia in cancer patients. Erythropoietin has been proven to effectively: • • • • Increase hematocrit Decrease the need for blood transfusions Reverse fatigue Improve overall sense of well-being Erythropoietin is FDA-approved for the treatment of anemia in patients with nonmyeloid cancers (cancers that do not involve blood cells), whose anemia is a result of chemotherapy. Treatment with erythropoietin causes a gradual increase in red blood cell production. The body uses iron in red blood cell production. Thus, supplemental iron may be required to adequately support erythropoietin-stimulated erythropoiesis. Virtually all patients receiving erythropoietin therapy will eventually require supplemental iron therapy. Copyright©2008 CancerConsultants.com. All Rights Reserved. 42 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Low white blood cell count: The blood cell growth factors approved by the FDA for the prevention of chemotherapy-induced neutropenia are Neupogen® (filgrastim) and Neulasta® (pegfilgrastim). Multiple clinical trials have shown that Neulasta® and Neupogen® reduce the severity and duration of low white blood cell counts associated with many kinds of chemotherapy regimens. By increasing white blood cell counts, Neupogen® has been shown to decrease a patient’s risk of fever and admission to the hospital. The drawback of Neupogen®, however, is that it must be administered daily. In two clinical trials, a single dose of Neulasta® has been proven to be as effective as an average of 11 daily injections of Neupogen® for the management of neutropenia. The most common side effect you may experience with Neulasta® is aching in the bones. If this happens, it can usually be relieved with a non-aspirin pain reliever, such as acetaminophen. It is also possible to have an allergic reaction to Neulasta®. Low platelet count: The blood cell growth factor approved by the FDA for the prevention of low platelet count is called Neumega®. Clinical studies have shown that Neumega® prevents thrombocytopenia and decreases the need for platelet transfusions in patients at high risk for developing a low platelet count. Neumega® has been reported to cause palpitations, fluid retention and diarrhea as well as other side effects in some patients. Transfusions: In some cases, low blood counts may be so severe that you may need to undergo a blood transfusion. Red blood cells and platelets are often transfused. Sources for transfusional blood include blood banks or your own blood that you had stored for future use before undergoing treatment. Transfusions may be associated with complications, including allergic reactions that may range from mild to life-threatening. In general, it is better to prevent low blood counts than to treat them once they occur. References 1. Glaspy JA, Jadeja J, Justice G. Optimizing the management of anemia in patients with cancer: a randomized, active-controlled study investigating the dosing of darbepoetin alfa [abstract]. Proceedings of the American Society of Clinical Oncology 38th annual meeting; May 18-21, 2002. Abstract 1446. 2. Kotasek D, Albertson M, Mackey J. Randomized, double-blind, placebo-controlled, dose-finding study of darbepoetin alfa administered once every 3 (Q3W) or 4 (Q4W) weeks in patients with solid tumors [abstract]. Proceedings of the American Society of Clinical Oncology 38th annual meeting; May 18-21, 2002. Abstract 1421. 3. Vose J, Crump M, Lazarus H. Randomized, multicenter, open-label study of pegfilgrastim compared with daily filgrastim after chemotherapy for lymphoma. Journal of Clinical Oncology. 2003;21: 514-519. 4. Green M, Koelbl H, Baselga J. A randomized double-blind multicenter phase III study of fixed-dose single-administration pegfilgrastim versus daily filgrastim in patients receiving myelosuppressive chemotherapy. Annals of Oncology. 2003:14:29-35. Copyright©2008 CancerConsultants.com. All Rights Reserved. 43 CHEMOTHERAPY QUESTIONS & ANSWERS, continued When to Call Your Doctor The development of any of the following symptoms during your chemotherapy treatment may indicate a serious condition. If you experience any of the following throughout your cancer treatment, please inform your doctor. • • • • • • • • • • • • • • • • • • Fever higher than 100.5º F Shaking chills Vomiting that continues 48 hours after treatment Bleeding or bruising Shortness of breath/chest pain Severe constipation or diarrhea Painful or frequent urination Blood in the urine or stool Soreness, redness, swelling, pus, or drainage at your VAD site Irregular or rapid heart beat Pain in a new place Pain that is not relieved by your pain medication Headache that is not relieved by Tylenol® Inability to eat and continued weight loss Mouth sores Nasal congestion, drainage, cough One or more of the following symptoms in conjunction with repetitive diarrhea or vomiting (signs of dehydration): ° Dry, cracked lips ° Dry, sticky tongue ° Increased thirst ° Decreased urination ° Increased weakness ° Increased pulse rate Dizziness/lightheadedness (especially when rising to a standing position) Copyright©2008 CancerConsultants.com. All Rights Reserved. 44 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Most Frequently Asked Questions about Chemotherapy How does chemotherapy work? Chemotherapy kills rapidly-dividing cells in a variety of ways, depending on the drug. Since there are many different types of cancers that all grow differently, many chemotherapy drugs have been developed to target these various growth patterns. Each drug has a different way of working and is effective at a specific time in the life cycle of the cell it targets. For example, some chemotherapy drugs work by: • • • Damaging DNA, Preventing cells from dividing, or Disrupting cellular metabolism or other critical functions. How is chemotherapy given? Chemotherapy can be given: • • • • Intravenously (IV), By mouth in the form of a pill, With a shot (injection), or By intrathecal and intraventricular injection (meaning into the spinal fluid surrounding the spinal cord or brain). Many types of chemotherapy can be given at home. Through instruction, you and your family members can learn how to administer chemotherapy in pill form or by injection with small syringes and needles similar to those that people with diabetes use to administer insulin. In some cases, a nurse will administer chemotherapy in an outpatient clinic. In other cases, it may be necessary to go to the hospital to receive treatment. Chemotherapy is typically given in cycles, which is a treatment followed by a period of rest. A cycle can last one or more days, but is usually one, two, three, or four weeks long. A course of chemotherapy is comprised of multiple cycles. Each course is different, but generally consists of four to six cycles. It may take a relatively short period of time to receive some chemotherapy drugs, while others take hours. It all depends on the treatment regimen that your doctor recommends. If your chemotherapy is given through an IV, your doctor may suggest an implanted venous access device (VAD) such as a Hickman® catheter or Port-a-Cath. VADs are surgically placed in a large vein near the heart and can stay in place for long periods of time. By using a VAD, you will not have to have smaller catheters repeatedly placed in your arm veins. How often will I receive chemotherapy? Generally, treatments are given daily, weekly, or monthly. How often you receive chemotherapy depends on the type of cancer and which drug or combination of drugs you receive. Your doctor will help you determine the most effective treatment schedule for you. Chemotherapy is usually given in cycles with rest periods between each administration. Copyright©2008 CancerConsultants.com. All Rights Reserved. 45 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Chemotherapy may be used in combination with surgery. When chemotherapy is given before surgery it is referred to as neoadjuvant chemotherapy. The goal of neoadjuvant chemotherapy is to shrink the cancer before it is surgically removed. If the chemotherapy is given after surgery, it is referred to as adjuvant chemotherapy. The goal of adjuvant chemotherapy is to kill any cancer cells left in the body after surgery. Regardless of whether it is given before or after surgery, chemotherapy will still be administered in cycles that depend on the type of cancer and which drug or combination of drugs. What chemotherapy will I receive? You will receive chemotherapy that is best suited to achieve your goals of therapy. When selecting a treatment or treatments, your doctor will consider: • • • • • • • Your diagnosis How far along your cancer is in its development The expected behavior of the cancer Where the cancer originated Your age Other medical problems you may have Any potential side effects from the treatment. How is my chemotherapy scheduled? Chemotherapy is typically given in cycles, which is a treatment followed by a period of rest. A cycle can last one or more days, but is usually one, two, three or four weeks long. A course of chemotherapy is comprised of multiple cycles. Each course is different, but generally consists of four to six cycles. The actual administration of the chemotherapy drugs may take minutes to several hours, depending on the drug or drugs given. If your chemotherapy is given through an IV, your doctor may suggest an implanted venous access device (VAD) or Port-a-Cath. VADs are surgically placed in a large vein near the heart and can stay in place for long periods of time. By using a VAD you will not have to have smaller catheters repeatedly placed in arm veins. What are the side effects of chemotherapy? Chemotherapy works by destroying cancer cells; unfortunately, it cannot tell the difference between a cancer cell and a healthy cell. The delivery of cancer therapy often affects the body’s normal tissues or organs that are not affected by cancer. Side effects, or complications of treatment are the undesired consequence of affecting normal cells. Side effects of treatment may cause inconvenience, discomfort, and occasionally even fatality to patients. Additionally and perhaps more importantly, side effects may prevent delivery of the full dose of chemotherapy on schedule. This is extremely important to understand since your expected outcome from chemotherapy is based on delivering treatment at the full dose and schedule prescribed in the treatment plan. Because the expected outcome from therapy is based on delivering treatment at the prescribed dose and schedule, a change from the treatment plan may reduce your chance of achieving an optimal outcome. This is extremely important to understand. In other words, side effects not only cause discomfort and unpleasantness, but may also compromise your chance of cure by preventing the delivery of therapy at its optimal dose and time. Copyright©2008 CancerConsultants.com. All Rights Reserved. 46 CHEMOTHERAPY QUESTIONS & ANSWERS, continued The most common side effects of chemotherapy are low blood counts, nausea, vomiting, hair loss, and fatigue. Some side effects may be temporary and merely annoying. Others, such as infection or a low white blood count, can be life-threatening. For example, one of the most serious potential side effects of chemotherapy is a low white blood cell count – a condition called neutropenia (new-truh-pee-nee-ah) – which can put you at risk for severe infections or treatment interruptions. Fortunately, last 20 years has brought a great deal of progress in the development of treatments to help prevent and control the side effects of cancer therapy. These developments have • • • Led to vast improvements in the management of symptoms associated with cancer treatment Allowed for greater accuracy and consistency concerning the administration of cancer treatment Made many cancer treatments more widely available to patients throughout the world Why am I so tired? Many people who receive chemotherapy experience fatigue. Fatigue has many causes but frequently occurs because of anemia caused by the chemotherapy. Your daily activities should be planned according to how you feel, and you should take rest periods throughout the day as often as you feel necessary. Anemia can be effectively treated. To learn more, go to fatigue. Will my chemotherapy make me sick? Without receiving special anti-nausea medications, most patients will experience some nausea after treatment with chemotherapy. Nausea and vomiting may last 24-48 hours. The severity of nausea and vomiting mainly depends on which chemotherapy drugs were used. A number of very effective medications called anti-emetics or anti-nausea drugs are now available to help lessen or prevent nausea and vomiting. These medications may be given to you intravenously during your chemotherapy, or you may be given a prescription medication to take at home. To learn more, go to nausea and vomiting. What tests will be performed? Your doctor determines what kinds of tests are needed. If you are receiving chemotherapy, you may have blood work done anywhere from the day of or up to 7 days before your scheduled treatment. This blood work will include a complete blood count (CBC), chemistry profile, and any necessary cancer markers. A blood sample for a complete blood count (CBC) will also be collected seven to fourteen days following your chemotherapy. It is important to be aware of possible symptoms of reduced red blood cell (RBC), white blood cell (WBC), or platelet (PLT) production. Be sure to report any of the following: • • • Fever (over 100.5º F), congestion, or a cold. Earlier we’ve defined fever as 100.5 A rash, blister, easily bruised skin, signs of bleeding, an infected cut, itching or burning in the genital area. Weakness, fatigue, or shortness of breath. Copyright©2008 CancerConsultants.com. All Rights Reserved. 47 CHEMOTHERAPY QUESTIONS & ANSWERS, continued Why is my complete blood count (CBC) tested after treatment? Chemotherapy destroys rapidly dividing cells, a characteristic of cancer cells. However, red blood cells, white blood cells, and platelets also divide rapidly and are frequently damaged by chemotherapy. Your red blood cell count, white blood cell count, and platelet count may all go down. Your doctor monitors these counts to determine the toxicity of treatment and to predict your risk for complications, as well as to plan future therapy. For more information, see section on Understanding and Monitoring Your Blood Counts. Will I lose my hair because of my treatment? Hair loss occurs with some, but not all, chemotherapy drugs. The amount of hair loss varies from a slight thinning to complete baldness and affects the scalp, eyelashes and eyebrows, legs, armpits, and pubic area. Hair loss will typically begin two or three weeks after your first treatment. The amount of hair that you lose will depend on the type of chemotherapy drug you are taking. Hair typically begins to grow back approximately 2-3 weeks after treatment is finished. The hair may grow back differently than it was before treatment. For example color or texture (curly or straight) may be different. Remember that hair loss associated with chemotherapy is temporary and the hair WILL grow back. In the meantime, here are a few tips to help you cope with the loss: • • • • • • You may wish to cut your hair before it starts falling out. The experience of losing the hair is sometimes worse than dealing with it once it’s gone. If you expect to lose all or a lot of your hair, cutting it first may be easier to cope with. Plan ahead; shop for a wig before your hair is gone, especially if you wish to match your natural color. Or, take this opportunity to try something different. Try hats or head scarves; these are good alternatives or a compliment to a wig. Remember to cover your head or use sunscreen on your scalp. Skin that has been covered with hair may be particularly sensitive to UV rays of the sun. Ask your insurance company if they cover the cost of the wig. Treat your new hair gently once it grows back. Avoid chemicals, bleach, peroxide, or colors. Copyright©2008 CancerConsultants.com. All Rights Reserved. 48 RADIATION THERAPY QUESTIONS & ANSWERS Radiation Therapy Cancer treatment may vary depending upon the type of cancer, the stage of cancer, and the goal of treatment. Often, one or more treatment modalities may be used in order to provide the most complete treatment for the patient. Increasingly, it is common to use several treatment modalities concurrently (together) or in sequence. This is referred to as multi-modality treatment of the cancer and the modalities may include surgery, chemotherapy, biological therapy, and/or radiation therapy. For the majority of newly diagnosed cancer patients, the optimal treatment may be a multi-modality approach composed of standard therapies that have been established through extensive medical research. For other patients, the most appropriate therapy may still be under investigation and may be available only through a clinical trial. Radiation therapy works by damaging the DNA in the cancer cell, thereby disabling the cancer cells from reproducing and growing. The cancer cells then die and the cancer shrinks. The objective of radiation therapy is to kill enough cancer cells to maximize the probability of cure and minimize the side effects. Under some circumstances, radiation therapy may also be used as palliation, or palliative care, which is aimed at reducing symptoms but not curing the underlying disease. Radiation is usually administered in the form of high-energy beams that deposit the radiation dose in the body where cancer cells are located. Radiation therapy, unlike chemotherapy, is considered a local treatment. This means that cancer cells are only killed at the location in the body where the radiation is delivered, called the radiation field. If cancer exists outside the radiation field, those cancer cells are not destroyed by the radiation. Techniques for Delivering Radiation Therapy Radiation therapy may be delivered externally or internally. External radiation delivers high-energy rays directly to the cancer from a machine outside the body. Internal radiation, or brachytherapy, is the implantation of a small amount of radioactive material (seeds) in or near the cancer. External Beam Radiation Therapy (EBRT) EBRT is given via machines called linear accelerators, which produce high-energy external radiation beams that penetrate the tissues and deliver the radiation dose deep in the areas where the cancer resides. These modern machines and other state-of-the-art techniques have enabled radiation oncologists to significantly reduce side effects while improving the ability to deliver radiation. Copyright©2008 CancerConsultants.com. All Rights Reserved. 49 RADIATION THERAPY QUESTIONS & ANSWERS, continued EBRT is typically delivered on an outpatient basis for approximately 6 to 8 weeks. EBRT begins with a planning session, or simulation, during which a special CT is performed with the patient in the treatment position. Marks are placed on the surface of the patient. This information is then used by the radiation oncologist to develop a patient specific treatment plan. During treatment, the patient lies on a table and is treated with radiation from multiple directions. The actual area receiving radiation treatment may be large or small, depending on the features of the cancer. Radiation can be delivered specifically to an organ or encompass the surrounding area, including the lymph nodes. Intensity Modulated Radiation Therapy (IMRT) IMRT is an advanced form of radiation therapy that allows doctors to customize the radiation dose by modulating, or varying, the amount of radiation given to different parts of the area being treated. The radiation intensity is adjusted with the use of computercontrolled, moveable “leaves” which either block or allow the passage of radiation from the many beams that are aimed at the treatment area. The leaves are carefully adjusted according to the shape, size, and location of the tumor. As a result, more radiation can be delivered to the tumor cells while less is directed at the normal cells that are nearby. An analogy for IMRT is a shower nozzle that shoots many different streams of water from different directions, except that each stream can be turned on or off, or set to deliver different intensities. This is unlike standard radiation techniques that allow only a constant flow of radiation from each beam. Image-guided Radiation Therapy (IGRT) IGRT is a new approach to delivering radiation therapy that allows for more accurate delivery of radiation to the target tissue. IGRT involves imaging during the course of radiation treatment. A computer compares images taken at the time of treatment to images taken during the planning phase. Through this process, IGRT is able to account for changes in the patient’s body or position that may shift the exact location of the cancer. This allows increased accuracy of very complex treatment approaches. It also provides documentation of the degree of accuracy. IGRT is used in conjunction with EBRT or IMRT. RAPIDARC Rapidarc is a new, state of the art treatment technology that allows patients to be treated much faster than standard radiation treatments. This technology treats patients while the machine rotates which reduces treatment times from 20 minutes down to 2 minutes. This can be used to treat pelvis, lung, and head and neck patients resulting in shorter, more accurate treatments. This technology is used in conjunction with IMRT and IGRT. Copyright©2008 CancerConsultants.com. All Rights Reserved. 50 RADIATION THERAPY QUESTIONS & ANSWERS, continued Brachytherapy Internal radiation is known by a number of names, including “brachytherapy,” “seeds,” or “implants.” These terms refer to treatment in which radioactive material is placed directly into or near the cancer. Brachytherapy may be used to provide an additional boost of radiation to an area also being treated with external radiation therapy, or may be used as the only type of radiation therapy. Brachytherapy may be permanent or temporary. In permanent brachytherapy, radioactive seeds are inserted and permanently left in place. After the procedure, the patient will temporarily contain a small amount of radiation from the seeds, although this amount is not generally dangerous to most other people. Some physicians may advise patients to avoid close contact with young children or pregnant women for several weeks. Over time, the radioactivity diminishes. In temporary brachytherapy, the radioactive material is inserted for a specified period of time and then removed before the patient goes home. Temporary brachytherapy may be administered at a lower dose over a longer period of time (low dose rate, or LDR) or a higher dose over a shorter period of time (high dose rate, or HDR). During LDR brachytherapy, patients are generally hospitalized for as long as the radioactive implants are in place (often two to three days). In contrast, it may be possible to receive HDR brachytherapy on an outpatient basis. Brachytherapy has proven to be useful in the treatment of several different types of cancer, including prostate, cervix, uterus, vagina, head and neck, and breast. Stereotactic Radiosurgery (SRS) Stereotactic Radiosurgery (SRS) allows non-invasive treatment of brain tumors, arteriovenous malformation, and other selected conditions. It is an outpatient treatment that delivers a high dose of radiation to a highly defined target. Treatments can be prescribed to deliver the total dose of radiation in a single treatment or in a fractionated manner up to 5 treatments. Cyberknife The latest most advanced technology in combating cancer with radiosurgery is now offered by the physicians at The START Center for Cancer Care. It is the Cyberknife, which gives patients a novel alternative in radiation. The Cyberknife delivers exact doses of radiation to tumors anywhere in the body, even tumors that are out of reach of other radiosurgery systems or traditional surgeries. If deemed a candidate for Cyberknife, patients undergoing this state of the art treatment: • • • Benefit from a painless, non-invasive procedure. Complete the treatments in fewer sessions than conventional radiotherapy. Benefit from no recovery or rehabilitation time. Copyright©2008 CancerConsultants.com. All Rights Reserved. 51 RADIATION THERAPY QUESTIONS & ANSWERS, continued • • • • Have the advantage of the maximum dose of radiation with sub-millimeter accuracy to the tumor without affecting healthy tissue. Have the benefit of treating multiple tumors in different locations during a single session. Have a reduction in infections, hemorrhage and loss of hearing and feeling, sometimes associated with conventional surgeries. Benefit from a convenient outpatient procedure. Xsight Lung is a new non-invasive technique to treat lung cancer using Cyberknife Radiosurgery. Lung tumors have been problematic for radiation oncologists because the tumors move as the patient breathes making it difficult to localize the tumor. Previously, Cyberknife has overcome this by following the location of a metal marker seed that is surgically placed in the tumor. Cyberknife used imaging technology to determine the location of the marker and then the Cyberknife machine would move as the marker seed moved. However, the insertion of the marker seed has some inherent risks. Xsight Lung is a significant advance in the treatment of lung cancer because it allows the Cyberknife unit to follow the tumor without using a marker seed. This allows the physicians to spare more of the healthy lung tissue without the additional risks inherent to the insertion of the marker seed. Copyright©2008 CancerConsultants.com. All Rights Reserved. 52 RADIATION THERAPY QUESTIONS & ANSWERS, continued What to Expect During Radiation Treatment Radiation treatment must be individualized for each patient depending on the size and location of their cancer. In order to tailor radiation treatment to meet the specific needs of individual patients, the radiation process involves several components, including consultation, simulation, treatment planning, and finally, the actual treatment. Consultation: The consultation is an important visit that allows both you and the radiation oncologist to gain more information. During the consultation, the radiation oncologist will obtain a medical history and perform a physical examination. Many patients find it helpful to prepare for the consultation by bringing x-rays, medical records, a list of medications, insurance information, and referral forms. During the consultation, the radiation oncologist may communicate a great deal of information in a short period of time. You may find it useful to prepare a list of questions prior to the consultation to assure they are all answered. You may also find it beneficial to bring another person to the consultation to help understand the information from the physician. After the consultation, the radiation oncologist may order additional tests, await results of other pending tests or consultations, or obtain additional records and reports. Multidisciplinary care is increasingly important for optimal cancer care, therefore the radiation oncologist will typically communicate with any other treating physicians to determine the appropriate course of treatment. In addition, the radiation oncologist will likely send a complete report of their evaluation to the referring physician and any other physicians requested by the patient. Once all of the necessary information has been gathered and the treatment team has communicated, a decision may be made to use radiation treatment. At this point, the radiation oncologist will discuss the treatment plan and alternatives with you and will present a consent form for you to sign prior to treatment. It is important to read and understand the consent form prior to signing it. CT Simulation: After the initial consultation and decision to use radiation treatment, the next session is usually a planning session, which is called a simulation. Simulation is used to determine the radiation treatment fields and most of the treatment planning. The CT simulator does not deliver radiation treatment, but instead allows the radiation oncologist and technologists to see the area to be treated. Images are obtained and transferred to the planning system where a virtual 3-dimensional image of the patient is created and the treatment delivery plan is developed. For the simulation session, temporary marks are made on your skin with magic markers to identify the treatment areas. The room is periodically darkened while the treatment fields are being set. Alignment is critical during simulation and is facilitated by lasers mounted on the wall and ceiling. Special individually constructed immobilization devices may be used to help achieve this alignment. While you may see red lines of light, the low energy lasers are for alignment purposes only and you will not feel burning or anything else from the laser light. Copyright©2008 CancerConsultants.com. All Rights Reserved. 53 RADIATION THERAPY QUESTIONS & ANSWERS, continued In most centers, the patient is given multiple “tattoos,” which mark the treatment fields and replace the marks previously made with magic markers. These tattoos are not elaborate and consist of no more than pinpricks followed by ink, appearing like a small freckle. Tattoos enable the radiation technologists to set up the treatment fields each day with precision, while allowing you to wash and bathe without worrying about obscuring the marks that indicate where treatment will be delivered. Sometimes several simulation sessions are necessary in order to optimize treatment and are often performed prior to planned “boost” or “reduced field” treatments as part of the overall treatment plan. Treatment planning: Several steps occur after simulation and prior to treatment; however, you do not need to be present during most of these procedures. During treatment planning, the dosimetrists perform special calculations to help assure that the proper radiation dose will be delivered. Computerized treatment planning may facilitate these calculations. Computers have become extremely sophisticated in planning radiation therapy delivery. Computers are even capable of extremely complex three-dimensional representation of the treatment area and surrounding normal tissues. It may take several days for treatment planning to be completed after simulation and prior to treatment. After all treatment planning is complete, radiation therapy treatments are ready to begin. Radiation treatment: Radiation treatment is usually given in another room separate from the simulation room. The treatment plans and treatment fields that result from the simulation session are transferred over to the treatment room, which contains a linear accelerator focused on a patient table similar to the one in the simulation room. The treatment plan is verified and treatment started only after the radiation oncologist and technologists have rechecked the treatment field and calculations, and are thoroughly satisfied with the “setup”. During radiation treatment, you must lie very still on the treatment table while the radiation beam is targeted to the exact area of the tumor. The machine and treatment table may rotate up to 360 degrees if the treatment requires the radiation to hit the tumor from all angles. The technologists will not be in the room during the treatment, but they will be monitoring the treatment via a video camera and an audio connection with the treatment room. You will not feel the radiation as it is being delivered. Radiation therapy is generally given once a day, five days a week, usually at the same time each day. Occasionally, treatment is given less frequently or twice a day. The number of treatments depends on multiple factors and varies from 5-10 to 40 or more, which means that treatment may last anywhere from one to eight weeks or more. Radiation treatments are generally given as outpatient treatments and involve relatively little time each day. While the first few visits might last for an hour or more, typically a daily radiation treatment will take about 15-30 minutes in the treatment room and the actual treatment only lasts a few minutes. It is important not to miss treatments. Extending treatments beyond the recommended time period may reduce the chance of controlling the cancer. Copyright©2008 CancerConsultants.com. All Rights Reserved. 54 RADIATION THERAPY QUESTIONS & ANSWERS, continued Side Effects of Radiation Therapy Although patients do not feel anything during a radiation treatment, the effects of radiation gradually build up over time. Most patients have very few initial side effects; however, many patients experience fatigue as treatment continues. The vast majority of patients are able to complete radiation therapy without significant difficulty. Side effects and potential complications of radiation therapy are infrequent and, when they do occur, are typically limited to the areas that are receiving treatment with radiation. The chance of experiencing side effects, however, is highly variable. A dose that causes some discomfort in one patient may cause no side effects in other patients. If side effects occur, you should inform the technologists and radiation oncologist, because treatment is almost always available and effective. Side effects are usually temporary and resolve once the radiation is completed. The most common side effect of radiation are: • • Skin reaction Fatigue Side effects that commonly occur with radiation to the head and neck are: • • • • Mucositis Xerostomia Changed sense of taste and/or smell Hypothyroidism Other less common side effects are: • • • • • Hair loss Nausea/Vomiting Diarrhea Loss of appetite Low blood counts (myelosuppression) While not as common with the advent of modern radiation delivery techniques, side effects that may occur with radiation to the chest are: • • Lung fibrosis Heart complications In addition to the above temporary side effects, in certain cases, patients may develop long-term side effects, also called “late complications”, such as: • • Secondary cancers Hypothyroidism These long-term side effects are also less common with the advent of modern radiation techniques. Copyright©2008 CancerConsultants.com. All Rights Reserved. 55 RADIATION THERAPY QUESTIONS & ANSWERS, continued Most Common Side Effects of Radiation Therapy Skin reaction: A common side effect of radiation therapy is skin irritation in the area of the body that is being treated. The skin reaction can range from mild redness and dryness (similar to a sunburn) to severe peeling (desquamation) of the skin in some patients. The majority of skin reactions to radiation therapy go away a few weeks after treatment is completed. In some cases, the treated skin will remain slightly darker than it was before and it may continue to be more sensitive to sun exposure. It is important to notify your nurse or physician when your skin becomes irritated because redness and dryness can eventually progress to peeling with oozing of fluid in the area. They can suggest measures to relieve your discomfort and possibly minimize further irritation. There are effective topical medications for treatment of radiation induced skin irritation, as well as a number of precautions that may minimize skin irritation during radiation therapy, such as: • • • • • • • • • • • • • • • • Keep the treated area dry and free from irritation. Cornstarch, gently patted on with a powder puff, will keep the skin dry. Wash the skin in the treatment area only with mild soaps. Use a mild shampoo, such as baby shampoo, if the head is being treated. When using a towel, pat the area dry instead of rubbing. If you must shave in the treated area, use an electric razor to prevent cuts. Avoid using shaving lotions or scented creams. Do not use perfumes, deodorants, or makeup in the treated area. Avoid using heating pads or ice packs on the skin in the treated area. Wear loose-fitting clothing that does not rub on the skin in the treated area. Avoid harsh fabrics over the treatment area, such as wool, corduroy, or starched cloth. Lightweight cotton is recommended. Avoid sun exposure in the treated area. If you expect to be in the sun for more than a few minutes, wear protective clothing (such as a hat with a broad brim and shirt with long sleeves) and use a sunscreen. Ask your doctor or nurse about using sunscreen lotions of SPF 15 or higher. Check with your nurse or physician regarding the use of creams or lotions. Usually, samples of safe topical medications are available in the radiation clinic. Unless necessary, do not use adhesive tape, including band aids and paper tape on the treated area. Breast cancer patients should not use deodorant if the axilla is in the treatment field. Create your own non-irritating deodorant: 1/4 cup baking soda and 1/4 cup of corn starch mixed together and applied with cotton balls. Do not swim in salt water, lakes, pools, or ponds. Always report any discomforts or concerns to your nurse or doctor. Copyright©2008 CancerConsultants.com. All Rights Reserved. 56 RADIATION THERAPY QUESTIONS & ANSWERS, continued Fatigue: Fatigue is a feeling of tiredness, weariness, weakness, exhaustion, or a profound lack of energy. Fatigue is one of the most common side effects of radiation therapy. Patients are not restricted from normal activity during radiation therapy; however, they should balance normal activity with periods of rest. Fatigue is typically more severe 2-4 hours after treatment. The feeling of fatigue should wear off several weeks after the completion of radiation therapy. The following suggestions may help you manage fatigue resulting from radiation therapy: • • • • • • • • Limit your activities, if possible. Exercise each day to maintain your strength. Prepare meals ahead of time and freeze them. Use convenience foods that are ready to eat. Accept offers of help from friends and relatives. Drink three quarts of fluid each day to avoid the build-up of cellular waste products. Increase rest by getting more sleep at night and taking naps during the day. Try to eat even when you are tired. Sometimes a little food will increase energy. Side Effects Associated with Radiation Therapy to the Head and Neck Mucositis (sore mouth or throat): Radiation therapy that is delivered to the head and neck area may cause mucositis. Mucositis is inflammation of the lining of the mouth and throat, called the mucus membranes. When radiation is administered directly to or near the head and neck region, chest, abdomen, or anal-rectal regions, it may cause damage to the mucosal lining of the entire gastrointestinal tract. This results in inflammation and sloughing of the mucosal cells, causing pain and increasing the risk of infection. Patients who have a sore mouth or gums need to take special care of their teeth, as they are a primary site for infection and pain. These patients may need to utilize frequent oral hygienic measures and antiseptic mouthwashes. In addition, some patients find it helpful to rinse the mouth with water frequently in order to remove food and bacteria and promote healing. Patients with mucositis should also select foods that will not further irritate an already tender mouth, for example: • • • • • • • • • Choose soft foods that are easy to chew and swallow. Avoid foods that irritate the mouth such as citrus fruits and foods that are spicy, salty, rough, coarse, or dry. Cook foods until they are soft and tender. Cut foods into small pieces. Mix food with butter, thin gravies or sauces to make it easier to swallow. Puree food in a blender or food processor. Use a straw to drink liquids. Eat foods cold or at room temperature, as hot food can irritate a tender mouth. Use anesthetic lozenges and sprays to numb the mouth and throat long enough to eat meals. Copyright©2008 CancerConsultants.com. All Rights Reserved. 57 RADIATION THERAPY QUESTIONS & ANSWERS, continued Xerostomia (dry mouth): Radiation therapy that is delivered to the head and neck area may also result in xerostomia. Xerostomia is a chronic dry-mouth condition, which is caused by damage to the salivary glands as a result of radiation therapy. Xerostomia can have a negative effect on quality of life by greatly impairing a patient’s ability to speak, chew, swallow, and taste. Coping with a dry mouth can be difficult, but the following tips may help. • • • • • • • Try consuming sweet or tart foods or beverages, such as lemonade, to help your mouth produce saliva. (Avoid these, however, when experiencing a sore mouth or throat.) Suck on sugar-free, hard candy or popsicles or chew sugar-free gum; this may also help to produce more saliva. Eat soft and pureed foods that are easier to swallow. Keep lips moist with lip salves. Eat foods with sauces, gravies, and salad dressings to make them moist and easier to swallow. Sip water every few minutes to make swallowing and talking easier. If the dry mouth problem is severe, ask your physician or dentist about products that coat and protect the mouth and throat. Changed sense of taste and/or smell: Radiation therapy or cancer itself may cause a change of taste or smell that typically goes away once treatment is complete. Foods may have a bitter or metallic taste, or simply less taste. The following is a list of suggestions that may help to make food taste better. • • • • • • Stop eating foods that cause an unpleasant taste and choose foods that look and smell good to you. Serve foods at room temperature. Try using small amounts of flavorful seasonings. Try tart foods such as oranges or lemons that may have more taste (unless you are experiencing a sore mouth or throat). Marinate meat, chicken, or fish in sweet sauces. If red meat tastes or smells strange, switch to chicken, turkey, eggs, or dairy products. Copyright©2008 CancerConsultants.com. All Rights Reserved. 58 RADIATION THERAPY QUESTIONS & ANSWERS, continued Less Common Side Effects of Radiation Therapy Hair loss: Radiation therapy only causes hair loss in the area being treated. Hair loss typically begins 2-4 weeks after the initiation of treatments. Some individuals experience thinning of the hair, while others experience complete hair loss. Hair loss caused by radiation is temporary. Typically, regrowth of hair begins 6-8 weeks after completion of radiation therapy. The best way to deal with hair loss is to prepare for it before it happens. Your physician will inform you of your chances for hair loss before your treatments begin. Consider the following tips for coping with hair loss: • • • • • • • • • Get a short, stylish haircut prior to beginning radiation in order to prepare yourself for the change in your appearance. If considering a wig, see a wig stylist before radiation treatment begins so that the stylist can match a wig to your natural hair color and texture. Ask your doctor for a prescription for a wig, as some insurance companies will cover this cost. Once radiation treatments begin, use a mild shampoo, pat the hair dry, and comb the hair carefully, without tugging. Only use a hairdryer if necessary and keep it on a low heat setting. Avoid hair dyes, rollers, curling irons, or perms. Sleep on a satin pillowcase to avoid friction between hair and scalp. Consider scarves, turbans, or wigs. Some patients feel more in control if they shave their head completely, rather than dealing with the hair falling out. Nausea/vomiting: Sometimes radiation therapy causes nausea (feeling queasy or sick to your stomach) and/or vomiting (throwing up), especially when the radiation is delivered to the abdominal area. Nausea/vomiting can happen immediately after radiation, can be delayed, or can occur in anticipation of receiving treatment. Several drugs, called antiemetics, are FDA approved for the prevention of nausea and vomiting. If you do experience nausea immediately after radiation, you may find it helpful to refrain from eating several hours prior to the treatment and for 1-2 hours afterward. In contrast, if you experience anticipatory nausea, it might be helpful to eat a bland snack, such as toast or crackers, before treatment. The following is a list of suggestions for coping with nausea: • • • • • • • • • Eat small meals. Eat and drink slowly. Eat often. Avoid foods that are fried or high in fat. Drink cool liquids between meals. Eat foods that have only a mild aroma and that can be served cool or at room temperature. Stick to any special diet that your doctor or dietician gives you. For a severely upset stomach, try a clear liquid diet (broth and juices) or bland foods that are easy to digest, such as dry toast and gelatin. If nausea/vomiting persists, your physician can prescribe an antiemetic to prevent nausea. Copyright©2008 CancerConsultants.com. All Rights Reserved. 59 RADIATION THERAPY QUESTIONS & ANSWERS, continued Diarrhea: Radiation treatment that is delivered to the abdominal area can cause diarrhea, which usually begins in the third or fourth week of radiation therapy. Your physician may recommend that you change your diet and/or prescribe medicine to help with the diarrhea. The following may help you manage diarrhea: • • • • • As soon as diarrhea starts, switch to a clear liquid diet. Avoid foods that are high in fiber or can cause cramps or a gassy feeling (raw vegetables, coffee, beans, cabbage, spicy food). Eat small, frequent meals. Avoid dairy products. Eat foods that are high in potassium, such as bananas, potatoes, and apricots, because diarrhea causes potassium loss. Loss of appetite: Loss of appetite is a common factor with cancer and its treatment. Nausea, vomiting, and depression can contribute to a loss of appetite. While you may not want to eat, it is important to maintain proper nutrition throughout treatment. The following suggestions may help you maintain your nutritional intake: • • • • • Eat whenever you are hungry. Several smaller meals throughout the day might be more appropriate than three larger meals. Eat often. Taking just a few bites of food every hour can ensure that you get more protein and calories. Have a calm, relaxed mealtime. Add variety to your menu. Create a calm and appealing ambiance with music, candles, and friends. Low blood counts (myelosuppression): Blood counts, or the number of blood cells in circulation, can be affected by radiation therapy. Many radiation therapy institutions make it a policy to check the blood counts at least once during the radiation treatments. Low blood counts may cause changes in sleep or rest patterns during the radiation therapy period and some patients describe a sense of tiredness and fatigue. Notify your nurse or doctor if you experience any of these symptoms because treatment is available for low blood counts. Other less common side effects may occur in certain situations and will be discussed with you as appropriate. Copyright©2008 CancerConsultants.com. All Rights Reserved. 60 RADIATION THERAPY QUESTIONS & ANSWERS, continued Possible Side Effects with Radiation to the Chest Lung fibrosis: Lung fibrosis is scarring of the lung tissue and causes difficulty breathing. Fibrosis can be a significant long-term (late) complication following radiation treatment for Hodgkin’s disease and other cancers requiring radiation to the lungs. However, this decrease in lung function appears to improve over time and is thought to be reversible. Heart complications: Heart disease is also a late complication of radiation to the middle portion of the torso, called the mediastinum. The risk of heart disease increases with higher radiation doses and larger field sizes. Possible Long-Term Side Effects of Radiation Therapy Secondary cancers: A second cancer can be induced by cancer treatment, including radiation, chemotherapy, or the combination of radiation and chemotherapy. Treatment for Hodgkin’s lymphoma at a young age will ultimately result in a higher incidence of second cancers. Hypothyroidism: Hypothyroidism (abnormally low levels of thyroid hormone) is one of the more frequently encountered late complications of radiation therapy in patients where the radiation field includes the neck. This may occur in up to one-third of patients receiving radiation therapy. It is important for patients who have received radiation therapy to be tested on a regular basis because signs and symptoms of hypothyroidism occur very late and are subtle. Copyright©2008 CancerConsultants.com. All Rights Reserved. 61 RADIATION THERAPY QUESTIONS & ANSWERS, continued Prevention and Management of Radiation Side Effects There are several methods being utilized for the prevention of radiation therapy side effects. These mainly include altering the manner in which radiation is delivered and administering drugs that protect normal cells from radiation damage. Radiation Delivery Methods Two delivery methods that were originally used to reduce radiation side effects include dose fractionation, or splitting the total dose of radiation therapy into multiple doses and physical shielding with lead blocks to reduce the area of exposure. Fractionation and hyperfractionation: Radiation therapy was originally given in one large dose. More than a half-century ago it was found that it was less toxic and more effective to administer radiation on a daily basis, a method called dose fractionation. Fractionation allows the delivery of a larger total dose of radiation to the cancer than would have been possible as a single dose. Currently, most radiation treatments are administered daily, 5 days a week. The 5 days per week is strictly for the convenience of maintaining a normal work week. The 24-hour interval and the two-day interval between doses allows for recovery of normal tissues between doses while cancer cells, in general, have less capability for recovery. There is no doubt that using fractionation has reduced side effects compared to single-dose delivery. While cancer cells tend to be less resilient than normal tissues, there is a chance that the intervals between fractionated doses of radiation may allow cancer cells to recover. Recent findings indicate that some cancers are best treated by reducing the 24-hour interval between doses to 6-8 hours, in order to enhance the toxic effects on cancer cells, while still preserving an adequate time interval for the recovery of normal cells. This technique, called hyperfractionation, is being widely used to treat a variety of cancers. Hyperfractionation requires sophisticated equipment and therefore it is important for patients to be treated at specialty medical centers that have experience and staff trained in this technique. Intensity modulated radiation therapy (IMRT): IMRT delivers varying intensity of radiation with a rotating device. The intensity is varied by the placement of “leaves,” which either block or allow the passage of radiation. The rotating component of this technique allows for more specific targeting of the cancer, sparing normal tissues from damage due to radiation exposure. In conventional radiation therapy, the beam is usually delivered from several different directions, possibly 5-10. The greater the number of beam directions, the more the dose will be confined to the target cancer cells, sparing normal cells from exposure. IMRT delivers radiation from every point on a helix, or spiral, in contrast to only a few points. Copyright©2008 CancerConsultants.com. All Rights Reserved. 62 RADIATION THERAPY QUESTIONS & ANSWERS, continued Three-dimensional conformal radiation: Three-dimensional conformal radiation therapy is a promising approach for the treatment of some cancers with decreased toxicity to normal tissues. Using computerized tomography (CT) scans and other scans, radiation oncologists have developed methods for determining the tumor size and shape in 3 dimensions. This allows high-dose external beam radiation therapy to be delivered primarily to the cancer with less damage to normal cells. For example, three-dimensional conformal radiation has allowed radiation oncologists to reduce the amount of radiation to the breast by 50%, which should decrease the risk of secondary breast cancer. It is important for conformal radiation to be administered at special cancer centers with sophisticated equipment and trained staff. Drug Therapy While preventing radiation side effects from occurring is the ideal approach to management, sometimes side effects are inevitable. In these situations, several types of drugs can be used to decrease the side effects of radiation. Drug therapies for radiationinduced side effects fall into two categories: � Those that protect the non-cancerous tissue from radiation damage through systemic administration. � Those that are applied topically to mucus membranes to decrease or treat radiation damage. Radiation protectors: Radioprotectants are drugs that selectively protect normal cells, but not cancer cells, from the effects of radiation. Over the past 50 years, many radiation protectors have been tested in laboratories to determine their efficacy in preventing radiation damage to normal cells and tissues. Ethyol®: Ethyol® is a radiation protector and the only drug that has been approved by the FDA for xerostomia (dry mouth) in patients receiving radiation therapy for cancers of the head and neck. Xerostomia is a chronic dry-mouth condition, which is caused by damage from radiation therapy to the salivary glands. Xerostomia can greatly impair a patient’s ability to speak, chew, swallow and taste and therefore, can have a negative effect on a patient’s quality of life. Results from a clinical trial indicated that the incidence of severe xerostomia for patients receiving Ethyol® was 51%, compared to 78% for patients receiving radiation therapy alone. One year following completion of radiation therapy, only 35% of patients who had received Ethyol® were still experiencing symptoms of xerostomia, whereas 57% of patients who had received radiation therapy alone were still experiencing symptoms. Steroids: Steroids are naturally occurring hormones produced by the adrenal glands. As part of your radiation therapy treatment, your physician may prescribe steroids such as Prednisone® or Decadron® (generic name is dexamethasone). These drugs help decrease swelling in body tissues. Dexamethasone has also been shown to prevent radiationinduced vomiting, especially in treatment of cancers of the abdomen. Copyright©2008 CancerConsultants.com. All Rights Reserved. 63 RADIATION THERAPY QUESTIONS & ANSWERS, continued Topical agents: Some drugs can be applied topically to mucus membranes to decrease or treat radiation damage. The topical agent sucralfate may protect mucus membranes by several mechanisms and is often used during and after radiation therapy for the prevention and treatment of mucositis (mouth sores). Topical antiseptics, such as chlorhexidine or benzydamine, have been used for the prevention of mucositis, but recent research indicates that these are not effective. In a Mayo Clinic study involving 52 patients with head and neck cancers who received radiation therapy, chlorhexidine was found to be more toxic, and no more effective than placebo in the prevention of mucositis. German researchers reported that chlorhexidine mouthwashes were not effective in treating mucositis in patients with a low white blood cell count. Despite a significant decrease in the aerobic and anaerobic bacterial flora on the oral mucous membranes, the risk of mucositis seemed to be enhanced. The patients treated with chlorhexidine seemed to have more problems with inflammation, resulting in mucositis. Strategies to Improve Prevention and Management of Radiation Side Effects The development of more effective cancer treatments requires that new and innovative therapies be evaluated with cancer patients. Clinical trials are studies that evaluate the effectiveness of new drugs or treatment strategies. Future progress in the prevention and management of radiation side effects will result from the continued evaluation of new treatments in clinical trials. Participation in a clinical trial may offer patients access to better treatments and advance the existing knowledge about treatment of this cancer. Patients who are interested in participating in a clinical trial should discuss the risks and benefits of clinical trials with their physician. Areas of active investigation aimed at improving the prevention and management of radiation side effects include the following: • • • • Keratinocyte growth factor (KGF, palifermin) Antioxidants Interleukin 11 Prostaglandins Keratinocyte growth factor (KGF, palifermin): This is a growth factor that has been shown to stimulate growth of epithelial cells, which make up the mucus membrane and line the mouth and throat. Keratinocyte growth factor is currently being tested in patients to prevent chemotherapy damage to the mucus membranes of the gastrointestinal tract. Antioxidants: The antioxidant agent Cu/Zn superoxide dismutase (SOD) has shown promise in reducing early and late radiation-induced tissue injury. In one clinical trial, 448 patients with bladder cancer were randomly allocated to receive either SOD or placebo after each radiation treatment. The patients who received SOD experienced fewer rectal problems and less bladder inflammation and skin toxicity than those who received placebo. Copyright©2008 CancerConsultants.com. All Rights Reserved. 64 RADIATION THERAPY QUESTIONS & ANSWERS, continued Interleukin 11: Interleukin 11 is a growth factor that is similar but not identical to what the body normally produces. Interleukin 11 has been approved by the FDA to stimulate platelet recovery in patients with low platelet counts due to chemotherapy. Clinical trials are currently underway to determine if Interleukin 11 will prevent side effects, especially to the mucus membranes and gastrointestinal tract, associated with chemotherapy and radiation therapy. Prostaglandins: Prostoglandins are a group of compounds that affect the healing of inflammation and wounds. Misoprostol is a prostaglandin that is effective in treating complications that arise in patients with prostate cancer who receive radiation treatment. Inflammation of the rectum (radiation proctitis) is a known complication of radiation therapy in the treatment of prostate cancer. Available medical treatment is usually ineffective and has focused on relieving symptoms after damage has occurred. One clinical study evaluated the effects of misoprostol in patients undergoing radiation therapy treatment for prostate cancer. In the study, nine patients received misoprostol rectal suppositories and seven patients received placebo. The results indicated that misoprostol rectal suppositories significantly reduced acute and chronic radiation proctitis symptoms in patients receiving radiation therapy for prostate cancer. References 1. Brizel DM, Wasserman TH, Henke M, et al. Phase III Randomized Trial of Amifostine as a Radioprotector in Head and Neck Cancer. J Clin Oncol 2000;18:3339-3345. 2. Sanchiz F, Milla A, Artola N, Julia JC, et al. Prevention of radioinduced cystitis by orgotein: a randomized study. Anticancer Res 1996;16(4A):2025-8. 3. Foote RL, Loprinzi CL, Frank AR, et al. Randomized Trial of Chlorhexidine Mouthwash for Alleviation of Radiation InducedMucositis. J Clin Oncol 1994;12:2630-2633. 4. Pitten FA, Kiefer T, Buth C, et al. Do cancer patients with chemotherapy-induced leukopenia benefit from an antiseptic chlorhexidine-based oral rinse? A double-blind, block-randomized, controlled study. J Hosp Infect 2003;53:283-91. 5. Khan AM, Birk JW, Anderson JC, Georgsson M, et al. A prospective randomized placebo-controlled double-blinded pilot study of misoprostol rectal suppositories in the prevention of acute and chronic radiation proctitis symptoms in prostate cancer patients. Am J Gastroenterol 2000;95(8):1961-6. Copyright©2008 CancerConsultants.com. All Rights Reserved. 65 RADIATION THERAPY QUESTIONS & ANSWERS, continued Radiation Therapy FAQs What is radiation therapy? Radiation therapy, or radiotherapy, is the treatment of cancer and other diseases using ionizing radiation. This radiation can be delivered externally or internally. How does radiation work? Radiation therapy works by damaging the DNA in the cancer cell, thereby disabling the cancer cell from reproducing and growing. The cancer cells then die and the cancer shrinks. Will I feel the radiation or will it hurt? No, external beam radiation treatments are painless, like having an x-ray taken. Although radiation therapy is not painful, it can cause unwanted side effects. The skin where radiation is aimed may feel like it has been sunburned and will need to be protected from the sun. Will I become radioactive? External beam radiation does not cause you to become radioactive, and you pose no risk of radiation exposure to people near you. If you have a radioactive implant in place, some visitors, such as pregnant women and small children, will not be allowed to get too close and visiting time may be limited or restricted until the implant is removed. Your doctor or nurse will tell you when these precautions are necessary. Are there risks involved with radiation therapy? The radiation used to damage or destroy cancer cells can also damage normal cells. When this happens, you may experience side effects. However, the risk of side effects is usually outweighed by the benefits of killing cancer cells. Any side effects will be carefully monitored by the radiation oncologist. What should I know about the risks of radiation therapy? The risks, problems, and side effects that can occur with radiation therapy depend on the type and the dose and the part of the body that is being treated. Radiation that involves the abdomen may cause diarrhea; radiation involving the head and neck can cause mouth sores. The most common side effects of radiation are fatigue, mouth sores, and skin problems. Before your treatments, your doctor will explain ways to help prevent or reduce potential side effects. What are the typical side effects of radiation therapy? The most common side effects of radiation therapy reported by patients are fatigue and skin irritation at the site of treatment. Other side effects depend on the area of the body being treated and the dosage being given, such as: • • • Dry or sore mouth or throat may occur when treatment is being given in the mouth, throat or neck area. Some coughing and excess mucus production may occur if treatment is given to the lung area. Mild nausea and/or diarrhea may occur if treatment involves the abdominal area. Copyright©2008 CancerConsultants.com. All Rights Reserved. 66 RADIATION THERAPY QUESTIONS & ANSWERS, continued Most of these side effects will go away on their own within 4 to 6 weeks after treatment is completed. Some long-term effects may include changes in the color and elasticity of skin in the treatment area. Discuss any concerns you may have about side effects and ask about medications to counteract them with the radiation oncologist before the start of your treatment. Will the radiation therapy make me sick? Most patients do not experience any nausea with radiation therapy, unless the area being treated with radiation is around the stomach. If you experience nausea, report this and any other symptoms to your doctor. Effective medications exist to reduce and/ or prevent your symptoms. Will I lose my hair? No, you will not lose the hair on your head unless that is the area being treated. Hair loss only occurs in the area that is being treated with radiation therapy. For instance, if the area being treated is your arm, you can expect to lose the hair on that arm during the treatment. How long will my radiation treatment take? Most of the time, external beam radiation is delivered in daily treatments, or fractions, over a period of 5 to 7 weeks. The patient will generally receive these treatments Monday through Friday, and then have the weekend off. A daily fraction will take about 15-30 minutes in the treatment room; however, the actual treatment only lasts a few minutes. Who will administer my radiation treatments? A doctor who specializes in radiation therapy is called a radiation oncologist. The radiation oncologist will prescribe the type and amount of radiation treatment that is appropriate and work closely with a team of healthcare professionals in determining the best way to deliver that treatment. Those healthcare professionals may include the following: • • • • Radiation physicists are experts who make sure the machines are working properly and that they deliver accurate radiation doses. The physicist also works closely with the doctor in planning your treatment. Dosimetrists are specialists who work with the doctor and physicist to create the treatment plan and calculate the radiation dose delivered to the tumor and the surrounding normal tissues. Radiation therapists are professionals who position you and operate the machines to deliver the radiation treatment on the linear accelerator. Radiation oncology nurses are caregivers who will help coordinate your care, manage side effects, and help you and your family learn about your treatment. Can someone come to my treatments with me? Friends or family are welcome to accompany you to your treatments. However, federal regulations prohibit anyone who is not a patient or a person wearing a film badge monitor to be in the radiation controlled area during the time radiation equipment is being operated. Those accompanying you will likely be asked to wait in the reception area during the treatment. This also serves to protect the privacy of other patients. Only patients and staff are allowed in the treatment area during treatment hours. Copyright©2008 CancerConsultants.com. All Rights Reserved. 67 RADIATION THERAPY QUESTIONS & ANSWERS, continued Can I continue my regular routine/activities while undergoing radiation treatments? You should continue with your normal routines. Most patients continue full-time occupations or leisure activities through the course of treatments. When you feel tired, do not over exert yourself; take time to rest when needed. Try to get plenty of sleep and maintain a healthy diet. Will I be alone during my treatments? Because radiation effects are accumulated and radiation therapists treat many patients each day, it would be a long-term health risk for them to be in the room during the radiation treatments. To ensure that you are okay and your treatment delivery is going well, you will be in voice contact with your radiation therapists and constantly monitored by a video camera. If you should need assistance, simply tell the therapists and they will terminate the treatment and immediately tend to your needs. What cancers are treated with brachytherapy? Brachytherapy is used predominantly to treat early stage prostate cancer; however, it may also be used in breast, cervical, head and neck, and other cancers. What is involved in the implantation of a radioactive seed into the prostate (brachytherapy)? For most of these patients, radioactive seed implantation into the prostate is a one-time, non-surgical, low-impact procedure. Radioactive seed implantation into the prostate is typically performed in an outpatient hospital setting by a team of physicians consisting of a urologist, radiation oncologist, and a radiation physicist. Spinal anesthesia is typically performed, but general anesthesia may occasionally be utilized. Some centers perform this procedure in their hospital operating rooms. Both outpatient and inpatient settings are acceptable. Most patients can return to normal activity, including work, within one to three days, with little or no pain. Will radioactive seeds be painful? After the implantation of radioactive seeds into the prostate, there typically is some soreness underneath the scrotum. Occasionally patients describe feeling like they are “sitting on a golf ball”. This is due to the slight swelling and bleeding associated with the surgery. It gradually resolves. Most patients require only mild analgesics like acetaminophen (Tylenol®). Narcotic pain medications are rarely required. How soon after implantation of radioactive seeds into the prostate can I resume exercise or other vigorous activities? The insertion of the needles causes some trauma to the vessels surrounding the prostate. Therefore, immediately after the implant, any exercise or activity that puts pressure on the prostate should be avoided. You should avoid lifting heavy objects or doing vigorous exercise for at least three to four days after the implant. Very vigorous exercise after this period may cause some minor bleeding in the bladder. This is not harmful, but you should limit your exercise until the bleeding stops. Activities such as bike riding, horseback riding, motorcycle riding in which there is pressure on the prostate should be avoided for at least six months. The repetitious jarring of the prostate with these activities can cause some swelling and impair urination. Copyright©2008 CancerConsultants.com. All Rights Reserved. 68 RADIATION THERAPY QUESTIONS & ANSWERS, continued Will I be radioactive after the seed implantation? Yes, but the radiation is confined to the area of the implant. Although the seeds are radioactive, patients are not. Because the radioactivity is so low and the placement is so precise, virtually all the radioactivity is absorbed into the prostate. However, special precautions should be taken when a patient is in contact with small children and pregnant women in the first two months after treatment. You nurse or doctor will advise you what precautions are necessary and when. Does the radiation from seed implants pose any danger to my sexual partner? No, the seeds are of low energy and pose little risk to your partner. The semen is not radioactive. You may resume sexual activity very soon after the procedure. Occasionally, there may be blood in the semen or some slight pain at climax. Copyright©2008 CancerConsultants.com. All Rights Reserved. 69 70 GLOSSARY GLOSSARY GLOSSARY Definitions & Phonetic Pronunciations A APC gene: a gene that slows the growth of cells in the body. Changes in this gene can cause familial adenomatous polyposis (FAP) and Gardner syndrome. People who have a mutation in this gene can develop hundreds of polyps in the colon. See also Gardner syndrome, familial adenomatous polyposis. abdomen (ab-duh-men): the part of the body between the chest and the pelvis. It contains the stomach (with the lower part of the esophagus), small and large intestines, liver, gallbladder, spleen, pancreas, and other organs. The abdomen is lined by a membrane called the peritoneum. ablative (ab-lay-tive) therapy: treatment that removes or destroys the function of an organ. For example, removing the ovaries or testicles or taking medicines that cause them to stop making the hormones which help some types of cancer grow. abscess (ab-ses): a collection of pus in tissues, organs, or other parts of the body. adenocarcinoma (ad-no-kar-suh-NO-muh): cancer that starts in the glandular tissue, such as in the ducts or lobules of the breast. adenoma (add-no-muh): a benign (non-cancerous) growth starting in the glandular tissue. adhesions (ad-hee-zhunz): scar tissue that forms after surgery. If it tightens, it may bind together organs that are normally separate. This can sometimes cause partial or total blockage of the intestine. adjuvant (ad-juh-vunt) therapy: treatment used in addition to the main treatment. It usually refers to hormonal therapy, chemotherapy, radiation therapy, or immunotherapy added after surgery to increase the chances of curing the disease or keeping it in check. adrenal gland (uh-dree-nul): one adrenal gland is located at the top of each kidney. Its main function is to make hormones which control metabolism, fluid balance, and blood pressure. It also makes small amounts of “male” hormones (androgens) and “female” hormones (estrogens and progesterone). advance directives: legal documents that tell the doctor and family what a person wants for future medical care in the event that the patient becomes unable to make decisions for him or herself. This may include whether to start or when to stop life-sustaining treatments. Another type of advance directive lets you choose a person to make decisions for you later if you become unable to do it for yourself. See living will and health care power of attorney. advanced cancer: a general term describing stages of cancer in which the disease has spread from where it started (the primary site) to other parts of the body. When the cancer has spread only to the nearby areas, it is called locally advanced cancer. If it has spread to distant parts of the body, it is called metastatic cancer. 71 G L O S S A R Y, c o n t i n u e d AJCC Staging System: American Joint Committee on Cancer staging system (also called the TNM system), which describes the extent of a cancer’s spread in Roman numerals from 0 through IV. See also staging. allogeneic (al-o-jen-nay-ick) bone marrow transplant: uses marrow from a donor whose tissue type closely matches the patient’s. This can be from a related donor or an unrelated donor. See also stem cell transplant. alopecia (al-o-PEE-shuh): hair loss. This often happens with chemotherapy treatment or radiation therapy to the head. In most cases, the hair grows back after treatment ends. alveoli (al-vee-o-lie): air sacs of the lungs. alternative therapy: an unproven therapy that is recommended instead of standard (proven) medical treatment. Some alternative therapies have dangerous or even life-threatening side effects. With others, the main danger is that the patient may lose the chance to benefit from standard treatment. The American Cancer Society recommends that patients thinking about using any alternative or complementary therapy discuss it first with a member of their health care team. See also complementary therapy. Amsterdam criteria (am-stir-dam cry-teer-ee-uh): a set of conditions common in people with hereditary non-polyposis colon cancer (HNPCC). Only about 60% of people who meet all of the criteria actually have HNPCC, but people who meet the criteria may want to consider genetic testing for it. Compare to Bethesda criteria. See also hereditary nonpolyposis colon cancer. anastomosis (uh-nas-tuh-MO-sis): the site where 2 structures are surgically joined together. androgen (an-dro-jen): any male sex hormone. The major androgen is testosterone. androgen blockade: use of drugs to disrupt the actions of male hormones. anecdotal (an-neck-doe-tul): individual or personal report, an incomplete description from one or more patients. anemia (uh-neem-ee-uh): low red blood cell count. anesthesia (an-es-thee-zhuh): the loss of feeling or sensation as a result of drugs or gases. General anesthesia causes loss of consciousness (“puts you into a deep sleep”). Local or regional anesthesia numbs only a certain area. anesthesiologist (an-es-thee-zee-AHL-uh-jist): a doctor who specializes in giving medicines or other agents that prevent or relieve pain, especially during surgery. aneuploid (an-you-ploid): See ploidy. angiogenesis (an-jee-o-JEN-uh-sis): the formation of new blood vessels. Some cancer treatments work by blocking angiogenesis, thus preventing blood from reaching the tumor. angiography (an-jee-AH-gruf fee): a test in which a contrast dye is injected directly into a blood vessel that goes to the area that is being studied. A series of x-ray images are then taken to show surgeons the location of blood vessels around a tumor. 72 G L O S S A R Y, c o n t i n u e d anorexia (an-uh-rek-see-uh): loss of appetite; may be caused by either the cancer itself or as a side effect of treatments such as chemotherapy. anterior (an-teer-ee-yer): at or near the front. antibiotic: drugs used to kill micro-organisms that cause disease. Antibiotics may be made naturally by living organisms or they may be created in the lab. Since some cancer treatments can reduce the body’s ability to fight off infection, antibiotics may be used to treat or prevent these infections. antibody: a protein produced by immune system cells and released into the blood. Antibodies defend the body against foreign agents, such as bacteria. These agents contain certain substances called antigens. Each antibody works against a specific antigen. See also antigen. anti-emetic (an-tie-eh-MEH-tik): a drug that prevents or relieves nausea and vomiting, common side effects of chemotherapy. anti-estrogen (an-tie-ess-tro-jen): a substance (for example, the drug tamoxifen) that blocks the effects of estrogen on tumors. Antiestrogens are used to treat breast cancers that depend on estrogen for growth. antigen (an-tuh-jen): a substance that causes the body’s immune system to respond. This response often involves making antibodies. For example, the immune system’s response to antigens that are part of bacteria and viruses helps people resist infections. Cancer cells have certain antigens that can be found by lab tests. They are important in cancer diagnosis and in watching response to treatment. Other cancer cell antigens play a role in immune reactions that may help the body’s resistance against cancer. antimetabolites (an-tie-muh-TAB-o-lites): substances that interfere with the body’s chemical processes, such as those that create proteins, DNA, and other chemicals needed for cell growth and reproduction. In treating cancer, antimetabolite drugs disrupt DNA production, which in turn prevents cell division and growth of tumors. See also DNA. antioxidants (an-tie-OX-uh-dunts): compounds that hold back chemical reactions with oxygen (oxidation). Some vitamins, such as vitamins C and E and beta-carotene are antioxidants. Antioxidants that are found in foods are thought to reduce the risk of some cancers. However, use of certain antioxidants supplements has been linked to higher cancer risk in some people. apheresis (a-fur-REE-sis) or pheresis (fur-ree-sis): a procedure in which blood is taken, part of the blood is removed, and the rest of the blood is infused back into the donor. May be called plasmapheresis if plasma is removed, leukaphoresis if white blood cells are removed, or plateletpheresis when platelets are removed. apoptosis (a-pop-toe-sis): programmed cell death. Apoptosis is controlled by genes that cause a cell to die at a specific time, for example, when DNA is damaged. This type of cell death is different from the process of cell death by decay. Some drugs used to treat cancer cause apoptosis. aspiration (asp-er-A-shun): to draw out by suction. See also fine needle aspiration biopsy. 73 G L O S S A R Y, c o n t i n u e d asymptomatic (a-simp-tuh-MAT-ik): not having any symptoms of a disease. Many cancers can develop and grow without producing symptoms, especially in the early stages. Screening tests such as mammograms and colonoscopies help to find these early cancers before symptoms start, when the chances for cure are usually highest. See also screening. atypical (a-tip-uh-kul): not usual; abnormal. Also called atypia (a-tip-ee-yuh). Often refers to the appearance of cancerous or pre-cancerous cells. See also hyperplasia. autologous (aw-tahl-uh-gus) bone marrow transplant: a complex and sometimes risky treatment that may be used when cancer is advanced or has recurred, or as the main treatment in some types of leukemia or lymphoma. A portion of the patient’s bone marrow is removed, cleansed, treated, and stored. The patient is given high doses of chemotherapy to kill the cancer cells. The drugs also destroy the remaining bone marrow, thus robbing the body of its natural ability to fight infection. The cleansed marrow is then given by transfusion (transplanted) to restore the patient’s immune defenses. The best place to have a bone marrow transplant is at a comprehensive cancer center or other facility that has the technical skill and experience to perform it safely. Bone marrow transplants can also be received from a donor. See allogeneic bone marrow transplant. See also stem cell transplant. axilla (ax-ill-uh): the armpit. axillary (ax-ill-air-ee) dissection: removal of the lymph nodes in the armpit (axillary nodes). They are looked at under a microscope to see if they contain cancer. B BPH: see benign prostatic hyperplasia. BRCA1: a gene which, when damaged (mutated), places a woman at much greater risk of developing breast and/or ovarian cancer, compared with women who do not have the mutation. BRCA2: a gene which, when damaged or mutated, puts the woman at a much higher risk for developing breast cancer and/or ovarian cancer than the general population. barium enema (bear-ee-um en-uh-muh): a method used to help diagnose colorectal cancer. Barium sulfate, a chalky substance, is used to enlarge and partly fill the colon. When the colon is about half-full of barium, air is pushed in to cause the colon to expand further. This allows good x-ray films to be taken. Also called a double contrast barium enema. basal cell carcinoma: the most common type of skin cancer. It begins in the lowest layer of the epidermis, called the basal cell layer. It usually develops on sun-exposed areas, especially the head and neck. Basal cell cancer grows slowly and is not likely to spread to distant parts of the body. basic science: lab studies that are not aimed at specific problems, but that provide the knowledge and background required for later applied research. behavioral research: research into what motivates people to act as they do. The results of such research can be used to help encourage people to adopt healthy lifestyles and follow life-saving screening and treatment guidelines. 74 G L O S S A R Y, c o n t i n u e d benign (be-nine): not cancer; not malignant. benign tumor: an abnormal growth that is not cancer and does not spread to other areas of the body. benign prostatic hyperplasia (be-nine pros-tat-tick hi-per-PLAY-zhuh): non-cancerous enlargement of the prostate that may cause problems with urination such as trouble starting and stopping the flow. Also referred to as BPH. beta carotene: a form of vitamin A that is found mainly in yellow and orange vegetables and fruits. It functions as an antioxidant and may play a role in cancer prevention. However, high doses of beta carotene supplements in smokers may increase lung cancer risk. Bethesda criteria (beth-ez-duh cry-teer-ree-yuh): a set of conditions that are common in people with hereditary non-polyposis colon cancer (HNPCC). Most people who meet these criteria actually do not have HNPCC, but may want to consider further testing for it. Compare to Amsterdam criteria. See also hereditary non-polyposis colon cancer. bilateral (bi-lat-er-ul): on both sides of the body; for example, bilateral breast cancer is cancer in both breasts. Compare to unilateral. biologic response modifiers: substances that boost the body’s immune system to fight against cancer; interferon is one example. Also called biologic therapy. biomarkers: see tumor markers. biopsy (by-op-see): the removal of a sample of tissue to see whether cancer cells are present. There are several kinds of biopsies. In some, a very thin needle is used to draw fluid and cells from a lump. In a core biopsy, a larger needle is used to remove more tissue. bladder: a hollow organ in the pelvis with flexible, muscular walls. The bladder stores urine as it is produced by the kidneys. blood count: a count of the number of red blood cells and white blood cells in a given sample of blood. B-lymphocytes (limf-o-sites) or B-cells: white blood cells that are help make antibodies. bone marrow: the soft, spongy tissue in the hollow middle of flat bones of the body where new blood cells are made. bone marrow aspiration and biopsy: a procedure in which a needle is placed into the cavity of a bone, usually the hip or breast bone, to remove a small amount of bone marrow so that it can be looked at under a microscope. bone marrow transplant: a treatment that restores blood-forming stem cells that have been destroyed by high doses of chemotherapy and/or radiation therapy. The bone marrow may come from the patient (autologous) or a donor (allogeneic.) See autologous bone marrow transplant, allogeneic bone marrow transplant, and stem cell transplant. 75 G L O S S A R Y, c o n t i n u e d bone scan: an imaging method that gives important information about the bones, including the location of cancer that may have spread to the bones. It can be done on an outpatient basis and is painless, except for the needle stick when a low-dose radioactive substance is injected into a vein. Pictures are taken to see where the radioactivity collects, pointing to an abnormality. bone survey (skeletal): an x-ray of all the bones of the body; often done when looking for cancer that has spread to the bones. brain scan: an imaging method used to find anything not normal in the brain, including brain cancer and cancer that has spread to the brain from other places in the body. This scan can be done in an outpatient clinic. It is painless, except for the needle stick when a radioactive substance is injected into a vein. The pictures taken will show where radioactivity collects, indicating an abnormality. brachytherapy (brake-ee-THER-uh-pee): internal radiation treatment given by placing radioactive seeds or pellets directly into the tumor or close to it. Also called interstitial radiation therapy or seed implantation. breast cancer: cancer that starts in the breast. The main types of breast cancer are ductal carcinoma in situ, invasive ductal carcinoma, lobular carcinoma in situ, invasive lobular carcinoma, medullary carcinoma, and Paget disease of the nipple (see definitions under these headings). Some breast specialists believe that lobular carcinoma in situ is not a true cancer. breast conservation therapy or breast-conserving therapy: surgery to remove a breast cancer and a small area of normal tissue around the cancer without removing any other part of the breast. The lymph nodes under the arm may be removed, and radiation therapy is also often given after the surgery. This method is also called lumpectomy, segmental excision, limited breast surgery, or tylectomy. breast implant: a sac used to increase breast size or restore the contour of a breast after mastectomy. The sac is filled with silicone gel (a synthetic material) or sterile saltwater (saline). breast reconstruction: surgery that rebuilds the breast contour after mastectomy. A breast implant or the woman’s own tissue is used. If desired, the nipple and areola may also be recreated. Reconstruction can be done at the time of mastectomy or any time later. breast self-exam (BSE): a way to check one’s own breasts for lumps or suspicious changes. Women over age 20 might choose to do BSE regularly, usually at a time other than the days before, during, or immediately after her menstrual period. bronchi (brong-ki): in the lungs, the 2 main air passages leading from the windpipe (trachea). The bronchi provide a passage for air to move in and out of the lungs. bronchiole (brong-key-ol): one of the smaller sub-divisions of the bronchi. bronchoscopy (brong-kos-kuh-pee): looking at the bronchi using a flexible, lighted tube called a bronchoscope. 76 G L O S S A R Y, c o n t i n u e d C CA 19-9: a tumor marker sometimes produced by colorectal, stomach, bile duct, and pancreatic cancers. It may also be produced in pancreatitis, liver disease, and other noncancer conditions. See tumor markers. CEA: see carcinoembryonic antigen. CT-guided needle biopsy: a procedure that uses special x-rays to show a mass, while the radiologist advances a biopsy needle toward it. The images are repeated until the doctor is sure the needle is in the tumor or mass. A biopsy is then taken from it to be looked at under the microscope. CT scan or CAT scan: see computed tomography. cachexia (ka-kek-see-uh): a profound state of general poor health and malnutrition (poor dietary intake). calcifications: (kals-if-ik-a-shuns) tiny calcium deposits within the breast, alone or in clusters, often found by mammography. These are also called microcalcifications. They are a sign of changes within the breast that may need to be followed by more mammograms, or by a biopsy. They may be caused by breast cancer or by benign breast conditions. cancer: cancer is not just one disease but a group of diseases. All forms of cancer cause cells in the body to change and grow out of control. Most types of cancer cells form a lump or mass called a tumor. The tumor can invade and destroy healthy tissue. Cells from the tumor can break away and travel to other parts of the body. There they can continue to grow. This spreading process is called metastasis. When cancer spreads, it is still named after the part of the body where it started. For example, if breast cancer spreads to the lungs, it is still breast cancer, not lung cancer. Some cancers, such as blood cancers, do not form a tumor. Not all tumors are cancer. A tumor that is not cancer is called benign. Benign tumors do not grow and spread the way cancer does. They are usually not a threat to life. Another word for cancerous is malignant. cancer care team: the group of health care professionals who work together to find, treat, and care for people with cancer. The cancer care team may include any or all of the following and others: primary care physicians, pathologists, oncology specialists (medical oncologist, radiation oncologist), surgeons (including surgical specialists such as urologists, gynecologists, neurosurgeons, etc.), nurses, oncology nurse specialists, and oncology social workers. Whether the team is linked formally or informally, there is usually one person who takes the job of coordinating the team. cancer cell: a cell that divides and reproduces abnormally and can spread throughout the body, crowding out normal cells and tissue. cancer-related check-up: a routine health examination for cancer in persons without obvious signs or symptoms of cancer. The goal of the cancer-related check-up is to find the disease, if it exists, at an early stage, when chances for cure are greatest. Depending on the person’s sex and age, this check-up may include a digital rectal examination, clinical breast examination, Pap smear, PSA blood test, and skin examination. See also detection. 77 G L O S S A R Y, c o n t i n u e d cancer-related fatigue: an unusual and persistent sense of tiredness that can occur with cancer or cancer treatments. It can be overwhelming, last a long time, and interfere with everyday life. Rest does not always relieve it. cancer screening tests: see screening. cancer susceptibility genes: genes (the basic unit of heredity) inherited from one’s parents that greatly increase the risk of a person’s developing cancer. About 5% to15% of all cancers are caused by these genes. cancer vaccine: a vaccine used in the treatment (not prevention) of some cancers. It is made from pieces of tumors and works by causing the immune system to recognize and attack the cancer cells. carcinoembryonic antigen (car-sin-o-em-bre-ON-ic an-tuh-jin): a substance normally found in fetal tissue. If found in an adult, it may suggest that a cancer, especially one starting in the digestive system, may be present. Tests for this substance may help in finding out if a colorectal cancer has come back after treatment. The test is not helpful for screening for colorectal cancer because of the large number of false positives and false negatives. See tumor marker, screening, false positive, and false negative. carcinogen (car-sin-o-jin): any substance that causes cancer or helps cancer grow. For example, tobacco smoke contains many carcinogens that greatly increase the risk of lung cancer. carcinoid tumors or carcinoids: tumors that develop from neuroendocrine cells, usually in the digestive tract, lung, or ovary. The cancer cells from these tumors release certain hormones into the bloodstream. In about 10% of people, the hormone levels are high enough to cause facial flushing, wheezing, diarrhea, a fast heartbeat, and other symptoms throughout the body. carcinoid syndrome: A group of symptoms produced by cancer cells that release high amounts of hormones, which cause facial flushing, wheezing, diarrhea, a fast heartbeat, and other symptoms. carcinoma (car-sin-o-ma): a malignant tumor that begins in the lining layer (epithelial cells) of organs. At least 80% of all cancers are carcinomas. carcinoma in situ (car-sin-o-ma in sy-too): an early stage of cancer in which the tumor is confined to the organ where it first developed. The disease has not invaded other parts of the organ or spread to distant parts of the body. Most in situ carcinomas are highly curable. case manager: the member of a cancer care team, usually a nurse or oncology nurse specialist, who coordinates the patient’s care throughout diagnosis, treatment, and recovery. The case manager acts as a guide through the complex system of health care by helping cut through red tape, getting responses to questions, managing crises, and connecting the patient and family to needed resources. catheter (cath-it-ur): a thin, flexible tube through which fluids enter or leave the body; for example, a tube to drain urine. cell: the basic unit of which all living things are made. Cells replace themselves by splitting and forming new cells (this process is called mitosis). The processes that control the formation of new cells and the death of old cells are disrupted in cancer. 78 G L O S S A R Y, c o n t i n u e d cell cycle: the series of steps that a cell must go through to divide; some chemotherapy drugs act by interfering with the cell cycle. centigray: see radiation dose. centimeter (sin-tuh-mee-ter): a metric measure of length. It takes about 2 1/2 centimeters to equal 1 inch. Also, 1/100 of a meter. cervix (ser-vix): the neck of the womb (uterus). cGy: short for centigray, a unit of radiation equal to the rad, an older term. chemoprevention (key-mo-pre-VEN-shun): prevention or reversal of disease using drugs, chemicals, vitamins, or minerals. While this idea is not ready for widespread use, it is a very promising area of study. The Breast Cancer Prevention Trial has shown that the drug tamoxifen can prevent some cases of breast cancer among women with high risk of the disease. But the drug may have some serious side effects. chemotherapy (key-mo-THER-uh-pee): treatment with drugs to destroy cancer cells. Chemotherapy is often used, either alone or with surgery or radiation, to treat cancer that has spread or come back (recurred), or when there is a strong chance that it could recur. Often called chemo. chromosome (krom-uh-som): chromosomes carry genes, the basic units of heredity. Humans have 23 pairs of chromosomes, one member of each pair from the mother, the other from the father. Each chromosome can contain hundreds or thousands of individual genes. chronic obstructive pulmonary (ob-struck-tiv pull-mun-err-ee) disease: lung disease, such as emphysema or chronic bronchitis, that makes it harder to breathe. More common in smokers; also known as COPD. clinical breast examination: an examination of the breasts done by a health professional such as a doctor or nurse. clinical stage: see staging. clinical trials: research studies to test new drugs or other treatments to compare current, standard treatments with others that may be better. Before a new treatment is used on people, it is studied in the lab. If lab studies suggest the treatment will work, the next step is to test its value in patients. These human studies are called clinical trials. The main questions the researchers want to answer are: • Does this treatment work? • Does it work better than what we’re now using? • What side effects does it cause? • Do the benefits outweigh the risks? • Which patients are most likely to find this treatment helpful? 79 G L O S S A R Y, c o n t i n u e d colon: the large intestine. The colon is a muscular tube about 5 feet long. It is divided into 4 sections: the ascending, transverse, descending, and sigmoid colon. It continues the process of absorbing water and mineral nutrients from food that was started in the small intestine. colonoscope (co-lahn-uh-scope): a slender, flexible, hollow lighted tube about the thickness of a finger. It is inserted through the rectum up into the colon. A colonoscope is much longer than a sigmoidoscope, and allows the doctor to see much more of the colon’s lining. The colonoscope is connected to a video camera and video display monitor so the doctor can look closely at the inside of the entire colon. (This procedure is called a colonoscopy.) colonoscopy (ko-lun-AH-skuh-pee): a procedure that allows a doctor to see inside the large intestine to find polyps or cancer. colony stimulating factors (CSF): types of growth factors that promote growth and division of blood-producing cells in the bone marrow. CSFs are naturally produced in the body. But extra amounts may be given as a treatment to reduce or prevent certain side effects of chemotherapy that may be caused by not having enough blood cells. colorectal cancer screening: testing done to detect abnormalities early, before signs and symptoms start. This allows for earlier detection of cancer, when it is most curable. It also allows doctors to find and remove polyps, which can prevent cancer from developing. See also screening, fecal occult blood test, fecal immunochemical test, barium enema, sigmoidoscopy, colonoscopy, and polyp. colostomy (kuh-lahs-tuh-me): a procedure in which the end of the colon is attached to an opening created in the abdominal wall to get rid of body waste (stool). A colostomy is sometimes needed after surgery for cancer of the rectum. People with colon cancer sometimes have a temporary colostomy but they rarely need a permanent one. combined modality therapy: two or more types of treatment used alternately or together to get the best results. For example, surgery for cancer is often followed by chemotherapy to destroy any cancer cells that may have spread from the original site. complementary therapy: treatment used along with standard medical treatment. Some complementary therapies may help relieve certain symptoms of cancer, relieve side effects of standard cancer therapy, or improve a patient’s sense of well-being. The ACS recommends that patients thinking about using any alternative or complementary therapy discuss it first with a member of their health care team, since many of these treatments are unproven and some can be harmful. See also alternative therapy. computed tomography (to-mahg-ruh-fee): an imaging test in which many x-rays are taken from different angles of a part of the body. These images are combined by a computer to make crosssectional pictures of internal organs. Except for the injection of a dye (needed in some but not all cases), this is a painless procedure that can be done in an outpatient clinic. It is often referred to as a “CT” or “CAT” scan. concurrent treatment: treatment or therapy that is given at the same time as another treatment. 80 G L O S S A R Y, c o n t i n u e d Cone Beam Imaging (CBI): the first system in San Antonio with this advanced technology that alllows high quality CT images that are taken on the treatment machine to improve the accuracy of the radiation. conformal proton beam therapy: a technique for giving radiation therapy that uses proton beams rather than standard radiation. Protons are parts of atoms that cause little damage to the tissues they pass through but are very effective in killing cells at the end of their path. Proton beam therapy is still new and not offered in many treatment centers, but it may be able to deliver more radiation to the cancer while reducing the damage to normal tissues. See also conformal radiation therapy. conformal radiation therapy: a newer type of radiation treatment that uses a special computer which helps shape the beams of radiation to the shape of the tumor and delivers the beams from different directions. This allows healthy tissue to be exposed to less radiation. control group: in research or clinical trials, this is the group that does not receive the treatment being tested. In cancer research, this group most often gets standard treatment (which has already been tested and is in general use.) When no standard treatment exists, the control group may get a placebo or sham treatment. Also called the comparison group. See also clinical trials. conventional therapy or treatment: see standard therapy. COPD: see chronic obstructive pulmonary disease. corticosteroid: (kor-ti-ko-STEER-oid) any of a number of steroid substances that come from the cortex of the adrenal glands. They are sometimes used as an anti-cancer treatment or to reduce nausea cryoablation (cry-o-ah-BLAY-shun): use of extreme cold to freeze and destroy cancer cells. cryosurgery: see cryoablation. curative treatment: treatment aimed at producing a cure. Compare with palliative treatment. Cyberknife: this advanced technology in radiosurgery, uses robotics and image-guidance to deliver exact doses of radiation. It is a non-invasive and painless procedure. cyst (sist): a fluid-filled mass that is usually not cancer (benign). The fluid can be removed for analysis. See needle aspiration. cystoscopy (sis-tah-sko-pee): looking at the inside of the bladder with a thin, flexible, lighted tube called a cystoscope. cytogenetics (sy-toe-juh-net-icks): tests done to look for abnormal changes in chromosomes. This is often done on bone marrow samples in patients with leukemia. cytokine (sy-toe-kine): A substance that is produced by cells of the body’s immune system that can affect the immune response. Cytokines can also be produced in the lab and given to people to help the body’s immune responses against cancer. 81 G L O S S A R Y, c o n t i n u e d cytology (sy-tahl-uh-jee): the branch of science that deals with the structure and function of cells. Also refers to tests to diagnose cancer and other diseases by looking at cells under the microscope. cytometry (sy-tahm-uh-tree): the counting and measuring of cells using a machine called a flow cytometer. cytotoxic (sy-toe-tok-sick): toxic to cells; cell-killing. D D & C or dilation and curettage (die-lay-shun and cure-uh-tazh): a test in which the cervix is opened slightly so that a sample of tissue from the lining of the uterus can be removed and studied. DES: see diethylstilbestrol. DNA: deoxyribonucleic (dee-ok-see-ri-bo-new-CLEE-ick) acid or DNA: the genetic “blueprint” found in the nucleus of each cell. DNA holds genetic information on cell growth, division, and function. See also mutation. DNA repair: the process of correcting the genetic mistakes that are made each time a cell divides. If the repair process does not go right, it can increase the chances of a person having some forms of cancer. DRE: see digital rectal exam. dermatologist (der-muh-tahl-uh-jist): a doctor who specializes in skin diseases. detection: finding disease. Early detection means that the disease is found at an early stage, before it has grown large or spread to other sites. Note: many forms of cancer can reach an advanced stage without causing symptoms. Mammography can help find breast cancer early, and the prostate-specific antigen (PSA) blood test is useful in finding prostate cancer. See also screening. diagnosis: identifying a disease by its signs or symptoms, and by using imaging tests and laboratory findings. For most types of cancer, the earlier a diagnosis of cancer is made, the better the chance for long-term survival. dietary supplement: a product, such as a vitamin, mineral, or herb, intended to improve health but not to diagnose, treat, cure, or prevent disease. Because dietary supplements are not considered “drugs,” their manufacturers do not have to prove they are effective, or even safe. In many cases, studies have found that some do not contain what is listed on the label, and some contain impurities or ingredients not listed. diethylstilbestrol (die-ETH-ul-still-bes-trahl): a man-made form of estrogen. dietitian/registered dietitian/nutritionist: an expert in the area of food and diet; a registered dietitian (RD) has at least a bachelor’s degree and has passed a national competency exam. The term nutritionist is also used, but there are no educational requirements associated with this title. 82 G L O S S A R Y, c o n t i n u e d differentiation (dif-uhr-en-she-A-shun): the normal process through which cells mature so they can carry out the jobs they were meant to do. Cancer cells are less differentiated than normal cells. Pathologists grade the cells to evaluate and report the degree of a cancer’s differentiation. digital mammography: a method of storing an x-ray image of the breast as a computer image rather than on the usual x-ray film. Digital mammography can be combined with computerassisted diagnosis (CAD), a process in which the radiologist uses the computer to help interpret or “read” the mammogram. digital rectal exam (DRE): an exam in which the doctor inserts a lubricated, gloved finger into the rectum to feel for anything not normal. This simple test, which is not painful, can detect many rectal cancers and some prostate cancers. disease-free survival rate: the percentage of people with a certain cancer who still have no evidence of disease (cancer) at a certain period of time (usually 5 years) after treatment. dissection (di-sek-shun): surgery to divide, separate, or remove tissues. See also axillary dissection. distant cancer: cancer that has spread far from its original location or primary site to distant organs or lymph nodes. Sometimes called distant metastases. See also primary site; compare to local or localized cancer. dopamine (dope-uh-meen): a chemical messenger in the brain and nervous system. Dopamine is thought to control balance, movement, and other body functions. It also affects the mood and is linked to feelings of pleasure. dosimetrist (do-sim-uh-trist): a person who plans and calculates the proper radiation dose for cancer treatment. doubling time: for cancer in general, the time it takes for a cell to divide or for a cancer to double itself in size. Cancers vary in doubling time from 8 to 600 days, averaging 100 to 120 days. Thus, a cancer may be present for many years before it can be found. drug resistance: refers to the ability of cancer cells to become resistant to the effects of the chemotherapy drugs used to treat cancer. duct ectasia (ek-ta-zhuh): widening of the ducts of the breast, often related to breast inflammation called periductal mastitis. Duct ectasia is a benign (not cancerous) condition. Symptoms of this condition are a nipple discharge, swelling, retraction of the nipple, or a lump that can be felt. ductal carcinoma in situ or DCIS (ductal car-sin-o-ma in sy-too): cancer cells that start in the milk passages (ducts) but have not grown through the duct walls into the surrounding tissue. This is a highly curable form of breast cancer that is treated with surgery, or surgery plus radiation therapy. Also called intraductal carcinoma. durable power of attorney for health care: a legal document that allows you to appoint a person to make medical decisions for you if you become unable to do so for yourself. This is a type of advanced directive. See also advanced directive. dysphagia (dis-fay-zhe-uh): having trouble swallowing or eating. 83 G L O S S A R Y, c o n t i n u e d dysplasia (dis-play-zhuh): abnormal changes of groups of cells that may lead to cancer. E edema (uh-deem-uh): build-up of fluid in the tissues, causing swelling. Edema of the arm or leg can develop after surgery or radiation. Arm edema can also develop after radical mastectomy or axillary dissection of lymph nodes. Leg edema can develop if lymph nodes in the groin are removed. See also lymphedema. efficacy (ef-i-kuh-see): effectiveness. The ability of a treatment to produce the desired result. electrofulguration (e-lek-tro-ful-ger-A-shun): a type of treatment that destroys cancer cells by burning with an electrical current. Also known as electrocautery. embolization (em-bo-li-ZAY-shun): a type of treatment that reduces the blood supply to the cancer by the injection of materials to plug up the artery that supplies blood to the tumor. emesis (em-eh-sis): vomiting endocrine (en-duh-krin) glands: glands that release hormones into the bloodstream. The ovaries are one type of endocrine gland. endocrine therapy: manipulation of hormones in order to treat a disease or condition. See also hormone therapy. endocrinologist (en-duh-kruh-NAHL-uh-jist): a doctor who specializes in diseases related to the glands of the endocrine system, such as the thyroid, pancreas, and adrenal glands. endometrium (en-do-mee-tree-um): the lining of the womb (uterus). endoscopy (en-dahs-kuh-pee): inspection of body organs or cavities using a flexible, lighted tube called an endoscope. enterostomal therapist (en-ter-es-STO-mal ther-uh-pist): a health professional, often a nurse, who teaches people how to care for ostomies (surgically created openings such as a colostomy) and other wounds. enucleation (ee-noo-klee-AY-shun): surgical removal of something without cutting into it. Sometimes used to describe removal of a whole tumor; also may describe removing the whole eyeball while leaving eye muscles and other contents of the eye socket. enzyme (en-zime): proteins that increase the rate of chemical reactions in living cells. epidemiology (ep-ih-deem-ee-AHL-uh-jee): the study of diseases in populations by collecting and analyzing statistical data. In the field of cancer, epidemiologists look at how many people have cancer; who gets specific types of cancer; and what factors (such as environment, job hazards, family patterns, and personal habits, such as smoking and diet) play a part in the development of cancer. 84 G L O S S A R Y, c o n t i n u e d esophageal (eh-sof-uh-JEE-uhl) speech: a special type of speech used by some people after surgery for cancer of the voice box (larynx). Air is swallowed and a “belching” type of speech can be produced. New devices, improved surgery, and the use of chemotherapy and radiation therapy instead of surgery, have reduced the need for learning esophageal speech. estrogen: a female sex hormone produced mostly by the ovaries, and in smaller amounts by the adrenal cortex. In women, levels of estrogen fluctuate on nature’s carefully designed schedule, regulating the development of secondary sex characteristics, including breasts; regulating the monthly cycle of menstruation; and preparing the body for fertilization and reproduction. In breast cancer, estrogen may promote the growth of cancer cells. See estrogen receptor assay, estrogen replacement therapy, and hormone therapy. estrogen replacement therapy: the use of estrogen from other sources after a woman’s body no longer makes its own supply. This type of hormone therapy is used to relieve symptoms of menopause. It can provide protective effects against bone thinning (osteoporosis) after menopause. Since estrogen nourishes some types of breast cancer, scientists question whether estrogen replacement therapy increases breast cancer risk. Some new drugs called selective estrogen receptor modulators (SERMs) are being studied. They seem to have many of the helpful effects of estrogen replacement without increasing breast cancer risk; in fact, recent studies suggest that some SERMs may actually reduce breast cancer risk. See estrogen, menopause, and osteoporosis. estrogen receptor assay: the estrogen receptor assay is a laboratory test done on a sample of the cancer in order to see whether estrogen receptors are present. The growth of normal breast cells and some breast cancers is stimulated by estrogen. Estrogen receptors are molecules that function as cells’ “welcome mat” for estrogen circulating in the blood. Breast cancer cells without these receptors (called estrogen-receptor negative or ER negative) are unlikely to respond to hormonal therapy. Estrogen-receptor positive cancers are more likely to respond to hormonal therapy. etiology (ee-tee-ahl-uh-jee): the cause of a disease. In cancer, there are probably many causes. Research is showing that both genetics and lifestyle are major factors in many cancers. excision (ex-sih-zhun): removal by surgery. This can include a tumor or a body part. external beam radiation therapy (EBRT): radiation that is focused from a source outside the body on the area affected by the cancer. It is much like getting a diagnostic x-ray, but for a longer time. Compare to brachytherapy. F false negative: test result implying a condition does not exist when in fact it does. false positive: test result implying a condition exists when in fact it does not. familial adenomatous polyposis or FAP: (fa-mil-e-uhl ad-no-muh-tus pa-lee-po-sis)FAP: an inherited condition that is a risk factor for developing colorectal cancer at a young age. People with this syndrome develop polyps in the colon and rectum. Usually one or more of these polyps becomes cancerous if it is not removed. FAP is caused by changes in the APC gene. See also APC gene. fascia (fash-uh): a sheet or thin band of fibrous tissue that covers muscles and some organs of the body. 85 G L O S S A R Y, c o n t i n u e d fatigue (fuh-teeg): a common symptom during cancer treatment, a bone-weary exhaustion that doesn’t get better with rest. For some, this can last for some time after treatment. fecal immunochemical test (fee-kuhl im-you-no-KIM-uh-kuhl test) (also called FIT): a newer test to look for “hidden” blood in the stool, which could be a sign of cancer. The test is not affected by vitamins or foods, though it still requires 2 or 3 specimens. See also fecal occult blood test, false positive, and colorectal cancer screening. fecal occult blood test: a test for “hidden” blood in the feces (stool). The presence of such blood could be a sign of cancer. See also fecal immunochemical test and colorectal cancer screening. feces (fee-sees): solid waste matter; stool. fibrocystic (fi-bro-sis-tick) changes: a term that describes certain benign changes in the breast. Symptoms of this condition are breast swelling or pain. The doctor or nurse will also look for the presence of nodules, lumpiness, or a discharge from the nipples. Because these symptoms or other signs can look a lot like breast cancer, a mammogram or a biopsy of breast tissue may be needed to show that there is no cancer. fibrosis: formation of scar-like (fibrous) tissue. This can happen anywhere in the body. fine needle aspiration (FNA) biopsy: a procedure in which a thin needle is used to draw up (aspirate) samples to be looked at under a microscope. See also biopsy. first-degree relative: a parent, sibling (brother or sister), or child. FISH: short for fluorescent in situ hybridization; a cytogenetic blood test used to find specific DNA sequences on chromosomes. It can be used to diagnose, to evaluate prognosis (disease outlook), or to look at the remission of a disease, such as cancer. See also cytogenetics. fistula (fist-chu-luh): an abnormal passage, opening, or connection between 2 internal organs or from an internal organ to the surface of the body. five (5)-year survival rate: the percentage of people with a given cancer who are expected to survive 5 years or longer after diagnosis. Five-year survival rates are based on the most recent information available, but they may include information from patients treated several years earlier. These numbers do not take into account advances in treatment that have often occurred. They are not helpful in predicting an individual case. They only paint a very general picture of how people in the past have done with the same type of cancer. See also relative 5-year survival rate. flow cytometry (flow sy-tahm-uh-tree): a test of tumor tissue to see how fast the tumor cells are reproducing and whether the tumor cells contain a normal or abnormal amount of DNA. This test is used to help predict how aggressive a cancer is likely to be. See also ploidy, deoxyribonucleic acid, and S-phase fraction. focus (fo-kus): a point at which rays of light or radiation beams come together. Also used to describe a region of disease in the body. The plural can be focuses or foci (fo-si). 86 G L O S S A R Y, c o n t i n u e d frozen section: a very thin slice of body tissue that has been quick-frozen and then looked at under a microscope. This method is sometimes used during an operation because it gives a quick diagnosis, and can tell a surgeon whether or not to continue with the procedure. The diagnosis is confirmed in a few days by a more detailed study called a permanent section. G GI tract: see gastrointestinal tract. Gardner syndrome: like familial adenomatous polyposis, Gardner syndrome is an inherited condition in which polyps develop at a young age and often lead to cancer. It can also cause benign (not cancerous) tumors of the skin, soft connective tissue, and bones. See APC gene, familial adenomatous polyposis. gastric (gas-trick): of or referring to the stomach. gastroenterologist (gas-tro-en-ter-AHL-uh-jist): a doctor who specializes in diseases of the digestive (gastrointestinal) tract, such as the esophagus, stomach, small intestine, colon, and rectum. gastrointestinal (gas-tro-in-TEST-uh-nul) tract: the digestive tract. It is made up of those organs and structures that process and prepare food to be used for energy; for example, the stomach, small intestine, and large intestine. gene: a piece of DNA that has information on hereditary traits such as hair color, eye color, and height, as well as susceptibility to certain diseases. See also deoxyribonucleic acid. genetic counseling: the process of counseling people who may have a gene that makes them more likely to develop cancer. The purpose of counseling is to explore what the genetic test results might mean, help them decide whether or not they wish to be tested, and to support them before and after the test. genetic counselor: a specially trained health professional who helps people as they consider genetic testing, as they adjust to the test results, and as they consider whatever screening and preventive measures are best for them. genetic testing: tests performed to see if a person has certain gene changes known to increase cancer risk. Such testing is not recommended for everyone, but for people with specific types of family history. Genetic counseling should be part of the genetic testing process. gene therapy: a new type of treatment in which defective genes are replaced with normal ones. The new genes are delivered into the cells by viruses or proteins. genome (jee-nome): the total DNA in a single cell, representing all of the genetic information of the organism. germ cell: the reproductive cells of the body, that is, ova (eggs) or sperm. glands: a cell or group of cells that produce and release substances used nearby or in another part of the body. 87 G L O S S A R Y, c o n t i n u e d Gleason grade: the prostate cancer grading system used most often is called the Gleason system. A pathologist assigns a Gleason grade ranging from 1 through 5 based on how much the cancer cells under the microscope look like normal prostate cells. Those that look a lot like normal cells are graded as 1, while those that look the least like normal cells are graded as 5. See also Gleason score, and grade. Gleason score: the combination of the two Gleason grades used in classifying each prostate cancer based on how the cells look under the microscope. Because prostate cancers often have areas with different grades, a grade is assigned to the two areas that make up most of the cancer. These two grades are added to give a Gleason score between 2 and 10. The higher the Gleason score, the faster the cancer is likely to grow and the more likely it is to spread beyond the prostate. Also known as the Gleason sum. grade: the grade of a cancer reflects how abnormal it looks under the microscope. There are several grading systems for different types of cancers. Each grading system divides cancer into those with the greatest abnormality, the least abnormality, and those in between. Grading is done by a pathologist who looks at the tissue from the biopsy. It is important because cancers with more abnormal-appearing cells tend to grow and spread more quickly and have a worse prognosis (outlook). gray (Gy): see radiation dose. graft versus host disease (GVHD): the condition that results when the immune cells of a transplant (usually a bone marrow transplant) from a donor attack the tissues of the person receiving the transplant. growth factors: naturally occurring proteins that cause cells to grow and divide. Too much growth factor production by some cancer cells helps them grow quickly. New treatments to block these growth factors are being tested in clinical trials. Other growth factors help normal cells recover from side effects of chemotherapy. guaiac (gwi-ack): substance used to test the stool to see if it contains blood. gynecologic (guy-nuh-kuh-lah-jik) oncologist: a doctor who specializes in cancers of the female reproductive organs. gynecologist (guy-nuh-kahl-uh-jist): a doctor who specializes in women’s health. H health care power of attorney: see durable power of attorney for health care. Health Insurance Protability and Accountability Act (HIPAA): a federal act that protects people who change jobs, are self-employed, or who have pre-existing medical conditions. HIPAA standardizes an approach to the continuation of healthcare benefits for individuals and members of small group health plans and establishes parity between the benefits extended to these individuals and those benefits offered to employees in large group plans. The act also contains provisions designed to ensure that prospective or current enrollees in a group health plan are not discriminated against based on health status. hematologist (he-muh-TAHL-uh-jist): a doctor who specializes in diseases of the blood and blood-forming tissues. 88 G L O S S A R Y, c o n t i n u e d hematoma (he-muh-TO-muh): a collection of blood outside a blood vessel caused by a leak or an injury. A bruise is an example of a hematoma. hematuria (he-muh-TUR-ee-uh): blood in the urine. hemorrhoids (hem-uh-royds): large varicose veins inside the rectum or colon. They don’t cause cancer or become cancerous, but they can cause pain, itching, and irritation. They can also cause slight bleeding, which can result in a positive fecal occult blood test or fecal immunochemical test even when no cancer is present. See fecal occult blood test, fecal immunochemical test, and colorectal cancer screening. hepatomegaly (hep-at-o-MEG-uh-lee): enlargement of the liver. HER2 gene (sometimes called HER2/neu): this oncoprotein is present in very small amounts on the outer surface of normal breast cells. About 25% to 30% of breast cancers have too much of this protein. HER stimulates cell growth, and breast cancers that produce too much of this protein tend to be more aggressive. A monoclonal antibody used to treat this type of breast cancer attaches to the HER2 protein, slow the growth of the breast cancer cells, and may also stimulate the immune system to more effectively attack the cancer. Some other types of cancer also have too much HER2 protein. Studies of monoclonal antibody therapy for these cancers are in progress. hereditary cancer syndrome: conditions linked with cancers that occur in several family members because of an inherited, mutated gene. hereditary non-polyposis (huh-red-i-ter-ee non-pah-lee-PO-sis) colon cancer (HNPCC): an inherited condition that greatly increases a person’s risk for developing colorectal cancer, as well as endometrial cancer, ovarian cancer, small bowel cancer, or cancer of the lining of the kidney or the ureters. People with this condition tend to develop cancer at a young age without first having many polyps. high risk: when the chance of developing cancer is greater than that normally seen in the general population. People may be at high risk from many factors, including heredity (such as a family history of breast cancer), personal habits (such as smoking), or the environment (such as overexposure to sunlight). HIPAA: Health Insurance Portability and Accountability Act of 1996. This act clarified and modified elements of the Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA). Among other provisions, HIPAA eliminates health insurance descrimination based on preexisting conditions, incorporating instead a waiting period of 12 to 18 months. histology (hiss-tah-luh-jee): how cells or tissues look when studied under a microscope. The histologic examination is done by a pathologist. See also pathologist. Hodgkin disease: an often curable type of cancer that affects the lymphatic system. Named for the doctor who first identified it; previously called Hodgkin’s disease. home health nurse: a nurse who gives treatment or medicines in the home, teaches patients how to care for themselves, and assesses their condition to see if further medical attention is needed. 89 G L O S S A R Y, c o n t i n u e d homogeneous (home-uh-jee-ne-us): cells or tissue that look the same throughout. See also histology. hormone: a chemical substance released into the body by the endocrine glands such as the thyroid, adrenal, or ovaries. Hormones travel through the bloodstream and set in motion various body functions. Testosterone and estrogen are examples of male and female hormones. hormone receptor: a protein located on a cell’s surface (or within the cell cytoplasm) that binds to a hormone. Tumors can be tested for hormone receptors to see if they can be treated with hormones or anti-hormones. See also hormone receptor assay. hormone receptor assay: a test to see if a breast tumor is likely to be affected by hormones or if it can be treated with hormones. See also estrogen receptor assay and progesterone receptor assay. hormone replacement therapy: the use of estrogen and progesterone from an outside source after the body has stopped making its own supply because of natural or induced menopause. This type of hormone therapy is often given to relieve symptoms of menopause and has been shown to offer protection against thinning of the bones (osteoporosis) in women after menopause. Recent studies have found that combined hormone replacement therapy (estrogen plus progesterone) slightly increases breast cancer risk, as well as the risk of heart disease and blood clots. See also estrogen replacement therapy. hormone therapy: treatment with hormones, using drugs that interfere with hormone production or hormone action, or the surgical removal of hormone-producing glands. Hormone therapy may kill cancer cells or slow their growth. hospice: a special kind of care for people in the final phase of illness, as well as their families and caregivers. The care usually takes place in the patient’s home or in a home-like facility. hot flush: sudden brief feeling of body warmth, along with flushing of the skin and sweating; common during menopause. Also called hot flash. hyperalimentation (hy-per-al-ih-men-TAY-shun): giving liquid nutrition into a vein (intravenously or IV). hyperplasia (hy-per-PLAY-zhuh): too much growth of cells or tissue in a specific area, such as the lining of the prostate. See also benign prostatic hyperplasia. hypertension (hy-per-TEN-shun): high blood pressure. hyperthermia (hy-per-THERM-ee-uh) therapy: treatment of disease by raising body temperature. hypertrophy (hy-per-truh-fee): the enlargement of an organ or part due to an increase in the size of its cells. hysterectomy (hiss-ter-EK-tuh-me): an operation to remove the uterus through an incision in the abdomen or through the vagina. Removal of the ovaries (oophorectomy) may be done at the same time. 90 G L O S S A R Y, c o n t i n u e d I IVP: see intravenous pyelogram ileostomy (ill-ee-OSS-tuh-me): an operation in which the end of the small intestine, the ileum, is brought out through an opening in the abdomen. Unformed, liquid stool leaves the intestine through this opening into a bag called an appliance. Image Guided Radiation Therapy (IGRT): diagnostic quality images increase the accuracty of patient setups and improve the accuracy of radiation delivery. imaging studies: methods used to make pictures of internal body structures. Some imaging methods used to help diagnose or stage cancer are x-rays, CT scans, magnetic resonance imaging (MRI), and ultrasound. immune system: the complex system by which the body resists infection by germs, such as bacteria or viruses, and rejects transplanted tissues or organs. The immune system may also help the body fight some cancers. immunocytochemistry (im-yuh-no-sy-toe-KEM-iss-tree) or immunohistochemistry ( im-yuh-nohis-toe-KEM-iss-tree): a laboratory test that uses antibodies to detect specific chemical antigens in cells or tissue samples viewed under a microscope. This procedure can be used to help detect and classify cancer cells. It is also one of the methods used for estrogen receptor assays and progesterone receptor assays. See also monoclonal antibodies. immunology (im-yuh-nahl-uh-jee): study of how the body resists infection and certain other diseases. Knowledge gained in this field is important to those cancer treatments based on the principles of immunology. immunosuppression (im-yuh-no-suh-PREH-shun): a state in which the ability of the body’s immune system to respond is decreased. This condition may be present at birth, or it may be caused by certain infections (such as human immunodeficiency virus or HIV) or by certain cancer therapies (such as cancer-cell killing (cytotoxic) drugs, radiation, and bone marrow transplant). immunotherapy (im-yuh-no-THER-uh-pee): treatments that promote or support the body’s immune system response to a disease such as cancer. implant: a small amount of radioactive material placed in or near a cancer. Also, an artificial form used to restore the shape of an organ after surgery, for example, a breast implant. impotence (im-puh-tense): not being able to have or keep an erection of the penis. incidence (in-sih-dens): the number of new cases of a disease that occur in a group of people each year. Compare to prevalence. incision (in-sih-zhun): cut made during surgery. incontinence (in-kon-tuh-nence): partial or complete loss of urinary or bowel control. indigent (in-dij-ent): not having enough money to meet one’s needs. 91 G L O S S A R Y, c o n t i n u e d informed consent: a legal document that explains a course of treatment, the risks, benefits, and possible alternatives; also the process by which patients agree to treatment. infraclavicular (in-fruh-kluh-VICK-yuh-ler) nodes: lymph nodes located under the collar bone (clavicle). ingest (in-jest): to take in by mouth; to eat or drink. inherited disease: illness to which a person is susceptible because of a gene passed from his or her parents at birth. Examples of inherited diseases related to colorectal cancer include hereditary non-polyposis colon cancer or familial adenomatous polyposis. See mutation. in situ (in sy-too): in place; localized and confined to one area. A very early stage of cancer. interferon (in-ter-fear-on): a protein produced by cells. Interferon helps regulate the body’s immune system, boosting activity when a threat, such as a virus, is found. Scientists have learned that interferon helps fight against cancer, so it is used to treat some types of cancer. interleukins (in-ter-loo-kins): see cytokine. internal radiation: treatment in which a radioactive substance is implanted in the body; see also brachytherapy. Compare to external beam radiation therapy. interstitial (in-ter-stih-shul) radiation therapy: a type of treatment in which a radioactive implant is placed directly into the tissue (not in a body cavity). intestines (in-test-ins): the part of the digestive tract from the end of the stomach (pylorus) to the anus, which absorbs nutrients and water from food into the bloodstream. It includes the small intestine, which is sometimes called the small bowel, and the large intestine, which is also called the large bowel or colon. intravenous (IV): a method of giving fluids and medicines using a needle or a thin tube that is put into a vein. intravenous pyelogram (in-tra-veen-us pile-uh-gram): a special kind of x-ray procedure. A dye is injected into the bloodstream. It travels to the kidneys, ureters, and bladder and helps to clearly outline these organs on the x-rays. Referred to as IVP. invasive cancer: cancer that has spread beyond the layer of cells where it first developed and has grown into nearby tissues. invasive ductal carcinoma: a cancer that starts in the milk passages (ducts) of the breast and then breaks through the duct wall, where it invades the fatty tissue of the breast. When it reaches this point, it can spread (metastasize) elsewhere in the breast, as well as to other parts of the body through the bloodstream and lymphatic system. Invasive ductal carcinoma is the most common type of breast cancer, accounting for about 80% of breast malignancies. Also known as infiltrating ductal carcinoma. 92 G L O S S A R Y, c o n t i n u e d invasive lobular carcinoma: a cancer that starts in the milk-producing glands (lobules) of the breast and then breaks through the lobule walls and grows into the nearby fatty tissue. From there, it may spread elsewhere in the breast. About 15% of invasive breast cancers are invasive lobular carcinomas. It is often hard to detect by physical examination or even by mammography. Also called infiltrating lobular carcinoma. investigational: under study; often used to describe drugs used in clinical trials that are not yet available to the general public. L LHRH (luteinizing hormone-releasing hormone) (loo-tee-uh-ny-zing): a hormone produced by the hypothalamus, a tiny gland in the brain. LHRH analogs: man-made hormones, chemically similar to LHRH. They block the production of the male hormone testosterone and are sometimes used as a treatment for prostate cancer. laparoscope (LAP-uh-ruh-scope): a long, flexible, slender tube inserted into the abdomen through a very small incision. See also laparoscopic surgery. laparoscopic (lap-uh-ruh-SKAH-pick) surgery: surgery done through a small incision through which a narrow tube-like instrument called a laparoscope (see above) is inserted. Other tubes are inserted in other nearby incisions to allow the surgeon to work inside the abdomen and remove part of the colon or other organ, which is shown on a television monitor. The small incisions led to the name “keyhole surgery.” This surgery is more difficult than open surgeries, and requires a skilled surgeon who has done a lot of them. laryngectomy (lair-en-jek-tuh-me): surgery to remove the voice box (larynx), usually because of cancer. leiomyoma (lie-o-my-o-muh): a benign (non-cancerous) fibrous tumor of the uterus. About 40% of women have leiomyomas by age 40. Usually there are no symptoms, but the tumors can cause abnormal uterine bleeding and other symptoms depending on their size and location in the uterus. It is also called uterine fibroid tumor or fibroma. lesion (lee-zhun): a change in body tissue; sometimes used as another word for tumor. May also be used to describe a change in the appearance or texture of skin, such as an open sore, scab, or discolored area. leukemia (loo-key-me-uh): cancer of the blood or blood-forming organs. There are two major classes of leukemia, myeloid and other, non-myeloid types. People with leukemia often have a very high number of white blood cells (leukocytes). See leukocytosis, myeloid leukemia, and non-myeloid cancers. leukocytosis (loo-ko-sy-TOE-sis): having more than the usual number of white blood cells. leukopenia: (loo-ko-PEE-nee-uh): decrease in the white blood cell count, often a side effect of chemotherapy. leukoplakia (loo-ko-PLAY-key-uh): white patches on the tongue or inside the cheeks. These are often pre-malignant. 93 G L O S S A R Y, c o n t i n u e d limited breast surgery: also called lumpectomy, segmental excision, and tylectomy. This surgery removes the breast cancer and a small amount of tissue around the cancer, but preserves most of the breast. It is almost always combined with axillary lymph node removal and is usually followed by radiation therapy. linear accelerator: a machine used in radiation therapy to treat cancer. It gives off gamma rays and electron beams. This is called external-beam radiation therapy. living will: a legal document that allows a person to decide what should be done if he or she becomes unable to make health care decisions; a type of advance directive. See also advance directives. lobectomy (lob-bek-tuh-me): surgery to remove a lobe of an organ -- usually the lung. lobular carcinoma in situ (LCIS): a very early type of breast cancer that develops within the milk-producing glands (lobules) of the breast and has not grown through the wall of the lobules. Researchers think that most cases of lobular carcinoma in situ do not progress to invasive lobular cancer. Still, having this type of cancer places a woman at increased risk of developing an invasive breast cancer later in life. For this reason, it’s important for women with lobular carcinoma in situ to have a physical examination 3 times a year and an annual mammogram. lobules: the glands in a woman’s breasts that produce milk. local excision (lo-kul eck-si-zhun): surgery to remove small superficial (surface) cancers or polyps. local or localized cancer: a cancer that is confined to the organ where it started; that is, it has not spread to distant parts of the body. lump: any kind of mass in the breast or elsewhere in the body. lumpectomy (lum-peck-tuh-me): surgery to remove the breast tumor and a small amount of surrounding normal tissue. See also breast conservation therapy. lymph (limf): clear fluid that flows through the lymphatic vessels and has cells known as lymphocytes. These cells are important in fighting infections and may also have a role in fighting cancer. See also lymphatic system, lymph nodes, lymphocytes, and lymphadenectomy. lymph nodes: small bean-shaped collections of immune system tissue, such as lymphocytes, found along lymphatic vessels. They remove cell waste, germs, and other harmful substances from lymph. They help fight infections and also have a role in fighting cancer, although cancers sometimes spread through them. Also called lymph glands. See also lymph, lymph system, and lymphadenectomy. lymph node biopsy: a test in which all or part of a lymph node is removed and looked at under a microscope to find out if cancer has reached the lymph nodes. lymph node dissection: see lymphadenectomy. 94 G L O S S A R Y, c o n t i n u e d lymphadenectomy (limf-ad-uh-NECK-tuh-me): surgical removal of one or more lymph nodes. After removal, the lymph nodes are looked at under a microscope to see if cancer has spread. Also called lymph node dissection. See also lymphatic system, lymph, lymph nodes, and lymphocytes. lymphatic system: the tissues and organs (including lymph nodes, spleen, thymus, and bone marrow) that produce and store lymphocytes (cells that fight infection) and the channels that carry the lymph fluid. The entire lymphatic system is an important part of the body’s immune system. Invasive cancers sometimes get into the lymphatic vessels (channels) and spread (metastasize) to lymph nodes. See also lymph, lymph nodes, lymphocytes, and lymphadenectomy. lymphedema (limf-uh-dee-muh): a complication in which excess fluid collects in the arms or legs. This often happens after the lymph nodes and vessels are removed by surgery, or injured from radiation or from a tumor that changes the normal drainage of the fluid. This can happen even years after treatment and can be a life-long condition. See lymph, lymph nodes, and lymphatic system. lymphocytes: a type of white blood cell that helps the body fight infection. lymphocytosis (limf-o-sy-TOE-sis): having an excess of lymphocytes. lymphokines (limf-o-kines): see cytokine. lymphoma (lim-foam-uh): a cancer of the lymphatic system, a network of thin vessels and nodes throughout the body that helps to fight infection. Lymphoma involves the type of white blood cells called lymphocytes. The 2 main types of lymphoma are Hodgkin disease and nonHodgkin lymphoma. The treatments for these 2 types of lymphomas are very different. Lynch syndrome: an old term used to describe hereditary non-polyposis colorectal cancer (HNPCC); an inherited tendency to develop certain cancers. See hereditary non-polyposis colorectal cancer. M MRI: see magnetic resonance imaging. macroglobulinemia (mack-row-glob-yuh-lin-EE-mee-uh): a condition with abnormally large proteins in the blood, which may reduce or clog blood flow in the smaller blood vessels. Waldenstrom macroglobulinemia is a type of non-Hodgkin lymphoma with such proteins. . macrophage: (mack-row-faj): a type of white blood cell that engulfs and destroys foreign materials. magnetic resonance imaging (MRI): a method of taking pictures of the inside of the body. Instead of using x-rays, MRI uses a powerful magnet to send radio waves through the body. The images appear on a computer screen as well as on film. Like x-rays, the procedure is physically painless, but some people may feel confined inside the MRI machine. malignant (muh-lig-nunt) tumor: a mass of cancer cells that may invade surrounding tissues or spread (metastasize) to distant areas of the body. See also tumor and metastasis. 95 G L O S S A R Y, c o n t i n u e d mammogram, mammography: an x-ray of the breast; a method of finding breast cancer that can’t be felt. Mammograms are done with a special type of x-ray machine used only for this purpose. A mammogram can show a developing breast tumor before it is large enough to be felt by a woman or even by a highly skilled health care professional. Screening mammography is used to help find breast cancer early in women who don’t have any symptoms. Diagnostic mammography helps the doctor learn more about breast masses or the cause of other breast symptoms. margin: the edge of a tissue sample removed during surgery. A negative surgical margin means that no cancer cells were found on the outer edge of the removed tissue, and is a sign that no cancer was left behind. A positive surgical margin indicates that cancer cells are found at the outer edge of the removed sample and is usually a sign that some cancer remains in the body. mass: any sort of lump, which may or may not be cancer. See also tumor. mastectomy (mas-tek-tuh-me): surgery to remove all or part of the breast and sometimes other tissue. Modified radical mastectomy removes the breast, skin, nipple, areola, and most of the axillary lymph nodes on the same side, leaving the chest muscles intact. Partial or segmental mastectomy removes only the part of the breast that has the cancer and a margin of healthy breast tissue surrounding the tumor. Prophylactic mastectomy is a mastectomy done before any evidence of cancer can be found, for the purpose of preventing cancer. Quadrantectomy (quadrunt-EK-tuh-me) is a partial mastectomy in which the quarter of the breast that has a tumor is removed. Simple mastectomy or total mastectomy removes only the breast and areola. mediastinoscopy (me-dee-uh-stine-AH-skuh-pee): examination of the chest cavity using a lighted, flexible tube inserted under the chest bone (sternum). This allows the doctor to see the lymph nodes in this area and remove samples to check for cancer. medical oncologist: a doctor who is specially trained to diagnose and treat cancer with chemotherapy and other drugs. medical power of attorney: see durable power of attorney for health care. medullary (med-you-lair-ee) carcinoma: a special type of infiltrating ductal carcinoma with especially sharp boundaries between tumor tissue and normal tissue. About 5% of breast cancers are medullary carcinomas. The outlook (prognosis) for this kind of cancer is considered to be better than average. melanoma (mel-uh-no-muh): a cancerous (malignant) tumor that begins in the cells that produce the skin coloring (melanocytes). Melanoma is almost always curable in its early stages. However, it is likely to spread, and once it has spread to other parts of the body the chances for a cure are much less. menarche (men-ar-key): a woman’s first menstrual period. Early menarche (before age 12) is a risk factor for breast cancer, possibly because the earlier a woman’s periods begin, the longer her exposure to estrogen. menopause (men-uh-paws): the time in a woman’s life when monthly cycles of menstruation stop forever and the level of hormones produced by the ovaries decreases. Menopause usually takes place in women in their late 40s or early 50s, but it can also be brought about by surgical removal of both ovaries (oophorectomy), or by some chemotherapies that destroy ovarian function. 96 G L O S S A R Y, c o n t i n u e d messenger RNA: the molecule that carries the information from the DNA genetic code to areas in the cytoplasm of the cell that make proteins. metastasis (meh-tas-tuh-sis): cancer cells that have spread to one or more sites elsewhere in the body, often by way of the lymph system or bloodstream. Regional or local metastasis is cancer that has spread to the lymph nodes, tissues, or organs close to the primary site. Distant metastasis is cancer that has spread to organs or tissues that are farther away (such as when prostate cancer spreads to the bones, lungs, or liver).The plural of this word is metastases. See also primary site, lymph nodes, and lymph system. metastasize (meh-tas-tuh-size): the spread of cancer cells to one or more sites elsewhere in the body, often by way of the lymph system or bloodstream. See also metastasis and lymph system. metastatic (met-uh-stat-ick): a way to describe cancer that has spread from the primary site (where it started) to other structures or organs, nearby or far away (distant). See also primary site and metastasis. micrometastases (mike-row-muh-TAS-tuh-sis): the spread of cancer cells in groups so small that they can only be seen under a microscope. microsatellite instability (MSI) (my-crow-SAT-uh-lite in-stuh-BILL-uh-tee): a type of genetic mutation often linked to hereditary non-polyposis colon cancer (HNPCC). This mutation causes size differences in sections of DNA that are normally the same size in all a person’s cells. Testing for MSI is done on tissue taken from the cancer to find out if this DNA is of different lengths; if it is, HNPCC genetic testing is usually offered. See also hereditary non-polyposis colon cancer, DNA, mutation, and genetic counseling. microwave therapy: a way of treating cancer in a few sites, such as the liver, by applying heat to destroy the cells. millimeter: a metric measure of length. It takes about 25 millimeters to equal 1 inch. Also 1/1000 of a meter. millirem: see radiation dose. millisievert: see sievert. modified radical mastectomy: see mastectomy. monoclonal (ma-nuh-KLO-nuhl) antibodies: man-made antibodies that are designed to lock onto specific antigens. Antigens are substances that can be recognized by the immune system. Monoclonal antibodies that have been attached to chemotherapy drugs or radioactive substances are being studied for their potential to seek out antigens unique to cancer cells and deliver these treatments directly to the cancer, thus killing the cancer cell and not harming healthy tissue. Monoclonal antibodies are also often used to help detect and classify cancer cells under a microscope. Other studies are being done to see if radioactive atoms attached to monoclonal antibodies can be used in imaging tests to detect and locate small groups of cancer cells. See antibody, antigen, and immunocytochemistry. morbidity: a measure of the new cases of a disease in a population; the number of people who have a disease. 97 G L O S S A R Y, c o n t i n u e d mortality: a measure of the rate of death from a disease within a given group of people. mucinous carcinoma (myoo-sin-us car-sin-o-ma): a type of carcinoma that is formed by mucusproducing cancer cells. mucositis (myoo-ko-site-us): inflammation of a mucous membrane, such as the lining of the mouth. multidrug resistance (MDR): resistance of tumor cells to several unrelated drugs after being exposed to a single chemotherapy drug. May also refer to infections that can no longer be cured by the usual antibiotics. mutation: a change in the DNA of a cell. Most mutations do not produce cancer, and a few may even be helpful. However, all types of cancer are thought to be due to mutations that damage a cell’s DNA. Some cancer-related mutations can be inherited, which means that the person is born with the mutated DNA in all the body’s cells. But most mutations happen after the person is born, and are called somatic mutations. This type of mutation happens in one cell at a time, and only affects cells that arise from the single mutated cell. See also somatic mutation, inherited mutation, deoxyribonucleic acid, gene, and cancer susceptibility gene. myeloid (my-uh-loid) leukemia: Several kinds of leukemia that include chronic myelogenous leukemia (CML) and acute myeloid leukemia (AML). There are 8 subtypes of acute myeloid leukemia -- M0 (Undifferentiated AML), M1 (Myeloblastic leukemia with minimal maturation), M2 (Myeloblastic leukemia with maturation), M3 (Promyelocytic leukemia), M4 (Myelomonocytic leukemia), M5 (Monocytic leukemia), M6 (Erythroid leukemia), and M7 (Megakaryoblastic leukemia). See also leukemia and non-myeloid cancers. N necrosis (nuh-crow-sis): the death of living tissues. Necrotic refers to tissue that has died. needle aspiration: a type of needle biopsy that removes fluid from a cyst or cells from a tumor. In this procedure, a needle is used to reach the cyst or tumor, and with suction, draw up (aspirate) samples to be looked at under a microscope. If the needle is thin, the procedure is called a fine needle aspiration or FNA. See also biopsy. needle biopsy: removal of fluid, cells, or tissue with a needle so that it can be looked at under a microscope. There are 2 types: fine needle aspiration (FNA) and core biopsy. FNA uses a thin needle to draw up (aspirate) fluid or small tissue fragments from a cyst or tumor. A core needle biopsy uses a thicker needle to remove a cylindrical sample of tissue from a tumor. needle localization: a procedure used to guide a surgical breast biopsy when the lump is hard to locate or when there are areas that look suspicious on the x-ray but there is not a distinct lump. A thin needle is placed into the breast. X-rays are taken and used to guide the needle to the suspicious area. The surgeon then uses the path of the needle as a guide to find the abnormal area to be removed. neoadjuvant (nee-o-AD-juh-vunt) therapy: treatment given before the main treatment. Compare to adjuvant therapy. neonatologist (nee-o-nay-TAHL-uh-jist): a doctor who specializes in the care of the newborn (until about 6 weeks of age). 98 G L O S S A R Y, c o n t i n u e d neoplasm (nee-o-plaz-um): an abnormal growth (tumor) that starts from a single altered cell; a neoplasm may be benign or malignant. Cancer is a malignant neoplasm. nephrologist (neh-frahl-uh-jist): a doctor who specializes in diseases of the kidneys. neuropathy (nur-ah-puth-ee): nerve abnormality or damage which causes numbness, tingling, pain, muscle weakness, or even swelling. It may be caused by injury, infection, disease (cancer, diabetes, kidney failure, or poor nutrition, for example), or by drugs. Peripheral neuropathy is a type of neuropathy that starts in nerves farthest away from the brain, such as the hands and feet. neurosurgeon (nur-o-SUR-jun): a doctor specializing in operations to treat nervous system disorders. neutropenia (new-trow-PEEN-ee-uh): a decrease in the number of neutrophils (white blood cells that respond quickly to infection) in the blood. If a person has less than 1,500/mm3 neutrophils, he or she is considered to be neutropenic and at risk for infection. With fewer than 500 cells/ mm3 the risk of infection is high. neutrophils (new-trow-fills): white blood cells that fight bacterial infection. nipple discharge: any fluid coming from the nipple. It may be clear, milky, bloody, tan, gray, or green. nodal status: indicates whether the cancer has spread to lymph nodes (node-positive) or has not spread to lymph nodes (node-negative). See also lymph node and lymphatic system. nodule: a small, solid lump that can be felt. This term is sometimes used to refer to a small tumor seen on x-ray. non-Hodgkin lymphoma: a cancer of the lymphatic system. The lymphatic system is a network of thin vessels and nodes throughout the body that helps to fight infection. What distinguishes nonHodgkin lymphoma from Hodgkin lymphoma is the absence of a type of cell called the ReedSternberg cell. This cell is present only in Hodgkin lymphoma. The treatment methods for Hodgkin and non-Hodgkin lymphomas are very different. Previously called non-Hodgkin’s lymphoma. non-myeloid cancers: all cancers other than myeloid leukemias. These non-myeloid cancers include all types of carcinoma, all types of sarcoma, melanoma, lymphomas, lymphocytic leukemias (ALL and CLL), and multiple myeloma. See also leukemia and myeloid leukemia. nuclear medicine scan: a method for finding diseases of internal organs such as the brain, liver, or bone. Small amounts of a radioactive substance (isotope) are injected into the bloodstream. The isotope collects in certain organs and a special camera called a scintillation camera is used to produce an image of the organ and show areas of disease. See radioisotope. nucleus (new-klee-us): the center of a cell where the DNA is found and where it reproduces. Studying the size and shape of a cell’s nucleus under the microscope can help pathologists tell cancer cells from benign cells. nurse practitioner: a registered nurse with a master’s or doctoral degree. Licensed nurse practitioners diagnose and manage illness and disease, usually working closely with doctors. 99 G L O S S A R Y, c o n t i n u e d O occupational therapist: a specially trained therapist who works with people who have disabilities to help them relearn how to perform daily activities. off label: refers to the use of a drug to treat a condition other than that for which it was approved by the Food and Drug Administration. omentum: a large fatty sheet in the abdomen that drapes like an apron over the stomach, intestines, and other organs. oncogenes (on-kuh-jeenz): genes that promote cell growth and multiplication. These genes are normally present in all cells. But oncogenes may undergo changes that activate them, causing cells to grow too quickly and form tumors. Compare to tumor suppressor genes. oncologist (on-call-uh-jist): a doctor with special training in the diagnosis and treatment of cancer. oncology (on-call-o-jee): the branch of medicine concerned with the diagnosis and treatment of cancer. oncology clinical nurse specialist: a registered nurse with a master’s degree in oncology nursing who specializes in the care of cancer patients. Oncology nurse specialists may prepare and give treatments, monitor patients, prescribe and provide supportive care, and teach and counsel patients and their families. oncology social worker: a person with a master’s degree in social work who is an expert in coordinating and providing non-medical care to patients. The oncology social worker counsels and assists people with cancer and their families, especially in dealing with the nonmedical issues that can result from cancer, such as financial problems, housing (when treatments must be taken at a facility away from home), and child care. oophorectomy (oof-uh-rek-tuh-me): surgery to remove the ovaries. ophthalmologist (off-thuhl-mal-uh-jist): a medical doctor who specializes in diseases of the eye. oral: refers to the mouth. For example, medicines that are taken orally are taken by mouth. Oral cancer is cancer of the mouth. oral and maxillofacial surgeon: a surgeon who specializes in surgery of the mouth, jaw, and face. orchiectomy (or-key-ek-tuh-me): surgery to remove the testicles; also called castration. See also hormone therapy. orthopedic (or-thuh-pee-dik) surgeon: a surgeon who specializes in diseases and injuries of the bones. osteoporosis (os-tee-o-puh-ROW-sis): thinning of bone tissue, causing less bone mass and weaker bones. Osteoporosis can cause pain, deformity (especially of the spine), and broken bones. This condition is common among postmenopausal women. 100 G L O S S A R Y, c o n t i n u e d ostomy (os-tuh-me): a general term meaning an opening, especially one made by surgery. See also colostomy, ileostomy, urostomy, and tracheostomy. otolaryngologist (o-toe-lair-in-gol-uh-jist): a doctor who specializes in diseases of the ear, nose, and throat. Also called a head and neck surgeon. ovary (o-vuh-ree): reproductive organ in the female pelvis. Normally a woman has two ovaries. They contain the eggs (ova) that, when joined with sperm, result in pregnancy. Ovaries are also the primary source of estrogen. See also estrogen. P p53: an important tumor suppressor gene that is not working properly in many cancers. The protein that this gene makes (also called p53) normally causes damaged cells to die. Mutations, or changes, in this gene can be inherited or they can happen during a person’s life. When they do happen, they can increase risk of many types of cancer. See also mutation. PET scan: see positron emission tomography. PSA: see prostate-specific antigen. Paget (paa-jet) disease of the nipple: a rare form of breast cancer that begins in the milk passages (ducts) and spreads to the skin of the nipple and areola. This affected skin may look crusted, scaly, red, or oozing. The prognosis is generally better if these nipple changes are the only sign of breast disease and no lump can be felt. Named for the doctor, Paget, who first identified it; also known as Paget’s disease. pain specialist: oncologists, neurologists, anesthesiologists, neurosurgeons, and other doctors, nurses, or pharmacists who are experts in pain control. palliative (pal-ee-uh-tiv) treatment: treatment that relieves symptoms, such as pain, but is not expected to cure the disease. Its main purpose is to improve the patient’s quality of life. Sometimes chemotherapy and radiation are used in this way. palpation (pal-pay-shun): using the hands to examine. A palpable mass is one that can be felt. pancreatectomy (pan-cree-uh-TEK-tuh-me): surgery to remove the pancreas. Pap test: this test involves scraping cells from a woman’s cervix and looking at them under a microscope to see if abnormal cells are present. Also called a Pap smear. papillary (pap-uh-lair-ee): having cancer cells arranged in tiny, finger-like projections. Used to describe the appearance of some tumors of the ovaries, uterus, thyroid gland, and other organs. pathologic stage: see staging. pathologist (path-all-uh-jist): a doctor who specializes in diagnosis and classification of diseases by lab tests such as looking at cells under a microscope. The pathologist determines whether a tumor is benign or cancerous, and if cancerous, the exact cell type and grade. pediatric oncologist: a doctor who specializes in cancers of children 101 G L O S S A R Y, c o n t i n u e d pediatrician: a doctor who specializes in the care of children. pelvic examination: an examination of a woman’s uterus and other pelvic organs. It is used to help find cancers of the reproductive organs. The doctor will visually examine external structures and palpate (feel) the internal organs such as the ovaries and cervix. pelvic exenteration (ex-en-ter-A-shun): surgery to remove the organs that are in the pelvis. pelvis (pell-vis): the part of the skeleton that forms a ring or basin of bones below the belly (abdomen). Pelvis may also refer to the general area of the body between the hip bones, below the abdomen. The pelvis contains the bladder, reproductive organs, and the rectum. In women, it also contains the uterus and fallopian tubes; in men, the prostate. peritoneum (pear-i-tuh-NEE-um): membrane that lines the abdomen and covers most of its organs. Peritoneal cavity refers to the area enclosed by the peritoneum. permanent section: a method of preparing tissue to be looked at under a microscope. The tissue is soaked in formaldehyde, processed in various chemicals, surrounded by a block of wax, sliced very thin, attached to a microscope slide, and stained. This process usually takes 1 to 2 days. It allows a clear view of the sample so that the presence or absence of cancer can be determined. pheresis (fuh-ree-sis): see apheresis. Photodynamic (foe-toe-die-NAM-ick) therapy (PDT): a treatment sometimes used for cancers of the skin, esophagus, lung, or bladder. PDT begins with the injection of a non-toxic chemical into the blood. This chemical is allowed to collect in the tumor for a few days. A special type of laser light is then focused on the cancer. This light causes the chemical to change so that it can kill cancer cells. The advantage of PDT is that it can kill cancer cells with very little harm to normal cells. phyllodes tumor (fie-loads): rare breast tumor, usually benign, which grows quickly and can become quite large. Also called phylloides tumor or cystosarcoma phyllodes. physical therapist: a health professional who uses exercises and other methods to restore or maintain the body’s strength, mobility, and function. physiologic (fiz-ee-o-LA-jick): pertaining to the processes of the body or its systems. May be used to describe a particular body function or organ as normal. phytochemical (fie-toe-KEM-ih-kul): substance produced by plants that may produce health benefits when eaten or ingested; for example, antioxidants. See antioxidants. placebo (pluh-see-bo): an inert, inactive substance that may be used in studies (clinical trials) to compare the effects of a given treatment with no treatment. Commonly called, a “sugar pill.” plastic or reconstructive surgeon: a surgeon specializing in restoring appearance or in rebuilding or replacing removed or injured body parts. platelet (plate-let): a part of the blood that plugs up holes in blood vessels after an injury. Chemotherapy can cause a drop in the platelet count, a condition called thrombocytopenia that carries a risk of excessive bleeding. 102 G L O S S A R Y, c o n t i n u e d pleura (plur-uh): the membranes around the lungs and lining the chest cavity. pleurodesis (plu-rod-is-sis): injection of a agent between the layers of the pleura that causes them to fuse to seal off leaks. This procedure helps prevent fluid or air from building up in the pleural cavity, the area between the pleura. See pleura. pneumonectomy (new-muh-NECK-tuh-me): surgery to remove a lung. ploidy (ploy-dee): a measure of the amount of DNA contained in a cell. Ploidy is a marker that helps predict how quickly a cancer is likely to spread. Cancers with the same amount of DNA as normal cells are called diploid (dip-loid) and those with either more or less than that amount are aneuploid (an-you-ploid). About two-thirds of breast cancers are aneuploid. polycythemia vera (pah-lee-sy-THEME-e-uh vair-uh): a chronic blood disorder of unknown cause where the bone marrow makes too many red blood cells, white blood cells, and platelets. This leads to a higher concentration of hemoglobin with larger amounts of red blood cells, which is the main feature of this disease. But with time, the high platelet count may become more of a problem and patients can suffer from problems with blood clots because of this and their “thickened” blood. Often, the spleen is enlarged. Over time, the bone marrow is replaced by fibrous tissue (myelofibrosis). Although it is not a true cancer, it often turns into acute myelogenous leukemia (AML) after many years. polyp (pah-lup): a growth from a mucous membrane commonly found in organs such as the rectum, the uterus, and the nose. polypectomy (pah-lup-eck-tuh-me): surgery to remove a polyp. positron emission tomography (PET): (pahs-uh-trahn ee-mish-uhn tom-ahg-ruh-fee): a PET scan creates an image of the body (or of biochemical events) after the injection of a very low dose of a radioactive form of a substance such as glucose (sugar). The scan computes the rate at which the tumor is using the sugar. In general, high-grade tumors use more sugar than normal and lowgrade tumors use less. PET scans are especially useful in taking images of the brain, although they are becoming more widely used to find out if cancers of the breast, colon, rectum, ovary, or lung have spread. PET scans may also be used to see how well a tumor is responding to treatment. posterior (post-eer-ee-uhr): the back or near the back of an organ or the body. poultice (pole-tiss): soft paste or thick liquid that is usually heated, applied to a cloth, and placed over an inflamed or painful area. Herbs, leaves, or foods are commonly used for this in folk medicine and home remedies. pre-cancerous: changes in cells that may, but do not always, become cancer. Also called premalignant. predisposition: susceptibility to a disease that can be triggered under certain conditions. For example, some women have a family history of breast cancer and are therefore more likely (but not necessarily destined) to develop breast cancer. pre-malignant: See pre-cancerous. 103 G L O S S A R Y, c o n t i n u e d prevalence (preh-vul-uns): a measure of the proportion of persons in the population with a particular disease at a given time. Compare with incidence. prevention: the reduction of cancer risk by eliminating or reducing contact with things known to cause cancer, or by changing conditions that contribute to cancer (such as obesity or lack of exercise.) A change in lifestyle, such as quitting smoking, for example, reduces the risk of lung and other cancers. primary care physician: the doctor a person would normally see first when a problem arises. A primary care doctor could be a general practitioner, a family practice doctor, a gynecologist, a pediatrician, or an internal medicine doctor (an internist). primary site: the place where cancer begins. Primary cancer is usually named after the organ in which it starts. For example, cancer that starts in the breast is always breast cancer, even if it spreads (metastasizes) to other organs such as bones or lungs. primary treatment: the first, and usually the most important, treatment. progesterone (pro-jes-ter-own): a female sex hormone released by the ovaries during every menstrual cycle to prepare the uterus for pregnancy and the breasts for milk production (lactation). progesterone receptor assay: a laboratory test done on a sample of the breast cancer that shows whether the cancer depends on progesterone for growth. Progesterone and estrogen receptor tests provide more complete information to help decide the best cancer treatment for the patient. prognosis (prog-no-sis): a prediction of the course of disease; the outlook for the chances of survival. progression: spreading or growing disease, with or without treatment. prophylactic (pro-fuh-LACK-tik) mastectomy: see mastectomy. prostate (pros-tate; note that there is no “r” in the second syllable): a gland found only in men. It is just below the bladder and in front of the rectum. The prostate makes a fluid that is part of semen. The tube that carries urine, the urethra, runs through the prostate. prostatectomy: surgical removal of all or part of the prostate gland. Prostate-specific antigen (PSA): a protein made by the prostate gland. Levels of PSA in the blood often go up in men with prostate cancer as well as other conditions. The PSA test is used to help screen for prostate cancer. It is also used to check the results of treatment. prostatitis (pros-tuh-TIE-tus): inflammation of the prostate. Prostatitis is not cancer. prosthesis (pros-thee-sis): an artificial replacement part of the body, such as a breast prosthesis. protein: a large molecule made up of a chain of smaller units called amino acids. Proteins serve many vital functions within and outside of the cell. 104 G L O S S A R Y, c o n t i n u e d protocol (pro-tuh-call): a formal outline or plan, such as a description of what treatments a patient will receive and exactly when each should be given. See also regimen. proton beam therapy: see conformal proton beam therapy. psychiatrist: a medical doctor specializing in mental health and behavioral disorders. Psychiatrists provide counseling and can also prescribe medicines. psychologist: a health professional who assesses a person’s mental and emotional status and provides counseling. psychosocial (sy-ko-so-shul): the psychological and/or social aspects of health, disease, treatment, and/or rehabilitation. pulmonologist: a doctor who has specialized experience and knowledge in the diagnosis and treatment of pulmonary (lung) conditions and diseases. Q quality of life: overall enjoyment of life, which includes a person’s sense of well-being and ability to do the things that are important to him or her. R RNA: see ribonucleic acid. radiation dose: the amount of radiation an object (such as human tissue) receives. There are several units used to describe radiation doses: rad (“radiation absorbed dose”): a basic unit of the amount of radiation transferred to an object. This measurement does not take into account the type of radiation, which can influence the effect on different body tissues. The rad has largely been replaced by the gray (see next). gray (Gy): the newer, international unit of measurement of radiation transfer. One gray equals 100 rads. (Therefore, one rad equals one centigray [cGy].) rem (“roentgen equivalent man”): a basic unit of radiation exposure which is based on both the dose and the type of radiation. Because of this, it is more commonly used to describe radiation exposure than is the rad. Often reported in units of millirem (mrem), which is one-thousandth of a rem. The rem is sometimes replaced by the sievert (see sievert). radiation oncologist: a doctor who specializes in using radiation to treat cancer. radiation therapist: a person with special training to work the equipment that delivers radiation therapy. radiation therapy: treatment with high-energy rays (such as x-rays) to kill or shrink cancer cells. The radiation may come from outside the body (external radiation) or from radioactive materials placed directly in the tumor (brachytherapy or internal radiation). Radiation therapy may be used to shrink the cancer before surgery, to destroy any remaining cancer cells after surgery, or as the main treatment. It may also be used as palliative treatment for advanced cancer. radical prostatectomy: surgery to remove the entire prostate gland, the seminal vesicles, and nearby tissue. 105 G L O S S A R Y, c o n t i n u e d radioactive implant: a source of high-dose radiation that is placed directly into or around a tumor to kill the cancer cells. See also brachytherapy. radiocontrast dye: any material used in imaging studies such as x-rays, MRIs, and CT scans to help outline the body parts being examined. These may be injected or ingested (drunk). Also called dye, contrast dye, radiocontrast medium. See also imaging studies. radiofrequency ablation (ray-dee-oh-free-kwin-see uh-blay-shun): treatment that uses highenergy radio waves to heat and destroy abnormal tissues. A thin, needle-like probe is guided into the tumor by ultrasound or CT scan. The probe releases a high-frequency current that heats and destroys cancer cells. RFA is sometimes used to treat tumors in the liver, and is being studied for use in several other areas of the body. radioisotope (ray-dee-oh-EYE-suh-tope): a type of atom that is unstable and prone to break up (decay). Decay releases small fragments of atoms and energy. Exposure to certain radioisotopes can cause cancer. But radioisotopes are also used to find and treat cancer. In certain imaging procedures, for example, radioisotopes are injected into the body where they then collect in areas where the disease is active, showing up as brighter areas on the pictures. See also imaging studies. radiologic technologist: a health professional (not a doctor) trained to position patients for x-rays, take the images, and then develop and check the images for quality. The films taken by the technologist are sent to a radiologist to be read. radiologist: a doctor with special training in diagnosis of diseases by interpreting or reading x-rays and other types of diagnostic imaging studies; for example, CT and MRI scans. radionuclide (ray-dee-oh-NOO-klide) bone scan: an imaging test which uses a small amount of radioactive contrast material given in the vein. The radioactive material settles in areas of the bone to which the cancer may have spread (“hot spots”), and shows up on the picture. See also imaging studies. randomized or randomization: a process in clinical trials that uses chance to assign participants to different groups that compare treatments. Randomization means that each person has an equal chance of being in the treatment and comparison groups. This helps reduce bias in the results that might happen, if, for example, the healthiest people all were assigned to a particular treatment group. See also control group and clinical trials. recurrence: the return of cancer after treatment. Local recurrence means that the cancer has come back at the same place as the original cancer. Regional recurrence means that the cancer has come back after treatment in the lymph nodes near the primary site. Distant recurrence is when cancer spreads (metastasizes) after treatment to distant organs or tissues (such as the lungs, liver, bone marrow, or brain). See also primary site, metastasis, and metastasize. red blood cells: blood cells that contain hemoglobin, the substance that carries oxygen to all of the cells of the body. See also anemia. regimen (reh-juh-men): a strict, regulated plan (such as diet, exercise, or medicine schedule) designed to reach certain goals. In cancer treatment, a plan to treat cancer. See also protocol. 106 G L O S S A R Y, c o n t i n u e d regional involvement or regional spread: the spread of cancer from its original site to nearby areas such as lymph nodes, but not to distant sites. See also metastasis. rehabilitation: activities to help a person adjust, heal, and return to a full, productive life after injury or illness. This may involve physical restoration (such as the use of prostheses, exercises, and physical therapy), counseling, and emotional support. relapse: reappearance of cancer after a disease-free period. See recurrence. relative 5-year survival rate: the percentage of people with a certain cancer who have not died from it within 5 years. This number is different from the 5-year survival rate in that the relative 5-year survival rate does not include people who have died from unrelated causes. See also 5-year survival rate. rem: see radiation dose. remission: complete or partial disappearance of the signs and symptoms of cancer in response to treatment; the period during which a disease is under control. A remission may not be a cure. rescue treatment: procedures or treatments such as bone marrow transplantation that “rescue” a patient’s immune system and blood-forming organs from the effects of high-dose chemotherapy. resection: surgery to remove part or all of an organ or other structure. respiratory therapist: under the direction of a doctor, the respiratory therapist gives breathing treatments and helps manage patients on ventilators. retinoids: vitamin A and synthetic compounds similar to vitamin A. ribonucleic acid (ri-bo-new-CLEE-ick acid): a nucleic acid found in all cells that transmits genetic messages between structures in the cell. Usually referred to as RNA. risk factor: anything that is related to a person’s chance of getting a disease such as cancer. Different cancers have different risk factors. For example, unprotected exposure to strong sunlight is a risk factor for skin cancer; smoking is a risk factor for lung, mouth, larynx, and other cancers. Some risk factors, such as smoking, can be controlled. Others, like a person’s age, can’t be changed. S sarcoma (sar-ko-muh): a malignant tumor growing from connective tissues, such as cartilage, fat, muscle, or bone. scan: a study using either x-rays or radioisotopes to produce images of internal body organs. See radioisotope. scintillation (sin-till-LAY-shun) camera: device used in nuclear medicine scans to detect radioactivity and produce images that help diagnose cancer and other diseases. See nuclear medicine scan. 107 G L O S S A R Y, c o n t i n u e d screening: the search for disease, such as cancer, in people without symptoms. For example, screening measures for prostate cancer include digital rectal examination and the PSA blood test. Screening may refer to coordinated programs in large groups of people. The same tests used for screening may also be used as diagnostic tests, which look for cancer in a person after there is some sign of a problem. For instance, a PSA test would be a diagnostic test if it was used in a man who had a lump on his prostate or urinary symptoms. secondary tumor: a tumor that forms as a result of spread (metastasis) of cancer from the place where it started. sedation (suh-day-shun): to make sleepy, calm, or relaxed. Drugs to cause sedation are often used along with medicines to numb an area for a procedure or certain types of surgery. See also anesthesia. sentinel lymph node biopsy: a newer procedure that might replace standard lymph node dissection. Blue dye and/or a radioisotope tracer is injected into the tumor site at the time of surgery and the first (sentinel) node that picks up the dye is removed and biopsied. If the node is cancer-free, fewer nodes are removed. See also lymph node and radioisotope. sex therapist: a mental health professional with special training in counseling people about sexual changes, problems, and communication (for example, after treatment for cancer). side effects: unwanted effects of treatment such as hair loss caused by chemotherapy, and fatigue caused by radiation therapy. sievert (Sv): the newer, international unit of measurement of radiation exposure. One sievert equals 100 rem. Often reported in millisieverts (mSv), which are thousandths of a sievert (or about 1/10 of a rem). See also radiation dose. sigmoidoscope (sig-moid-uh-scope): a slender, flexible, hollow, lighted tube about the thickness of a finger. It is inserted through the rectum up into the colon. This allows the doctor to look at the inside of the rectum and part of the colon for cancer or for polyps. The sigmoidoscope is connected to a video camera and video display monitor so the doctor can look closely at the inside of your colon. Polyps are small growths that can become cancerous. This test may be somewhat uncomfortable, but it should not be painful. sigmoidoscopy (sig-moid-AH-skuh-pee): a procedure in which a doctor can look into the rectum and the descending portion of the colon for polyps or other abnormalities. sign: a physical change you can see. Compare to symptom. simulation: a process involving special x-ray pictures that are used to plan radiation treatment so that the area to be treated is precisely located and marked for treatment. See also external beam radiation therapy. SKY: short for spectral karyotyping; a cytogenetic blood test used to see all the pairs of chromosomes in a cell in different colors. Also called chromosome painting. See also cytogenetics. social worker: a health professional who helps people find community resources and provides counseling and guidance to help with issues such as insurance coverage and nursing home placement. 108 G L O S S A R Y, c o n t i n u e d somatic mutation: a change in DNA that starts in one cell of the body after an embryo is formed. All the cells that arise from it will have the same mutation, which in some cases can form cancer. This kind of mutation is different from any inherited mutations that are present at birth in all the cells of the body. Somatic mutations are not passed on to children. Compare to inherited mutation. See also mutation and deoxyribonucleic acid. speech therapist: a person specially trained to work with people to help them speak clearly. Speech therapists help re-establish communication skills and also make sure that patients can easily eat and drink. sphincter (sfink-ter): a ring-like muscle that can open and close to control the passage of substances in the body. s-phase fraction: the percentage of cells that are replicating their DNA. DNA replication usually means that a cell is getting ready to split into 2 new cells. A low s-phase fraction is a sign that a tumor is slow-growing; a high s-phase fraction shows that the cells are dividing rapidly and the tumor is growing quickly. spinal tap: a procedure in which a thin needle is placed in the spinal canal to withdraw a small amount of spinal fluid or to give medicine into the central nervous system through the spinal fluid. Also called lumbar puncture or LP. spindle cell: a cell that, when viewed under a microscope, looks like a long oval. Some types of sarcomas, melanomas, and carcinomas have this type of cell. There are also normal cells of the body that are shaped like spindles. spiral CT: a special scanner that takes cross-sectional pictures around the body. See also computerized tomography. sputum cytology (spu-tum sy-tahl-uh-jee): a study of phlegm cells under a microscope to see if they are normal or not. squamous (skway-mus) cell carcinoma (car-sin-o-mah): cancer that begins in the flat, nonglandular cells of the body, for example, the skin or the lining of the body’s organs. staging: the process of finding out whether cancer has spread and if so, how far; that is, to learn the stage of the cancer. There is more than one system for staging different types of cancer. The TNM staging system, which is used most often, gives 3 key pieces of information: • • • T refers to the size of the tumor N describes whether the cancer has spread to nearby lymph nodes, and if so, how many M shows whether the cancer has spread (metastasized) to other organs of the body Letters or numbers after the T, N, and M give more details about each of these factors. To make this information clearer, the TNM descriptions can be grouped together into a simpler set of stages, labeled with Roman numerals (usually from I to IV). In general, the lower the number, the less the cancer has spread. A higher number means a more serious cancer. 109 G L O S S A R Y, c o n t i n u e d The 2 main types of staging are: • • clinical staging: an estimate of the extent of cancer based on physical exam, biopsy results, and imaging tests. pathologic staging: an estimate of the extent of cancer by studying the samples removed during surgery. standard therapy: standard treatment. See therapy. stem cells: any type of cell that may mature into different types of cells. In cancer treatment, they usually are the immature blood cells found in the bone marrow and in the blood. Even though they start out the same, these stem cells can mature into all types of blood cells. stem cell transplant: procedure used to restock the bone marrow when it has been destroyed by chemotherapy, radiation, or disease. Stem cells can be taken from bone marrow or circulating blood to be transfused into the patient. Stem cells may be the patient’s own (autologous), or may come from someone else (allogeneic). Bone marrow transplants (BMTs) were the first method for replacing stem cells. stenosis (steh-no-sis): a narrowing (stricture) of a duct or canal. stent: a very small tube or “straw-like” device that is inserted to support and hold open a tubeshaped organ, such as a blood vessel or intestine. stereotactic needle biopsy (steer-e-o-TACK-tick buy-op-see): a method of needle biopsy that is useful in some cases in which calcifications or a mass can be seen on mammogram but cannot be felt. A computer maps the location of the mass to guide the placement of the needle. See also needle aspiration and needle biopsy. stereotactic radiosurgery: this new treatment method focuses high doses of radiation at a tumor while limiting the exposure that normal tissue receives. The treatment may be useful for tumors that are in places where regular surgery would harm essential tissue, for example, in the brain or spinal cord, or when the patient’s condition does not permit regular surgery. sterility: the inability to have children, which can result from some types of cancer treatment. Also known as infertility. stoma: an opening, especially an opening made by surgery to allow elimination of body waste. See also colostomy, ileostomy, and urostomy. stomatitis (sto-muh-TIE-tus): inflammation or ulcers of mouth area. Stomatitis can be a side effect of some kinds of chemotherapy. supraclavicular (sue-pruh-clah-VICK-you-lar) lymph nodes: lymph nodes that are found just above the collarbone (clavicle). surgeon: a doctor who operates. surgical biopsy: removal of tissues using open surgery so that the tissues can be looked at under a microscope to find out if they contain cancer cells. Also called open surgical biopsy. Biopsies may also be done laparoscopically, or with thin needles. See biopsy, laparoscope, and fine needle aspiration biopsy. 110 G L O S S A R Y, c o n t i n u e d surgical oncologist: a doctor who specializes in using surgery to treat cancer. survival rate: the percentage of people still alive within a certain period of time after diagnosis or treatment. For cancer, a 5-year survival rate is often given. This does not mean that people can’t live more than 5 years, or that those who live for 5 years are necessarily permanently cured. See also relative 5-year survival rate. survivor: not generally used as a medical word, survivor can have several different meanings when applied to people with cancer. Some people use the word to refer to anyone who has been diagnosed with cancer. For example, someone living with cancer may be considered a survivor. Some people use the term when referring to one who has completed cancer treatment. And still others call a person a survivor if he or she has lived several years past a cancer diagnosis. The American Cancer Society believes that each individual has the right to define his or her own experience with cancer and considers a cancer survivor to be anyone who defines himself or herself this way, from the time of diagnosis throughout the balance of his or her life. survivorship: the state of being a cancer survivor, that is, having been diagnosed with cancer. See also survivor. synchronous (sin-kruh-nus): at the same time; for example, cancer in both breasts at the same time is synchronous. symptom: a change in the body caused by an illness or condition, as described by the person experiencing it. Compare to sign. synergistic (sin-er-jis-tick): acting together. A synergistic agent can act together with other agents to produce an effect greater than that of the sum of each one acting alone. Some chemotherapy drugs act synergistically. systemic (sis-tem-ick) disease: in cancer, this term means that a cancer that started in one place has spread to distant organs or structures. systemic therapy: treatment that reaches and affects cells throughout the body; for example, chemotherapy. T TNM staging system: see staging. tamoxifen (tuh-mok-si-fin): this drug blocks the effects of estrogen on many organs, such as the breast. Estrogen promotes the growth of some breast cancers. Research suggests that tamoxifen may lower the risk of breast cancer in women with certain risk factors. targeted therapy: treatment that attacks some part of cancer cells that make them different from normal cells. Targeted therapies tend to have fewer side effects than the general chemotherapy drugs. Taxol: a drug first made from the bark or needles of yew trees that can now be made in the laboratory. It is used to treat breast, ovarian, and other types of cancer. terminal: generally understood to mean that the cancer is no longer considered curable, and the patient is dying. 111 G L O S S A R Y, c o n t i n u e d testicles (tess-tick-ulls): the male reproductive glands found in the scrotum. The testicles (or testes) produce sperm and the male hormone testosterone. testosterone (tes-toss-ter-own): the male hormone, made mostly in the testes. It stimulates blood flow, growth in certain tissues, and the secondary sexual characteristics. In men with prostate cancer, it can also make the tumor grow. therapy: any of the measures taken to treat a disease, treatment. See also alternative therapy, complementary therapy, and unproven therapy. thoracic surgeon: a doctor who operates on organs in the chest cavity. thrombocytopenia (throm-bo-sy-toe-PEEN-e-uh): a decrease in the number of platelets in the blood; can be a side effect of chemotherapy. See platelets. tissue: a collection of cells, united to perform a particular function. T-lymphocytes (limf-o-sites) or T-cells: white blood cells made in the thymus gland. They produce cytokines and play a large role in the immune response against viruses, transplanted organs and tissues, and cancer cells. See cytokines. toxicity (tock-sis-i-tee): in medical treatment, the harmful effects of a medicine or treatment, especially at higher doses.trachea (tray-key-uh): the “windpipe.” The trachea connects the larynx (voice box) with the bronchi (the 2 large air passages that lead into the lungs) and serves as the main passage for air coming from the nose and mouth into the bronchi and lungs. tracheostomy (tray-key-ah-stuh-me): surgery to create an opening of the trachea through the neck. See trachea. transrectal ultrasound (trans-rec-tul ull-truh-sound): the use of sound waves to create a picture of the prostate on a screen to help detect tumors. Also called TRUS. transverse rectus abdominus (trans-verse rek-tus ab-dom-in-us) muscle flap procedure: a method of breast reconstruction in which tissue from the lower abdominal wall which receives its blood supply from the rectus abdominus muscle is used. The tissue from this area is moved up to the chest to create a breast mound. An implant is usually not needed. Moving muscle and tissue from the lower abdomen to the chest results in flattening of the lower abdomen (a “tummy tuck”). Also called a TRAM flap or rectus abdominus flap procedure. tumor: an abnormal lump or mass of tissue. Tumors can be benign (non-cancerous) or malignant (cancerous). tumor bank: a collection of many hundreds of patients’ tumor specimens that are stored for future use and research to understand the biology of cancer as well as research to identify new targets for the development of new therapies. tumor flare: short-term worsening of symptoms or cancer markers. tumor markers: substance produced by cancer cells and sometimes normal cells. They are not very useful for cancer screening because other body tissues not related to a cancer can produce the substance, too. But tumor markers may be very useful in monitoring for response to treatment when a cancer is diagnosed or for a recurrence. Tumor markers include CA 125 112 G L O S S A R Y, c o n t i n u e d (ovarian cancer), CEA (GI tract cancers), and PSA (prostate cancer). tumor necrosis (neck-row-sis) factor (TNF): a substance given off by activated white blood cells that can cause the death of tumor cells. See also necrosis. tumor suppressor genes: genes that slow down cell division or cause cells to die at the right time. Alterations of these genes can lead to too much cell growth and development of cancer. U ultrasound: an imaging method in which high-frequency sound waves are used to outline a part of the body. The sound wave echoes are picked up and displayed on a television screen. Also called ultrasonography. umbilical cord blood transplant: the use of stem cells in blood removed from the umbilical cords of newborns (a very rich source) to replace the blood-forming cells in patients whose own blood-forming cells have been destroyed by radiation or chemotherapy. unilateral: affecting one side of the body. For example, unilateral breast cancer occurs in one breast only. Compare to bilateral. unproven therapy: any therapy that has not been scientifically tested and approved. unstaged cancer: cancer that has been diagnosed but has not yet been staged, so that the full extent of the cancer is not yet known. See staging. urethra (yoo-ree-thruh): the tube that carries urine from the bladder to the outside. In women, this tube is fairly short; in men it is longer, passing through the penis, and it also carries the semen. urine cytology (yur-in sy-tahl-uh-jee): urine is examined under a microscope to look for cancerous and precancerous cells. Cytology can also be done on bladder washings. Bladder washing samples are taken by placing a salt solution into the bladder through a tube (catheter) and then removing the solution for testing. urologist (yur-ol-uh-jist): a doctor who specializes in treating problems of the urinary tract in men and women, and of the genital area in men. urostomy (yur-os-tuh-me): surgery to send urine through a new passage and then through an opening in the abdomen. In a continent urostomy, the urine is stored inside the body and drained a few times a day through a tube placed into an opening called a stoma. uterine fibroid tumor (yew-ter-in fi-broyd too-mer): a non-cancerous tumor that is made of fibrous or connective tissue. It is the most common tumor found in women. It can be in the uterine wall or protrude into the lining of the uterus. Usually there are no symptoms but it can cause abnormal bleeding and other symptoms depending on its size and location in the uterus. It is also called fibroma. uterus: the womb; the pear-shaped organ in women that holds and nourishes the growing embryo and fetus. The uterus has 3 areas: the body or upper part; the isthmus or the narrowed central area; and the cervix, the lower portion. 113 G L O S S A R Y, c o n t i n u e d V vaccine: a modified version of a germ or other substance related to a disease, usually given by injection. It is used to stimulate the immune system to resist that disease for a period of time, or even permanently. Development of cancer vaccines is the subject of intense research. vagina (vuh-jie-nuh): the passage leading from the vulva (the female genital organs that are on the outside of the body) to the uterus. virtual colonoscopy: examination of the colon for polyps or masses using special computerized tomography (CT) scans. The images are combined by a computer to make a 3- dimensional (3-D) model of the colon, which doctors can “travel through” on a computer screen. It is not yet clear if this new technique is as effective as other screening methods for colon cancer. See computerized tomography and colonoscopy. virus: very small organisms (micro-organisms) that cause infections. Viruses are too small to be seen with a regular microscope. They reproduce only in living cells. W watchful waiting: in some cases of prostate cancer, close monitoring that is done instead of starting active treatment right away. This may be a reasonable choice for older men with small tumors that might grow very slowly. If the situation changes, active treatment can be started. Also called expectant management. white blood cells (WBCs): blood cells that help defend the body against infections. There are many types of white blood cells. Certain cancer treatments such as chemotherapy can reduce the number of these cells and make a person more likely to get infections. wire localization: a method used during a surgical breast biopsy when the lump is hard to find or when there is an area that looks suspicious on the x-ray. A thin, hollow needle is placed into the breast and x-rays are taken to guide the needle to the area in question. A fine wire is inserted through the center of the needle. A small hook at the end of the wire keeps it in place. The hollow needle is then removed, and the surgeon uses the path of the wire as a guide to find the abnormal area to be removed. X x-rays: one form of radiation that can be used at low levels to produce an image of the body on film or at high levels to destroy cancer cells. Last Medical Review: 3/25/2008 4/23/2008 Last ©2008 American Cancer Society 114 Revised: PERSONAL RECORDS & JOURNALS PERSONAL RECORDS & JOURNALS INFORMATION RECORD Name: __________________________________________________________________________________ Telephone Number: ________________________________________________________________________ Hours: __________________________________________________________________________________ (if you need to, call and ask for your Nurse) After hours, weekends, holidays: (210) 593-5700 — Ask for your Primary Doctor Diagnosis: _______________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 115 QUESTIONS TO ASK YOUR DOCTOR ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 116 NAMES OF MEDICATIONS AND DOSAGES ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ Have available: 1. Record of your last blood count: WBC, platelets, ANC 2. Date of last chemotherapy treatment 3. Your doctor’s name 4. Your nurse’s name & telephone number 5. Emergency telephone number 117 118 Date Medication Dosage Given by NAMES OF MEDICATIONS AND DOSAGES Pre-Meds Notes MEDICATION ALLERGY RECORD List Medication Allergies Reaction 119 TEMPERATURE & BLOOD PRESSURE RECORD Date Time Temperature 120 Date Time Blood Pressure COMPLETE BLOOD COUNT (CBC) RECORD Date WBC hgh hct 121 Platelet NE% / segs bands AGC SURGERIES & DIAGNOSTIC TESTS RECORD ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 122 PERSONAL RADIATION TREATMENT RECORD Mon. Tues. Wed. Thur. 123 Fri. Sat. Sun. CALENDAR OF ACTIVITIES Mon. Tues. Wed. Thur. 124 Fri. Sat. Sun. NOTES & JOURNAL ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 125 NOTES & JOURNAL ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 126 NOTES & JOURNAL ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ 127 ALL DOCTORS INVOLVED IN YOUR CARE Doctor Telephone Number 128 INDEX INDEX INDEX Page Addresses & Telephone Numbers-Local businesses . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30-32 Admissions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Blank Calendar . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 123-124 CBC Record . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 121 Chemotherapy. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35-48 Clinical Cancer Research . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15-19 Clinical Trials . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15-19 CyberKnife . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51, 52, 81 Diet, Nutrition & Complementary Therapies. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 Electronic Medical Records. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Emergencies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5 Explanation of Charges, Financial & Insurance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-13 Glossary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 71-114 Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 129 Information Record . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 115 Insurance. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-13 Image Guided Radiation Therapy (IGRT) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50, 91 Intensity Modulated Radiation Therapy (IMRT) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50, 62 Introduction-English . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 Introduction-Spanish. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Locations/Maps . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 Medication Allergy Record . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 119 Names of Medications & Dosages. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 117 Notes & Journal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 125-128 Notice of Privacy Practices (HIPAA) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-13 Parking . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 Patient Advocacy. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Patient Rights & Responsibilities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-8 Personal Records & Journals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 115-128 Privacy Policy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-8 Questions & Answers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33-69 Questions Commonly Asked by Patients Taking Chemotherapy. . . . . . . . . . . . . . . . . . . . . . . . . 35-48 Questions Commonly Asked by Patients Taking Radiation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 49-69 Questions to Ask your Doctor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33-34 Radiation Therapy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 49-69, 123 Research . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15-19 Resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29 Support Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21-32 Temperature Record . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 120 Volunteer Auxiliary. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22 Wellness Center/Spa. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 129 Please let us know if this book has been helpful. We appreciate your comments and suggestions. Contact Patient Advocacy at (210) 593-2652 or patient.advocacy@stoh.com, Monday-Friday 8:00 a.m. - 5:00 p.m. 130
© Copyright 2025