Neonatal Society Spring Meeting 19th March 2015 Institute of Child
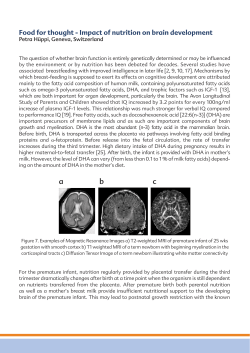
Neonatal Society Spring Meeting 19th March 2015 Institute of Child Health, London Spring Meeting, 19th March 2015 Institute of Child Health, London 30 Guilford Street, London WC1N 1EH 09.15 Coffee Session1: Chair – Dr James Boardman, Meetings Secretary 09.45 K Turner, University of Kent Is preterm birth associated with accelerated telomere shortening? 10.00 R Kumar, Birmingham Women’s NHS Foundation Trust Hospital Improving trends in the outcome of live inborn babies with congenital diaphragmatic hernia following development of a centralised management protocol 10.15 P Seddon, Royal Alexandra Children’s Hospital, Brighton Respiratory monitoring by pulse oximetry plethysmogram analysis in preterm infants 10.30 P Shangaris, University College London Correction of hemoglobin levels in a heterozygous humanized mouse model of thalassemia after fetal gene therapy 10.45 N Aladangardy, Homerton University Hospital Withdrawal of life sustaining treatment for newborn infants: the WiLST study 11.00 Tea / coffee Session 2: Chair – Professor Howard Clark, President Elect 11.30 M Ezzati, University College London Limb remote ischemic post-conditioning protects cerebral white matter in a piglet model of perinatal asphyxia 11.45 R Lee-Kelland, University of Bristol Excessive hypothermia during and temperature instability after completion of therapeutic hypothermia are associated with a poorer neurodevelopmental outcome 12.00 Keynote Lecture: Minimally invasive surfactant delivery in the preterm infant Professor Peter Dargaville, University of Tasmania 13.00 Lunch break Session 3: Chair – Dr David Carr, Committee member 14.00 A Walker, Birmingham Women’s NHS Foundation Trust Outcome of antenatally detected encephalocele; tertiary centre experience over a 10 year period 14.15 B Ibrahim, Imperial College London One-year mortality of very preterm infants admitted to neonatal units in England 14.30 E Moore, University of Edinburgh Preterm birth is associated with atypical social cognition in infancy 14.45 S Mulla, Norfolk and Norwich University Hospitals NHS Foundation Trust Severe biochemical disturbances after introduction of a new regional parenteral nutrition formulation matching current ESPGHAN recommendations 15.00 N Przysiezna, Imperial College London Postnatal age related metabolic changes in faecal water from premature babies 15.15 S Sparrow, University of Edinburgh Preterm birth is associated with alterations in the methylome at sites that influence neural development 15.30 Afternoon Tea / Coffee Session 3: Chair – Dr Richard Thwaites, General Secretary 16.00 J Whistler, University of Nottingham The impact of route of delivery on skeletal muscle metabolism in piglets 16.15 N Andreas, Imperial College London The association between breast milk macronutrient content and maternal BMI 16.30 I Mawson, Guy’s and St Thomas’ NHS Foundation Trust Does the sensitivity of pulse oximetry screening depend on the type of critical congenital heart disease? An adjunct to the pulse oximetry screening debate 16.45 The McCance Lecture: Why preclinical trials fail to translate Professor Malcolm Macleod, University of Edinburgh Introduced by Professor Neena Modi, President of the Neonatal Society 17.45 Drinks and Close of Meeting Title (Upper case) IS PRETERM BIRTH ASSOCIATED WITH ACCELERATED TELOMERE SHORTENING? Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 2 2 1 Kara Turner , Shermi George , John Greenall , Darren Griffin and Vimal Vasu Corresponding author e-mail address: 1,2 K.J.Turner-24@kent.ac.uk Institution(s) 1. School of Biosciences, University of Kent 2. Department of Neonatal Medicine, William Harvey Hospital, Ashford, Kent, TN24 0LZ Introduction (include hypothesis) By term age preterm infants manifest an ‘aged’ phenotype characterised by altered body fat distribution, insulin resistance and hypertension. Telomeres are nucleoprotein structures at the end of human chromosomes that shorten with age and in association with the above morbidities. The aim of this study was to determine telomere length in a cohort of preterm infants at term equivalent age and in comparison to a cohort of term born infants. Our a priori hypothesis was that preterm at term infants would have shorter telomeres than term born controls. ohypothesisthat telomere length is reduced in preterm infants by term equivalent age. Methods (include source of funding and ethical approval if required) With institutional research ethics approval and informed parental consent, blood samples were drawn from preterm infants (<32 weeks completed gestation) within 48 hours after birth (n=18) and at term equivalent age (n=18) alongside routine sampling. Blood samples were also drawn from term born controls (≥37 weeks completed gestation) within 48 hours after birth (n=27) where sampling was deemed necessary for other clinical purposes. DNA was extracted from blood and relative telomere length was assessed by qRT-PCR. Results Consistent with previously published data, telomere length appears to be highly variable among the newborn population. Telomere length is negatively correlated with gestational age, however we could find no evidence to indicate that overall telomere length was different between preterm infants sampled at birth compared to those sampled at term equivalent age. Furthermore our results identify that relative telomere length is shortest in term born controls. To the best of our knowledge this is the first study to measure telomere length in preterm infants at term equivalent age. Conclusions Our results do not support the hypothesis that telomere length is reduced in the preterm infant by term equivalent age. Given the high variability in telomere lengths among newborn infants, a longitudinal study in the future may provide valuable detail on the rate of telomere attrition in relation to signs of an ‘aged phenotype’. References (include acknowledgement here if appropriate) Turner K et al. Telomere length analysis and preterm infant health. Biomark Med. 2014; 8(4): 485-498 Okuda K et al. Telomere length in the newborn. Pediatr Res. 2002;52(3):377–381. Senior author supporting presentation on day of meeting: Vimal Vasu Title (Upper case) IMPROVING TRENDS IN THE OUTCOME OF LIVE INBORN BABIES WITH CONGENITAL DIAPHRAGMATIC HERNIA FOLLOWING DEVELOPMENT OF A CENTRALISED MANAGEMENT PROTOCOL Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 2 1 1 R Kumar , A Shenvi , A Bedford Russell , AK Ewer and SV Rasiah Corresponding author e-mail address: 1 Rohit.kumar@bwnft.nhs.uk Institution(s) 1) 2) Birmingham Women’s NHS Foundation Trust Hospital University Hospital of North Midlands Introduction (include hypothesis) Background: The incidence of congenital diaphragmatic hernia (CDH) is 1:2500 live births. In accordance with findings from 1 the MBRRACE-UK CDH report , significant variations in practice were associated with high mortality. Since 2010, care has been centralised within two West Midlands Newborn Networks. All antenatally detected cases of CDH are referred to the regional perinatal centre for fetal medicine assessment, surgical and neonatal counselling. Babies are managed postnatally using agreed guidelines developed by surgical, PICU and neonatal teams. Methods (include source of funding and ethical approval if required) Aim: To review the outcomes of all inborn and live-born babies with CDH, in a regional neonatal intensive care unit (NICU) between January 2000 and December 2014 (15 years), following the implementation of a regional care pathway. Methods: All live-born babies with CDH were identified using the clinical diagnosis code and Badger electronic records. A retrospective review of the patient’s clincal case notes was then done. Results Year 2000-2004 2005-2009 2010-2014 N (Live Inborn Babies) 17 43 68 Transferred to PICU 9 (53%) 20 (47%) 36 (53%) PICU Surgical Survival 8 (88%) 19 (95%) 34 (95%) Transferred for ECMO 0 6 (14%) 14 (21%) ECMO Survival 0 4 (67%) 8 (57%) Overall Survival 8(47%) 23 (53%) 42(62%) The table above summarises the outcomes over five year epochs, the centralised management protocol was implemented in 2010 and the overall survival for 2014 was 73%. Conclusions Centralised management of CDH resulted in all antenatally diagnosed babies being delivered in the regional NICU and reduced variation in postnatal management. There is an improving trend in survival; however benefits have taken 4 years to be realised. ECMO referral has increased. Postsurgical survival without ECMO is excellent. These figures provide important information when counselling parents antenatally. References (include acknowledgement here if appropriate) 1) MBRRACE-UK Perinatal Confidential Enquiry Congenital Diaphragmatic Hernia Report 2014 Senior author supporting presentation on day of meeting: Dr Alison Bedford Russell Title (Upper case) RESPIRATORY MONITORING BY PULSE OXIMETRY PLETHYSMOGRAM ANALYSIS IN PRETERM INFANTS Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 1 1 2 3 Paul Seddon , Sonia Sobowiec-Kouman , Grace Castronovo , Heike Rabe and David Wertheim . Corresponding author e-mail address: seddop@gmail.com Institution(s) 1 Respiratory Unit, Royal Alexandra Children’s Hospital, Brighton, UK. Trevor Mann Baby Unit, Royal Sussex County Hospital, Brighton, UK. 3 Faculty of Science, Engineering and Computing, Kingston University, UK 2 Introduction (include hypothesis) We have previously shown that respiratory data can be derived from pulse oximetry plethysmogram (pleth) recordings in newborn term babies and older infants (Wertheim et al., 2009, Wertheim et al., 2014). The aim of this study was to examine if respiratory rate can be derived from pleth traces in preterm infants. Methods (include source of funding and ethical approval if required) Pulse oximeter pleth, saturation (SpO2) and thoracic/abdominal respiratory inductance plethysmography (RIP) bands were recorded for five minutes from 15 spontaneously breathing infants using a SOMNOscreen Plus system (Somnomedics GmbH, Germany). The pleth data were low pass filtered (LPF) to derive respiratory data using software that we developed using MATLAB (The MathWorks, Inc., USA). Further software was developed in order to display the LPF pleth data together with the thoracic and abdominal band traces as well as SpO2 and pulse rate. Funding was from the NIHR, RfPB scheme; approval was from NRES West Midlands Committee. Results Median (range) gestation at birth was 33 (25-36) weeks and median (range) post-conceptional age at time of recording was 35 (32-37) weeks. Periods of the recordings were analysed, excluding segments with clear artefact and / or low amplitude. Visual assessment of the recordings showed good agreement between the LPF pleth and RIP band data in traces. The median pulse rate in the analysed sections was 145 / minute. Respiratory rate calculated from the LPF pleth data (median 57, range 32 to 66 breaths/ minute) was compared with that computed from the bands (median 62, range 32 to 72 breaths/ minute); the median difference (LPF – band) was -4 and the maximum difference was -9 breaths / minute. Conclusions Our results indicated good agreement between respiratory rate from LPF pleth traces and RIP bands. This study suggests that respiratory rate can be derived from good quality pleth recordings in spontaneously breathing preterm infants in the first few weeks after birth. References (include acknowledgement here if appropriate) Wertheim D, Olden C, Savage E and Seddon P. Arch Dis Child Fetal Neonatal Ed., 2009; 94: F301-3. Wertheim D, Parsley C, Burgess S, Dakin C and Seddon P. Acta Paediatr., 2014; 103: e222-4. Senior author supporting presentation on day of meeting: Dr Paul Seddon Title (Upper case) CORRECTION OF HEMOGLOBIN LEVELS IN A HETEROZYGOUS HUMANIZED MOUSE MODEL OF THALASSEMIA AFTER FETAL GENE THERAPY Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) Panicos Shangaris1,2, Stavros P Loukogeorgakis1,3, Sindhu Subramaniam1, Mike Blundell7, Nahla Bakhamis2, Shanrun Liu4, Simon Eaton1, Durrgah Ramachandra1, Panayiotis Maghsoudlou1, Luca Urbani1, Simon Waddington2, Joy Archer5, Mike Antoniou6, Adrian J Thrasher7, Thomas Ryan5, Paolo De Coppi1 and Anna David2 Corresponding author e-mail address: p.shangaris@ucl.ac.uk Institution(s) 1Surgery Unit, Institute of Child Health, University College London; 2Institute for Women's Health, Maternal & Fetal Medicine, University College London; 3Center for Fetal Research, The Children's Hospital of Philadelphia, Philadelphia, PA; 4University of Alabama at Birmingham, Birmingham, AL; 5Central Diagnostic Services, Queen's Vet School Hospital, University of Cambridge ; 6Department of Medical and Molecular Genetics, King’s College London; 7Molecular Immunology Unit, Institute of Child Health Introduction (include hypothesis) Beta thalassaemia is a genetic blood disease that causes life-threatening anemia. Hematopoietic stem cell (HSC) transplantation successfully cures the disease but in only 30% of patients. We hypothesized that in utero gene therapy (IUGT) to the fetal HSC compartment with the corrected beta globin gene might cure the disease before birth. Methods (include source of funding and ethical approval if required) A humanized mouse model of thalassemia (Cooley’s anemia;CA) was used in which heterozygous animals are affected by anemia, splenomegaly and extra-medullary hematopoiesis. At E13.5 a “GLOBE” vector (HIV-2 based lentiviral vector that incorporates a mini hemoglobin beta gene, the beta-globin promoter and HS2/3β-LCR element) was injected into the liver of each fetus (n=12). At 12 weeks of age, recipient blood, liver, spleen and bone marrow were collected for complete blood count, blood film, as well as RNA and DNA isolation. Extra-medullary hematopoiesis was examined in the spleen and liver using flow cytometry (CD71+/Ter119+cells) and histo-pathological analysis. Results Compared to non-injected heterozygous pups (control), IUGT increased hemoglobin levels [11.3±0.4g/dl (n=6) vs. 7.6±0.6g/dl (n=8); p<0.01], red blood cell count [9.3±0.3*1012/L vs. 6.2±0.5*1012/L; p<0.01), and hematocrit [41.2±2.2% vs. 27.2±2.0; p<0.01]. Moreover, treated CA animals had reduced spleen weight [130±5mg vs.310±21mg; p <0.01], as well as reduced extra-medullary hematopoiesis in the liver [0.7±0.1% (n=4) vs. 6.0±0.9% (n=5); p<0.01] and spleen [6.6±1.8 (n=4) vs. 23.1±1.4 (n=3); p<0.05]. qPCR analysis demonstrated increased gene expression of human beta globin and reduced expression of human gamma globin in blood and bone marrow of IUGT offspring. HPLC analysis confirmed these findings at protein level. The average vector copy number in the liver was 0.1. Conclusions IUGT resulted in phenotypic normalization in a heterozygous humanized mouse model of CA. Increased levels of beta globin and associated down-regulation of gamma globin is consistent with a switch from fetal to adult human hemoglobin, confirming successful prenatal correction of the genetic defect. References (include acknowledgement here if appropriate)n/a Check box if presenting author is a trainee: basic science trainee clinical trainee All authors have approved the abstract, actual or potential conflicts of interest have been declared to the meetings secretary, and the abstract has not been presented previously: Presented at ASH & ESGCT Senior author supporting presentation on day of meeting: Dr Anna David Title (Upper case) WITHDRAWAL OF LIFE SUSTAINING TREATMENT FOR NEWBORN INFANTS: The WiLST Study Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1,2 1,3 3 3 Narendra Aladangady , Chloe Shaw , Katie Gallagher and Neil Marlow for Collaborator Group Corresponding author e-mail address: Narendra.aladangady@homerton.nhs.uk Institution(s) 1.Neonatal Unit, Homerton University Hospital, London; 2,Centre for Paediatrics, Barts and the London School of Medicine and Dentistry, QMUL, London; 3.Institute for Women’s Health, University College London, London. Introduction (include hypothesis) 1 Withdrawal of Life Sustaining Treatment (LST) for newborn infants was first described in 1973 . There are no prospective multicentre studies of the outcomes for babies for whom redirecting Life Sustaining Treatment has 2,3 been considered . Aim: To determine the short-term outcomes of infants for whom clinicians or parents have started discussions about the withholding or withdrawal of LST and/or institution of “do not resuscitate” (DNR) orders. Methods (include source of funding and ethical approval if required) Utilising a secure on-line database (RedCap), we prospectively collected neonatal unit outcomes (death or discharge home) and care practices for babies for whom limiting LST was considered over one year in 9 hospitals in the NEL Neonatal Network. The study was funded by a Programme Development Grant (NIHR) and approved by the East London REC. Results Data from 88 infants (58 males) were studied; mean gestational age 30.1 (SD: 6.8) weeks, birthweight 1592g (SD: 1165). Limiting LST was discussed with parents of 67 infants and in 2 cases discussions were only among the clinical team. Limiting LST was first raised by clinicians in 64 cases and by parents in 3 cases; 23 discussions concerned withholding LST, and 47 withdrawing LST. Following initial discussions, 33 parents (49%) were not in agreement with the clinical team. The parents of 13 infants (27.7%) did not agree for withdrawal of LST. In contrast, of 24 parents specifically asked, all agreed to make a DNR Order. Fifty infants (56.8%) died following limitation of LST, 25 (28.3%) died receiving full intensive care support, 5 (5.7%) survived despite parents agreeing to limit LST and 8 (9.1%) infants survived as result of non-agreement to limit LST. Following limitation of LST, a significantly lower proportion of parents were offered an autopsy (n= 25) or agreed to one (n=6) compared to infants died receiving full intensive care support (17 parents offered and 10 agreed; p=0.018). Conclusions A significant number of parents do not agree with professional opinion to limit LST for their infants and a significant proportion of these infants survive. Reasons for non-agreement are being sought as part of our continuing study. References (include acknowledgement here if appropriate) 1.Duff and Campbell. N Engl J Med 1973; 2.Nuffield Council on Bioethics 2006 and 3.N Aladangady. Early Human Development 2012. Senior author supporting presentation on day of meeting: Narendra Aladangady Title (Upper case) LIMB REMOTE ISCHEMIC POST-CONDITIONING PROTECTS CEREBRAL WHITE MATTER IN A PIGLET MODEL OF PERINATAL ASPHYXIA Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 1 1 1 1 1 1 1 M Ezzati , K D Broad , G Kawano , E Rocha Ferreira , D Alonso Alconada , I Fierens , J Rostami , J Hassell , I 2 3-4 3-4 5 5 6 1 Tachtsidis , P Gressens , B Fleiss , D Yellon , D J Hausenloy , X Golay , N J Robertson Corresponding author e-mail address: n.robertson@ucl.ac.uk Institution(s) 1 Institute for Women’s Health, University College London, 2 Medical Physics and Biomedical Engineering, UCL, 3 Department of Perinatal Imaging and Health, King’s College London, 4 Inserm, U1141, Paris, 5 The Hatter Cardiovascular Institute, UCL, 6 Institute of Neurology, UCL Introduction (include hypothesis) Despite therapeutic hypothermia, ~ 50% treated babies have adverse outcomes; additional simple, safe, effective treatments are needed. Ischaemic postconditioning is a powerful innate protective mechanism against ischaemic-reperfusion injury (1). We aimed to determine if remote ischaemic postconditioning (RIPostC) after cerebral hypoxia-ischaemia (HI) is neuroprotective in a piglet model. Methods (include source of funding and ethical approval if required) *UK Home Office Guidelines [Animals (Scientific procedures) Act, 1986]. After HI, randomisation to: (i) No intervention (n=8); or (ii) RIPostC - four 10 minute cycles of bilateral lower limb ischaemia /reperfusion immediately after HI (n=8). Magnetic resonance spectroscopy was acquired at 24 & 48 h; assessment of regional cell death by immunohistochemistry and gene expression by microarray and qPCR. Results Cerebral white matter protection was seen with four 10 minute cycles of hind-limb ischaemia /reperfusion, evidenced by improved brain energy metabolism at 48h with reduced lactate/N-acetyl aspartate in white matter (p=0.005) and increased NTP/exchangeable phosphate pool (p=0.039). On immunohistochemistry, cell death was reduced in periventricular white matter (PvWM) (p=0.03), internal capsule (p=0.002) and corpus callosum (CC) (p=0.021); there was reduced microglial activation in the CC (p=0.001) and higher numbers of surviving oligodendrocytes in the CC (0.029) and PvWM (p=0.001). Changes in gene expression included the ATPsensitive potassium channel and endothelin A receptor, changes previously seen with RIPostC protection. Phosphorylated ERK activity was increased in the white matter, indicating activation of pro-survival cell pathways. Conclusions Four cycles of 10 minute hind limb ischaemia /reperfusion immediately after cerebral hypoxia-ischaemia protected cerebral white matter. RIPostC was well tolerated and simple to perform. Such a degree of protection is likely to translate into a meaningful clinical effect; further studies are needed. References (include acknowledgement here if appropriate) (1). Pignataro et al., In vivo and in vitro characterization of a novel neuroprotective strategy for stroke: ischaemic post conditioning. J Cereb Blood Flow Metab 2008:28(2):232-41. * MRC grant (MR/J00457X/1) Senior author supporting presentation on day of meeting: Professor NJ Robertson Title (Upper case) Excessive Hypothermia During And Temperature Instability After Completion Of Therapeutic Hypothermia Are Associated With A Poorer Neurodevelopmental Outcome. Authors 1,2 1,2 1 1 Richard Lee-Kelland, MRCPCH , Ela Chakkarapani, MD , Sally Jarry, PHD , Xun Liu, PHD , Emma Scull1 1,2 Brown and Marianne Thoresen, PHD . Corresponding author e-mail address: Richardleekelland@gmail.com Institution(s) 1.) University of Bristol. 2.) St Michael’s Hospital, University Hospitals Bristol. Introduction (include hypothesis) o Therapeutic hypothermia at rectal temperature 33.5 C is now standard of care for babies with neonatal encephalopathy (NE). Infants receiving hypothermia have been noted to overshoot the target temperature during 1 2 both passive and active cooling, even with a servo controlled device . This may reflect a dysfunction in autonomic regulation secondary to cerebral damage. Our hypothesis is that excessive hypothermia during cooling and temperature instability post therapeutic hypothermia are associated with a poorer neurodevelopmental outcome. Methods (include source of funding and ethical approval if required) A case note review of 145 neonates treated with therapeutic hypothermia under the CoolCap/TOBY protocol was undertaken. We recorded hourly rectal temperature measurements during passive cooling, active (servo o controlled) cooling, rewarming and for 24h post rewarming. The target temperature during cooling was 33.5 C. o Excessive hypothermia during passive/active cooling was defined as a temperature <33.0 C. After rewarming, o o Temperature instability was defined as hypothermia <36.0 C and hyperthermia ≥38 C. Temperature was o maintained by using a heated bed, overhead heating or the servo controlled device set at 36.5 C. Outcomes were assessed by neurodevelopmental assessment at 18 months using converted Bayley II mental development 3 index (MDI). Poorer neurodevelopmental outcome was defined as Bayley II MDI <85 (<1SD from the mean). Significance was assessed via chi squared test (p<0.05 two-sided). Results Excessive hypothermia occurred in 31% of infants during the passive or active cooling phase. The excessive hypothermia group had a significantly higher proportion of infants with a poorer neurodevelopmental outcome compared with the rest of the cohort (57% vs 37% P=0.03). Following rewarming 56% of infants became hypothermic, despite being cared for in an incubator or with other external heating. Only one infant at one time point became hyperthermic. The proportion of children with a poorer neurodevelopmental outcome was significantly higher in the group that became hypothermic following rewarming compared to the rest of the cohort (44% vs 19% respectfully P = 0.018). Conclusions Excessive hypothermia during active cooling and temperature instability leading to hypothermia after rewarming are associated with a poorer neurodevelopmental outcome. We do not know whether optimising therapeutic hypothermia to prevent excessive hypothermia will improve neurodevelopmental outcome. Hyperthermia is negligible following therapeutic hypothermia using current practise. References (include acknowledgement here if appropriate) 1.) 2.) 3.) Fairchild, K., Sokora, D., Scott, J., & Zanelli, S. (2010). Therapeutic hypothermia on neonatal transport: 4-year experience in a single NICU. Journal of Perinatology, 30(5), 324–329. Massaro AN et al. Short-term outcomes after perinatal hypoxic ischemic encephalopathy: a report from the Children's Hospitals Neonatal Consortium HIE focus group. (2014) Journal of Perinatology 13, 1-7 Jary, S., Whitelaw, A., Walløe, L., & Thoresen, M. (2013). Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Developmental Medicine and Child Neurology, 55(11), Senior author supporting presentation on day of meeting: Dr Ela Chakkarapani Title (Upper case) OUTCOME OF ANTENATALLY DETECTED ENCEPHALOCELE; TERTIARY CENTRE EXPERIENCE OVER A 10 YEAR PERIOD. Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 2 1,3 Amy Walker, , Desidero Rodrigues, Denise Williams, Corresponding author e-mail address: 1 4 Tamas Marton, Ann Tonks, Andrew K Ewer. 1,5 amy@thewalkers.me.uk Institution(s) 1 3 2 Birmingham Women’s NHS Foundation Trust, Birmingham Children’s Hospital 4 5 West Midlands Regional Genetics Service, West Midlands Perinatal Institute, University of Birmingham. Introduction (include hypothesis) Encephalocele is a rare congenital abnormality of the central nervous system (CNS) with protrusion of the meninges and brain through a defect in the skull. There is a lack of information about the outcome of these 1 pregnancies. The aim of this study was to collate outcome data on all cases of encephalocoele so that antenatal counselling may be more informative. Methods (include source of funding and ethical approval if required) Cases of antenatally diagnosed encephalocele between 01/01/00 and 31/12/09, were identified from fetal medicine, regional anomaly, genetics and pathology databases. Notes were reviewed to collate pregnancy and neurodevelopmental outcomes. Ethical approval was obtained. Results 53 cases were identified. 40 posterior, 4 anterior and 1 interparietal. In 8, site was not classified. 43% had other CNS abnormalities; (ventriculomegaly - 9, microcephaly - 5 , spinal bifida – 5, holoprosencephaly - 2 other CNS abnormalities – 2). Non-CNS abnormalities occurred in 18 cases (15 renal, 3 cardiac). 40 pregnancies were terminated, 6 resulted in live births and 7 were lost to follow up. 58% of cases had chromosomal testing - 4 were abnormal. Post-mortem was performed in 53% of cases identifying 7 additional CNS defects and 11 non-CNS abnormalities.14 cases had a diagnosis of Meckel Gruber syndrome (MG). Of the live births, 3 died within 2 months of age and 3 were still alive. Two long-term survivors have learning difficulties, the other had reported normal development at 21 months. Conclusions This is the largest cohort of antenatally diagnosed encephalocele. As with other reported data we have a high termination rate. With only 3 long-term survivors the outcome remains guarded for this condition. References (include acknowledgement here if appropriate) 1. Ultrasound Obstet Gynecol. 2014 Sep 5. doi: 10.1002/uog.14661. [Epub ahead of print]Fetal Cephalocele: First-Trimester Sonographic Spectrum In A Review Of 35 Cases.Sepulveda W1, Wong AE, Andreeva E, Odegova N, Martinez-Ten P, Meagher S. Senior author supporting presentation on day of meeting: Dr Andrew K Ewer Title (Upper case) ONE-YEAR MORTALITY OF VERY PRETERM INFANTS ADMITTED TO NEONATAL UNITS IN ENGLAND Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) Buthaina Ibrahim, Yevgeniy Statnikov, Daniel Gray, Neena Modi, Sonia Saxena and the Medicines for Neonates Investigator Group* Corresponding author e-mail address: b.ibrahim@imperial.ac.uk * Neena Modi, Peter Brocklehurst, Jane Abbott, Kate Costeloe, Elizabeth Draper, Azeem Majeed, Jacquie Kemp, Deborah Ashby, Alys Young, Stavros Petrou Institution(s) Department of Primary Care and Public Health, Charing Cross campus; Section of Neonatal Medicine, Department of Medicine, Chelsea and Westminster Hospital campus, Imperial College London, SW10 9NH, UK Introduction (include hypothesis) Globally 130 million babies are born every year and nearly 4 million die in the first 28 postnatal days [1]. Infants born very preterm constitute approximately one third of these deaths [2]. The survival to discharge of preterm infants has been the focus of many studies however, there are few objective estimates of later survival. The purpose of this study was to describe mortality over the first year among very preterm infants by gestational age and differences in maternal characteristics by gestational age band. Methods (include source of funding and ethical approval if required) We analysed data on infants, with a completed gestational age between 23+0 and 32+6 weeks, born in England between 1 January 2010 and 31 December 2010 and admitted to a neonatal unit (NNU). Data were extracted from a birth cohort created by linking the National Neonatal Research Database (NNRD) and the Hospital Episode Statistics (HES). We assessed differences in the frequency distributions of maternal characteristics by gestational weeks: maternal age (<20 years, 20-24 years, 25-29 years, 30-34 years and ≥35), ethnicity (White, Asian or Asian British, Black or Black British, Mixed and other Ethnic Groups) and social deprivation (defined using the Index of Multiple Deprivation quintile categories). We used chi-squared test to compare categorical variables by gestational age band. We determined mortality in the early neonatal (0-6 days), late neonatal (7-27 days) and postneonatal (28-365 days) periods by gestational age. This abstract presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (RP-PG-0707-10010). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Results We identified 7,463 live-born infants; 1.7% (n=129) were births at 23 weeks, 3.7% (n=273) at 24 weeks, 4.1 (n=307) at 25 weeks, 6.3% (n=468) at 26 weeks, 7.2% (n=535) at 27 weeks, 9.8 (n=733) at 28 weeks, 10.7% (n=801) at 29 weeks, 13.1% (n=977) at 30 weeks, 17.8 (n=1329) at 31 weeks and 25.6% (n=1911) at 32 weeks. There were significant differences in maternal age, ethnicity and social deprivation by gestational age. The frequency of mothers younger than 20 years of age, of black ethnicity and from the most deprived areas was higher in infants born at 23 weeks than those born at 32 weeks (23 weeks: 23.4%, 13.3% and 46.6%, respectively; 32 weeks:7.8%, 6.4% and 32.2%, respectively; p-values .0001, <.0001 and .009, respectively). Of all infants, 228 (3.1%) died during the early neonatal period, with mortality ranging from 35.7% at 23 weeks to 0.5% at 32 weeks, and 122 (1.7%) died during the late neonatal period, with mortality ranging from 18.1% at 23 weeks to 0.3% at 32 weeks. 178 infants (2.4%) died before in the postneonatal period and mortality ranged from 14.7% at 23 weeks to 0.7% at 32 weeks. Conclusions We found that among very preterm infants there were significant differences in maternal age, ethnicity and social deprivation. Early neonatal, late neonatal and postneonatal mortality was 3.1%, 1.7% and 2.4%, respectively.Our results for postneonatal mortality were similar to those reported by ONS for live-births in 2010 although we found higher mortality for infant born at 23 and 24 gestational weeks (14.7% and 11,7%; 7.6% and 9.9%). This may be explained by live born babies that die before admission to a NNU that are not therefore included in the NNRD, and to the fact that in the ONS reports there were high proportions of ‘Not Stated’ gestational ages concentrated in the North East Region. Our study reinforces the relevance of socio-economic circumstances in relation to preterm birth, and the importance of complete, accurate data recording. References (include acknowledgement here if appropriate) [1] Zupan, J. Perinatal mortality in developing countries. N Engl J Med 2005; 352: 2047-8 [2] Zeitlin, J et al. Differences in rates and short-term outcome of live births before 32 weeks of gestation in Europe in 2003: results from the MOSAIC cohort. Pediatrics 2008; 121: e936-44 Senior author supporting presentation on day of meeting: Professor Neena Modi Title (Upper case) PRETERM BIRTH IS ASSOCIATED WITH ATYPICAL SOCIAL COGNITION IN INFANCY Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1. Dr Emma J Moore, 2. Dr Karri Gillespie-Smith 3. Dr Sue Fletcher-Watson, 1,3. Dr James P Boardman Corresponding author e-mail address: emma.moore@ed.ac.uk Institution(s) 1.MRC Centre for Reproductive Health, University of Edinburgh; 2. Psychology, University of West of Scotland 3. Centre for Clinical Brain Sciences, University of Edinburgh Introduction (include hypothesis) 1,2 Preterm infants are at increased risk of developing neurocognitive and psychiatric impairment in childhood . Early identification of children at risk could facilitate early interventions designed to improve outcome. Eyetracking is a technique that can objectively and quantifiably assess eye-gaze behaviour in response to stimuli in 3 non-verbal populations and allows inferences to be made about underlying cognitive function. Here we test the hypothesis that social cognition in infancy is altered by preterm birth. Methods (include source of funding and ethical approval if required) +3, +2 +6 43 preterm infants (mean postmenstrual age [PMA] birth,29 range 23 -34 ; 17 males) and 42 term infants (≥ 37 weeks PMA, 21 males) were assessed between 6 and 18 months corrected PMA using the Tobii x60 eyetracker. Infants were presented with stimuli of increasing complexity: static face, face with objects within a gridlike array and pairs of naturalistic scenes with and without social content. Time to first fixation, fixation duration and location of fixation were recorded and analysed using Student’s t-tests, repeated measures ANOVA, and non-parametric tests as required. Informed parental consent and ethical approval were obtained. Results There was no significant difference in age at testing between groups; 8.77 months (preterm) and 8.48 months (term), p= 0.581. Preterm infants demonstrated a reduced preference to social information when compared to term infants as demonstrated by a difference score of fixation duration (eyes- mouth) within the face, p= 0.045 (figure 1). This pattern was repeated in more complex tasks in fixation duration; grid-like array (median fixation duration to face 1.16 vs. 1.3s, p=0.023); naturalistic scene (mean fixation of social content 1.1 vs. 1.4s and non-social content 0.79 vs. 0.72s, p=0.026). Conclusions Eye-gaze behaviours in response to stimuli depicting social content of varying complexity differ between preterm infants and term controls, when assessed in late infancy. These data suggest that the development of social cognition is altered by preterm birth. References (include acknowledgement here if appropriate) 1. Bhutta AT et al JAMA 2002 2. Johnson S et al JAACAP 2010 3. Jones W, Klin A. Nature. 2013 Funding: Theirworld. Senior author supporting presentation on day of meeting: Dr James Boardman Title SEVERE BIOCHEMICAL DISTURBANCES AFTER INTRODUCTION OF A NEW REGIONAL PARENTERAL NUTRITION FORMULATION MATCHING CURRENT ESPGHAN RECOMMENDATIONS Authors 1 1 1 1 1 2 1 Shaveta Mulla , Sarah Cowey , Rosie Close , Sara Pullan , Rosalind Howe , Lynne Radbone , Paul Clarke . Corresponding author e-mail address: shavetamulla@gmail.com Institutions 1 Neonatal Unit, Norfolk and Norwich University Hospitals NHS Foundation Trust, Norwich, UK. 2 East of England Neonatal Operational Delivery Network, UK. Introduction Enhanced early postnatal nutrient supply to very low birth weight infants is associated with improved growth [1] velocity, white matter maturation and head growth. Current ESPGHAN guidelines recommend a maximum amino 2+ acid content of 4.0 g/kg/day and a Ca :PO4 ratio within the range 1.3-1.7:1 for preterm parenteral nutrition (PN). In January 2013 East of England regional NICUs introduced a new PN formulation that essentially accorded with 2+ these latest ESPGHAN recommendations. Our aqueous bag contained 3.3 g amino acids, 1.7 mmol Ca , and 1.1 2+ mmol PO4 per 100 mL and, including lipid, achieved a first-week Ca :PO4 ratio in the range 1.4-1.3:1. During 2013 several regional NICUs, including our own, reported cases of severe hypercalcaemia and/or hyposphataemia in preterm infants during the first postnatal week. Our hypotheses were that these electrolyte disturbances were due [2, 3] 2+ to the ‘refeeding syndrome’, and that increasing the PO4 content to match Ca in an equimolar ratio would prevent these abnormalities. We report our audit of first-week biochemistry in preterm babies who received the new PN formulation in epochs before and after provision of increased phosphate supplementation. Methods We retrospectively reviewed casenotes, PN charts, and serum biochemistry of all preterm infants in our NICU, who received the new regional PN formulation in two discrete ~6-month epochs before (Phase 1) and after (Phase 2) the date of ad hoc-increased PO4 supplementation (December 2nd 2013). The PN recipe was otherwise unchanged across epochs. We assessed the incidence and severity of biochemical derangements occurring with PN delivery in 2+ the first postnatal week. We pre-defined severe hypercalcaemia as serum Ca >3.0 mmol/L, hypophosphataemia as PO4 <1.5 mmol/L, and severe hypophosphataemia as PO4 <1.0 mmol/L. We analysed by intention to treat. Results Data for 102 infants were reviewed. There were no significant differences in baseline characteristics or amino acid 2+ intakes between the two epochs. The table shows median (range) first-week serum Ca and PO4 concentrations in the phases and numbers of infants with deranged biochemistry: Phase 1, N = 51 Phase 2, N = 51 P value Calcium 2+ Peak Ca concentration, mmol/L 3.05 (2.67─3.73) 2.84 (2.20─3.15) <0.0001 2+ Ca >3.0 mmol/L, n (%) 31 (61) 11 (22) 0.0001 Phosphate Nadir PO4 concentration, mmol/L 1.37 (0.43─1.98) 1.59 (0.59─2.62) 0.004 PO4 <1.5 mmol/L, n (%) 31 (6 ) 11 (22) 0 0001 PO4 <1.0 mmol/L, n (%) 17 (33) 7 (14) 0.04 Conclusions 2+ Introduction of the latest ESPGHAN-recommended intakes for amino acids with the recommended Ca :PO4 ratio for preterm PN led to severe hypercalcaemia and hypophosphataemia in most preterm babies in our NICU. Extra 2+ phosphate supplementation to achieve an equimolar Ca :PO4 ratio significantly reduced the incidence and severity 2+ of these biochemical disturbances, while maintaining the recommended amino acid, Ca and PO4 intakes. Our audit findings have assisted a revised regional PN formulation and may inform future ESPGHAN recommendations. References 1. Strømmen K, et al. Neonatology. 2015; 107: 68-75. 3. Bonsante F, et al. PLoS One. 2013; 8: e72880. 2. Moltu SJ, et al. Clin Nutr. 2013; 32: 207-12. Senior author supporting: Dr Paul Clarke Title (Upper case) POSTNATAL AGE RELATED METABOLIC CHANGES IN FAECAL WATER FROM PREMATURE BABIES Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) Przysiezna N1, Wijeyesakera AD2, Parkinson JR1, Hyde MJ1, Uthaya S1, Holmes E2, Modi N1 Corresponding author e-mail address: n.przysiezna12@imperial.ac.uk Institution(s) 1 Section of Neonatal Medicine, Department of Medicine, Imperial College London, Chelsea & Westminster campus, 369 Fulham Road, London, UK; 2 Computation Systems Medicine, Sir Alexander Fleming Building, Imperial College London, South Kensington, SW7 2AZ Introduction (include hypothesis) The composition of biofluids can provide useful information regarding health, physiology and may identify biomarkers of disease risk. Microbiota colonising the gut in early life may be a causal factor in long term health outcomes. Given their hospital environment it is to be expected that preterm babies will have a considerably different pattern of colonisation compared to term born infants. Here we used stool water metabonomics as a surrogate for gut microbiota activity, to answer the research question: Is there a time (post-natal age) dependant trend in the composition of stool water. Methods (include source of funding and ethical approval if required) The study was conducted with Research Ethics Committee (09/H0707/88) approval as part of the NIHIR funded doubleblind 2x2 factorial randomised trial of early nutrition (NEON). Weekly stool samples were collected from 160 infants and stored at -80°C until analysis (total number of samples = 1187). Stool water was extracted and analysed using onedimensional 1H NMR spectroscopy at 300K on a Bruker LC-NMR 600 MHz spectrometer, using standard parameters and Bruker pre-processing algorithms. The spectra were phased, baseline corrected and referenced using an in-house script (MATLAB). We used probabilistic normalisation and analysed the spectra using Principal Component Analysis (PCA) and Orthogonal Partial Least Squares analysis (O-PLS). Results Analysing data from all babies (time points from 1 to 21 weeks postnatal age), we showed that the metabolic profile of stool samples from preterm infants altered over time (Fig 1). The PCA plot indicates that the variation in the metabolic profile of the faecal water decreases with increasing postnatal age. The greatest variation is seen during the first four weeks of postnatal life. The following metabolites increased with postnatal age: alanine, acetate, trimethylamine and tyramine. The source of acetate and trimethylamine is likely to be bacterial metabolism. Figure 1: PCA scores scatter plot from NMR spectra of stool samples representing multiple time points for 160 premature infant. Samples coloured according to postnatal age (in weeks). Conclusions Indirect assessment of gut microbiota activity in preterm infants indicates that the variation observed in the first few weeks of life is reduced after a month. This overlaps with increasing amounts of enteral feeding and decreasing reliance on parenteral nutrition. Given the high exposure to breast milk in this cohort and that breast fed infants have lower microbial variability this may explain our findings. Infants are also likely to be commonly exposed to hospital specific bacteria. References (include acknowledgement here if appropriate) 1. Parkinson JRC et al (2013) Pediatrics. 131:E1240 Senior author supporting presentation on day of meeting: n.modi@imperial.ac.uk Title (Upper case) PRETERM BIRTH IS ASSOCIATED WITH ALTERATIONS IN THE METHYLOME AT SITES THAT INFLUENCE NEURAL DEVELOPMENT. Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 2 3 1 1 3 Sarah A Sparrow , Jonathan Manning , Chinthika Piyasena , Rozi Pataky , Emma Moore Amanda J Drake , and James P 1,4 Boardman Corresponding author e-mail address: sarahannemitchell@hotmail.co.uk Institution(s) 1 2 MRC Centre for Reproductive Health, University of Edinburgh; Centre for Regenerative Medicine, University of Edinburgh 4 University/BHF Centre for Cardiovascular Sciences, University of Edinburgh; and Centre for Clinical Brain Sciences, University of Edinburgh. 3 Introduction (include hypothesis) Early exposure to the extra-uterine environment is closely associated with altered brain development and long term neurodevelopmental impairment. DNA methylation, involving the addition of a methyl group to cytosine nucleotides, influences gene expression and is fundamental to normal neural development. DNA methylation is dynamic and can be influenced by stressful early life environmental exposures. We test the hypothesis that preterm birth affects the methylome, leading to differences between preterm infants at term equivalent age and term controls. Methods (include source of funding and ethical approval if required) Subjects included 36 preterm infants (mean postmenstrual age [PMA] at birth 28+3 weeks, range 23+2 to 32+5) at term equivalent age (mean 39+5 weeks' PMA, range 38+0 to 42+4) and 36 term controls (mean 41+2 weeks' PMA, range 38+3 to 47+1), matched for sex. Ethical approval and informed parental consent were obtained. DNA was extracted from buccal cells. DNA methylation was measured at over 485,000 sites throughout the methylome using Illumina HM450 BeadChip array. Differential Methylation was assessed using RnBeads v 0.99.13. Results 18 protein coding genes and 33 protein coding associated promoters showed significantly different methylation between preterm and term infants (FDR-corrected combined p value <= 0.05). Genes of interest with regards to CNS development and signalling included: Gene % diff. p-value Description SLC2A1 2.2 .04 Solute carrier family 2 (facilitated glucose transporter), member 1 APOL1 2.7% .043 apolipoprotein L, 1 QPRT 3.7% .0077 quinolinate phosphoribosyltransferase NPBWR1 9.7% .021 neuropeptides B/W receptor 1 RTP4 11.1% .00086 receptor (chemosensory) transporter protein 4 GPR21 4.1% .0086 G protein-coupled receptor 21 Conclusions Preterm birth is associated with alterations in the methylome at sites that influence neural function. DNA methylation may provide a molecular link between the stress of preterm birth and accompanying alterations in brain development. References (include acknowledgement here if appropriate) 1. 2. 3. Murphy S et al PloS ONE 2012 Klengel et al. Nature Neuroscience 2013 Khulan B et al. Translational Psychiatry 2014 Senior author supporting presentation on day of meeting: James P Boardman Title (Upper case) THE IMPACT OF ROUTE OF DELIVERY ON SKELETAL MUSCLE METABOLISM IN PIGLETS Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) James Whistler, Alison Mostyn, Matthew J. Hyde Corresponding author e-mail address: alison.mostyn@nottingham.ac.uk Institution(s) School of Veterinary Medicine and Science, Sutton Bonington Campus, University of Nottingham, Leicestershire, LE12 5RD and Neonatal Medicine, Imperial College London, Chelsea and Westminster Campus, 369 Fulham Road, London, SW10 9NH. Introduction (include hypothesis) The occurrence of pre-labour Caesarean section (CS) delivery is increasing, despite limited research on the effects on neonatal metabolism. We have previously described differences in adipose tissue in offspring (1) delivered by CS delivery; and attributed these to the loss of the intrapartum cortisol surge . We now explore the impact of route of delivery on skeletal muscle (SM) metabolic pathways in porcine neonates. We hypothesise that CS delivery will reduce SM metabolic processes which are essential for neonatal survival. pathways in porcine neonates Methods (include source of funding and ethical approval if required) Four pregnant sows were randomly allocated to CS at 112 days gestation (~115 days is full term) or spontaneous vaginal delivery (VD). Both CS (n=4) and VD (n=5) offspring were fed a sow milk replacer. At 7 days of age piglets were humanely euthanased and SM sampled. Gene expression was assessed using real time PCR, tissue glycogen, lipid and protein were measured by biochemical assay. All animal work had full local (2) ethical and national Home Office approval; further information on the methods are described by Hyde et al . Data was analysed using SPSS and Arraymining.net. Results 11β-Hydroxysteroid dehydrogenase type 2 (CS=0.89±0.02, VD=1±0.02; p=0.03) and insulin-like growth factor 1 (CS=0.95±0.02, VD=1±0.01; p=0.03) expression was reduced in the CS group while pyruvate dehydrogenase kinase 4 was increased (CS=1.19±0.06, VD=1±0.02; p=0.03). A significant reduction in glycogen was observed in the VD group (CS=67.8±0.2, VD=32.4±0.3; p=0.03), however, tissue lipid and protein concentrations were similar. Serum hormone and metabolite concentrations were made available via MJH and significant reductions in glucose, lactate and triglyceride were identified. A significant negative relationship between IGF1 expression 2 and fractional growth rate was observed in the CS group only (R =0.91, P=0.05). Cluster analysis segregated the data into two independent clusters: one single cluster included all VD offspring and all the CS offspring in the second cluster. Conclusions Despite the small animal numbers, this study demonstrates striking differences in crucial metabolic pathways, particularly glycogenolysis, between Caesarean section and vaginally delivered neonatal offspring. The longterm impacts of these changes remain to be elucidated. References (include acknowledgement here if appropriate) 1. Thickett A, et al.Proc Nutr Soc. 2011;70:E28. 2. Hyde MJ, et al.Clin Sci. 2009;118:47. UG research project funded by The School of Veterinary Medicine and Science, University of Nottingham Senior author supporting presentation on day of meeting: Matthew Hyde Title (Upper case) THE ASSOCIATION BETWEEN BREAST MILK MACRONUTRIENT CONTENT AND MATERNAL BMI Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) 1 1 1 2 Nicholas J. Andreas , Matthew J. Hyde , Suzan Jeffries , Elaine Holmes & Neena Modi Corresponding author e-mail address: 1 n.andreas11@imperial.ac.uk Institution(s) 1 2 Section of Neonatal Medicine, Department of Medicine, Imperial College London, UK Section of Computational and Systems Medicine, Faculty of Medicine, Imperial College London, UK Introduction (include hypothesis) Previous research on donor breast milk has suggested a positive correlation between maternal Body Mass Index 1 (BMI) and breast milk concentration of protein, carbohydrate and fat . We sought to further study the relationship between maternal BMI and fore and hind milk composition, over the first three months of lactation. We tested the hypothesis that we would observe differences in breast milk composition between high and normal BMI mothers. Methods (include source of funding and ethical approval if required) We obtained fore and hind milk samples from 95 mothers delivering at full-term, at seven days and three months post-partum. 52 mothers had a BMI <25, 43 a BMI >25. Samples were frozen at -80°C until analysis, when they were thawed and homogenised using sonication prior to analysis. Macronutrient content was determined using mid-infrared spectroscopy (Miris Human Milk Analyser loaned by MIRIS AB, Sweden), in accordance with manufacturer instructions. We used ANOVA (SPSS) to assess the relationship of breast milk macronutrient content in relation to maternal BMI. The study received Research Ethics approval (12/LO/0203) and was funded by Westminster Medical School Research Trust. Results We obtained a total of 284 samples (1 week, fore milk=95, hind milk=40; 3 months, fore milk=90, hind milk=59). We found no statistically significant or clinically relevant correlations between maternal BMI and breast milk protein, carbohydrate or fat content at either of the time points, nor did maternal pregnancy weight gain influence the concentration of macronutrients. In agreement with previous reports at three months only 24% of women with a BMI >25 were still breast feeding compared to 75% of mothers with a BMI <25. Also in keeping with other reports, we found that hind milk has significantly more fat and less carbohydrate than fore milk, regardless of stage of lactation. However, protein concentration in fore and hind milk differed with stage of lactation: at 7 days, there was no difference between fore and hind milk; but at 3 months there was more protein in hind milk (p=0.009). Between 7 days and 3 months of lactation, in fore milk, the concentration of fat remained stable, carbohydrate increased and protein decreased; in hind milk there were significant increases in fat and carbohydrate, but a significant decrease in protein. Conclusions In contrast to previous research, we did not observe any association between maternal BMI and breast milk macronutrient content at any of the time points studied. Our data suggest that breast milk composition is regulated independent of maternal BMI. References (include acknowledgement here if appropriate) 1 Michaelsen, K. F. J Pediatr Gastroenterol Nutr. 1990 11(2); p. 229-39 Senior author supporting presentation on day of meeting: Professor Neena Modi Title (Upper case) DOES THE SENSITIVITY OF PULSE OXIMETRY SCREENING DEPEND ON THE TYPE OF CRITICAL CONGENITAL HEART DISEASE? AN ADJUNCT TO THE PULSE OXIMETRY SCREENING DEBATE. Authors (Presenting author underlined. If no author is a Society member please provide the name of the member introducing the author to the Society) I. Mawson, P. Babu, G. Fox, J. Simpson Corresponding author e-mail address: John.simpson@gstt.nhs.uk Institution(s) Neonatal and Cardiology Departments, Evelina London Children’s Hospital, Guy’s and St Thomas’ NHS Foundation Trust. Introduction (include hypothesis) The aim was to investigate the sensitivity of newborn pulse oximetry (Pulsox) screening for each type of critical congenital heart disease (CCHD). The hypothesis was that Pulsox screening sensitivity varies depending on the type of CCHD being identified and depending on the threshold used for further investigation. A meta-analysis in 1 2012 described Pulsox screening’s sensitivity as moderate, with high specificity and low false positive rates. Due to small numbers of infants with CCHD in studies little data is available on Pulsox sensitivity by diagnosis. Methods (include source of funding and ethical approval if required) Retrospective review of admission pre-ductal oxygen saturations of infants with antenatally diagnosed CCHD delivered at a cardiac neonatal unit between 2010- 2014. Saturations were recorded at median of <1hr (range <1-9hrs) after delivery. Data was stratified by CCHD diagnosis and analysed according to three different oxygen saturation thresholds, ≤90%, ≤92%, and ≤95%. Sensitivities (with 95% confidence intervals) of Pulsox screening using each threshold were calculated using Microsoft Excel for the whole data set and for each CCHD diagnosis. Calculations were repeated for a group representing infants well enough for postnatal ward care. Results 276 neonates were identified. 208 (78.2%) were clinically well, admission to the neonatal unit occurred purely due to antenatal CCHD diagnosis. In this group Pulsox was more sensitive using ≤95% threshold at 71.6%(65.577.8%) compared to ≤92% (52.3%(45.6-59.2%))and ≤90% (46.2%(39.4-52.9%)). The 95% confidence intervals (95%CI) for Pulsox sensitivities using a threshold of ≤90% and ≤92% did not overlap with the 95%CI of the Pulsox sensitivity using ≤95%. Pulsox sensitivity was increased by 37.5-52.7% using ≤95% threshold compared to ≤90% for hypoplastic left heart (HLH), tetralogy of fallot (TOF) and interrupted aortic arch (IAA). Using the highest threshold (≤95%) Pulsox sensitivity for aortic stenosis (AS) was 20%(0.0-55.1%), pulmonary stenosis was 36.4%(7.9-64.8%), and coarctation was 41.5%(26.4-56.5%) whereas sensitivity for pulmonary atresia (PA) at threshold ≤90% was 66.7%(40.0-93.3), TGA 83.9%(74.7-93.0%) and TAPVD 100.0%(100.0-100.0%). Conclusions Pulsox sensitivity is influenced by CCHD diagnosis and is highest using ≤95% threshold (overall and especially for HLH, IAA and TOF). In coarctation, AS and PS, the minority of cases were detected irrespective of saturation threshold. TGA, PA and TAPVD would be detected in the majority regardless of the threshold. References (include acknowledgement here if appropriate) 1. Thangaratinam S, Brown K, Zamora J, et al. “Pulse oximetry screening for critical congenital heart defects in asymptomatic newborn babies: a systematic review and meta-analysis.” The Lancet 2012;379:2459-64 Senior author supporting presentation on day of meeting: Dr G. Fox Self Certificate of Attendance Please complete the form below and have it signed by a member of the neonatal society committee if you wish to claim RCPCH CPD points Neonatal Society Spring Meeting The Institute of Child Health, London 19th March 2015 Name of person claiming CPD points: (Blockletters)………………………………………. Place of Work:…………………………………………………………………. Number of CPD points claimed :…………………………………………….. (1 point per hour of attendance – up to a maximum of 5 CPD Points) Claimant’s Signature………………………….. Name and signature of Neonatal Society Committee member ………………………………………………………… Howard Clark/Richard Thwaites/Neena Modi/James Boardman Andrew Ewer/Topun Austin/Divyen Shah/David Carr (please delete as appropriate)
© Copyright 2025