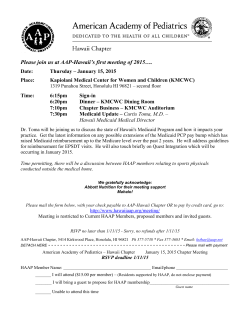
PDF - InsideHealthPolicy.com
InsideHealthPolicy.com’s Inside CMS exclusive news on the most powerful agency in health care Vol. 18, No. 2 - January 15, 2015 House E&C Panel To ‘Build Upon’ Last Year’s SGR Deal The House Energy & Commerce health subcommittee Wednesday (Jan. 14) announced a two-day hearing next week to “build upon” last year’s bipartisan deal to replace the Sustainable Growth Rate formula, and E&C Chair Fred Upton (R-MI) said the plan is to get the bill through Congress by the end of March when the current physician pay patch expires. However, many lobbyists doubt lawmakers can reach an agreement that fast, especially if they decide to open up last year’s bill. “Subcommittee members will look to build upon the bipartisan, bicameral agreement on policy reached in the 113th Congress and discuss options to permanently resolve this issue in a fiscally responsible manner,” Upton said in the Jan. 14 release. It is unclear what changes or additions might be considered. One physician lobbyist interprets the statement to mean subcommittee members will likely discuss how to pay for the bill. Upton pointed out in his statement that his committee unanimously passed last year’s bipartisan, bicameral SGR bill (H.R. 4302). However, the two parties couldn’t agree on how to pay for that policy deal. The fallout started when House GOP leadership said it would pay for SGR reform by axing the ACA’s individual mandate, then revised that to a mandate delay. The Senate responded by proposing to continued on page 10 CMS’ DME, Home Health, Hospice RAC Stalled By Performant Recovery Protest CMS is again facing protests in its recovery audit contractor program, with Performant Recovery protesting the award of the first national durable medical equipment, home health and hospice contract days after the agency awarded it to Connolly, LLC late last month. Some following the issue say the protest is not surprising, and one lobbyist said CMS seems to be doing its best to mitigate the effects of the protests by extending other CMS contracts. The agency awarded the DME, home health and hospice RAC contract — one of two contracts not already under protest from CGI Federal Inc. — to Connolly on Dec. 30. CMS said over the summer it hoped to award all of the RAC contracts before the end of the year, but with delays from the CGI protest continued on page 14 Anthem Strikes Deal With Gilead On Hep C Rx, But Still Restricts Coverage A newly penned deal between Gilead Sciences and Anthem on Harvoni (the third deal on hepatitis C drugs in as many weeks) is far from the last for Gilead, Wall Street analysts say, and the drug maker might strike a deal with Aetna soon. While Anthem is receiving favorable pricing in exchange for being partial to Gilead’s product, a company spokesperson said Anthem still restricts coverage of the drug to patients who have advanced liver disease or who are at greatest risk for liver complications. Express Scripts, which in December announced an exclusive formulary agreement for AbbVie’s competing Viekira Pak, has no coverage restrictions. Patient advocates and Medicaid directors are happy that pharmacy benefit continued on page 16 CMS Sued For Retroactively Changing Drug Compounding Reimbursement An Alabama company is suing CMS after receiving a re-pricing letter saying the company owed the government about $25 million due to billing changes for compounded drugs. A lawyer for the company questioned whether CMS can retroactively change prices and an industry attorney said the case may change how much authority the agency is willing to give Medicare Administrative Contractors. James Hoover, a lawyer for Alabama Pain Center, questions CMS’ use of the sub-regulatory process and says the agency’s bid to retroactively apply a local coverage decision is unconstitutional. Stephanie Trunk, an industry attorney following the case, predicts the controversy could spur CMS to come continued on page 18 OIG To Study How DME Bidding Affects Beneficiary Access To Supplies The HHS Office of Inspector General plans to look into whether Medicare beneficiaries’ access to durable medical equipment has been hurt by the competitive bidding program, following a request from lawmakers this summer that OIG probe the program. The American Association for Homecare is pleased with the OIG’s plan, and in an email Friday (Jan. 9) says the upcoming study will likely show access issues that the suppliers have long alleged the bidding program creates. OIG late last month told Rep. Tom Price (R-GA) that, after 137 House members asked the OIG to look into the DME competitive bidding program in July, it will conduct a national study looking at beneficiaries’ access to DME. “We plan to review documents from providers and Medicare claims data for a nationally representative sample of beneficiaries to determine and compare the rates at which beneficiaries successfully obtained needed items subject to competitive bidding,” the OIG letter to Price says. If beneficiaries have not received DME they need, the OIG says it will look for the reason behind that, as well. The study will look at both the first and second round of the program. Lawmakers in July expressed concern that CMS’ controversial competitive bidding program was cutting back on access, and they asked OIG to look into why beneficiaries who received DME before competitive bidding went into effect stopped receiving DME after. The OIG says it has been discussing its plans for the study with Price’s staff. When the second round of the program was gearing up, then-CMS Principal Deputy Administrator Jon Blum said the agency had virtually no complaints from beneficiaries about the program, and the Government Accountability Office and OIG gave the first rebid of the program favorable reviews in two April studies — though the GAO study noted that the number of beneficiaries who used DME decreased more in competitive bid areas than in other areas. CMS told the GAO the reduction could be the result of overuse in the non-bid areas, so the decreases don’t necessarily mean there are access problems. DME suppliers, however, have long alleged that falling prices for DME under competitive bidding, a lack of transparency and fewer suppliers participating in the program would lead to access issues for beneficiaries. The second round of competitive bidding, which expanded the program from nine major metropolitan areas to 91 areas, went into affect in July 2013 and led to prices in the program falling on average by 45 percent from fee schedule prices for DME and an average of 72 percent for diabetic test strips. “[W]e feel confident that the access issues we have been talking about all along will be uncovered by this process,” AAHomecare President Tom Ryan said in an AAHomecare alert to members. The OIG already is conducting a limited-scope review in 11 states around allegations that unlicensed suppliers were granted contracts in the second round of the program. Lawmakers had also encouraged the OIG to undertake a study in that area. The OIG is also conducting a post-award review of Round 2 of competitive bidding, and the OIG says that review may look at licensure issues based on what is found in the 11-state review. — Michelle M. Stein Hot Documents Now Available on InsideHealthPolicy.com The following new documents are available on InsideHealthPolicy.com, our new online health news service. Subscribers to InsideHealthPolicy.com also have access to hundreds of other health-related documents, daily news updates, and a searchable archive of back issues. Aetna Says Medicare Plan Finder Data On Pharmacies Inaccurate Rand: Ending Federal Exchange Subsidies Would Cut Exchange Enrollment By 9.6M House Passes ACA 40-Hour Work Week Mikulski Announces Senate Appropriations Subcommittee Ranking Members Advocate Urge HHS’ OCR To Act On Discrimination Complaint CCIIO Releases Model Auto-Enrollment Confirmation Messages Sens. McCain, Klobuchar Reintroduce Rx Import Rill Pew Urges MedPAC To Let Plans Use Patient Review And Restriction Programs To Curb Opioid Abuse AMA Files Friend-Of-Court Brief With SCOTUS On Medicaid Equal Access Measure Ahead Of Jan. 20 Oral Arguments Leavitt Partners Analyzes Potential Federal/State Reactions Following King v. Burwell Decision National Governors Association Suggests States Let Pharmacists Take On Bigger Role In Health Care Bipartisan Group Of Senators Introduce Bill To End ACA’s Medical Device Tax Grassley Presses Tavenner On CMS’ Role In Iowa Co-Op Failure Not an online subscriber? Inside CMS subscribers can get a free, two-week trial to InsideHealthPolicy.com by calling 1-800-424-9068 or signing up at http://www.insidehealthpolicy.com/health_signup.asp. 2 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 National Governors Association Suggests Bigger Role For Pharmacists The National Governors Association is encouraging states to consider amending laws and regulations to give pharmacists a bigger role in delivering care. The organization released a paper on Tuesday (Jan. 13) that highlights approaches some states have taken, including medication management and letting pharmacists directly care for beneficiaries. “Although they are most often associated with dispensing medications in retail pharmacies, their role is evolving to include providing direct care to patients as members of integrated health care provider teams,” the paper states. Integrating pharmacists into chronic-care delivery teams is one of the more promising approaches to improving health outcomes because pharmacists play a critical role in medication management of chronic disease. The group states that a limited number of studies indicate that pharmacists who provide medication therapy management improve outcomes and reduce costs. California, Montana, New Mexico and North Carolina created what they call an advanced practice pharmacy designation to expand pharmacists’ scope of practice. That designation allows pharmacists to care for patients directly, including primary care. Also, some states, such as Minnesota, Mississippi, and Ohio allow team-based models that rely on medication therapy management pharmacy services for chronically ill patients or patients who are unlikely to take their medications. Administrative barriers limit pharmacists from practicing to the top of their professional training and education, the paper states. Recognizing pharmacists as providers in state laws and regulations is a key step toward making better use of pharmacists, NGA says. Currently most states pay fees for drugs and the dispensing of them, and that product-based reimbursement drives pay policies for pharmacy services rather than the direct-care that pharmacists provide. Medicare and Medicaid also often prohibit pharmacists from practicing, particularly within integrated care teams. Medicare Part B does not define pharmacists as providers so they cannot bill for patient care services. Many state and private health plans align pay policies with Medicare policies and as a result do not let pharmacists bill for patient care services. Pharmacists also are not recognized as providers in accountable care organizations, which CMS champions as the epitome of team-based health care built on fee-for-service. Conversely, Medicare Part D reimburses for medication therapy management when provided under contract with prescription drug plan sponsors, but those services under Medicare Part D are defined narrowly to include medication review but not services such as chronic disease management, care coordination or other follow-up care Health information technology is another barrier to broadening the scope of pharmacists role in health care, NGA says. — John Wilkerson TRICARE Votes Against Restrictions On Compound Drugs A TRICARE beneficiary panel rejected recommendations to limit coverage of compound drugs, giving hope to compounding pharmacists that CMS might follow suit. An Express Scripts representative was one of the board members to vote against the recommendations, even though the pharmacy benefit manager limits coverage of compounded drugs on commercial formularies. The recommendation called for restricting TRICARE coverage to compounded drugs taken for FDA-approved indications. The Department of Defense’s Pharmacy and Therapeutic Committee said it forwarded the recommendation to the beneficiary panel to curb inappropriate use of compounded drugs. Aaron Lopez, director of public affairs with Professional Compounding Centers of America, a supplier of compounded drugs and supplies, said rejecting the recommendation is important for active duty military, “especially for injured soldiers coming home with special needs that only compounds can handle.” Lopez added that he’s hopeful this decision may be a starting point for more coverage of compounds in civilian life, whether through CMS or private insurers. David Ball, a spokesman for the International Academy of Compounding Pharmacists, said the impact of the vote on other government insurance programs is unclear. “It’s hard to say. Each of those government entities has a different medical organization in place,” Ball said. “We’re hoping it will be a precedent and that other government plans will take note and follow suit.” Ball said the IACP hopes all government insurance programs cover compounded drugs, including TRICARE, Medicare, Medicaid, and the federal employee prescription benefit. Rob Noel, senior vice president with United Compounding Management, said he’s not sure this will spur any changes with CMS or other government agencies but believes they will at least take notice. “I think other government agencies will sit up and say ‘Why did they change their behavior here?’” The vote by an Express Scripts representative on the committee to reject the recommendation also spawned mixed reviews from some in the compounding industry as the company has put some payment restrictions on compounds. In INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 3 2014 the company decided not to cover more than 1,000 bulk ingredients used to make compound drugs. “We hold out hope Express Scripts will go this way,” Lopez said. Noel said he was not surprised by the Express Scripts vote. “I presume as Express Scripts is the PBM for the Department of Defense that they had deep knowledge as to the needs of that population and made decisions based on that deep knowledge,” he said. Express Scripts did not explain the vote but said in a statement that they are committed to making sure TRICARE beneficiaries get the medications they need, and they offer clients a number of ways to control costs, though the decision to implement the solution is ultimately up to the client. Express Scripts’ policy regarding compounding has caused some changes in the industry, with PCCA creating PersonalMed and uniting pharmacies to work together to negotiate rates with pharmacy benefit manager companies. — Rebecca Beitsch FFM States: No Talk Of Creating Own Exchanges If SCOTUS Favors King States that rely on the federally facilitated exchange still lack a backup plan in the event that the Supreme Court outlaws federal health care subsidies for those enrolled in federal exchanges, according to several health stakeholders and officials working in states with federal or partnership insurance exchanges. Jodi Ray, project director of Florida Covering Kids & Families; Jennifer Koehler, executive director of GetCoveredIllinois; Phillip Bergquist, health center operations director for the Michigan Primary Care Association; and Ryan Barker, health policy vice president at the Missouri Foundation for Health, all said in a Thursday (Jan. 8) conference call led by Families USA that there is no talk of creating marketplaces in their own states should the health care law be gutted if the high court rules against the Obama administration in the King v. Burwell lawsuit this summer. Ray said there is nothing she can speak to as far as contingency planning, while Bergquist added that lawmakers and other health care officials are “pretty speculative at this point” on potential backup options. Families USA Executive Director Ron Pollack said on the conference call that it’s difficult to imagine an easy fix if King wins the lawsuit since Congress has been “tripping all over itself” to undermine the ACA. Congress never intended such a distinction between availability of subsidies in the federal and state exchanges, Pollack said. He added that state politicians never thought their decision to use the federally facilitated marketplace would have any impact on their ability to get tax credits for citizens. He pointed to Wisconsin Republican Gov. Scott Walker, who told the Wall Street Journal in March 2013 that there is “no real substantive difference between a federal exchange, or a state exchange, or the in between, the hybrid, the partnership.” “This really isn’t an exchange that the states run or even run in a partnership,” Walker said. “The federal government determines what’s going to be covered, how it’s going to be covered. And the only distinction is whether or not a state can say that they’re running it, put up a sign that says they are running it.” Projections of the lawsuit’s potential impact are increasingly dire: A RAND Corporation report released Thursday found that doing away with government subsidies for the low- and moderate-income people insured through the FFM would dramatically increase costs and cut 9.6 million people out of the individual market due to an inability to afford coverage. Enrollment in the 34 FFM states would drop from 13.7 million people to 4.1 million, the analysis said. FFM states have higher proportions of low-income citizens who are more likely to drop their coverage without financial help, RAND Health found. The Robert Wood Johnson Foundation also reported Thursday (Jan. 8) that average non-group premiums would go up $1,460 per year, from $4,130 to $5,590, if the administration loses the suit; the number of non-elderly uninsured adults in FFM states would go up by 8.2 million; and the number of non-elderly adults with non-group insurance would go down by 9.7 million if subsidies are eliminated. HHS Secretary Sylvia Burwell has so far stood firm in her insistence that the administration’s legal interpretation is correct and that consumers should not be worried. At a Dec. 23 press conference, Burwell avoided questions about whether the federal government was working on post-trial backup plans with state officials. “Unilateral action is no doubt being discussed by those in the administration,” Pollack said, adding that he believes no contingency planning will be made public at this point because HHS feels its case is on solid ground. But the administration’s approach could lead to a last-minute scramble to help the nearly 10 million Americans expected to be affected if the administration loses the case in June. In some states, past and present legislation block possible options for change, should local lawmakers try to fix the situation themselves. Illinois’ Democrat-controlled legislature last month failed to vote on a bill to create a state-based exchange before it adjourned for the year, meaning the state would not be able to apply for $270 million in exchange development money from the federal government. There is “no indication that there is any movement” to build an Illinois-run exchange following the bill’s expiration, Koehler said. Republican Governor-elect Bruce Rauner also opposes Obamacare, making a governor-led push for a state 4 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 marketplace unlikely. And in 2012, Missouri voters passed a ballot measure blocking Democratic Gov. Jay Nixon from issuing an executive order to create an exchange. A state marketplace could only be established through the state legislature or by popular vote, Barker said, or if that ballot measure is eventually overturned. Additionally, a Missouri state senator prefiled a bill Dec. 1 that would ban Missouri insurance companies from accepting federal subsidies — a proposal that, if passed, would complicate matters no matter which way the Supreme Court rules. Two identical bills were introduced in the past two years. The state insurance director “shall suspend the issuer’s license to transact business in Missouri” if a company accepts remuneration, and the suspension will stay in place until the company returns the subsidy and shows that it will decline any such future remuneration, according to the bill’s text. Barker said that his policy department has had lengthy discussions on the future of health care in Missouri but lacks the power to do anything but prepare for what may come. Koehler and Bergquist agreed that the best solution for FFM states would be one that is uniform for all, given that the ruling would apply to more than 30 states. “If the Supreme Court should decide that subsidies only apply to state-based exchanges, there would have to be some sort of national solution arrived at in Congress,” Koehler said. —Rachel S. Karas CA Proposes Renewing Medicaid Waiver, Sets Aside $300M For Hep C Rx California Gov. Jerry Brown (D) is proposing to renew for another five years the “Bridge to Reform” Medicaid 1115 waiver that the state used to expand coverage prior to implementation of the Affordable Care Act, and also wants to set aside $300 million to help offset the cost of hepatitis C drugs, such as Sovaldi and Harvoni, due to the large number of patients in state programs. Several new drugs have been approved for the treatment of hepatitis C, with the regimens costing about $85,000, states Brown’s budget, released Friday (Jan. 9). There are thousands of inmates in state prisons, patients in state hospitals, and participants in Medi-Cal and the AIDS Drug Assistance Program who are infected with hepatitis C, so the budget reserves $300 million to account for the fiscal impact of these high-cost drugs. The Brown administration also plans to convene a workgroup of affected entities who will examine ways to address the state’s approach regarding high-cost drug utilization policies and payment structures, the budget says. The California Association of Health Plans (CAHP) applauded the move as “prudent” and noted that the costs may only be the tip of the iceberg. “The high rates of Hepatitis C infections coupled with six-figure prices for new drugs will soon become a budget buster across state programs,” CAHP said in a release. “These drug prices are unsustainable, and it’s more important now than ever to be working towards an affordable, sustainable health care system. We appreciate that the Governor has recognized this growing liability in the state budget and hope to further investigate the full impact of high priced drugs on our state,” the group added. Regarding the Medicaid waiver, the budget says that the main objectives will be to strengthen primary care, avoid unnecessary institutionalization, and use Medi-Cal to test new ways of providing services. The initial five-year, $10 billion Medicaid waiver was approved in November 2010, and included $2.9 billion for expanding coverage, $3.3 billion for improving safety net hospitals and $3.9 billion for uncompensated care. The budget assumes a continuation of the funding for public hospitals, but updates will come as part of the revised budget, which will be out in May after the Department of Health Care Services submits the waiver. The budget also assumes a net cost of $2 billion for the state share of Medicaid expansion requirements, including simplified eligibility, enrollment, and retention rules. Another $14.3 billion is expected in state costs for the optional expansion that covers adults up to 138 percent of poverty. An estimated 3.3 million additional people are expected to enroll in Medi-Cal by the end of the fiscal 2016 budget year for a total 12.2 million people, or 32 percent of the state’s population. The budget allocates an additional $150 million for 2015 to help support Medicaid eligibility determinations. The state’s automatic eligibility system is not finished so the state must rely on county workers to manually review eligibility. It proposes $240 million for 2016, but officials will monitor the progress of the system in case additional funding is needed. “Once the eligibility system stabilizes, the state will conduct time studies to inform a new Medi-Cal county administration budgeting methodology,” the budget says. The budget also assumes $150 million for Medi-Cal coverage of behavioral health services per new federal guidance that requires such coverage under Medicaid. It further proposes to create a 90-day annual enrollment period, similar to Covered California’s enrollment, during which certain non-disabled Medicaid enrollees would be able to switch managed care plans. The proposal would not impact the ability of individuals to apply for and be enrolled in Medi-Cal coverage at any time throughout the year and would result in savings of $1.6 million. The state expects about 2 million residents will be insured through Covered California by the end of the 2016 budget INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 5 year. The state received about $1 billion from the federal government for building Covered California prior to 2015. Per the ACA, exchanges must be self-sustaining after 2015, and plans will pay user fees that support the state-based exchange. The state also proposes to apply a tax on managed care plans. The tax will replace an assessment that is currently in effect. The federal government recently indicated that the original tax was not allowed because it had been narrowly applied to only Medi-Cal plan. In response to the proposal, the CAHP praised the state for halving its uninsured rate. “Health plans look forward to working constructively with the Administration on a proposal that maintains or increases federal support for Medi-Cal,” CAHP said. “With the Medi-Cal program serving nearly one in three Californians, it is important to ensure existing and new funding streams directly support the program and do not impact the affordability of health care for any Californians.” The plans — and the budget — points out that the state received the lowest percentage of federal Medicaid support. The federal government paid about half of Medicaid claims for the non-expansion population. — Amy Lotven Senate Device-Tax Repeal One Dem Shy Of Passage, Warren Not A Cosponor A bipartisan Senate bill repealing the ACA’s contentious medical device tax appears to be only one Democrat shy from passage. Five Democratic senators cosigned the legislation, introduced Tuesday (Jan. 13), but Sen. Elizabeth Warren (D-MA), a long-time supporter of repealing the tax who reportedly was courted as a cosponsor, is not on the bill. Warren has supported repealing the device tax since winning her Senate seat in 2012. Her office did not respond to Inside Health Policy for this article, and other news reports also say she has declined to discuss whether she will support the bill, called the “Medical Device Access and Innovation Protection Act.” Senate Finance Committee Chair Orrin Hatch (R-UT) introduced the bill, and nine other senators cosponsored it: Sens. Amy Klobuchar (D-MN), Pat Toomey (R-PA), Joe Donnelly (D-IN), Richard Burr (R-NC), Al Franken (D-MN), Rob Portman (R-OH), Bob Casey (D-PA), Dan Coats (R-IN) and Jeanne Shaheen (D-NH). “Every dollar medical device manufacturers spend on this onerous tax is a dollar taken away from American innovation, job growth, and the ability to provide groundbreaking medical technologies to patients in need,” Hatch said. “Both Republicans and Democrats understand just how bad this tax really is, and we owe it to the American people to ensure the development of life-saving medical devices are not plagued by high costs that will, ultimately be passed on to patients. This is a common-sense bill, and I’m hopeful Congress will act swiftly to repeal this misguided tax once and for all.” The Advanced Medical Technology Association (AdvaMed), the Medical Imaging & Technology Alliance (MITA) and the Medical Device Manufacturers Association (MDMA) support Hatch’s bill. “This tax is an anchor on American economic growth,” said Stephen Ubl, president and CEO of AdvaMed. The legislation comes on the heels of a similar House bill that at 254 cosponsors, including 27 Democrats, and was also supported by the three medical device industry groups. — Erin Durkin Senators Introduce Rx Import Bill Amid Debate Over Prices Sens. John McCain (R-AZ) and Amy Klobuchar (D-MN) last week reintroduced legislation allowing Americans to import drugs from Canada, a proposal that has lay dormant for a good decade and that still isn’t getting much attention from advocates of lower drug prices. The Affordable Care Act gradually closes Medicare’s drug benefit coverage gap, and the law led to many more people receiving drug coverage outside of Medicare, but some say the fear of rising drug prices keeps the legislation in the picture, if just barely. “Not really our top priority,” said National Coalition on Health Care Director John Rother, who also leads the Coalition for Sustainable Rx Prices. Asked why the legislation is still needed with the closing coverage gap, Klobuchar told Inside Health Policy it has as much to do with pressuring drug companies to lower their prices as it does with giving people a way to find less-expensive drugs that otherwise are identical to those sold here. She said that even though individual seniors might be less exposed to high prices than in the past, tax payers must still foot the bill for brand drugs that are on average twice as expensive here as in Canada. Generics in the United States are cheaper than in Canada. Likewise, an AARP spokesperson said reimportation and other price-containment policies are needed now as much as ever because of the high cost of brand name and specialty medicines. The drug price debate reared its head last year after Gilead priced its hepatitis C drug Sovaldi at $84,000 for a 12week course. FDA late in the year approved the second generation of that drug, called Harvoni, which costs $94,500 and is a once-daily pill taken without the interferon that for decades made patients very sick. FDA then approved AbbVie’s Viekira Pak in December, which also is interferon-free and has a similarly stellar cure rate but a more complicated 6 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 regimen. Viekira Pak costs $83,319. Pharmacy benefit managers and health plans began negotiating discounts on the drugs following Viekira Pak’s approval, but the amount of the discounts is not public. FDA already allows people to import a 90-day personal supply of drugs, which happens to match the typical 12-week course of hepatitis C drugs. Despite broader drug coverage in recent years, many people have plans that restrict hepatitis C drugs to those with advanced liver disease. Gilead discounts its heapatitis C drugs in other countries — Sovaldi sells for less than $1,000 for a 12-week course in Egypt. Sources say it might make sense for those people to turn to health care tourism and “drug reimportation,” but for the most part, the fight over drug costs is between drug makers and health plans, not drug makers and beneficiaries. Under the McCain/Klobuchar bill, imported prescription drugs would have to be purchased from approved Canadian pharmacies and dispensed by licensed pharmacists. Drugs would have to be the same dosage, form, and potency as drugs sold here. — John Wilkerson Pew Urges MedPAC To Recommend Pharmacy Lock-In Policies Pew Charitable Trusts is urging Congress’ Medicare payment advisers to recommend that lawmakers allow Part D (drug) plans to lock beneficiaries into certain pharmacies or physicians to cut back on opioid abuse. Pew says that locking beneficiaries into certain pharmacies or prescribers is a pro-active way for plans to address drug abuse, and such a program can be built with enough safeguards to make sure beneficiaries’ legitimate access to these medications is not at risk. Beneficiary lock-in programs, which Pew notes are used in both commercial and Medicaid plans, allow for plans to restrict beneficiaries deemed high risk to a certain pharmacy or pharmacies and one or more physicians to receive drugs that could be abused like opioids. Pew says the lock-in programs, or patient review and restriction programs, are used by both private plans and states because of their effectiveness in dealing with abuse of prescription drugs, and particularly opioids. State Medicaid programs using such programs have seen savings along with a reduction in narcotic prescriptions, abuse and visits to multiple doctors and emergency rooms, Pew says, pointing to a study from the Centers for Disease Control and Prevention. Former CMS Medicare chief Jon Blum expressed interest in the possibility of locking beneficiaries susceptible to abuse into certain pharmacies while heading the program, though currently Medicare plans are not allowed to institute such programs. However, Pew’s drug abuse project says giving plans authority to institute these programs would reduce inappropriate use of prescription drugs and make sure those who need them still have access. The Medicare Payment Advisory Commission plans to discuss the status of the Part D program at its January meeting this week. In October, the commission looked at potentially inappropriate opioid use in Part D. Pew says that Medicare plans can use drug utilization reviews and point-of-sale edits to allow plans to deny prescriptions or impose quantity limits on drugs that are susceptible to abuse. “As noted by several commission members at the MedPAC [October] meeting, these strategies represent retrospective interventions, which may be limited in their effectiveness. In addition, point-of-sale edits can delay or prevent access to medications for those with legitimate pain,” Pew’s Jan. 12 letter to MedPAC. Pew suggests that instead, plans should be able to lock-in beneficiaries to a specific pharmacies or providers. Finite enrollment periods in such programs along with appeals and beneficiaries’ input on which pharmacies and prescribers they should be locked into help provide some safeguards for the program. Pew also says that limiting beneficiaries to one pharmacy or doctor, which is generally how such programs are set up, also helps with care coordination. Pharmacy benefit managers have been in favor of lock-in programs, and applauded House Ways & Means health subcommittee chair Kevin Brady (R-TX) and Ways & Means ranking Democrat Jim McDermott (WA) for including a lock-in proposal in their Medicare program integrity bill, which was introduced in December. McDermott has said the bill will set the stage for continuing discussions around Medicare program integrity this Congress. AARP has said it is in favor of a beneficiary lock-in in principle, but there must be enough beneficiary protections in practice. But some other beneficiary advocates commenting on the draft program integrity bill said that without certain beneficiary protections, they are wary of placing these decisions in the hands of plans and PBMs that they allege don’t have a good track record in dealing with drug appeals to begin with. One beneficiary advocate, however, said the bill introduced in December included a much improved version of a beneficiary lock-in program. Stacy Sanders, federal policy director at the Medicare Rights Center, said any lock-in plan needs to have beneficiary protections in place including data sharing, CMS oversight, an appeals system, the involvement of physicians and clinicians, and provider and beneficiary education. If a program is constructed well and is targeted, then it could be workable with the right safeguards, she said. The Medicare Rights Center told MedPAC in an October letter that if they decide to recommend a beneficiary lockINSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 7 in program, they should also consider including these protections. “With respect to ‘lock-in’ proposals, this purpose can only be advanced through a carefully designed program that balances the need to ensure access to medically necessary prescription drugs with the need to reduce fraud and assist beneficiaries addicted to prescription medications,” the Medicare Rights Center letter says. — Michelle M. Stein Upton, DeGette Lay Out Basic Framework For 21st Century Cures Bill House Energy & Commerce chair Fred Upton (R-MI) and Rep. Diana DeGette (D-CO) on Tuesday laid out five broad goals of the 21st Century Cures draft bill they plan to introduce later this month: targeting clinical trials to the “right group” of patients; better integrating the patient perspective into the regulatory process through public-private partnerships; promoting better access to and sharing of data among researchers; increasing and targeting funding for scientific research; and incentivizing new drugs and devices for unmet medical needs by relying more on post-market studies and possibly offering exclusivity or reimbursement incentives. In a Jan. 13 CNN op-ed on the upcoming bill, Upton and DeGette write that after a year of hearings on the initiative they are ready to put forward bipartisan legislation that will promote finding cures for 7,000 diseases and ensure the United States is a leader in the field of medical innovation. “Our legislation will modernize all of these categories, removing outdated hurdles that can prevent innovation from flourishing or from fleeing the United States.,” Upton and DeGette write. The bipartisan duo do not detail specific provisions of the forthcoming draft, but lay out brief justifications of the four goals laid out in the piece that offer a framework for the legislation. Streamlining clinical trails. The lawmakers say clinical trails should use technology like genetic screening to create smaller, more-targeted clinical trials that ensure the “right treatments” are developed for “the right group of patients.” They say the legislation will also streamline the paperwork process for clinical trials to make it easier to recruit patients and adapt the operation of trials as new information becomes available. “[T]he old approach of automatically applying a therapy to a broad group of patients is no longer the best path forward, particularly for those diseases for which we do not have a treatment or cure,” Upton and DeGette write. Integrating the patient perspective into the regulatory process. The lawmakers say they want to build off the FDA’s Patient-Focused Drug Development Program to incorporate patients perspectives into the regulatory process by using public-private partnerships to help “build the science” around biomarkers and patient-reported outcomes. “We also will create a predictable process for the qualification of biomarkers and patient-reported outcomes so we can utilize these tools in the development process,” they write. Promoting better access to and sharing of data. Upton and DeGette say the bill will promote better access and sharing of genomic and other clinical data among researchers and foster interoperability. The bill will also “assist developers and entrepreneurs” develop patient-focused technologies by reducing regulatory uncertainty as they design new apps and products. “With the explosion of technology, we can collect, monitor and analyze information like never before, helping patients stay healthy and adopt healthy habits while also making treatments safer and more effective,” they write. Increasing and targeting funding for scientific research. The pair says the legislation help young scientists have more access to resources to fund their research and encourage them to conduct their research in the U.S. “Many of our most promising investigators — many with great ideas and cutting edge training — are hamstrung by the challenges of securing much-needed support,” they write. Incentivizing new drugs and devices for unmet medical needs. Upton and DeGette say the legislation will streamline the premarket process and create mechanisms to “better capture” evidence post-market in the development of drugs and devices designed to target unmet medical needs. They say the bill will also “examine incentives” like exclusivity and simplifying the reimbursement process. “America has a strong history of finding solutions to diseases through medical innovation. Today, partnerships with patients and advocates, health care workers and researchers, and government and the private sector can speed the cycle of finding faster cures,” Upton and DeGette write. Upton has said he expects to have final language for the bill in March, and hopes to have a vote on the legislation by Memorial Day with the goal of having the measure on the president’s desk by the end of the year. Stakeholders at a recent IIR-sponsored FDA/CMS Summit said they view work on the 21st Century Cures Initiative this spring to be a staging ground for negotiations over the sixth iteration of the Prescription Drug User Fee Act (PDUFA) in 2016 and 2017, and Janet Woodcock, director of FDA’s Center for Drug Evaluation and Research (CDER), said the 21st Century Cures initiative is a “front burner” priority for the agency. — Todd Allen Wilson 8 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 Ahead of FDA’s LDT public workshop... Clinical Lab Group Outlines Legal Arguments Against FDA’s LDT Oversight The American Clinical Laboratory Association, the group heading up efforts to quash FDA’s planned oversight of laboratory developed tests (LDTs), released a paper Wednesday (Jan. 7) blasting FDA’s proposed regulatory framework as “a dramatic overreach” without “any statutory basis.” The paper, authored by ACLA’s recently tapped counsel, Harvard University law professor Laurence Tribe and former Solicitor General Paul Clement, now a partner with Bancroft PLLC, lays out potential legal arguments against the framework and was released a day before FDA’s Thursday (Jan. 8) public meeting on the issue. At issue is FDA’s plan, laid out in draft guidance, to apply the existing device classification system to LTDs over a nine-year implementation period. The ACLA paper alleges FDA lacks statutory standing for its proposed regulatory framework because LDTs do not fit under the definition of a “device.” If FDA moves forward, the authors say, the agency would not be not equipped to bear the regulatory burden and would interfere with the practice of medicine. The paper also takes issue with FDA’s use of a guidance document to advance new regulatory policy, saying this strategy circumvents requirements of rulemaking, including the requirement for an economic impact analysis. Statutory overreach. The paper argues that LDTs do not fit under the definition of a “device” and therefore the Food, Drug and Cosmetic Act does not provide authority to the agency to regulate these tests. “FDA ignores the fact that the statute does not classify based on functionality, but on whether something is a physical article that a manufacturer commercially distributes in interstate commerce,” states the paper. The paper also criticizes FDA’s premise that doctors are relying on laboratory tests that are “unapproved” devices, saying it underscores the extreme implication of the agency’s interpretation of FDCA: that the entire medical profession has, unbeknownst to doctors, been involved in the widespread illegal distribution of unapproved medical devices since 1976. “Under FDA’s theory, every doctor who sends a specimen for analysis via a laboratory-developed testing service is really soliciting an unlawful medical device,” the authors state. Innovation implications. ACLA’s paper alleges that FDA oversight of such tests would “sharply curtail” the number of tests available to doctors and their patients, pointing out that a large number of critical diagnostic tests are available only as in-house laboratory tests. FDA oversight would “stunt and stifle” innovation and competition in the diagnostic testing field, the authors state. Regulatory burden. “As a practical matter, moreover, FDA is manifestly not equipped to bear the massive regulatory burden it claims that Congress intended it to shoulder,” argues the group. “FDA has projected that it would take near a decade for it to phase in its asserted regulatory authority over laboratory-developed testing services. That it would take that many years to handle the full scope of the administrative responsibilities it asserts is yet another indication that Congress never intended for FDA’s preexisting (and ill-suited) regulations over drugs and devices in interstate commerce to sweep in laboratory-developed testing services.” Inadequate public comment. Further, the attorneys say the agency failed to undertake the notice-and-comment procedures that would be required to create the proposed framework, and that the use of a guidance document was an improper way to move forward on the new policy. They also note that the guidance document does not consider the cost and economic impact of the proposed requirements, which is required when the agency goes through the rulemaking process. No economic impact analysis. “The absence of an economic impact analysis is a particularly glaring omission given the sweeping practical effects of FDA’s radical change in policy,” the paper states. “As noted, FDA’s assertion of jurisdiction will significantly burden clinical laboratories, superimposing a duplicative bureaucratic regime on a vibrant and constantly evolving laboratory testing industry that is already closely regulated under CLIA, and that FDA has no prior experience in regulating.” But the Advanced Medical Technology Association, which supports FDA’s regulatory plan, said the lab group’s legal arguments are an “attempt to obscure the fact tests are a regulated tool that doctors us in the care of patients.” AdvaMed Diagnostics Executive Director Andrew Fish said the practice of medicine exemption does not appropriately extend to the development of tests. “The test itself is a medical device,” said Fish. A former senior FDA reviewer also said he feels that the matter of whether FDA has jurisdiction over LDTs is a reasonably settled issue and stakeholders should focus on working with the agency. FDA is interested in listening to stakeholders’ views on how the agency can best regulate these tests, said Lakshman Ramamurthy, director of FDA and regulatory policy at Avalere Health, adding that the agency should find a balance between safety and innovation. He also described FDA’s draft guidance as just laying the “groundwork” for the agency’s framework. — Erin Durkin INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 9 E&C Plans SGR Hearing . . . begins on page one simply not pay for the bill, which Republicans refuse to go along with. Lawmakers ended up passing a temporary pay patch instead. The health subcommittee hearing will be held on Jan. 21 and Jan. 22 in 2322 Rayburn House Office Building. The committee has not yet posted a list of witnesses. The American Medical Association views passage of an SGR replacement bill as one of its top 2015 priorities. “Congress will need to act early this year to avoid a 21 percent pay cut scheduled to take effect April 1 under the sustainable growth rate (SGR) formula” AMA says in a January issue advocacy alert. “Because Congress missed its opportunity last year to repeal the SGR formula using a bipartisan legislative framework, the AMA and physicians will continue communicating with lawmakers—including those newly elected—to make reforming the Medicare payment system a priority for the new Congress,” the alert adds. AMA expresses hope that Congress will not again resort to a temporary payment patch as it has done in prior years to avert SGR-driven cuts. The physician group notes in a separate document on its web site that the 21.2 percent cut to physician payments slated to go into effect April 1 is a considerable drop from the nearly 30 percent cut projected just a few years ago. “The reduction is thanks to nearly flat growth in utilization of physician services over the past several years,” AMA notes. In addition to addressing the SGR formula, the AMA says in its January advocacy alert that it will be tackling other issues related to the Medicare fee schedule, including the value-based payment modifier, elimination of the global surgical period and potentially misvalued codes. The SGR bill’s treatment of misvalued codes was an area of debate last year. Last year’s bipartisan SGR replacement bill called for a 0.5 percent payment update for five years under the fee-forservice model as a transition, while allowing for further updates if needed. — John Wilkerson Murray Resumes Bid To Extend ACA’s Medicaid Primary Care Bump Despite losing a similar battle last year, Sen. Patty Murray (D-WA) intends to reintroduce a bill that would extend for two years the ACA’s Medicaid primary care pay bump that expired Jan. 1. But the measure, despite its strong support from primary care physician groups and the administration last year, could face roadblocks as state Medicaid officials, health plans and congressional advisers may not be pushing to restore it this year, sources say. A source close to the issue said the health committee’s ranking Democrat plans to introduce the same measure as last year, allowing doctors as well as physicians assistants, nurse practitioners and gynecologists who see Medicaid patients to be reimbursed at the same level as Medicare. A similar bill will be sponsored in the House by Rep. Kathy Castor (D-FL). Murray’s office did not respond to questions on the bill’s cost and whether it would retroactively reimburse doctors for Medicaid patients they see after Jan. 1. The source said it will be introduced in the next few weeks or months and may be attached to other legislation such as a measure to avert Medicare physician payment cuts. A health care lobbyist said there may also be ways to do this administratively. The National Association of Medicaid Directors and Medicaid Health Plans of America say they are supportive of the general idea of doctors getting paid more, but say the pay bump was complicated and did not work as expected, attracting few additional doctors to the program. States’ reports to the congressional Medicaid and CHIP Payment and Access Commission said the pay increase had “at best a modest effect on provider participation” in the program. The data came from seven states and the District of Columbia. Matt Salo, executive director of NAMD, said the bill is not a top priority for his group because of the complications involved with the pay increase, but some of the group’s member states are committed to closing the gap. Even if the extension doesn’t pass, there are about 15 states that will use their own funds to fully or partially continue the higher rates, according to the Kaiser Family Foundation. “This legislation is a straightforward step toward helping more women and families get affordable, quality health care—a goal that both Republicans and Democrats should be able to agree on—and I’m committed to continuing to fight for it this Congress,” Murray said in a recent statement. In a November meeting, an American Medical Association council voted in favor of both continuing the pay bump past 2014 and extending the increase to gynecologists providing primary care. The American College of Physicians has already sent a letter to Congress urging lawmakers to restore the pay increase, as the expiration has cut physician payments by about 40 percent. A survey released by the group last year found that 40 percent of primary care physicians surveyed said they would stop accepting Medicaid patients and 6 percent said they would drop out of the program altogether if the pay bump expired at the end of December. ACP also endorsed last year’s Senate bill, the Ensuring Access to Primary Care for Women & Children Act. That measure was also backed by the American Academy of Family Physicians, American Academy of Pediatrics, American 10 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 College of Nurse-Midwives, American Congress of Obstetricians and Gynecologists, American Osteopathic Association, National Association of Pediatric Nurse Practitioners, National Nursing Centers Consortium, and Society of Hospital Medicine. Last year’s bill was cosponsored by Sen. Sherrod Brown (D-OH). Rep. John Lewis (D-GA) introduced a House version that would have continued Medicaid pay parity for five years rather than the two years proposed by the Senate bill. The Center for Health Care Strategies Inc., in a brief released last September, said there had not been enough time since the “pay bump” began in January 2013 to assess whether it had been effective, especially given roll-out problems that left many primary care providers not receiving increased pay for more than nine months after the program’s start. Additionally, the CHCS said changes needed to be made to the pay bump if it’s extended in order for the program to meet its goals. It is unclear if the White House will include the payment bump in its upcoming budget request, as it did last year. The provision in the 2015 budget request, at a of $5.44 billion, would have also extended the increase to physician assistants and nurse practitioners. That move followed a concerted lobby by primary care providers for the extension, which they told White House officials in a private meeting late last year was particularly important in light of insurers’ moves toward narrow provider networks. — Rebecca Beitsch States, Insurers Upset By HHS Proposal to Streamline Rate Reviews State regulators and insurers oppose an attempt by HHS to regulate and standardize states’ health insurance rate review processes, including a plan to publish all final rates at the same time ahead of the first day of open enrollment, as laid out in several sections of the department’s proposed rule on 2016 benefits and payment parameters. The stakeholders argue that HHS’ proposal would stifle states’ ability to run rate reviews, delay the filing review process for on- and offexchange markets, and lessen public access to information about rate hikes. The proposed rule aims to streamline the rate filing process by creating a uniform timeline across all states under which issuers must send a completed rate filing justification to CMS and the state, if needed. A health insurance issuer must submit their justification by whichever of the following is earlier: the date by which a state requires that a proposed rate increase be filed with the state or the date specified by the responsible department secretary. HHS is also more tentatively looking to choose a deadline at the end of the federal exchange’s QHP application window when issuers would submit their justifications for proposed rate increases in individual and small group markets for both QHPs and non-QHPs at the same time. The agency’s proposal adds that states would be able to set earlier rate filing deadlines to meet their unique needs. “The proposed approach would assure that all rate increases in every relevant State market for both QHPs and nonQHPs are filed by a consistent time each year,” the proposed rule states. “This would improve predictability and transparency, reduce the opportunity for anti-competitive behavior, and establish a more meaningful opportunity for consumers and other stakeholders to comment on proposed rate increases before rates are finalized.” Another section of the proposal changes the time frame and way in which a state with an effective rate review program provides public access to information on proposed and final rate increases, if it chooses to make those details public. These amendments include: • For proposed and final rate increases, states must make information in Parts I through III of the rate filing justification that are available on the CMS site accessible through their own website, or direct consumers to the CMS website. • States must have a way to receive public comments on those proposed rate increases. • CMS suggests a possible deadline of 10 business days after receipt of all rate filings in the appropriate market for information to be posted about the proposed rate increases that are subject to review. • On final rate increases, the information would be required to be posted no later than the first day of annual open enrollment. States could make more details available earlier than this deadline at their discretion. • If a state does make information on proposed increases available earlier than the date specified by the secretary, or before the first day of open enrollment, the state must tell CMS in writing of its intent to do so no later than 30 days prior to when it expects to make the information public. State officials and national insurance advocates largely disagree with HHS’ thinking and say that the guidelines would stifle states’ ability to run rate reviews according to their own capacity and staffing needs. They believe the mandates would place significant pressure on state regulators, possibly delay the filing review process for on- and offexchange markets, and lessen public access to information about the proposed and final rate increases. Administrative costs and challenges are disruptive and would unnecessarily delay the rate filing process, stakeholders warned in their comment letters submitted last month. “To require all states to develop their own websites would be costly and unnecessary, especially considering that the federal government has or should have a system already in place for this activity,” National Association of Insurance Commissioners officials says in a comment letter. “States would also have to fund this system into the future if the rules INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 11 are adopted, without the aid of federal grant money since those funds are set to expire. This creates an additional unfunded mandate upon the states.” Insurance commissioners also strongly oppose the idea of publishing all final rates at the same time ahead of the first day of open enrollment, calling it neither a requirement of the law nor a move that would fulfill “any recognized purpose of the Affordable Care Act.” HHS should not preempt state regulations and procedures that already dictate final rate publishing, they say. America’s Health Insurance Plans writes in its comments that it opposes using the same definition of “plan” for rate reviews and health insurance issuer standards. The group worries that the definition “results in the current product level rate filings being expanded into multiple and unwarranted versions of the rate filing process that will create duplication of work and uploads. It will create unnecessary pressures on insurers and state regulators, increasing the costs and burdens on both. The proposal also has the potential to create delays in the filing and review process for all rates.” Hawaii’s insurance division calls the filing process proposal “unrealistic” and problematic in practical implementation, while North Carolina points out that the changes would conflict with state sunshine laws, increase processing time, adversely impact state review of single risk pool filings, insurance policy form review and plan level reviews; and would not be helpful to the public. “(T)he Department utilizes a ‘Public Online Portal’ which provides the public access to all regulatory filings made to the Life & Health Division as soon as those filings are submitted to the State via the NAIC’s System for Electronic Rate and Form Filings,” North Carolina insurance department assistant director Jean Holliday writes. “The Department cannot suppress a filing from appearing in the Public Portal, nor are we aware of a way in which we could suppress a filing should we wish to. Public information provisions found in State laws should be respected and not interfered with by this type of federal standard which in NC would actually reduce public access rather than improve it.” Wisconsin Deputy Insurance Commissioner Daniel Schwartzer adds that both a quarterly and annual rate filing would not be feasible for most companies, and it is already difficult for carriers to assess emerging claims experience and then price appropriately under the current timeline. Companies would be forced to guess about emerging claims experience, leading to uninformed rate change requests, he says. Schwartzer also rejects the idea of a uniform filing timeline because the state’s rate filings are not available to the public while under review. California argued that it would undermine the state’s leverage in negotiations with insurers, and would reward dilatory conduct for those who wait until the last minute to file their potential rate increases. “(W)hen CDI raises concerns regarding a rate increase, after undertaking a thorough initial review, much of its ability to achieve favorable results for consumers rests on CDI’s ability to refrain from completing review of the filing until full information is provided and rate increases are moderated in compliance with CDI’ s requests. Each of the proposed changes noted above would have the effect of imposing a deadline for final rate determination that would undermine CDI’s negotiating leverage with health insurers, as insurers could refuse to respond to CDI’s requests until the deadline compelled the premature close of the rate review process. If, instead, the rate review process is allowed to proceed until CDI obtains a reduction in a proposed rate or rate increase, consumers receive a rebate for any higher charge in the bills for the early month of the next coverage year. Establishing a deadline early in the process would freeze the higher rate in place, rewarding insurer intransigence.” “CDI does not have the authority to disapprove rate filings, but only to determine whether proposed rates are ‘unreasonable.’ Although health insurers are required by law to provide CDI with information in support of their rate filings, many insurers are slow to do so,” California Insurance Commissioner Dave Jones writes in his comments. “There are even times when the rate negotiation between the insurer and the Department results in a rebate or credit on the first month’s bill, which is a better outcome for the policyholder than the Department being required by federal regulation to stop rate negotiation at an earlier point to the detriment of the policyholder.” But Connecticut’s state-run exchange enthusiastically supports the suggestions in its comment letter. “This proposed rule goes far in ensuring that non-marketplace plans cannot set their rates after looking at the rates for the marketplace plans which have been required to submit their rates earlier, thereby removing the unfair pricing advantage,” Access Health CT policy and strategy manager Chad Brooker writes. “Several QHP issuers in Connecticut have brought this “shadow pricing” to the attention of the Marketplace as well as the State Department of insurance. This requirement provides the necessary efforts to end these unfair activities that jeopardize issuer participation in Marketplaces.” The National Conference of State Legislatures urges CMS not to include the rate review provision in the final rule. “The imposition of new reporting timelines will require some states to make major changes in the way the[y] conduct business with their insurance carriers,” the group’s health and human services policy director, Joy Johnson Wilson, writes. “If CMS includes this provision in the final rule, we urge you to delay implementation until the 2017 plan year to permit states to make the necessary changes to forms and state timelines.” Comments on the proposed rule were due Dec. 22. Sources watching the proposal expect HHS to issue a final rule as early as late February or March. — Rachel S. Karas 12 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 FDA Urged To Further Clarify Framework For Regulating LDT Stakeholders are pushing for more clarity on key aspects of FDA’s proposed framework for regulating laboratory developed tests (LDTs), including how the agency will classify risks and harmonize its requirements with those of CMS. The issues came up at a public workshop held by FDA last week on challenges related to its proposed LDT framework, which has received backlash from the laboratory community as being a statutory overreach and burdensome. The agency laid out in draft guidance earlier last year its plan to apply the existing device classification system to LTDs over a nine-year implementation period. At the public workshop stakeholders urged FDA to release more guidance around the area of risk assessment. “It probably would be helpful if the agency would consider publishing... a document laying out a way risk should be assessed,” said Advanced Medical Technology Association Diagnostics Executive Director Andrew Fish. He raised concerns that everyone would have a different idea of what high risk is unless FDA provides more information in this area. FDA’s draft guidance explains that the agency will rely upon the existing medical device classification system to evaluate the risk of a category of LDTs and will use expert advisory panels to help classify devices not previously classified by FDA. “The entire framework is predicated on risk classification,” said Amy Miller, executive vice president of the Personalized Medicine Coalition (PMC). “I think there’s a lot of confusion about what is the highest risk, and about that line where the highest risk ends and where moderate risk begins.” Fish also suggested that advisory panels be convened for specific clinical areas and health conditions. “A bunch of risk considerations are situational,” said Fish. He also added that he supports the idea of allowing payers to provide input to the advisory panels, as these stakeholders are looking to FDA’s review to make a decision. Miller, in public comments, also pushed for harmonization between the CMS’ Clinical Laboratory Improvement Amendments requirements and FDA’s manufacturing recommendations. “Two large critical pieces of the framework are missing,” she said. “First, guidance on LDT risk classification, and second, harmonization between the CLIA program and FDA’s manufacturing recommendations.” She said these two pieces of information are substantial enough that the agency should release another draft, and recommended releasing the requested documents as a draft package as it would lead to more robust revision of the framework. Sheila Walcoff, CEO and founder of Goldbug Strategies LLC and prior senior counselor to the HHS secretary, also pushed for the harmonization between FDA and CLIA requirements, adding that where there is overlap, FDA should rely on previously existing CLIA requirements. FDA said it will consider several factors in determining the risk an LDT poses to patients, including: whether the device is intended for use in high risk disease/conditions or patient populations; whether the device is used for screening or diagnosis; the nature of the clinical decision that will be made based on the test result; whether a physician or pathologist would have other information about the patient to assist in making a clinical decision; the alternative diagnostic and treatment options available to the patient; the potential consequences or impact of erroneous results; and the number and type of adverse events associated with the device. — Erin Durkin Administration, State Officials Prep Public For Upcoming Tax Season Federal and state officials are preparing the public to include new information in their tax filings this year that will determine whether people must pay a fine for not buying insurance or owe the government money for receiving more premium tax credits than they deserved. On Tuesday (Jan. 13), California’s exchange issued a statement stressing that people who fail to purchase coverage will be subject to increasing tax penalties, HHS and the Treasury Department said this week that they are putting together resources to help Americans navigate the new filing rules, and CMS says it is distributing the new 1095-A tax forms by Feb. 2. Both HHS Secretary Sylvia Burwell and Treasury Secretary Jack Lew stressed in statements that the majority of Americas will simply need to check a box attesting that they have coverage, but some people will have to take further action. “For the vast majority of Americans, tax filing under the Affordable Care Act will be as simple as checking a box to show they had health coverage all year,” Lew said. “A fraction of taxpayers will take different steps, like claiming an exemption if they could not afford insurance or ensuring they received the correct amount of financial assistance. A smaller fraction of taxpayers will pay a fee if they made a choice to not obtain coverage they could afford. We are working to ensure that whatever their experience, consumers can easily access clear information since this is the first year they will see certain changes to their tax returns.” “In the coming weeks, HHS will work with other agencies, tax preparers and community organizations to arm these INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 13 consumers with the information they need to know as they prepare to file their taxes,” Burwell added. “We will also be providing helpful tools so that the millions of taxpayers who qualify for an exemption can receive one.” The departments stress that while including health insurance information will soon be a “routine step” in filing, this is the first year and there will be many questions. Those with marketplace coverage will receive a new form in the mail from the marketplace — Form 1095-A — that they will use to reconcile subsidies received upfront. CMS says it will distributing the 1095-A forms and filing instructions by Feb. 2. The information will also be posted on consumer’s online accounts, CMS says. State-based marketplaces must also send out the forms. Consumers who cannot afford coverage or meet other criteria can receive an exemption, the departments says. The administration recently broadened the exemptions that can be addressed via the tax filing process rather than having to apply through an exchange. Those who can afford coverage and opted not to purchase it will be required to pay a fee. HHS and Treasury noted that they are putting together resources for helping with tax filing and will partner with tax-preparation firms to spread the word. The administration will also be conducting direct outreach to enrollees, by phone, email and text, with personalized information most relevant to their tax status. “We will focus on providing targeted messaging to consumers who benefited from an advanced premium tax credit last year to help them offset the cost of their Marketplace premiums,” they write. The administration will also be providing guidance through community organizations, non-profits and exchange navigators and other assisters. Meanwhile, California’s exchange on Tuesday (Jan. 13) stepped up its messaging to consumers, stressing that they must purchase coverage by the end of open enrollment to avoid increased penalties next year. For 2014, consumer without coverage will be fined the greater of $95 or 1 percent of their income, and the fine increases to $325 or 2 percent of income for 2015, and to $695 or 2.5 percent of income for 2016. “It’s important that consumers understand now that the cost of remaining uninsured is rising,” Covered California Executive Director Peter Lee said. “This year, a family of four earning $70,000 a year could pay close to $1,000 in their taxes if they remain uninsured in 2015.” Because the tax filing deadline occurs after the open enrollment deadline, several stakeholders have been urging HHS to create a special enrollment period for those who realize after the fact that they may be on the hook for a penalty in 2015 — yet have no recourse. Rachel Klein of Families USA says her group discussed the idea with HHS several times, including in various comment letters, but has yet to hear whether the department will take action. Families’ is hopeful that HHS will create the SEP, however, because it makes a lot of sense, she says. But, she adds, it is likely that HHS would not make any announcements until the close of open enrollment. An HHS spokesperson had no comment on the potential SEP. Illustrating the potential confusion, a recent Harris Poll sponsored by Turbo Tax found that while about twothird of Americans (66 percent) understood they would be subject to a penalty for failing to have health insurance, an overwhelming majority incorrectly believed they could purchase coverage by Dec. 31, 2014 in order to avoid the fine. The Affordable Care Act required most Americans to have coverage as of Jan. 1, 2014, although there is a three-month grace period. — Amy Lotven CMS Faces Another RAC Protest . . . begins on page one slowing down the process, the DME, home health and hospice RAC is the first of the new round of contracts to be awarded. Performant Recovery, which holds one of the current RAC contracts, protested CMS’ decision to award the contract to Connolly on Jan. 6, just days after it was awarded, according to the Government Accountability Office’s website. The protest will last until at least mid-April when protest information is due to the GAO. When asked about the rationale behind the protest, a lawyer for Performant Recovery had no comment. But a transcript of parent company Performant Financial’s November third quarter earnings call obtained from Seeking Alpha shows that the company believes they submitted a strong application for the contract to CMS. “Obviously, we believe we submitted a good response. We think our results are very strong in the program,” Performant Financial’s CEO Lisa Im said when asked about her confidence in Performant’s ability to win the DME, home health and hospice RAC contract. Im also said that Performant had the highest accuracy of the recovery auditors in the latest report to Congress. “So how confident are we? I think we’re as confident as we can be, but again, there were clearly other submissions to the RFQ, so we’ll have to wait and see,” Im said. One lobbyist following the issue said the rash of protests mean it could be a long time until providers and 14 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 suppliers see the program changes put forward by CMS implemented. But the lobbyist added that it seems CMS is doing the best it can to mitigate the delay in awarding the new contracts by extending a limited version of the current contracts. CMS originally proposed five changes to the program last February when the agency began winding down the RACs in preparation for new contracts. Then more changes were added Dec. 30 at the same time that CMS announced the new DME, home health and hospice RAC. The original changes include requiring the RACs to wait 30 days before sending claims to Medicare Administrative Contractors; requiring RACs to confirm receipt of discussion requests within three days; establishing separate limits on documentation requests for each hospital department; and requiring RACs to adjust the number of documents they request based on providers’ denial rates. The agency also said it would make RACs wait longer to collect fees. New changes include cutting the time for RACs to complete complex reviews, requiring RACs to review all provider and claim types, requiring a 95 percent accuracy rating for automatic reviews and an overturn rate of less than 10 percent at the first level of appeals, as well as some other changes that would mainly affect hospitals. All of the changes will take effect when the new contracts are awarded. Kim Brummett, vice president of regulatory affairs at the American Association for Homecare, said that the protest gives those affected by the changes to the RACs more time to figure out how those changes will apply to different types of suppliers and providers. She also said it will give suppliers more time to understand how the changes CMS has put forward will work in practice. Additional scrutiny of DME, home health and hospice providers and suppliers will also be postponed, Brummett noted. — Michelle M. Stein CMS Lets Schools Bill Medicaid For Some Free Health Services CMS sent a letter to state Medicaid directors saying that schools may now be reimbursed for some health services that up to now have been offered to Medicaid-enrolled students free of charge. Started in 1997, a CMS policy known as the “free care rule” barred Medicaid from reimbursing schools for health services offered to students for free. However, many groups asked CMS to overturn the rule because it discouraged schools from providing such services as vaccinations, health screenings and asthma care. Mary-Beth Malcarney, a professor with George Washington University’s school of public health and a member of the Childhood Asthma Leadership coalition, said the rule was having a particularly negative impact on schools in low income districts that are more likely to have a higher number of students enrolled in Medicaid and would not be able to rely on a wealthy tax base to otherwise fund such programs. “If a school can’t charge Medicaid, these programs are less likely to be offered, and that’s what we’ve seen over time,” Malcarney said. Ed Walz, vice president of First Focus, a children’s health advocacy group, and another member of the coalition that lobbied for the change, said schools are an important place for children to receive care for asthma and other diseases that need to be managed. “Children spend much of their day in school, and providing asthma management care in the school building means less time in the doctor’s office and more time in the classroom. But an obscure HHS policy, the so-called ‘free care rule,’ had effectively denied this care for children covered by Medicaid,” Walz said. The letter said schools may now start billing Medicaid for the Medicaid-enrolled students receiving treatment so long as the service is covered under the program and the school meets all federal and state provider requirements. —Rebecca Beitsch CMS’ Mental Health Parity Proposal Doesn’t Apply To All Medicaid The White House’s Office of Management and Review is reviewing a proposed rule to require parity of medical and behavioral benefits in Medicaid managed care plans, CHIP plans and plans that cover Medicaid-expansion populations. Advocates for mental health patients also want the regulation to apply to traditional Medicaid fee-for-service, which would require some states to pay for more residential care services, but CMS indicated in a letter to Medicaid directors that the rule would only apply to fee-for-service in the Children’s Health Insurance Program and in the Medicaidexpansion population. “This proposed rule would address the requirements under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) to Medicaid Alternative Benefit Plans (ABPs), Children’s Health Insurance Program (CHIP), and Medicaid managed care organizations (MCOs),” a summary of the proposal states. The law requires plans to offer equal benefits for behavioral and medical services. CMS finished a rule in November 2013 that applies the law to commercial plans and plans covered by the Employee Retirement Income Security Act. That rule, which HHS wrote with the Department of Labor and the Department of Treasury, did not apply to plans in Medicaid managed care, CHIP or Medicaid-expansion plans. Mark Covall, president and CEO of the National Association of Psychiatric Health Systems, said he hopes CMS will INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 15 require the same level of parity in this regulation as it did in the previous rule. He said there are two essential parts of the law: quantitative and nonquantitative limits. Quantitative limits are more straight-forward, such as limits on the number of days patients may stay in facilities and out-of-pocket costs. Nonquantitative limits deal with such policies as precertification. Covall said it is common for plans to place nonquantitative limits on behavioral health services, such as by requiring precertification for mental health and addiction services, while not limiting medical services in that same manner. Covall said it is important that the parity rules apply to Medicaid managed care because many states are turning to managed care for their Medicaid programs. Nevertheless, his group has been urging CMS to apply the law to Medicaid fee-for-service, too. Covall said the law does not specifically exclude Medicaid fee-for-service. Rather, it’s a technical matter: The mental health law amended the Health Insurance Portability and Accountability Act, which does not apply to Medicaid fee-for-service. However, a letter to Medicaid directors in January 2013 makes it clear that Medicaid fee-for-service is not covered under the proposed rule, unless states use fee-for-service for CHIP or to cover residents as part of expanding Medicaid. Covall said nonquantitative limits are the types of policies that managed care plans would use to manage patients. Still, scope of service is a type of quantitative limit that can be a problem in fee-for-service, such as when benefits are offered on the medical side that are not offered on the mental health side, and applying the law to fee-for-service would fix that, he added. — John Wilkerson More Hep C Rx Deals Expected . . . begins on page one managers and insurance companies are getting discounts on the drugs. However, the companies are not diclosing discount amounts so it’s difficult for others to determine the significance of the agreements. “We still don’t know if it’s really good news or marginally good news,” National Association of Medicaid Directors Executive Director Matt Salo said. Gilead first reached a deal with CVS Caremark, which was reported on Monday (Jan. 5). That deal covered Medicaid formularies, as well as Medicare and commercial plans, and Salo said states that use CVS might be content to let the company get the best price for them. For other states, the agreement opens the door for states to get steeper discounts, he said, although he did not know of states entering negotiations with Gilead or AbbVie just yet. CVS did not respond to questions about whether the pharmacy benefit manager received a discount from Gilead or whether it will restrict coverage of Harvoni. A spokesperson for Medicaid Health Plans of America said states will likely continue to struggle with the cost of hepatitis C medications and will have to continue restricting coverage to the sickest patients. “Our take on the deals is that they’re a good first step. We welcome the price competition — anything that will help bring the prices down. The bad part is, they’re starting at such astronomical levels that it’s barely going to make a dent.” MHPA Director of Marketing and Communications Joe Reblando said. Lynda Dee, a patient advocate at the Fair Pricing Coalition, said it’s better for patients to get Viekira Pak without restrictions than Harvoni with restrictions. Both Viekira Pak and Harvoni showed cure rates above 90 percent in clinical trials, but Harvoni and its predecessor Sovaldi have longer track records and Harvoni is a once-daily drug. Viekira Pak has a more complicated regimen of four to six pills daily and some patients must take it with ribavirin. Ribaviron does not make patients nearly as sick as interferon, which was part of hepatitis C drug regimens for decades until Harvoni was approved. However, it can lower red blood cell counts and fatigue patients. “It may be easier to take Gilead’s one pill once a day Harvoni, but what good is it if your insurance doesn’t cover it or has many so restrictions that it is essentially inaccessible unless you have cirrhosis,” Dee said. “AbbVie’s Viekira has very similar cure rates and should be much more accessible without the appalling prior authorization restrictions.” Jill Becher, a spokesperson for Anthem, said most people don’t show signs of hepatitis C infection before being diagnosed, and severe liver damage often takes decades to develop and does not occur in everyone who has the disease. “The newer hepatitis C drugs have been approved through the FDA breakthrough therapy process and tested in far fewer people than typical clinical trials, which means our knowledge is more limited on these drugs. Given the concerns and relative benefits and harms, it made more sense to wait to provide benefit coverage to treat the population with more limited effects of the infection until there has been broader use of the drugs and we know the long-term effects, potential harms and outcomes of the various alternative therapies,” Becher said by email. There will likely be several more deals to come, industry analysts said. Evercore ISI wrote in an investor note that it believes that Aetna, which has a long-term agreement with CVS, will make a deal with Gilead, too. The analysts say it’s not clear whether Aetna will make its own formulary decisions or follow CVS’ formulary changes. — John Wilkerson 16 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 FDA Guidance Agenda Doesn’t List Biosimilar Naming, Includes Labeling The controversial issue of biosimilar naming is seemingly absent from the FDA drug center’s 2015 guidance agenda as all signs point to the agency approving the first U.S. biosimilar by early March. The guidance agenda slates four biosimilar documents the agency plans to put out this year including one on labeling, but there is no mention of a guidance specifically on the naming issue. A high-level Avalere Health executive said the labeling guidance is likely to cover naming, but the head of an alliance that includes the Biotechnology Industry Organization says the labeling guidance will probably not resolve the naming issue. The agency’s Center for Drug Evaluation and Research listed guidance documents the agency plans to publish in 2015, naming four biosimilar guidances currently under development: Biosimilars: Additional Questions and Answers Regarding Implementation of the Biologics Price Competition and Innovation Act of 2009; Considerations in Demonstrating Interchangeability to a Reference Product; Labeling for Biosimilar Biological Products; and Statistical Approaches to Evaluation of Analytical Similarity Data to Support a Demonstration of Biosimilarity. While the guidance detailing the labeling of biosimilar products may reference naming, Alliance for Safe Biologic Medicines Executive Director Michael Reilly said that labeling is a separate issue and will likely not resolve the naming debate. “I view naming as a larger policy issue that hasn’t been resolved, and labeling as more of a regulatory issue,” Reilly said. But Gillian Woollett, senior vice president of Avalere Health, said she expects FDA’s labeling guidance to include naming, and points out that the term “name” is not used in the Biologics Price Competition and Innovation Act. She noted that the agency isn’t obligated to release naming guidance under the statute. “The Agency has never committed to a naming guidance,” she said. Reilly said that FDA’s stance on naming will have a more global implication, whereas its approach to labeling of biosimilars will have a smaller impact. The issue of labeling addresses what information is needed to assist physicians and patients, Reilly said, adding that labeling will likely become a bigger debate, but has so far not gotten as much attention. The agenda was released released Tuesday (Jan. 6) on the eve of an FDA advisory panel meeting over the first biosimilar application, Sandoz’s filgrastim, the potential approval of which may signal FDA’s position on naming as well as other issues, according to sources. CBER’s Oncological Drug Advisory Committee recommended Wednesday (Jan. 7) that the agency approve Sandoz’s product as the first biosimilar in the United States. Industry, physician and patient stakeholders have weighed in on whether biosimilars should share international nonproprietary names (INNs) with their reference products, or have distinguishable names. The innovator biologics industry has advocated distinct names but others, including an American Medical Association council and the Generic Pharmaceutical Association, have argued for shared INNs. “Any change in current nomenclature rules or standards should be informed by a better and more complete understanding of how such changes, including requiring a unique identifier for biologic [United States Adopted Names] would impact prescriber attitudes and patient access, and affect post marketing surveillance,” said AMA’s Council on Science and Public Health in recommendations to the group to urge for FDA to finalize its guidance. “Actions that solely enhance product identification during surveillance but act as barriers to clinical uptake are counterproductive.” Over the summer the World Health Organization unveiled a naming scheme that would add biological qualifiers — an alphabetic code — to the INN. Stakeholders pushing back against the idea of a shared INN had said such a scheme would imply interchangeability and that distinct names are needed to track adverse events. — Erin Durkin SUBSCRIPTIONS: 703-416-8500 or 800-424-9068 custsvc@iwpnews.com NEWS OFFICE: 703-416-8577 Fax: 703-416-8543 insidecms@iwpnews.com Health Group Publisher: Senior Health Group Editor: Chief Editor: Associate Editor: Contributing Editors: Donna Haseley (donna.haseley@iwpnews.com) John Wilkerson (jwilkerson@iwpnews.com) Michelle M. Stein (mstein@iwpnews.com) Rebecca Beitsch (rbeitsch@iwpnews.com) Amy Lotven (alotven@iwpnews.com) Rachel S. Karras ( (rkarras@iwpnews.com) Production Manager: Production Specialists: Lori Nicholson (lori.nicholson@iwpnews.com) Daniel Arrieta, Michelle Moodhe Inside CMS is published every Thursday by Inside Washington Publishers, P.O. Box 7167, Ben Franklin Station, Washington, DC 20044. Subscription rates: $705 per year in U.S. and Canada; $755 per year elsewhere (air mail). © Inside Washington Publishers, 2015. All rights reserved. Contents of Inside CMS are protected by U.S. copyright laws. No part of this publication may be reproduced, transmitted, transcribed, stored in a retrieval system, or translated into any language in any form or by any means, electronic or mechanical, without written permission of Inside Washington Publishers. INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 17 Re-Pricing Letter Could Be First Of Its Kind . . . begins on page one up with more uniform rules for Part B reimbursement and to reduce Medicare Administrative Contractors’ authority at the local level. According to the brief filed on behalf of Alabama Pain Center, the company had been working with Medicare Administrative Contractor Cahaba and getting guidance on billing since 2008. In 2013, Alabama Pain Center received a local coverage article (LCA) from Cahaba setting a new fee schedule for the compounded drugs they administer. In 2014, Alabama Pain Center was investigated by AdvanceMed, a Zone Program Integrity Contractor that concluded Cahaba had overpaid for the drugs over a four-year span. After much back and forth, AdvanceMed said a re-pricing of the drugs was underway and later alleged the company owed about $25 million based on a review of about 60 claims. Hoover said it is unconstitutional and violates rulemaking for the government to apply the new prices set forward in the LCA or re-pricing letter retroactively. Hoover also argues the re-pricing letter is a substantive rule and should have been subject to prior notice and comment. Others in the compounding world have said they haven’t seen a case like this before. Trunk, a partner at Arent Fox who specializes in drug pricing, said this is her first time seeing retroactive pricing. The Alabama Pain Center makes and administers these drugs in their office and bills them under Medicare Part B. Trunk said Part B is a section of Medicare in which reimbursement rules might be less clear for compounded drugs than for drug prices under Part D, especially given that the center is mixing drugs with potentially different prices. Trunk said Hoover gave a solid argument that what CMS did could not be applied retroactively, but regardless of how the case turns out, she thinks it could lead to some changes. “This may ultimately lead to CMS coming up with more uniform national rules on the Part B side,” she said, possibly modeling the rules after Part D and giving less authority to MACs on the local level. The International Academy of Compounding Pharmacists said the group is not involved in the case, but sees disparities in which entities can bill Medicare for compounded drugs. —Rebecca Beitsch Vit als: A Vitals continued on next page Health P olicy Blog Po Excerpts of Inside Health Policy Blogs Childhood Asthma Leadership Coalition Pushes To Continue CHIP The Childhood Asthma Leadership Coalition is urging congressional CHIP payment advisors to extend the Children’s Health Insurance Program beyond its September 2015 expiration date. The coalition — comprised of different asthma groups, child welfare groups and health advocates — argued that other health programs don’t sufficiently deal with childhood health problems or are too expensive for families. In a recent letter to Medicaid and CHIP Payment and Access Commission, the coalition said that 2 million children stand to lose coverage as they would not fall under Medicaid. The group further argues that CHIP not only provides a more affordable option for low-income families but also provides children with better health care that is more specific to their needs. The letter says CHIP not only provides better asthma coverage to a population with a “greater burden of the disease” but is also more generous with coverage of other treatments like speech pathology. The alternatives are more expensive and offer poorer quality care, the coalition says. CHIP tends to cost around $60 a year for the poorest families that qualify for CHIP whereas plans in the exchange would cost about $450 a year. Due to the ACA’s so-called “family glitch,” the coalition also is concerned children may go without coverage. The glitch blocks spouses and children from access to exchange subsidies if a parent has an offer of coverage that is consid- 18 ered affordable for the individual, even if it is not affordable for the family. – Rebecca Beitsch Issa Reintroduces Bill That Would Replace ACA By Allowing FEHBP For All Rep. Darrell Issa (R-CA) on Tuesday (Jan. 6) introduced the Access to Insurance for All Americans Act, his second shot at a bill that aims to replace the Affordable Care Act with the national health program run by the Office of Personnel Management (OPM) and offer all U.S. citizens the same health care already held by federal employees. Unlike the ACA, Issa’s plan lacks an individual mandate and does not offer consumers federal subsidies to help defray the costs of buying coverage, though private employers could subsidize their employees’ premium costs. The bill would expand the Federal Employee Health Benefits Program, a federally run private insurance market available nationwide that includes most major insurers and a range of 300 plans. It’s not a new idea: Issa floated the same bill, cosponsored by Rep. Kerry Bentivolio (R-MI), in 2013 before it died in committee. “Affordable, high quality, private plans can be offered to Americans without mandates, new taxes, bureaucratic hurdles, or adding to our deficit,” Issa said in a release Wednesday (Jan. 7). “We should repeal the President’s healthcare law and replace it with reform that is patientcentered where you control your personal health decisions, not Washington.” Issa touts his bill as giving Americans guaranteed INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 access to coverage at the same rate regardless of health status, pre-existing conditions or age, without the narrow networks included in many Obamacare plans. Consumers would have the same ability to choose a plan that best fits their needs based on cost and coverage. He also proposes that private employers could subsidize their employees’ premium costs. Though the plan could potentially provide a back-up if the Supreme Court rules against the administration in the King v. Burwell lawsuit and eliminates subsidies for residents using federally-run exchanges, experts disagree on whether the bill would work as envisioned. In a 2009 RAND Corporation report, health expert Rachel Effros wrote that making tax credits available in order to purchase a FEHBP plan “may risk the crowd-out of some kinds of employer-sponsored coverage, if employers decide to drop coverage because of the availability of an alternative subsidized mechanism for employees to purchase health insurance.” “If individuals move from employer-sponsored coverage with some tax subsidization to the individual market with even larger subsidies, the subsidy may end up only slightly reducing the number of uninsured for a very high price,” she said in the report. Effros added that “(e)stimates of the magnitude of the effect depend heavily upon assumptions about the cost of premiums, the extent to which premiums would be subsidized, uptake levels by both the uninsured and those currently insured, and health spending changes with the provision of insurance.” Plans in the federal program are “generous and therefore expensive,” she noted, which would limit enrollment if no subsidies are offered. Other experts contend that if FEHBP is opened to everyone, prices are likely to increase for its current enrollees — resulting in higher premiums for all. OPM declined to comment as the legislation is still subject to change. – Rachel S. Karas HHS Officials Join Enroll America Calls Aimed At Encouraging Latino Enrollment Key HHS officials are scheduled to join Enroll America in back-to-back press calls, the first in Spanish and the second in English, as part of a push to encourage Latino enrollment in the health insurance exchanges. The calls took place Wednesday (Jan. 14), one day before the Jan. 15 deadline for coverage effective Feb. 1, and a month prior to the Feb. 15 close of open enrollment. Mayra Alvarez, director of the State Exchange Group at the Center for Consumer Information and Insurance Oversight (CCIIO), joined the Spanish-language call, while HHS Secretary Sylvia Burwell participated in the English version. The calls are a part of a “National Latino Week of Action,” and come as the administration has made outreach to Latinos, who face the largest rate of uninsured, a key goal for the second open enrollment. According to a Gallup survey out last week, Hispanics still have a high rate of uninsurance (32.4 percent), but the rate has dipped by 6.3 percentage points since the fourth quarter of last year. – Amy Lotven House Passes Bill To Amend Full-Time Work Definition To 40 Hours The House Thursday (Jan. 8) passed the “Save American Workers Act,” a proposal that would change the Affordable Care Act’s definition of full-time work from an average of 30 hours a week to 40-hour workweek for the purpose of the employer mandate. The 252-172 vote fell almost entirely along party lines, with 12 Democrats favoring the bill and no Republicans opposing the measure. Business advocates applauded the bill’s passage as a move needed to improve the economy and boost employment. “We commend the House’ action today and fully support the legislation,” Brian Marcotte, president and CEO of the National Business Group on Health, said in a statement. “We believe this change will boost employment, increase opportunities for people working part-time to add hours, and help the economy, particularly for smaller employers and those employers in retail, hospitality and other service industries.” The Senate is considering a twin bill sponsored by Sens. Susan Collins (R-ME) and Joe Donnelly (D-IN). The White House first leaned toward compromising on the measure, but will now fight hard to prevent its passage after the Congressional Budget Office released new numbers that project enactment of the measure would increase the federal deficit by $53.2 billion from 2015 through 2025. CBO also says the bill would increase the number of uninsured people by fewer than 500,000. President Obama has threatened a veto should the measure reach his desk. “Today, House Republicans are unfortunately showing once again that they would rather focus on partisan political fights than on helping our economy grow and create jobs,” Sen. Patty Murray (WA), the health committee’s top Democrat, said in a statement. “It’s shocking that with so many workers and families struggling, House Republicans are putting forward legislation that would deny workers the health care coverage they depend on and encourage companies to game the system by cutting time for the millions of workers who put in 40 hours a week. The last thing any worker wants is a smaller paycheck and higher health care costs — so Republicans are going to have a lot of explaining to do.” – Rachel S. Karas Five New Democrats Tapped For House Energy And Commerce Committee The House Democratic Caucus named five new members to the House Energy and Commerce Committee during the first week of the congressional session. Yvette Clarke (NY), David Loebsack (IA), Kurt Schrader (OR), Joseph Kennedy, III (MA) and Tony Cárdenas (CA) are the new Democrats on the panel. Of the five, Cárdenas, Kennedy and Schrader — along with Doris Matsui (CA) and Ben Ray Lujan (NM) — will join the health subcommittee that oversees food and drug policy, as well as FDA oversight. Schrader is co-chair of the New Democratic Coalition Caucus’ Health Care Task Force, which is charged with “the successful implementation of health care reforms that will expand access to and affordability of coverage, improve quality and delivery of care and slow the rate of growth in health care spending,” according to the task force’s mission. – David Hood INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 19 Klobuchar Reintroduces Gov’t Drug-Price Control Bill Sens. Amy Klobuchar (D-MN) and Tim Kaine (D-VA) introduced Wednesday (Jan. 7) a bill that would give the HHS secretary power to directly negotiate with drug makers the price of pharmaceuticals under Medicare. Klobuchar introduced similar legislation in past sessions of Congress, when Democrats controlled the Senate, and those bills did not gain traction. The bill would undo a provision that was part of the GOP-sponsored 2003 law called the Medicare Prescription Drug, Improvement, and Modernization Act, which created the Medicare prescription drug benefit called Part D. Although hepatitis C drugs Sovaldi and Harvoni made waves last year with their price, most lobbyists do not expect a Republican-controlled Congress to entertain government price controls this year. Sens. Richard Blumenthal (D-CT), Angus King (I-ME), Bernie Sanders (I-VT), and Jeanne Shaheen (D-NH) cosponsored the bill. – John Wilkerson Leavitt Partners White Paper Examines Possible Post-King Scenarios A Supreme Court ruling against the administration in the high-profile King V. Burwell case would place Republicans in a precarious position of winning their bid to unravel Obamacare but also facing consumers losing healthcare, and if Congress does decide to act following such a ruling the GOP could work to extract concessions from the administration as part of a replacement plan, according to one post-decision scenario put forth by consulting firm Leavitt Partners in a white paper out Monday. The paper outlines several scenarios that Congress, the states and the administration could take should the court rule that ACA subsidies cannot flow through exchanges established by the states, while noting that it is unlikely lawmakers and the administration will reveal any contingencies until later this year. “The impact that the King v. Burwell case could have on ACA implementation is not lost on anyone,” Leavitt writes. “The Obama administration has undoubtedly started planning for potential contingencies under possible King outcomes. However, with a new Republican majority and months to go before a King ruling, we do not expect to learn about these contingency plans until well into 2015,” Leavitt Partners writes. The court is slated to hear oral arguments on March 4, and a decision is expected in late June. Republicans who have “tied their own hands” by their outspoken antagonism toward the law, have a couple of options should SCOTUS rule for King, the paper says. The first, least complex and least likely option would be for the GOP to amend the law in a way that firmly establishes the subsidies were meant for all Americans regardless of who establishes an exchange. The optics of this “rescue” would be poor for a political party that has voted more than 30 times to repeal the law, the paper says. The second “slightly more plausible” scenario would see Congress pairing a long or short-term fix to the ACA with “material concessions” from Democrats on other parts of the ACA. Leavitt Partners says such concessions could address the employer mandate, thresholds related to the premium tax credits, risk corridors, medical device tax repeal, Independent Payment Advisory Board repeal, more stringent security and income verification or more flexibility for states on marketplace infrastructure. “Seeking concessions and changes in policy at the national level and punting marketplace decisions to the states would grant Republicans the ability to eliminate unpopular provisions, chair state’s rights and afford states a chance to adopt ideal solutions for their respective marketplaces,” Leavitt writes. A third scenario could see GOP members taking no action, but this could run some risk and could be perceived as political “brinkmanship,” similar to the 2011 debt ceiling crisis that was blamed on the GOP and resulted in little gain, Leavitt says. Should Congress take no action, it would fall to the states, the paper says. There are a number of contingency plans that would be available, yet each option varies on the timing needed for implementation, costs and state political obstacles. The administration has yet to announces any planning or flexibility in the state exchange criteria. Although the administration publicly says it expect SCOTUS will side with it, the consequences of a losing the subsidies are so significant that CMS will be expected to have options available, the firm suggests. Leavitt suggests several fall-back ideas that may be under consideration by the administration. Under the first, HHS would be a “technology administrator” and endorse a hybrid state-based marketplace that allows FFM and partnership states to use the FFM technology platform, but requires states to assume or retain ownership of the other marketplace functions. This would require a clearer definition of a state exchange. CMS does have some discretion, and “we believe that CMS would be wiling to re-evaluate the anatomy of what has been considered a statebased marketplace to date,” Leavitt writes. Relying on regional marketplaces, in which several states gets together under one marketplace, is another option and several states had indicated an interest in the idea — which is allowable under the law. However, the politics and decision 20 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 points involved with setting up such an exchange would be tedious and time consuming. Another idea would be for states to utilize existing marketplace technologies. States could adopt a “multi-tenant shared service marketplace solution” that allows two or more states to roll out the exchange technology platform and finance the costs through user fees. Unlike the regional market, this “marketplace as a service” (MaaS) scenario would provide states with autonomy and control of their exchanges. Key benefits of this model would be faster and more reliable implementation as well as lower costs. The ACA also created “innovation waivers” that allow states to deviate from the ACA as long as they continue to support its core goals. States could move in that direction, however, any plans must be approved by CMS and the waivers do not take effect until 2017, Leavitt points out. The paper stresses that any costs would be a major issue for most of the affected states. CMS could offer a new funding opportunity, but it is unlikely that a GOP-led Congress would appropriate the funding. States could require a fee, but that may be unpopular, and Leavitt notes that CMS officials have indicated that the federal marketplace is “barely sustaining itself” under the 3.5 percent user fee. For this reason, “we should not expect CMS to lower the cost of providing this technology.” Timing is also an obstacle, the paper says. SCOTUS is expected to rule in late June, while the next open enrollment period is set to start in October. The time needed to establish a new marketplace would be contingent on CMS criteria As far as state reactions, Leavitt places the affected states into four camps. The first is states with an existing plan to transition to a state-based exchange, and that category includes only two states: Arkansas and New Mexico. Then there are states that may take proactive steps toward an SBM, which includes Delaware, Illinois, Iowa, New Hampshire, Pennsylvania, Virginia and West Virginia. The third camp includes states that may do some research on necessary steps to create an SBM. These states have been opposed to the law, but are either moderate enough or have populations large enough that the loss of the subsidies could disrupt their individual markets, Leavitt writes. These states are: Alaska, Arizona, Georgia, Maine, Michigan, Missouri, Montana, Ohio, South Dakota and Tennessee. The remaining FFM states are likely to “dig in their heels” and would seek concessions from the administration prior to any actions. The list includes: Alabama, Florida, Indiana, Kansas, Louisiana, Mississippi, Nebraska, New Jersey, North Carolina, North Dakota, Oklahoma, South Carolina, Texas, Utahn, Wisconsin and Wyoming. — Amy Lotven Court Blocks CMS From Recouping Children’s Hospitals’ Medicaid DSH A federal district court of D.C. last week (Dec. 29) blocked CMS from recouping Medicaid Disproportionate Share Hospital payments from two children’s hospitals that sued the agency because of changes to Medicaid DSH reimbursement rules as the case proceeds. Some following the issue say that if the suit is successful — and the judge’s opinion on the preliminary injunction says the case is likely to succeed — it could limit what types of changes to rules CMS can make through Frequently Asked Questions documents or other sub-regulatory guidance. Two children’s hospitals sued HHS because they allege CMS used a FAQ to change Medicaid DSH reimbursement rules to count private insurance payments made on behalf of those eligible for Medicaid against a hospital’s DSH payments. Children’s hospitals may treat severely ill children who qualify for Medicaid not because of their parents’ economic status but because of their specific disease or condition. CMS said in an FAQ that private insurance payments to hospitals for these children’s care counts against a hospital’s Medicaid DSH payment when the agency calculates the limit to how much DSH money a hospital can receive, even though Medicaid never paid for care. CMS released a final rule in 2008 requiring that states provide an annual report and audit of its DSH program, including verification that states’ payments to each DSH hospital are not more than the “total annual uncompensated care costs” for such hospitals, or the hospitals’ specific DSH limits. One analyst following the issue said that hospital specific limits on DSH were meant to make sure hospitals aren’t making money off of DSH payments, but added that children’s hospitals aren’t really making money off DSH. The FAQ on the rule indicated that auditors should also take private insurance payments into account when calculating the hospitals’ limits, but BakerHostetler attorney Susan Feigin Harris said in an article written for the American Health Lawyers Association last year that for reimbursement purposes “the term ‘dual eligible’ patients has not been defined as patients that qualify for Medicaid and private health insurance ever before and no similar definition exists in any federal or state law.” The court on Dec. 29 granted a preliminary injunction to two children’s hospitals suing CMS to stop the agency from recouping DSH money from 2011. The Texas Children’s Hospital was expected to repay $21.7 million and Seattle Children’s Hospital would have needed to return $7 million in reimbursements they received for 2011 DSH above their hospital specific limit, according to BakerHostetler. Part of the hospitals’ argument against CMS’ Medicaid reimbursement rule and FAQ is that CMS changed the final INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015 21 rule significantly with the FAQ recharacterizing private insurance payments as Medicaid dollars, and it did so without going through the necessary notice-and-comment rulemaking process. CMS is testing the limits of what it can do with sub-regulatory guidance in this instance, the analyst said. If CMS can make changes to a rule through this type of guidance, that could be a problem for any hospital that relies on rulemaking, the analyst said. “The parties agree that the defendants have a policy of requiring the inclusion of private-insurance for Medicaid services in the calculation of a hospital-specific limit, but they disagree on the legal basis for that policy,” the judge says in his opinion granting the preliminary injunction. “The defendants maintain that FAQ 33 is not the source of the policy, but it took some time for them to identify what is the source. During the December 8, 2014 status hearing, the government could not do so” (emphasis theirs). The opinion notes CMS now says the 2008 rule provides the basis for its policy, but the judge says that “(a)lthough the defendants claim that the Rule supports them, they largely ignore its text in favor of selected portions of its Preamble.” The opinion says the hospitals’ case is likely to succeed on its merits. “Children’s hospitals provide a disproportionate share of services to critically ill Medicaid program patients. Eliminating their payments arbitrarily and recharacterizing private insurance payments as Medicaid payments should be vetted by Congress and the health care community, rather than slipped through a frequently asked question on a website,” said Feigin Harris in a statement on the judge’s preliminary injunction. One lawyer following the issue says a number of hospitals are likely affected by CMS’ change to the Medicaid DSH hospital specific limits, but it’s unclear which providers are affected or if they are aware they could have been subject to the recoupment without the injunction. Hospitals must have a perfect storm of circumstances to be affected — it depends on how a state calculates its DSH payments, which are set through a Medicaid state plan amendment, and it depends on the number of patients hospitals treat who are eligible for Medicaid but have private insurance and high costs in a given year. The latter could fluctuate year to year, the lawyer said, and could be affected by a small number of very sick children. Feigin Harris says in her article for the American Health Lawyers Association that the children’s hospitals are not opposing the few instances where Medicaid might have been billed after another insurer paid, but they “have fought what appears to be a disconnect, both at the state and CMS level,” in understanding that. The lawyer says private insurance in some instances pays more for severely ill children than it has in the past since the Affordable Care Act lifted yearly limits on insurance coverage. — Michelle M. Stein AIDS Advocates To HHS: Take Action Against High-Cost Drug Tiers The health advocates who filed a discrimination complaint six months ago against four qualified health plan (QHP) issuers in Florida for placing certain drugs in higher cost tiers are urging HHS’ Office for Civil rights to take immediate action on their case. AIDS Institute and the National Health Law Program (NHeLP) say in a Jan. 8 letter to OCR that while they appreciate that HHS recently indicated it will be monitoring the discriminatory behavior, the OCR should send a stronger message that discrimination will not be tolerated. Last May, the groups filed the complaint against Coventry One, Cigna, Humana and Preferred Medical charging they had unlawfully discriminated against people with HIV/AIDS by placing all HIV drugs — even generics — on high-cost tiers. Since then three of the four issuers have reached agreements with Florida’s insurance office to limit the cost of the drugs. However, the AIDS Institute and NheLP point out that the agreements are only with the state Florida and do not address the underlying complaint. Additionally, the groups point out that in reviewing QHPs offered in 2015, the same plans continue to place HIV drugs in high-cost tiers and many other plans are doing the same. The advocates further say that while they appreciate that HHS says in its proposed 2016 Notice of Benefits and Payment Parameters that plans placing most or all drugs used to treat a certain condition on a high-cost tier violates the ACA non-discrimination requirements, such language neither has the force of law nor compels issuers to stop those practices. “The ACA was designed to remedy this very situation, by prohibiting health insurers from discriminating against persons who need health care the most,” they write. “We urge you to take action on our pending complaint without further delay and to send a clear message to health insurance companies that discriminatory practices must end,” they add. — Amy Lotven 22 INSIDE CMS — www.InsideHealthPolicy.com — January 15, 2015
© Copyright 2024