Document 219674
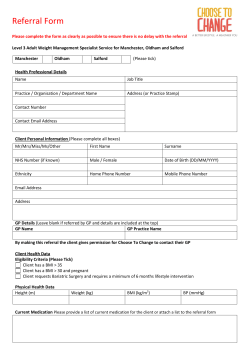
How to Expand the Reach of CR into Underserved Populations Sherry L. Grace, PhD Associate Professor, York University Director of Research, CVR&P University Health Network Overview • • Scope of the problem Strategies: 1. Automatic referral 2. Modifiable barriers 3. Program tailoring Sex Differences in CR Use • In U.S. and Canada, only approximately 15-30% of eligible patients participate in CR – with the rate for women being much lower at approximately 11-20% • In a cohort of all Medicare beneficiaries who had an index hospitalization in 1997 in a U.S hospital with a qualifying diagnosis, significantly fewer women (14.3%) than men (22.1%) received CR. • Others have shown that the percentage of women in CR is 20% lower than what would be expected based on coronary morbidity data Jackson, 2005; Grace 2002, 2010; Schuster 1999; Ades 1992; Sanderson 2010; Mosca 2007 Age Differences in CR Use • Despite its proven benefits and need, older patients are significantly less likely to be referred to CR. • In a population-based study, MI patients 70 yrs + were 77% less likely to participate in CR than those younger than 60, independent of other characteristics. • This is despite the fact that CPG recommend patients participate in CR regardless of age, – and that older patients adhere well to CR once they are enrolled. Oldridge 1992; Pasquali 2001; Ades 1992; Grace 2002; Cooper 2002, Witt 2004 1. Referral Strategies – Can they increase reach? CRCARE: Cardiac Rehab Care Continuity through Automatic Referral Evaluation Pasquali, S. K., Alexander, K. P., Lytle, B. L., Coombs, L. P., & Peterson, E. D. (2001). Testing an intervention to increase cardiac rehabilitation enrollment after coronary artery bypass grafting. The American Journal of Cardiology, 88(12), 1415-1416, A6. JACC 50(7): e100 AHA GWTG Program GWTG is a national initiative of the AHA to improve guidelines adherence in patients hospitalized with cardiovascular disease. GWTG uses collaborative learning sessions, conference calls, e-mail and staff support to assist hospital teams improve acute and secondary prevention care systems. A web-based Patient Management Tool is used for point of care data collection and decision support, on-demand reporting, communication and patient education SIMPLE, ONE PAGE, ON-LINE FORM CR Interactively checks patient’s data with the AHA guidelines ©2001 Outcome Sciences, Inc. Liaison Referral Strategy: PT, NP, RN, Peer 11 Participating Ontario Sites Sudbury Regional William Osler Ottawa Heart St. Mary’s (KW) York Central Sunnybrook UHN Windsor Regional Hotel Dieu-Grace Trillium Hamilton Health Sciences CRCARE Flow Diagram 5781 CAD inpatients approached from 11 hospitals 1537 ineligible N =2636 participants 1608 declined 62% response rate Chart Extraction In-Hospital Survey 391 ineligible N =1807 participants 438 declined 80.5% retention 1 YR Follow-up Mailed Survey Grace et al., in press AIM CR Referral RESULTS: CR Referral Rates by Referral Strategy 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Male Female 86% 71% ** 64% 34% Automatic + Liaison n=471 Automatic Allied Only Health/Liaison n=551 Only n=490 Usual n=297 n=1809 **p < 0.01; x2 = 9.25, κ = .14 CR Enrollment RESULTS: CR Enrollment Rates by Referral Strategy 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Male Female 75% 61% ** 55% 30% Automatic + Liaison n=471 Automatic Allied Only Health/Liaison n=551 Only Usual n=297 n=1809 n=490 **p < 0.01; x2 = 7.12, κ = .11 RESULTS: Agreement b/w Referral and Enrollment by Referral Strategy Referral Strategy Automatic + Liaison Automatic Only Liaison Only Usual N=1809. kappa Males Females .61 .52 .73 .76 .69 .76 .70 .85 Summary: Referral Strategies • Limitations: non-randomized, unadjusted analyses presented • Systematic referral mechanisms using a universal process can achieve high and comparable referral rates for men & women – Bedside chats may introduce bias? • 54-85% of referred women will enroll, depending on referral strategy employed – While more women referred through nonsystematic means will enroll (cherry-picking?), ultimately fewer women will be given the initial referral • So best practice to ensure women receive referral, but ultimately they will be less likely to enroll than referred males 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% ** 90% 73% <66 yrs ≥66 yrs *** 70% * CR Referral RESULTS: CR Referral Rates by Age & Strategy 39% Automatic + Liaison n=471 Automatic Allied Only Health/Liaison n=551 Only n=490 Usual n=297 N=1809 **p < 0.01; ***p < 0.001 CR Enrollment RESULTS: CR Enrollment Rates by Referral Strategy 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% ** 80% <66 yrs ≥66 yrs * 65% ** 58% 35% Automatic + Liaison n=471 Automatic Allied Only Health/Liaison n=551 Only n=490 * Usual n=297 N=1809 **p < 0.01; x2 = 7.12, κ = .11 RESULTS: Agreement b/w Referral and Enrollment by Strategy Referral Strategy kappa <66 yrs ≥66 yrs Automatic + Liaison .57 .58 Automatic Only Liaison Only .74 .70 .69 .81 Usual .68 .83 N=1809. Summary: Referral and Age • Similarly to the findings by sex, using universal processes can result in the highest referral rates, even for older patients • Following the non-universal strategies, the older referred patients are more likely to enroll (likely because they were cherrypicked as the highly-motivated, ideal candidates?!) • Requires further study and replication 2. CR Barriers by Age and Sex Identification of modifiable barriers to address, and expand reach? CR Barriers Scale • CR barriers are assessed through 19 items, which were developed based on a review of the literature, pilot-tested, and show good psychometric properties • Items rated on a 5-point Likert-type scale that ranges from 1=strongly disagree to 5=strongly agree, – higher scores indicating greater barriers • Participants are asked to rate their level of agreement with the statements regardless of CR referral or enrollment Grace et al., 2004; Grace et al., 2009; Grace et al., 2009 Total CR Barriers Scale Scores by Sex and Age Mean SD Males (n=902) 2.5 1.01 Females (n=360) 2.6 0.99 Older (>=65 y; n=698) *** 2.6 1.0 Younger (<65 y; n=575) 2.4 1.0 Note. ***p<.001 Sex Differences in CR Barriers for NonParticipants (n=226 females; n=507 males) Already exercise at home *** Don't need CR * I didn't know about CR Exercise in my community Females Males ** MD doesn't encourage me Manage on my own ** Heart condition not serious 1 2 3 4 5 Note. ***p<.001; **p<.01; *p<.05 Sex Differences for Non-Participants Cont’d ** Exercise tiring or painful Distance Many people don’t go Females Males * Transportation ** Other health problems Cost Work 1 2 3 4 5 Note. **p<.01; *p<.05 Sex Differences for Non-Participants Cont’d * Family Not improve health Females Males Time Caregiving Not offered in my first language 1 Note. *p<.05 2 3 4 5 Sex Differences in CR Barriers for Participants (n=133 females; n=396 males) Already exercise at home * Exercise tiring or painful Work * Females Males Already exercise in community Other health problems Family Manage on my own 1 2 3 4 5 Note. *p<.05 Sex Differences for Participants Cont’d Time Distance Heart condition not serious Females Males Many people don't go Transportation Caregiving I don't need CR 1 2 3 4 5 Sex Differences for Participants Cont’d Cost MD doesn't encourage me Females Males Not improve health I didn't know about CR Not offered in my first language 1 2 3 4 5 Sex Differences: Summary • Overall, there were no significant differences in total CR barriers – This is contrary to previous literature which highlights women’s CR barriers, (Heid et al., 2004; Lieberman et al., 1998; Plach et al., 2002; Marcuccio et al., 2003) although sex differences had yet to be tested through an overall barrier scale • However, male CR participants were significantly more likely to rate work responsibilities as a barrier than females • Among patients not participating in CR, males rated the following barriers significantly more highly than did females: already exercising at home or in the community, and confidence in self-managing their condition – Female CR participants were significantly more likely to rate the tiring or painful nature of exercise as a barrier than males – Female CR non-participants rated the following barriers significantly more highly than did males: transportation, family responsibilities, lack of CR awareness, perceiving exercise as tiring or painful, and comorbid conditions Sex Differences: Implications • Future research is needed to explore interventions to promote greater CR participation among women, and men • Sex-specific recommendations to overcome some of the identified CR barriers such as provision of childcare or home help, and offering exercise variety and choice are made in a review (Beswick et al., 2005) Results – CR Barriers for <65 years (n=575) vs >=65 years (n=698) ** Already exercise at home Already exercise in community I don't need CR ** Exercise tiring or painful Heart condition not serious * I didn't know about CR ** Note. **p<.01; *p<.05 >= 65 < 65 ** Manage on my own 1 2 3 4 5 Age Differences Cont’d *** MD doesn't encourage me Distance Many people don't go *** Other health problems *** Work >=65 <65 *** Transportation Family Note. ***p<.001; *p<.05 * 1 2 3 4 5 Age Differences Cont’d Time *** Cost >=65 <65 *** Not improve health * Caregiving 1 2 3 4 5 Note. ***p<.001; *p<.05 Age Differences in CR Barriers: Implications • Physicians should be encouraged to prescribe CR to elderly patients following coronary events and procedures, (Ferrrara, 2006) to provide written information about CR, and to actively encourage patient participation • Exercise modes and intensities should be carefully prescribed considering older patients’ comorbidities and lower exercise capacity CRBS Resources • Shanmugasegaram, S., Gagliese, L., Oh, P., Stewart, D. E., Brister, S., Chan, V., & Grace, S. L. (Under Review). Psychometric validation of the cardiac rehabilitation barriers scale. Clinical Rehabilitation • http://www.yorku.ca/sgrace/crbarrierssc ale.html Age and Sex Differences JCRP 2009; 29(3), 183-187 REVIEW: Beswick, J Adv N 2005 3. Yet another strategy to increase reach into under-served populations is to offer tailored programming…. WOMEN-ONLY CR CR4HER Pilot & RCT • Completed pilot study • Single-blind pragmatic randomized controlled trial with 3 parallel arms: co-ed, women-only, home based • OBJ 1: to compare women’s CR program adherence, to determine which condition results in the greatest adherence. • 2ndary: to compare (a) exercise capacity, and (b) exercise, diet, medication adherence and smoking behaviour by condition. – Accrual underway A Randomized Trial of Women’s Adherence to Women’s Only, Homebased, and Traditional Cardiac Rehabilitation by Program Model Put your Title here (Cardiac Rehabilitation for Heart Event Recovery [CR4HER]) Sherry L. Grace, PhD – PI1-4; C. Chessex2,3; P. Oh3,4; H.M. Arthur5; L. Pilote6; S. Brister2,3; T. Colella3,4; K. Melvin2,3; D.E. Stewart2,3 1York University, 2University Health Network, 3University of Toronto, 4Toronto Rehabilitation Institute, 5McMaster University, 6McGill University Health Centre sgrace@yorku.ca Introduction Methods • Heart disease is a leading cause of morbidity and mortality for women in Canada (Heart and Stroke Trial Design Foundation of Canada, 2003). • Cardiac rehabilitation (CR) is an outpatient secondary prevention program composed of structured exercise training and comprehensive education and counseling • CR has been shown to reduce mortality by 25%, to reduce the need for rehospitalization and the use of interventional procedures, and to have beneficial effects on cardiac risk factors, psychosocial wellbeing, health behaviours and exercise capacity, all in a cost-effective manner (Taylor, Brown). Women are less likely to adhere to CR programs than men (Grace, 2002; Daly, 2002; Carhart, 1998). Women report these programs as failing to meet their needs and care preferences (Filip, 1999; Moore, 1996). • Alternative models of CR such as homebased and women-only programs have been developed • little is understood about women’s perceptions of and adherence to these Objectives program models. The primary objective of this study is to compare women’s CR program adherence, to determine which condition results in the greatest adherence. The secondary objectives of this study are to: compare (a) exercise capacity, and (b) exercise, diet, medication adherence and smoking behaviour by condition. Third, this study will explore psyc hos ocial and other factors affecting women’s CR adherenc e by condition. Procedure Informed Cons ent Randomization • Referral to 1 of 3 CR program models is made according to a computer-generated randomization sequence • Stratified by diagnosis/procedure • Allocation is concealed Eligibi lity Sc reening Phy s ic ian Clearanc e for CR • Multicentre, single-blind pragmatic randomized (1:1) trial with 3 parallel arms: Pre-tes t s urvey c ompletion + pedometer Randomiz ation 1.mixed-sex traditional hospital-based CR; 2.women-only hospital-based CR; Co-ed CR (n=109) Intak e & D/C as s mt 3.monitored home-based CR (telephone) Pos t-CR s urvey in mail + pedometer Women-Only , n=109 Intak e & D/C as s mt Pos t-CR s urvey in mail + pedometer Home-bas ed, n=109 Intak e & D/C as s mt Pos t-CR s urvey in mail + pedometer • Each intervention is guideline-based (CACR) Participants • Female patients recruited as cardiac inpatients, or outpatients newly referred to CR • Location and setting: Toronto (UHN, MSH, SHSC, TRI) and Hamilton (HHS), ON Outcome Measures • Primary DV of program adherence will be assessed via masked program-report of number of on-site or telephone sessions prescribed and completed • Inclusion Criteria: • CAD, ACS, revascularization, and/or valve surgery • Proficient in English language • to compute % of prescribed sessions completed • Secondary Outcomes: Exercise capacity will be measured by an exercise stress test (Modified Bruce protocol) • written approval from to participate in CR by the patient’s cardiac specialist or GP (in the case of inpatients) • Eligible for home-based CR • i.e., low to moderate risk as demonstrated by: [1] lack of complex ventricular dysrhythmia, • [2] NYHA Class of 1 or 2, and LVEF >40%, or [3] CCS Class 1 or 2. • Exclusion criteria: musculoskeletal, neuromuscular, visual, cognitive or nondysphoric psychiatric condition, or any serious or terminal illness not otherwise specified which would preclude CR eligibility based on CACR guidelines (Stone et al, 2009) • Assessment of exercise behaviour will be via pedometer and self-report (Godin LTEQ). • Diet Habit Survey (Conner) • Medication Adherence Scale (Morisky) Blinding • Participants and CR programs cannot be blind to condition assignment. • We have attempted to ensure exercise staff are blind to condition • A blinded research assistant enters and extracts all study data post-randomization, to mitigate against the risk of ascertainment bias Statistical methods • Analyses will be conducted on an ‘intent-to-treat’ basis • Primary outcom e: an analysis of c ovariance will be perform ed, with program model as the independent variable and % of s essions com pleted as the dependent variable • Secondary objectives comparing exercise c apacity and cardiac risk-reducing behaviours by c ondition, ANCOVAs will be us ed • Finally, an exploratory analysis of factors affecting CR adherenc e by program m odel will be performed using ANOVA. Funding • Smoking: self-report • Third Obj: Cardiac Rehabilitation Barriers Scale (Grace) Sample Size • • Based on pilot study, we require 261 participants with 87 randomized to each condition, to ensure 80% power at the 5% significance level to detect a difference in program adherence. Recruiting 326 at baseline to take attrition into account Registration The trial is registered at ClinicalTrials.gov, number: NCT01019135 Acknowledgements • CRCARE study co-investigators: Stewart, Anand, Gupta, Reid, Alter, Oh, Rush • Study staff and grad students: notably Kelly Russell, Shamila Shanmugasegaram • CONTACT: sgrace@yorku.ca
© Copyright 2025