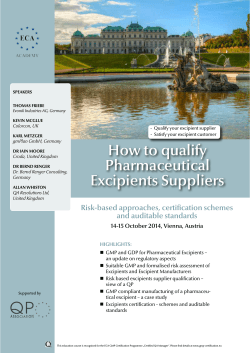
PHARMACY european INDUSTRIAL FEATURES
european INDUSTRIAL PHARMACY FEATURES 4 7 11 14 18 19 22 THE POTENTIAL IMPACT OF ICH Q8, 9 & 10 ON THE QUALIFIED PERSON The QP is attracting more and more duties and responsibilities which will require more delegation and management involvement by Richard Smalley FRAMEWORK FOR A CONTINUING PROFESSIONAL DEVELOPMENT (CPD) – A UK PERSPECTIVE UK pharmacists wishing to register with the new General Pharmaceutical Council will need to commit to CPD and submit regular records. This article tells you why and how. by Fred Ayling HOW TO ACHIEVE EFFECTIVE COMPLIANCE WITH EU GMP PART II IN API MANUFACTURE Dealing with practical aspects of compliance – an auditor’s tour of the QC laboratories. by Norman Franklin NEAR-INFRARED SPECTROSCOPY: A POWERFUL TOOL FOR PAT/QBD NIR has a wide range of applications in the pharmaceutical industry in production and quality assurance. by Emil W Ciurczak THE NEXT FIFTY YEARS: DEVELOPING OUR CORE VALUES FOR A CHANGING WORLD Report from PGEU symposium, Stockholm, 15 June 2009. by Pär Tellner THE INDUSTRIAL PHARMACIST’S ROLE IN PROVIDING PATIENT INFORMATION The importance of the pharmacist is emphasised. by Roland Schots SAFER MEDICINES SUPPLY – ANTICOUNTERFEITING USING 2-D BARCODING The Data Matrix 2-D code is described. by Inger Näsman REGULARS 3 20 21 24 26 27 28 EDITORIAL COMMENT REGULATORY REVIEW NEWS FROM THE EIPG PHARMACEUTICAL FORUM BOOK REVIEW JOB VACANCIES DATES FOR YOUR DIARY ISSUE 4 • OCTOBER 2009 www.industrialpharmacy.eu www.eipg.eu Associate Editors european INDUSTRIAL PHARMACY Belgium: Philippe Van der Hofstadt Bulgaria: Valentina Belcheva Issue 4 October 2009 Czech Republic: Miloslava Rabiskova ISSN 1759-202X Denmark: Michiel Ringkjøbing Elema EDITOR Joe Ridge, MRPharmS PRODUCTION Sue Feather Finland: Tuula Lehtela France: Jean-Pierre Paccioni SUBSCRIPTIONS Jill Monk Germany: Armin Hoffmann EDITORIAL BOARD Michael Anisfeld Michael Gamlen Linda Hakes Larry Hurst John Jolley Pär Tellner Great Britain: Jane Nicholson Greece: Kiriasis Savvas Hungary: Sylvia Marton European Industrial Pharmacy is published three times a year by: Euromed Communications Ltd Passfield Business Centre, Lynchborough Road, Passfield, Liphook, Hampshire GU30 7SB Ireland: Anna O’Mahony Italy: Piero Iamartino Latvia: Inta Saprovska Malta: Claude Farrugia Netherlands: Ineke Kleefsman, Michiel Storimans Portugal: bastonaria@ordemfarmaceuticos.pt Tel: +44 (0)1428 752222 Fax: +44 (0)1428 752223 Email: info@euromed.uk.com www.industrialpharmacy.eu Annual subscription rate £58 european INDUSTRIAL PHARMACY Spain: Mercé Pujol discussion group: www.pharmweb.net/gmp.html Sweden: Pär Tellner Switzerland: Renato Kaiser GMP Forum The online discussion group for industrial pharmacy www.pharmweb.net/gmp.html Views expressed in European Industrial Pharmacy are those of the contributors and not necessarily endorsed by the Publisher, Editor, Editorial Board, or by our corporate sponsors who accept no liability for the consequences of any inaccurate or misleading information ©2009 Euromed Communications Ltd Cover picture: Representation of microwells used for protein quantification assays. european INDUSTRIAL PHARMACY is the official publication of the European Industrial Pharmacists Group (Groupement des Pharmaciens de l’Industrie en Europe) www.eipg.eu 2 eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 E D I TO R I A L C O M M E N T Dear Colleagues I would like to welcome you to the fourth issue of the European Industrial Pharmacy journal which is dedicated to informing all Pharmacists working in this sector throughout Europe. You will notice that we have introduced a new format with the following features: ♦ A selection of GMP related questions and answers originating from the GMP Forum which our publisher, Euromed, sponsors. It is hoped that such Q&A will be an informative resource for many Pharmacists and Pharmaceutical Scientists working within a GMP, quality or regulatory setting. will change and provide what you would like to see, so please feel free to send us your suggestions and ideas to either myself (Luigi.G.Martini@gsk.com), to Jane Nicholson, Executive Director for EIPG (jane@nicholj.plus.com ) or directly to Euromed (info@euromed.uk.com). From the EIPG perspectives we have been very busy in responding to a number of working parties and European Commission Directives and we are working closely with EFPIA, on the variability in the interpretation and implementation of GMP initiatives. IPG has made it a priority to aid EFPIA and other related bodies in contributing to the following workstreams: ♦ Developing the role of the Qualified Person ♦ A job postings board to encourage firms and recruiting agencies to display opportunities within the sector. It is clear that during these challenging times we must continue to extol and advertise the skill sets of the pharmacy degree and the Industrial Pharmacist. A Pharmaceutical Industry without Pharmacists would be a very sorrowful state of affairs. We hope that the vacancy board will encourage more opportunities for Pharmacists. These changes have been created in response to feedback from you the readers. We intend to make this Journal a ‘living journal’ in that we ♦ Harmonising the implementation of new guidances and regulations originating from the Commission. EIPG has made representation to the following European institutions: ♦ Submission to the Commission on their proposals to amend Directive 2001/83/EC (anticounterfeiting measures) EIPG working parties have produced the following: ♦ Final draft of the EIPG Guidelines on Good Distribution Practice of Medicinal Products led by Claude Farrugia (Malta) ♦ Revisions to the EIPG Code of Practice for Qualified Persons led by John Jolley (Great Britain) and Piero Iamartino (Italy) ♦ Of particular note has been EIPG’s Continuing Professional Development guidance document for the regulatory affairs professional which has received widespread praise. I would like to thank the truly pan-European efforts of Valerie Lacamoire (France), Kelsey Mower (Great Britain) and Ursula Schickel (Germany) who have worked together extremely well and made this document the success it is. I would like to thank you all for your continued support and once again would encourage your feedback; this is truly your journal. With very best wishes ♦ Representation to the Committee for environment, public health and food safety and to the European Council on the Commission’s legal proposals on the provision of information to patients on prescription products. Gino Martini FRPharmS President, EIPG gmp-review news free news service for gmp revıew subscribers Monthly news service will keep you up-to-date on new developments in GMP and associated regulations. gmp-review news will be sent by email only to current gmp revıew subscribers. Subscribers should contact subs@euromed.uk.com to register european INDUSTRIAL PHARMACY • Issue 4 October 2009 3 THE POTENTIAL IMPACT OF ICH Q8, 9 & 10 ON THE QUALIFIED PERSON by Richard Smalley T he International Conference on Harmonisation has created and finetuned the series of inter-connected GMP guides ICH Q8, Q9 and Q10. These are possibly the most wide-ranging and influential GMP guides to have been written. They represent both a clear step-change in approach AND a more aligned strategy between the world’s biggest pharmaceutical markets. The intention of this article is not to review the detail of the guides, which most people are familiar with by now, but to identify the potential impact of implementing these on the European Qualified Person (QP). Conférence internationale sur l’Harmonisation a LQ10arédigé et mis au point la série de guides ICH Q8, Q9 et de BPF (GMP) interdépendants. Ils pourraient s’agir des guides de BPF les plus exhaustifs et les plus influents jamais rédigés. Ils représentent à la fois un changement progressif évident dans leur approche ET une stratégie plus concertée entre les plus grands marchés pharmaceutiques du monde. Le but de cet article n’est pas d’examiner les guides en détail, qui sont déjà bien connus par la majorité des personnes, mais d’identifier la portée potentielle de leur mise en œuvre sur la « Personne qualifiée » à l’échelle européenne. As some background information, different bodies including the EFPIA Adhoc GMP Team have focused on the growing challenges to the role of the QP and view the situation with concern. GMP developments are resulting in increased regulatory responsibilities and often more pressure on Quality Assurance departments. As a general trend, increased automation/instrumentation means more data are generated and potentially there is more to review. Whilst Annex 16 allows QPs to delegate routine duties to appropriate personnel, increasing delegation does not mean abdication of accountability. RICHARD JOHN SMALLEY is Associate Director, Global Quality Assurance, UCB Pharma SA, Brussels, Belgium. He is a member of the PQG team creating a guide for Supply Chain Risk Management for publication in 2009. 4 It is now universally recognised that the economic and regulatory environment in which the pharmaceutical industry exists is fundamentally different to that 20 years ago. The pressure on manufacturers to provide consistent profits in the face of falling numbers of new blockbuster drugs and the reduced prices that national health services/governments will pay for medicines have provided the impetus for making cost savings. In parallel with this has been strong encouragement, from the FDA in particular, of key initiatives that could change the way that companies develop, control and release their products. All of this describes the “what” relating to the ICH guides, but the “how” is in practice somewhat trickier. A big part of the “how” problem is “who” will be responsible for leading, managing and making key decisions? There are differences in the breadth of responsibilities and management seniority of QPs across Europe, with some being limited to batch review and others taking the senior role of a manufacturing site. Commonly the QP is regarded as the most senior Quality Assurance person in any manufacturing site’s organisation with direct responsibility for all aspects of both the effective operation of the quality system and product quality. Therefore, for the implementation of the ICH guides, the QP as usual will be the meat in the sandwich between “operations” and the Competent Authorities; it is expected that they will feel a lot of pressure as both the “arbitrator of common sense” and the “protector of the patient”. ICH Q8 implications The agreed “Desired State” will result in: ♦ Specifications being based on a mechanistic understanding of how formulation and process factors impact product performance. ♦ A continuous “real time” assurance of quality. ♦ QPs should have more confidence as patient safety is being protected by more robust manufacturing processes firmly based on robust knowledge of the product. In order to do this, QPs in future must understand the whole process at this level and use their knowledge to make decisions. To do this effectively, QPs increasingly must have a strong understanding of statistical techniques since these are necessary to extract information from data. Whilst they might not perform this step, they must eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 THE POTENTI AL IMPAC T OF ICH Q8, 9 & 10 ON THE QUALIFI ED PERSON (Cont.) understand it and then the information must be evaluated by the QP to obtain knowledge. Finally such knowledge can then be used to make effective decisions (Figure 1). In future Marketing Authorisations will define a ‘Design Space’, but who will Regulatory Agencies/Competent Authorities hold accountable for ensuring that there is a system for managing changes within the Design Space? The simple answer is probably the Qualified Person! Also in future, changes made within the Design Space will not require regulatory submissions, so who will approve changes within the Design Space? Other questions are: ♦ How is the QP going to manage their knowledge when batch process settings can be changed within the Design Space? ♦ How will this be managed in practice by the “Pharmaceutical Quality System”? And the answers to all of these are (probably) that it is up to the QP to decide… On a highly positive note, specifications will be based on the mechanistic understanding of how formulation and process factors impact product performance. Therefore, with a greater “knowledge window” and clearer scientific justifications for the specifications, this should mean that fewer greyarea decisions need to be made by the QP, since fewer grey areas will exist. One thing that will not change is that whilst it may also be easier to make decisions if the required knowledge exists, the regulatory position will probably remain that “Out Of Licence is Out Of Licence !” ICH Q9 implications Many of us have already experienced much more emphasis on formal risk management than ever in the past. The MHRA have commented (Ian Trussell, MHRA speaker at the QP Symposium 2008) that many troubles anyone who has experience of the Risk Assessment tools being applied (eg. in other industries, in n Decisio Safety departments or within forward thinking companies). It is dge dependent on the training and Knowle experience of the people, the tool used and the accuracy of the data / tion Informa information (to name just a few). Will there be standard or accepted tools for Risk Analysis? …And if you don’t use these (but an alternative) will you be criticised? Will these tools Data be quick enough? eg. standard FMEA is thorough but time-consuming. When will a preliminary hazard Figure 1. Understanding the implications of analysis approach be enough? ICH Q8. companies inspected in 2007/2008 were still using Risk Assessments to “justify bad decisions” or incidents that had occurred but were not paying sufficient attention to the use of a full Risk Management process for proactively working on prioritised risks (Figure 2). The normal process of Risk Assessment and Risk Control will conclude with a final risk acceptance decision, leading to the question “Who is going to be the final approver of Risk Acceptance documents?” Once again the EU regulatory authorities may well be tempted to say “The Qualified Person”, if the decision has the potential to impact product quality, safety or efficacy. (Just try and prove that it doesn’t and even then you’ll probably still need a QP to sign this justification.) Therefore it is important that a company’s internal procedures are clear on where the responsibility lies. This is somewhat helped by Annex 20 being issued but the bigger question of “Will this fully clarify the ‘QP discretion’ conundrum?” is still unanswered. Risk Management is a process, so in principle the QP need not get involved but could just review the output. The potentially variable standard of the output is what european INDUSTRIAL PHARMACY • Issue 4 October 2009 There is obviously still work to do here, but the answers are capable of being generated from this guidance. The problem can be pre-existing regulatory positions that could be seen as being “exceptions to the rule” or taking precedence over the logic of balanced risk. There are efforts being made to clarify the what, when and how, which are questions not clearly answered by ICH Q9: ♦ BARQA guide to implementing Quality Risk Management has been issued. ♦ PQG guide for Supply Chain Risk Management (for use by both pharmaceutical company supplier management departments and by suppliers to the pharmaceutical industry) will be circulated for consultation in Q2 2009. On a final note it is good to see that MHRA accepts the benefits of Risk Management (see Hampton Report and MLX 345 consultation) for its risk-based inspection programme, covering high and low risks for GLP, GCP, GPvP, GMP, GDP. ICH Q10 implications Existing, established GMPs require that: ♦ The QP should be involved in the implementation and 5 THE POTENTI AL IMPAC T OF ICH Q8, 9 & 10 ON THE QUALIFI ED PERSON (Cont.) maintenance of the Quality Management System. Initiate Quality Risk Management Process ♦ The QP should ensure that the Product Quality Review is performed in a timely manner and is adequate. Risk Identification Risk Analysis Risk Evaluation unacceptable Risk Communication ICH Q10 very clearly requires that “senior management” is ultimately responsible for the Quality System. However, the task of developing and maintaining an effective quality system is going to be delegated and the obvious (but overloaded) recipient would be yet again “The Qualified Person”. My personal hope is that the QP should NOT have to be the architect and guardian of the Pharmaceutical Quality System (PQS), but rather the QP should be an auditor of the PQS. To achieve this, the QP must monitor and be able to influence the content and implementation of the PQS. Risk Assessment Risk Control Risk Reduction Risk Acceptance Output/Result of the Quality Risk Management Process An area that is of great interest to many in the changing environment we now work in is subcontractor control. Here, the QP needs to assure the basics of: Risk Review Review Events ♦ The existence of a written contract. ♦ Any proposed changes are in accordance with the MA. ♦ A system has been used to assess the competence of the contract acceptor. ♦ All products delivered by the contract acceptor comply with the specification and are released by a QP. The QP needs to manage this risk and ensure that the quality system includes: ♦ Formal agreement of “Must Haves”. ♦ Excellent systems for communicating changes. ♦ Excellent systems for review. Details which still need to be worked out, and we can only speculate on them, including how this will affect Annex 16 of EU GMP. We can also hope that universal 6 Figure 2. Risk management. acceptance of the Q10 standard will help MRAs between US and EU. Key messages The ICH Quality guides that are now in place and being developed mean that QPs must, in future, have a good understanding of statistical techniques for data interpretation. The QP if not accountable for Design Space changes, the QRM process, the final Risk Acceptance decision and the effectiveness of the PQS, will certainly be seen by Competent Authorities to hold a key role. It is clear that the regulators will take action against irresponsible, negligent and unprofessional QPs, and this is only right and proper in order to protect patients. However, with involvement and responsibility increasing further, the risk of QPs being over-worked, over-stressed and not supported adequately becomes greater than ever before. It is therefore vital for QPs to keep up with the evolving expectations in order to be able to assist in implementing the new paradigm. Due to the demands on their time, the role of QP will require even more delegation and even more management activities. GMP Forum The online discussion group for industrial pharmacy www.pharmweb.net/gmp.html eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 FRAMEWORK FOR A CONTINUING PROFESSIONAL DEVELOPMENT (CPD) – A UK PERSPECTIVE by Fred Ayling 2010, a new regulator, the General Pharmaceutical InewnCouncil (GPhC), will be established in Great Britain. This body will take over the regulatory functions currently undertaken by the Royal Pharmaceutical Society of Great Britain. As part of these functions, the GPhC will implement mandatory CPD requirements for pharmacists and pharmacy technicians. The approach taken to CPD for pharmacists in Great Britain is significantly different to elsewhere in Europe. It is based on one that the RPSGB has been developing since 1998 and has been made available to pharmacists since 2002. At the point at which CPD remained voluntary, more than 20,000, over half of the membership, had made a start at recording their CPD. This is in comparison to other professions, where voluntary uptake has been informally reported at being in only single figure percentages. For a number of years the RPSGB’s Code of Ethics has required pharmacists to undertake and keep records of their CPD. It is anticipated that later this year the RPSGB will start asking pharmacists to submit their CPD records for review. When the GPhC is established in 2010 it will be able to ask pharmacists for CPD records dating back to 2008 and it is anticipated that it will require pharmacists to submit a record once every five years. What is different about CPD in Great Britain? FRED AYLING is Director of CPD Services, Ltd. He was the Royal Pharmaceutical Society’s CPD Manager from 1998 to 2007. email: fred@cpdservices.co.uk Most pharmacists will be used to an approach of accumulating a set number of points for hours of attendance at formal events over a period of time. These events may or may not be accredited. In Great Britain, this approach is referred to as continuing education rather than continuing professional development. european INDUSTRIAL PHARMACY • Issue 4 October 2009 Continuing professional development is different in a number of ways. It is perhaps best understood as an approach adopted by pharmacists for the selfmanagement of their development, based on a four-stage cycle. At the first stage of the cycle each pharmacist is expected to identify personal learning objectives that are specific, measurable, achievable, relevant and timed; they should also have a clearly identified performance outcome; that is, something the pharmacist will be able to do, either differently or better in some way. This approach is important because it helps the pharmacist to take ownership of their learning and it means that they focus their development on what is actually going to make a difference. Although this reflection stage of the management cycle is self-directed, it does not mean that pharmacists necessarily act in isolation when setting these objectives. Indeed, it would be best practice to ensure, where appropriate, that they involve others, such as colleagues, peers and those who use their services. This method of setting objectives fits well with an employer’s performance review systems, although it should be stressed that a pharmacist’s development will extend beyond this. Each person will have their own career aspirations and there may be aspects to their development that an employer is not interested in. Also there may be issues that a pharmacist would not be comfortable discussing with the person undertaking their performance review, or with their employer generally. It is also important to remember that many pharmacists in Great Britain are self-employed, or are an employee-owner without a line manager to undertake a performance review. It is at this reflection stage of the management cycle where competences may play a part. Competency audit may be used to identify learning objectives. Competences for industrial pharmacists have proved something of an issue in Great Britain. The RPSGB has published a set of ‘competences’ which are really just a high level list of the types of things that industrial pharmacists should know something about. There are only seven items in the list and it is not really detailed or thorough enough to be of much practicable use. Fortunately, the RPSGB’s 7 F R A M E W OR K F OR C P D – A U K P E R SP E C T I V E (C o n t . ) through discussion, observations and other means of learning-by-doing. That’s to say, we learn through experience every bit as much as we learn through attending courses. Reflection Evaluation Planning Action Figure 1. The learning cycle. electronic recording systems allow pharmacists to add their own competences into the system. These additional competences may be provided or set by an employer or by a relevant organisation, such as those for competent persons that are published by the European Industrial Pharmacy Group (EIPG). At the next stage of the management cycle, the pharmacist is asked to plan how they are going to address the learning objective they have identified. There are two aspects to this, firstly prioritising the objective and secondly, identifying appropriate activities. Clearly the pharmacist will have a number of learning objectives at any one time and so prioritising is important. They will need to provide a realistic target date for meeting the objective and to think about the degree of impact their learning objective will have on them, their employer or contracting body, colleagues and the users of their services or products. In terms of identifying appropriate activities, the RPSGB is not prescriptive. If the appropriate activity is informal, such as having a discussion with someone, reading a book or undertaking a web search, that is fine. If it is formal, such as attending a course, it does not need to be accredited. What is important is that the pharmacist describes why one activity is more appropriate than another. This provides great flexibility for the pharmacist and reflects the way we learn. We often learn 8 At the action stage of the cycle, the pharmacist undertakes the activities they have identified and then sums up the key learning points. This ‘summing up’ is important as it has been demonstrated that we only retain a fraction of the information that we are told when engaging in a learning event, whatever that may be. Two pharmacists engaging in the same learning event will take away different things. That is because they will come to the event with different levels of existing knowledge or skills and they will have different expectations in terms of what they want to go away with. Reflecting on their learning has a twofold benefit; it reinforces the key points they have learnt and provides a list that can be used in the future as a handy reference. In the final stage of the management cycle, the pharmacist evaluates their learning. Have they successfully addressed the learning objective they identified? If not, why not, and what are they going to do next, if anything? If the learning objective has been successfully addressed, how have they been able to apply what they have learnt in practice? What are they now doing that they didn’t do before? What feedback or indicators do they have on the effectiveness of their learning? Do they need to build on this; perhaps identify a new objective and so start the management cycle again? The CPD cycle? The management cycle described above is referred to as the CPD cycle. But in simple terms it is a management cycle that those involved in research or project management will be familiar with: identify, plan, act and evaluate. The RPSGB presents this cycle as in Figure 1. It refers to the identification stage as reflection. This is because the RPSGB wishes to promote a reflective approach to pharmacists’ development. This is based on the observations made by Donald A Schon in his book: The reflective practitioner: how professionals think in action. Schon observed that faced with the same event and the need to take action (make a decision, give certain advice, provide a solution and so on) professionals acted differently. This was because they brought their personal and professional experiences to bear when acting. Different professionals would provide different advice or come to different conclusions or solutions. It was not necessarily the case that one action was better or more right than another. It does follow though that if there are a range of actions in a given situation, some actions may be better than others and indeed some may be poor. The idea behind reflective practice is that it encourages the pharmacist to step back and understand that there are a range of actions and that the one they choose will be based, for good and bad, on their own experiences. By thinking this through, it is hoped that the pharmacist may be more objective and so make better decisions. So, at the identification stage, the RPSGB regards a pharmacist as reflecting on events to help them find the right or best learning objectives that arise out of them. A number of issues have arisen from this. Although pharmacists who have qualified in recent years will have been taught about reflective practice, GMP Forum The online discussion group for industrial pharmacy www.pharmweb.net/gmp.html eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 F R A M E W OR K F OR C P D – A U K P E R SP E C T I V E (C o n t . ) those who have been qualified longer may be less familiar with this concept and have less understanding of the term ‘reflection’. Also, it is not always the case that much reflection really needs to go on when identifying learning objectives. It is often quite clear and self-evident what learning needs to be undertaken as a result of a certain event. If someone asks us a straightforward question, we don’t need to do much or any reflection to realise what we need to know and that we need to go away and look the answer up! opportunity that you may learn something. On a personal note, I tend to simply refer to this stage of the CPD cycle as identification. I also regard reflective practice as happening at any stage, as at each stage I find myself making decisions that I have reflected on. For example, at planning I am reflecting on what I anticipate the impact of my learning will be and which activities are going to be appropriate based on previous experiences. Why CPD instead of CE? A common misconception about the CPD cycle is that it is an annual exercise; the pharmacist would sit down once a year, identify their objectives and spend the next year addressing them. Although taking time out once a year to do just this is good practice, learning objectives will arise at any time throughout the year and may need to be addressed in a couple of months, weeks, days or hours. So a CPD record is a live, ongoing document and it is possible to move through the cycle in hours or years, depending on the learning objective. When the RPSGB piloted CPD and launched it nationwide in 2002, it also allowed pharmacists to start their CPD at the action stage of the cycle. This meant that pharmacists could record CPD that occurred when a learning objective had not previously been identified, for example, reading a journal or attending a routine seminar without a learning objective in mind, but simply because there was an In 2007, the RPSGB allowed pharmacists to start their CPD at the planning and evaluation stages. Although a few pharmacists had requested this, the feedback I have received from most of the trainers supporting pharmacists is that this has added confusion and given no real benefit. It can be quite difficult to find examples of CPD that starts at these stages and my advice is to ignore this option unless you can see any specific benefits. When we looked at the research that had been undertaken in the area of continuing education, it was clear that there was no evidence that attending courses actually made a difference. One of the leading authorities in this area is Dave Davis and his team from the Faculty of Medicine, at the University of Toronto. In their review of the literature1, they made the observation that there is a ‘diminished impact of CME along this continuum’. The thinking in the field was that it was more important to accredit the learner rather than the course. A learner who is motivated and committed may attend a course that is poor but will not leave it at that; he or she will instead find another way of learning what needs to be learnt. This is not to say that courses are not an important part of professional development and, indeed, that some form of quality assurance is required. Continuing Education should not be relegated as CPD’s poor cousin but instead regarded as part of a wider process of CPD. The suggestion is that it is Skills Knowledge Attitudes european INDUSTRIAL PHARMACY • Issue 4 October 2009 important for pharmacists to take ownership of their learning and that each pharmacist will have his or her own starting point in terms of their knowledge, skills or competences and their own end point of where they need to be. It is also important that the approach to CPD encompasses all the manners in which we learn, including informal learning, as not to do so could lead to pharmacists not appreciating and engaging in all the development opportunities available to them. To bring about more effective development pharmacists were also encouraged to think about learning that would make a difference as they moved through the cycle. A professional develops over time. There are rarely big leaps, but more commonly it is the accumulation of lots of little bits of learning that can add up to something quite significant. CPD should be about continuous improvement and in developing their approach the RPSGB wanted to encourage pharmacists not just to think about what they don’t do well but what they already do well and how they could build on that. How can it be recorded? Pharmacists can record their CPD in three ways. There is an online recording system, CPD Online; PCbased software, CPD Desktop; or a paper-based system using a format provided by the RPSGB or a format accredited by them. CPD Online is by far the best format in terms of its functionality. More than 50% of pharmacists are recording their CPD in this way, that’s over 20,000 people. CPD Online allows pharmacists to tailor various aspects of the recording system, including competences and options from Skills Performance Attitudes Patient outcomes 9 F R A M E W OR K F OR C P D – A U K P E R SP E C T I V E (C o n t . ) other menus. It also allows pharmacists to share aspects of their CPD with others online. These may be friends and colleagues or their employer, so making it easier to integrate into employers’ HR systems. The pharmacist is in control of who sees what and when. Regular backups also mean that the pharmacist cannot accidentally delete their CPD record or lose it if their computer system crashes. A personal development plan that interacts with their CPD record is also provided to help the pharmacist identify learning objectives. Recording consists of a mixture of free text and selections made by means of checkboxes and dropdown menus. Once familiar with the system, it should take about 30 minutes to record one entry in a CPD record, taking in all four stages of the CPD cycle. Review and feedback CPD will be reviewed according to the good management practice described by the RPSGB reviewers. They will consider whether the learning objectives are specific, measurable, achievable, relevant and timed; whether there has been a thoughtthrough option appraisal at the planning stage; and whether the CPD has actually made a difference. The purpose of the review is primarily to look at how the pharmacist has been managing his CPD and to provide him with meaningful and formative feedback. Some of it will be used to establish whether the pharmacist has met the required standards, but most aspects will simply be used to provide feedback. For example, when receiving feedback the pharmacist will be able to see at a glance where his CPD has been focused in terms of competences. For good reasons, it may be quite narrow or broad and there is no reason why any two pharmacists should have the same focus. The intention is simply to provide feedback to help the pharmacist understand where they may take their professional development in the future. Although the RPSGB is taking a formative approach, they and the GPhC will need to set a minimum requirement. I do not expect it to be terribly taxing but then the intention is to engage pharmacists in a formative way and not to be heavy-handed. Reference 1. Davis D, O’Brien MAT, Freemantle N, et al. Impact of formal continuing medical education – do conferences, workshops, rounds and other traditional continuing education activities change physician behaviour or healthcare outcomes? JAMA 1999; 282: 867–874. the key to gmp gmp revıew gmp revıew is the first newsletter dedicated to the analysis of international pharmaceutical regulations and providing informed comment on good manufacturing practice. Researched and edited by an expert team, gmp revıew will provide you with a clear, practical guide to the often complex and jargon-ridden regulations that are continually being produced. See our website for details or call +44 (0)1428 752222 www.euromed.uk.com 10 eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 HOW TO ACHIEVE EFFECTIVE COMPLIANCE WITH EU GMP PART II IN API MANUFACTURE – An auditor’s tour of the QC laboratories by Norman Franklin This article describes an auditor’s tour of the Quality Control laboratory areas, covering analytical standards, OOS results, impurities, batch release, etc. ending with a walk through the laboratories. I f an audit team is conducting the audit, and this team consists of two specialists, one with a production background and one with a quality control background, they will already have split up, and the person with the quality control background will have transferred to the lab area whilst his (her) colleague was covering production. NORMAN FRANKLIN was a member of the ICH Q7a Expert Working Group and is now a Principal Associate of Interactive Consulting Associates GmbH, a GMP training and contract auditing company in Zug, Switzerland. E: norman.franklin@ interactive-consulting.ch Some of the checking of the “Laboratory Controls” (see Chapter 11) can, and should, be done before arriving on site, for example checking whether the API specification, the extent of the tests and the limits applied comply with the pharmacopoeia requirements (see §11.13). In particular it should have been checked if the impurities listed and limited are those listed in the pharmacopoeia and are ones liable to arise from the route of synthesis (see §11.13). If there are discrepancies here between the route of synthesis and the impurities tested this is a HIGH RISK for the patient. If the solvents used in the synthesis are not given in the flow sheet supplied with the Pre-Audit questionnaire it must be noted which solvents are used, from start to finish of the synthesis, and what limits are being applied; this can be compared later against the ICH limits for solvents. It is not usual in the Pre-Audit questionnaire to ask for copies of the specifications of the critical starting materials, but this should be reviewed on site (see §11.12). Analytical standards One of the topics that received very little attention in earlier GMP guides was the european INDUSTRIAL PHARMACY • Issue 4 October 2009 use of analytical standards. The FDA pointed out to other members of the ICH Q7 Expert Working Group (EWG) that, particularly in Asia, there was a lack of understanding of the administration and use of analytical standards. This author can only confirm that this problem is not limited to Asian API manufacturers, and lack of compliance with these sections is a HIGH RISK for the patient. Thus the auditor should check very carefully where the QC labs obtain their primary standards (see §11.17 and 11.18) and, even more important, how do they ensure that their secondary (or daily working) standards maintain the assigned assay value. It must always be remembered that if the secondary standard has lost 1% of its assigned value, but this has not been compensated for, then every batch of API test against this standard will have an assay value 1% higher than the true value (which can mean the batches are released with an assay value of 98.7% when in reality the true assay value is only 97.8%). The EU GMP Guide Part II gives, in §11.17 to 11.19 detailed advice to API manufacturers as to their responsibilities, and perhaps the most important sentence which the auditor should check is “Secondary reference standards should be periodically requalified in accordance with a written protocol” (see §11.19). In this context it is not acceptable to reanalyse the secondary reference standard just twice against the primary standard every 24 months just because the product is known to be stable for 24 months. Even a loss of 0.3% in the assay over this period, whilst acceptable in a stability study, will result in production batches being released with an assay value 0.3% higher than the true value. Out-of-specification results Knowing that the assay results are reliable is a prerequisite for knowing whether these (or any other results) are “Out-ofSpecification” (OOS). For the first time the concepts arising out of the BARR Judgement1 have been incorporated into an international GMP guide and are now an essential part of EU GMP. Thus it is NOT ACCEPTABLE just to repeat an analysis twice and accept the results if 2 out of the 3 test results meet the 11 EFFECTIVE C OMPLIANC E WITH EU GMP PART I I IN API MANUFACTURE (Cont .) specification limits. The principle of the Barr judgement is that if an analytical result does not meet the specification, either the product itself is out-of-specification and thus needs to be rejected, or the analytical results are incorrect. Each API manufacturer must therefore have a procedure for dealing with such OOS results (see §6.53 and §11.15). It is usual (and correct) for an auditor to ask to see a “flow sheet” which identifies the decision points and actions to be taken – step by step – if there is an OOS result. If an auditor has not found an OOS result when reviewing the laboratory records (the luck of the draw) then the procedures taken to resolve an specific OOS case as suggested by the API manufacturer can be used. However it must be remembered that this may be a “polished case” which does not reflect the investigations actually carried out in daily practice. It must also be remembered that an OOS can arise because the specification itself is too tight, or is not related to the capability of the process. The API manufacturer should have considered this possibility and reacted accordingly if the OOS is found time and time again. It must be remembered that OOSs are “critical deviations” because they could reflect the lack of quality of the batch of API involved. Thus they need to be resolved (see §2.22-4). In spite of some earlier comments to the contrary, it is not now necessary to treat the discontinuation of an analytical test as an OOS because no results were obtained to compare with the specification limit2. Nevertheless, such a discontinuation should be treated as a “deviation” and be explained. If a certain analytical test often needs to be discontinued then the reason for this needs to be thoroughly investigated (see §6.53) and an auditor should check this. It 12 is a RISK situation if certain tests need to be frequently re-run – can one rely on those which ran smoothly? Impurity profiles Very few API manufacturers have appreciated the implications of §11.2 particularly §11.21 and §11.22. This author frequently finds that API manufacturers confuse the “GMP Impurity Profile” with the impurity profile included in a Marketing Application (MA). Although the impurity profile in the MA will be part of the “GMP impurity profile” this latter is more of a “total fingerprint” of all the impurities detected even down to 10 or less ppm if they can be detected. For the manufacturer this “GMP impurity profile” is the fingerprint of the site where the product is made, and if it is suspected that material may be supplied from several different sites, but all carrying the name of the same exporting or importing company, then one needs to establish this “GMP impurity profile” for the site audited. Under such circumstances the auditors may be asked to take a sample themselves of the API in question at the site they are auditing (see §11.22). Such site switches are not only fraudulent but could be a HIGH RISK for the patient if a different synthetic route is followed with new and unknown impurities. The review of the Certificates of Analysis should have been carried out before leaving the home office, and thus the review on site should consist of checking the raw data “It is not acceptable just to repeat an analysis twice and accept the results if only 2 out of the 3 test results meet the specification limits” generated for the batches in question. This topic will also be covered later in this paper. Responsibility for batch release Coupled with the review of the Certificate of Analysis (CoA) should be the review of who is responsible for the release of the batches of API (see §2.14) and are these persons adequately educated and trained (see §3.10). It is also important to determine how this release is done (see §6.70), because basically, as the user of the API, the MP manufacturer places considerable trust in the persons and the procedures used at the API manufacturer. These topics are therefore HIGH RISK situations. Firstly, who carries out the release? These people are generally known, but there is not always a formal act to confirm this, nor are their signatures always on record to be checked against the signatures on the CoA. The auditor should be checking this carefully. It must be remembered that in the Haiti poisoning affair it was not possible to determine who had actually signed the CoA for the “Synthetic Glycol” and therefore this requirement was added by the members of ICH Q7a EWG (see §11.43). Knowing who these persons are enables one to check the education and experience of such persons (see §3.10). In spite of the Japanese requirement that these persons must be trained pharmacists (and the request by other competent authorities to only use a “Qualified Person” for such an assignment), the members of the EWG did not follow these requests and left the education and experience qualifications open. Thus an auditor can only record what education and training the “release persons” possess, but it may eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 EFFECTIVE C OMPLIANC E WITH EU GMP PART I I IN API MANUFACTURE (Cont .) be difficult to openly state “The qualifications and experience of the persons authorized to release batches of API are inadequate” as this is an “opinion” and not a “fact” and experienced auditors always try and just present the “facts” as found during the audit. It would however be possible to list the education and training of the persons responsible for release so that the MP manufacturer himself can judge whether he is willing to accept a CoA signed by such persons or this could be a HIGH RISK situation. As part of this assessment it should be checked HOW the release of a batch of API is carried out. There should be a “Check List” of documents which must have been reviewed and signed before release, eg. the laboratory reports with the signatures of the analyst who checked the records for accuracy (see §6.60); the BMR signed by production that they have checked these (see §2.3-3 and §6.52); the review of the BMRs by the Quality Unit (QU) for the correct and completed critical steps and parameters (see §2.22-3); the recorded check that the deviations have been reviewed (see §6.72) and closed out (see §2.22-4); and the check that any OOS investigations have been completed and resolved (see §6.72 and 11.15); and that the data finally required for the issue of a CoA is accurate and complete, (see §11.42), then the release procedure is a HIGH RISK situation because batches may be released without adequate control of the relevant data. Stability The auditor needs to cover the procedures and facilities used to monitor the on-going stability of the APIs produced on site. Although it is admitted that for inorganic APIs such as KCl, such studies have little relevance for the behaviour on storage (the natural stability programme was initiated some 50 “It is a risk situation if certain tests need to be frequently re-started” million years ago and has not yet been completed), nevertheless there should be an on-going stability programme in place, even if this is being carried out under contract. It important to check whether selected batches are being placed on stability (see §11.54), particularly if the audit of the change control system indicates that there have been major process or even equipment changes such as a new type of dryer for the API (see §13.16). If the stability testing programme is not being carried out in-house, where the auditor can check if the principles of ICH Q1A (RS) are being followed, then the contract with the stability testing laboratory should be checked (see §16.12) as should the evidence that samples have been shipped there over the last 15 months (see §11.54); preliminarily reports from the testing labs can also be checked, if they are available (see §11.55 and 11.56). This should be the case, otherwise it is a RISK situation as it is not known if the current batches of the API are as stable as the development batches. Retention samples Another section of the GMP guide for APIs that has also not always been understood is that on reserve or retention samples, in spite of the clear statement in the guide that the purpose of the reserve or retention sample is NOT for future stability testing. It is this statement which makes it clear that the packaging used to store the reserve or retention sample should protect it as far as possible from change during storage, so that when it comes to the future evaluation of european INDUSTRIAL PHARMACY • Issue 4 October 2009 the quality of the sample this should as far as possible reflect the quality AT THE TIME of RELEASE (see §11.70). Although incorrect packaging of the reserve or retention sample is not a real risk for the patient, it does indicate a lack of understanding of the EU GMP Guide Part II, (which may then be the case with other requirements, as was discussed earlier under the “GMP impurity profile). A walk through the laboratories It is usual to take a walk though the laboratories. Most laboratory managers are proud of their new equipment and like to demonstrate its capabilities – or may complain about their lack of space to the auditor(s) – (NEVER take sides during an audit – report the facts). As an auditor, however, one must be careful that one is not blinded by such advances in equipment design or capability unless the equipment can be correctly calibrated, and has been adequately qualified on installation. One can, however, use this tour to check simple items such as adequate identification of reagent containers, adequate records of calibration of equipment such as spectrophotometers, etc. (see §5.30 to 5.35), and that analytical procedures are easily accessible to the staff. One can also see at the lab bench what system is used to record the laboratory raw data, such as lab notebooks, preprinted sheets, or even test procedures where the analyst enters, in the empty boxes, the values read off or to be used in calculations (see §6.14). References 1. USA FDA v Barr Laboratories. Judgement and reasoning given by Judge Wolin on Feb 4 1993 in US NJ Circuit Court. 2. FDA Guidance for Industry. Investigating Out-of-Specification Test Results for Pharmaceutical Production US DHSS, FDA, CDER October 2006. 13 NEAR-INFRARED SPECTROSCOPY: A POWERFUL TOOL FOR PAT/QbD by Emil W Ciurczak A lthough near-infrared (NIR) was the first wavelength region outside of the visible to be discovered (by Sir William Herschel in 1800), it was not really used much for the first 150 years. By 1970, there were only a dozen or so papers published utilizing the technique. When Karl Norris (US Dept of Agriculture) introduced methods for determining moisture, oil, starch, and protein in the late 1970s and early 1980s, the interest in NIR soared. By the early 1980s, all shipments of grain from the US were analyzed by NIR. Since agricultural products are produced by, in essence, uncontrolled chemical processes, it was assumed that pharmaceutical products, manufactured by stringently controlled processes, should be easily monitored. DR EMIL W CIURCZAK has advanced degrees in Chemistry from Rutgers and Seton Hall Universities and has been in the pharmaceutical industry since 1970. Most of his research has been on pharmaceutical applications of NIR where he has published over three dozen articles in refereed journals and presented nearly two hundred technical papers. email: emil.ciurczak@gmail.com 14 In the early 1980s, quantitative work was being done at Glaxo (UK) by Ken Leiper. In the US (spurred on by EMEA suggestions), Sandoz (East Hanover, NJ, USA) was qualifying all its incoming raw materials by NIR: 100% testing of all lots! This was made possible by the Mahalanobis distance software developed by Dr. Howard Mark of Technicon. In 1987, Principal Component Analysis and Partial Least Squares software was introduced. Applications soared from that point. Some of these applications are highlighted by category. Basic theory Near-infrared spectra are the overtones and combinations of vibrations originating in the conventional or midrange infrared (2500 to 25,000nm or 4000 to 400cm-1). The main absorbances are from C-H, N-H, or O-H bonds, the skeletal modes being too small to be significant. As a consequence, hydrogen bonding strongly affects the spectra. Since most NIR spectra are generated on “as is” materials, scattering from powders and suspended solids is also a major contributor to sample spectra. Absorptivities in the NIR are much smaller (10-1000 times lower) than in the mid-range infrared (MIR), while the sources of radiation are stronger and the detectors orders of magnitude lower in noise. This combination allows analysts to use pure samples, yet allow them to measure low levels of analytes in complex samples. Since NIR samples were originally complex agricultural samples, where synthetic standards were impossible to create, new computational methods were needed. One of the greatest contributions of Karl Norris was his introduction of the Multiple Linear Regression algorithm. In his calculations, a decade before complex mathematics and computers were available several wavelengths were used as an extension of classical Beer’s law calculations. The wavelength most representing the analyte of interest is found and placed in a linear regression equation. Often, this wavelength does not represent a “pure” peak and therefore the linear function does not completely fit. In that case one or more other wavelengths, often representing the matrix, are added as either secondary factors or divisors, allowing an equation to be generated that gives satisfactory results. In 1987, Principal Components Analysis (PCA) was introduced. This matrix-algebra based computation uses all (or most) of the wavelengths of the spectra to generate equations describing the differences between materials. Thus, the fact that single wavelengths are difficult to isolate for a property of analyte became irrelevant. Adding chemical values to the equations generated quantitative equations capable of very fine work. Later that year, Partial Least Squares (PLS) was introduced. PLS, is similar to PCA, but uses the chemical values to produce “factors” for the equation rather than spectral differences. In short, PCA uses spectral difference, making it excellent for qualitative uses, while PLS measures how the spectra change with chemical or physical property changes, making it better at quantitative analyses. eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 NEAR-INFRARED SPEC TROSCOPY: A POWERFUL TOOL FOR PAT/ QbD (Cont .) Identity and quality While agricultural applications were usually quantitative, the first widespread application of NIR in Pharma was for qualifying incoming raw materials. While NIR spectra are not as “crisp” as the mid-range infrared (MIR) spectra with which analysts were accustomed, the ease of using as-is samples outweighs all the sample preparations. Using available software, the reflectance spectra of disparate raw materials (see Figure 1) can be used to generate domains in computer-space for estimation of both identity and quality of a material (Figure 2). Since the resultant NIR spectrum of any material is dependent upon both its chemical and physical properties, use of some variant of PCA gives, in essence, the “quality” of a material as well as its identity. What is meant by “quality?” Figure 1. NIR Reflectance Spectra of Several Common Pharma Raw Materials. [orange = mannitol, red = lactose, pink = povidone, green = starch) Using the spectral shifts, the physical properties of a “proper” raw material may be determined. There is no need to identify (at first) why a material is rejected by the software, a rejection simply means that it is not similar to previously analyzed samples. A library of acceptable materials, including all allowable variations of moisture, particle size, polymorphic form, degree of crystallinity and so forth is constructed. The software (available from nearly every instrument manufacturer) generates an equation which is then used to determine whether a new material is within acceptable parameters or not. [If not, compendial or functional tests may be run to ascertain acceptability; if acceptable, the spectrum is added to the library and a new equation is generated.] Quantitative applications Since NIR was originally used for quantitative analysis, it is not surprising that there are so many applications in Pharma. The leading application is for water. Not surprising, since water has the highest Figure 2. Cluster Analysis of several calcium and sodium salts of small acids. [For instance, calcium salts of propionate (orange), lactate (light blue), formate (green), and acetate (dark blue), sodium salts of acetate (purple) and propionate (brown).] Similar acid anions are easily separated by cation differences. Spectral differences are also based on crystal structure. european INDUSTRIAL PHARMACY • Issue 4 October 2009 15 NEAR-INFRARED SPEC TROSCOPY: A POWERFUL TOOL FOR PAT/ QbD (Cont .) absorptivity, as in MIR. However, unlike MIR, water is a nuisance in NIR and aqueous analyses are also routinely performed. First, in water analyses, the level of detection and quantification depends on the matrix. In a freezedried matrix, NIR can easily determine values below 0.1% water. In a fluid bed drier (FBD), several tenths of a percent are easily determined in a moving matrix. Since FBD moisture levels are usually set as “below 1.0%”, this level is most often sufficient. Tablets may be assayed for their active pharmaceutical ingredient (API) either in transmission or reflection mode quite easily. Again, the levels are best detected well above 0.1% API. One advantage is that all excipients are determinable; this allows determination of the true content uniformity of all the components within a tablet or capsule. Physical changes can also be easily quantified. Figure 3 shows a series of calibration samples made to quantify polymorphic changes in an API. Similar work has been done to determine the degree of crystallinity in excipients and drugs, even during a mixing or granulation process. This is an important feature, since crystalline changes during processing can affect the dissolution and/or bioavailability profile of a solid dosage form or its manufacturability. Using the proper models, a large number of analytes/physical parameters may be measured simultaneously in a single sample. This means that a raw material can simultaneously be identified and have its moisture, polymorphic form, and average particle size measured from a single sample scan. Work is being done on other physical parameters, important to PAT, such as porosity, crushability, surface area, and density in order to add these to the toolbox for routine screening of raw materials. Counterfeiting or adulteration Figure 3. Calibration curve for two polymorphic forms of an API (Active Pharmaceutical Ingredient) Figure 4. NIR chemical Image of tablet; various excipients and API are highlighted with false colors. The chemistry of each particle as well as its distribution are easily determined. (Courtesy of Malvern Instruments.) 16 The ability to determine all the materials within a material allows an analyst to determine counterfeit products. Using techniques such as NIR Chemical Imaging (Figure 4), the excipients can be determined as well as the active ingredient. Using PLS or PCA software, the physical attributes of a tablet (in QbD terms, the “process signature”) may be determined. The hardness, speed of production, etc. are all part of the “goodness” of a tablet, leading to changes in dissolution profile, degradation, etc. Recent problems with raw materials and intermediates from developing countries, caused by outsourcing strategies of the larger companies, can be addressed by NIR, as well. An example is the recently discovered lots of heparin contaminated (possibly on purpose) with oversulfated chondroitin. The FDA eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 NEAR-INFRARED SPEC TROSCOPY: A POWERFUL TOOL FOR PAT/ QbD (Cont .) packaged in larger quantities, however, so the 84 remaining tablets in the 100 tablet bottle stay unknown after the 16 are used for testing. As with end product testing, nothing is learned about the process. Figure 5. 2nd Derivative NIR spectra of oversulfated chondroitin (blue) and heparin (red). Figure 6. Increasing Levels of melamine (monomer) in gluten. discovered what the adulterant was by use of capillary electrophoresis and two-dimensional NMR. While this is a good research project, it is cumbersome for a routine approach. Using NIR on contaminated heparin samples shows obvious differences (Figure 5). The check for heparin quality may be performed more quickly and on a routine basis with NIR. Any unexplained differences could then be investigated by more sophisticated means. Another adulteration problem was the use of melamine to raise the protein assay (by chemical means, such as Kjeldahl digestion) in milk and imported gluten. Figure 6 shows the NIR determination of melamine in gluten. Stability One other application, beginning to be investigated is stability testing. Under QbD/PAT, thousands of units of product are examined (if not 100%). Under cGMP, a minimal number of units is tested at stability time points: six tablets/capsules for dissolution and ten for assay or content uniformity. Most drugs are european INDUSTRIAL PHARMACY • Issue 4 October 2009 One paradigm being tested is to scan all the tablets/capsules in a bottle at each stability time point. The analyst could then use the software to identify which of any units are different. If any outliers are noted, these could be subjected to further testing on a “for research purposes only” basis (avoiding adverse FDA or EMEA scrutiny). With a number of batches recorded, statistic-magic can be performed. As an example, results from the 100% scrutiny can be compared with batch records (QbD/PAT measures many parameters to acquire design space). As a hypothetical case, assume that at the expiry date for lot “A,” 10% of the units show “differences” by NIR, while batch “B” shows 25%. This begs the question “what happened during production to cause this difference?” Over time, the design space could be tweaked to give longer and more predictable expiration times. There is even a possibility of using this data to extend the expiration date for a product, potentially saving sample recalls and increasing profits. Summary In essence, NIR is a tool that can be used before and after production as well as being a production monitor. The chemical and physical attributes of raw materials, intermediates, and products can be measured and controlled with existing hardware and software. The added benefit of screening for counterfeits and adulterated materials makes NIR a powerful ally for the Pharma industry in its pursuit of assuring quality medication. 17 THE NEXT 50 YEARS: DEVELOPING OUR CORE VALUES FOR A CHANGING WORLD REPORT FROM PGEU SYMPOSIUM, STOCKHOLM, 15 JUNE, 2009 by Pär Tellner T he first presentation was given by Professor Claire Anderson, from The Centre for Pharmacy, Health and Society at the Nottingham School of Pharmacy, who gave an overview of factors influencing the pharmaceutical sector. She also referred to a study made in UK on community pharmacist core values, which found that the most common core values were patient best interest and respect for medicines. She also thought that pharmacy will focus more on personalized treatment and prevention. Thomas Lönngren from EMEA talked about the regulatory system, the role of the EMEA and future challenges. The Commission will reflect on the Clinical Trial Directive and the fact that there is no harmonization of the national approvals of clinical trials in Europe. He also told us about the recent positive opinions on OTC-switches (Alli and pantoprazol) and negative opinion on an OTC-switch for Viagra. Thomas clearly indicated that the different security level of the national pharmacy system is a very important factor for CHMP when deciding if they should approve an OTC-switch or not. He wonders if and how PGEU could help CHMP with that assessment. Thomas brought up the challenges on how to control manufacturing and clinical trials, when these important activities are to a much greater extent performed in the growing economies, eg. China, India and South-east Asia. He also 18 discussed the problem that although we invest more in R&D, the number of new substances is decreasing. He thought that further harmonization of regulatory requirements, better advice in early development and how to better reward innovation could be of some help. However, he believes that the failures seen are a result of more complex targets. Finally he said that EMEA need to give scientific advice and issue clinical guidelines in close collaboration with Health Technology Assessment bodies, in order for industry not to have different clinical development programs. EMEA also need to develop how they come to their conclusions on risk/benefit in the EPARs, to facilitate the HTA bodies’ work. Dominique Monnet from the European Centre for Disease Prevention and Control (ECDC) gave a presentation on “The potential of pharmacists to contribute to infectious disease prevention and control”. He thought that community pharmacists could identify infectious diseases, inform the patients, participate in public awareness campaigns and vaccinate against seasonal diseases. In Portugal, community pharmacists have started to give vaccinations. The interest from the population is huge, despite the fact that they have to pay for the service at the pharmacies, while the service is free of charge at the health care centres. 40 % of the administrations of flu vaccine in Portugal were made at pharmacies. Dominique also informed us that ECDC will arrange the 2nd European Antibiotic Awareness Day, 18 November 2009 and that pharmacists could contribute to decrease the resistance problems by responsible dispensing of antibiotics. Balázs Hankó from Hungary informed us that the Hungarian government has decided to give all Hungarian pharmacists a PharmD degree. The decision is valid retrospectively. Professor David Taylor gave a presentation of UK Pharmacy developments. He told us that for example over 2 million Medicines Use Reviews have been made in 2009, good results with pharmacists’ prescriptions, NHS Health checks, smoking cessation programs, etc. Richard Bergström, Director General of LIF Sweden, who today represented EFPIA, questioned whether the industry and pharmacists are collaborating enough. They have a lot in common, he said. They are both in business to make money by helping people but unfortunately there is no common agenda. Richard believes a new collaborative approach is needed with patient support and disease management programs, follow-up systems, new channels of delivery and joint recruitment of patients for clinical research. Somewhat surprisingly, this presentation was seen as provocative. Anders Olauson from the European Patient Forum gave a presentation on” How should the profession move forward”. Anders told us that pharmacists have an active role in patient advice and medication therapy management, and could give patient care services ranging eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 THE NEXT 50 Y EARS: DEVELOPING OUR C ORE VALUES (Cont .) from monitoring to nutrition support. Anders also said that pharmacists are the most accessible and trusted HCP. In contrast to PGEU’s opinion, EPF sees a role for industry to give quality secured information to patients, eg. via public private partnerships. The PGEU is the Pharmaceutical Group of the European Union (Le Groupement Pharmaceutique) a European association representing Community Pharmacists. PGEU members are the national associations and representative bodies of community pharmacists in 30 European countries including the EU member states and EEA members. www.pgeu.eu or www.gpue.eu (in French) Pär Tellner is Compliance Officer and Director of Veterinary Medicine at LIF the research-based Pharmaceutical Industry in Sweden THE INDUSTRIAL PHARMACIST’S ROLE IN PROVIDING PATIENT INFORMATION by Roland Schots Medical information impacts most key operations in the pharmaceutical industry including Regulatory Affairs, Medical information and promotion, Pharmacovigilance, Manufacturing, Quality Assurance. Regulatory Affairs comes first because the information to the patients must reflect accurately the particulars of the medicinal preparation as approved by the Health Authorities. This means that any Product Information (reference for the Patient Information Leaflet) must be in compliance with the Marketing Authorisation granted by the responsible Authorities. Wording, layout and readability have to meet European and national regulations (QRDtemplate – EMEA). This is also the case for veterinary drugs. Product information may only be changed postapproval by the Health Authorities. The valid texts are provided by Regulatory Affairs to the Medical information and promotion department. The approved Product information also is the reference when clinical or quality complaints are reported (clinical complaints are managed by the Pharmacovigilance department). Medical information and promotion to patients is allowed for non-reimbursed drugs but the information is subject to strict restriction and is even prohibited for some classes of products (eg. cytostatics, narcotics, etc.). The right product information has to match with the right product and this means a well organised QAsystem that reduces risks of mislabelling in the Packaging unit. This brief survey emphasises the role pharmacists, by their education, have to play at several stages of patient information. They are indeed active at the different steps leading to the final information communicated to the patients. Mr Roland Schots is a QP for radiopharmaceutical manufacturing and adviser for Regulatory Affairs to Belgian and multinational companies. GMP Forum The online discussion group for industrial pharmacy www.pharmweb.net/gmp.html european INDUSTRIAL PHARMACY • Issue 4 October 2009 19 REGULATORY REVIEW: Review of major developments in GMP and the regulation of medicines in the EU and on the International Scene, July to September 2009 by Steve Fairchild The last review period saw the issue of a statement of intent from the United States FDA for more robust enforcement of serious non-compliances with GMP. The FDA also issued important guidance on dealing with potential melamine contamination in pharmaceutical starting materials and on anti-counterfeiting measures for finished products. In Europe we saw a climb-down on proposals for legislation to impose GMP on “certain” pharmaceutical excipients. Europe Conclusions on the EC study on pharmaceutical excipients The European Commission (DG Ent.) announced that it does not intend to develop a new directive applying GMP to “certain” pharmaceutical excipients, as foreseen in earlier EU legislation. Whilst DG Ent. has accepted the need to apply GMP to certain of these materials, the responsibility for identifying them and ensuring compliance with GMP will now rest primarily with pharmaceutical manufacturers (and presumably their Qualified Persons). EudraGMP database This database was set up by the EMEA 2 years ago to provide a common resource for EU GMP inspectorates to use in planning and performing GMP inspections. The EMEA has now made certain fields in the database available for public scrutiny. However, it is unlikely to be of much use at present due to the limited fields covered (eg. GMP deficiencies cannot be accessed) and lack of data from the Member States’ regulatory authorities. However, there is some sign of progress with data entries as the 20 MHRA has announced that in future it will transmit data into EudraGMP automatically. Common deficiencies from UK GMP inspections The UK’s MHRA has published a package of information on its website derived from the analysis of follow–up correspondence for GMP inspections carried out in 2007 and 2008. Whilst this information is interesting it is difficult to draw any conclusions from them about either compliance or inspection trends. Communication of serious GMP deficiencies and rapid alerts for product defects A new procedure has been issued by the EMEA according to which the regulatory authorities of the EU Member States will exchange information about serious deficiencies found during GMP inspections, together with recommended actions. In addition, the existing procedure for communicating serious product defects (rapid alerts) has been updated. British Pharmacopoeia 2010 The 2010 edition of the BP has been published recently with an effective date of January 1st 2010. It contains several new monographs and standards along with material from the European Pharmacopoeia 6th Edition Supplement 6.5. United States of America FDA’s “Vision” on enforcement The FDA’s Commissioner has set out the Agency’s commitment to improve its regulatory and enforcement system. This will involve tighter deadlines for responses to inspection findings, streamlining of the Warning Letter process, the possibility of immediate action, closer collaboration with regulatory “partners” and a more structured approach to following up and closing out Warning Letters. Guidance for Industry: Pharmaceutical components at risk of melamine contamination This guidance results from serious health problems in China due to the adulteration of milk with melamine. It set out to alert finished products manufacturers, compounders, repackers, and suppliers to the potential risk of melamine contamination in pharmaceutical components. It also sets out specific actions to be taken to detect and prevent melamine contamination of “at risk” components which include lactose and povidone. New questions and answers on GMP for penicillin products The FDA updated its set of GMP Q&A to include the manufacture of penicillin active ingredients and finished products. This confirms what was generally understood to be the FDA’s position and industry practice. Draft guidance on drug anticounterfeiting measures The FDA has published a draft guidance document that facilitates the incorporation of physico-chemical identifiers (PCIDS) in drug products. This guidance should provide an incentive to protect the public from counterfeit products. Proposed revision of US Pharmacopoeia (USP) monographs for excipients The USP has published draft revised monographs for Propylene Glycol, Sorbitol Solution, Sorbitol Sorbitan Solution and Noncrystallizing Sorbitol Solution to include specific tests for adulteration. For further information on these and other topics we suggest you refer to current and past editions of “gmpreview News” published by Euromed Communications. (See: www.euromed.uk.com) eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 NEWS FROM THE EIPG Pharmine meeting A meeting of the Pharmacy Education in Europe (PHARMINE) has been held at the PGEU (European Community Pharmacists Group) offices in Brussels. Progress with the seven working groups was discussed and the timing for reports on undergraduate and post-registration in industrial and hospital pharmacy practice was agreed. The Pharmine consortium consists of four universities (Brussels, Nancy, London and Lisbon and EU partner associations representing the different branches of pharmacy. Industrial Pharmacy is represented by EIPG. The aim is to put forward an EU PATstandard & QbD half page ad education 1/9/09 for pharmacy 11:48 and training to be adopted by both the older and newer member states as well as candidates for EU membership and countries in nonEU areas such as Africa, China, India and South America. Further information on this project can be found on the PHARMINE website www.pharmine.org EFPIA meets EMEA Contact has been made with EFPIA in preparation for a December meeting with the EMEA and other interested parties to discuss variability in the interpretation and implementation of GMP issues. Commission’s legal proposals on the provision of information to patients has been acknowledged by the European Council. Our comments can be found on the EIPG website. CPD in sales and marketing The continuing professional development needs for staff in Sales and Marketing are under consideration. If you are interested in including your ideas for discussion within the working group, please contact Kiriasis Savvas at savvas@normahellas.gr Information to patients Jane Nicholson Executive Director EIPG Pagerepresentation 1 EIPG on the 7th Annual an 25 d th Reg re Se is ce p te ive tem r b up be y to r 2 £2 00 00 9 January 19 - 20, 2010 off New Connaught Rooms, London, UK ! PAT and Quality by Design www.patandqbd.com Ensure your regulatory submission is approved first time by successfully navigating the regulatory guide lines surrounding PAT and QbD Establish best practice for the use of PAT and real-time-release in commercial manufacture Build a successful change management strategy when implementing QbD across the wider business and incorporating it into your lifecycle management programme Establishing a watertight business case for your senior management: Where do you start? Ensure product and process quality from the beginning by successfully building QbD into your development process QbD approaches for Biopharmaceuticals: Translating the lessons learnt from small molecules CALL: +44 (0)20 7368 9300 / 0800 652 2363 FAX: +44 (0)20 7368 9301 european INDUSTRIAL PHARMACY • Issue 4 October 2009 EMAIL: enquire@iqpc.co.uk 21 SAFER MEDICINES SUPPLY – ANTICOUNTERFEITING USING 2-D BARCODING by Inger Näsman Background ounterfeit medicines are a serious problem in many Cdeveloping countries. It is a well known and big problem in the countries but also a growing problem in Europe and USA. WHO estimates that about 7-10% of the world’s pharmaceuticals are counterfeit and in some developing countries counterfeit drugs range from 25-50%. Counterfeit medicines are now finding their way into the legal supply chain. For example in the UK recalls have been made of counterfeit Lipitor, Plavix and Zyprexa. In USA more than 50 cases were investigated by FDA in 2006. The European Commission is now taking action and proposes a means to guarantee the integrity of product packs along the supply chain and the possibility to identify individual packs. Coding and tracing Today, authentication of individual packs is not possible – product traceability is in best cases ensured at batch level. However, several countries are now taking steps to introduce traceability systems. Belgium, Greece and Italy are already requesting serial numbers on packs and Spain, Turkey and Serbia are currently working on introducing mandatory serialisation. INGER NÄSMAN is a Director of LIF – the Research-based Pharmaceutical Industry in Sweden 22 Different solutions in different countries have many disadvantages and EFPIA is therefore proposing a standardised system for coding and identification of pharmaceuticals in Europe using the Data Matrix code. The code should contain information on Global Trade Identification Number (GTIN), a random serial number, batch number and expiry date. The combination of GTIN and the random serial number gives a unique identification of an individual pack. Data Matrix has been chosen because it is robust and cost competitive and has also been used successfully by international Federation of Animal Health (IFAH) for coding animal health products. The concept is an end-to-end system and verification should be done at the point of dispensing to verify: ♦ The existence of the number in the database ♦ That the product has not been dispensed before But the system also provides more advantages for the quality of dispensing in pharmacies since you can check that: ♦ The right product is chosen ♦ The product has not expired ♦ Absence of recall for this product/batch Pilot in Sweden EFPIA is currently performing a pilot in Sweden to check the concept. In the pilot the database and the response time for pharmacists will be checked. Twenty-five different products has been chosen and will be scanned in 25 different pharmacies until at least 100,000 packs has been authenticated. The pilot will be finalised early 2010. Products and labelling Products that are sold in several packs were chosen and applications to allow additional labelling with the 2-D code were sent to MPA. The distribution to the selected pharmacies was made by the two one-channel distributors in Sweden, KD Pharma and Tamro, who were also responsible for making the extra labelling. Of course when the system is up and running the labelling will be conducted at the point of manufacture. eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 SAFER M EDI CINES SUPPLY - ANTI-COUNTERF EI TING USING 2-D B ARCODING (C ont.) Scanning Better patient safety In Swedish pharmacies the personnel scan a barcode on all packs to check that the right product is selected and therefore makes scanning of the new 2-D code only a small change in routine. The additional software is incorporated into the pharmacy software to make the check as easy as possible. Swedish pharmacies are currently under deregulation but only pharmacies belonging to the State-owned chain, Apoteket, has been chosen for the pilot, therefore only one software needed to be altered. There is no perfect solution to guarantee safety and eradicate counterfeits, but the use of the Data Matrix can help fight counterfeits and the technology can be implemented quickly and at an acceptable cost. Authentication at the point of dispensing, together with e-prescriptions would also reduce dispensing errors and allow more effective and efficient product recalls and automatic detection of expired products. GMP Forum The online discussion group for industrial pharmacy www.pharmweb.net/gmp.html european INDUSTRIAL PHARMACY • Issue 4 October 2009 23 PHARMACEUTICAL FORUM The following questions and responses are a selection of those published on an open online discussion group www.pharmweb.net/gmp.html. The Forum serves as a means of exchanging views on international regulations affecting the pharmaceutical industry. Readers of European Industrial Pharmacy are invited to contribute to the Forum. BSE/TSE free certificate Is it a requirement of MHRA that all the Q raw materials used in drug product manufactured for the UK should have a Response 4 – I agree that is most unusual to perform a physical audit of a manufacturer of common excipients. The previous responder referred to audit data which could mean a questionnaire to obtain basic information. Obviously if it was found that materials of bovine origin were being used in common equipment, an audit or alternative supplier would be necessary. I was present at an EU Inspection when this topic was discussed. It was easy to state that the excipient in question was BSE/TSE free, but the Inspector mentioned that he knew that the site processed bovine materials – would the company please check, that bovine materials were not processed in the equipment used for that particular excipient. Note: a check was required, not necessarily an audit. certificate of freedom from BSE/TSE? I understand that a BSE/TSE free certificate is required for only those materials manufactured from animal origin. Response 1 – You’ll need to do a supplier evaluation first to be confident the supplier does not manufacture other products with animal materials. Response 2 – The issue of potential contamination with prions needs to be addressed in your risk assessment for materials to be used in any product, wherever they will be marketed. Relation between GMP and ISO standards I would appreciate advice on how to Q manage the existence of both GMP and ISO standards in the same company. The company is a manufacturer of medicinal products, but there is also production of medical devices, dietetic supplements, etc. Please keep in mind that materials of animal origin may be used in the manufacture of materials even if they are not supposed to be present in the finished material. This includes active ingredients, excipients and materials used in the manufacture of container components. Response 1 – According to today’s GMP regulations, Your suppliers should be asked to confirm whether or not materials of animal origin have been used in the manufacture of each material you use. When you have this information you are then in a position to consider whether you need a TSE certificate for any of those materials or if you can change the supplier to obviate this need – eg. where there is a source of the material concerned that uses vegetable rather than animal materials. If there is no animal material used (and you have audit data to support this) then there no need to obtain a TSE certificate. Response 3 – Audits could targeted at sites with a excipients production where there is use of potential animal derivatives – eg. tallow derivatives, gelatin, collagen, etc. Note that I used the word ‘use’ – this could be in the production of materials which might not contain animal derivatives themselves when placed on the market but were exposed to them during the manufacturing process. The frequency of audit would depend on the extent of use of animal derivatives in the plant. There might be less need for audit if the materials are covered by a current, valid EDQM CEP. 24 API sites should be audited anyway regardless of the type of material if the output is to be used in the EU due to QP obligations. the differences are not so big. Actually ICH Q10: Pharmaceutical Quality System, is based on the ISO 9001 standard. On the other hand, ISO 13485 for medical devices follows the principles of GMP. I was involved in the establishment of a quality standard for a biotech company which complied with ISO 9001, ISO 13485, GMP and biologics, I can advise you to go through an in-house harmonization process. Response 2 – Except for some common areas linked to “systems” like quality manual, complaint handling, annual review, etc. where you will have to check that both referentials are matched, there is no real opposition to implementing both standards in the same company. There is, in my opinion, no place for a litigious situation between them. Response 3 – The main reason for any business to exist is to create profit by providing a service or product. Fulfilling of GMP requirements ensures (or attempts to ensure) product quality directly. ISO is more a disciplined way of working to and to continuously evolve the working practices for betterment of the services provided. eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 P H AR M A C E U T I C A L F O R U M ( C o n t . ) Once GMP requirements are fulfilled, the customer can be satisfied he has a good product. Once ISO requirements are fulfilled, the customer knows he is working with a disciplined and reliable organisation. Top priority must be given to GMP and then align it to match ISO requirements. GMP requirements lay down what is required and these have to be incorporated into the system by addressing them with respect to the ISO clauses. Response 4 – While not disagreeing with any of the previous correspondence about the relevance of ISO and GMP, it has to be stated that ISO standards in many cases are not policed, so they are used and often abused. On the other hand, GMP is policed by your regulators and you will be quickly closed down for persistent non-compliance. Response 5 – For medical devices in the EU, ISO standards are widely used for quality systems. Their implementation is monitored by Notified Bodies (and the Notified Bodies are monitored by the Competent Authorities). Audit of ISO standards can be done effectively in other sectors too. There needs to be reliable third party auditor rather than just a statement from the company that they are implementing ISO standards. Response 6 – It should be remembered that ISO documents are ‘standards’ while EU GMP ones are LAW. Ozone sanitization in HVAC Let’s say that every Sunday evening, we Q added ozone into the air handling units (AHU) and made it circulate for 2 hours. Then flushed with fresh air and started working again on Monday morning. This will help control microbial growth and has the same effect as periodic hot water sanitization. Lets forget the human safety issue. Are there any quality issues with this? What’s FDA’s attitude? Response 1 – I don’t know about the FDA’s attitude but why do you suggest this? What is your process and what is the concept of your HVAC system? What are you seeking to achieve? Is it really necessary? There are other and better ways of controlling the microbiological environment of a clean area without such a draconian treatment. If the HVAC system is correctly designed, installed and operated you should not need the type of treatment you mention. Why choose ozone? What would be the long term impact of very frequent oxidizing agent contact on the physical properties/structure of the system/components (ventilator, ducting, extractors, etc). Some companies working with infectious or transmissible agents use hydrogen peroxide as a precaution to disinfect the AHU at the end of a production campaign. That can be a validated process using BIs. However, whilst aggressive, this is an occasional treatment that is not done every day. Response 2 – Apart from both ozone or hydrogen peroxide, formaldehyde fumigation during shutdowns will work very well and effectively. This procedure is validated for effectiveness and recirculation of fumigated air will disinfect all the ducting and HVAC system. Response 3 – I built and validated a facility that included three four-room suites, one of which was sterile. They were periodically sterilised using a design that included special dampers in the HVAC system that allowed the system to run on total recirculation. The program was PLC controlled and quite simple. On initiation the HVAC dampers ran and transformed a total loss system into a total recirculation system. This was allowed to run and stabilise for around 30 minutes. In each room there were wall mounted, pressurized containers of formaldehyde, each one fitted with an electrical solenoid valve, which the PLC could activate. Once the recirculation flow was established, the PLC initiated a set program of sequential discharge from these containers. This would continue for approximately six hours, exhausting the supply of formaldehyde. The PLC would then revert the HVAC flow to total loss and dump everything into the countryside. I managed the build and validation, but left the quality control to production. Response 4 – Formaldehyde gassing can work quite efficiently and was widely used, certainly in the EU. It’s a rather unpleasant and dangerous product whose one advantage is that you can smell it at very low air concentration. Some people’s sense of smell is better than any Draeger tube. It was banned by the EU in 2007 via a previously issued European Directive concerning the placing of biocides on the (European) market. I don’t believe it has been used in the USA. These days, companies should use alternatives such as hydrogen peroxide. However, it would be interesting to know if its use is tolerated in other regions of the world. Readers are invited to send their Q&As to www.pharmweb.net/gmp.html european INDUSTRIAL PHARMACY • Issue 4 October 2009 25 BOOK REVIEW Patient Safety By Ivana Silva Published by: The Pharmaceutical Group of the European Union (PGEU) Price: Freely downloadable at www.pgeu.eu in English and French atient Safety is one of the PPharmaceutical priorities of the Group of the European Union (PGEU) and several initiatives have taken place in the past three years to highlight community pharmacists’ engagement in this particular field. In March 2007 we published a brochure entitled “Maximizing Patient Safety in Europe through the safe use of medicines”, available in English and French and downloadable from the PGEU website (www.pgeu.eu). The publication stresses the place of medicines safety within the overall topic of Patient Safety, a central issue on the current EU health agenda. It sets out some of the key issues that must be addressed if medication errors are to be avoided. The publication calls for a systematic approach to patient and medicine safety issues across all health professions and in all health care settings. The publication also describes some of the initiatives undertaken at member state level in the field of medication safety, highlighting the contribution community pharmacists make to promoting medicines safety, while recognising that there is still scope to achieve more. It is interesting to note that this document was mentioned within the European Commission Work plan 2008 in relation to its roadmap for a Regulation amending Regulation (EC) 726/2004 and a Directive amending Directive 2001/83/EC on Modernising Pharmacovigilance for 26 Pharmaceuticals as a relevant data source. Building upon this work, PGEU also published in May 2008 its booklet on “Targeting Adherence: improving patient outcomes in Europe through community pharmacists’ intervention”, outlining relevant research in this area and several community pharmacists’ initiatives in different EU countries to tackle nonadherence to medicines, a problem estimated to cost the European Union 125 billion Euro annually. In the past two years PGEU was also involved in the discussions leading to the Patient Safety Communication and Council Recommendation proposal prepared by the European Commission, published last December 2008. PGEU’s main points were the need to take into account all sectors of healthcare (primary, secondary, and tertiary) and all healthcare professionals, and to involve not only Member States but also stakeholders both in European and National initiatives aimed at developing and implementing Patient Safety strategies. The final Council Recommendation was published this year, in June, and PGEU was pleased to see that focus has been given to medication errors as an area that needs to be given more attention. Currently PGEU is also involved in the EU-funded project EUNetPaS, which started in 2008 and will end in 2010. PGEU has been particularly active in the project’s work-package dealing with medication safety. PGEU’s message has been focused on the need to ensure a systemic approach to all healthcare settings which are part of the patient journey in the healthcare system, and underlines the importance of avoiding medication errors occurring at the interface of hospital and ambulatory care. Ivana Silva works within the Pharmaceuticals and Profession Affairs division of the PGEU. email: i.silva@pgeu.eu eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009 job vacancies Junior Project Manager, Switzerland My client is an innovative and enterprising global Medical technologies company who are well established and well respected within the industry. They are looking for a Clinical Research Specialist to join their growing team. Switzerland: 110.00–125.000 S francs Call Ludo: +44 (0)207 234 0550 Regulatory Affairs, full life cycle exposure We are working with a number of Pharmaceutical and Biotech companies who offer excellent benefit packages as well as training and development. UK wide: £30,000–£75,000 Call Abid: +44 (0)207 940 2108 GCP Auditor International GCP Auditor opportunity with assured career path. OpEx-half-page-advert 1/9/09 11:21 UK: £45,000–£55,000 Call Stephen: +44 (0)207 940 2105 NonStop Recruitment is a market leader in European pharmaceutical Recruitment with specialist consultants covering major markets such as UK, Germany, Switzerland, France, Italy and the Netherlands. These consultants recruit for all major roles within the pharmaceutical industry, including clinical research, quality assurance, sales and marketing, pharmacovigilance, business development and regulatory affairs. Medical Scientific Liaison – Work for a Large Pharmaceutical Company The company is about to put one of their main products on the market and this is an exciting time to join them. Italy: €40,000–€60,000 Call John: +44 (0)207 940 2106 Senior Clinical Research Associate Join one of the leading pharmaceutical companies and get the career progression you have been looking for! Germany: €50,000–€60,000 Call Marketa: +44 (0)207 234 0550 Scientific Section Leader/Immunology 6 month contract with one of the world-leading pharmaceutical companies, fantastic opportunity for Dutch/English bilingual R&D freelancers based in NL. Page 1 Netherlands: Hourly rate €40 flexi Call Jaroslav: +44 (0)207 940 2105 Senior Medical Information Associate Career progression skills to be gained, allowing you excellent and broad development. South East England: £30,000–£40,000 Call Harriett: +44 (0)207 940 2102 Account Consultant Development of professional networks across Southern Europe with a global Blue Chip company. France: £40,000 basic = 46,000 euros basic + $80,000 uncapped OTE = 54,000 euros uncapped OTE Call Tomas: +44 (0)207 940 2105 Health Economics Manager, Progress Fast, Germany This is a great opportunity to join an expanding company that won’t pigeonhole you. Germany: £50,000–£75,000 Excellent Package Call Austen: +44 (0)207 940 2102 Main conference: 8th and 9th December 2009 Pre-Conference Workshop: 7th December 2009 CCT Venues, Two East Poultry Avenue, Smithfield, London EC1A 9PT 18 Internationally Renowned Experts Share Their In-House Expertise Including: Dr Fadel Hamed, Associate Director, Head of Operational Excellence, Genentech Dr Ian Clegg, Head of PAT, Pfizer Dermot O’Rouke, Operational Excellence Manager, Drug Substance, Wyeth Biotech Tom Cochrane, Business Process Development Manager, Napp Pharmaceuticals Mark O’Reilly, Associate Director, Operational Excellence, Elan Pharmaceuticals Jennifer Miller, Executive Director, Global Research and Development, Pfizer Michael Cummane, Business Excellence Manager, Abbott Vascular Dr Andres Kanstrup, Principal Scientist and LEAN Manager, Novo Nordisk 0800 652 2363 or +44 (0)20 7368 9300 So why should you attend this event over any others? > 16 internationally renowned presenters deliver their key insights and best practices to help evolve your strategy and effectively implement best practice into your business > Learn how to best control your external supply chain to meet your operational excellence targets > Identify strategies for reducing manufacturing plant down time, while maintaining quality > Uncovering new strategies for applying lean Six Sigma in R&D w w w. o p e x p h a r m a . c o m / G M P D M +44 (0)20 7368 9301 enquire@iqpc.co.uk Sponsors DATES FOR YOUR DIARY OCTOBER 26-28 October 2009 – Antalya, Turkey 3rd BBBB Conference on Pharmaceutical Sciences (EUFEPS) www.bbbb-eufeps.org 27-28 October 2009 – Barcelona, Spain BioProduction 2009 (Informa) www.bio-production.com N OV E M B E R 3 November 2009 – London, UK The 11th Joint Conference on the Qualified Person (RPSGB) www.rpsgb.org 4-5 November 2009 – Dessau, Germany Disposables in biopharmaceutical development and manufacturing (APV) www.apv-mainz.de 10-11 November 2009 – London, UK APS Vaccines 2009 (APSGB) www.apsgb.org 16-18 November 2009 – London, UK Shelf life and stability testing of pharmaceuticals and biotechnology products (ECEC) www.ECEC.co.uk 9-12 November 2009 – Manchester, UK Essential elements of a quality management system (DBA) www.dba-global.com 17-18 November 2009 – Manchester, UK GMP and good distribution practice symposium (MHRA) www.mhra.gov.uk 18-20 November 2009 – Venice, Italy 12th APIC/CEFIC European Conference on Active Pharmaceutical Ingredients (APIC) www.api-conference.org 23-25 November 2009 – Cambridge, UK Tabletting technology for the pharmaceutical industry (RPSGB/APS) www.rpsgb.org 24 November 2009 – London, UK Supplier quality management (Management Forum) www.management-forum.co.uk 2-3 December 2009 – Amsterdam, The Netherlands HVAC systems and the pharmaceutical manufacturing environment (VIP) www.vipltd.co.uk 7-10 December 2009 – Amsterdam, The Netherlands Pharmaceutical GMP (DBA) www.dba-global.com 8-9 December 2009 – London, UK 4th Annual Operational Excellence (IQPC) www.opexpharma.com/gmpdm 9-11 December 2009 – Edinburgh, Scotland DDL20 – celebration twenty years of drug delivery to the lungs (DDL) www.ddl-conference.org.uk JANUARY D E C EM B E R 18-20 January 2010 – London, UK PAT and quality by design (IQPC) www.patandqbd.com 1-2 December 2009 – Manchester, UK Practical application of quality by design (DBA) www.dba-global.com 27-28 January 2010 – Amsterdam, The Netherlands Cool Chain Europe 2010 (IQPC) www.coolchaineurope.com World Leader in GMP gap analyses, seminars and individual GMP training Hard hitting web-based GMP training in the comfort and convenience of your office or home (save on expensive and inconvenient travel: These seminars are offered as web-based learning: GMP and Quality System Consulting: With over 200 clients in 27 countries, we pride • ourselves that every single one of our clients has passed an FDA inspection the very first time through (when they have listened to us) • Passing an FDA Inspection – Guaranteed • Managing the QC Lab in a GMP Manner • Fundamentals and Essentials of Validation • Effective Investigations and Corrective Actions • Effective Quality Assurance Auditing We have wide expertise in evaluating GMP and • Quality Systems at your facilities and in For full details and registration check our website at: www.globepharm.org/seminars.html/course Let us assist you. Speedily and cost effectively. Contact us at: consulting@globepharm.org 28 performing third-party supplier and contract manufacturer audits eur opean INDUSTRIAL PHARMACY • Issue 4 October 2009
© Copyright 2025