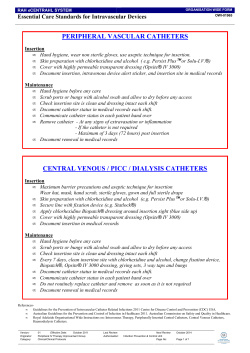
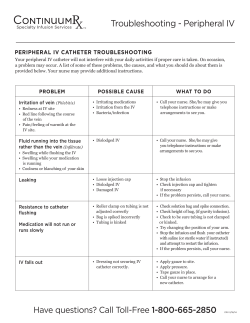
IDENTIFICATION OF PROXIMAL APPLICATION AND REMOVAL HUMERUS INSERTION SITE INSERTION TECHNIQUE
IDENTIFICATION OF PROXIMAL HUMERUS INSERTION SITE A A: Place the patient’s hand over the abdomen (elbow adducted and humerus internally rotated). INSERTION TECHNIQUE APPLICATION AND REMOVAL EZ-IO SYSTEM STEP 1: Locate the insertion site. STEP 6: Attach the primed EZ-Connect B REf. STEP 7: Remove the adhesive from the back 9058 of the EZ-Stabilizer dressing and apply it to the skin. QTY EZ-IO ® power driver 1 hospital protocol. Stabilise extremity. You should be able to feel this ball, even on obese patients, by pushing deeply. B: Place the ulnar aspect of STEP 8: Confirm placement. Flush the EZ-IO your hand vertically over the axilla. catheter with normal saline (5-10 ml for adults; 2-5 ml for infants/children). This may require multiple flushes. Place the ulnar aspect of your other hand along the midline of the upper arm laterally. C Paediatrics only STEP 2: Clean the insertion site per EZ-IO® POWER DRIVER extension set, firmly secure to the catheter hub with clamp open. Place your palm on the patient’s shoulder anteriorly. The area that feels like a “ball” under your palm is the general target area. ORDERING INFORMATION C: Place your thumbs STEP 3: Gently press the needle through the skin until the tip touches the bone. The 5 mm black mark on the catheter must be visible prior to insertion. Squeeze the trigger, apply gentle steady pressure. EZ-IO® NEEDLE + STABILIZER KITS REf. Prior to flush, consider intraosseous 2% preservative- and epinephrine-free lidocaine IO for patients responsive to pain – follow institutional protocols/policy. QTY 9079P 45 mm needle + stabilizer 5 9001P 25 mm needle + stabilizer 5 9018P 15 mm needle + stabilizer 5 together over the arm. This identifies the vertical line of insertion on the proximal humerus. D: Palpate deeply up the STEP 9: Deliver medication and fluids STEP 4: Stabilise the hub and remove the driver and the stylet. Place the stylet in an appropriate sharps container. humerus to the surgical neck. D This may feel like a golf ball on a tee – the spot where the “ball” meets the “tee” is the surgical neck. The insertion site is 1 to 2 cm above the surgical neck, on the most prominent aspect of the greater tubercle. STEP 5: Place the EZ-Stabilizer dressing over the catheter hub. as ordered. If adequate IO flow rates cannot be achieved with an infusion pump, a pressure bag should be considered. Each kit includes a sterile 15 G EZ-IO needle set, EZ-Stabilizer dressing, EZ-Connect ® extension set, EZ-IO ® patient wrist band and NeedleVISE® 1 port sharp block ® ® AUSTRALIA/NEW ZEALAND +61 (0)3 9081 0600 AUSTRIA +43 (0)1 402 47 72 BELGIUM +32 (0)2 333 24 60 CHINA (SHANGHAI) +86 (0)21 6163 0965 CHINA (BEIJING) +86 (0)10 6418 5699 CZECH REPUBLIC +420 (0)495 759 111 FRANCE +33 (0)5 62 18 79 40 GERMANY +49 (0)7151 406 0 GREECE +30 210 67 77 717 INDIA +91 (0)44-2836 5040 ITALY +39 0362 58 911 JAPAN +81 (0)3 3379 1511 NETHERLANDS +31 (0)88 00 215 00 PORTUGAL +351 22 541 90 85 SINGAPORE +65 6439 3000 SCAN AND GET SLOVAK REPUBLIC +421 (0)3377 254 28 THE EZ-IO® APP SOUTH AFRICA +27 (0)11 807 4887 SPAIN +34 918 300 451 SWITZERLAND +41 (0)31 818 40 90 UNITED KINGDOM +44 (0)1494 53 27 61 For detailed information see www.arrowezio.com REMOVAL STEP 10: Using a sterile Luer-lock syringe as a handle, attach to hub of needle, maintain alignment and rotate clockwise while pulling straight up. Avoid rocking the needle on removal, dispose of catheter with syringe attached in an approved sharps container. TELEFLEX HEADQUARTERS INTERNATIONAL, IRELAND Teleflex Medical Europe Ltd., IDA Business and Technology Park, Dublin Road, Athlone, Co Westmeath Phone +353 (0)9 06 46 08 00 · Fax +353 (0)14 37 07 73 orders.intl@teleflex.com Teleflex, Arrow, EZ-IO, EZ-Connect and EZ-Stabilizer are trademarks or registered trademarks of Teleflex Incorporated or its affiliates. NeedleVISE is a product of Atrion Medical Products Inc. Vidacare LLC is a wholly owned subsidiary of Teleflex Incorporated. © 2014 Teleflex Incorporated. All rights reserved. US-REV MC-000280 24 HOUR CLINICAL SUPPORT: +1-800-680-4911 The products in this catalogue may not be available in all countries. Please contact your local representative. All data current at time of printing (09/2014). Subject to technical changes without further notice. 94 07 74 - 00 00 01 · REV A · MC / GH · 09 14 15 EZ-IO ® Power Driver EZ-Stabilizer ® Dressing EZ-IO ® Needle Sets 45 mm 25 mm 15 mm EZ-Connect ® Extension Set EZ-IO® INTRAOSSEOUS VASCULAR ACCESS SYSTEM Pocket Guide INSERTION SITES PAIN MANAGEMENT GUIDE The Arrow EZ-IO Intraosseous vascular access system provided by Teleflex offers multiple sites for safe and fast vascular access in emergent, urgent or medically necessary cases for up to 72 hours. TYPICAL PAIN LEVELS EXPERIENCED BY CONSCIOUS AND ALERT PATIENTS DURING MEDICAL PROCEDURES EZ-IO SYSTEM INSERTION SITES Do NOT use the powered EZ-IO vascular access system in the sternum ADVANTAGES OF PROXIMAL HUMERUS SITE INCLUDE: •f low rates average 5 l/hour •3 seconds to heart with medication/fluids •lower insertion & infusion pain •less medication required for pain management •no reported compartment syndrome due to IO placement Potential complications may include local or systemic infection, hematoma, extravasations or other complications associated with percutaneous insertion of sterile devices. PAIN MANAGEMENT GUIDE Periosteum Haversian canal Spongy Bone Many medically necessary procedures involve pain and may cause anxiety. 0 • One peripheral IV needle insertion • EZ-IO system insertion* • EZ-IO system infusion with appropriate Lidocaine dosing* 2-3 • Multiple IV attempts • Foley catheter* 4-5 • Nasogastric tube* • Incision and drainage of an abscess 5-6 • Central venous catheter* • Arterial blood gas/arterial line* • Lumbar puncture 7-8 • IO infusion without Lidocaine • Shoulder reduction without pre-medication • Chest tube insertion 8-9 2 4 6 8 INSERTION EZ-IO system insertion pain is quick and immediate. Insertion pain rates as a 3 on a 0-10 pain scale.1 INFUSION The pain associated with EZ-IO system infusion can be manageable with correct dosing and application of 2% preservative and epinephrine-free lidocaine (per hospital protocol). Volkmann’s canal Pain sensors skin and periosteum (somatic pain) Pain sensors blood vessels (visceral pain) Vein Artery Nerve 10 * Data on file. Data in chart for illustrative purposes only Compact bone IO BLOOD SAMPLING FLUIDS AND MEDICATIONS FLUIDS AND MEDICATIONS LABORATORY ANALYSIS/BLOOD SAMPLING Virtually any fluid or medication that can be safely infused via peripheral IV route may be safely infused through the intraosseous (IO) route. Incompatible drugs and fluids should be infused sequentially in a manner consistent with standard IV infusion practice. However, if the choice is made to infuse chemotherapy agents, it should be done with extreme caution. Verify placement/patency prior to all infusions. Use caution when infusing hypertonic solutions, chemotherapeutic agents, or vesicant drugs. •Heparin • Hydroxocobalamin (B12) •Hydromorphone (e.g. Dilaudid) •Insulin •Isoprenaline (e.g. isoproterenol, Isuprel) •Ketamine •Labetalol (e.g. Normodyne) •Levetiracetam (e.g. Keppra) •Lidocaine (e.g. Xylocaine) • Linezolid (e.g. Zyvox) • Lorazepam (e.g. Ativan) • Magnesium sulfate •Mannitol •Methylprednisolone (e.g. Solu-Medrol) •Metoprolol (e.g. Lopressor) • Midazolam (e.g. Versed) •Mivacurium (e.g. Mivacron) • Morphine sulfate Nalbuphine (e.g. Nubain) • Naloxone (e.g. Narcan) •Neostigmine (e.g. Prostigmin) •Nitroglycerin •Nitroprusside (e.g. Nipride) •Norcuron • Norepinephrine (Levarterenol, Levophed) • Normal saline • Ondansetron (e.g. Zofran) Based on preclinical and clinical evidence comparing IO and venous or arterial sources a number of common laboratory values correlate well; other values show clinical similarity without statistically significant correlation, therefore caution should be exercised with their interpretation. Certain point of care analysers have been studied with acceptable results. Check with your laboratory for IO specimen processing capabilities. For more information regarding IO lab analysis, refer to the Vidacare publication Science and Fundamentals of Intraosseous Vascular Access, available at: www.teleflex.com/ezioeducation. The following recommendations have been developed based on research done by Teleflex Incorporated. Study data was based on IO blood specimens obtained prior to any infusions or flush. The intraosseous (IO) space contains a matrix of blood vessels and nerves. This structure provides rapid distribution of fluids and medications, and also contains numerous sensory receptors that register pressure variations. This pressure can be very uncomfortable or painful for a responsive patient. RECOMMENDED ANAESTHETIC FOR PATIENTS RESPONSIVE TO PAIN: • Observe recommended cautions/contraindications to using 2% preservative and epinephrine-free lidocaine (intravenous lidocaine). • Confirm lidocaine dose per institutional protocol. • For adults, usual initial dose is 40 mg. • For peadiatrics, usual initial dose is 0.5 mg/kg, not to exceed 40 mg. • Prime extension set with lidocaine. Note that the priming volume of the EZ-Connect extension set is approximately 1.0 ml. • Slowly infuse lidocaine over 120 seconds. Allow lidocaine to dwell in IO space for 60 seconds. • Flush with normal saline. • Slowly administer an additional lidocaine dose (1/2 of initial dose) IO over 60 seconds. Repeat PRN. • Consider systemic pain control for patients not responding to IO lidocaine. Note: See back panel for additional information on the use of lidocaine and other medications with the Arrow EZ-IO System. • • • Connect a syringe directly to the EZ-IO Catheter hub. The first 2 ml of IO blood aspirate may be discarded or considered for point of care testing. Specimens must be identified as IO blood. The use of any medication, including lidocaine, given IV or IO is the responsibility of the treating physician, medical director or qualified prescriber and not an official recommendation of Teleflex Incorporated or its subsidiaries. Teleflex is not the manufacturer of lidocaine, and the user should be familiar with the manufacturer’s instructions or directions for use for all indications, side-effects, contraindications, precautions and warnings of lidocaine. Teleflex disclaims all liability for the use, application or interpretation of the use of this information in the medical treatment of any patient. Dosing recommendations were developed based on research; for references, research and dosing charts, please visit www.eziocomfort.com. 1 hilbeck TE, Miller LJ, Montez D, Puga T. Hurts so good; easing IO P pain and pressure. JEMS 2010;35(9):58-69. (Vidacare Conducted Study-citation speaks only to flow rates humerus greater than tibia; flush & using pressure) 24 HOUR CLINICAL SUPPORT: +1-800-680-4911 • Adenosine (e.g. Adenocard) •Albumin • Alfentanil (e.g. Alfenta) •Aminophylline •Amiodarone (e.g. Cordarone) •Ampicillin •Anascorp (scorpion antivenin) • Anesthetic agents • Antibiotics (multiple) • Antitoxins (various) • Atracurium besylate (e.g. Tracrium) •Atropine • Azactam (e.g. Aztreonam) • Blood and blood products • Calcium chloride • Calcium gluconate • Cefepime hydrochloride (e.g. Maxipime) • Ceftriaxone (e.g. Rocephin) • Contrast media (Omnipaque) •Dexamethasone (e.g. Decadron) •Dextran • D5 ½NS • Dextrose 10% • Dextrose 25% • Dextrose 50% • Diazepam (e.g. Valium) • Diazoxide (e.g. Hyperstat) • Digoxin (e.g. Lanoxin) • Diltiazem (e.g. Cardizem) •Diphenhydramine (e.g. Benadryl) • Dobutamine hydrochloride (e.g. Dobutrex) •Dopamine •Ephedrine •Epinephrine • Esmolol (e.g. Brevibloc) •Etomidate •Fentanyl • Fluconazole (e.g. Diflucan) • Flumazenil (e.g. Romazicon) •Fosphenytoin (e.g. Cerebyx, Prodilantin) • Furosemide (e.g. Lasix) •Gentamicin • Haloperidol (e.g. Haldol) •Pancuronium (e.g. Pavulon) •Paracetamol (i.e. acetaminophen) •Phenobarbital •Phenylephrine (e.g. Neo-Synephrine) • Phenytoin (e.g. Dilantin) • Piperacillin (e.g. Zosyn) •Plasmanate • Potassium chloride •Promethazine (e.g. Phenergan) • Propofol (e.g. Diprivan) • Propranolol (e.g. Inderal) • Remifentanil (e.g. Ultiva) • Ringer’s lactate •Rocuronium (e.g. Zemuron) • Sodium bicarbonate • Standard IV solutions •Succinylcholine (e.g. Anectine) •Tenecteplase (e.g. TNKase) •Thiamine •Thiopental (e.g. Pentothal) • Tobramycin sulfate •Vancomycin •Vasopressin (e.g. Pitressin, Argipressin) •Vecuronium
© Copyright 2025