CD64 distinguishes macrophages from dendritic
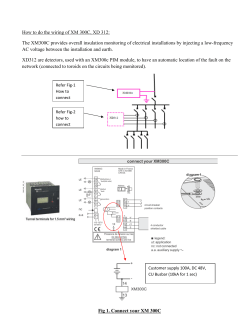
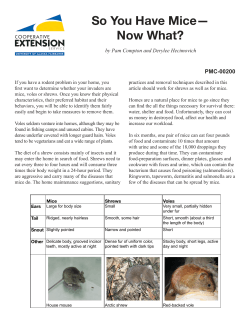
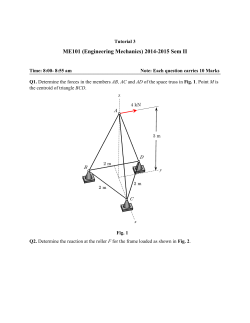
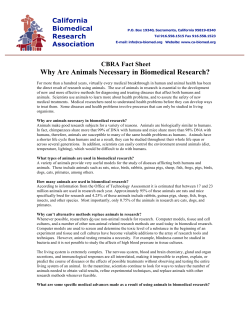
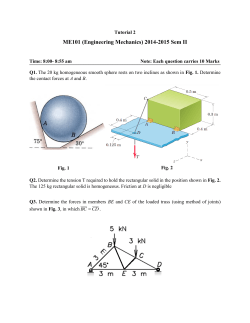
DOI: 10.1002/eji.201242847 Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Samira Tamoutounour∗1,2,3 , Sandrine Henri∗1,2,3 , Hugues Lelouard1,2,3 , B´eatrice de Bovis1,2,3 , Colin de Haar4 , C. Janneke van der Woude4 , Andrea M. Woltman4 , Yasmin Reyal5 , Dominique Bonnet5 , Dorine Sichien6,7 , Calum C. Bain8 , Allan McI. Mowat8 , Caetano Reis e Sousa9 , Lionel F. Poulin10 , Bernard Malissen1,2,3 and Martin Guilliams1,2,3 1 Centre d’Immunologie de Marseille-Luminy (CIML), Aix Marseille Universit´e, Marseille, France 2 INSERM U1104, Marseille, France 3 CNRS UMR7280, Marseille, France 4 Department of Gastroenterology and Hepatology, Erasmus MC University Medical Center, Rotterdam, The Netherlands 5 Haematopoietic Stem Cell Laboratory, Cancer Research UK, London Research Institute, London, UK 6 Department for Molecular Biomedical Research, VIB, Ghent, Belgium 7 Laboratory of Immunoregulation and Mucosal Immunology, Ghent University, Ghent, Belgium 8 Centre for Immunology, Institute of Infection, Immunity and Inflammation, University of Glasgow, Scotland 9 Immunobiology Laboratory, Cancer Research UK, London Research Institute, London, UK 10 Center for Infection and Immunity of Lille, Pasteur Institute of Lille, Lille, France Dendritic cells (DCs) and monocyte-derived macrophages (Ms) are key components of intestinal immunity. However, the lack of surface markers differentiating Ms from DCs has hampered understanding of their respective functions. Here, we demonstrate that, using CD64 expression, Ms can be distinguished from DCs in the intestine of both mice and humans. On that basis, we revisit the phenotype of intestinal DCs in the absence of contaminating Ms and we delineate a developmental pathway in the healthy intestine that leads from newly extravasated Ly-6Chi monocytes to intestinal Ms. We determine how inflammation impacts this pathway and show that T cell-mediated colitis is associated with massive recruitment of monocytes to the intestine and the mesenteric lymph node (MLN). There, these monocytes differentiate into inflammatory Ms endowed with phagocytic activity and the ability to produce inducible nitric oxide synthase. In the MLNs, inflammatory Ms are located in the T-cell zone and trigger the induction of proinflammatory T cells. Finally, T cell-mediated colitis develops irrespective of intestinal DC migration, an unexpected finding supporting an important role for MLN-resident inflammatory Ms in the etiology of T cell-mediated colitis. Keywords: CD64 r Colitis r Dendritic cells r Intestine r Ms Supporting Information available online Correspondence: Dr. Bernard Malissen e-mail: bernardm@ciml.univ-mrs.fr C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim ∗ These authors contributed equally to this work. www.eji-journal.eu Frontline CD64 distinguishes macrophages from dendritic cells in the gut and reveals the Th1-inducing role of mesenteric lymph node macrophages during colitis 1 2 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 Introduction Results The intestinal lamina propria (LP) contains cells that express high levels of CX3 CR1, the receptor for the fractalkine chemokine [1, 2]. Based on their monocytic origin and on their inability to migrate to the mesenteric lymph nodes (MLNs) such CX3 CR1hi cells have been defined as macrophages (Ms) [1–3]. CX3 CR1hi Ms contribute to the intestinal LP homeostasis through the production of anti-inflammatory cytokines and the clearance of commensal bacteria that breach the epithelial barrier [4]. In contrast, during intestinal inflammation, microenvironmental signals promote the differentiation of extravasated monocytes into proinflammatory Ms with the ability to produce interleukin (IL)-12, IL-23, tumor necrosis (TNF)-α and inducible nitric oxide synthase (iNOS) [5–7]. However, little is known about the developmental trajectories that lead extravasated monocytes to either antior proinflammatory intestinal Ms. This is primarily due to the fact that a surface marker permitting unequivocal identification of Ms within the intestine and their distinction from dendritic cells (DCs) is lacking. The interstitial DCs (Int-DCs) present throughout the LP derive from blood precursors known as pre-DCs [2]. Under steady-state conditions, the Int-DCs found in the intestinal LP induce oral tolerance by carrying antigens originating from food or from harmless bacteria to the MLNs [8, 9]. The CD103+ Int-DCs found in the steady-state LP have the selective ability to express aldehyde dehydrogenase (ALDH) and thereby produce retinoic acid (RA). As a result, upon migration to MLNs they trigger the differentiation of naive CD4+ T cells specific for food and microbiota antigens into induced Foxp3+ regulatory T (iTreg) cells [10–13]. In contrast, the Int-DCs that develop in inflamed LP upon exposure to pathogens lose their capacity to generate iTreg cells and, upon migration to the MLNs, trigger the differentiation of naive, antigen-responsive CD4+ T cells into T helper type 1 (Th1) cells that are specific for the invading pathogen and produce mainly IFN-γ [9, 14]. We have previously reported that the monocyte-derived cells that are present in skeletal muscle express high levels of CD64, the high-affinity IgG receptor FcγR [15]. By using the expression of CD64, we also succeeded in distinguishing Ms from DCs in the LP of the large and small intestine and the MLNs of both mice and humans. We thus reinvestigated at a high resolution MF and DC development in the intestinal LP under healthy conditions and studied how it was affected by inflammation. In this process, we found that during T cell-mediated colitis a similar developmental pathway gives rise to inflammatory Ms in both the intestinal LP and in the MLNs. Moreover, we made the highly unanticipated observation that T cell-mediated colitis unfolds in absence of a normal influx of LP-derived migratory DCs (Mig-DCs) and showed that the numerically dominant inflammatory Ms that develop within the MLNs also contribute to the induction of proinflammatory CD4+ T cells during T cell-mediated colitis. CD64 expression distinguishes Ms from DCs C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim We sought to identify a surface marker that would allow the distinction of Ms from DCs in the intestine and the MLNs. Using mice expressing an enhanced green fluorescent protein (EGFP) under the control of the gene coding for the CX3 CR1 chemokine receptor (CX3 CR1-EGFP mice; [16]), we found that all the CX3 CR1hi Ms of the LP of the small and large intestine expressed CD64 (Fig. 1A). Moreover, by combining CD64 and CD11c expression, we observed that the MHC class II (MHCII)-positive cells present in the LP of the small and large intestine could be readily separated into a CD11chi CD64− and a CD11c− to int CD64+ subset (Fig. 1B and C). Ly-6Chi monocytes express CCR2, a chemokine receptor that promotes their egress from the bone marrow into the blood, and as a result CCR2-deficient (Ccr2−/− ) mice show markedly reduced numbers of circulating Ly-6Chi monocytes and tissue Ms [17]. In contrast, DCs are not affected by CCR2 deficiency [18]. Therefore, we used this differential CCR2 requirement to determine whether the presence of CD11chi CD64− and CD11c− to int CD64+ cells in the intestinal LP depended on CCR2 expression. Accordingly, mice coexpressing CD45.1 and CD45.2 were lethally irradiated and reconstituted with a 1 to 1 mixture of BM cells isolated from CD45.1+ wild-type (WT) mice and from CD45.2+ Ccr2−/− mice. These B6 (CD45.1) WT + B6 (CD45.2) Ccr2−/− → B6 (CD45.1CD45.2) competitive chimeras were analyzed 8 weeks after BM transfer. As expected, Ly-6Chi blood monocytes were primarily composed of CD45.1+ Ccr2+ donor cells whereas neutrophils were comprised of almost equal percentages of CD45.1 and CD45.2 donor cells (Fig. 1E). CCR2-deficient and WT donor cells contributed equally to the CD11chi CD64− intestinal LP cells (Fig. 1B and C). The capacity to develop in a CCR2-independent manner combined with a specific absence in mice lacking the ligand for the Fms-like tyrosine kinase receptor 3 (Flt3L; Supporting Information Fig. 1A), strongly suggest that the CD11chi CD64− intestinal LP cells correspond to Int-DCs. In contrast, the CD11c− to int CD64+ intestinal LP cells showed percentages of CD45.1 and CD45.2 donor cells identical to those of Ly-6Chi blood monocytes (Fig. 1B and C). Consistent with the view that CD11c− to int CD64+ intestinal LP cells constitute monocyte-derived Ms, they developed independently of Flt3L (Supporting Information Fig. 1A). A similar conclusion applied to the few CD11c− to int CD64+ cells found among the MHCII+ cells present in the MLNs of mice kept under specific pathogen-free conditions (Fig. 1D). Therefore, by combining CD64 and CD11c expression, it is possible to unequivocally distinguish CD11c− to int CD64+ Ms from CD11chi CD64− DCs among the MHCII+ cells of the intestinal LP and of the MLNs without having to rely on the use of CX3 CR1-EGFP reporter mice. www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Figure 1. CD64 expression distinguishes monocyte-derived Ms from DCs in the intestinal LP and the MLNs. Cells were prepared from (A) the LP of the small and large intestine of CX3 CR1-EGFP mice and (B–E) the LP of the small and large intestine, the MLNs and the blood of B6 (CD45.1) WT + B6 (CD45.2) Ccr2−/− → B6 (CD45.1-CD45.2) chimeras. (A–D) After excluding NK cells, B cells, T cells, eosinophils, and neutrophils, the specified cells were analyzed by flow cytometry. (A) MHCII+ cells of the specified organs were analyzed for CX3 CR1(EGFP) and CD64 expression. Percentages of CX3 CR1hi CD64+ cells are indicated. (B–D) MHCII+ cells from the LP of the small and large intestine and from the MLNs were analyzed for CD11c and CD64 expression. The CD11chi CD64− and CD11c− to int CD64+ subsets were then analyzed for the percentages of CD45.1+ (WT) and CD45.2+ (Ccr2−/− ) donor cells. (E) CD11b+ blood cells were divided into Ly-6G+ neutrophils and Ly-6Chi Ly-6G− monocytes and analyzed for the percentages of CD45.1+ (WT) and CD45.2+ (Ccr2−/− ) donor cells. The percentages of cells found in each of the specified gates are indicated. (A) Data are representative of three independent experiments and (B–E) data are representative of at least 12 chimeric mice corresponding to three independent experiments. C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.eji-journal.eu 3 4 Samira Tamoutounour et al. CD8α + -type and CD11b+ -type intestinal DCs Conventional DCs can be categorized into CD8α+ - and CD11b+ type DCs [19, 20]. The CD11chi CD64− Int-DCs of the LP and their migratory counterparts present in the MLNs showed the same dichotomy and comprised CD8α+ - and CD11b+ -type DCs that can be unambiguously identified by their CD24+ CD11b− and CD11b+ CD64− phenotype, respectively (Supporting Information Fig. 1B). As expected, CD11b+ -type DCs expressed CD172α (SIRPα) whereas CD8α+ -type DCs were CD172α− (Supporting Information Fig. 1B). In contrast to CD64+ Ms that lacked CD103 (data not shown), a substantial fraction of CD24+ CD11b− and CD11b+ CD64− DCs found in the LP and the MLNs expressed CD103 (Supporting Information Fig. 1C). Notably, CD24+ CD11b− DCs were CX3 CR1− , whereas CD11b+ CD64− DCs were CX3 CR1int (Supporting Information Fig. 1C), emphasizing that in the intestine CX3 CR1 expression is not restricted to monocyte-derived cells (Fig. 1A). Likewise, F4/80 was expressed at high and intermediate levels on CD11c− to int CD64+ Ms and CD11b+ CD64− DCs, respectively (Supporting Information Fig. 1C). Therefore, by identifying Ms on the basis of their CD11c− to int CD64+ phenotype and subsequently subdividing CD11chi CD64− DCs into CD24+ CD11b− and CD11b+ CD64− cells, it is possible to overcome several of the limitations previously encountered in the identification of Ms and DC subsets in the intestinal LP and the MLNs. CD64 marks Ms in humans To evaluate whether CD64 could be also used to identify intestinal Ms in humans, we generated humanized mice and determined whether the HLA-DR+ cells found in their intestinal LP also contained CD64+ Ms in addition to DCs. CD34+ human stem cells from cord-blood were transfected with GFP and then injected into NOD-scid-IL-2Rγ−/− (NSG) mice. Eleven weeks after reconstitution, the GFP+ HLA-DR+ cells found in the intestinal LP could be readily divided into CD64− to low and CD64hi cells (Supporting Information Fig. 2A). The CD64− to low cells were composed of BDCA3+ and BDCA1+ cells, which represent the human equivalent of mouse CD8α+ - and CD11b+ -type DCs, respectively [19]. In contrast, the CD64hi cells were low for both BDCA3 and BDCA1 and likely corresponded to LP Ms (data not shown). To support our conclusion that human intestinal Ms expressed CD64, we analyzed colon biopsies obtained from patients suffering from ulcerative colitis. The HLA-DR+ LP cells found in healthy sections of the human colon contained BDCA3+ and BDCA1+ DCs as well as CD64hi cells that based on expression of CD14 likely corresponded to monocyte-derived cell (Supporting Information Fig. 2B). Interestingly, analysis of diseased tissue samples from the same patients showed a dramatic increase in the proportion of CD14+ CD64hi Ms among HLA-DR+ LP cells as compared with healthy tissue samples. Therefore, HLA-DR+ Ms were CD64hi in both steady state and inflamed human colon whereas colonic DCs were CD64− to low . C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim Eur. J. Immunol. 2012. 42: 1–17 Connecting recently extravasated Ly-6Chi monocytes to intestinal Ms The CD11b+ cells found in the LP of the small intestine comprised CX3 CR1int and CX3 CR1hi cells (Fig. 2A). In contrast to the CX3 CR1hi cells that are only constituted of Ms (Fig. 2B), the CX3 CR1int cells were heterogeneous and contained CD11b+ type Int-DCs that can be readily gated out on the basis of their CD11chi CD64− phenotype (Fig. 2C). Analysis of the remaining, Int-DC-deprived, CX3 CR1int cells on a Ly-6C-MHCII plot led to the identification of three populations (Fig. 2C). Population 1 (P1) resembled Ly-6Chi blood monocytes in terms of FSC-SSC profile (data not shown) and of its Ly-6Chi , CD64low , MHCII− , CD11c− to low , CX3 CR1int , and CD11b+ phenotype (Fig. 2C and D). P1 cells in the LP can also be identified on the basis of their unique CD11b+ Ly-6Chi phenotype (Fig. 2E). Population 2 (P2) was composed of Ly-6Cint to hi MHCII+ cells whereas population 3 (P3) had a Ly-6Clow MHCII+ phenotype identical to that of the CX3 CR1high Ms that are denoted as P4 cells (Fig. 2B and C). Note that the P3 and P4 cells can only be distinguished on the basis of their distinct levels of expression of the CX3 CR1(EGFP) reporter (Fig. 2). Therefore, in WT mice, P3 and P4 cells cannot be distinguished and are considered below as a single Ly-6Clow MHCII+ CD64+ P3/P4 population. The P2 cells “bridged” the diagonally opposite positions occupied by the P1 and the P3/P4 cells, a feature expected for developmental intermediates linking recently extravasated Ly-6Chi MHCII− monocytes to CX3 CR1int and CX3 CR1high Ms. When CD11b+ LP cells from WT mice were analyzed on a Ly-6C-CD64 plot they comprised Ly-6C− CD64− cells that were CCR2 independent and corresponded to CD11b+ Int-DCs (Fig. 3A). The remaining cells (red gate; Fig. 3A) strictly depended on CCR2 expression for their development and were thus of monocytic origin (Fig. 3A). They adopted a similar waterfall-shaped distribution on Ly-6C-CD64 and Ly-6C-MHCII plots (Fig. 3A), a feature consistent with the fact that CD64 and MHCII expression followed the same trend along the putative P1 → P2 → P3 → P4 developmental series. For the sake of brevity, the gate including the P1, P2, and P3/P4 cells is thus referred here as the “Mo-waterfall gate” and the waterfall-shaped distribution as the “Mo-waterfall” (Fig. 3B) A similar Mo-waterfall was also observed in the LP of the large intestine (Fig. 3C). To validate the hypothesis that a precursor-product relationship exists between the P1, P2, and P3/P4 stages that composed the Mo-waterfall (specified by red arrows in Figure 3A, bottom panels), Ly-6Chi monocytes were labeled with CFSE and adoptively transferred into healthy Ccr2−/− mice. We used Ccr2−/− hosts because they have a selective reduction in circulating Ly-6Chi monocytes that should facilitate the engraftment of the transferred CFSE+ monocytes. Analysis of the CFSE+ donor cells found in the LP of the small intestine 12 h after transfer showed some increase in MHCII and CD64 expression (Fig. 3D). By 72 h after transfer, most donor cells expressed both MHCII and CD64 and had downregulated Ly-6C expression. A small fraction of the www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Figure 2. CD64, Ly-6C, CD11b, CD11c, MHCII, and CX3CR1 expression in blood monocytes and in CX3 CR1int and CX3 CR1hi cells of the LP of the small intestine. Cells were prepared from the specified organs of CX3 CR1-EGFP mice. (A) After excluding NK cells, B cells, T cells, eosinophils, and neutrophils, the remaining cells were analyzed by flow cytometry for CD11b and CX3 CR1 expression. (B) Analysis of CD11b+ CX3 CR1hi cells for CD11c, CD64, Ly-6C, MHCII, and CX3 CR1 expression. (C) Analysis of CD11b+ CX3 CR1int cells for CD11c, CD64, Ly-6C, MHCII, and CX3 CR1 expression. In the CX3 CR1int DCs plots, CD11chi CD64− Int-DCs were excluded from CD11b+ CX3 CR1int cells prior to analysis. The P1 (Ly-6Chi MHCII− CD64low CX3 CR1int ), P2 (Ly-6Cint to hi MHCII+ CD64low CX3 CR1int ), P3 (Ly-6Clow MHCII+ CD64+ CX3 CR1int ) and P4 (Ly-6Clow MHCII+ CD64+ CX3 CR1hi ) stages are highlighted. (D) Analysis of CD11b+ Ly-6Chi blood monocytes for CD64, Ly-6C, CD11c, MHCII, and CX3 CR1 expression. (E) Analysis of CD11b+ Ly-6Chi monocytes of the small intestine for CD64, Ly-6C, CD11c, MHCII, and CX3 CR1 expression. The percentages of cells found in each of the specified gates are indicated. Data are representative of at least three independent experiments. Ly-6Clow MHCII+ CD64+ donor cells also expressed CD11c. In contrast, when the CFSE-labeled Ly-6Chi monocytes were kept in culture, they did not change their original Ly-6Chi CD64low MHCII− phenotype upon time (Fig. 3E). These data demonstrate that upon entry into the intestinal LP, Ly-6Chi monocytes sequentially give rise to the P1, P2, and P3/P4 populations and that this progression was accompanied by the upregulation of CX3 CR1, MHCII, CD64, and CD11c molecules and by the downregulation of Ly-6C (Fig. 3A and B). Moreover, the cells traversing this developmental series maintained CD172α expression and, importantly for the rest of this study, did not express CCR7 (Supporting information Fig. 3B and C). Therefore, by combining CD64 expression C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim with Ly-6C and MHCII expression it is possible to track the progressive differentiation of newly extravasated Ly-6Chi monocytes into Ms within healthy intestinal LP (Supporting Information Fig. 3). T cell-mediated colitis induces a massive differentiation of Ly-6Chi monocytes into Ms To analyze the effect of inflammation on the dynamics of MF and DC differentiation in the intestinal LP and the MLNs, we used a model of T cell-mediated colitis that relied on Cd3e5/5 mice www.eji-journal.eu 5 6 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 Figure 3. A developmental series links extravasated Ly-6Chi monocytes to intestinal Ms. Cells were prepared from the LP of the small intestine of the specified mice. After excluding NK cells, B cells, T cells, eosinophils, and neutrophils, the remaining CD11b+ cells were analyzed by flow cytometry. (A) CD11b+ cells from B6 (CD45.1) WT + B6 (CD45.2) Ccr2−/− → B6 (CD45.1-CD45.2) chimeras were analyzed for Ly-6C and CD64 expression. They comprise Ly-6C− CD64− Int-DCs and cells that adopt a waterfall-shaped flow cytometric distribution. The gate including those last cells is shown in red and denoted as the “Mo-waterfall gate.” Ly-6C− CD64− Int-DCs and cells belonging to the Mo-waterfall gate were analyzed for the percentages of CD45.1+ (WT) and CD45.2+ (Ccr2−/− ) donor cells. Expression of Ly-6C, CD11c, MHCII, CD64, and CX3 CR1 is also shown for cells belonging to the Mo-waterfall gate. Red arrows highlight the putative developmental path followed during Ly-6Chi monocyte differentiation in the LP. (B, C) The same Mo-waterfall is also observed in the LP of the small (B) and large (C) intestine of CX3 CR1-EGFP mice using Ly-6C-MHCII plot. The levels of CX3 CR1, CD172α, and CCR7 are shown for the P1, P2, and P3/P4 populations. The percentages of cells found in each of the specified gates are indicated and are representative of three independent experiments. (D, E) Sorted Ly6-Chi monocytes from B6 mice were CFSE labeled and transferred into healthy Ccr2−/− mice (monocyte transfer) or kept in culture (monocytes in culture). Twelve hours and 72 h after transfer, expression of Ly-6C, MHCII, CD11c, and CD64 were analyzed on donor-derived CFSE+ cells isolated from the LP (D) or from the cultures (E). The percentages of cells found in each of the specified gates are indicated. Data shown are representative of two experiments with three recipient mice at each time point. that lack T cells but not B cells [21]. Transfer of CD4+ Foxp3− T cells into Cd3e5/5 mice allows their extensive proliferation and differentiation into effector CD4+ T cells that produce mainly IFN-γ and that home to the large intestine where they trigger a severe colonic inflammation, typified by weight loss, diarrhea, and rectal prolapse (Supporting Information Fig. 4; [22]). Using this model, we first analyzed the evolution of MF and DC populations in the LP during the development of T cell-mediated colitis. Under steady-state conditions, WT and Cd3e5/5 mice contained similar large numbers of CD64+ Ms in the LP of the large intestine (Fig. 4A and data not shown). Upon transfer of CD4+ Foxp3− T cells into Cd3e5/5 mice, the numbers of CD64+ Ms increased in a rapid and massive manner in the LP of the large intestine (Fig. 4A and B and Supporting Information Fig. 5A). The numbers of CD8α+ - and CD11b+ -type Int-DCs also increased although to a lesser extent (Fig. 4A and B). Therefore, as observed in patients suffering from ulcerative colitis (Supporting Information Fig. 2B), the colitis observed in Cd3e5/5 mice is also associ- C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim ated with a large increase in the proportion of CD64+ Ms among MHCII+ LP cells. The Mo-waterfall found in the inflamed LP differed from the one observed under healthy conditions in that it consisted primarily of Ly-6Chi MHCII− (P1) and Ly-6Cint to hi MHCII+ (P2) cells and yielded comparably few Ly-6Clow MHCII+ (P3/P4) cells (compare Fig. 3C and Fig. 4C). Consistent with this last observation, adoptive transfer of CFSE-labeled Ly-6Chi BM monocytes into colitic Cd3e5/5 × Ccr2−/− mice gave rise to CD64+ LP Ms that had a predominant Ly-6Cint to hi MHCII+ phenotype (Fig. 4E). The same conclusion can be reached after marking the Ly-6Chi blood monocytes present in Cd3e5/5 mice undergoing T cell-mediated colitis via intravenous injection of latex beads [23]. Four days after injection of latex beads, the bead-labeled cells showed a blunted waterfall-shaped distribution (Fig. 4D). Therefore, in mice undergoing colitis, blood monocytes are constantly recruited to the large intestine LP where they predominantly differentiate into Ly-6Cint to hi MHCII+ CD64+ Ms. www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Figure 3. Continue. Colitis is associated with the differentiation of Ly-6Chi monocytes into Ms in the MLNs Unexpectedly, colitic Cd3e5/5 mice also displayed a rapid accumulation of CD64+ Ms in the MLNs (Fig. 5 A and B and Supporting Information Fig. 5B). To determine whether these Ms corresponded to LP-derived migratory Ms, we determined if they expressed CCR7, a chemokine receptor required for the migration of intestinal DCs to the MLNs [24]. In contrast to the LP-derived Mig-DCs, the Ms found in the MLNs of colitic Cd3e5/5 mice were CCR7− (Fig. 5C). It is thus likely that the Ms that accumulate in the MLNs of colitic Cd3e5/5 mice do not represent the migratory counterpart of intestinal Ms and originate from blood monocytes that seeded the MLNs and differentiated in situ. Consistent with this view, after excluding CD11b+ -type DCs, the remaining CD11b+ monocytic cells present in the MLNs of colitic Cd3e5/5 mice showed a waterfall-shaped distribution that consisted primarily of Ly-6Chi MHCII− and Ly-6Cint to hi MHCII+ cells C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim and that resembled the blunted Mo-waterfall found in the LP of colitic mice (Fig. 5D). Moreover, the Ly-6Chi MHCII− cells had an FSC-SSC profile typical of undifferentiated blood monocytes and their progression through the Mo-waterfall was associated with an increase in both cell size and granularity (Fig. 5D). Consistent with this last observation, adoptive transfer of CFSElabeled Ly-6Chi monocytes into colitic Cd3e5/5 Ccr2−/− mice gave rise in the MLNs to CD64+ Ms that were predominantly Ly-6Cint to hi MHCII+ (Fig. 5E). Importantly, in both the LP and the MLNs, the differentiation of adoptively transferred Ly-6Chi monocytes into CD64+ Ms followed the same kinetics (compare Fig. 4E and 5E). In the case the Ms found in the MLNs of colitic Cd3e5/5 mice will have represented migratory counterpart of intestinal Ms, a protracted kinetic of reconstitution would have been expected in the MLNs as compared with that in the LP. Therefore, in Cd3e5/5 mice undergoing T cell-mediated colitis, Ly-6Chi blood monocytes are massively recruited to the MLNs where they differentiate into Ms. The fact that they do not www.eji-journal.eu 7 8 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 Figure 4. Blood Ly-6Chi monocytes are continuously recruited into the large intestine of colitic Cd3e5/5 mice where they differentiate into Ms. (A) Pie charts show the relative percentage of CD64+ Ms, CD24+ CD11b− , and CD11b+ CD64− Int-DCs in the LP of the large intestine of WT B6 mice and of Cd3e5/5 mice that had received CD4+ Foxp3− T cells (IBD). Cd3e5/5 mice were analyzed 4 weeks after transfer of CD4+ Foxp3− T cells. (B) Kinetics of accumulation of the specified cells in Cd3e5/5 mice that had received CD4+ Foxp3− T cells. (A, B) Data are representative of at least three independent experiments with a minimum of three mice per group in each experiment. Error bars correspond to the SEM. (C, D) Cells were prepared from the LP of the large intestine of Cd3e5/5 mice that had received CD4+ Foxp3− T cells 3 weeks before. Four days prior to analysis, blood monocytes were labeled in vivo through intravenous injection of Alexa-647 beads. The Mo-waterfall (Fig. 3A) was analyzed for the presence of cells containing beads. Data shown are representative of at least three independent experiments. (E) Sorted Ly6-Chi monocytes were CFSE labeled and transferred into colitic Cd3e5/5 × Ccr2−/− mice. Twelve hours and 72 h after transfer, expression of Ly-6C, MHCII, CD11c, and CD64 were analyzed on donor-derived CFSE+ cells isolated from the LP of the large intestine. The percentages of cells found in each of the specified gates are indicated. Data shown are representative of two experiments with two recipient mice at each time point. represent the migratory counterpart of intestinal Ms is congruent with previous studies demonstrating that intestinal Ms do not migrate to the MLNs under healthy or TLR-induced inflammatory conditions [3]. Ly-6Chi monocytes differentiate into iNOS-expressing inflammatory Ms during T cell-mediated colitis A fraction of the CD64+ Ms that developed in the MLNs of colitic Cd3e5/5 mice that had received CD4+ Foxp3− T cells became iNOS+ (Fig. 6A and B). iNOS+ Ms also developed in the LP of the large intestine, but with slower kinetics compared with MLNs (Fig. 6A and B). The majority of iNOS+ Ms present in the large intestine LP and the MLNs were Ly-6Cint to hi MHCII+ (Fig. 6C). In contrast, DCs remained iNOS− at all time points (Fig. 6A). Therefore, during T cell-mediated colitis, a fraction of the blood monocytes that are recruited to the large intestine LP and the MLNs differentiate into iNOS-expressing inflammatory CD64+ Ms. C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim T cell-mediated colitis develops in mice with impaired migration of DCs to the MLNs To evaluate the requirement of LP-derived Mig-DCs in the development of T cell-mediated colitis, we generated Cd3e5/5 × Ccr7−/− mice in which the CCR7-dependent migration of Int-DCs from the intestinal LP to the MLNs is impaired [24]. Cd3e5/5 × Ccr7−/− mice and Cd3e5/5 control mice were reconstituted with CD4+ Foxp3− T cells isolated from CCR7-sufficient mice to avoid adventitious effects due to the lack of CCR7 on T cells, and analyzed 4 weeks after transfer. As expected, while both types of mice had comparable numbers of Int-DCs in the LP of the large intestine (Fig. 7A), the MLNs of Cd3e5/5 × Ccr7−/− mice contained numbers of CD8α+ -type and CD11b+ -type MigDCs that were reduced fourfold and sevenfold respectively, as compared with that in the Cd3e5/5 mice (Fig. 7A). In contrast, the numbers of MLN-resident Ms were comparable in both types of mice (Fig. 7A). Unexpectedly, preventing a normal influx of LP-derived Mig-DCs resulted in exacerbated T cellmediated colitis as shown by the increased percentage of IFN-γproducing effector T cells in the large intestine and the MLNs www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Figure 5. Extravasated Ly-6Chi monocytes differentiate into Ms in colitic MLNs. Cells were prepared from the MLNs of WT B6 mice and of Cd3e5/5 mice that had received CD4+ Foxp3− T cells (IBD), and defined as CD64+ Ms, CD24+ CD11b− , and CD11b+ CD64− Mig-DCs (see Supporting Information Fig. 5B). (A) Pie charts show the relative percentage of the specified cells for the two groups of mice. Cd3e5/5 mice were analyzed 4 weeks after transfer of CD4+ Foxp3− T cells. (B) Kinetics of accumulation of the specified cells. (A, B) Data shown are representative of at least three independent experiments with a minimum of three mice per group in each experiment. Error bars correspond to the SEM. (C) CCR7 expression on CD64+ Ms, CD24+ CD11b− , and CD11b+ CD64− Mig-DCs found in the MLNs of Cd3e5/5 mice 4 weeks after transfer of CD4+ Foxp3− T cells. (D) The FSC-SSC profile of the cells belonging to the specified sections of the Mo-waterfall found in the MLNs of Cd3e5/5 mice was analyzed 4 weeks after transfer of CD4+ Foxp3− T cells. (C, D) Data shown are representative of at least three independent experiments. (E) Sorted Ly6-Chi monocytes were CFSE labeled and transferred into colitic Cd3e5/5 × Ccr2−/− mice. Twelve hours and 72 h after transfer, expression of Ly-6C, MHCII, CD11c, and CD64 were analyzed on donor-derived CFSE+ cells isolated from the MLNs. The percentages of cells found in each of the specified gates are indicated. Data shown are representative of two experiments with two recipient mice at each time point. (Fig. 7B and C). This amplified inflammatory response was also associated with a more rapid weight loss (Fig. 7D). Therefore, in the Cd3e5/5 model, T cell-mediated colitis unfolds irrespective of a normal influx of LP-derived Mig-DCs. MLN-resident inflammatory Ms induce IFN-γ-producing effector T cells in vitro We next analyzed whether the numerically dominant inflammatory Ms that develop within the MLNs can participate in the induction of colitogenic T cells. First, we assessed whether they were located within the T-cell zone of the MLNs, a prerequisite for the activation of naive CD4+ T cells. Although CD64 expression would have constituted the best way of localizing MLN-resident inflammatory Ms, our fixation protocol prevented the use of this marker. Considering that iNOS+ inflammatory Ms expressed high levels of CD11c and that iNOS expression is restrained to these cells in the MLNs of colitic mice (Fig. 6A and B), we relied on iNOS and CD11c coexpression to locate MLN-resident inflam- C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim matory Ms. Confocal microscopy showed that iNOS+ CD11c+ inflammatory Ms were primarily found within the T-cell zone of the MLNs of colitic Cd3e5/5 mice (Fig. 6D). Moreover, MLNresident inflammatory Ms had a high phagocytic activity and lacked a DC-morphology (Supporting Information Fig. 6). Next, we assessed whether the inflammatory Ms that develop in the MLNs of colitic Cd3e5/5 mice were capable of converting na¨ıve CD4+ T cells into effector T cells in vitro and we compared them with the LP-derived Mig-DCs that are also found in colitic MLNs. Considering that colitic MLNs still contains some tolerogenic ALDH+ Mig-DCs (data not shown) that may have led us to underestimate the IFN-γ-producing capacity of ALDH− Mig-DCs, LP-derived Mig-DCs were sorted into ALDH+ and ALDH− cells. The various sorted cell types were pulsed with an ovalbumin (OVA)derived peptide and cocultured with OVA-specific OT-II CD4+ T cells. After 5 days of culture, OT-II T cells were analyzed for the production of IFN-γ and IL-17 (Fig. 6E). Surprisingly, among the analyzed MLN cells, inflammatory Ms, together with ALDH− CD8α+ -type Mig-DCs, possessed the strongest capacity to induce IFN-γ production by naive OT-II T cells. Therefore, the numerically dominant inflammatory Ms that develop in the www.eji-journal.eu 9 10 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 Figure 6. MLN-resident inflammatory Ms are iNOS+ , located in the T-cell zone and excel in the induction of IFN-γ-producing effector T cells in vitro. Cells were prepared from the MLNs and the large intestine LP of Cd3e5/5 mice that had received CD4+ Foxp3− T cells. After excluding NK cells, B cells, T cells, eosinophils, and neutrophils, the remaining MHCII+ cells were analyzed for CD64, CD11c, CD24, CD11b, CCR7, and intracellular iNOS expression. The distinct cell subsets were identified as specified in Supporting Information Fig. 5. (A) Percentage of iNOS+ cells within the specified subsets at various time points after T-cell transfer. (B) iNOS expression within the Ms found in the MLNs and the LP of the large intestine of colitic Cd3e5/5 mice. (C) iNOS+ cells from the MLNs and the large intestine of colitic Cd3e5/5 mice were analyzed for their position on the Mo-waterfall using Ly-6C-MHCII plot. (A–C) Data shown are representative of at least three independent experiments corresponding to three mice per group. The error bars correspond to the SEM. *p < 0.05, Student’s t-test. (D) MLNs from colitic Cd3e5/5 mice were analyzed by confocal microscopy 4 weeks after transfer of CD4+ Foxp3− T cells. Sections were stained with anti-CD11c, anti-CD3ε, anti-CD45R (B220), and anti-iNOS antibodies. As shown in the insets (lower right panel), iNOS+ cells were in close contact with CD3ε+ T cells. Scale bars, 20 μm. Data shown are representative of three independent experiments. (E) Cells isolated from MLNs of B6 mice (steady state) and of Cd3e5/5 mice that had received CD4+ Foxp3− T cells 2 weeks earlier (IBD Day 15), were subjected to an assay measuring ALDH at the single-cell level and Mig-DC subsets were FACS-sorted into ALDH+ and ALDH− fractions. The sorted Ms and DCs were loaded with OVA323–339 -peptide and cocultured with CFSE-labeled OT-II T cells. After 5 days of culture, OT-II T cells were restimulated with PMA and ionomycin and analyzed for intracellular IFN-γ and IL-17. The very small numbers of Ms found in steady-state MLNs prevented their sorting. Data are shown as mean + SEM of triplicate cultures pooled from at least 3 independent experiments. *p < 0.05, Student’s t-test. MLNs of colitic mice were located in the T-cell zone and excelled in the generation of Th1 effectors in vitro. MLN-resident Ms from colitic mice induce IFN-γ-producing effector T cells in vivo To determine whether MLN-resident inflammatory Ms were capable of triggering the differentiation of CD4+ T cells into IFN-γ-producing effector T cells in vivo, we developed the adoptive transfer experiment outlined in Fig. 8A. Consistent with pre- C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim vious data [25], when CD4+ T cells were labeled with CFSE and transferred into Cd3e5/5 host, two coincident and independent phenomena occurred [22]. A fraction of the transferred CD4+ T cells proliferated very slowly, accounting for the CFSEhigh cells observed at day 8 after transfer (Fig. 8B, upper panels). In contrast, a fraction of them proliferated extensively, yielding a prominent population of CFSElow cells. These fast-proliferating, CFSElow CD4+ T cells were capable of producing IFN-γ and their generation was strictly dependent on interaction with MHCII molecules expressed on the surface of the antigen-presenting cells of the host (Fig. 8B, middle panels). It is those fast-proliferating T cells that www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS are responsible for the induction of colitis when transferred in the absence of Treg cells. Antigenic peptides derived from the enteric bacteria and presented by MHCII molecules have been shown to be responsible for this TCR-driven fast proliferation whereas the slow proliferation is independent of MHCII molecules and IL-7-driven [26–30]. We took advantage of this model to determine whether upon transfer into Cd3e5/5 x MHCII/ mice, MLN-resident inflammatory Ms isolated from MHCII-sufficient, colitic mice were capable of rescuing the fast proliferation of cotransferred CD4+ T cells and their differentiation into IFN-γ-producing effectors. As shown in Fig. 8B, transfer of CD64+ Ms from MLNs of colitic mice was sufficient to trigger the fast proliferation of a fraction of the cotransferred CD4+ T cells and their differentiation into IFN-γ-producing effectors. The fact that we could only transfer relatively small numbers of CD64+ Ms per mouse likely explained that the magnitude of the CD4+ T-cell responses was smaller than that observed after injecting T cells into MHCII-sufficient Cd3e5/5 mice. Regardless of this limitation, our data demonstrate that inflammatory CD64+ Ms isolated from the MLNs of colitic mice can induce the proliferation and differentiation of CD4+ T cells into IFN-γ-producing effector T cells in vivo. Discussion Figure 7. Cd3e5/5 × Ccr7−/− mice develop severe T cell-mediated colitis. (A–C) 4 weeks after transfer of CD4+ Foxp3− T cells into Cd3e5/5 mice and Cd3e5/5 × Ccr7−/− mice, cells from the MLNs and the LP of the large intestine were analyzed. (A) Cells were subdivided into the specified subsets and their numbers determined. (B, C) Cells from (B) the MLNs and (C) the large intestine LP were restimulated in vitro with PMA plus ionomycin to assess for their capacity to produce IFN-γ and IL-17. Percentages of IFN-γ+ and IL-17+ cells among CD4+ T cells from Cd3e5/5 mice and Cd3e5/5 × Ccr7−/− mice are shown. (D) Weight fluctuation of Cd3e5/5 mice and Cd3e5/5 × Ccr7−/− mice transferred with CD4+ Foxp3− T cells. Data are shown as mean +− SEM of at least three (A–C) and six (D) mice per group and are pooled from three independent. * p < 0.05, Student’s t-test. C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim We have shown that in healthy and inflamed intestinal LP and MLNs, CD64 expression makes it possible to accurately identify Ms and to delineate a developmental series — called the Mowaterfall — that starts from extravasated Ly-6Chi monocytes and leads to intestinal Ms. Using Ly-6C-MHCII and Ly-6C-CD64 plots, the corresponding stages of this monocyte-derived developmental series have been denoted as P1 (Ly-6Chi MHCII− CD64low CX3 CR1int LP monocytes), P2 (Ly-6Cint to hi MHCII+ CD64low CX3 CR1int intermediate cells), P3 (Ly-6Clow MHCII+ CD64+ CX3 CR1int MF), and P4 (Ly-6Clow MHCII+ CD64+ CX3 CR1hi MF) (Supporting Information Fig. 3). Interestingly, we found that in humanized mice and humans, CD64 was highly expressed by HLA-DR+ cells that coexpressed CD14; a finding strongly suggesting that high CD64 expression marks cells of monocytic origin in humans. In support of this conclusion, a recent study demonstrated that the CD14hi and CD14lo subsets of HLA-DR+ Ms were uniformly CD64+ in both healthy and inflamed human intestine, whereas MHCII+ CD14− cells that include DCs were mostly CD64− [31]. Therefore, CD64 can be used in both mice and human to distinguish Ms from CD8α+ /BDCA-3+ -type and CD11b+ /BDCA-1+ type DCs, and to study how Ms originate from extravasated Ly-6Chi monocytes in healthy and inflamed conditions (Fig. 9). Although monocyte-derived MHCII+ cells found in the intestinal LP have been subdivided into CD11c− Ms and CD11c+ monocyte-derived DCs (Mo-DCs) by some authors [[2], [32], [33]], CD11c shows a continuous density distribution from negative to low among monocyte-derived MHCII+ LP cells (Fig. 2 and 3), a finding emphasizing the difficulty in using CD11b to define discrete stages amongst monocyte-derived MHCII+ LP cells. www.eji-journal.eu 11 12 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 Figure 8. MLN-resident CD64+ Ms from colitic Cd3e5/5 mice trigger the differentiation of Th1 cells in vivo. (A) Outline of the adoptive transfer model. Cd3e5/5 mice were injected i.v. with 2 × 106 CD4+ Foxp3− T cells to induce colitis. Two weeks later, when colitis was largely established, inflammatory CD64+ Ms were sorted from the MLNs. Cd3e5/5 × MHCII/ hosts were injected i.v. with the sorted inflammatory CD64+ Ms (2 × 106 ) and 1 day later with CFSE-labeled CD4+ T cells (2 × 106 ). In parallel experiments, CFSE-labeled CD4+ T cells (2 × 106 ) were injected into Cd3e5/5 (positive control) and Cd3e5/5 × MHCII/ (negative control) hosts. (B) Eight days after T-cell transfer, CD4+ T-cell proliferation was assessed by measuring CFSE dilution and IFN-γ and IL-17 production evaluated after a step of in vitro stimulation with PMA plus ionomycin. Percentages of IFN-γ+ and IL-17+ cells among slow (CFSEhigh ) and fast (CFSElow ) proliferating CD4+ T cells isolated from the specified mice are shown. Data shown are representative of three independent experiments consisting of five mice per group. During T cell-mediated colitis, extravasated Ly-6Chi monocytes differentiate into CD64+ MHCII+ inflammatory Ms that are CCR7− and, consistent with results from Pabst et al. [3], cannot migrate to the MLNs. This characteristic prevents their participation in the activation of na¨ıve T cells in the MLNs. However, giving their high MHCII expression, inflammatory Ms can potentially present antigens to tissue-resident memory T cells and to the iTreg cells that reach the LP [32, 34]. Along that line, due to its high affinity for IgG, the expression of CD64 may possibly arm LP Ms with IgG specific for previously encountered pathogens and allow them to efficiently initiate recall responses upon subsequent pathogen reexposure [15]. Although the inflammatory conditions achieved during T cell-mediated colitis do not induce LP Ms to migrate to MLNs, it remains possible that some bacterial adjuvants confer MLN-homing property to some LP Ms as shown for muscle Mo-DCs [33]. Unexpectedly, T cell-mediated colitis was also found associated with a massive recruitment of blood Ly-6Chi monocytes in the MLNs, where they differentiated into inflammatory Ms via a blunted Mo-waterfall similar to the one observed in the LP of inflamed intestine. These MLN-resident inflammatory Ms did not display a dendritic morphology and were phagocytic, a hallmark of Ms. In addition, they expressed high levels of MHCII molecules and were located in the T-cell zone, which are two pre- C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim requisites for proper interactions with naive CD4+ T cells. Consistent with these attributes, MLN-resident inflammatory Ms were capable of generating IFN-γ-producing T cells in vitro and in vivo. Therefore, during T cell-mediated colitis, MLN-resident inflammatory Ms likely synergize with LP-derived ALDH− Mig-DCs to induce the differentiation of na¨ıve T cells into proinflammatory T cells. Upon transfer of CD4+ Foxp3− T cells, we showed that Cd3e5/5 × Ccr7−/− recipient mice developed an exacerbated colitis as compared with Cd3e5/5 recipient mice. This result is consistent with our hypothesis that MLN-resident inflammatory Ms actively participate in the induction of T cell-mediated colitis irrespective of the presence of Mig-DCs and with the view that the RA-producing ALDH+ LP-derived Mig-DCs that are still present in colitic mice contribute to dampen colitic disease (Fig. 6E). It is important to stress that our results do not question a role for ALDH− LP-derived Mig-DCs in the generation of proinflammatory T cells during colitis. However, they differ from previous studies in that they reveal that the inflammatory Ms that expand massively in the MLNs of colitic mice and outnumber Mig-DCs are also capable of inducing proinflammatory CD4+ T cells. It remains to be determined how the inflammatory Ms that permanently reside in the MLNs gather enteric antigens in the absence of LP-derived Mig-DCs. Akin to the situation recently www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS Figure 9. A model of the independent developmental processes that generate Ms and DCs in the intestine and the MLNs under healthy and inflammatory conditions. (A) Two independent processes continuously occur in the healthy (steady state) intestine. First, CD8α+ - and CD11b+ -type Int-DCs develop in the LP from blood-derived pre-DC precursors and constitutively migrate to the MLNs in a CCR7-dependent manner. The resulting Mig-DCs contain ALDH+ DCs that are primarily endowed with tolerogenic properties. Second, a developmental series — called the Mo-waterfall — unfolds in the LP. It starts with extravasated Ly-6Chi MHCII− monocytes (P1) and leads to LP-resident antiinflammatory Ms termed P3 (Lyand 6Clow MHCII+ CD64+ CX3 CR1int ) P4 (Ly-6Clow MHCII+ CD64+ CX3 CR1hi ) via a P2 intermediate stage. (B) Under inflammatory conditions (e.g. T cell-mediated colitis), three independent processes occur in the intestinal LP and in the MLNs. First, CD8α+ - and CD11b+ -type Int-DCs develop in the intestinal LP and subsequently migrate to the MLNs. Among those Mig-DCs, ALDH− CD8α+ -, and CD11b+ -type DCs are capable of inducing proinflammatory CD4+ T cells. Second, massive numbers of Ly-6Chi monocytes (inf P1) seed the inflamed LP and predominantly develop into inflammatory Ly-6Cint to hi MHCII+ CD64hi Ms (inf P2) that do not migrate to the MLNs during T cell-mediated colitis. Third, Ly-6Chi blood monocytes are massively recruited to the MLNs where they locally differentiate into inflammatory Ly-6Cint to hi MHCII+ CD64+ Ms (inf P2). These MLN-resident inflammatory Ms are located in the T-cell zone and capable of generating Th1 cells in vitro and in vivo. As a result, during T cell-mediated colitis, MLN-resident inflammatory Ms likely synergize with ALDH− Mig-DCs to induce the differentiation of na¨ıve T cells into proinflammatory T cells. described for mice depleted of innate lymphoid cells [35], the lack of T cells in Cd3e5/5 × Ccr7−/− mice may favor the dissemination of commensal bacteria to the MLNs and their capture by the resident Ms. In conclusion, we have defined a novel gating strategy that is based on the differential expression of CD64 and that allows C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim the unequivocal identification of Ms in the intestine of mice and humans in both healthy and inflamed conditions (Fig. 9). On that basis, we demonstrated that T cell-mediated colitis is associated with a massive recruitment of monocytes to the intestinal LP where they differentiated into LP-resident inflammatory Ms. Coincidentally, T cell-mediated colitis also induced the www.eji-journal.eu 13 14 Samira Tamoutounour et al. massive recruitment of monocytes to the MLNs and their differentiation into MLN-resident inflammatory Ms capable of converting na¨ıve T cells into effector Th1 cells. In the case functionally similar inflammatory Ms develop in the MLNs of patients suffering from inflammatory bowel disease, they might constitute potential targets for the management of inflammatory digestive diseases. Materials and methods Eur. J. Immunol. 2012. 42: 1–17 cells. Analysis was performed using FlowJo software (Tree Star, Inc.). Assessment of phagocytosis FACS-sorted DC and MF subsets were seeded on Alcian bluetreated coverslips and incubated with 5% FCS supplemented RPMI containing yellow green fluorescent 0.5 μm Fluoresbrite microspheres (Polysciences, Inc.) for 1 h at 37◦ C before washing, fixation, staining for MHCII and iNOS and analysis by confocal microscopy. Mice CX3 CR1-EGFP [16], Foxp3-EGFP [25], Cd3e5/5 [21], OT-II [36], Ccr2−/− [37], CCR7−/− [38], and Cd3e5/5 × MHCII/ mice [25] were maintained on a C57BL/6 background and under specific pathogen-free conditions. All experiments were done in accordance with French and European guidelines for animal care. Cell preparation DCs were isolated from the MLNs and the LP of the small and large intestine as described in [11]. Generation of BM chimeras Seven to –8-week-old B6 CD45.1 × CD45.2 mice were lethally irradiated with two doses of 550 rads, 5 h apart, and then injected i.v. with 2 × 106 BM cells. BM cells were obtained from femurs and tibias of WT B6 CD45.1 or of Ccr2−/− CD45.2 mice. T cell-mediated colitis T cells were purified by magnetic separation from spleens and LNs of Foxp3-EGFP mice using a CD4 negative isolation kit (Dynal). Cells were then stained with PE-conjugated anti-CD4 (RM4–5) antibody and CD4+ Foxp3− T cells (2 × 106 ) were sorted and injected intravenously into Cd3e5/5 mice. Flow cytometry Cells were stained and analyzed using a FACS LSRII system (BD Biosciences). Allophycocyanin-Cy7-conjugated antiNK1.1 (PK136), anti-CD3 (17A2), anti-Ly-6G (1A8), anti-CD19 (6D5), and PE-conjugated anti-CD64 (X54–5/7.1) were all from Biolegend, allophycocyanin-conjugated anti-CCR3 (83103) was from R&D, PE-Cy7-conjugated anti-CD11c (N418), Alexa-700conjugated anti-MHC Class II (I-A/I-E) (M5/114.15.2), PE-Cy5.5conjugated anti-CD45.2 (104), allophycocyanin-conjugated antiCD45.1 (A20), PE-Cy5-conjugated anti-CD24 (M1/69), and PECy5-conjugated anti-CD5 (53–7.3) were all from eBioscience, Pacific-Blue-conjugated anti-CD11b (M1/70), PE- or biotinconjugated anti-CD103 (M290), allophycocyanin-conjugated antiCD172α (P84), FITC-conjugated anti-Ly6C (AL21), PacificBlue-conjugated anti-CD4 (RM4–5), biotin-conjugated anti-CCR7 (4B12) were all from BD Pharmingen. Biotin-conjugated antibodies were detected using streptavidin conjugated with QuantumDot605 (Invitrogen). Intracellular iNOS staining was performed using unlabeled anti-rabbit iNOS (M19, Santa Cruz) and allophycocyanin-conjugated anti-rabbit IgG (Invitrogen). ALDH+ cells were identified as described [11], and intracellular cytokines staining performed as described [33]. Prior to DC and MF analysis, B cells, T cells, NK cells, eosinophils and neutrophils were systematically gated out using a “dump-channel” corresponding to cells positive for CD19, CD3, NK1.1, CCR3 or Ly-6G C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim In vivo labeling of Ly-6Chi monocytes Blood monocytes were labeled with latex beads as described [23]. Adoptive transfer of Ly-6Chi MHCII− monocytes Bone marrow and spleens from RAG−/− mice were harvested. Cells were stained for CD11b, Ly6C, Ly6G, MHCII, CCR3, and CD11c. Ly-6Chi monocytes were sorted as CD11b+ Ly-6G− CCR3− CD11c− MHCII− Ly-6Chi cells with a purity of more than 95% and labeled with CFSE (Molecular Probes). A 2 × 106 CFSElabeled Ly-6Chi monocytes were transferred intravenously into healthy Ccr2−/− mice or Cd3e5/5 × Ccr2−/− colitic mice. In parallel 2 × 104 CFSE-labeled Ly-6Chi monocytes were maintained in vitro in complete medium in the presence of 1 × 106 WT BM cells. Adoptive transfer of inflammatory CD64+ Ms Cd3e5/5 mice were injected i.v. with 2 × 106 CD4+ Foxp3− T cells to induce colitis. Two weeks later, when colitis was largely installed, inflammatory CD64+ Ms were isolated from the MLNs. Cd3e5/5 × MHCII/ hosts were first injected i.v. with 2 × 106 www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 inflammatory CD64+ Ms and then, 1 day later, with 2 × 106 CFSE-labeled CD4+ T cells. In parallel experiments, 2 × 106 CFSElabeled CD4+ T cells were injected into Cd3e5/5 and Cd3e5/5 × MHCII/ . Eight days after T-cell transfer, CD4+ T-cell proliferation and cytokine production were evaluated. HIGHLIGHTS Humanized mice Humanized mice experiments were developed and analyzed as described [40]. Statistical analysis Preparation of CFSE-labeled T cells OT-II T cells were purified by magnetic separation from pooled spleen and LN using a CD4 negative isolation kit (Dynal). For CFSE labeling, purified cells were resuspended in PBS and labeled with 2.5 μM 5- and 6-carboxy-fluorescein diacetate succinimidyl ester (CFSE) (Molecular Probes) for 3 min at room temperature. Culture of CFSE-labeled OT-II T cells 3 × 103 DCs or Ms were cocultured with 2 × 104 CFSE-labeled OT-II T cells in 200 μL in the presence of ovalbumin (323–339) peptide (0.06 μg/mL). After 5 days of culture, cells were restimulated with PMA and ionomycin for 5 h before intracellular cytokine staining. Proliferation was measured by loss of CFSE staining. Immunofluorescence staining MLNs were fixed with 3.2% paraformaldehyde for 1 h, washed in PBS, infused overnight in 35% sucrose, and frozen in TissueTek OCT compound (Electron Microscopy Sciences, Hatfield, PA). After permeabilization for 5 min in PBS containing 0.5% saponin, 2% bovine serum albumin, 1% fetal calf serum, and blockade of Fc binding with 1% goat serum for 30 min, 12 μm cryostat tissue sections were labeled overnight at 4◦ C with rabbit anti-iNOS (Santa Cruz Biotechnology), hamster anti-CD11c (N418, Biolegend) and rat anti-CD45R (RA3–6B2, Biolegend) antibodies or control antibodies followed by incubation for 1 h at room temperature with secondary antibodies and SYTOX Blue for nuclei staining. Slides were mounted in Prolong Gold (Invitrogen) and observed with a Zeiss LSM 510 or a Zeiss LSM 780 confocal microscope (Carl Zeiss, Jena, Germany). Comparative experiments were tested for statistical significance using the unpaired Student’s t-test in GraphPad Prism software (version 4.0; GraphPad). Acknowledgments: We thank M. Malissen, H. Luche, B. Lucas, G. Randolph, and L. Leserman for discussions. We thank M. Barad, P. Grenot, and A. Zouine for assistance with cell sorting and M. Fallet and M. Barad for assistance with confocal microscopy. This work was supported by CNRS, INSERM, European Communities Framework Program 7 (MASTERSWITCH Integrating Project; HEALTH-F2–2008-223404 and NANOASIT Euronanomed Project), AFM, FRM, ANR (Skin DCs) and by doctoral and postdoctoral fellowships from Minist`ere de la Recherche (S.T.), and a Marie Curie Fellowship from the European Communities (M.G., project number 237109). Y.R., C.R.E.S., and D.B. have funding from the Cancer Research UK. Y.R. is supported by Leukaemia and Lymphoma Research. L.F.P. is supported by a CNRS/INSERM ATIP/AVENIR program. A.M.M. and C.C.B. were supported by the Medical Research Council and Wellcome Trust (UK). Conflict of interests: The authors declare no financial or commercial conflict of interest. References 1 Varol, C., Vallon-Eberhard, A., Elinav, E., Aychek, T., Shapira, Y., Luche, H., Fehling, H. J. et al., Intestinal lamina propria dendritic cell subsets have different origin and functions. Immunity 2009. 31: 502–512. 2 Bogunovic, M., Ginhoux, F., Helft, J., Shang, L., Hashimoto, D., Greter, M., Liu, K. et al., Origin of the lamina propria dendritic cell network. Immunity 2009. 31: 513–525. 3 Schulz, O., Jaensson, E., Persson, E. K., Liu, X., Worbs, T., Agace, W. W. Characterization of DCs and Ms from human colon biopsies Colon biopsy specimens were obtained from patients with a history of ulcerative colitis during colonoscopy after informed consent and with the approval of the Ethics Committee of Erasmus University Medical Centre, Rotterdam. Endoscopic signs of inflammation were used to define the biopsies as inflamed. LP mononuclear cells were isolated from the biopsies as previously described [39]. C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim and Pabst, O., Intestinal CD103+, but not CX3CR1+, antigen sampling cells migrate in lymph and serve classical dendritic cell functions. J. Exp. Med. 2009. 206: 3101–3114. 4 Bain, C. C. and Mowat, A. M., Intestinal macrophages – specialised adaptation to a unique environment. Eur. J. Immunol. 2011. 41: 2494–2498. 5 Dunay, I. R., Damatta, R. A., Fux, B., Presti, R., Greco, S., Colonna, M. and Sibley, L. D., Gr1(+) inflammatory monocytes are required for mucosal resistance to the pathogen Toxoplasma gondii. Immunity 2008. 29: 306– 317. 6 Platt, A. M., Bain, C. C., Bordon, Y., Sester, D. P. and Mowat, A. M., An independent subset of TLR expressing CCR2-dependent macrophages www.eji-journal.eu 15 16 Samira Tamoutounour et al. Eur. J. Immunol. 2012. 42: 1–17 6843– in the bone marrow and present them to T cells after maturing in the 7 Siddiqui, K. R., Laffont, S. and Powrie, F., E-cadherin marks a subset of 24 Jang, M. H., Sougawa, N., Tanaka, T., Hirata, T., Hiroi, T., Tohya, K., Guo, inflammatory dendritic cells that promote T cell-mediated colitis. Immu- Z. et al., CCR7 is critically important for migration of dendritic cells in nity 2010. 32: 557–567. intestinal lamina propria to mesenteric lymph nodes. J. Immunol. 2006. promotes colonic inflammation. J. Immunol. 2010. 184: 6854. 8 Worbs, T., Bode, U., Yan, S., Hoffmann, M. W., Hintzen, G., Bernhardt, G., Forster, R. et al., Oral tolerance originates in the intestinal immune periphery. J. Exp. Med. 2006. 203: 583–597. 176: 803–810. 25 Wang, Y., Kissenpfennig, A., Mingueneau, M., Richelme, S., Perrin, P., system and relies on antigen carriage by dendritic cells. J. Exp. Med. 2006. Chevrier, S., Genton, C. 203: 519–527. LatY136F mutant mice unfolds independently of TCR-MHC engagement 9 Maloy, K. J. and Powrie, F., Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 2011. 474: 298–306. 10 Edelson, B. T., Kc, W., Juang, R., Kohyama, M., Benoit, L. A., Klekotka, P. A., Moon, C. et al., Peripheral CD103+ dendritic cells form a unified subset developmentally related to CD8alpha+ conventional dendritic cells. J. Exp. Med. 2010. 207: 823–836. et al., Th2 lymphoproliferative disorder of and is insensitive to the action of Foxp3+ regulatory T cells. J. Immunol. 2008. 180: 1565–1575. 26 Kieper, W. C., Troy, A., Burghardt, J. T., Ramsey, C., Lee, J. Y., Jiang, H. Q., Dummer, W. et al., Recent immune status determines the source of antigens that drive homeostatic T cell expansion. J. Immunol. 2005. 174: 3158–3163. 11 Guilliams, M., Crozat, K., Henri, S., Tamoutounour, S., Grenot, P., Dev- 27 Martin, B., Becourt, C., Bienvenu, B. and Lucas, B., Self-recognition is ilard, E., de Bovis, B. et al., Skin-draining lymph nodes contain dermis- crucial for maintaining the peripheral CD4+ T cell pool in a nonlym- derived CD103(-) dendritic cells that constitutively produce retinoic acid and induce Foxp3(+) regulatory T cells. Blood 2010. 115: 1958–1968. 12 Coombes, J. L., Siddiqui, K. R., Arancibia-Carcamo, C. V., Hall, J., Sun, C. M., Belkaid, Y. and Powrie, F., A functionally specialized population of phopenic environment. Blood 2006. 108: 270–277. 28 Min, B., Yamane, H., Hu-Li, J. and Paul, W. E., Spontaneous and homeostatic proliferation of CD4 T cells are regulated by different mechanisms. J. Immunol. 2005. 174: 6039–6044. mucosal CD103+ DCs induces Foxp3 +regulatory T cells via a TGF-beta 29 Mingueneau, M., Roncagalli, R., Gregoire, C., Kissenpfennig, A., Miazek, and retinoic acid-dependent mechanism. J. Exp. Med. 2007. 204: 1757– A., Archambaud, C., Wang, Y. et al., Loss of the LAT adaptor con- 1764. verts antigen-responsive T cells into pathogenic effectors that func- 13 Sun, C. M., Hall, J. A., Blank, R. B., Bouladoux, N., Oukka, M., Mora, J. R. and Belkaid, Y., Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 T reg cells via retinoic acid. J. Exp. Med. 2007. 204: 1775–1785. 14 Laffont, S., Siddiqui, K. R. and Powrie, F., Intestinal inflammation abrogates the tolerogenic properties of MLN CD103+ dendritic cells. Eur. J. Immunol. 2010. 40: 1877–1883. tion independently of the T cell receptor. Immunity 2009. 31: 197– 208. 30 Feng, T., Wang, L., Schoeb, T. R., Elson, C. O. and Cong, Y., Microbiota innate stimulation is a prerequisite for T cell spontaneous proliferation and induction of experimental colitis. J. Exp. Med. 2010. 207: 1321– 1332. 31 Bain, C. C., Scott, C. L., Uronen-Hansson, H., Gudjonsson, S., Jans- 15 van der Poel, C. E., Spaapen, R. M., van de Winkel, J. G. and Leusen, J. H., son, O., Grip, O., Guilliams, M. et al., Resident and pro-inflammatory Functional characteristics of the high affinity IgG receptor, FcgammaRI. macrophages in the colon represent alternative context dependent fates J. Immunol. 2011. 186: 2699–2704. of the same Ly6Chi monocyte precursors. Mucosal. Immunol. 2012. in 16 Jung, S., Aliberti, J., Graemmel, P., Sunshine, M. J., Kreutzberg, G. W., press. Sher, A. and Littman, D. R., Analysis of fractalkine receptor CX(3)CR1 32 Denning, T. L., Norris, B. A., Medina-Contreras, O., Manicassamy, S., function by targeted deletion and green fluorescent protein reporter gene Geem, D., Madan, R., Karp, C. L. et al., Functional specializations of insertion. Mol. Cell Biol. 2000. 20: 4106–4114. intestinal dendritic cell and macrophage subsets that control Th17 and 17 Serbina, N. V. and Pamer, E. G., Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat. Immunol. 2006. 7: 311–317. 18 Geissmann, F., Manz, M. G., Jung, S., Sieweke, M. H., Merad, M. and Ley, K., Development of monocytes, macrophages, and dendritic cells. Science 2010. 327: 656–661. 19 Guilliams, M., Henri, S., Tamoutounour, S., Ardouin, L., Schwartz-Cornil, I., Dalod, M. and Malissen, B., From skin dendritic cells to a simplified classification of human and mouse dendritic cell subsets. Eur. J. Immunol. 2010. 40: 2089–2094. 20 Heath, W. R. and Carbone, F. R., Dendritic cell subsets in primary and secondary T cell responses at body surfaces. Nat. Immunol. 2009. 10: 1237– 1244. 21 Malissen, M., Gillet, A., Ardouin, L., Bouvier, G., Trucy, J., Ferrier, P., Vivier, E. et al., Altered T cell development in mice with a targeted mutation of the CD3-epsilon gene. Embo. J. 1995. 14: 4641–4653. 22 Martin, B., Banz, A., Bienvenu, B., Cordier, C., Dautigny, N., Becourt, C. and Lucas, B., Suppression of CD4+ T lymphocyte effector functions by CD4+CD25+ cells in vivo. J. Immunology 2004. 172: 3391–3398. 23 Tacke, F., Ginhoux, F., Jakubzick, C., van Rooijen, N., Merad, M. and Randolph, G. J., Immature monocytes acquire antigens from other cells C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim regulatory T cell responses are dependent on the T cell/APC ratio, source of mouse strain, and regional localization. J. Immunol. 2011. 187: 733–747. 33 Langlet, C., Tamoutounour, S., Henri, S., Luche, H., Ardouin, L., Gregoire, C., Malissen, B. et al., CD64 expression distinguishes monocyte-derived and conventional dendritic cells and reveals their distinct role during intramuscular immunization. J. Immunol. 2012. 188: 1751–1760. 34 Hadis, U., Wahl, B., Schulz, O., Hardtke-Wolenski, M., Schippers, A., Wagner, N., Muller, W. et al., Intestinal tolerance requires gut homing and expansion of FoxP3 +regulatory T cells in the lamina propria. Immunity 2011. 34: 237–246. 35 Sonnenberg, G. F., Monticelli, L. A., Alenghat, T., Fung, T. C., Hutnick, N. A., Kunisawa, J., Shibata, N. et al., Innate lymphoid cells promote anatomical containment of lymphoid-resident commensal bacteria. Science 2012. 336: 1321–1325. 36 Barnden, M. J., Allison, J., Heath, W. R. and Carbone, F. R., Defective TCR expression in transgenic mice constructed using cDNA-based alpha- and beta-chain genes under the control of heterologous regulatory elements. Immunol. Cell. Biol. 1998. 76: 34–40. 37 Boring, L., Gosling, J., Chensue, S. W., Kunkel, S. L., Farese, R. V., Jr., Broxmeyer, H. E. and Charo, I. F., Impaired monocyte migration and reduced type 1 (Th1) cytokine responses in C-C chemokine receptor 2 knockout mice. J. Clin. Invest. 1997. 100: 2552–2561. www.eji-journal.eu Eur. J. Immunol. 2012. 42: 1–17 HIGHLIGHTS 38 Forster, R., Schubel, A., Breitfeld, D., Kremmer, E., Renner-Muller, I., Abbreviations: EGFP: enhanced green fluorescent protein · Int-DC: inter- Wolf, E. and Lipp, M., CCR7 coordinates the primary immune response stitial DC · iTreg cell: induced Foxp3+ regulatory T cell · LP: lamina by establishing functional microenvironments in secondary lymphoid propria · Mig-DC: migratory DC · MHCII: MHC class II organs. Cell 1999. 99: 23–33. 39 Ng, S. C., Plamondon, S., Al-Hassi, H. O., English, N., Gellatly, N., Kamm, M. A., Knight, S. C. et al., A novel population of human CD56+ human leucocyte antigen D-related (HLA-DR+) colonic lamina propria cells is associated with inflammation in ulcerative colitis. Clin. Exp. Immunol. Full correspondence: Dr. Bernard Malissen, Centre d’Immunologie de Marseille-Luminy, Case 906, 13288 Marseille Cedex 9, France Fax: +33-491269430 e-mail: bernardm@ciml.univ-mrs.fr 2009. 158: 205–218. 40 Poulin, L. F., Reyal, Y., Uronen-Hansson, H., Schraml, B., Sancho, D., Murphy, K. M., Hakansson, U. K. et al., DNGR-1 is a specific and universal marker of mouse and human Batf3-dependent dendritic cells in lymphoid and non-lymphoid tissues. Blood 2012. C 2012 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim Received: 20/7/2012 Revised: 26/8/2012 Accepted: 28/8/2012 Accepted article online: 31/8/2012 www.eji-journal.eu 17
© Copyright 2025