How Could tHe CommunItY workForCe allevIate Some oF tHe
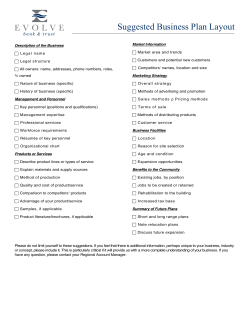
www.cfwi.org.uk BPC Community care:Layout 1 07/10/2013 12:43 Page 1 CF W O R K F O R C E B R I E F I N G WI SCANNING How Could tHe CommunItY workForCe allevIate Some oF tHe PreSSure on general PraCtItIonerS and ImProve joInt workIng aCroSS PrImarY and CommunItY Care? HEALTH AND SOCIAL CARE SYSTEM DESIGN Achieving better integration between health, social care and support organisations DEMOGRAPHIC AND SOCIAL Planning to meet the needs of an ageing population with an ageing workforce P rimary care faces challenges ahead as a result of the ageing population, rising patient expectations, increase in complex comorbidities, and the financial climate. Between 1995 and 2008, the number of gP consultations rose by 11 per cent (deloitte, 2012). For the average patient, the number of consultations per year rose from 3.9 in 1995 to 5.5 in Fig.1 FINANCIAL AND ECONOMIC Planning service delivery given the uncertainty about levels of funding in the future and how this will affect future demand for and supply of care services 2008, with the biggest increases taking place among the over-70 population (Health and Social Care Information Centre, 2009). If the pattern of consultations remains unchanged, Deloitte expects there will be a total of 433 million GP consultations by 2035 and 180 million of these consultations would be for people aged 65 and over, nearly double the current number (Deloitte, 2012). CfWI modelling (shown in figure 1) used in reviewing the GP workforce projects a sustained rise in demand, and an undersupply across general practice (CfWI, 2013). Given that some GPs will take on commissioning responsibilities, their time is going to be even more stretched in the future. Meeting increased demand through GPs alone may not be possible. This briefing explores how the wider community workforce could be used to alleviate some of this pressure. 55,000 50,000 Demand and supply forecasts for GPs in four medical scenarios Demand: scenario 1-6 Supply: scenario 1-6 Supply: baseline GPs Demand: baseline GPs The scenarios are based on a range of views gathered by stakeholders. To find out more about the scenarios please access our report at www.cfwi.org.uk/publications/gp-indepth-review-preliminary-findings . Source: CfWI (2013) Full-time equivalent Big picture challenges HORIZON 45,000 40,000 35,000 30,000 2010 2015 2020 2025 2030 Year THE CENTRE FOR WORKFORCE INTELLIGENCE 209-215 Blackfriars Road London SE1 8NL T +44(0)20 7803 2707 E enquiries@cfwi.org.uk www.cfwi.org.uk | www.horizonscanning.org.uk BPC Community care:Layout 1 07/10/2013 12:43 Page 2 workForCe BrIeFIng | HOW COulD THE COMMuNITy WORKFORCE AllEvIATE SOME OF THE PRESSuRE ON GENERAl PRACTITIONERS AND IMPROvE JOINT-WORKING ACRO redesigning the gP practice workforce: Nurse practitioners redesigning the gP practice workforce: Physician assistants One way to alleviate pressure on GPs is to base other types of community worker in GP surgeries. Nurse practitioners, for example, could redesign primary care activities and optimise skill mix to reduce pressure on GP time and address financial challenges. However, while a review by laurant found quality of care is similar for nurses and doctors, it is not clear if using nurse practitioners decreases the doctor's workload (laurant et al, 2009). Physician assistants (PAs) are mid-level practitioners that have a scienceorientated first degree. Healthcare professionals with a first level qualification in, for example, nursing, physiotherapy or who are working as a paramedic can also apply to a physician assistant course. The PA role has a history of over 40 years in the united States (uS), where there are now over 80,000 working PAs, and, within Europe, the Netherlands adopted the model seven years ago and now has 700 PAs. However, the role is still relatively new to the uK with about 200 PAs currently known to be working across approximately 30 acute trusts (Parle and Ross 2012). The uK has recently been exploring the use of PAs in clinical practice and the university of Southampton is due to publish research commissioned by the National Institute of Health Research (NIHR) investigating the contribution of physician assistants to primary care in England. Nurses tend to provide more health advice and achieve higher levels of patient satisfaction than doctors. However, although they have lower salary costs, nurses may order more tests and use other services, which could offset these cost savings. Indeed, a study in the Netherlands found that adding nurse practitioners to GP surgeries did not reduce the workload of GPs (laurant et al, 2004). The number of contacts during surgery hours increased in the intervention group, particularly for patients with chronic obstructive pulmonary disease or asthma, and there was no significant change in the number of out-of-hours consultations or in workload of GPs. The home care organisation Buurtzorg in the Netherlands has demonstrated an alternative model of delivering care which reduced the number of unplanned episodes and resources used per patient. Small self-steering teams of nurses visit patients to deliver all of the home care patients’ needs. Although this has higher costs per hour there are overall productivity gains through fewer hours in total (KPMG, 2013). CF WI © 2013 CENTRE FOR WORKFORCE INTELLIGENCE Centre FOR workForCe IntellIgenCe Recent English and Scottish pilots of PAs employed in general practice or out-ofhours services reported that PAs were well accepted by patients, undertook work previously done by medical staff, consulted medical staff less frequently and exhibited greater diagnostic skills than extended roles in nursing. Although there is a relatively small number of PAs in England currently, there is a potential scope for an increasing service contribution to general practice in England in the future. In the united States, for example, around 45 per cent of the PAs distributed by primary care specialty, work in family medicine (AAPA, 2010). The flexibility of PAs also makes them attractive contributors to secondary care provision. In the uS, physician assistants will usually work in several specialties in their career. Physician assistants are a workforce that can complement the work of GPs and the wider practice skill mix in seeing younger patients with fewer indicators of co-morbidity and fewer medically acute problems and can be deployed to triage patients and/or see same day appointments. the wider community workforce: Pharmacists Another way to alleviate pressure on GPs is to divert demand to the wider community workforce. The community workforce is largely composed of generalist community workers, but with the increasing prevalence of long-term conditions and co-morbidities, there may also be a need for more specialists in the community. This could be in the form of community workers with specialist interests, or specialists who work in the community. GPs have traditionally been seen as the gatekeepers to the system. But community pharmacists could play a role in providing services, and signposting people to other areas of the health and social care system. They are local, accessible and convenient, and it has long been recognised that pharmacists are a ‘major untapped resource for health improvement’ (DH, 2005). Primary care pharmacists work closely with GPs and can offer advice on good prescribing, which can lead to more effective first-time prescriptions and can help to address capacity issues in the NHS. Participants at the recent CfWI pharmacy in-depth review scenario generation workshop (held in January 2013) considered that there was a good case for an expanding role for pharmacists. This could involve routine testing, helping to manage long-term conditions, and advising patients on the use of technology. There is mixed evidence about the impact of pharmacists in primary care (Ballantyne, 2011). Pharmacist-led medication reviews can have positive medication-related outcomes, but these do not seem to translate into measurable benefits to patients or health services (Holland et al, 2006). In BPC Community care:Layout 1 07/10/2013 12:43 Page 3 ACROSS PRIMARy AND COMMuNITy CARE? CfwI gP in-depth review project CfwI have been commissioned by the department of Health to conduct an in-depth review of the gP workforce. the review will assess: ¡ ¡ ¡ ¡ current workforce numbers to forecast supply key drivers affecting workforce demand regional variations in demand and make recommendations for future workforce planning. This work is due to be published in 2013. More information about this project can be found at the following link: www.cfwi.org.uk/our-work/medicaland-dental-1/gp-in-depth-review The review will also address issues such as GP workload and the 2015 recruitment target and beyond, as well as wider issues around primary care delivery. one study, GPs did not follow up on recommendations made by pharmacists, with a suggestion of lack of respect shown to pharmacists by physicians. In another, patients saw doctors as having ‘higher authority’, and this was a barrier to pharmacists providing advice (Ballantyne, 2011). It may be necessary to change the public perception of pharmacists’ roles and to highlight the importance of working in a multidisciplinary way to improve outcomes of pharmacy-led interventions. redesigning the gP practice workforce: Social workers Surrey County Council is exploring the idea of putting social workers into GP practices (Surrey County Council, 2012). This has previously been tried by other councils. Many local areas have assigned social care staff to surgeries, and they participate in regular meetings held at practices to help patients stay in their own homes and communities. This could help to improve joint working across health and social care workforces. In an iMPOWER survey, more than half of GPs admitted they don’t understand the wider care services available for patients and just 15 per cent of GPs said they understand all the options (iMPOWER, 2013). 78 per cent of social workers believe GPs often don’t understand or encourage alternative options to residential care. According to Jeremy Cooper, the findings reveal GPs, social workers and local authorities are locked in a dysfunctional relationship, with lack of understanding between them generating unnecessary demand for residential care – the highest cost area of adult social care. Helping GPs understand the wider social care services available could help deflate demand, keeping 60,000 people out of residential care and saving more than £600 million a year (iMPOWER, 2013). redesigning the gP practice workforce: Community patient groups Community patient groups are a valuable, untapped resource to support patients. They increasingly provide services and help to improve care in the community. Patientview has been tracking patient groups for over a decade, and has seen huge increases in their number (CfWI interview with Patientview, 2013). Patientview’s latest statistics, which it believes underestimates the actual size of the patient group sector, shows 20,841 patient groups in the uK, most of which are local or regional. In a survey of 170 local or regional groups, Patientview found that 89 per cent of groups supply information to patients, 80 per cent offer peer-to-peer support, 45 per cent provide advocacy on behalf of patients, 36 per cent raise money for medical research, and 18 per cent supply healthcare services such as cancer screening. Scaling this up shows there could be well over 3,000 patient groups supplying services in the community. This represents a great opportunity for more care to be delivered in the research study A randomised trial investigated the impact of pharmacist interventions for heart failure patients: home visits by pharmacists who provided education about conditions and medication to patients, and gave follow-up advice to GPs. There were no significant differences in hospital admissions at six months, quality of life, or mortality between the two groups. In addition, analysis suggested overall primary care activity (including home visits, attendances at general practices, and phone calls) increased by 17 per cent (Holland et al, 2007). community and empower patients, but requires patient groups and other elements of the health and social care workforce to support and complement each other. Better links need to be forged between all elements of the community workforce to maximise these opportunities. redesigning the gP practice workforce: Case management Increasing numbers of GP patients are older people, and are likely to have many professionals involved in their care, for example district nurses, domiciliary care workers, and community workers who specialise in specific long-term conditions. Case management is needed to coordinate the input of these professionals. This is often done by GPs, but to varying degrees of success because of the time required. GPs are an expensive resource to use for this activity, which could potentially be done by another member of the community workforce, such as a community matron. It would require organisational and time management skills. It would also entail a good understanding of different professions’ roles and the services available, and how to draw on these roles and services. the role of technology There is potential to use the wider community workforce more effectively, but technology may also play a role in addressing these challenges. Telehealth and telecare could have an impact over the short-medium term, and may even transform the whole community model. As the system becomes increasingly complex, with sub specialities and multiple services available, complex decision-support tools could be developed. This could lead to a situation where there is a role in primary care to help direct patients to the services they need. BPC Community care:Layout 1 07/10/2013 12:43 Page 4 workForCe BrIeFIng what are the implications for education and training? Delivering more care in the community (and using the community workforce to alleviate pressure on GPs and improve joint working) will require an increase in the proportion of the health and social care workforce based in the community. Recent CfWI engagement found the majority of nurses continue to work mainly in hospitals, and that any progress with shifting care into the community has tended to happen on a local scale and in specific areas such as mental health (CfWI, 2013). The number of full-time equivalent (FTE) community nurses has only marginally increased over the last decade, from 14.5 per cent of qualified nurses in 2001 to 15.1 per cent in 2011 (RCN, 2012). One of the main barriers is the lack of change in the education and training approach, and in the curriculum to develop future nurses (CfWI, 2013). It may be important to deliver more training in the community to prepare members of the workforce to work in this setting, addressing both the skills they need and expectations about what their job will involve. The age demographic of the existing community nursing workforce is older than that of acute nurses. This suggests that newly qualified nurses are still working in acute rather than community settings after their training. In Guy’s and St Thomas’ Foundation Trust, a ward and community rotation programme, supported by a ‘buddy’ scheme, is currently being piloted to encourage nurses to work in both acute and community settings. Great Ormond Street Hospital (GOSH) has combined inpatient and outreach roles to expose nurses to working across settings, enabling greater flexibility and integration of care (CfWI, 2013). Training workforces together could improve joint working across health and social care workforces. This could normalise the concept of joint working, and remove some of the oft-mentioned barriers around different languages and cultures. The Surrey Health & Social Care joint Training Partnership (SjTP) is a collaboration between health and social care agencies which delivers joint learning and development training. This learning and training enables health and social care staff to train together with service users, carers and members of the voluntary sector to support the delivery of integrated care (Surrey County Council/The learning Enterprise, 2012). New roles may also be developed in the future, with implications for education and training. In 2010, Skills for Health developed scenarios to consider possible future workforce roles, one of which was ‘personal health navigator’ (Skills for Health, 2010). This person could be a care coordinator, carrying out activities such as advocate, broker and information organiser. Another future role identified was a level 4 generic community worker. This role could involve working with people with long‐term conditions and would be part health, part social care and part education. references Ballantyne Pj (2011). Assessing pharmacists’ impacts in primary health care: are we asking the right questions? Southern Med Review 4(1), 17-21. Accessed online Mar 2013: http://apps.who.int/medicinedocs/ documents/s18432en/s18432en.pdf Centre for workforce Intelligence (2013a). GP In-depth review, preliminary findings. Accessed online Apr 2013: www.cfwi.org.uk/ publications/gp-in-depth-review-preliminaryfindings Centre for workforce Intelligence (2013b). Shift of Care: Acute to Community. unpublished report deloitte (2012). Primary Care Today and Tomorrow. Accessed online Mar 2013: www.deloitte.com/view/en_GB/uk/researchand-intelligence/deloitte-research-uk/ deloitte-uk-centre-for-health-solutions/ bb6e38f609817310vgnvCM3000001c 56f00aRCRD.htm department of Health (2005). Choosing Health through Pharmacy: A programme for pharmaceutical health 2005-15. london: Department of Health Health and Social Care Information Centre (2009). Trends in Consultation Rates in General Practice 1995-2009. Accessed online Mar 2013: www.hscic.gov.uk/article/ 2021/Website-Search?productid=729&q= general+practice+consultation+rates& topics=13204&sort=Relevance&size= 10&page=3&area= both#top © 2013 Centre FOR workForCe IntellIgenCe Holland r et al (2006). Where now for pharmacist led medication review? Journal of Epidemiology and Community Health, 60 (2), 92-93. Holland r et al (2007). Effectiveness of visits from community pharmacists for patients with heart failure: Heart Med randomised controlled trial. BMJ 334: 1098. Accessed online Mar 2013: www.bmj.com/content/ 334/7603/1098 imPower (2013). Home Truths: GPs inflate demand for residential care. Accessed online Mar 2013: www.impower.co.uk/en/ hometruths-gps-inflate-demand-for-residentialcare-403.html kPmg (2013). Value Walks: successful habits for improving workforce motivation and productivity. Accessed online Apr 2013: www.kpmg.com/Global/en/ IssuesAndInsights/ArticlesPublications/ value-walks/Documents/improvingworkforce-motivation-productivityv3.pdf laurant m et al (2004). Impact of nurse practitioners on workload of general practitioners: randomised controlled trial. BMJ, 328: 907. Accessed online Mar 2013: www.bmj.com/content/328/7445/927 laurant m et al (2009). Cochrane summary: shift of provision from doctors to nurses. Accessed online Mar 2013: http://summaries.cochrane.org/CD001271/ in-primary-care-it-appears-thatappropriately-trained-nurses-can-produceas-high-quality-care-and-achieve-as-goodhealth-outcomes-for- patients-as-doctors. -however-the-research-available-is-quitelimited Parle and ross (2012). Briefing document on Physician Assistants/Associates for Health Education England. unpublished report. royal College of nursing (2012). Policy Briefing 09/12: The Community Nursing Workforce in England. Accessed online Mar 2013: www.nursingtimes.net/Journals/2012/05/ 11/u/q/b/The-Community-NursingWorkforce-in- England.pdf Skills for Health (2010). Rehearsing Uncertain Futures: Full Report. Accessed online Mar 2013: www.skillsforhealth.org.uk/ component/ docman/doc_view/344rehearsing-uncertain-futures.html Surrey County Council (2012). Plans for social workers to join GP surgeries. Accessed online Mar 2013: http://news.surreycc.gov.uk/ 2012/06/ 28/plan-for-social-workers-tojoin-gp-surgeries/ Surrey County Council and the learning enterprise (2012). Surrey Health and Social Care Joint Training Partnership- Course Programme April 2012-March 2013. Accessed online Mar 2013: www.surreycc.gov.uk/__data/assets/pdf_file /0005/486833/Surrey-Health-and-SocialCare-Joint-Training-Brochure.pdf the american academy of Physician assistants (2010). Annual Physician Assistant Census 2010. Accessed online Apr 2013: www.aapa.org/uploadedFiles/ content/Research/2010%20Census%20 Report%20National%20_Final.pdf
© Copyright 2025