CONTACT INFORMATION FOR PROVIDERS DEPARTMENT PHONE
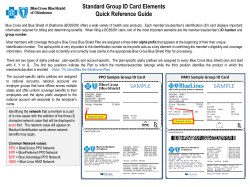
CONTACT INFORMATION FOR PROVIDERS DEPARTMENT CUSTOMER/PROVIDER SERVICE PHONE NUMBER E-MAIL CONTACT FOR ISSUES RELATED TO: BlueCard Claim Inquiries including New England Health Plan (complete listing of NEHP prefixes available on our provider website at www.bcbsvt.com under the provider manual & reference guidelines link then general documents) BlueCard Eligibility/Benefits (800) 395-3389 (800) 676-2583 customerservice@bcbsvt.com (802) 225-7698 CBA Blue (complete listing of CBA Blue prefixes available on our provider website at www.bcbsvt.com under the provider manual & reference guidelines link then general documents) Federal Employee Program (alpha prefix R) (888) 222-9206 Not Available (802) 846-2755 (800) 328-0365 fepcustomerservice@bcbsvt.com (802) 225-7700 Blue Cross and Blue Shield of Vermont products (complete listing available on our provider website at www.bcbsvt.com under the provider manual & reference guidelines link then general documents) (800) 924-3494 customerservice@bcbsvt.com (802) 371-3658 FRAUD HOTLINE (800) 337-8440 N/A N/A To report suspected fraudulent activity INTEGRATED HEALTH MANAGEMENT (800) 922-8778 customerservice@bcbsvt.com (802) 371-3491 Physician to Physician calls Prior Approval submission Referral Authorization submission Pre-Certification/Pre-Admission (Formerly Medical Services) Contact information for providers Updated: November 2014 customerservice@bcbsvt.com FAX (802) 225-7698 Benefits Claim status/adjustment/denial Check traces Coordination of benefits Eligibility Negative balance issues Prior Approval status Referral Authorization(NEHP only) Remittance Advice issues MANAGED MENTAL HEALTH Vermont Collaborative Care (VCC) (800) 922-8778 customerservice@bcbsvt.com Prior Approval (PA) Forms (802) 371-3491 Prior Approval of Managed Mental Health Services (888) 620-1746 http://groups.rxmedicareplans.co m/pdfs/CoverageDeterminationPh ysician.pdf (855) 633-7673 All pharmacy related questions/issues including prior approval submission and prior approval status. (877) 493-1947 https://expressPA.pahub.com (888) 255-1006 (877) 727-3784 Not Available (877) 378-4727 All pharmacy related questions/issues including prior approval submission and prior approval status (800) 701-0080 www.aimspecialtyhealth.com Not Available NOTE: Alpha prefixes FAH and FAO do not use VCC. Benefits are through CIGNA. Prefix FAC and R (FEP) only requires VCC approval for inpatient services. PHARMACY BENEFIT MANAGERS Employer Group Wrap (EGWP)Plan Medicare Part D coverage administered by BCBSVT via the New England Joint Enterprise product, Blue Medicare RX. This is used by some large group retirees, such as Vermont Education Health Initiative (VEHI). Express Scripts, Inc. (ESI) NOTE: Alpha prefixes CWS, FAC, FAH and FAO do not use ESI. Benefits are through CIGNA. Federal Employee Program (alpha prefix of “R”) pharmacy benefits are managed by Caremark. State of Vermont members, alpha prefix DVT, EVT and FVT have pharmacy benefits directly through ESI. They have their own ID cards and ID numbers for the benefit. RADIOLOGY AIM Specialty Health NOTE: FEP (prefix R) does not require prior approval. Contact information for providers Updated: November 2014 Submission, status of prior approval for radiology services TECHNICAL HELP DESK Electronic Data Interchange - EDI Website Technical Support/Enrollment PROVIDER ENROLLMENT OR CREDENTIALING PROVIDER RELATIONS Contact information for providers Updated: November 2014 (800) 334-3441 option 1 helpdesk@bcbsvt.com (802) 371-3659 All website issues including password/user name (800) 334-3441 option 2 editechsupport@bcbsvt.com (802) 225-7696 835/837 set up or information New clearinghouse information (888) 449-0443 Option 2 providerfiles@bcbsvt.com (802) 371-3489 Enrollment. credentialing or demographic changes (888) 449-0443 Option 1 providerrelations@bcbsvt.com (802) 371-3489 Contractual or educational issues.
© Copyright 2025