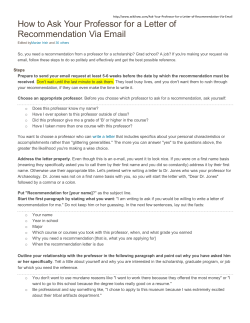
Document 63292
Schwerpunkt English Version of "Das Fibromyalgiesyndrom. Definition, Klassifikation, klinische Diagnose und Prognose". DOI 10.1007/s00482-012-1169-x © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 AWMF-Register Nr. 041/004 W. Eich1 · W. Häuser2 · B. Arnold3 · W. Jäckel4 · M. Offenbächer5 · F. Petzke6 · M. Schiltenwolf7 · M. Settan8 · C. Sommer9 · T. Tölle10 · N. Üçeyler9 · P. Henningsen11 1 Department of Internal Medicine II (General Internal and Psychosomatic Medicine), Heidelberg University Hospital, Heidelberg 2 Internal Medicine 1, Saarbrücken Hospital, Saarbrücken 3 Pain Therapy Department, Dachau Hospital, Dachau 4 Quality Management and Social Medicine Department, Freiburg University Hospital, Freiburg im Breisgau 5 GRP - Generation Research Program, Human Science Center, LudwigMaximilians-University Munich, Bad Tölz 6 Pain and Outpatient Clinic, Göttingen University Medicine, Göttingen 7 Conservative Orthopedia, Orthopedic University Hospital, Heidelberg 8 German Fibromyalgia Association, Bad Seckach 9 Neurology Hospital, University Hospital Würzburg 10 Neurology Hospital, Technical University Munich 11 Clinic and Policlinic for Psychosomatic Medicine, Psychotherapy and Psychological Medicine, Klinikum rechts der Isar, Technical University Munich Fibromyalgia syndrome Definition, classification, clinical diagnosis and prognosis Das Fibromyalgiesyndrom. Background and questions The fibromyalgia syndrome (FMS), its definition, classification and diagnosis among various medical associations, doctors, psychologists and patients is controversial [61]. The definition, classification and diagnosis of chronic pain in multiple areas of the body (chronic widespread pain, CWP) has been partially determined by the political claims of professional medical societies and the pension rights of the patients. The working group focused on the following key questions: 1.What are the core symptoms of FMS? 2.What differences and overlapping symptoms exist between FMS and somatoform and depressive disorders? 3.What criteria should be used to diagnose FMS? 4.What exclusion diagnostics are necessary? 5.When are professional psychotherapeutic diagnostics meaningful? 6.Are there different courses and severities of FMS? 7.What is the prognosis (including life expectancy) of patients with FMS? Materials and methods The parameters of the literature search and analysis and the preparation of the recommendations are described in the article “Methodological fundamentals used in developing the guideline”. Results Preliminary remarks The following findings apply to adults. For the definition, classification, clinical diagnosis and prognosis of chronic pain in multiple areas of the body in children and adolescents, see the article titled “Definition, diagnosis and treatment therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. Key recommendations are italicized. Definition of chronic pain in multiple areas of the body Consensus-based statement Definition of chronic widespread pain (CWP): CWP can be defined according to the American College of Rheumatology (ACR) 1990 criteria and the modified provisional ACR 2010 criteria. EL 5, strong consensus Comment. Pain can be categorized according to clinical criteria into monolocular pain (e.g., in one part of the body), regional pain (e.g., in one specific area of the body, such as the shoulder or arm) and pain in multiple areas of the body. Population-based studies have shown that most people with musculoskeletal pain have more than one pain location [18, 45]. The ACR classification criteria from 1990 defines CWP in multiple body regions [58] as pain >3 months of continuous pain in the following areas: Faxial skeleton (i.e., cervical spine, anterior chest, thoracic or lumbar spine) and Fright and left halves of the body and Fabove and below the waist. Widespread pain may also be an indication of at least 7–19 of the predefined types of pain described in the Widespread Pain Index (WPI; modified preliminary ACR 2010 criteria [20, 64]). Der Schmerz 3 · 2012 | 1 Schwerpunkt Widespread pain can have specific causes (e.g., inflammatory rheumatic disease and diffuse bone metastases). In most patients affected with CWP, there are no specific causes of somatic disease [45]. Definition of FMS Evidence-based statement FMS was defined in the ACR 1990 classification criteria by CWP and painful pressure in at least 11 out of 18tender points. EL 2b, strong consensus Comment. People with chronic pain, sleep disorders and fatigue have been described since biblical times. Smythe [51] provided a historical overview of examples of famous people, such as Florence Nightingale and Charles Darwin, who were “lifelong invalids, yet lived to a ripe old age”. In the rheumatology literature, the symptom complex is known as soft tissue rheumatism or fibrositis. According to Smythe [50], fibrositis has an imprecise symptomatology with multilocular pain and stiffness lasting for more than 3 months with distinctive local hyperalgesia, chronic fatigue and sleep disorders. Additionally, a depressive mood is often involved. The term fibromyalgia was first used by Hench (1976) [25]. In 1990, the ACR defined specific criteria for fibromyalgia that are distinct from inflammatory rheumatic diseases and arthritis. The ACR classification criteria of FMS represents a consensus definition based on clinicians’ descriptions of the clinical picture of the disorder. The combination of the above-mentioned criteria distinguished patients with primary (no organic disease) and secondary (co-morbidity inflammatory rheumatic disease) fibromyalgia from control patients with inflammatory rheumatic diseases and regional pain syndromes (e.g., osteoarthritis) with a sensitivity of 88% and a specificity of 81% [58]. These classification criteria were not conceptualized by the ACR authors as diagnostic criteria [61]. Symptom complex of FMS Evidence-based statement People with CWP are described in population-based studies and are present 2 | Der Schmerz 3 · 2012 in facilities that treat all of the stages of clinical care. Widespread pain is associated with other physical and mental complaints. EL 2b, strong consensus Comment. Patients with CWP differ from patients with local and regional pain syndromes that are caused by an increase in the severity of physical and mental symptoms (distress). According to the ACR 1990 criteria, patients with CWP and FMS are different from patients with CWP without FMS because their physical and mental symptoms are more severe [7, 19, 56], and their tender points are markers of distress [60]. In a representative German population sample of 2,504 individuals in 2009, an asymptotic distribution of pain locations and physical and mental complaints were described. In a cluster analysis, four groups of individuals were identified: pain-free individuals without physical or mental discomfort (“healthy cluster”), individuals with oligolocular pain and mild physical or psychological symptoms (“regional pain cluster”), individuals with widespread pain, mild physical pain symptoms and no mental discomfort (“CWP cluster”) and individuals with widespread pain and severe physical and mental symptoms (“FMS cluster”) [19]. On the basis of a continuum representing the severity of physical (including the number of pain locations) and psychological symptoms, individuals with CWP were located on the outer region of the continuum, and people with FMS were at the end of the continuum [60]. Core symptoms of FMS Evidence-based statement In addition to CWP, the other core symptoms of FMS include sleep disorders (non-restorative sleep) and fatigue or exhaustion (physical or mental). EL 3b, strong consensus Comment. All of the members of a German FMS self-help organization reported numerous physical and mental complaints as a result of a symptom questionnaire developed by the organization. The primary symptoms (in >97% of those affected) were muscle pain in various loca- tions, back pain, fatigue, joint pain in various locations, poor sleep quality, morning stiffness, exhaustion in the morning, weak concentration, lack of stimulation, reduced performance and forgetfulness [16]. These complaints were also indicated as the most common by patients with FMS from various German clinical facilities who were diagnosed based on the ACR 1990 classification criteria [17], patients with FMS who were diagnosed based on the clinical criteria from the United States (US) database for rheumatic diseases [63] and patient and expert consensuses on the “key domains of FMS” [41]. Classification of FMS as a functional somatic syndrome Consensus-based statement FMS can be classified as a functional somatic syndrome. EL 5, majority Comment. Functional somatic syndromes are defined by a clinical complex of physical symptoms, a defined time period and the absence of the causative somatic disease factors that explain the symptoms (e.g., structural tissue damage, biochemical disorder or specific laboratory findings). The individual medical societies define functional somatic syndromes associated with their respective symptoms and do not consider additional physical and mental complaints [40] associated with other disciplines in the definition. Fibromyalgia is described in the International Classification of Diseases in the German version of the World Health Organization (WHO) in the chapter titled “Diseases of the musculoskeletal system and connective tissue” and the subsection titled “Other soft tissue diseases not classified elsewhere” (M79.70) [8]. Definition/overlap of FMS with persistent somatoform pain disorder (F45.40) and chronic pain disorder with psychological and somatic factors (F45.41) Evidence-based statement The criteria for FMS (ICD-10 M79.70), persistent somatoform pain disorder (F45.40) and chronic pain disorder with psychological and somatic factors Abstract · Zusammenfassung (F45.41) overlap and include different clinical characteristics in individuals with CWP without specific somatic disease factors. FMS is not synonymous with a persistent somatoform pain disorder or a chronic pain disorder with psychological and somatic factors. EL 3a, strong consensus Comment. The International Classification of Diseases published by the WHO includes the possibility of classifying chronic physical discomfort without somatic disease factors in the chapters on somatic diseases and in the chapter titled “Psychological and behavioral disorders” under somatoform disorders (F45). As a result, patients in Germany with fibromyalgia-like symptoms are not coded as M79.70 but as a persistent somatoform pain disorder (F45.40) or somatization disorder (F45.1) by many doctors and psychologists. There is an intensive debate regarding the classification of physical ailments without somatic disease factors in the latest revision of the International Classification of Diseases [32]. The following are the opposing positions: Felimination of the somatoform disorder diagnostic category and classification of physical complaints without somatic disease factors only for physical diseases [33] and Fpreservation of the somatoform disorder category in the “Psychological and behavioral disorders” chapter with clarification of the criteria [37]. Persistent somatoform pain disorders are not clearly defined by the ICD-10 criteria. The diagnostic criteria of persistent somatoform pain disorders are not listed with respect to the primary criteria of a somatoform disorder that must be met for accurate classification and how many criteria must be met. Overall criteria for somatoform disorders: FMedical findings do not explain the type and the extent of the symptoms or the suffering or emotional involvement of the patient (e.g., a discrepancy between how the patient feels and the medical findings). Schmerz 2012 · DOI 10.1007/s00482-012-1169-x © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 W. Eich · W. Häuser · B. Arnold · W. Jäckel · M. Offenbächer · F. Petzke · M. Schiltenwolf · M. Settan · C. Sommer · T. Tölle · N. Üçeyler · P. Henningsen Fibromyalgia syndrome. Definition, classification, clinical diagnosis and prognosis Abstract Background. The updated German S guidelines for managing patients with fibromyalgia syndrome (FMS) published by the Association of the Scientific Medical Societies in Germany (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinäre Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. The clinical diagnosis of FMS should be based on the 1990 American College of Rheumatology (ACR) classification criteria (with the examination of tender points), the modified diagnostic criteria from the ACR 2010 (without the examination of tender points) or the criteria published in the German AWMF guidelines for FMS.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Definition · Classification · Diagnosis, clinical · Guideline Das Fibromyalgiesyndrom. Definition, Klassifikation, klinische Diagnose und Prognose Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center FRepeated presentation of physical symptoms in conjunction with persistent requests for medical examina- for Evidence Based Medicine. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Die klinische Diagnose des FMS kann sowohl nach den Klassifikationskriterien des American College of Rheumatology (ACR) von 1990 (mit Untersuchung der „tender points“) als auch ohne Untersuchung von „tender points“ anhand der modifizierten vorläufigen diagnostischen Kriterien des ACR von 2010 oder der Kriterien der deutschen AWMF-Leitlinie zum Fibromyalgiesyndrom erfolgen. Schlüsselwörter Fibromyalgiesyndrom · Definition · Klassifikation · Klinische Diagnose · Leitlinie tions despite repeated negative results (dysfunctional disease behavior). FPatient resists attempts to discuss the possibility of a psychological cause, Der Schmerz 3 · 2012 | 3 Schwerpunkt even when the beginning and duration of the symptoms are closely related to unpleasant life events, difficulties or conflicts (somatic fixation). FThe understanding reached regarding the physical or psychological cause of the symptoms is often disappointing to the patients and doctors (dysfunctional relationship behavior). FThe attention-seeking (histrionic) behavior of patients, as listed in the “Etiology and pathophysiology of fibromyalgia syndrome” chapter [49], is not sufficiently explained by the physical symptoms of FMS through somatic disease factors. This criterion applies to most FMS patients. No studies were identified demonstrating that patients with FMS took the initiative to request another organic diagnosis by exclusion after they had been diagnosed with FMS. Case studies from clinical facilities [15] and cohort studies by FMS self-help organizations [1] report that the majority of those affected by the question of subjective causes of the disease indicate that both physical and psychological factors are involved. A somatic fixation was determined in these samples in only a few patients with FMS. Studies on dysfunctional patient–physician behavior and attention-seeking relationship behavior in patients with FMS were not found. A multicenter German study evaluating the utilization of medical services showed that only a fraction of patients with FMS had an increased number of medical consultations compared to the entire German population [33]. Criteria for persistent somatoform pain disorder: a)severe excruciating pain >6 months, b)no sufficient evidence obtained from adequately conducted somatic testing to explain the symptoms, c)occurs in conjunction with emotional conflicts or psychosocial problems that are important causal factors due to their severity and d)exclusion of 1psychogenic pain during the course of a depressive disorder or schizophrenia and 4 | Der Schmerz 3 · 2012 1pain due to known or psychophysiological mechanisms, such as muscle tension pain or migraine. Criteria a and b apply to patients with FMS. Criterion c applies to many, but not all, patients with FMS. Case studies from clinical facilities have shown that relevant psychosocial stress was temporally related to the development of or increase in CWP in 60–80% of patients with FMS [15]. Psychosocial stressors are associated with an increased risk of FMS [49]. Regarding criterion d, systematic review articles showed that co-morbid depressive disorders occur in 30–80% of patients with FMS [11]. The psychophysiological mechanisms of pain in FMS are described in the “Pathophysiology” chapter [49]. Longitudinal studies from the Swedish twin register have provided evidence of a common factor using path analysis (determined more by environmental factors than by genetic factors), which can affect both functional somatic disorders (e.g., FMS, irritable bowel syndrome, headaches and chronic fatigue syndrome) and psychological disorders (e.g., depression and generalized anxiety disorder) [28, 29]. A dimensional analysis of the FMS symptom complex based on physical and psychological complaints, psychosocial stressors, availability of medical services and subjective beliefs regarding of the cause of the illness is more appropriate than the categorical classification of FMS as a persistent somatoform pain disorder [24]. The criteria of a chronic pain disorder with somatic and psychological factors (F 45.41) are as follows: pain that is present for at least 6 months in one or more anatomical regions, which originated due to a physiological process or a physical disorder. Although psychological factors play an important role in the severity, exacerbation or continuation of the pain, they are not the direct cause. The pain induces clinically significant distress and impairment in social, occupational or other important functional areas. Pain disorders that are specifically associated with mood, anxiety, somatization or psychotic disorders should not be considered in this context [8]. This diagnostic category can be used for patients with symptoms of CWP that originated due to inflammatory rheumatic disease or arthritis and because the current extent of their pain symptoms (i.e., number of pain sites, impairments) can be explained by psychosocial processes instead of inflammatory processes in cases of remission or mild clinical courses of the inflammatory symptoms. Definition/overlap of FMS with depressive disorders Evidence-based statement FMS can be associated with depressive disorders (EL1b). However, FMS is not to be classified as a depressive disorder. (EL 3a), strong consensus Comment. Population-based and clinical studies reveal an association between CWP, FMS and depressive disorders. However, not every patient with a depressive disorder reports pain, and not every patient with FMS is depressed [43]. The main symptoms of FMS, including pain and fatigue, are also possible symptoms of depressive disorders. Among patients with depressive disorders, 30–60% reported pain [2]. The most common physical symptom in patients with major depression disorders in pharmacological studies was fatigue [53]. Six percent of the patients in these studies reported ≥6 pain localizations [54]. The association rates of multilocular (>2) pain and mood disorders were between 2.8–19.6% in the World Mental Health Survey [13]. In a clinical study, 13% of patients with major depression fulfilled the ACR 1990 criteria for FMS [55]. In a German study, 38% of patients with depressive disorders (F32–34, F43.2) fulfilled the survey criteria for FMS (≥7/19 pain sites and fatigue ≥6/10 using the visual analogue scale) [20]. A subgroup of patients who were diagnosed as depressed also showed fibromyalgia-like symptoms. In a representative sample of the German population in 2009, 12.5% of individuals with FMS met the survey criteria for major depression and 12.5% met the criteria for another depression syndrome, as measured using the depression module of the health questionnaire for patients [18]. A systematic review of clinical studies showed a prevalence rate of 30–70% for depressive disorders in patients with FMS [11]. The symptomatology of a percentage of patients diagnosed with FMS also meets the criteria for depressive disorders (e.g., major or minor depression or atypical depression). Despite a partial overlap in the symptoms and neuroendocrine mechanisms, one review article concluded that major depressive disorders and FMS should not be regarded as variants of the same disease [44]. types (e.g., Down syndrome and Marfan syndrome) [34]. Fibromyalgia versus fibromyalgia syndrome Comment. Because the conditions that define FMS are distributed in the general population and clinical populations within a continuum (see statement “Symptom complex of FMS”), any classification of severity depends on the criteria and thresholds used. There is no generally accepted classification for the degree of severity of functional disorders in general and for FMS in particular. The German Guideline “Non-specific, functional and somatoform physical symptoms” differentiates between mild and severe manifestations ([14], . Tab. 1). In clinical populations of FMS, different clusters of patient groups or severity levels have been distinguished. An increase in physical distress and subjective disturbances were associated with increased drug consumption and physical and mental health comorbidities [6, 48]. In clinical trials, a severity level classification for FMS can be obtained using the Fibromyalgia Impact Questionnaire (FIQ) [46]. Consensus-based statement Because symptomatology is defined by a symptom complex, the term “fibromyalgia syndrome” is more appropriate than the term “fibromyalgia”. EL 5, consensus Comment. Functional somatic syndromes do not exhibit a distinctive clinical picture (such as myocardial infarction). The basis for the definition of functional somatic syndromes is a continuum of complaints. The definition of a disease pattern results from the establishment of a threshold by an expert consensus and/ or by clinical studies. The same approach is used to describe pronounced continuous biological variables, such as the degree of constriction of the coronary vessels and blood sugar levels. The authors are aware that the term “syndrome” is not used consistently in the medical literature. The concept of a syndrome is understood in these guidelines as “the aggregation of symptoms, which by themselves are not characteristic of the disease, to form a characteristic disease pattern”. Other functional somatic syndromes include irritable bowel syndrome or urethra syndrome. FMS is classified as a first-order syndrome or a symptom complex with unknown or unclear etiology, heterogeneous pathogenesis and a defined phenotype (see statement “Core symptoms of FMS”). Second-order syndromes (sequences) are defined by unknown etiologies, homogeneous pathogenesis and defined phenotypes (e.g., Cushing’s syndrome). Thirdorder syndromes are defined by homogeneous etiologies, unknown or insignificant pathogenesis and defined pheno- Progression of FMS Evidence-based statement Different forms of FMS progression with varying severity can be distinguished based on clinical characteristics. However, a generally accepted classification of the degree of severity does not exist. EL 5, strong consensus Case study of a patient with mild FMS: A 37-year-old female patient reported recurring back pain episodes starting at the age of 11 without radiation to other areas. However, the pain began to extend to her entire back and to all of her extremities 2.5 years ago. Since that time, she reported experiencing pain almost every day of the year. However, in the summer months or during vacations to Mediterranean countries, she experienced little or no pain. For 2 years, she experienced a constant pain level, with an average pain intensity of 6/10, ranging from the lowest pain intensity of 2/10 to the maximum pain intensity of 9/10 on an 11-point numerical scale (NRS). Additional physical discom- forts included an increased stiff feeling in her hands and an increased cold sensitivity with no autonomic symptoms. Carrying heavy loads (such as hot boxes) was no longer possible, and the patient could walk but was unable to jog. There were no restrictions on domestic work. The patient had unobtrusive biographical anamnesis. At the time of the case study, the patient was married, had a self-employed husband and did not have any children. She had no current mental complaints or emotional disorders, and there were no reports of psychiatric and psychotherapeutic treatments in her patient history. Case study of a patient with a severe history of FMS: A 54-year-old female patient experienced recurring hip pain as a child and reported recurrent joint and back pain beginning in early adulthood. However, 8 years prior to the case study, the pain expanded to her entire back and to both of her arms and legs. At that time, the patient experienced continuous pain with an average pain intensity of 8/10, with the lowest pain intensity of 7/10 and the maximum pain intensity of 10/10 on the NRS, with no pain-free or low-pain intervals. For approximately 5 years, the patient has experienced mostly non-restorative sleep and increased daytime sleepiness with rapid exhaustion, limited physical or mental stress, increased feelings of stiffness in the hands, increased cold sensitivity, recurrent abdominal pain in alternating locations, an increase in the frequency of feces by 3–10 movements, the imperative and urgent need to urinate and defecate (gastroenterological and urological clarification without pathological findings) and arrhythmia (cardiological investigation without pathological findings and therapy with a β-blocker). She could only do light household chores, such as cooking and putting the dishes away; other domestic duties, including cleaning and laundry, were assumed by a housekeeper or her daughter. She gave up on her painting hobby 1 year ago due to pain in her arms and has been unable to work for the past 2 years but receives steady unemployment benefits. Regarding biographical anamnesis, the patient experienced physical trauma perpetrated by an alcoholic father as a Der Schmerz 3 · 2012 | 5 Schwerpunkt Tab. 1 Clinical characteristics of mild and severe manifestations of fibromyalgia syndrome (transitional, no mandatory criteria) (modified after the AWMF guideline entitled “Non-specific, functional and somatoform physical symptoms” [14]) Criterion Physical symptoms Mild manifestation Predominant musculoskeletal discomfort Duration of physical symptoms Psychological symptoms Subjective disease diagnosis Subjective disturbances (e.g., profession, family and free time) Use of medical services Psychosocial stress Practitioner–patient relationship Severe manifestation Numerous complaints, including musculoskeletal and other organ systems Relapsing, minor or discomfort- Persistent, none or rare low or free intervals discomfort-free intervals Limited Pronounced Appropriate (e.g., dependent Inappropriate (e.g., persistent on stress and temperature) fears of serious disease despite an exclusion diagnosis) Missing or minor High Minor Few and mild stressors (family, profession) Cooperative High (doctor-hopping) Numerous and/or severe stressors (family, profession) “Difficult”, frustrating Tab. 2 Criteria for the clinical diagnosis of FMS ACR 1990 classification criteria [58] Obligate core symptom CWP according to the ACR 1990 criteria (see statement “Definition of chronic pain in multiple areas of the body”) None Diagnostic exclusions None Modified provisional ACR 2010 diagnostic criteria [64] Regional pain index at ≥7/19 pain locations on the regional pain scale AWMF – FMS diagnostic criteria guidelines [21] CWP according to the ACR 1990 criteria (see statement “Definition of chronic pain in multiple areas of the body”) Symptom intensity score ≥5a Fatigue (physical and/or psychological) and sleep disorders and/or nonrestorative sleep and swelling and/or stiffness in the hands and/or feet and/or face Exclusion of a physical illness that would sufficiently explain the typical pattern of symptoms Exclusion of a physical illness that would sufficiently explain the typical pattern of symptoms aSymptom severity score: sum of fatigue, non-restorative sleep and cognitive problems (0: not available to 3: extremely pronounced); headache, abdominal pain and depression (0: absent, 1: present; range of total scores: 0–12). According to the modified ACR 2010 provisional diagnostic criteria, FMS can be diagnosed in 3–6 pain locations on the regional pain scale and can have a symptom severity score ≥9 [64]. However, this diagnostic criterion is incompatible with the primary symptoms of FMS, which include CWP. Regional pain, such as in the neck, upper arm or forearm, may also occur at three pain locations on the regional pain scale. Therefore, the use of this diagnostic criterion is not recommended.The rate of agreement between the 1990 ACR criteria and the diagnostic criteria of the German AWMF guidelines for FMS was 87% [21] in a multicenter study. ACR American College of Rheumatology; AWMF Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften; CWP chronic widespread pain; FMS fibromyalgia syndrome. child and a suicide attempt in her youth. Other stressful life events and psychosocial problems include a drug-addicted daughter who committed suicide and experiences with conflicts in the workplace. 6 | Der Schmerz 3 · 2012 Prevalence of FMS in Germany Evidence-based statement Other obligate symptoms able to drive alone for the past 2 years and can only shop in small stores within the vicinity of her home. The patient has experienced withdrawal from social contacts for 2 years. For the past 3 years, she has been depressed most of the time and has a lack of desire and motivation. She has received outpatient psychiatric treatment for the past 2 years and has taken several unsuccessful psychiatric drug regimens. She has increasing anxiety traceable back to her childhood, such as a fear of the dark and abandonment, and experienced panic attacks and an increase in avoidance behavior at the age of 18. She has not been The prevalence of FMS in Germany is approximately 3.5%. EL 2c, consensus Comment. In a summary of 10 studies representing the general adult population from various countries, the prevalence of FMS was between 0.7% and 3.3%. The prevalence was between 1.0% and 4.9% in women and between 0.0% and 1.6% in men. The female-to-male ratio was between 2–21:1 [12]. In Germany, the prevalence of FMS based on the ACR criteria of 1990 in a population of 35- to 74-year-old women was 5.5% [46]. In a representative sample of the population in Germany, the point prevalence of widespread pain (backache and pain in all four extremities) was 8.6%. The point prevalence of FMS (according to the survey criteria of ≥7/19 pain locations and fatigue of ≥6/10 on the visual analogue scale) was 3.8% [95% confidence interval (95% CI) 3.6–4.0]. The ratio of women to men was 1.2:1 [18]. In a European study (including Germany), the point prevalence of CWP was determined based on the pain criteria from the London Fibromyalgia Epidemiology Study Screening Questionnaire. The point prevalence of FMS was estimated based on the frequency of FMS in rheumatology practices using the CWP criterion from the London Fibromyalgia Epidemiology Study Screening Questionnaire. The point prevalence of CWP in Germany was 11%, and the point prevalence of FMS was 3.2% (95% CI 2.1–4.3). The female-to-male ratio for FMS was 1.6:1 [5]. In clinical settings, the female-to-male ratio is 8–12:1 [21]. The higher prevalence rates among men in recent epidemiolog- Tab. 3 Important differential diagnostics of chronic widespread pain in multiple body regions (modified from [30]) Internal diseases Chronic inflammatory rheumatic disease Chronic hepatitis C Chronic inflammatory bowel disease Celiac disease Osteoporosis Hyper-/hypoparathyroidism Hyper-/hypothyreosis Vitamin D deficiency Neurological diseases Inflammatory myopathy Metabolic myopathy Degenerative myopathy Endocrinal myopathy Myotonia Toxic myalgia Myalgia in rare diseases (e.g., stiff person syndrome) Myalgia by alteration to the central and peripheral nervous system Tab. 4 Painful myopathy triggered by medications and drugs (modified from [4]) Inflammatory myopathy Cimetidine D-Penicillamine Cocaine Levodopa Penicillin Procainamide Sulfonamide Zidovudine Other myopathies ACTH Carbimazole Clofibrate Cromoglycate Cyclosporin Enalapril Ezetimibe HMG-CoA reductase inhibitor Metoprolol Minoxidil Proton pump inhibitor Salbutamol ical studies [5, 18] compared to the rates in clinical institutions can be explained as follows: 1.Not using the tender point criteria for the clinical diagnosis of FMS in epidemiological studies leads to a more frequent diagnosis of FMS in men with CWP because the average pressure pain intensity is lower in men than in women. In the general population [58] and clinical samples, men have fewer pressure-sensitive tender points than women. 2.It is possible that FMS in men with CWP is not diagnosed because FMS is considered a “female sickness” [22]. 3.Women with chronic physical discomforts demand more medical services than men with the same discomforts [14]. Clinical diagnosis Clinical consensus point The clinical diagnosis of FMS can be determined according to the ACR 1990 classification criteria, the symptom-based Myopathy and neuropathy Amiodarone Colchicine Heroin Interferon L-Tryptophan Vincristine criteria of the German FMS S3 guidelines or the current modified ACR 2010 criteria. The clinical diagnosis is based on the anamnesis of a typical symptom complex, clinical examination and the exclusion of physical diseases, which could satisfactorily explain this symptom complex. Strong consensus Comment. Although the ACR 1990 classification criteria for FMS [58] were designed as classification criteria and not as diagnostic criteria, they were subsequently used for diagnosis in daily clinical routines and studies. The use of the tender point examination was criticized due to the lack of acceptance by non-rheumatologists, lack of objectivity in implementation, missing data on the reliability of the results outside of rheumatology settings and the lack of validity [21, 61]. Based on patient surveys, comparisons between patients with arthritis and rheumatoid arthritis and expert consensus [61], the tentative diagnostic criteria for FMS were developed by a group of experts from the ACR. In the modified pre- liminary ACR 2010 criteria, the medical assessment of the physical symptoms was replaced by a patient self-assessment using a questionnaire [64]. In the consensus conference of the German S3 guidelines for FMS [10], the AWMF criteria were developed for the clinical diagnosis of FMS ([21], . Tab. 2). The historically described symptom triad of CWP, fatigue and sleep disorders is a required diagnostic criterion, and these symptoms are considered core symptoms in the diagnosis of FMS. Obligatory somatic diagnosis at the initial evaluation Clinical consensus point If the initial assessment indicates possible CWP, the following measures are recommended: Fcompletion of a sketch of the pain or the regional pain scale by the patient, Ftargeted exploration of other core symptoms, such as fatigue or sleep disorders, Fcomplete medical anamnesis, including drug history, Fcomplete physical examination, including skin, neurological and orthopedic findings Fbasic laboratory tests: 1erythrocyte sedimentation rate, C-reactive protein and full blood count (e.g., polymyalgia rheumatica, rheumatoid arthritis), 1creatine kinase (CK) (e.g., muscular disorders), 1calcium (e.g., hypercalcemia), 1basal thyroid-stimulating hormone (e.g., hypothyroidism), Ffor indications of somatic causes of the symptoms, further diagnostics may be necessary depending on the suspected diagnosis. Strong consensus Comment. CWP and fatigue can be symptoms of several internal and neurological disorders (. Tab. 3, 4). Muscle and joint pain in multiple body regions without evidence of a neuropathy or myopathy can be caused by many drugs. Statins are frequently prescribed, and 10–15% of the patients receiving statin therapy develop myalgia of varying degrees with and withDer Schmerz 3 · 2012 | 7 Schwerpunkt Mortality How often were you affected by the following complaints in the past 2 weeks? Not at all 01 Low interest or pleasure in your activities 02 Depression, melancholy or hopelessness 03 Nervousness, anxiety or tension 04 Not being able to stop or control your worries On a single day On more than half of the days Almost every day 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 Fig. 1 8 PHQ-4: patient health questionnaire out an increase in CK [38]. Arthralgias and myalgias are side effects of aromatase inhibitors [57] and interferons [42]. Additional technical diagnostics Clinical consensus point In a typical symptom complex and the absence of clinical references to internal, orthopedic or neurological diseases (anamnesis and clinical examination without reference to other diseases as causes of pain and fatigue, including unremarkable basic laboratory test results), additional technical diagnostics, such as follow-up laboratory tests, neurophysiology or imaging are not recommended. Strong consensus Comment. A Norwegian longitudinal study in outpatient primary care indicated that radiological examination had a low diagnostic value in patients with CWP [35]. A Canadian study in outpatient primary and secondary care demonstrated that there was no diagnostic value gained from the determination of autoantibodies associated with inflammatory rheumatic diseases in the anamnestic indication of CWP, fatigue and the lack of ankle swelling or references to internal organ diseases [52]. Screening for psychological stress symptoms Clinical consensus point In the initial evaluation of CWP, screening for increased mental workload of symptoms, such as anxiety and depression, is recommended. Strong consensus 8 | Der Schmerz 3 · 2012 Comment. The most common co-morbid mental disorders in FMS are depressive and anxiety disorders [11]. Screening (via a questionnaire or questions from the doctor to the patient) is possible using the German version of the patient health questionnaire (PHQ)-4 [37] (. Fig. 1). Values ≥3 are observed as the limit for possible depressive disorder (questions 1 and 2) or possible generalized anxiety disorder, panic disorder or posttraumatic stress disorder (questions 3 and 4) and correspond to a percentile rank of 93.4% (depression) and 95.2% (fear) relative to a representative German population sample [37]. Professional psychotherapeutic investigation Clinical consensus point A professional psychotherapeutic investigation by a specialist in psychiatry and psychotherapy, psychosomatic medicine, psychotherapy or a medical or psychological psychotherapist is recommended in the following cases: a)indications of increased psychological distress (e.g., anxiety or depression), b)anamnestic information on current severe psychosocial stressors, c)anamnestic information on current or previous psychiatric treatments, d)anamnestic information on serious biographical stress factors, e)maladaptive in coping with disease, f)subjective attributes of mental illness Consensus Evidence-based staement Mortality is not increased in FMS. EL 2b, strong consensus Comment. In a retrospective case control study of 8,186 patients with FMS treated in rheumatology practices (US National Data Bank for Rheumatic Diseases) from 1974–2009, the death rate was not elevated compared to 12,329 patients with osteoarthritis (US National Death Index). The standardized risk of suicide was increased when compared to the US population [odds ratio (OR) 3.3, 95% CI 2.2– 5.1] [65]. In a retrospective cohort study in Denmark, 1,361 patients with FMS were observed from 1984–1999. The mortality risk was not elevated, although the female patients had an increased risk of suicide (OR 10.5, 95% CI 4.5–20.7) [9]. Use of medical services Evidence-based statement FMS causes high direct and indirect medical expenses in Germany in terms of utilization of health care and health benefits, respectively. EL 2b, strong consensus Comment. Only studies from Germany were considered. In “IMS Mediplus”, a database of 900 general medical practices in Germany, the use of outpatient services was compared for 4,983 patients with FMS and 4,983 age- and gender-matched controls from 2/2006–2/2007. Patients with FMS reported twice as many visits to general practitioners, transfers to specialists and sick leave compared to the control patients during the investigation period. The medical expenses for patients with FMS (e.g., doctor visits, medications, inpatient treatments and sick leave) were estimated to be $9,573 compared to $329 for the controls [3]. In a study of the former Barmer health insurance (Barmer Ersatzkasse, BEK) from 1 July 2008 to 30 June 2009 for 19,592 insured individuals (0.3% of the total insured in the population) diagnosed with FMS, the annual direct medical costs were calculated to be 3,160 € (outpatient and inpatient treatment), and the indirect medical costs were 721 € (sick pay). Data from the control group were not reported [39]. Conclusion The validation of the first version of the German S3 guidelines based on clinical consensus and symptom-based diagnostic criteria [22] and the participation of guideline group members toward the development of the modified provisional 2010 ACR diagnostic criteria [64], which provides a diagnosis of FMS without tender point examination, continues the efforts to facilitate the diagnosis of FMS by non-rheumatologists. By comparing the recommendations of the S3 guidelines to “non-specific/functional/somatoform disorders of the body” [24] for diagnostic labeling and treatment of the symptom complex, the working group hopes to end the debate of the classification of CWP without sufficient explanatory somatic disease factors. We hope to focus toward filling in the following research gaps: Fdevelopment of reliable and internationally accepted degrees of severity for non-specific/functional/somatoform physical disorders in general and in FMS patients in particular and Fprospective cohort studies on the importance of secondary disease gain, social factors, such as unemployment and pension loss, iatrogenic chronification and diagnostic labels for patients with FMS. Corresponding address Prof. Dr. W. Eich Department of Internal Medicine II (General Internal and Psychosomatic Medicine), Heidelberg University Hospital Im Neuenheimer Feld 10, 69210 Heidelberg Germany wolfgang.eich@med.uni-heidelberg.de Conflict of interest. See . Tab. 5 in “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Akritidou I, Köllner V, Häuser W (2008) Fibromyalgie – eine Somatisierungsstörung? Ergebnisse der Umfrage der Deutschen Fibromyalgievereinigung zu Begleitsymptomen der Fibromyalgie (Fibromyalgia – a somatic disorder? Results from the survey of the German Fibromyalgia Association on accompanying symptoms of fibromyalgia). Psychother Psychosom Med Psychol 19:113 2. Bair MJ, Robinson RL, Katon W, Kroenke K (2003) Depression and pain comorbidity: a literature review. Arch Intern Med 163:2433–2445 3. Berger A, Dukes E, Martin S, Edelsberg J, Oster G (2007) Characteristics and healthcare costs of patients with fibromyalgia syndrome. Int J Clin Pract 61:1498–508 4. Berghoff C, Bayas A, Gold R et al (2005) Differenzialdiagnose bei Myalgien. Bundeseinheitliche Konsensuspapiere der Neuromuskulären Zentren im Auftrag der Deutschen Gesellschaft für Muskelkranke. V. (DGM) (Differential diagnosis in myalgias. Standard consensus documents of the neuromuscular centers on behalf of the German society for people suffering from muscle disease). Nervenheilkunde 24:709–716 5. Branco JC, Bannwarth B, Failde I et al (2009) Prevalence of fibromyalgia: a survey in five European countries. Semin Arthritis Rheum 39:448–453 6. Calandre EP, Garcia-Carrillo J, Garcia-Leiva JM et al (2011) Subgrouping patients with fibromyalgia according to the results of the fibromyalgia impact questionnaire: a replication study. Rheumatol Int 31:1555–1559 7. Cöster L, Kendall S, Gerdle B et al (2008) Chronic widespread musculoskeletal pain – a comparison of those who meet criteria for fibromyalgia and those who do not. Eur J Pain 12:600–610 8. Deutsches Institut für Medizinische Dokumentation und Information (DIMDI) German Institute for Medical Documentation and Information (DIMDI). ICD 10-GM. Version 2012. International Statistical Classification of diseases and related health problems [Internationale Statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme], 10. Revision – German Modification. http:// www.dimdi.de/static/de/klassi/diagnosen/icd10/ htmlgm2012/. Accessed 20 May 2012 9. Dreyer L, Kendall S, Danneskiold-Samsøe B et al (2010) Mortality in a cohort of Danish patients with fibromyalgia: increased frequency of suicide. Arthritis Rheum 62:3101–3108 10. Eich W, Häuser W, Friedel E et al (2008) Definition, Klassifikation und Diagnose des Fibromyalgiesyndroms (Definition, classification and diagnosis of fibromyalgia syndrome). Schmerz 22:255–266 11. Fietta P, Fietta P, Manganelli P (2007) Fibromyalgia and psychiatric disorders. Acta Biomed 78:88–95 12. Gran JT (2003) The epidemiology of chronic generalized musculoskeletal pain. Best Pract Res Clin Rheumatol 17:547–561 13. Gureje O, Von Korff M, Kola L et al (2008) The relation between multiple pains and mental disorders: results from the World Mental Health Surveys. Pain 135:82–91 14. Hausteiner-Wiehle C, Schäfert R, Sattel H et al (2012) S3-Leitlinie zum Umgang mit Patienten mit nicht-spezifischen, funktionellen und somatoformen Körperbeschwerden (S3 guidelines for the management of patients with non-specific, functional and somatoform symptoms) (in print) 15. Häuser W, Bernardy K, Arnold B (2006) Das Fibromyalgiesyndrom – eine somatoforme Schmerzstörung? (Fibromyalgia syndrome – a somatoform pain disorder?) Schmerz 20:128–39 16. Häuser W, Zimmer C, Felde E, Köllner V (2008) Was sind die Kernsymptome des Fibromyalgiesyndroms? Umfrageergebnisse der Deutschen Fibromyalgievereinigung (What are the core symptoms of fibromyalgia syndrome? Survey results of the German Fibromyalgia Association) Schmerz 22:176–183 17. Häuser W, Akritidou I, Felde E et al (2008) Schritte zu einer symptombasierten Diagnose des Fibromyalgiesyndroms – Beschwerdeprofile von Patienten unterschiedlicher klinischer Kontexte (Steps towards a symptom-based diagnosis of fibromyalgia syndrome – discomfort profiles of patients in different clinical contexts). Z Rheumatol 67:511– 515 18. Häuser W, Schmutzer G, Glaesmer H, Brähler H (2009) Prävalenz und Prädiktoren von Schmerzen in mehreren Körperregionen. Ergebnisse einer repräsentativen deutschen Bevölkerungsstichprobe (Prevalence and predictors of widespread pain. The results of a representative population sample in Germany). Schmerz 23:461–470 19. Häuser W, Schmutzer G, Brähler E, Glaesmer H (2009) A cluster within the continuum of biopsychosocial distress can be labeled “fibromyalgia syndrome”- evidence from a representative German population survey. J Rheumatol 36:2806– 2812 20. Häuser W, Schild S, Kosseva M et al (2010) Validierung der deutschen Version der regionalen Schmerzskala zur Diagnose des Fibromyalgiesyndroms (Validation of the German version of the regional pain scale for the diagnosis of fibromyalgia syndrome). Schmerz 24:226–235 21. Häuser W, Hayo S, Biewer W et al (2010) Diagnosis of fibromyalgia syndrome – a comparison of Association of the Medical Scientific Societies in Germany, survey, and American College of Rheumatology criteria. Clin J Pain 26:505–511 22. Häuser W, Kühn-Becker H, Wilmoswky H von et al (2011) Demographic and clinical features of patients with fibromyalgia syndrome of different settings: a gender comparison. Gend Med 8:116–125 23. Häuser W, Bernardy K, Kopp I (2012) Methodenreport (Methods report). Schmerz 26:232-246 24. Hanel G, Henningsen P, Herzog W et al (2009) Depression, anxiety, and somatoform disorders: vague or distinct categories in primary care? Results from a large cross-sectional study. J Psychosom Res 67:189–197 25. Hench PK, Mitler MM (1986) Fibromyalgia. 1. Review of a common rheumatologic syndrome. Postgrad Med 80:47–56 26. Henningsen P, Zipfel S, Herzog W (2007) Management of functional somatic syndromes. Lancet 369:946–955 27. Kamaleri Y, Natvig B, Ihlebaek CM, Bruusgaard D (2008) Localized or widespread musculoskeletal pain: does it matter? Pain 138:41–46 28. Kato K, Sullivan PF, Evengård B, Pedersen NL (2009) A population-based twin study of functional somatic syndromes. Psychol Med 39:497–505 29. Kato K, Sullivan PF, Pedersen NL (2010) Latent class analysis of functional somatic symptoms in a population-based sample of twins. J Psychosom Res 68:447–453 30. Köllner V, Bernardy K, Sommer C, Häuser W (2009) Diagnosis and therapy of fibromyalgia syndrome. Dtsch Med Wochenschr 134:1163–1174 Der Schmerz 3 · 2012 | 9 Schwerpunkt 31. Kroenke K (2007) Somatoform disorders and recent diagnostic controversies. Psychiatr Clin North Am 30:593–619 32. Kroenke K, Sharpe M, Sykes R (2007) Revising the classification of somatoform disorders: key questions and preliminary recommendations. Psychosomatics 48:277–285 33. Kosseva M, Schild S, Wilhelm-Schwenk M et al (2010) Komorbide depressive Störungen als Mediator der Assoziation von Misshandlungen in Kindheit/Jugend und Fibromyalgiesyndrom (Comorbid depressive disorders as a mediator of the association of mistreatment in childhood/adolescence and fibromyalgia syndrome). Schmerz 24:474–484 34. Leiber B (1990) Die klinischen Syndrome (Clinical syndromes). Urban & Schwarzenberg, Stuttgart 35. Lindgren H, Bergman S (2005) The use and diagnostic yield of radiology in subjects with longstanding musculoskeletal pain – an eight year follow up. BMC Musculoskelet Disord 6:53 36. Löwe B, Mundt C, Herzog W et al (2008) Validity of current somatoform disorder diagnoses: perspectives for classification in DSM-V and ICD-11. Psychopathology 41:4–9 37. Löwe B, Wahl I, Rose M et al (2010) A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 122:86–95 38. Mammen AL, Amato AA (2010) Statin myopathy: a review of recent progress. Curr Opin Rheumatol 22:644–650 39. Marschall U, Arnold B, Häuser W (2011) Treatment and healthcare costs of fibromyalgia syndrome in Germany: analysis of the data of the Barmer health insurance (BEK) from 2008 to 2009. Pain 25:402–404, 406–410 40. Mayou R, Farmer A (2002) ABC of psychological medicine: functional somatic symptoms and syndromes. BMJ 325:265–268 41. Mease PJ, Arnold LM, Crofford LJ et al (2008) Identifying the clinical domains of fibromyalgia: contributions from clinician and patient Delphi exercises. Arthritis Rheum 59:952–960 42. Nikfar S, Rahimi R, Abdollahi M (2010) A meta-analysis of the efficacy and tolerability of interferon-β in multiple sclerosis, overall and by drug and disease type. Clin Ther 32:1871–1888 43. Okifuji A, Turk DC, Sherman JJ (2000) Evaluation of the relationship between depression and fibromyalgia syndrome: why aren’t all patients depressed? J Rheumatol 27:212–219 44. Pae CU, Luyten P, Marks DM (2008) The relationship between fibromyalgia and major depressive disorder: a comprehensive review. Curr Med Res Opin 24:2359–2371 45. Rustøen T, Wahl AK, Hanestad BR et al (2004) Prevalence and characteristics of chronic pain in the general Norwegian population. Eur J Pain 8:555– 565 46. Schaefer C, Chandran A, Hufstader M et al (2011) The comparative burden of mild, moderate and severe Fibromyalgia: results from a cross-sectional survey in the United States. Health Qual Life Outcomes 9:71 47. Schochat T, Raspe H (2003) Elements of fibromyalgia in an open population. Rheumatology (Oxford) 42:829–835 48. Silverman S, Sadosky A, Evans C et al (2010) Toward characterization and definition of fibromyalgia severity. BMC Musculoskelet Disord 11:66 49. Sommer C, Häuser W, Burgmer M et al (2012) Etiology and pathophysiology of fibromyalgia syndrome. Schmerz 26:259-267 10 | Der Schmerz 3 · 2012 50. Smythe H (1986) Tender points: evolution of concepts of the fibrositis/fibromyalgia syndrome. Am J Med 81:2–6 51. Smythe H (1989) Fibrositis syndrome: a historical perspective. J Rheumatol Suppl 19:2–6 52. Suarez-Almazor ME, Gonzalez-Lopez L, Gamez-Nava JI et al (1998) Utilization and predictive value of laboratory tests in patients referred to rheumatologists by primary care physicians. J Rheumatol 25:1980–1985 53. Vaccarino AL, Sills TL, Evans KR, Kalali AH (2009) Multiple pain complaints in patients with major depressive disorder. Psychosom Med 71:159–162 54. Vaccarino AL, Sills TL, Evans KR, Kalali AH (2008) Prevalence and association of somatic symptoms in patients with major depressive disorder. J Affect Disord 110:270–276 55. Vishne T, Fostick L, Silberman A et al (2008) Fibromyalgia among major depression disorder females compared to males. Rheumatol Int 28:831– 836 56. White KP, Nielson WR, Harth M et al (2002) Chronic widespread musculoskeletal pain with or without fibromyalgia: psychological distress in a representative community adult sample. J Rheumatol 29:588–594 57. Winters L, Habin K, Flanagan J, Cashavelly BJ (2010) “I feel like I am 100 years old!” managing arthralgia from aromatase inhibitors. Clin J Oncol Nurs 14:379–382 58. Wolfe F, Smythe HA, Yunus MB (1990) The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172 59. Wolfe F, Ross K, Anderson J, Russell IJ (1995) Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol 22:151–156 60. Wolfe F (1997) The relation between tender points and fibromyalgia symptom variables: evidence that fibromyalgia is not a discrete disorder in the clinic. Ann Rheum Dis 56:268–271 61. Wolfe F (2003) Stop using the American College of Rheumatology criteria in the clinic. J Rheumatol 30:1671–1672 62. Wolfe F (2009) Fibromyalgia wars. J Rheumatol 36:671–678 63. Wolfe F, Clauw DJ, Fitzcharles MA et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600–610 64. Wolfe F, Clauw DJ, Fitzcharles MA et al (2011) Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol 38:1113–1122 65. Wolfe F, Hassett AL, Walitt B, Michaud K (2011) Mortality in fibromyalgia: a study of 8,186 patients over thirty-five years. Arthritis Care Res 63:94–101 Schwerpunkt English Version of "Ätiologie und Pathophysiologie des Fibromyalgiesyndroms". DOI 10.1007/s00482-012-1174-0 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 C. Sommer1 · W. Häuser2 · M. Burgmer3 · R. Engelhardt4 · K. Gerhold5 · F. Petzke6 · T. Schmidt-Wilcke7 · M. Späth8 · T. Tölle9 · N. Üçeyler1 · H. Wang10 · A. Winkelmann11 · K. Thieme12 1 Neurologische Klinik, Universitätsklinikum Würzburg 2 Innere Medizin 1, Klinikum Saarbrücken gGmbH, Saarbrücken 3 Klinik für Psychosomatische Medizin und Psychotherapie, Universitätsklinikum Münster 4 Zentralinstitut für die kassenärztliche Versorgung in Deutschland, Berlin 5 Klinik für Pädiatrie mit Schwerpunkt Pneumologie/Immunologie und Berlin School of Public Health, Charité – Universitätsmedizin Berlin 6 Schmerz-Tagesklinik und -Ambulanz, Universität Göttingen 7 Department of Anesthesiology, Chronic Pain and Fatigue Research Center, University of Michigan, Ann Arbor (Michigan) 8 Rheumatologische Praxis, München-Gräfelfing 9 Klinik für Neurologie, Technische Universität München, Munich 10 Department für Orthopädie und Unfallchirurgie, Stiftung Orthopädische Universitätsklinik Heidelberg 11 Klinik und Poliklinik für Physikalische Medizin und Rehabilitation, Klinikum der Universität München, Munich 12 Institut für Medizinische Psychologie, Philipps-Universität Marburg Etiology and pathophysiology of fibromyalgia syndrome Background and goals Methods Etiology There is extensive scientific literature on the etiology and pathophysiology of fibromyalgia syndrome (FMS) which makes it difficult for the individual practitioner to stay up-to-date. Recent review articles focus either on biological or psychological aspects. The classification of FMS (physical illness vs. mental disorder), contents of patient education, and the preferred treatment methods are closely related to the identified etiologic and pathophysiologic factors. Therefore, we decided to perform a literature review and a formal consensus process on the pathogenesis and pathophysiology of FMS and chronic widespread pain (CWP). We aimed to analyze the content and quality of published studies on these topics in order to identify possible risk factors for the development of FMS and CWP and also to identify factors that are unrelated to the two syndromes. The methodology of the literature search and analysis, and preparation of recommendations are presented in the article “Methodological fundamentals used in developing the guideline”. Risk indicators and factors Results Preliminary note The following findings apply to adults. For the etiology and pathophysiology of FMS and CWP in children and adolescents please refer to the chapter “Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. Evidence-based observation Current evidence does not allow definite conclusions to be drawn about the etiology of CWP/FMS. It is unclear whether the risk indicators of CWP and FMS described in the following observations are risk factors. Strong consensus Comment. Risk indicators are characteristics whose presence indicates a greater risk of illness without playing a causative role. Risk factors (etiologic factors) are characteristics that are causally associated with an increased risk of disease. Risk indicators and risk factors for disease are identified by retrospective and prospective cohort studies. The design of these studies, however, do not allow proof of a causal relationship. The following criteria increase the likelihood of a causal relationship: dose–effect relationship and experimental evidence, i.e., randomizedDer Schmerz 3 · 2012 | 1 Schwerpunkt Tab. 1 Predictors of chronic widespread pain (CWP) in prospective population-based cohort studies Study design Prospective population-based cohort study of 1,658 adults between 25–65 years of age; follow-up after 36 months Prospective cohort study of 1,081 newly employed individuals at 12 different work places; follow-up after 24 months Prospective population-based cohort study; 3,171 adults without CWP between 25–65 years of age; follow-up after 15 months Prospective cohort study of 768 individuals without CWP but with a profile indicating increased risk for CWP, out of a population-based sample of 11,000 individuals; follow-up after 15 months EPIFUND: 2,509 patients from three British general practitioners between 25–65 years of age; follow-up after 15 months 1958 British Cohort Study: 18,558 individuals; followup after 45 years Risk indicator (statistical predictor) Repetitive movements of wrists Increased illness behavior Regional pain at baseline measurement Increased physical symptoms Crouching activity >15 min Monotonous work Risk (95% CI) OR 1.8 (1.2–2.7) OR 9.0 (3.7–22.2) OR 2.1 (1.3–3.3) OR 3.3 (1.5–7.4) OR 2.0 (1.1–3.6) OR 1.9 (1.1–3.2) Reference [25, 26, 27] Increased physical symptoms Increased illness behavior Sleep disorder HPA axis dysfunction OR 1.8(1.1–3.1) OR 3.3(2.3–4.8) OR 2.7(1.6–3.2) OR 8.5 (1.5–47.9) [14] Gene polymorphisms affecting the HPA axis ACTH-precursor-receptor SERPINA6, rs941601, genotype CT Genotype TT Corticosteroid-binding globulin MC2R rs11661134, genotype AG and AA Decreased health-related quality of life Teacher reports of persistent behavioral abnormalities at ages 7, 11 and 16 years of age β2-adrenergic receptor (ADRB2) combinations, e.g. H2-H2 Hospitalization after traffic accident Institutionalization Maternal death Financial need Multiple physical symptoms at the age of 7 years OR 1.61 (1.0–2.6) OR 1.2 (1.0–1.3) OR 2.2 (1.1–4.4) OR 2.2 (1.2–4.4) [19] RR 4.0 (2.6–6.2) RR 2.1 (1.4–3.2) [33] [34] RR 1.8 (1.1–2.9) RR 1.5 (1.1–2.1) RR 1.7 (1.3–2.4) RR 2.0 (1.1–3.7) RR 1.6 (1.3–1.9) RR 1.5 (1.0–2.3) [18] [30, 31] [16] [28] ACTH adrenocorticotropic hormone; CI confidence interval; CWP chronic widespread pain; HPA hypothalamic–pituitary–adrenal; OR odds ratio; RR relative risk. controlled trials that demonstrate elimination of risk when the risk factor is eliminated. The literature search yielded 3,107 hits. There were 6 prospective cohort studies with a follow-up duration ranging from 15 months to 45 years on biopsychosocial risk indicators for the development of CWP. There were 2 prospective cohort studies with a follow-up duration ranging from 11–24 years on biopsychosocial risk indicators for the development of FMS and 2 systematic reviews of case–control studies. There were no studies on dose– effect relationships. Experimental studies on risk factors for CWP and FMS were not found. 2 | Der Schmerz 3 · 2012 Risk indicators of CWP Evidence-based observation The following biologic, mechanical, and psychosocial factors are associated with the development of CWP (risk indicators): Fbiological factors: gene polymorphisms (β2-adrenergic receptors, ACTH precursor receptor, corticosteroid binding globulin), dysfunction of the hypothalamic–pituitary–adrenal (HPA) axis (EL 2b); Fmechanical factors: uncomfortable postures at work (crouching, repetitive movements of wrist), monotonous work (EL 2b); Fpsychological factors: increased physical complaints and illness behavior; low physical health-related quality of life; sleep disorders (EL 2b); permanent threat to life (EL 2c); Fchildhood: hospitalization after traffic accident; institutionalization; maternal death; financial need (EL 2b). Strong consensus Comment. The results of prospective cohort studies are summarized in . Tab. 1. A study from Israel [1] compared 1,024 people from a town (Sderot) that was repeatedly attacked by rocket fire with 1,006 people who lived in another town (Okafim) with a similar socioeconomic and demographic profile, but who were not exposed to rocket fire. Trauma-related symptoms and physical complaints were more frequent and the point prevalence of CWP was higher in Sderot (11.1%) than in Ofakim [8.3%; odds ratio (OR) 1.37]. Abstract · Zusammenfassung Risk indicators for FMS Evidence-based observation The following biological and psychosocial factors are associated with the development of FMS: Fbiological factors: inflammatory– rheumatic diseases (EL 2b), Fgene polymorphisms of the 5HT2-receptor (EL 3a), Flife style: smoking, overweight, lack of physical activity (EL 2b) Fpsychological factors: physical abuse in childhood and adulthood, sexual abuse in childhood and adulthood (EL 3a), stress at the work place (EL 3b). Strong consensus Comment. See . Tab. 2. Genetic factors are likely present since FMS tends to cluster in families [38]. Candidate genes in the serotonergic, dopaminergic, and catecholaminergic systems may play a role. However, this is also the case in other chronic pain syndromes and therefore these findings are not specific for FMS [3, 4]. In a retrospective cohort study of 62,000 members of a U.S. health insurance an association with FMS was found for rheumatoid arthritis [RR (relative risk) for women 4.5 (95% CI 3.6–5.5), RR for men 6.1 (95% CI 4.2–8.8)] and with systemic lupus erythematosus [RR for women, 5.8 (95% CI 4.2–8.0); RR for men not significant; [46]). Out of 9,739 patients with rheumatoid arthritis without FMS (U.S. National Data Bank for Rheumatic Diseases) on average 19.8% met the criteria for FMS at least once during 4.4 years of observation; 7.4% met the criteria at the end of the observation period. Poverty [HR (hazard ratio) 1.64 (95% CI 1.47–1.82)], overweight [HR 1.60 (95% CI 1.43–1.79)], depressive symptoms [HR 2.28 (95% CI 1.97–2.64)], numerous physical comorbidities [HR 2.53 (95% CI 2.36–2.71)], and low physical activity [HR 2.53 (95% CI 2.36–2.71)] predicted FMS [47]. In a 2-year prospective observational study of 4,791 hospital employees (4,250 women, 541 men), increased bullying in the workplace, low freedom of action, and high workload increased the risk Schmerz 2012 · DOI 10.1007/s00482-012-1174-0 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 C. Sommer · W. Häuser · M. Burgmer · R. Engelhardt · K. Gerhold · F. Petzke · T. Schmidt-Wilcke · M. Späth · T. Tölle · N. Üçeyler · H. Wang · A. Winkelmann · K. Thieme Etiology and pathophysiology of fibromyalgia syndrome Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinäre Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. Results. Current data do not identify distinct etiologic or pathophysiological factors mediating development of FMS. The development of FMS is associated with inflammatory rheumatic diseases (EL2b), with gene polymorphisms of the 5-hydroxytryptamine (HT)2 receptor (EL3a), lifestyle factors (smoking, obesity, lack of physical activity; EL2b), physical and sexual abuse in childhood and adulthood (EL3a). Conclusion. FMS is most likely the result of various pathogenetic factors and pathophysiological mechanisms.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Guideline · Systematic review · Etiology · Pathophysiology Ätiologie und Pathophysiologie des Fibromyalgiesyndroms Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center for Evidence Based Medicine. of physician-diagnosed FMS [22]. Due to problems with the study design (no detection of pain using validated instruments at the beginning and end of the study), the Ergebnisse. Die aktuelle Studienlage erlaubt keine eindeutigen Aussagen zur Ätiologie und Pathophysiologie des FMS. Die Entwicklung eines FMS ist mit entzündlich-rheumatischen Erkrankungen (EL2b), Genpolymorphismen des 5-Hydroxytryptamin(HT)2-Rezeptors (EL3a), Lebensstilfaktoren (Rauchen, Übergewicht, mangelnde körperliche Aktivität; EL2b), körperlicher Misshandlung und sexuellem Missbrauch in Kindheit und Erwachsenenalter (EL3a) assoziiert. Schlussfolgerung. Das FMS ist wahrscheinlich die Endstrecke verschiedener ätiopathogenetischer Faktoren und pathophysiologischer Mechanismen. Schlüsselwörter Fibromyalgiesyndrom · Leitlinie · Systematische Übersicht · Ätiologie · Pathophysiologie level of evidence was downgraded for this study. Der Schmerz 3 · 2012 | 3 Schwerpunkt Tab. 2 Predictors of fibromyalgia syndrome (FMS) in prospective population-based cohort studies and systematic reviews, respectively Study design Risk indicator (predictor) Risk (95% CI) Adventist Health Study 1 and 2: cohort study of 3,136 women; follow-up after 25 years Nord-Trøndelag Health Study. Population-based cohort study of 15,990 individuals; follow-up after 11 years Population-based cohort study of 214 women; followup after 5 years Number of allergies Tobacco smoking OR 4.0 (2.3–6.9) OR 2.4 (1.3–4.2) Overweight (BMI 25–29.9) Obesity (BMI >30) Overweight and lack of physical activity RR 1.7 (1.4–2.1) RR 1.6 (1.2–2.3) RR 2.1 (1.4–3.2) [32] Increased physical symptoms Depression Regional pain for >6 years Mobbing at the workplace High workload Decreased discretion in making decisions C-allele of the 5HT2A receptor 102T CC-allele of the 5HT2A receptor 102T CT-allele of the 5HT2A receptor 102T Physical abuse in childhood Physical abuse in adulthood Sexual abuse in childhood Sexual abuse in adulthood RR 4,6 (1,7–12,2) RR 2,3 (1,3–4,0) RR 2,8 (1,2–6,7) OR 4.1 (2.0–9.6) OR 2.1 (1.2–3.9) OR 2.1 (1.1–4.0) [12] OR 1.3 (1.1–1.7) OR (1.5, 1.0–2.3) [24] Cohort study of 4,791 hospital employees; follow-up after 2 years (outcome: physician-diagnosed FMS) Meta-analysis of 21 case– control studies regarding genetic variants Meta-analysis of 18 studies with 13,095 individuals Reference [8] [22] OR 1.8 (1.2–3.9) OR 2.5 (1.8–3.4) OR 3.1 (1.0–9.4) OR 1.9 (1.4–2.8) OR 2.2 (1.1–4.7) [15] insurance who had recently suffered an automobile accident examined the occurrence of widespread pain (WP) after 12 months of follow-up; 7.8% of patients had WP. Physical symptoms after the accident (RR 2.5, 95% CI 1.2–5.1), high utilization of health care services prior to the accident (RR 3.6, 95% CI 1.6–7.9), somatization prior to the accident (RR 1.7, 95% CI 0.99–2.8), and older age (RR 3.3, 95% CI 1.5–7.1) predicted WP [48]. In a prospective cohort study of 7,462 members of a health insurance company with whiplash injuries of the cervical spine, 266 individuals had localized pain after the accident and were followed-up at 4, 6, and 12 months. The cumulative incidence of CWP was 21%. CWP was reported most commonly in the early time period after the accident. The risk of developing CWP was greater in individuals with depressive symptoms at baseline measurement (OR 3.2, 95% CI 1.6–6.3) [20]. CWP at 12 months was rare (49). The examination of 53 of 153 survivors 3.5 years after a major train accident demonstrated that 15% fulfilled FMS criteria [5]. BMI body mass index; CI confidence interval; FMS fibromyalgia syndrome; OR odds ratio; RR relative risk. Pathophysiology Vitamin D deficiency, infectious diseases, and accidents Evidence-based observation Data on the association between FMS and vitamin D deficiency, infectious diseases, and accidents are inconsistent. EL 3b. Strong consensus Comment Vitamin D deficiency: In population-based studies [29] and in case–control studies [17], an association of CWP with decreased vitamin D levels has been reported. However, in case–control studies no difference in vitamin D levels were found between patients with FMS and healthy controls [10, 42]. Infections: Prospective studies are not available. In case–control studies, the association of chronic hepatitis C and FMS is contradictory. The results of two case– control studies showing an increased prevalence of FMS in patients with chronic hepatitis B and HTLV-1 infection, re- 4 | Der Schmerz 3 · 2012 spectively, have not been replicated [38, 39]. Case–control studies investigating the association of Lyme disease with FMS are not available. In a large single-center observational study of 287 patients, 22 patients (8%) developed FMS. Fifteen patients diagnosed with FMS participated in the 4.5-year observational study. Symptoms of Lyme disease improved in 14 of 15 patients following antibiotic therapy but FMS symptoms persisted in all patients [11]. Following Lyme disease, 5% of patients report persistent musculoskeletal pain, fatigue, and difficulties in concentrating [6]. Accidents: Data are contradictory. A total of 154 patients who were hospitalized after a whiplash injury were examined after 1.5 and 3 years for the presence of FMS; 53 patients with fractures served as a control group. After 3 years of followup, 3 of 126 patients with whiplash injury and 1 of 53 patients with fracture were diagnosed with FMS [43]. A prospective cohort study of 957 members of a health Altered central pain processing, dysfunction of the HPA axis, peripheral pain generators Evidence-based observation It is possible that the following pathophysiological mechanisms play a pathogenic role in FMS: Faltered central pain processing (EL 3b), Fdysfunction of the HPA axis (EL 2b), and Fperipheral pain generators (EL 3b). Strong consensus Comment. The literature search yielded 763 hits. These included a systematic review of biomarkers [9], no other systematic reviews of other pathophysiological mechanisms, and numerous narrative review articles (e.g., [2, 3, 13, 35, 37, 38, 40]). Systematic reviews completed by members of the working group regarding cytokines [44] and central nervous system im- aging (Burgmer and Petzke, 2011, personal communication) revealed the following substantial problems that limit the significance of the available studies: 1. Lack of longitudinal studies: due to the cross-sectional design of most studies, statements regarding causation are not possible. It is unclear whether the described pathophysiological changes are epiphenomena of other processes or whether they are confounded by other variables (e.g., changes in cytokine patterns because of depression). 2. Confounding of the results due to comorbidities: due to the frequent comorbidity of FMS with other psychiatric disorders and functional disorders, it is difficult to define a “pure FMS” group [36]. The potential influence of these comorbidities has not been sufficiently controlled in these studies. One study that controlled for comorbid depressive disorder found no consistent differences in the gray matter between FMS patients and healthy controls [21]. 3. Lack of specificity of findings: in most studies on pathophysiology, the healthy control subjects were healthy individuals of the same age and sex as the affected individuals, but not patients with other chronic pain syndromes and mental disorders. It is unclear whether the described pathophysiological abnormalities are specific for FMS. 4. Methodological problems: the heterogeneity of analysis makes a comparison of study results difficult [35]. The sample sizes of most studies are small (<25 individuals per group). In addition, the quality of these studies is mostly low. 5. Ignoring the probable heterogeneity of the FMS population. Because of the problems mentioned, we chose not to summarize the numerous studies presented—neither in a narrative fashion nor in the form of a meta-analysis. Instead a few pathophysiological mechanisms for which the data are largely consistent are discussed. HPA axis: Dysfunction of the HPA axis as a pathophysiological factor is discussed in many review articles (e.g., [3]). Data on cortisol secretion and individual tests of the HPA axis are inconsistent and the role of comorbid depression is unclear [9]. The best evidence for the role of a disturbed HPA axis derives from a prospective population-based study. Out of 11,000 individuals, 768 were chosen because their psychosocial profile indicated an increased risk for the development of CWP. Then, 463 subjects were randomly selected and 267 (58%) eventually agreed to participate in the study, of whom 241 completed the study. After 15 months, 12% of these individuals had newly developed CWP. A lack of suppression in the dexamethasone suppression test (OR 3.53, 95% CI 1.17–10.65), low morning serum cortisol levels, and high evening saliva cortisol levels were associated with the development of CWP [28]. Autonomic nervous system: A number of differences in the function of the autonomic nervous system among patients with FMS and healthy subjects have been described (e.g., decreased heart rate variance, a tendency for syncope, altered cutaneous capillary responsiveness). However, a causal relationship could not be proven [38]. Immune system: Many studies addressed the issue of immune dysfunction in FMS. Some groups detected autoantibodies whose significance is still unclear [9]. Among the cytokines, interleukin-6 is increased in the plasma or serum of patients with FMS [44]. In one longitudinal study, elevated cytokine levels normalized after multimodal therapy [45]. Neurotransmitter: The neurotransmitter substance P is increased in the cerebrospinal fluid (CSF) of patients with FMS, but also in other chronic pain syndromes, so that substance P is more of a marker for chronic pain than for FMS specifically. Serotonin levels in CSF and serum are decreased. The CSF levels of the neurotrophic factors nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) are increased, but the significance of these findings is unclear. Data for other neuropeptides and neurotransmitters are inconsistent [39]. Peripheral nervous system and muscle: It was hypothesized that peripheral pain generators contribute significantly to the initiation or maintenance of FMS [41]. In a subgroup of patients with FMS, polyneuropathy was present [7]. Modulation of muscle afferent fibers may play a role [38]. Altered central pain processing: The studies on central pain processing in FMS cannot be reliably interpreted due to the use of different methods (e.g., PET, fMRI, EEG), different study designs (e.g., measurement while resting or during stimulation), the lack of longitudinal studies, and the low quality of the methods used and of data analysis. Augmentation of pain processing and a tendency for altered structure and functions of brain areas that are important for the cognitive–emotional processing of pain and descending pain inhibition have been reported. However, due to the general lack of patients with other chronic pain syndromes in the control groups, these findings cannot be interpreted as being FMS specific [35]. Disorders of the thyroid hormone system, disorders of the female sex hormones, disorders of the renin–angiotensin–aldosterone system, structural muscle changes, cosmetic breast implants Evidence-based observation The following statements from the first version of the guidelines still apply: there is no evidence of a link between FMS and Fdisorders of the thyroid hormone system, Fdisorders of the female sex hormones, Fdisorders of the renin–angiotensin– aldosterone system, Fstructural muscle changes, and Fcosmetic breast implants. EL 2c, strong consensus Comment. See [39] Mechanisms of learning Evidence-based observation The following statements from the first version of the guidelines still apply: learning mechanisms such as operant conditioning, and sensitization play a role in the chronicity of FMS. EL 2b, strong consensus Comment. See [39] Der Schmerz 3 · 2012 | 5 Schwerpunkt Biopsychosocial model Evidence-based observation A biopsychosocial model with respect to predisposition, initiation, and chronicity of FMS is postulated. Physical and/ or biological and/or psychosocial stressors in the context of an appropriate genetic predisposition and learning history produce autonomic, endocrine, and central nervous system reactions that result in the symptoms of FMS, such as pain, fatigue, and sleep disorders, autonomic and psychological symptoms. There is heterogeneity in the genetic predisposition, learning history, and in the autonomic, endocrine, and central nervous system reactions. FMS is a final pathway of various pathogenetic factors and pathophysiological mechanisms. Strong consensus Comment. See [39] Discussion It is difficult to summarize the evidence on the etiology and pathophysiology of CWP and FMS due to several factors. There is an extensive literature on individual factors that are related to CWP or FMS and which may play a role in the etiology or pathophysiology of these conditions. Since the publication of the first version of these guidelines, multiple other factors have been examined, including gene polymorphisms, smoking, overweight and nutrition, vitamins, neuroendocrine factors, immunologic factors, mitochondrial function, different infections, central pain processing, and individual biographical aspects. Unfortunately, for the majority of these studies, due to limitations in methodology and design, it remains unclear whether the findings indicate random associations, factors inherent to the conditions studied, consequences of disease, or if they indeed represent relevant factors in etiology or pathophysiology. As was mentioned in the first version of these guidelines, there are some factors for which there is definitely no relationship with FMS. These conclusions are still accurate and apply to the thyroid hormone system, the renin–angiotensin–al- 6 | Der Schmerz 3 · 2012 dosterone system, female sex hormones, structural muscle changes, Lyme disease, and cosmetic breast implants. The best evidence for positive correlations of causative factors with the development of CWP or FMS has been obtained from prospective cohort studies. Several biologic factors could be identified, including the presence of inflammatory– rheumatic diseases, genetic factors, lifestyle factors such as smoking, overweight, and decreased physical activity, and psychological factors, such as physical abuse or sexual abuse. Additional prospective, population-based studies with an analysis of dose–effect relationships, and interactions of presumed risk factors are required. Conclusion for clinical practice Several factors reduce the meaningfulness of many studies on pathophysiology, such as their sectional design, the lack of consideration of confounding comorbidities, the small number of study subjects, and the use of very heterogeneous methods. The pathophysiological factors that are probably associated with FMS have been listed above. However, because of the aforementioned limitations, it is difficult to assess a causal relationship. There is an urgent need for further research. Future research should employ standardized methods, control for current medication use and psychological comorbidities, and include adequate control groups consisting of healthy individuals and individuals with other chronic pain syndromes. In addition, studies with larger sample sizes are required to simultaneously examine different potential neuroimmunological and neurobiological factors, and their reciprocal relationships. Corresponding address C. Sommer Neurologische Klinik, Universitätsklinikum Würzburg Josef-Schneider-Str. 11, 97080 Würzburg Germany sommer@uni-wuerzburg.de Conflict of interest. See Tab. 5 in “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Ablin JN, Cohen H, Clauw DJ et al (2010) A tale of two cities – the effect of low intensity conflict on prevalence and characteristics of musculoskeletal pain and somatic symptoms associated with chronic stress. Clin Exp Rheumatol 28(6 Suppl 63):15–21 2. Arnold LM (2010) The pathophysiology, diagnosis and treatment of fibromyalgia. Psychiatr Clin North Am 33(2):375–408 (Review) 3. Bradley LA (2009) Pathophysiology of fibromyalgia. Am J Med 122(12 Suppl):22–30 4. Branco JC (2010) State-of-the-art on fibromyalgia mechanism. Acta Reumatol Port 35:10–15 5. Buskila D, Ablin JN, Ben-Zion I et al (2009) A painful train of events: increased prevalence of fibromyalgia in survivors of a major train crash. Clin Exp Rheumatol 27(5 Suppl 56):79–85 6. Cairns V, Godwin J (2005) Post-Lyme borreliosis syndrome: a meta-analysis of reported symptoms. Int J Epidemiol 34:1340–1345 7. Caro XJ, Winter EF, Dumas AJ (2008) A subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIg. Rheumatology (Oxford) 47:208–211 8. Choi CJ, Knutsen R, Oda K et al (2010) The association between incident self-reported fibromyalgia and nonpsychiatric factors: 25-years follow-up of the Adventist Health Study. J Pain 11:994–1003 9. Dadabhoy D, Crofford LJ, Spaeth M et al (2008) Biology and therapy of fibromyalgia. Evidencebased biomarkers for fibromyalgia syndrome. Arthritis Res Ther 10:211 10. Rezende Pena C de, Grillo LP, Chagas Medeiros MM das (2010) Evaluation of 25-hydroxyvitamin D serum levels in patients with fibromyalgia. J Clin Rheumatol 16:365–369 11. Dinerman H, Steere AC (1992) Disease associated with fibromyalgia. Ann Intern Med 117:281–285 12. Forseth KO, Husby G, Gran JT, Førre O (1999) Prognostic factors for the development of fibromyalgia in women with self-reported musculoskeletal pain. A prospective study. J Rheumatol 26:2458–2467 13. Geenen R, Bijlsma JW (2010) Deviations in the endocrine system and brain of patients with fibromyalgia: cause or consequence of pain and associated features? Ann N Y Acad Sci 1193:98–110 14. Gupta A, Silman AJ, Ray D et al (2007) The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study. Rheumatology (Oxford) 56:360–371 15. Häuser W, Kosseva M, Üçeyler N et al (2011) Emotional, physical and sexual abuse in fibromyalgia syndrome – a systematic review with meta-analysis. Arthritis Care Res 63:808–820 16. Harkness EF, Macfarlane GJ, Nahit E et al (2004) Mechanical injury and psychosocial factors in the work place predict the onset of widespread body pain: a two-year prospective study among cohorts of newly employed workers. Arthritis Rheum 50:1655–1664 17. Heidari B, Shirvani JS, Firouzjahi A et al (2010) Association between nonspecific skeletal pain and vitamin D deficiency. Int J Rheum Dis 13:340–346 18. Hocking LJ, Smith BH, Jones GT et al (2010) Genetic variation in the beta2-adrenergic receptor but not catecholamine-O-methyltransferase predisposes to chronic pain: results from the 1958 British Birth Cohort Study. Pain 149:143–151 19. Holliday KL, Nicholl BI, Macfarlane GJ et al (2010) Genetic variation in the hypothalamic-pituitaryadrenal stress axis influences susceptibility to musculoskeletal pain: results from the EPIFUND study. Ann Rheum Dis 69:556–560 20. Holm LW, Carroll LJ, Cassidy JD et al (2007) Widespread pain following whiplash-associated disorders: incidence, course, and risk factors. J Rheumatol 34:193–200 21. Hsu MC, Harris RE, Sundgren PC et al (2009) No consistent difference in gray matter volume between individuals with fibromyalgia and agematched healthy subjects when controlling for affective disorder. Pain 143:262–267 22. Kivimäki M, Leino-Arjas P, Virtanen M et al (2004) Work stress and incidence of newly diagnosed fibromyalgia: prospective cohort study. J Psychosom Res 57:417–422 23. Jensen KB, Petzke F, Carville S et al (2010) Anxiety and depressive symptoms in fibromyalgia are related to poor perception of health but not to pain sensitivity or cerebral processing of pain. Arthritis Rheum 62:3488–3495 24. Lee YH, Choi SJ, Ji JD, Song GG (2010) Candidate gene studies of fibromyalgia: a systematic review and meta-analysis. Rheumatol Int 32:417–426 25. McBeth J, Macfarlane GJ, Hunt IM, Silman AJ (2001) Risk factors for persistent chronic widespread pain: a community-based study. Rheumatology (Oxford) 40:95–101 26. McBeth J, Macfarlane GJ, Benjamin S, Silman AJ (2001) Features of somatisation predict the onset of chronic widespread pain: results of a large population-based study. Arthritis Rheum 44:940–946 27. McBeth J, Harkness EF, Silman AJ, Macfarlane GJ (2003) The role of workplace low-level mechanical trauma, posture and environment in the onset of chronic widespread pain. Rheumatology (Oxford) 42:1486–1494 28. McBeth J, Silman AJ, Gupta A et al (2007) Moderation of psychosocial risk factors through dysfunction of the hypothalamic-pituitary-adrenal stress axis in the onset of chronic widespread musculoskeletal pain: findings of a population-based prospective cohort study. Arthritis Rheum 56:360–371 29. McBeth J, Pye SR, O’Neill TW et al (2010) Musculoskeletal pain is associated with very low levels of vitamin D in men: results from the European Male Ageing Study. Ann Rheum Dis 69:1448–1452 30. Jones GT, Silman AJ, Power C, Macfarlane GJ (2007) Are common symptoms in childhood associated with chronic widespread body pain in adulthood? Results from the 1958 British Birth Cohort Study. Arthritis Rheum 56:1669–1675 31. Jones GT, Power C, Macfarlane GJ (2009) Adverse events in childhood and chronic widespread pain in adult life: results from the 1958 British Birth Cohort Study. Pain 143:92–96 32. Mork PJ, Vasseljen O, Nilsen TI (2010) Association between physical exercise, body mass index, and risk of fibromyalgia: longitudinal data from the Norwegian Nord-Trøndelag Health Study. Arthritis Care Res 62:611–617 33. Nicholl BI, Macfarlane GJ, Davies KA et al (2009) Premorbid psychosocial factors are associated with poor health-related quality of life in subjects with new onset of chronic widespread pain – results from the EPIFUND study. Pain 141:119–126 34. Pang D, Jones GT, Power C, Macfarlane GJ (2010) Influence of childhood behaviour on the reporting of chronic widespread pain in adulthood: results from the 1958 British Birth Cohort Study. Rheumatology 49:1882–1888 35. Petzke F (2010) CNS processing of pain in functional somatic syndromes. Schmerz 24:146–155 36. Rhudy JL (2010) Respiration-induced hypoalgesia: additional evidence for pain modulation deficits in fibromyalgia? Pain 149:1–2 37. Russell IJ, Larson AA (2009) Neurophysiopathogenesis of fibromyalgia syndrome: a unified hypothesis. Rheum Dis Clin North Am 35:421–435 38. Saxena A, Solitar BM (2010) Fibromyalgia: knowns, unknowns, and current treatment. Bull NYU Hosp Jt Dis 68:157–161 39. Sommer C, Häuser W, Gerhold K et al (2008) Ätiopathogenese und Pathophysiologie des Fibromyalgiesyndroms und chronischer Schmerzen in mehreren Körperregionen. Schmerz 22:267–282 40. Staud R (2010) Is it all central sensitization? Role of peripheral tissue nociception in chronic musculoskeletal pain. Curr Rheumatol Rep 12:448–454 41. Staud R, Robinson ME, Weyl EE, Price DD (2010) Pain variability in fibromyalgia is related to activity and rest: role of peripheral tissue impulse input. J Pain 11:1376–1383 42. Tandeter H, Grynbaum M, Zuili I et al (2009) Serum 25-OH vitamin D levels in patients with fibromyalgia. Isr Med Assoc J 11:339–342 43. Tishler M, Levy O, Amit-Vazina M (2011) Can fibromyalgia be associated with whiplash injury? A 3-year follow-up study. Rheumatol Int 31:1209– 1213 44. Üceyler N, Häuser W, Sommer C (2011) Systematic review with meta-analysis: cytokines in fibromyalgia syndrome. BMC Musculoskelet Disord 12:245 45. Wang H, Moser M, Schiltenwolf M, Buchner M (2008) Circulating cytokine levels Compared to pain in patients with fibromyalgia – a prospective longitudinal study over 6 months. J Rheumatol 35:1366–1370 46. Weir PT, Harlan GA, Nkoy FL et al (2006) The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on International Classification of Diseases, 9th Revision codes. J Clin Rheumatol 12:124–128 47. Wolfe F, Häuser W, Hassett AL et al (2011) The development of fibromyalgia – I: examination of rates and predictors in patients with rheumatoid arthritis (RA). Pain 152:291–299 48. Wynne-Jones G, Jones GT, Wiles NJ et al (2006) Predicting new onset of widespread pain following a motor vehicle collision. J Rheumatol 33:968– 974 Der Schmerz 3 · 2012 | 7 Schwerpunkt English Version of "Das Fibromyalgiesyndrom. Allgemeine Behandlungsgrundsätze, Versorgungskoordination und Patientenschulung". DOI 10.1007/s00482-012-1167-z © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 W. Eich1 · W. Häuser2 · B. Arnold3 · K. Bernardy4 · W. Brückle5 · U. Eidmann6 · K. Klimczyk7 · V. Köllner8 · H. Kühn-Becker9 · M. Offenbächer10 · M. Settan11 · M. von Wachter12 · F. Petzke13 1 Department of General Internal and Psychosomatic Medicine, Heidelberg Medical University Hospital, Heidelberg 2 Internal Medicine 1, Saarbrücken Hospital, Saarbrücken 3 Department of Pain Management, Dachau Hospital, Dachau 4 Department of Pain Management, BG University Hospital Bergmannsheil GmbH, Ruhr University Bochum 5 Fürstenhof Clinic, Bad Pyrmont 6 German Rheumatism Association, Wuppertal 7 Enzensberg Clinic, Hopfen am See 8 Department of Psychosomatic Medicine, Bliestal Clinics, Blieskastel 9 Pain Center, Zweibrücken 10 Human Sciences Center, Ludwig Maximilian University Munich 11 German Fibromyalgia Association, Seckach 12 Department of Psychosomatic Medicine, Ostalb Hospital Aalen 13 Day and Outpatient Clinic for Pain, University Medical Center Göttingen, George August University Göttingen Fibromyalgia syndrome General principles and coordination of clinical care and patient education Due to its usually chronic course and the highly subjective suffering and functional limitations of many patients, fibromyalgia syndrome (FMS) presents physicians from all fields with complex care and cooperative tasks. The following key questions were formulated by the supervisory team for the update of this guidelines chapter: 1.Should the diagnosis of FMS be explicitly communicated to the affected individual? 2.Which information concerning symptoms, treatment goals and options should be given at the initial diagnosis? 3.Is patient education worthwhile? 4.Which specialties should coordinate the treatment of FMS? 5.Does a graded treatment approach make sense? 6.When is a stationary, multimodal therapy indicated? 7.How should “therapeutically refractory” courses continue to be treated? Materials and methods Initial diagnosis The methods for the literature research and analysis, as well as for the preparation of recommendations, are presented in the article “Methodological fundamentals used in developing the guideline”. Information at the initial diagnosis Results Preliminary note The following findings and recommendations apply to adults. The general principles of treatment and coordination of care for children and adolescents are covered in the article “Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. The key recommendations are italicized. Evidence-based recommendation The patients with chronic pain in multiple body regions who meet the criteria of FMS should be informed of the FMS diagnosis. EL 4, strong recommendation, strong consensus Comment. In the case of an initial diagnosis of a disease/disorder, releasing the diagnosis is an ethical medical obligation. This measure is highly feasible and carries little risk. Therefore, an upgrade of the recommendation level by two levels was performed. No randomized control trials (RCTs) have been conducted on the issue of whether an FMS diagnosis positively or negatively affects the health and functioning of those affected. From the perspective of those affected, the diagnostic labeling of a complex complaint, which may have led to lengthy, frustrating medical diagnostics and therapy, may provide psychologDer Schmerz 3 · 2012 | 1 Schwerpunkt ical relief and a more adequate basis for their treatment. A Canadian study showed greater patient satisfaction with their state of health and a lower incidence of symptoms 18 months after diagnosis [38]. The data regarding the impact of an FMS diagnosis on the further use of medical services are inconsistent, and there are no studies from Germany on this topic. Recent studies from the general medical sector in Great Britain and France indicate a possible reduction in direct medical costs as a result of an earlier diagnosis of FMS [3, 18]. Criteria for recommending therapeutic procedures effects) are not determined after 4 weeks, the medication should be stopped. The assessment of the benefits of exercise therapy and psychotherapeutic procedures is recommended after 3 months. Clinical consensus point Mild forms of FMS Initial therapy after the initial diagnosis For the selection of therapeutic measures, the preferences and comorbidities of the patient, within the guideline recommendations, should be considered. Strong consensus After an initial diagnosis of FMS, the patient should be informed regarding recommended and non-recommended FMS treatment measures. Strong consensus Comment. Regarding treatment recommendations, the consideration of patient preferences (e.g., possible weight gain under antidepressant therapy) and comorbidities (e.g., aqua jogging instead of walking with comorbid knee arthritis) is a medical ethical obligation. Clinical point of consensus Comorbidities Clinical point of consensus The patient should be advised that their complaint is not an organic disease (fibromyalgia, in the sense of a rheumatic disease) but is instead based on a functional disorder. The legitimacy of the ailment should be assured. The patient’s symptoms should be explained in a clear manner with the aid of a biopsychosocial disease model, which builds on the subjective disease theory of the patient, e.g., by means of psychophysiological relationships (stress, vicious circle model). Information regarding the harmlessness of the ailment should be given. The possibilities for the patient to alleviate these symptoms through their own activities should be emphasized. Strong consensus Comment. The recommendations of the FMS guidelines on the basic measures were adapted based on the recommendations for the German (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF) S3 guideline recommendations for the management of patients with “non-specific, functional and somatoform physical complaints” [15]. 2 | Der Schmerz 3 · 2012 Clinical point of consensus Comorbid mental disorders and physical illnesses should be treated according to the current guidelines. EL 2a (indirect evidence), strong consensus Comment. For the treatment of common comorbid disorders other than FMS (e.g., back pain, arthritis and depression), the evidence and recommendation grades for individual therapeutic procedures are found in the relevant guidelines [9, 11, 22]. Therapy evaluation Clinical point of consensus The benefits (symptom reduction and performance improvement versus side effects and cost) should be regularly evaluated by patients and clinicians. Therapy should only be continued in the case of a positive benefit. Strong consensus Comment. The time frame of the evaluation may be different for drug and nondrug therapies. In the first 2 weeks of drug therapy, the compatibility (collection of subjective side effects) of the medication is especially important. The assessment of the effectiveness of the treatment is usually possible after 4 weeks [32]. If benefits (the positive effects that outweigh the side Clinical point of consensus For mild forms of FMS, the patient should be encouraged to perform adequate physical and psychosocial activity. Strong consensus Comment. The distinction between mild and severe cases can be found in the chapter “Definition, classification and diagnosis of fibromyalgia syndrome” [12]. The recommendations for the FMS guidelines on basic measures were adapted based on the German S3 guideline “Recommendations for the management of patients with non-specific, functional and somatoform physical complaints” [15]. Psychosocial activity involves mental activity and the maintenance of hobbies and social contact. Severe cases Clinical point of consensus In severe cases, physical therapy, temporary drug therapy and multimodal therapy should be discussed with the patient. Consensus Note: “multimodal” — at least one physically activity with at least one psychotherapeutic procedure Comment. The distinction between mild and severe cases can be found in the chapter “Definition, classification and diagnosis of fibromyalgia syndrome” [12]. The recommendation for initial therapy is based on the recommendation degree of the therapies mentioned (strong recommendation). The recommendations of the FMS guidelines on basic measures were adapted based on the German (AWMF) S3 guideline “Recommendations for the management of patients with non-specific, functional and somatoform physical complaints” [15]. Abstract · Zusammenfassung Lack of response to multimodal therapy in severe cases Schmerz 2012 · DOI 10.1007/s00482-012-1167-z © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 Clinical point of consensus W. Eich · W. Häuser · B. Arnold · K. Bernardy · W. Brückle · U. Eidmann · K. Klimczyk · V. Köllner · H. Kühn-Becker · M. Offenbächer · M. Settan · M. von Wachter · F. Petzke The patients with severe cases who do not respond adequately to the above mentioned measures should be treated with multimodal programs following the German Operations and Procedures Code (“Operationen- und Prozedurenschlüssel”, OPS) and using disorder-specific psychological and/or drug therapy for physical comorbidities. Strong consensus Comment. According to the German OPS, multimodal therapy is performed in the context of multimodal complex treatments, e.g., (semi-)inpatient multimodal pain therapy (OPS paragraphs 8-91c and 8-918.x), multimodal rheumatologic complex treatment (OPS paragraph 8-983.01/2) or an inpatient psychosomatic–psychotherapeutic hospital treatment (OPS paragraph 9-60.x to 9-64.x). Multimodal pain management requires an interdisciplinary diagnosis in at least two disciplines (compulsory psychiatric, psychosomatic or psychological discipline) and is characterized by the concomitant use of at least three of the following active therapy procedures under medical supervision: psychotherapy, special physiotherapy, relaxation treatment, occupational therapy, medical training therapy, sensorimotor training, workplace training, art or music therapy or other exercise therapies. Multimodal pain management also includes a review of the treatment process through a standardized therapeutic assessment with interdisciplinary team discussion [4]. The intensity of multimodal pain therapy for patients with severe cases of chronic pain syndromes should be >100 h (>25 h of psychotherapy) [26]. The integration of specific modules for mental disorders (e.g., major depression) in multimodal programs is recommended [17]. Regarding disorder-specific psychological and/or drug therapy for unipolar depression, refer to the national guidelines [11]. Fibromyalgia syndrome. General principles and coordination of clinical care and patient education Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinäre Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. A diagnosis of FMS should be explicitly communicated with the afflicted individual. A step-wise treatment, depending on the severity of FMS and the responses to therapeutic measures, is recommended. Therapy should only be continued if the positive effects outweigh the side effects.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Review, systematic · Meta-analysis · Guidelines · Coordination of care · Patient education Das Fibromyalgiesyndrom. Allgemeine Behandlungsgrundsätze, Versorgungskoordination und Patientenschulung Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchischer Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center of Evidence Based Medicine. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Die Diagnose eines FMS soll dem Betroffenen explizit mitgeteilt werden. Eine stufenweise Behandlung in Abhängigkeit vom Schweregrad des FMS und dem Ansprechen auf Therapiemaßnahmen wird empfohlen. Therapien sollen nur fortgeführt werden, wenn die positiven Wirkungen die Nebenwirkungen überwiegen. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Versorgungskoordination · Patientenschulung Der Schmerz 3 · 2012 | 3 Schwerpunkt Duration of drug therapy Evidence-based recommendation In the case of a response to drug therapy, after a treatment duration of at least 6 months, a drug cessation trial should be considered for the patient. EL 2a (indirect evidence), recommendation, consensus Comment. The maximum duration of the RCT study with amitriptyline, duloxetine and pregabalin was 6 months [31]. The results of subsequent open RCT studies conducted for up to 6 months showed a sustained reduction in symptoms for only a subset of patients. Duration of endurance training Evidence-based recommendation The patients who experience an improvement with aerobic endurance training should continue this training permanently. EL 1a, strong recommendation, strong consensus Comment. Only for aerobic training was it shown through RCTs that the positive effects at the initiation of training disappear after some time, yet persist with continuous exercise [35, 36]. At the beginning of endurance training, instruction by trainers/physical therapists experienced in the care of chronically ill people may be useful to match the intensity level to individual performance, which is necessary to achieve symptom reduction, e.g., in the form of formulated functional training. The purpose of this guide is to enable afflicted individuals to have independent endurance training (either alone or in a sports group) [28]. Long-term therapy Clinical point of consensus For long-term therapy, procedures that afflicted individuals can perform independently (e.g., individual performance for adapted endurance and/or strength training, stretching or heat therapy) should be used for the purpose of selfmanagement. Strong consensus 4 | Der Schmerz 3 · 2012 Comment. For this consensus point, procedures that have a proven efficacy for their temporary use have been recommended. The long-term use of these measures can be implemented to a large extent and carries little risk. F cognitive behavioral therapy: patient education, psychoeducation and exercises/homework on behavioral change with individual feedback by a psychotherapist (direct personal contact or Internet contact). Coordination of care For the analysis, the two methods of education and psychoeducation were combined. Studies with cognitive behavioral therapy are referenced in the psychotherapy paper [34]. The literature search yielded 934 hits. The results of two studies were published twice [6, 7, 25, 37]. One study was excluded from the meta-analysis because patient education was combined with other methods [21]. One study was excluded because the results for the FMS subgroup were not reported [30]. Fourteen studies (of which four were with psychoeducation) with 1,053 patients and an average treatment duration of 10 (6– 20) weeks were qualitatively analyzed (Evidence report, Tab. 1) [5, 7, 8, 10, 13, 14, 16, 19, 20, 24, 27, 29, 33, 39]. The quality of evidence was moderate (moderate methodological quality, moderate external validity; Evidence report, Tab. 2). Patient education was inferior in the control groups with respect to the selected target variables (Evidence report, Tab. 3 and Fig. 1). The standardized mean differences (SMDs; patient education group versus control group) were not very useful for determining effectiveness because in some studies, patient education served as the control group and a higher therapeutic dose was used in the active treatment group. The results of selfefficacy for pain were inconsistent; three studies showed no improvement in selfefficacy (at the beginning and the end of therapy) in the education group [8, 16, 20], and three studies showed an improvement [19, 26, 28]. Education was superior to pain self-efficacy with respect to pain improvement in one study of a wait-list control group [29]. In one study, aerobic training and multimodal therapy were superior to education with respect to the improvement in pain self-efficacy [27]. The acceptance was low (38% dropout rate) and did not differ significantly from that of the control group (Evidence report, Fig. 1). The side effects were not systematically collected or reported. The side ef- Long-term therapy Clinical point of consensus Treatment coordination should, if possible, be performed by a doctor who has the necessary knowledge and experience in the treatment of FMS. Consensus Comment. No specialist in Germany considers him/herself to be predestined to assume a “pilot” role for FMS patients. It is therefore recommended that affected individuals consult a doctor who has knowledge and experience in the treatment of FMS patients and who is prepared to assume a pilot role. Based on the experience of those afflicted, it may be difficult in rural areas of Germany to find a suitable physician close to home. Patient education Evidence-based recommendation Patient and psychological education can be considered a basic measure. EL 1a, open recommendation, strong consensus Comment. The boundaries between patient education, psychoeducation and cognitive behavioral therapy are fluid. The various education methods have been distinguished as follows: F education (patient education): information regarding the disease and course of treatment in a group and/or in writing and/or on the Internet by a qualified person, fostering discussion and emotional exchange within a group; F psychoeducation: patient education and information/motivation for selfmanagement (e.g., physical activity and stress reduction) in group lectures and/or in writing and/or on the Internet by a qualified person; and fects of patient education are very rare and minor. Patient education sessions are offered by FMS self-help organizations on an outpatient basis and are part of (semi-)inpatient treatment programs. Informing patients regarding the diagnosis and treatment possibilities is an ethical obligation. Due to the high feasibility, low risks and ethical obligation, an upgrade of the recommendation level by two levels was recommended. Psychoeducation is essential as a preparation for active therapy. Patient-centered communication Evidence-based recommendation Patient-centered communication can be used. EL 3a, open recommendation, strong consensus Comment. This analysis included studies in which the doctors received special training in patient communication, such as shared decision-making [6] and communication skills (e.g., information exchange, conversational structure and empathy) [23]. The literature search yielded 20 hits. Two studies with 148 patients and treatment durations of 1 and 52 weeks were used in the analysis [2, 5, 6, 23]. In one study, a follow-up examination was conducted after 52 weeks (Evidence report, Tab. 4). Due to the small sample size, gradation of the evidence was decreased by 2°. Quantitative data synthesis was not possible due to the different time measurement points. Patient-centered communication was not effective based on the specified endpoints. Patient-centered communication and shared decision making improved the quality of the doctor– patient relationship from both the patient and physician points of view [6]. The patients appreciated the communication skills of doctors who had received training in patient-centered communication more than those of doctors in the control group (typical medical communication). The acceptance was moderate. The dropout rate was 25/107 (23.4%) and did not differ significantly from that of the control group. Side effects were not detected and were not expected. Patient- centered communication can be provided within psychosomatic primary care. Including patients in the decision-making process is an ethical obligation. Due to the lack of risks, the high feasibility and ethical obligations, an upgrade of the recommendation by 2° was made. The following recommendations of the first guideline remain valid Transfer to the hospital by general practitioner/specialist Clinical point of consensus Treatment of FMS is usually on an outpatient basis. In the following situations, admission to a hospital is recommended: Finpatient treatment needs for comorbid physical and mental disorders and F(semi-)inpatient multimodal pain therapy. The indication for (semi-)inpatient treatment from the hospital doctor is based on the inclusion-indication lists of medical societies such as the inclusion indication list (“Aufnahmeindikationsliste”, AIL) of the German Society for the Study of Pain [1]. Strong consensus Cause for (semi-)inpatient rehabilitation measurements Clinical point of consensus Instigation of (semi-)inpatient rehabilitation measures is recommended, based on the criteria of the International Classification of Functioning (ICF), when Fparticipation in the labor force is at risk, Fparticipation in social life or ability for self-sufficiency is at risk, and Fstrongly recommended outpatient therapeutic measures are unavailable or insufficiently effective. Strong consensus Discussion established doctors, hospitals and physicians in acute care hospitals and rehabilitation facilities), the strong consensus that was reached for all recommendations is emphasized. The recommendations for treatment and coordination of care were adapted to the existing health care structure in Germany. In addition to the first guideline, stepwise care (depending on the response to recommended therapies) graded according to the severity of FMS treatment was included. The following care and research requirements exist: FFurther development of care structures and processes: 1cooperationandnetworkingacross fields, 1avoidance of overcare, undercare and lack of care, and 1advancement of existing care structures, including a comprehensive offering of high quality care near the patient’s home. F Therapy: 1definition of responder criteria (a combination of several core symptoms of FMS), 1identification of predictors for a positive and negative treatment outcome, 1studies on “optimal dose finding” for non-drug therapies, 1evaluation of graded treatment models, and 1studies on the indication for and effectiveness of rehabilitation. Corresponding address Prof. Dr. W. Eich Department of General Internal and Psychosomatic Medicine, Heidelberg Medical University Hospital Im Neuenheimer Feld 10, 69210 Heidelberg Germany wolfgang.eich@med.uni-heidelberg.de Conflict of interest. See Tab. 5 in “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. Given the different interests of the people involved in establishing the guidelines (patients, clinicians, doctors, psychologists, general practitioners, specialists, Der Schmerz 3 · 2012 | 5 Schwerpunkt References 1. AdHoc Kommission AEP/DRG der Deutschen Gesellschaft zum Studium des Schmerzes (2004) DGSS. Aufnahmeindikationsliste [Inclusion-Indication List]. (English version: Ad Hoc Commission AEP/DRG of the German Society for the Study of Pain) http://www.dgss.org/fileadmin/pdf/ail.pdf. Accessed 04 May 2012 2. Alamo MM, Moral RR, Pérula de Torres LA (2002) Evaluation of a patient-centred approach in generalized musculoskeletal chronic pain/fibromyalgia patients in primary care. Patient Educ Couns 48:23–31 3. Annemans L, Wessely S, Spaepen E et al (2008) Health economic consequences related to the diagnosis of fibromyalgia syndrome. Arthritis Rheum 58:895–902 4. Arnold B, Häuser W, Bernateck M et al (2012) Systematische Übersicht, Metaanalyse und Leitlinie: Multimodale Therapie des Fibromyalgiesyndroms (Systematic review, meta-analysis and guidelines: multimodal therapy for fibromyalgia syndrome). Schmerz 26:287-290 5. Astin JA, Berman BM, Bausell B et al (2003) The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J Rheumatol 30:2257–2262 6. Bieber C, Muller KG, Blumenstiel K et al (2006) Long-term effects of a shared decision-making intervention on physician-patient interaction and outcome in fibromyalgia. A qualitative and quantitative 1 year follow-up of a randomized controlled trial. Patient Educ Couns 63:357–366 7. Bieber C, Müller KG, Blumenstiel K et al (2008) A shared decision-making communication training program for physicians treating fibromyalgia patients: effects of a randomized controlled trial. J Psychosom Res 64:13–20 8. Buckelew SP, Conway R, Parker J et al (1998) Biofeedback/relaxation training and exercise interventions for fibromyalgia: a prospective trial. Arthritis Care Res 11:196–209 9. Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) (2010) Nationale Versorgungsleitlinie Kreuzschmerz – Langfassung Version 1.X. (cited: 24.05.11) (German Medical Association (GMA), National Association of Statutiry Health Insurance Physicians (NASHIP), Association of the Scientific Medical Societies of Germany (AWMF) (2010) National Disease Management Guidelines Programme – Long version). http://www.versorgungsleitlinien.de/themen/kreuzschmerz. Accessed 4 May 2012 10. Burckhardt CS, Mannerkorpi K, Hedenberg L, Bjelle A (1994) A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol 21:714–720 11. DGPPN, BÄK, KBV et al (eds) für die Leitliniengruppe Unipolare Depression (English version: DGPPN, GMA, NASHIP et al (eds) for the Unipolar Depression Guidelines Group). http://www.depression. versorgungsleitlinien.de/. Accessed 4 May 2012 12. Eich W et al (2012) Definition, Klassifikation und Diagnose des Fibromyalgiesnydroms (English version: Definition, classification and diagnosis of fibromyalgia syndrome). Schmerz 26:247-258 13. Fontaine KR, Haas S (2007) Effects of lifestyle physical activity on health status, pain, and function in adults with fibromyalgia syndrome. J Musculoskeletal Pain 15:3–9 6 | Der Schmerz 3 · 2012 14. Fontaine KR, Conn L, Clauw DJ (2010) Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Res Ther 12:R55 15. Hausteiner-Wiehle C, Schäfert R, Sattel H et al (Steuerungsgruppe [Supervisory team]) (2012) S3Leitlinie zum Umgang mit Patienten mit nicht-spezifischen, funktionellen und somatoformen Körperbeschwerden (English version: S3 guidelines for handling patients with non-specific, functional and somatoform physical complaints) (in press) 16. King SJ, Wessel J, Bhambhani Y et al (2002) The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol 29:2620–2627 17. Lange M, Petermann F (2010) Influence of depression on fibromyalgia: a systematic review. Schmerz (Pain) 24:326–333 18. Lamotte M, Maugars Y, Le Lay K, Taïeb C (2010) Health economic evaluation of outpatient management of fibromyalgia patients and the costs avoided by diagnosing fibromyalgia in France. Clin Exp Rheumatol 28 (Suppl 63):64–70 19. Lorig KR, Ritter PL, Laurent DD, Plant K (2008) The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum 59:1009–1017 20. Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C (2000) Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol 27:2473–2481 21. Mannerkorpi K, Nordeman L, Ericsson A et al (2009) Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med 41:751–760 22. National Institute for Clinical Excellence and Health (NICE) guideline 59. Osteoarthritis. The care and management of adults with osteoarthritis, http://guidance.nice.org.uk/CG59/Guidance/pdf/ English. Accessed 4 May 2012 23. Moral RR, Alamo MM, Jurado MA, Torres LP de (2001) Effectiveness of a learner-centred training programme for primary care physicians in using a patient-centred consultation style. Fam Pract 18:60–63 24. Nicassio PM, Radojevic V, Weisman MH et al (2000) A comparison of behavioral and educational interventions for fibromyalgia. J Rheumatol 24:2000– 2007 25. Oliver K, Cronan TA, Walen HR, Tomita M (2001) Effects of social support and education on health care costs for patients with fibromyalgia. J Rheumatol 28:2711–2719 26. Pöhlmann K, Tonhauser T, Joraschky P, Arnold B (2009) The Dachau multidisciplinary treatment program for chronic pain. Efficacy data of a diagnosis-independent multidisciplinary treatment program for back pain and other types of chronic pain. Schmerz 23:40–46 27. Rooks DS, Gautam S, Romeling M et al (2007) Group exercise, education, and combination selfmanagement in women with fibromyalgia: a randomized trial. Arch Intern Med 167:2192–2200 28. Winkelmann A et al (2012) Physiotherapie und physikalische Therapie des Fibromyalgiesyndroms (English version: physiotherapy and physical therapy for fibromyalgia syndrome). Schmerz 26:276286 29. Soares JJM, Grossi G (2002) A randomised, controlled comparison of educational and behavioural interventions for woman with fibromyalgia. Scand J Occup Ther 9:35–45 30. Solomon DH, Warsi A, Brown-Stevenson T et al (2002) Does self-management education benefit all populations with arthritis? A randomized controlled trial in a primary care physician network. J Rheumatol 29:362–368 31. Sommer et al (2012) Medikamentöse Therapie des Fibromyalgiesyndroms (Drug therapy for fibromyalgia syndrome). Schmerz (in press) 32. Straube S, Derry S, Moore RA et al (2010) Pregabalin in fibromyalgia-responder analysis from individual patient data. BMC Musculoskelet Disord 5:150 33. Stuifbergen AK, Blozis SA, Becker H et al (2010) A randomized controlled trial of a wellness intervention for women with fibromyalgia syndrome. Clin Rehabil 24:305–318 34. Thieme K et al (2012) Psychotherapie bei Patienten mit Fibromyalgiesyndrom (Psychotherapy in patients with fibromyalgia syndrome). Schmerz (in press) 35. Tomas-Carus P, Häkkinen A, Gusi N et al (2007) Aquatic training and detraining on fitness and quality of life in fibromyalgia. Med Sci Sports Exerc 39:1044–1050 36. Tomas-Carus P, Gusi N, Häkkinen A et al (2008) Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. J Rehabil Med 40:248–252 37. Vlaeyen JW, Teeken-Gruben NJ, Goossens ME et al (1996) Cognitive-educational treatment of fibromyalgia: a randomized clinical trial. I. Clinical effects. J Rheumatol 23:1237–1245 38. White KP, Nielson WR, Harth M et al (2002) Does the label “fibromyalgia” alter health status, function, and health service utilization? A prospective, within-group comparison in a community cohort of adults with chronic widespread pain. Arthritis Rheum 47:260–265 39. Williams DA, Kuper D, Segar M et al (2010) Internet-enhanced management of fibromyalgia: a randomized controlled trial. Pain 151:694–702 Schwerpunkt English Version of "Physiotherapie und physikalische Verfahren beim Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie". DOI 10.1007/s00482-012-1171-3 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 A. Winkelmann1 · W. Häuser2 · E. Friedel3 · M. Moog-Egan4 · D. Seeger5 · M. Settan6 · T. Weiss7 · M. Schiltenwolf8 1 Klinik und Poliklinik für Physikalische Medizin und Rehabilitation, Klinikum der Universität München, Munich 2 Innere Medizin 1, Klinikum Saarbrücken 3 Klinik Bad Kissingen, Kissingen 4 Neuro Orthopaedic Institute, Adelaide 5 Schmerztagesklinik und –ambulanz, Universitätsmedizin Göttingen 6 Deutsche Fibromyalgie Vereinigung, Bad Seckach 7 Praxisklinik Mannheim 8 Konservative Orthopädie, Orthopädische Universitätsklinik, Heidelberg Physiotherapy and physical agent therapies for fibromyalgia syndrome Systematic review, meta-analysis and guidelines The board of the working groups proposed following questions for the planned revision of the guidelines: 1.Do physiotherapy and therapy agent treatments provide short- and longterm effect for the treatment of fibromyalgia syndrome (FMS)? 2.Which risks are associated with the use of physiotherapy and therapy agents (i.e., passive treatment modalities such as hot/cold packs, massage, electrotherapy, laser and ultrasound) for the treatment of FMS? 3.Which physiotherapy and therapy agent treatments are not recommended for the treatment of FMS? Results Materials and methods Aerobic training with low to moderate intensity (e.g. faster walking, Nordic walking, cycling or ergometer training, dancing, aqua jogging) should be implemented 2–3 times per week for at least 30 continuous minutes. EL1a, strong recommendation, strong consensus The methods used for the literature search and analysis, and for the compilation of the recommendations are reported in the article “Methodological fundamentals used in developing the guidelines”. Preliminary note: the following statements and recommendations are aimed at adults. For the general treatment objectives and treatment coordination for children and teenagers, please refer to the article “Definition, diagnosis and therapy for chronic pain and so-called fibromyalgia syndrome in children and adolescents”. Key recommendations are italicized. Strong recommendation Aerobic training Evidence-based recommendation Comment. For the analysis, studies with physical training, in which at least 60% of the therapy time was spent on aerobic training, were included. Studies, in which aerobic training was combined with psychological therapies, are included and listed in the article “Multicomponent therapy for fibromyalgia syndrome”. For the classification of the intensity of the aerobic training, following criteria were used: Flow intensity: 50–70% Hfmax (maximal heart rate), Fmoderate intensity: 70–85% Hfmax and Fhigh intensity: 85–100% Hfmax. The literature search produced 285 results. Two studies were excluded from the analysis, as the reported clinical end stage did not meet our inclusion criteria [102, 112]. Fourty two studies [1, 4, 10, 15, 19, 22, 27, 28, 29, 33, 36, 40, 44, 45, 49, 53, 55, 58, 60, 66, 67, 70, 72, 74, 76, 77, 81, 82, 84, 87, 89, 90, 91, 93, 95, 100, 101, 105, 109, 111, 112, 116], with a total of 2,071 patients and an average duration time of the study of 12 (3–24) weeks, were included in the qualitative analysis. A total of 16 studies carried out a follow-up at an average of 41 (4–208) weeks (Evidence Report, Tab. 6). Der Schmerz 3 · 2012 | 1 Schwerpunkt The quality of the evidence was moderate (moderate methodological quality, moderate external validity) (Evidence Report, Tab. 7) The efficacy was high. The standard mean differences (SMDs; aerobic training—controls) at the end of the therapy on pain, fatigue and quality of life were low. The SMDs (aerobic training—controls) at follow-up for pain and quality of life were low (Evidence Report, Tab. 8 and Fig. 2). The subgroup analysis showed no difference between land-based and waterbased, or a combination of both, aerobic training. Studies in which the patients continued to implement the aerobic training program showed long-term (>3 months) effectiveness at follow-up. Most of the studies implemented an aerobic training program with low to moderate intensity for 30 min at least twice a week. The acceptance was moderate (dropout rate 223/932=24%) and was not greatly different from that of the controls (Evidence Report, Fig. 2). Side effects were not systematically recorded. Relevant side effects, such as stress fractures, high blood pressure and cardiac dysrhythmia were reported as individual cases. Aerobic training can be done independently or a part of a sports group, if necessary with guidance as part of the physiotherapy treatment or sport therapy group. Strength training Evidence-based recommendation Low to moderate intensity strength training should be employed. There is evidence for a training frequency of 60 min twice a week. EL1a, strong recommendation, strong consensus Comment. The literature search produced 57 studies. Three studies were excluded from the analysis, as they did not meet the inclusion criteria; one study was excluded, as it did not have an appropriate control group [51, 78, 107, 108]. Six randomised, controlled trials (RCTs) with 246 patients and average study duration of 17 (12–21) weeks were analysed [5, 50, 57, 61, 87, 109]. A followup was only carried out in one study after 12 weeks (Evidence Report, Tab. 9). The quality of the evidence was moderate 2 | Der Schmerz 3 · 2012 (moderate methodological quality, moderate external validity; Evidence Report, Tab. 10). The efficacy was moderate. The effect size in comparison to the controls (usual care, stretching) on pain, sleep and fatigue at the end of the therapy was moderate (Evidence Report, Tab. 11 and Fig. 3). Side effects were not systematically recorded. The dropout rate in the studies was 18.6% and not greatly different than that of the control groups (Evidence Report, Fig. 3). Strength training is available as part of the physiotherapy treatment paid for by the social health insurance and/or can be performed independently following initial guidance by the physiotherapist or sport instructor. ties budget2. The quality assurance of the additional qualification and continuous education of the therapists is the sole responsibility of the association offering the functional training [83]. The German fibromyalgia association and the German rheumatism league offer courses for functional trainers. These courses are recognised by both the social health insurance and pension insurance. Functional training consists of both aerobic training and stretching exercises. Thus there exists indirect evidence for the efficacy (see recommendations “Aerobic training” and “Functional training”). As it is coupled with low risks and high patient preference, a higher recommendation has been made. Functional training1 Thermal baths Recommendations Evidence-based recommendation Evidence-based recommendation Functional training (land- and waterbased callisthenics) should be carried out twice a week, for at least 30 min each. EL 2a, strong evidence, strong consensus Thermal baths should be used. There is evidence available, which supports thermal baths 5 times a week over a period of 2–3 weeks. EL 1a, recommendation, strong consensus Comment. Functional training (landand water-based callisthenics in groups under the guidance of a physiotherapist) is a benefit offered by the social health insurance and pension insurance and can be prescribed for FMS for a duration of 24 months. A prescription for a longer period of time is possible, but only after individual revision and when the benefits are necessary, appropriate and affordable. It can be particularly necessary, when cognitive or psychological impairment does not allow for the long-term accomplishment of the exercise program without the guidance of a physiotherapist [59]. The functional training in qualified exercise groups is encouraged as additional service to rehabilitation related to § 43, paragraph 1 sentence 1 SGB V in combination with § 44 paragraph 1 number 4 SGB IX and is not part of the healthcare modali- Comment. The literature search found 142 studies. Studies which included physical exercise (aerobic training, stretching, breathing exercises) in warm water are included in the section “Aerobic training” and “Stretching”. In this section studies regarding balneo therapy (moor bath, steam bath, sand bath and sauna), hydrotherapy (warm water including whirlpool), spa therapy (bathing in mineralised water) and thalasso therapy (bathing in salt water) are summarised. Studies, which included hydrogalvanic baths, were analysed separately. One study, which included sauna treatment, was excluded due to missing randomisation [80]. One study, which used moor packs as treatment, was also excluded, as an additional therapy with trazadone was included [14]. Two studies were 2 1 Functional training and rehabilitation sport were devised by the pension insurance and the rheumatic league in Germany to encourage patients with pain and chronic mobility limitation to move (again) as well as improve social interaction in a group setting. In Germany, the prescription of physiotherapy treatment and related therapy agents is regulated by a healthcare modalities budget (“Heilmittel Budget”). This budget determines the number and modalities of treatment that can be prescribed and must be strictly adhered to by the medical practitioner. Abstract · Zusammenfassung excluded from the meta-analysis, as these studies included a combination of multimodal treatment [63, 118]. One study was excluded, as the results of the FMS patients were not recorded separately [96]. The results from one study was published twice [20, 75]. Seven studies with 396 patients and average treatment duration of 4 (1.2–12) weeks were included in the analyses [4, 6, 7, 20, 31, 32, 39, 63]. Five studies included follow-ups after an average of 20 (6–36) weeks (Evidence Report, Tab. 12). A quantitative analysis of five studies, which included thermal baths as treatment, was possible. The quality of the evidence was moderate (moderate methodological quality, moderate external validity) (Evidence Report, Tab. 13). The efficacy was low. The SMD (thermal bath—controls) on pain at the end of the therapy was high (Evidence Report, Tab. 14 and Fig. 4). The acceptance was high (drop-out rate of 5%) and did not differ greatly from the controls (Evidence Report, Fig. 4). The risks were presumably moderate: side effects were not systematically recorded. Individual cases of skin changes and cardiac dysrhythmia were described. Thermal baths as a treatment of choice for chronic pain syndromes are not listed in the health care catalogue3. The availability is reduced (costs for self payment, not available in all rehabilitation centers). Open recommendations Stretching Evidence-based recommendation Stretching and flexibility training can be considered. There is evidence available for a training frequency of 2–3 times 60 min/week. EL 2a, recommendation open, strong consensus Comment. The literature search found 85 studies. Seven studies with eight treatment arms and a total of 322 patients and 3 In Germany a so-called health care catalogue (“Heilmittel Katalog”) governs what can be prescribed for which diseases and diagnoses. It also governs the total amount of treatments that can be prescribed and is closely related to the health care budget. Schmerz 2012 · DOI 10.1007/s00482-012-1171-3 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 A. Winkelmann · W. Häuser · E. Friedel · M. Moog-Egan · D. Seeger · M. Settan · T. Weiss · M. Schiltenwolf Physiotherapy and physical agent therapies for fibromyalgia syndrome. Systematic review, meta-analysis and guidelines Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinären Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields. Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for Evidence-Based Medicine. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. Low to moderate intensity aerobic exercise and strength training are strongly recommended. Chiropractic, laser therapy, magnetic field therapy, massage and transcranial current stimulation are not recommended.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Review, systematic · Meta analysis · Guideline · Aerobic exercise Physiotherapie und physikalische Verfahren beim Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke average treatment duration of 14 (5–20) weeks were included in the analysis [5, 21, 69, 70, 105]. Three studies included a follow-up after 12 weeks (Evidence Report, Tab. 15). erfolgte nach dem Schema des Oxford Center for Evidence Based Medicine. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Ausdauer- und Krafttraining geringer bis mittlerer Intensität werden stark empfohlen. Chirotherapie, Lasertherapie, Magnetfeldtherapie, Massage und transkranielle Magnetstimulation werden nicht empfohlen. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Aerobes Training The quality of evidence was moderate (minimal methodological quality, high external validity) (Evidence Report, Tab. 16). The low methodological quality meant that the level of evidence was adjusted down. Der Schmerz 3 · 2012 | 3 Schwerpunkt At the end of treatment, the effect of stretching on the reduction of pain and restrictions on the quality of life was inferior to the active control groups (Evidence Report, Tab. 7 and Fig. 4). The acceptance was moderate (dropout rate of 15%) and did not differ greatly from the controls (Evidence Report, Fig. 5). The practical applicability is high: within the treatment scope for physiotherapy, stretching is included in the health care catalogue and/or can be accomplished by the patients on their own following supervision by the physiotherapist. Based on the minimal risks and the practicality of stretching, the recommendation level is upgraded by one level. Strong negative recommendations Massage Evidence-based recommendation Massage should not be used. EL 2a, EG strong negative recommendation, strong consensus Comment. The literature search found 228 studies. One study with self-massage and stretching was excluded [36]. One study was excluded, as the clinical endpoints did not meet the inclusion criteria [63]. Six RCTs with 213 patients and average treatment duration of 8 (3–20) weeks were analysed [3, 17, 25, 34, 37, 97]. Three studies included a follow-up after 25 (24– 26) weeks (Evidence Report, Tab. 18). The quality of evidence was low (Evidence Report, Tab. 9). Due to the low quality of the evidence, a downgrade of the evidence level was made. Massage was not effective (Evidence Report, Tab. 20 and Fig. 6). The acceptance was high (dropout <10%) and did not differ significantly from the controls (internet evidence report illustration 6). Side effects were not systematically recorded or reported. The availability is complete. Massage for chronic pain syndromes (including FMS) is listed in the health care catalogue. Quadrant intervention Evidence-based observation An operative quadrant operation should not be performed. EL 4, strong negative recommendation, strong consensus Comments. The literature search found three studies. In contrast to current knowledge of the ethiopathogenesis and pathophysiology for FMS, Bauer [11, 12] assumes that FMS can be traced to the compression of vascular-neural bundles at acupressure points. The efficacy of this is not clearly established. A microsurgical release of the ‘adhesion’ (so called quadrant intervention) in a case study of 118 patients lead to freedom from pain in 60% of the patients [11, 12]. The results of the follow-ups (up to 12 months later) of 700 patients, who were operated on between 2003 and 2005, have only been published on Bauer’s homepage on the internet. The for spring 2009 announced data for the three year follow-up, have to date not been published [13]. This treatment method has as yet not been tested by other authors or in other studies. Neither has the author of the quadrant intervention compared this treatment method with effective treatment methods such as medication and aerobic training. The potential risks of the operation (e.g., wound infection, adhesion) are high. The applicability is minimal. The costs of the operation are not covered by the social health insurance or by the private health insurance. Based on the potential risks, the lack of applicability, and the ethical obligations (preservation of the patient from physical and financial damages), the level of recommendation has been downgraded by 2 levels. Negative recommendations Chiropractic Evidence-based recommendation Chiropractic should not be implemented. EL 3a, negative recommendation, strong consensus Comment. Studies with craniosacral therapy are listed in a separate heading. 4 | Der Schmerz 3 · 2012 The literature search found 25 studies. One study was published as a poster for a study protocol [115]. Three RCTs with 100 patients were analysed (Evidence Report, Tab. 21). As the methodological quality of the studies was low (Evidence Report, Tab. 22) and the number of studies analysed also low, the level of evidence was downgraded by two levels. A quantitative data analysis could not be carried out, as the predetermined variables were not recorded or reported. The qualitative data analysis did not result in a consistent indication of the efficacy of treatment. In one study, chiropractic was no more effective than being on the waiting list in regards to pain reduction [16]. In another study, chiropractic in combination with electrotherapy resulted in a reduction in pain in some patients [102]. In a further study, strength training alone and in combination with chiropractic treatment lead to an improvement in the quality of life [78]. None of the studies reported side effects to the treatment. The dropout rate was between 0 and 10%. Rare and grave complications (e.g., dissection of the carotid artery) have been reported in the literature [43]. Chiropractic is not listed as a prescribed treatment for chronic pain syndromes in the health care catalogue. Hyperbaric oxygen therapy Evidence-based statement Hyperbaric oxygen therapy should not be used. EL 3a, negative recommendation, strong consensus Comment. The literature search found nine studies. In one RCT 26 patients, who had 15 sessions of hyperbaric oxygen therapy, were compared with 24 patients in the control group (usual care). At the end of the treatment series, there was a greater reduction in the level of pain in the patients in the hyperbaric oxygen therapy group compared with the control group. Side effects were not reported [117]. The quality of evidence in the study was low. Hyperbaric oxygen therapy for the treatment of FMS is not included in the health care catalogue. Serious complications are reported in the literature [71, 85]. Thus a negative recommendation was made. Cold (chamber) therapy Laser therapy Evidence-based recommendation Evidence-based recommendation Cold chamber therapy should not be used as a treatment of choice. EL 3b, negative recommendation, strong consensus Laser therapy should not be used. EL 3a, negative recommendation, strong consensus Comment. The literature search found 36 studies. The results of a nonrandomised crossover study were not included, as the clinical end point was reached after 24 h after the treatment [88]. In a case study with 120 patients (41% with FMS) the short-term effects of full body cold treatment (cold chamber) were examined. A separate analysis of the FMS patients was not published. A short-term reduction in pain, (average of 1.5 h) by half of the initial pain level, was reported. At the end of the 4-week treatment period, an average pain reduction of 13% was reported, which most likely is due to the treatments, which were carried out along side the cold chamber treatment. A total of 55 of 120 patients, mainly with FMS, discontinued the cold chamber treatment [73]. In regards to side effects, 7% of the participants reported burns, headaches, shortness of breath, dizziness, increase in pain intensity and anxiety. In one RCT 28 patients were treated with infrared light and 38 patients with cold chamber. The dropout rate for the cold chamber was 47%, for the infrared light treatment 0%. The patients, who discontinued the cold chamber treatment, did not differentiate in the level of pain reduction from the group receiving the infrared light treatment (both groups showed significant improvement in the level of pain reduction) [63]. The methodological quality of the studies was low. The quality of evidence for cold therapy is low. Efficacy (continued pain reduction) is not shown. The level of acceptance is low, the potential risks high. Thus the recommendation level is reduced by one level. Dissenting opinion from the patient selfhelp groups: The experience of individual patients is very positive. Comment. The literature search found 46 studies. Two studies were excluded from the analyses as laser therapy was combined with other physical therapy modalities [62, 69]. Three studies with 122 patients, and average treatment duration of 2 weeks, were analysed [8, 47, 48] (Evidence Report, Tab. 23). The quality of evidence was low (Evidence Report, Tab. 24). Due to the small number of cases and the low quality level of evidence, a downgrade of 2 levels of evidence was made. The level of efficacy was moderate. The SMDs (laser—sham laser) at the end of the treatment were high for pain and moderate for tiredness and sleep (Evidence Report, Tab. 25 and Fig. 7). The level of acceptance was high (dropout rate 0%) (Evidence Report, Fig. 7). Side effects were not reported. In the studies, laser therapy was applied at a low level of energy. At higher levels of energy, e.g., 7-W Laser, improper use can not only lead to heat reaction, but also to tissue damage. The practicality is low. Laser therapy for FMS is not listed in the health care catalogue. This treatment method is not offered in routine clinical practice. Due to the potential risks and the lack of availability, a downgrade of the recommendation level followed. Magnetic field therapy Evidence-based recommendation: Magnetic field therapy should not be used. EL 2a, negative recommendation, strong consensus Comment. The literature search found 30 studies. One experimental study with one single treatment was excluded from the analysis [94]. Four studies with five study arms and 178 patients and average treatment duration of 11 (1–26) weeks were included in the analysis (Evidence Report, Tab. 26; [2, 26, 98, 99]). The low number of participants (<200) in the studies re- sulted in a downgrading of the level of evidence. The quality of evidence was moderate (high methodological quality, moderate external validity) (Evidence Report, Tab. 27). The efficacy of magnetic field therapy was moderate. The SMDs (magnetic field therapy—sham magnetic field therapy) on pain and the quality of life at the end of the intervention period were high (Evidence Report, Tab. 28 and Fig. 8). The acceptance was moderate (dropout rate 16%) and did not differ greatly from the controls (Evidence Report, Fig. 8). Three quarters of the studies reported side effects. The practicality is minimal. Magnetic field therapy for FMS is not listed in the health care catalogue. There are not enough medicinal and patient reports available about the efficacy of this system in Germany. Thus a downgrade of the evidence level followed. Based on the formal criteria, an open recommendation would be possible. This is however not in line with the preferences of the involved company representatives and patient groups. This resulted in a further downgrading in the recommendation of the level of evidence. Transcutaneous nerve stimulation Evidence-based recommendation Transcutaneous nerve stimulation (TENS) should not be used. EL 3a, negative recommendation, consensus Comment. The literature search found 31 studies. One study was excluded, as TENS was combined with other physical agents interventions [62]. Three RCTs with 82 patients and average study duration of 5 (3–5) weeks were analysed (Evidence Report, Tab. 29; [30, 64, 97]). The quality of evidence was moderate (low methodological quality, moderate external validity; Evidence Report, Tab. 30). The clinical end points of the studies were published incompletely. Due to the low number of studies and the low methodological quality, the evidence was downgraded by two levels. A quantitative analysis was completed despite incomplete data presentation. TENS was not effective (Evidence ReDer Schmerz 3 · 2012 | 5 Schwerpunkt port, Tab. 31 and Fig. 9). Even the pre- and post comparisons showed no significant SMDs. The acceptance was high (dropout rate 4%) and did not differ greatly from the controls. Side effects were not reported. Relevant side effects are not described in the literature. TENS as treatment option is provided in the health care catalogue. Transcranial direct current stimulation Evidence-based recommendation Transcranial direct current stimulation should not be used. EL 2a, negative recommendation, strong consensus Comment. The literature search found 45 studies. The results of one of the studies was published twice [41, 110]. Four studies with six treatment arms and 129 patients and average treatment duration of 15 (5–20) treatments were analysed [23, 41, 79, 110]. All studies carried out a follow up after an average of 4 (3– 8) weeks (Evidence Report, Tab. 32). The low number of study participants (<200) resulted in a downgrading of the evidence level. The quality of the evidence was moderate (high methodological quality, moderate external validity) (Evidence Report, Tab. 33). The efficacy was low. The SMD (transcranial direct current stimulation vs sham transcranial direct current stimulation) on sleep was low at the end of the studies (Evidence Report, Tab. 34 and Fig. 10). The acceptance was high (dropout rate of 5%; Evidence Report, Fig. 10). The side effects rate was high: head and neck pain was 10% greater than in the control group. This treatment is an experimental treatment method for chronic pain, which, as yet, is not part of the routine clinical treatment. As a result of the high risks and low availability, the level of recommendation was downgraded by two levels. 6 | Der Schmerz 3 · 2012 Neither positive nor negative recommendation possible Full body heat treatment with water-filtered mild infrared-A radiation and hot full body packs Evidence-based statement Due to the limited availability of studies, no negative or positive statement is possible. Strong consensus Comment. Here RCTs are summarised, in which full body heat treatment was induced by other methods than described in the section “Thermal baths” (balneo, spa and thalossa therapy). The literature search found 11 studies. No placebo-controlled studies were found for the full body heat treatment with water-filtered mild infrared-A-radiation (6×15 min in 3 weeks). In one RCT full body heat therapy was combined with a 3-week multimodal in-patient treatment (69 patients). Here the therapy group was superior to the multimodal only in-patient (70 patients) treatment in regards to pain reduction and improvement in the quality of life. The positive effects on pain and quality of life were maintained at follow-up at 3 and 6 months. One patient dropped out due to intolerance to the heat treatment [18]. This procedure is not part of the routine clinical intervention. In one RCT 7 patients received full body hot packs (no details were reported), 8 patients received aerobic training and 11 patients received general exercises. None of the groups showed a significant change in pain, fatigue, insomnia and quality of life [77]. Hydrogalvanic bath Evidence-based statement It is not possible to make either a positive or negative statement due to the limited number of studies. Strong consensus Comment. In one RCT one group of 25 patients received 10 mg amitriptyline over a period of 8 weeks and the other group received 10 mg amitriptyline plus a total of 10 treatments hydrogalvanic baths at 20 min for each treatment. At the end of the treatment period, both groups showed improvement in the quality of life. The combined treatment was superior to the mono-therapy with amitriptyline in the improvement of quality of life. No side effects were established [35]. In one study, 12 patients were treated with hydrogalvanic baths (20 min twice a week) or with progressive muscle relaxation over a period of 5 weeks. At the end of the treatment period both groups significantly reduced their pain intensity without there being a significant difference between the two groups [46]. Craniosacral therapy Evidence-based statement It is not possible to make either a positive or negative statement due to the limited number of studies. Strong consensus Comment. The literature search found 27 studies. The data from one RCT was published twice [24] 68). In one RCT 52 patients were treated with craniosacral therapy (60 min twice a week for 9 weeks) and compared with 52 patients in a placebo group (disconnected ultrasound). A follow-up followed after 1 year. The quality of evidence in the study was low. Craniosacral therapy was superior to the control group in regards to the reduction of pain, tiredness and insomnia, and at follow-up in regards to insomnia [68]. Lymphatic drainage Evidence-based statement It is not possible to make either a positive or negative statement due to the limited data level. Strong consensus Comment. The literature search found seven studies. In one RCT 25 patients received connective tissue massage and 25 patients received manual lymphatic drainage over a period of 3 weeks. At the end of the treatment period, lymphatic drainage resulted in a significant reduction in pain, insomnia, tiredness and restrictions in the quality of life and was superior to the connective tissue massage in regards to improvement of the quality of life [34]. In a case study, 17 patients were treated for 12 sessions (60 min each) over a period of 4 weeks. At the end of the treat- Tab. 1 Changes in the recommendation levels for physical agents and physiotherapy in the first and second version of the guidelines Intervention Chiropractic Functional training Strength training Full body heat treatment with water filtered mild infrared-A radiation Full body cold therapy Exercise therapy Recommendation level 2008 Open Open Not considered Recommended Open Open Laser Lymphatic drainage Open Open Magnetic field therapy Massage Osteopathy Open Negative Open Physiotherapy Open Transcranial direct current stimulation Ultrasound/electrotherapy Open Open ment, pain, tiredness and insomnia were reduced and the quality of life had improved. At a follow-up after 5 months, pain and tiredness were reduced [9]. The dropout rate was between 0 and 4%. Side effects were not recorded. Relevant side effects are not reported in the literature. Lymphatic drainage for FMS is not specifically contained in the health care catalogue. Physiotherapy (combined active and passive intervention) Evidence-based statement It is not possible to make either a positive or negative statement due to the limited number of studies. Strong consensus Comment. Individual content of physiotherapy treatment are analysed in the sections “Strength training” and “Stretching” as well as in the article “Complementary and alternative therapies in fibromyalgia syndrome” under the section “Meditative movement therapies”. Physiotherapy uses passive—for example movement carried out by the therapist—and active—independently car- Recommendation level 2012 Negative recommendation Strong recommendation Strong recommendation Neither positive nor negative recommendation possible Negative recommendation Neither positive nor negative recommendation possible Negative recommendation Neither positive nor negative recommendation possible Negative recommendation Strong negative Neither positive nor negative recommendation possible Neither positive nor negative recommendation possible Negative recommendation Neither positive nor negative recommendation possible ried out—movements and interventions as well as the inclusion of physical agents for the treatment and prevention of diseases. For the inclusion in this analysis it was required that passive and active movements were combined. The combination with physical agents was optional. Studies, which included active movements only (with and without physiotherapy guidance) are analysed in the sections “Stretching” and “Strength training”. Studies, which included active movements only (with and without physiotherapy guidance) in combination with movement, breathing exercises and relaxation or meditation are described in the article “Complementary and alternative therapies in fibromyalgia syndrome” under the section “Meditative movement therapies”’. The literature search found 442 studies. One study was excluded, as it did not include randomisation and the physiotherapy program was not described adequately [56]. One study was excluded, as the as “Physiotherapy” described program did not include passive movement [114]. Two RCTs with the above-described criteria were found. In one RCT, 34 patients served as a control group receiving a kine- siotherapy treatment to the cervical spine and ultrasound to pain points over a period of 3 weeks on 5 days for a total of 15 treatments. The experimental group received 50 mg of sertraline per day over a period of 6 months. In the physiotherapy group no significant reduction in pain and insomnia was ascertained, but in the sertraline theses were attained [42]. In one RCT 2 physiotherapy programs were compared: 10 patients received kinesiotherapy and active muscle stretching, and 10 patients received myofascial release according to Mézières twice a week for 75 min each over a duration of 12 weeks. At the end of the treatment period both groups showed a significant improvement in the quality of life. This was not maintained at follow-up 12 weeks later [104]. Discussion In comparison to the first version of the guidelines [91], a stronger recommendation could be given by the quantitative data analysis for aerobic training. The indirect evidence for the efficacy of functional training resulted in a stronger recommendation in the current version of the guidelines. The new version of the guidelines provides a stronger recommendation for strength training. In the first version this intervention was not dealt with. The evidence for the lack of efficacy of massage resulted in a strong negative recommendation. The quantitative data synthesis with absent proof of efficacy resulted in a negative recommendation for TENS and transcranial direct current stimulation, the consideration of limited availability and risks in a negative recommendation for chiropractic, full body cold treatment, laser and magnetic field therapy. Changed criteria for a positive recommendation (presence of at least two studies) resulted in, after an open recommendation for physiotherapy, lymphatic drainage and ultrasound in the first version of the guidelines, the statement that neither a positive nor a negative recommendation is possible due to the restricted current level of data available (. Tab. 1). Further research, in the form of randomised clinical trials, is required for functional training, physiotherapy, lymphatic drainage, magnetic field theraDer Schmerz 3 · 2012 | 7 Schwerpunkt py, TENS (with adequate stimulation) as well as long-term studies looking into selfmanagement with infrared cabins and ‘bio sauna’. Conclusion for clinical practice It is strongly recommended that aerobic training (e.g., faster walking, Nordic walking, cycling or ergometer training, dancing, aqua jogging) and strength training should be performed on a regular basis at least 2–3 times a week. Recommended is functional training, as well as from the therapy agents, the thermal baths. Stretching can be considered. The current state of research means that no recommendation can be given for physiotherapy (defined as the implementation of active and passive treatment interventions), craniosacral therapy, hydrogalvanic bath, lymphatic drainage and full body heat treatment with water-filtered mild infrared-A radiation. Not recommended are chiropractic, hyperbaric oxygen therapy, cold chamber treatment, laser therapy, TENS and transcranial direct current stimulation. Strong negative recommendations are issued for operative quadrant intervention and massage. Corresponding address Dr. A. Winkelmann Klinik und Poliklinik für Physikalische Medizin und Rehabilitation, Klinikum der Universität München, Munich Ziemssenstr. 1, 80336 Munich Germany Andreas.Winkelmann@med.uni-muenchen.de Conflict of interest. See Tab. 5 in “Methodological fundamentals used in developing the guidelines” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Alentorn-Geli E, Padilla J, Moras G et al (2008) Six weeks of whole-body vibration exercise improves pain and fatigue in women with fibromyalgia. J Altern Complement Med 14:975–981 2. Alfano AP, Taylor AG, Foresman PA et al (2001) Static magnetic fields for treatment of fibromyalgia: a randomized controlled trial. J Altern Complement Med 7:53–64 8 | Der Schmerz 3 · 2012 3. Alnigenis M, Nergis Y, Bradley JD et al (2001) Massage therapy in the management of fibromyalgia: a pilot study. J Musculoskel Pain 9:55– 67 4. Altan L, Bingol U, Aykac M et al (2004) Investigation of the effects of pool-based exercise on fibromyalgia syndrome. Rheumatol Int 24:272– 277 5. Altan L, Korkmaz N, Bingol U, Gunay B (2009) Effect of Pilates training on people with fibromyalgia syndrome: a pilot study. Arch Phys Med Rehabil 90:1983–1988 6. Ammer K, Melnizky P (1999) Medicinal baths for treatment of generalized fibromyalgia. Forsch Komplementarmed 6:80–85 7. Ardiç F, Ozgen M, Aybek H et al (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446 8. Armagan O, Tascioglu F, Ekim A, Oner C (2006) Long-term efficacy of low level laser therapy in women with fibromyalgia: a placebo-controlled study. J Back Musculoskel Rehabil 19:135–140 9. Asplund R (2003) Manual lymph drainage therapy using light massage for fibromyalgia sufferers: a pilot study. J Orthop Nurs 7:192–196 10. Assis MR, Silva LE, Alves AM et al (2006) A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum 55:57–65 11. Bauer J, Heine H (1999) Möglichkeiten chirurgischer Intervention bei fibromyalgischen Beschwerden (Rücken und untere Extremitäten)— Beziehungen zu Akupunkturpunkten. Biol Med 28:135–141 12. Bauer J, Heine H (2000) Akupunkturpunkte und Quadrantenschmerz. Biol Med 29:282–288 13. Bauer. http://www.fms-bauer.com/downloads/ FMS-FAQ-OP-DE.pdf. Accessed 16 May 2012 14. Bellometti S, Galzigna L (1999) Function of the hypothalamic adrenal axis in patients with fibromyalgia syndrome undergoing mud-pack treatment. Int J Clin Phramacol Res 9:27–33 (Excluded: additional treatment with trazodone) 15. Bircan C, Karasel SA, Akgün B et al (2008) Effects of muscle strengthening versus aerobic exercise program in fibromyalgia. Rheumatol Int 28:527– 532 16. Blunt KL, Rajwani MH, Guerriero RC (1997) The effectiveness of chiropractic management of fibromyalgia patients: a pilot study. J Manipulative Physiol Ther 20:389–399 17. Brattberg G (1999) Connective tissue massage in the treatment of fibromyalgia. Eur J Pain 3:235– 244 18. Brockow T, Wagner A, Franke A et al (2007) A randomized controlled trial on the effectiveness of mild water-filtered near infrared whole-body hyperthermia as an adjunct to a standard multimodal rehabilitation in the treatment of fibromyalgia. Clin J Pain 23:67–75 19. Buckelew SP, Conway R, Parker J et al (1998) Biofeedback/relaxation training and exercise interventions for fibromyalgia: a prospective trial. Arthritis Care Res 11:196–209 20. Buskila D, Abu-Shakra M, Neumann L et al (2001) Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int 20:105–108 21. Calandre EP, Rodriguez-Claro ML, Rico-Villademoros F et al (2009) Effects of pool-based exercise in fibromyalgia symptomatology and sleep quality: a prospective randomised comparison between stretching and Ai Chi. Clin Exp Rheumatol 27(Suppl 56):21–28 22. Carbonell-Baeza A, Aparicio VA, Martins-Pereira CM et al (2010) Efficacy of biodanza for treating women with fibromyalgia. J Altern Complement Med 16:1191–1200 23. Carretero B, Martín MJ, Juan A et al (2009) Lowfrequency transcranial magnetic stimulation in patients with fibromyalgia and major depression. Pain Med 10:748–753 24. Castro-Sánchez AM, Matarán-Peñarrocha GA, Sánchez-Labraca N et al (2011) A randomized controlled trial investigating the effects of craniosacral therapy on pain and heart rate variability in fibromyalgia patients. Clin Rehabil 25:25– 35 25. Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J et al (2011) Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. DOI10.1155/2011/561753 26. Colbert AP, Markov MS, Banerj M, Pilla AA (1999) Magnetic mattress pad use in patients with fibromyalgia: a randomised double-blind pilot study. J Back Musculoskel Rehabil 13:19–31 27. Da Costa D, Abrahamowicz M, Lowensteyn I et al (2005) A randomized clinical trial of an individualized home-based exercise programe for women with fibromyalgia. Rheumatology (Oxford) 44:1422–1427 28. Andrade SC de, Carvalho RF de, Soares AS et al (2008) Thalassotherapy for fibromyalgia: a randomized controlled trial comparing aquatic exercises in sea water and water pool. Rheumatol Int 29:147–152 29. Melo Vitorino DF de, Carvalho BC de, Prado GF do (2006) Hydrotherapy and conventional physiotherapy improve sleep time and quality of life of fibromyalgia patients: randomised clinical trial. Sleep Med 7:293–296 30. Di Benedetto P, Iona LG, Zidarich V (1993) Clinical evaluation of S-adenosyl-methionine versus transcutaneous electrical nerve stimulation in primary fibromyalgia. Curr Ther Res 53:222–230 31. Dönmez A, Karagulle MZ, Tercan N et al (2005) SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26:168–172 32. Evcik D, Kizilay B, Gokcen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59 33. Evcik D, Yigit I, Pusak H, Kavuncu V (2008) Effectiveness of aquatic therapy in the treatment of fibromyalgia syndrome: a randomized controlled open study. Rheumatol Int 28:885–890 34. Ekici G, Bakar Y, Akbayrak T, Yuksel I (2009) Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: a randomized controlled trial. J Manipulative Physiol Ther 32:127–133 35. Eksioglu E, Yazar D, Bal A et al (2007) Effects of Stanger bath therapy on fibromyalgia. Clin Rheumatol 26:691–694 36. Etnier JL, Karper WB, Gapin JI et al (2009) Exercise, fibromyalgia, and fibrofog: a pilot study. J Phys Act Health 6:239–246 37. Field T, Diego M, Cullen C et al (2002) Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. J Clin Rheumatol 8:72–76 38. Field T, Delage G, Hernandez-Reuf M (2003) Movement and massage therapy reduce fibromyalgia pain. J Bodyw Mov Ther 7:49–52 39. Fioravanti A, Perpignano G, Tirri G (2007) Effects of mud-bath treatment on fibromyalgia patients: a randomized clinical trial. Rheumatol Int 27:1157–1161 40. Fontaine KR, Haas S (2007) Effects of lifestyle physical activity on health status, pain, and function in adults with fibromyalgia syndrome. J Musculoskeletal Pain 15:3–9 41. Fregni F, Gimenes R, Valle AC et al (2006) A randomized, sham-controlled, proof of principle study of transcranial direct current stimulation for the treatment of pain in fibromyalgia. Arthritis Rheum 54:3988–3998 42. González-Viejo MA, Avellanet M, HernándezMorcuende MI (2005) A comparative study of fibromyalgia treatment: ultrasonography and physiotherapy versus sertraline treatment. Ann Readapt Med Phys 48:610–5 (Article in French) 43. Gouveia LO, Castanho P, Ferreira JJ (2009) Safety of chiropractic interventions: a systematic review. Spine (Philadelphia, PA 1976) 34:E405–413 44. Gowans SE, deHueck A, Voss S et al (2001) Effect of a randomized, controlled trial of exercise on mood and physical function in individuals with fibromyalgia. Arthritis Rheum 45:519–529 45. Gowans SE, Dehueck A, Voss S et al (2004) Sixmonth and one-year followup of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum 51:890–898 46. Günther V, Mur E, Kinigadner U, Miller C (1994) Fibromyalgia—the effect of relaxation and hydrogalvanic bath therapy on the subjective pain experience. Clin Rheumatol 13:573–578 47. Gür A, Karakoc M, Nas K et al (2002) Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int 22:188–193 48. Gür A, Karakoc M, Nas K et al (2002) Efficacy of low power laser therapy in fibromyalgia: a single-blind, placebo-controlled trial. Lasers Med Sci 17:57–61 49. Gusi N, Tomas-Carus P, Hakkinen A et al (2006) Exercise in waist-high warm water decreases pain and improves health-related quality of life and strength in the lower extremities in women with fibromyalgia. Arthritis Rheum 15:66–73 50. Häkkinen A, Häkkinen K, Hannonen P, Alen M (2001) Strength training induced adaptations in neuromuscular function of premenopausal women with fibromyalgia: comparison with healthy women. Ann Rheum Dis 60:21–26 51. Häkkinen K, Pakarinen A, Hannonen P et al (2002) Effects of strength training on muscle strength, cross-sectional area, maximal electromyographic activity, and serum hormones in premenopausal women with fibromyalgia. J Rheumatol 29:1287–1295 (Excluded: target variables (hormone values) not suited for analysis) 52. Häuser W, Klose P, Langhorst J et al (2010) Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther 12 R79 53. Ide MR, Belini MA, Caromano FA (2005) Effects of an aquatic versus non-aquatic respiratory exercise program on the respiratory muscle strength in healthy aged persons. Clinics (Sao Paulo) 60:151–158 54. Isomeri R, Mikkelson M, Latikka P, Kammonen K (1993) Effects of amitriptyline and cardiovascular fitness training on pain in patients with primary fibromyalgia. J Musculoskeletal Pain 3/4:253– 256 55. Jentoft ES, Kvalvik AG, Mengshoel AM (2001) Effects of pool-based and land-based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Rheum 45:42–47 56. Joshi MN, Joshi R, Jain AP (2009) Effect of amitriptyline vs. physiotherapy in management of fibromyalgia syndrome: What predicts a clinical benefit? J Postgrad Med 55:185–189 (Excluded: no randomization) 57. Jones KD, Burckhardt CS, Clark SR et al (2002) A randomized controlled trial of muscle strengthening versus flexibility training in fibromyalgia. J Rheumatol 29:1041–1048 58. Jones KD, Burckhardt CS, Deodhar AA et al (2008) A six-month randomized controlled trial of exercise and pyridostigmine in the treatment of fibromyalgia. Arthritis Rheum 58:612–622 59. Kassenärztliche Bundesvereinigung, GKV Spitzenverband (2011) 29. Änderung der Vereinbarung über Vordrucke für die vertragsärztliche Versorgung vom 1. April 1995. Dtsch Arztebl 108:B1171–1174 60. King SJ, Wessel J, Bhambhani Y et al (2002) The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol 29:2620–2627 61. Kingsley JD, Panton LB, Toole T et al (2005) The effects of a 12-week strength-training program on strength and functionality in women with fibromyalgia. Arch Phys Med Rehabil 86:1713– 1721 62. Külcü DG, Demirel GG (2009) Fibromiyalji Sendromlu Bir Grup Hastada Fizik Tedavi Programının Uykusuzluk Şiddeti Üzerine Etkisi. Turk Fiz Tıp Rehab Derg 55:64–67 63. Kurzeja R, Gutenbrunner C, Krohn-Grimberghe B (2003) Fibromyalgia Comparison of whole-bodycryotherapy with two classical thermotherapy methods. Akt Rheumatol 28:158–163 (Excluded: clinical endpoints not included) 64. Löfgren M, Norrbrink C (2009) Pain relief in women with fibromyalgia: a cross-over study of superficial warmth stimulation and transcutaneous electrical nerve stimulation. J Rehabil Med 41:557–562 65. Lund I, Lundeberg T, Carleson J et al (2006) Corticotropin releasing factor in urine—a possible biochemical marker of fibromyalgia. Responses to massage and guided relaxation. Neurosci Lett 403:166–171 (Excluded: reported target variables not suited for analysis) 66. Mannerkorpi K, Nordeman L, Cider A, Jonsson G (2010) Does moderate-to-high intensity Nordic walking improve functional capacity and pain in fibromyalgia? A prospective randomized controlled trial. Arthritis Res Ther 12(5): R189 67. Martin L, Nutting A, MacIntosh BR et al (1996) An exercise program in the treatment of fibromyalgia. J Rheumatol 23:1050–1053 68. Matarán-Peñarrocha GA, Castro-Sánchez AM, García GC et al (2011) Influence of craniosacral therapy on anxiety, depression and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med 561753 69. Matsutani LA, Marques AP, Ferreira EA et al (2007) Effectiveness of muscle stretching exercises with and without laser therapy at tender points for patients with fibromyalgia. Clin Exp Rheumatol 25:410–5 70. McCain GA, Bell DA, Mai FM, Halliday PD (1988) A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum 31:1135–1141 71. McDonagh M, Helfand M, Carson S, Russman BS (2004) Hyperbaric oxygen therapy for traumatic brain injury: a systematic review of the evidence. Arch Phys Med Rehabil 85:1198–1204 72. Mengshoel AM, Komnaes HB, Forre O (1992) The effects of 20 weeks of physical fitness training in female patients with fibromyalgia. Clin Exp Rheumatol 10:345–349 73. Metzger D, Zwingmann C, Protz W, Jäckel WH (2000) Whole-body cryotherapy in rehabilitation of patients with rheumatoid diseases—pilot study. Rehabilitation 39:93–100 74. Munguía-Izquierdo D, Legaz-Arrese A (2008) Assessment of the effects of aquatic therapy on global symptomatology in patients with fibromyalgia syndrome: a randomized controlled trial. Arch Phys Med Rehabil 89:2250–2257 75. Neumann L, Sukenik S, Bolotin A et al (2001) The effect of balneotherapy at the Dead Sea on the quality of life of patients with fibromyalgia syndrome. Clin Rheumatol 20:15–19 76. Nichols DS, Glenn TM (1994) Effects of aerobic exercise on pain perception, affect, and level of disability in individuals with fibromyalgia. Phys Ther 74:327–332 77. Norregaard J, Lykkegaard JJ, Mehlsen J (1997) Exercise training in treatment of fibromyalgia. J Musculoskelet Pain 5:71–79 78. Panton LB, Figueroa A, Kingsley JD et al (2009) Effects of resistance training and chiropractic treatment in women with fibromyalgia. J Altern Complement Med 15:321–328 (Excluded: combination of strength training and chiropractic therapy) 79. Passard A, Attal N, Benadhira R et al (2007) Effects of unilateral repetitive transcranial magnetic stimulation of the motor cortex on chronic widespread pain in fibromyalgia. Brain 130:2661–2670 80. Piso U, Kuether G, Gutenbrunner Chr, Gehrke A (2001) Analgesic effects of sauna in fibromyalgia. Physikalische Medizin Rehabilitationsmedizin Kurortmedizin 11(3):94–99 (Excluded: no randomization) 81. Ramsay C, Moreland J, Ho M et al (2000) An observer-blinded comparison of supervised and unsupervised aerobic exercise regimens in fibromyalgia. Rheumatology (Oxford) 39:501–515 82. Redondo JR, Justo CM, Moraleda FV et al (2004) Long-term efficacy of therapy in patients with fibromyalgia: a physical exercise-based program and a cognitive-behavioral approach. Arthritis Rheum 15:184–192 83. Rehabilitationsträger (2011) Rahmenvereinbarung über den Rehabilitationssport und das Funktionstraining vom 01.01.2011. http://www. bar-frankfurt.de/fileadmin/dateiliste/publikationen/empfehlungen/downloads/Rahmenvereinbarung_Rehasport_2011.pdf. Accessed 16 May 2012 84. Richards SC, Scott DL (2002) Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. BMJ 325:185 85. Rivalland G, Mitchell SJ, Schalkwyk JM van (2010) Pulmonary barotrauma and cerebral arterial gas embolism during hyperbaric oxygen therapy. Aviat Space Environ Med 81:888–890 86. Roizenblatt S, Fregni F, Gimenez R et al (2007) Site-specific effects of transcranial direct current stimulation on sleep and pain in fibromyalgia: a randomized, sham-controlled study. Pain Pract 7:297–306 (duplicate) Der Schmerz 3 · 2012 | 9 Schwerpunkt 87. Rooks DS, Gautam S, Romeling M et al (2007) Group exercise, education, and combination self-management in women with fibromyalgia: a randomized trial. Arch Intern Med 167:2192– 2200 88. Samborski W, Stratz T, Sobieska M et al (1992) Intraindividueller Vergleich einer Ganzkörperkältetherapie und einer Wärmebehandlung mit Fangopackungen bei der generalisierten Tendomyopathie (GTM). Z Rheumatol 51:25–31 (Excluded: follow-up time too short) 89. Sañudo B, Galiano D, Carrasco L et al (2010a) Aerobic exercise versus combined exercise therapy in women with fibromyalgia syndrome: a randomized controlled trial. Arch Phys Med Rehabil 91:1838–1843 90. Sañudo B, Hoyo M de, Carrasco L et al (2010b) The effect of 6-week exercise programme and whole body vibration on strength and quality of life in women with fibromyalgia: a randomised study. Clin Exp Rheumatol 28(Suppl 63):40–45 91. Schachter CL, Busch AJ, Peloso PM, Sheppard MS (2003) Effects of short versus long bouts of aerobic exercise in sedentary women with fibromyalgia: a randomized controlled trial. Phys Ther 83:340–358 92. Schiltenwolf M, Häuser W, Felde E et al (2008) Physiotherapie, medizinische Trainingstherapie und physikalische Therapie beim Fibromyalgiesyndrom. Schmerz 22:303–312 93. Şencan S, Ak S, Karan A et al (2004) A study to compare the therapeutic efficacy of aerobic exercise and paroxetine in fibromyalgia syndrome. J Back Musculoskeletal Rehabil 17:57–61 94. Shupak NM, McKay JC, Nielson WR et al (2006) Exposure to a specific pulsed low-frequency magnetic field: a double-blind placebo-controlled study of effects on pain ratings in rheumatoid arthritis and fibromyalgia patients. Pain Res Manag 11:85–90 (Excluded: only one application) 95. Stephens S, Feldman BM, Bradley N et al (2008) Feasibility and effectiveness of an aerobic exercise program in children with fibromyalgia: Results of a randomized controlled pilot trial. Arthritis Rheum 59:1399–1406 96. Sukenik S, Baradin R, Codish S et al (2001) Balneotherapy at the Dead Sea area for patients with psoriatic arthritis and concomitant fibromyalgia. Isr Med Assoc J 3:147–150 97. Sunshine W, Field TM, Quintino O et al (1996) Fibromyalgia benefits from massage therapy and transcutaneous electrical stimulation. J Clin Rheumatol 2:18–22 98. Sutbeyaz ST, Sezer N, Koseoglu F, Kibar S (2009) Low-frequency pulsed electromagnetic field therapy in fibromyalgia: a randomized, doubleblind, sham-controlled clinical study. Clin J Pain 25:722–728 99. Thomas AW, Graham K, Prato FS et al (2007) A randomized, double-blind, placebo-controlled clinical trial using a low-frequency magnetic field in the treatment of musculoskeletal chronic pain. Pain Res Manag 12:249–258 100. Tomas-Carus P, Häkkinen A, Gusi N et al (2007) Aquatic training and detraining on fitness and quality of life in fibromyalgia. Med Sci Sports Exerc 39:1044–1050 101. Tomas-Carus P, Gusi N, Häkkinen A et al (2008) Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. J Rehabil Med 40:248–252 10 | Der Schmerz 3 · 2012 102. Tyers S, Smith RB (2001) A comparison of cranial electrotherapy stimulation alone or with chiropractic therapies in the treatment of fibromyalgia. Am Chiropr 23:39–41 103. Uhlemann H, Strobel I, Müller-Landner U, Lange U (2007) Prospektive klinische Pilotstudie zur Wirksamkeit konditionierender Maßnahmen bei Patienten mit Fibromyalgie. Akt Rheumatol 32:27–33 104. Valencia M, Alonso B, Alvarez MJ et al (2009) Effects of 2 physiotherapy programs on pain perception, muscular flexibility and illness impact in women with fibromyalgia: a pilot study. J Manipulative Physiol Ther 32:84–92 105. Valim V, Oliveira L, Suda A et al (2003) Aerobic fitness effects in fibromyalgia. J Rheumatol 30:1060–1069 106. Valkeinen H, Alen M, Hannonen P et al (2004) Changes in knee extension and flexion force, EMG and functional capacity during strength training in older females with fibromyalgia and healthy controls. Rheumatology (Oxford) 43:225–228 107. Valkeinen H, Häkkinen K, Pakarinen A et al (2005) Muscle hypertrophy, strength development, and serum hormones during strength training in elderly women with fibromyalgia. Scand J Rheumatol 34:309–314 (Excluded: target values (hormone values) not suited for analysis) 108. Valkeinen H, Häkkinen A, Hannonen P et al (2006) Acute heavy-resistance exercise-induced pain and neuromuscular fatigue in elderly women with fibromyalgia and in healthy controls: effects of strength training. Arthritis Rheum 54:1334–1339 (Excluded: no suitable control group) 109. Valkeinen H, Alén M, Häkkinen A et al (2008) Effects of concurrent strength and endurance training on physical fitness and symptoms in postmenopausal women with fibromyalgia: a randomized controlled trial. Arch Phys Med Rehabil 89:1660–1666 110. Valle A, Roizenblatt S, Botte S et al (2009) Efficacy of anodal transcranial direct current stimulation (tDCS) for the treatment of fibromyalgia: results of a randomized, sham-controlled longitudinal clinical trial. J Pain Manag 2:353–361 111. Santen M van, Bolwijn P, Verstappen F et al (2002) A randomized clinical trial comparing fitness and biofeedback training versus basic treatment in patients with fibromyalgia. J Rheumatol 29:575–581 112. Santen M van, Bolwijn P, Landewé R et al (2002) High or low intensity aerobic fitness training in fibromyalgia: does it matter? J Rheumatol 29:582–587 113. Verstappen FTJ, Santen-Hoeuft HMS van, Bolwijn S (1997) Effect of a group activity program for fibromyalgia patients on physical fitness and well-being. J Musculoskeletal Pain 5:17–28 114. Vitorino DF, Carvalho LB, Prado GF (2006) Hydrotherapy and conventional physiotherapy improve total sleep time and quality of life of fibromyalgia patients: randomized clinical trial. Sleep Med 7:293–296 (Excluded: criteria not fulfilled) 115. Wise P, Walsh M, Littlejohn G (2002) Efficacy of chiropractic treatment on fibromyalgia syndrome: a randomized controlled trial. Eur J Chiropr 49:198 116. Wigers SH, Stiles TC, Vogel PA (1996) Effects of aerobic exercise versus stress management treatment in fibromyalgia. A 4.5 year prospective study. Scand J Rheumatol 25:77–86 117. Yildiz S, Kiralp MZ, Akin A et al (2004) A new treatment modality for fibromyalgia syndrome: hyperbaric oxygen therapy. J Int Med Res 32(3):263–267 118. Yurtkuran M, Celiktas M (1996) A randomized, controlled trial of balneotherapy in the treatment of patients with primary fibromyalgia syndrome. Phys Rehab Kur Med 6:109–112 (Excluded: combination with multimodal therapy) Schwerpunkt English Version of "Multimodale Therapie des Fibromyalgiesyndroms. Systematische Übersicht, Metaanalyse und Leitlinie". DOI 10.1007/s00482-012-1173-1 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 B. Arnold1 · W. Häuser2 · M. Arnold3 · M. Bernateck4 · K. Bernardy5 · W. Brückle6 · E. Friedel7 · H.J. Hesselschwerdt8 · W. Jäckel9 · V. Köllner10 · E. Kühn11 · F. Petzke12 · M. Settan13 · M. Weigl14 · E. Winter15 · M. Offenbächer16 1 Abteilung Schmerztherapie, Klinikum Dachau 2 Innere Medizin 1, Klinikum Saarbrücken 3 Helmholtz Zentrum München, Deutsches Forschungszentrum für Gesundheit und Umwelt (GmbH), München 4 Interdisziplinäre Schmerzambulanz, Medizinische Hochschule Hannover 5 Klinik Der Fürstenhof Bad Pyrmont 6 Abteilung für Schmerztherapie, Berufsgenossenschaftliche Universitätsklinik Bergmannsheil GmbH, Ruhr Universität Bochum 7 Klinik Bad Kissingen 8 Abteilung Orthopädie und Rheumatologie, Theresienklinik, Bad Krozingen 9 Abteilung Qualitätsmanagement und Sozialmedizin, Universität Freiburg 10 Fachklinik für Psychosomatische Medizin, Bliestal Kliniken, Blieskastel 11 Deutsche Rheuma-Liga, Ellwangen 12 Schmerz-Tagesklinik und –Ambulanz, Universitätsmedizin Göttingen, Georg-August Universität Göttingen 13 Deutsche Fibromyalgie Vereinigung, Seckach 14 Klinik für Physikalische Medizin und Rehabilitation, Klinikum Großhadern, München 15 Klinik für Anästhesiologie, Klinik Havelhöhe, Berlin 16 Humanwissenschaftliches Zentrum, Ludwig-Maximilians-Universität München Multicomponent therapy of fibromyalgia syndrome Systematic review, meta-analysis and guideline For the planned revision of the guideline, the steering group of the workgroup posed the following questions: 1.Is multicomponent therapy in FMS effective short-term and long-term? 2.What study duration is needed for a multicomponent therapy to be effective? 3.Which patients should be offered a multicomponent therapy? 4.What are the crucial components in multicomponent therapy? Materials and methods Details on literature search and analysis as well as on the development process of the recommendations are listed in the article “Methodological fundamentals used in developing the guideline” in this issue. Results The following conclusions are valid for adult patients. For multicomponent therapy of chronic pain in several body parts of children and adolescents, see article “Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. Key recommendations are italicized. Multicomponent therapy Evidence-based recommendation Multicomponent therapy should be applied. EL1a, strong recommendation, strong consensus Duration of multicomponent therapy Evidence-based recommendation Duration of therapy should be at least 24 h. EL1a, strong recommendation, strong consensus Comment to the two recommendations above. In the German Operation and Procedure Code (“Operationen- und Prozedurenschlüssel”, OPS), multicomponent therapy is applicable in the context of a multicomponent complex treatment such as inpatient/outpatient multicomponent pain therapy (OPS items 8-91c and 8-918.x, respectively) or an inpatient psychosomatic–psychotherapeutic clinical treatment (OPS items 9-60.x to 9-64.x). According to OPS item 8-918.x, a multicomponent pain therapy requires interDer Schmerz 3 · 2012 | 1 Schwerpunkt disciplinary diagnostics by at least 2 distinct disciplines (obligatory one psychiatric, psychosomatic or psychological discipline) and is defined by the simultaneous application of at least 3 of the following therapies under medical administration: psychotherapy, special psychotherapy, relaxation techniques, ergotherapy, medical training therapy, sensomotoric training, employment training, art or music therapy or other practicing therapies. Furthermore, multicomponent pain therapy involves monitoring of the treatment progress via a standardized therapeutic assessment through interdisciplinary team meetings [7]. In the literature, “multidisciplinary approaches” in FMS are defined as the combination of at least one activating procedure (endurance, strength or flexibility training) with at least one psychotherapeutic procedure (patient education and/or cognitive behavioral therapy) [4]. Accordingly, studies combining at least one activating with at least one psychotherapeutic procedure were classified as “multicomponent studies” and therefore included into the analysis. Literature search obtained 760 such studies. One study was excluded as the clinical endpoints did not meet the criteria for inclusion [21]. A second study was excluded because multicomponent therapy was combined with amitriptyline treatment [22]. The outcomes of one study were published twice [17, 18]. All studies that were included in the analysis met the criteria of a multidisciplinary therapy. Whether these studies meet the criteria of a multicomponent therapy (monitoring of the treatment progress via a standardized therapeutic assessment through interdisciplinary team meetings) could not be investigated based on the published study descriptions. Seventeen studies with 18 study arms, 1,572 patients and an average study duration of 11 weeks (3–26 weeks) were analyzed [2, 3, 4, 6, 8, 9, 10, 12, 13, 14, 15, 16, 18, 19, 21, 23, 24]. In 8 studies, followups after an average of 8 months (range 4–24 months) were conducted (Evidence Report Tab. 35). The quality of evidence was moderate (high quality of methods, moderate external validity) (Evidence Report, Tab. 36). 2 | Der Schmerz 3 · 2012 Multicomponent therapy was highly effective. The standardized mean differences (SMDs) of multicomponent therapy vs. controls at the end of therapy were low for pain and fatigue and moderate for quality of life. The SMDs for multicomponent therapy vs. controls at follow-up were low for fatigue and quality of life (Evidence Report, Tab. 37 and Fig. 11). Subgroup analysis showed that significant effects on pain, fatigue and quality of life were obtained only at a study duration of 24 h or more (the maximum within the included studies was 64 h) [10]. The acceptance was moderate [dropout rate 107/712 (12%)] and was not significantly different compared to controls (Evidence Report Fig. 11). Side effects were not systematically determined (or reported, respectively). According to clinical experience, multicomponent therapy has no significant side effects. As in the majority of the analyzed studies patients with comorbid depression or anxiety disorder were excluded, multicomponent therapy in more severe cases is not sufficiently represented. For treatment in cases of more severe disease progression, more intensive multicomponent programs are recommended (see recommendation in the article “Fibromyalgia syndrome: general principles of and coordination of clinical care and patient education”). Discussion Quantitative data analysis confirmed the outcome of the first version of this guideline [1] where multicomponent therapy (MT) was strongly recommended. The following recommendations should be considered to avoid methodological constraints in future studies of MT in FMS: 1.medication and concomitant treatment should be documented along the study progress and should be taken account of as covariates, 2.comorbidity of mental conditions, psychosocial stress and coping with stress should be determined at the beginning, the end, and at follow-up of therapy and should also be included as covariates, 3.predefined dichotomous parameters of the outcome (return to employment, number of patients with defined reduction of pain etc.) allow for the determination of prognostic parameters to MT, 4.identification of predictors of positive as well as negative outcomes of therapy, 5.randomized comparative clinical trials to identify the crucial components in MT, 6.randomized comparative clinical trials on the efficiency of MT dependent on therapy intensity including the documentation of long-term effects, and 7.randomized comparative clinical trials to identify the needed duration of therapy in a multicomponent program dependent on the severity of disease. Conclusion for clinical practice The review of more recent literature confirmed the strong recommendation of multicomponent therapy as given in the first version of this guideline. In the analyzed studies, multicomponent therapy was defined as a combination of one somatically activating therapy with one psychological procedure and was implemented in an outpatient setting. The studies included in the analysis did not meet the high quality standards of an inpatient/outpatient multicomponent therapy as specified in the German OPS. There are no studies at hand which could validate the recommendation of a scaling of the intensity of treatment based on case severity. Therefore, the recommendation of the application of more intensive multicomponent programs in cases of more severe disease progressions relies on clinical consensus. Corresponding address Dr. B. Arnold Abteilung Schmerztherapie, Klinikum Dachau Krankenhausstr. 15, 85221 Dachau Germany bernhard.arnold@amperkliniken.de Conflict of interest. See Tab. 5 in “Methodological Abstract · Zusammenfassung fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. Schmerz 2012 · DOI 10.1007/s00482-012-1173-1 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 References B. Arnold · W. Häuser · M. Arnold · M. Bernateck · K. Bernardy · W. Brückle · E. Friedel · H.J. Hesselschwerdt · W. Jäckel · V. Köllner · E. Kühn · F. Petzke · M. Settan · M. Weigl · E. Winter · M. Offenbächer 1. Arnold B, Häuser W, Bernardy K et al (2008) Multimodale Therapie des Fibromyalgiesyndroms. Schmerz 22:334–338 2. Brockow T, Wagner A, Franke A et al (2007) A randomized controlled trial on the effectiveness of mild water-filtered near infrared whole-body hyperthermia as an adjunct to a standard multimodal rehabilitation in the treatment of fibromyalgia. Clin J Pain 23:67–75 3. Buckelew SP, Conway R, Parker J et al (1998) Biofeedback/relaxation training and exercise interventions for fibromyalgia: a prospective trial. Arthritis Care Res 11:196–209 4. Burckhardt CS, Mannerkorpi K, Hedenberg L, Bjelle A (1994) A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol 21:714–720 5. Burckhardt CS (2006) Multidisciplinary approaches for management of fibromyalgia. Curr Pharm Des 12:59–66 6. Cedraschi C, Desmeules J, Rapiti E et al (2004) Fibromyalgia: a randomised, controlled trial of a treatment programme based on self management. Ann Rheum Dis 63:290–296 7. Deutsches Institut für Medizinische Information und Dokumentation. Operationen- und Prozedurenschlüssel (OPS) Version 2011 http://www.dimdi.de/static/de/klassi/prozeduren/ops301/opshtml2011/index.htm. Accessed 26 April 2012 8. Fontaine KR, Conn L, Clauw DJ (2010) Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Res Ther 12: R55 9. Gowans SE, deHueck A, Voss S, Richardson M (1999) A randomized, controlled trial of exercise and education for individuals with fibromyalgia. Arthritis Care Res 12:120–128 10. Hammond A, Freeman K (2006) Community patient education and exercise for people with fibromyalgia: a parallel group randomized controlled trial. Clin Rehabil 20:835–846 11. Häuser W, Bernardy K, Arnold B et al (2009) Efficacy of multicomponent treatment in fibromyalgia syndrome: a meta-analysis of randomized controlled clinical trials. Arthritis Rheum 61:216–224 12. Keel PJ, Bodoky C, Gerhard U, Muller W (1998) Comparison of integrated group therapy and group relaxation training for fibromyalgia. Clin J Pain 14:232–238 13. King SJ, Wessel J, Bhambhani Y et al (2002) The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol 29:2620–2627 14. Lemstra M, Olszynski WP (2005) The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain 21:166–174 15. Lera S, Gelman SM, López MJ et al (2009) Multidisciplinary treatment of fibromyalgia: does cognitive behavior therapy increase the response to treatment? J Psychosom Res 67:433–441 16. Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C (2000) Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol 27:2473–2481 Multicomponent therapy of fibromyalgia syndrome. Systematic review, meta-analysis and guideline Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinären Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. The use of multicomponent therapy (the combination of aerobic exercise with at least one psychological therapy) for a minimum of 24 h is strongly recommended for patients with severe FMS.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Review, systematic · Meta-analysis · Guideline · Multimodal therapy Multimodale Therapie des Fibromyalgiesyndroms. Systematische Übersicht, Metaanalyse und Leitlinie Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie DIVS von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potentielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke er- 17. Mannerkorpi K, Ahlmén M, Ekdahl C (2002) Sixand 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol 31:306–310 folgte nach dem Schema des Oxford Center for Evidence Based Medicine. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Der Einsatz von multimodaler Therapie (Kombination von aerobem Training mit mindestens einem psychologischen Verfahren) mit mindestens 24 h Therapiedauer wird für Patienten mit schwereren Verläufen des FMS stark empfohlen. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Multimodale Therapie 18. Mannerkorpi K, Nordeman L, Ericsson A et al (2009) Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med 41:751–760 Der Schmerz 3 · 2012 | 3 Schwerpunkt 19. Rooks DS, Gautam S, Romeling M et al (2007) Group exercise, education, and combination selfmanagement in women with fibromyalgia: a randomized trial. Arch Intern Med 167:2192–2200 20. Skouen JS, Grasdal A, Haldorsen EM (2006) Return to work after comparing outpatient multidisciplinary treatment programs versus treatment in general practice for patients with chronic widespread pain. Eur J Pain 10:145–152 (excluded: target variables not suitable for analysis) 21. Souza JB, Bourgault P, Charest J, Marchand S (2008) Interactional school of fibromyalgia: learning to cope with pain – a randomised controlled study. Rev Bras Reumatol 48:281–225 22. Targino RA, Imamura M, Kaziyama HH et al (2008) A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med 40:582–588 (excluded: combination with defined medication) 23. Koulil S van, Lankveld W van, Kraaimaat FW et al (2010) Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res (Hoboken) 62:1377– 1385 24. Zijlstra TR, Laar MA van de, Bernelot Moens HJ et al (2005) Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology (Oxford) 44:539– 546 4 | Der Schmerz 3 · 2012 Schwerpunkt English Version of "Psychotherapie von Patienten mit Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie". DOI 10.1007/s00482-012-1179-8 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 V. Köllner1 · W. Häuser2 · K. Klimczyk4 · H. Kühn-Becker5 · M. Settan6 · M. Weigl7 · K. Bernardy3 1 Department of Psychosomatic Medicine, Mediclin Bliestal Clinics, Blieskastel 2 Department of Internal Medicine 1, Klinikum Saarbrücken 3 Department of Pain Medicine, University Clinic Bergmannsheil GmbH, Ruhr University Bochum 4 Interdisciplinary Pain Center, Clinic Enzensberg, Hopfen am See 5 Pain Center Zweibrücken 6 German Organisation for Fibromyalgia, Seckach 7 Department of Physical Medicine and Rehabilitation, University Clinic Großhadern Munich Psychotherapy for patients with fibromyalgia syndrome Systematic review, meta-analysis and guideline For the planned revision of the guideline the steering group posed the following questions: 1.Is psychotherapy in fibromyalgia syndrome (FMS) effective in short- and long-term? 2.What are the risks involved when implementing psychotherapy in FMS? 3.Which types of psychotherapy are not recommended in FMS? fibromyalgia syndrome in children and adolescents”. Key recommendations are italicized. Methods Psychotherapy in FMS is recommended in the following clinical constellations: Fmaladaptive disease management (e.g. catastrophizing, inappropriate physical avoidance behavior or dysfunctional perseverance) and/or Frelevant modulation of the symptoms due to stress of daily life and/or interpersonal problems and/or Fcomorbid mental disorders. The methods used in the literature search and analysis, and preparation of the recommendations can be found in the article “Methodological fundamentals used in developing the guideline”. Results Preliminary note The following findings pertain to adults. For information on the psychotherapy of children and adolescents with chronic pain in several body regions, refer to the paper “Definition, diagnosis and therapy of chronic widespread pain and so-called Indication for psychotherapy Note: The following recommendation of the first version of the guideline is still valid. Clinical consensus Strong consensus Strong recommendations Relaxation training combined with aerobic exercise (multicomponent therapy) Evidence-based recommendation Relaxation training combined with aerobic exercise (multicomponent therapy) should be used. EL 1a, strong recommendation, strong consensus Comment. Four studies of multicomponent therapy [3] with 414 patients and an average study duration of 16 (6–26) weeks used a combination of relaxation training and aerobic exercise (Evidence Report, Tab. 38; [11, 30, 36, 37]). The quality of the evidence was moderate (Evidence Report, Tab. 39). The efficacy was low. Low effects on pain and quality of life were found at the end of treatment (Evidence Report, Tab. 40 and Fig. 12). Der Schmerz 3 · 2012 | 1 Schwerpunkt Cognitive behavioral therapy combined with aerobic exercise (multicomponent therapy) Evidence-based recommendation Cognitive behavioral therapy combined with aerobic exercise (multicomponent therapy) should be used. EL1a, strong recommendation, strong consensus Comment. Six studies with 7 study arms of multicomponent therapy [3] with 542 patients and an average study duration of 10 (6–16) weeks used a combination of cognitive behavioral therapy and aerobic exercise (Evidence Report, Tab. 41; [8, 18, 26, 50]). Methodological quality was moderate (Evidence Report, Tab. 42). The efficacy was moderate: moderate effects on fatigue at the end of treatment and follow-up and moderate effects on quality of life at the end of treatment were found (Evidence Report, Tab. 43 and Fig. 13). Open recommendations Biofeedback Evidence-based recommendation Biofeedback can be used. EL 2a, open recommendation, strong consensus Comment. The literature search resulted in 147 hits. Seven RCTs (5 with EMG biofeedback, 2 with EEG biofeedback) with 321 patients and an average therapy duration of 22 (1–104) weeks were included in the analysis. Four studies conducted a follow-up after an average of 13 (1–26) weeks (Evidence Report, Tab. 44; [4, 7, 15, 29, 33, 41, 51]). The quality of the evidence was moderate (low methodological quality, moderate external validity; Evidence Report, Tab. 45). The low methodological quality resulted in a downgrade of the level of evidence. The efficacy was low: the standardized mean difference (SMD; biofeedback vs. controls) of pain at the end of therapy was significant (Evidence Report, Tab. 46 and Fig. 14). The dropout rate was 12% and did not significantly differ from controls (Evidence Report, Fig. 14). 2 | Der Schmerz 3 · 2012 Side effects were reported inconsistently. One study of EEG biofeedback reported twice as many side effects in the biofeedback group as in the control group [33], whereas another study reported no “significant” side effects in both groups [41]. No indication of serious side effects was found in the literature. The availability of biofeedback is limited (can be an element of cognitive behavioral therapy). Hypnosis and guided imagery Evidence-based recommendation Hypnosis/guided imagery can be used. EL 3a, open recommendation, strong consensus Comment. The literature search resulted in 55 hits. The data of one study were specified in two publications [19, 20]. Four studies were excluded because they were either experimental (one single session) [10, 19, 20] or because they were combined with cognitive behavioral therapy [9, 39]. Five randomised controlled trials (RCTs) with an average therapy duration of 16 (6– 26) weeks and 146 patients and were analysed. A follow-up examination was reported in two studies with an average duration of 8 weeks (4 and 12 weeks; Evidence Report, Tab. 47; [1, 23, 25, 40, 45]). The quality of the evidence was moderate (low methodological quality, moderate external validity; Evidence Report, Tab. 48). The low case number and the low methodological quality in the studies resulted in a downgrade of the level of evidence by 2 levels. The efficacy was average. The SMDs of pain at the end of therapy and follow-up were high compared to controls (conventional therapy, cognitive behavioral therapy, relaxation training; Evidence Report, Tab. 49, Fig. 15). Side effects were not documented systematically. Risks were probably infrequent but potentially severe [32]. The dropout rate in the studies was 15% and did not differ from controls (Evidence Report, Fig. 15). Hypnosis is covered in compulsory health insurance (psychosomatic primary care). Cognitive behavioral therapy Evidence-based recommendation Cognitive behavioral therapy can be used as monotherapy. EL 1a, open recommendation, consensus Comment. The umbrella term cognitive behavioral therapy includes studies involving cognitive therapy, operant conditioning, behavior therapy and cognitive behavioral therapy. Studies involving mindfulness-based stress reduction (MBSR) can be found in the paper “Complementary and alternative therapies for fibromyalgia syndrome”. Studies covering psychoeducation can be found in the paper “Fibromyalgia syndrome. General principles and coordination of clinical care and patient education”. Studies combining cognitive behavioral therapy and medical training therapy can be found in the paper “Multicomponent therapy of fibromyalgia syndrome”. Literature research resulted in 439 hits. Three studies were excluded because they combined cognitive behavioural therapy with other psychotherapeutic methods [10, 34, 39]. One study was published twice [52, 53]. A total of 13 studies with 659 patients and an average study duration of 11 (5–15) weeks were evaluated. Eleven studies conducted a follow-up after an average of 52 (6–208) weeks (Evidence Report, Tab. 50; [2, 8, 13, 14, 18, 21, 28, 31, 42, 43, 46, 47, 48, 53, 54]). The quality of the evidence was moderate (moderate methodological quality, moderate external validity; Evidence Report, Tab. 51). Cognitive behavioral therapy was not effective in relation to the target variables. However, the SMDs (cognitive behavioral therapy vs. controls) at the end of therapy and at follow-up showed a positive trend regarding pain (Evidence Report, Tab. 52, Fig. 16). The SMDs (cognitive behavioral therapy vs. controls) of depression at the end of therapy and at follow-up were low. The SMDs (cognitive behavioral therapy vs controls) of self-efficacy regarding pain at the end of therapy and at time of catamnesis were high [5]. Abstract · Zusammenfassung The dropout rate was moderate (14%) and did not differ significantly from controls (Evidence Report, Fig. 16). Side effects were not reported systematically (possible symptom increase). Severe side effects were not illustrated in the literature [32]. Cognitive behavioral therapy is included in the guidelines for psychotherapy of the statutory health insurance and is therefore covered. Due to the low risks and wide availability, the recommendation was upgraded by one level. Negative recommendations Relaxation training Evidence-based recommendation Relaxation training should not be used as monotherapy. EL 2a, negative recommendation, strong consensus Comment. The literature search resulted in 207 hits. One study was excluded because the target variables of the study did not fulfill the inclusion criteria of the systematic review [35]. Eight studies with 460 patients and an average study duration of 10 (3–26) weeks were analysed. Three studies conducted a follow up after an average of 22 (16–26) weeks. In all studies relaxation training served as the control group and was compared with other forms of active therapy [16, 17, 24, 26, 30, 38, 44, 45] (Evidence Report, Tab. 53). The quality of the evidence was moderate (low methodological quality, moderate external validity; Evidence Report, Tab. 54). Due to the low methodological quality the recommendation was downgraded. Relaxation training was not effective. As far as pain reduction, relaxation training was inferior to active controls at the end of therapy. No significant differences in sleep disturbance and restrictions on quality of life were found (Evidence Report, Tab. 55 and Fig. 17). The dropout rate was moderate (16%) and did not differ significantly from controls (Evidence Report, Fig. 17). Side effects were not reported systematically. Severe side effects were not described in the literature. Schmerz 2012 · DOI 10.1007/s00482-012-1179-8 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 V. Köllner · W. Häuser · K. Klimczyk · H. Kühn-Becker · M. Settan · M. Weigl · K. Bernardy Psychotherapy for patients with fibromyalgia syndrome. Systematic review, meta-analysis and guideline Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinären Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for Evidence- Based Medicine. The recommendations were based on level of evidence, efficacy (metaanalysis of the outcomes pain, sleep, fatigue and health-related quality of life), acceptability (total dropout rate), risks (adverse events) and applicability of treatment modalities in the German health care system. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. Cognitive behavioral therapy combined with aerobic exercise (multicomponent therapy) is strongly recommended. Relaxation as single therapy should not be applied.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Systematic review · Meta-analysis · Guideline · Psychotherapy Psychotherapie von Patienten mit Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom AWMF Registernummer 041/004 wurde ab März 2011 vorgenommen. Methodik. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie DIVS von neun wissenschaftlichen Fachgesellschaften und zwei Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potentielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt. Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center for EvidenceBased Medicine. Grundlage der Empfehlungen waren die Evidenzstärke, die Wirksam- Relaxation training is included in the list of medical services covered by the statutory health insurance (psychosomat- keit (Metaanalyse der Zielvariablen Schmerz, Schlaf, Müdigkeit und gesundheitsbezogene Lebensqualität), die Akzeptanz (Abbruchrate in Studien), Risiken (Nebenwirkungen) und die Anwendbarkeit der Therapieverfahren im deutschen Gesundheitssystem. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Kognitive Verhaltenstherapie in Kombination mit Ausdauertraining (multimodale Therapie) wird stark empfohlen. Entspannungstraining als Monotherapie soll nicht eingesetzt werden. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Psychotherapie ic primary care, element of cognitive behavioral therapy). Der Schmerz 3 · 2012 | 3 Schwerpunkt Tab. 1 Modifications of level of recommendation for psychotherapy in the first and second version of the guidelines Therapy method Biofeedback Cognitive behavioral therapy Therapeutic writing Level of recommendation 2008 Negative recommendation Strong recommendation Level of recommendation 2012 Recommended Open recommendation Recommended Negative recommendation Therapeutic writing Evidence-based finding Therapeutic writing should not be used as monotherapy. EL 2a, negative recommendation, strong consensus Comment. The literature search resulted in 13 hits. One study was published twice [6, 27]. Two studies with 166 patients were analysed [6, 22]. Due to the short study duration (one week), the first examination was not conducted at the end of therapy but rather after 4 and 12 weeks, and the last follow-up after 12 and 40 weeks respectively. To have comparable time intervals the data was chosen for the analysis 12 weeks after the end of the intervention (Evidence Report, Tab. 56). The quality of the evidence was moderate (high methodological quality, moderate external validity) (Evidence Report, Tab. 57). The evidence level was downgraded due to insufficient data. No efficacy was found compared to controls (conventional writing; Evidence Report, Tab. 58, Fig. 18). Acceptability was moderate. The dropout rate was 16% and did not differ from controls (Evidence Report, Fig. 18). Side effects were not reported. Based on psychotherapeutic experience, psychological decompensation resulting from the measure is possible. Principally, the measure may be used based upon psychosomatic primary care or psychotherapeutic guidelines. No positive or negative recommendation possible Other forms of psychotherapy (client-centered therapy (Rogers), couple and family therapy, humanistic therapy, systematic therapy) Evidence-based finding Neither a positive nor negative recommendation of other forms of psychotherapy (client-centered therapy (Rogers), couple and family therapy, humanistic therapy, systematic therapy) is possible due to insufficient data. Strong consensus Comment. The literature search resulted in 60 hits. Neither controlled or uncontrolled nor case studies were found in other forms of psychotherapy used as monotherapy (client-centered therapy (Rogers), couple and family therapy, humanistic therapy, systematic therapy). In a Dutch non-randomized study, 50 patients received a combination of cognitive behavioral therapy (9 sessions) and couple therapy (10 sessions) over a period of 9 months. No significant differences in pain and sleep were found at the end of therapy when compared to controls [12]. Psychodynamic psychotherapy and psychoanalysis therapy Evidence-based finding Due to insufficient data, neither a positive nor negative recommendation of psychodynamic psychotherapy and psychoanalysis therapy is possible. Strong consensus Comment. The literature research resulted in 21 hits. Neither (un-)controlled studies of psychodynamic therapy nor studies of interpersonal therapy were found. 4 | Der Schmerz 3 · 2012 In Germany, 2 RCTs were found using psychodynamic therapy in patients with FMS/somatoform pain disorder, the results of which have not yet been published (Egle 2007, personal communication: Scheidt 2010, personal communication). In 1 RCT, 54 patients received equal parts of cognitive behavioral therapy and interpersonal therapy over a period of 8 weeks, 2 h per week. They were compared with the waiting group of 47 patients. No significant differences were found in pain and quality of life at the end of therapy and at follow-up (12 weeks) [34]. Discussion In comparison with the first version of the guidelines [49], lower recommendations for cognitive behavioral therapy were made because of the modifications made in establishing the recommendations (taking into account the quantity and quality of evidence, meta-analysis, taking into consideration the risks and availability instead of qualitative analysis of the main results of the studies). Due to the quantitative data synthesis, the recommendation for therapeutic writing changed from positive to negative, and for biofeedback, from negative to positive (. Tab. 1). Research desiderata: F studies of dose–response relationships of psychotherapy, F randomized clinical trials comparing standard psychotherapy with “customized” psychotherapy (e.g. different approaches for subgroups of various types of pain management or with comorbid major depression) and F development of easily assessable short-term psychotherapy for minor manifestations and review of cost effectiveness. Corresponding address Prof. Dr. V. Köllner Department of Psychosomatic Medicine, Mediclin Bliestal Clinics 66440 Blieskastel Germany Volker.Koellner@mediclin.de Conflict of interest. See Tab. 5 in “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Alvarez-Nemegyei J, Negreros-Castillo A, NuñoGutiérrez BL et al (2007) Ericksonian hypnosis in women with fibromyalgia syndrome. Rev Med Inst Mex Seguro Soc 45:395–401 (Spanish) 2. Ang DC, Chakr R, Mazzuca S et al (2010) Cognitivebehavioral therapy attenuates nociceptive responding in patients with fibromyalgia: a pilot study. Arthritis Care Res (Hoboken) 62:618–623 3. Arnold B, Häuser W, Bernateck M et al (2012) Systematische Übersicht, Metaanalyse und Leitlinie: Multimodale Therapie des Fibromyalgiesyndrom. Schmerz 26:287-290 4. Babu AS, Mathew E, Danda D, Prakash H (2007) Management of patients with fibromyalgia using biofeedback: a randomized control trial. Indian J Med Sci 61:455–461 5. Bernardy K, Füber N, Köllner V, Häuser W (2010) Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome – a systematic review and metaanalysis of randomized controlled trials. J Rheumatol 37:1991–2005 6. Broderick JE, Junghaenel DU, Schwartz JE (2005) Written emotional expression produces health benefits in fibromyalgia patients. Psychosom Med 67:326–334 7. Buckelew SP, Conway R, Parker J et al (1998) Biofeedback/relaxation training and exercise interventions for fibromyalgia: a prospective trial. Arthritis Care Res 11:196–209 8. Burckhardt CS, Mannerkorpi K, Hedenberg L, Bjelle A (1994) A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol 21:714–720 9. Castel A, Pérez M, Sala J et al (2007) Effect of hypnotic suggestion on fibromyalgic pain: comparison between hypnosis and relaxation. Eur J Pain 11:463–468 10. Castel A, Salvat M, Sala J, Rul M (2009) Cognitivebehavioural group treatment with hypnosis: a randomized pilot trail in fibromyalgia. Contemp Hypn 26:48–59 11. Cedraschi C, Desmeules J, Rapiti E et al (2004) Fibromyalgia: a randomised, controlled trial of a treatment programme based on self management. Ann Rheum Dis 63:290–296 12. De Voogd JN, Knipping AA, Blécourt ACE de, Rijswijk MH van (1993) Treatment of fibromyalgia syndrome with psychomotor therapy and marital counselling. J Musculoskel Pain 1:273–281 13. Edinger JD, Wohlgemuth WK, Krystal AD, Rice JR (2005) Behavioral insomnia therapy for fibromyalgia patients: a randomized clinical trial. Arch Intern Med 165:2527–2535. 14. Falcao DM, Sales L, Leite JR, Feldman D, Valim V, Natour J (2008) Cognitive behavioral therapy for the treatment of fibromyalgia syndrome: A randomized controlled trial. J Musculoskel Pain 16:133–140 15. Ferraccioli G, Ghirelli L, Scita F et al (1987) EMG-biofeedback training in fibromyalgia syndrome. J Rheumatol 14:820–825 16. Field T, Diego M, Cullen C et al (2002) Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. J Clin Rheumatol 8:72–76 17. Field T, Delage G, Hernandez-Reuf M (2003) Movement and massage therapy reduce fibromyalgia pain. J Bodyw Mov Ther 149–152 18. Fontaine KR, Conn L, Clauw DJ (2010) Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Res Ther 12:R55 19. Fors EA, Götestam KG (2000) Patient education, guided imagery and pain related talk in fibromyalgia coping. Eur J Psychiatr 14:233–240 20. Fors EA, Sexton H, Götestam KG (2002) The effect of guided imagery and amitriptyline on daily fibromyalgia pain: a prospective, randomized, controlled trial. J Psychiatr Res 36:179–187 21. Garcia J, Simon MA, Duran M et al (2006) Differential efficacy of a cognitive-behavioral intervention versus pharmacological treatment in the management of fibromyalgic syndrome. Psychol Health Med 11:498–450 22. Gillis ME, Lumley MA, Mosley-Williams A et al (2006) The health effects of at-home written emotional disclosure in fibromyalgia: a randomized trial. Ann Behav Med 32:135–146 23. Grøndahl JR, Rosvold EO (2008) Hypnosis as a treatment of chronic widespread pain in general practice: a randomised controlled pilot trial. BMC Musculoskelet Disord 9:124 24. Günther V, Mur E, Kinigadner U, Miller C (1994) Fibromyalgia – the effect of relaxation and hydrogalvanic bath therapy on the subjective pain experience. Clin Rheumatol 13:573–578 25. Haanen HC, Hoenderdos HT, Romunde LK van et al (1991) Controlled trial of hypnotherapy in the treatment of refractory fibromyalgia. J Rheumatol 18:72– 75 26. Hammond A, Freeman K (2006) Community patient education and exercise for people with fibromyalgia: a parallel group randomized controlled trial. Clin Rehabil 20:835–846 27. Junghaenel DU, Schwartz JE, Broderick JE (2008) Differential efficacy of written emotional disclosure for subgroups of fibromyalgia patients. Br J Health Psychol 13:57–60 28. Kashikar-Zuck S, Swain NF, Jones BA, Graham TB (2005) Efficacy of cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. J Rheumatol 32:1594–1602 29. Kayiran S, Dursun E, Dursun N et al (2010) Neurofeedback intervention in fibromyalgia syndrome; a randomized, controlled, rater blind clinical trial. Appl Psychophysiol Biofeedback 35:293–302 30. Keel PJ, Bodoky C, Gerhard U, Muller W (1998) Comparison of integrated group therapy and group relaxation training for fibromyalgia. Clin J Pain 14:232–238 31. King SJ, Wessel J, Bhambhani Y et al (2002) The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol 29:2620–2627 32. Kleinhauz M (1999) Negative Reaktionen bei der Anwendung von Hypnose. Hypn Kognit 8:1–12 33. Kravitz HM, Esty ML, Katz RS, Fawcett J (2006) Treatment of fibromyalgia syndrome using low-intensity neurofeedback with the flexyx neurotherapy system: a randomized controlled clinical trial. J Neurother 10:41–58 34. Langford MM (2010) The efficacy of a combined cognitive-behavioural and interpersonal therapy approach to the treatment of fibromyalgia syndrome: a randomized controlled trial. Dissertation Abstracts International: Section B: The Sciences and Engineering 71(3-B):2052 35. Lund I, Lundeberg T, Carleson J et al (2006) Corticotropin releasing factor in urine -a possible biochemical marker of fibromyalgia. Responses to massage and guided relaxation. Neurosci Lett 403:166–171 (Reported target variables not suited for analysis) 36. Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C (2000) Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol 27:2473–2481 37. Mannerkorpi K, Nordeman L, Ericsson A et al (2009) Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med 41:751– 760 38. Martin L, Nutting A, MacIntosh BR et al (1996) An exercise program in the treatment of fibromyalgia. J Rheumatol 23:1050–1053 39. Martínez-Valero C, Castel A, Capafons A et al (2008) Hypnotic treatment synergizes the psychological treatment of fibromyalgia: a pilot study. Am J Clin Hypn 50:311 40. Menzies V, Taylor AG, Bourguignon C (2006) Effects of guided imagery on outcomes of pain, functional status, and self-efficacy in persons diagnosed with fibromyalgia. J Altern Complement Med 12:23–30 41. Nelson DV, Bennett RM, Barkhuizen A et al (2010) Neurotherapy of fibromyalgia? Pain Med 11:912– 919 42. Nicassio PM, Radojevic V, Weisman MH et al (1997) A comparison of behavioural and educational interventions for fibromyalgia. J Rheumatol 24:2000– 2007 43. Redondo JR, Justo CM, Moraleda FV et al (2004) Long-term efficacy of therapy in patients with fibromyalgia: a physical exercise-based program and a cognitive-behavioral approach. Arthritis Rheum 51:184–192 44. Richards SC, Scott DL (2002) Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. BMJ 325:185 45. Rucco V, Feruglio C, Genco F, Mosanghini R (1995) Autogenic training versus Erickson’s analogical technique in treatment of fibromyalgia syndrome. Riv Eur Sci Med Farmacol 17:41–50 (Italian) 46. Soares JJF, Grossi G (2002) A randomised, controlled comparison of educational and behavioral interventions for woman with fibromyalgia. Scand J Occup Ther 9:35–45 47. Thieme K, Gromnica-Ihle E, Flor H (2003) Operant behavioral treatment of fibromyalgia: a controlled study. Arthritis Rheum 49:314–320 48. Thieme K, Flor H, Turk DC (2006) Psychological pain treatment in fibromyalgia syndrome: efficacy of operant behavioral and cognitive behavioral treatments. Arthritis Res Ther 8:R121 49. Thieme K, Häuser W, Batra A et al (2008) Psychotherapie bei Patienten mit Fibromyalgiesyndrom. Schmerz 22:295–302 50. Koulil S van, Lankveld W van, Kraaimaat FW et al (2010) Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res (Hoboken) 62:1377–1385 51. Santen M van, Bolwijn P, Verstappen F et al (2002) A randomized clinical trial comparing fitness and biofeedback training versus basic treatment in patients with fibromyalgia. J Rheumatol 29:575–581 52. Vlaeyen NJG, Goossens JWS, Rutten-Van Mölken MEJB (2005) Efficacy of a cognitive-educational group treatment programme for patients with fibromyalgia. Teeken-Gruben, Gedrag & Gezondheid: Tijdschrift voor Psychologie en Gezondheid 23:191– 205 53. Vlaeyen JW, Teeken-Gruben NJ, Goossens ME et al (1996) Cognitive-educational treatment of fibromyalgia: A randomized clinical trial. I. Clinical effects. J Rheumatol 23:1237–1245 54. Wigers SH, Stiles TC, Vogel PA (1996) Effects of aerobic exercise versus stress management treatment in fibromyalgia. A 4.5 year prospective study. Scand J Rheumatol 25:77–86 Der Schmerz 3 · 2012 | 5 Schwerpunkt English Version of "Medikamentöse Therapie des Fibromyalgiesyndroms. Systematische Übersicht und Metaanalyse". DOI 10.1007/s00482-012-1172-2 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 C. Sommer1 · W. Häuser2 · R. Alten3 · F. Petzke4 · M. Späth5 · T. Tölle6 · N. Üçeyler1 · A. Winkelmann7 · E. Winter8 · J. Bär9 1 Neurologische Klinik, Universitätsklinikum Würzburg 2 Innere Medizin 1, Klinikum Saarbrücken gGmbH, Saarbrücken 3 Schlossparkklinik Berlin 4 Schmerz-Tagesklinik und -Ambulanz, Universitätsmedizin Göttingen, Georg-August-Universität Göttingen 5 Rheumatologische Praxis, München-Gräfelfing, Munich-Gräfelfing 6 Klinik für Neurologie, Technische Universität München, Munich 7 Klinik und Poliklinik für Physikalische Medizin und Rehabilitation, Klinikum der Universität München, Munich 8 Klinik für Innere Medizin mit Schwerpunkt Psychosomatik, Charité Universitätsmedizin Berlin 9 Klinik für Psychiatrie und Psychotherapie, Friedrich-Schiller-Universität Jena Pharmacological treatment of fibromyalgia syndrome Systematic review and meta-analysis For the revision of the guideline the working groups asked the following questions: 1.Is pharmacological treatment effective in the short- and long-term in fibromyalgia syndrome (FMS)? 2.Which risks are associated with pharmacological treatment of FMS? 3.Which drugs should be avoided in treatment of FMS? Materials and methods The methodology of literature search and analysis, and preparation of recommendations are presented separately in the article “Methodological fundamentals used in developing the guideline”. Results Preliminary notes a)The following findings apply to adults. For the pharmacological treatment of FMS and chronic widespread pain in children and adolescents please refer to the paper “Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. b)In Germany no drug is licensed for the treatment of FMS. We performed quantitative analyses for drug classes but not for individual drugs. Exceptions are duloxetine, milnacipran (MLN) and pregabalin (PGB), since these substances have been investigated in several large studies during registration trials. Recommendations Duloxetine Evidence-based recommendation FMS patients with comorbid depressive disorder and/or generalized anxiety disorder should be treated with duloxetine (60 mg/day) for a limited period of time. EL 1a, recommendation, consensus Remark: In Germany duloxetine is not licensed for the treatment of FMS. It is licensed for the treatment of depressive disorders and generalized anxiety disorders. Comment. Duloxetine is a serotonin– noradrenalin reuptake inhibitor with a five-fold stronger effect on serotonin than on noradrenalin. Literature search revealed 46 hits. One study was excluded from meta-analysis, because it contained an 8 week non-blinded pre-phase and did not have a placebo group during the double-blind phase [29]. For quantitative analysis of data on drug effectiveness five randomized, controlled trials (RCT) with 8 drug treatment arms (different dose regimens of duloxetine) were included investigating 1,397 patients. The mean study duration was 20 (12–26) weeks (Evidence Report, Tab. 59; [4, 5, 8, 30, 94]). Quality of evidence was moderate (Evidence Report, Tab. 60). In contrast to the RCT with milnacipran (MLN) and pregabalin (PGB), patients with major depression (all studies) and with generalized anxiety disorders (one study) were included in duloxetine studies. The effectiveness of duloxetine was moderate (Evidence Report, Tab. 61 and Fig. 19). Standardized mean differences (SMD) of duloxetine versus placebo for pain, sleep, and healthrelated quality of life were low. Small posDer Schmerz 3 · 2012 | 1 Schwerpunkt itive effects of duloxetine on sleep were reported only in one study, although data were obtained in all studies. Sleep disturbance is a frequent side effect of duloxetine; therefore the reported positive results should be interpreted with caution. The acceptance of duloxetine was low: the dropout rate was high (33%) and did not differ from placebo controls (Evidence Report, Fig. 19). Risks were high: several subjectively relevant side effects of duloxetine were observed in >10% compared to placebo. Very rare severe (potentially life-threatening) complications like suicidality and liver toxicity have been reported during duloxetine treatment [29]. The recommendation was downgraded due to the limited availability and the potential risks. Tricyclic antidepressants Evidence-based recommendation Amitriptyline (AMT; 10–50 mg/day) should be used for a limited period of time. EL 2a, recommendation, strong consensus Remark: In Germany AMT is not licensed for the treatment of FMS. It is licensed for the treatment of chronic pain in the context of a comprehensive therapy concept. Comment. Literature search revealed 103 hits. Three studies were excluded due to inappropriate endpoints [20, 66, 83]; 3 studies were excluded due to the combination of AMT with other treatment methods [44, 64, 106], and 1 study because of missing randomization. Data of 1 study were only available as an abstract [40]. For quantitative analysis 18 studies with 19 drug treatment arms and a mean study duration of 8 (2–24) weeks were assessed investigating 1,014 patients. AMT was applied in 14 studies, nortriptyline and dothiepin were used in one study each (Evidence Report, Tab. 62, [11, 13, 24, 25, 26, 27, 28, 39, 46, 49, 52, 53, 57, 59, 61, 69, 99, 114]). Quality of evidence was moderate; methodological quality and external validity were low (Evidence Report, Tab. 63). Evidence was downgraded by one point due to low methodological quality. 2 | Der Schmerz 3 · 2012 Effectiveness was moderate. SMD of tricyclic antidepressants versus placebo at the end of treatment were moderate for pain, sleep, and fatigue and also for health-related quality of life (Evidence Report, Tab. 64, Fig. 20). Acceptance was moderate with a dropout rate of 14% that did not differ from placebo (Evidence Report, Fig. 20). Side effects were not assessed systematically. According to the Summary of Product Characteristics (SmPC) subjective relevant side effects are reported in >10% of patients under AMT compared to placebo. These include symptoms like drowsiness and dry mouth. Potentially life-threatening side effects like liver and bone marrow toxicity were very rarely reported (<0.1%). AMT is licensed for the treatment of chronic pain in the context of a comprehensive therapy concept. Open recommendations Duloxetine Evidence-based recommendation Treatment with duloxetine (60 mg/day) can be considered for a limited time period in patients without comorbid depressive disorder or generalized anxiety disorder, if treatment with AMT is not possible (e.g. due to contraindications), was not effective or was not tolerated (“off-label use”). EL 1a, open recommendation, consensus Comment. When using duloxetine in patients without comorbid depressive disorder or generalized anxiety disorder the following criteria for “off-label use” should be considered: F proven effectiveness, F positive risk–benefit profile, F lack of alternatives, F individual trial for curing the disease. Therefore “off-label use” is permitted only in severe cases when alternative treatment options are missing. The perspective for treatment success on the basis of current scientific knowledge is mandatory. Moreover, detailed patient information is obligatory. Patients must be informed about of “off-label use” and about possible liabili- ties. It is necessary to reach a decision in consensus with the patient. Pregabalin Evidence-based recommendation Treatment with pregabalin (PGB; 150– 450 mg/day) can be considered for a limited time period, if treatment with AMT is not possible (e.g. due to contraindications), was not effective or was not tolerated (“off-label use”). EL 1a, open recommendation, consensus Comment. When using PGB in patients without comorbid depressive disorder or generalized anxiety disorder the following criteria for “off-label use” should be considered: F proven effectiveness, F positive risk–benefit profile, F lack of alternatives, F individual trial for curing the disease. Therefore “off-label use” is permitted only in severe cases when treatment alternatives are lacking. The perspective for treatment success on the basis of current scientific knowledge is mandatory. Moreover, detailed patient information is obligatory. Patients must be informed about of “offlabel use” and about possible liabilities. It is necessary to reach a decision in consensus with the patient. Literature search for anticonvulsants revealed 154 hits. Studies on PGB and gabapentin (GPT) were found. The study using GPT is referred to in the section on evidence-based recommendations for GPT. One study investigating PGP could not be used for quantitative analysis [34]; 4 studies with 12 drug treatment study arms and a study duration of 12 (8– 14) weeks investigating 4,132 patients were analyzed (Evidence Report, Tab. 65; [7, 33, 76, 86]). Quality of evidence was moderate with moderate quality of methods and low external validity. Patients with generalized anxiety disorders were not explicitly included (Evidence Report, Tab. 66). The effectiveness of PGB was moderate: SMD of PGB versus placebo at the end of treatment were small for pain and sleep and not significant for fatigue and health-re- Abstract · Zusammenfassung lated quality of life (Evidence Report, Tab. 67, Fig. 21). Acceptance was low: the dropout rate was 32%; the relative risk for dropout was higher in the drug treatment compared to the placebo group. Risks of PGB were high: the difference of the frequency of some subjectively relevant side effects was >10% in the drug treatment group compared to placebo (Evidence Report, Fig. 21; [60]). Practicability is limited. In Germany PGB is not licensed for the treatment of FMS, but for the treatment of generalized anxiety disorders and of neuropathic pain. Due to the low patients’ acceptance, the limited license, and the ethical commitment to protect patients from harm the recommendation was downgraded by two points. Serotonin reuptake inhibitors Evidence-based recommendation Serotonin reuptake inhibitors (SSRI; fluoxetine: 20–40 mg/day, paroxetine: 20–40 mg/day) can be considered for a limited time period in patients with comorbid depressive disorder and anxiety disorder. EL 2a, open recommendation, consensus Note: In Germany fluoxetine and paroxetine are licensed for the treatment of depressive and anxiety disorders, but not for FMS. Comment. The literature search revealed 130 hits. Three studies were excluded because study endpoints did not fulfill inclusion criteria [23, 48, 81]. Thirteen studies with a mean study duration of 10 (4– 26) weeks were qualitatively analyzed including 610 patients (Evidence Report, Tab. 68; [1, 3, 11, 24, 40, 53, 54, 56, 64, 80, 83, 100, 115]). Methodological quality of evidence was low; external validity was moderate (Evidence Report, Tab. 69). Therefore the level of evidence was downgraded. Effectiveness was moderate. SMD of SSRI versus placebo were significant for pain, sleep, and health-related quality of life; effect size was small (Evidence Report, Tab. 70, Fig. 22). Acceptance was moderate. The dropout rate was 19% and did not differ from Schmerz 2012 · DOI 10.1007/s00482-012-1172-2 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 C. Sommer · W. Häuser · R. Alten · F. Petzke · M. Späth · T. Tölle · N. Üçeyler · A. Winkelmann · E. Winter · J. Bär Pharmacological treatment of fibromyalgia syndrome. Systematic review and meta-analysis Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinäre Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The recommendations were based on level of evidence, efficacy (meta- analysis of the outcomes pain, sleep, fatigue and health-related quality of life), acceptability (total dropout rate), risks (adverse events) and applicability of treatment modalities in the German health care system. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. Amitriptyline and—in case of comorbid depressive disorder or generalized anxiety disorder—duloxetine are recommended. Off-label use of duloxetine and pregabalin can be considered in case of no comorbid mental disorder. Strong opioids are not recommended.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Systematic review · Meta-analysis · Guideline · Combined modality therapy Medikamentöse Therapie des Fibromyalgiesyndroms. Systematische Übersicht und Metaanalyse Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center for Evidence Based Medicine. Grundlage der Empfehlungen waren die Evidenzstärke, die Wirksamkeit (Metaanalyse der Zielvariablen Schmerz, Schlaf, Müdigkeit und gesundheitsbezogene Lebensqualität), die Akzeptanz (Abbruchrate in Studien), Risiken (Nebenwirkungen) und die Anwendbarkeit der Therapieverfahren im deutschen Gesundheitssystem. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Amitriptylin und – bei komorbiden depressiven Störungen oder generalisierter Angststörung – Duloxetin werden empfohlen. Der Off-label-Gebrauch von Duloxetin oder Pregabalin kann im Falle von fehlenden komorbiden depressiven Störungen oder fehlender generalisierter Angststörung erwogen werden. Starke Opioide werden nicht empfohlen. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Multimodale Therapie Der Schmerz 3 · 2012 | 3 Schwerpunkt placebo (Evidence Report, Fig. 22). Side effects were not systematically assessed in the studies. Rare severe side effects are described in literature, e.g. bleedings [2]. Practicability is limited: in Germany the analyzed SSRI are not licensed for the treatment of FMS, but for the treatment of depression and partly of anxiety disorders. The evidence level was downgraded due to potential risks and the lack of a license for FMS in Germany. Stong negative recommendations Antiviral drugs Evidence-based recommendation Antiviral drugs should not be used. EL 2b, strong negative recommendation, strong consensus Comment. The literature search revealed five hits. In one RCT 30 patients each received valaciclovir 1 g or placebo for 6 weeks. At the end of treatment no differences were found regarding pain and health-related quality of life. In both groups 4 out of 30 patients stopped treatment [70]. Severe side effects of virostatics are reported in the literature. Virostatics are neither licensed for FMS nor for frequent comorbidities. Due to the high risks and the low availability the negative recommendation was further downgraded. Anxiolytics Evidence-based recommendation Anxiolytics should not be used. EL 2a, strong negative recommendation, strong consensus Comment. The literature search revealed 36 hits. Two studies were suitable for analysis: one study each with alprazolam and bromazepam [88, 92]. A quantitative data synthesis could not be performed. Due to the limited data the evidence level was downgraded. Quality of evidence was moderate [see studies on nonsteroidal antirheumatics (NSAR)]. Anxiolytics were ineffective: in a study over 8 weeks no difference was found between treatment with placebo plus alprazolam (up to 3 mg/day; 17 patients) and treatment with double placebo 4 | Der Schmerz 3 · 2012 (14 patients) with regard to pain reduction and improvement of health-related quality of life [92]. In a study over 8 weeks no difference was found between treatment with bromazepam (3 mg/day; 42 patients) and placebo (42 patients) with regard to the number of patients that experienced a reduction in pain intensity or in morning stiffness of at least 25% [88]. Bromazepam is not licensed for the treatment of FMS, but for the treatment of chronic anxiety and of chronic stress (limited practicability). Anxiolytics can be used for the treatment of anxiety disorders [12]. Due to the high risks, the ethical commitment to protect patients from harm, and the limited availability the negative recommendation further downgraded. Dopamine agonists Evidence-based recommendation Dopamine agonists should not be used. EL 2a, strong negative recommendation, strong consensus Comment. The literature search revealed 56 hits. Three studies with a study duration of 12 weeks including 300 patients were analyzed (Evidence Report, Tab. 71; [37, 51, 62]). Due to the limited data the evidence level was downgraded. The quality of evidence was moderate with moderate quality of methodology and external validity (Evidence Report, Tab. 72). Dopamine agonists were not effective (no superiority to placebo in reducing pain or increasing health related quality of life; Evidence Report, Tab. 73, Fig. 23). Acceptance was low: the dropout rate was 55.5% and was not higher than in the placebo group (Evidence Report, Fig. 23). Frequent side effects (>10% compared to placebo) were sleep disturbance, nausea, weight loss, and abdominal pain. Rare severe side effects of dopamine agonists are reported in the literature. Dopamine agonists are licensed for the treatment of FMS. Pramipexole is licensed for the treatment of Parkinson’s disease and of the moderate and severe restless legs syndrome. The level of negative recommendation was downgraded by one point because do- pamine agonists are not licensed for FMS and due to the low patients’ acceptance. Hormones (calcitonin, testosterone, estrogens, glucocorticosteroids, thyroid hormones, growth factors) Evidence-based recommendation Hormones (calcitonin, testosterone, estrogens, glucocorticosteroids, thyroid hormones, growth factors) should not be used. EL 3a, strong negative recommendation, strong consensus Comment. The literature search revealed 128 hits. The level of evidence was downgraded due to the limited number of studies. Due to the potential risks and the lacking license for FMS or for frequent comorbidities a downgrade of evidence levels by one point was performed for all substances. One RCT was found for calcitonin. In a cross-over RCT 11 patients received 100 IU calcitonin s.c. or saline for 4 weeks. No intergroup difference was found with regard to pain, fatigue, sleep, and pain reduction. One of the 11 patients stopped treatment with calcitonin because of side effects. Side effects appeared frequently (nausea, erythema) [18]. One RCT was found using testosterone-like substances. In a cross-over RCT 52 postmenopausal women were treated with dehydroepiandrosterone (DHEA; 50 mg/day) for 1 month; results were not different compared to placebo with regard to pain, sleep disturbance, and fatigue [53]. One RCT was found using estrogen-like substances. In an Iranian study 50 postmenopausal women were treated with the selective estrogen modulator raloxifene 60 mg for 16 weeks; 50 women received placebo. Raloxifene was superior to placebo with regard to pain, sleep, and fatigue. The dropout rate was 4% [95]. No relevant side effects were reported. Estrogens or the combination of estrogen and gestagen can be used for the treatment of climacteric symptoms like hot flush considering possible risks [36]. One RCT was found investigating the effect of glucocorticosteroids. In a USAmerican cross-over RCT with 20 patients, oral prednisone (15 mg/day) treat- ment for 14 days was not superior to placebo in reducing pain, sleep disturbance, and fatigue [31]. In another RCT of 8 and 9 months duration, 7 and 4 euthyroid patients, respectively, were alternately treated with supraphysiological doses of T3 (93.75–150 μg/ day) or placebo. Significant pain reduction was reported at the end of the T3 treatment phase. No side effects were reported in this study; however, they seem possible (induction of hyperthyroidism; [71, 72]). Two studies were found investigating growth hormones [15, 35]. Quantitative analysis was not possible. In one study 25 patients were treated with growth hormone (0.0125 mg/kg s.c.) or placebo for 9 months. Health-related quality of life was higher in the growth hormone group compared to the placebo group. In another study 12 patients were treated with growth hormone (0.0125 mg/kg s.c.) or placebo for 1 year in addition to a multimodal and pharmacological treatment (AMT, fluoxetine, tramadol). At the end of the study health-related quality of life was higher in the group with additional growth hormone treatment; also pain and fatigue were lower compared to the placebo group. Dropout rates were low (0–13.6%). Side effects (edema, anemia, carpal tunnel syndrome, hyperglycemia, hypertriglyceridemia) were observed only in the growth hormone group. Hypnotics Evidence-based recommendation Hypnotics should not be used. EL 3a, strong negative recommendation, strong consensus Comment. The literature search revealed 143 hits. Three RCT were found. A quantitative analysis was not possible due to a lack of appropriate data. Due to the low methodological quality of evidence and the limited number of RCT available the level of evidence was downgraded by two points. The effectiveness of hypnotics is not proven. In a cross-over RCT 19 patients were treated with 5–15 mg zolpidem or placebo for 2 weeks [76]. No intergroup differences were found for pain, sleep, and fatigue. In another RCT 14 patients were treated with zopiclone 7.5 mg/day and 19 patients with placebo [55]. After 8 weeks no significant differences were found with regard to pain and sleep. In one RCT 22 patients were treated with zopiclone 7.5 mg/day and 23 patients with placebo [38]. At the end of treatment zopiclone was superior to placebo in reducing sleep disturbances and fatigue, but not in pain reduction. Dropout rates were 4–10%. Hypnotics can be misused. Hypnotics are not licensed for the treatment of FMS. However, they are licensed for the treatment of sleep disturbances during a limited time period. Due to the high risks and the limited practicability the negative recommendation was further downgraded by one point. Interferons Evidence-based recommendation Interferons should not be used. EL 3a, strong negative recommendation, strong consensus Comment. The literature search revealed 5 hits. In one RCT 28 patients each received placebo, 15 IU, 50 IU or 150 IE interferon-α s.c. At the end of treatment no intergroup difference was found for pain, sleep, and fatigue. Dropout rates were not reported separately for each group [93]. The side effects reported were mild and as for the authors not related to the medication. Severe side effects are reported in the literature after treatment with high doses of interferons. Due to the high risks and the low practicability the negative recommendation was further downgraded by one point. Intravenous (i.v.) ketamine Evidence-based recommendation I.v. ketamine should not be used. EL 4a, strong negative recommendation, strong consensus Comment. The literature search revealed 17 hits. Two experimental studies (infusion therapy once and twice) were exclud- ed [10, 104]. No studies with oral ketamine application were found. In a cross-over study 20 patients received ketamine 1 mg/kg body weight for 3 days versus placebo [78]. No intergroup differences were found for pain intensity and health-related quality of life. Study quality was low. Due to the limited data and the low methodological quality the recommendation was downgraded by two points. Severe neuropsychiatric side effects are reported. Due to the potential risks and the low practicability the negative recommendation was further downgraded by one point. Local anesthetics Evidence-based recommendation Intravenous local anesthetics should not be used. EL 3a, strong negative recommendation, strong consensus Comment. The literature search revealed 62 hits. Three studies investigating 177 patients and with a study duration of 4 weeks each were included in qualitative analysis. The quality of evidence and methodology were low and also the number of patients investigated. Therefore the level of evidence was downgraded by two points. Local anesthetics were ineffective. A quantitative data analysis was not possible due to insufficient data presentation in the publications. In both placebo-controlled studies no intergroup difference was found for pain reduction when using lidocaine or placebo [73, 86]. In one study no intergroup difference was found for the reduction of fatigue [73]. The add-on therapy with lidocaine or placebo in addition to AMT did not increase pain reduction [112]. Acceptance was moderate (dropout rate: 0–16%). The risks are high. Pain was >10% more frequently reported during lidocaine infusion than during placebo [73]. In an observational study using 550 mg lidocaine/6 h for 6 consecutive days lung edema and supraventricular tachycardia were reported [91]. Due to the potential risks, the ethical commitment to protect patients from harm, and the low practicability the negaDer Schmerz 3 · 2012 | 5 Schwerpunkt tive recommendation was downgraded by two points. Neuroleptics Sodium oxybate Neuroleptics should not be used. EL 3a, strong negative recommendation, strong consensus Serotonin receptor (5-HT3) antagonists Comment. The literature search revealed 17 hits. One RCT and three case series were found. Due to the limited data the grade of evidence was downgraded. In the RCT 24 female patients were treated with ritanserin 10 mg/day and 27 female patients were treated with placebo for 16 weeks [81]. At the end of treatment no intergroup difference was found for pain, sleep, and fatigue. Three patients in the ritanserin group discontinued the study. In Germany neuroleptics is neither licensed for the treatment of FMS nor for the treatment of frequent psychiatric comorbidities. Due to the potential risks, the ethical commitment to protect patients from harm and the low practicability the negative recommendation was downgraded by two points. Serotonin receptor (5-HT3) antagonists should not be used. EL 3a, strong negative recommendation, strong consensus Evidence-based recommendation Sodium oxybate should not be used. EL 3a, strong negative recommendation, strong consensus Comment. Sodium oxybate increases the turnover of 5-hydroxytryptamine, interacts with the opioid system, and GABA antagonistic effects are assumed. The literature search revealed 13 hits. Three studies with five study arms investigating 358 patients were included in the analysis; the mean study duration was 7 (4–8) weeks (Evidence Report, Tab. 74; [77, 95, 98]). Methodological quality of evidence was low (Evidence Report, Tab. 75). The obtained data were incompletely reported (selective reporting). Therefore the level of evidence was downgraded by two points. The effectiveness of sodium oxybate was moderate (Evidence Report, Tab. 76, Fig. 24). SMD of sodium oxybate versus placebo for pain, sleep, fatigue, and health-related quality of life were significant at the end of treatment. SMD was low for health-related quality of life and moderate for pain, fatigue, and sleep. Acceptance was moderate (dropout rate: 24%) and was not different from placebo (Evidence Report, Fig. 24). Risks were high. Frequent side effects (>10% difference to placebo) were nausea, drowsiness, and headache or paresthesias. In 6% of the patients treated with 6 g/day urinary incontinence was observed. In Germany sodium oxybate is neither licensed for the treatment of FMS nor for the treatment of frequent psychiatric comorbidities. Sodium oxybate is licensed for the treatment of narcolepsy. Due to the high risks, the ethical commitment to protect patients from harm, and lack of license the recommendation was downgraded by two points. 6 | Der Schmerz 3 · 2012 Evidence-based recommendation Strong opioids Evidence-based recommendation Strong opioids should not be used. EL 4b, strong negative recommendation, strong consensus Comment. One RCT was excluded from analysis, because it was an experimental study with one-time morphine application [103]. No RCT were found for other strong opioids (buprenorphine, fentanyl, hydromorphone, oxycodone). In one case series 16 patients received fentanyl 25 µg/h transdermally over 72 h. Treatment was continued for 4–8 weeks. No pain reduction or increase in health-related quality of life was found. All patients reported on side effects (confusion, nausea, vomiting). Seven of the 16 patients discontinued treatment [22]. The availability is limited. In Germany fentanyl is not licensed for the treatment of FMS, but for the treatment of severe pain. Due to the low patients’ acceptance, the high risks, and the limited license the rec- ommendation was downgraded by two points. Evidence-based recommendation Comment. The literature search revealed 43 hits. Three RCT were analyzed. In one study three different dosages of tropisetron (5, 10, 15 mg) were compared with placebo. For quantitative analysis only the 5 mg study arm was considered, because the two other study arms did not differ from placebo [104]. Three studies investigating 260 patients and with a mean study duration of 1 week (5–10 days) were analyzed (Evidence Report, Tab. 77; [41, 63, 105]). Due to the limited data and the low quality of evidence (low methodological quality and low external validity) the level of evidence was downgraded by two points (Evidence Report, Tab. 78). The difference of SMD comparing serotonin receptor (5-HT3) antagonists with placebo was not significant (Evidence Report, Tab. 79, Fig. 25). The dropout rate was low (4.6%) and was not different from placebo (Evidence Report, Fig. 25). One frequent subjective side effect (>10% versus placebo) was obstipation. Serotonin receptor (5-HT3) antagonists are not licensed for the treatment of FSM or of comorbidities. Due to the side effects and the lack of license the negative recommendation was further downgraded by one point. Negative recommendations Cannabinoids Evidence-based recommendation Cannabinoids should not be used. EL 3a, negative recommendation, strong consensus Comment. The literature search revealed 9 hits. Two RCT were analyzed [101, 113]. A quantitative data analysis was not possi- ble, because none of the studies were placebo-controlled. Due to the limited data the evidence level was downgraded by one point. The quality of evidence was moderate. A quantitative data analysis was not possible. The effectiveness was low. In a cross-over study 32 patients were treated with nabilone 0.5 mg or AMT 10 mg [113]. Nabilone was superior to AMT in improving sleep quality. No intergroup difference was found for pain reduction or improvement of health-related quality of life. In a RCT 20 patients received nabilone 0.5–1 mg/day and 20 patients received placebo for 4 weeks. At the end of the study nabilone was superior to placebo with regard to pain reduction and improvement of health-related quality of life. In one study 3 of 32 patients discontinued. The other study does not give details [101]. Frequently observed side effects were dizziness (nabilone: 47%; placebo: 6%; [110]), drowsiness (nabilone: 35%; AMT: 14%), and nausea (nabilone: 31%; AMT: 14%; [101]). Misuse of nabilone is rare [114]. In Germany nabilone is neither licensed for the treatment of FMS, nor for the treatment of frequent psychiatric comorbidities. Due to potential risks and the lack of license the recommendation was downgraded by one point. Flupirtine Evidence-based recommendation Flupirtine should not be used. EL 4, negative recommendation, consensus Comment. Flupirtine is not a muscle relaxant [109]. Only two small case series are available investigating the effect of flupirtine in FMS; both report on pain reduction [106, 116]. Severe liver toxicity as a side effect is reported in the literature [87]. Due to a lack of licence and the potential side effects the recommendation was downgraded by one point. Milnacipran Evidence-based recommendation Milnacipran (MLN) should not be used. EL 1a, negative recommendation, consensus Comment. MLN is a serotonin–noradrenalin reuptake inhibitor with a threefold higher effect on serotonin than on noradrenalin. Literature search revealed 37 hits. Two studies were published twice [47, 111]. Five studies with 8 study arms and investigating 4,088 patients were analyzed; mean study duration was 19 (15–27) weeks (Evidence Report, Tab. 80; [9, 21, 32, 75, 111]). The quality of evidence and of methodology was moderate; external validity was low (Evidence Report, Tab. 81). SMD of MLN versus placebo at the end of therapy were significant for pain and health-related quality of life but not substantially (Evidence Report, Tab. 82, Fig. 26). Acceptance for MLN was low: dropout rate was high (33%) and was not different from placebo (Evidence Report, Fig. 26). The risks of MLN were high: the difference of the frequency of some subjectively relevant side effects was >10% compared to placebo. In Germany MLN is neither licensed for the treatment of FMS nor for the treatment of frequent psychiatric comorbidities. Monoamine oxidase inhibitors Evidence-based recommendation Monoamine oxidase inhibitors should not be used. EL 2a, negative recommendation, strong consensus Comment. The literature search revealed 27 hits. One RCT was excluded because moclobemide and placebo, respectively, were combined with biofeedback therapy [117]. Two RCT were analyzed investigating 149 patients and with a mean study duration of 7 (4–12) weeks (Evidence Report, Tab. 83; [50, 59]). Due to limited data the level of evidence was downgraded. The quality of evidence was moderate with moderate methodological quality and low external validity (Evidence Report, Tab. 84). With regard to pain, sleep, and fatigue monoamine oxidase inhibi- tors did not differ from placebo (Evidence Report, Tab. 85, Fig. 27). Acceptance was moderate (dropout rate: 22%) and was not different from placebo (Evidence Report, Fig. 27). Nausea was a relevant side effect with a difference of >10% compared to placebo. Rare severe side effects are reported in literature. Monoamine oxidase inhibitors are not licensed for the treatment of FMS, but for the treatment of depressive disorders. Muscle relaxants Evidence-based recommendation Muscle relaxants should not be used. EL 2a, negative recommendation, strong consensus Comment. The literature search revealed 45 hits. Eleven studies were analyzed. One study was excluded from quantitative analysis, because carisoprodol was combined with caffeine and acetaminophen [110]. Due to a lack of standard deviations one study with several study arms (e.g. 7 patients treated with cyclobenzaprine 10 mg) could not be used for quantitative analysis [46]. Nine studies with a mean study duration of 6 (1–26) weeks and investigating 527 patients could partially be used for analysis; six of these studies were performed placebo-controlled [14, 23, 26, 45, 46, 85, 97, 110]. In eight RCT the centrally active agent cyclobenzaprine was applied. Cyclobenzaprine additionally has properties of tricyclic antidepressants. In one RCT chlormezanone was used; chlormezanone additionally has properties of benzodiazepines (Evidence Report, Tab. 86). The quality of evidence was moderate (Evidence Report, Tab. 87). Due to the low methodological quality the level of evidence was downgraded by one point. The quantitative data synthesis was limited due to a lack of standard deviations in the majority of studies. Drug effectiveness can only be assessed for the endpoint pain. Effectiveness was low: SMD of muscle relaxants versus placebo at the end of treatment was low for pain (Evidence Report, Tab. 88, Fig. 28). Acceptance and tolerability were moderate: the dropout rate in the RCT was Der Schmerz 3 · 2012 | 7 Schwerpunkt 20% and did not differ from placebo (Evidence Report, Fig. 28). The relative risk for dropout was lower compared to placebo. The risks of cyclobenzaprine are high: very rare, but potentially life-threatening side effects (confusion, skin lesions, liver toxicity) are described in the literature. None of the substances that have been investigated in the studies is licensed in Germany. Due to the potential risks, the lack of license, and ethical commitment to protect patients from harm the recommendation was downgraded by two points. Nonsteroidal antirheumatics Evidence-based recommendation Nonsteroidal antirheumatics (NSAR) should not be used. EL 3a, negative recommendation, strong consensus Comment. The literature search revealed 79 hits. Four studies with a mean duration of 5 (1.2–8) weeks and investigating 181 patients were considered for quantitative analysis (three studies with ibuprofen, one study with tenoxicam; Evidence Report, Tab. 89; [42, 45, 92, 118]). No studies were found with cyclooxygenase (COX)2 inhibitors. The quality of evidence was moderate with moderate methodological quality and high external validity (Evidence Report, Tab. 90). Due to the low methodological quality and the low number of cases the level of evidence was downgraded by two points. A quantitative data synthesis was only possible for the outcome pain. No effectiveness was reported. SMD of NSAR versus placebo was not significant at the end of treatment (Evidence Report, Tab. 91, Fig. 29). One study found no intergroup difference between placebo and tenoxicam concerning the number of subjects that reached pain reduction and reduction in morning fatigue scores of at least 25% [42]. Reduction of pain and of sleep disturbance was not different between cyclobenzaprine monotherapy and the combination of cyclobenzaprine with ibuprofen 600 mg [45]. Side effects were not systematically assessed in the studies. In the SmPC on NSAR, e.g. gastrointestinal bleeding is 8 | Der Schmerz 3 · 2012 reported as frequent and severe side effect. The dropout rate was moderate in the studies (20%) and was not different compared to placebo (Evidence Report, Fig. 29). In Germany NSAR are not licensed for the treatment of FMS, but for the treatment of mild and moderate pain of the musculoskeletal system. Due to potential risks and the ethical commitment to protect patients from harm the recommendation was further downgraded by one point. No positive or negative recommendation possible Gabapentin Evidence-based recommendation Due to the limited data available for gabapentin (GPT) neither a positive nor a negative recommendation is possible. Strong consensus Comment. One RCT was found which investigated the effect of GPT 1,200– 2,400 mg versus placebo in 75 patients each for 12 weeks [6]. The quality of evidence was moderate with high methodological quality and low external validity. At the end of treatment GPT was superior to placebo in reduction of pain and sleep disturbance and improvement of health-related quality of life. Patients’ acceptance was moderate: the dropout rate was 24% for GPT and 17.3% for placebo. Side effects with a difference of >10% to placebo were dizziness and drowsiness. Very rare (<0.01%) severe side effects (hematological impairment, liver toxicity, acute renal failure, dermatological problems) are given for GPT in expert reports. The practicability is low: in Germany GPT is licensed for the treatment of epilepsy and of neuropathic pain, but not for the treatment of FMS or comorbid psychiatric disorders. Noradrenaline reuptake inhibitors Evidence-based recommendation Due to the limited data available for noradrenaline reuptake inhibitors (NRI) nei- ther a positive nor a negative recommendation is possible. Strong consensus Comment. The results of one study with esreboxetine [79] were not yet published. One published study with the NRI esreboxetine was found [10]. In this study 134 patients were treated with esreboxetine (dose increase from 1 to 8 mg/day) and 133 patients received placebo for 8 weeks. The dropout rate was 20.1% in the esreboxetine group and 20.3% in the placebo group. Esreboxetine was superior to placebo in terms of reducing pain, fatigue, and improving health-related quality of life. Study quality was high, the external validity was low. Reported side effects were insomnia, drowsiness, dry mouth, nausea, hyperhidrosis, voiding disturbance (only in men) and urinary retention (only in men). Esreboxetine is not available worldwide. Pfizer has stopped registration trials for esreboxetine in FMS. Weak opioids Evidence-based recommendation Due to the limited data available (tramadol) or lack of data (other weak opioids) neither a positive nor a negative recommendation is possible for weak opioids. Strong consensus Comment. The literature search revealed 74 hits. Only RCT with tramadol, but not with tilidine or codeine were found. One RCT was excluded from the analysis, because it was an experimental study with twice i.v. application of tramadol [19]. One further study was excluded due to double publication [16, 17]. One study with tramadol and tramadol/acetaminophen, respectively, was included into the analysis investigating 384 patients and with a mean treatment duration of 9.5 (6–13) weeks [16]. Due to the limited number of studies the level of evidence was downgraded. In both studies tramadol and tramadol/acetaminophen, respectively, were superior to placebo with regard to pain reduction and improvement of health-related quality of life. Acceptance was low (dropout rate: 40%). However, the dropout rate was higher the placebo groups Tab. 1 Changes in level of recommendation for pharmacological treatment of FMS in the first and second version of the guidelines Treatment Amitriptyline Anxiolytics Cannabinoids Dopamine agonists Duloxetine Recommendation 2008 Strong recommendation Negative recommendation Not considered Open recommendation Recommendation Flupirtine Hormones (calcitonin, testosterones, estrogens, glucocorticosteroids, thyroid hormones, growth hormones) Hypnotics Ketamine Local anesthetics Milnaciprane Monoamine oxidase inhibitors Sodium oxybate Neuroleptics Nonsteroidal antirheumatics Metamizole Muscle relaxants Weak opioids (tramadole) Strong opioids Acetaminophen Pregabalin Serotonin reuptake inhibitors (fluoxetine, paroxetine) No statement Negative recommendation Negative recommendation Negative recommendation Negative recommendation No statement Open negative recommendation Negative recommendation Negative recommendation Negative recommendation Negative recommendation Open negative recommendation Open recommendation Open recommendation Negative recommendation Open recommendation Recommendation Serotonin receptor agonists (tropisetrone) Virostatics Open recommendation Negative recommendation compared to the tramadol groups. The most frequently reported side effect with a difference of >10% to placebo was nausea. Rare severe side effects (misuse) are reported in the literature [108]. The availability is limited. In Germany tramadol is not licensed for the treatment of FMS, but for the treatment of moderate to severe pain. Acetylsalicylic acid, acetaminophen, and metamizole Evidence-based recommendation Due to the lack of data neither a positive nor a negative recommendation is possible for acetyl salicylic acid, acetaminophen, and metamizole. Strong consensus Comment. No studies were found for acetylsalicylic acid, acetaminophen, and metamizole. Recommendation 2012 Recommendation Strong negative recommendation Negative recommendation Strong negative recommendation Recommendation when comorbid depressive disorder or generalized anxiety disorder Negative recommendation Strong negative recommendation Strong negative recommendation Strong negative recommendation Strong negative recommendation Strong negative recommendation Negative recommendation Strong negative recommendation Strong negative recommendation Strong negative recommendation No positive or negative recommendation Negative recommendation No positive or negative recommendation Strong negative recommendation No positive or negative recommendation Open recommendation (“off-lable use”) Open recommendation when comorbid depressive disorder Strong negative recommendation Strong negative recommendation Discussion Compared to the first version of the guideline the basis of recommendations was changed: Quantity and quality of evidence were considered, meta-analysis was performed, risks and availability were considered instead of pure qualitative analysis of the main study results. This led to a downgrade of recommendations for some drugs (e.g. AMT) [102]. Taking into account the licensed indications, a positive recommendation resulted only for FMS with comorbid psychological disorders for duloxetine, fluoxetine, and paroxetine. Due to insufficient data the open recommendation for the weak opioid tramadol was abolished (. Tab. 1). The following research objectives were identified: a)studies investigating the sustained effect after treatment cessation, b)randomized, controlled studies comparing “old” (cheap) drugs like AMT with “new” (expensive) drugs like PGB, c)direct comparison of active treatments (e.g. two forms of psychotherapy or psychotherapy versus pharmacological treatment) and d)inclusion of patients with comorbid psychological disorders and eventually their subgroup analysis. Corresponding address Prof. Dr. C. Sommer Neurologische Klinik, Universitätsklinikum Würzburg Josef-Schneider-Str. 11, 97080 Würzburg Germany sommer@uni-wuerzburg.de Conflict of interest. See Tab. 5 in the “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. Der Schmerz 3 · 2012 | 9 Schwerpunkt References 1. Anderberg UM, Marteinsdottir I, von Knorring L (2000) Citalopram in patients with fibromyalgia—a randomized, double-blind, placebo-controlled study. Eur J Pain 4:27–35 2. Andrade C, Sandarsh S, Chethan KB, Nagesh KS (2010) Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry 71:1565–1575 3. Arnold LM, Hess EV, Hudson JI et al (2002) A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 112:191– 197 4. Arnold LM, Lu Y, Crofford LJ et al (2004) A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum 50:2974–2984 5. Arnold LM, Rosen A, Pritchett YL et al (2005) A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain 119:5–15 6. Arnold LM, Goldenberg DL, Stanford SB et al (2007) Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial. Arthritis Rheum 56:1336–1344 7. Arnold LM, Russell IJ, Diri EW et al (2008) A 14-week, randomized, double-blinded, placebocontrolled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain 9:792–805 8. Arnold LM, Clauw D, Wang F et al (2010a) Flexible dosed duloxetine in the treatment of fibromyalgia: a randomized, double-blind, placebocontrolled trial. J Rheumatol 37:2578–2586 9. Arnold LM, Gendreau RM, Palmer RH et al (2010b) Efficacy and safety of milnacipran 100 mg/day in patients with fibromyalgia: results of a randomized, double-blind, placebocontrolled trial. Arthritis Rheum 62:2745–2756 10. Arnold LM, Chatamra K, Hirsch I, Stoker M (2010c) Safety and efficacy of esreboxetine in patients with fibromyalgia: an 8-week, multicenter, randomized, double-blind, placebo-controlled study. Clin Ther 32:1618–1632 11. Ataoglu S, Ataoglu A, Erdogan F, Sarac J (1997) Comparison of paroxetine, amitriptyline in the treatment of fibromyalgia. Turk J Med Sci 27:535–539 12. AWMF Leitlinie Angststörung. http://www.awmf. org/leitlinien/detail/ll/028-022.html. Accessed 02 June 2012 13. Azad KAK, Alam MN, Haq SA et al (2000) Vegetarian diet in the treatment of fibromyalgia. Bangladesh Med Res Counc Bull 26:41–47 14. Bennett RM, Gatter RA, Campbell SM (1988) A comparison of cyclobenzaprine and placebo in the management of fibrositis. A double-blind controlled study. Arthritis Rheum 31:1535–1542 15. Bennett RM, Clark SC, Walczyk J (1998) A randomized, double-blind, placebo-controlled study of growth hormone in the treatment of fibromyalgia. Am J Med 104:227–231 16. Bennett RM, Kamin M, Karim R, Rosenthal N (2003) Tramadol and acetaminophen combination tablets in the treatment of fibromyalgia pain: a double-blind, randomized, placebo-controlled study. Am J Med 114:537–545 10 | Der Schmerz 3 · 2012 17. Bennett RM, Schein J, Kosinski MR et al (2005) Impact of fibromyalgia pain on health-related quality of life before and after treatment with tramadol/acetaminophen. Arthritis Rheum 53:519–527 (Duplicate publication) 18. Bessette L, Carette S, Fosse A (1998) A placebo controlled crossover trial of subcutaneous salmon calcitonin in the treatment of patients with fibromyalgia. Scand J Rheumatol 27:112–116 19. Biasi G, Manca S, Manganelli S, Marcolongo R (1998) Tramadol in the fibromyalgia syndrome: a controlled clinical trial versus placebo. Int J Clin Pharmacol Res 18:13–19 (Experimental study) 20. Bibolotti E, Borghi C, Pasculii E et al (1986) The management of fibrositis. A double-blind comparison of maprotiline, chlomipramine and placebo. Clin Trials 23:269–280 (Endpoints not suitable for analysis) 21. Branco JC, Zachrisson O, Perrot S et al (2010) A European multicenter randomized double-blind placebo-controlled monotherapy clinical trial of milnacipran in treatment of fibromyalgia. J Rheumatol 37:851–859 22. Callejas Rubio JL, Fernández Moyano A, Navarro Hidalgo D, Palmero Palmero C (2003) Percutaneous fentanyl in fibromyalgia. Med Clin (Barc) 120:358–359 23. Cantini F, Bellandi F, Niccoli L et al (1994) Fluoxetin combined with cyclobenzaprine in the treatment of fibromyalgia. Minerva Med 85:97–100 24. Capaci K, Hepgüler S (2002) Comparison of the effects of amitriptyline and paroxetine in the treatment of fibromyalgia syndrome. Pain Clinic 14:223–228 25. Carette S, McCain GA, Bell DA, Fam AG (1986) Evaluation of amitriptyline in primary fibrositis. A double-blind, placebo-controlled study. Arthritis Rheum 29:655–659 26. Carette S, Bell MJ, Reynolds WJ et al (1994) Comparison of amitriptyline, cyclobenzaprine, and placebo in the treatment of fibromyalgia. A randomized, double-blind clinical trial. Arthritis Rheum 37:32–40 27. Carette S, Oakson G, Guimont C, Steriade M (1995) Sleep electroencephalography and the clinical response to amitriptyline in patients with fibromyalgia. Arthritis Rheum 38:1211– 1217 28. Caruso I, Sarzi Puttini PC, Boccassini L et al (1987) Double-blind study of dothiepin versus placebo in the treatment of primary fibromyalgia syndrome. J Int Med Res 15:154–159 29. Chappell AS, Littlejohn G, Kajdasz DK et al (2009) A 1-year safety and efficacy study of duloxetine in patients with fibromyalgia. Clin J Pain 25:365– 375 30. Chappell AS, Bradley LA, Wiltse C et al (2009) A six-month double-blind, placebo-controlled, randomized clinical trial of duloxetine for the treatment of fibromyalgia. Int J Gen Med 1:91– 102 31. Clark S, Tindall E, Bennett RM (1985) A double blind crossover trial of prednisone versus placebo in the treatment of fibrositis. J Rheumatol 12:980–983 32. Clauw DJ, Mease P, Palmer RH et al (2008) Milnacipran for the treatment of fibromyalgia in adults: a 15-week, multicenter, randomized, double-blind, placebo-controlled, multiple-dose clinical trial. Clin Ther 30:1988–2004 33. Crofford LJ, Rowbotham MC, Mease PJ et al (2005) Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, doubleblind, placebo-controlled trial. Arthritis Rheum 52:1264–1273 34. Crofford LJ, Mease PJ, Simpson SL et al (2008) Fibromyalgia relapse evaluation and efficacy for durability of meaningful relief (FREEDOM): a 6-month, double-blind, placebo-controlled trial with pregabalin. Pain 136:419–431 (Study design not suitable for meta-analysis) 35. Cuatrecasas G, Gonzalez MJ, Alegre C et al (2010) High prevalence of growth hormone deficiency in severe fibromyalgia syndromes. J Clin Endocrinol Metab 95:4331–4337 36. Deutsche Gesellschaft für Gynäkologie und Geburtshilfe. Hormontherapie (HT) in der Peri- und Postmenopause. http://www.awmf.org/leitlinien/detail/ll/015-062.html. Accessed 02 June 2012 37. Distler O, Eich W, Dokoupilova E et al (2010) Evaluation of the efficacy and safety of terguride in patients with fibromyalgia syndrome: results of a twelve-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum 62:291–300 38. Drewes HM (1991) Zopiclone in the treatment of sleep abnormalities in fibromyalgia. Scand J Rheumatol 20:288–293 39. Eksioglu E, Yazar D, Bal A et al (2007) Effects of stanger bath therapy on fibromyalgia. Clin Rheumatol 26:691–694 40. Erhan E, Uyar M, Turan et al (2000) Ağrı. Fibromyalji tedavisinde amitriptilin ve fluvoksaminin karşılaştırılması 1:32–36 [Turkish] (Only abstract available. Authors did not respond to emails) 41. Färber L, Stratz T, Brückle W et al (2000) Efficacy and tolerability of tropisetron in primary fibromyalgia—a highly selective and competitive 5-HT3 receptor antagonist. German Fibromyalgia Study Group. Scand J Rheumatol Suppl 113:49–54 42. Fernández-Rodriguez A, Hernánz-Mediano W, Gutierrez-Rubio A et al (1996) Comparison of tenoxicam and bromazepan in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled trial. Pain 65:221–225 43. Finckh A, Berner IC, Aubry-Rozier L (2005) A randomized controlled trial of de-hydroepiandrosterone in postmenopausal women with fibromyalgia. J Rheumatol 32:1336–1340 44. Fors EA, Sexton H, Gotestam KG (2002) The effect of guided imagery and Amitriptyline on daily fibromyalgia pain: a prospective, randomized, controlled trial. J Psychiatr Res 36:179–187 (Combination of AMT with guided imagination) 45. Fosaluzza V, Vita S de (1992) Combined therapy with cyclobenzaprine and ibuprofen in primary fibromyalgia syndrome. Int J Clin Pharmacol Res XII:99–102 46. Garcia J, Simon MA, Duran M et al (2006) Differential efficacy of a cognitive-behavioral intervention versus pharmacological treatment in the management of fibromyalgic syndrome. Psychol Health Med 11:498–450 47. Gendreau RM, Thorn MD, Gendreau JF et al (2005) Efficacy of milnacipran in patients with fibromyalgia. J Rheumatol 32:1975–1985 48. Giordano N, Geraci S, Santacroce C et al (1999) Efficacy and tolerability of paroxetine in patients with fibromyalgia syndrome: a single-blind study. Curr Ther Res 60:696–702 (Description of endpoints not suitable) 49. Ginsberg F, Mancaux A, Joos E (1996) A randomized placebo-controlled trial of sustained-release amitriptyline in primary fibromyalgia. J Musculoskel Pain 4:37–47 50. Ginsberg F, Joos E, Geczy J et al (1998) A pilot randomized placebo-controlled study of pirlindole in the treatment of primary fibromyalgia. J Musculoskel Pain 6:6–17 51. Glaxo Protocol No ROF102100. A randomised, double-blind, placebo controlled, parallel group study to investigate the safety and efficacy of controlled-release ropinirole (CR) (1–24 mg) administered once daily for 12 weeks in subjects with fibromyalgia. http://www.clinicalstudyresults.org/documents/company-study_5744_0. pdf. Accessed 09 August 2010 52. Goldenberg DL, Felson DT, Dinerman H (1986) A randomized, controlled trial of amitriptyline and naproxen in the treatment of patients with fibromyalgia. Arthritis Rheum 29:1371–1377 53. Goldenberg D, Mayskiy M, Mossey C et al (1996) A randomized, double-blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis Rheum 39:1852 54. Gonzalez-Viejo MA, Avellanet M, HernandezMorcuende MI (2005) A comparative study of fibromyalgia treatment: ultrasonography and physiotherapy versus sertraline treatment. Ann Readapt Med Phys 48(8):610–615 (French) 55. Gronblad M, Nykanen J, Konttinen Y (1993) Effect of zopiclone on sleep quality, morning stiffness, widespread tenderness and pain and general discomfort in primary fibromyalgia patients. A double-blind randomized trial. Clin Rheumatol 12:186–191 56. Gülec H, Capkin E, Sayar K (2007) The evaluation of the effectiveness of amitriptyline versus venlafaxine in female patients diagnosed with fibromyalgia syndrome. Klinik Psikofarmakoloji Buelteni 17:68–73 (Turkish) 57. Gür A, Karakoc M, Nas K et al (2002) Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int 22:188–193 58. Hamaty D, Valentine JL, Howard R et al (1989) The plasma endorphin, prostaglandin and catecholamine profile of patients with fibrositis treated with cyclobenzaprine and placebo: a 5-month study. J Rheumatol Suppl 19:164–168 59. Hannonen P, Malminiemi K, Yli-Kerttula U et al (1998) A randomized, double-blind, placebo-controlled study of moclobemide and amitriptyline in the treatment of fibromyalgia in females without psychiatric disorder. Br J Rheumtol 37:1279–1286 60. Häuser W, Bernardy K, Uçeyler N, Sommer C (2009) Treatment of fibromyalgia syndrome with gabapentin and pregabalin-a meta-analysis of randomized controlled trials. Pain 145:69–81 61. Heymann RE, Helfenstein M, Feldman D (2001) A double-blind, randomized, controlled study of amitriptyline, nortriptyline and placebo in patients with fibromyalgia. An analysis of outcome measures. Clin Exp Rheumatol 19:697–702 62. Holman AJ, Myers RR (2005) A randomized, double-blind, placebo-controlled trial of pramipexole, a dopamine agonist, in patients with fibromyalgia receiving concomitant medications. Arthritis Rheum 52:2495–2505 63. Hrycaj P, Stratz T, Mennet P (1996) Pathogenetic aspects of responsiveness to ondansetron (5-hydroxytryptamine type 3 receptor antagonist) in patients with primary fibromyalgia syndrome-a preliminary study. J Rheumatol 23:1418–1423 64. Hussain SA, Al-Khalifa II, Jasim NA, Gorial FI (2010) Adjuvant use of melatonin for treatment of fibromyalgia. J Pineal Res. DO:10.1111/j.1600079X.2010.00836.x 65. Isomeri R, Mikkelsson M, Latikka P, Kammonen K (1993) Effects of amitriptyline and cardiovascular fitness training on pain in patients with primary fibromyalgia. J Muscul Pain 1:253–260 (Combination of AMT with stretching) 66. Jaeschke R, Adachi J, Guyatt G et al (1991) Clinical usefulness of amitriptyline in fibromyalgia: the results of 23 N-of-1 randomized controlled trials. J Rheumatol 18:447–451 (Endpoints reported not suitable for analysis) 67. Jang ZY, Li CD, Qiu L et al (2010) Combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome: a multi-central randomized controlled trial. Zhongguo Zhen Jiu 30:265–269 ([Article in Chinese]. Endpoints reported in English abstract not suitable for analysis) 68. Joshi MN, Joshi R, Jain AP (2009) Affect of amitriptyline vs. physiotherapy in management of fibromyalgia syndrome: What predicts a clinical benefit? J Postgrad Med 55:185–189 (No randomization) 69. Kempenaers C, Simenon G, Vander Elst M (1994) Effect of an antidiencephalon immune serum on pain and sleep in primary fibromyalgia. Neuropsychobiology 30:66–72 70. Kendall SA, Schaadt ML, Graff LB et al (2004) No effect of antiviral (valacyclovir) treatment in fibromyalgia: a double blind, randomized study. J Rheumatol 31:783–784 71. Lowe JC, Reichman AJ, Yellin BA (1997) The process of change during T3 treatment for euthyroid fibromyalgia: a double-blind placebo-controlled crossover study. Clin Bulletin Myofas Ther 2:91–124 72. Lowe JC, Garrison R, Reichman AJ et al (1997) Effectiveness and safety of T3 (triiodothyronine) therapy for euthyroid fibromyalgia: a doubleblind placebo-controlled response-driven crossover study. Clin Bulletin Myofas Ther 2:31–58 73. McCleane G (2000) Does intravenous lidocaine reduce fibromyalgia pain? A randomized, double-blind, placebo controlled cross-over study. Pain Clinic 12:181–185 74. Mease PJ, Russell IJ, Arnold LM et al (2008) A randomized, double-blind, placebo-controlled, phase III trial of pregabalin in the treatment of patients with fibromyalgia. J Rheumatol 35:502– 514 75. Mease PJ, Clauw DJ, Gendreau RM et al (2009) The efficacy and safety of milnacipran for treatment of fibromyalgia. a randomized, doubleblind, placebo-controlled trial. J Rheumatol 36:398–409 76. Moldofsky H, Lue FA, Mously C (1996) The effect of zolpidem in patients with fibromyalgia: a dose ranging, double blind, placebo controlled, modified crossover study. J Rheumatol 23:529– 533 77. Moldofsky H, Inhaber NH, Guinta DR, AlvarezHorine SB (2010) Effects of sodium oxybate on sleep physiology and sleep/wake-related symptoms in patients with fibromyalgia syndrome: a double-blind, randomized, placebo-controlled study. J Rheumatol 37:2156–2166 78. Müller A, Rempp C, Kopferschmitt J et al (2005) Effects of intravenous ketamine administered for 3 days in patients with fibromyalgic pain: double-blind, crossover study versus placebo. Douleurs: Evaluation – Diagnostic – Traitement 6:151–159 (French) 79. Musculoskeletal report: Pfizer Stops Work on Esreboxetine for FM. http://www.mskreport.com/ articles.cfm?articleID=3293. Accessed 02 June 2012 80. Nørregaard J, Volkmann H, Danneskiold-Samsøe B (1995) A randomized controlled trial of citalopram in the treatment of fibromyalgia. Pain 61:445–449 81. Olin R, Klein R, Berg PA (1998) A randomised double-blind 16-week study of ritanserin in fibromyalgia syndrome: clinical outcome and analysis of autoantibodies to serotonin, gangliosides and phospholipids. Clin Rheumatol 17:89– 94 82. Ozerbil O, Okudan N, Gokbel H, Levendoglu F (2006) Comparison of the effects of two antidepressants on exercise performance of the female patients with fibromyalgia. Clin Rheumatol 25:495–497 (Endpoints reported not suitable) 83. Patkar AA, Masand PS, Krulewicz S et al (2007) A randomized, controlled, trial of controlled release paroxetine in fibromyalgia. Am J Med 120:448–454 84. Pattrick M, Swannell A, Doherty M (1993) Chlormezanone in primary fibromyalgia syndrome: a double blind placebo controlled study. Br J Rheumatol 32:55–58 85. Pfizer. Protocol No. A0081100: A 14 week, randomized, double-blind, placebo-controlled trial of pregabalin twice daily in patients with fibromyalgia. http://pdf.clinicalstudyresults.org/documents/company-study_4636_0.pdf. Accessed 31 March 2009 86. Posner IA (1994) Treatment of fibromyalgia syndrome with intravenous lidocaine: a prospective, randomized pilot study. J Musculoskel Pain 2:55–65 87. Puls F, Agne C, Klein F et al (2011) Pathology of flupirtine-induced liver injury: a histological and clinical study of six cases. Virchows Arch 458:709–716 88. Quijada-Carrera J, Valenzuela-Castaño A, Povedano-Gómez J et al (1996) Comparison of tenoxicam and bromazepan in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled trial. Pain 65:221–225 89. Quimby LG, Gratwick GM, Whitney CD (1989) A randomized trial of cyclobenzaprine for the treatment of fibromyalgia. J Rheumatol Suppl 19:140–143 90. Raphael JH, Southall JL, Kitas GD (2003) Adverse effects of intravenous lignocaine therapy in fibromyalgia syndrome. Rheumatology (Oxford) 42:185–186 91. Russell IJ, Kamin M, Bennett RM et al (2000) Efficacy of Tramadol in treatment of Pain in Fibromyalgia. J Clin Rheumatol 6:250–257 92. Russell IJ, Fletcher EM, Michalek JE et al (1991) Treatment of primary fibrositis/fibromyalgia syndrome with ibuprofen and alprazolam. A double-blind, placebo-controlled study. Arthritis Rheum 34:552–560 93. Russell IJ, Michalek JE, Kang YK, Richards AB (1999) Reduction of morning stiffness and improvement in physical function in fibromyalgia syndrome patients treated sublingually with low doses of human interferon-alpha. J Interferon Cytokine Res 19:961–968 Der Schmerz 3 · 2012 | 11 Schwerpunkt 94. Russell IJ, Mease PJ, Smith TR et al (2008) Efficacy and safety of duloxetine for treatment of fibromyalgia in patients with or without major depressive disorder: results from a 6-month, randomized, double-blind, placebo-controlled, fixed-dose trial. Pain 136:432–444 95. Russell IJ, Perkins AT, Michalek JE, Oxybate SXB26 Fibro\myalgia Syndrome Study Group (2009) Sodium oxybate relieves pain and improves function in fibromyalgia syndrome: a randomized, double-blind, placebo-controlled, multicenter clinical trial. Arthritis Rheum 60:299–309 96. Sadreddini S, Molaeefard M, Noshad H et al (2008) Efficacy of Raloxifen in treatment of fibromyalgia in menopausal women. Eur J Intern Med 19:350–355 97. Santandrea S, Montrone F, Sarzi-Puttini P et al (1993) A double-blind crossover study of two cyclobenzaprine regimens in primary fibromyalgia syndrome. J Int Med Res 21:74–80 98. Scharf MB, Baumann M, Berkowitz DV (2003) The effects of sodium oxybate on clinical symptoms and sleep patterns in patients with fibromyalgia. J Rheumatol 30:1070–1074 99. Scudds RA, McCain GA, Rollman GB, Harth M (1989) Improvements in pain responsiveness in patients with fibrositis after successful treatment with amitriptyline. J Rheumatol Suppl 19:98–103 100. Sencan S, Karan A, Muslumanoglu L et al (2004) A study to compare the therapeutic efficacy of aerobic exercise and paroxetine in fibromyalgia syndrome J Back Musculoskeletal Rehabil 17:57–61 101. Skrabek RQ, Galimova L, Ethans K, Perry D (2008) Nabilone for the treatment of pain in fibromyalgia. J Pain 9:164–173 102.Sommer C, Häuser W, Berliner M et al (2008) Medikamentöse Therapie des Fibromyalgiesyndroms. Schmerz 22:313–323 103.Sörensen J, Bengtsson A, Ahlner J et al (1997) Fibromyalgia—are there different mechanisms in the processing of pain? A double blind crossover comparison of analgesic drugs. J Rheumatol 24:1615–1621 (Experimental study) 104.Sörensen J, Bengtsson A, Bäckman E et al (1995) Pain analysis in patients with fibromyalgia. Effects of intravenous morphine, lidocaine, and ketamine. Scand J Rheumatol 24:360–365 (Experimental study) 105.Späth M, Stratz T, Neeck G et al (2004) Efficacy and tolerability of intravenous tropisetron in the treatment of fibromyalgia. Scand J Rheumatol 33:267–270 106.Stoll LA (2000) Fibromyalgia symptoms relieved by Flupirtine: an open-label case series. Psychosomatics 41:371–372 107.Targino RA, Imamura M, Kaziyama HH et al (2008) A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med 40:582–588 (Combination of AMT with multimodal therapy or acupuncture) 108.Tjäderborn M, Jönsson AK, Ahlner J, Hägg S (2009) Tramadol dependence: a survey of spontaneously reported cases in Sweden. Pharmacoepidemiol Drug Saf 18:1192–1198 109.Ueberall MA, Mueller-Schwefe GH, Terhaag B (2011) Efficacy and tolerability of flupirtine in subacute/chronic musculoskeletal pain—results of a patient level, pooled re-analysis of randomized, double-blind, controlled trials. Int J Clin Pharmacol Ther 49:637–647 12 | Der Schmerz 3 · 2012 110.Vaeroy H, Abrahamsen A, Forre O, Kass E (1989) Treatment of fibromyalgia (fibrositis syndrome): a parallel double blind trial with carisoprodol, paracetamol and caffeine (Somadril comp) versus placebo. Clin Rheumatol 8:245–250 111.Vitton O, Gendreau M, Gendreau J et al (2004) A double-blind placebo-controlled trial of milnacipran in the treatment of fibromyalgia. Hum Psychopharmacol 19(Suppl 1):27–35 112.Vlainich R, Issy AM, Gerola LR, Sakata RK (2010) Effect of intravenous lidocaine on manifestations of fibromyalgia. Pain Pract 10:301–305 113.Ware MA, Fitzcharles MA, Joseph L, Shir Y (2010) The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg 110:604–610 114.Ware MA, St Arnaud-Trempe E (2010) The abuse potential of the synthetic cannabinoid nabilone. Addiction 105:494–503 115.Wolfe F, Cathey MA, Hawley DJ (1994) A doubleblind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 23:255–259 116.Wörz R (1991) Flupirtin bei chronischen myofasziellen Schmerzzuständen. Fortschr Med 109:158–160 117.Yavuzer G, Küçükdeveci A, Araslı T, Elhan A (1998) Moclobemid treatment in primary fibromyalgia syndrome. Eur J Phys Med Rehabil 8:35– 38 (Combination with biofeedback) 118.Yunus MB, Masi AT, Aldag JC (1989) Short term effects of ibuprofen in primary fibromyalgia syndrome: a double blind, placebo controlled trial. J Rheumatol 16:527–532 Schwerpunkt English Version of "Komplementäre und alternative Verfahren beim Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie". DOI 10.1007/s00482-012-1178-9 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 J. Langhorst1 · W. Häuser2 · K. Bernardy3 · H. Lucius4 · M. Settan5 · A. Winkelmann6 · F. Musial7 1 Innere Medizin V, Naturheilkunde und Integrative Medizin, Kliniken Essen-Mitte, Essen 2 Klinikum Saarbrücken, Innere Medizin 1, Klinikum Saarbrücken 3 Abteilung für Schmerztherapie, Berufsgenossenschaftliche Universitätsklinik Bergmannsheil GmbH, Ruhr Universität Bochum 4 Schmerzambulanz Schlei-Klinikum/FKSL, Schleswig 5 Deutsche Fibromyalgie Vereinigung, Seckach 6 Klinik und Poliklinik für Physikalische Medizin und Rehabilitation, Klinikum der Universität München 7 National Research Center in Complementary and Alternative Medicine (NAFKAM), Department of Community Medicine, Faculty of Health Science, University of Tromsø Complementary and alternative therapies for fibromyalgia syndrome Systematic review, meta-analysis and guidelines In revising the guidelines, the task groups considered the following questions: 1.Are the complementary and alternative therapies for fibromyalgia syndrome (FMS) effective over short and long periods of time? 2.What are the risks of using complementary and alternative procedures to treat FMS? 3.Which complementary and alternative procedures should be refused in treating FMS? Methodology The procedures utilized for researching and analyzing the literature are presented in the article “Methodological fundamentals used in developing the guideline”. Results The following findings apply to adults. Complementary and alternative procedures for chronic pain affecting multiple body regions in children and youths are discussed in the article entitled “Def- inition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents”. Key recommendations are italicized. Highly recommended Meditative movement therapies (tai chi, qigong, yoga) Evidence-based recommendation Meditative movement therapies (tai chi, qigong, yoga) should be considered. EL1a, highly recommended, strong consensus Comment. The meditative movement therapies analyzed included body-awareness therapy, qigong, tai chi, yoga, and Feldenkrais therapy. A search of the literature identified 46 reports. One trial on Feldenkrais therapy was excluded because it was not randomized [39]. One randomized controlled trial (RCT) with yoga was available only as an abstract [31]. Nine RCTs with 420 patients in therapeutic trials lasting an average of 11 (6– 20) weeks were analyzed. Seven of the trials included follow-up assessments performed on average 20 (6–78) weeks after the treatments had been completed (Evidence Report, Tab. 92; [4, 9, 11, 17, 28, 39, 42, 52, 59]). The evidence was of moderate quality (moderate methodological quality, moderate external validity) (Evidence Report, Tab. 93), as was the efficacy. However, meditative movement therapies were superior to the control group therapies in reducing pain, fatigue, and sleep disorders as assessed at the completion of the respective trials (Evidence Report, Tab. 94 and Fig. 30). Acceptance in the treatment groups was moderate (dropout rate 19%) and did not differ significantly from that of the placebo groups (Evidence Report, Fig. 30). Adverse effects were not reported in the analyzed trials. Availability is limited. Exercise therapies are not covered by health insurance in Germany. They are a part of multimodal therapeutic inpatient Der Schmerz 3 · 2012 | 1 Schwerpunkt programs at some hospitals and are offered by some adult education centers. Acupuncture Acupuncture for comorbid back pain is covered by health insurance in Germany. Because of its potential risks and limited availability, the strength of recommendation was downgraded one level. Evidence-based recommendation Negative recommendation Recommendation open Treatment with acupuncture for a limited period of time may be considered. EL 2a, degree of recommendation open, strong consensus Comment. A search of the literature identified 340 reports. Three RCTs were excluded because the target variables did not fulfill the inclusion criteria [27] or because acupuncture was combined with other active therapeutic procedures [36, 54]. One review [10] included four Chinese trials: two compared acupuncture with amitriptyline and two compared acupuncture in combination (one with cupping and one with an antidepressant) with an antidepressant alone. These studies, which were not contained in the designated databanks and were only published in Chinese, were excluded from the analysis. Thus, 9 RCTs with 414 patients treated for an average of 7 (2–15) weeks were analyzed. Three trials included follow-up assessments after a median of 17 (12–28) weeks (Evidence Report, Tab. 95; [2, 18, 29, 30, 34, 41, 43, 49, 53]). The evidence was of moderate quality (poor methodological quality, moderate external validity) (Evidence Report, Tab. 96). The quality of evidence was downgraded due to the limited methodological quality. Efficacy was limited. The standard mean deviation (SMD) (verum acupuncture vs. sham acupuncture) at the completion of therapy with regard to pain indicated a small effect size (Evidence Report, Tab. 97 and Fig. 31). The dropout rate was 8.2%, which did not differ from that of the control group (Evidence Report, Tab. 31). Adverse effects were systematically reported in only one study. The frequency of severe adverse effects from acupuncture is controversial. However, severe complications such as bleeding or pneumothorax have been reported in the literature [16]. 2 | Der Schmerz 3 · 2012 Mindfulness-based stress reduction as monotherapy Evidence-based recommendation Mindfulness-based stress reduction should not be used as monotherapy. EL 2a negative recommendation, consensus Comment. A search of the literature identified 8 relevant reports. Four RCTs with 371 patients treated with mindfulness-based stress reduction (MBSR) for an average of 8 weeks were analyzed [4, 26, 50, 51]. In three of the trials patients of both arms of the studies were assessed at follow-up an average of 8 weeks after treatment. In one of the trials [26] follow-up evaluations of the MBSR, but not the control group, were carried out after 3 years in 26 of 39 patients (Evidence Report, Tab. 98). The evidence was of moderate quality (poor methodological quality, moderate external validity; Evidence Report, Tab. 99). The secondary end points of one trial were not reported and not made available upon inquiry [51]. Since it is possible that negative results had not been published, the level of evidence was downgraded. MBSR was not effective and was not superior to control treatments with respect to reducing pain or improving quality of life (Evidence Report, Tab. 100 and Fig. 32). Acceptance was moderate (dropout rate 22%) and did not differ significantly from that of the controls (Evidence Report, Fig. 32). Adverse effects were not reported nor have any been mentioned in the literature. Availability is limited. MBSR is not covered by health insurance in Germany. MBSR is offered as part of multimodal therapeutic inpatient programs in a few hospitals. Homeopathy Evidence-based recommendation Homeopathy should not be considered. EL1a negative recommendation, consensus Minority opinion (Complementary and Alternative Medicine Work Group: Langhorst J, Bernardy K, Lucius H, Settan M, Winkelmann A, Musial F): homeopathic therapy may be considered. EL 1a, recommendation open Comment. A search of the literature identified 20 reports. The data of one trial were published twice [7, 8]. Five RCTs with 204 patients and an average trial length of 15 weeks were qualitatively analyzed (Evidence Report, Tab. 101; [7, 8, 23, 24, 46]). The evidence was of moderate quality (moderate methodological quality, moderate external validity), and moderate external validity (Evidence Report, Tab. 102). There was no consistent evidence that homeopathy was effective. Two trials could be quantitatively evaluated [8, 46]. The SMDs (homeopathy versus control at completion of therapy) showed that homeopathy tended to positively affect quality of life (Evidence Report, Tab. 103 and Fig. 33). In the two trials that could not be meta-analyzed, qualitative analysis revealed no consistent evidence that homeopathy was effective. In one trial there was no statistical difference in the reduction of pain and sleep disturbance. One subgroup analysis did show significantly reduced pain and sleep disturbance for those patients who presented at least more than three characteristic symptoms of the prescribed homeopathic medication [23]. One trial showed that a homeopathic treatment reduced pain and sleep disturbance better than a placebo [24]. A subsequent analysis of that trial with appropriate statistical methods did not confirm a significant difference between homeopathic and placebo treatments in the first crossover treatment phase [15]. Acceptance was moderate. The dropout rate, 13%, did not differ significantly from that of the placebo group (Evidence Report, Fig. 33). The risks are probably low: adverse effects were not determined. Relevant side effects are not known from the literature. Abstract · Zusammenfassung Schmerz 2012 · DOI 10.1007/s00482-012-1178-9 © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 J. Langhorst · W. Häuser · K. Bernardy · H. Lucius · M. Settan · A. Winkelmann · F. Musial Complementary and alternative therapies for fibromyalgia syndrome. Systematic review, meta-analysis and guidelines Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinären Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The recommendations were based on level of evidence, efficacy (metaanalysis of the outcomes pain, sleep, fatigue and health-related quality of life), acceptability (total dropout rate), risks (adverse events) and applicability of treatment modalities in the German health care system. The formulation and grading of recommendations was accomplished using a multistep, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. Meditative movement therapies (qigong, tai chi, yoga) are strongly recommended. Acupuncture can be considered. Mindfulness-based stress reduction as monotherapy and dance therapy as monotherapy are not recommended. Homeopathy is not recommended. In a minority vote, homeopathy was rated as “can be considered”. Nutritional supplements and reiki are not recommended.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Fibromyalgia syndrome · Systematic review · Meta-analysis · Guidelines · Complementary therapies Komplementäre und alternative Verfahren beim Fibromyalgiesyndrom. Systematische Übersicht, Metaanalyse und Leitlinie Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolg- The availability is limited: the costs are covered by only a few of the health insurance funds. Minority vote: In the trial reported by Fischer in 1989, homeopathic treatment reduced pain and improved sleep better than a placebo [24]. A subsequent analysis of this trial with modified statistical methods did not show that the homeopathic treatment was sig- te über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center for Evidence Based Medicine. Grundlage der Empfehlungen waren die Evidenzstärke, die Wirksamkeit (Metaanalyse der Zielvariablen Schmerz, Schlaf, Müdigkeit und gesundheitsbezogene Lebensqualität), die Akzeptanz (Abbruchrate in Studien), Risiken (Nebenwirkungen) und die Anwendbarkeit der Therapieverfahren im deutschen Gesundheitssystem. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. nificantly better than the placebo in the initial crossover treatment phase. The author assumed that there is a carry-over effect, i.e., that the effects of the treatment period being observed are partly determined by the effects of the preceding treatment period [15]. However, this was not established by statistical analysis (p=0.07). Since the carry-over effect was not formally demonstrated, the homeo- Ergebnisse und Schlussfolgerung. Meditative Bewegungstherapien (Qigong, Tai-Chi, Yoga) werden stark empfohlen. Die Therapie mit Akupunktur kann erwogen werden. Achtsamkeitsbasierte Stressreduktion als Monotherapie und Tanztherapie als Monotherapie werden nicht empfohlen. Homöopathie wird nicht empfohlen, wobei in einem Minderheitenvotum eine offene Empfehlung („kann erwogen werden“) favorisiert wurde. Nahrungsmittelergänzungsprodukte und Reiki werden nicht empfohlen. Schlüsselwörter Fibromyalgiesyndrom · Systematische Übersicht · Metaanalyse · Leitlinie · Komplementäre Therapien pathic treatment would remain statistically superior. Nutritional supplements Evidence-based recommendation Nutritional supplements (algae and malic acid/magnesium preparations; anthocyanins; carnitine; S-adenosyl methionine, SAM; soya oil; vitamin–dietary minDer Schmerz 3 · 2012 | 3 Schwerpunkt eral preparations) should not be applied. EL3, negative recommendation, strong consensus Comment. Anthocyanins are plant pigments. In the European Union, they are permitted in unlimited amounts as food additives under the number E163. S-adenosyl methionine (SAM) is an essential amino acid. In the USA, SAM is sold as a nutritional supplement under the Dietary Supplement Health and Education Act of 1999. Under this law, nutritional supplements circumvent regulation by the Food and Drug Administration (FDA). SAM can be obtained over the internet. Carnitine is a vitamin-like substance. It can be produced by the body but is usually provided by meat in the diet. In Germany it is permitted for treating the carnitine deficiency of renal insufficiency and special forms of muscular dystrophy. Carnitine can be obtained over the internet. 5-Hydroxytryptophan is an amino acid naturally occurring in bananas and the seeds of African black beans. The substance is not an authorized medication in Germany but can be obtained over the internet as a “natural mood-elevator”. A search of the literature identified 130 reports. Two trials with SAM were excluded from the analysis because the clinical endpoint [53] or the presentation thereof [54] was not suitable for analysis. Eleven trials with 12 arms and 517 patients and an average length of treatment of 6 (1–12) weeks were analyzed. None of the trials included a follow-up [1, 12, 21, 22, 25, 35, 44, 47, 48, 57, 58]. Only one preparation (SAM) was the subject of more than one trial (3 trials, 121 patients) (Evidence Report, Tab. 104). The evidence was initially downgraded because so few trials were available. And since the quality of evidence was limited (limited methodological quality, limited external validity; Evidence Report, Tab. 105), it was further downgraded. The efficacy was limited. The SMDs (nutritional supplements versus controls) on pain, sleep, and fatigue at the completion of therapy were showed small effect sizes (Evidence Report, Tab. 106 and Fig. 34). Acceptance was moderate (dropout rate 12%) and did not differ significantly 4 | Der Schmerz 3 · 2012 from that of the placebo groups; Evidence Report, Fig. 34). The risks were high: gastrointestinal adverse effects were 10% more frequent with SAM and 5-HT than in the control group. The recommendation was downgraded a further level because of the high risks and low availability. Reiki Evidence-based recommendation Reiki should not be applied. EL 2b, negative recommendation, strong consensus Comment. A search of the literature identified 19 reports. One trial had no control group [19]. In one trial the 25 patients were treated for 8 weeks by either a reiki master or an actor, receiving either reiki (direct contact) or a “distance treatment”. None of the treatments had a significant effect on pain, fatigue, sleep, or quality of life [3]. In spite of the limited data available, a statement on this treatment is included here because of the negative results of the trial. Dance therapy Evidence-based recommendation Dance therapy should not be applied as monotherapy. EL 2b, negative recommendation, strong consensus Comment. A search of the literature identified 9 reports. The data of one trial listed in the NIH databank as completed and evaluated could not be found in the other databanks [6]. In a Swedish RCT with 36 patients, dance therapy (once a week for 6 months) did not reduce pain in the therapy group when compared with controls neither at the completion of the trial nor at follow-up assessment 6 months later [32]. Although few data are available, a statement about this therapy is included here because of the negative results of the trials. Neither positive nor negative recommendation possible Dietary intervention (vegetarian diet, elimination diet, therapeutic fasting) Evidence-based assessment Due to the limited available data, neither a positive nor a negative recommendation is possible. Strong consensus Comment. A search of the literature identified 27 reports. In one RTC, 37 patients were given a vegetarian diet, and 41 patients, amitriptyline (AMT; 10–100/day), depending on the severity of the patient’s sleep disorder, for a period of 6 weeks. Both treatments resulted in pain reduction. At the completion of therapy, AMT was more effective than the vegetarian diet in reducing pain [5]. In a controlled trial, a 3-month lowsalt uncooked vegetarian diet (18 patients) was superior to a normal diet in reducing pain and improving function [37]. In a controlled trial from the US, 40 patients received an exclusion diet (e.g., of wheat, nutritional supplements) based on immunological tests. They were compared with 11 patients who continued their normal diets. Patients of both groups participated in group discussions. At the end of the trial, the patients on exclusion diets reported a 50% reduction in pain, whereas the controls reported no changes [20]. Melatonin Evidence-based assessment Due to the limited data available, neither a positive nor a negative recommendation is possible. Strong consensus Comment. A search of the literature identified 34 reports. In a non-controlled Argentinean trial with 19 patients, 3 mg melatonin/day for 4 weeks improved sleep and decreased the tender-point score [14]. In a RTC, 24 patients received 5 mg melatonin/day, 24 patients 20 mg fluoxetine/ day, 27 patients 20 mg fluoxetine/day plus 3 mg melatonin/day, and 23 patients 20 mg fluoxetine/day plus 5 mg melatonin/day. A placebo control was not carried out. Pain was significantly reduced Tab. 1 Changes from the first edition of the guidelines in the degree of recommendation for complementary and alternative therapies Therapeutic procedure Mindfulness-based stress reduction as sole treatment Acupuncture Breathing therapy Elimination diet Foot reflexology massage therapy Homeopathy Meditative Movement Therapies Reiki Vegetarian diet/therapeutic fasting Recommendation 2008 No statement possible Recommendation 2012 Strongly negative Strongly negative Minority opinion: open Open Open Open Open Open Negative Minority vote: open Strongly positive Negative No statement possible Open No statement Open in all arms of the trial, but sleep was significantly improved only in the melatonin groups [33]. Melatonin is approved for the short-term treatment of primary insomnia in patients older than 55 years. Music therapy Evidence-based assessment Due to the limited data available, neither a positive nor a negative recommendation is possible. Strong consensus Comment. In a US RCT with 26 patients and passive musical therapy, musically fluctuating vibrations (60–300 Hz) were not superior to sinusoidal vibrations in reducing the intensity of pain [13]. In a German controlled trial, a program of active music therapy in a group of 12 patients with various pain syndromes including FMS patients was superior to control therapy in reducing pain and pain-related disability at the completion of therapy [45]. Discussion As pointed out in the first edition of the guidelines [40], complementary and alternative medicine (CAM) is widely used by patients with FMS (87–91%). However, these various therapies remain to be satisfactorily evaluated and their effectiveness established, since few good controlled trials on CAM therapies for fibromyalgia are available. Further research in this area is desirable and necessary. Not considered No statement possible No statement In the first edition of the guidelines [40], the recommendations were designated “open” for breathing therapy, elimination/vegetarian diets, and foot massage therapy. In this update, they again cannot be either positively or negatively recommended because of the absence of satisfactory trials. The open recommendation for homeopathy has been changed to a negative recommendation due to the results of a quantitative data synthesis. However, the relatively sparse data can be interpreted in different ways (see Minority opinion). The recommendation for acupuncture was changed from negative to open as a result of new trials and quantitative data synthesis (Tab. 1). As a rule, complementary procedures are applied in an interdisciplinary and integrative medical setting. Frequently they constitute a useful supplement within the framework of a multimodal therapeutic concept. One advantage of some complementary therapeutic procedures (e.g., qigong or tai chi) is that patients can apply the procedures themselves and are not dependent on a therapist. Especially needed are randomized clinical trials on the effectiveness of music and dance therapies, homeopathy, and dietary intervention. Many basic therapeutic approaches of complementary medicine, e.g., acupuncture, are thought to activate intrinsic physiological mechanisms. Frequently the exact mediators of potential therapeutic effects are still not understood. Thus, not only clinical trials to evaluate the complementary therapies are needed, but also trials in the realm of basic research. In addition, more information about how frequently FMS patients in Germany utilize complementary procedures and what motivates them to do so is needed. Conclusion with regard to practice FMS patients frequently utilize complementary and alternative medicine therapies. Complementary procedures as a rule are applied in an interdisciplinary and integrative medicine setting. They can be a useful supplement within the framework of a multimodal therapeutic concept. The use of meditative exercise therapies (tai chi, qigong, yoga) is strongly recommended. Acupuncture can be applied for a limited period of time. Dietary supplements and Reiki should not be utilized, nor should mindfulnessbased stress reduction or dance therapy be utilized as the sole treatments. Corresponding address Prof. Dr. J. Langhorst Innere Medizin V, Naturheilkunde und Integrative Medizin, Kliniken Essen-Mitte Am Deimelsberg 34a, 45276 Essen Germany J.Langhorst@kliniken-essen-mitte.de Conflict of interest. See Tab. 5 in “Methodological fundamentals used in developing the guideline” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Ali A, Njike VY, Northrup V et al (2009) Intravenous micronutrient therapy (Myers’ Cocktail) for fibromyalgia: a placebo-controlled pilot study. J Altern Complement Med 15:247–257 2. Assefi NP, Sherman KJ, Jacobsen C (2005) A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med 143:10–19 3. Assefi N, Bogart A, Goldberg J, Buchwald D (2008) Reiki for the treatment of fibromyalgia: a randomized controlled trial. J Altern Complement Med N 14:1115–1122 4. Astin JA, Berman BM, Bausell B et al (2003) The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J Rheumatol 30:2257–2262 5. Azad KAK, Alam MN, Haq SA et al (2000) Vegetarian diet in the treatment of fibromyalgia. Bangladesh Med Res Counc Bull 26:41–47 Der Schmerz 3 · 2012 | 5 Schwerpunkt 6. Baptista A (2012) Effectiveness of dance on patients with fibromyalgia. http://www.clinicaltrials. gov/ct2/show/NCT00961805?term=fibromyalgia +and+dance+therapy&rank=1. Accessed 25 May 2012 7. Bell IR, Lewis DA II, Brooks AJ et al (2004) Individual differences in response to randomly assigned active individualized homeopathic and placebo treatment in fibromyalgia: implications of a double-blinded optional crossover design. J Altern Complement Med 10:123–131 8. Bell IR, Lewis DA II, Brooks AJ et al (2004) Improved clinical status in fibromyalgia patients treated with individualized homeopathic remedies versus placebo. Rheumatology (Oxford) 43:577–582 9. Calandre EP, Rodriguez-Claro ML, Rico-Villademoros F et al (2009) Effects of pool-based exercise in fibromyalgia symptomatology and sleep quality: a prospective randomised comparison between stretching and Ai Chi. Clin Exp Rheumatol 27(6 Suppl 56):S21–28 10. Cao H, Liu J, Lewith GT (2010) Traditional Chinese Medicine for treatment of fibromyalgia: a systematic review of randomized controlled trials. J Altern Complement Med 16:397–409 11. Carson JW, Carson KM, Jones KD et al (2010) A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain 151:530–539 12. Caruso I, Sarzi Puttini P, Cazzola M, Azzolini V (1990) Double-blind study of 5-hydroxytryptophan versus placebo in the treatment of primary fibromyalgia syndrome. J Int Med Res 18:201–209 13. Chesky KS, Russell J, Lopez Y, Kondraske GV (1997) Fibromyalgia tender point pain: A double-blind, placebo-controlled pilot study of music vibration using the music vibration table(tm). J Musculoskeletal Pain 5:33–52 14. Citera G, Arias MA, Maldonado-Cocco JA et al (2000) The effect of melatonin in patients with fibromyalgia: a pilot study. Clin Rheumatol 19:9–13 15. Colquhoun D (1990) Re-analysis of clinical trial of homoeopathic treatment in fibrositis. Lancet 336(8712):441–442 16. Capili B, Anastasi JK, Geiger JN (2010) Adverse event reporting in acupuncture clinical trials focusing on pain. Clin J Pain 26:43–48 17. Silva GD da, Lorenzi-Filho G, Lage LV (2007) Effects of yoga and the addition of Tui Na in patients with fibromyalgia. J Altern Complement Med 13:1107– 1113 18. Deluze C, Bosia L, Zirbs A et al (1992) Electroacupuncture in fibromyalgia: results of a controlled trial. BMJ 305:1249–1252 19. Denison B (2004) Touch the pain away: new research on therapeutic touch and persons with fibromyalgia syndrome. Holist Nurs Pract 18:142– 151 20. Deuster PA, Jaffe RM (1998) A novel treatment for fibromyalgia improves clinical outcomes in a community-based study. J Musculoskeletal Pain 6:133– 149 21. Di Benedetto P, Iona LG, Zidarich V (1993) Clinical evlautaion of S-Adenosyl-Methionine versus transcutaneous electrical nerve stimulation in primary fibromyalgia. Curr Ther Res 53:222–230 22. Edwards AM, Blackburn L, Christie S et al (2000) Food supplements in the treatment of primary fibromyalgia: A double-blind, crossover trial of anthocyanidins and placebo. J Nutr Env Med 10:189– 199 6 | Der Schmerz 3 · 2012 23. Fisher P (1986) An experimental double-blind clinical trial method in homeopathy. Use of a limited range of remedies to treat fibrositis. Br Homeopath J 75:142 24. Fisher P, Greenwood A, Huskisson EC et al (1989) Effect of homeopathic treatment on fibrositis (primary fibromyalgia). BMJ 299:365–366 25. Fontani G, Suman AL, Migliorini S et al (2010) Administration of omega-3 fatty acids reduces positive tender point count in chronic musculoskeletal pain patients. J Altern Complement Med 735. DOI 10.2202/1553-3840.1366 26. Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U (2007) Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom 76:226–233 27. Guo X, Jia J (2005) Comparison of therapeutic effects on fibromyalgia syndrome between dermalneurological electric stimulation and electric acupuncture. Chin J Rehabil 9:171–173 (Target variables not suitable for analysis) 28. Haak T, Scott B (2008) The effect of Qigong on fibromyalgia (FMS): a controlled randomized study. Disabil Rehabil 30:625–633 29. Harris RE, Tian XT, Williams DA et al (2005) Treatment of fibromyalgia with formula acupuncture: Investigation of needle placement, needle stimulation and treatment frequency. J Altern Complement Med 11:663–671 30. Harris RE, Zubieta JK, Scott DJ et al (2009) Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs). Neuroimage 47:1077–1088 31. Holmer ML (2004) The effects of yoga on symptoms and psychosocial adjustment in fibromyalgia syndrome patients. Abstracts International: Section B: The Sciences and Engineering 65(5-B)2630. (Dissertation). Only abstract available 32. Horwitz EB, Kowalski J, Theorell T, Anderberg UM (2006) Dance/movement therapy in fibromyalgia patients: Changes in self-figure drawings and their relation to verbal self-rating Scales. Arts Psychother 33:11–25 33. Hussain SA, Al-Khalifa II, Jasim NA, Gorial FI (2010) Adjuvant use of melatonin for treatment of fibromyalgia. J Pineal Res. 2010 Dec 16. DOI 10.1111/j.1600-079X.2010.00836.x 34. Itoh K, Kitakoji H (2010) Effects of acupuncture to treat fibromyalgia: a preliminary randomised controlled trial. Chin Med 5:11 35. Jacobsen S, Danneskiold-Samsoe B, Andersen RB (1991) Oral S-adenosylmethionine in primary fibromyalgia. Double-blind clinical evaluation. Scand J Rheumatol 20:294–302 36. Jang ZY, Li CD, Qiu L et al (2010) Combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome: a multi-central randomized controlled trial. Zhongguo Zhen Jiu 30:265–269 (Combination of acupuncture with other methods) 37. Kaartinen K, Lammi K, Hypen M et al (2000) Vegan diet alleviates fibromyalgia symptoms. Scand J Rheumatol 29:308–313 38. Kendall SA, Brolin-Magnusson K, Sören B et al (2000) A pilot study of body awareness programs in the treatment of fibromyalgia syndrome. Arthritis Care Res 13(5):304–311 39. Kendall SA, Ekselius L, Gerdle B et al (2001) Feldenkrais intervention in fibromyalgia patients: a pilot study. J Musculoskelet Pain 9:25–35 40. Langhorst J, Häuser W, Irnich D et al (2008) Komplementäre und alternative Therapien beim Fibromyalgiesyndrom. Schmerz 22:324–333 41. Lautenschläger J, Schnorrenberger CC, Müller W (1989) Acupuncture in generalized tendomyopathia (fibromyalgia syndrome). Dtsch Ztschr Akup 32:122–128 (in German) 42. Mannerkorpi K, Arndorw M (2004) Efficacy and feasibility of a combination of body awareness therapy and qigong in patients with fibromyalgia: a pilot study. J Rehabil Med 36:279–281 43. Martin DP, Sletten CD, Williams BA, Berger H (2006) Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Mayo Clin Proc 81:749–757 44. Merchant RE, Andre CA, Wise CM (2001) Nutritional supplementation with Chlorella pyrenoidosa for fibromyalgia syndrome: A double-blind, placebocontrolled, crossover study. J Musculoskelet Pain 9:37–54 45. Mueller-Busch HC, Hoffmann P (1997) Active music therapy for chronic pain: a prospective study (Aktive Musiktherapie bei chronischen Schmerzen. Eine prospektive Untersuchung). Schmerz 11:91– 100 46. Relton C, Smith C, Raw J et al (2009) Healthcare provided by a homeopath as an adjunct to usual care for Fibromyalgia (FMS): results of a pilot Randomised Controlled Trial. Homeopathy 98:77–82 47. Rossini M, Di Munno O, Valentini G et al (2007) Double-blind, multicenter trial comparino acetyl l-carnitine with placebo in the treatment of fibromyalgia patients. Clin Exp Rheumatol 25:182–188 48. Russell IJ, Michalek JE, Flechas JD, Abraham GE (1995) Treatment of fibromyalgia syndrome with Super Malicregistered trade mark: A randomized, double blind, placebo controlled, crossover pilot study. J Rheumatol 22:953–958 49. Sandberg M, Lundeberg T, Gerdle B (1999) Manual acupuncture in fibromyalgia: a long-term pilot study. J Musculoskeletal Pain 7:39–51 50. Schmidt S, Grossman P, Schwarzer B et al (2011) Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. Pain 152:361–9 51. Sephton SE, Salmon P, Weissbecker I et al (2007) Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis Rheum 57:77– 85 52. Stephens S, Feldman BM, Bradley N et al (2008) Feasibility and effectiveness of an aerobic exercise program in children with fibromyalgia: results of a randomized controlled pilot trial. Arthritis Rheum 59:1399–406 53. Sprott H (1998) Efficacy of acupuncture in patients with fibromyalgia. Clin Bull Myofascial Ther 3:37– 43 54. Targino RA, Imamura M, Kaziyama HH et al (2008) A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med 40:582–588 (Combination of acupuncture with amitriptyline and multimodal therapy) 55. Tavoni A, Jeracitano G, Cirigliano G (1998) Evaluation of S-adenosylmethionine in secondary fibromyalgia: a double-blind study. Clin Exp Rheumatol 16:106–107 56. Tavoni A, Vitali C, Bombardieri S, Pasero G (1987) Evaluation of S-adenosylmethionine in primary fibromyalgia. A double-blind crossover study. Am J Med 83:107–110 57. Volkmann H, Norregaard J, Jacobsen S et al (1997) Double-blind, placebo-controlled cross-over study of intravenous S-adenosyl-L-methionine in patients with fibromyalgia. Scand J Rheumatol 26:206–211 58. Wahner-Roedler DL, Thompson JM, Luedtke CA et al (2008) Dietary soy supplement on fibromyalgia symptoms: a randomized, double-blind, placebocontrolled, early phase trial. Evid Based Complement Alternat Med 14(Suppl 1):25 59. Wang C, Schmid CH, Rones R et al (2010) A randomized trial of tai chi for fibromyalgia. N Engl J Med 363:743–754 Der Schmerz 3 · 2012 | 7 Schwerpunkt English Version of "Definition, Diagnostik und Therapie von chronischen Schmerzen in mehreren Körperregionen und des sogenannten Fibromyalgiesyndroms bei Kindern und Jugendlichen. Systematische Literaturübersicht und Leitlinie". DOI 10.1007/s00482-012-1168-y © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag all rights reserved 2012 B. Zernikow1, 2 · K. Gerhold3 · G. Bürk4 · W. Häuser5 · C.H. Hinze6 · T. Hospach7 · A. Illhardt8 · K. Mönkemöller9 · M. Richter10 · E. Schnöbel-Müller6 · R. Häfner6 1 Deutsches Kinderschmerzzentrum, Vestische Kinder- und Jugendklinik, Universität Witten/Herdecke, Datteln 2 Vodafone Stiftungslehrstuhl für Kinderschmerztherapie und Pädiatrische Palliativmedizin, Universität Witten/Herdecke, Witten 3 Universitätskinderklinik, Charité – Universitätsmedizin Berlin 4 MVZ Kinder und Jugendliche Herne 5 Innere Medizin 1, Klinikum Saarbrücken, Klinikum Saarbrücken gGmbH, Saarbrücken 6 Deutsches Zentrum für Kinder- und Jugendrheumatologie, Garmisch-Partenkirchen 7 Olgahospital - Kinderklinik Stuttgart 8 St. Josef-Stift Sendenhorst 9 Kinderkrankenhaus der Stadt Köln 10 Kinderklinik, Universitätsklinik Dresden Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents Systematic literature review and guideline Epidemiologic studies reveal a high prevalence (between 25% and 46%) of chronic pain in children and adolescents, an increased prevalence with age and a higher prevalence in girls [14, 32, 58, 68]. The most common locations of pain—in order of descending frequency—are head, abdomen and musculoskeletal system; some of the children and adolescents report pain in several regions [14, 32, 58, 67]. About 3% of children and adolescents develop severe, disabling chronic pain with negative effects on school attendance, recreational activities, contact with peers and family and emotional distress, such as anxiety and depression [32, 55]. A subset of these children and adolescents suffer from additional symptoms, for example disordered sleep [45, 57] or fatigue [19]. In children and adolescents who suffer from generalized pain of the musculoskeletal system, additional symptoms and muscle tenderness, the diagnosis juvenile fibromyalgia syndrome (JFMS) is used. The definitions of JFMS, however, have substantial operationalizational problems. The authors of the update of these guide- lines therefore chose to use the term “socalled JFMS”. For the planned update of the guidelines, the following research questions were addressed by use of a comprehensive literature review: 1.What are the core symptoms of the so-called JFMS? 2.What differences/overlap exist between so-called JFMS and somatoform pain disorder? 3.According to which criteria should the so-called JFMS be diagnosed? 4.Which diagnostic examinations are required to rule out alternative diagnoses? 5.When is a psychological evaluation reasonable? 6.Are there different courses or degrees of severity of the so-called JFMS? 7.Which information about symptoms, therapeutic goals and treatment opportunities should be made available at the time of diagnosis? 8.Is patient education useful? 9.Which subspecialty should coordinate the care of the so-called JFMS? 10.Is a graded treatment approach useful? 11.Which physical, physical therapeutic, psychotherapeutic, pharmacologic and complementary approaches are useful in the so-called JFMS? 12.Which physical, physical therapeutic, psychotherapeutic, pharmacologic and complementary approaches should be advised against in the socalled JFMS? 13.When is an inpatient multimodal treatment indicated? Materials and methods The methods of literature search and preparation of recommendations are presented in the article “Methodological fundamentals used in developing the guidelines”. Results The literature search yielded 265 hits. Due to the low number of high quality studies, there was no gradation of the level of eviDer Schmerz 3 · 2012 | 1 Schwerpunkt dence according to the quantity or quality of the evidence. Definition and classification Clinical consensus For children and adolescents there are currently no standardized and validated criteria for defining chronic pain in multiple body regions leading to clinically significant impairment in everyday life and that does not occur within a defined somatic disease. Strong consensus Comment. In childhood and adolescence, pain, regardless of its location, is defined as chronic if it lasts for at least 3 months or is recurrent over this time period [33, 47, 54]. Persistent or recurrent pain may fluctuate greatly in intensity, quality, frequency, predictability and may occur either in single or multiple body regions. The focus on the temporal dimension of chronic pain has recently been criticized. Studies indicate that children, who suffer from shorter-lasting pain, are often significantly impaired in their daily lives and require treatment [28, 33]. The aspect of pain-related impairment has only recently been explicitly considered in the context of epidemiological and clinical studies [29, 30, 54]. Rief et al. [64] included the issue of impairment as a central criterion within a new diagnostic category of “chronic pain disorder with somatic and psychological factors” (ICD-10 F45.41). Studies on the incidence of this diagnosis in childhood and adolescence are lacking. According to Sherry [46, 73], in the case of chronic pain in children and adolescents with mostly musculoskeletal pain, “diffuse” and “idiopathic localized” musculoskeletal pain can be defined. Another commonly used term is “chronic widespread (musculoskeletal) pain (CWP)” [15, 50]. For further consideration, it is important to note that not all CWP goes along with pain-related impairment in everyday life, distress or a subjective sense of illness. However, this is described for the so-called juvenile fibromyalgia syndrome (JFMS). Traditionally, the so-called JFMS is defined according to the Yunus criteria [83]: 2 | Der Schmerz 3 · 2012 a)generalized musculoskeletal aching at ≥3 sites, b)duration for at least 3 months, c)normal laboratory test results, d)at least 5 of 11 tender points, e)at least 3 of the following 10 features: 1.chronic anxiety or tension, 2.fatigue, 3.poor sleep, 4.chronic headaches, 5.irritable bowel syndrome, 6.subjective soft tissue swelling, 7.numbness, 8.pain modulation of physical activity, 9.pain modulation by weather factors, 10.pain modulation by anxiety and/ or stress. Other publications on JFMS used the definition of the American College of Rheumatology (ACR) in 1990 for adults. The specificity and sensitivity of the Yunus criteria and the ACR criteria have rarely been investigated in children and adolescents. In a study by Reid [61], only 75% of pediatric patients fulfilled both the Yunus as well as the 1990 ACR criteria. The pain is typically highly variable; therefore, the Yunus criteria are met only irregularly. Both the Yunus and the 1990 ACR criteria have substantial problems in their operationalization: 1.The so-called tender points are problematic for the following reasons: a)From studies on quantitative sensory testing (QST) in children and adolescents it is known that the pressure pain threshold when using a pressure gauge device (FDN 100, Wagner Instruments, USA) depends on the age and sex of the child and the location tested [3]. Fifty percent of healthy children report pain at a pressure ranging from 163–1,039 kPa (100 kPa=1 kg/cm2), whereas the upper and lower 95% confidence interval (95% CI) vary according to age, sex and location of pressure application between 82–1,890 kPa. The testing of tender points using thumb pressure or technical devices with a pressure independent of the age, sex and loca- tion of pressure application may not lead to valid results, since the pressure–pain threshold in healthy children is influenced by these factors. Tenderness thresholds from about 3 kg/cm2 (300 kPa/cm2) or 3 kg/1.5 cm2 (depending on the study and thumb size) or even 5 kg/1.5 cm2 were considered as pathologic [7]. Depending on age, gender and location of pressure application, many healthy children report pain at these pressures. b)In the published studies, the socalled tender points were generally not standardized, often only examined by thumb pressure and not examined in a double-blind fashion. However, for the thumb pressure not only the compressive force, but also the support surface is critical. c)When two pediatric rheumatologists examined tender points in the same child, their agreement was around 44%, not better than chance [9]. d)Some studies show that children with juvenile idiopathic arthritis (JIA) have identical tender point pain thresholds as children with so-called JFMS [62]. e)If tender points are positive, socalled control points are often positive as well [72]. Häfner et al. [21] found that tender points were variable and fluctuated. 2.The so-called minor symptoms of the Yunus criteria have not been defined. Headaches should be classified according to the International Headache Society (IHS) criteria, e.g., chronic tension headache, episodic tension headache, migraine, medication-induced headache. The same is true for the diagnosis irritable bowel syndrome, for which the Rome criteria should be required [20]. 3.For psychological symptoms such as anxiety and depression and functional impairment due to chronic pain, a standardized survey with established instruments should be implemented (see below). Abstract · Zusammenfassung Due to these limitations of operationalization, the term JFMS has been rejected by leading rheumatologists and researchers since it is not scientifically established or clinically helpful [73]. The guideline committee agrees to this opinion. Based on the work by Rief et al. the authors of the present guidelines suggest, that, in the future, the diagnosis “chronic pain disorder in several body regions with somatic and psychological factors” should be used for children with chronic widespread pain (CWP), who also suffer from other symptoms such as headache or abdominal pain, non-restorative sleep, muscle tenderness, fatigue, irritable bowel syndrome, anxiety, depression and a strong pain-related impairment in everyday life. In adults, Rief et al. [64] suggested to optimize the classification of chronic pain in ICD-10 (section F) according to the biopsychosocial model. Thus far, chronic pain has been classified as “somatoform pain disorder” (F 45.4). For this diagnosis, psychologic factors were considered to trigger the pain. Since this relationship could not always be confirmed in studies, a new proposal for the diagnosis “chronic pain disorder with somatic and psychological factors” (F45.41) was created [64]. The clinical picture is dominated by pain lasting for at least 6 months in one or more anatomical regions. This pain is assumed to have been triggered either by psychological processes or a physical disorder. Psychological factors are considered to play an important role in the degree of severity, exacerbation or maintenance of pain, but to a minor degree a causative role. The pain causes clinically significant distress and impairment in social, occupational or other important areas of functioning. The pain is not voluntarily produced or pretended (as in factitious disorder or simulation). For children and adolescents, the pain disorder should last for at least 3 months (for reasoning, see above). In this guideline we will use the term of the “so-called JFMS”, because the cited studies describe JFMS patients even though the diagnosis JFMS cannot be operationalized (see above). The authors of these guidelines agree that the diagnosis JFMS is neither scientifically established, Schmerz 2012 · DOI 10.1007/s00482-012-1168-y © Deutsche Schmerzgesellschaft e.V. Published by Springer-Verlag - all rights reserved 2012 B. Zernikow · K. Gerhold · G. Bürk · W. Häuser · C.H. Hinze · T. Hospach · A. Illhardt · K. Mönkemöller · M. Richter · E. Schnöbel-Müller · R. Häfner Definition, diagnosis and therapy of chronic widespread pain and so-called fibromyalgia syndrome in children and adolescents. Systematic literature review and guideline Abstract Background. The scheduled update to the German S3 guidelines on fibromyalgia syndrome (FMS) by the Association of the Scientific Medical Societies (“Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften”, AWMF; registration number 041/004) was planned starting in March 2011. Materials and methods. The development of the guidelines was coordinated by the German Interdisciplinary Association for Pain Therapy (“Deutsche Interdisziplinären Vereinigung für Schmerztherapie”, DIVS), 9 scientific medical societies and 2 patient self-help organizations. Eight working groups with a total of 50 members were evenly balanced in terms of gender, medical field, potential conflicts of interest and hierarchical position in the medical and scientific fields.Literature searches were performed using the Medline, PsycInfo, Scopus and Cochrane Library databases (until December 2010). The grading of the strength of the evidence followed the scheme of the Oxford Centre for EvidenceBased Medicine. The formulation and grading of recommendations was accomplished using a multi-step, formal consensus process. The guidelines were reviewed by the boards of the participating scientific medical societies. Results and conclusion. The diagnosis FMS in children and adolescents is not established. In so-called juvenile FMS (JFMS), multidimensional diagnostics with validated measures should be performed. Multimodal therapy is warranted. In the case of severe pain-related disability, therapy should be primarily performed on an inpatient basis.The English full-text version of this article is available at SpringerLink (under “Supplemental”). Keywords Chronic pain · Fibromyalgia syndrome · Review, systematic · Guideline · Children and adolescents Definition, Diagnostik und Therapie von chronischen Schmerzen in mehreren Körperregionen und des sogenannten Fibromyalgiesyndroms bei Kindern und Jugendlichen. Systematische Literaturübersicht und Leitlinie Zusammenfassung Hintergrund. Die planmäßige Aktualisierung der S3-Leitlinie zum Fibromyalgiesyndrom (FMS; AWMF-Registernummer 041/004) wurde ab März 2011 vorgenommen. Material und Methoden. Die Leitlinie wurde unter Koordination der Deutschen Interdisziplinären Vereinigung für Schmerztherapie (DIVS) von 9 wissenschaftlichen Fachgesellschaften und 2 Patientenselbsthilfeorganisationen entwickelt. Acht Arbeitsgruppen mit insgesamt 50 Mitgliedern wurden ausgewogen in Bezug auf Geschlecht, medizinischen Versorgungsbereich, potenzielle Interessenkonflikte und hierarchische Position im medizinischen bzw. wissenschaftlichen System besetzt.Die Literaturrecherche erfolgte über die Datenbanken Medline, PsycInfo, Scopus und Cochrane Library (bis Dezember 2010). Die Graduierung der Evidenzstärke erfolgte nach dem Schema des Oxford Center for Evidence Based Medicine. Die Formulierung und Graduierung der Empfehlungen erfolgte in einem mehrstufigen, formalisierten Konsensusverfahren. Die Leitlinie wurde von den Vorständen der beteiligten Fachgesellschaften begutachtet. Ergebnisse und Schlussfolgerung. Die Diagnose eines juvenilen FMS (JFMS) wurde als wissenschaftlich nicht etabliert eingestuft. Beim sog. JFMS wird eine multidimensionale Diagnostik mit validierten Instrumenten gefordert. Die Therapie sollte multimodal erfolgen, bei starker schmerzbedingter Beeinträchtigung auch primär stationär. Schlüsselwörter Chronische Schmerzen · Fibromyalgiesyndrom · Systematische Übersicht · Leitlinie · Kinder und Jugendliche Der Schmerz 3 · 2012 | 3 Schwerpunkt nor helpful. Therefore, they propose to use the term “chronic pain disorder in several body regions with somatic and psychological factors” instead. Clinical diagnosis Clinical consensus In children and adolescents with chronic pain in multiple body regions (CWP) a multidimensional diagnosis of pain and other physical and psychological symptoms is recommended. Validated tools and methods should be used. Strong consensus Comment. As no pathognomonic individual diagnostic findings for so-called JFMS are available, the diagnosis is based on the presence or absence of a characteristic constellation of symptoms and signs after exclusion of all other diseases that may also have such a constellation of symptoms and signs. Therefore, the differential diagnosis and exclusion of other diagnoses is of particular importance. The differential diagnosis itself depends on the clinical picture. Various organic diseases have to be considered: (systemic) inflammatory conditions such as juvenile idiopathic arthritis, malignant conditions such as leukemias [8, 77] and endocrine– metabolic diseases [42, 49]. Psychological problems/disorders should be considered since they are even more common, e.g., depression (subtypes according to DSMIV, see below), anxiety disorders (subtypes according to DSM-IV, see below), posttraumatic stress disorders (PTSD) and dissociative disorders with or without selfinjurious behavior. There is also the possibility of mental illness of parents, as seen in Munchhausen by proxy syndrome. In a study by Degotardi et al. [11] 2 of 77 children, all of whom met the Yunus criteria and all of whom were diagnosed by pediatric rheumatologists as JFMS, were eventually diagnosed with severe psychiatric disorders (“schizoaffective disorder” and “depression with suicidal ideation”) during further psychological evaluations. In the course of the study an additional 3% of the enrolled children had a “need for psychiatric referral.” KashikarZuck et al. studied 102 adolescents with the diagnosis of so-called JFMS regard- 4 | Der Schmerz 3 · 2012 ing psychiatric disorders using standardized tests and an extensive psychological exploration: 19% suffered from depression according to DMS-IV criteria [major depression (n=7), dysthymic disorder (n=8), depressive disorder not otherwise specified (NOS) (n=5)], 55% an anxiety disorder [panic disorder (n=6), agoraphobia (n=4), specific phobia (n=0), social phobia (n=11), obsessive-compulsive disorder (n=3), posttraumatic stress disorder (n=5), generalized anxiety disorder (n=17), or separation anxiety disorder (n=3)] and 24% suffered from attention deficit hyperactivity disorder (ADHD) [37, 38]. Therefore, the clinical assessment should include a profound medical and psychological examination, preferably by use of validated tools such as the German Paediatric Pain Questionnaire (“Deutscher Schmerzfragebogen für Kinder und Jugendliche”, DSF-KJ) [71]. Specifically, the following examinations should be conducted: Fbasic laboratory diagnostic, e.g., erythrocyte sedimentation rate, complete blood count with differential count, C-reactive protein, creatine kinase. Further diagnostic studies (e.g., antinuclear antibodies, rheumatoid factor, imaging, electroencephalography, electrocardiography, genetic studies, biopsy) are indicated if there is a clinical suspicion for an alternative cause of the pain, and Fpsychological standard diagnostics such as the “Depressionsinventar für Kinder- und Jugendliche (DIKJ)” (depression inventory for children and adolescents), “Angstfragebogen für Schüler (AFS)” (fear questionnaire for students). If applicable, polysomnography Epidemiology Evidence-based observation The prevalence of CWP is strongly agedependent and ranges between 1 and 15% in children and adolescents. Diffuse musculoskeletal pain in combination with other physical or psychological symptoms such as tension-type headaches, fatigue, sleep disturbance and emotional distress is present in <1% of children and adolescents between the ages of 8–15 years in international studies. There is a female predominance. Strong consensus Comment. When reviewing epidemiological studies, distinction must be made with regard to the sample studied—specifically, between studies that examined only the presence of CWP [15, 50] and studies that studied children who also suffered from other symptoms indicative of the diagnosis of so-called JFMS. Epidemiological studies in school children focused on children between 10 and 12 years and reported prevalences of CWP of 1% [50], 7.5% [52] and 9.9% [51]. In a follow-up study by Mikkelson et al. [50], adolescents between the ages of 14 and 16 years had a prevalence of CWP of 15%. In a German representative population sample, 302 adolescents were in the age group between 14 and24 years; none of them fulfilled the FMS criteria according to the survey criteria [22]. Since the diagnosis of adult FMS by means of tender points was abandoned in the latest ACR criteria [81], epidemiological studies of the prevalence of so-called JFMS need to be re-evaluated. Of the 7 children who were classified as having so-called JFMS (prevalence approximately 1% among school children 9–15 years) in the study by Clark et al. in 1998 [9], there was only one child who fulfilled all examined additional criteria (sleep disturbances, morning stiffness, fatigue, sadness). Three children fulfilled only one criterion each; neither the severity of symptoms nor the impairment of the children by the symptoms was reported. Other studies that found a significantly higher prevalence of so-called JFMS of 6.2% for 9- to 15-year-old school children based their diagnosis mainly on muscle tenderness [7], which, due to the methodological difficulties described above, can be criticized. Disease course Evidence-based observation In most patients with CWP, or so-called JFMS, the disease course is variable with alternating episodes of increased, decreased or absent symptoms. Evidence level 2b, strong consensus Comment. In a study on the course of CWP in childhood and adolescence, only 10% of children who had CWP at baseline complained of persistent symptoms after 1 and 4 years [50]. The evaluation of studies on the course of the so-called JFMS is complicated by the fact that the diagnosis itself is not valid, due to the methodological problems described in detail above. Moreover, in most studies, the study population was not assessed with standardized instruments. Essentially, children and adolescents with a pain disorder diagnosed in a non-standard fashion were examined in a non-standard fashion, and described by the authors as having so-called JFMS. In clinical studies, the persistence of long-term symptoms is described in a subset of patients. Malleson et al. [46] conducted a retrospective survey based on medical records. Twenty-eight of 35 patients diagnosed with JFMS had more than one appointment in the rheumatology clinic. After a variable observation period between 1 and 48 months, 17 of 28 patients with so-called JFMS had persistent symptoms after an average of 27 months [46]. In a retrospective study, Siegel et al. [74] assessed 44 patients over 6 years with so-called JFMS. Subsequent phone interviews, on average 2.6 years (range 0.1–7.6 years) after diagnosis, demonstrated an increase in the number of reported symptoms. On a visual analog scale (VAS) from 1–10 (1=complete disability; 10=no disability), the patients assessed their current impairment as being less pronounced than in the previous year (previous year 5.1±3.1 vs. currently 6.9±1.6). The patients received a standard outpatient treatment (tricyclic antidepressants, non-opioid analgesics, exercise program) [74]. The study results are promising; however, there is a core critical point: the authors changed their study methods between the time of outpatient treatment (unstructured survey) and the telephone interview (structured survey). In addition, no standardized instrument to assess pain-related disability was used, e.g., the Functional Disability Inventory [36, 79]. Gedalia et al. [18] conducted a retrospective study over a period of 4 years. Fifty of 59 patients with so-called JFMS were seen more than once in the outpatient clinic. At an average follow-up of 18 months (range 3–65 months), 60% of the children improved, 36% experienced no change and 4% experienced a worsening of pain symptoms. The therapy consisted of a combination of pharmacological and nonpharmacological interventions; at the time of follow-up 74% of children were taking medications [18]. Of 48 U.S. American children and adolescents diagnosed with JFMS, after an average of 3.7 years, 62.5% suffered from CWP, and 60.4% fulfilled criteria for socalled JFMS [40]. Population-based studies in children and adolescents reveal a more favorable disease course: In a population of Israeli school age children, Buskila et al. [6] diagnosed so-called JFMS in 21 of 337 patients (6.2%) according to the ACR criteria; after 30 months of follow-up, the ACR criteria were met by only 4 of 21 children. In the Finnish study by Mikkelsson et al. [52], only 4 of 16 school age children with so-called FMS fulfilled the ACR criteria of so-called JFMS after a follow-up of 1 year. Exacerbating factors for CWP include the following: daily hassles, pain-related catastrophizing, lack of self-efficacy and lack of positive family support [43] Etiology Somatic complaints (headache and abdominal pain), behavioral problems and increased physical activity Evidence-based observation Somatic complaints (headache and abdominal pain), behavioral problems and increased physical activity frequently occur prior to CWP. There are no studies on the relationship of these factors to socalled JFMS. Evidence level 2b, strong consensus Psychosocial problems Evidence-based observation Studies regarding psychosocial problems in patients with so-called JFMS demonstrate controversial findings. Evidence level 3b, strong consensus Comment. A biopsychosocial perspective is necessary to understand the origin and maintenance of chronic pain [78]. Chronic pain in children is the result of a dynamic process of biological factors (e.g., an underlying somatic disease), physical components (e.g., a lowered threshold of pain), psychological factors (e.g., painrelated fears, dealing with pain and pain coping) and sociocultural conditions (e.g., pain-related parenting, social attitudes, gender roles, social interactions in dealing with pain). All of these factors interact with each other. Risk factors for the development of a so-called JFMS or chronic pain disorder of the musculoskeletal system have not been investigated to date. In an English population-based prospective follow-up study over a study period of 12 months, 1,440 school children were examined for risk factors for the development of CWP. These risk factors included physical symptoms such as headache on more than 7 of 30 days [relative risk (RR) 2.50, 95% CI 1.16–5.39], abdominal pain at 1–7, but not less than one or more than 7 days per month (RR 1.8, 95% CI 1.1–2.9), as well as increased physical activity of more than 6 h per week (RR 2.03, 95% CI 1.05–3.94). Prosocial behavior was identified as a protective factor for CWP (RR 0.50; 95% CI 0.28–0.90) [34]. In a case control study, no significant differences in psychological distress were observed between patients with a so-called JFMS and JIA [60]. In contrast, Conte et al. [10] reported a higher incidence of anxiety and depression in patients with so-called JFMS compared to healthy subjects and patients with JIA. In a case control study of a private psychiatric hospital, 32 adolescents who met the criteria of so-called JFMS reported more physical and emotional problems than the control group of 30 adolescents with other mental disorders [44]. A case–control study of 55 patients with so-called JFMS and 55 healthy controls showed that adolescent patients with so-called JFMS described themselves as more withdrawn and less popular and, thus, were more likely than their peers to be socially isolated [39]. This was not the case for patients with JIA. Der Schmerz 3 · 2012 | 5 Schwerpunkt Family history Pathophysiology Evidence-based observation Evidence-based observation So-called JFMS and adult FMS occur together in families. Evidence level 2b, strong consensus Due to the lack of studies, no comment can be made on the pathophysiology of so-called JFMS. Strong consensus Comment. The increased joined occurrence of adult FMS and so-called JFMS in first-degree relatives has consistently been reported in several studies [1, 6, 53, 65, 76]. In an Israeli study of 37 families with FMS (at least 2 relatives), 74% of siblings and 53% of parents were diagnosed with FMS according to the ACR criteria [5]. The studies on familial clustering, however, do not provide evidence that the increased incidence of adult FMS and so-called JFMS is genetically determined. The results of an American study of over 40 families with FMS (at least 2 first-degree relatives) were consistent with a genetic linkage to the HLA region [82]. A Finnish longitudinal cohort study of 11-year-old twins (583 monozygotic pairs, 588 same-sex dizygotic and 618 different-sex dizygotic pairs) demonstrated a CWP prevalence of 9.9% and mostly discordance; a genetic basis could not be shown [51]. Non-genetic, psychological factors for the increased incidence of chronic pain in children of adult chronic pain patients are much more likely to play a role than genetic models (role modeling etc.) [2, 56]. Coordination of care Parental factors Evidence-based observation Parents of patients with so-called JFMS frequently show increased anxiety, a history of chronic pain, depressive symptoms and chronic diseases. Evidence level 3b, strong consensus Comment. Parents of children and adolescents with so-called JFMS: Fmore frequently report chronic pain [35, 70], Ftend to show increased anxiety [10], Fmore frequently demonstrate depressive symptoms [10, 35], and Fsuffer from more somatic symptoms [10]. 6 | Der Schmerz 3 · 2012 Evidence-based recommendation Children and adolescents with CWP should be presented to a clinical specialist familiar with chronic pain in childhood on an outpatient basis. In the case of long school absences, severe limitations in activities of daily living, physical inactivity or increasing social isolation, inpatient treatment in a facility that offers a special treatment program for children and adolescents with chronic pain, should be recommended. Evidence level 4, strong consensus Comment. In a study by Hechler et al. [28] on the stratification of therapy in a sample of children and adolescents with chronic pain (headaches, abdominal pain or musculoskeletal pain), the criteria for stratification of therapy were studied. The intensity of initial therapy (outpatient therapy, outpatient group therapy, inpatient therapy) turned out to be correct for the majority of children. An intensification of therapy was rarely needed. In this study, children were assigned to multimodal inpatient treatment based on the following criteria: chronic pain for at least 3 months, no successful therapy in the previous setting, high pain-related impairment [Pain Disability Index (PDI) >36] and the presence of 3 of the following 4 criteria: Fpain duration >6 months, Faverage pain intensity in the last 7 days ≥5 [visual analog scale (NRS) 0–10], Fpain peaks ≥8 (NRS 0–10) at least twice a week, and Fat least 5 school days of absence during the last 20 school days. Children and adolescents with so-called JFMS who do not (yet) express this level of severe impairment, should initially be treated as outpatients. Local or part-time inpatient multimodal treatment is rarely offered for children and adolescents with chronic pain of the musculoskeletal system in Germany. Therefore, for the less severely affected children, an individual multimodal program should be planned based on the existing facilities in Germany (e.g., outpatient psychotherapy, physical therapy, regular visits to the pediatrician). There are only a few centers offering multimodal inpatient therapy; thus, treatment often takes place remote from the hometown. Even though only studies with a level of evidence grade 4 are available, the authors agreed in a unanimous consensus to recommend this modality with a strength level B given the following criteria are met: low risk, high acceptance rate among patients (adherence to therapy between 95% [13] and 98% [16]) and ethical necessity, since normal childhood development is endangered. General principles of treatment Therapeutic goals Evidence-based recommendation Goals of treatment should be pain relief, restoration of functioning, reduction of school absenteeism, dissolving social isolation, strengthening self-awareness, mobilizing domestic resources and the development of strategies for coping with pain. The inclusion of the family, the training of strategies in everyday life and the treatment of mental co-morbidities are also important. Evidence level 2c, strong consensus Comment. The general principles of therapy have been formulated comprehensively in prospective outcome trials [12, 13, 16, 23, 24, 25, 26]. Patient education Clinical consensus Patient and parent education and selfhelp groups for children, adolescents and parents may be offered. Strong consensus Psychotherapy Clinical consensus Scientifically established methods of psychotherapy should be used for children and adolescents with so-called JFMS part of a multimodal pain therapy. Strong consensus Comment. A U.S. randomized study in cross-over compared active coping with pain to self-monitoring in 30 adolescents; at the end of the study both groups demonstrated a reduction of functional limitations and depression [41]. A significant reduction of pain could not be demonstrated. This study had major methodological problems; neither the sample size was calculated nor was a primary outcome measure predetermined. The authors believe that, according to experts and studies about multimodal pain therapy, scientifically established psychotherapies (cognitive behavioral therapy, trauma therapy, systemic family therapy, analytical therapy) in children with so-called JFMS should only be carried out as part of a multimodal pain therapy or for treatment of psychiatric co-morbidity. The content of the therapy should be adjusted to the individual child or adolescent and his/her situation. Local outpatient psychotherapy should be considered on a case-by-case basis. Physical therapy and physical measures Clinical consensus Physical therapy should be used as part of multimodal pain therapy. Strong consensus Comment. In a randomized-controlled trial (RCT), 14 patients with so-called JFMS were treated with aerobic exercise of moderate intensity and 16 were treated with Qi-Gong. At the end of therapy, the group performing aerobic training reported a greater reduction in pain, fatigue and impairment in quality of life than the group performing Qi-Gong. In the Qi-Gong group, there was significant change in pain, fatigue and impairment in quality of life [75]. A recent study by Kashikar-Zuck [37] showed that adoles- cents who suffered from so-called JFMS and who were physically active (“high activity” as measured by actigraphy), had less pain, were judged by their parents as being less depressed and were functionally less impaired as compared to adolescents who were moving less (“low activity”). However, the cross-sectional design did not allow establishing a cause-effect relationship. Studies on the efficacy of other methods of physical therapy and physical measures are not available. Nevertheless, these therapies are recommended by the authors with a level of recommendation grade B since they are preferred by the patients, are accompanied by a high level of adherence and have low risk of potential adverse effects, and since they are easy to implement in Germany, both on an outpatient and on an inpatient basis. Pharmacologic therapy Evidence-based recommendation Pharmacologic therapy should not be performed in children with CWP or socalled JFMS. Co-morbidities (e.g., depression in adolescence) should be treated according to the available guidelines. Evidence level 4, consensus Comment. Controlled drug studies are not available. In a U.S. case series of 15 patients, it was reported that aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) were not effective; 73% of children responded to cyclobenzaprine 5–25 mg/day [66]. Two observational studies reported on the use of NSAIDs and/or psychotropics in combination with exercise therapy [74] or a complex multimodal treatment [63]. Saccomani et al. [69] described a clinical improvement with trazodone or amitriptyline in 2 Italian patients. Children and adolescents were generally excluded from drug trials in adult FMS patients. Tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRI) are not approved for the treatment of children and adolescents in Germany (off-label therapy). Clinical experience suggests that there can be a role for drug therapy in the treatment of comorbidities of the individual multimodal therapy concept. However, focusing on medications must be avoided. The potential risks of drug therapy, the lack of approval of most drugs used as well as the failure to show a benefit for the individual patient justify, according to the authors’ opinion, a recommendation against drug therapy. Multimodal therapy Clinical consensus In patients with so-called JFMS, multimodal pain management should be performed. In cases of severe impairment or unsuccessful other approaches, this should be pursued in an inpatient unit, in case of less severe impairment, initially in an outpatient unit. Strong consensus Comment. Multimodal pain therapy, in the context of these guidelines, is understood to be a combination of at least one method of activating physical therapy with at least one method of psychotherapy, as described by the working group multimodal therapy [4]. In the case of outpatient multimodal pain therapy, the pediatric rheumatologist or pediatric pain specialist assumes the coordination of care. Stipulations of inpatient multimodal pain therapy for children in Germany are described in the OPS (“Operationenund Prozedurenschlüssel”) under paragraph 8–918.x. There are no RCTs on the efficacy of multimodal therapies in so-called JFMS. In pediatric studies on the effectiveness of multimodal treatment programs (outcome studies, level of evidence 2c), there was always a more or less large proportion of children and adolescents with CWP and additional psychosomatic/psychological complaints/abnormalities. The proportion of these children was 40% (n=23) in the study by Eccleston et al. [17], and in the study by Hechler and Dobe [25], the proportion of children with predominant musculoskeletal pain was 14% (n=28). In the latter work, the chronically ill children and adolescents in 40% of cases reported pain in more than one region (n=61). Three months after completion of inpatient multimodal pain therapy, 75% of children reported significant positive changes in pain intensity, 63% a significant improvement in pain-related Der Schmerz 3 · 2012 | 7 Schwerpunkt disability and 45% significant changes in the days absent from school (30% of the children had no significantly increased school absenteeism at baseline). Clinically significant changes in the emotional impairment were exhibited in 13–26% of patients, whereby 50–60% had no emotional distress at baseline. More than half of the children (55%) demonstrated overall improvement 3 months following treatment [25]. In their recent analysis of 200 children and adolescents with chronic pain, Dobe et al. [13] showed that the success of the multimodal inpatient program was independent of the site of pain. It is recommended children and parents receive instructions for home therapy during multimodal inpatient treatment. The continuation of parts of the multimodal program in everyday life is crucial for the prognosis. Relaxation techniques and physical therapy, exercise therapy and other athletic activities, physical activities and the coping with stressors and psychological problems (e.g., by use of social support) are important tasks to take home [12, 23, 25, 27]. Contraindications for multimodal inpatient treatment are serious psychiatric illnesses such as the presence of psychosis or anorexia nervosa [13]. Suicidal ideation in adolescents with chronic pain or depression—a frequently described comorbidity in children with chronic pain in multiple body regions—has been reported. Therefore, the diagnosis and treatment of children and adolescents with socalled JFMS should always be conducted by a multidisciplinary team, involving child and adolescent psychologists or psychiatrists. Discussion The first version of the guideline for socalled JFMS was substantially revised [48]. It has been shown that the diagnosis of JFMS is not yet scientifically established, so that the concept of so-called JFMS was implemented in this paper. The question of how children and adolescents with chronic pain in several body regions accompanied by other symptoms should be diagnosed and classified is an urgent question for future research. This raises 8 | Der Schmerz 3 · 2012 the question of whether the clinical picture of JFMS exists or whether the children and adolescents with these symptoms suffer from other specified diseases. A second new feature of the guidelines is the requirement for a standardized diagnostic procedure, which also includes validated psychological assessments. Since it is known that the so-called JFMS does not represent a well-established disease, it is even more important to recognize defined organic and mental diseases, such as posttraumatic stress disorder in order to identify and deliver appropriate therapy. As in the first version of the guideline, multimodal treatment approaches are warranted for affected children. In addition to the general principle of “outpatient before inpatient care”, we present criteria that, when present, suggest assignment to multimodal inpatient treatment. These criteria do not relate primarily to pain intensity or duration of the disease, but in particular to pain-related adverse effects such as school absenteeism, a marked reduction of the activities of daily living or social withdrawal. As in the first version of the guidelines, drug therapy is not recommended for the treatment of the so-called JFMS. Co-morbid mental disorders should be treated according to the respective guidelines. In summary, the revised and updated second version of this guideline clearly recommends a comprehensive reassessment of the so-called JFMS taking into account current work on quantitative sensory testing (QST), psychological assessment of chronic pain as well as the success of multimodal pain management programs in children and adolescents. Controlled studies for the diagnosis of children who present with a symptom complex that reminds of adult FMS, and RCTs of children suffering from chronic musculoskeletal pain and other physical and mental symptoms, are urgently needed to clarify the diagnosis of JFMS and to provide evidence for multimodal pain treatment for these children. Corresponding address Prof. Dr. B. Zernikow Deutsches Kinderschmerzzentrum, Vestische Kinder- und Jugendklinik, Universität Witten/Herdecke Dr. Friedrich-Steiner-Str. 5, 45711 Datteln Germany b.zernikow@deutsches-kinderschmerzzentrum. de Conflict of interest. See . Tab. 5 in “Methodological fundamentals used in developing the guidelines” by W. Häuser, K. Bernardy, H. Wang, and I. Kopp in this issue. References 1. Arnold LM, Hudson JI, Hess EV et al (2004) Family study of fibromyalgia. Arthritis Rheum 50:944–952 2. Arruda MA, Guidetti V, Galli F et al (2010) Frequent headaches in the preadolescent pediatric population: a population-based study. Neurology 74:903– 908 3. Blankenburg M, Boekens H, Hechler T et al (2010) Reference values for quantitative sensory testing in children and adolescents: developmental and gender differences of somatosensory perception. Pain 149:76–88 4. Burckhardt CS (2006) Multidisciplinary approaches for management of fibromyalgia. Curr Pharm Des 12:59–66 5. Buskila D, Neumann L (1996) Assessing functional disability and health status of women with fibromyalgia: validation of a Hebrew version of the Fibromyalgia Impact Questionnaire. J Rheumatol 23:903–906 6. Buskila D, Neumann L, Hershman E et al (1995) Fibromyalgia syndrome in children: an outcome study. J Rheumatol 22:525–528 7. Buskila D, Press J, Gedalia A et al (1993) Assessment of nonarticular tenderness and prevalence of fibromyalgia in children. J Rheumatol 20:368 8. Cabral DA, Tucker LB (1999) Malignancies in children who initially present with rheumatic complaints. J Pediatr 134:53–57 9. Clark P, Burgos-Vargas R, Medina-Palma C et al (1998) Prevalence of fibromyalgia in children: a clinical study of Mexican children. J Rheumatol 25:2009–2014 10. Conte PM, Walke GA, Kimura Y (2003) Temperament and stress response in children with juvenile primary fibromyalgia syndrome. Arthritis Rheum 48:2923–2930 11. Degotardi PJ, Klass ES, Rosenberg BS et al (2006) Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. J Pediatr Psychol 31:714–723 12. Dobe M, Damschen U, Reiffer-Wiesel B et al (2006) Dreiwöchige stationäre multimodale Schmerztherapie bei Kindern und Jugendlichen mit chronischen Schmerzen. Schmerz 20:51–60 13. Dobe M, Hechler T, Behlert J et al (2011) Chronisch schmerzkranke, schwer beeinträchtigte Kinder und Jugendliche: Langzeiterfolge einer dreiwöchigen stationären Schmerztherapie. Schmerz 25:411–422 14. Du Y, Knopf H, Zhuang W, Ellert U (2011) Pain perceived in a national community sample of German children and adolescents. Eur J Pain 15:649–657 15. Eccleston C (2008) Children with chronic widespread pain: hunting the snark. Pain 138:477–478 16. Eccleston C, Malleson P (2003) Managing chronic pain in children and adolescents. Br Med J 326:1408–1409 17. Eccleston C, Malleson P, Clinch J et al (2003) Chronic pain in adolescents: evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch Dis Child 88:881–885 18. Gedalia A, García CO, Molina JF et al (2000) Fibromyalgia syndrome: experience in a pediatric rheumatology clinic. Clin Exp Rheumatol 18:415–419 19. Gold JI, Mahrer NE, Yee J, Palermo T (2009) Pain, fatigue and health-related quality of life in children and adolescents with chronic pain. Clin J Pain 25:407–412 20. Gulewitsch MD, Enck P, Hautzinger M, Schlarb AA (2011) Irritable bowel syndrome symptoms among German students: prevalence, characteristics, and associations to somatic complaints, sleep, quality of life, and childhood abdominal pain. Eur J Gastroenterol Heptol 23:311–316 21. Häfner R, Michels H, Richter M (2004) Fibromyalgie im Kindes- u Jugendalter. Padiatr Prax 65:681–689 22. Häuser W, Schmutzer G, Glaesmer H, Brähler E (2009) Prävalenz und Prädiktoren von Schmerzen in mehreren Körperregionen. Schmerz 23:461–470 23. Hechler T, Blankenburg M, Dobe M et al (2010) Effectiveness of a multimodal inpatient treatment for pediatric chronic pain: a comparison between children and adolescents. Eur J Pain 14:97 24. Hechler T, Dobe M, Damschen U et al (2010) The pain provocation technique for adolescents with chronic pain: preliminary evidence for its effectiveness. Pain Med 11:897–910 25. Hechler T, Dobe M, Kosfelder J et al (2009) Effectiveness of a three-week multimodal inpatient pain treatment for adolescents suffering from chronic pain: statistical and clinical significance. Clin J Pain 25:156–166 26. Hechler T, Kosfelder J, Denecke H et al (2008) Schmerzbezogene Copingstrategien von Kindern und Jugendlichen mit chronischen Schmerzen – Überprüfung einer deutschen Fassung der Paediatric Pain Coping Inventory (PPCI). Schmerz 22:442–457 27. Hechler T, Kosfelder J, Vocks S et al (2010) Changes in pain-related coping strategies and their importance for treatment outcome following multimodal inpatient treatment: Does sex matter? J Pain 11:472–483 28. Hechler T, Martin A, Blankenburg M et al (2011) Specialized multimodal outpatient treatment for children with chronic pain: treatment pathways and long-term outcome. Eur J Pain 15:976–984 29. Hechler T, Martin A, Blankenburg M et al (2011) Specialized multimodal outpatient treatment for children with chronic pain: treatment pathways and long-term outcome. Eur J Pain 15:976–984 30. Hoftun GB, Romundstad PR, Zwart JA, Rygg M (2011) Chronic idiopathic pain in adolescencehigh prevalence and disability: The young HUNT study 2008. Pain (in press) 31. Hübner B, Hechler T, Dobe M et al (2009) Schmerzbezogene Beeinträchtigung bei Jugendlichen mit chronischen Schmerzen – Erste Überprüfung des Pediatric Pain Disability Index (P-PDI). Schmerz 23:20–32 32. Huguet A, Miro J (2008) The severity of chronic paediatric pain: an epidemiological study. J Pain 9:226–236 33. Huguet A, Miro J, Nieto R (2008) The Inventory of Parent/Caregiver Response to the Children’s Pain Experience (IRPEDNA): development and preliminary validation. Pain 134:128–139 34. Jones GT, Silman AJ, Macfarlane GJ (2003) Predicting the onset of widespread body pain among children. Arthritis Rheum 48:2615–2621 35. Kashikar Zuck S, Lynch AM, Slater S et al (2008) Family factors, emotional functioning, and functional impairment in juvenile fibromyalgia syndrome. Arthritis Care Res 59:1392–1398 36. Kashikar-Zuck S, Flowers SR, Claar RL et al (2011) Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain 152:1600–1607 37. Kashikar-Zuck S, Flowers SR, Verkamp E et al (2010) Actigraphy-based physical activity monitoring in adolescents with juvenile primary fibromyalgia syndrome. J Pain 11:885–893 38. Kashikar-Zuck S, Johnston M, Ting TV et al (2010) Relationship between school absenteeism and depressive symptoms among adolescents with juvenile fibromyalgia. J Pediatr Psychol 35:996–1004 39. Kashikar-Zuck S, Lynch AM, Graham TB et al (2007) Social functioning and peer relationships of adolescents with juvenile fibromyalgia syndrome. Arthritis Rheum 57:474–480 40. Kashikar-Zuck S, Parkins IS, Ting TV et al (2010) Controlled follow-up study of physical and psychosocial functioning of adolescents with juvenile primary fibromyalgia syndrome. Rheumatology (Oxford) 49:2204–2209 41. Kashikar-Zuck S, Swain NF, Jones BA, Graham TB (2005) Efficacy of cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. J Rheumatol 32:1594–1602 42. Keenan GF, Ostrov BE, Goldsmith DP, Athreya BH (1993) Rheumatic symptoms associated with hypothyroidism in children. J Pediatr 123:586–588 43. Libby CJ, Glenwick DS (2010) Protective and exacerbating factors in children and adolescents with fibromyalgia. Rehabil Psychol 55:151–158 44. Lommel K, Kapoor S, Bamford J et al (2009) Juvenile primary fibromyalgia syndrome in an inpatient adolescent psychiatric population. Int J Adolesc Med Health 21:571–580 45. Long AC, Krishnamurthy V, Palermo TM (2007) Sleep disturbances in school-age children with chronic pain. J Pediatr Psychol 33:258–268 46. Malleson PN, al-Matar M, Petty RE (1992) Idiopathic musculoskeletal pain syndromes in children. J Rheumatol 19:1786–1789 47. McGrath PA (1999) Chronic pain in children. In: Crombie IK, Croft PR, Linton SJ et al (eds) Epidemiology of pain. IASP Press, Seattle, WA, pp 81–101 48. Michels H, Gerhold K, Häfner R et al (2008) Fibromyalgiesyndrom bei Kindern und Jugendlichen. Schmerz 22:339–348 49. Michels H, Mengel E, Huppertz HI, Schaefer RM (2006) Morbus Gaucher, Mukopolysaccharidose Typ I (Scheie) und Morbus Fabry. Monatsschr Kinderheilkd 154:347–359 50. Mikkelsson M, El-Metwally A, Kautiainen H et al (2008) Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain 138:681–687 51. Mikkelsson M, Kaprio J, Salminen JJ et al (2001) Widespread pain among 11 year old Finnish twin pairs. Arthritis Rheum 44:481–485 52. Mikkelsson M, Salminen JJ, Sourander A, Kautiainen H (1998) Contributing factors to the persistence of musculoskeletal pain in preadolescents: a prospective 1-year follow-up study. Pain 77:67–72 53. Neumann L, Buskila D (1997) Quality of life and physical functioning of relatives of fibromyalgia patients. Semin Arthritis Rheum 26:834–839 54. Palermo TM (2000) Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr 21:58–69 55. Palermo TM (2009) Enhancing daily functioning with exposure and acceptance strategies: an important stride in the development of psychological therapies for pediatric chronic pain. Pain 142:189–190 56. Palermo TM, Eccleston C (2009) Parents of children and adolescents with chronic pain. Pain 146:15–17 57. Palermo TM, Wilson AC, Lewandowski AS et al (2011) Behavioral and psychosocial factors associated with insomnia in adolescents with chronic pain. Pain 152:89–94 58. Perquin CW, Hazebroek-Kampschreur AAJM et al (2000) Pain in children and adolescents: a common experience. Pain 87:51–58 59. Ravens Sieberer U, Gosch A, Rajmil L et al (2008) The KIDSCREEN 52 quality of life measure for children and adolescents: psychometric results from a cross cultural survey in 13 European countries. Value Health 11:645–658 60. Reid GJ, Lang BA, McGrath PJ (1997) Primary juvenile fibromyalgia. Psychological adjustment, family functioning, coping, and functional disability. Arthritis Rheum 40:752–760 61. Reid GJ, McGrath PJ, Lang BA (2005) Parent-child interactions among children with juvenile fibromyalgia, arthritis, and healthy controls. Pain 113:201–210 62. Reid RW, Zimmerman AA, Laussen PC et al (1997) The efficacy of tranexamic acid versus placebo in decreasing blood loss in pediatric patients undergoing repeat cardiac surgery. Anesth Analg 84:990–996 63. Richter M, Häfner R, Schurer A et al (2004) Das Garmischer Modell für die Behandlung von Schmerzpatienten in der Kinder-und Jugendrheumatologie [The Garmisch Model for Treating Pain in Pediatric and Adolescent Rheumatology]. Akt Rheumatol 29:158–163 64. Rief W, Zenz M, Schweiger U et al (2008) Redefining (somatoform) pain disorder in ICD-10: a compromise of different interest groups in Germany. Curr Opin Psychiatry 21:178–181 65. Roizenblatt S, Tufik S, Goldenberg J et al (1997) Juvenile fibromyalgia: clinical and polysomnographic aspects. J Rheumatol 24:579–585 66. Romano TJ (1991) Fibromyalgia in children; diagnosis and treatment. W V Med J 87:112–114 67. Roth-Isigkeit A (2006) Zur Epidemiologie von anhaltenden und/oder wiederkehrenden Schmerzen bei Kindern. Monatsschr Kinderheilkd 154:741– 754 68. Roth-Isigkeit A, Thyen U, Raspe HH et al (2004) Reports of pain among German children and adolescents: an epidemiological study. Acta Pediatr 93:258–263 69. Saccomani L, Vigliarolo MA, Sbolgi P et al (1993) Juvenile fibromyalgia syndrome: 2 clinical cases. Med Surg Ped 15:99–101 70. Schanberg LE, Anthony KK, Gil KM et al (2001) Family pain history predicts child health status in children with chronic rheumatic disease. Pediatrics 108:E47 Der Schmerz 3 · 2012 | 9 Schwerpunkt 71. Schroeder S, Hechler T, Denecke H et al (2010) Deutscher Schmerzfragebogen für Kinder, Jugendliche und deren Eltern (DSF-KJ) – Ein multimodaler Fragebogen zur Diagnostik und Therapie chronischer Schmerzen im Kindes- und Jugendalter. Schmerz 24:23–37 72. Sherry DD (2001) Diagnosis and treatment of amplified musculoskeletal pain in children. Clin Exp Rheumatol 19:617–620 73. Sherry DD, Malleson PN (2002) The idiopathic musculoskeletal pain syndromes in childhood. Rheum Dis Clin North Am 28:669–685 74. Siegel DM, Janeway D, Baum J (1998) Fibromyalgia syndrome in children and adolescents: clinical features at presentation and status at follow-up. Pediatrics 101:377–382 75. Stephens S, Feldman BM, Bradley N et al (2008) Feasibility and effectiveness of an aerobic exercise program in children with fibromyalgia: results of a randomized controlled pilot trial. Arthritis Care Res 59:1399–1406 76. Stormorken H, Brosstad F (1992) Fibromyalgia: family clustering and sensory urgency with early onset indicate genetic predisposition and thus a true disease. Scand J Rheumatol 21:207 77. Trapani S, Grisolia F, Simonini G et al (2000) Incidence of occult cancer in children presenting with musculoskeletal symptoms: a 10-year survey in a pediatric rheumatology unit. Semin Arthritis Rheum 29:348–359 78. Turk DC, Monarch ES (1996) Biopsychosocial perspective on chronic pain. In: Turk DC, Gatchel RJ (eds) Psychological approaches to pain management: a practitioner’s guide. The Guilford Press, New York, pp 3–29 79. Walker LS, Greene JW (1991) The Functional Disability Inventory: measuring neglected dimensions of child health status. J Pediatr Psychol 16:39–58 80. Wang SJ, Fuh JL, Juang KD, Lu SR (2009) Migraine and suicidal ideation in adolescents aged 13–15 years. Neurology 72:1146 81. Wolfe F, Clauw DJ, Fitzcharles MA et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600–610 82. Yunus MB, Khan MA, Rawlings KK et al (1999) Genetic linkage analysis of multicase families with fibromyalgia syndrome. J Rheumatol 26:408–412 83. Yunus MB, Masi AT (1985) Juvenile primary fibromyalgia syndrome. A clinical study of thirty three patients and matched normal controls. Arthritis Rheum 28:138–145 10 | Der Schmerz 3 · 2012
© Copyright 2025