New ESPGHAN guidelines for the diagnosis of Coeliac Disease in Steffen Husby
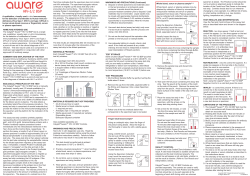
New ESPGHAN guidelines for the diagnosis of Coeliac Disease in Children and Adolescents Steffen Husby Hans Christian Andersen Children’s Hospital Odense University Hospital, Denmark Agenda • • • • Change in clinical paradigm Definitions of coeliac disease New diagnostic guidelines Algorithms Interlaken ESPGHAN criteria (1979) 1. 2. 3. 4. 5. Small intestinal biopsy: villous atrophy Gluten free diet for 1-2 years Biopsy: normal. Re-introduction of gluten Biopsy: villous atrophy McNeish et al. Arch Dis Childh 1979;54:783 Revised ESPGHAN criteria 1990 1. Small intestinal biopsy: villous atrophy 2. Clinical and serological improvement after 2-3 months • • No further biopsy Provided age > 2 years Walker‐Smith et al. Arch Dis Child 1990;65:99 Celiac disease as a multiorgan autoimmune disease General: Puberty & growth delay Malignancies Anemia CNS: Ataxia, seizures Depression Heart: Carditis GI system: Diarrhea, vomiting Distension, pain Malnutrition, weight loss Hepatitis, cholangitis Bone: Osteoporosis, fractures Arthritis Dental anomalies Skin & mucosa: Dermatitis herpetiformis Aphtous stomatitis Hair loss Reproductive system: Miscarriage Infertility Modified from Rewers, Gastroenterology 2005 Patient Adrenal antibodies Type 1 Diabetes Coeliac disease Dermatitis herpetiformis Autoimmune hypothyroidism Hansen et al. unpublished Towards a new definition of coeliac disease Chronic Multi-organ Small intestinal inflammation Transglutaminase-related ESPGHAN working group, 2011 Suggestion: New definition an immune-mediated systemic disorder elicited by gluten and related prolamines in genetically (mainly HLA) susceptible individuals characterized by a combination of: • gluten dependent clinical manifestations • anti-tissue transglutaminase (TG2) antibodies • enteropathy Husby et al. JPGN 2012 ESPGHAN classification Silent CD: positive CD antibodies and biopsy findings, not sufficient symptoms to warrant clinical suspicion of CD Latent CD: positive CD antibodies, no villous atrophy. The patient has had a glutendependent enteropathy. Patient may/may not have symptoms Potential CD: positive antibodies, but no villous atrophy. Patient may/may not have symptoms. CD may or may not develop The Oslo Definitions Coeliac disease is a chronic small intestinal immune-mediated enteropathy precipitated by exposure to dietary gluten in genetically predisposed individuals. Discourage the use of classical vs. non-classical, typical vs. atypical Discourage the use of the term latent CD Ludvigsson et al. Gut 2012 ESGPHAN member Questionnaire 85 % of those who are compliant to the 1990 criteria want them to be changed • challenge policy: 100 % • HLA should be included for DX 80% C.Ribes et al. JPGN 2012 Previous evidence-based guidelines for CD diagnosis AHRQ (USA, 2004) Adults and children NICE guidelines (UK, 2009) Adults and children For GP’s and general paediatricians None questioned the biopsy Rostom A, et al.. Celiac Disease. EvidenceReport/ Technology Assessment No. 104. AHRQ Publication No. 04-E029-2, 2004 NICE Clinical Guidelines 86. Coeliac Disease: Recognition and assessment of coeliac disease. UK, May 2009 Guidelines: AHRQ (USA, 2004) Main issues 1. 2. 3. 4. 5. Sensitivity/specificity of serological tests Prevalence / incidence of CD CD associated lymphoma Consequences of testing for CD Interventions for adherence to a glutenfree diet Conclusions Sensitivity and specificity of EMA and TG2 ab quite high 2. CD common, prevalence in the general population likely close to 1:100 3. Education/participation in coeliac societies improves compliance with a GFD 1. Rostom A, et al.. Celiac Disease. EvidenceReport/Technology Assessment No. 104. AHRQ Publication No. 04‐E029‐2, 2004 Evidence-based criteria for clinical decisions 1. 2. 3. Formulate an answerable question Track down the best evidence Critically appraise the evidence for • Validity • Impact (size of the benefit) • Applicability 4. 5. Integrate with clinical expertise and patient values Evaluate our effectiveness and efficiency Clinical circumstances Evidence-based medicine Patient preferences and values • keep a record/improve the process Devereaux 2004 Literature search Search 1: n=1,418 EMBASE, Medline 01.01.2004-15.07.2007 Search 2: n=402 Medline 17.07.07-15.09.2008 Search 3: n=778 Embase 15.07.2007-01.09.2009 Medline 15.09.2008-01.09.2009 n=2,598 Entering Level 1 screening n=2,242 + 22 no full text excluded n=334 Full text Entering Level 2 screening n=247 excluded n=87 Entering Level 3 screening n = 16 publications Included in data synthesis N = 71 excluded based on E1-8: No biopsy Age Quality etc. Giersiepen et al. 2010 Grading Evidence Type of study: Diagnosis Study Quality Level 1: Good quality patient-oriented evidence Validated clinical decision rule Systematic Review(SR)/meta- Level 2: Limited quality patientoriented evidence Unvalidated clinical decision rule SR/meta-analysis of lower quality Level 3: Other evidence Consensus guidelines, extrapolations from bench research, usual practice, opinion, disease-oriented evidence, case series etc. analysis of high quality studies High quality diagnostic cohort study studies or studies Lower quality diagnostic cohort study or diagnostic case control study Ebell MH et al. JABFP 2004 Example statement: Increased prevalence of CD in children with % • • • • • • • • Type 1 diabetes Down’s syndrome Autoimmune thyroid disease Turner syndrome Williams’ syndrome IgA deficiency Autoimmune liver disease First degree relatives with CD 2–12 5-12 up to 7 2-5 up to 9 2-8 12-13 10-20 Recommendation: (↑↑) offer testing for CD of children and adolescents with the following conditions: Type 1 diabetes Down’s syndrome Autoimmune thyroid disease Turner syndrome Williams’ syndrome IgA deficiency Autoimmune liver disease 1st degree relatives with CD Coeliac Antibodies • IgA Anti-TG2 antibody • IgA Endomysial antibody (EMA) • IgA and IgG Deamidated Gliadin Peptide (DPG) antibody • NOT: IgA and IgG anti-gliadin antibodies DISEASE PREDICTION BY ANTIBODIES (pooled estimates with 95% confidence values; § indicates high hetereog neity) EMA /IgA Anti-TG2 /IgA Anti-DGP /IgG Anti-DGP /IgA AGA /IgA Positive likelihood ratio Negative likelihood ratio Odd’s ratio 31.8 0.067§ 553 (18.6-54.3) (0.038-0.118) (218-1402) 21.8§ 0.060§ 469§ (12.9-36.8) (0.040-0.090) (250-880) 13.6 0.061§ 234 (8.1-22.8) (0.017-0.221) (100-546) 9.4 0.121§ 86.1 (6.8-13.1) (0.072-0.203) (56-132) 7.3§ 0.186§ 40.6§ (4.5-11.8) (0.095-0.362) (14-117) Giersiepen, Evidence report, JPGN 2012 Development of symptomatic coeliac disease in EMA positive subjects 3654 3617 3644 9 2001 1994 Diagnosed celiac: 0 56 1.5% 10 27 1:99 Mäki, N Engl J Med 2003 Predictive values for TG2 antibody Positive predict. value Toftedal et al. JCLM 2010 Median ELISA values in 14 commercial anti-TG2 assays (data kindly provided by UK NEQAS) 1000 AU 100 10 10 20 30 AU in Varelisa [Celikey] ‘High’ sample xULN Aesku 135 9.0 Binding Site 33.3 8.3 BMD Luminex 43 DiaSorin 57 Euroimmun 200 10.0 Eurospital* 95 13.6 Generic Assays 89 4.5 Genesis 69 9.9 Immco 48.3 2.4 Inova* 95.5 4.8 Orgentec 65.5 9.9 Phadia ELIA 69.0 9.9 Phadia ImmunoCAP 73.9 10.6 Phadia Varelisa 30.1 10.0 40 *logarithmic assays Child / Adolescent with Symptoms suggestive of CD Anti-TG2 IgA & total IgA* Anti-TG2 positive Transfer to Paediatric GI Anti-TG2 < 10 x normal EMA & HLA DQ8/DQ2 EMA pos. HLA pos. CD+ EMA pos. HLA neg. Consider false neg. HLA test. Consider biopsies Not CD Consider further diagnostic testing if: IgA deficiency Age: < 2 years History: - low gluten intake - drug pretreatment - severe symptoms - associated diseases Paed. GI discusses with family the 2 diagnostic pathways and consequences considering patient’s history & anti-TG2 titers Anti-TG2 > 10 x normal Anti-TG2 negative EMA neg. HLA neg. Consider false pos. anti-TG2 Not available EMA neg. HLA pos. OEGD & biopsies Marsh 0-1 Unclear case Consider: false pos. serology false neg. biopsy or potential CD Marsh 2 or 3 CD+ Child / Adolescent with Symptoms suggestive of CD Anti-TG2 IgA & total IgA* Anti-TG2 positive Transfer to Paediatric GI Anti-TG2 < 10 x normal EMA & HLA DQ8/DQ2 EMA pos. HLA pos. CD+ GFD & F/u EMA pos. HLA neg. Consider false neg. HLA test. Consider biopsies Not CD Consider further diagnostic testing if: IgA deficiency Age: < 2 years History: - low gluten intake - drug pretreatment - severe symptoms - associated diseases Paed. GI discusses with family the 2 diagnostic pathways and consequences considering patient’s history & anti-TG2 titers Anti-TG2 > 10 x normal Anti-TG2 negative EMA neg. HLA neg. Consider false pos. anti-TG2 Not available EMA neg. HLA pos. OEGD & biopsies Marsh 0-1 Unclear case Consider: false pos. serology false neg. biopsy or potential CD Extended evaluation of HLA/serology/biopsies Marsh 2 or 3 CD+ GFD & F/u Child / Adolescent with Symptoms Suggestive of CD Anti‐TG2 & total IgA* Anti‐TG2 positive Anti‐TG2 negative Transfer to Paediatric Gastroenterologist Paed. GI discusses with family the 2 diagnostic pathways and consequences considering patient’s history & anti‐TG2 titers Positive Anti‐TG2 > 10 x normal Positive Anti‐TG2 < 10 x normal EMA & HLA testing for DQ2/DQ8 EMA pos. HLA pos. CD+ EMA pos. HLA neg. EMA neg. HLA neg. Consider false neg. HLA test Consider biopsies Consider false pos. Anti‐TG2 GFD & F/u *or specific IgG based tests Not available EMA neg. HLA pos. Not CD Consider further diagnostic testing if: IgA deficient Age: < 2 years History: ‐ low gluten intake ‐ drug pretreatment ‐ severe symptoms ‐ associated diseases OEGD & biopsies Marsh 0‐1 Unclear case Consider: false pos. serology false neg. biopsy or potential CD Extended evaluation of HLA/serology/biopsies Marsh 2 or 3 CD+ GFD & F/u * Rationale for omitting biopsies in selected cases Serological tests improved over last years Histology not as perfect as thought 20 yrs ago (lower sensitivity and specificity than serology) Risk-benefit ratio has changed: risk and cost of invasive procedure (OEGD, histological work-up) versus risk of false positive diagnosis Asymptomatic person at genetic risk for CD Explain implication of positive test result(s) and get consent for testning HLA DQ2 / DQ8 (+/- TG2) HLA positive DQ2 and/or DQ8 Consider retesting in intervals or if symptomatic TG2 & total IgA* Titer > 3 x normal OEGD & biopsies From bulbus & 4 pars descendens, proper histological work up Marsh 2 or 3 CD+ GFD & F/u No CD, no risk for CD HLA negative DQ2 and/or DQ8 Titer < 3 x normal TG2 negative Not CD EMA EMA positive EMA negative Consider: False neg. Results, exclude IgA deficiency and history of low gluten intake or drugs Marsh 0-1 Unclear case F/u on normal diet. Consider: False pos. serology, false neg. biopsy or potential CD Consider: Transient/false pos. antiTG2 F/u on normal diet with further serological testing *Or specific IgG based tests Asymptomatic person at genetic risk for CD Explain implication of positive test result(s) and get consent for testning HLA DQ2 / DQ8 (+/- TG2) HLA positive DQ2 and/or DQ8 Consider retesting in intervals or if symptomatic TG2 & total IgA* Titer > 3 x normal OEGD & biopsies From bulbus & 4 pars descendens, proper histological work up Marsh 2 or 3 CD+ GFD & F/u Titer < 3 x normal Not CD, no risk for CD HLA negative DQ2 and/or DQ8 TG2 negative Not CD EMA EMA positive EMA negative Consider: False neg. Results, exclude IgA deficiency and history of low gluten intake or drugs Marsh 0-1 Unclear case F/u on normal diet. Consider: False pos. serology, false neg. biopsy or potential CD Consider: Transient/false pos. anti-TG2 F/u on normal diet with further serological testing *Or specific IgG based tests Asymptomatic Person at Genetic Risk for CD Explain implication of positive test result(s) and get consent for testing HLA DQ testing (+/‐Anti‐TG2) HLA positive for DQ2 and/or DQ8 Positive Anti‐TG2 < 3x normal no risk for CD Consider retesting in intervals or if symptomatic Anti‐TG2 & total IgA* Positive Anti‐TG2 > 3x normal Not CD, HLA negative for DQ2 and/or DQ8 Not CD Anti‐TG2 negative EMA OEGD & biopsies: 1 x bulbus & 4 x pars descendens, proper EMA positive histological work up Marsh 2 or 3 CD+ GFD & F/u EMA negative Consider: age, false neg. results, exclude IgA deficiency and history of low gluten intake or drugs Marsh 0‐1 - Unclear case F/u on normal diet Consider: false pos. serology, false neg. biopsy or potential CD Consider: Transient / false pos. anti‐TG2 F/u on normal diet with further serological testing *or specific IgG based tests * Why different algorithms for symptomatic and asymptomatic (at risk) patients? 1. 2. 3. False positive or transient TG2 antibody levels more frequent in genetically at risk persons than symptomatic cases TG2 titres with normal histology (Marsh 0) are often of low titre (<3 x upper limit of normal) In asymptomatic patients with low antibody levels there no urgency to perform biopsies compared to symptomatic patients with the same low levels. Conclusions 1. The new guidelines will offer the option of omitting biopsies in selected cases with symptoms suggestive of CD without increasing the risk of misclassification. 2. Preconditions are • • • • high quality serology including EMA taking quantitative antibody levels into account HLA typing full information to parents/patient on consequences • • • • • • • • • • • • • • • • • ESPGHAN Working Group on Celiac David Branski Disease Diagnosis Carlo Catassi Steffen Husby Sibylle Koletzko Ilma Korbonay-Szabo Luisa Mearin Markku Maki Alan Phillips Carmen Ribes Luca Ronfani Raanan Shamir Riccardo Troncone Alessandro Ventura Klaus Peter Zimmer Tunde Koltai Klaus Giersiepen Monika Lelgemann Hans Christian Andersen
© Copyright 2025