Therapeutics Today Bell’s palsy
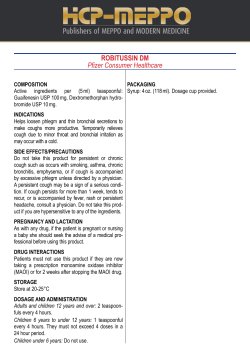
Therapeutics Today September 2006 Number 9 For personal use only. Not to be reproduced without permission of the editor. Bell’s palsy is an isolated unilateral lower motor neurone palsy. A recent article reviewed Bell’s palsy (BsP) and its current management (DTB 2006; 44: 49-52). BsP is estimated to affect 1:5,000 persons, most commonly people aged 15 to 60 years. Men and women are affected equally but a higher incidence (45:100,000) is reported in pregnant women. The majority (71%) of patients recover normal function without any treatment, however 13% of patients are left with a slight facial weakness and 16% with a moderate to severe weakness. BsP is due to inflammation of the facial nerve in the internal auditory canal. The cause of the inflammation is unknown, however one hypothesis is that it may result from reactivation of herpes simplex virus. Diagnosis: Patients with BsP have impairment of facial movements, including blinking on the affected side. Patients can also experience retro-auricular pain, hyperacusis, altered taste and reduced tear formation. It is important to exclude other causes of facial paralysis, which can be responsible for up to 25% of acute palsies affecting the facial nerve. These include a CNS lesion due to stroke (although these may cause upper motor neuron symptoms), local brain tumours, chronic otitis media, multiple sclerosis and Ramsay-Hunt syndrome. Management: Eye care is important, as patients may have reduced tear formation and difficulty closing their eye on the affected side. Patients should be advised to use lubricating eye drops during the day and ointment at night and, in addition, patients with poor eye closure should tape their eyes during the night. Emergency referral to an ophthalmologist is required for those patients whose cornea remains exposed when closing their eyes and/or if they experience eye discomfort, irritation or discharge, eye redness or change in vision. Pharmacotherapy: Although the evidence base is lacking, corticosteroids have been the principal drug treatment for BsP for many years. A common regimen is oral prednisolone 40-80 mg daily for one week, with gradual tapering in the second week. More recently the antiviral agent aciclovir has been used (based on the possible involvement of herpes simplex). Clinical trial results have been inconclusive as to the effectiveness of this form of therapy and aciclovir or other antiviral agents are not licensed for use in BsP. Corticosteroids used in combination with aciclovir were shown to improve outcome compared with corticosteroids alone in one study. Acupuncture and physiotherapy have also been tried in the management of patients with BsP, but the evidence base is also lacking. Referral to a neurologist or ENT specialist is indicated for those patients with atypical symptoms or signs of BsP or when recovery is delayed. The authors note that many patients with BsP resolve without any drug therapy. Poor memory? You know there was a fascinating article on your favourite subject in Therapeutics Today, but you can’t remember when it was published. Rack your brains no more – an index to past issues of the newsletter is now available on the NMIC website (www.nmic.ie). Click on <Therapeutics Today Newsletters> followed by <Therapeutics Today Index>. The index is in alphabetical order by drug name (or drug class), followed by the topic covered in the article. The title of the article and the issue number are then provided. All past issues are available online, by post or fax from the NMIC. Are there alternatives to HRT for menopausal symptoms? The Royal College of Obstetricians and Gynaecologists recently reviewed the various alternatives to HRT. Among those discussed were: Phytoestrogens. Epidemiological studies have suggested a beneficial effect for soy and red clover, in terms of menopausal (MP) symptoms, osteoporosis, cardiovascular disease and certain cancers (breast, ovarian, endometrial, colon), but randomised controlled trials (RCTs) with soy have shown conflicting results. Evidence of benefit was stronger with soy isoflavone supplements compared with other soy products. Although breast cancer was not a problem with use of up to 2 years, there were some concerns about a low risk of endometrial hyperplasia with long-term soy use. Short-term RCTs with red clover isoflavones showed improvements in MP symptoms but these were not always significant. Longterm safety data regarding breast or endometrial cancer are lacking. Herbalism: Although black cohosh is recommended for MP symptoms in some EU countries, there are safety concerns with its use (Therapeutics Today 2006; 8). Many other preparations, such as evening primrose oil, Dong quai, Ginkgo biloba, Ginseng, St John’s Wort and Agnus Castus, have been used but have little or no evidence base for efficacy. The paper concludes that such preparations have lower efficacy (50-60%) compared with HRT (8090%) and are not without adverse effects. [Editor’s note: The full paper dealing with other alternatives to HRT is available at: www.rcog.org.uk/index] How to manage cough in adults. Cough is one of the commonest presentations in primary care. The British Thoracic Society recently published guidance on its management in adults. Acute cough may be defined as cough lasting < 3 weeks. It is estimated to cost the UK economy at least £979 million (£875 million due to loss of productivity and £104 million due to healthcare and medicines costs). Acute cough is most commonly associated with viral upper respiratory tract infection; in the absence of significant co-morbidity it is normally benign and self-limiting. However cough is the commonest presenting symptom in patients with acute exacerbations of asthma and chronic obstructive pulmonary disease (COPD). Cough can also be the first indication of a serious condition and further investigation is required in patients presenting with concomitant haemoptysis, prominent systemic illness, suspicion of inhaled foreign body and suspicion of lung cancer. Patients with acute viral cough do not require prescribed treatment. However, patients may report benefit from OTC preparations even though many of these have little evidence of a pharmacological effect. The guideline recommends a “home remedy” such as honey and lemon for such patients. If OTC antitussives are required, dextromethorphan, menthol and sedative antihistamines have demonstrated suppression of the cough reflex and may be useful. Opiate antitussives are not recommended due to their toxicity profile. Chronic cough may be defined as cough lasting > 8 weeks. It is more likely to occur in middle-aged women and is commonly caused by smoking (dose-related effect). Many cases are caused by an aggravant such as asthma, drugs (e.g. ACE inhibitors), environmental exposures, gastro-oesophageal reflux and upper airway pathology in susceptible individuals. It may also be a prominent and debilitating symptom in respiratory diseases including COPD, lung cancer, diffuse parenchymal lung disease and bronchiectasis. The guideline recommends that chronic cough should only be considered idiopathic following a thorough assessment at a specialist cough clinic. Evaluation should include a detailed history, including occupational history, physical examination (including assessment of health status and cough severity), chest X-ray and spirometry in all patients. Other investigations including bronchoscopy and high resolution CT might also be required. A systematic approach to diagnosis and treatment remains the most effective way to manage chronic cough, with treatment directed at the cause of the cough. (Download the full guideline from www.britthoracic.org.uk/guidelinescough). Every effort has been made to ensure that this information is correct and is prepared from the best available resources at our disposal at the time of issue. References are available on request. This newsletter is produced by the National Medicines Information Centre, St. James’s Hospital (SJH), Dublin 8 and Dept of Therapeutics Trinity College Trinity Centre, SJH. Tel: Direct Line (01) 473 0589 or 1850 727 727 Fax: (01) 473 0596 Email: nmic@stjames.ie
© Copyright 2025