
Concurrent Vismodegib and Radiotherapy for
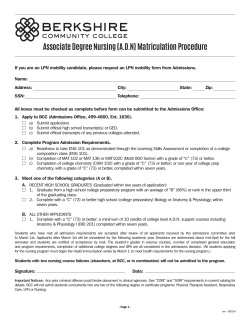
Research Case Report/Case Series Concurrent Vismodegib and Radiotherapy for Recurrent, Advanced Basal Cell Carcinoma Erqi L. Pollom, MD; Timothy T. Bui, BS; Anne Lynn S. Chang, MD; A. Dimitrios Colevas, MD; Wendy Y. Hara, MD Editorial IMPORTANCE Vismodegib is a targeted agent recently approved for treating patients who develop recurrent or locally advanced basal cell carcinoma (BCC), and will inevitably be integrated into existing therapy for advanced BCC as it becomes increasingly used. Improved understanding of how vismodegib interacts with other treatment modalities, including radiotherapy, would help optimize multidisciplinary therapy and clinical outcomes. OBSERVATIONS We report 2 cases of recurrent, advanced BCC treated from April 1, 2012, through October 31, 2014, with concurrent radiotherapy and vismodegib. Concurrent treatment appeared to be well tolerated and efficacious, with both patients having no evidence of progressive disease at last follow-up. CONCLUSIONS AND RELEVANCE We found that the combination of vismodegib and radiotherapy is feasible for patients with recurrent or locally advanced BCC and that combined use of currently available therapies for advanced BCC warrants further prospective study. JAMA Dermatol. doi:10.1001/jamadermatol.2015.0326 Published online April 15, 2015. A lthough surgical resection is curative in most patients with basal cell carcinoma (BCC), recurrent or more advanced disease may be treated with a combination of surgery and radiation.1 Cisplatin is sometimes used for patients with metastatic BCC,2 but no systemic therapy was approved for the treatment of BCC until recently with the advent of vismodegib. Response rates to systemic vismodegib were 30% and 43% for patients with metastatic and locally advanced BCC, respectively, with a median duration of response of 7.6 months.3 As vismodegib becomes increasingly used, it will be important to address how to best integrate this new agent into existing therapy for advanced BCC. Improved understanding of how vismodegib interacts with radiation in this disease would help determine the optimal timing and sequencing of these various treatment modalities to enhance response rate and progression-free survival. Only one case of radiotherapy with vismodegib has previously been reported for the treatment of squamous cell carcinoma.4 We report the treatment of 2 cases of recurrent head and neck BCC using this novel combination of vismodegib and concurrent radiotherapy. Report of Cases With institutional review board approval of Stanford University, a search of patients who received vismodegib and concurrent radiotherapy was conducted. Two patients were idenjamadermatology.com Author Affiliations: Department of Radiation Oncology, Stanford University School of Medicine, Stanford, California (Pollom, Bui, Hara); Department of Dermatology, Stanford University School of Medicine, Stanford, California (Chang); Department of Medicine (Oncology), Stanford University School of Medicine, Stanford, California (Colevas). Corresponding Author: Wendy Y. Hara, MD, Department of Radiation Oncology, Stanford University School of Medicine, 875 Blake Wilbur Dr, Mail Code 5847, Stanford, CA 943055847 (wendy.hara@stanford.edu). tified as having been treated with visomodegib and concurrent radiotherapy from April 1, 2012, through October 31, 2014. Treatment-related toxic effects were classified according to the Common Terminology Criteria for Adverse Events. Case 1 A man in his 60s presented with a left nasal tip BCC that was initially treated with Mohs surgery. Although this lesion had received no prior treatment and his surgery revealed no aggressive features, he developed pain and numbness 10 months later in the V2 distribution of the left cranial nerve and was initially medically managed for trigeminal neuralgia. However, his symptoms progressed during the next 3.5 years. He was ultimately evaluated and found to have left cranial nerve V1 to V3, VI, and VII palsies on examination. Concern was raised for perineural spread of the tumor that involved left cranial nerve V1 to V3, VI, and VII and the left cavernous sinus on skull base magnetic resonance imaging (MRI). Biopsy of the left V2 nerve confirmed BCC with perineural invasion. Positron emission tomography–computed tomography revealed no distant disease. He was prescribed vismodegib, 150 mg/d, with concurrent radiotherapy. The clinical area of the disease, which included the left infraorbital nerve, left cranial nerves V2, V3, and VII (including greater superficial petrosal and auriculotemporal nerve), left Meckel cave, and cavernous sinus, was treated with 66 Gy in 33 fractions. The left infratemporal fossa and parotid were treated with 50 Gy in 33 fractions. Volumetric modulated arc technique with image guidance and 6-MV (Reprinted) JAMA Dermatology Published online April 15, 2015 Copyright 2015 American Medical Association. All rights reserved. Downloaded From: http://archderm.jamanetwork.com/ by a STANFORD Univ Med Center User on 04/23/2015 E1 Research Case Report/Case Series Vismodegib and Radiation for Advanced Basal Cell Carcinoma Figure 1. Pretreatment and Posttreatment Magnetic Resonance Imaging (MRI), Pretreatment Positron Emission Tomography (PET), and Radiotherapy Plan for Patient 1 A B C D E F A, Pretreatment PET showing increased uptake in the left infraorbital foramen (white arrow). B, Pretreatment T1 postcontrast MRI showing enhancement of the left cranial nerve V3 through the foramen ovale in a coronal section of the skull base (white arrow). C, Pretreatment T1 postcontrast MRI showing enhancement of the prepontine cistern component of left cranial nerves VI (white arrow) and V (red arrow) in an axial section of the skull base. D, Radiotherapy plan with 66-Gy (magenta), 60-Gy (blue), and 40-Gy (cyan) isodose lines. E, Posttreatment T1 postcontrast MRI showing stable to decreased enhancement of left cranial nerve V3 in a coronal section of the skull base. F, Posttreatment T1 postcontrast MRI showing stable to decreased enhancement of left cranial nerves V and VI in an axial section of the skull base. photons were used. The patient developed grade 1 dermatitis and grade 1 mucositis during radiotherapy but was able to complete the full course of treatment without any breaks, and his pain improved by midtreatment. He continued to take vismodegib for an additional 3 months after radiotherapy but stopped taking it because of taste changes, loss of appetite, muscle cramping, and fatigue. With a follow-up of 9 months, including MRI every 3 months, he had stable disease apparent on imaging, had improvement in his left facial weakness, and continued to be pain free (Figure 1). degib, 150 mg/d, to try to shrink the lesion before resection. After 2 months of vismodegib therapy, the patient underwent an MRI of the orbit, which again revealed a left lateral orbital lesion, which measured 6.3 × 5.6 mm. He underwent a left globe-sparing resection with positive margins, followed by adjuvant radiotherapy, while continuing to take vismodegib. The radiotherapy target volume, which encompassed the postoperative bed at the left lateral orbit, was treated to a total dose of 51 Gy in 17 fractions using mixed 6-MeV and 9-MeV electrons. This radiotherapy schedule was chosen after discussion with the patient and consideration of his social and transportation issues. He developed grade 1 dermatitis in the radiation field during his radiotherapy. He stopped taking vismodegib 2 weeks after completion of radiotherapy because of increased fatigue, weight loss, and shortness of breath. With a follow-up of 12 months, including posttreatment MRI and regular ophthalmologic evaluations, he continues to be disease free, with dry eye managed by eye drops as his only radiation-associated toxic effect. The left globe and lacrimal gland received mean doses of 12.5 and 22.3 Gy, respectively. Before Case 2 A man in his 70s presented with a left lower eyelid and lateral canthal BCC that was initially treated with Mohs surgery. Three years later, he developed diplopia and a new mass over the left lateral canthus at the site of his previous left lower lid reconstruction. Computed tomography of the orbit revealed thickening that measured 6.5 × 7.4 mm in the region of the left lower eyelid and lateral canthus, and left orbital biopsy revealed infiltrative BCC. The patient opted for treatment with vismoE2 JAMA Dermatology Published online April 15, 2015 (Reprinted) Copyright 2015 American Medical Association. All rights reserved. Downloaded From: http://archderm.jamanetwork.com/ by a STANFORD Univ Med Center User on 04/23/2015 jamadermatology.com Vismodegib and Radiation for Advanced Basal Cell Carcinoma Case Report/Case Series Research Figure 2. Pretreatment and Posttreatment Magnetic Resonance Imaging (MRI) and Radiotherapy Plan for Patient 2 A B C A, Pretreatment T1 postcontrast MRI showing left lateral orbital recurrence (white arrow) in an axial section of the skull base. B, Radiotherapy plan with 51-Gy (red), 40-Gy (blue), 20-Gy (magenta), and 10-Gy (green) isodose lines. C, Corresponding posttreatment axial section of the skull base (white arrow) at 8 months after radiotherapy completion. radiation, his left eye vision without correction was 20/60 (right eye vision, 20/20). At last follow-up, his vision was 20/100 in the left eye without correction (right eye vision, 20/40). Figure 2 shows pretreatment and posttreatment imaging and a radiotherapy plan. vitro, it enhanced radiosensitivity in their in vivo non–small cell lung cancer models, suggesting that this effect may be mediated through paracrine stromal signaling. Although vismodegib’s potential for radiosensitization and synergistic efficacy with radiotherapy is promising, there is also concern for potential synergistic toxic effects. There is scarce clinical experience to guide us on using vismodegib with concurrent radiotherapy for BCC. There has been one case report of a patient who was taking vismodegib for BCC and then developed left parietal and left zygomatic squamous cell carcinomas, which were successfully treated with radiotherapy while continuing vismodegib treatment.4 We are the first, to our knowledge, to report the treatment of BCC using concurrent radiotherapy and vismodegib. Concurrent treatment appeared to be well tolerated and efficacious, with both patients having no evidence of progressive disease at last follow-up, despite discontinuing vismodegib treatment because of adverse effects and not using any subsequent therapy. Even though proximity to normal structures can limit the use of radiotherapy in advanced BCC, both patients completed radiotherapy without significant adverse effects. Discussion Vismodegib, an exciting advance in the treatment of advanced BCC, with 30% to 60% objective responses reported,3,5-7 is effective for patients with metastatic or locally advanced BCC who are not candidates for or who have had disease recurrence after surgery and/or radiation therapy. However, there are limitations to this drug because treatment duration can be limited by adverse effects, including muscle spasms, alopecia, dysgeusia, weight loss, and fatigue. Acquired resistance to Hedgehog pathway inhibition after initial response is also an increasing concern.8 In addition, cases of vismodegib-associated squamous cell carcinoma within and distant to BCC have been reported.9-11 There has been great interest in expanding the use of vismodegib and using it not just as monotherapy but as an adjunct to existing treatments. Vismodegib therapy is being explored in the neoadjuvant setting in an attempt to reduce tumor volumes to facilitate resection12,13 or radiotherapy and even in the concurrent setting with radiotherapy.14 The interaction between radiotherapy and Hedgehog pathway inhibition has not been well studied, but available preclinical data support combining vismodegib with radiotherapy. Stimulation of Hedgehog signaling has been reported to reduce radiosensitivity in hepatocellular carcinoma,15 and inhibition of Hedgehog signaling in an esophageal cancer cell line was reported to increase radiosensitivity.16 Zeng et al17 found that although Hedgehog pathway inhibition did not alter radiosensitivity in ARTICLE INFORMATION Accepted for Publication: February 4, 2014. jamadermatology.com Conclusions It can be difficult to determine optimal therapy for this heterogeneous and complex patient population with advanced BCC. Treatment should continue to be multidisciplinary, with consideration of local and systemic therapy, so that this patient population with a poor prognosis can be treated aggressively. We found that the combination of vismodegib and radiotherapy is feasible for these patients, and combined use of currently available therapies for advanced BCC warrants further prospective study. Published Online: April 15, 2015. doi:10.1001/jamadermatol.2015.0326. Author Contributions: Drs Pollom and Hara had full access to all the data in the study and take (Reprinted) JAMA Dermatology Published online April 15, 2015 Copyright 2015 American Medical Association. All rights reserved. Downloaded From: http://archderm.jamanetwork.com/ by a STANFORD Univ Med Center User on 04/23/2015 E3 Research Case Report/Case Series Vismodegib and Radiation for Advanced Basal Cell Carcinoma responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Pollom, Colevas, Hara. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Pollom, Hara. Critical revision of the manuscript for important intellectual content: Bui, Chang, Colevas, Hara. Administrative, technical, or material support: Bui. Study supervision: Pollom, Chang, Colevas, Hara. Conflict of Interest Disclosures: None reported. REFERENCES 1. Mendenhall WM, Amdur RJ, Hinerman RW, Cognetta AB, Mendenhall NP. Radiotherapy for cutaneous squamous and basal cell carcinomas of the head and neck. Laryngoscope. 2009;119(10): 1994-1999. 2. Moeholt K, Aagaard H, Pfeiffer P, Hansen O. Platinum-based cytotoxic therapy in basal cell carcinoma: a review of the literature. Acta Oncol. 1996;35(6):677-682. 3. Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366(23):2171-2179. 4. Gathings RM, Orscheln CS, Huang WW. Compassionate use of vismodegib and adjuvant radiotherapy in the treatment of multiple locally advanced and inoperable basal cell carcinomas and squamous cell carcinomas of the skin. J Am Acad Dermatol. 2014;70(4):e88-e89. E4 5. Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361(12): 1164-1172. 6. Chang AL, Solomon JA, Hainsworth JD, et al. Expanded access study of patients with advanced basal cell carcinoma treated with the Hedgehog pathway inhibitor, vismodegib. J Am Acad Dermatol. 2014;70(1):60-69. 7. LoRusso PM, Rudin CM, Reddy JC, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res. 2011;17(8):2502-2511. 8. Rudin CM, Hann CL, Laterra J, et al. Treatment of medulloblastoma with hedgehog pathway inhibitor GDC-0449. N Engl J Med. 2009;361(12):1173-1178. 9. Zhu GA, Sundram U, Chang AL. Two different scenarios of squamous cell carcinoma within advanced basal cell carcinomas: cases illustrating the importance of serial biopsy during vismodegib usage. JAMA Dermatol. 2014;150(9):970-973. 10. Iarrobino A, Messina JL, Kudchadkar R, Sondak VK. Emergence of a squamous cell carcinoma phenotype following treatment of metastatic basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2013;69(1):e33-e34. 11. Orouji A, Goerdt S, Utikal J, Leverkus M. Multiple highly and moderately differentiated squamous cell carcinomas of the skin during vismodegib treatment of inoperable basal cell carcinoma. Br J Dermatol. 2014;171(2):431-433. 12. ClinicalTrials.gov. Vismodegib for Treatment of Basal Cell Carcinoma. NCT01543581. https://www .clinicaltrials.gov/ct2/show/NCT01543581. Accessed February 25, 2015. 13. ClinicalTrials.gov. A Study Evaluating the Efficacy and Safety of Vismodegib (GDC-0449) in Operable Basal Cell Carcinoma. NCT01201915. https://www .clinicaltrials.gov/ct2/show/NCT01201915. Accessed February 25, 2015. 14. ClinicalTrials.gov. NCT01835626. Phase II Study of Radiation Therapy and Vismodegib for Advanced Head/Neck Basal Cell Carcinoma. https://www .clinicaltrials.gov/ct2/show/NCT01835626. Accessed February 25, 2015. 15. Chen YJ, Lin CP, Hsu ML, Shieh HR, Chao NK, Chao KS. Sonic hedgehog signaling protects human hepatocellular carcinoma cells against ionizing radiation in an autocrine manner. Int J Radiat Oncol Biol Phys. 2011;80(3):851-859. 16. Sims-Mourtada J, Izzo JG, Apisarnthanarax S, et al. Hedgehog: an attribute to tumor regrowth after chemoradiotherapy and a target to improve radiation response. Clin Cancer Res. 2006;12(21): 6565-6572. 17. Zeng J, Aziz K, Chettiar ST, et al. Hedgehog pathway inhibition radiosensitizes non-small cell lung cancers. Int J Radiat Oncol Biol Phys. 2013;86 (1):143-149. JAMA Dermatology Published online April 15, 2015 (Reprinted) Copyright 2015 American Medical Association. All rights reserved. Downloaded From: http://archderm.jamanetwork.com/ by a STANFORD Univ Med Center User on 04/23/2015 jamadermatology.com
© Copyright 2025







![[ PDF ] - journal of evidence based medicine and](http://cdn1.abcdocz.com/store/data/000719962_1-eaaa1bfa1486ae0102724ca68b7dd1e4-250x500.png)
