Last Chance for Early Registration Discounts
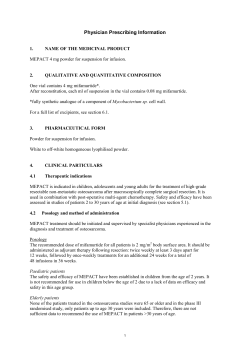
volume 21
Your Monthly AAN Membership Magazine
issue 12
december 2008
Last Chance for Early Registration Discounts
for Winter Conference in Sunny Florida
December 15, 2008, is your last chance
to save with early registration and hotel
discounts for the 2009 AAN Winter
Conference in the “Sunshine State”
of Florida. Register quickly and easily by
visiting www.aan.com/winter09 today.
• Obtain the latest updates in neurology
from a faculty of renowned experts
on a variety of topics
Set for January 16 through 18 at Disney’s
Contemporary Resort in Lake Buena Vista,
the Winter Conference will serve as a
welcome retreat from the cold of winter,
offering top education programming in a
compact, three-day weekend.
• Network one-on-one with some of the
top experts in your areas of interest
The Winter Conference provides an
excellent opportunity to:
• Earn up to 19.5 AMA PRA Category
1 credits™
• Benefit from the intimate atmosphere
of a smaller conference size
• Learn how to recognize and proactively
avoid financial or legal pitfalls
• Fulfill your continuing medical
education requirements as a necessary
step towards Maintenance of Certification
This year’s program includes:
• Friday, January 16
- How to Treat Neurological Disease
with Botulinum Toxin Workshop
© Disney
“Participants will interact with outstanding
faculty with renowned expertise in their
neurologic subspecialty and wonderful
teaching skills,” said Steven L. Lewis, MD,
FAAN, director of the Winter Conference’s
Neurology Update Program.
• Discover effective tips on how to
code correctly and receive the
compensation that you deserve
- Neurology Update I
- Practice Management 202:
Expanding Your Practice: What You
Need to Know to Ensure Success
- Therapy Program: Multiple Sclerosis
- Practice Management 102: Coding
and Billing—A Case-Based Approach
Continued on page 9
New Endowment Fund Created to Support
Medical Students, Residents, Fellows
A generous donation to the AAN Foundation
has established the Dr. Mario and Dianne
Oliveira Neurology Education Endowment
Fund, named for the longtime neurologist
and his wife, who is a former president
and board member of the AAN Alliance.
They have created a permanent endowment
through their estate plan to fund scholarships
to medical students, residents, and fellows
to attend education and scientific
programming offered by the AAN.
p4
Presidential Plenary Session
Features Clinically Relevant
Research
“Neurology has had a major impact in my
life and in the lives of the patients whom
I was able to help throughout the years,”
said Mario M. Oliveira, MD, FAAN. “The
American Academy of Neurology was a
strong force in allowing me to maintain
proficiency in this ever-fascinating field.
By making this gift of education, I hope
to give others the opportunity to follow
a similar path.”
Continued on page 22
p10
Continuum Explores
Latest in Acute Ischemic
Stroke Care
Dr. Mario and Dianne Oliveira
p15
Alzheimer’s Visionary
Is AAN Advocate
of the Year
table of contents
Official publication of the
american academy of neurology
Cover |Last Chance for Early Registration
Discounts for Winter Conference
in Sunny Florida
New Endowment Fund Created
to Support Medical Students,
Residents, Fellows
13–14 | membership
13 Last Chance to Renew Your AAN
Membership, Continue Benefits
13 Application Deadline for Journalism
Fellowship Award Is January 9, 2009
14 AAN Partner Offers Toll-Free Risk
3 | President’s Column
3 Grassroots Advocacy Provides
Fulcrum for Change
Management Consultation Service
15–16 | Advocacy IN ACTION
15 Alzheimer’s Care Visionary Named
4–9 | annual meeting
4 2009 Presidential Plenary Session
Features Clinically Relevant Research
5 Enjoy Convenience of Online
Registration for 2009 Annual Meeting
6 Annual Meeting Opportunities Improve
Your Practice
8 Continuum-based Education Course
Offered at Annual Meeting
AAN Palatucci Advocacy Leadership
Forum Advocate of the Year
16 2009 Neurology on the Hill Gives
Members a Voice in Washington
17 | focus on practice
17 Electronic Prescribing Offers Speed,
Convenience, Savings
8 Call for Artists: Auction Gallery to
Showcase Member Works
21 | MEMBER BENEFITS
8 Free Special Events for New and
International Members
22–23 | foundation
9 2009 Neuro Idol Seeks Members
with Unique Talents
22Foundation Offers 60/60 Proposition
23 Foundation Friends
The Mission of the AAN is
to promote the highest quality
patient-centered neurologic
care and enhance member
career satisfaction.
The Vision of the AAN is to be
indispensable to our members.
Contact Information
American Academy of Neurology
1080 Montreal Avenue
St. Paul, MN 55116 USA
Phone:(800) 879-1960 or
(651) 695-2717 (Int’l)
Fax: (651) 361-4800
Email: memberservices@aan.com
Website: www.aan.com
AAN Executive Director
Catherine M. Rydell, CAE
Editor-in-Chief
James P. Kelly, MD
9 Volunteer Opportunities at
Annual Meeting Offer Savings
23 | other news
9–10 | EDUCATION
23 Apply Now for the UCNS NeuroOncology Certification Examination
Managing Editor
Jason Kopinski
10 2009 RITE Registration Deadline
Approaching
24 | DATES AND DEADLINES
Editor
Tim Streeter
25–31 | dENDRITE
Writers
Ryan Knoke
Jay Mac Bride
Sarah Parsons
Designers
Jim Hopwood
Siu Lee
Doug Forbes
Andrew Imholte
Dendrite Coordinator
Amy Schoch
Correction: In the November AANnews article on the Palatucci Advocacy Leadership
Forum attendees, Tissa Wijeratne, MD, should have been listed under Advisors, and
Robert E. Shapiro, MD, PhD, should have been listed under Faculty.
Email
aannews@aan.com
AANnews is published monthly
by the American Academy
of Neurology.
President’s column
Since the Academy’s State Affairs Committee (SAC) was established in 2003, it has complemented,
on a state level, our federal efforts spearheaded by the Legislative Affairs Committee. Combined,
they provide a two-pronged approach to promoting the profession of neurology and our patients’
needs, and we have grown collectively in our ability to be proactive in both venues. Thanks to the
SAC, we are enjoying more productive alliances with state neurology societies. If your state society
is contemplating growing, please call the AAN, as our dedicated staff is available to help in this
process. We also encourage AAN members to participate in our award-winning advocacy training
program, which is changing lives on a local level across the world.
Stephen M. Sergay, MB BCh, FAAN
President, AAN
Grassroots Advocacy Provides Fulcrum for Change
By William H. Fleming, III, MD
The mission of the Academy’s State Affairs Committee (SAC) is
simple: To promote the welfare of patients with neurologic disease
by development of advocacy efforts by the Academy’s member
physicians within their communities.
To better facilitate communication and cooperation, the SAC meets
alongside the Academy’s Legislative Affairs Committee, which
addresses federal legislation and advocacy, during the Neurology
on the Hill event each spring. In the fall, the SAC meets with the
State Society Leaders Roundtable. The committee operates the
Palatucci Advocacy Work Group and the State Liaison Work Group.
The Academy continues to strengthen our outreach to the state
societies. At the recent third annual roundtable, 23 states were
represented by 30 participants, including several society executive
directors who offered valuable perspectives from their leadership
experiences. Participants heard a presentation on member
recruitment and retention strategies, and discussed such topics
as funding challenges, planning strategies for meetings, legal
questions, and advocacy issues.
Through mid-November, our advocacy staff attended 21 state
neurology society meetings and interacted with more than 700
society members, with plans to attend five additional meetings in
2008. Academy-hosted speakers have given more than a dozen
presentations on topics related to advocacy, medical economics,
and practice in 2008. This outreach has helped strengthen these
state organizations and kept us in the loop on threats to our
profession and quality of care.
The Donald M. Palatucci Advocacy Leadership Forum is our
committee’s most visible program, and we are pleased to report
we received a record 94 applications for training in San Diego this
January. We look forward to the addition of 30 new advocates to
the 180 members who have participated in the program since 2003
and are actively working on behalf of neurology in their states and
communities. We are also thankful to UCB, Inc. for continuing to
fund the program again in 2009.
The Academy has been tracking or actively
engaged in numerous bills that have been
passed or continue to be contemplated
by state lawmakers. These topics have
garnered considerable attention and likely
will be hot-button issues in 2009:
Anti-epilepsy Drugs: AED bills were
introduced in 15 states in 2008. A
new law was passed in Utah, while
significant action was taken in
Connecticut and Pennsylvania.
William H. Fleming, III, MD
Stroke: Significant stroke legislation was passed in Georgia,
Indiana, Missouri, Oklahoma, Tennessee, and Virginia.
Mandatory Reporting: Legislation to repeal mandatory
reporting provisions in California was vetoed by Governor
Schwarzenegger. Michigan legislators are contemplating a
bill to give physicians immunity from civil or criminal liability
should they choose not to report any knowledge or concerns
about a person’s physical or mental qualifications to operate
a motor vehicle.
Stem Cells: Several stem cell initiatives were introduced in
state legislatures across the country. Earlier this year, Louisiana
prohibited any use of public funding for stem cell research.
EMG: Bills have been introduced in New York and New Jersey
that would limit to licensed physicians the right to practice
needle EMGs.
We anticipate another very busy year in 2009, and we urge all
AAN members—inside and outside the US—to get involved in
grassroots advocacy, whether in their city, county, state, prefecture,
or province. You can be the difference between poor health policy
and the quality care our patients deserve.
AANnews • December 2008
annual meeting
2009 Presidential Plenary Session Features
Clinically Relevant Research
Clinically relevant research will be presented by leading lecturers
at the 2009 Presidential Plenary Session at the 61st Annual Meeting
in Seattle. The session will take place on Tuesday, April 28 from
9:00 a.m. to 12:00 p.m. in the Washington State Convention and
Trade Center and is open to all meeting participants. The session,
moderated by Stefan M. Pulst, MD, FAAN, Science Committee and
Scientific Program Subcommittee Chair, concludes with the annual
AAN business meeting. Lectures include:
Presidential Lecture
Stephen M. Sergay, MB BCh, FAAN
AAN President, Tampa, FL
“Doctoring, 2009: Embracing the Challenges to the Ethos of the Physician”
Stephen M. Sergay, MB BCh, FAAN, was
born in Johannesburg, South Africa,
and educated at the University of
Witwatersrand in Johannesburg,
graduating from medical school in 1970.
Stephen M. Sergay,
MB BCh, FAAN
Following post-graduate medical training
in hospitals in Johannesburg, he moved to
the United States and obtained his neurologic training at the
Peter Bent Brigham, Beth Israel and Children’s Hospitals Program
in Boston. Sergay worked as a neurologist at the Lahey Clinic
Foundation in Boston before moving to Tampa, where he is the
managing partner of a five-person neurology group.
Sergay has chaired the AAN Membership Committee and the
Public and Professional Information Committee (now known as
the Public Relations Committee), and served on the Foundation
Board of Trustees, where he ran its strategic planning. He led the
1997 AAN Strategic Planning and chaired the AAN Commission
on Subspecialization. This commission resulted in the creation of
the United Council of Neurologic Subspecialties, which he chaired
from 2003 to 2006. He has served on the AAN Board of Directors
and has been president since April 2007. He also serves on the
boards of AAN Enterprises, Inc., and the AAN Foundation. Sergay
is the AAN representative to the World Federation of Neurology,
and has been appointed to its education executive committee and
Africa task force.
As AAN President, Sergay’s focus has been on creating a more
strategic, nimble, and proactive Academy, with more data-driven
decision-making. On taking office, he initiated the Future of the
Profession and AAN Task Force to set in place a method of
accomplishing his goals. His core values as a neurologist and
Academy member are embodied in the AAN’s present mission
statement. Sergay strongly believes that the AAN’s primary focus
is the neurologist, and will work to center Academy priority-setting
with this in mind during the remainder of his term.
December 2008 • AANnews
Robert Wartenberg Lecture
Kenneth M. Heilman, MD, FAAN
University of Florida, Gainesville, FL
“Cognitive Motor Disorders: The Apraxias”
Born in Brooklyn, NY, Kenneth M.
Heilman received his medical degree from
the University of Virginia in 1963 and
trained in medicine at Cornell-Bellevue.
He was chief of medicine at USAF-NATO
Hospital, Izmir, Turkey (1965 to 1967).
Kenneth M. Heilman,
MD, FAAN
After discharge, he took a neurology
residency-fellowship at the Harvard
Neurological Unit (Boston City) with
Drs. Denny-Brown and Geschwind. He joined the faculty at the
University of Florida in 1970 as an assistant professor, and was
later promoted to associate professor (1973), professor (1975), the
James E. Rooks, Jr., Professor (1990), and Distinguished Professor
(1998). He is also a professor of psychology and chief of the
VAMC Neurology Service. As director of the behavioral
neurology/neuropsychology post-doctoral program, he has
trained more than 60 fellows, many of whom are now leaders.
His research has focused on four domains: attention-neglect,
cognitive-motor systems-apraxia, emotional communication,
and creativity. He is the author, co-author, and/or editor of
14 books and more than 500 publications. Heilman and his
coworkers have described several new diseases/syndromes,
including orthostatic tremor.
His membership in honorary organizations and honors include
Alpha Omega Alpha, Sigma Xi, the Dana Foundation, and the
University of Florida Clinical Research Award and Lifetime
Achievement Award. He is a past president of the International
Neuropsychology Society and the Society for Cognitive and
Behavioral Neurology, which gave him the Outstanding
Achievement Award. The American Speech and Hearing
Association gave him its Distinguished Service Award. He is an
Honorary Member of the American Neurological Association
and a Fellow of the AAN, where he has served on numerous
committees and subcommittees, including the Science
Committee and the Norman Geschwind Prize in Behavioral
Neurology Subcommittee.
Houston H. Merritt Lecture
Louis R. Caplan, MD, FAAN
Beth Israel Deaconess Medical Center,
Boston
“‘Evidence’ and the Effective
Clinical Neurologist”
Louis R. Caplan, MD, FAAN, was born in
Baltimore. He attended Williams College in
Williamstown, MA, and the University of
Maryland Medical School and graduated
Louis R. Caplan, MD, FAAN
summa cum laude and valedictorian in
1962. Caplan was an intern and junior resident in medicine at
the Boston City Hospital from 1962 to 1964. During this time,
he decided to become a neurologist. He was stimulated by
neuroanatomy professors Drs. Nauta and Kuypers in medical
school, but contact with Dr. Derek Denny-Brown, the chief of
neurology at Harvard and the Boston City Hospital Harvard
Neurological Unit, cemented his choice. Neurologists were few
at that time, and advisers told him that he would also have to
practice psychiatry to earn a living.
From 1962 to 1964, Caplan served in the US Army as an internist
but worked in the neurology clinic. He returned to Boston and did
neurology residency from 1966 to 1969 on the Harvard
Neurological Unit at the Boston City Hospital under Denny-Brown.
During the 1969 to 1970 year, he was a Cerebrovascular Disease
Fellow at the Massachusetts General Hospital with Dr. C. Miller
Fisher. In July 1970, he became a staff neurologist at the Beth Israel
Hospital in Boston and Assistant Professor of Neurology at Harvard
Medical School. He and Dr. Jay P. Mohr founded the Harvard
Cooperative Stroke Registry. In 1978, Caplan moved to Chicago
to become neurologist-in-chief at the Michael Reese Hospital and
professor of neurology at the University of Chicago. He returned to
Boston in 1984 to become neurologist-in-chief at the New England
Medical Center and professor and chairman of the Department
of Neurology and professor of medicine at Tufts. In 1998, Caplan
returned to the Beth Israel Deaconess Medical Center and Harvard
Medical School. He is now professor of neurology at Harvard
Medical School and senior neurologist at the Beth Israel Deaconess
Medical Center, Boston.
Caplan has been the author or editor of 35 books and more than
600 articles and chapters in medical journals and books. He has
been the chairman of the Stroke Council of the American Heart
Association and a number of neurological and stroke organizations.
He has been on the editorial board of 29 medical journals. He has
trained 58 stroke fellows, including 28 international fellows.
Enjoy Convenience of Online Registration
for 2009 Annual Meeting
Planning your visit to the Annual Meeting in Seattle can be made easy by
visiting www.aan.com/amrapreg. The website allows you to search the entire
Education Program, book hotel and travel arrangements, and mark your
calendar for important events.
Early Registration Savings Deadline: March 20, 2009
Register early to avoid increased general registration and Education Program
fees. Any registrations received after March 20 will not be processed. After
March 20, registration is available on-site only. On-site registration opens at
8:00 a.m. on Saturday, April 25, at the Washington State Convention and
Trade Center. US and Canadian registrants who submit their registration form
before March 20, will receive Annual Meeting name badges and Education
Program tickets by mail.
Abstract Authors to Receive Notification in Late January
Authors who have submitted abstracts for the 2009 Annual Meeting will be notified by mail at the end of next month whether their
abstract was accepted for the Scientific Program.
For more information, contact Erin Jackson at ejackson@aan.com or (651) 695-2704.
AANnews • December 2008
annual meeting
Annual Meeting Opportunities Improve Your Practice
The 2009 Annual Meeting provides a variety of opportunities to
help members begin their practices, improve practice efficiency,
learn about advocacy, and keep current with the latest in coding,
reimbursement, and office technology.
BRAINS Colloquium
Saturday, April 25, 1:00 p.m.–5:00 p.m.
The BRAINS Colloquium is intended to provide attendees with
up-to-date information on the “business” of neurology and an
opportunity to further develop practice management skill sets.
Faculty will address the logistics of taking calls and the different
calling options, implementing an electronic health record, as well
as salary and staffing issues that come along with an atmosphere
of declining reimbursement.
Practice Course: Starting Your Career:
The Early Years
Saturday, April 25, 6:00 p.m.–8:00 p.m.
Earn 2.0 CME credits in this course designed for residents or
fellows who are making initial career decisions. Faculty will
cover the essentials in evaluating the academic, private practice,
administrative, and regulatory position options in neurology,
including an overview of the job opportunities, how to negotiate
initial work-related contracts and conditions, incorporation of the
latest electronic-based tools in your workplace, and how to achieve
career goals.
Patient Safety Colloquium: Medication Safety Across
Your Practice Settings
but the evidence on what works and what doesn’t work regarding
improved health care efficiency and outcomes has been mixed.
The purpose of this colloquium is to review the best available
evidence on P4P, particularly with regard to improving the quality
of primary versus specialty (neurologic) care. Specific models of
P4P that have shown the most promise in large health care systems
will be emphasized.
Guidelines, Practice, and Advocacy Open House
Sunday, April 26, 9:00 a.m.–12:00 p.m.
Featuring Digital Demos: Technology Solutions that You Can Afford
This colloquium will empower neurologists to participate in the
implementation of medication safety and understand safety
issues related to herbal medication and medication interactions.
Additional objectives include learning the value of internet
tools and safe prescribing practices. The colloquium enables
neurologists to develop patient safety initiatives for patients with
neurologic conditions.
Monday, April 27, 3:00 p.m.–5:30 p.m.
Practice Colloquium: Improving Quality Through
Incentives: Lessons from Model Programs
Sunday, April 26, 1:30 p.m.–4:30 p.m.
Incentivizing quality—or “pay-for-performance” (P4P)—has
received substantial national emphasis over the past several years,
Attendees enjoyed the practice information available at the 2008 Guideline, Practice,
and Advocacy Open House.
December 2008 • AANnews
Get your copy of the AAN Spring 2009 Quality CD with guideline
and clinical performance measure tools before they are gone!
Talk with authors of guideline and clinical performance measures
posters. Discover how measures can improve the quality of
care you provide. Learn how you can get involved in advocacy
efforts, implement patient safety tips, use performance measures
in everyday practice, and stay current with the latest in coding and
reimbursement. Attend the “Digital Demos” presentation to learn
about low-cost, easy-to-implement electronic office solutions
that can help move your practice into the 21st century and take
advantage of Medicare PQRI bonuses. Free to all attendees.
Please RSVP to guidelines@aan.com by Wednesday, April 22.
Controversial Issues in Practice Session
• E/M: Minimize Mistakes, Maximize Reimbursement
(Wednesday, April 29)
Wednesday, April 29, 5:15 p.m.–7:00 p.m.
This session will highlight a yet-to-be-announced hot topic
in the practice of neurology.
Coding Lunches
Get the latest reimbursement updates at six coding lunches
from 12:00 p.m.–1:00 p.m., covering a range of disorders:
• Neuromuscular Disease (Sunday, April 26)
• Dementia (Monday, April 27)
• Cerebrovascular Disease (Monday, April 27)
• Child Neurology (Monday, April 27)
• Movement Disorders (Friday, May 1)
Avoid reimbursement denials and reduce liability with the
Academy’s Practice Survival Kit. This specially priced
package includes everything you need for accurate coding,
including online reference, E/M pocket coding guide, and a
CD filled with practice syllabi. Save on all three when you
buy the Practice Survival Kit, or purchase separately the
practice tools you need most. Stop by the AAN Store™ and
pick yours up before they are gone! Other practice tools are
available at the AAN Store.
Earn Additional AAN Benefits When You Attend
Practice Courses
• Epilepsy (Friday, May 1)
Practice Courses
Gather the basics of coding, practice management, and incorporating
electronic health records into your practice at these courses:
• The Practice of Neurology: Issues in Coding and
Reimbursement (Saturday, April 25)
• Making Sure Your Electronic Health Record System is a
RED: Annual
Meeting
Award Luncheon
Ad
Success
(Sunday,
April 26)
Usage: To be placed in AANnews
Specs: 8.5” x 5.5” (full bleed +.125”): 4C
Practice Survival Kit from the AAN Store
AAN members can earn additional benefits when they attend
Annual Meeting practice courses. Some courses qualify you for
a discount on malpractice insurance when you attend a practice
course at the Annual Meeting. Visit the AAN Partners Program
booth at the AAN Store for details.
For more information about practice-related events, visit
www.aan.com/AMpractice.
Join AAN Leaders in Honoring the Best
and Brightest in Neuroscience Research!
Wednesday, April 29, 12:00 p.m.–1:30 p.m.
Grand Ballroom A-D, Sheraton Seattle Hotel
Reserve your tickets today—or reserve an
entire table for your department—for the
2009 American Academy of Neurology/
American Academy of Neurology
Foundation Awards Luncheon.
From enterprising high school students
to world-renowned researchers, this
not-to-be-missed event recognizes the
top accomplishments in neuroscience
research. Individual tickets are $50.
Department tables can be reserved.
Medical students and Junior members
of the AAN may attend this event at no
cost by requesting a ticket.
Microsoft Co-Founder Paul G. Allen to Speak
Well-known philanthropist, Microsoft co-founder, and owner of the
Seattle Seahawks NFL and Portland Trail Blazers NBA franchises,
Paul G. Allen has been selected as the 2009 recipient of the Public
Leadership in Neurology Award. Allen will be honored for his
commitment to brain research, including his $100 million contribution
to the founding of the Allen Institute for Brain Science in his hometown
of Seattle.
Buy your tickets today!
www.aan.com/am
annual meeting
Continuum-based Education Course Offered
at Annual Meeting
New for 2009, the Annual Meeting offers a program that is
designed to help neurologists stay current in clinical practice.
Continuum Test Your Knowledge: A Multiple-Choice Question
Review covers a range of topics in general neurology and
neurology of systemic disease for 6.5 CME credits.
The program format uses case-based, multiple-choice questions
and brief didactic presentations. Faculty will engage participants
in clinical problem solving through audience participation. The
questions and supporting materials are derived from recent issues
of Continuum: Lifelong Learning in Neurology®.
“We’re excited to bring Continuum’s format to a course setting,”
said Ralph F. Józefowicz, MD, FAAN, program director and
Education Committee Chair. “Participants should be able to
increase and refresh their knowledge of core topics in neurology
through presentation of common and uncommon clinical
problems. Participants also should be able to work through
difficult clinical presentations both logically and successfully.”
This program, designed for practitioners, fellows, residents, and
academicians, will cover six subjects, each presented by a
preeminent expert in the field who has also demonstrated superior
skills at presenting material of this type
to large audiences. Expert faculty will
use the question-based format as a
springboard for discussion of timely and
important topics and developments across
the spectrum of neurology. The topics
and faculty are:
• Multiple Sclerosis: Aaron E. Miller,
MD, FAAN, New York
• Neuromuscular Diseases: Richard J.
Barohn, MD, FAAN, Kansas City
• Stroke: David Lee Gordon, MD,
FAHA, Oklahoma City
Ralph F. Józefowicz,
MD, FAAN
• Spinal Cord, Root, and Plexus Disorders: José Biller, MD, FAAN,
FACP, FAHA, Chicago
• Movement Disorders: Steven Frucht, MD, New York
• Neurologic Manifestations of Systemic Disease: Steven L.
Lewis, MD, FAAN, Chicago
For more information, contact Kris Fridgen at kfridgen@aan.com
or (651) 695-2726.
Call for Artists: Auction Gallery to Showcase Member Works
The AAN is looking for member artists to
donate their creations to raise money for
research in neurology. Your work will be
displayed at the Art for Research: An AAN
Gallery Show at the Annual Meeting in
Seattle. Donated works will be sold with
the proceeds going to support clinical
research training in neuroscience. The
event is sponsored by the AAN Foundation
to support clinical research in neurology.
Pieces will be featured prominently in the
6th Floor, West Lobby throughout the week.
Academy members and/or their families
may donate pieces for the show. Members,
patients and their caregivers, and industry
representatives may participate three ways:
• Donate a piece of art for the AAN to sell
• Sell a piece of art with partial proceeds
going to support research
• Submit art for showcase only for a fee
The Gallery Show accepts paintings,
sculptures, textiles, ceramics, and more. For
additional details on this event and to learn
how to contribute, contact Valerie Mendoza
at vmendoza@aan.com or (651) 695-2730.
Free Special Events for New and International Members
The Academy invites new and international members to attend free
special programs at the Annual Meeting to help them get the most
out of their AAN membership.
New Member Information Session
A New Member Information Session on Sunday, April 26, from
5:00 p.m. to 6:00 p.m., is free and open to all new AAN members
who joined the Academy since January 1, 2009. This first-time
event is designed to welcome these new members into the Academy
and help them learn about the AAN, its resources, and benefits.
Attendees can enjoy refreshments and camaraderie as they network
with Academy leaders and their fellow neurology professionals.
December 2008 • AANnews
International Attendee Summit
The International Attendee Summit on Monday, April 27, from
7:00 a.m. to 9:00 a.m., offers an excellent opportunity for
international meeting attendees to meet with Academy leadership
and have their voices heard on matters significant to them. There
will be an opportunity to socialize and share perspectives with
ellow international colleagues.
Members interested in attending these events are asked to reserve
their space by contacting Laurie Weyandt at lweyandt@aan.com
or (651) 695-2799.
2009 Neuro Idol Seeks Members with Unique Talents
If you have a talent and a secret desire to perform in front of an audience, then Neuro Idol
may be your big break!
The AAN is looking for performers to take the spotlight and showcase their musical and other
talents during Neuro Idol at the Annual Meeting Celebration for Research. Returning for its
fourth year, this cabaret-style show is a big hit at the Annual Meeting, with previous acts that
have included rock and classical musicians, vocalists, and magicians.
Don’t keep your talents hidden any longer. Share them with your colleagues and join in on the fun!
To sign up to be a performer, or for more information, contact Erin Jackson at
ejackson@aan.com or (651) 695-2704.
Volunteer Opportunities at Annual Meeting Offer Savings
The Annual Meeting offers several opportunities for members to
volunteer their time and talents and obtain free Annual Meeting
registration, program, and workshop fees, and other benefits.
Education and Scientific Program Monitors
Monitors are needed for all Education Program offerings and
scientific platform sessions to distribute and collect evaluation
materials and assist directors, faculty, session co-chairs, and staff
as required. The AAN will waive all monitors’ Annual Meeting
registration and program fees as well as grant CME credit for the
monitored program. Space is available on a first-come, first-served
basis. For an application form or more information, contact
Kyle Krause at kkrause@aan.com or (651) 695-2733.
EMG Skills Workshop Volunteers
Volunteers are needed to participate in the EMG Skills Workshops
on Monday, April 27, from 9:00 a.m. to 6:00 and on Friday, May 1,
from 9:00 a.m. to 6:00 p.m. Participants will receive a waived meeting registration and workshop fee as well as payment of $40 per
noninvasive session and $60 per invasive session. Space is available
on a first-come, first-served basis. For more information, contact
Naomi Soderbeck at nsoderbeck@aan.com or (651) 695-2814.
education
Last Chance for Early Registration Discounts
for Winter Conference in Sunny Florida
Continued from cover
• Saturday, January 17
- Neurology Update II
- Practice Management 302: Shaking
the Practice Tree—How to Get More
Fruit to Your Practice’s Bottom Line
- Epilepsy Update
• Sunday, January 18
- Neurology Update III
The December 15 early registration
deadline is quickly approaching. Save
on registration and hotel costs by visiting
www.aan.com/winter09 today. For more
information, contact Member Services at
(800) 638-3030 or Naomi Soderbeck at
nsoderbeck@aan.com or (651) 695-2814.
The 2009 AAN Winter Conference is an
ABPN-approved program for Maintenance
of Certification that is geared toward
practitioners, academicians, residents,
fellows, practice managers, and office
administrators.
Learn About the AAN’s
New Malpractice Insurance
Program at the Winter
Conference
Neurology-specific malpractice insurance
is available to Academy members through
The Neurologists Program (TNP)—the only
program designed exclusively for neurologists. TNP staff will attend the AAN Winter
Conference to answer questions about
insurance through TNP, and to provide more
information about risk management resources
designed for neurologists. The TNP is a
member benefit made possible by the AAN
Partners Program. For more information,
visit www.tnpinsurance.com or call
(800) 245-3333.
AANnews • December 2008
education
Continuum Explores Latest Developments
in Acute Ischemic Stroke Care
This month’s issue of Continuum: Lifelong
Learning in Neurology® focuses on new
approaches to care for acute ischemic
stroke and offers the reader an opportunity
to earn up to 10 hours of AMA PRA
Category 1 Credit™. This issue also contains a Quintessentials® module, which
has been approved for 3 AMA PRA
Category 1 Credits.
“It is critically important for neurologists
to be armed with current acute stroke
information that can empower them to
lead primary stroke centers and have the
knowledge base to treat their stroke patients
in a timely and effective manner.”
“In the past few years important progress
has been made in several areas of acute
ischemic stroke that are cogently reviewed
in this issue of Continuum with an eye
towards delivering practical information to
the clinician,” said Faculty Chair Steven R. Levine, MD, Professor of
Neurology and Director of Cerebrovascular Education at the Stroke
Center at the Mount Sinai School of Medicine and Medical Center.
“It is critically important for neurologists to be armed with current
acute stroke information that can empower them to lead primary
stroke centers and have the knowledge base to treat their stroke
patients in a timely and effective manner.”
This issue of Continuum begins with diagnosis of stroke and
stroke mimics in the emergency setting, and then investigates the
pathophysiology of and intervention for acute ischemic stroke.
Complications, prevention, and management of ischemic stroke
are then explored, along with emerging therapies. Subsequent
chapters address primary stroke center certification and a
“how to” guide for clinicians interested in becoming involved
in clinical stroke research. Completing the issue are discussions
of ethical perspectives and practice issues in neurology, and a
series of self-assessment tools, including the Quintessentials
practice improvement module.
Upon completion of this course, participants will have
been provided:
• An approach to understanding the pertinent history,
clinical evaluation, and management of the patient with
acute ischemic stroke
• The differential diagnosis of a potential patient with
acute ischemic stroke, including stroke mimics, in the
emergency setting
• A current understanding of the pathophysiology of acute
ischemic stroke, including why we approach acute stroke
the way we do
• A review of current acute ischemic stroke interventions
(US Food and Drug Administration approved and evidence-
10
December 2008 • AANnews
— Steven R. Levine, MD
based care, including IV thrombolysis, recombinant tissue-type
plasminogen activator)
• An overview of acute ischemic stroke rehabilitation
• A discussion of complications of ischemic stroke: prevention
and management (covering the most common and preventable
complications in the acute hospital setting)
• A review of emerging therapies for acute ischemic stroke
• A practical and comprehensive guide to the certification
of primary stroke centers (including The Joint Commission
requirements) and educating patients about stroke/stroke
education in the community
• A “how to” guide for private practitioners to become involved
in stroke research
The issue covers the following core competencies:
• Patient Care
• Medical Knowledge
• Practice-Based Learning and Improvement
• Interpersonal and Communication Skills
• Professionalism
• Systems-Based Practice
Continuum: Lifelong Learning in Neurology is published
six times per year and includes a multiple-choice self-assessment
examination. A Quintessentials module is also included twice
a year with certain Continuum issues. Subscribers have the
convenience of accessing CME online by visiting www.aan.com/
go/elibrary/continuum/cme, where they can complete the multiplechoice questions and receive CME credits within two business days.
To subscribe to Continuum, contact Lippincott Williams &
Wilkins at (800) 361-0633, (301) 223-2300 (international), or
www.lww.com/aancontinuumsub.
membership
Last Chance to Renew Your AAN Membership,
Continue Benefits
December 31 Deadline Approaching: Pay Dues Online Today
Members are encouraged to pay their AAN membership dues
before December 31, 2008, to avoid experiencing an interruption in
benefits. As an AAN member, you will want to take full advantage
of membership by keeping your dues current. Paying your 2009
AAN membership dues online is the quickest, easiest, and most
secure way to ensure that your benefits are protected. Renew today
at www.aan.com/dues.
As an Academy member, your involvement and dues revenue are
critical to the AAN’s ability to provide unparalleled support and resources for you and your profession. Because of your commitment
in 2008, the AAN was able to:
• Create eight new practice guidelines that can help improve
patient outcomes
• Advocate for your profession and patients with Congress
through Neurology on the Hill and other member-driven
activities like VOCUS
• Drive legislation that authorized the creation of the Epilepsy
Centers of Excellence at the Department of Veterans’ Affairs
• Raise $880,000 for clinical research training fellowships in
neurology, resulting in seven additional fellowships for
promising young researchers
• Offer a record number of courses at the 60th Annual Meeting
in Chicago
• Provide more ways to help you prepare for recertification with
the introduction of the NeuroSAE™ (Neurology Self-Assessment
Examination) and Continuum Online CME
• Develop new product offerings through the AAN Partners
Program and the AAN Store™—all designed to help you meet
your most challenging practice needs
In addition, your AAN membership provides you with a host of
other benefits including access to the members-only area of the
AAN website, and your subscriptions to the AAN’s premier
scientific journal Neurology®, Neurology Today®, AANnews®,
Neurology Now® patient magazine, and other Academy
publications designed to keep you abreast of the latest advances
in the field. Your AAN membership can pay for itself with
money-saving discounts on Annual Meeting and Regional
Conference registration. Keep up-to-date in your work with
access to invaluable continuing medical education, practice tools
and resources, advocacy representation and training, and a host
of other exclusive Academy products, programs, and services.
AAN membership dues have not increased for the 2009 year—
this is your opportunity to reap member benefits at an incredible
value. Complete your dues payment online today by visiting
www.aan.com/dues.
If you do not have online access, you may contact AAN Member
Services at (800) 879-1960 or (651) 695-2717 (international).
Students: Renew Your FREE AAN
Membership Today, Keep Benefits
in the Coming Year
Students also will want to be sure to renew their FREE
AAN membership by the December 31 deadline to ensure
their AAN member benefits are continued into 2009.
Simply print and complete the renewal form located at
www.aan.com/student and send it to the address or
fax number located at the bottom of the form. It’s that
easy—and it’s free!
Application Deadline for Journalism Fellowship Award
Is January 9, 2009
AAN members who are medical writers
are urged to apply for the 12th annual AAN
Journalism Fellowship Award, or encourage
medical journalists they are acquainted
with to submit applications. The Journalism
Fellowship Award is bestowed on journalists who exemplify excellence in medical,
health, and science reporting.
The AAN recognizes the important contributions made by members of the news
media who help raise the public’s awareness of neurologic disorders through print,
broadcast, and online news stories regarding
advancements in neurologic research.
Winners will receive special recognition,
airfare, and hotel with a five-night maximum
stay to attend the 2009 AAN Annual Meeting
in Seattle from April 25 to May 2, 2009.
More information on the award is available
at www.aan.com/go/press/journalism, or
contact Rachel Seroka at rseroka@aan.com
or (651) 695-2738.
AANnews • December 2008
13
membership
TNP Malpractice Insurance Offers
Online Education, Premium Discount
The Neurologists’ Program (TNP) malpractice insurance program has
launched a web-based education program specifically developed
for neurologists and available exclusively to TNP insureds. Upon
completion, participants will earn up to 5.25 CME credits and may
be eligible to receive a discount up to 10-percent on their insurance
premium with TNP.
Participants will receive a five-percent discount in addition to the
regular five-percent AAN member discount. This valuable risk
management program raises health care providers’ awareness of
patient safety and professional liability issues within clinical practice.
Program components include neurology standards of care, informed
consent, and documentation. In addition, TNP continues to
work with the AAN to develop risk management resources that
complement those already available through the Academy.
TNP is provided by Professional Risk Management Services, Inc.
(PRMS), through the AAN Partners Program, an extension of your
Academy member benefits.
To learn more about TNP, visit www.tnpinsurance.com or
call (800) 245-3333. For more information about member
benefits available through the AAN Partners Program, visit
www.aan.com/partners or contact AAN Member Services at
(800) 879-1960.
Malpractice Insurance Program Expands
TNP’s malpractice insurance for neurologists is now available
in New Jersey, along with Delaware, Georgia, Kentucky,
Massachusetts, North Carolina, Ohio, Pennsylvania, and
Washington, DC.
Educational, Pr actical, Powerful.
The AAN’s Award-Winning
Patient Education Magazine
" , Ê */
Ê6 Ê
/ 9
/
/-ÊEÊ
, Ê -ÊÊUÊÊn
ovembe
r/decem
ber 2008
Super Dad
&QJMFQTZ
)FSPFT
Greg Grunberg plays a gifted detective on the hit
show Heroes. But to his 12-year-old-son Jake, he’s
more than a TV hero. He’s a caregiver and advocate,
helping Jake overcome the daily challenges of living
with epilepsy and enjoy the gift of childhood.
&3("/%
(3&((36/# &/&44
4&"8"3
40/+",&3"* 065&1*-&14:
"#
&44
3*4,:#64*/ SNBJM
GP
"SFXFSFBEZ TUT UF
UJD
OF
HF
PSEFS
/P0OF
&4
63
5IF4&*;
"CPVU
8BOUTUP5BML
(3"7*4
.:"45)&/*" UJPOT
VMB
5SJBMTBOE5SJC
J[F
)PXUPNBYJN "/
ZPVS%36(1
DFQU
-FBSOJOHUP"D 04*4
&3
.6-5*1-&4$-
Tell your patients to join the more than 200,000 readers who have
signed up for FREE subscriptions at www.neurologynow.com.
•
Advocacy in action
Alzheimer’s Care Visionary Named AAN Palatucci
Advocacy Leadership Forum Advocate of the Year
Daniel C. Potts, MD, of Tuscaloosa, AL, has
been championing new approaches to care
for people with Alzheimer’s and dementia
that help them explore their untapped skills
and enhance the quality of their lives. For
his advocacy efforts in this area an d the
inspiring example of his leadership, Potts
has been named Palatucci Advocacy
Leadership Forum Advocate of the Year.
“The forum has changed my life, and
hopefully will change the lives of countless
suffering dementia patients and their
caregivers.”
— Daniel C. Potts, MD
“Before my selection to the Palatucci
forum, all I had was a story about my
father—powerful though it was—and the
desire to make things better for Alzheimer’s patients and their
caregivers,” said Potts, a graduate of the 2008 Donald M. Palatucci
Advocacy Leadership Forum. “The forum provided the means by
which to make the story known, and the tools and support to
create and implement an action plan to accomplish my goals. The
forum has changed my life, and hopefully will change the lives of
countless suffering dementia patients and their caregivers.”
Potts drew his inspiration from the experiences of his late father,
Lester, who was transformed from a rural Alabama lumberman to
watercolor artist when he participated in an art therapy program
at Caring Days dementia daycare center. The younger Potts has
since focused his advocacy efforts on dementia patients still living
in community settings and their caregivers. He promotes a model
of caregiving in which new or hidden talents in each patient are
sought out and developed, thereby promoting dignity, self-worth,
and caregiver respite. The comprehensive dementia daycare model,
of which Caring Days is an example, is being advocated on the
local, state, and national levels. Successes have included plans for
a capital campaign to expand the mission of Caring Days, securing
grant money to create and support mobile daycare centers in west
Alabama, articles on advocacy in national publications, speeches
to regional and national organizations that promote caregiver
respite, a presentation at the Alzheimer’s Association’s Dementia
Care Conference, and discussions with the AAN and Alzheimer’s
Foundation of America to develop legislation to support dementia
daycare centers nationally.
The board of Caring Days has adopted Potts’s plan to provide
dementia daycare in rural west Alabama, and is preparing a capital
campaign for a new facility and expanded services. Potts has
worked with the Area Agency on Aging to advocate for the west
Alabama region to host a pilot program for the concept of mobile
dementia daycare through a grant from the US Department of
Lester E. Potts, with his son Daniel and wife Ethelda, and a display of some
of his artwork.
Senior Services. Potts has spoken throughout Alabama, Tennessee,
North Carolina, and Mississippi about his advocacy plan, in
addition to giving a poster presentation at the Alzheimer’s
Association’s Dementia Care Conference in California.
Potts has written a book of poetry, The Broken Jar, illustrated
with his father’s art. Proceeds from the book go to Caring Days
to support its dementia care programs. Two art shows and a
walk to raise money for dementia daycare have also featured
The Broken Jar and the story of his father’s art.
Potts will bring his experience and insights to the 2009 Palatucci
Forum, where he will advise the new class of advocacy trainees.
AANnews • December 2008
15
Advocacy in action
2009 Neurology on the Hill Gives Members
a Voice in Washington
December 14 Application Deadline Approaching
Continuing the advocacy momentum that has led to real
health policy changes in Washington, the AAN will again host
Neurology on the Hill March 23 and 24, 2009, in Washington, DC.
The December 14 deadline to apply for the event is quickly
approaching and interested members are encouraged to visit
www.aan.com/noh09 today to apply.
For neurologists who don’t want to leave it up to Congress to
decide what is best for them and their patients, the seventh annual
Neurology on the Hill will allow them to make their voices heard
and give Washington a second opinion. The two-day event will
provide participants a unique opportunity to:
• Learn about current health care issues affecting neurology,
including physician reimbursement, and the need for increased
funding of the National Institutes of Health for research in
neurologic disorders
• Hear from Congressional leaders about the political process
• Take neurology’s message to their representatives and senators
• Develop working relationships with members of Congress,
their staff, and fellow neurologists
No prior experience is necessary, and the event is FREE for
Participants at the 2008 Neurology on the Hill.
participants. The AAN covers travel expenses, accommodations,
and meals, as well as provides training, tools, and talking points.
Applications must be received by December 14, but because
space is limited, interested members are encouraged to visit
www.aan.com/noh09 today to apply. For more information,
contact Melissa Larson at mlarson@aan.com or (651) 695-2748.
focus on pr actice
Electronic Prescribing Offers Speed, Convenience, Savings
The AAN Annual Meeting will offer “Digital
Demos: Technology Solutions That You Can
Afford,” a free event on April 28, 2009, in
Seattle. This is the third article in a series of
six designed to help members understand the
benefits and considerations regarding digital
technology in the office.
Currently, only 2 percent of the 1.47 billion
prescriptions written annually in the United
States are sent electronically. A study by
Brown University has suggested that by
using electronic prescribing software,
practices can reduce staff time spent on
refills from 87 minutes to 43 minutes per day.
“We also can use eRx software to send
prescriptions to the pharmacy, maintain our
medication list, check for insurance formulary
coverage, check for drug-drug interactions,
check for allergy contraindications, and check
for appropriate dosing regimen.”
Daniel B. Hier, MD, MBA, FAAN, a member of the Medical
Economics and Management Committee, has been an active user
of electronic prescribing (“ePrescribing” or “eRx”) for more than
five years. He has investigated a number of these programs and
will make a presentation on electronic prescribing at the Digital
Demos program.
—Daniel B. Hier, MD, MBA, FAAN
Hier notes that there are several packages available. “Some
ePrescribing software is available free of cost (for example eRxNow
at www.nationalerx.com). A variety of EHR vendors and IT vendors
now offer ePrescribing software that is compatible with the
SureScripts network for eRx. Among these vendors are Allscripts,
Zix, DrFirst, RxNT, eClinicalworks, eMDs, and NextGen. Costs
per month vary from free to as much as $20 to $30 per month
per physician.”
“Electronic prescribing has many potential benefits for neurologists,”
said Hier. “Our biggest gain from eRx comes from the ability to
refill prescriptions electronically. We can communicate directly
with pharmacists through the Internet over the Surescripts Pharmacy
Health Information Exchange. Nearly all eRx vendors use this
network to connect physicians to pharmacies. Using this network,
we can authorize refills on our patients without the need for a
paper prescription, a fax, or a phone call.
“We also can use eRx software to send prescriptions to the
pharmacy, maintain our medication list, check for insurance formulary
coverage, check for drug-drug interactions, check for allergy
contraindications, and check for appropriate dosing regimen.”
Currently, federal law prohibits prescribing many sedative and
narcotic drugs electronically, so not all drugs can be ePrescribed
at present. However, steps are being taken to relax these
federal restrictions.
The Centers for Medicare & Medicaid Services is anxious to see
physicians use electronic prescribing,” said Hier. “Under a new
Medicare payment bill that was passed in last summer, starting
in January 2009, physicians who prescribe for Part D patients will
get a 2-percent payment bonus. This bonus will phase down over
five years so that physicians using paper prescriptions in 2012 will
see a Medicare payment cut.”
Electronic prescribing software is either free-standing (not integrated
into an electronic health record, or “EHR”) or integrated (comes
with the EHR). Hier said that an eRx that comes integrated with the
EHR is more efficient because the allergy list, drug list, problem list,
and patient demographics are fully available through the EHR. With
a free-standing eRx module, some or all of this information may
need to be re-entered by the practice.
AANnews • December 2008
17
Genelle
ACTIVE
MOM
Previously on a
daily injectable
MS therapy
ACHIE
NOW WITH THE
THINNEST NEEDLE IN MS
BETASERON provides support as powerful
as the efficacy you depend on
BETAPLUS™
tAFFORDABLE
– Ensures qualified patients pay no more than $50 per month*
tDEPENDABLE
– Exclusive BETA Nurse access anytime, day or night
V ABLE
www.betaseron.com
Call BETAPLUS at 1-800-788-1467 to learn more
*Some restrictions apply. Patients enrolled in any type of government insurance are not eligible. Void where prohibited by law, taxed, or restricted.
BETASERON (interferon beta-1b) is indicated for the treatment of relapsing forms of multiple sclerosis to reduce the frequency of clinical exacerbations.
Patients with multiple sclerosis in whom efficacy has been demonstrated include patients who have experienced a first clinical episode and have
MRI features consistent with multiple sclerosis.
The most commonly reported adverse reactions are lymphopenia, injection-site reaction, asthenia, flu-like symptom complex, headache, and pain.
Gradual dose titration and use of analgesics during treatment initiation may help reduce flu-like symptoms. BETASERON should be used with
caution in patients with depression. Injection-site necrosis has been reported in 4% of patients in controlled trials. Patients should be advised of
the importance of rotating injection sites. Female patients should be warned about the potential risk to pregnancy. Cases of anaphylaxis have been
reported rarely. See “Warnings,” “Precautions,” and “Adverse Reactions” sections of full Prescribing Information.
BETASERON is a registered trademark of Bayer HealthCare Pharmaceuticals Inc.
Please see brief summary of full Prescribing Information on following page.
©2008 Bayer HealthCare Pharmaceuticals Inc.
Wayne, NJ 07470
521-09-0094-08a
Printed in USA.
All rights reserved.
August 2008
10011479
Brief Summary of Full Prescribing Information
INDICATIONS AND USAGE
Betaseron (Interferon beta-1b) is indicated for the treatment of relapsing forms of multiple
sclerosis to reduce the frequency of clinical exacerbations. Patients with multiple sclerosis
in whom efficacy has been demonstrated include patients who have experienced a first clin ical episode and have MRI features consistent with multiple sclerosis.
CONTRAINDICATIONS
Betaseron is contraindicated in patients with a history of hypersensitivity to natural or recombinant interferon beta, Albumin (Human), USP, or any other component of the formulation.
WARNINGS
Depression and Suicide
Betaseron (Interferon beta-1b) should be used with caution in patients with depression, a
condition that is common in people with multiple sclerosis. Depression and suicide have
been reported to occur with increased frequency in patients receiving interferon compounds,
including Betaseron. Patients treated with Betaseron should be advised to report immediately any symptoms of depression and/or suicidal ideation to their prescribing physicians. If a
patient develops depression, cessation of Betaseron therapy should be considered.
In the four randomized controlled studies there were three suicides and eight suicide
attempts among the 1532 patients in the Betaseron treated groups compared to one suicide
and four suicide attempts among the 965 patients in the placebo groups.
Injection Site Necrosis
Injection site necrosis (ISN) has been reported in 4% of patients in controlled clinical
trials (see ADVERSE REACTIONS). Typically, injection site necrosis occurs within the
first four months of therapy, although post-marketing reports have been received of ISN
occurring over one year after initiation of therapy. Necrosis may occur at a single or multiple injection sites. The necrotic lesions are typically three cm or less in diameter, but larger
areas have been reported. Generally the necrosis has extended only to subcutaneous fat.
However, there are also reports of necrosis extending to and including fascia overlying muscle. In some lesions where biopsy results are available, vasculitis has been reported. For
some lesions debridement and, infrequently, skin grafting have been required.
As with any open lesion, it is important to avoid infection and, if it occurs, to treat the infection. Time to healing was varied depending on the severity of the necrosis at the time treatment was begun. In most cases healing was associated with scarring.
Some patients have experienced healing of necrotic skin lesions while Betaseron therapy continued; others have not. Whether to discontinue therapy following a single site of necrosis is dependent on the extent of necrosis. For patients who continue therapy with Betaseron after injection site
necrosis has occurred, Betaseron should not be administered into the affected area until it is fully
healed. If multiple lesions occur, therapy should be discontinued until healing occurs.
Patient understanding and use of aseptic self-injection techniques and procedures should be
periodically reevaluated, particularly if injection site necrosis has occurred.
Anaphylaxis
Anaphylaxis has been reported as a rare complication of Betaseron use. Other allergic reactions have included dyspnea, bronchospasm, tongue edema, skin rash and urticaria (see
ADVERSE REACTIONS).
Albumin (Human), USP
This product contains albumin, a derivative of human blood. Based on effective donor
screening and product manufacturing processes, it carries an extremely remote risk for
transmission of viral diseases. A theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD) also is considered extremely remote. No cases of transmission of viral diseases
or CJD have ever been identified for albumin.
PRECAUTIONS
Information for Patients
All patients should be instructed to carefully read the supplied Betaseron Medication Guide.
Patients should be cautioned not to change the dose or schedule of administration without
medical consultation.
Patients should be made aware that serious adverse reactions during the use of Betaseron
have been reported, including depression and suicidal ideation, injection site necrosis, and
anaphylaxis (see WARNINGS). Patients should be advised of the symptoms of depression
or suicidal ideation and be told to report them immediately to their physician. Patients should
also be advised of the symptoms of allergic reactions and anaphylaxis.
Patients should be advised to promptly report any break in the skin, which may be associated with blue-black discoloration, swelling, or drainage of fluid from the injection site, prior
to continuing their Betaseron therapy.
Patients should be informed that flu-like symptoms are common following initiation of therapy with Betaseron. In the controlled clinical trials, antipyretics and analgesics were permitted for relief of these symptoms. In addition, gradual dose titration during initiation of
Betaseron treatment may reduce flu-like symptoms.
Female patients should be cautioned about the abortifacient potential of Betaseron (see
PRECAUTIONS, Pregnancy-Teratogenic effects).
Instruction on Self-injection Technique and Procedures
Patients should be instructed in the use of aseptic technique when administering Betaseron.
Appropriate instruction for reconstitution of Betaseron and methods of self-injection should be
provided, including careful review of the Betaseron Medication Guide. The first injection should
be performed under the supervision of an appropriately qualified health care professional.
Patients should be cautioned against the re-use of needles or syringes and instructed in safe disposal procedures. A puncture resistant container for disposal of used needles and syringes should
be supplied to the patient along with instructions for safe disposal of full containers. Patients should
be advised of the importance of rotating areas of injection with each dose, to minimize the likelihood
of severe injection site reactions, including necrosis or localized infection.
Laboratory Tests
In addition to those laboratory tests normally required for monitoring patients with multiple
sclerosis, complete blood and differential white blood cell counts, platelet counts and blood
chemistries, including liver function tests, are recommended at regular intervals (one, three,
and six months) following introduction of Betaseron therapy, and then periodically thereafter in
the absence of clinical symptoms. Thyroid function tests are recommended every six months
in patients with a history of thyroid dysfunction or as clinically indicated. Patients with myelosuppression may require more intensive monitoring of complete blood cell counts, with differential and platelet counts.
Drug Interactions
No formal drug interaction studies have been conducted with Betaseron. In the placebo controlled studies in MS, corticosteroids or ACTH were administered for treatment of relapses
for periods of up to 28 days in patients (N=664) receiving Betaseron.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
Carcinogenesis: Interferon beta-1b has not been tested for its carcinogenic potential in animals.
Mutagenesis: Betaseron was not mutagenic when assayed for genotoxicity in the Ames bacterial test in the presence or absence of metabolic activation. Interferon beta-1b was not
mutagenic to human peripheral blood lymphocytes in vitro, in the presence or absence of
metabolic inactivation. Betaseron treatment of mouse BALBc-3T3 cells did not result in
increased transformation frequency in an in vitro model of tumor transformation.
Impairment of fertility: Studies in normally cycling, female rhesus monkeys at doses up to
0.33 mg/kg/day (32 times the recommended human dose based on body surface area, body
surface dose based on 70 kg female) had no apparent adverse effects on either menstrual
cycle duration or associated hormonal profiles (progesterone and estradiol) when administered over three consecutive menstrual cycles. The validity of extrapolating doses used in
animal studies to human doses is not known. Effects of Betaseron on normally cycling
human females are not known.
Pregnancy-Teratogenic effects
Pregnancy Category C: Betaseron was not teratogenic at doses up to 0.42 mg/kg/day when
given to pregnant female rhesus monkeys on gestation days 20 to 70. However, a dose related abortifacient activity was observed in these monkeys when Interferon beta-1b was administered at doses ranging from 0.028 mg/kg/day to 0.42 mg/kg/day (2.8 to 40 times the
recommended human dose based on body surface area comparison). The validity of extrapolating doses used in animal studies to human doses is not known. Lower doses were not
studied in monkeys. Spontaneous abortions while on treatment were reported in patients
(n=4) who participated in the Betaseron RRMS clinical trial. Betaseron given to rhesus monkeys on gestation days 20 to 70 did not cause teratogenic effects; however, it is not known if
teratogenic effects exist in humans. There are no adequate and well-controlled studies in
pregnant women. If the patient becomes pregnant or plans to become pregnant while taking
Betaseron, the patient should be apprised of the potential hazard to the fetus and it should be
recommended that the patient discontinue therapy.
Nursing Mothers
It is not known whether Betaseron is excreted in human milk. Because many drugs are
excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Betaseron, a decision should be made to either discontinue nursing or discontinue the drug, taking into account the importance of drug to the mother.
Pediatric Use
Safety and efficacy in pediatric patients have not been established.
Geriatric Use
Clinical studies of Betaseron did not include sufficient numbers of patients aged 65 and over
to determine whether they respond differently than younger patients.
ADVERSE REACTIONS
In all studies, the most serious adverse reactions with Betaseron were depression, suicidal ideation
and injection site necrosis (see WARNINGS). The incidence of depression of any severity was
approximately 30% in both Betaseron-treated patients and placebo-treated patients. Anaphylaxis
and other allergic reactions have been reported in patients using Betaseron (seeWARNINGS). The
most commonly reported adverse reactions were lymphopenia (lymphocytes<1500/mm3), injection site reaction, asthenia, flu-like symptom complex, headache, and pain. The most frequently
reported adverse reactions resulting in clinical intervention (e.g., discontinuation of Betaseron,
adjustment in dosage, or the need for concomitant medication to treat an adverse reaction symptom) were depression, flu-like symptom complex, injection site reactions, leukopenia, increased
liver enzymes, asthenia, hypertonia, and myasthenia.
Because clinical trials are conducted under widely varying conditions and over varying lengths of
time, adverse reaction rates observed in the clinical trials of Betaseron cannot be directly compared
to rates in clinical trials of other drugs, and may not reflect the rates observed in practice. The
adverse reaction information from clinical trials does, however, provide a basis for identifying the
adverse events that appear to be related to drug use and for approximating rates.
The data described below reflect exposure to Betaseron in the four placebo controlled trials of
1407 patients with MS treated with 0.25 mg or 0.16 mg/m2, including 1261 exposed for
greater than one year. The population encompassed an age range from 18-65 years. Sixtyfour percent (64%) of the patients were female. The percentages of Caucasian, Black, Asian,
and Hispanic patients were 94.8%, 3.5%, 0.1%, and 0.7%, respectively.
The safety profiles for Betaseron-treated patients with SPMS and RRMS were similar.
Clinical experience with Betaseron in other populations (patients with cancer, HIV positive
patients, etc.) provides additional data regarding adverse reactions; however, experience in
non-MS populations may not be fully applicable to the MS population.
Table 1 enumerates adverse events and laboratory abnormalities that occurred among all patients
treated with 0.25 mg or 0.16 mg/m2 Betaseron every other day for periods of up to three years in
the four placebo controlled trials (Study 1-4) at an incidence that was at least 2.0% more than
that observed in the placebo patients (System Organ Class, MedDRA v. 8.0).
Table 1: Adverse Reactions and Laboratory Abnormalities
System Organ Class MedDRA
Placebo Betaseron
(n=965)
(n=1407)
v. 8.0 # Adverse Reaction
Blood and lymphatic system disorders
Lymphocytes count decreased
66%
86%
(< 1500/mm3) x
Absolute neutrophil count decreased
5%
13%
(< 1500/mm3) x
White blood cell count decreased
4%
13%
(<3000/mm3) x
Lymphadenopathy
3%
6%
Nervous system disorders
Headache
43%
50%
Insomnia
16%
21%
Incoordination
15%
17%
Vascular disorders
Hypertension
4%
6%
Respiratory, thoracic and mediastinal disorders
Dyspnea
3%
6%
Gastrointestinal disorders
Abdominal pain
11%
16%
Hepatobiliary disorders
Alanine aminotransferase increased
4%
12%
(SGPT > 5 times baseline) x
Aspartate aminotransferase increased
1%
4%
(SGOT > 5 times baseline) x
Skin and subcutaneous tissue disorders
Rash
15%
21%
Skin disorder
8%
10%
Musculoskeletal and connective tissue disorders
Hypertonia
33%
40%
Myalgia
14%
23%
Renal and urinary disorders
Urinary urgency
8%
11%
Reproductive system and breast disorders
Metrorrhagia *
7%
9%
6%
8%
Impotence **
General disorders and administration site conditions
26%
78%
Injection site reaction (various kinds)o
Asthenia
48%
53%
37%
57%
Flu-like symptoms (complex) §
Pain
35%
42%
Fever
19%
31%
Chills
9%
21%
Peripheral edema
10%
12%
Chest pain
6%
9%
Malaise
3%
6%
Injection site necrosis
0%
4%
#
x
except for "injection site reaction (various kinds)o" and "flu-like symptom complex§ "
the most appropriate MedDRA term is used to describe a certain reaction and its synonyms and related conditions.
laboratory abnormality
* pre-menopausal women
** men
o "Injection site reaction (various kinds)" comprises all adverse events occurring at the
injection site (except injection site necrosis), i.e. the following terms: injection site
reaction, injection site hemorrhage, injection site hypersensitivity, injection site
inflammation, injection site mass, injection site pain, injection site edema and injection site atrophy.
§ "Flu-like symptom complex" denotes flu syndrome and/or a combination of at least
two AEs from fever, chills, myalgia, malaise, sweating.
Injection Site Reactions
In four controlled clinical trials, injection site reactions occurred in 78% of patients receiving Betaseron with injection site necrosis in 4%. Injection site inflammation (42%), injection site pain (16%), injection site hypersensitivity (4%), injection site necrosis (4%), injection site mass (2%), injection site edema (2%) and non-specific reactions were significantly
associated with Betaseron treatment (see WARNINGS and PRECAUTIONS). The incidence of injection site reactions tended to decrease over time. Approximately 69% of
patients experienced the event during the first three months of treatment, compared to
approximately 40% at the end of the studies.
Flu-Like Symptom Complex
The rate of flu-like symptom complex was approximately 57% in the four controlled clinical
trials. The incidence decreased over time, with only 10% of patients reporting flu-like symptom complex at the end of the studies. For patients who experienced a flu-like symptom
complex in Study 1, the median duration was 7.5 days.
Laboratory Abnormalities
In the four clinical trials, leukopenia was reported in 18% and 6% [of patients in Betaseron- and
placebo-treated groups, respectively. No patients were withdrawn or dose reduced for neutropenia in Study 1. Three percent (3%) of patients in Studies 2 and 3 experienced leukopenia and
were dose-reduced. Other abnormalities included increase of SGPT to greater than five times
baseline value (12%), and increase of SGOT to greater than five times baseline value (4%). In
Study 1, two patients were dose reduced for increased hepatic enzymes; one continued on treatment and one was ultimately withdrawn. In Studies 2 and 3, 1.5% of Betaseron patients were
dose-reduced or interrupted treatment for increased hepatic enzymes. In Study 4, 1.7% of
patients were withdrawn from treatment due to increased hepatic enzymes, two of them after a
dose reduction. In Studies 1-4, nine (0.6%) patients were withdrawn from treatment with
Betaseron for any laboratory abnormality, including four (0.3%) patients following dose reduction. (see PRECAUTIONS, Laboratory tests).
Menstrual Irregularities
In the four clinical trials, 97 (12%) of the 783 pre-menopausal females treated with
Betaseron and 79 (15%) of the 528 pre-menopausal females treated with placebo reported
menstrual disorders. One event was reported as severe, all other reports were mild to moderate severity. No patients withdrew from the studies due to menstrual irregularities.
Postmarketing Experience
The following adverse events have been observed during postmarketing experience with
Betaseron and are classified within body system categories:
Blood and lymphatic system disorders: Anemia, Thrombocytopenia
Endocrine disorders: Hypothyroidism, Hyperthyroidism, Thyroid dysfunction
Metabolism and nutrition disorders: Hypocalcemia, Hyperuricemia, Triglyceride increased,
Anorexia, Weight decrease
Psychiatric disorders: Confusion, Depersonalization, Emotional lability
Nervous system disorders: Ataxia, Convulsion, Paresthesia, Psychotic symptoms
Cardiac disorders: Cardiomyopathy
Vascular disorders: Deep vein thrombosis, Pulmonary embolism
Respiratory, thoracic and mediastinal disorders: Bronchospasm, Pneumonia
Gastrointestinal disorders: Pancreatitis, Vomiting
Hepatobiliary disorders: Hepatitis, Gamma GT increased
Skin and subcutaneous tissue disorders: Pruritus, Skin discoloration, Urticaria
Renal and urinary disorders: Urinary tract infection, Urosepsis
General disorders and administration site conditions: Fatal capillary leak syndrome*.
*The administration of cytokines to patients with a pre-existing monoclonal gammopathy
has been associated with the development of this syndrome.
Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. Serum samples were
monitored for the development of antibodies to Betaseron during Study 1. In patients receiving 0.25 mg every other day 56/124 (45%) were found to have serum neutralizing activity at
one or more of the time points tested. In Study 4, neutralizing activity was measured every
6 months and at end of study. At individual visits after start of therapy, activity was observed
in 16.5% up to 25.2% of the Betaseron treated patients. Such neutralizing activity was measured at least once in 75 (29.9%) out of 251 Betaseron patients who provided samples during treatment phase; of these, 17 (22.7%) converted to negative status later in the study.
Based on all the available evidence, the relationship between antibody formation and clinical safety or efficacy is not known.
These data reflect the percentage of patients whose test results were considered positive for antibodies to Betaseron using a biological neutralization assay that measures the ability of immune
sera to inhibit the production of the interferon-inducible protein, MxA. Neutralization assays are
highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of neutralizing activity in an assay may be influenced by several factors including sample
handling, timing of sample collection, concomitant medications, and underlying disease. For
these reasons, comparison of the incidence of antibodies to Betaseron with the incidence of
antibodies to other products may be misleading.
Anaphylactic reactions have rarely been reported with the use of Betaseron.
DRUG ABUSE AND DEPENDENCE
No evidence or experience suggests that abuse or dependence occurs with Betaseron therapy; however, the risk of dependence has not been systematically evaluated.
OVERDOSAGE
Safety of doses higher than 0.25 mg every other day has not been adequately evaluated. The
maximum amount of Betaseron that can be safely administered has not been determined.
Rx Only.
REFERENCES
References furnished upon request.
U.S. Patent No. 4,588,585; 4,961,969; 5,702,699; 6,994,847
Distributed by:
Bayer HealthCare Pharmaceuticals Inc.
Wayne, NJ 07470
Manufactured by: Chiron Corporation, Emeryville, CA 94608
U.S. License No. 1106
© 2007, Bayer HealthCare Pharmaceuticals Inc. All rights reserved.
Printed in U.S.A.
Part Number 10011479
April 2007
Revision date 10/06
(6052802 BH)
06-521-0272dBH
American Academy of Neurology
Member Benefits
FREE publications featuring
up-to-date information on scientific
research and news affecting the
neuroscience community
• Neurology Online CME
Federal, state, and local advocacy
efforts representing your interests
and concerns
• Neurology ® journal
• Continuum: Lifelong Learning
in Neurology ®
• Donald M. Palatucci Advocacy
Leadership Forum
• Neurology Today ®
• Quintessentials®
• Neurology on the Hill
• Neurology Now
• Annual Meeting
• Viste Neurology Public Policy
Fellowship
• AANnews
®*
®
Wide range of FREE or reduced-rate
CME opportunities
• Regional programs
• Online AAN Membership Directory
• AAN Pocket Guidelines (free
PDA download)
• Continuum: Lifelong Learning
in Neurology ® (free to Junior
members only)
Discounts on AAN events, products,
tools, and resources
• Annual Meeting registration
• Fall and Winter Conference
registration
• CME course fees
• NeuroSAE™ (Neurology
Self-Assessment Examination) fee
• Resident In-service Training
Examination (RITE) fee
• AAN Store™
• AAN Dendrite™ Careers in
Neurology listing
• Syllabi on CD-ROM
• Virtual Annual Meeting
Tools for practice assistance
• ICD-9-CM Coding Book &
Online CPT®
• State neurology society support
• Vocus online advocacy tool
• AAN Pocket Guidelines
AAN Partners Program offering
competitively priced, high-quality
products and services to meet
your needs
• E/M Pocket Coding Guide
• Malpractice insurance
• HIPAA resources
• Payment processing
• Regulatory compliance assistance
via the website
• Credit cards
• AAN Dendrite™ Careers in
Neurology listing
• Medical insurance
• AAN Practice Guidelines
• Practice manager opportunities
through BRAINS
• Life insurance
• Long-term care insurance evaluation
• Disability insurance
• Business overhead insurance
Public outreach and patient
education materials
• Home and auto insurance
• Neurology Now ®
• Epocrates products
• The Brain Matters® Website
• Patient education book series
and brochures
• PDA hardware and software
Involvement, networking, and
peer recognition
• Sections, committees, work groups,
task forces
• Awards, scholarships, prizes
*
Available online only to international members
For more information, contact AAN Member Services Monday through
Friday from 8:00 a.m. to 5:00 p.m. CT at memberservices@aan.com,
(800) 879-1960, or (651) 695-2717 (international), or visit the
AAN website at www.aan.com/go/membership/benefits.
foundation
Foundation Offers 60/60 Proposition
The AAN Foundation is asking Academy
members who have never before donated
to the Foundation to mark the 60th
anniversary of the founding of the
American Academy of Neurology
with a $60 donation.
“This is a great low-cost way for members who have not yet joined our family
of contributors to our neurologic research
programs to mark this Academy milestone,”
said Austin J. Sumner, MD, FAAN, Chair
of the AAN Foundation. “We believe one
dollar for each year of the Academy’s
service to the neurology community is
an affordable entry point, in spite of this
challenging economic climate. One
hundred percent of member donations
support neurology and strengthen the
Academy by funding young researchers
and helping neurology residents attend
“If you are a member of the AAN, you have
benefited from 60 years of work on your
behalf. Your contribution will help ‘pay it
forward’ to the next generations of neurology
professionals.”
— Austin J. Sumner, MD, FAAN
the AAN Annual Meeting. A gift to the
AAN Foundation is a gift to your future as
a neurologist. And that is why A.B. Baker
launched the AAN in 1948—to ensure the
future of neurology.”
Sumner encourages past donors to mark the
anniversary with an additional gift of $60,
or increase their year-end contribution by
that amount. Donations to the AAN
Foundation are tax-deductible.
“If you are a member of the AAN, you
have benefited from 60 years of work
on your behalf,” said Sumner. “Your
contribution will help ‘pay it forward’
to the next generations of neurology
professionals.”
New Endowment Fund Created to Support
Medical Students, Residents, Fellows
Continued from cover
The couple hopes the endowed fund will
inspire medical students to choose a career
path in neurology and that it will enhance
educational opportunities to better equip
medical students, residents, and fellows
to be excellent neurologists.
“The American Academy of Neurology was a strong force in
allowing me to maintain proficiency in this ever-fascinating
field. By making this gift of education, I hope to give others the
opportunity to follow a similar path.”
Mario Oliveira was born in Paris and
raised in Rio de Janeiro. He graduated in
1956 with an MD degree from the Federal
University National Faculty of Medicine. He
moved to the United States in 1957, and trained in neurology at
the Medical College of Wisconsin at Marquette University in
Milwaukee. He stayed on staff as an instructor, rising to Clinical
Professor of Neurology in 1975. Since leaving Wisconsin in 1982,
Oliveira has had a private practice in Colorado Springs and teaches
neuropathology to pathology residents at Penrose Hospital.
Dianne Oliveira chaired various AAN Alliance committees and served
as a board member from 1982 to 1995 and president from 1991
to 1993. After a career as a teacher, she has been a homemaker
and part-time medical office manager in her husband’s practice.
Currently, she is an English tutor and group facilitator for immigrants
22
December 2008 • AANnews
— Mario M. Oliveira, MD, FAAN
at the Pikes Peak Library district Litsource program in Colorado
Springs, where she has been an active volunteer in many
community organizations.
Both Mario and Dianne Oliveira have supported education and
research for neurologic disorders through the Foundation over many
years in numerous ways. The creation of the Dr. Mario and Dianne
Oliveira Neurology Education Endowment Fund is the capstone to
their lifelong commitment to neurology medical education and will
benefit future generations of medical students.
Foundation Friends
The AAN Foundation greatly appreciates gifts received from the following donors between September 1 and September 30, 2008. Gifts
of $100 and greater are recognized in AANnews. For secure on-line giving options, visit www.aan.com. For more information about the
AAN Foundation or its programs, contact Kathie Lazar Robinson at klazarrobinson@aan.com or (866) 770-7570.
ANNUAL FUND
($500–$999)
Christian Baumann, MD
THE FUND FOR BRAIN
RESEARCH
Research – Stroke
($100–$499)
Lisa Dunn (In memory of Irma Josine O’Connor)
($100–$499)
Astri L. Lindberg (In memory of Irma Josine O’Connor)
Alberto A. Martinez-Arizala, MD, FAAN
Rochelle Pleet (In memory of
Dr. Milton Ettinger)
THE MILTON ALTER, MD,
FUND FOR CLINICAL
RESEARCH IN MS AND STROKE
($500–$999)
Richard L. Werner
AAN RESIDENT FUND
($500–$999)
John Corboy, MD, FAAN
Research – Alzheimer’s
($100–$499)
Terry Raskyn
“I support the AAN Foundation because it allows me to designate
my contribution in the way I see most fit, which is for the Resident
Scholarship fund. This fund allows us each year to offer more
AAN Annual Meeting scholarships to the bright young minds
that are the future of neurology in the USA and the world.”
—John Corboy, MD, FAAN
Denver, CO
AAN Member since 1987
other news
Apply Now for the UCNS Neuro-Oncology
Certification Examination
The deadline to apply for the United Council for Neurologic Subspecialties certification
examination in Neuro-Oncology is January 15, 2009. Applications and payment of
$1,500 are required for the examination. The examination will take place the week
of July 13 through 17, 2009. Applications can be downloaded from www.ucns.org.
For more information, visit the UCNS website or contact Todd Bulson at tbulson@ucns.org
or (651) 695-2813.
AANnews • December 2008
23
7
14
21
28
8
15
22
29
SUN
MON
9
16
23
30
10
17
24
31
upcoming dates and deadlines
DECEMBER 2008
13
20
27
4
11
18
25
5
12
19
26
THU
FRI
SAT
SUN
MON
TUE
WED
1
2
9
16
23
30
3
10
17
24
31
1
8
15
22
2
9
16
23
3
10
17
24
4
11
18
25
JANUARY 2009
SUN
MON
TUE
WED
THU
FRI
SAT
7
14
21
28
1
8
15
22
29
2
9
16
23
30
3
10
17
24
31
4
11
18
25
5
12
19
26
6
13
20
27
FRI
SAT
2
9
16
23
30
3
10
17
24
31
2009
DECEMBERJANUARY
1
MON Tyler
TUE Award
WED
THU
H.SUN
Richard
1
Applications Due
4
5
6
7
8
Jeff Sorenson
11
12
13
14
15
(651)
18 695-2728
19
20
21
22
jsorenson@aan.com
25
26
27
28
29
12
19
26
11
18
25
DECEMBER 14
2009
NeurologyFEBRUARY
on the Hill Applications
Due
SUN
MON
TUE
WED
THU
FRI
SAT
www.aan.com/go/advocacy/active/noh
1
2
3
4
5
6
7
Melissa Larson
8
9
10
11
12
13
14
(651) 695-2748
15
16
17
18
19
20
21
mlarson@aan.com
22
23
24
25
26
27
28
DECEMBER 15
Winter Conference Early
Registration Deadline
www.aan.com/winter09
DECEMBER 31
AAN Award for Creative Expression
of Human Values in Neurology
Applications Due
Karen Kasmirski
(651) 695-2731
kkasmirski@aan.com
DECEMBER 31
UCNS Accreditation Deadline
for Behavioral Neurology &
Neuropsychiatry, Headache Medicine,
Neurocritical Care, Neuroimaging,
and Neuro-Oncology
Tracy King
(651) 695-2816
tking@ucns.org
4
11
18
25
5
12
19
26
TUE
6
13
20
27
WED
7
14
21
28
8
15
22
29
6
13
20
27
7
14
21
28
8
15
22
29
9
16
23
30
10
17
24
31
THU
FRI
SAT
5
12
19
26
6
13
20
27
7
14
21
28
FEBRUARY 2009
JANUARY FEBRUARY
9
2009
SUN Journalism
MON
TUE Fellowship
WED
THU
FRI
AAN
1
2
3
4
5
6
Award
Deadline
8
9
10
11
12
13
www.aan.com/go/press/journalism
15
16
17
18
19
20
Rachel
Seroka
22
23
24
25
26
27
(651) 695-2738
rseroka@aan.com
SAT
7
14
21
28
JANUARY 9–10
Equilibrium Part II for
Program Directors
Sarah Tonn
(651) 695-2819
stonn@aan.com
JANUARY 20
2009 RITE Cancellation Deadline Lori Strachota
(651) 695-2706
lstrachota@aan.com
FEBRUARY 20
Late-Breaking Science Deadline www.aan.com/go/am/science/latebreaking
FEBRUARY 20–21
North Carolina Neurological
Association
Nancy Lowe
(800) 722-1350 ext. 111
nlowe@ncmedsoc.org
FEBRUARY 27–28
2009 RITE Test Dates Mary Cress
(651) 695-2754
mcress@aan.com
JANUARY 31 A.B. Baker Award for Lifetime
Achievement in Neurologic
Education Application Deadline
Nancy Poechmann
(651) 695-2812
npoechmann@aan.com
DECEMBER 31
2009 RITE Registration Deadline
Lori Strachota
(651) 695-2706
lstrachota@aan.com
2010 / Toronto
April 10–17
AAN Annual Meetings
2009 / Seattle
April 25–May 2
Regional conferences
2009 / Lake Buena Vista, FL
January 16–18
24
December 2008 • AANnews
2011 / Honolulu
April 9–16
NORTH EAST
Dendrite Rate Information
Rates are charged per ad, up to 100 words
A word consists of one or more letters or
numbers surrounded by a space on each side.
Ads appear on the Academy Website and in
print in the AANnews.
Member
NonMember
One month ad, up to 100 words
$300
$400
Three month ad, up to 100 words
$750
$1,000
Additional words
$3.00/per word
$4.00/per word
Confidential Blind Box reply
$50.00
$50.00
All ads appear in paragraph format. The title
or header of the ad will appear in bold at no
additional charge. There is no bolding or
capitalization allowed in any other portion
of the ad.
Ad copy must be received no later than
December 15, 2008, to appear in the
February 2009 issue. The same deadline
applies to changes/cancellations, which
must be received in writing.
Advertisements can now be entered electronically
at www.aan.com/dendrite. Advertisements must
be paid for at the time of submission. For
further inquiries, contact Amy Schoch at
(651) 695-2749; email: aschoch@aan.com.
For payment information, contact Elaine Mund
at (651) 695-2751; email: emund@aan.com.
The American Academy of Neurology
reserves the right to decline, withdraw, or edit
advertisements at its discretion. Every care
is taken to avoid mistakes but responsibility
for clerical or printer errors does not exceed
the cost of the ad.
Replies to Blind Box Numbers
Address replies to blind box numbers to:
The Dendrite: Box ______________________
American Academy of Neurology
1080 Montreal Ave., St. Paul, MN 55116
All replies will be forwarded within
one week of receipt.
Increase Your Audience by
Advertising in Neurology!
Looking to reach a larger audience for
your open positions in neurology? Place
an ad in the journal Neurology ®! Maximize
your range and impact for job postings,
fellowships, meetings, and more with a
classified listing. Start now by contacting
at Danni.Morinich@wolterskluwer.com
or (215) 521-8405.
BC/BE Neurologists Lahey Clinic, BC/BE Neurologists Lahey
Clinic is seeking two BC/BE Neurologists. All subspecialties
will be considered, but we have particular interest in recruiting
Neurologists who wish to see patients with cognitive or
movement disorders. These positions will be based at our
outpatient facility at Lahey Clinic North Shore, in Peabody,
MA, which is currently undergoing a 65,000 square-foot
expansion and will be a 100-physician facility. These
Neurologists will also spend one day per week in the outpatient
clinic at Lahey Clinic Medical Center in Burlington, MA. The
candidate will teach residents and students, and attend on the
ward and consult services in Burlington. These positions are
expected to be available in June of 2009. The Department
consists of 18 Neurologists, all of whom have subspecialty
expertise, 2 Neuropsychologists, a Physiatrist, six mid-level
providers, research staff, and a clinical neurophysiology unit.
We are part of the Tufts Neurology Residency Program. Our
department is dedicated to clinical expertise, education, and
research, in a cooperative and supportive environment. We
are part of a comprehensive Neuroscience Center, which
includes Neurosurgery, Neuroradiology, and Interventional
Radiology. Please forward cover letter and CV, in Word
Format, to Paul T. Gross, MD, Chair Department of Neurology,
Lahey Clinic, 41 Mall Road, Burlington, MA, 01805.
Consultative Neurologist Opportunity in Gettysburg The
practice has 13 fellowship trained neurologists in a
comprehensive consultative service that includes EMG, EEG,
chemodenervation, transcranial Doppler and more. Other
services include deep brain stimulator placement, neuroimaging, carotid ultrasound, sleep study, intrathecal pump placement
and stereotatic neurosurgery. This position will focus on general
neurology. Telephone call only with back up support by our
larger team. Position offers excellent salary and benefits,
including health insurance, CME with stipend, paid relocation
and more. For more information or to apply, contact Carol
Stowell at 1-866-230-1477 or cstowell@wellspan.org. For
more information about WellSpan visit www.wellspan.org.
Practice Opportunity-Southern New Jersey (Near Philadelphia).
Very busy, four-person, private practice is expanding and
seeks BC/BE Neurologist. Fellowship and/or experience in
EMG is required. We are an academically oriented practice
with in-office MRI and CT facilities. Competence in reading
MRI and CT scans is of great value. A competitive financial
package leading to partnership is offered to a well-trained,
hard-working, personable individual. Phone: 609-871-8961;
Fax: 609-877-5555; E-mail: neurology231@comcast.net
Jersey Shore Area 1 hour from NY and Phila. Established
private practice group of six BC adult neurologists with multiple
board certifications seeking BC/BE Adult Neurologist (PT or FT).
Fellowship training preferred, all subspecialties considered. Staff
appointments at major medical center with university affiliation
and residency program. Office includes EEG, EMG and evoked
potentials. Hospital consult service includes comprehensive
stroke center, inpatient video EEG, ambulatory EEG,
intraoperative monitoring. Competitive salary/benefit package
with attractive call schedule and partnership track. Email CV
to neuromare@aol.com or fax to 732-774-6816.
Vermont - Neurologist Beautiful Mountain Region. Hospitalemployed consultative neurology opportunity. Outpatient
clinic care. Inpatient consults. EMG, EEG, Evoked Potentials.
Call coverage is by choice. Vacation, holidays and CME total
40 days. The financial offer includes salary with incentive and
loan repayment. J-1 visa holders are invited to inquire. Live
and work in a traditional New England community with an
energetic business district, rich cultural amenities, year-round
recreational venues and lovely historic district. Named by
National Geographic as the #1 town for adventure. Contact
Lianne Harris, New England Health Search. Phone
207-866-5680; E-mail Lharris@nehs.net.
Chair, Dept of Neurology, NYU School of Medicine The NYU
School of Medicine announces its search for the Chair of the
Department of Neurology. The Dean and faculty consider
this an exceptional opportunity to lead a preeminent academic
department in the city of New York and in close collaboration
with the other schools and colleges of New York University.
Chair, Department of Neurology, NYU School of Medicine &
its Affiliated Academic Medical Centers. The Chair of the
department has responsibility for the research, education and
clinical activities of a faculty that works in several institutions
along our unique biomedical corridor. A successful candidate
will have an MD degree and will have demonstrated leadership
experience in a large academic medical center with a
distinguished record of clinical, research and teaching
responsibilities. Applications and nominations with
accompanying curriculum vitae should be sent electronically,
for confidential review by the search committee, to: Rebecca
Elwork, M.H.S.A., Project Manager for Education, Faculty
and Academic Affairs, Rebecca.Elwork@nyumc.org. The
NYU School of Medicine was founded in 1841 and is an
equal opportunity, affirmative action employer and provides
a drug-free workplace. www.nyumc.org
Great Neurology Opportunity in Beautiful Vermont VISTA
Physician Search and Consulting has a client in Northeastern
Vermont seeking a full-time BC/BE Neurologist. This is
primarily an out-patient opportunity with a Monday-Friday,
8am–5pm work schedule. The office is hospital-based with
support staff. This is an employed opportunity with competitive
compensation and relocation. Excellent benefits package
includes 35 days of vacation, CME with allowance, health,
dental, company paid disability and life insurance, malpractice
insurance, retirement plan, and flexible spending account.
Send your CV with cover letter to Tonya Harmon at
Tonya.harmon@vistastaff.com or call 1-800-366-1884 ext 6505.
Seacoast Region of New Hampshire 110-bed acute care
hospital located in the seacoast region is seeking 2 Neurologists,
1 now and the 2nd in 2009. Private practice with 2 FT MD’s
and 1 PT. Prefer a candidate with fellowship training. Consults
at three local hospitals within a 10 mile radius. Call Schedule:
1:3 weekdays 1:8 on weekends. Salary: 180K plus 10K for
the first year. Partnership in 2-years. Benefits include 3 weeks
vacations. Insurance: health, dental and malpractice. 1 week
CME with stipend of 2K. Medical staff includes more than
250 physicians and other healthcare providers, representing
39 specialties. Email lorileo@neprc.com
Neuro Hospitalist Opportunity - Boston, MA 100% Inpatient
Neurologist. Neurology group located south of Boston is in the
process of developing a Neuro-Hospitalist program at local
284 bed Hospital, just 13 miles south of Boston, MA. The
Neuro-Hospitalist will handle inpatient hospital work only.
This would be a two-three year commitment, which at the end
of the commitment, would provide the physician an opportunity
to join the private practice on a clinical basis or they could
continue on as a Neuro-Hospitalist. Shift schedule (M-F Days
only), with rotating weekend coverage. Program is looking to
hire 2 inpatient Neurologists. Email lorileo@neprc.com
General Neurology Foundation Medical Partners, located in
Nashua, New Hampshire has an outstanding opportunity for
BC/BE General Neurologist, to join a thriving practice with a
large referral base. Subspecialty interests would be welcomed
into the practice. Weekend call is 1:7. Office is conveniently
located across from the hospital. Foundation Medical Partners
is a 150 provider multi- specialty group practice, affiliated
with Southern New Hampshire Medical Center. The Medical
Center is a 190 bed, Level II Trauma Center, with state of the
art equipment and services. Nashua, located one hour north
of Boston and one hour to the ocean and mountains is both
income tax and sales tax free. We offer competitive salary
and benefits package. Email leslie.mcgrath@snhmc.org
Neurology-Massachusetts Angels Neurological Centers, the
leader in neurological care in Massachusetts has openings
available immediately and July 2009 for full time or part-time
neurologists. We are recruiting General neurology and all
subspecialties and neurology hospitalists. Join 14 providers
including Neuro-ophthalmology, Epilepsy, neurophysiology,
neuromuscular and pediatric neurology. Call is one in four.
Benefits include: Generous salary, bonus benefits, malpractice
insurance, health insurance, dental insurance, disability
insurance, life insurance, accident insurance, cancer
insurance, hospitalization insurance, 401 K and many more.
Apply in confidence now. Fax CV to Mazen Eneyni, M.D.
(781) 871-3771 or email: meneyni@angelsneuro.com
Medical Staff Development Neurologist Needed in NW PA
Meadville Medical Center, located in the Great Lakes Area of
NW PA, is searching for a general neurologist to replace a
physician moving into administration. Very competitive salary
with full benefits or private practice opportunity with income
guarantee. Sign on bonus. Call 1:3. Meadville, PA, is a great
place to raise your family, and is located within easy access
AANnews • December 2008
25
of Pittsburgh, Cleveland and Erie. Service area is 90,000.
Meadville Medical Center is a progressive, independent,
regional community Medical Center. For information,
please contact Judith Janes, Medical Staff Development,
at 814/333-5701 or jjanes@mmchs.org.
Vermont – Neurologist Beautiful Mountain Region. Hospitalemployed consultative neurology opportunity. Outpatient
clinic care. Inpatient consults. EMG, EEG, Evoked Potentials.
Call coverage is by choice. Vacation, holidays and CME total
40 days. The financial offer includes salary with incentive
and loan repayment. J-1 visa holders are invited to inquire.
Live and work in a traditional New England community with
an energetic business district, rich cultural amenities, yearround recreational venues and lovely historic district. Named
by National Geographic as the #1 town for Adventure.
Contact Lianne Harris, New England Health Search.
Phone 207-866-5680; E-mail Lharris@nehs.net.
Seacoast New Hampshire Successful consultative Neurology
Group looking for B/C-B/E Adult Neurologist to join our
growing practice. General Neurology background necessary,
interest in stroke a plus. Competitive salary and benefits w/
opportunities for partnership. Enjoy the beautiful, family focused
lifestyle this region has to offer with access to skiing and
proximity to the scenic coastline. Federally designated as an
underserved area. Applicants should fax CV to 603-750-4072
or call 603-749-0913.
Neurologist Central CT Partnership opportunity to join
dynamic Neurology group seeking to replace retiring
associate. Call 1:6, modern office attached to university
affiliated tertiary care hospital in Hartford, CT. BC/BE with
EMG certification and neurophysiology a plus. Competitive
salary and benefits. Desirable upscale communities, 2 hours
to NYC and Boston. For details, please contact Christine
Bourbeau at 800.892.3846 or fax/email your CV to
860.714.8894. Email: cbourbea@stfranciscare.org
Medical Malpractice Insurance for Neurologists Visit
www.tnpinsurance.com to learn more about The Neurologists’
Program (TNP) - the only medical malpractice insurance
program designed specifically for neurologists. TNP was
selected by the American Academy of Neurology (AAN) for
the AAN Partners Program. AAN members receive a 5%
premium discount. Other discounts available include: loss
free, group practice, part time practice, and more. TNP
insureds also have toll-free access to the Risk Management
Consultation Service helpline for one-on-one risk management
consultations. From the policy itself to the risk management
advice and guidance provided, TNP has one focus—
neurology. For more information, and to be notified when
TNP is available in your state, visit www.tnpinsurance.com,
e-mail TNP@prms.com, or call (800) 245-3333, ext. 389.
Movement Disorders Specialist The Department of
Neurology at Penn State Milton S. Hershey Medical Center is
recruiting for a full-time Movement Disorders Specialist. The
position is at the Assistant/Associate Professor level. This is an
exciting opportunity for an individual with expertise in
movement disorders to join a growing comprehensive clinical
and research program. Candidates should be board certified or
board eligible in neurology and have completed fellowship
training in movement disorders, or have comparable
experience. Applicants should submit a letter of interest with a
C.V. to David Good, MD, Professor and Chair, Department
of Neurology-EC037, Penn State University College of
Medicine, 30 Hope Drive, Hershey, PA 17033, e-mail
dgood@psu.edu. Job Requisition #22022. Penn State is
committed to affirmative action, equal opportunity, and the
diversity of its workforce. EOE-AA-M/F/H/V.
Because in Life, Every Moment Matters Imagine... Practicing
as part of a team dedicated to optimal outcomes, service,
safety and effectiveness of care in a culture that values
teaching, research and best practices...Quality Matters. A
collaborative environment within a fully integrated health
system that supports and respects the skills and talents of their
physicians and rewards them accordingly...Respect Matters.
Joining a physician-led organization where you elect your
peers to manage, govern and guide...Leadership Matters.
Your clinical and personal life matter to Guthrie. So does
working in a stimulating and rewarding environment. Guthrie
is seeking a general neurologist to join our thriving
Department of Neurology. This selective search offers a
robust compensation package including: salary guarantee,
26
December 2008 • AANnews
paid relocation, paid malpractice and sign on bonus. Guthrie
Clinic: 800.724.1295, sullivan_cary@guthrie.com.
Neuroscience Group/Boston Suburbs Well-established,
quality oriented neuroscience group looking to add an
additional neurologist. Sub-specialty training in Sleep
Medicine is desirable but not necessary. Excellent opportunity
for motivated individuals to join a highly skilled team of
physicians. Please send CV to: Howard M. Gardner, M.D.,
Medical Director, New England Neurological Associates,
P.C., 354 Merrimack Street, Lawrence, MA 01843 or email to
jtf@neneuro.com. Visit us on the Web at www.neneuro.com.
Portland, Maine - Neurologists Great quality of life - in and
out of the office. Large physician-owned group seeks general
neurologists and/or fellowship-trained neurologists in movement
disorders, multiple sclerosis, headache, or critical care. Affiliated
with Maine Medical Center (MMC), a 550-bed referral and
teaching hospital. Collaboration with MMC includes developing
a Neuroscience Institute, which supports initiatives in stroke,
epilepsy, and other neuro programs, and providing education
to UVM medical students and residents. Office has on-site
MRI, diagnostic EEG lab, co-location with Neurosurgery. Oncall is 1 in 10. Competitive salary, full benefits, shareholder
track with straight-forward buy-in. Portland – designated as a
top travel destination by Frommer’s - is a beautiful, historic
city on Casco Bay with world-class attractions. Fax cover
letter and CV to (207) 883-1010, Attn: Practice Administrator. Email to danowski@maineneurology.com. Phone
(207)883-1414 x357. Visit www.maineneurology.com.
Academic Neuromuscular Specialist The Department of
Neurology, Penn State Milton S. Hershey Medical Center is
recruiting for a full-time faculty member at the Assistant or
Associate Professor level to join our 3-person academic
neuromuscular group. We are an ALS center, and also have
a large MDA clinic and a busy EMG laboratory. Candidates
should have clinical expertise in neuromuscular diseases and
strong backgrounds in EMG. Our service area of over 2 million
provides us with a diverse referral population for clinical care
and research. Interested individuals should send a C.V. and a
letter of interest to Zachary Simmons, M.D., Director,
Neuromuscular Program and ALS Center, Penn State Hershey
Medical Center, Department of Neurology – EC037, 30 Hope
Drive, Hershey, PA 17033; e-mail: zsimmons@psu.edu. Job
Requisition #22019. Penn State is committed to affirmative
action, equal opportunity, and the diversity of its workforce.
EOE-AA-M/F/H/V.
Neurologist Geisinger Health System’s Neurosciences Institute
seeks a general neurologist and stroke neurologist to join its
growing, multidisciplinary team. Positions are available at
Geisinger Wyoming Valley Medical Center and Geisinger
South Wilkes-Barre in Wilkes-Barre, PA, which offers an
excellent quality of life and easy accessibility to NYC and
Philadelphia. Join a dynamic, collegial group of five neurologists
with various subspecialties, and have the opportunity to
conduct research and teach. Geisinger is a physician-led,
patient-focused, integrated delivery system that utilizes a
mature electronic health record connecting more than 700
physicians over a 40-county area serving 2.5 million people.
For more information, please contact Peggy Graf, Physician
Recruiter, at 1-800-845-7112 or psgraf@geisinger.edu or for
more information visit www.join-geisinger.org/516/neurology
Northern New Jersey Well established and respected 4 person
adult, private practice neurology group is looking for a BE/BC
Neurologist. Twenty minutes from NYC. Subspecialty training
in EMG or Stroke/vascular intervention preferred. Position
includes affiliation with large teaching tertiary care hospital
with academic responsibilities. In addition to excellent support
services the hospital has in-patient Video EEG monitoring and
is a JHCO certified primary Stroke center and NJ licensed
Comprehensive Stroke Center. Significant opportunity for growth
with generous salary and benefits leading to partnership. Fax CV
to 973-471-6360 or e-mail neurone@ix.netcom.com
Stroke Neurologist The Section of Neurology at the
Dartmouth- Hitchcock Medical Center in Lebanon, New
Hampshire is seeking an academic Stroke Neurologist to
support activities in patient care, teaching and research.
Candidates should have demonstrated by prior training and
experience superior skills in all aspects of vascular neurology.
Subspecialty expertise and research interest required.
Outstanding opportunities in neurological disorders involving
the central nervous system, education of residents and
students, and research opportunities are associated with this
position. The individual will practice at the DartmouthHitchcock Clinic and will have an academic appointment as
a member of the faculty of the Dartmouth Medical School.
All neurology faculty participate in the training of medical
students, residents, and fellows. The Dartmouth medical
community is collegial and collaborative. DartmouthHitchcock Medical Center is located in the beautiful Upper
Valley of New Hampshire with easy access to the coastal
waters and the mountains. Hanover, New Hampshire has
been designated as one of the most desirable places to live in
the country. Dartmouth College attracts outstanding scholars
and has a rich variety of programs in the performing arts.
Letters of recommendation and CV should be sent to: Kevin
D. Williams - Practice Manager, Neurology and Neurosurgery, Dartmouth-Hitchcock Medical Center, One Medical
Center Drive, Lebanon, NH 03756 Phone: 603-650-4341.
kevin.d.williams@hitchcock.org; Dartmouth-Hitchcock
Clinic is an affirmative action/equal opportunity employer
and is especially interested in identifying female and minority
candidates. www.dhmc.org
Princeton NJ A five member group looking for a BE/BC Adult
Neurologist, fellowship training preferred. Office has all
neurodiagnostic equipment and we have a consultation
practice. Competitive salary and benefits leading to partnership.
Fax resume to (609) 896 9733 or reply to Blind Box #3221.
SOUTH EAST
Coastal Florida Neurology Positions Two major Coastal
Florida hospitals have tremendous and urgent need for
neurologists to join a group practice. We have needs for
both inpatient, outpatient, or mixture of both. If you have
a desire to live on the beautiful coast of South Florida,
please call (800) 779-8804.
Academic/Private Adult Neurology & Neuro-Hospitalist
Florida International University College of Medicine seeking
candidates for Founding Faculty appointment in new College
of Medicine dual position in prestigious private practice.
Responsibilities include developing specialty neurology
clinics, curriculum development and teaching, participating
clerkship training for medical students, maintaining private
practice. Successful candidate should be exceptionally welltrained, strong entrepreneurial spirit. NEURO-HOSPITALIST
Also seeking BE/BC Neurologist for busy practice at prestigious
private hospital. Duties include hospital consults MondayFriday, on-call participation nights /weekends. Academic
appointment at new College of Medicine considered for
qualified candidate. APPLY: www.fiujobs.org for position 6004.
Questions, please email Dr. Hortsmyer at horstmyj@fiu.edu.
Neurologist Seek BC/BE Neurologist for FT position with
academic credentials sufficient to qualify for the Georgetown
University Medical School faculty and with research interests
and/or potential. He/she will make rounds on the in-patient
Neurology service, in-patient consults, weekends and holidays
in turn. Will see his own patients in the out-patient area, as
well as Compensation and Pension patients. If qualified,
incumbent may be asked to read EEGs, Sleep studies,
participate in the Pain, SCI, or movement disorders program.
Will teach residents and medical students, attend conferences, keep up GME credits and read sufficiently to stay
abreast of the important developments in the field. Please fax
your information and CV to (202) 745-8231, attention
Debbie Taylor or Jackie Allmond.
Wake Forest University-Asst, Assoc or Professor Academic
Pediatric Neurology – Assistant, Associate or Professor. The
Division of Pediatric Neurology, Department of Neurology
at the Wake Forest University Health Sciences is seeking an
outstanding BC/BE Pediatric Neurologist for appointment at
the Assistant, Associate or Professor rank. We are seeking
candidates with subspecialty training in Pediatric Neurology
who are either ABPN certified or eligible. Responsibilities
would include in and out patient care, teaching medical
students, and residents. Currently, the Section of Pediatric
Neurology has three faculty members. In 2002, a new Brenner
Children’s Hospital was opened at Wake Forest University
Medical Center. Brenner offers the latest treatment advances
in Pediatric Medicine. The setting is designed to put children
at ease and to provide state-of-the-art medical care. The
Children’s Hospital has more than 75 pediatric specialists.
We encourage minorities and women to apply for this position.
For more information on Wake Forest University Baptist
Medical Center, please visit our web site at www.wfubmc.edu.
Interested candidates who are eligible for licensure in North
Carolina should send curriculum vitae and three letters of
reference to: Allison Brashear, M.D., Professor and Chair,
Department of Neurology, Wake Forest University Health
Sciences, Winston-Salem, NC 27157. Phone (336) 716-3545;
Fax (336) 716-9489. Email abrashea@wfubmc.edu. WFUHS
is an affirmative action and equal opportunity employer.
Neurology Positions-Florida Busy group in Lakeland, FL,
between Tampa and Orlando, seeks Neurologist and
Epileptologist to establish a level 3 or 4 Epilepsy Center.
Clinical neurophysiology services include EEG, EMG, evoked
potential capabilities, Sleep Disorder Center as well as stateof-the-art neuroimaging capabilities (MRI, CT, CTA, SPEC and
PET). Electronic Medical Record. Salary guarantee + bonus
the first year; partnership after 2 years. Growing population
of 500,000. Abundant recreation year round – tennis, golf,
running, cycling, boating and fishing; access to museums,
theaters, colleges, shopping, festivals, sports events, Disney
World, Sea World and other attractions; 500+ lakes and
numerous parks. No State Income Tax. Watson Clinic,
(800) 854-7786, Fax (863) 680-7951, Email:
mstephens@watsonclinic.com.
Atlanta Neurology Position Hospital employed position in
metro Atlanta. One hospital practice. Attractive salary and
full hospital benefits including malpractice with tail. Popular
and historic in-town location active with development and
redevelopment. A stone’s throw to one of the city’s most
popular and largest private schools. Easy access to Midtown,
Downtown, the airport and all of Atlanta’s major professional
sports. Email bselvey@williamlaine.com
Neurointensivists Sinai Hospital of Baltimore, a 478-bed
teaching hospital is seeking a Neurocritical care specialist
due to growing patient volumes, increasing acuity and
program expansion in neurology, neurosurgery and
interventional neuroradiology. Must be certified/eligible for
UCNS Neurocritical Care subspecialty certification. Please
call Michael A. Williams, MD, FAAN, Medical Director of
Brain & Spine Institute, at 410-601-6125.
Pediatric Neurology Opportunity-DC Metro Area A private
pediatric subspecialty group with a true physician focus is
offering a unique opportunity for full-time, board certified/
eligible Pediatric Neurologists. Based in Fairfax, Virginia,
our practice provides the highest level of neurologic are; we
support level III neonatal and pediatric ICUs with cutting
edge treatments and diagnostic evaluations. We offer: a
competitive salary & benefits package, Intensivist and
Hospitalist programs at areas hospitals, call sharing, and
opportunities to follow both academic and clinical pursuits. If
you would like to become an integral member of our growing
team, please send your CV to recruiter@mcapmd.com.
Neurologist for Beach Resort Community Seeking BC/BE
Neurologist to join 2 physician Neurology practice in a
quaint resort community. This well-established practice
serves a rapidly growing area, including an expanding
community hospital with an active neuro-diagnostics lab and
hospitalist program. Neurology call is 1 in 4. Office
environment is state-of-the art with EMG/NCV, EEG, sleep
studies and EMR on the premises. Experience in EEG/EMG/
Sleep Study interpretation is desirable. This position offers
excellent income potential with benefits and partnership
track. We boast excellent schools and a safe family
environment with the obvious recreational benefits of coastal
living. Call (302) 644-8880.
Washington DC/Northern Virginia Suburbs Neurology Busy
suburban Washington, DC/Northern Virginia neurology
practice is seeking 1-2 additional BC/BE Neurologists to join
our group in 2009. This is an outstanding opportunity for a
motivated, hard-working Neurologist to join a successful,
well-respected practice. We are an expanding group
currently with 6 neurologists and an anesthesiologist
(practicing procedural pain medicine). We have a busy office
and hospital consultative practice, with a large referral base.
Our office facilities include full electrophysiological testing
(EEG, EPs, EMG/NCS), vascular ultrasound, and an on site
Sleep Lab. We are seeking general neurologists, but encourage
applicants with subspecialty training (including Movement
Disorders and MS) to apply, as there is an excellent opportunity
to cultivate those subspecialties within our group. Applicants
interested in a primarily neuro-hospitalist position are also
encouraged to apply. Competitive compensation, excellent
benefits, and partnership track are offered. The N. VA/
Washington DC area is a wonderful place to live, with many
cultural and recreational activities. We encourage all interested
applicants to send their CV to ESklarMD@alfaneuro.com or
administrator@alfaneuro.com, or call 703-845-1557.
Adult Neurologist Neurologists Needed. Neurological
Associates, Inc., located in Richmond, VA., has been providing
adult neurological care to the residents of Richmond and
surrounding areas since 1969. We have 14 neurologists with
multiple interests and a separate sleep medicine lab. Our
practice includes EEG, EMG, Carotid Doppler’s, an Infusion
Center, Botox, Neuro-opthalmology, and a Clinical Research
department. We are always open, and receptive, to new
ideas and innovations. With a population of over one million
people for the Greater Richmond Area, Richmond offers the
amenities of a big city, including first class restaurants, and a
vibrant night life. This central location makes it the ideal
home base for day trips. Mountains, beaches, historic areas
and our nation’s Capitol, are just a few of the attractions
within a 100-mile radius of the region. Richmond is viewed
as a national leader in meaningful education reform, having
one of the finest public school systems in the nation, two
major universities, and a medical school. Send CV and l
etter of interest to: HR@brainsR.us
NORTH CENTRAL
BC/BE Neurologist in Madison, WI The Department of
Neurology at the University of Wisconsin School of Medicine
and Public Health seeks candidates for a BC/BE General Neurologist, with subspecialty interest, to join our practice at 20 S
Park St. This physician will function as a generalist, with
subspecialty interest in Stroke (with Directorship at a local
community hospital); Headache management, or EMG as
Clinician-Teacher track Assistant Professor, Associate
Professor, or Professor. With 6 board certified Neurologists
and 1 PA; a full spectrum practice and balanced lifestyle can
be enjoyed with minimal outreach requirements, and an
attractive shared call arrangement. With the University of
Wisconsin and several technical colleges, along with cultural,
sporting and recreational events situated amongst three lakes;
Madison is well known for offering a small town feel in a
medium sized city and a great place to raise a family. Please
send curriculum vitae and the names of at least three
references to Thomas Sutula, M.D., Ph. D., Chair, Department
of Neurology-5132, University of Wisconsin School of Medicine
and Public Health, 600 Highland Ave., Room H6/574 CSC,
Madison, WI 53792 and to Frederick Edelman, M.D.,
Department of Neurology, 20 S Park St., Madison, WI 53715.
Submission of application information online is preferred;
please forward to applications@neurology.wisc.edu. Wisconsin
Caregiver and Open Records laws apply; background check
required prior to offer of employment. UW-Madison is an
Affirmative Action/Equal Opportunity Employer.
Neurologist Affiliated Community Medical Centers is a
physician-owned multispecialty clinic with 11 affiliate sites
located in Western and Southwestern MN. This opportunity is
primarily an outpatient practice with light call. It offers a two
year guaranteed salary, signing bonus, production incentive
plan, outstanding benefits and profit sharing plan. Full
partnership after two years. Willmar is a family oriented
town with a population of 20,000 which offers a multitude
of recreational opportunities and an excellent educational
system. Email karib@acmc.com
Neurologists MeritCare Medical Group is seeking BC/BE
Neurologists to join our clinics in Fargo, North Dakota and
Bemidji, Minnesota. MeritCare located in Fargo, ND is a fully
integrated, multi-specialty group of 400+ physicians located
on our main campus and in 28 regional primary care clinics.
Fargo is a tri-college community of 190,000 offering excellent
schools, safe neighborhoods and a wide range of cultural
activities and easy access to Minnesota lake country. Bemidji,
a community surrounded by 200 lakes, is located on the shores
of Lake Bemidji. Bemidji State University offers a variety of
cultural and athletic entertainment. This is an opportunity to
practice where other people vacation. MeritCare offers
comprehensive benefits package, relocation allowance and
paid malpractice insurance. To learn more about either of
these excellent practice opportunities contact: MeritCare
Health System Jean Keller, Physician Recruiter Phone:
701-280-4853.
Neuro-Oncology faculty position The Department of
Neurology at the University of Michigan is seeking applicants
for a neuro-oncology faculty position. The University has a
well-established program in neuro-oncology that includes
specialists in neurosurgery, radiation oncology, neuroradiology
and neuropathology. The position is offered at the Assistant/
Associate Professor rank in both the clinical and tenure
tracks. The successful candidate will be appointed in a track
commensurate with their experience and qualifications.
Applicants must be board certified or eligible in neurology with
fellowship training in neuro-oncology. Interested candidates
should contact Larry Junck, M.D., ljunck@umich.edu
734-936-7910. The University of Michigan is a nondiscriminatory, affirmative action employer and encourages
women and minorities to apply.
General & Subspecialty op’s with Marshfield Clinic General
and Subspecialty opportunities with Marshfield Clinic.
Marshfield Clinic is a 775 physician led organization with 41
centers throughout Wisconsin. Currently, we’re experiencing
growth at two of our largest facilities and are offering these
outstanding practice opportunities: General Neurology – Eau
Claire (expanding practice). Subspecialty interest is supported
by the department. Behavioral and Headache Neurologist Marshfield Center. Marshfield Clinic Neurosciences includes
22 neurologists representing a full range of Neurology
subspecialties and 6 neurosurgeons, 3 neuroradiologists and
3 neuropsychologists. Research opportunities abound but
are not prerequisite. The work atmosphere is academic and
collegial. As a physician with Marshfield Clinic you can
expect a very competitive salary and a benefit package that
includes liberal vacation, 10 days CME time w/$5,800
allowance, well funded retirement plan, health, dental,
life, disability and malpractice insurance, moving expense
allowance and more. If you are interested in learning more
about these opportunities, please contact: Sandy Heeg,
Physician Recruitment, Marshfield Clinic, 1000 N Oak Ave.,
Marshfield, WI 54449. Phone: 1-800-782-8581, ext. 19781;
Fax #: 715-221-9779. E-mail: heeg.sandra@marshfieldclinic.org
website: www.marshfieldclinic.org/recruit Marshfield Clinic
is an Affirmative Action/Equal Opportunity employer that
values diversity. Minorities, females, individuals with
disabilities and veterans are encouraged to apply. Sorry.
Not a health professional shortage area.
Neuro-Hospitalist Opportunity w/Marshfield Clinic NeuroHospitalist opportunity w/Marshfield Clinic. Marshfield Clinic
is a 775 physician led organization with 41 centers throughout
Wisconsin. This position is primarily hospital-based as a
member of a Neuro-Hospitalist service provided through a
large tertiary Neurology group. The physician hired will work
in rotation with other members of the Neuro-Hospitalist
service, providing consultation and patient care including
neurocritical care, throughout the hospital. This position
offers the opportunity of incorporating other areas of interest
and we would encourage applicants with interest in neurocritical care, cerebrovascular disease, and research to apply.
Subspecialty education and research are strongly supported.
Members of the Marshfield Clinic Neurology Department are
the primary medical staff for Saint Joseph’s Hospital, a 525
bed acute care tertiary teaching hospital that serves central
and north central Wisconsin. Sub-specialists are represented
in Sleep Medicine, Epilepsy, Movement Disorders, Stroke,
Neuromuscular Disease, Neuro-oncology, Dementia and
Neuroimmunology. As a physician with Marshfield Clinic
you can expect a very competitive starting salary of $300,000,
and a benefit package that includes liberal vacation, 10 days
CME time w/$5,800 allowance, well funded retirement plan,
health, dental, life, disability and malpractice insurance,
moving expense allowance and more. If you are interested
in learning more about these opportunities, please contact:
Sandy Heeg, Physician Recruitment, Marshfield Clinic, 1000
N Oak Ave., Marshfield, WI 54449. Phone: 1-800-782-8581,
ext. 19781; Fax #: 715-221-9779. E-mail: heeg.sandra@
marshfieldclinic.org website: www.marshfieldclinic.org/recruit
Marshfield Clinic is an Affirmative Action/Equal Opportunity
employer that values diversity. Minorities, females, individuals
with disabilities and veterans are encouraged to apply. Sorry.
Not a health professional shortage area.
AANnews • December 2008
27
Medical Malpractice Insurance for Neurologists Visit
www.tnpinsurance.com to learn more about The Neurologists’
Program (TNP) - the only medical malpractice insurance
program designed specifically for neurologists. TNP was
selected by the American Academy of Neurology (AAN) for
the AAN Partners Program. AAN members receive a 5%
premium discount. Other discounts available include: loss
free, group practice, part time practice, and more. TNP
insureds also have toll-free access to the Risk Management
Consultation Service helpline for one-on-one risk management
consultations. From the policy itself to the risk management
advice and guidance provided, TNP has one focus—
neurology. For more information, and to be notified when
TNP is available in your state, visit www.tnpinsurance.com,
e-mail TNP@prms.com, or call (800) 245-3333, ext. 389.
Neurologist Neurology Consultants, P.C. Davenport, Iowa.
Don’t make your final decision without visiting Davenport.
Seeking BE/BC Neurologist(s) to join established and well
respected neurology group in eastern Iowa community of
400,000. Mississippi River community with metropolitan
amenities for those with an active lifestyle and close
proximity to country life for those who enjoy the outdoors.
Reasonable cost of living. The adjacent 502-bed Medical
Center has a 20-bed monitored neurology unit. Share call
with 5 general neurologists. Opportunity to practice
subspecialty interests in addition to providing a full range of
general neurology care, including EMGs. Accredited sleep
lab and infusion center in-house. Two year track to
partnership. Generous benefits, including health insurance,
malpractice, CME and vacation time, and 401k. Guaranteed
2 year salary with productivity incentives. If interested please
contact Mary Boyd, Physician Recruitment, Genesis Medical
Center 888-437-5480 or Jerri Sharp, Office Manager,
Neurology Consultants, P.C. 563-383-5169.
Neurologist Altru Health System is seeking a BC/BE General
Neurologist to join its Neuroscience Department. Altru
Neuroscience has a long history of excellence and is the
premiere neuroscience group in the region. Full EEG and
EMG services are provided. A patient referral area of over
225,000 guarantees a busy practice with interesting pathology.
Altru’s Neuroscience Department is committed to working as
a team to better serve our patients. Call is 1:4. This is an
excellent practice opportunity with a competitive compensation
and benefits package. To inquire, contact Kerri Hjelmstad at
800-437-5373 ext. 6596 or khjelmstad@altru.org www.altru.org
Child Neurology - Children’s Hospital Join a dynamic and
growing team of Child Neurologists at a top-notch children’s
hospital with university affiliation, focused on clinical and
academic neurology. Huge metro and multi-state service
area, state-of-the-art equipment, optional supported research
capabilities in an outstanding new research facility. Opportunity
to focus on your subspecialty areas of expertise. Equal shared
call; unique work schedule with protected time. Excellent
income and benefits package offered. Robust, wealthy metro
area known for its exceptional lifestyle with two medical
schools, Fortune 500 headquarters, high quality lifestyle,
nationally ranked schools, enviable fine arts, and outstanding
sports/recreation. Email gstrohm@sherriff.com
Pediatric Neurology Carle Clinic Association, a 330-physician
owned and operated multispecialty group practice, is seeking
an additional BE/BC Pediatric Neurologist in UrbanaChampaign, Illinois. Carle Foundation Hospital, a 305-bed
facility that is a designated Level I Trauma Center and Level
III Co-Perinatal Unit, has a Pediatric Hospitalist service and
a Pediatric ICU service. Pediatric subspecialties include
Gastroenterology, Developmental-Behavioral, Pulmonology,
and Neurosurgery. Option for academic and/or research
affiliation with the University of Illinois. Competitive
compensation package and excellent benefits offered
(including paid malpractice insurance). Urbana-Champaign
has a population of 180,000, is home to the University
of Illinois, and is located 2 hours from Chicago and
Indianapolis. Please contact: Dawn Goeddel Telephone:
(800) 436-3095, extension 4103 Fax: (217) 337-4119
E-mail: dawn.goeddel@carle.com
Academic Neurologist The Wright State University (WSU)
Boonshoft School of Medicine, Department of Internal Medicine
seeks an academic neurologist at the Assistant or Associate
Professor level to be actively involved in a developing
Neurology Division. The successful candidate will provide
clinical care, participate in teaching medical residents and
28
December 2008 • AANnews
students, and develop laboratory-based or clinical research.
Part-time position is negotiable but full-time is preferred.
Candidates must possess an M.D. or D.O. degree and be
board eligible/certified in Neurology. All sub-specialties will
be considered. For position description and requirements,
please visit http://www.wright.edu/hr/job. Interested applicants
should submit their curriculum vitae and names of three
references to Bradley Jacobs, MD, MS, ATTN: Pam Berry,
Department f Internal Medicine, Wright State University, PO
Box 927, Dayton, OH 45401-0927 (email to bradley.jacobs@
wright.edu). Review of applications will begin December 15,
2008 and continue until the position is filled. WSU is an AA/
EO employer and promotes diversity in its workforce.
Excellent Midwest location for a BE/BC Neurologist Alegent
Health Clinic, a large multi-specialty physician organization
is seeking a Neurologist to join our team. The physician will
join the region’s premier healthcare system. Subspecialty
training is welcome but it is not required. Excellent
compensation package includes highly competitive base salary
with production incentives, comprehensive benefits package
including a relocation allowance, generous CME and more.
Omaha is a city on the move. With a metro population of
800,000+, growth and promise include new businesses,
new neighborhoods and new attractions. Email
Brenda.krull@alegent.org or call 877-244-8027.
Pediatric Neurologist The Division of Pediatric Neurology
at the 190-bed Helen DeVos Children’s Hospital in Grand
Rapids, MI has multiple openings for Pediatric Neurologists
and a Division Chief. Our vital, dynamic and growing
program of five physicians is focused on both clinical
neurology and research. The program features state-of-the-art
equipment including a fully digital EEG lab, inpatient video
EEG, and portable EMG. Call is shared equally among the
physicians. Qualifications include: board certified or board
eligible in Neurology with special qualification in Child
Neurology. EEG, EMG epilepsy or neuromuscular training a
plus. A desire in developing other subspecialty interests also
a plus. A new 200-bed Helen DeVos Children’s Hospital is
under construction, scheduled for completion in 2011.
The hospital services a population of over 3 million with
150 pediatric specialists in 40 pediatric specialties and is
a primary teaching hospital for Michigan State University.
MSU is scheduled to have a full four year medical school
operational in Grand Rapids by 2010. Grand Rapids,
Michigan’s second largest city with a metropolitan
population of 750,000 is located 35 minutes from the
beautiful shores of Lake Michigan. Grand Rapids is known
as the cultural, educational and economic hub of West
Michigan. Email diana.dieckman@devoschildrens.org
Neurorehabilitation Fellowship Please use the membership
of Dr. Rodger Elble Memorial Medical Center/Southern
Illinois University School of Medicine in Springfield, Illinois
has an opportunity for a 1-year clinical fellowship in neurorehabilitation for a BC/BE neurologist. Facilities include a CARFaccredited 30 bed acute inpatient rehab unit equipped to
accommodate stroke, spinal cord injury and traumatic brain
injury patients. The fellow will assist in managing patients
on the unit, and attend outpatient rehab, MS, ALS, and MDA
clinics. Additional experience in electrophysiology and
prosthetics/orthotics are available. Candidates must have
completed an accredited neurology residency program. Send
CVs to David Gelber, MD, 800 N 1st Street, Springfield, IL
62702; phone 217/528-7541, dgelber@springfieldclinic.com.
Visit MMC and SIU websites at www.memorialmedical.com
and www.siumed.edu/neuro SIU School of Medicine is an
EO/AA Employer.
Board Certified/Board Eligible Child Neurologist Seeking a
BC/BE Child Neurologist for full-time position at the Associate,
Assistant or Associate Professor (tenure or non-tenure clinical
track) level. Requirements: MD/DO Degree BC/BE in Psychiatry
and Neurology with Special Competence in Child Neurology
Candidates applying for a tenure track position must
demonstrate evidence of scholarly investigation Desirable
qualifications: Clinical experience in child neurology Strength
in teaching Experience in patient-oriented or basic research
Strong oral and written communication/interpersonal skills
Iowa City is a university town with diverse recreational
activities, superb public schools, and affordable, safe neighborhoods. University of Iowa Children’s Hospital and the Carver
College of Medicine have outstanding facilities for patient-care,
education, and research. More information at http://www.
uihealthcare.com/depts/uichildrenshospital/index.html.
Neurology Ohio-Consider this fantastic new Neurology
opportunity. Live and work in a community ideally located
15 miles from Dayton, Ohio and 50 miles from Columbus
and Cincinnati. Enjoy access to a leading-edge 12-bed
acute physical medicine and rehabilitation unit and a fully
accredited 4-bed sleep center. Special interest and/or training
in Movement or Behavioral Disorder is desired. Balance your
practice and lifestyle while enjoying outstanding cultural and
recreational opportunities with affordable housing and a strong
educational system. This is the perfect blend of big city living
and small town atmosphere. Email givekich@strelcheck.com
Stroke Medical Director Great exciting opportunity to develop
a Stroke Center for the new state-of-the-art Aurora Medical
Center that will be opening in 2010 in Grafton, Wisconsin.
We are recruiting for a Medical Director who is BC/BE
fellowship-trained in Stroke to develop the Stoke Center
at our new regional medical center. This person will be
responsible for putting together the stroke team, work toward
JCAHO accreditation and will be putting together the
protocols for the department. Enjoy a large referral base from
Aurora Advance Healthcare, a highly successful group of 250
+ physicians along with the physicians from Aurora Medical
Group. The medical center will have a 24-hour emergency
department, Vince Lombardi Cancer Center and a complete
array of other hospital services. A supportive practice
environment, well-trained ancillary staff, and a state-of-theart facility all enhance this attractive position. Generous
compensation package includes competitive income
guarantee, aggressive productivity incentive, relocation
allowance and full array of benefits including fully-paid
malpractice insurance; an employer-matching 403B
retirement fund, and an employer-funded pension. For more
information contact Judy Nelson at 800 307-7497 Ext 15
or email judy.nelson@aurora.org
BC/BE Neurologist Wisconsin-Metro Milwaukee Wisconsin –
Metro Milwaukee Employed or Private Practice. Traditional
or Inpatient Focused. Eclectic Urban or Lake County
Suburban. It’s all here. Aurora Medical Group, a highly
successful group of nearly 700 employed physicians seeks
BC/BE Neurologists for two practices. AMG-Oconomowoc
offers a general practice with unlimited potential to develop a
full scope neurology program in one of the fastest growing,
most affluent areas of Wisconsin. Enjoy referrals from 50+
physicians in this collegial group. Sleep or headache fellowship
a plus. AMG-Milwaukee seeks a general Neurologist that enjoys
inpatient medicine as a busy Neurologist in the heart of
downtown Milwaukee retires. This well-rounded practice
includes EMGs and a broad spectrum of office patients;
inpatient pain management and neuropathy consultations;
and teaching within Aurora’s residency programs. You’ll
benefit from the large referral base of AMG primary care
physicians throughout Milwaukee. The Center for
Neurological Disorders, a thriving private practice at St. Luke’s
Medical Center in Milwaukee, seeks a BC/BE general
Neurologist to help expand the cutting-edge technology of St.
Luke’s neuroscience program into two suburban areas. The
Center treats a broad range of disorders and has pioneered
innovative treatments and participated in advanced research
studies. Opportunity for partnership is available. To learn
more, contact Michelle Forray at 800-307-7497 or visit our
website at www.AuroraHealthCare.org/physicianopportunities
Neurologist Marquette General Neurology offers an excellent
opportunity for a BC/BE EMG- proficient- subspecialty interest
or certification welcome or electrodiagnostic medicine
certified neurologist to join an expanding practice. The Upper
Michigan Neuroscience Center at Marquette General
provides state-of-the-art care including: neurosurgery,
neuroradiology, interventional radiology, comprehensive
neurophysiology, physical medicine and rehabilitation,
complete imaging modalities Resources are complemented
by a medical staff of over 200 representing 64 specialties.
Competitive compensation & benefit package. Enjoy an
unmatched quality of life in a university community & a
pristine environment exempt from many of the pressures
of urban living. Our four-seasons climate & unique terrain
create numerous recreational opportunities. Contact:
Mike Gokey; msgokey@mgh.org, 906-225-6919 or E
ric Knauss; etknauss@mgh.org, 906-225-3447. 580 W.
College Ave, Marquette, MI. 49855 Visit www.mgh.org and
click on the physician job opportunities icon.
Neurology Opportunities-Dementia Mpls/St. Paul, MN
HealthPartners Medical Group, HealthPartners Neuroscience
Center, Regions Hospital, and the Regions Alzheimer’s
Research Center in Minneapolis/St. Paul, MN are looking for
a dementia specialist to head the Center for Dementia and
Alzheimer’s Care (BC/BE Neurologist with an interest in
dementia). As a key partner in the neurology clinic and an
associate in a large multidisciplinary group of physicians you
are guaranteed a busy practice. The position includes seeing
general neurology patients with an emphasis on memory loss
and dementia, but also creating care models for primary care,
specialty care and hospitalized patients that maximize the
quality of care for these patients. HealthPartners is well
recognized regionally and nationally as a leader in health
care quality and care model development. The system
emphasizes creating best care models and protocols in order
to maximize the value of the care provided to their patients.
The Regions Alzheimer’s Research Center is recognized for
its cutting edge research on dementia care. With this well
funded position, the opportunity to collaborate with the Regions
Alzheimer’s Center, and the chance to do what is best for
dementia patients, a rewarding career is assured. Our team
of eight neurologists has subspecialty interests and training in
stroke, epilepsy, neuromuscular disease, sleep, dementia,
movement disorders and multiple sclerosis. We are affiliated
with the University of Minnesota Medical School, participating
in teaching programs for students, residents and practitioners.
The dementia team includes a neuropsychologist, a physician’s
assistant and a nurse coordinator as well as other key stake
holders: 300 primary care doctors, 20 gerontologists, 4
geropsychiatrists, and 55 hospitalists. For consideration,
please forward your CV and cover letter to Lori Fake at
lori.m.fake@healthpartners.com or FAX (952) 883-5395.
For more information, call (800) 472-4695 or apply
online at www.healthpartners.jobs. EO Employer
HealthPartners Medical Group www.healthpartners.com
www.regionshospital.com
Neurologist-Michigan Join a group of three neurologists at a
new leading-edge Neuroscience Center located on the shores
of beautiful Lake Superior. This practice successfully combines
neurology and neurosurgery. This Level II hospital has an
outstanding emergency, inpatient rehabilitation and a
radiology department. Opportunity exists to pursue and
cultivate your subspecialty interest. This city is home to
Northern Michigan University offering residents a broad array
of cultural activities. Recreational opportunities including
sailing, fishing, golf, mountain biking, skiing and hiking.
This gorgeous area is well renowned for its towering pines,
majestic rivers and crystal blue streams. Email
givekich@strelcheck.com
Multi-specialty group seeks Neurologist Physician-owned,
multi-specialty group practice with 100+ providers, has an
exceptional opportunity for a BC/BE Neurologist to join two
others. You will see patients with a full spectrum of disease
states and have an opportunity to participate in clinical trials.
We provide staff and support for EMG, Lumbar Punctures,
Polysomnograpy, Botox, Occipital Block and a full-time, plus
a registered EEG technologist. We offer a market competitive
income guarantee with a production incentive income
thereafter; service area 300,000; great payer mix; life/health/
disability and medical malpractice insurance all paid; $6,600
annual CME allowance; potential shareholder status after one
year; 401(k) profit sharing plan. Our picturesque community,
population 50,000+ provides a great setting to practice
medicine and raise a family plus year-round indoor/outdoor
recreational at nearby lakes and resorts; excellent public and
private schools with award winning academics and sports
teams; state university and three colleges with combined
enrollment of over 18,000; shopping mall with five anchor
stores and more new retail construction. One hour from
Minneapolis/St. Paul southern metro; easy access
to international airport. No J-1 openings. Email
ddavito@mankato-clinic.com
Neurologists-Kalamazoo, MI Bronson Neurological Services
has an outstanding clinical opportunity in southwest Michigan
for an energetic Neurologist with interest/experience in
Movement Disorder or Dementia to lead their Neurodegenerative Program. Individual must be BE/BC and be willing to
serve a multi-disciplinary patient population including
regional clinics in Southwest Michigan. Full-time, hospital
employed position with competitive compensation and
comprehensive benefits. Bronson Methodist Hospital, a tertiary
referral center serving all of southwest Michigan and northern
Indiana, maintains a dedicated Neurovascular Unit for focused
care, is a Certified Primary Stroke Center by the Joint
Commission and is a Level 1 Trauma Center. For more
information about Bronson Methodist Hospital go to
www.bronsonhealth.com. Kalamazoo, located between
Detroit and Chicago, offers diverse cultural opportunities,
economic diversification and very affordable real estate.
Public, private and parochial schools are recognized for
their academic excellence. For more information about
Kalamazoo visit www.kalamazoomi.com. Contact Cadace
Lee at 800-594-9022 or e-mail: leeca@bronsonhg.org.
BC/BE Neurologists BC/BE Neurologists: Unique Opportunity
to join in practice with eight well-established, familyoriented, Board certified adult neurologists. Three unique
positions available: 1. City-wide Parkinson’s specialty clinic,
already established, with an opening for a movement
disorder sub-specialty trained candidate. 2. Neuro-intensive/
stroke subspecialty trained candidate to join an established
acute stroke program. 3. General neurologist with subspecialty training. This is a private practice with wellestablished referral networks and opportunities to participate
in teaching residents and medical students. Competitive
salary, excellent corporate benefits, outstanding partnership
potential. The Twin Cities have wonderful culture, education
and recreation opportunities at a reasonable cost of living.
Contact: Neurological Associates of St. Paul, P.A., Thomas
Jacques, M.D., 1650 Beam Ave, Suite 200, Maplewood, MN
55109 phone 651-221-9051, Fax 651-223-5220
Hospital-based Neurologist, NCC or Vascular Bronson
Neurological Services has an outstanding clinical opportunity
in southwest Michigan for an energetic BE/BC hospital-based
Neurologist with interest/experience in Stroke or Neurocritical Care Medicine to participate in the development of their
growing Neurocritical Care and Neurovascular Services. Fulltime, hospital employed position with competitive compensation and comprehensive benefits. Bronson Methodist Hospital,
a tertiary referral center serving all of southwest Michigan and
northern Indiana, maintains a dedicated Neurovascular Unit
for focused care, is a Certified Primary Stroke Center by the
Joint Commission and is a Level 1 Trauma Center. For more
information about Bronson Methodist Hospital go to
www.bronsonhealth.com. Kalamazoo, located between
Detroit and Chicago, offers diverse cultural opportunities,
economic diversification and very affordable real estate.
Public, private and parochial schools are recognized for
their academic excellence. For more information about
Kalamazoo visit www.kalamazoomi.com.
SOUTH CENTRAL
Neurologist - Best Small Town City Stillwater Medical Center
is a progressive 130-bed, JCAHO-accredited facility located
in a lovely university town in North Central Oklahoma.
Stillwater, listed as the # 6 “Best Small Town City” in America,
is located in the heart of Oklahoma’s countryside just 60 miles
from the two largest cities in the state, Oklahoma City and
Tulsa. A trust authority of the City of Stillwater, Stillwater
Medical Center serves a primary population of 68,500 and a
secondary area of approximately 110,000. Stillwater Medical
Center has been named one of Solucient’s Top 100 Performance
Improvement Hospitals. We are currently recruiting for a
General Neurologist to join our community. This position
represents an excellent professional and financial opportunity
for a motivated Neurologist. The Medical Center is offering
a competitive financial package from loan guarantee to
employment. With a diverse and multi-cultural population,
Stillwater is known as “Oklahoma’s Education Community,”
home of Oklahoma State University. The Stillwater Public
School district has been rated among the “Top 100” districts
in the U.S., and Expansion Management Magazine gives
Stillwater High School its highest “Gold Medal” rating for
workforce preparation. A city designed with the charm of a
smaller community, Stillwater offers a variety of cultural
activities such as live theater, concerts, special art exhibits,
and university lectures. The region also offers exceptional
outdoor recreational activities as well as easy access to four
superb golf courses and excellent shopping within a one-hour
drive. If this opportunity sounds appealing and you would
like further information, please respond. I look forward to
speaking with you soon. Reply to Blind Box #3894.
Neurologist Needed in Dallas, TX Baylor University Medical
Center in Dallas, TX is seeking a BE/BC Neurologist for a
position on its inpatient Neurologic Hospitalist Staff. We are
looking for exemplary residents, fellows or practicing physicians
who would like to join a collaborative team of world-class
specialists including neurosurgeons, neuro-oncologists, general
neurologists, vascular neurology specialists, radiation
oncologists, neuro-pathologists, and neuro-radiologists. We
are considering candidates who are interested in pursuing a
career in Dallas, and establishing their practice, as well as
candidates who would be available for a single year.
Contact Meghan Speer, Baylor Physician Recruitment, at
972-860-8506 or MeghanS@baylorhealth.edu if interested.
Adult Neurologist Wanted We are a busy adult neurology
group in the Dallas-Fort Worth area, and urgently need to
add 1 or 2 more members. We have ambulatory EEG, EMG,
sleep lab, multiple sclerosis clinic, neuromuscular clinic, and
infusion center. Excellent salary. Email mcm@prodigy.net
Lucrative Mid-Atlantic Medical Directorship Thriving
hospital-based or private neurology position with top regional
medical center in charming Mid-Atlantic community. Easily
develop sub-specialty. Medical Directorship with 100k
directorship stipend. Excellent financial package, 295k salary,
50k signing bonus, benefits. 1 hour from Metro. Tort Reform
State. Beautiful mountains and rivers. Exceptional recreational
activities– white-water rafting, snow skiing, hunting and
fishing. Excellent public and private schools. Will consider
h1 and j1. Brian White 1-888-339-7444, brian@xrhs.net, fx
940/234-5315.
General Neurologist Neurological Consultants of Kansas City
Inc, is searching for a general neurologist, looking to join a
team where aggressive stroke reversal therapy is the norm.
We are the only integrated inpatient and outpatient program
dedicated to improving outcomes in patients with diseases of
the nervous system and spine. Saint Luke’s Hospital has been
a leader in Healthcare for the KC area and has received numerous quality awards. Are interested in learning more about this
opportunity, please forward your CV to: Neurological
Consultants of KC Inc Attn: HR 4400 Broadway Suite 520
Kansas City, MO 64111 kcmorem@aol.com
General Neurologist Ochsner Health System in New Orleans
is seeking a Board Certified/Board Eligible General Neurologist
to join our group of Neurology physicians. Subspecialty
interests represented within the institution include epilepsy,
headache, movement disorders, neuromuscular disease,
neurophysiology, sleep disorders, and stroke. While this is
primarily an outpatient position, there is also responsibility
on the hospital consult service and the opportunity to teach
residents, house staff, and medical students. Candidates
currently completing training as well as those with practice
experience are welcomed to apply. Ochsner Health System is
a non-profit, academic, multi-specialty healthcare delivery
system dedicated to patient care, research, and education.
The system includes 7 hospitals and 40 health centers
throughout Southeast Louisiana. Our staff includes 600+
physicians in 80 medical specialties and sub-specialties.
Ochsner conducts over 300 ongoing clinical research trials
annually. Salary is competitive and commensurate with
experience, and we offer an excellent benefits package.
We also enjoy the advantage of practicing in a favorable
malpractice environment in Louisiana. Please visit our website,
www.ochsner.org for more information. New Orleans amenities
include: multiple medical schools and academic centers,
professional sports teams, world-class dining and cultural
interests, and world-renowned live entertainment and
music. Please e-mail CV to profrecruiting@ochsner.org,
Ref #ANOGN05, or call 800-488-2240. EOE.
WEST
Neurologists The Nevada Neurosciences Institute at Sunrise
Hospital (NNI) is currently seeking a general neurologist to
join two board certified neuro-hospitalists in a thriving 5physician practice in Las Vegas, NV. The NNI is southern
Nevada’s first comprehensive clinical neurosciences center,
providing access to world-class doctors and pioneering
medical research. Housed at Sunrise Hospital, NNI offers an
evolving lineup of neurosciences expertise, including a
JCAHO Certified Primary Stroke Center, Neurosurgery,
Interventional Neuroradiology, as well as centers for Epilepsy
AANnews • December 2008
29
and Multiple Sclerosis. All existing neurologists are fellowship
trained and highly regarded within their specialty. Located in
the heart of Las Vegas, Sunrise Hospital and Medical Center,
is a state-of-the-art 701-bed acute care facility with
comprehensive inpatient and outpatient services. The
medical complex includes Nevada’s only dedicated
Children’s Hospital and specializes in women’s and children’s
services; cardiovascular, oncology, neurology, medical and
surgical services. Generous compensation and benefits
package with relocation expenses will be provided. Practice
management support provided by HCA Physician Services.
If you or someone you know is interested, please contact
Linda Erwin, HCA Healthcare, 800-824-9275;
Linda.Erwin@HCAHealthcare.com.
BC/BE Neurologist Great opportunity for a general BC/BE
Neurologist with EMG capability. ABQ Health Partners is the
largest physician-owned, multi-specialty group practice in the
Southwest, with 18 locations in Albuquerque, Rio Rancho, and
Santa Fe. Albuquerque offers a mild four season climate, nearby
skiing and lakes, and a number of unique and multicultural
activities. For more information and to view additional job
openings, visit our website at: www.abqhp.com or contact
Deborah Baca, Manager Physician Recruitment & Retention
at: (505) 262-7296. EOE
Neurologist - Las Vegas, NV Las Vegas Neurology Practice
seeking a BC/BE Neurologist. The ideal candidate will have
expertise in General Neurology, EMG, EEG and sub-specialty
training in Sleep and Epilepsy. The Practice offers: excellent
base salary ($250,000+ based on subspecialty & experience),
sign-on & production bonuses with a partnership track, no
state tax, out-patient & in-patient positions, Monday – Friday,
7am – 4pm Out-Patient only schedule available. Paid CME
and vacation time, EMR, support staff including: MAs, PAs,
and NCV/EEG Technicians. Help with relocation, housing,
legal, and accounting needs. For inquiries call (888) MSOLVNV (1-888-676-5868) and leave a message so that we may
respond to your inquiry. Please E-mail your CV and cover
letter to: Recruit@MedStaffOptions.com
Pediatric Neurologist No Adult Care/No Primary Call. Join
our Pediatric Center with nine pediatricians and pediatric
subspecialists as a full-time Pediatric Neurologist. Busy
practice from day one, with strong regional referral network
to our tertiary care center. Pediatricians take all first call and
there is no shared call with adult neurology. Beautiful facility,
national clinical quality awards, physician leadership.
Located near the magnificent Rocky Mountains in Billings,
Montana. Friendly college community with great schools,
safe neighborhoods and family activities. Exciting outdoor
recreation just minutes from home. 300 days of sunshine.
Email rdwoods@mountainmedgroup.com
Neurologists-Arizona BC/BE Neurologists-Phoenix, AZ Metro
area. As a physician, your Perfect Practice Environment likely
includes a culture which embraces a balance between life
and work; Banner Health has held this philosophy from the
beginning - it’s one of the main reasons our physicians tend
to settle in with us. And our Arizona location offers a perfect
environment for outdoor activities year round. Banner Baywood
Medical Center (BBMC) is seeking Neurologists to be part of
its growing Stroke Program and also be part of the team that
will help it grow into an expanded Neuroscience Program.
Stroke training preferred. BBMC recently completed a new
seven-story patient tower in 2006, adding 120-plus beds to
the existing 242. The expansion also included a new 26-bed
ICU, additional operating rooms, and expanded Pharmacy,
Lab, and Radiology. Banner Desert Medical Center (BDMC)
is currently seeking two board certified or board eligible
Neurologists. BDMC is expanding their Neurosciences
program and is looking to employ these physicians as part of
Banner Medical Group. Stroke training preferred. BDMC is the
largest, most comprehensive hospital in the East Valley of
Metro Phoenix with 611 licensed beds and 1200 physicians
representing 65 specialties. The hospital is among the top
two percent in the nation in Emergency Room volume treating
nearly 100,000 patients annually. Excellent compensation
and benefits. For more information, contact: Banner Health
Physician Recruitment; Phone: 866-585-5418; Fax: 602-6403652; or E-mail: bannerazdocs@bannerhealth.com Visit our
website at: www.bannerdocs.com Not a J-1 opportunity. EOE
Cerebrovascular Neurologist - Arizona Cerebrovascular
Neurologist-Medical Director of Stroke Program. Phoenix, AZ
Metro area. As a physician, your Perfect Practice Environment
likely includes a culture which embraces a balance between
life and work; Banner Health has held this philosophy from
the beginning - it’s one of the main reasons our physicians
tend to settle in with us. And our Arizona location offers a
perfect environment for outdoor activities year round. We’re
seeking a well-trained physician to provide leadership,
direction and guidance of our established and growing Stroke
Program at Banner Baywood Medical Center in Phoenix/Mesa,
AZ. The right candidate will be able to take this program to
the next level, continuing the standards of care for a Primary
Stroke Center and future expansion and integration of a
Neurosciences Program. The hospital is accredited by JACO
as a primary stroke center in the east valley. Opportunity
exists to have combined inpatient/outpatient practice if
desired. Excellent compensation and benefits. For more
information, contact: Banner Health Physician Recruitment;
Phone: 866-585-5418; Fax: 602-640-3652; or E-mail:
bannerazdocs@bannerhealth.com Visit our website at:
www.bannerdocs.com Not a J-1 opportunity. EOE
PACIFIC
Fellowship training for Post-residency M.D.’s Extended
fellowship training opportunities for Post-Residency M.D.’s,
leading to acquisition of Ph.D. Degree in Neuroscience from
the University of California, San Diego. Extended periods of
funding are available for M.D.’s who have completed
residency training and wish to pursue extended fellowships in
clinical and/or basic neuroscience. Full funding is available
to support applicants in a variety of fields, including nervous
system aging, degeneration, regeneration, gene therapy,
development, ion channels, basic investigations of nervous
system electrophysiology, and others. Applicants may apply
to the neuroscience graduate program with the aim of
successfully completing the requirements for a Ph.D. in
neuroscience, funded at competitive post-M.D. salary levels.
Training is available at the University of California-San Diego,
Salk Institute for Biological Studies, and Scripps Research
Foundation. The goal of this program is to train outstanding
physician scientists. For more information, contact Mark H.
Tuszynski, M.D., Ph.D. Department of Neurosciences-0626,
University of California-San Diego, La Jolla, CA. 92093.
Phone (858)534-8857. Email: mtuszynski@ucsd.edu.
Applicants must be U.S. citizens or permanent residents.
Pediatric Neurologist-Portland, OR Providence St. Vincent
Medical Center is seeking a Pediatric Neurologist to join busy
practice providing outpatient consultations and NICU services.
Candidates should have strong interest in general neurological conditions; subspecialty interest in genetic metabolic,
neuromuscular, and developmental disorders and epilepsy
desirable. Providence St. Vincent’s Pediatrics Department
includes pediatric hospitalists and subspecialists in cardiology,
endocrinology, emergency, gastroenterology, neurology, sleep,
radiology and surgery. Advanced NICU with Level III nursery,
pediatric rehab division, and pediatric developmentalists.
Portland features world-class urban amenities and outdoor
recreation with nearby mountains, forests and beaches.
Details: Patti Langdon, (503) 216-5458; Patti.Langdon@
providence.org ; www.providence.org/physicianopportunities
Neurology Residency Training - PGY2 Position Avail UCLA
Dept of Neurology is seeking applicants for two neurology
PGY2 residency positions that will begin on July 1, 2009.
Applicants should have completed a traditional internship in
internal medicine or transitional year of training in ACGMEaccredited programs by the time of joining our program. Please
send a CV, letters of recommendation, USMLE scores, and a
personal statement to: Gloria Gorden, MPH, Director, Office
of Education, UCLA Dept of Neurology, 710 Westwood Plaza,
1240 RNRC, Los Angeles, CA 90095. Fax 310-206-4733. Email
address: GWGorden@mednet.ucla.edu. Emails are preferred.
Neurology Opportunity, Walla Walla, Washington Walla
Walla Clinic, a collegial 37-member multispecialty group
nestled in the heart of Southeast Washington’s wine country,
is seeking a BE/BC Neurologist. This is a true consultative
Neurology position; EMG’s, EEG’s and Botox. Benign call
schedule, 4.5 day work week; busy, ready-made practice and
strong referral base. Competitive compensation package
leading to partnership; pension plan, 401 K, paid medical,
dental and malpractice insurance. Historic Walla Walla offers
nearly 300 days of sunshine per year, abundant recreational
activities, 100 wineries, vibrant theater and symphony,
excellent schools and no state income tax. Email
karen.uden@stratummed.com
MS Medical Director and MS Neurologist The MS Center at
Evergreen Hospital Medical Center in Kirkland, Washington
is seeking two exceptional neurologists specializing in the
treatment of MS to fill Medical Director and MS Neurologist
positions. The MS Center is part of the Evergreen Neuroscience
Institute (ENI), which is the umbrella organization for MS,
Parkinson’s, Movement Disorders and Stroke. In existence for
approximately two years, the MS Center has received a strong
commitment from Evergreen administration to meet the needs
of the MS community. In May 2009, ENI will move to a new
state-of-the-art facility on the Evergreen campus which will
house clinical care, research and a specialized neuro-rehab
space with the strong support of a vibrant local MS community.
As an MS “center of excellence” and the sole center for the
MS community on Seattle’s Eastside, we provide coordinated,
comprehensive care, research and education to improve the
lives of those who have and care for those with MS. The
Center offers patients direct and convenient access to expert
providers and state-of-the-art services, including neurology,
radiology, urology, rehab medicine and clinical trials. At the
heart of the MS Center is a thriving outpatient clinical practice
that serves a diverse patient population from the five-state
region of Washington, Alaska, Wyoming, Montana and
Idaho. Patient visits are projected to exceed 3,000/year. The
staff includes an experienced fellowship-trained Physiatrist
who specializes in MS practice and research. Staff support
includes a rehab psychologist, RN, medical assistant, and full
neuro-rehab team. Numerous ancillary classes and programs
are in place with a focus on wellness. These positions offer
exceptional opportunities to lead and further develop an MS
program that offers leading-edge treatment and rehabilitation
in an atmosphere where patients and families come first,
where hope and compassion combine with powerful
medicine to create life-changing care. These are unique
opportunities to work in a comprehensive MS Center with the
flexibility to combine a clinical practice with research in a
strongly supportive hospital affiliated environment. Call
coverage is limited to the MS population. Call coverage for
stroke or other general neurology call is not required.
Adequate time is allotted in the clinic in order to deliver superb
care. The position offers a very competitive, guaranteed base
salary and includes a generous benefit package including
4 weeks of vacation and a matching 457 retirement plan.
Relocation assistance is also available. For more information
about the MS Center at Evergreen please visit our web site
www.evergreenhealthcare.org. Interested physicians may
contact Jacqueline Carie, Physician Recruiter at
Evergreen Healthcare, (425) 899-2540 or email
jacarie@evergreenhealthcare.org.
Hawaii Permanente Medical Group/Kaiser Permanente
Positions available in Honolulu & Maui. Hawaii’s most
established multi-specialty group of 400+ physicians recruiting
for BC/BE Neurologists in two locations. Main medical center
in Honolulu: busy outpatient clinic, with call, neuromuscular
fellowship trained preferred. Wailuku, Maui: busy outpatient
clinic, with call, (EEG, EMG/NCV and evoked potential
capabilities). Excellent interpersonal skills are required.
Applicants must a have a commitment to quality care, patient
advocacy, and involvement in patient and professional
education. We offer competitive salary, comprehensive
benefits, relocation assistance, with easy access to the best
beaches as well as outstanding recreational activities unique
to the islands. Send CV to: Physician Recruitment, HPMG,
501 Alakawa Street, Suite 255, Honolulu, HI 96817-5764;
or FAX (808) 432-4620; email: Janice.Omori@kp.org. EOE.
Movement Disorders Fellowship The Parkinson’s disease and
Movement Disorders Clinic at the USC/Keck School of
Medicine is offering a one-two year fellowship starting July
2009. Training will involve participation in an active
movement disorders clinic with 4 fellowship trained faculty.
Fellowship includes in depth exposure to the diagnosis and
management of a large variety of movement disorders
including PD and related disorders, tremor, dystonia and
spasticity. Fellows will be trained to inject botulinum toxins
and participate in a large clinical trials program. Training
includes an active program for the evaluation and treatment
of DBS patients. Requirements: Neurology Residency eligible
for California Medical License. Contact: Gloria Regalado at
gregalado@surgery.usc.edu
Join a Neurology Practice Like no Other Founded by a
Respected Neurologist experienced in MS and Headache
(Subspecialty Certified). Active Clinical Trials program,
including Migraine, Alzheimer’s, MS, Epilepsy, Parkinson’s.
Infusion Suite, Neurodiagnostic Testing and BOTOX.
Experienced Staff including PA, NP, RN and Administrator.
Suburban Southern California Community with Excellent
Public Schools. Flexible Contract and Schedule. No Hospital
Call. University Affiliation Available. Email CV to neuro.
resume@sbcglobal.net or FAX to 714-738-3758 or reply
to Blind Box #3878.
Neurologist-Bureau of Medicine and Surgery Camp
Pendleton, CA. Handle the most difficult cases in inpatient/
outpatient environment. Train/supervise interns, residents,
fellows. Care for active duty service members, dependents,
retired adult patients. Outstanding benefits: pay incentives,
malpractice coverage, lifetime health insurance you can carry
into retirement (Navy pays portion, you pay with pre-taxed
dollars), retirement plan w/401-K type plan, employer
matching, and ability to retire between 55-57 w/10 years of
service. Also life insurance, long term care insurance, 12-26
paid vacation days, 13 paid sick days, 10 paid Federal
holidays each year. Requirements: accredited MD/DO, physician license by any state, at least 5 yrs Neurology residency
training or equivalent experience/training, U. S. citizenship,
BC/BE desired but not required. E-mail your resume to
medjobs@navy.mil, include Neurologist in your subject line,
and cut/paste your resume into your e-mail message as we
cannot accept attachments. Or mail your resume to U. S.
Department of Navy, HRSC-NE, 111 S. Independence Mall
East, Attn: BUMED/Neurologist, Philadelphia, PA, 19106. For
more information, contact Charlotte Cleghorn 215-408-5441.
Neurology Opportunities in Olympia, Washington
Established group of five neurologists seeking two more: one
general, one with stroke/vascular fellowship or training.
Fellowship preferred, except for pediatrics or sleep. EMG
trainingTNP_hlfpg_color.pdf
preferred. Great 11/14/2008
call, competitive
and
12:10:53compensation
PM
benefits. Group participates in clinical research and teaching
through UW, plus teaching FP residents at Providence St.
Peter Hospital here. St. Peter boasts a superb neuroscience
program and diagnostic equipment, including 64 slice CT,
1.5t MRI, bi-plane angiography, and intra-operative
monitoring. Providence has other physician opportunities
in Alaska, California, Montana, Oregon and Washington.
For details, please contact Kris Cable,
kris.cable@providence.org; (503) 216-5468;
www.providence.org/physicianopportunities.
Private Practice Neurologist Well-established, multi-specialty
neurology practice in North County San Diego seeks two
BC/BE Neurologists with a strong work ethic and desire to
provide top quality care. Subspecialty training in Movement/
Neuro-degenerative Disorders is desired. Subspecialty training
in video EEG required. Opportunity to pursue clinical research.
Shared call. Practice is paperless office with an EHR.
Competitive salary and benefits package with partnership
opportunity. Please see our web site at www.neurocenter.com.
Interested candidates should submit CV to
tibbsv@neurocenter.com
Stroke Neurologist – Seattle, Washington Virginia Mason
Medical Center seeks a BC/BE Neurologist to join the
Neuroscience Institute & Stroke Center. Virginia Mason is
a multi-specialty clinic and hospital located in the heart of
downtown Seattle. Our JCAHO-certified Stroke Center is the
recent recipient of the Gold Performance Achievement
Award from the American Heart Association and received the
Stand-up for Patient Safety Award from the National Patient
Safety Foundation this year. Our vision to be the Quality
Leader in stroke and neurologic care. Work F/T, Mon-Fri,
with call 1:10 for weekends & evenings. This position is
approximately 50% stroke, 40% general neurology and 10%
research. A fellowship or strong background in stroke as well
as skills in leadership and program development are required.
We seek an individual who is interested in research,
developing novel acute therapies for stroke, and teaching.
Excellent compensation & a rich benefit package will be
offered. To apply, send CV to: Gail.Donovan@vmmc.org
or call 206-341-0448.
Neurologist Group Health Permanente, the Northwest’s
Premier Multi-Specialty Group is currently seeking BC/BE
Neurologists to join our team in Tacoma, WA. The ideal
candidate(s) will have a full range of hospital skills as well as
an interest in working in an innovative group practice. Flexible
schedules and outstanding teams make this opportunity
worth exploring. Competitive salary and generous benefits
packages offered. Email vanassen.j@ghc.org
Neurologist Clinician-Educator Santa Clara Valley Medical
Center in San Jose, CA is seeking an adult neurologist board
certified or eligible in neurology. Subspecialty training in
neuromuscular disorders, epilepsy, clinical neurophysiology,
stroke or outpatient neurology preferred. Responsibilities
include outpatient clinical care, consultation services and
Stroke Center. Should be committed to teaching neurology
residents and students and eligible for appointment as Stanford
Affiliated Clinician-Educator. SCVMC is a 570 bed public
teaching hospital and integrated health system. Submit
curriculum vitae with names and addresses of three
references to: Jeffrey Fraser, MD, Department of Neurology,
751 S. Bascom Avenue, San Jose, CA 95128.
Jeff.Fraser@hhs.sccgov.org
Join Providence Brain Institute in Portland, OR Portland,
Oregon--Providence Health & Services is seeking an excellent
BE/BC Neurologist (subspecialty interest welcome) to join our
strong multidisciplinary team dedicated to quality neurological
services. New physician will be part of Providence Brain
Institute (PBI), our renowned care and research program.
Subspecialty interest not required, but welcome. PBI includes
regional Multiple Sclerosis and Stroke centers as well as
neurosurgery, orthopedic spine, dementia, epilepsy and other
clinical and research programs. Excellent administrative,
research and nursing staff, and ample research opportunities.
Practice on the campus of Providence St. Vincent Medical
Center in beautiful west Portland. Excellent compensation
and benefits package. Please contact Patti Langdon,
503-216-5458; Patti.Langdon@Providence.org or through
our Web site, www.providence.org/physicianopportunities
Risk management questions?
We’ve got you covered!
In your day-to-day practice, you may face situations or requests that may trouble you,
raise questions or cause concern. TNP insureds can rest assured.
The toll-free Risk Management Consultation Service helpline is available to all TNP
insureds and provides direct access to risk managers who provide advice tailored to the
insured’s specific needs. We regularly respond to a broad range of professional liability
issues associated with requests to release medical records, informed consent, treatment
guidelines, documentation, medication events and more.
From the policy itself to the risk management advice and guidance we provide, TNP
has one focus - neurology. Contact us today to learn more about the only insurance
program designed specifically for neurologists and let our expertise work for you.
www.tnpinsurance.com ~ (800) 245-3333, ext. 389
TNP is growing! Visit us online to see if TNP is available in your state.
TNP is an AAN member benefit offered
through the AAN Partners Program.
CYMBALTA�
Drug-Placebo Difference in
Number of Cases of Suicidality
per 1000 Patients Treated
Increases Compared to Placebo
<18
14 additional cases
18-24
5 additional cases
Decreases Compared to Placebo
25-64
1 fewer case
≥65
6 fewer cases
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but
the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several
months. However, there is substantial evidence from placebo-controlled maintenance trials in
adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored
appropriately and observed closely for clinical worsening, suicidality, and unusual changes
in behavior, especially during the initial few months of a course of drug therapy, or at times
of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility,
aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania,
have been reported in adult and pediatric patients being treated with antidepressants for major
depressive disorder as well as for other indications, both psychiatric and nonpsychiatric.
Although a causal link between the emergence of such symptoms and either the worsening of
depression and/or the emergence of suicidal impulses has not been established, there is
concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly
discontinuing the medication, in patients whose depression is persistently worse, or who are
experiencing emergent suicidality or symptoms that might be precursors to worsening depression
or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the
patient’s presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as
rapidly as is feasible, but with recognition that discontinuation can be associated with certain
symptoms [see Warnings and Precautions, Discontinuation of Treatment with Cymbalta].
Families and caregivers of patients being treated with antidepressants for major depressive
disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about
the need to monitor patients for the emergence of agitation, irritability, unusual changes in
behavior, and the other symptoms described above, as well as the emergence of suicidality,
and to report such symptoms immediately to health care providers. Such monitoring should
include daily observation by families and caregivers. Prescriptions for Cymbalta should be
written for the smallest quantity of capsules consistent with good patient management,
in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder—A major depressive episode may be the initial
presentation of bipolar disorder. It is generally believed (though not established in controlled
trials) that treating such an episode with an antidepressant alone may increase the likelihood
of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any
of the symptoms described above represent such a conversion is unknown. However, prior to
initiating treatment with an antidepressant, patients with depressive symptoms should be
adequately screened to determine if they are at risk for bipolar disorder; such screening should
include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and
depression. It should be noted that Cymbalta (duloxetine) is not approved for use in treating
bipolar depression.
Hepatotoxicity—There have been reports of hepatic failure, sometimes fatal, in patients treated
with Cymbalta. These cases have presented as hepatitis with abdominal pain, hepatomegaly,
and elevation of transaminase levels to more than twenty times the upper limit of normal with
or without jaundice, reflecting a mixed or hepatocellular pattern of liver injury. Cymbalta should
be discontinued in patients who develop jaundice or other evidence of clinically significant liver
dysfunction and should not be resumed unless another cause can be established.
Cases of cholestatic jaundice with minimal elevation of transaminase levels have also been
reported. Other postmarketing reports indicate that elevated transaminases, bilirubin, and alkaline
phosphatase have occurred in patients with chronic liver disease or cirrhosis.
Cymbalta increased the risk of elevation of serum transaminase levels in development program
clinical trials. Liver transaminase elevations resulted in the discontinuation of 0.3% (82/27,229)
of Cymbalta-treated patients. In these patients, the median time to detection of the transaminase
elevation was about two months. In placebo-controlled trials in any indication, elevation of
ALT >3 times the upper limit of normal occurred in 1.1% (85/7,632) of Cymbalta-treated
patients compared to 0.2% (13/5,578) of placebo-treated patients. In placebo-controlled studies
using a fixed dose design, there was evidence of a dose response relationship for ALT and AST
elevation of >3 times the upper limit of normal and >5 times the upper limit of normal, respectively.
Because it is possible that duloxetine and alcohol may interact to cause liver injury or that
duloxetine may aggravate pre-existing liver disease, Cymbalta should ordinarily not be
prescribed to patients with substantial alcohol use or evidence of chronic liver disease.
Orthostatic Hypotension and Syncope—Orthostatic hypotension and syncope have been
reported with therapeutic doses of duloxetine. Syncope and orthostatic hypotension tend to
occur within the first week of therapy but can occur at any time during duloxetine treatment,
particularly after dose increases. The risk of blood pressure decreases may be greater in patients
taking concomitant medications that induce orthostatic hypotension (such as antihypertensives)
or are potent CYP1A2 inhibitors [see Warnings and Precautions and Drug Interactions] and in
patients taking duloxetine at doses above 60 mg daily. Consideration should be given to
discontinuing duloxetine in patients who experience symptomatic orthostatic hypotension and/
or syncope during duloxetine therapy.
Serotonin Syndrome—The development of a potentially life-threatening serotonin syndrome
may occur with SNRIs and SSRIs, including Cymbalta treatment, particularly with concomitant
use of serotonergic drugs (including triptans) and with drugs which impair metabolism of
serotonin (including MAOIs). Serotonin syndrome symptoms may include mental status
changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile
blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination)
and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of Cymbalta with MAOIs intended to treat depression is contraindicated
[see Contraindications].
If concomitant treatment of Cymbalta with a 5-hydroxytryptamine receptor agonist (triptan)
is clinically warranted, careful observation of the patient is advised, particularly during treatment
initiation and dose increases [see Drug Interactions].
The concomitant use of Cymbalta with serotonin precursors (such as tryptophan) is not
recommended [see Drug Interactions].
Abnormal Bleeding—SSRIs and SNRIs, including duloxetine, may increase the risk of bleeding
events. Concomitant use of aspirin, non-steroidal anti-inflammatory drugs, warfarin, and other
anti-coagulants may add to this risk. Case reports and epidemiological studies (case-control
and cohort design) have demonstrated an association between use of drugs that interfere with
Cymbalta� (duloxetine hydrochloride)
Cymbalta� (duloxetine hydrochloride)
(duloxetine hydrochloride) Delayed-release Capsules
Brief Summary: Consult the package insert for complete prescribing information.
WARNING: SUICIDALITY AND ANTIDEPRESSANT DRUGS
Antidepressants increased the risk compared to placebo of suicidal thinking and
behavior (suicidality) in children, adolescents, and young adults in short-term studies
of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering
the use of Cymbalta or any other antidepressant in a child, adolescent, or young adult must
balance this risk with the clinical need. Short-term studies did not show an increase
in the risk of suicidality with antidepressants compared to placebo in adults beyond
age 24; there was a reduction in risk with antidepressants compared to placebo in adults
aged 65 and older. Depression and certain other psychiatric disorders are themselves
associated with increases in the risk of suicide. Patients of all ages who are started on
antidepressant therapy should be monitored appropriately and observed closely for
clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers
should be advised of the need for close observation and communication with the
prescriber. Cymbalta is not approved for use in pediatric patients. [See Warnings and
Precautions and Use in Specific Populations.]
INDICATIONS AND USAGE: Major Depressive Disorder—Cymbalta is indicated for the acute
and maintenance treatment of major depressive disorder (MDD).
Generalized Anxiety Disorder—Cymbalta is indicated for the acute treatment of generalized
anxiety disorder (GAD).
Diabetic Peripheral Neuropathic Pain—Cymbalta is indicated for the management of
neuropathic pain (DPNP) associated with diabetic peripheral neuropathy.
Fibromyalgia—Cymbalta is indicated for the management of fibromyalgia (FM).
CONTRAINDICATIONS: Monoamine Oxidase Inhibitors—Concomitant use in patients taking
monoamine oxidase inhibitors (MAOIs) is contraindicated due to the risk of serious, sometimes
fatal, drug interactions with serotonergic drugs. These interactions may include hyperthermia,
rigidity, myoclonus, autonomic instability with possible rapid fluctuations of vital signs, and
mental status changes that include extreme agitation progressing to delirium and coma. These
reactions have also been reported in patients who have recently discontinued serotonin reuptake
inhibitors and are then started on an MAOI. Some cases presented with features resembling
neuroleptic malignant syndrome [see Warnings and Precautions].
Uncontrolled Narrow-Angle Glaucoma—In clinical trials, Cymbalta use was associated with
an increased risk of mydriasis; therefore, its use should be avoided in patients with uncontrolled
narrow-angle glaucoma [see Warnings and Precautions].
WARNINGS AND PRECAUTIONS: Clinical Worsening and Suicide Risk—Patients with major
depressive disorder (MDD), both adult and pediatric, may experience worsening of their
depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual
changes in behavior, whether or not they are taking antidepressant medications, and this risk may
persist until significant remission occurs. Suicide is a known risk of depression and certain
other psychiatric disorders, and these disorders themselves are the strongest predictors of
suicide. There has been a long-standing concern, however, that antidepressants may have
a role in inducing worsening of depression and the emergence of suicidality in certain patients
during the early phases of treatment.
Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and
others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality)
in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD)
and other psychiatric disorders. Short-term studies did not show an increase in the risk of
suicidality with antidepressants compared to placebo in adults beyond age 24; there was a
reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD,
obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of
24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses
of placebo-controlled trials in adults with MDD or other psychiatric disorders included a
total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over
77,000 patients. There was considerable variation in risk of suicidality among drugs, but a
tendency toward an increase in the younger patients for almost all drugs studied. There were
differences in absolute risk of suicidality across the different indications, with the highest
incidence in MDD. The risk of differences (drug vs placebo), however, were relatively stable
within age strata and across indications. These risk differences (drug-placebo difference in the
number of cases of suicidality per 1000 patients treated) are provided in Table 1.
Table 1
Age Range
PV 5909 AMP
PV 5909 AMP
serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to
SSRIs and SNRIs use have ranged from ecchymoses, hematomas, epistaxis, and petechiae
to life-threatening hemorrhages.
Patients should be cautioned about the risk of bleeding associated with the concomitant use
of duloxetine and NSAIDs, aspirin, or other drugs that affect coagulation.
Discontinuation of Treatment with Cymbalta—Discontinuation symptoms have been
systematically evaluated in patients taking duloxetine. Following abrupt or tapered discontinuation
in placebo-controlled clinical trials, the following symptoms occurred at a rate greater than or
equal to 1% and at a significantly higher rate in duloxetine-treated patients compared to those
discontinuing from placebo: dizziness, nausea, headache, fatigue, paresthesia, vomiting,
irritability, nightmares, insomnia, diarrhea, anxiety, hyperhidrosis and vertigo.
During marketing of other SSRIs and SNRIs (serotonin and norepinephrine reuptake inhibitors),
there have been spontaneous reports of adverse events occurring upon discontinuation of
these drugs, particularly when abrupt, including the following: dysphoric mood, irritability,
agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations),
anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and
seizures. Although these events are generally self-limiting, some have been reported to be severe.
Patients should be monitored for these symptoms when discontinuing treatment with
Cymbalta. A gradual reduction in the dose rather than abrupt cessation is recommended
whenever possible. If intolerable symptoms occur following a decrease in the dose or upon
discontinuation of treatment, then resuming the previously prescribed dose may be considered.
Subsequently, the physician may continue decreasing the dose but at a more gradual rate.
Activation of Mania/Hypomania—In placebo-controlled trials in patients with major depressive
disorder, activation of mania or hypomania was reported in 0.1% (2/2489) of duloxetine-treated
patients and 0.1% (1/1625) of placebo-treated patients. No activation of mania or hypomania
was reported in DPNP, GAD, or fibromyalgia placebo-controlled trials. Activation of mania or
hypomania has been reported in a small proportion of patients with mood disorders who were
treated with other marketed drugs effective in the treatment of major depressive disorder. As
with these other agents, Cymbalta should be used cautiously in patients with a history of mania.
Seizures—Duloxetine has not been systematically evaluated in patients with a seizure
disorder and such patients were excluded from clinical studies. In placebo-controlled clinical
trials, seizures/convulsions occurred in 0.03% (3/9445) of patients treated with duloxetine and
0.01% (1/6770) of patients treated with placebo. Cymbalta should be prescribed with care in
patients with a history of a seizure disorder.
Effect on Blood Pressure—In clinical trials across indications, relative to placebo, duloxetine
treatment was associated with mean increases of up to 2.1 mm Hg in systolic blood pressure
and up to 2.3 mm Hg in diastolic blood pressure. There was no significant difference in the
frequency of sustained (3 consecutive visits) elevated blood pressure. In a clinical pharmacology
study designed to evaluate the effects of duloxetine on various parameters, including blood
pressure at supratherapeutic doses with an accelerated dose titration, there was evidence of
increases in supine blood pressure at doses up to 200 mg twice daily. At the highest 200 mg
twice daily dose, the increase in mean pulse rate was 5.0 to 6.8 beats and increases in mean
blood pressure were 4.7 to 6.8 mm Hg (systolic) and 4.5 to 7 mm Hg (diastolic) up to 12 hours
after dosing.
Blood pressure should be measured prior to initiating treatment and periodically measured
throughout treatment [see Adverse Reactions, Vital Sign Changes].
Clinically Important Drug Interactions—Both CYP1A2 and CYP2D6 are responsible for
duloxetine metabolism.
Potential for Other Drugs to Affect Cymbalta—CYP1A2 Inhibitors—Co-administration of
Cymbalta with potent CYP1A2 inhibitors should be avoided [see Drug Interactions].
CYP2D6 Inhibitors—Because CYP2D6 is involved in duloxetine metabolism, concomitant
use of duloxetine with potent inhibitors of CYP2D6 would be expected to, and does, result in
higher concentrations (on average of 60%) of duloxetine [see Drug Interactions].
Potential for Cymbalta to Affect Other Drugs—Drugs Metabolized by CYP2D6—
Co-administration of Cymbalta with drugs that are extensively metabolized by CYP2D6 and that
have a narrow therapeutic index, including certain antidepressants (tricyclic antidepressants
[TCAs], such as nortriptyline, amitriptyline, and imipramine), phenothiazines and Type 1C
antiarrhythmics (e.g., propafenone, flecainide), should be approached with caution. Plasma
TCA concentrations may need to be monitored and the dose of the TCA may need to be reduced
if a TCA is co-administered with Cymbalta. Because of the risk of serious ventricular arrhythmias
and sudden death potentially associated with elevated plasma levels of thioridazine, Cymbalta
and thioridazine should not be co-administered [see Drug Interactions].
Other Clinically Important Drug Interactions—Alcohol—Use of Cymbalta concomitantly
with heavy alcohol intake may be associated with severe liver injury. For this reason, Cymbalta
should ordinarily not be prescribed for patients with substantial alcohol use [see Warnings and
Precautions and Drug Interactions].
CNS Acting Drugs—Given the primary CNS effects of Cymbalta, it should be used with caution
when it is taken in combination with or substituted for other centrally acting drugs, including
those with a similar mechanism of action [see Warnings and Precautions and Drug Interactions].
Hyponatremia—Hyponatremia may occur as a result of treatment with SSRIs and SNRIs,
including Cymbalta. In many cases, this hyponatremia appears to be the result of the syndrome
of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than
110 mmol/L have been reported and appeared to be reversible when Cymbalta was discontinued.
Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also,
patients taking diuretics or who are otherwise volume depleted may be at greater risk [see Use
in Specific Populations]. Discontinuation of Cymbalta should be considered in patients with
symptomatic hyponatremia and appropriate medical intervention should be instituted.
Use in Patients with Concomitant Illness—Clinical experience with Cymbalta in patients
with concomitant systemic illnesses is limited. There is no information on the effect that
alterations in gastric motility may have on the stability of Cymbalta’s enteric coating. In extremely
acidic conditions, Cymbalta, unprotected by the enteric coating, may undergo hydrolysis to
form naphthol. Caution is advised in using Cymbalta in patients with conditions that may slow
gastric emptying (e.g., some diabetics).
Cymbalta has not been systematically evaluated in patients with a recent history of myocardial
infarction or unstable coronary artery disease. Patients with these diagnoses were generally
excluded from clinical studies during the product’s premarketing testing.
Hepatic Insufficiency—Cymbalta should ordinarily not be used in patients with hepatic
insufficiency [see Warnings and Precautions and Use in Specific Populations].
Severe Renal Impairment—Cymbalta should ordinarily not be used in patients with end-stage
renal disease or severe renal impairment (creatinine clearance <30 mL/min). Increased plasma
concentration of duloxetine, and especially of its metabolites, occur in patients with end-stage
renal disease (requiring dialysis) [see Use in Specific Populations].
Controlled Narrow-Angle Glaucoma—In clinical trials, Cymbalta was associated with an
increased risk of mydriasis; therefore, it should be used cautiously in patients with controlled
narrow-angle glaucoma [see Contraindications].
Glycemic Control in Patients with Diabetes—As observed in DPNP trials, Cymbalta treatment
worsens glycemic control in some patients with diabetes. In three clinical trials of Cymbalta for
the management of neuropathic pain associated with diabetic peripheral neuropathy, the mean
duration of diabetes was approximately 12 years, the mean baseline fasting blood glucose was
176 mg/dL, and the mean baseline hemoglobin A1c (HbA1c) was 7.8%. In the 12-week acute
treatment phase of these studies, Cymbalta was associated with a small increase in mean fasting
blood glucose as compared to placebo. In the extension phase of these studies, which lasted
up to 52 weeks, mean fasting blood glucose increased by 12 mg/dL in the Cymbalta group and
decreased by 11.5 mg/dL in the routine care group. HbA1c increased by 0.5% in the Cymbalta
and by 0.2% in the routine care groups.
Urinary Hesitation and Retention—Cymbalta is in a class of drugs known to affect urethral
resistance. If symptoms of urinary hesitation develop during treatment with Cymbalta, consideration
should be given to the possibility that they might be drug-related. In post marketing experience,
cases of urinary retention have been observed. In some instances of urinary retention associated
with duloxetine use, hospitalization and/or catheterization has been needed.
Laboratory Tests—No specific laboratory tests are recommended.
ADVERSE REACTIONS: Clinical Trial Data Sources—The data described below reflect exposure
to duloxetine in placebo-controlled trials for MDD (N=2327), GAD (N=668), DPNP (N=568) and
FM (N=876). The population studied was 17 to 89 years of age; 64.8%, 64.7%, 38.7%, and
94.6% female; and 85.5%, 84.6%, 77.6%, and 88% Caucasian for MDD, GAD, DPNP, and FM,
respectively. Most patients received doses of a total of 60 to 120 mg per day.
The stated frequencies of adverse reactions represent the proportion of individuals who
experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction
was considered treatment-emergent if it occurred for the first time or worsened while receiving
therapy following baseline evaluation. Reactions reported during the studies were not necessarily
caused by the therapy, and the frequencies do not reflect investigator impression (assessment)
of causality.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates
observed in the clinical trials of a drug cannot be directly compared to rates in the clinical
trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions Reported as Reasons for Discontinuation of Treatment in PlaceboControlled Trials—Major Depressive Disorder—Approximately 9% (209/2327) of the patients
who received duloxetine in placebo-controlled trials for MDD discontinued treatment due to an
adverse reaction, compared with 4.7% (68/1460) of the patients receiving placebo. Nausea
(duloxetine 1.3%, placebo 0.5%) was the only common adverse reaction reported as a reason
for discontinuation and considered to be drug-related (i.e., discontinuation occurring in at least
1% of the duloxetine-treated patients and at a rate of at least twice that of placebo).
Generalized Anxiety Disorder—Approximately 15.3% (102/668) of the patients who
received duloxetine in placebo-controlled trials for GAD discontinued treatment due to an
adverse reaction, compared with 4.0% (20/495) for placebo. Common adverse reactions
reported as a reason for discontinuation and considered to be drug-related (as defined above)
included nausea (duloxetine 3.7%, placebo 0.2%), vomiting (duloxetine 1.3%, placebo 0.0%),
and dizziness (duloxetine 1.0%, placebo 0.2%).
Diabetic Peripheral Neuropathic Pain—Approximately 14.3% (81/568) of the patients who
received duloxetine in placebo-controlled trials for DPNP discontinued treatment due to an
adverse reaction, compared with 7.2% (16/223) for placebo. Common adverse reactions
reported as a reason for discontinuation and considered to be drug-related (as defined above)
were nausea (duloxetine 3.5%, placebo 0.4%), dizziness (duloxetine 1.6%, placebo 0.4%),
somnolence (duloxetine 1.6%, placebo 0.0%), and fatigue (duloxetine 1.1%, placebo 0.0%).
Fibromyalgia—Approximately 19.5% (171/876) of the patients who received duloxetine in
3 to 6 month placebo-controlled trials for FM discontinued treatment due to an adverse reaction,
compared with 11.8% (63/535) for placebo. Common adverse reactions reported as a reason
for discontinuation and considered to be drug-related (as defined above) included nausea
(duloxetine 1.9%, placebo 0.7%), somnolence (duloxetine 1.5%, placebo 0.0%), and fatigue
(duloxetine 1.3%, placebo 0.2%).
Adverse Reactions Occurring at an Incidence of 5% or More and at least Twice Placebo
Among Duloxetine-Treated Patients in Placebo-Controlled Trials—Pooled Trials for all
Approved Indications—The most commonly observed adverse reactions in Cymbalta-treated
patients (incidence of at least 5% and at least twice the incidence in placebo patients) were nausea,
dry mouth, constipation, somnolence, hyperhidrosis, and decreased appetite.
In addition to the adverse reactions listed above, DPNP trials also included dizziness and
asthenia.
Adverse Reactions Occurring at an Incidence of 5% or More Among Duloxetine- Treated
Patients in Placebo-Controlled Trials—The incidence of treatment-emergent adverse reactions
in placebo-controlled trials (N=4843 Cymbalta; N=3048 placebo) for approved indications that
occurred in 5% or more of patients treated with duloxetine and with an incidence greater than
placebo were: nausea, headache, dry mouth, fatigue (includes asthenia), insomnia∗ (includes
middle insomnia, early morning awakening, and initial insomnia), dizziness, somnolence∗
(includes hypersomnia and sedation), constipation∗, diarrhea, decreased appetite∗ (includes
anorexia), and hyperhidrosis. ∗Events for which there was a significant dose-dependent
relationship in fixed-dose studies, excluding three MDD studies which did not have a placebo
lead-in period or dose titration.
Adverse Reactions Occurring at an Incidence of 2% or More Among Duloxetine- Treated
Patients in Placebo-Controlled Trials—Pooled MDD and GAD Trials—Table 3 in full PI gives
the incidence of treatment-emergent adverse reactions in MDD and GAD placebo-controlled trials
(N=2995 Cymbalta; N=1955 placebo) for approved indications that occurred in 2% or more of
Cymbalta� (duloxetine hydrochloride)
Cymbalta� (duloxetine hydrochloride)
PV 5909 AMP
PV 5909 AMP
patients treated with duloxetine and with an incidence greater than placebo were: Cardiac
Disorders—palpitations; Eye Disorders—vision blurred; Gastrointestinal Disorders—nausea,
dry mouth, diarrhea, constipation∗, abdominal pain (includes abdominal pain upper, abdominal
pain lower, abdominal tenderness, abdominal discomfort, and gastrointestinal pain), vomiting;
General Disorders and Administration Site Conditions—fatigue (includes asthenia);
Investigations—weight decreased∗; Metabolism and Nutrition Disorders—decreased appetite
(includes anorexia); Nervous System Disorders—dizziness, somnolence (includes hypersomnia
and sedation), tremor; Psychiatric Disorders—insomnia (includes middle insomnia, early
morning awakening, and initial insomnia), agitation (includes feeling jittery, nervousness,
restlessness, tension, and psychomotor agitation), anxiety, decreased libido (includes loss of
libido), orgasm abnormal (includes anorgasmia), abnormal dreams (includes nightmare);
Reproductive System and Breast Disorders—erectile dysfunction, ejaculation delayed, ejaculation
disorder (includes ejaculation failure and ejaculation dysfunction); Respiratory, Thoracic, and
Mediastinal Disorders—yawning; Skin and Subcutaneous Tissue Disorders—hyperhidrosis;
Vascular Disorders—hot flush. ∗Events for which there was a significant dose-dependent
relationship in fixed-dose studies, excluding three MDD studies which did not have a placebo
lead-in period or dose titration.
Diabetic Peripheral Neuropathic Pain—Treatment-emergent adverse events that occurred in
2% or more of patients treated with Cymbalta in the premarketing acute phase of DPNP placebocontrolled trials (N=115 Cymbalta 20 mg once daily; N=228 Cymbalta 60 mg once daily; N=225
Cymbalta 60 mg twice daily; N=223 placebo) with an incidence greater than placebo
were: Gastrointestinal Disorders—nausea, constipation, diarrhea, dry mouth, vomiting, dyspepsia,
loose stools; General Disorders and Administration Site Conditions—fatigue, asthenia, pyrexia;
Infections and Infestations—nasopharyngitis; Metabolism and Nutrition Disorders—
decreased appetite, anorexia; Musculoskeletal and Connective Tissue Disorders—muscle
cramp, myalgia; Nervous System Disorders—somnolence, headache, dizziness, tremor; Psychiatric
Disorders—insomnia; Renal and Urinary Disorders—pollakiuria; Reproductive System and
Breast Disorders—erectile dysfunction; Respiratory, Thoracic and Mediastinal Disorders—
cough, pharyngolaryngeal pain; Skin and Subcutaneous Tissue Disorders—hyperhidrosis.
Fibromyalgia—Treatment-emergent adverse events that occurred in 2% or more of patients
treated with Cymbalta in the premarketing acute phase of FM placebo-controlled trials (N=876
Cymbalta; N=535 placebo) and with an incidence greater than placebo were: Cardiac Disorders—
palpitations; Eye Disorders—vision blurred; Gastrointestinal Disorders—nausea, dry mouth,
constipation, diarrhea, dyspepsia; General Disorders and Administration Site Conditions—
fatigue (includes asthenia); Immune System Disorders—seasonal allergy; Infections and
Infestations—upper respiratory tract infection, urinary tract infection, influenza, gastroenteritis
viral; Investigations—weight increased; Metabolism and Nutrition Disorders—decreased appetite
(includes anorexia); Musculoskeletal and Connective Tissue Disorders—musculoskeletal pain,
muscle spasm; Nervous System Disorders—headache, dizziness, somnolence (includes
hypersomnia and sedation), tremor, paraesthesia, migraine, dysgeusia; Psychiatric Disorders—
insomnia (includes middle insomnia, early morning awakening, and initial insomnia), agitation
(includes feeling jittery, nervousness, restlessness, tension, and psychomotor agitation), sleep
disorder, abnormal dreams (includes nightmare), orgasm abnormal (includes anorgasmia),
libido decreased (includes loss of libido); Reproductive System and Breast Disorders—ejaculation
disorder (includes ejaculation failure and ejaculation dysfunction), penis disorder; Respiratory,
Thoracic, and Mediastinal Disorders—cough, pharyngolaryngeal pain; Skin and Subcutaneous
Tissue Disorders—hyperhidrosis, rash, pruritus; Vascular Disorders—hot flush.
Effects on Male and Female Sexual Function—Changes in sexual desire, sexual performance
and sexual satisfaction often occur as manifestations of psychiatric disorders or diabetes, but
they may also be a consequence of pharmacologic treatment. Because adverse sexual reactions
are presumed to be voluntarily underreported, the Arizona Sexual Experience Scale (ASEX), a
validated measure designed to identify sexual side effects, was used prospectively in 4 MDD
placebo-controlled trials. In these trials, patients treated with Cymbalta experienced significantly
more sexual dysfunction, as measured by the total score on the ASEX, than did patients treated
with placebo. Gender analysis showed that this difference occurred only in males. Males treated
with Cymbalta experienced more difficulty with ability to reach orgasm (ASEX Item 4) than
males treated with placebo. Females did not experience more sexual dysfunction on Cymbalta
than on placebo as measured by ASEX total score. Physicians should routinely inquire about
possible sexual side effects. See Table 6 in full PI for specific ASEX results.
Vital Sign Changes—In clinical trials across indications, relative to placebo, duloxetine
treatment was associated with mean increases of up to 2.1 mm Hg in systolic blood pressure
and up to 2.3 mm Hg in diastolic blood pressure. There was no significant difference in the
frequency of sustained (3 consecutive visits) elevated blood pressure [see Warnings and
Precautions]. Duloxetine treatment, for up to 26-weeks in placebo-controlled trials typically
caused a small increase in heart rate compared to placebo of up to 3-4 beats per minute.
Weight Changes—In placebo-controlled clinical trials, MDD and GAD patients treated with
Cymbalta for up to 10 weeks experienced a mean weight loss of approximately 0.5 kg, compared
with a mean weight gain of approximately 0.2 kg in placebo-treated patients. In DPN placebocontrolled clinical trials, patients treated with Cymbalta for up to 13-weeks experienced a mean
weight loss of approximately 1.1 kg, compared with a mean weight gain of approximately 0.2 kg
in placebo-treated patients. In fibromyalgia studies, patients treated with Cymbalta for up to
26 weeks experienced a mean weight loss of approximately 0.4 kg compared with a mean
weight gain of approximately 0.3 kg in placebo-treated patients. In one long-term fibromyalgia
60-week uncontrolled study, duloxetine patients had a mean weight increase of 0.7 kg.
Laboratory Changes—Cymbalta treatment in placebo-controlled clinical trials, was associated
with small mean increases from baseline to endpoint in ALT, AST, CPK, and alkaline phosphatase;
infrequent, modest, transient, abnormal values were observed for these analytes in Cymbaltatreated patients when compared with placebo-treated patients [see Warnings and Precautions].
Electrocardiogram Changes—Electrocardiograms were obtained from duloxetine-treated
patients and placebo-treated patients in clinical trials lasting up to 13-weeks. No clinically significant
differences were observed for QTc, QT, PR, and QRS intervals between duloxetine-treated and
placebo-treated patients. There were no differences in clinically meaningful QTcF elevations
between duloxetine and placebo. In a positive-controlled study in healthy volunteers using
duloxetine up to 200 mg twice daily, no prolongation of the corrected QT interval was observed.
Other Adverse Reactions Observed During the Premarketing and Postmarketing Clinical
Trial Evaluation of Duloxetine—Following is a list of treatment-emergent adverse reactions
reported by patients treated with duloxetine in clinical trials. In clinical trials of all indications,
27,229 patients were treated with duloxetine. Of these, 29% (7,886) took duloxetine for at least
6 months, and 13.3% (3,614) for at least one year. The following listing is not intended to
include reactions (1) already listed in previous tables or elsewhere in labeling, (2) for which a
drug cause was remote, (3) which were so general as to be uninformative, (4) which were not
considered to have significant clinical implications, or (5) which occurred at a rate equal to or
less than placebo.
Reactions are categorized by body system according to the following definitions: frequent
adverse reactions are those occurring in at least 1/100 patients; infrequent adverse reactions
are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer
than 1/1000 patients. Cardiac Disorders—Frequent: palpitations; Infrequent: myocardial infarction and tachycardia; Ear and Labyrinth Disorders—Frequent: vertigo; Infrequent: ear pain and
tinnitus; Endocrine Disorders—Infrequent: hypothyroidism; Eye Disorders—Frequent: vision
blurred; Infrequent: diplopia and visual disturbance; Gastrointestinal Disorders—Frequent: flatulence; Infrequent: eructation, gastritis, halitosis, and stomatitis; Rare: gastric ulcer, hematochezia, and melena; General Disorders and Administration Site Conditions—Frequent:
chills/rigors; Infrequent: feeling abnormal, feeling hot and/or cold, malaise, and thirst; Rare:
gait disturbance; Infections and Infestations—Infrequent: gastroenteritis and laryngitis;
Investigations—Frequent: weight increased; Infrequent: blood cholesterol increased;
Metabolism and Nutrition Disorders—Infrequent: dehydration and hyperlipidemia; Rare:
dyslipidemia; Musculoskeletal and Connective Tissue Disorders—Frequent: musculoskeletal
pain; Infrequent: muscle tightness and muscle twitching; Nervous System Disorders—
Frequent: dysgeusia, lethargy, and parasthesia/hypoesthesia; Infrequent: disturbance in attention,
dyskinesia, myoclonus, and poor quality sleep; Rare: dysarthria; Psychiatric Disorders—
Frequent: abnormal dreams and sleep disorder; Infrequent: apathy, bruxism, disorientation/
confusional state, irritability, mood swings, and suicide attempt; Rare: completed suicide; Renal
and Urinary Disorders—Infrequent: dysuria, micturition urgency, nocturia, polyuria, and urine
odor abnormal.; Reproductive System and Breast Disorders—Frequent: anorgasmia/orgasm
abnormal; Infrequent: menopausal symptoms, and sexual dysfunction; Respiratory, Thoracic
and Mediastinal Disorders—Frequent: yawning; Infrequent: throat tightness; Skin and
Subcutaneous Tissue Disorders—Infrequent: cold sweat, dermatitis contact, erythema,
increased tendency to bruise, night sweats, and photosensitivity reaction; Rare: ecchymosis;
Vascular Disorders—Frequent: hot flush; Infrequent: flushing, orthostatic hypotension, and
peripheral coldness.
Postmarketing Spontaneous Reports—The following adverse reactions have been identified
during postapproval use of Cymbalta. Because these reactions are reported voluntarily from a
population of uncertain size, it is not always possible to reliably estimate their frequency or
establish a causal relationship to drug exposure.
Adverse reactions reported since market introduction that were temporally related to duloxetine
therapy and not mentioned elsewhere in labeling include: anaphylactic reaction, aggression and
anger (particularly early in treatment or after treatment discontinuation), angioneurotic edema,
erythema multiforme, extrapyramidal disorder, glaucoma, gynecological bleeding, hallucinations,
hyperglycemia, hypersensitivity, hypertensive crisis, muscle spasm, rash, supraventricular
arrhythmia, tinnitus (upon treatment discontinuation), trismus, and urticaria.
Serious skin reactions including Stevens-Johnson Syndrome that have required drug
discontinuation and/or hospitalization have been reported with duloxetine.
DRUG INTERACTIONS: Both CYP1A2 and CYP2D6 are responsible for duloxetine metabolism.
Inhibitors of CYP1A2—When duloxetine 60 mg was co-administered with fluvoxamine 100 mg,
a potent CYP1A2 inhibitor, to male subjects (n=14) duloxetine AUC was increased approximately
6-fold, the Cmax was increased about 2.5-fold, and duloxetine t1/2 was increased approximately
3-fold. Other drugs that inhibit CYP1A2 metabolism include cimetidine and quinolone antimicrobials
such as ciprofloxacin and enoxacin [see Warnings and Precautions].
Inhibitors of CYP2D6—Concomitant use of duloxetine (40 mg once daily) with paroxetine
(20 mg once daily) increased the concentration of duloxetine AUC by about 60%, and greater
degrees of inhibition are expected with higher doses of paroxetine. Similar effects would be
expected with other potent CYP2D6 inhibitors (e.g., fluoxetine, quinidine) [see Warnings and
Precautions].
Dual Inhibition of CYP1A2 and CYP2D6—Concomitant administration of duloxetine 40 mg
twice daily with fluvoxamine 100 mg, a potent CYP1A2 inhibitor, to CYP2D6 poor metabolizer
subjects (n=14) resulted in a 6-fold increase in duloxetine AUC and Cmax.
Drugs that Interfere with Hemostasis (e.g., NSAIDs, Aspirin, and Warfarin)—Serotonin
release by platelets plays an important role in hemostasis. Epidemiological studies of the casecontrol and cohort design that have demonstrated an association between use of psychotropic
drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding
have also shown that concurrent use of an NSAID or aspirin may potentiate this risk of bleeding.
Altered anticoagulant effects, including increased bleeding, have been reported when SSRIs or
SNRIs are coadministered with warfarin. Patients receiving warfarin therapy should be carefully
monitored when duloxetine is initiated or discontinued [see Warnings and Precautions].
Lorazepam—Under steady-state conditions for duloxetine (60 mg Q 12 hours) and
lorazepam (2 mg Q 12 hours), the pharmacokinetics of duloxetine were not affected by
co-administration.
Temazepam—Under steady-state conditions for duloxetine (20 mg qhs) and temazepam
(30 mg qhs), the pharmacokinetics of duloxetine were not affected by co-administration.
Drugs that Affect Gastric Acidity—Cymbalta has an enteric coating that resists dissolution
until reaching a segment of the gastrointestinal tract where the pH exceeds 5.5. In extremely
acidic conditions, Cymbalta, unprotected by the enteric coating, may undergo hydrolysis to
form naphthol. Caution is advised in using Cymbalta in patients with conditions that may slow
gastric emptying (e.g., some diabetics). Drugs that raise the gastrointestinal pH may lead to an
earlier release of duloxetine. However, co-administration of Cymbalta with aluminum- and
magnesium-containing antacids (51 mEq) or Cymbalta with famotidine, had no significant
effect on the rate or extent of duloxetine absorption after administration of a 40 mg oral dose.
It is unknown whether the concomitant administration of proton pump inhibitors affects duloxetine
absorption [see Warnings and Precautions].
Cymbalta� (duloxetine hydrochloride)
Cymbalta� (duloxetine hydrochloride)
PV 5909 AMP
PV 5909 AMP
Drugs Metabolized by CYP1A2—In vitro drug interaction studies demonstrate that duloxetine
does not induce CYP1A2 activity. Therefore, an increase in the metabolism of CYP1A2 substrates
(e.g., theophylline, caffeine) resulting from induction is not anticipated, although clinical studies
of induction have not been performed. Duloxetine is an inhibitor of the CYP1A2 isoform in
in vitro studies, and in two clinical studies the average (90% confidence interval) increase
in theophylline AUC was 7% (1%-15%) and 20% (13%-27%) when co-administered with
duloxetine (60 mg twice daily).
Drugs Metabolized by CYP2D6—Duloxetine is a moderate inhibitor of CYP2D6. When
duloxetine was administered (at a dose of 60 mg twice daily) in conjunction with a single 50-mg
dose of desipramine, a CYP2D6 substrate, the AUC of desipramine increased 3-fold [see
Warnings and Precautions].
Drugs Metabolized by CYP2C9—Duloxetine does not inhibit the in vitro enzyme activity of
CYP2C9. Inhibition of the metabolism of CYP2C9 substrates is therefore not anticipated,
although clinical studies have not been performed.
Drugs Metabolized by CYP3A—Results of in vitro studies demonstrate that duloxetine does
not inhibit or induce CYP3A activity. Therefore, an increase or decrease in the metabolism of
CYP3A substrates (e.g., oral contraceptives and other steroidal agents) resulting from induction
or inhibition is not anticipated, although clinical studies have not been performed.
Drugs Metabolized by CYP2C19—Results of in vitro studies demonstrate that duloxetine
does not inhibit CYP2C19 activity at therapeutic concentrations. Inhibition of the metabolism of
CYP2C19 substrates is therefore not anticipated, although clinical studies have not been performed.
Monoamine Oxidase Inhibitors—Switching Patients to or from a Monoamine Oxidase
Inhibitor—At least 14 days should elapse between discontinuation of an MAOI and initiation of
therapy with Cymbalta. In addition, at least 5 days should be allowed after stopping Cymbalta
before starting an MAOI [see Contraindications and Warnings and Precautions].
Serotonergic Drugs—Based on the mechanism of action of SNRIs and SSRIs, including
Cymbalta, and the potential for serotonin syndrome, caution is advised when Cymbalta is
co-administered with other drugs that may affect the serotonergic neurotransmitter systems,
such as triptans, linezolid (an antibiotic which is a reversible non-selective MAOI), lithium, tramadol,
or St. John's Wort. The concomitant use of Cymbalta with other SSRIs, SNRIs or tryptophan
is not recommended [see Warnings and Precautions].
Triptans—There have been rare postmarketing reports of serotonin syndrome with use of
an SSRI and a triptan. If concomitant treatment of Cymbalta with a triptan is clinically warranted,
careful observation of the patient is advised, particularly during treatment initiation and dose
increases [see Warnings and Precautions].
Alcohol—When Cymbalta and ethanol were administered several hours apart so that peak
concentrations of each would coincide, Cymbalta did not increase the impairment of mental
and motor skills caused by alcohol.
In the Cymbalta clinical trials database, three Cymbalta-treated patients had liver injury as
manifested by ALT and total bilirubin elevations, with evidence of obstruction. Substantial
intercurrent ethanol use was present in each of these cases, and this may have contributed to
the abnormalities seen [see Warnings and Precautions].
CNS Drugs—[see Warnings and Precautions].
Drugs Highly Bound to Plasma Protein—Because duloxetine is highly bound to plasma
protein, administration of Cymbalta to a patient taking another drug that is highly protein
bound may cause increased free concentrations of the other drug, potentially resulting in
adverse reactions.
USE IN SPECIFIC POPULATIONS: Pregnancy—Teratogenic Effects, Pregnancy Category C—
In animal reproduction studies, duloxetine has been shown to have adverse effects on embryo/
fetal and postnatal development.
When duloxetine was administered orally to pregnant rats and rabbits during the period of
organogenesis, there was no evidence of teratogenicity at doses up to 45 mg/kg/day (7 times
the maximum recommended human dose [MRHD, 60 mg/day] and 4 times the human dose of
120 mg/day on a mg/m2 basis, in rat; 15 times the MRHD and 7 times the human dose of 120 mg/day
on a mg/m2 basis in rabbit). However, fetal weights were decreased at this dose, with a
no-effect dose of 10 mg/kg/day (2 times the MRHD and ≈1 times the human dose of
120 mg/day on a mg/m2 basis in rat; 3 times the MRHD and 2 times the human dose of 120 mg/day
on a mg/m2 basis in rabbits).
When duloxetine was administered orally to pregnant rats throughout gestation and lactation,
the survival of pups to 1 day postpartum and pup body weights at birth and during the
lactation period were decreased at a dose of 30 mg/kg/day (5 times the MRHD and 2 times
the human dose of 120 mg/day on a mg/m2 basis); the no-effect dose was 10 mg/kg/day.
Furthermore, behaviors consistent with increased reactivity, such as increased startle response
to noise and decreased habituation of locomotor activity, were observed in pups following
maternal exposure to 30 mg/kg/day. Post-weaning growth and reproductive performance of
the progeny were not affected adversely by maternal duloxetine treatment.
There are no adequate and well-controlled studies in pregnant women; therefore, duloxetine
should be used during pregnancy only if the potential benefit justifies the potential risk to
the fetus.
Nonteratogenic Effects—Neonates exposed to SSRIs or serotonin and norepinephrine reuptake
inhibitors (SNRIs), late in the third trimester have developed complications requiring prolonged
hospitalization, respiratory support, and tube feeding. Such complications can arise immediately
upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea,
seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia,
hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are
consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation
syndrome. It should be noted that, in some cases, the clinical picture is consistent with
serotonin syndrome [see Warnings and Precautions].
When treating pregnant women with Cymbalta during the third trimester, the physician
should carefully consider the potential risks and benefits of treatment. The physician may
consider tapering Cymbalta in the third trimester.
Labor and Delivery—The effect of duloxetine on labor and delivery in humans is unknown.
Duloxetine should be used during labor and delivery only if the potential benefit justifies the
potential risk to the fetus.
Nursing Mothers—Duloxetine is excreted into the milk of lactating women. The estimated
daily infant dose on a mg/kg basis is approximately 0.14% of the maternal dose. Because the
safety of duloxetine in infants is not known, nursing while on Cymbalta is not recommended.
However, if the physician determines that the benefit of duloxetine therapy for the mother
outweighs any potential risk to the infant, no dosage adjustment is required as lactation did
not influence duloxetine pharmacokinetics.
Pediatric Use—Safety and effectiveness in the pediatric population have not been established
[see Boxed Warning and Warnings and Precautions]. Anyone considering the use of Cymbalta
in a child or adolescent must balance the potential risks with the clinical need.
Geriatric Use—Of the 2,418 patients in premarketing clinical studies of Cymbalta for MDD,
5.9% (143) were 65 years of age or over. Of the 1,074 patients in the DPNP premarketing studies,
33% (357) were 65 years of age or over. Of the 1,761 patients in FM premarketing
studies, 7.9% (140) were 65 years of age or over. Premarketing clinical studies of GAD did not
include sufficient numbers of subjects age 65 or over to determine whether they respond
differently from younger subjects. In the MDD and DPNP studies, no overall differences in safety
or effectiveness were observed between these subjects and younger subjects, and other reported
clinical experience has not identified differences in responses between the elderly and younger
patients, but greater sensitivity of some older individuals cannot be ruled out. SSRIs
and SNRIs, including Cymbalta have been associated with cases of clinically significant
hyponatremia in elderly patients, who may be at greater risk for this adverse event [see
Warnings and Precautions].
Gender—The half-life of duloxetine is similar in men and women. Dosage adjustment based
on gender is not necessary.
Smoking Status—Duloxetine bioavailability (AUC) appears to be reduced by about one-third
in smokers. Dosage modifications are not recommended for smokers.
Race—No specific pharmacokinetic study was conducted to investigate the effects of race.
Hepatic Insufficiency—[see Warnings and Precautions].
Severe Renal Impairment—[see Warnings and Precautions].
DRUG ABUSE AND DEPENDENCE: Abuse—In animal studies, duloxetine did not demonstrate
barbiturate-like (depressant) abuse potential. While Cymbalta has not been systematically studied
in humans for its potential for abuse, there was no indication of drug-seeking behavior in the
clinical trials. However, it is not possible to predict on the basis of premarketing experience
the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed.
Consequently, physicians should carefully evaluate patients for a history of drug abuse and
follow such patients closely, observing them for signs of misuse or abuse of Cymbalta (e.g.,
development of tolerance, incrementation of dose, drug-seeking behavior).
Dependence—In drug dependence studies, duloxetine did not demonstrate dependence
producing potential in rats.
OVERDOSAGE: Signs and Symptoms—In postmarketing experience, fatal outcomes have
been reported for acute overdoses, primarily with mixed overdoses, but also with duloxetine
only, at doses as low as 1000 mg. Signs and symptoms of overdose (duloxetine alone or with
mixed drugs) included somnolence, coma, serotonin syndrome, seizures, syncope, tachycardia,
hypotension, hypertension, and vomiting.
Management of Overdose—There is no specific antidote to Cymbalta, but if serotonin
syndrome ensues, specific treatment (such as with cyproheptadine and/or temperature
control) may be considered. In case of acute overdose, treatment should consist of those general
measures employed in the management of overdose with any drug.
NONCLINICAL TOXICOLOGY: Carcinogenesis, Mutagenesis, and Impairment of Fertility—
Carcinogenesis—Duloxetine was administered in the diet to mice and rats for 2 years.
In female mice receiving duloxetine at 140 mg/kg/day (11 times the maximum recommended
human dose [MRHD, 60 mg/day] and 6 times the human dose of 120 mg/day on a mg/m2
basis), there was an increased incidence of hepatocellular adenomas and carcinomas. The
no-effect dose was 50 mg/kg/day (4 times the MRHD and 2 times the human dose of 120 mg/day
on a mg/m2 basis). Tumor incidence was not increased in male mice receiving duloxetine at
doses up to 100 mg/kg/day (8 times the MRHD and 4 times the human dose of 120 mg/day
on a mg/m2 basis).
In rats, dietary doses of duloxetine up to 27 mg/kg/day in females (4 times the MRHD and
2 times the human dose of 120 mg/day on a mg/m2 basis) and up to 36 mg/kg/day in males
(6 times the MRHD and 3 times the human dose of 120 mg/day on a mg/m2 basis) did not
increase the incidence of tumors.
Mutagenesis—Duloxetine was not mutagenic in the in vitro bacterial reverse mutation assay
(Ames test) and was not clastogenic in an in vivo chromosomal aberration test in mouse bone
marrow cells. Additionally, duloxetine was not genotoxic in an in vitro mammalian forward gene
mutation assay in mouse lymphoma cells or in an in vitro unscheduled DNA synthesis (UDS)
assay in primary rat hepatocytes, and did not induce sister chromatid exchange in Chinese
hamster bone marrow in vivo.
Impairment of Fertility—Duloxetine administered orally to either male or female rats prior to
and throughout mating at doses up to 45 mg/kg/day (7 times the maximum recommended
human dose of 60 mg/day and 4 times the human dose of 120 mg/day on a mg/m2 basis) did
not alter mating or fertility.
PATIENT COUNSELING INFORMATION: See FDA-approved Medication Guide and Patient
Counseling Information section of full PI.
Literature revised August, 11, 2008
PV 5909 AMP
PRINTED IN USA
Cymbalta� (duloxetine hydrochloride)
Cymbalta� (duloxetine hydrochloride)
PV 5909 AMP
Eli Lilly and Company
Indianapolis, IN 46285, USA
www.Cymbalta.com
Copyright © 2008, Eli Lilly and Company. All rights reserved.
PV 5909 AMP
Presenting effective
pain relief for your patients
with fibromyalgia.
Cymbalta is approved for the
management of fibromyalgia.
Important Safety Information
• Antidepressants increased the risk of suicidal thinking
and behavior (suicidality) in short-term studies in
children, adolescents, and young adults with major
depressive disorder (MDD) and other psychiatric disorders.
• Patients of all ages started on therapy should be
monitored appropriately and observed closely for
clinical worsening, suicidality, or unusual changes
in behavior.
• Cymbalta is not approved for use in pediatric patients.
Cymbalta should not be used concomitantly with monoamine oxidase inhibitors
(MAOIs) or in patients with uncontrolled narrow-angle glaucoma.
Clinical worsening and suicide risk: All patients being treated with an
antidepressant for any indication should be monitored appropriately and
observed closely for clinical worsening, suicidality, and unusual changes
in behavior, especially within the first few months of treatment and when
changing the dose. Consider changing the therapeutic regimen if the depression
is persistently worse or there are symptoms that are severe, sudden, or were not
part of the patient’s presentation. If discontinuing treatment, taper the medication.
Families and caregivers of patients being treated with antidepressants for any
indication should be alerted about the need to monitor patients.
Hepatic failure, sometimes fatal, has been reported in patients treated with
Cymbalta. Cymbalta should be discontinued in patients who develop jaundice
or other evidence of clinically significant liver dysfunction and should not be
resumed unless anotherr cause can be established.
Cymbalta should ordinarily not be prescribed to patients with substantial
alcohol use or evidence of chronic liver disease.
Cases of orthostatic hypotension and/or syncope as well as cases of hyponatremia
have been reported.
Development of a potentially life-threatening serotonin syndrome may
occur with SNRIs and SSRIs, including Cymbalta treatment, particularly
with concomitant use of serotonergic drugs, including triptans. Concomitant
use is not recommended.
SSRIs and SNRIs, including Cymbalta, may increase the risk of bleeding
events. Patients should be cautioned about the risk of bleeding associated with
concomitant use of Cymbalta and NSAIDs, aspirin, warfarin, or other drugs that
affect coagulation.
On discontinuation, adverse events, some of which may be serious, have been
reported with SSRIs and SNRIs. A gradual reduction in dose rather than abrupt
cessation is recommended when possible.
Co-administration of Cymbalta with potent CYP1A2 inhibitors or thioridazine
should be avoided.
Caution is advised in using Cymbalta in patients with conditions that may
slow gastric emptying (eg, some diabetics).
Cymbalta should ordinarily not be administered to patients with any hepatic
insufficiency or patients with end-stage renal disease (requiring dialysis) or severe
renal impairment (CrCl <30 mL/min).
As observed in DPNP clinical trials, Cymbalta treatment worsens glycemic
control in some patients with diabetes. In the extension phases up to 52 weeks,
an increase in HbA1c in both the Cymbalta (0.5%) and routine care groups (0.2%)
was noted.
If symptoms of urinary hesitation develop during Cymbalta treatment, this
effect may be drug-related. In postmarketing experience, urinary retention
has been observed.
The most commonly reported adverse events (≥5% and at least twice placebo)
for Cymbalta vs placebo in controlled clinical trials (N=4843 vs 3048) were:
nausea, dry mouth, somnolence,* constipation,* decreased appetite,* and
increased sweating.
* Events for which there was a significant dose-dependent relationship in
fixed-dose studies, excluding three MDD studies which did not have
a placebo lead-in period or dose titration.
See Brief Summary of full Prescribing Information,
including Boxed Warning, on following pages.
DD54733 1108 PRINTED IN USA © 2008, ELI LILLY AND COMPANY.
ALL RIGHTS RESERVED. Cymbalta is a registered trademark of Eli Lilly and Company.
www.insidecymbalta.com
© Copyright 2025