Yu-Chun Chen, Jau-Ching Wu, Laura Liu, Tzeng-Ji Chen, Wen-Cheng Huang... Henrich Cheng ; originally published online June 20, 2011;
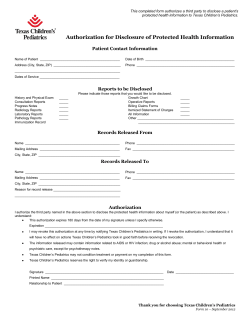
Correlation Between Ventriculoperitoneal Shunts and Inguinal Hernias in Children: An 8-Year Follow-up Yu-Chun Chen, Jau-Ching Wu, Laura Liu, Tzeng-Ji Chen, Wen-Cheng Huang and Henrich Cheng Pediatrics 2011;128;e121; originally published online June 20, 2011; DOI: 10.1542/peds.2010-3906 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://pediatrics.aappublications.org/content/128/1/e121.full.html PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly publication, it has been published continuously since 1948. PEDIATRICS is owned, published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2011 by the American Academy of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES Correlation Between Ventriculoperitoneal Shunts and Inguinal Hernias in Children: An 8-Year Follow-up AUTHORS: Yu-Chun Chen, MD, MSc,a Jau-Ching Wu, MD,b,c,d Laura Liu, MD,e Tzeng-Ji Chen, MD, PhD,f,g Wen-Cheng Huang, MD, PhD,b,c and Henrich Cheng, MD, PhDb,c,d aInstitute for Medical Biometry and Informatics, Heidelberg University, Heidelberg, Germany; bDepartment of Neurosurgery, Neurological Institute, Taipei Veterans General Hospital, Taipei, Taiwan; cSchool of Medicine, National Yang-Ming University, Taipei, Taiwan; dInstitute of Pharmacology, National Yang-Ming University, Taipei, Taiwan; eDepartment of Ophthalmology, Chang-Gung Memorial Hospital, and College of Medicine, ChangGung University, Taoyuan, Taiwan; fInstitute of Hospital and Health Care Administration, School of Medicine, National YangMing University, Taipei, Taiwan; and gDepartment of Family Medicine, Taipei Veterans General Hospital, Taipei, Taiwan WHAT’S KNOWN ON THIS SUBJECT: In the entire English literature, only 3 studies have associated ventriculoperitoneal shunt in children with higher incidence of inguinal hernia. The 3 studies were institutional based, so the true incidence and association between a ventriculoperitoneal shunt and subsequent inguinal hernia remain unclear. WHAT THIS STUDY ADDS: This study used a nationwide longitudinal cohort, the National Health Insurance Research Database, which contains data on ⬎1.5 million preschool-aged children across institutions for both hernia surgery and ventriculoperitoneal shunts in children to determine their association. KEY WORDS ventriculoperitoneal shunt, inguinal hernia, incidence ABBREVIATIONS CNS—central nervous system CSF—cerebrospinal fluid VPS—ventriculoperitoneal shunt IH—inguinal hernia ICD-9—International Classification of Disease, Ninth Revision HR—hazard ratio abstract OBJECTIVE: The goal of this study was to investigate the correlation between ventriculoperitoneal shunts (VPSs) and inguinal hernias (IHs) in children. Drs Chen and Wu provided the conception and design, acquisition of data, analysis and interpretation of data, and drafting and revision of the article; Dr Liu performed the interpretation of data and drafting and revision of the article; Dr Chen conducted the acquisition and analysis of data; Dr Huang conducted the acquisition and interpretation of data; and Dr Cheng performed the acquisition of data. All authors provided final approval on the manuscript that was submitted. METHODS: Study subjects were identified from a nationwide cohort of 1 537 843 children aged 0 to 5 years from 1996 to 2000. They were assigned to the VPS group (n ⫽ 675), who received VPS, or a control group (n ⫽ 6704) of age- and gender-matched children. Both groups (N ⫽ 7379) were followed up for 8 years for IH. Kaplan-Meier and Cox regression analyses were performed. The views in this article are those of the authors. The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, the Department of Health, or National Health Research Institutes. RESULTS: After the 8-year follow-up, 353 of the 7379 study subjects (78 from the VPS group and 275 from the control group) underwent IH surgery. The 8-year cumulative incidence rate of IH-repair surgery was 13.3% in the VPS group, significantly higher than that in the control group (4.1%; P ⬍ .001). Children in the VPS group were more likely to develop IH than the control group (hazard ratio: 3.62; P ⬍ .001), even after adjusting for age, gender, and comorbidities (adjusted hazard ratio: 6.63; P ⬍ .001). The average time interval between VPS and IH surgery was 1.73 years earlier in the VPS group than those in the control group (1.29 vs 3.02 years; P ⬍ .001). www.pediatrics.org/cgi/doi/10.1542/peds.2010-3906 doi:10.1542/peds.2010-3906 Accepted for publication Mar 18, 2011 Address correspondence to Jau-Ching Wu, MD, Department of Neurosurgery, Neurological Institute, Taipei Veterans General Hospital, Room 509, 17F, No 201, Shih-Pai Road, Sec 2, Beitou, Taipei 11217, Taiwan. E-mail: jauching@gmail.com PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2011 by the American Academy of Pediatrics FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose. PEDIATRICS Volume 128, Number 1, July 2011 CONCLUSIONS: Children who received a VPS when younger than 5 years were more likely to have IH; the highest risk was during the first 2 years after VPS surgery. A high index of suspicion for inguinal manifestations is recommended during their follow-up. Pediatrics 2011;128: e121–e126 Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e121 Hydrocephalus is a common disease in pediatric neurosurgery. It can be associated with various diseases of the central nervous system (CNS), including hemorrhage, infection, congenital malformations, spinal dysraphism, and neoplasm. Despite its diverse etiology, hydrocephalus shares a common pathology of a mismatched production and absorption of cerebrospinal fluid (CSF). Thus, the treatments of choice are CSF diversion shunts, such as an internal shunt; endoscopic third ventriculostomy; or an external shunt (ventriculoperitoneal shunt [VPS]). In the past decades, there has been tremendous effort to lower the complication rate and extend the survival of these shunts.1,2 Currently, a VPS is the most widely used. Little attention is given to the extracranial complications of VPS insertion in children.3 There are case reports implying the association between a VPS and inguinal complications, such as hernia, hydrocele, catheter migrations into the scrotum, and implantation of glial cells in the hernial sac.4–11 These inguinal complications after VPS surgery are assumed to be related to increased intraabdominal pressure caused by the diverted CSF during the progress of closure of the processus vaginalis in early childhood.12–14 In the entire English literature, only 3 studies have associated VPS placement in children with a higher incidence of inguinal hernia (IH).14–16 However, these previous reports use institution-based data and are of relatively small numbers. Therefore, the true incidence and association between VPS surgery and subsequent IH remain unclear. To ascertain the correlation between IH and VPS surgery in children, a high follow-up rate and a relatively large number of children who underwent VPS insertion are both necessary. The National Health Insurance Research Database, provided by the National e122 CHEN et al Health Research Institutes of Taiwan, is a national database containing 26 million administered insurants accumulated from January 1996 to December 2008. It covers almost the entire country, or ⬎99% of the population. This study used a nationwide longitudinal cohort, the National Health Insurance Research Database, which uniquely provides an investigation across institutions for both IH and VPS surgery in children to determine their association. METHODS Data Source After the deidentification and encryption processes, the National Health Research Institutes recompiled medical claims and made them publically available for researchers in Taiwan. To protect privacy, individual and hospital identifiers were unique to the research database and could not be used to trace each individual patient or health service provider. This study was exempted from full institutional review board review because of the deidentified feature of the National Health Insurance Research Database. The Bureau of National Health Insurance performed cross-checking and validation on medical charts and claims to ensure the accuracy of diagnosis coding of the National Health Insurance Research Database. Study Cohort The flow of data processing in this retrospective cohort is summarized in Fig 1. During the 5-year enrollment period (January 1, 1996, to December 31, 2000), 1 537 843 children born were entered as the study cohort of preschool-aged (0- to 5-year-old) children. Identification of the VPS and Control Groups From the study cohort, patients hospitalized with a discharge summary of first-time containing the International Classification of Disease, Ninth Revision (ICD-9) procedure code of VPS (02.34) during the enrollment period were identified as patients with a newly inserted VPS (n ⫽ 696) during the specific admission. The date of the VPS surgery was designated as the first date of each patient’s Preschool-aged cohort: population born between 1/1/1996 to 12/31/2000 (N = 1 537 843) Systematic sampling Preschool-aged cohort received VPS procedure during 1/1/1996 to 12/31/2000 (n = 696) Sampled preschool-aged cohort unexposed to VPS procedure (n = 63 330) Age and gender matching (1:10) Exclude: (n = 21) Any hernia repair before VPS procedure Age- and gender-matched controls (n = 6750) Exclude: (n = 46) Any hernia repair before index date VPS group (n = 675) Comparison group (n = 6704) FIGURE 1 Processing flow of the cohort. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES specific hospitalization. IH-repair surgery was determined by the outpatient or hospitalization records with procedure codes of IH repair (ICD-9 procedure code 53.0 –1). The 21 patients who received any hernia repair surgery (ICD-9 53.X) before their VPS events were excluded. Therefore, the VPS group comprised 675 children younger than 5 years old who received a VPS (n ⫽ 675). A comparison control group was randomly extracted from the remainder of the original cohort. This group comprised 1 to 10 age-and gendermatched controls for every patient in the VPS group. An index date was designated as its matched case’s VPS surgery date. After excluding patients who received IH-repair surgery before their index date (n ⫽ 46), the control group had 6704 age- and gender-matched children (Fig 1). Determination of IH Surgery and Covariates All patients in both groups were followed-up for 8 years. IH surgery was determined by the outpatient or hospitalization records. Comorbidities, including hereditary diseases of the CNS (ICD-9 330 –331, 332.0, 333–337, and 340), congenital anomalies of the nervous system (ICD-9 740.0 –2, 741.00 –3, 741.90 –3, 742.0 – 4, 742.51, 742.53, 742.59, and 742.8 –9), intracranial injury (800 – 804 and 850 – 854), malignant neoplasm of the brain and other nervous system (ICD-9 191–192), cerebrovascular diseases (ICD-9 430 – 438), CNS infections (ICD-9 003.21, 036.0 –1, 045– 049, 052.0, 053.0, 054.3, 054.72, 055.0, 056.01, 062– 064, 066.2, 072.1–2, 100.81, 112.83, 114.2, 115.01, 115.11, 115.91, 130.0, 138, 139.0, 320 –324, 326, and V12.02), and disorders related to short gestation, low birth weight, and fetal malnutrition (ICD-9 764.0 –2, 764.9, 765.0 –2, and V21.30 –5) were obtained from discharge codes of hospiPEDIATRICS Volume 128, Number 1, July 2011 tal records from birth date to date of IH repair or the end of follow-up. Statistical Analysis All the data were linked by using SQL server 2008 (Microsoft Corp, Redmond, WA) and analyzed by using SPSS software (SPSS Inc, Chicago, IL). 2 and independent t tests were used to assess differences in age, gender, and comorbidities between the VPS and control groups. The Kaplan-Meier method and log-rank test were used to estimate and compare the 8-year incidence rates of IH-repair surgery after VPS. The Cox proportional hazard model was used to compare the incidence rate of IH-repair surgery between the groups after adjustment for the covariates. A 2-tailed level of .05 was considered statistically significant. RESULTS The mean (SD) age of the VPS group (index date) was 6.37 (8.33) months. A total of 353 children received IH surgery at the mean age of 3.1 (2.2) years. Among them, 78 were from the VPS group and 275 were from the control group. By proportion, 11.6% of children in the VPS group and 4.1% of those in the control group received IH surgery during follow-up. The mean time interval between the VPS date (index date) and the IH surgery was 2.63 (2.11) years. Comparison of Comorbidities Children in the VPS group had significantly more comorbidities than the control group, including hereditary diseases of the CNS, congenital anomalies of the nervous system, intracranial injury, malignant neoplasm of the brain and other nervous system, cerebrovascular diseases, CNS infections, and disorders related to short gestation, low birth weight, and fetal malnutrition (P ⬍ .05; Table 1). These comorbidities were the most commonly identified diagnoses that were likely associated with the etiologies of hydrocephalus requiring the VPS or related to the IH. Incidence of IH and Hazard Ratios During the 8-year study, the average incidence rate of IH-repair surgery was 13.3% in the VPS group, significantly higher than that in the control group (4.1%; log-rank test, P ⬍ .001). This finding suggests that children in the VPS group were more likely to develop an IH than those in the control group (hazard ratio [HR]: 3.62; P ⬍ .001). After adjustments for age, gender, and the aforementioned comorbidities, children in the VPS group were still more likely to develop an IH than those in the control group (adjusted HR: 6.63; P ⬍ .001; Table 2). The incidence rate of IH had a feature of time dependence during the follow-up period. The stratified HRs, by the follow-up time and with adjustments for age, gender, and comorbidities, were different in each period of time (Table 3). The risk for IH surgery in the VPS group was at least 11-fold higher than that of the control group during the first 2 years after VPS (firstyear adjusted HR: 19.67 [95% CI: 9.89 – 39.12]; P ⬍ .001; second-year adjusted HR: 11.36 [95% CI: 4.22–30.54]; P ⬍ .001). After 2 years, this risk was similar in both groups (adjusted HR after the third year of follow-up was not significantly different). As such, in the control group, the cumulative incidence rate of IH increased in a steady rate all the way to the end of this cohort, whereas in the VPS group, the cumulative incidence rate of the IH increased at a more rapid rate (steeper slope; Fig 2) in the first 2 years after the VPS operation. After 2 years, this increase slowed down, turning into a more gradual slope, and became parallel to that of the control group afterward (Fig 2). Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e123 TABLE 1 Demographic Characteristics and Comorbidities of the VPS and Control Groups (N ⫽ 7379) Control Group/ No VPS (N ⫽ 6704) n Demographic factors Gender Male Female Ageb Neonates Infants Toddlers Preschool-aged Comorbidities Hereditary diseases of the CNS Yes No Congenital anomalies of the nervous system Yes No Intracranial injury Yes No Malignant neoplasm of the brain and other nervous system Yes No Cerebrovascular disease Yes No CNS infection Yes No Disorders related to short gestation, low birth weight, and fetal growth retardation Yes No % Pa VPS Group (N ⫽ 675) n % DISCUSSION .9578 3841 2863 57.3 42.7 388 287 57.5 42.5 1718 4089 809 88 25.6 61.0 12.1 1.3 175 409 82 9 25.9 60.6 12.1 1.3 38 6666 0.6 99.4 491 184 72.7 27.3 25 6679 0.4 99.6 362 313 53.6 46.4 662 6042 9.9 90.1 161 514 23.9 76.1 .9971 ⬍.001 ⬍.001 ⬍.001 ⬍.001 13 6691 0.2 99.8 44 631 6.5 93.5 28 6676 0.4 99.6 206 469 30.5 69.5 140 6564 2.1 97.9 219 456 32.4 67.6 ⬍.001 ⬍.001 ⬍.001 184 6520 2.7 97.3 187 488 27.7 72.3 2 test. Neonate, newborn up to first 28 days of life; infant, neonatal period up to 12 months; toddler, 1 to 2 years old; preschoolaged, 3 to 5 years old. a b TABLE 2 Crude and Adjusted HRs for IH Repair During the 8-Year Follow-up Period Among Preschool-Aged Patients With a VPS, 1996 –2000 (N ⫽ 7379) 8-y follow-up period, n (%) Yes No Crude HR (95% CI) Adjusted HR (95% CI)b Total Sample Control Group (No VPS) VPS Group 353 (4.8) 7026 (95.2) — — 275 (4.1) 6429 (95.9) 1.00 1.00 78 (11.6) 597 (88.4) 3.62 (2.81–4.65)a 6.63 (3.96–11.09)a P ⬍ .001. Adjustments were made for the patients’ age, gender, hereditary diseases of the CNS, congenital anomalies of the nervous system, intracranial injury, malignant neoplasm of the brain and other nervous system, cerebrovascular disease, CNS infection, and disorders related to short gestation, low birth weight, and fetal growth retardation. a b Timing of IH Surgery The VPS group received IH surgery earlier than the control group. The mean age on receiving IH surgery in the VPS e124 CHEN et al surgery in the VPS group was 1.73 years shorter than that in the control group (mean: 1.29 vs 3.02 years; t test, P ⬍ .001). group was significantly younger by 1.75 years than that of the control group (1.71 vs 3.46 years; t test, P ⬍ .001). The average time interval to IH This study used a nationwide database to recruit a cohort of children younger than 5 years of age, who numbered ⬎1.5 million. A group of 675 children who had VPS surgery was then extracted, together with 6704 age- and gender-matched children as the control group to make a 1 to 10 comparison. After 8 years of follow-up, children with a VPS were significantly more likely to develop an IH (Table 2) than the controls. The correlation between VPS in children and subsequent IH is shown by this cohort study. In the literature, children who receive a VPS are postulated to have a higher risk of subsequent IH-repair surgery. Few single-institution observational studies report an increased rate of IH after VPS placement in children, ranging from 10% to 30%.12,14–16 Grosfeld and Cooney12 first reported the correlation of the development of IH after VPS surgery in children in 1974. A study of 134 patients by Moazam et al16 demonstrated a similar correlation later in 1984. Clarnette et al14 reported a 15% rate of developing IH after VPS insertion in 430 children in 1998, whereas Celik et al15 reported 23.8% of 88 children developed clinical inguinal manifestations after VPS surgery in 2005. Compared with the present study, these studies had smaller patient numbers, shorter follow-up durations, and lower follow-up rates, and were all single-institution based. Nonetheless, their findings are comparable and are the bases for the rationale of the present study. Our study further corroborates the association between VPS and subsequent IH-repair surgery via a cross-institutional, large number, and controlled longitudinal cohort. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES TABLE 3 HRs of Subsequent IH-Repair Surgery at Different Time Points During the 8-Year Follow-up Period in Preschool-Aged Patients With VPS, 1996 –2000 (N ⫽ 7379) Follow-up Time Point (Years After VPS Surgery) Adjusted HR (95% CI)a P First year (0–1) Second year (1–2) Third year (2–3) Fourth year (3–4) Eighth year (4–8) 19.67 (9.89–39.12) 11.36 (4.22–30.54) 0.34 (0.02–5.06) 0.75 (0.06–10.34) 0.48 (0.07–3.25) ⬍.001 ⬍.001 .440 .835 .455 a Adjustments were made for the patients’ age, gender, hereditary diseases of the CNS, congenital anomalies of the nervous system, intracranial injury, malignant neoplasm of the brain and other nervous system, cerebrovascular disease, CNS infection, and disorders related to short gestation, low birth weight, and fetal growth retardation. FIGURE 2 Results of the Kaplan-Meier analysis.a P ⬍ .001. The time interval from VPS insertion to IH development in children is a very clinically relevant issue for parents and pediatricians but is seldom reported. It is reportedly 5.3 months for notice of clinical inguinal manifestation from the experience of by Celik et al15 in 21 patients. The average time interval in the current study was ⬃1.29 years. Furthermore, this study demonstrated for the first time that the incidence rate of IH after VPS surgery in children may change because it is time dependent (Fig 2). The risk of IH development in children after VPS insertion was more than 10 times higher than that of the control group during the first 2 years but became similar afterward. This implies that the PEDIATRICS Volume 128, Number 1, July 2011 adverse effect of the VPS on IH has a duration of ⬃2 years. Such findings are valuable when consulting family and general physicians for care of these children who receive shunts. This study has several strengths. First, the nationwide database, provided by a monopolistic health insurance system operated by the government, permitted the extremely high follow-up rate attained. Because the universal insurance system covers 99% of the population and health care providers, the chance of loss to follow-up is very low and only exists if they discontinue citizenship. Theoretically, all subsequent IH surgery can be identified even if performed in different hospitals, which is not uncommon for these pediatric patients. Thus, the rate of follow-up in our study is higher than those of previously reported institution-based studies.12,14–16 Second, the control group of age- and gender-matched children (n ⫽ 6684) are also very comparable in terms of ethnicity, geographic location, and access to health care. Because age and gender are important factors of IH, the 1-to-10 matchup makes the comparison distinct and with enhanced statistical power. These 2 features make the present investigation on such an issue authentic. However, the study also has several limitations. First, the VPS group is composed of children with more congenital anomalies or prematurity, which is evident from the comorbidity comparison (Table 1). These congenital anomalies, and prematurity itself, can substantially predispose children for IH later in childhood.17–19 Adjustments by using the Cox proportional hazard model have been used to address this inherent issue. Second, a detailed operative note review, both of the VPS insertion or the IH repair, was not conducted in this study. Types of shunting catheters, including pressure-valve selection, and the severity of hydrocephalus were not taken into account. These factors may exert influences on intraabdominal pressure and may possibly affect the development of IH. All of these intraoperative findings and postoperative complications, such as shunt malfunction and infection, were not analyzed. The anatomic classification of IH, although assumed to be almost all indirect type,18 was also not considered. Third, the time of IH-repair surgery, instead of that of diagnosis, is regarded as the proxy for the development of IH. Therefore, the actual time interval between VPS and IH surgery may be shorter than the results here. However, due to the characteristic easy ac- Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e125 cess to health care services in Taiwan, especially for children, long treatment delay is not expected.20,21 Fourth, those children who had an abdominal operation for the VPS might be under increased scrutiny by family and caregivers, and a hernia is therefore more apt to be detected and perhaps treated. The definite cause of increased risk of IH after VPS insertion in children is unclear. However, it is inferred by several reports to be due to increased intraabdominal pressure.12,14,15 Our study used a cohort study design with the fitted multivariate Cox regression model to demonstrate a cause-and-effect relationship between VPS surgery and IH, which seems supportive to the hypothesis. But the high incidence rate of pre- vious IH in the VPS group (incidence rate of VPS versus comparison: 3.0% vs 0.7%; 2 test, P ⬍ .001) may challenge the hypothesis and deserves additional analysis. Furthermore, the absorptive capacity of the peritoneal cavity for diverted CSF has not been quantified and may be compromised by other comorbidities such as prematurity. It is unknown whether it is the excessive amount of CSF resulting in increased peritoneal pressure or the irritation of the fluid content itself that causes IH development. The anatomic differences between boys and girls can also make for disparate vulnerabilities to IH after VPS surgery.14 However, these issues are beyond the scope of this study and require future investigations. CONCLUSIONS Children receiving a VPS who are younger than 5 years of age were more likely to have IH. The risk was highest during the first 2 years after VPS surgery. There should be a high index of suspicion for inguinal manifestations when following-up children after they receive a VPS. ACKNOWLEDGMENTS This study was based partly on data from the National Health Research Institutes database provided by the Bureau of National Health Insurance, the Department of Health, and managed by the National Health Research Institutes in Taiwan. REFERENCES 1. Drake JM. The surgical management of pediatric hydrocephalus. Neurosurgery. 2008; (suppl 2):633– 640; discussion 640 – 642 2. Stein SC, Guo W. Have we made progress in preventing shunt failure? A critical analysis. J Neurosurg Pediatr. 2008;(1):40 – 47 3. Murtagh FR, Quencer RM, Poole CA. Extracranial complications of cerebrospinal fluid shunt function in childhood hydrocephalus. AJR Am J Roentgenol. 1980; 135(4):763–766 4. Scherzer AL. Letter: hydrocele following placement of a ventriculoperitoneal shunt. J Pediatr. 1975;86(5):811 5. Stahl TJ, Snyder CL, Leonard AS. Giant inguinal hernia in a 5-year-old boy with hydrocephalus: a case report. J Pediatr Surg. 1989; 24(11):1198 –1200 6. Ozveren MF, Kazez A, Cetin H, Ziyal IM. Migration of the abdominal catheter of a ventriculoperitoneal shunt into the scrotum— case report. Neurol Med Chir (Tokyo). 1999;39(4): 313–315 7. Guillén A, Costa JM, Castelló I, Claramunt E, Cardona E. Unusual abdominal complication of ventriculoperitoneal shunt [in Spanish]. Neurocirugia (Astur). 2002;13(5): 401– 404 8. Assencio-Ferreira VJ. Complication of ven- e126 CHEN et al 9. 10. 11. 12. 13. 14. triculoperitoneal shunting: inguinal hernia with scrotal migration of catheter [in Portuguese]. Arq Neuropsiquiatr. 2003;61(4): 1072–1073; author reply 1073 Henriques JG, Pinho AS, Pianetti G. Complication of ventriculoperitoneal shunting: inguinal hernia with scrotal migration of catheter. Case report [in Portuguese]. Arq Neuropsiquiatr. 2003;61(2B):486 – 489 Yuksel KZ, Senoglu M, Yuksel M, Ozkan KU. Hydrocele of the canal of Nuck as a result of a rare ventriculoperitoneal shunt complication. Pediatr Neurosurg. 2006;42(3): 193–196 Magee JF, Barker NE, Blair GK, Steinbok P. Inguinal herniation with glial implants: possible complication of ventriculoperitoneal shunting. Pediatr Pathol Lab Med. 1996; 16(4):591–596 Grosfeld JL, Cooney DR. Inguinal hernia after ventriculoperitoneal shunt for hydrocephalus. J Pediatr Surg. 1974;9(3):311–315 Grosfeld JL, Cooney DR, Smith J, Campbell RL. Intra-abdominal complications following ventriculoperitoneal shunt procedures. Pediatrics. 1974;54(6):791–796 Clarnette TD, Lam SK, Hutson JM. Ventriculoperitoneal shunts in children reveal the natural history of closure of the processus vaginalis. J Pediatr Surg. 1998;33(3): 413– 416 15. Celik A, Ergün O, Arda MS, Yurtseven T, Erşahin Y, Balik E. The incidence of inguinal complications after ventriculoperitoneal shunt for hydrocephalus. Childs Nerv Syst. 2005;21(1):44 – 47 16. Moazam F, Glenn JD, Kaplan BJ, Talbert JL, Mickle JP. Inguinal hernias after ventriculoperitoneal shunt procedures in pediatric patients. Surg Gynecol Obstet. 1984;159(6): 570 –572 17. Zamakhshardy M, Ein A, Ein SH, Wales PW. Predictors of metachronous inguinal hernias in children. Pediatr Surg Int. 2009; 25(1):69 –71 18. Brandt ML. Pediatric hernias. Surg Clin North Am. 2008;88(1):27– 43, vii–viii 19. Kapur P, Caty MG, Glick PL. Pediatric hernias and hydroceles. Pediatr Clin North Am. 1998;45(4):773–789 20. Rachel Lu JF, Chiang TL. Evolution of Taiwan’s health care system. Health Econ Policy Law. 2011;6(1):85–107 21. Lee YC, Huang YT, Tsai YW, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225 Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 Correlation Between Ventriculoperitoneal Shunts and Inguinal Hernias in Children: An 8-Year Follow-up Yu-Chun Chen, Jau-Ching Wu, Laura Liu, Tzeng-Ji Chen, Wen-Cheng Huang and Henrich Cheng Pediatrics 2011;128;e121; originally published online June 20, 2011; DOI: 10.1542/peds.2010-3906 Updated Information & Services including high resolution figures, can be found at: http://pediatrics.aappublications.org/content/128/1/e121.full.h tml References This article cites 19 articles, 1 of which can be accessed free at: http://pediatrics.aappublications.org/content/128/1/e121.full.h tml#ref-list-1 Subspecialty Collections This article, along with others on similar topics, appears in the following collection(s): Neurological Surgery http://pediatrics.aappublications.org/cgi/collection/neurologic al_surgery_sub Surgery http://pediatrics.aappublications.org/cgi/collection/surgery_su b Permissions & Licensing Information about reproducing this article in parts (figures, tables) or in its entirety can be found online at: http://pediatrics.aappublications.org/site/misc/Permissions.xht ml Reprints Information about ordering reprints can be found online: http://pediatrics.aappublications.org/site/misc/reprints.xhtml PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly publication, it has been published continuously since 1948. PEDIATRICS is owned, published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2011 by the American Academy of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014
© Copyright 2025