The shared care record - Capital & Coast District Health Board
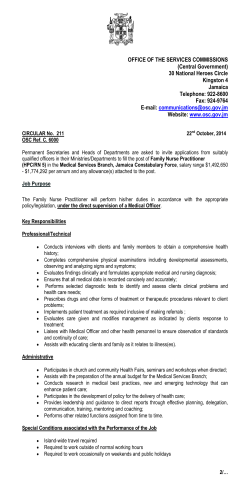
Health Matters Ca p i t al & C o a s t D H B s t a f f n e w s I SSUE 2 • MARCH 2015 The shared care record Why aren’t we using it ? Dr Bryan Betty, GP equipment invoices Leadership Matters What every leader should know pg 4 Why you shouldn’t be signing them pg 3 A Day in the Life Mortuary Technicians pg 12 Message from ELT: I have been asked to write a few words, as a member of the Executive Management Team, to introduce the March issue of Health Matters. catherine epps, Executive Director, Allied Health, Scientific & Technical There is much to comment on and be proud of in an organisation that continues to challenge and transform itself to better meet the needs of our consumers within the resources that we have. This issue of Health Matters picks up on several of the key areas of focus for this organisation at the moment: clinical improvements, health targets, and working with our neighbours. All of these things bring a different improvement focus to them, and a need for strong team work to ensure that we deliver on what is expected of us. In terms of the workforces I represent, the Allied Health, Scientific and Technical (AHS&T) professions will be contributing to all of the above workstreams between them. I am also pleased to share that with the recent changes to the way we deliver services across Laboratories, Radiology, Mental Health, Addictions and Intellectual Disability services, that approximately half the AHS&T workforce are now part of a sub-regional service. This is a huge Health Matters achievement and reflective of the ability of these professions to continue to transform the way they deliver services in order to best meet the needs of our patients, population, and system. By coincidence, it is also my turn to write the executive blog and so I have written some personal thoughts on how we deliver the changes to the health system without unintended consequences. You are welcome to read that online as well at ccdhbcheckinwelcome.blogspot.co.nz We are all tasked with improving the way we work, and so I hope this issue of Health Matters both informs and inspires you to keep focused and involved in what we can achieve together. Catherine If you have story ideas or feedback on Health Matters, please email them to us at healthmatters@ccdhb.org.nz Weakness, delirium, or fever without a focus »»Individualise care »»Be mindful of the prevalence of asymptomatic bacteriuria »»Seek other causes Specific UTI symptoms »»Test or treat as usual 2015 Issue 2 l Health Matters 10-16 March Brain Awareness week: www.neurological.org.nz 10 -16 March Kidney Health Awareness Week 12 March Walk To Work Day; World Oral Health Day 16-22 March Food and Hydration Week 22 – 30 March Muscular Dystrophy Awareness and Appeal Week 24 March World Tuberculosis Day 24 – 30 March Hearing Week 31 March Staff Forum - 3-4pm Meeting Room, Kapiti GET AR T ear n Smoking advice target February update 93% of inpatients offered advice No symptoms of UTI »»Do not test urine »»Do not test if a urine test was done by someone else or for ‘routine’ 2 Up & coming Nearly there - keep it up! Get the best out of that test! Sharing is Caring H Dr Peter Hicks and Dr Andre Cromhout using the Shared Care Record. ospital clinicians are being called on to better utilise the Shared Care Record, as usage statistics show access has levelled off following its launch almost one year ago. Launched locally last year, 43 GP practices’ representing 80.7 percent of our DHB population patients are signed up to the Shared Care Record. However, statistics show only 13 percent of those records were accessed by hospital clinicians in January this year. This indicates the Shared Care Record is not being used as well as it could be, particularly when it comes to avoidable and unnecessary test duplication. “The system is in place, now we’re just asking clinicians to keep it ‘front of mind’ when patients come to see them,” says Dr Bryan Betty, Porirua GP (on the front cover). “Often it is the most up to date record of a patient’s medical history. In an acute situation this information is obviously quite important for anyone trying to work through clinical issues.” letters received from hospitals or other specialists around the country are sent, and all blood test and x-ray results, as well as classifications for any short or long term conditions they may have. Knowing what patients have been prescribed is key when it comes to avoiding serious medication errors, as patients may not always be able to tell clinicians what they’ve been taking, for a variety of reasons. Some tests may have to be retaken in hospital but others may be potentially wasting resources and time, he says. “You might have a patient come in who presents acutely for the first time, maybe with chest pain or an infection of some kind. An elderly person may be confused, so having access to what they have been prescribed is really important.” Dr Betty says. The Shared Care Record gives hospital clinicians access to an inbox where all Wellington Hospital ICU specialist Dr Peter Hicks says there are some features Monthly $ $ $ $ Financial UPDATE to note in particular, such as the icon which indicates whether clinicians can access patients’ record information but its usefulness will be greatly improved later this year when access is extended to other Central Region DHBs. “In the next few months we hope to add access to broader range of primary care information by extending our coverage to records at the MidCentral, Hutt Valley, and Wairarapa DHBs.” If you’ve had to sign an invoice in the last month, you’re doing it wrong. T here are currently over 3000 suppliers on CCDHB’s database, but you may not know that 80 percent of all health spending in New Zealand comes from just 79 of them. If you’re not ordering supplies through IPROC, you’re probably being overcharged. Purchase orders take advantage of the national contracts we have negotiated to ensure best value for money. Otherwise you may be paying more for the same item. A purchase order also enables us to instantly check whether you have been overcharged or if goods have been underdelivered, saving weeks of paper work. No matter which way you look at it, it just makes sense. You can access IPROC to log a purchase order via your Oracle log-in. Annual leave Last month we reported that collectively you took 4764 less days of annual leave over Christmas and New Year than last year – but that’s only about one less day per person. So why not take a longlong weekend this Easter? 2015 Issue 2 l Health Matters 3 One call solves all at dietetic clinic A new patient-orientated approach to bookings by the hospital’s dietetic clinic has seen a dramatic drop in appointment non-attendance, from 50 per cent of patients to zero in the last six months. Percentage of patients DNA'ed (%) 70 No Clinics in March Diabetes Dietitian DNA rates (%) 60 50 New 40 Follow Up 30 Linear (New) 20 Linear ( Follow Up) 10 0 Month By following up on referrals and calling patients directly, dietitian Nicole Walker found that both she and her patients are getting more out of their appointments. “The high level of bookings missed meant clinical time was being wasted and the waiting list of people who weren’t being seen was growing. “By calling the patient directly, confirming their appointment time, and what they wanted to achieve, the patient felt more in control, better cared for, and also came better prepared to their appointments. “I can tell them exactly what they need to do, whether to create a food diary or bring in any extra information. “I went from having 30 to 40 patients on my waitlist down to zero and patients only waiting two to ten working days for an appointment.” “By creating this relationship the patients feel more obligated to show up and like they already know me, just through one phone call the appointment became far more personalised.” Nicole says that it takes her about 30 minutes to call her patients per week, but she estimates that she’s saving two to three hours a week through the reduction of non-attendances. “If they have any simple enquiries that can be attended to over the phone I can help them on the spot, rather than having them come all the way into the clinic. “It also allows me to discover who physically cannot attend appointments and refer the community dietetic service.” Feedback from patients has been very positive and the system is now being used by the General Outpatient Dietitian in Wellington to contact her urgent patients. “Some people may see it as ‘another thing to do’ and it takes a while to get the hang of, but the results are so good and the relationship with the patients becomes far stronger,” Nicole says. “Hopefully as we progress we could look at other places in the hospital with high DNAs to see if this system could help them.” ‘Leadership Matters’ website launched to support staff Hospital leaders can enjoy some extra support thanks to a new internal website, ‘Leadership Matters’, that was launched this month by HR. The website contains practical advice on essential management processes such as giving and receiving feedback, and the role of leaders in promoting open communication. “Fundamentally, the site is to support and inform leaders to help them work more effectively with their teams”, Mike Hughes, organisational development consultant and team leader, says. “We’re not trying to dictate what managers should do, but instead we want to provide people with some processes, structures and models to support their work.” The website will be updated monthly with documents produced both inhouse and from outside organisations that will be tailored to suit the needs of the 3DHBs and healthcare. “We hope it will aid managers at all levels of the organisation as well as those staff who are moving from technical roles into their first managerial positions, helping them to avoid common pitfalls, as well as providing them with pathways to success.” You can find a link to ‘Leadership Matters’ on the front page of the intranet. If you have any feedback on the website or suggestions for future content you can direct it to leadershipmatters@ccdhb.org.nz. Nicole Walker in her clinic 4 2015 Issue 2 l Health Matters ” Kenepuru Hospital “ Took Deb to Kenepuru Hospital for minor surgery on her hand. Staff were very friendly, a volunteer noticed we were lost and helped. Great place. Kenepuru Hospital ” “ Hello, our family wishes you to know that our 90 plus father had to visit the clinical measurement team on Tuesday 17 Feb. The first contact was with Ash who bent over backwards to get an appointment which suited. Unbelievable manner and kindness shown to us. ED Target statistics 91.4% 7.5 4400 6 We both enjoyed everybody we met and can’t say enough great things about the treatment that was given. We would like you to know that it is much appreciated. Clinical Measurement Unit “ ” My wife was transferred to Wellington hospital from Palmerston North to have an angioplasty. We cannot fault the service and care she received, it certainly instilled my faith in the capabilities and professionalism of Wellington Hospital staff and doctors. ” Interventional Radiology Ward CLOSE performance against 6hr target for February. hours to discharge 95% of ED patients patients presented and completed their care 379 less patients than February last year More patients per day were needed to be discharged within 6 hours to attain the 95% target Staff Profile - Matt Kelly Subregional Infection Specialist Next person was a lovely ECG male Tech - who ever hired this lovely person - take a bow!!!!! He treated my dad with such kindness, respect and dignity, my dad was blown away. While waiting to see the Cardio registrar, dad went on about how happy he was, and what a nice boy he had just seen, and how he had made his day. Then the registrar, he was AWESOME!!! Dad suffers from dementia and this person talked to dad and included him in all conversations. This is a gift sadly lacking in many medical personnel. He even pulled me up when I was trying to explain Pradaxa, as ‘rat poison’. He explained that this could frighten dad to not take the medication that he needs. As we were leaving dad wanted to know when we would be coming back here, as everyone was so nice to him. SUC CE S “ Thank you Kenepuru Hospital. Had a small op there yesterday and the service was great. Pleasantly surprised to receive follow up call from the nurse today – thanks Lynley. S! H -O UH Compliments What is your background in Healthcare? I graduated from Otago University in 2002 and began working as a house surgeon between Wellington, Hutt and Wairarapa. I did this for two years until 2005, when I did some brief work in India at a charity hospital. In 2008 I travelled to Liverpool, where I studied a Diploma in Tropical Medicine. This allowed me to work in Malawi for 15 months. Not long after that I returned to Liverpool where I did my fellowship year, returning to Wellington to finish my training in general medicine and infectious diseases. Could you explain your role as an infectious diseases physician? The position was created in 2013 by Hutt Hospital to provide consistent infectious diseases expertise in the region. The role links in closely with some of the broader aims that are held by the Hutt in the 3DHB project. I am based out of the Hutt but my work is part of the subregional 3DHB infection team. I also spend half a day every week in Wellington working with the Capital and Coast’s Infection Services. Most of my time is spent helping people treat complex infections and working with the infection prevention and control team to prevent healthcare-acquired infection. I also spend my time helping to educate staff on topics such as how to use antibiotics wisely. Wow. That sounds quite full on.… It is but I love how broad the role is. My days are extremely varied and my work spreads across almost every department in the hospital. I have found everyone I’ve worked with to be extremely supportive. What’s your ideal weekend? At the moment? A weekend away from the kids with my wife. Favourite music? Alternative rock like the Killers and Kings of Leon. Favourite movie and why? Braveheart, no explanation needed. 2015 Issue 2 l Health Matters 5 ital p s o h o ered t ebruary, and v i l e d s duate eir graduation in F. a r g e f i h rated t h e DH B Midw s celeb th e se t with t ive en guide w midw placem e ir n e r ow help h u n t o l n il F t just a w g e e b em , “no s sh y h t a s e , k r a o to m ducat the aim t midwives”. idwife e h m it l a w ic y e n lin m, ir journ confide Kath , c e t h u t b , n for the s o g e s in iv e it t w c a x id u grad rd t o ent m g a nd e k forwa com pet o allengin o l h c e ly w e s , bu t xtrem ay.” if ficultie step of the w will be e d r t a u e o y h “This every not wit g them h s a nd in ig t h r o f p o full a n d s up helping A fresh delivery of mi dwife graduates enjoye d a morning tea as they met their new team Vicky’s Book Three and a half years ago, oncology patient Vicki Joy Wal sh couldn’t remember how to put on her shoe. She had no idea this y Da was ’s just the start of a long battle with ildren Hospi celebrates National Ch an aggressive brain cancer known as onal Children’s Day with Nati d ate ebr cel we nth Gliob mo astoma Multiforme (GBM), which s Thi . e of our youngest inpatients som for s bag die goo and e cak can double in size within three to four weeks. has been providing a home Wellington Children’s Hospital r ove t jus injured children for GBM is almost always fatal but her cancer has been away from home for sick and dorm ant since rs. March 2012, and Vicki has since self-published yea 100 a book called ‘Don’t be afraid – The journey is just the begin cared for just over 5000 tal spi Ho n’s ldre Chi ning’ the r , yea Last these kids come from as far outlining her experience from diagnosis. l, pita hos y tiar ter a As n. childre ke’s Bay, to Marlborough in nor th as Taranaki and the Haw CCDHB neurology clinical leader Mr Andrew Park er says the South Island. patients with GBM usually present with headache s, seizures or in charity par tner, the progressive neurological deficits, depending on wher Special thanks also to our ma e the tumour tion and HOSPI for their is growing in the brain. Wellington Hospitals Founda ’ lars dol of nds usa tho of ds suppor t and the many hundre e raised with generous Mr Parker says the long-term aid of therapy is worth of equipment they hav to reduce GBM s. kid our p hel from to what was once a fatal condition to a chronic disea t por community sup se, and allow patients who are frequently young and highl y productive, to get on with their lives. “The fact that Vicki is still alive marks her as spec ial. At the start of her treatment she was just another perfectly ordinary patient, and that’s what’s inspiring. If she can make it, then so can the others who follow.” 6 al Child on Nation s g a b ie d ds o u t g o o Hospital Hospi han Children’s 2015 Issue 2 l Health Matters th rens Day in e for the central Nora Thompson standing with course materials which was region’s new Certificate of Healthcare Capability looks to integrate launched this month. The seven month course y into health the Treat y, Tikanga Māori, and cultural competenc accessible. If you care practices and to make Māori learning more g any further would like to find out how you can join, or are seekin ll@ccdhb.org.nz. information please email katherine.reweti.russe Māori nursing stude n awarded scholarship ts s ps stand i nursing scholarshi Recipients of Māor ea McCance proudly with Andr 27 young Māori nursi ng students were aw arded scholarships to Whitireia’s nursing sc hool from CCDHB las t week. This is the first year th e scholarships have be en awarded since th were created in a pa ey rtnership between th e CCDHB and Whitire Bachelor of Nursing ia’s Maori, aiming to enco urage more Maori to join the health workforce . “Currently Māori ma ke up 13 percent of th e district ’s population only six percent of ou but r nursing staff. These scholarships are a ste stone to creating a he pp ing alth work force more representative of the people that we treat, and improving the he alth of our communitie Andrea McCance, CC s,” DHB’s Director of Nu rsing and Midwifery says. Less hear t s rheum atic fe tops as ver drops The rheum a tic fever pre vention prog a big th ank y ramme wants ou to all DH to extend B staff a s da month h a s s ta relea sed th hown a 14 pe is rcent decrea hospitalisati se in rheum a on in New Z ti c fever ealand since the commen the better p cement of ublic service target in 20 12. a stand d Francesca Au man an e yn Ha lly Ho s Intern pharmacist ote better patient l’s atrium to prom ita sp Ho on gt in ell in W d their safety, as es to medicines an m co it en wh g in macy Week, understand for better care Phar AN PL t’s Le ’s SC part of the HQ 22 - 28 February New ‘Hip’ videos Brave nurses Lesa, Pravina and Kara stand outside ED after shaving their heads for cancer TOP 5 intranet stories for February 1039 views Health Matters Issue 1 666 views Sharpening up on Phlebotomy 542 views New 3DHB MHAIDS launched 413 views Pharmacies provide sharp relief 316 views Busy People Boot Camp A new video series on hip and knee replacement surgery was launched by the Ministry of Health last mont h, aiming to help better prepare patients for surgery. The videos were developed between the Waitemat a DHB and the National Orthopaedic Enhanced Recovery After Sugery team (ERAS), and are now available on both the Ministry’s website and youtube account for publi c access. A key part of ERAS is involving patients in the prepa ration for surgery. If people know what to expect, they are better prepared, recover faster, have fewer complicati ons, and can get out of hospital quicker. Last year there were 407 joint replacement surgeries at Wellington hospital. You can find the videos at www.health.govt.nz. 2015 Issue 2 l Health Matters 7 Immunisation looking sharp I ON mmunisation rates have continued to boom in the Capital and Coast as 97 percent of eight month olds had their primary course of immunisation on time this February. This exceeds the Ministry of Health target of 95 percent. This success has come about thanks to the combination of a highly targeted effort by our PHOs, a focus on seamless communication between healthcare providers, and a shift in the culture around immunisation by hospital staff, says Helen Hartley, CCDHB immunisation facilitator. “One of our major aims has been to see a change in the workforce so that anytime contact is made with a healthcare provider parents are prompted to immunise their child.” “With the development of the National Immunisation Register we have a list of the immunisation status of every child born since 2005. This information is faxed daily to the Children’s wards and a weekly list is sent to Childrens Outpatients department, identifying booked children who are overdue for immunisations.” The National Immunisation Register also communicates and updates information everyday about childrens’ immunisation status to GPs, PHOs, and community outreach providers, as well as maintaining linkages with Plunket and Tamariki providers. Let’s celebrate and pay tribute to those individuals and teams of volunteers who make a difference to New Zealanders’ health. calling for nominations for the 2015 Minister of Health 2015 Minister of Health NomiNaTioNs oPEN volunteer awards Health volunteers make extraordinary contributions, to an extraordinary number of people, in an extraordinary number of ways. These awards celebrate health volunteers from all walks of life and give New Zealanders the opportunity to recognise and celebrate the inspirational commitment of health volunteers. Nominations open 1 March to 31 March 2015 8 Nominate someone today http://volunteerawards.health.govt.nz 2015 Issue 2 l Health Matters Combined with a highly targeted effort by PHOs and outreach providers, the disparity between the immunisation rates of Māori and Pacific people and other ethnic groups has all but disappeared. TARGE T “Historically, PHOs may have sent letters to remind parents about immunising their child only after they had become overdue. Providers are now working in a very proactive way by getting families on board early as an enrolled patient, as well as offering them services such as home immunisation if they cannot make it to a clinic.” Midwives and Lead Maternity Carers are also offered immunisation education opportunities to ensure new parents receive the best information possible. Immunisation Statistics 3379 eight-month olds were immunised at CCDHB in the past year. 96% of eight-month olds were fully immunised in the last three months. This compares to 91 percent of eight month olds immunised in the same period last year. 95% is the immunisation target for eight-month olds this year. With the addition of the 50 immunisation champions working with Occupational Health and Safety Services in our hospital, there are now a number of chances to provide immunisation opportunities to parents. “This means that at every stage of a family’s journey through the hospital they can be reminded to immunise.” “It’s just about everyone chipping in,” says Helen. Volunteer Awards now open N ominations are now open for the 2015 Minister of Health Volunteer Awards. http://volunteerawards.health.govt.nz/ Whether it’s offering a cup of tea to patients in hospital emergency departments, driving cancer patients to appointments, fundraising or simply lending a helping hand and support, the 2015 Minister of Health Volunteer Awards are an opportunity to recognise the many volunteers who generously give their time, skills, experience and care to help others. All nominees receive formal recognition of their contribution. In addition, awards category winners and the overall Health Volunteer(s) of the Year are invited to a special awards presentation where they receive framed certificates. You can nominate someone by completing a nomination form online at Nominations close at 5pm on Tuesday 31 March 2015. The 2015 Minister of Health Volunteer Awards will be presented during National Volunteer Week from 21–27 June 2015, New Zealand’s largest celebration of volunteering. Long Service: Elizabeth Tough Professional and Technical Advisor, Haemotology Hospi Update What are some of the changes you’ve seen? There’s a lot more automation in the lab now, especially in microbiology. I’m glad that I chose haematology because it is still quite hands on. I’ve always enjoyed the more active tasks rather than dealing with numbers. T his month Elizabeth celebrates her 48th year with CCDHB. Elizabeth started her training at Wellington Hospital Pathology Laboratory in 1967 and has been working in the hospital labs specialising in haematology ever since. Why haematology? I’ve always enjoyed the level of attention to detail that it requires, you have to be very observant and able to pick out minute patterns. Dear Debbie... Still enjoying it? Absolutely! Every day there is something new and interesting, a patient who has a different pathology that we haven’t seen before and fascinating diagnoses. Any thoughts of retirement? Not currently, I could retire whenever I want but I still enjoy the work so I see no reason to stop. the ve me an update on Could you please gi Executive? Wellington Hospitals Foundation presented two state of the art ‘Alcotest Units’ costing $7,000.00 each to the Emergency Department. These Units will enable quick, safe and repeatable testing of intoxicated patients presenting to Wellington Hospital’s Emergency Department, and are believed to be a first for a New Zealand hospital. Chief recruitment of our Tony Hi Tony, New Tool to Assess Intoxicated Patients the Interim a half I have been d an ar ye st pa e th for e Board As you are aware, b-committee of th su a ar ye st La B. r CCDH Chief Executive fo a permanent Chief Executive on w ne a t ui cr re to was established n this month. t advertising bega en tm ui cr re d an ct . However, three year contra expires this month on siti po rim te in e e Board The contract for th beyond this date th go to y el lik is s es t proc the as the recruitmen on. This will ensure siti po CE rim te in current have extended the chief executive until a permanent th pa t en rr cu its DHB continues on Have You Seen HOSPI’s Pawprints? Special HOSPI pawprint paths to help patients and vistiors find their way to Wellington Children’s Hospital lead from the Hospital Atrium, Emergency Department and Theatre. The pawprint paths include Hospi graphics in varying states of adventure (parachuting, skateboarding and riding a penny farthing bicycle). is appointed. Kind regards, Debbie 2015 Issue 2 l Health Matters 9 antibiotic of the month: Rifampicin R ifampicin should always be prescribed in combination with another antibiotic as rifampicin resistance develops quickly. Is used for the treatment of tuberculosis and other serious staphylococcal infections. Has a role in the treatment of implant infections as it is one the limited number of antibiotics with greater activity against bacteria in biofilms. Has great oral bioavailability. IV = ORAL – only use the intravenous route if the oral route is unavailable. Achieves extensive distribution into tissues and bodily fluids including urine, tears, sweat and aqueous humor, resulting in an orange-red discolouration of these body fluids. Pre-warn your patients! Is generally well tolerated. The most common side effects are GI upset and cutaneous reactions such as flushing or mild skin rash that are usually mild and self-limiting. Can result in elevation of serum hepatic transaminase levels which is often self-limiting. In rare cases severe hepatitis can occur requiring discontinuation. For this reason close monitoring of liver function tests is recommended during the first 2 months of therapy. Is a potent CYP3A4 inducer and therefore can increase the metabolism of other drugs that are metabolised by this pathway, leading to sub-therapeutic levels of these drugs. Examples include warfarin, oral contraceptive pill, corticosteroids, methadone and many other drugs. Close clinical monitoring, therapeutic drug monitoring, and selection of an alternative drug maybe required. If you are unsure if a drug interaction exist then check with your ward pharmacist. Is a restricted antibiotic on the Hospital Medicines List. Respiratory or Infectious Diseases/Microbiology approval required. This information is brought to you by the CCDHB Antimicrobial Stewardship Committee. If you have questions or concerns about antibiotic use, please contact: Dr Mark Jones, Clinical Microbiologist (#6574) Dr Nigel Raymond, Infectious Diseases Physician (#6406) Dr Matthew Kelly, Infectious Diseases Physician (Hutt Hospital) Brijul Morar, Infectious Diseases pharmacist (#6114) Royal farewell for Vicky Noble A room packed full of staff from across the hospital shed a few tears saying goodbye to Vicky Noble last month, as she was inundated with gifts and gratitude. Speakers praised Vicky for her approachability, leadership, advocacy, and strong sense of ethics in her position as the Director of Primary and Integrated Care Nursing over the past six years. 10 2015 Issue 2 l Health Matters Māori, Pacific and disability services spoke strongly of the positive impact that Vicky’s work had on primary care nursing and the community. Her work has been widely appreciated across the sub region thanks to collaborations with the Hutt and Wairarapa DHBs and outside organisations including Plunket, Work and Income, and many youth outreach programmes. “I’m so proud to have worked for both SIDU and Capital and Coast, we’ve been through a huge amount as a team”, Vicky says, “Every day presents the most extraordinary opportunities to improve our health care services and I feel it has been a huge privilege to have been in my position”. Vicky will be travelling to join her husband who is currently working in Myanmar. ! r a t S a e r ’ You 5 years Helen Meehan, Radiation Therapist Clare Couch, Clinical Psychologist Jethro Donaldson, Medical Physics Registrar Katherine Lynch, Midwife Grace Gorte, Ward 20 Nurse Sally Jackson, Genetic Associate Sophie Harley, Staff Nurse Patricia Cederwall, Administration Clerk Alaine Over, Medical Typist Brendan Young, Dental Surgeon Noel Mason, Purehurehu Cara Jones, Ward 19 Nurse Shiji George, Registered Nurse Adaline Tohill, Consumer Council Shona Urquhart, Occupational Health Nurse Catherine Birch, Staff Nurse Julie Kyle, NICU Karen Barns, Staff Nurse Clive Cameron, Hospital Advisory Committee Robyn Hughes, Hospital Advisory Committee Kevin McDermott, Inwards Goods Christian Kalderimis, Advisory Committee Elizabeth Solomona, Consumer Council Sisilia Peini, Rangipapa Nurse January Almendras, Renal Dialysis Unit Susan Corin, NICU Nurse Peter Rintoul, Plumber Workshops Lynne Cowley, Ward 18 Nurse Kerry Thornbury, Hospital Advisory Committee Rachel Reynolds, ICU Nurse 30+ years Heta Makiri, Kaiawhina Coordinator Sesilia Antonio, Laundry Worker Miria Kapene, Laundry Worker Judith Spooner, Midwife Special Thanks and Recognition The CCDHB would like to give a big thanks to those staff members who have reached a milestone 5, 10, 15, 20 or more years with the hospital this month. 10 years Ruth Ferrer, Ward 5 Nurse Penelope Flaws, Clinical Coordinator Shannon Unka, NICU Nurse Rebecca Mellish, Board Member Anita O’Boyle, Midwife Educator Louisa Fruean, Community Nurse Patrician Martin, Charge Nurse Manager Tonie Ikivihi, Community Mental Health Nurse Catherine Young, Mental Health Nurse Katherine Neas, Clinical Geneticist Rose Toomaga, Health Care Associate Arthur Skelton, Mental Health Support Worker Patricia Janes, Scientific Officer Valerie Spooner, Speech Therapist Briar Coleman, Senior Anaesthetic Technician Isabella Sciascia-Visani, Scientific Officer Penelope Wyatt, Clinical Midwife Specialist 15 years Dayantha Sananayake, Sterile Services Technician Michael Daly, Social Worker Agadha Wickremesekera, Neuro Surgeon Cheowleen NG, Registered Nurse Kathleen Knowles, Duty Nurse Manager Susan Black, Charge Nurse Manager Cho Kho, Registered Nurse Lynette Stewart, Charge Nurse Manager Robert Nielsen, Community Nurse Donna Hesp, Staff Nurse Katrina Bootsma, NICU Nurse Patricia Henaghan, ICU Nurse Colleen Peel, Community Nurse Manager Fafili Levave, Mental Health Support Worker 20 years Victoria Conwell, Staff Nurse Outpatients Wynona Elliot, Theatre Support Assistant Janet Dunbar, Nurse Clinician Joanne Gibbons, Community Nurse Marilyn Gibson, NICU Denise Braid, Charge Nurse Manager Donna Bresaz, After Hours Coordinator Janice Lucas, Pathway Nurse Coordinator Hilika Lefao, Laundry Worker Devi Morar, Laundry Worker Jennifer Wickens, Community Nurse Fiona Mellars, Clinical Nurse Specialist Gilian Hawke, Senior Consultant Clinical Psychologist 25 years Lynne Turkington, Medical Records Coordinator Rosaline Ahmed, Healthcare Assistant Shelley James, Charge Midwife Manager Lorna Jennings, Registered Nurse Joy Herbert, Clerical Assistant Duncan McPhail, Senior Anaesthetic Technician Rosemary Escott, ICU Charge Nurse Manager Gerrigje Nicholls, Charge Nurse Manager Alan Vekula, Warehouse Supervisor Elizabeth Tough, Haematology Technical Specialist 2015 Issue 2 l Health Matters 11 A Day in the Life: Mortuary Technicians M ortuary technician David Walker says people react in different ways when he tells them what he does for a living. “Sometimes they excuse themselves and don’t want to know about it, or they become completely fascinated by it and start asking lots of questions.” As technical head, he works with three other mortuary technicians at Wellington Hospital - Monday to Friday from 8am to 5pm. The team also operate an on-call roster for all hospital and coronial afterhours viewings and autopsies. Crime shows like CSI, while lifting the profile of forensic pathology, are predictably unrealistic, says David. “TV CSI investigators examine the deceased with a scanner of some sort, determining that the person died, for example, of heart failure. If anyone’s got one of those machines please send it to us – it’d make our job a lot easier!” In reality, mortuary technicians assist forensic pathologists at the time of autopsy by making the initial incisions and removing the organs for the pathologist to inspect. A mortuary technician’s role is similar to a theatre assistant’s, says Tim Reen. “Other health professionals are often amazed at the extent of our practical skills when it comes to removing organs and reconstructing bodies.” The team also provide the hospital’s ‘return to patient service’, returning tissue samples to live patients or deceased patients’ families if requested for cultural or other reasons. Undeniably the ability to deal with Mortuary technicians Rachel Kinnaird, Maari Gray, David Walker, and Tim Reen “raw emotion” is equally important as the clinical skill, because mortuary technicians arrange viewings with families and explain the autopsy process and the coroner’s involvement, if necessary. The first 10 – 15 minute discussion with families is an important opportunity for the team to discuss the processes involved and hopefully make it easier in some small way for them, David says. Being mindful of the fact that the people they deal with have families and are connected emotionally to their relatives provides some context to what is essentially a clinical role, Maari Gray says. “When you know family are very much involved, a human element infuses to the clinical side. We’re a multi-cultural society and are often requested to adapt to different ways of doing things. Ours is a constantly evolving knowledge base.” Maari says working with families and whānau acknowledges that death is about the living, and breaks down the Life should n ot be a journ ey to the gra intention of a ve with the rriving safely in preserved bo a pretty and dy, but rathe well r to skid in b a cloud of sm roadside in oke, thoroug h ly used up, tota out, and loud lly worn ly proclaimin g “Wow! Wh at a Ride!” Hunter S. T h om pson 12 2015 Issue 2 l Health Matters FACT FILE Wellington Hospital’s mortuary cares for an average of 550 hospital deaths per year, and an average of 400 people who have died in the community and require an autopsy. Mortuary positions are few and far between – there are only around 30 in New Zealand. It is not necessary to notify mortuary staff of a death in hospital unless family are wishing to arrange a viewing in the Bereavement Suites (Ngaio and Rata). separation between “us over here and the family over there”. “We are neither ghoulish or CSI lookalikes and want to break down old and new preconceived ideas about the mortuary and those who work within it.” It is a select profession and two years of training takes place on the job prior to gaining eligibility to sit the qualifying exam. A background in science, nursing, or funeral directing is helpful but not essential, David says. At the end of the day, the team are here to support each other. Rachel Kinnaird says it’s a job that requires a strong stomach, but “you have to care about people and see them as you would your own family”.
© Copyright 2025