Oxidative stress in aldosteronism Yao Sun , Robert A. Ahokas
Cardiovascular Research 71 (2006) 300 – 309 www.elsevier.com/locate/cardiores Review Oxidative stress in aldosteronism Yao Sun a, Robert A. Ahokas d, Syamal K. Bhattacharya e, Ivan C. Gerling b, Laura D. Carbone c, Karl T. Weber a,* a b Division of Cardiovascular Diseases, Department of Medicine, University of Tennessee Health Science Center, 920 Madison Ave., Suite 300, Memphis, TN 38163, USA Division of Endocrinology, Department of Medicine, University of Tennessee Health Science Center and Veterans Administration Medical Center, Memphis, TN, USA c Division of Connective Tissue Diseases, Department of Medicine, University of Tennessee Health Science Center and Veterans Administration Medical Center, Memphis, TN, USA d Department of Obstetrics and Gynecology, University of Tennessee Health Science Center, Memphis, TN, USA e Department of Surgery, University of Tennessee Health Science Center, Memphis, TN, USA Received 5 December 2005; received in revised form 20 February 2006; accepted 6 March 2006 Available online 13 March 2006 Time for primary review 22 days Congestive heart failure (CHF) is more than a failing heart and salt-avid state. Also present is a systemic illness which features oxidative stress in diverse tissues, a proinflammatory phenotype, and a wasting of soft tissue and bone. Reactive oxygen and nitrogen species contribute to this illness and the progressive nature of CHF. Aldosteronism, an integral component of the neurohormonal profile found in CHF, plays a permissive role in leading to an altered redox state. Because of augmented urinary and fecal excretion of Ca2+ and Mg2+ and consequent decline in plasma-ionized [Ca2+]o and [Mg2+]o that accompanies aldosteronism, parathyroid glands release parathyroid hormone (PTH) in an attempt to restore Ca2+ and Mg2+ homeostasis; this includes bone resorption. However, PTH-mediated intracellular Ca2+ overloading, considered a Ca2+ paradox, leads to oxidative stress. This can be prevented by: spironolactone, an aldosterone receptor antagonist that rescues urinary and fecal cation losses; parathyroidectomy; amlodipine, a Ca2+ channel blocker; N-acetylcysteine, an antioxidant. In addition to the role played by aldosteronism in the appearance of secondary hyperparathyroidism is the chronic use of a loop diuretic, which further enhances urinary Ca2+ and Mg2+ excretion, and reduced Ca2+ stores associated with hypovitaminosis D. This broader perspective of CHF and the ever increasing clinical relevance of divalent cations and oxidative stress raise the question of their potential management with macro- and micronutrients. An emerging body of evidence suggests the nutritional management of CHF offers an approach that will be complementary to today’s pharmaceutical-based strategies. D 2006 European Society of Cardiology. Published by Elsevier B.V. All rights reserved. Keywords: Aldosterone; Oxidative stress; Parathyroid hormone; Calcium; Magnesium 1. Introduction The past decade has witnessed an ever-emerging body of evidence that implicates oxidative and nitrosative stress in the pathophysiologic expressions of the clinical syndrome congestive heart failure (CHF). CHF has its origins rooted in * Corresponding author. Tel.: +1 901 448 5750; fax: +1 901 448 8084. E-mail address: KTWeber@utmem.edu (K.T. Weber). a salt-avid state mediated largely by circulating hormones of the renin – angiotensin –aldosterone system (RAAS), which appear in response to reduced renal perfusion [1 –4]. The interplay between RAAS effector hormones and oxidative stress and the pathophysiologic importance of reactive oxygen (ROS) and nitrogen species in CHF can be viewed from several vantage points. From a cardiovascular perspective, H2O2 in low concentrations contributes to the signal transduction involved in the regulation of vasomotor reactivity [5], but which in greater abundance can lead to 0008-6363/$ - see front matter D 2006 European Society of Cardiology. Published by Elsevier B.V. All rights reserved. doi:10.1016/j.cardiores.2006.03.007 Downloaded from by guest on October 28, 2014 Abstract Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 2. Oxidative stress in aldosteronism: experimental studies 2.1. Animal model A widely used experimental model of aldosteronism consists of uninephrectomized rats receiving a continuous infusion of ALDO (0.75 Ag/h) by implanted minipump together with 1% NaCl/0.4% KCl in drinking water (ALDOST). This regimen suppresses plasma renin activity and angiotensin II while raising plasma ALDO levels to those seen in human CHF and which are inappropriate for increased or normal dietary Na+. This model of aldosteronism is analogous to the administration of another mineralocorticoid, deoxycorticosterone acetate, with 1% dietary NaCl (DOCAST), except that plasma renin, AngII, and ALDO are each suppressed. Oxidative stress is present at a systemic level throughout weeks 1 – 6 ALDOST as evidenced by a reduction in plasma a1-antiproteinase activity, an inverse correlate of global oxidative stress [13,14]. 2.2. The proinflammatory/fibrogenic vascular phenotype As recently reviewed [8], inflammatory cells invade the perivascular space of intramural coronary arteries at > 3weeks of ALDOST and then involve myofibroblasts expressing types I and III fibrillar collagens, eventuating in a perivascular/interstitial fibrosis [21,30]. Similar lesions are also found in the mesentery and intramural vasculature of the kidneys in rats receiving either ALDOST or DOCAST [31,32]. Such vascular remodeling in the heart involves both the normotensive right and left atria, right ventricle, and pulmonary artery as well as the hypertensive left ventricle and aorta. Their appearance is not related to: hemodynamic factors; the hypertrophic growth of cardiomyocytes; ALDO itself (in the setting of dietary Na+ deprivation); or 1% NaCl alone. An 8% Na+ diet suppresses renin and ALDO; it too leads to hypercalciuria and ultimately a fall in plasmaionized Ca2+ with SHPT and the appearance of these vascular lesions in normo- and hypertensive rats [33,34]. These findings further implicate the permissive role played by ALDO (for any given level of dietary Na+) in the setting of SHPT. The invasion of the coronary and systemic vasculatures by inflammatory cells occurs in the absence of prior organ injury, thereby making it unlikely that there is a circulating self-antigen and antibody response to it that accounts for this vascular remodeling. Instead, an autoactive immune system is suggested and referred to as an immunostimulatory state (vide infra). 2.3. The presence of oxi/nitrosative stress Various lines of evidence, demonstrated by several independent laboratories, have identified the presence of oxidative and nitrosative stress in rats receiving ALDOST. In either case, elevated plasma ALDO is inappropriate for dietary Na+. Schiffrin and coworkers found an increase in thiobarbituric acid-reactive substances (TBARs) and 8-isoprostanes in blood, direct indices of oxidative stress, while increased NADPH-oxidase generation of superoxide by vascular tissue is evidenced by lucigenin chemiluminescence [35 –37]. By gene chip array technology, the transcriptome Downloaded from by guest on October 28, 2014 dysfunction of the endothelium [6] and overwhelm antioxidant defenses to prove cytotoxic, adversely influencing cardiomyocyte survival in the failing heart [5,7]. A broader perspective yields the realization that it is the presence of an altered redox state at a systemic level that is involved in the wasting of diverse tissues and which contributes to the progressive nature of CHF [8 –12]. Essentially, a systemic illness accompanies CHF. It has several prominent features: a) the presence of oxidative stress in such tissues as skin, skeletal muscle, heart, peripheral blood mononuclear cells (PBMC; lymphocytes and monocytes), and blood [9 –11,13,14]; b) an immunostimulatory state with activated circulating lymphocytes and monocytes and whose transcriptome reveals an upregulated expression of antioxidant defenses and proinflammatory genes together with downregulated counter-regulatory or anti-inflammatory defenses [14 –20]; c) a proinflammatory vascular phenotype, where CD4+ lymphocytes and ED1+ monocytes/macrophages invade the intramural arterial circulation of systemic organs and the right and left heart [21]; and d) a catabolic state with loss of lean tissue, fat, and bone [22 – 25]. Mechanisms involved in the pathogenesis of this systemic illness and its pathophysiologic expressions, including the role of oxidative stress and RAAS effector hormones, are under active investigation at both the bench and bedside. Secondary aldosteronism is an integral component of the neurohormonal profile found in patients with CHF [1–4]. Fiebeler and Luft [26] have suggested that aldosterone– mineralocorticoid receptor (MR) binding has a direct effect on PBMC and vascular smooth muscle cells, where it favors the induction of oxidative stress with ROS regulating MR behavior. Funder [27] argues ROS generation serves to activate cortisol–MR complexes in vascular smooth muscle and cardiomyocytes that normally are tonically inhibited by cortisol. Under these conditions, it is suggested, glucocorticoids transduce a mineralocorticoid-like excess state. Touyz and Schiffrin [28] and Li and coworkers [29] implicate endothelin (ET)-1-induced oxidative stress, via an NADPH oxidase pathway, with chronic mineralocorticoid excess (relative to normal or increased dietary Na+). We have suggested aldosterone (ALDO) and dietary Na+ play a permissive role while parathyroid hormone (PTH)-mediated intracellular Ca2+ overloading that accompanies secondary hyperparathyroidism (SHPT) is integral to the appearance of oxidative stress [8]. Macro- and micronutrient supplements may hold the therapeutic potential to regulate these responses. 301 302 Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 2.4. The role of secondary hyperparathyroidism and intracellular Ca2+ overloading Iterations in intracellular Ca2+ and Mg2+ concentrations are found in circulating lymphocytes and platelets in aldosteronism and contribute to the pathophysiologic basis for the appearance of oxidative stress [13,14,43– 46]. In PBMC harvested weekly from rats with ALDOST, an early and persistent increase in total intracellular Ca2+ (see Fig. 1, left panel) and a rise in cytosolic-free [Ca2+]i at week 2 and beyond are found (Fig. 1, right panel) which is prevented by parathyroidectomy (Fig. 1, right panel) or amlodipine; an associated fall in [Mg2+]i is attenuated by a Mg2+supplemented diet [13,14,47,48]. The excessive intracellular Ca2+ accumulation is also found in myocardium and skeletal muscle and is prevented by parathyroidectomy (see Fig. 2) [48]. In keeping with Ca2+ overloading is a loss of mitochondrial potential with apoptosis of cardiac and skeletal muscle myocytes [12,49]. An increase in PBMC production of H2O2 is prevented by cotreatment with either amlodipine or N-acetylcysteine [13]. Thus in PBMC, organelles such as mitochondria and endoplasmic reticulum are first saturated by Ca2+, followed by a rise in their cytosolic-free concentrations. Others have reported increased intracellular [Ca2+]i in many different cell types in response to SHPT [50]. The Ca2+ overloading of diverse cells is accompanied by systemic evidence of oxidative stress. There is an increased rate of production of H2O2 by PBMC and upregulation of their relevant antioxidant defense genes [14]. The importance of intracellular Ca2+ overloading to the induction of oxidative stress is further supported by the protective effects of parathyroidectomy or a Ca2+ channel blocker [13,48]. Based on metabolic studies conducted in patients with primary aldosteronism [51 – 56], 24 h urinary and fecal excretion of these divalent cations was monitored in rats receiving ALDOST for 1 – 6weeks [47,48,57]. A fourfold increase ranging in microgram quantities of Ca2+ and Mg2+ excreted in urine at week 1 ALDOST was seen and which was persistent thereafter. The stimulus to hypercalciuria and hypermagnesuria that accompanies ALDOST is not well understood. However, the probable mechanism is thought to be related to an expansion of the extravascular space, resulting in decreased proximal tubular resorption, thereby increasing distal delivery of Na+, Mg2+ and Ca2+ with the mineralocorticoid promoting distal tubular Na+ resorption Fig. 1. Total intracellular Ca2+ (left panel) and cytosolic-free [Ca2+]i (right panel) in peripheral blood mononuclear cells (PBMC) in controls (C) and with weeks of aldosterone/salt treatment (ALDOST) without (hatched bar) or with (dark bar) prior parathyroidectomy. Broken and dotted lines (right panel) connote mean T S.E.M. for controls. Left panel adapted from Chhokar VS, et al. Circulation 2005; 111: 871 – 878; right panel reproduced from Vidal A, et al. Am J Physiol Heart Circ Physiol 2006; 290: H286 – H294, with permission. Downloaded from by guest on October 28, 2014 of circulating lymphocytes and monocytes (PBMC) revealed a heightened mRNA expression of antioxidant defenses, such as glutathione peroxidase (GSH-Px) and Mn-superoxide dismutase (SOD), while H2O2 production by these PBMC is increased [13 – 15]. Inflammatory cells that invade the vasculature reveal immunohistochemical evidence of gp91phox activation, a subunit of NADPH oxidase; the presence of 3-nitrotyrosine, a stable product of short-lived peroxynitrite, derived from the reaction of nitric oxide with superoxide; and the activation of a redox-sensitive nuclear transcription factor (NF)-nB [21]. Furthermore, in situ hybridization revealed an increased mRNA expression of a proinflammatory gene cascade in these invading cells and which is regulated by NFnB. This includes intercellular adhesion molecule (ICAM)-1, vascular cell adhesion molecule (VCAM)-1, monocyte chemoattractant protein (MCP)-1 and tumor necrosis factor (TNF)-a [21,35,36,38]. Further evidence in support of a role played by oxidative stress in the vascular remodeling found in aldosteronism are vasculoprotective responses to: antioxidants, pyrrolidine dithiocarbamate and N-acetylcysteine [21]; tempol, a superoxide dismutase mimetic [37]; and apocynin, an NADPH oxidase inhibitor [39,40]. When spironolactone (Spiro), an ALDO receptor antagonist, is coadministered with ALDOST these lesions are not seen [21,41]. Cotreatment with a Ca2+ channel blocker is also vasculoprotective [13,42]. Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 303 Fig. 2. Total Ca2+ content in myocardium and skeletal muscle in controls, and during 4 – 6 weeks of ALDOST without or with prior parathyroidectomy and a Ca2+-supplemented diet (Ca2+ PTx). Reproduced from Vidal A, et al. Am J Physiol Heart Circ Physiol 2006; 290: H286 – H294, with permission. promoting the loss of thiamine, a micronutrient [67]. Hydrochlorothiazide promotes Ca2+ reabsorption without altering hypermagnesuria [68]. Spiro co-treatment rescues Ca2+ and Mg2+ losses associated with furosemide use and the hypermagnesuria seen with hydrochlorothiazide, thus preserving bone mineral density under either scenario [67,68]. 2.5. Macro- and micronutrients in preventing SHPT and oxidative stress Reduced levels of extracellular Ca2+ and Mg2+, reflected by their fallen ionized levels in the presence of accentuated urinary and fecal excretion of these cations, accompany aldosteronism that account for elevations in plasma PTH and PTH-mediated intracellular Ca2+ overloading and global oxidative stress. The efficacy of dietary supplements of these macronutrients in preventing such responses is called into question. In rats with DOCAST, co-treatment with dietary Mg2+ supplements attenuated elevations in cytosolic-free Ca2+ that appear in lymphocytes and platelets, and prevented increased H2O2 production by PBMC and ET-1 overproduction by the heart and vasculature [13,45,69,70]. A regimen of calcitriol and dietary Ca2+ and Mg2+ supplements prevented the fall in plasma-ionized [Ca2+]o and rise in plasma PTH, which, in turn, prevented Ca2+ loading of PBMC and rise in PBMC H2O2 production [71]. Micronutrients include such trace minerals as Zn and Se. Zn and Se are each integral to the activity of endogenous antioxidant defenses, including Cu/Zn-SOD and Se-GSHPx. Diets deficient in Zn or Se are accompanied by a reduction in the activities of these oxireductases, which can be restored with dietary replacements [72,73]. Hypozincemia has been found in rats with ALDOST and who were receiving standard laboratory chow that satisfies minimal daily requirements of this mineral together with an associated fall in the Cu/Zn-SOD activity of PBMC [74]. Hyposelenemia is also found in these rats and its impact on Se-GSH-Px is under investigation. The origins of hypo- Downloaded from by guest on October 28, 2014 without influencing increased Mg2+ and Ca2+ excretion [53,58 –61]. A similar response was also found in feces; however, here milligram quantities of Ca2+ and Mg2+ were lost through this route. Spiro cotreatment attenuated the loss of these divalent cations at each site [47]. The early and persistent excretion of Ca2+ and Mg2+ led to a fall in their plasma-ionized concentrations throughout weeks 1 – 6 ALDOST. Fig. 3 depicts this sequence of events. The decline in plasma [Ca2+]o and [Mg2+]o are each major stimuli to the parathyroid glands’ secretion of PTH. Plasma PTH levels increased at week 1 and remained so over ensuing weeks with continued ALDOST [47]. In keeping with elevated PTH, bone resorption ensued to restore extracellular Ca2+ and Mg2+ homeostasis. Bone mineral density of tibia and femur, as evidenced by dual-energy Xray absorptiometry (DXA), reduced by 10% at week 4 and 50% by week 6 of ALDOST; a corresponding reduction in Ca2+ and Mg2+ concentrations of these bones was found by atomic absorption spectroscopy [47,57]. The fall in mineral density was accompanied by a decline in bone strength as evidenced by a reduced resistance to flexor stress [47]. The decline in bone mineral density provided biologic evidence of a persistent state of SHPT. Whether given orally or intravenously, Na+ loading leads to increased urinary Ca2+ excretion and this holds true for normotensive young adults, hypertensive elderly patients, and salt-sensitive, hypertensive African-Americans [62 – 64]. Chronic Na-related hypercalciuria, especially when the diet is deficient in Ca2+, leads to increased serum PTH with increased Ca2+ and reduced Mg2+ concentrations in various cell types [64,65]. PTH-mediated renal formation of 1,25(OH)2D provides for a compensatory increment in gastrointestinal Ca2+ absorption, which is not seen in patients with hypoparathyroidism following PTx [62,66]. In chronic aldosteronism, Ca2+ losses from gut dominate over such compensatory resorption, but can be attenuated by Spiro [47]. Diuretics modify urinary Ca2+ and Mg2+ excretion in aldosteronism. Spiro attenuates such losses while furosemide, a loop diuretic, augments these events, as well as 304 Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 elevated circulating PTH that mediates an excessive accumulation of intracellular Ca2+ in diverse cells. SHPT accompanies aldosteronism because of the urinary and fecal losses of Ca2+ and Mg2+ and consequent decline in their plasma-ionized concentrations. Spiro prevents SHPT and rescues bone mineral density by attenuating these losses and fall in plasma-ionized [Ca2+]o and [Mg2+]o. Reactive oxygen species, as evidenced by the heightened PBMC production of H2O2, function as intracellular messengers to activate downstream signaling molecules that either up- or downregulate genes of the PBMC transcriptome and which account for their proinflammatory phenotype. These autoactivated circulating immune cells likely contribute to the systemic illness that accompanies PTH-mediated Ca2+ overloading of diverse cells and the proinflammatory vascular phenotype. SHPT represents an obligatory covariant responsible for the generalized wasting that accompanies the secondary aldosteronism of CHF, including bone resorption and the apoptosis of cardiac and skeletal muscle myocytes. 3.1. The CHF syndrome Fig. 3. A paradigm depicting the appearance of secondary hyperparathyroidism (SHPT) in rats receiving aldosterone (ALDO) and 1% NaCl in drinking water. Elevations in circulating parathyroid hormone (PTH) promote an excessive accumulation of intracellular Ca2+ and induction of oxidative stress in PBMC via NADPH oxidase with generation of superoxide, peroxynitrite (OONO ) and H2O2, which overwhelm antioxidant defenses such as superoxide dismutase (SOD). H2O2 participates in signal transduction, activation of a redox-sensitive nuclear transcription factor (NF)-nB, transcription and cell activation leading to an immunostimulatory state. Various interventions which interrupt this sequence of events at different stages of progression are shown by a horizontal wavy line. Spiro, spironolactone; PTx, parathyroidectomy; CCB, Ca2+ channel blocker; apocynin, an NADPH oxidase inhibitor; tempol, an SOD mimetic; and antioxidants, N-acetylcysteine (NAC) and pyrrolidine dithiocarbamate (PDTC). zincemia and hyposelenemia in rats with aldosteronism remain to be thoroughly explored as does the protective impact of dietary supplements. A dietary flavonoid, quercetin, prevents increased TBARS in plasma and heart while raising total glutathione levels in liver and heart and GSH-Px activities at these sites in rats with DOCAST [75]. Furthermore, sesamin, a lignin derived from sesame oil, inhibits increased superoxide production by the aorta in rats receiving DOCAST [76]. 2.5.1. Summary Thus, in rats with aldosteronism, the presence of oxidative stress at a systemic level is in keeping with Characteristic signs and symptoms comprise the CHF syndrome, where expanded intra- and extravascular volumes are rooted in a salt-avid state mediated, in part, by secondary aldosteronism [4]. Serum ALDO levels are increased in patients who are decompensated with salt and water retention (NYHA Class III and IV heart failure), which is not the case for those asymptomatic patients with compensated (NYHA Class I and II) heart failure unless potent loop diuretics usage reduces intravascular volume and renal perfusion to activate the circulating RAAS [1 –3]. 3.2. Proinflammatory CHF phenotype Elevations in circulating IL-6 and TNF-a accompany the proinflammatory CHF phenotype [22,23,77,78]. The extent to which cytokines and chemokines (e.g., MCP-1) are elevated relates to the severity of heart failure, but not its etiologic origins. This suggests neurohormonal activation is likely contributory to the phenotype, not the cardiomyopathic process itself. The source of circulating cytokines in CHF remains uncertain. Candidate cellular sources include activated lymphocytes and monocytes, as well as osteoblasts under the influence of PTH to promote osteoclastogenesis [19,20,79,80]. Circulating lymphocytes and monocytes, harvested from patients with CHF and studied ex vivo, demonstrated increased chemokine production in response to provocation with lipopolysaccharide and which was greater than that seen with cells obtained from healthy volunteers [17,18]. Serum from patients with CHF raises superoxide generation Downloaded from by guest on October 28, 2014 3. Secondary aldosteronism in CHF: clinical studies Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 by cultured monocytes obtained from healthy blood donors and which may relate to increased serum MCP-1 levels that could be blocked by neutralizing antibody to this chemokine. A role for PTH in mediating these responses has not been examined. An upregulated PBMC transcriptome has been found in CHF with increased expression of cytokines and chemokines and their receptors [17,18]. 3.3. Oxidative stress in CHF During June 1 – August 31, 2005, we addressed the presence of SHPT and hypovitaminosis D in 25 AA: 20 who were hospitalized because of their CHF; and 5 who were ambulatory and asymptomatic with compensated heart failure with comparable reductions in ejection fraction < 35% [93]. Patients were stratified, on historical grounds, as protracted CHF ( 4weeks) in 11 and short-term CHF (1 –2 weeks) in 9. All had been treated with an ACE inhibitor or AT1 receptor antagonist, furosemide and in many cases low-dose spironolactone. Serum PTH (mean T S.E.M.; range) was elevated in all those with protracted CHF (127 T 13; 82– 243 pg/mL) and in 3 of 9 with shortterm CHF (59 T 8; 18 – 99pg/mL); none of the compensated patients had SHPT (42 T 5, 17 –53 pg/mL). Ionized hypocalcemia and hypomagnesemia was present in both groups with CHF. We found hypovitaminosis D (< 30 ng/mL) in: all 11 with protracted CHF; 8 of 9 with short-term CHF; and 4 of 5 with compensated failure. Melanin is a natural sunscreen. Thus, hypovitaminosis D is prevalent in AA even during summer months and especially when housebound with symptomatic heart failure. The aldosteronism of protracted CHF and chronic furosemide usage each exaggerate Ca2+ and Mg2+ losses to compromise cation balance to lead to ionized hypocalcemia and hypomagnesemia with SHPT in AA, where hypovitaminosis D has already compromised Ca2+ balance. Reduced serum 25(OH)D has been previously reported in some Caucasian patients with CHF followed during winter months in Germany [91]. A role for restoring 25(OH)D levels to >30 ng/mL in preventing SHPT and oxidative stress in the overall management of CHF remains to be addressed. 3.4. Secondary hyperparathyroidism in CHF 3.5. Secondary hyperparathyroidism and the failing heart Elevations in serum PTH have been found in 18 –40% of predominantly Caucasian patients awaiting cardiac transplantation in the United States and western Europe [24,25,88 –91]. In addition to aldosteronism in mediating urinary and fecal Ca2+ and Mg2+ excretion is the contribution of furosemide, a potent loop diuretic that further accentuates urinary Ca2+ and Mg2+ excretion. Many of these patients with advanced CHF were found to have osteopenia and osteoporosis likely due to SHPT [24,25]. In 9 patients (8 African-Americans, AA), consecutively admitted to the Regional Medical Center Hospital in Memphis this past winter (February, 2005) because of their CHF with systolic dysfunction (ejection fraction <35%), we found elevated serum PTH (mean T S.E.M.; range; normal 12 –65 pg/mL) was documented. This included 5 who were medically untreated (204 T 60; 86– 393pg/mL) and 4 with treated CHF (134 T 14; 105 – 164 pg/mL) that included furosemide [92]. However, abnormalities in albumin-corrected serum Ca2+, serum Mg2+ or phosphorus were not present. Calculated creatinine clearance in untreated and treated patients with CHF was 74 T 15 and 83 T 21mL/min, respectively, and did not differ between them. In this preliminary study, 25(OH)D was not monitored. As noted earlier, a proinflammatory vascular phenotype accompanies the SHPT of aldosteronism. This includes a perivascular/interstitial fibrosis of the right and left ventricle which will adversely influence myocardial stiffness [94]. PTx attenuates the appearance of such reactive fibrosis [48,95]. Microscopic scars, a reparative fibrosis replacing cardiomyocytes lost to necrosis, are also seen in the right and left heart in aldosteronism [94]. The pathogenic origin of cardiomyocytic necrosis is uncertain, but could relate to excessive intracellular Ca2+ overloading and oxidative stress. In addition to an adverse structural remodeling of myocardium found in SHPT are direct effects of PTH on cardiomyocyte metabolism and function [96,97]. These include (see Fig. 4) impaired mitochondrial phosphorylation and reduced ATP synthesis, which accompany Ca2+ overloading and reduced Ca2+ efflux as a result of impaired Ca2+-ATPase activity [96]. An inverse correlation exists between PTH and ejection fraction in end-stage renal failure [98]. Correction of SHPT by PTx or calcitriol treatment is associated with improved systolic function [99,100]. Diastolic dysfunction found in primary HPT is improved by PTx [101]. Finally, PTH-mediated bone resorption involves Downloaded from by guest on October 28, 2014 Oxidative stress has been found to be an integral feature of the illness that accompanies CHF and which involves diverse tissues. The presence of oxidative stress therefore appears at a systemic level, irrespective of the etiologic origins of CHF, and which correlate with its clinical severity [81 – 83]. Furthermore, evidence of reduced antioxidant defenses has also been reported [84 – 86]. Such endogenous defenses, provided by Cu/Zn-SOD and Se-GSH-Px, respectively, scavenge superoxide and H2O2, and are upregulated in stressed tissues [22]. These endogenous defenses, however, may be overwhelmed in CHF, thus creating an antioxidant deficit [23]. In addition, the activity of these oxireductases is dependent on Zn and Se, respectively, which may be reduced if the bioavailability of these trace minerals is compromised [24,25]. Consequences of oxidative stress in CHF are thought to be concentration-dependent and include: signal transduction and cell signaling in low concentration [87]; and programmed cell death with activation of apoptotic pathways and ultimately necrotic pathways [5,7]. 305 306 Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 setting of reduced extracellular Ca2+, a Ca2+ paradox, has the potential to lead to the appearance of oxidative stress. SHPT is an important covariant involved in the systemic illness that accompanies CHF. 4. Conclusions and future directions Fig. 4. Several factors can contribute to the appearance of secondary hyperparathyroidism (SHPT) in human CHF. These include: hypovitaminosis D; aldosteronism; and chronic use of furosemide, a loop diuretic. PTH has direct and indirect effects that compromise ventricular function. These respectively include: Ca2+ overload, decreased energy stores, and mitochondrial phosphorylation; and increased cytokine production by osteoblasts with increased circulating IL-6 and TNF-a having a negative impact on cardiomyocyte contractility. 3.6. Macro- and micronutrients in CHF In recognizing the importance of oxidative stress and its potential role in the progressive nature of heart failure, attention has been drawn to macro- and micronutrients as contributors and combatants. Deficits of extracellular Ca2+ and Mg2+ and hypovitaminosis D, accompanied by SHPT with intracellular Ca2+ overloading, are associated with the induction of oxidative stress. Deficiencies of zinc and selenium, related to inadequate dietary sources or promoted by their urinary losses that accompany ACE inhibitors or AT1 receptor blockers, reduce the activities of Cu/Zn-SOD and Se-GSH-Px which serve as antioxidant defenses, thus augmenting the susceptibility and severity of oxidative stress. The contribution of micronutrients to the pathophysiology of heart failure and its management is beginning to receive much deserved attention [91,106 – 110]. 3.6.1. Summary SHPT accompanies the aldosteronism of CHF. Elevations in circulating PTH occur in response to falling plasmaionized [Ca2+]o and [Mg2+]o that result from aldosterone/ Na+-mediated urinary and fecal excretion of these cations. Chronic furosemide treatment is also contributory as is the case for reduced sunlight exposure with hypovitaminosis D. SHPT with intracellular Ca2+ overloading of cells in the Acknowledgements We acknowledge the invaluable contribution of Richard A. Parkinson, MEd, Assistant Director for Scholastic Services, in presenting these materials. This work was supported, in part, by NIH/NHLBI grant R01-HL73043. References [1] Swedberg K, Eneroth P, Kjekshus J, Wilhelmsen L. Hormones regulating cardiovascular function in patients with severe congestive Downloaded from by guest on October 28, 2014 osteoblast formation of IL-6 and TNF-a to induce osteoclastogenesis [102]. These cytokines are known to inhibit mitochondrial energy production and impair cardiomyocyte contractility [103 –105]. Elevations in circulating IL-6 and TNF-a found in CHF [23] may represent surrogate biomarkers of SHPT. The CHF syndrome is more than a failing heart and a state of salt and water retention. A broader perspective takes into account the importance of neurohormonal activation and its contribution to an accompanying systemic illness that features oxidative stress, a proinflammatory phenotype, and tissue wasting. The road to wasting in CHF is paved with lost minerals. The accompanying decline in extracellular Ca2+ and Mg2+ and consequent elaboration of PTH seeks to restore homeostasis of these cations. SHPT is a covariant of CHF; it has far-reaching consequences involving diverse tissues and which is mediated by intracellular Ca2+ overloading. Not unlike patients with chronic renal failure, where issues related to the prevention and management of SHPT are integral to optimal management, today’s treatment of patients with CHF must also take into account Ca2+ and Mg2+ balance. This includes: the urinary and fecal loss of these cations that occurs in response to aldosteronism, which can be attenuated by an aldosterone receptor antagonist; medications which further threaten their balance (e.g., loop diuretics); adequate dietary intake; the presence of hypovitaminosis D that occurs as a result of a housebound lifestyle, especially in AA who require more sunlight to maintain their 25(OH)D stores; and skeletal health, particularly amongst the elderly, where SHPT may threaten already reduced bone mineral density. The importance of oxidative stress in CHF calls into question the capacity of antioxidant defenses, such as Cu/ZnSOD and Se-GSH-Px. Zn and Se balance in patients with CHF needs to be addressed more comprehensively, including the potential efficacy of dietary supplements with these micronutrients. In coming years, the nutritional management of CHF, including macro- and micronutrients, will undoubtedly receive greater and well-deserved attention. Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 [2] [3] [4] [5] [6] [7] [8] [9] [10] [12] [13] [14] [15] [16] [17] [18] [19] [20] [21] Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT. Aldosteroneinduced inflammation in the rat heart. Role of oxidative stress. Am J Pathol 2002;161:1773 – 81. [22] Anker SD, Chua TP, Ponikowski P, Harrington D, Swan JW, Kox WJ, et al. Hormonal changes and catabolic/anabolic imbalance in chronic heart failure and their importance for cardiac cachexia. Circulation 1997;96:526 – 34. [23] Anker SD, Clark AL, Teixeira MM, Hellewell PG, Coats AJ. Loss of bone mineral in patients with cachexia due to chronic heart failure. Am J Cardiol 1999;83:612 – 5. [24] Lee AH, Mull RL, Keenan GF, Callegari PE, Dalinka MK, Eisen HJ, et al. Osteoporosis and bone morbidity in cardiac transplant recipients. Am J Med 1994;96:35 – 41. [25] Shane E, Mancini D, Aaronson K, Silverberg SJ, Seibel MJ, Addesso V, et al. Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am J Med 1997; 103:197 – 207. [26] Fiebeler A, Luft FC. The mineralocorticoid receptor and oxidative stress. Heart Fail Rev 2005;10:47 – 52. [27] Funder JW. RALES, EPHESUS and redox. J Steroid Biochem Mol Biol 2005;93:121 – 5. [28] Touyz RM, Schiffrin EL. Reactive oxygen species in vascular biology: implications in hypertension. Histochem Cell Biol 2004;122:339 – 52. [29] Li L, Fink GD, Watts SW, Northcott CA, Galligan JJ, Pagano PJ, et al. Endothelin-1 increases vascular superoxide via endothelinA – NADPH oxidase pathway in low-renin hypertension. Circulation 2003;107:1053 – 8. [30] Sun Y, Ratajska A, Zhou G, Weber KT. Angiotensin converting enzyme and myocardial fibrosis in the rat receiving angiotensin II or aldosterone. J Lab Clin Med 1993;122:395 – 403. [31] Sun Y, Zhang J, Zhang JQ, Ramires FJA. Local angiotensin II and transforming growth factor-h1 in renal fibrosis of rats. Hypertension 2000;35:1078 – 84. [32] Schiffrin EL, Larivie´re R, Li JS, Sventek P, Touyz RM. Deoxycorticosterone acetate plus salt induces overexpression of vascular endothelin-1 and severe vascular hypertrophy in spontaneously hypertensive rats. Hypertension 1995;25(Part 2):769 – 73. [33] Yu HC, Burrell LM, Black MJ, Wu LL, Dilley RJ, Cooper ME, et al. Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation 1998;98:2621 – 8. [34] Takeda Y, Yoneda T, Demura M, Furukawa K, Miyamori I, Mabuchi H. Effects of high sodium intake on cardiovascular aldosterone synthesis in stroke-prone spontaneously hypertensive rats. J Hypertens 2001;19(3 Pt 2):635 – 9. [35] Virdis A, Neves MF, Amiri F, Viel E, Touyz RM, Schiffrin EL. Spironolactone improves angiotensin-induced vascular changes and oxidative stress. Hypertension 2002;40:504 – 10. [36] Pu Q, Neves MF, Virdis A, Touyz RM, Schiffrin EL. Endothelin antagonism on aldosterone-induced oxidative stress and vascular remodeling. Hypertension 2003;42:49 – 55. [37] Iglarz M, Touyz RM, Viel EC, Amiri F, Schiffrin EL. Involvement of oxidative stress in the profibrotic action of aldosterone. Interaction with the renin – angiotensin system. Am J Hypertens 2004;17:597 – 603. [38] Yoshida K, Kim-Mitsuyama S, Wake R, Izumiya Y, Izumi Y, Yukimura T, et al. Excess aldosterone under normal salt diet induces cardiac hypertrophy and infiltration via oxidative stress. Hypertens Res 2005;28:447 – 55. [39] Li L, Chu Y, Fink GD, Engelhardt JF, Heistad DD, Chen AF. Endothelin-1 stimulates arterial VCAM-1 expression via NADPH oxidase-derived superoxide in mineralocorticoid hypertension. Hypertension 2003;42:997 – 1003. [40] Park YM, Park MY, Suh YL, Park JB. NAD(P)H oxidase inhibitor prevents blood pressure elevation and cardiovascular hypertrophy in aldosterone-infused rats. Biochem Biophys Res Commun 2004;313: 812 – 7. Downloaded from by guest on October 28, 2014 [11] heart failure and their relation to mortality. CONSENSUS Trial Study Group. Circulation 1990;82:1730 – 6. Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang C, et al. Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure: a substudy of the Studies of Left Ventricular Dysfunction (SOLVD). Circulation 1990;82:1724 – 9. Rousseau MF, Gurne O, Duprez D, Van Mieghem W, Robert A, Ahn S, et al. Beneficial neurohormonal profile of spironolactone in severe congestive heart failure: results from the RALES neurohormonal substudy. J Am Coll Cardiol 2002;40:1596 – 601. Weber KT. Aldosterone in congestive heart failure. N Engl J Med 2001;345:1689 – 97. Cai H. Hydrogen peroxide regulation of endothelial function: origins, mechanisms, and consequences. Cardiovasc Res 2005;68:26 – 36. Struthers AD. Aldosterone escape during angiotensin-converting enzyme inhibitor therapy in chronic heart failure. J Cardiac Failure 1996;2:47 – 54. Kumar D, Jugdutt BI. Apoptosis and oxidants in the heart. J Lab Clin Med 2003;142:288 – 97. Weber KT. The proinflammatory heart failure phenotype: a case of integrative physiology. Am J Med Sci 2005;330:219 – 26. Cesselli D, Jakoniuk I, Barlucchi L, Beltrami AP, Hintze TH, NadalGinard B, et al. Oxidative stress-mediated cardiac cell death is a major determinant of ventricular dysfunction and failure in dog dilated cardiomyopathy. Circ Res 2001;89:279 – 86. Miyamoto M, Kishimoto C, Shioji K, Lee JD, Shimizu H, Ueda T, et al. Cutaneous arteriolar thioredoxin expression in patients with heart failure. Circ J 2003;67:116 – 8. Tsutsui H, Ide T, Hayashidani S, Suematsu N, Shiomi T, Wen J, et al. Enhanced generation of reactive oxygen species in the limb skeletal muscles from a murine infarct model of heart failure. Circulation 2001;104:134 – 6. Burniston JG, Saini A, Tan LB, Goldspink DF. Aldosterone induces myocyte apoptosis in the heart and skeletal muscles of rats in vivo. J Mol Cell Cardiol 2005;39:395 – 9. Ahokas RA, Sun Y, Bhattacharya SK, Gerling IC, Weber KT. Aldosteronism and a proinflammatory vascular phenotype. Role of Mg2+, Ca2+ and H2O2 in peripheral blood mononuclear cells. Circulation 2005;111:51 – 7. Ahokas RA, Warrington KJ, Gerling IC, Sun Y, Wodi LA, Herring PA, et al. Aldosteronism and peripheral blood mononuclear cell activation. A neuroendocrine-immune interface. Circ Res 2003;93:e124. Gerling IC, Sun Y, Ahokas RA, Wodi LA, Bhattacharya SK, Warrington KJ, et al. Aldosteronism: an immunostimulatory state precedes the proinflammatory/fibrogenic cardiac phenotype. Am J Physiol, Heart Circ Physiol 2003;285:H813 – 21. Aukrust P, Ueland T, Mu¨ller F, Andreassen AK, Nordøy I, Aas H, et al. Elevated circulating levels of C – C chemokines in patients with congestive heart failure. Circulation 1998;97:1136 – 43. Dama˚s JK, Gullestad L, Aass H, Simonsen S, Fjeld JG, Wikeby L, et al. Enhanced gene expression of chemokines and their corresponding receptors in mononuclear blood cells in chronic heart failuremodulatory effect of intravenous immunoglobulin. J Am Coll Cardiol 2001;38:187 – 93. Dama˚s JK, Gullestad L, Ueland T, Solum NO, Simonsen S, Frøland SS, et al. CXC-chemokines, a new group of cytokines in congestive heart failure-possible role of platelets and monocytes. Cardiovasc Res 2000;45:428 – 36. Yndestad A, Dama˚s JK, Eiken HG, Holm T, Haug T, Simonsen S, et al. Increased gene expression of tumor necrosis factor superfamily ligands in peripheral blood mononuclear cells during chronic heart failure. Cardiovasc Res 2002;54:175 – 82. Yndestad A, Holm AM, Mu¨ller F, Simonsen S, Frøland SS, Gullestad L, et al. Enhanced expression of inflammatory cytokines and activation markers in T-cells from patients with chronic heart failure. Cardiovasc Res 2003;60:141 – 6. 307 308 Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 [62] Breslau NA, McGuire JL, Zerwekh JE, Pak CY. The role of dietary sodium on renal excretion and intestinal absorption of calcium and on vitamin D metabolism. J Clin Endocrinol Metab 1982;55:369 – 73. [63] Imaoka M, Morimoto S, Kitano S, Fukuo F, Ogihara T. Calcium metabolism in elderly hypertensive patients: possible participation of exaggerated sodium, calcium and phosphate excretion. Clin Exp Pharmacol Physiol 1991;18:631 – 41. [64] Zemel MB, Kraniak J, Standley PR, Sowers JR. Erythrocyte cation metabolism in salt-sensitive hypertensive blacks as affected by dietary sodium and calcium. Am J Hypertens 1988;1(4 Pt 1): 386 – 92. [65] Haller H, Thiede M, Lenz T, Ludersdorf M, Harwig S, Distler A, et al. Intracellular free calcium and ionized plasma calcium during mineralocorticoid-induced blood pressure increase in man. J Hypertens Suppl 1985;3(Suppl 3):S41 – 3. [66] Zikos D, Langman C, Gafter U, Delahaye B, Lau K. Chronic DOCA treatment increases Ca absorption: role of hypercalciuria and vitamin D. Am J Physiol 1986;251(3 Pt 1):E279 – 84. [67] Law PH, Sun Y, Bhattacharya SK, Chhokar VS, Weber KT. Diuretics and bone loss in rats with aldosteronism. J Am Coll Cardiol 2005;46:142 – 6. [68] Runyan AL, Chhokar VS, Sun Y, Bhattacharya SK, Runyan JW, Weber KT. Bone loss in rats with aldosteronism. Am J Med Sci 2005;330:1 – 7. [69] Suzuki H, Sano H, Fukuzaki H. Decreased cytosolic free calcium concentration in lymphocytes of magnesium-supplemented DOCA – salt hypertensive rats. Clin Exp Hypertens, A 1989;11:487 – 500. [70] Berthon N, Laurant P, Hayoz D, Fellmann D, Brunner HR, Berthelot A. Magnesium supplementation and deoxycorticosterone acetate – salt hypertension: effect on arterial mechanical properties and on activity of endothelin-1. Can J Physiol Pharmacol 2002; 80:553 – 61. [71] Goodwin KD, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT. Preventing oxidative stress in rats with aldosteronism by calcitriol and dietary calcium and magnesium supplements. Am J Med Sci in press. [72] Johnson F, Giulivi C. Superoxide dismutases and their impact upon human health. Mol Aspects Med 2005;26:340 – 52. [73] Thomson CD. Assessment of requirements for selenium and adequacy of selenium status: a review. Eur J Clin Nutr 2004;58: 391 – 402. [74] Thomas M, Vidal A, Bhattacharya SK, Ahokas RA, Johnson PL, Sun Y, et al. Hypozincemia and oxidative stress in rats with chronic aldosteronism. J Investig Med 2006;54(Suppl 1):S264. [75] Galisteo M, Garcia-Saura MF, Jimenez R, Villar IC, Zarzuelo A, Vargas F, et al. Effects of chronic quercetin treatment on antioxidant defence system and oxidative status of deoxycorticosterone acetate – salt-hypertensive rats. Mol Cell Biochem 2004;259:91 – 9. [76] Nakano D, Itoh C, Ishii F, Kawanishi H, Takaoka M, Kiso Y, et al. Effects of sesamin on aortic oxidative stress and endothelial dysfunction in deoxycorticosterone acetate – salt hypertensive rats. Biol Pharm Bull 2003;26:1701 – 5. [77] Tsutamoto T, Hisanaga T, Wada A, Maeda K, Ohnishi M, Fukai D, et al. Interleukin-6 spillover in the peripheral circulation increases with the severity of heart failure, and the high plasma level of interleukin6 is an important prognostic predictor in patients with congestive heart failure. J Am Coll Cardiol 1998;31:391 – 8. [78] Janssen SP, Gayan-Ramirez G, Van den Bergh A, Herijgers P, Maes K, Verbeken E, et al. Interleukin-6 causes myocardial failure and skeletal muscle atrophy in rats. Circulation 2005;111: 996 – 1005. [79] Grey A, Mitnick MA, Shapses S, Ellison A, Gundberg C, Insogna K. Circulating levels of interleukin-6 and tumor necrosis factor-alpha are elevated in primary hyperparathyroidism and correlate with markers of bone resorption-a clinical research center study. J Clin Endocrinol Metab 1996;81:3450 – 4. Downloaded from by guest on October 28, 2014 [41] Brilla CG, Matsubara LS, Weber KT. Anti-aldosterone treatment and the prevention of myocardial fibrosis in primary and secondary hyperaldosteronism. J Mol Cell Cardiol 1993;25:563 – 75. [42] Ramires FJA, Sun Y, Weber KT. Myocardial fibrosis associated with aldosterone or angiotensin II administration: attenuation by calcium channel blockade. J Mol Cell Cardiol 1998;30:475 – 83. [43] Nickerson PA, Yang F. Calcium distribution in aortic smooth muscle cells of deoxycorticosterone-hypertensive rats. A quantitative cytochemical study. J Submicrosc Cytol Pathol 1988;20:317 – 24. [44] Wuorela H. The effect of high calcium intake on intracellular free [Ca2+] and Na+ – H+ exchange in DOC – NaCl-hypertensive rats. Pharmacol Toxicol 1992;71:376 – 82. [45] Kh R, Khullar M, Kashyap M, Pandhi P, Uppal R. Effect of oral magnesium supplementation on blood pressure, platelet aggregation and calcium handling in deoxycorticosterone acetate induced hypertension in rats. J Hypertens 2000;18:919 – 26. [46] Delva P, Pastori C, Degan M, Montesi G, Brazzarola P, Lechi A. Intralymphocyte free magnesium in patients with primary aldosteronism: aldosterone and lymphocyte magnesium homeostasis. Hypertension 2000;35:113 – 7. [47] Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, et al. Hyperparathyroidism and the calcium paradox of aldosteronism. Circulation 2005;111:871 – 8. [48] Vidal A, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC, Weber KT. The calcium paradox of aldosteronism and the role of the parathyroid glands. Am J Physiol, Heart Circ Physiol 2006;290: H286 – 94. [49] Duchen MR. Mitochondria and Ca2+ in cell physiology and pathophysiology. Cell Calcium 2000;28:339 – 48. [50] Massry SG, Smogorzewski M. Mechanisms through which parathyroid hormone mediates its deleterious effects on organ function in uremia. Semin Nephrol 1994;14:219 – 31. [51] Conn JW. Aldosteronism in man. Some clinical and climatological aspects: Part I. JAMA 1963;183:775 – 81. [52] Conn JW. Aldosteronism in man. Some clinical and climatological aspects: Part II. JAMA 1963;183:871 – 8. [53] Horton R, Biglieri EG. Effect of aldosterone on the metabolism of magnesium. J Clin Endocrinol Metab 1962;22:1187 – 92. [54] Rastegar A, Agus Z, Connor TB, Goldberg M. Renal handling of calcium and phosphate during mineralocorticoid ‘‘escape’’ in man. Kidney Int 1972;2:279 – 86. [55] Gehr MK, Goldberg M. Hypercalciuria of mineralocorticoid escape: clearance and micropuncture studies in the rat. Am J Physiol 1986;251(5 Pt 2):F879 – 88. [56] Cappuccio FP, Markandu ND, MacGregor GA. Renal handling of calcium and phosphate during mineralocorticoid administration in normal subjects. Nephron 1988;48:280 – 3. [57] Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, et al. Loss of bone minerals and strength in rats with aldosteronism. Am J Physiol, Heart Circ Physiol 2004;287: H2023 – 6. [58] Bhattacharya SK, Williams JC. Modified method of urinary calcium and magnesium determinations by atomic absorption spectrophotometry using nitrous oxide-acetylene flame. Anal Lett 1979;12: 397 – 414. [59] Bhattacharya SK, Williams JC, Palmieri GMA. Determination of calcium and magnesium in cardiac and skeletal muscles by atomic absorption spectroscopy using stoichiometric nitrous oxide-acetylene flame. Anal Lett 1979;12:1451 – 75. [60] Nagy TR, Prince CW, Li J. Validation of peripheral dual-energy Xray absorptiometry for the measurement of bone mineral in intact and excised long bones of rats. J Bone Miner Res 2001;16:1682 – 7. [61] Combs NR, Kornegay ET, Lindemann MD, Notter DR, Wilson JH, Mason JP. Calcium and phosphorus requirement of swine from weaning to market weight: II. Development of response curves for bone criteria and comparison of bending and shear bone testing. J Anim Sci 1991;69:682 – 93. Y. Sun et al. / Cardiovascular Research 71 (2006) 300 – 309 [96] Smogorzewski M, Massry SG. Uremic cardiomyopathy: role of parathyroid hormone. Kidney Int Suppl 1997;62:S12. [97] Schlu¨ter KD, Piper HM. Cardiovascular actions of parathyroid hormone and parathyroid hormone-related peptide. Cardiovasc Res 1998;37:34 – 41. [98] Nasri H, Baradaran A, Naderi AS. Close association between parathyroid hormone and left ventricular function and structure in end-stage renal failure patients under maintenance hemodialysis. Acta Med Austriaca 2004;31:67 – 72. [99] McGonigle RJ, Fowler MB, Timmis AB, Weston MJ, Parsons V. Uremic cardiomyopathy: potential role of vitamin D and parathyroid hormone. Nephron 1984;36:94 – 100. [100] Lemmila¨ S, Saha H, Virtanen V, Ala-Houhala I, Pasternack A. Effect of intravenous calcitriol on cardiac systolic and diastolic function in patients on hemodialysis. Am J Nephrol 1998;18:404 – 10. [101] Na¨ppi S, Saha H, Virtanen V, Limnell V, Sand J, Salmi J, et al. Left ventricular structure and function in primary hyperparathyroidism before and after parathyroidectomy. Cardiology 2000;93:229 – 33. [102] Grey A, Mitnick MA, Masiukiewicz U, Sun BH, Rudikoff S, Jilka RL, et al. A role for interleukin-6 in parathyroid hormone-induced bone resorption in vivo. Endocrinology 1999;140:4683 – 90. [103] Tatsumi T, Matoba S, Kawahara A, Keira N, Shiraishi J, Akashi K, et al. Cytokine-induced nitric oxide production inhibits mitochondrial energy production and impairs contractile function in rat cardiac myocytes. J Am Coll Cardiol 2000;35:1338 – 46. [104] Cain BS, Meldrum DR, Dinarello CA, Meng X, Joo KS, Banerjee A, et al. Tumor necrosis factor-alpha and interleukin-1beta synergistically depress human myocardial function. Crit Care Med 1999;27:1309 – 18. [105] Joe EK, Schussheim AE, Longrois D, Ma¨ki T, Kelly RA, Smith TW, et al. Regulation of cardiac myocyte contractile function by inducible nitric oxide synthase (iNOS): mechanisms of contractile depression by nitric oxide. J Mol Cell Cardiol 1998;30:303 – 15. [106] de Lorgeril M, Salen P, Accominotti M, Cadau M, Steghens JP, Boucher F, et al. Dietary and blood antioxidants in patients with chronic heart failure. Insights into the potential importance of selenium in heart failure. Eur J Heart Fail 2001;3:661 – 9. [107] Witte KK, Clark AL, Cleland JG. Chronic heart failure and micronutrients. J Am Coll Cardiol 2001;37:1765 – 74. [108] Chmielinska JJ, Tejero-Taldo MI, Mak IT, Weglicki WB. Intestinal and cardiac inflammatory response shows enhanced endotoxin receptor (CD14) expression in magnesium deficiency. Mol Cell Biochem 2005;278:53 – 7. [109] Polidori MC, Pratico´ D, Savino K, Rokach J, Stahl W, Mecocci P. Increased F2 isoprostane plasma levels in patients with congestive heart failure are correlated with antioxidant status and disease severity. J Card Fail 2004;10:334 – 8. [110] Houston MC. Nutraceuticals, vitamins, antioxidants, and minerals in the prevention and treatment of hypertension. Prog Cardiovasc Dis 2005;47:396 – 449. Downloaded from by guest on October 28, 2014 [80] Takahashi S, Hakuta M, Aiba K, Ito Y, Horikoshi N, Miura M, et al. Elevation of circulating plasma cytokines in cancer patients with high plasma parathyroid hormone-related protein levels. Endocr Relat Cancer 2003;10:403 – 7. [81] Molavi B, Mehta JL. Oxidative stress in cardiovascular disease: molecular basis of its deleterious effects, its detection, and therapeutic considerations. Curr Opin Cardiol 2004;19:488 – 93. [82] Ungvari Z, Gupte SA, Recchia FA, Batkai S, Pacher P. Role of oxidative-nitrosative stress and downstream pathways in various forms of cardiomyopathy and heart failure. Curr Vasc Pharmacol 2005;3:221 – 9. [83] Wykretowicz A, Furmaniuk J, Smielecki J, Deskur-Smielecka E, Szczepanik A, Banaszak A, et al. The oxygen stress index and levels of circulating interleukin-10 and interleukin-6 in patients with chronic heart failure. Int J Cardiol 2004;94:283 – 7. [84] Shioji K, Nakamura H, Masutani H, Yodoi J. Redox regulation by thioredoxin in cardiovascular diseases. Antioxid Redox Signal 2003;5:795 – 802. [85] Takano H, Zou Y, Hasegawa H, Akazawa H, Nagai T, Komuro I. Oxidative stress-induced signal transduction pathways in cardiac myocytes: involvement of ROS in heart diseases. Antioxid Redox Signal 2003;5:789 – 94. [86] Demirbag R, Yilmaz R, Erel O, Gultekin U, Asci D, Elbasan Z. The relationship between potency of oxidative stress and severity of dilated cardiomyopathy. Can J Cardiol 2005;21:851 – 5. [87] Reth M. Hydrogen peroxide as second messenger in lymphocyte activation. Nat Immunol 2002;3:1129 – 34. [88] Stefenelli T, Pacher R, Woloszczuk W, Glogar D, Kaindl F. Parathyroid hormone and calcium behavior in advanced congestive heart failure [German]. Z Kardiol 1992;81:121 – 5. [89] Christ E, Linka A, Junga G, Odermatt M, Steinert H, Kiowski W, et al. Bone density and laboratory parameters of bone metabolism in patients with terminal heart disease [German]. Schweiz Med Wochenschr 1996;126:1553 – 9. [90] Schmid C, Kiowski W. Hyperparathyroidism in congestive heart failure. Am J Med 1998;104:508 – 9. [91] Zittermann A, Schleithoff SS, Tenderich G, Berthold HK, Korfer R, Stehle P. Low vitamin D status: a contributing factor in the pathogenesis of congestive heart failure? J Am Coll Cardiol 2003;41:105 – 12. [92] Khouzam RN, Dishmon DA, Farah V, Flax SD, Carbone LD, Weber KT. Secondary hyperparathyroidism in patients with untreated and treated congestive heart failure. Am J Med Sci 2006;331:30 – 4. [93] LaGuardia SP, Dockery BK, Bhattacharya SK, Nelson MD, Carbone LD, Weber KT. Hyperparathyroidism and hypovitaminosis D in African-Americans with heart failure [abstract]. J Investig Med 2006;54(Suppl 1):S302. [94] Weber KT, Brilla CG, Janicki JS. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc Res 1993;27:341 – 8. [95] Nickerson PA, Conran RM. Parathyroidectomy ameliorates vascular lesions induced by deoxycorticosterone in the rat. Am J Pathol 1981;105:185 – 90. 309
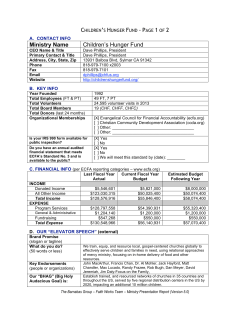
© Copyright 2025