Cesare Polito, Angela La Manna, Giuseppe Signoriello and Antonio Marte
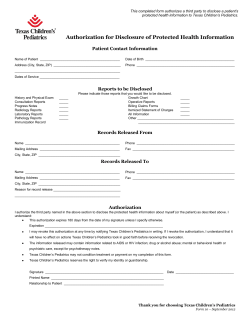
Recurrent Abdominal Pain in Childhood Urolithiasis Cesare Polito, Angela La Manna, Giuseppe Signoriello and Antonio Marte Pediatrics 2009;124;e1088; originally published online November 9, 2009; DOI: 10.1542/peds.2009-0825 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://pediatrics.aappublications.org/content/124/6/e1088.full.html PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly publication, it has been published continuously since 1948. PEDIATRICS is owned, published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2009 by the American Academy of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 Recurrent Abdominal Pain in Childhood Urolithiasis WHAT’S KNOWN ON THIS SUBJECT: Flank pain, hematuria, and dysuria are considered the warning signs of urinary tract involvement in children with RAP. WHAT THIS STUDY ADDS: In children with RAP and urolithiasis, hematuria and dysuria are inconstant, and in children younger than 8 years of age, the abdominal pain is often central/diffuse. Infrequent pain attacks and a family history of urolithiasis are additional warning signs of urinary stones. AUTHORS: Cesare Polito, MD,a Angela La Manna, MD,a Giuseppe Signoriello, MD,b and Antonio Marte, MDa,c Departments of aPediatrics, bPublic Health, and cPediatric Surgery, Second University of Naples, Naples, Italy KEY WORDS urolithiasis, hematuria, dysuria, recurrent abdominal pain ABBREVIATION RAP—recurrent abdominal pain www.pediatrics.org/cgi/doi/10.1542/peds.2009-0825 doi:10.1542/peds.2009-0825 Accepted for publication Jun 12, 2009 Address correspondence to Cesare Polito, MD, Second University of Naples, Department of Pediatrics, Via L. De Crecchio 2, 80138 Naples, Italy. E-mail: cesare.polito@golfonet.it abstract OBJECTIVE: Our goal was to establish the clinical presentation and features of pain attacks in children with recurrent abdominal pain (RAP) and urolithiasis. METHODS: We compared the rate of previous appendectomy among 100 consecutive patients with that of 270 control subjects. We also compared the frequency of pain attacks with that reported by children with functional or organic gastrointestinal RAP. PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2009 by the American Academy of Pediatrics FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose. RESULTS: Fifty-three patients had no history of dysuria or gross hematuria, and only 35 had hematuria at the first visit; 41 patients were evaluated for urolithiasis only because of a family history of kidney stones associated with RAP. Twenty-nine patients had been previously hospitalized for abdominal symptoms. Sixteen patients and 4 control subjects (1.5%) had undergone a previous appendectomy (P ⬍ .0001). Two to 28 months before the diagnosis of urolithiasis, 37 patients underwent abdominal ultrasonography, which did not show urinary stones. Sixty-nine percent of subjects younger than 8 years of age had central/diffuse abdominal pain. The mean frequency of pain attacks was 4 to 9 times lower than in patients with functional or organic gastrointestinal RAP. CONCLUSIONS: Because of the inconstant occurrence of dysuria and hematuria, the location of pain in areas other than the flank, and the lack of calculi shown on imaging studies performed after pain attacks, the urologic origin of pain may be overlooked and ineffective procedures performed. The possibility of urolithiasis should be considered in children with RAP who have a family history of urolithiasis and/or infrequent pain attacks, even when dysuria and hematuria are lacking, and in younger children even when pain is not lateral. Pediatrics 2009; 124:e1088–e1094 e1088 POLITO et al Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES Abdominal pain is the presenting symptom in 50% to 76.9% of children with urolithiasis,1–5 and it may occur as acute/subacute or recurrent abdominal pain (RAP).3,6,7 RAP is common among children and adolescents and has been associated with ⬎100 different conditions.6,8 In most cases, however, no organic disease can be found, and most episodes of RAP are considered to be a functional disorder that affects gastrointestinal motility6,8 and is often associated with emotional disorders.9 Pediatric urolithiasis is associated with significant morbidity, particularly because stones tend to recur; thus, its occurrence should not be underestimated. Identification of the clinical hallmarks of urinary tract involvement is crucial in selecting those children with RAP who require focused evaluation of the urinary tract. The location of pain in the flank as well as hematuria and dysuria are considered the only warning signs indicating more indepth investigation of urinary tract involvement in children with RAP.6,10 To date, no study has addressed the frequency of pain attacks in children with urolithiasis. Here we report the results of an observational study on children with RAP and urolithiasis. The goal was to assess the frequency and location of pain attacks, the occurrence of hematuria and dysuria, the rate of previous inconclusive hospitalizations for abdominal symptoms, and the rate of appendectomy, which may reflect failure to detect the urologic cause and depict the severity and costs of RAP. ciuria and/or hyperuricosuria, most of whom had no urinary stones, have been published.11,12 We evaluated 100 white patients aged 3 to 18 years with RAP who were first diagnosed as having urolithiasis and were consecutively observed from October 1, 1999, to November 14, 2008, in our clinical setting, which is mainly devoted to pediatric nephrology/urology patients, but also cares for general pediatrics patients and lacks emergency service. Urolithiasis was defined as imaging identification of a calculus or documented calculus passage. Micturating cystography was performed on children with recurrent urinary tract infections or pathologic ultrasound findings, such as hypoplastic or dysmorphic kidneys or hydronephrosis, to determine the vesicoureteric reflux. Tc99m MAG3 dynamic renal scintigraphy was performed on children with hydronephrosis to determine ureteropelvic obstruction. We did not systematically search for other possible causes of RAP. However, we excluded subjects with another potential source of RAP, as well as those whose report of symptoms was unreliable. Data collection was prospective and formed the basis of this observational study. We obtained approval from our institutional ethics committee, as well as signed informed-consent forms from the children’s parents. METHODS RAP was defined as at least 3 episodes of diffuse or localized abdominal pain over a period of at least 3 months.13 The basic investigation protocol included a detailed medical history, physical examination, blood and urinary studies, and renal and urinary tract ultrasound scans. In 1999, we began a prospective observational study of the clinical presentation and outcome of children with urinary solute excretion abnormalities leading to urolithiasis. Some of the findings on participants with hypercal- The prevalence of appendectomy in the history of the patients under study was compared with that of a control group of 270 subjects, 142 of whom were boys, aged 3 to 18.5 years (mean: 8.6 [SD: 3.9]). The control subjects were PEDIATRICS Volume 124, Number 6, December 2009 consecutively observed for acute respiratory tract infection during a period of 2 years (2001–2003), and the previous history of appendectomy was specifically investigated by 1 of the authors (Dr Polito). We assumed that the prevalence of appendectomy in this group reflected the prevalence in the general population. All children and parents were questioned about the location and frequency of pain attacks. Evaluation during the first visit was performed by 2 of the authors (Drs Polito and La Manna) on 43 and 57 different patients, respectively. Hence, we compared the referred location of pain and the frequency of pain attacks recorded by the 2 independent observers in 2 different groups of subjects. The location of pain elicited on abdominal palpation by Drs Polito and La Manna was also compared. The frequency of attacks in our patients was compared with that reported in children with functional RAP from our region14 and from the United States,15 and with functional/psychosomatic or organic gastrointestinal RAP from Norway16 and Sweden.17 No specific attempt was made to consistently quantitate the severity of pain. However, the pain was considered to be significant if it caused the child to interrupt an ongoing activity to complain of pain or the child became inactive after verbalizing the symptom of pain. Hypercalciuria was defined as calciuria of ⬎0.1 mmol (4 mg)/kg per day, and hyperuricuria was defined as urinary uric acid exceeding 815 mg/1.73 m2 per day18 on at least 2 of 3 nonconsecutive 24-hour urine collections made at home. The adequacy of urine collections was checked by comparing the measured creatinine excretion with normal values. Hyperoxaluria was defined as oxalate excretion of ⬎40 mg/ 1.73 m2 per day and hypocitraturia as Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e1089 Patients with urolithiasis aged 3–18 y, observed during the study period (n = 188) l l Without RAP ----------------------------------------------------------------------------- With RAP (n = 78) (n = 110) Hematuria/dysuria: 36 l Acute/subacute pain l +hematuria/dysuria: 26 l………………Excluded Acute-subacute pain: 12 l Incidental discovery: 3 l Ureteropelvic obstruction: 3 Urinary infection: 1 l Vesicoureteric reflux: 1 l Renal cysts: 2 l l Stipsis: 2 (n = 10) Celiac disease: 1 Mental retardation: 1 l l l l Elected (n = 100) Outpatients: 78 Hospitalized: 22 FIGURE 1 Enrollment and election of the patients included in the study. citrate excretion of ⬍400 mg/g creatinine.18 Cystinuria was assessed with the nitroprusside test in all patients and confirmed by quantitative measurement in nitroprusside-positive patients. Hematuria was defined as ⱖ5 red blood cells per high-power field in a centrifuged urine sample or hemoglobin ⬎1⫹ at dipstick. The 2 test, the 2 test for trend, and the Wilcoxon rank test were used for statistical analysis. A P value of ⬍.05 was considered significant. RESULTS Figure 1 shows the enrollment and election of the patients included in the study. Table 1 lists the clinical characteristics of the study participants. The mean age was 9.8 (SD: 3.8) years. The mean duration of RAP before the first visit was 12.5 months (SD: 11.4 [range: e1090 POLITO et al 3–50]). The mean duration of pain attacks was 127 minutes (SD: 105 [range: 10 – 600]). Nine patients had a urinary infection at the first visit, and 2 had previous urinary infections. Serum electrolyte, calcium, phosphate, creatinine, uric acid, bicarbonate, and parathyroid hormone levels were normal in all patients. Internal Validation There was no significant difference in the referred central or lateral pain location (P ⫽ .45 for both subjects younger and older than 8 years of age) or in the frequency of pain attacks (P ⫽ .79) recorded by Drs Polito and La Manna. Pain on abdominal palpation was elicited by Drs Polito and La Manna in 27 and 18 subjects, respectively. There was no significant difference in the rates of central and lateral pain elicited by the 2 observers (P ⫽ .45 for both subjects younger and older than 8 years old). History A history of urolithiasis in at least 1 first- or second-degree relative was present in 88 subjects. Two to 28 months (mean: 11.8) before the diagnosis of urolithiasis, 37 patients underwent abdominal ultrasound examination, the results of which were negative for urinary stones; however, 15 patients had microcalculi,19 that is, hyperechogenic spots ⱕ3 mm in diameter in renal calyces, 5 patients had mild pyelectasis, and 2 patients had mild pyelectasis plus microcalculi. The ultrasound examinations were performed elsewhere in 25 cases and in our setting in 12. In the present analysis, we considered as the “first visit” of Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES % TABLE 1 Characteristics of 100 Children With RAP and Urolithiasis Characteristic 100 Lumbar/flank n Gender Male Female Referral diagnosis RAP Gross hematuria and/or dysuria ⫹ RAP Microhematuria ⫾ dysuria ⫹ RAP Stone locationa Upper tract Pelvic Staghorn Ureteral Documented passage Urinary excretion abnormality, mean of the abnormal values (range) Hypercalciuria, 5.5 (4.1–11) mg/kg per dc Hyperuricuria, 880 (844–1121) mg/1.73 m2 per dc Hypercalciuria, 6.3 (4.4–10) mg/kg per dc ⫹ Hyperuricuria, 946 (844–1086) mg/1.73 m2 per dc Mild hyperoxaluria, 98 (64–130) mg/ 1.73 m2 per d Hypocitraturia, 177 (75–305) mg/g creatinine Cystinuria No abnormality found Mainly hypogastric 42 58 Central/diffuse 49 36 15 50 82b 2 2 3 11 46 0 Age groups, y 3–8 8,1–13 13,1–18 18 N. of cases (35) (45) (20) Chi-square for trend p < 0.01 17 FIGURE 2 Prevalence of pain locations in 3 age groups. 2 for trend, P ⬎ .01. 5 4 2 8 a Associated with microcalculi in 57 patients. For imaging documentation of stones, renal ultrasound was used for all patients, plain radiograph film for 25 patients, and intravenous urography for 11 patients. b Bilateral in 5 patients. c Twenty-nine patients with hypercalciuria or/and hyperuricuria also had mild hyperoxaluria or/and hypocitraturia. the latter 12 patients the time when stones were first recorded. A history of appendectomy was recorded significantly more often among the subjects with urolithiasis (16%; P ⬍ .0001) than in the control group (4 of 270 [1.5%]). The 16 subjects with urinary calculi underwent appendectomy 1 to 48 months before our first visit. In 9 of the 16 patients, dysuria and/or gross hematuria occurred 3 days to 18 months (mean: 9.5 months) after appendectomy. In 2 of the 16 patients, microscopic hematuria was recorded 1 and 20 months after appendectomy at our first visit. One of the patients who underwent appendectomy also underwent a Meckel scan during another hospitalization. Four additional paPEDIATRICS Volume 124, Number 6, December 2009 tients had previously been hospitalized for possible appendicitis. Another 9 patients had been hospitalized at least once for abdominal pain: 1 underwent a Meckel scan, 1 underwent gastroscopy, and 1 underwent contrast radiography of the upper digestive tract and gastroscopy. A total of 29 of our patients had been hospitalized at least once for abdominal symptoms. Pain Among the 35 patients younger than 8 years of age, the referred location of pain was lateral/flank in 10 (29%), cen- tral/diffuse in 24 (69%) and mainly hypogastric in 1. Among the 65 patients older than 8 years, the pain was lateral/flank in 55 (85%), central/diffuse in 7 (11%), and mainly hypogastric in 3. A significant decrease in the prevalence of central/diffuse location of pain with increasing age is apparent, with the most relevant decrease after 8 years (Fig 2). The mean frequency of pain attacks was 4 to 9 times lower than that reported in children with functional or organic gastrointestinal RAP (Table 2). Eighty-four patients had 4 or fewer days of pain per month. TABLE 2 Mean (SD) Frequency of Pain Attacks in Children With RAP and Urolithiasis and in Four Studies of Functional or Organic Gastrointestinal RAP Study Disorder (No. of Patients) Mean Age, y Frequency, Mean (SD), d/mo Present series, Campania, Italy Miele et al,14 Campania, Italy Urolithiasis (100) Functional dyspepsia (26) Irritable bowel syndrome (26) Functional dyspepsia (14) Irritable bowel syndrome (11) Functional abdominal pain (14) Organic (20) and functional (24) gastrointestinal RAP Psychosomatic (48), possibly psychosomatic (14), other etiologies (38) 9.8 8.2 5.0 11.6 11.6 11.0 8.3 3.1 (4.0)a 12.4 (11.1) 15.6 (10.6) 23.9 18.1 17.2 11.9 (8.5) 9.5 19.8b Ball and Weydert,15 Arizona Størdal et al,16 Norway Alfvén,17 Sweden a b Median: 1.5; ⱖ9 days/month in 9 subjects; ⱖ7 days/month in 12 patients; range: 0.5–20. Calculated from the reported frequency of 4.6 attacks per week. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e1091 There was no significant difference in the frequency of pain attacks between boys and girls (P ⫽ .60), between subjects younger and older than 8 years (P ⫽ .24), or between subjects with central/diffuse and lateral/flank location of abdominal pain (P ⫽ .25). Hematuria and Dysuria Fifty-three patients had no history of dysuria or gross hematuria, and only 35 had gross or microscopic hematuria at the first visit. Forty-one patients had no history of hematuria or dysuria and normal urinalysis results at the first visit. Of the 47 patients with a history of gross hematuria or dysuria, 22 (47%) had no dysuria and normal urinalysis results at the first visit. Central/diffuse location of abdominal pain, with no history of dysuria and hematuria and normal urinalysis results at our visit were recorded in 16 of our patients and in 12 of 35 (34%) of those aged 8 years or younger. Of the 45 subjects with pain on palpation of the abdomen, as many as 32 (71%) had neither hematuria nor dysuria at the time of the visit. Of the 37 patients who had negative ultrasound results before the first diagnosis of calculi, 21 (57%) had no history of dysuria or hematuria and underwent additional follow-up investigations only because of a family history of nephrolithiasis. DISCUSSION Because of the lack of populationbased studies, we do not know how many children with RAP have urolithiasis. Moreover, authors of studies on children with urolithiasis have reported the rate of those presenting with abdominal/flank pain with no specification of the proportion of acute/ subacute and chronic-recurrent abdominal pain.1–5 The lack of emergency service in our department likely enhanced the proportion of those with recurrent pain in respect to those e1092 POLITO et al with acute/subacute abdominal pain. Therefore, the present series is not representative of the universe of children with urolithiasis. This study shows a low frequency of pain attacks in children with urolithiasis, which has not yet been reported in the literature. The mean frequency of pain attacks was 4 to 9 times lower in our patients than in children with functional or organic gastrointestinal RAP from our own and other countries. In contrast, the maximum difference in the frequency of attacks among the various kinds of functional or organic gastrointestinal RAP was less than twofold (Table 2). Hence, the low frequency of pain attacks clearly distinguishes the population of children with urolithiasis from those with functional or organic gastrointestinal RAP. We cannot establish definite cutoff values. In our series, however, the mean frequency of pain attacks was 3.1 days/ month, whereas the median was 1.5 days/month (Table 2). A frequency of pain attacks of 4 days/month or less may empirically suggest urolithiasis, which has even been indicated as an index of healing of functional RAP,15 whereas this frequency was recorded in as many as 84% of our patients. RAP occurs in up to 19% of all children and adolescents, with a median prevalence of 8.4%,8 and is most often functional.6,9,16,17 Therefore, it is likely that the remaining 16% of our patients with more frequent pain attacks included a number of subjects with functional RAP incidentally associated with urolithiasis. Gross or microscopic hematuria and dysuria are the main “red-flag” symptoms reported for involvement of the urinary tract in children with RAP.6,8 Nevertheless, these symptoms occurred inconstantly in our patients. In fact, half of our patients had no history of dysuria or hematuria, and more than one third had no history of dys- uria or gross hematuria and normal urinalysis results at the first visit. The latter were investigated for urolithiasis because of RAP associated with a family history of urinary calculi, which accounts for a high risk of kidney stones.20,21 Actually, more than half of our patients who had a negative ultrasound scan result before the first diagnosis of urolithiasis had no history of dysuria or hematuria and underwent additional follow-up investigations because of a family history of kidney stones. Moreover, approximately half of our patients with a history of hematuria or dysuria did not have these symptoms at the first visit. Finally, hematuria and dysuria did not necessarily correlate with pain; as many as 71% of our patients with pain elicited by abdominal palpation had neither hematuria nor dysuria at the time of the visit. Pain attacks, as well as hematuria and dysuria, likely result from the mobilization and passage of calculi or crystals. Hence, it is not surprising that the occurrence of these symptoms was largely intermittent or sporadic. Although no study has specifically addressed children with RAP and urolithiasis, the inconstant occurrence of hematuria and dysuria has been reported in many series of children with kidney stones.1–5,7 It is worth keeping this fact in mind, because the lack of occurrence of hematuria and dysuria in clinical practice may erroneously lead to exclusion of the urinary tract as a possible cause of pain. The drawback is that even in most scientific reports on RAP, the urologic origin of pain was excluded only on the basis of “normal urinalysis and/or urine culture or of the lack of overt genitourinary problems”10; similar guidelines were established by the Rome III Committee for Functional Gastrointestinal Disorders.22 A central/diffuse location of abdominal pain was prevalent among patients Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 ARTICLES younger than 8 years in our study, and flank pain was the rule in patients older than 8 years (Fig 2). This could reflect the development of sensory discrimination during childhood and is in keeping with the acquisition of body outline around the age of 8.23 We previously found similar results in children with hypercalciuria and/or hyperuricosuria, most of whom, however, had no urinary stones.11 When abdominal pain is central/diffuse and is not associated with dysuria and hematuria, as in 34% of our patients aged under 8 years, it might well mimic functional RAP. Imaging studies performed immediately after pain attacks may fail to reveal urinary calculi, because the stones could have been passed shortly before the evaluation. In fact, 2 to 28 months before the diagnosis of urolithiasis, 37% of our patients underwent abdominal ultrasound scanning that did not show urinary calculi. This is in keeping with reports that ⬎10% of children with hypercalciuria and/or hyperuricosuria and no demonstrable stones on first evaluation may form calculi within 1 to 4 years.19,24–26 Actually, in 15 of our 37 patients, ultrasound showed microcalculi that could be considered the first step in stone formation.19,24 The finding of microcalculi, however, depends on interobserver and intraobserver variability and skills, and microcalculi are not generally rec- ognized.27,28 The possibility of a falsenegative ultrasound scan or plain radiograph film in a subject with bowel distension caused by recent colic should also be taken into account. Lowdose unenhanced computed tomography is more accurate than ultrasonography in detecting calculi and has been recommended for all children with persistent urolithiasis symptoms and nondiagnostic ultrasound scans.28 Compared with ultrasound, however, computed tomography involves higher costs and radiation, which are significant issues in children with possible urolithiasis because of the frequent recurrence of this condition. The inconstant occurrence of hematuria and dysuria, the central/diffuse location of abdominal pain in most young children, and the lack of calculi shown on imaging studies performed after an episode of pain may result in failure to identify the urologic origin of pain. This could explain, for the most part, the high rates of previous inconclusive hospitalizations for abdominal pain (29%) and appendectomy in the present series. Actually, the prevalence of appendectomy in our control group (1.5%) is comparable to that estimated from a large survey in the United States29 and is significantly (P ⬍ .0001) lower than the rate (16%) for our patients. Searching for urolithiasis in children with RAP may be difficult and expensive. In fact, a negative imaging study result after a pain attack does not exclude the previous and/or subsequent occurrence of urinary stones and may need to be repeated later. This is particularly important in the presence of a urinary solute excretion abnormality such as hypercalciuria or hypocitraturia, which, in turn, may require repeated30 and costly31 evaluations to be ascertained. Moreover, despite an upward trend in incidence, overt pediatric urolithiasis remains infrequent in Western countries,5,28 whereas RAP is frequent. It seems advisable to perform at least 2 renal ultrasound examinations 1 to 2 years apart and 3 nonconsecutive complete evaluations of urinary solute excretion abnormalities in outpatient children with RAP and a family history of urolithiasis, even in the absence of specific urinary signs and symptoms, and in younger patients, although the pain may be central or diffuse in the whole abdomen. Computed tomography may be particularly useful in the emergency department after a nondiagnostic ultrasound scan. Restricting these investigations to patients with infrequent painful episodes (4 days/month or less) will help improve the cost/benefit ratio of this approach. 5. VanDervoort K, Wiesen J, Frank R, et al. Urolithiasis in pediatric patients: a single center study of incidence, clinical presentation and outcome. J Urol. 2007;177(6):2300 –2305 6. Pearl RH, Irish MS, Caty MG, et al. The approach to common abdominal diagnoses in infants and children: part II. Pediatr Clin North Am. 1998;45(6):1287–1326 7. Vachvanichsanong P, Malagon M, Moore ES. Recurrent abdominal and flank pain in children with idiopathic hypercalciuria. Acta Paediatr. 2001;90(6):643– 648 8. Chitkara DK, Rawat DJ, Talley NY. The epidemiology of childhood recurrent abdominal pain in Western countries: a systematic review. Am J Gastroenterol. 2005;100(8): 1868 –1875 9. Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety and depression in primary care. Pediatrics. 2004; 113(4):817– 824 10. Weydert JA, Ball TM, Davis MF. Systematic review of treatments for recurrent abdominal pain. Pediatrics. 2003;111(1). Available at: www.pediatrics.org/cgi/content/full/ 111/1/e1 11. Polito C, Cioce F, Signoriello G, et al. Central/ diffuse abdominal perception of urological pain in children. Acta Paediatr. 2006;95(1): 82– 85 CONCLUSIONS REFERENCES 1. Coward RJ, Peters CJ, Duffy PG, et al. Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child. 2003;88(11):962–965 2. Edvardsson V, Elidottir H, Indridason OS, et al. High incidence of kidney stones in Icelandic children. Pediatr Nephrol. 2005;20(7): 940 –944 3. Dursun I, Poyrazoglu HM, Dusunsel R, et al. Pediatric urolithiasis: an 8-year experience of single centre. Int Urol Nephrol. 2008; 40(1):3–9 4. Spivacow FR, Negri AL, Del Valle EE, et al. Metabolic risk factors in children with kidney stone disease. Pediatr Nephrol. 2008; 23(7):1129 –1133 PEDIATRICS Volume 124, Number 6, December 2009 Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 e1093 12. Polito C, Marte A, La Manna A. Appendectomy in children with hypercalciuria/ hyperuricosuria. J Pediatr Urol. 2005;1(4): 279 –292 13. Apley J, Naish N. Recurrent abdominal pain: a field survey of 1000 school children. Arch Dis Child. 1958;33(168):165–170 14. Miele E, Simeone D, Marino A, et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics. 2004;114(1):73–78 15. Ball TM, Weydert JA. Methodological challenges to treatment trials for recurrent abdominal pain in children. Arch Pediatr Adolesc Med. 2003;157(11):1121–1127 16. Størdal K, Nygaard EA, Bentsen B. Organic abnormalities in recurrent abdominal pain in children. Acta Paediatr. 2001;90(6): 638 – 642 17. Alfvén G. One hundred cases of recurrent abdominal pain in children: diagnostic procedures and criteria for a psychosomatic diagnosis. Acta Paediatr. 2003;92(1):43– 49 18. Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatr Nephrol. 2005; 20(11):1587–1592 e1094 POLITO et al 19. Polito C, La Manna A, Cioce F, et al. Clinical presentation and natural course of idiopathic hypercalciuria in children. Pediatr Nephrol. 2000;15(3– 4):211–214 20. Polito C, La Manna A, Nappi B, et al. Idiopathic hypercalciuria and hyperuricosuria: family prevalence of nephrolithiasis. Pediatr Nephrol. 2000;14(12):1102–1104 21. Curhan GC, Willett WC, Speizer FE, et al. Family history and risk of kidney stones. J Am Soc Nephrol. 1997;8(10):1568 –1573 22. Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–1537 23. Savedra MC, Tesler MD, Holzemer WL, et al. Pain location: validity and reliability of body outline markings by hospitalized children and adolescents. Res Nurs Health. 1989; 12(5):307–314 24. La Manna A, Polito C, Marte A, Iovene A, Di Toro R. Hyperuricosuria in children: clinical presentation and natural history. Pediatrics. 2001;107(1):86 –90 25. Stapleton FB. Idiopathic hypercalciuria: association with isolated hematuria and risk for urolithiasis in children. Kidney Int. 1990; 37(2):807– 811 26. Garcia LD, Miller LA, Stapleton FB. Natural history of hematuria associated with hypercalciuria in children. Am J Dis Child. 1991; 145(10):1204 –1207 27. Alon US, Berembom A. Idiopathic hypercalciuria of childhood: 4- to 11-year outcome. Pediatr Nephrol. 2000;14(10 –11):1011– 1015 28. Hiorns MP. Imaging of urinary tract lithiasis: who, when and how? Pediatr Radiol. 2008; 38(suppl 3):S497–S500 29. Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5);910 –925 30. Parks JH, Goldfisher E, Asplin JR, Coe FL. A single 24-hour urine collection is inadequate for the medical evaluation of nephrolithiasis. J Urol. 2002;167(4):1607–1612 31. Alon US, Zimmerman H, Alon M. Evaluation and treatment of pediatric idiopathic urolithiasis: revisited. Pediatr Nephrol. 2004;19(5):516 –520 Downloaded from pediatrics.aappublications.org by guest on August 22, 2014 Recurrent Abdominal Pain in Childhood Urolithiasis Cesare Polito, Angela La Manna, Giuseppe Signoriello and Antonio Marte Pediatrics 2009;124;e1088; originally published online November 9, 2009; DOI: 10.1542/peds.2009-0825 Updated Information & Services including high resolution figures, can be found at: http://pediatrics.aappublications.org/content/124/6/e1088.full. html References This article cites 30 articles, 7 of which can be accessed free at: http://pediatrics.aappublications.org/content/124/6/e1088.full. html#ref-list-1 Subspecialty Collections This article, along with others on similar topics, appears in the following collection(s): Urology http://pediatrics.aappublications.org/cgi/collection/urology_su b Permissions & Licensing Information about reproducing this article in parts (figures, tables) or in its entirety can be found online at: http://pediatrics.aappublications.org/site/misc/Permissions.xht ml Reprints Information about ordering reprints can be found online: http://pediatrics.aappublications.org/site/misc/reprints.xhtml PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly publication, it has been published continuously since 1948. PEDIATRICS is owned, published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2009 by the American Academy of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275. Downloaded from pediatrics.aappublications.org by guest on August 22, 2014
© Copyright 2025