Prostate Cancer Diagnosis Among Men With Isolated
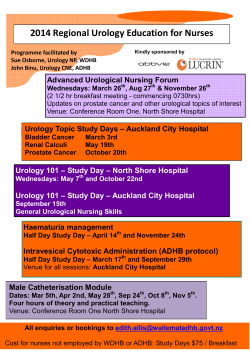
Published Ahead of Print on January 7, 2013 as 10.1200/JCO.2012.41.7634 The latest version is at http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.41.7634 JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T Prostate Cancer Diagnosis Among Men With Isolated High-Grade Intraepithelial Neoplasia Enrolled Onto a 3-Year Prospective Phase III Clinical Trial of Oral Toremifene Samir S. Taneja, Ronald Morton, Gary Barnette, Paul Sieber, Michael L. Hancock, and Mitchell Steiner See accompanying editorial doi: 10.1200/JCO.2012.46.6151 Samir S. Taneja, New York University Langone Medical Center, New York, NY; Ronald Morton, Gary Barnette, Michael L. Hancock, and Mitchell Steiner, GTx, Memphis, TN; Paul Sieber, Urological Associates of Lancaster, Lancaster, PA. Published online ahead of print at www.jco.org on January 7, 2013 Supported by GTx, Memphis, TN. Presented at the 2011 American Urological Association Annual Meeting, May 14-19, 2011, Washington, DC. Authors’ disclosures of potential conflicts of interest and author contributions are found at the end of this article. Clinical trial information: NCT00106691. Corresponding author: Samir S. Taneja, MD, Division of Urologic Oncology, 150 East 32nd St, Ste 200, New York, NY 10016; e-mail: samir.taneja@nyumc.org. © 2013 by American Society of Clinical Oncology 0732-183X/13/3099-1/$20.00 DOI: 10.1200/JCO.2012.41.7634 A B S T R A C T Purpose Prostate cancer (PCa) prevention remains an appealing strategy for the reduction of overtreatment and secondary adverse effects. We evaluated the efficacy of toremifene citrate 20 mg in PCa prevention among men with isolated high-grade prostatic intraepithelial neoplasia (HGPIN) on biopsy. Patients and Methods One thousand five hundred ninety men with HGPIN, or HGPIN and atypia, and no PCa on prostate biopsy were randomly assigned 1:1 to receive toremifene citrate 20 mg or placebo in a 3-year phase III, double-blind, multicenter trial. Men underwent annual biopsy until cancer detection or study end. Efficacy analysis was performed in 1,467 men who underwent at least one on-study biopsy. Baseline risk factors were evaluated to determine influence on cancer detection. Results Cancer was detected in 34.7% and 32.3% of men in the placebo and treatment groups, respectively, with no observed difference (P ⫽ .39, log-rank test) in PCa-free survival. The 3-year Kaplan-Meier PCa-free survival estimate was 54.9% (99% CI, 43.3% to 66.5%) in the placebo group and 59.5% (99% CI, 48.1% to 70.9%) in the treatment group. Exploration of baseline risk factors demonstrated no subset in which a risk reduction was observed. In the placebo group, 17.9%, 12.9%, and 13.6% of men at risk at the beginning of years 1, 2, and 3, respectively, were diagnosed with PCa. Conclusion Although toremifene 20 mg did not lower the PCa detection rate, men with isolated HGPIN have a high likelihood of eventual PCa diagnosis, demonstrating they are ideal candidates for inclusion in chemoprevention trials and require surveillance by periodic prostate biopsy. J Clin Oncol 30. © 2013 by American Society of Clinical Oncology INTRODUCTION Prostate cancer (PCa) is the most commonly diagnosed solid malignancy and the second-leading cause of cancer death among American men.1 Treatment of PCa results in the potential for significant long-term urinary and sexual dysfunction, making prevention of PCa among men at increased risk most desirable if it can be achieved with acceptable toxicity and cost.2-4 Challenges in broad implementation of chemoprevention for PCa include both selection of agent and defining an appropriate atrisk population. High-grade prostatic intraepithelial neoplasia (HGPIN) is a premalignant histologic entity.5-7 Its presence on prostate biopsy has been implicated as a surrogate measure of coexistent PCa, but with the adaptation of lower prostate-specific antigen (PSA) cutoffs for biopsy and increased biopsy core numbers at sampling, a lower likelihood of occult cancer detection on immediate repeat biopsy has been noted.8-11 The long-term risk of PCa among men with isolated HGPIN on biopsy is not well defined, and the optimal strategies for clinical management of these men have been controversial.12-14 We hypothesized that the high rate of coexistent cancer and the premalignant nature of HGPIN make these men ideal candidates for testing chemoprevention strategies. Estrogens play a significant role in prostate carcinogenesis and PCa proliferation in animal models.15,16 In a noncastrate environment, estrogen receptor (ER) ␣ serves as mediator of growthstimulatory signal transduction through initiation © 2013 by American Society of Clinical Oncology Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. Copyright 2013 by American Society of Clinical Oncology 1 Taneja et al of stromal paracrine effect on PCa epithelium, whereas ER- mediates a direct antiproliferative effect on the epithelial compartment.17 Toremifene citrate is an oral selective ER modulator approved by the US Food and Drug Administration for the treatment of advanced breast cancer. At low concentrations, toremifene selectively inhibits ER-␣.18,19 In both preclinical studies and a dose-finding phase IIb clinical trial, toremifene reduced the progression of premalignant HGPIN to PCa.20 On the basis of these studies, we undertook a randomized phase III, double-blind, placebo-controlled clinical trial of toremifene 20 mg for prevention of PCa in 1,590 men with isolated HGPIN on biopsy treated for 3 years. PATIENTS AND METHODS Study Design This was a 3-year, phase III, randomized, double-blind, placebocontrolled, multicenter clinical trial to evaluate the efficacy and safety of toremifene for prevention of PCa in men with isolated HGPIN on prostate biopsy. Men were randomly assigned 1:1 to receive toremifene 20 mg oral daily or matching placebo. Isolated HGPIN was defined as men with HGPIN, with or without coexistent atypical small acinar proliferation (ASAP), and no evidence of cancer on biopsy. A sample size of 1,260 men was estimated to detect a difference in PCa-free survival between treatment and placebo arms using a log-rank test, based on 1-year PCa-free survival rates of 81% and 73% in treatment and placebo arms, respectively, and a 3-year trial with no additional follow-up (␣ ⫽ .01, power ⫽ 90%). Final sample size increased to 1,590 men on US Food and Drug Administration request of additional patients for an ocular substudy late in the trial. The study was designed and conducted by the sponsor (GTx, Memphis, TN) and the principal investigator (S.S.T.). Local institutional review board approval was obtained at each of 140 sites (Appendix Table A1, online only), and all men signed informed consent before enrollment. Health Decisions (Raleigh, NC) provided data management, Bostwick Laboratories (Glen Allen, VA) provided central anatomic pathology services, and CRL Medinet (Lenexa, KS) provided central laboratory services. An independent data and safety monitoring board met semiannually to oversee the study and monitor patient safety. Participants The study included men age ⱖ 30 years diagnosed with isolated HGPIN on prostate biopsy confirmed by a central pathology reading. All men had baseline serum PSA ⱕ 10 ng/mL; adequate bone marrow, liver, and renal function; and a minimum 10-core negative prostate biopsy within 6 months of random assignment or two minimum negative six-core biopsies within 12 months of random assignment. The study excluded men with exposure to toremifene, finasteride within 30 days of random assignment, dutasteride within 90 days of random assignment, or PC-SPES or saw palmetto within 2 years of random assignment or a history of thromboembolic disease, chronic hepatitis, or cirrhosis. End Points The primary end point was PCa-free survival as determined by transrectal ultrasound– guided needle biopsy of the prostate. Secondary assessments included the effects of toremifene on detection of HGPIN, lipid levels, gonadal steroids, serum PSA, American Urological Association symptom score, and Gleason grade. Study Procedures Transrectal ultrasound– guided biopsies of the prostate with a minimum of 10 cores were obtained at months 12, 24, and 36 or until a diagnosis of PCa. All pathologic specimens were analyzed by the central anatomic pathology lab. Serum PSA levels were obtained at baseline, 3 months, and 6 months, and every 6 months thereafter. Serum hormones (testosterone, dihydrotestos2 © 2013 by American Society of Clinical Oncology terone, and estradiol) were obtained at baseline and every 6 months thereafter. All labs were analyzed at a central laboratory. Adverse events (AEs), recorded at baseline and at each interval monitoring visit, were assessed for duration, intensity, and necessary intervention. Each AE was additionally determined to be related to the study drug, concurrent disease, reaction to concomitant medication, or progressive disease states, when appropriate. Treatment compliance was calculated by applying the following formula: No. of pills dispensed – No. of pills returned or unused ⫻ 100/No. of pills to be taken during the study. Statistical Analyses The probability of development of PCa was estimated using the KaplanMeier method, and SEs of the estimates were calculated with the Peto-Pike formula.21,22 Time was calculated from the date of first dose of study drug until the date of PCa diagnosis or date of last visit for censored patients. The distributions of Gleason grades were compared between treatments using Fisher’s exact test. Change in serum hormones (total testosterone, dihydrotestosterone, and estradiol) from baseline to end of study were compared between arms using analysis of variance with treatment arm as the single factor. Presenting and demographic features of known or suspected prognostic significance for the development of PCa were explored using a Cox proportional hazards model. Factors were examined first in univariate models, and those factors significant at P ⬍ .20 were then included in a multivariate model. The variables included in the final model were baseline age, baseline PSA value, baseline ASAP status (present, absent), PSA velocity (last observation), and the time-dependent covariates of digital rectal examination (DRE) result (normal, abnormal) and prostate volume. P values are two-sided and unadjusted for multiple comparisons, and P ⬍ .01 is considered significant. RESULTS Study Participants Of 1,590 men who were randomly assigned, 787 and 803 men were assigned to receive toremifene or placebo, respectively (Fig 1). Median age of the men was 64 years (range, 41 to 87 years; Table 1). Safety analyses included 1,589 randomly assigned men who received ⱖ one dose of study medication. Efficacy analyses included 1,426 men in the modified intent-to-treat (MITT) cohort with ⱖ one on-study biopsy of the prostate. Biopsy compliance was 98%, 98%, and 100% among 1,361, 1,003, and 780 at-risk participants eligible for biopsy at years 1, 2, and 3, respectively. Among excluded patients, 85 patients in the placebo group and 77 patients in the toremifene group did not undergo an on-study prostate biopsy, one patient was found to have had PCa on baseline central pathology review, and one patient was not dosed. Treatment compliance was 97.2% (⫾ 27.3%) and 98.12% (⫾ 40.7%) among participants receiving placebo and toremifene, respectively. PCa-Free Survival The primary efficacy end point for the trial was PCa-free survival in the MITT cohort. Two hundred forty-nine cancer events (34.7%) occurred in the placebo group, and 229 cancer events (32.3%) occurred in the treatment group. The 3-year Kaplan-Meier cancer-free survival estimate was 54.9% (99% CI, 43.3% to 66.5%) in the placebo group and 59.5% (99% CI, 48.1% to 70.9%) in the treatment group (Fig 2). There was no observed difference (P ⫽ .39, log-rank test) in PCa-free survival. Among men in the MITT population with a single baseline core positive for HGPIN, the PCa progression-free survival estimate at 3 years was 60.1% (99% CI, 50.2% to 70.0%) compared with 51.4% (99% CI, 37.2% to 65.6%) for men with greater than one core demonstrating HGPIN (P ⬍ .001, log-rank test). JOURNAL OF CLINICAL ONCOLOGY Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. Prostate Cancer Detection Among Men With HGPIN Assessed for eligibilty (N = 3,004) Excluded Did not meet inclusion criteria Declined to participate Had other reasons (n = 1,414) (n = 1,176) (n = 166) (n = 72) Randomly assigned (n = 1,590) Assigned to toremifene (n = 787) Assigned to placebo (n = 803) Did not receive drug (n = 1) Included in safety analyses (n = 787) Included in safety analyses (n = 802) Excluded from efficacy analyses (n = 78) Had screening biopsy only (n = 77) Had prostate cancer at screening (n = 1) Excluded from efficacy analyses Had screening biopsy only (n = 85) (n = 85) Included in efficacy analyses (n = 709) Included in efficacy analyses (n = 717) Did not complete study (n = 122) Withdrew consent (n = 51) Adverse experience (n = 32) Investigator/sponsor decision (n = 17) Noncompliance (n = 3) Lost to follow-up (n = 11) Other protocol violation (n = 5) Other (n = 3) + 49 of the above were found to have prostate cancer on their end of study biopsy Did not complete study (n = 119) Withdrew consent (n = 54) Adverse experience (n = 25) Investigator/sponsor decision (n = 12) Noncompliance (n = 5) Lost to follow-up (n = 13) Other protocol violation (n = 2) Other (n = 8) + 51 of the above were found to have prostate cancer on their end of study biopsy Completed the 36-month study Completed cancer free Diagnosed with prostate cancer Completed the 36-month study Completed cancer free Diagnosed with prostate cancer (n = 587) (n = 407) (n = 180) (n = 598) (n = 400) (n = 198) Fig 1. CONSORT diagram showing patient enrollment, random assignment, and final analysis. Gleason Grade Among men diagnosed with PCa, 79.5% within the placebo group and 82.4% in the toremifene group had a Gleason score of 6. The next most commonly observed Gleason score was 7 (17.4% of the placebo group and 15.6% of the toremifene group), whereas 3.1% and 2% of patients in the placebo and toremifene groups, respectively, had Gleason scores of more than 7. The distributions of Gleason grades did not differ (P ⫽ .84) between the two groups. Exploratory Covariates A number of exploratory covariates, specified before data analysis, were examined for influence on cancer detection within the MITT population, including race, number of biopsy cores with HGPIN at baseline, age, presence of ASAP at baseline, family history of PCa, time www.jco.org from HGPIN diagnosis until random assignment, prostate volume, PSA velocity, and PSA. After accounting for all covariates, the hazard ratio for cancer detection in the toremifene group was 1.0 (99% CI, 0.8 to 1.3), consistent with the overall observation that there was no difference (P ⫽ .91) between the two groups. Among the covariates in the multivariate model described earlier, baseline PSA, presence of ASAP in the baseline biopsy, the last computed PSA velocity, and the time-dependent covariates of prostate volume and DRE result each were statistically significant (P ⬍ .001 for each) prognostic factors for the development of PCa (Table 2). PCa-Free Survival in Placebo Group As previously mentioned, 34.7% of men in the placebo group were diagnosed with PCa. Among men in the placebo group, the © 2013 by American Society of Clinical Oncology Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. 3 Taneja et al 1.0 Table 1. Baseline Demographics and Clinical Characteristics of Men Enrolled Onto the Trial and Randomly Assigned to Placebo or Toremifene Demographic or Clinical Characteristic Age, years Median Range Race White Black Other Ethnicity Hispanic Body mass index, kg/m2 Mean SD Relative with history of prostate cancer Father Sibling ASAP present at screening HGPIN diagnosed ⬎ 1 year before random assignment History of BPH Abnormal digital rectal examination Prostate volume, cm3 Mean SD PSA, ng/mL Mean SD No. of cores Median Range Mean SD Patients with single core with HGPIN No. of Patients % 65 41-85 Placebo (n ⫽ 802) No. of Patients % 65 38-87 0.6 0.4 0.2 693 76 18 88.1 9.7 2.2 684 94 24 85.3 11.7 3.0 30 3.8 31 3.9 28.8 4.8 102 46 137 13.0 5.8 17.4 94 56 168 11.7 7.0 20.9 90 496 285 11.4 63.0 39.9 80 494 304 10.0 61.6 41.5 48.6 23.6 47.9 22.4 4.5 2.6 4.3 2.5 12 6-83 14.6 6.6 500 63.5 12 6-46 14.5 5.4 503 62.7 36-month PCa-free survival probability was 52.2% (99% CI, 37.1% to 67.3%) for men with a normal DRE at baseline compared with 59.3% (99% CI, 40.9% to 77.7%) for men with an abnormal DRE. In the MITT placebo group, 17.9%, 12.9%, and 13.6% of men at risk at the beginning of years 1, 2, and 3, respectively, were diagnosed with PCa. Serum Hormone Levels In men treated with toremifene versus placebo, greater increases in total testosterone (31.1% ⫾ 63.6% v 2.2% ⫾ 102.9%, respectively; P ⬍ .001), dihydrotestosterone (46.4% ⫾ 60.2% v 17.7% ⫾ 48.3%, respectively; P ⬍ .001), and estradiol levels (53.2% ⫾ 151.5% v 11.9% ⫾ 67.9%, respectively; P ⬍ .001) were noted at final assessment. Adverse Events The number of men who died, had a serious AE, had any AE, or discontinued participation in the study because of an AE did not significantly differ between study groups (Table 3). The most commonly reported AEs for both groups were hypertension, arthralgia, © 2013 by American Society of Clinical Oncology Placebo Toremifene 20 mg Log-rank P = .39 0 365 730 1,095 1,200 Time (days) Fig 2. Kaplan-Meier analysis of cancer diagnosis among men treated with toremifene citrate and placebo. The 3-year Kaplan-Meier cancer-free survival estimate was 54.9% (99% CI, 43.3% to 66.5%) in the placebo group and 59.5% (99% CI, 48.1% to 70.9%) in the toremifene group. 28.7 4.6 Abbreviations: ASAP, atypical small acinar proliferation; BPH, benign prostatic hyperplasia; HGPIN, high-grade prostatic intraepithelial neoplasia; PSA, prostate-specific antigen; SD, standard deviation. 4 0.8 Probability Toremifene (n ⫽ 787) urinary tract infection, upper respiratory tract infection, prostatitis, and erectile dysfunction; rates for each of these AEs were similar for men assigned to either group. Venous thromboembolic events defined as pulmonary embolism or deep venous thrombosis were uncommon and balanced between groups. In the placebo group, there was one deep vein thrombosis and two pulmonary embolisms (0.4%), whereas in the toremifene group, there were three deep vein thromboses and one pulmonary embolism (0.5%). DISCUSSION The current phase III clinical trial did not show an effect of toremifene on the likelihood of PCa diagnosis in men with isolated HGPIN on baseline biopsy. Exploration of multiple covariates, including the volume of HGPIN at baseline, did not reveal a therapeutic effect in any subgroup. The likelihood of HGPIN on serial study biopsy was also not reduced by treatment. A randomized, phase IIb dose-finding clinical study of toremifene in 514 men with isolated HGPIN demonstrated a 21.8% (P ⫽ .048, Mantel-Cox analysis stratified by treatment site) cumulative relative risk reduction in PCa detected on follow-up biopsies performed 6 months and 12 months after initiation of therapy with toremifene citrate 20 mg.20 Distinctions between the current study and the previously reported phase IIb clinical study include more stringent baseline sampling criteria, longer treatment period (3 years v 1 year), and less frequent sampling (yearly v every 6 months). It was the intent of these design modifications to provide a more pure population of men with isolated HGPIN who were less likely to harbor occult malignancy, undiagnosed on inclusion biopsy, and, therefore, more likely to benefit from prolonged exposure to the drug. It is notable that the rate of cancer diagnosis on the year 1 scheduled biopsy in this trial did not differ greatly from the 6-month biopsy in the phase IIb trial, suggesting a significant rate of occult, coexistent cancer despite more extensive baseline sampling.20 To our knowledge, this is the largest prospective evaluation of men with isolated HGPIN reported to date. The study allows several JOURNAL OF CLINICAL ONCOLOGY Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. Prostate Cancer Detection Among Men With HGPIN Table 2. Univariate and Multivariate Analyses of Baseline and Clinical Features Potentially Predictive of Cancer Diagnosis Univariate Analysesⴱ Multivariable Analyses† Factor Hazard Ratio 95% CI P Hazard Ratio 95% CI P Age PSA at baseline Presence of ASAP at baseline PSA velocity Greater prostate volume (TRUS) Normal DRE 1.02 1.05 1.81 1.05 1.00 0.87 1.00 to 1.03 1.02 to 1.08 1.48 to 2.21 1.04 to 1.06 0.99 to 1.00 0.71 to 1.06 .019 .003 ⬍ .001 ⬍ .001 .002 .17 1.02 1.09 1.91 1.05 0.989 0.89 1.00 to 1.03 1.06 to 1.13 1.54 to 2.36 1.04 to 1.07 0.985 to 0.994 0.72 to 1.10 .009 ⬍ .001 ⬍ .001 ⬍ .001 ⬍ .001 .28 NOTE. Variables were examined first in univariate models, and those reaching significance at P ⬍ .20 were evaluated by a Cox proportional hazards model. The variables included in the final multivariate model were baseline age, baseline PSA value, baseline ASAP status (present, absent), PSA velocity (last observation), and the time dependent covariates of DRE result (normal, abnormal) and prostate volume. P values are two sided and unadjusted for multiple comparisons, and P ⬍ .01 is considered significant. Abbreviations: ASAP, atypical small acinar proliferation; DRE, digital rectal examination; PSA, prostate-specific antigen; TRUS, transrectal ultrasound. ⴱ Factor adjusted for treatment. †Factor adjusted for treatment and all other factors listed. observations regarding the 3-year risk of cancer in men with isolated HGPIN, the influence of serial annual sampling on cancer detection, and potential considerations for future clinical trial design in this at-risk population. By Kaplan-Meier estimate, the 3-year freedom from cancer rate in this trial was 52.2%, with 33.5% of men in the group diagnosed with cancer during the course of the study. The observed rate of detection on repeat biopsy in year 1 is higher than that reported in several smaller, retrospective series of men with isolated HGPIN.8,21,22 Whether the longitudinal rate of cancer detection re- Table 3. Most Commonly Observed Adverse Events (⬎ 3% in overall population) Among Men Treated With Placebo and Toremifene Citrate Toremifene 20 mg (n ⫽ 787) Placebo (n ⫽ 802) Adverse Event Hypertension Arthralgia Urinary tract infection Upper respiratory tract infection Prostatitis Erectile dysfunction Hematuria Back pain Dizziness Nasopharyngitis Benign prostatic hyperplasia Pain in extremity Fatigue Gastroesophageal reflux disease Pollakiuria Cataract Insomnia Sinusitis Urinary retention Constipation Headache www.jco.org Overall (N ⫽ 1,589) No. of Patients % No. of Patients % No. of Patients % 70 50 8.7 6.2 52 46 6.6 5.8 122 96 7.7 6.0 54 6.7 41 5.2 95 6.0 46 49 42 38 36 37 39 5.7 6.1 5.2 4.7 4.5 4.6 4.9 45 39 42 36 31 30 28 5.7 5.0 5.3 4.6 3.9 3.8 3.6 91 88 84 74 67 67 67 5.7 5.5 5.3 4.7 4.2 4.2 4.2 30 29 31 3.7 3.6 3.9 32 32 28 4.1 4.1 3.6 62 61 59 3.9 3.8 3.7 32 30 24 32 21 24 27 27 4.0 3.7 3.0 4.0 2.6 3.0 3.4 3.4 24 26 29 21 32 29 24 22 3.0 3.3 3.7 2.7 4.1 3.7 3.0 2.8 56 56 53 53 53 53 51 49 3.5 3.5 3.3 3.3 3.3 3.3 3.2 3.1 flects an increased risk of occult cancer or de novo cancer progression among men with HGPIN or, in part, the frequency of sampling cannot be determined in the absence of a control group of men without isolated HGPIN who are serially biopsied on an annual basis. Nonetheless, the observed rate of cancer detection has substantial implications for the management of these men, particularly those who are found to have HGPIN at a young age, in whom prolonged follow-up is necessary. Many of these men would ultimately be biopsied in clinical practice, diagnosed with cancer, and treated. To date, the long-term natural history of HGPIN in men has only been evaluated in small series. Lefkowitz et al12 demonstrated that empiric repeat biopsy 3 years after the diagnosis of HGPIN on 12-core biopsy resulted in a cancer detection of 25.8%, compared with 2.3% when biopsied within 1 year of diagnosis. Recent follow-up from the same group, using a surveillance strategy of serial biopsy every 2 to 3 years among men with stable PSA level, demonstrated that 22.3% and 23.4% of men were found to have cancer on repeat sampling at a mean interval of 34.4 and 66.2 months, respectively.23 Overall, 32.1% of men were found to have PCa at a median follow-up of 46.6 months, and 40 men had not yet undergone second repeat biopsy. Several other groups have demonstrated a relatively high rate of cancer detection on delayed repeat biopsy in men with HGPIN.13,14,24,25 Recently, in a single-institution retrospective cohort, it was suggested that the greatest magnitude of risk for cancer detection at prolonged follow-up is in men with multifocal HGPIN, whereas those with limited focality disease had disease risk comparable to men with benign baseline biopsies.13 We did observe a lower risk of cancer among men with a single core positive for HGPIN at baseline compared with men with two or more cores on univariate analysis, but this was not observed on multivariate analysis. At present, there is no consensus on the management of men with HGPIN, and no pervasive standard of care exists in community practice. Contemporary series have suggested that the risk of cancer detection on immediate rebiopsy of men with isolated HGPIN is quite low and may be no greater in men with HGPIN than those with benign biopsies.21 As such, immediate repeat biopsy is generally not recommended for men with HGPIN, but there are limited data on the long-term risk of cancer in these men. It is interesting to note that among men in the placebo arm of this trial, cancer was detected in © 2013 by American Society of Clinical Oncology Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. 5 Taneja et al 17.9%, 12.9%, and 13.2% of men biopsied in years 1, 2, and 3, respectively. This is distinct from screening cohorts in which a serial decline in cancer detection rate is typically noted on sequential sampling of men with elevated PSA and benign biopsy. In the European Randomized Study of Screening for Prostate Cancer, men underwent two rounds of screening biopsies separated by 4 years.26 Among men with negative baseline screening with follow-up PSA more than 4.0 ng/mL, the rate of cancer detection on second biopsy was 8.3%. In this series, baseline and repeat biopsies were sextant biopsies, suggesting that with baseline extended core biopsy, the rate of cancer detection may have been lower. Both the Prostate Cancer Prevention Trial (PCPT) and the Reduction by Dutasteride of Prostate Cancer Events (REDUCE) trial compared 5␣-reductase inhibitors with placebo as prevention agents for PCa.27,28 In the REDUCE trial, repeat biopsies performed in the placebo arm at 2 and 4 years demonstrated cancer in 17.2% and 11.9% of men, respectively.28 No difference in Gleason score was observed between placebo and treatment groups in this study; 20.5% of cancers identified in the placebo arm of the study were Gleason score ⱖ 7, demonstrating the potential for isolated HGPIN to coexist with high-grade disease and suggesting that biopsy surveillance is warranted in these men. In the REDUCE trial, 27.4% of men on placebo were found to have a Gleason score ⱖ 7 disease. When stratified by biopsy, only 21.4% of men demonstrated high-grade disease at the 4-year biopsy, compared with 30.3% of men at the 2-year sampling. Our observed rate of Gleason score 6 cancer may, in part, be a result of our frequent sampling regimen because it is, perhaps, intuitive that repeat sampling would result in a downward stage and grade migration. The fact that men with small-volume, Gleason 6 cancers are most often subjected to treatment, with potential for substantial adverse effects, supports the assertion that men with HGPIN on biopsy may be ideally suited for chemoprevention efforts. Men with isolated HGPIN on prostate biopsy are at a relatively high risk of cancer diagnosis in long-term follow-up by serial biopsy. The high rate of cancer diagnosis on surveillance biopsy in short-term REFERENCES 1. Jemal A, Siegel R, Xu J, et al: Cancer statistics, 2010. CA Cancer J Clin 60:277-300, 2010 2. Lieberman R: Chemoprevention of prostate cancer: Current status and future directions. Cancer Metastasis Rev 21:297-309, 2002 3. Brewster AM, Patterson SL, Forman MR, et al: Conference report: Eighth Annual AACR International Conference on Frontiers in Cancer Prevention Research. Cancer Prev Res 3:1044-1048, 2010 4. Lippman SM, Lee JJ: Reducing the “risk” of chemoprevention: Defining and targeting high risk— 2005 AACR Cancer Res and Prevention Foundation Award Lecture. Cancer Res 66:2893-2903, 2006 5. Schlesinger C, Bostwick DG, Iczkowski KA: High-grade prostatic intraepithelial neoplasia and atypical small acinar proliferation: Predictive value for cancer in current practice. Am J Surg Pathol 29:1201-1207, 2005 6. McNeal JE, Bostwick DG: Intraductal dysplasia: A premalignant lesion of the prostate. Hum Pathol 17:64-71, 1986 7. Bostwick DG, Qian J: High-grade prostatic intraepithelial neoplasia. Mod Pathol 17:360-379, 2004 6 © 2013 by American Society of Clinical Oncology follow-up suggests a high rate of coexistent cancer and/or de novo cancer progression among men with isolated HGPIN on biopsy. Long-term management of men with HGPIN should include surveillance by periodic prostate biopsy while balancing the risk of oversampling through too frequent biopsy. Although toremifene citrate 20 mg does not lower the risk of cancer in men with isolated HGPIN on prostate biopsy, these men do seem to represent an ideal group for consideration of prevention strategies. AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST Although all authors completed the disclosure declaration, the following author(s) and/or an author’s immediate family member(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO’s conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors. Employment or Leadership Position: Ronald Morton, GTx (C); Gary Barnette, GTx (C); Michael L. Hancock, GTx (C); Mitchell Steiner, GTx (C) Consultant or Advisory Role: Samir S. Taneja, GTx (C); Paul Sieber, GTx (C) Stock Ownership: Ronald Morton, GTx; Gary Barnette, GTx; Michael L. Hancock, GTx; Mitchell Steiner, GTx Honoraria: Paul Sieber, GTx Research Funding: Samir S. Taneja, Gtx; Paul Sieber, GTx Expert Testimony: None Other Remuneration: None AUTHOR CONTRIBUTIONS Conception and design: Samir S. Taneja, Gary Barnette, Mitchell Steiner Collection and assembly of data: Samir S. Taneja, Gary Barnette Data analysis and interpretation: Samir S. Taneja, Ronald Morton, Paul Sieber, Michael L. Hancock Manuscript writing: All authors Final approval of manuscript: All authors 8. Lefkowitz GK, Sidhu GS, Torre P, et al: Is repeat prostate biopsy for high-grade prostatic intraepithelial neoplasia necessary after routine 12-core sampling? Urology 58:999-1003, 2001 9. Weinstein MH, Epstein JI: Significance of high-grade prostatic intraepithelial neoplasia on needle biopsy. Hum Pathol 24:624-629, 1993 10. Herawi M, Kahane H, Cavallo C, et al: Risk of prostate cancer on first re-biopsy within 1 year following a diagnosis of high grade prostatic intraepithelial neoplasia is related to the number of cores sampled. J Urol 175:121-124, 2006 11. Kronz JD, Allan CH, Shaikh AA, et al: Predicting cancer following a diagnosis of high-grade prostatic intraepithelial neoplasia on needle biopsy: Data on men with more than one follow-up biopsy. Am J Surg Pathol 25:1079-1085, 2001 12. Lefkowitz GK, Taneja SS, Brown J, et al: Followup interval prostate biopsy 3 years after diagnosis of high grade prostatic intraepithelial neoplasia is associated with high likelihood of prostate cancer, independent of change in prostate specific antigen levels. J Urol 168:1415-1418, 2002 13. Lee MC, Moussa AS, Yu C, et al: Multifocal high grade prostatic intraepithelial neoplasia is a risk factor for subsequent prostate cancer. J Urol 184: 1958-1962, 2010 14. Abdel-Khalek M, El-Baz M, Ibrahiem el-H: Predictors of prostate cancer on extended biopsy in patients with high-grade prostatic intraepithelial neoplasia: A multivariate analysis model. BJU Int 94: 528-533, 2004 15. Risbridger GP, Bianco JJ, Ellem SJ, et al: Oestrogens and prostate cancer. Endocr Relat Cancer 10:187-191, 2003 16. Ho SM: Estrogens and anti-estrogens: Key mediators of prostate carcinogenesis and new therapeutic candidates. J Cell Biochem 91:491-503, 2004 17. Leav I, Lau KM, Adams JY, et al: Comparative studies of the estrogen receptors beta and alpha and the androgen receptor in normal human prostate glands, dysplasia, and in primary and metastatic carcinoma. Am J Pathol 159:79-92, 2001 18. Taneja SS, Smith MR, Dalton JT, et al: Toremifene: A promising therapy for the prevention of prostate cancer and complications of androgen deprivation therapy. Expert Opin Investig Drugs 15:293-305, 2006 19. Steiner MS, Raghow S: Antiestrogens and selective estrogen receptor modulators reduce prostate cancer risk. World J Urol 21:31-36, 2003 20. Price D, Stein B, Sieber P, et al: Toremifene for the prevention of prostate cancer in men with JOURNAL OF CLINICAL ONCOLOGY Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. Prostate Cancer Detection Among Men With HGPIN high grade prostatic intraepithelial neoplasia: Results of a double-blind, placebo controlled, phase IIB clinical trial. J Urol 176:965-970, 2006 21. Epstein JI, Herawi M: Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: Implications for patient care. J Urol 175:820-834, 2006 22. Netto GJ, Epstein JI: Widespread high-grade prostatic intraepithelial neoplasia on prostatic needle biopsy: A significant likelihood of subsequently diagnosed adenocarcinoma. Am J Surg Pathol 30:11841188, 2006 23. Godoy G, Huang GJ, Patel T, et al: Long-term follow-up of men with isolated high-grade prostatic intra-epithelial neoplasia followed by serial delayed interval biopsy. Urology 77:669-674, 2011 24. Roscigno M, Scattoni V, Freschi M, et al: Monofocal and plurifocal high-grade prostatic intraepithelial neoplasia on extended prostate biopsies: Factors predicting cancer detection on extended repeat biopsy. Urology 63:1105-1110, 2004 25. Akhavan A, Keith JD, Bastacky SI, et al: The proportion of cores with high-grade prostatic intraepithelial neoplasia on extended-pattern needle biopsy is significantly associated with prostate cancer on site-directed repeat biopsy. BJU Int 99:765-769, 2007 26. Roobol MJ, van der Cruijsen IW, Schröder FH: No reason for immediate repeat sextant biopsy after negative initial sextant biopsy in men with PSA level of 4.0 ng/mL or greater (ERSPC, Rotterdam). Urology 63:892-897, 2004 27. Thompson IM, Goodman PJ, Tangen CM, et al: The influence of finasteride on the development of prostate cancer. N Engl J Med 349:215-224, 2003 28. Andriole GL, Bostwick DG, Brawley OW, et al: Effect of dutasteride on the risk of prostate cancer. N Engl J Med 362:1192-1202, 2010 ■ ■ ■ www.jco.org © 2013 by American Society of Clinical Oncology Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. 7 Taneja et al Appendix Table A1. Investigators and Investigation Sites PI Last Name Bailen Belkoff Bhayani Cartwright Chu Colombo Cowan Efros Eure Fairchild Feldman Forrest Gervasi Gingrich Gittelman Lilly Hackett Palmer Harrison Hatcher Hudnall Castellanos Immergut Jablonski Jacob Jensen Kahnoski Kernen Kotkin Cantwell Kriteman Linder McMurray Hertzman Murdock Murphy O’Leary Oselinsky Pearson Pinto Shore Sieber Snoy Stallings Stein Stringer Taneja Teigland White, Jr. Zinner Klimberg Mazo Peterson Jones Goldenberg Cunningham PI First Name James L. Laurence H. Sam B. Charles Franklin Giovanni Barrett Mitchell Gregg Thomas Robert A. John B. Lawrence Jeffrey Marc Joel D. Kevin C. Thomas E. Emerson Paul A. Clayton H. Ronald Mark David H. David James C. Richard J. Kenneth Leonid Anthony Lewis S. Earle S. James G. Bernard L. Myron I. Brian P. Michael David Richard Arthur Neal D. Paul Frederick J. J. Walt Barry S. Thomas Samir Chris Charles F. Norman Ira W. Richard Andrew C. William Terry Samuel F. David Practice City State/Territory Metropolitan Urology, PSC Urologic Surgery, PC Washington University Urologic Research Center UroSearch - Dr Cartwright San Bernardino Urological Associates Specialty Care Research Urology Associates, PC AccuMed Research Associates Devine-Tidewater Urology Spokane Urology Connecticut Clinical Research Center Urology Specialists of Oklahoma Southwest Urology University of Pittsburgh South Florida Medical Research Seattle Urological Associates The Urological Center, PA Regional Urology, LLC Georgia Urology, PA Volunteer Research Group Urology San Antonio Research, PA Southwest Florida Urologic Associates Mid Atlantic Clinical Research Winter Park Urology Associates DMI Research Advanced Clinical Research Michigan Medical, PC Urology Michigan Institute of Urology (Research Department) Boston Clinical Trials Atlantic Urological Associates North Fulton Urology, PC Hamilton Urology PA Medical Affiliated Research Center Tri-State Urologic Services, PSC dba The Urology Group Myron I. Murdock, MD, LLC Urologic Associates of Allentown Brigham and Women’s Hospital State College Urologic Associates The Conrad/Pearson Clinic, PC Urological Associates of Bridgeport Carolina Urologic Research Center Urological Associates of Lancaster, Ltd Urology Group of New Mexico Arkansas Urology University Urological Research Institute UroSearch–Dr Stringer New York University Urology Associates McKay Urology Coastal Clinical Research Western Clinical Research Florida Foundation for Healthcare Research St Joseph’s/Candler Health System, Office of Research Urology Services Madigan Army Medical Center Urology of Indiana, LLC Delaware Valley Urology, LLC UroSearch–Dr Cunningham Jeffersonville Bala Cynwyd St Louis Ocala San Bernardino Peoria Englewood Garden City Norfolk Spokane Middlebury Tulsa Middleburg Heights Pittsburgh Aventura Seattle Hagerstown Shreveport Atlanta Knoxville San Antonio Fort Myers Rockville Orlando Pinellas Park Salt Lake City Grand Rapids Troy Brighton Daytona Beach Roswell Hamilton Huntsville Cincinnati Greenbelt Allentown Boston State College Germantown Trumbull Myrtle Beach Lancaster Albuquerque Little Rock Providence Ocala New York Charlotte Mobile Torrance Ocala Savannah Tacoma Greenwood Marlton Ocala IN PA MO FL CA IL CO NY VA WA CT OK OH PA FL WA MD LA GA TN TX FL MD FL FL UT MI MI MA FL GA NJ AL OH MD PA MA PA TN CT SC PA NM AR RI FL NY NC AL CA FL GA WA IN NJ FL (continued on following page) 8 © 2013 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. Prostate Cancer Detection Among Men With HGPIN Table A1. Investigators and Investigation Sites (continued) PI Last Name PI First Name Trochelman Chopp Tutrone, Jr. Bennett Lev Freedman Israeli Kane Naslund Sharkey Goldberg Burzon Ramos Mehlhaff Costa Roper Simon Bilhartz Barnswell D’Esposito Alabaster Scott Cohen Hopkins Lacy Malkowicz Krejci Pomeroy Nelson Morgan Rawl Parkhurst Fisher Kim Omarbasha Lovinggood Zachary Asroff Jayson Kaufman Boelter Levine Karsh Spirnak Goldberg Singh Kaminetsky Chao Patterson Biber Bilik Tarantino Grubman Fleshner R. Douglas Richard T. Ronald James K. Ronan Sheldon J. Ron S. Richard Michael Jerrold Kenneth Daniel Carlos E. Bryan A. Frank Ronald P. James David Carlton Robert F. A. Michael John Jeffrey K. Scott Alan Sushil S. Bruce Kent Brandon Roscoe Scott William R. John C. Joseph Hugh A.G. Francis Y. Bashar Perry James Mark Scott W. Maury A. Joel Mark Christopher W. Michael A. Lawrence I. John Patrick Gary Errol O. Jed Roberto Anthony Robert J. A. Joseph Arthur Jerold Neil E. Egerdie Aaron Barkin Buckley Casey Flax Blair Lorne Jack Roger Richard Stan Practice Summa Health System, Cancer Research Office The Urology Team PA Chesapeake Urology Research Associates Midtown Urology St Louis Urological Surgeons Sheldon J. Freedman, MD Staten Island Urological Research, PC Wake Urology Associates PA Maryland Prostate Center Advanced Research Institute Research Across America Coastal Urology Associates Panama City Urological Center, PA Oregon Urology Institute The Urology Institute Urology Enterprises Columbus Urology Research, LLC Urology Associates Metropolitan Urologic Services, PC Urological Surgeons of Long Island Southeast Urology Network Urologic Surgeons, Ltd Triangle Urological Group Salt Lake Research Urology, PC University of Pennsylvania/Division of Urology Anne Arundel Urology, PA Kansas City Urology Care, PA Hope Research Institute, LLC Med Atlantic (dba Virginia Urology) Columbia Urological Associates, PA Parkhurst Research Organization, LLC The Urological Institute of Northeastern New York Urologic Northwest Surgeons, PS Central New York Urology, PC Metropolitan Urological Specialists Urology Consultants (c/o DMI Research) Delaware Valley Urology, LLC Demaur Clinical Research Center Urology Research Options Adult and Pediatric Urology, PLLP Lake Success Urological Associates The Urology Center of Colorado Urology of Northern Ohio Urology Associates, PC Capital Urology University Urology Associates Asheboro Urology Clinic University of Tennessee, Department of Urology Midwest Urology and Radiation Oncology Florida Urology Specialists Connecticut Surgical Group, PC Central Jersey Clinical Research University Health Network–Princess Margaret Hospital Prostate Centre Urology Associates/Urologic Medical Research Urology South Shore Research The Male Health Centre Roger Buckley, MD The Fe/Male Health Centres Stanley Flax Medical Professional Corp City State/Territory Akron Austin Towson Atlanta Chesterfield Las Vegas Staten Island Raleigh Baltimore New Port Richey Dallas Brick Panama City Springfield Monroesville Marietta Columbus Nashville Elmont Garden City Memphis Reno Pittsburgh Salt Lake City Lincoln Philadelphia Annapolis Overland Park Phoenix Richmond Columbia Bethany Albany Tacoma Oneida Florissant Pinellas Park Mt Laurel Pembroke Pines Aurora Sartell Lake Success Denver Elyria Manhasset Columbus New York Asheboro Memphis Independence Sarasota Hartford Edison Toronto OH TX MD GA MO NV NY NC MD FL TX NJ FL OR PA GA OH TN NY NY TN NV PA UT NE PA MD KS AZ VA SC OK NY WA NY MO FL NJ FL CO MN NY CO OH NY OH NY NC TN MO FL CT NJ ON Kitchener Greenfield Park Toronto Willowdale Oakville Toronto ON QC ON ON ON ON (continued on following page) www.jco.org © 2013 by American Society of Clinical Oncology Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved. 9 Taneja et al Table A1. Investigators and Investigation Sites (continued) PI Last Name PI First Name Jansz Khonsari Kinahan Liquornik Love Mathur Patrick Woods Steinhoff Chetner Rendon Siemens Donnelly Eiley Tanguay Perrotte Ken Homa Thomas J. Morrie S. William R. Arun Allan Edward Gary Michael P. Richardo A. D. Robert Bryan David Simon Paul Maillette Izawa Damia Damia Becher Balbiani Kobelinsky Rossi Alain Johnathan Omar Oscar Edgardo Luis R. Marcelo Daniel Practice G. Kenneth Jansz Medicine Professional Corp Male/Female Health and Research Centre Southern Interior Medical Research Mor Urology Urology Resource Centre Urotec Allan B. Patrick, MD, Professional Corporation The Health Institute for Men Dr G. Steinhoff Clinical Research Alberta Urology Institute Research Centre Queen Elizabeth Health Sciences Centre Centre for Advanced Urological Research Prostate Cancer Institute Ultra-Med McGill Urology Associates Les Urologues Associés du Centre Hospitalier de l’Université de Montréal Groupe de Recherche en Urologie de la Mauricie London Health Sciences Centre Hospital Pirovano Hospital Italiano de Buenos Aires Centro Urologico Buenos Aires Sanatorio Municipal Policlinico Bancario de Buenos Aires SEDU (Servicio de Urología) City State/Territory Burlington Barrie Kelowna Newmarket Burlington Oshawa Fredericton Toronto Victoria Edmonton Halifax Kingston Calgary Pointe-Claire Montreal Montreal ON ON BC ON ON ON NB ON BC AB NS ON AB QC QC QC Trois-Rivières London QC ON Abbreviations: AB, Alberta; BC, British Columbia; NS, Nova Scotia; ON, Ontario; PI, primary investigator; QC, Quebec. 10 © 2013 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY Downloaded from jco.ascopubs.org on June 15, 2014. For personal use only. No other uses without permission. Copyright © 2013 American Society of Clinical Oncology. All rights reserved.
© Copyright 2025