Oncology & Haematology Conference Handbook
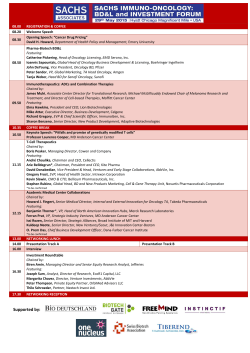
Oncology & Haematology Conference 2015 CONFERENCE HANDBOOK Friday 20 and Saturday 21 March 2015 Ko Awatea, Middlemore Hospital Campus, Auckland Proudly supported by: ACKNOWLEDGMENTS The Organising Committee would like to extend their gratitude to all the sponsors and exhibitors without whom this conference would not have been possible. Please take the time to visit all the exhibition stands to say hello, see what’s new, and complete the quiz competition to win an iPad Mini. In particular we acknowledge the following sponsors: Platinum Gold International Speaker Bronze 2 Oncology & Haematology Conference 2015 CONTENTS Welcome4 General Information 5 Social Programme 7 Keynote Speaker 8 Invited Speakers 9 Programme Friday 11 Saturday 14 Abstracts Oral 16 Exhibition Floor Plan 36 Exhibitor Directory 37 Exhibitor Information 38 Middlemore Campus Map Inside Back Page Venue Floor Plan Back page ORGANISING COMMITTEE Convenor Angela Knox, Clinical Nurse Manager, Haematology Day Ward, Middlemore Hospital Committee: Ella Liang, Nurse, Haematology Day Ward, Middlemore Hospital Janene Lawrence, Clinical Nurse Manager, Counties Manukau DHB Kathryn McWatt, Nurse Educator, Counties Manukau Health Hannah Milner, Nurse, Haematology Day Ward, Middlemore Hospital Anne-Marie Wilkins, Lead Cancer Nurse Coordinator, Middlemore Hospital CONFERENCE ORGANISERS ForumPoint2 Limited PO Box 1008, WMC Hamilton 3240 Contact: Paula Armstrong | Project Manager T: +64 7 838 1098 E: Paula@fp2.co.nz www.fp2.co.nz Oncology & Haematology Conference 2015 3 WELCOME On behalf of the organising committee, we warmly welcome you to Ko Awatea, Counties Manuaku and the 2015 NZNO Cancer Nurses: Oncology and Haematology Conference. We are sure you will enjoy the range of high quality national and international speakers throughout this programme. It is with great regret that Shelly Dolan is unable to be with us in person, but luckily through technology, she will be able to present and be available for an interactive session on Saturday. I would also encourage you to make the most of visiting the exhibitors, without their support, conferences such as this would not be possible. I hope you enjoy yourself, both at the social event and also in networking and catching up with old friends and making new ones. ORGANISING COMMITTEE Convenor Angela Knox 4 Oncology & Haematology Conference 2015 GENERAL INFORMATION REGISTRATION AND INFORMATION DESK The registration desk is staffed by Paula and Claire who welcome your enquiries on any conference detail or local information. The desk will be open on Friday 20 March from 8.00am. Useful Telephone Numbers Registration Desk Staff: Paula Tel: 027 649 2081 Ko Awatea Holiday Inn Auckland Airport Auckland Coop Taxis Super Shuttle Tel: (09) 267 0044 Tel: 0800 080 236 or (09) 275 1059 Tel: (09) 300 3000 Tel: 0800 748 885 or (09) 522 5100 from a mobile ATTENDEE LIST There is a list of attendees in your conference bag. CERTIFICATE OF ATTENDANCE A certificate of attendance can be found inside your registration envelope. EVALUATION An online evaluation survey will be emailed to attendees after the conference. We welcome your feedback and would be grateful for a few minutes of your time to complete this. INSURANCE Registration fees do not include personal, travel or health insurance of any kind. Neither the NZNO Cancer Nurses College nor ForumPoint2 Limited takes responsibility for delegates failing to take out adequate insurance cover. INTERNET ACCESS Complimentary Wifi access is available to conference delegates; Login information will be posted on the main lecture room screen and by the conference registration desk. The password will change daily. If you have difficulty logging on, please see the ForumPoint2 team at the conference registration desk. MESSAGES For anyone wishing to leave you a message during conference hours, please ask them to use the following number for the registration desk. Registration desk: 027 649 2081 MOBILE PHONES During conference sessions mobile phones must be set to silent or vibrate. We ask that mobile phones are not used while sessions are in progress. Oncology & Haematology Conference 2015 5 NAME BADGES All conference attendees and industry representatives are asked to wear their name badges at all times during the conference and social functions. It is your official entrance pass to the sessions, catering and exhibition. Please return your name badge and plastic registration envelope to the conference registration desk at the end of the conference for recycling. PARKING Paid parking is available in Car Park 4 via Gate 1 on Hospital Road. There is a limited amount of carparks in this area and is based on a first in scenario. PRESENTERS’ INFORMATION Oral presentations Presentations are being loaded in the room in which the speaker is presenting. Please go to load and check your presentation as soon as possible after your arrival at the conference. If you plan to present using your own laptop please speak to the technician on your arrival at the meeting. Please be in the conference room where you are presenting ten minutes before the start of the session to check your presentation, familiarise yourself with the AV set-up and meet the session chair. POWERPOINT PRESENTATIONS Where presenters have approved, PowerPoint presentations will be saved and posted to www.nzno.org.nz/groups/colleges/cancer_nurses_college following the conference. SESSIONS CHAIRS Ten minutes prior to your session commencing, please be in the conference room to meet the presenters. Please ensure each session starts and finishes at the advertised time. SPECIAL DIETS If you have advised us of any special dietary requirements on your registration form these have been notified to the caterers. There will be a “pre-ordered special dietary requirement” table located in Room 103 in the catering area for notified special diets. Please make yourself known to the catering staff at the conference dinner. If you have difficultly locating your appropriate meal options please contact the ForumPoint2 team at the conference registration desk. WATER REFILL STATION A kitchen area is located behind Wishbone café, there is a filtered water tap here for you to refill your water bottles. DISCLAIMER OF LIABILITY Whilst we have endeavoured to ensure that information on the conference website and printed material is accurate, details may be subject to change without notice. Any corrections or amendments will be notified as soon as possible. In the event of industrial disruptions, or service provider failures, the NZNO Cancer Nurses College nor ForumPoint2 Limited will not accept any responsibility for losses incurred by attendees or their partners. Although care has been taken to ensure accuracy, the conference committee does not accept liability for any errors in published abstracts. 6 Oncology & Haematology Conference 2015 Bus transfer schedule There will be two buses transferring delegates at the times stated below. The buses will depart, once full, promptly at the times stated below. Please ensure you are in the departure location at least five minutes prior to the time stated below. Date Departure time From To Friday 20 March 7.45am Holiday Inn Auckland Airport Ko Awatea, Middlemore Hospital Campus Friday 20 March 4.45pm Ko Awatea, Middlemore Hospital Campus Holiday Inn Auckland Airport Saturday 21 March 6.45am Holiday Inn Auckland Airport Ko Awatea, Middlemore Hospital Campus Saturday 21 March 2.45pm Ko Awatea, Middlemore Hospital Campus Holiday Inn Auckland Airport SOCIAL PROGRAMME Conference Dinner Friday 20 March 2015 7.00pm to midnight Venue: Jean Batten Ballroom, Holiday Inn Auckland Airport, Auckland Dress/Theme: The Roaring 20’s Your ticket includes your meal, a drink on arrival and entertainment. A cash bar will be operating, please bring cash, eftpos or credit card to purchase additional beverages. Entertainment: Get ready to dance the evening away to the fabulous sounds of The Shy and Retiring Company. Important Please take your ticket with you to the dinner (inside your name badge pocket), these will be collected. If you have a ticket for the dinner, but will no longer be attending, please advise the ForumPoint2 team at the conference registration desk. Oncology & Haematology Conference 2015 7 KEYNOTE SPEAKERS Dr Shelley Dolan Shelley worked in Critical Care until 1990 exploring specialities such as Trauma, Burns and Plastics, Coronary Care, Children’s ITU, neonatal ITU and General ITU in major units across the UK. Then in 1990, Shelley made a move to the critical care of the cancer patient. In 2000 Shelley was appointed as the Royal Marsden Nurse Consultant for Cancer: Critical Care. Finally, in June 2007 Shelley was delighted to be appointed as Chief Nurse of The Royal Marsden NHS Foundation Trust. As Chief Nurse, Shelley leads the nursing professionals at the Trust and is also the Board lead for clinical governance across all professional groups. In December 2012, Shelley was appointed as Clinical Director for The London Cancer Alliance an NHS body seeking to raise safety and quality for patients with cancer in 17 hospitals across London. Shelley’s first degree was in English, in 1996 she completed her MSc in cancer care and advanced practice, and in her Doctoral thesis sought to improve the early diagnosis of sepsis in people with cancer. Shelley lectures and teaches widely across the UK and internationally. Her most recent research studies have been in the fields of empowering the cancer patient at home through education and technology, the involvement of the patient in research, follow-up, ITU and the early identification of patients with sepsis. In 2009, Shelley was appointed to the clinical reference group for the Competition and Cooperation panel for the NHS. Shelley is also the Chair of the London Chelsea Research Ethics Committee. Shelley has published widely with her writing concentrating in the main on the person with cancer who is acutely or critically ill. Over the last 4 -5 years Shelley has also written and presented work on clinical leadership and nursing’s influence on cancer and healthcare policy development, nationally and internationally. Julie Cairns Julie is a NZRN who trained at Palmerston North Hospital. Julie has spent most of her professional life working in cancer nursing and senior management roles in Melbourne, Australia. From 2010 – 2014 Julie returned to New Zealand and worked in Auckland. During 2013 she was employed by the Ministry of Health, Cancer Program, to develop the Knowledge and Skills Framework for Cancer Nursing. In 2014 Julie returned to Melbourne to take up the role of General Manager, Ambulatory Cancer Services at the Olivia Newton John Cancer Wellness Centre at Austin Health. 8 Oncology & Haematology Conference 2015 Contributing Speakers Henry Chan, Laboratory Haematology Registrar, Auckland Anne Fraser, Oncology Nurse Practitioner, Blood and Cancer Service, Auckland Natalie James, National Cancer Lead, Cancer Nurse Coordinator Initiative Barry Keane, Nurse Director, Central Cancer Network Douglas Ormrod, Programme Manager, Genesis Oncology Trust Karyn Sangster, Director of Nursing Cancer, Counties Manukau DHB Andrew Simpson, National Clinical Director Cancer, Ministry of Health Richard Sullivan, Oncologist, Auckland DHB / Medical Director, Northern Cancer Network Heidi Watson, Nurse Specialist, Auckland DHB Before prescribing VELCADE please review the Minimum Prescribing Information below. VELCADE® (bortezomib) – Minimum Data Sheet Indications: untreated multiple myeloma unsuitable for high dose chemotherapy, in combination with melphalan and prednisone. Multiple myeloma, received at least one prior therapy, have progressive disease. As part of combination therapy, for induction therapy prior to high dose chemotherapy with autologous stem cell rescue for patients under 65 years of age with previously untreated multiple myeloma. Dose and method of use: 1.3 mg/m2 may be administered intravenously at a concentration of 1 mg/mLas a 3-5s bolus injection or subcutaneously at a concentration of 2.5 mg/mL, see full Data Sheet for dosing schedule; reduce or withhold dose with haematological toxicity or neuropathy. Retreatment may be considered for patients who had responded to treatment with VELCADE; see full Data Sheet. Contraindications: hypersensitivity to bortezomib, boron or mannitol. Precautions: DO NOT ADMINISTER INTRATHECALLY, peripheral neuropathy, hypotension, cardiac disorders, thrombocytopenia, gastrointestinal adverse events, pulmonary disorder, reversible posterior leukoencephalopathy syndrome, seizures, tumour lysis syndrome, hepatic events, hepatic impairment, renal impairment, fertility, lactation, driving or operating machinery. Freq. monitor CBC; pregnancy, lactation, children, see full Data Sheet. Interactions with other drugs: inhibitors or inducers of cytochrome P450 3A4 or 2C19, oral hypoglycaemics, caution to be used with concomitant medications that may be associated with peripheral neuropathy (such as amiodarone, anti-virals, isoniazid, nitrofurantion, statins), or with a decrease in blood pressure. Adverse events: infections, pyrexia, GI, haematological disturbances, peripheral neuropathy, hypotension, haematoma, headache, decreased appetite, general psychiatric disorders, dyspnoea, rash, blurred vision, vertigo, myalgia; fatigue, pyrexia, tumour lysis syndrome (uncommon), pulmonary disorders, others, see full Data Sheet. Presentation: VELCADE is a Prescription Medicine containing bortezomib 1mg or 3.5 mg per single dose vial. Date of Preparation: 18 December 2012. Please review approved Data Sheet before prescribing, available at www.medsafe.govt.nz or on request from Janssen New Zealand, PO Box 62185, Sylvia Park, Auckland, New Zealand. VELCADE is fully funded, Special Authority criteria apply. NZ-VEL0037 TAPSCH4224 December 2014 Oncology & Haematology Conference 2015 9 DON’T MISS THE NZNO ONCOLOGY AND HAEMATOLOGY CONFERENCE BREAKFAST SYMPOSIUM Saturday, March 21 7.30 am Management of patients with Myelodysplastic Syndromes (MDS) with Vidaza A practical session on how to best help your MDS patients with their Vidaza (azacitidine) treatment. Peter Shuttleworth, Haematology Nurse Coordinator, Austin Health, Victoria, Australia Venue: Ko Awatea, Middlemore Hospital Campus Agenda 6.45 am Complimentary bus pick up from Holiday Inn, Auckland Airport 7.00 am – 7.30 am Breakfast provided (sponsored by Celgene) 7.30 am – 8.30 am Educational session Peter Shuttleworth Peter has developed a vast experience in haematology and bone marrow transplant nursing since his career commenced over 20 years ago. He started his nursing career within the Haem/Onc/BMT unit at the Royal Children’s Hospital in Melbourne in 1993, before moving up the road to the Royal Melbourne Hospital (RMH) in 1996. In 1999 he became the haematology/ BMT Clinical Trials Nurse at RMH, and was involved in co-ordinating a number of studies in myeloma during the exciting introduction of immunomodulators and proteasome inhibitors. During this time, he was also involved in the phase III randomised trial of azacitidine in MDS and low blast count AML. 2010 saw an exciting change in direction, with Peter’ taking on the role of Haematology Clinical Nurse Consultant at the Austin Hospital, Melbourne. The Austin’s unit and it’s trial capacity was rapidly expanding at the time, and consequently Peter was responsible for co-ordinating the azacitidine patients with ALLG study involvement, as well as those patients managed within reimbursed indications. The majority of his time is spent co-ordinating and managing the outpatient and day oncology population across the range of haematology indications. In accordance with the Code of Practice - Medicines New Zealand, any costs (for example travel or meals) incurred by a partner/spouse, guests, or a family member travelling with a healthcare professional must not be paid for or subsidised by the company. Celgene Pty Ltd ABN 42 118 998 771. Level 7, 607 St Kilda Rd, Melbourne VIC 3004, Australia. ZCLG02005 10 Oncology & Haematology Conference 2015 Oncology & Haematology Conference 2015 11 Registration desk open Venue: Foyer, Ko Awatea Plenary 1 Mihi whakatau Whitiora Cooper Opening address Karyn Sangster ‘MIDDLE EARTH’ - visibility and effectiveness of autonomous nursing roles Julie Cairns Nursing roles and innovation Shelley Dolan 8.00am 8.30am - 10.30am 8.30am - 8.45am 8.45am - 9.00am 9.00am - 9.45am 9.45am - 10.30am FRIDAY PROGRAMME 10.30am - 11.00am Morning tea and exhibition Venue: Rooms 103 and 106 Venue: Lecture Theatre Chair: Angela Knox Buses depart Holiday Inn Auckland Airport for Ko Awatea, Middlemore Hospital 7.45am FRIDAY 20 MARCH 2015 NZNO Cancer Nurses College: Oncology and Haematology Conference 2015 12 Oncology & Haematology Conference 2015 The needs of adolescents/young adults with cancer Heidi Watson Chemotherapy dosing in the obese patient Henry Chan 1.10pm - 1.45pm 1.45pm - 2.20pm Venue: Lecture Theatre Chair: Anne-Marie Wilkins Plenary 3 1.10pm - 3.20pm 12.15pm - 1.10pm Lunch and exhibition Venue: Rooms 103 and 106 Day Ward Tour 2 New nurse-led developments for people with neuroendocrine tumours in New Zealand Avril Hull, Ben Lawrence 11.55am - 12.15pm Evidence on the handling and administration of biological agents - an update Jacky Chan Is a support group an effective Day Ward Tour 1 intervention to help address the specific unmet needs of carers of people living with or beyond a haematological malignancy Amanda Foster Optimising the patient journey – a dynamic approach Nicole Falkner, Larissa Ferguson 11.30am - 11.50am Concurrent Session 1C Meet at the ForumPoint2 registration desk 5 minutes prior to start time Concurrent Session 1B Venue: Lecture Theatre 2 Chair: Ella Liang Implementation of the EviQ Anti-Neoplastic Drug Administration course in the New Zealand setting: An Update Barry Keane 11.00am - 11.20am 11.30am - 12.15pm Concurrent Session 1A Venue: Lecture Theatre 1 Chair: Hannah Milner Plenary 2 11.00am - 11.20am Venue: Lecture Theatre Chair: Kathryn McWatt FRIDAY PROGRAMME Oncology & Haematology Conference 2015 13 Afternoon tea and exhibition Venue: Rooms 103 and 106 Plenary 4 ONP - Better care, better health, better outcomes…. or just cheap labour? Anne Fraser NZNO’s Visibility of Nursing Campaign Anne Brinkman Close of Day 1 Angela Knox Buses depart Ko Awatea, Middlemore Hospital Campus for Holiday Inn Auckland Airport NZNO Cancer Nurses College: Oncology and Haematology Conference Dinner Venue: Jean Batten Ballroom, Holiday Inn Auckland Airport Theme: Roaring 20’s 3.20pm - 3.50pm 3.50pm - 4.30pm 3.50pm - 4.15pm 4.15 pm - 4.30pm 4.30pm 4.45pm 7.00pm - late FRIDAY PROGRAMME Venue: Lecture Theatre Chair: Janene Lawrence NZNO Cancer Nurses College: Oncology and Haematology Annual General Meeting 2.20pm - 3.20pm 14 Oncology & Haematology Conference 2015 Sponsored Breakfast Session Management of patients with Myelodysplastic Syndromes (MDS) with Vidaza Peter Shuttleworth Plenary 5 ‘Crouch, Touch, Pause and Engage’ - Chemotherapy Redesign Project Julie Cairns Quality, safety and an excellent patient experience Shelley Dolan 7.30am - 8.30am 8.40am - 10.05am 8.40am - 9.20am 9.20am - 10.05am Concurrent Session 2B Venue: Lecture Theatre 2 Chair: Merip T-Ah Sam The Skills and Knowledge framework for cancer nursing Angela Knox 10.35am - 11.00am 11.10am - 11.55am Concurrent Session 2A Venue: Lecture Theatre 1 Chair: Hannah Milner Plenary 6 10.35am - 11.00am Venue: Lecture Theatre Chair: Kathryn McWatt 10.05am - 10.35am Morning tea and exhibition Venue: Rooms 103 and 106 Concurrent Session 2C Meet at the ForumPoint2 registration desk 5 minutes prior to start time Registration desk open and breakfast served 7.00am Venue: Lecture Theatre Chair: Angela Knox Buses depart Holiday Inn Auckland Airport for Ko Awatea, Middlemore Hospital 6.45am SATURDAY 21 MARCH 2015 SATURDAY PROGRAMME Oncology & Haematology Conference 2015 15 National perspective of cancer services Andrew Simpson Genesis Oncology Trust Clinical Fellowship for Cancer Nurses – where are the applicants? Douglas Ormrod Panel discussion: From your perspective, how are nursing contributions recognised, evaluated and utilised within this transforming culture? Andrew Simpson, Richard Sullivan, Julie Cairns, Natalie James Prize giving Closing Address Buses depart Ko Awatea, Middlemore Hospital Campus for Holiday Inn Auckland Airport 12.45pm - 1.05pm 1.05pm - 1.15pm 1.15pm - 1.55pm 1.55pm - 2.05pm 2.05pm - 2.35pm 2.45pm SATURDAY PROGRAMME Venue: Lecture Theatre Chair: Cathy Teague Plenary 7 Venue: Rooms 103 and 106 Day Ward Tour 4 Day Ward Tour 3 12.45pm - 2.35pm 11.55am - 12.45pm Lunch and exhibition Factors affecting pre-chemotherapy Should a suspicion of cancer patient education be disclosed?: A literature Sarah Ellery review Shelley Shea 11.35am - 11.55am Thrombosis and Cancer, is it time for routine pharmaceutical thromboprophylaxis? Martyn James, Debi Smith Collaboration in clinical care pathway development: Facilitating timely access to diagnosis and first treatment for colorectal cancer Melissa Warren 11.10am - 11.30am ABSTRACTS 1. Plenary 1 Friday 20 March 2015 9.00am – 9.45am “MIDDLE EARTH” - VISIBILITY AND EFFECTIVENESS OF AUTONOMOUS NURSING ROLES Julie Cairns Olivia Newton John Cancer Wellness Centre, Austin Health, Melbourne, Australia Nursing is traditionally viewed as a “cost”, and the largest one, rather than viewed as a “revenue”, or value adding opportunity in healthcare. Defining and promoting nursing practice that directly results in quality patient care outcomes is complex, and often difficult to separate out from other health care components and influencers. There is now much discussion about the need to focus attention on how nursing can contribute to improved patient outcomes and experience, which ultimately reduces cost and inefficiency in the health system. There is good evidence that quality nursing can impact on both of these. In the past few years with massive healthcare reforms afoot, both the US and the UK have made bold statements in relation to the future of nursing that signal where governments, the health care industry and the nursing profession need to focus their attention and resources. These statements include reference to the need for nurses to work to the full extent of their scope of practice, knowledge and skills which will lead to an increase in specialist and advanced nursing roles; a recognition that there will be a blurring of professional boundaries and therefore the need for a stronger (and more equal) partnership model with medicine and other healthcare professionals to redesign health systems; and the need for nursing to take a more entrepreneurial stance and direct and lead care. 1,2 A lot of research has been undertaken in the area of Nurse Sensitive Outcomes, mostly in the acute setting in the US and a focus on structural variables such as staffing levels. The identification and validation of Nurse Sensitive Indicators cuts to the core of professional nursing practice, and will form the basis of the discussion in this address, - and that is – How does nursing/nursing care make a difference to patient outcomes? And therefore provide a strong evidence base for nursing to be considered more of a value added/revenue activity rather than a “cost”. This keynote will review the issues around the research into the development of Nurse Sensitive Indicators, and also an overview of a model for the evaluation of effectiveness of nursing role/s in relation to nurses’ role performance and the impact on patient outcome and ongoing practice improvement. References 1. IOM (Institute of Medicine) 2010. The Future of Nursing: Leading Change, Advancing Health. Washington DC: The National Academies Press 2. Nursing: Towards 2015, Longley, Shaw, Dolan, October 2007, Nursing and Midwifery Council, UK 16 Oncology & Haematology Conference 2015 2. Plenary 1 Friday 20 March 2015 9.45am – 10.30am NURSING ROLES AND INNOVATION Shelley Dolan Chief Nurse The Royal Marsden NHS Foundation Trust & Clinical Director, The London Cancer Alliance. In 2015 the opportunities for cancer nursing across the world are very exciting. There is a global refocusing on person-centred care and outcomes coupled with improved experience. At such a time the door is open for cancer nurse leaders to seize the opportunity and embrace new roles for innovation always with the care of the patient and their family at the centre. In its submission to the Prime Ministers Taskforce in the UK the RCN designed a framework for the evolution of nursing roles. The framework mandates making quality, safety and innovation the backbone of any national or international nursing career framework. With a pre-registration and post registration curriculum that focuses on a person centred and whole systems approach, coupled with assurance and revalidation of nurses expertise and competence. The framework then proceeds to focus on clinical nursing leadership, shared systems for nursing Information Technology to ensure that essential patient information can be shared across care environments and that patients can be encouraged to use new technologies in their self -management and monitoring of symptomatology. Finally the framework focuses on safer nursing skill mix and numbers and on the promotion of innovation, audit and research to ensure continuous improvement of patient and family care. As a global cancer community we need to think about the care settings, domain and populations that we need to serve. It is evident across the better resourced countries that our cancer population is ageing, will increasingly have cancer and other comorbidities and will increasingly be wanting to be treated at home or out of hospital settings. New roles therefore need to span settings and ensure integration of the experience for the patient. Finally our cancer nursing leaders of the future will need extended skill sets in leadership across systems, innovation and change practice and embedding change in a sustainable way. Oncology & Haematology Conference 2015 17 3. Plenary 2 Friday 20 March 2015 11.20am – 11.35am IMPLEMENTATION OF THE EVIQ ANTI- NEOPLASTIC DRUG ADMINISTRATION COURSE IN THE NEW ZEALAND SETTING: AN UPDATE Barry Keane1, Paul Smith2 1 MidCentral Health & Central Cancer Network, 2 Wellington Blood and Cancer Centre & Central Cancer Network The New Zealand cancer nurses sector has for some time identified the need for an improved chemotherapy assessment and delivery training programme for nurses involved in the care of patients receiving chemotherapy. The Australian eviQ online Anti-neoplastic Drug Therapy Course (ADAC) has been identified as a suitable national replacement for the New Zealand setting. Based on the Australian experience, implementation could deliver a consistently well trained cancer nursing workforce more responsive to patient need both in terms of clinical assessment, treatment delivery and the ability to provide treatment close to patients’ homes. In partnership with key stakeholders the National Nurses in Cancer Care Collaborative, which includes the College of Cancer Nurses, has been working on a plan to introduce the ADAC programme to New Zealand. In the context of wide interest nationally, the implement the ADAC is planned for central region firstly, facilitated by the Central Cancer Network. This paper provides an update on progress with implementing the EviQ Anti Neoplastic Drug Administration Course (ADAC) in the New Zealand setting, including a reflection on some of the wider issues influencing cancer nursing development at the national level. 18 Oncology & Haematology Conference 2015 4. Concurrent Session 1A Friday 20 March 2015 11.30am – 11.50am OPTIMISING THE PATIENT JOURNEY – A DYNAMIC APPROACH Nicole Falkner1, Larissa Ferguson 2 1 CNC Upper GI and Liver, Counties Manukau DHB 2 CNC Lung, Counties Manukau DHB Presentation Summary: Cancer Nurse Coordinator collaboration within Counties Manukau Health, working towards the common goal of navigating the patient through the cancer journey. Several initiatives are being developed throughout Counties Manukau Health cancer services. One of these is a ‘Track and Trigger’ database developed by the lung tumour stream to assist efficient patient flow, highlight delays and support the current pilot of rapid access cancer clinics. Oncology & Haematology Conference 2015 19 5. Concurrent Session 1A Friday 20 March 2015 11.55am – 12.15pm NEW NURSE-LED DEVELOPMENTS FOR PEOPLE WITH NEUROENDOCRINE TUMOURS IN NZ Avril Hull, Ben Lawrence Auckland District Health Board, Auckland People with Neuroendocrine Tumours (NETs) face unique challenges that need individualized patient-focused solutions. NET is an umbrella term for a group of uncommon cancers that arise from neuroendocrine cells found throughout the body. NETs range from very slow to very fast growing, and sometimes secrete hormones that cause debilitating symptoms; making them a challenging group of cancers to treat. Based on worldwide statistics there might be 250 new NZ patients diagnosed each year. Fourteen months ago I established my role as a Nurse Specialist (CNS) for people with NETs under the care of Auckland’s oncology department. Despite a strong oncology background, I faced a steep learning curve, albeit both enlightening and humbling. As the only NET CNS in NZ, my experience has mirrored colleagues in the UK who describe a sense of isolation sometimes felt by both patients and nursing staff, the limitations of treatment options, and frustration at the lack of educational resources. My early focus was to develop a NZ-orientated patient information booklet on NETs. Awareness of NETs in NZ can be further developed by a new patient organisation called Unicorn Foundation NZ, and I support patients through this group by attending meetings that highlight the difficulties patients face. I have strong ties with The NETwork! Research project and the world-leading genomic research on NETs at the University of Auckland, and assist patents to participate in the project and help with sample collection. Currently there are no NZ based statistics, so I contribute to a national NET registry to ascertain NET incidence and prevalence in NZ. To improve clinical outcomes, I attend a new weekly NET MDM meeting where doctors present questions about patient care, and I will aim to ensure that the patient voice is represented. The sub-group of patients with slow growing disease has considerable potential to benefit from a long-term nurse led clinical care, including management of secretory symptoms and injection of drugs like octreotide for symptom control, and better continuity in care. At present I am establishing a weekly nurse-led clinic for patients with NETs in Auckland. Although this family of tumours are complex and rare, knowledge and support for this group of patients is developing rapidly in NZ, and oncology nurses can play a key role in improving the quality and experience of the patient journey. 20 Oncology & Haematology Conference 2015 6. Concurrent Session 1B Friday 20 March 2015 11.30am – 11.50am IS A SUPPORT GROUP AN EFFECTIVE INTERVENTION TO HELP ADDRESS THE SPECIFIC UNMET NEEDS OF CARERS OF PEOPLE LIVING WITH OR BEYOND A HAEMATOLOGICAL MALIGNANCY? Amanda Foster Support Services Coordinator, Leukaemia & Blood Cancer New Zealand Purpose: The term ‘carer’ is used broadly to describe someone offering unpaid support to a friend or family member and ‘care’ will vary depending on the individual needs of the patient which will change in accordance with their disease process. Extensive literature demonstrates that carers of cancer patients may experience high levels of depression, anxiety and stress and have poor overall wellbeing. In some cases carers have more unmet psychosocial needs than the patient. Research has shown that a support group can be an effective intervention for carers in a general oncology or palliative care setting. There is currently little evidence specifically identifying the needs of carers in a haematology setting or recommending interventions. Leukaemia & Blood Cancer New Zealand (LBC) is a national non-government organisation dedicated to supporting families affected by a blood cancer diagnosis and so is ideally placed to offer support for carers. The aim of this proposal is to pilot a support group for the carers of haematology patients and to assess the effectiveness of the intervention in helping to manage unmet needs. Methods: A support group specifically for carers of people living with or beyond a blood cancer diagnosis will be held at the LBC Midland Office. The group will be facilitated by an LBC Support Services Coordinator and a counsellor specialising in stress management and relationship counselling. Participants will be asked to complete a self administrated questionnaire at the completion of the support group. Results: It is expected that the results of this pilot will corroborate with similar research in the general oncology and palliative care setting, which show that support groups are an effective way to help manage informational and emotional support needs. They help relieve sense of isolation, reduce stress and anxiety levels and provide a platform for problem sharing and solving. Oncology & Haematology Conference 2015 21 7. Concurrent Session 1B Friday 20 March 2015 11.55am – 12.15pm EVIDENCE ON THE HANDLING AND ADMINISTRATION OF BIOLOGICAL AGENTS – AN UPDATE Jacky Chan Pharmacy Department, Middlemore Hospital Occupational health and safety exposure risks associated with cytotoxic medications are well established. However, there is little information regarding such risks with monoclonal antibodies (MABs). Traditionally, many institutions have treated MABs much like cytotoxic medications with similar pre-cautions and procedures. However, there are increasing variability to what different hospitals do in the preparation of MABs. We will review the risks to healthcare personnel associated with the handling and administration of biological agents, and the updated evidence of how and where a MAB should be prepared. 22 Oncology & Haematology Conference 2015 8. Plenary 3 Friday 20 March 2015 1.10pm – 1.45pm THE NEEDS OF ADOLESCENT/YOUNG ADULTS WITH CANCER Heidi Watson AYA’s present with a unique set of challenges for health professionals. They have distinct physical, psychological and developmental needs that are significantly different from those of children and adults. Their developmental needs can and often do compete with the demands of health care, with issues such as adherence becoming more of an issue during this time. There is recognition that existing structures and approaches to care are often not set up to deal with this population suitably. This potentially may have contributed to the relatively poor AYA cancer improvements in survival rates over the last 30 years in comparison to children. Current survival rates for AYA’s with cancer in New Zealand are below international comparisons. There is also a significant gap that exists in the survival of Maori/Pacific AYA’s in comparison to Non Maori/Pacific. (Ballantine K, Sullivan M. Adolescent and Young Adult Cancer Incidence and Survival in NZ 2000 to 2009: Child Cancer Network; 2013) To maximise health and psychosocial outcomes AYA’s require a complex range of services that have the ability to work across traditional health service boundaries and are delivered through a number of disciplines and professional groups. This presentation will deliver an overview of the needs of AYA cancer patients and the development of AYA cancer services in NZ. Oncology & Haematology Conference 2015 23 9. Plenary 3 Friday 20 March 2015 1.45pm – 2.20pm CHEMOTHERAPY DOSING IN THE OBESE PATIENT Henry Chan Laboratory Haematology Registrar, Auckland The prevalence of obesity is increasing in New Zealand and around the world. Other than the common medical conditions that people often associate with obesity, increased body mass index has also been linked to various malignancies. Although the exact linkage and mechanism in how obesity would trigger clonal proliferation remain uncertain at present, there is little doubt that the healthcare system will face more obese patients with malignancy as the general population continue to become more overweight. Dosing chemotherapy for obese patients can be contentious, as there are often fear concerning the toxicity of treatment when full uncapped doses are given at high quantity. Various dose reduction regimens are currently in use, but the scientific rationale behind some of these approaches is limited. To address this issue, the American Society of Clinical Oncology has recently performed a comprehensive review of the data, and they concluded that dose reduction should not be used when dosing chemotherapy for obese patients with malignancy, especially if the treatment aim is cure. The experience from the Department of Haematology in Middlemore Hospital supports this ASCO recommendation, as it has found no increased in toxicity amongst the obese patients who received full uncapped doses of R-CHOP chemotherapy. Importantly, while historical data show that obese patients do worse than normalweight patients, their result shows that both group have comparable survival outcomes. This finding has been supported by other recent publications, and it is postulated that the historically poor outcome amongst obese patients may have been due to the relative underdosing of chemotherapy resulted dose reduction regimens. 24 Oncology & Haematology Conference 2015 10. Plenary 4 Friday 20 March 2015 3.50pm – 4.15pm ONP - BETTER CARE, BETTER HEALTH, BETTER OUTCOMES…. OR JUST CHEAP LABOUR? Anne Fraser Oncology Nurse Practitioner, Blood and Cancer Service, Auckland Medical oncology is a core service underpinning successful treatment of cancer. As a modality of cancer care, it is facing significant challenges that threaten the sustainability of cancer care services in New Zealand. As a result of this growth in demand as well as changes in treatment practices, and expanded treatment options over the past ten years, current service provision is substantially stretched. This growth in demand, coupled with the existing constraints on the workforce, facilities and funding, severely compromises the sustainability of services in the future. The key challenges that underpin the need for services improvement are: • Overburdened and limited resources shortages • A significant projected increase in demand over the next 15 years, driven by the aging population, higher rates of survival, prolonged treatment times and expanding treatment options • Rising patient expectations Ministry of Health commissioned report, New Models of Care for Medical Oncology (Cranleigh Health, unpublished) recommended: Implementing a role delineation framework that identifies the tasks and functions on the patient care pathway that staff other than senior medical officers ( SMOs) can provide. This component would include taking on specialist nurses and introduce options for alternative medical staff in hospitals and communities to focus the capacity of medical oncologists at key care delivery points. Nurse practitioners are expert nurses who work within a specific area of practice incorporating advanced knowledge and skills. They practice both independently and in collaboration with other health care professionals to promote health, prevent disease and to diagnose, assess and manage people’s health needs. They provide a wide range of assessment and treatment interventions, including differential diagnoses, ordering, conducting and interpreting diagnostic and laboratory tests, and administrating therapies for the management of potential or actual health needs. They work in partnership with individuals, families, whanau and communities across a range of settings. Nurse practitioners prescribe medicines within their specific area of practice. Nurse practitioners also demonstrate leadership as consultants, educators, managers and researchers. and actively participate in professional activities, and in local and national policy development. This session will explore some of the challenges and practical implications around registering as an ONP in the NZ setting in the post Cranleigh setting. Oncology & Haematology Conference 2015 25 11. Plenary 4 Friday 20 March 2015 4.15pm – 4.30pm NZNO’S VISIBILITY OF NURSING CAMPAIGN Anne Brinkman NZNO At the 2014 NZNO AGM conference members identified two issues on which action is needed around NZ nursing’s image: • Publicly promote the value of nursing and nurses, and • Elevate the professional association profile of NZNO. The primary purpose of the Visibility in Nursing campaign is to reinforce professional pride, promote nursing, raising its profile and image publicly. In addressing this goal, a secondary benefit will be that the professional association profile of NZNO will be lifted accordingly. The campaign outcomes include: • Conveying pride in nursing • Projecting professionalism • Empowering members to articulate the value of nursing • Demonstrating value of nursing • Nurses as knowledgeable, skilled health professionals • Improving engagement at all levels 26 Oncology & Haematology Conference 2015 12. Plenary 5 Saturday 21 March 2015 8.40am – 9.20am “CROUCH, TOUCH, PAUSE, ENGAGE” – CHEMOTHERAPY REDESIGN PROJECT Julie Cairns Olivia Newton John Cancer Wellness Centre, Austin Health, Melbourne, Australia Introduction In 2013 the Victorian Chemotherapy Services Redesign Project was undertaken to improve the patient’s experience of the Chemotherapy Day Unit/s (CDUs). The objective of the project was to increase the capability of Victorian CDU management teams to employ lean business improvement techniques and consistent performance measures to support locally lead service improvement; to develop a CDU redesign toolkit and suite of performance measures; and to improve efficiency of participating CDU’s and share learnings. Context In April 2014, the Day Oncology centre at the Olivia Newton John Cancer Wellness Centre initiated a Chemotherapy Redesign project. The centre was witnessing an increasing number of patients and treatments, increasing complexity, increasing numbers of patients being recruited onto clinical trials, and an increase in the length of time of treatments resulting in a variation of access to treatment times. 56% of patient experienced a delay of >15mins from their appointment time to their treatment time. Chair utilisation rate was 65% against best practice of 80%. Aims/Objectives The overall aim was to improve the patient experience by reducing waiting times on the day of treatment. The key objectives were to reduce variation in waiting times, and to develop a suite of performance measures that could be used to support leaders and staff to effectively monitor and improve the service. Methodology Lean methodology was employed to undertake diagnostics to understand the patient experience and the different patient, service, and product flows. Data was collected around waiting times and the pathology collection process. IT scheduling systems were reviewed and activity, scheduling, and delay data was collected and analysed. Results Chair utilisation has increased from 65%, and is now consistently sitting at around 90%. 80% of patients receive their treatment within 15 mins of their scheduled appointment. A fast track process and area was implemented, chemotherapy regimen times were reviewed for the scheduler, and the pre chemotherapy patient education process redesigned. Oncology & Haematology Conference 2015 27 13. Plenary 5 Saturday 21 March 2015 9.20am – 10.05am QUALITY, SAFETY AND AN EXCELLENT PATIENT EXPERIENCE Shelley Dolan Chief Nurse The Royal Marsden NHS Foundation Trust & Clinical Director, The London Cancer Alliance Across the World there is a renewed concentration on refreshing and improving the quality and safety of healthcare. As we work together globally we have learnt more about designing processes and care that improve the quality and experience of care for people with cancer. In the UK The Point of Care Foundation and in the US The Magnet Hospitals Association has highlighted the need to remember that good staff engagement and care is an absolute prerequisite for excellent patient care. During the presentation the evidence from Schwartz rounds will be explored. Originating from the US a doctor with lung cancer reflected on the need in acute cancer care to make the unbearable bearable through small acts of kindness. The use of Schwartz rounds has resulted in a shared experience for staff, improved empathy , and staff having time to refresh their energy and think about what really matters in care. If acute cancer care is really to improve the engagement, empowerment and leadership of front line staff is pivotal. The presentation will include a ward accreditation system that has been designed by frontline nurses to ensure a holistic approach to the real time evaluation of care across the whole of the Royal Marsden. This real worked case is presented as one example of the work that is being led by clinical cancer nurses across the world to improve outcomes, quality and safety in acute cancer care. Finally the presentation focuses on the work that cancer nurses are collaborating on globally to influence and improve the experience of people with cancer as they are diagnosed and treated. Nurses in the UK and US have collaborated on using tools such as the Concerns Thermometer as part of a Holistic Needs Assessment to ensure that cancer care is really patient centred. 28 Oncology & Haematology Conference 2015 14. Plenary 6 Saturday 21 March 2015 10.35am – 11.00am THE SKILLS AND KNOWLEDGE FRAMEWORK FOR CANCER NURSING Angela Knox Clinical Nurse Manager, Haematology, Middlemore Hospital Chair NZNO Cancer Nurses College In collaboration with the Ministry of Health (MoH), the New Zealand Nurses Organisation (NZNO) Cancer Nurses College (CNC) and the Knowledge and skills framework reference group, the Skills and Knowledge framework for cancer nursing (KSFCN) has been completed. Following a national consultation process, the final draft of the KSFCN was rigorously reviewed and subsequently approved and endorsed for implementation by the National Nursing Consortium in November 2014. Cancer is the leading cause of death in New Zealand and as such requires the nurse to have the necessary education and tools to enable them to care for people with cancer across the health continuum in a number of settings. The KSFCN was developed with MoH support by cancer nurses for cancer nurses. The KSFCN is intended to complement your current professional development framework(s) as a tool to assist nurses working across the cancer care continuum to identify the specific knowledge and skills required to support their personal and professional development as generalist nurses caring for people with cancer and/or nurses who wish to specialise in cancer nursing. This presentation will provide an over view of the importance of the SKFCN for cancer nurses, with the purpose of encouraging you to utilise the framework in your practice area. Oncology & Haematology Conference 2015 29 15. Concurrent Session 2A Saturday 21 March 2015 11.10am – 11.30am COLLABORATION IN CLINICAL CARE PATHWAY DEVELOPMENT: FACILITATING TIMELY ACCESS TO DIAGNOSIS AND FIRST TREATMENT FOR COLORECTAL CANCER Melissa Warren Clinical Nurse Specialist – Cancer Care Coordination: Colorectal Cancer Capital and Coast District Health Board, Wellington Purpose The Clinical Nurse Specialist – Cancer Nurse Coordinator (CNC) is a new and evolving role in New Zealand. The main function of the CNC is to improve patient experience and outcomes by coordinating care and facilitating a timely diagnosis and initiation of treatment. Nationally there are 56 CNC’s, with the vast majority having a direct patient contact care coordination focus. A small number of CNC’s nationwide have been given a tumour specific pathway development project mandate by their District Health Boards. Methods A clinical project was undertaken to view the current process from initial referral to first treatment and beyond within the colorectal cancer service at Capital and Coast DHB. Retrospective process mapping of 15 patients (random sample) diagnosed and treated for colorectal cancer was carried out by a CNC, which identified potential areas where improvements may be made to improve patient experience, reduce inequalities and achieve efficiencies. Results Process mapping has proved a valuable tool in making all the steps within the colorectal cancer pathway visible; engaging MDT members in understanding the journey from beginning to end and owning any service problems that have emerged. Process mapping identified a number of areas where there is variability and delays within the colorectal cancer pathway; referrals, triage prioritisation, cross departmental systems, lack of pathway and supportive care. This has served as useful starting point from which to develop clinical care pathways collaboratively with the MDT; from GP referral to diagnostics and treatment and can be applied by senior cancer nurses looking to enhance the quality of care across the care continuum in their own cancer services. 30 Oncology & Haematology Conference 2015 16. Concurrent Session 2A Saturday 21 March 2015 11.35am – 11.55am FACTORS AFFECTING PRE-CHEMOTHERAPY PATIENT EDUCATION Sarah Ellery Canterbury Regional Cancer and Haematology Service, Oncology Department Canterbury District Health Board, Christchurch Purpose: Over the last 30 years health care and health care related education have evolved from a basis of paternalism to partnership. In order to understand existing literature and research on the current approach to pre-chemotherapy patient education an integrative review was undertaken to explore four questions: What are the factors affecting pre-chemotherapy patient education? Does evidence or best practice exist on how pre-chemotherapy should be delivered? What are the most commonly used methods and resources for delivering pre-chemotherapy patient education? Does evidence or best practice exist to identify what the content of pre-chemotherapy patient education should consist of? Methods: Integrative literature review Results: A number of the key points are summarised: • People with a cancer diagnosis have individual information needs which require consideration, and vary over time, throughout the cancer trajectory. • Assessment of information needs is poorly undertaken or absent. Thorough assessment is hindered by a number of health system constraints. • Culture, gender, age, socio-economic status, education, ability to cope and health literacy levels may influence the information people need, how and when they receive it, as well as impact on their self-care ability. • Providing education and information is a dynamic process and should be tailored to the individual. • Education is a formal and informal process. Informal opportunities should not be missed. Reinforcement should occur at each opportunity as it arises. • Formal education sessions should have a structured approach to delivery with consistency of content across all staff delivering education. • Content should be based on evidence and best practice where available. • Staff training in communication skills and adult learning theory may lead to more effective education. • Resource development and environment considerations also exist. Conclusion: In conclusion, opportunities exist to improve the pre-chemotherapy education process for the person with cancer and their family and friends as well as staff involved in the education process. Oncology & Haematology Conference 2015 31 17. Concurrent Session 2B Saturday 21 March 2015 11.10am – 11.30am THROMBOSIS AND CANCER, IS IT TIME FOR ROUTINE PHARMACEUTICAL THROMBOPROPHYLAXIS? Martyn James Thrombosis Nurse Specialist, Counties Manukau DHB This presentation will examine the evidence around the use of thromboprophylaxis in cancer patients. Venous thromboembolism (VTE) represents one of the most important causes of morbidity and mortality in cancer patients. According to population-based case–control studies, the 2-year cumulative incidence of VTE is between 0.8 and 8%. The thrombosis unit at Middlemore is dealing with a steadily increasing volume of patients who have malignancy associated VTE and are working towards strategies to reduce the incidence of this serious complication. 32 Oncology & Haematology Conference 2015 18. Concurrent Session 2B Saturday 21 March 2015 11.35am – 11.55am SHOULD A SUSPICION OF CANCER BE DISCLOSED?: A LITERATURE REVIEW Shelley Shea Nelson Marlborough District Health Board, Nelson A cancer diagnosis can create anxiety for patients and health practitioners alike, so discussion around a possible cancer diagnosis are often deferred until it has been confirmed through pathology or high-tech imaging. This reticence may result in communication difficulties which are unlikely to be helpful to either health practitioners or patients. Purpose: An exploration of the literature seeks to understand whether and how disclosure of a suspicion of cancer should occur. Methods: This literature review is based on the findings of an extensive literature review of publications pertaining to disclosure of a suspicion of cancer. The PubMed search engine and the following MESH terms were used: cancer diagnosis or early diagnosis or cancer suspicion and communication of “breaking bad news” or truth disclosure and physician-patient relationship. The search was restricted to adults, publications within 20 years, English language only and not screening, genetics and palliative care. Citations and reference lists were widely searched. Results: There are many opportunities to be had from pre-disclosing a diagnosis and this review has demonstrated a beginning understanding of the concept. Further research will enable clarification for clinicians on patient’s experiences whose views are often discordant with ours. The way a person reacts to a suspected cancer differs between individuals; this is because it is subjective to the context of the individual person. The truth should be told, but in a way that doesn’t remove hope, it should be offered rather than imposed onto patients. Knowledge should be gained of patient’s preferences in particular to learning difficult news and how that information should be presented. The truth should be told to individuals as per their wishes instead of assumptions being made based on what the patient needs to know. Not informing patients of a suspected cancer can lead to communication breakdowns amongst providers. Oncology & Haematology Conference 2015 33 19. Plenary 7 Saturday 21 March 2015 12.45pm – 1.05pm NATIONAL PERSPECTIVE OF CANCER SERVICES Andrew Simpson National Clinical Director, Cancer, Ministry of Health The Government has identified high quality health services and healthy communities as key priorities for health. Within these priorities are specific cancer-related activities that have a focus on cancer screening, speeding up access to diagnostics and treatment, improving personalised support to patients and implementing a new cancer health target. The Ministry recently released the New Zealand Cancer Plan 2015-18 which sets out all activities currently underway and planned for the next three years to implement the Government’s priorities for cancer. The New Zealand Cancer Plan also sets out a patient pathway framework to guide the focus of the National Cancer Programme which brings together the work of the Ministry, DHBs and regional cancer networks. Activities over recent years have focussed on service improvement, mainly through: • improving coverage and service delivery of cancer screening programmes and reducing barriers to access implementing a prostate cancer awareness and quality improvement programme • implementing the Faster cancer treatment programme through: • supporting the implementation a National Radiation Oncology Plan that outlines the linear accelerator and workforce requirements for radiotherapy • supporting the implementation of a new medical oncology model of care • establishing an Adolescent and Young Adult clinical network • supporting an effective National Child Cancer Network • ensuring that patients with cancer and their families have good psychological and social support. The successful implementation of the National Cancer Programme relies on a sector committed to working together and strong governance structures at national, regional and local levels. The nursing workforce has played an enormous role in contributing to the programme through: • participation on governance and advisory groups at all levels • work force and quality improvement initiatives eg the Cancer Nurse Coordinator Initiative, the Cancer Nurse Knowledge and Skills Framework • clinical leadership roles eg the National Nurse Lead- cancer nurse coordinator initiative. 34 Oncology & Haematology Conference 2015 20. Plenary 7 Saturday 21 March 2015 1.05pm – 1.15pm GENESIS ONCOLOGY TRUST CLINICAL FELLOWSHIP FOR CANCER NURSES – WHERE ARE THE APPLICANTS? Douglas Ormrod Programme Manager, Genesis Oncology Trust The Genesis Oncology Trust is an independent registered charity established in 2002 by Genesis Energy as part of the company’s commitment to the community. Genesis Energy customers donate more the $1 million annually to the Trust, and every $ is applied to the work of the Trust. To date the Trust has distributed more than $10 million to aid in the fight against cancer. The Genesis Oncology Trust funds a broad range of cancer-control research, training and education, including a Clinical Fellowship for Cancer Nurses which was established in 2011. This Fellowship will be awarded to a nurse who is committed to a clinical career with a major involvement in cancer treatment or care of those affected by cancer. It is intended for nurses so that they can enhance their practice and expertise through further clinical training and/or research and thus contribute to improved patient outcomes in New Zealand. The expectation is that at the end of the Fellowship the successful applicant will become established in clinical practice in New Zealand. The duration of the Fellowship is up to two years. To date interest in the Fellowship has not been overwhelming and only one award has been made. The purpose of this presentation is to provide information on the potential application of the award and to solicit feedback to determine if we can improve the structure of the award to attract more applications. Oncology & Haematology Conference 2015 35 EXHIBITION FLOOR PLAN 2 3 3,594 Room 103 9 90 1 s issued copied, ird party consent on Ltd. Angela Harold Drawn by: 3mtr x .81 Stand Size: 1:49 Scale: Initial Plan date: Revised Plan date: 20 May 2014 11 March 2015 Drawing Number: his drawing is reserved by 3 FP2 Project: Room/Level: Venue: 4 Event Co-ordinator: Maria Fomin 5 6 Show Dates: NZNOCNCIS 2015 Room 103 Ko Awatea Room 103 2015 Shell scheme type: Frontrunner info@peek.co.nz | www.p Room 106 3,979 erved by Client: 8 7 36 Drawn by: Oncology & Haematology Conference 2015 Room 106 Peek Display Client: FP2 Event Co-ordinator: Angela Harold Show Dates: 2014 Shell scheme type: Frontrunner EXHIBITOR DIRECTORY Aspen Pharmacare Stand number 9 Celgene2 GSK8 Janssen4 Leukaemia & Blood Cancer New Zealand 5 New Zealand Medical and Scientific Ltd 7 New Zealand Nurses Organisation (NZNO) Table Novartis Oncology 1 REM Systems 6 Roche NZ (Ltd) 3 Oncology & Haematology Conference 2015 37 EXHIBITOR INFORMATION ASPEN PHARMACARE Stand 9 P O Box 62027 Silvia Park Auckland 1644 T: +64 9 570 1080 F: +64 9 915 9581 E: aspen@aspenpharma.co.nz www.aspenpharma.co.nz Product on display: 1. Ferinject® Aspen Pharmacare offer a diverse range of tried and trusted brands in New Zealand. The product mix ranges across Ethical, Primary & Secondary care with key brands being Circadin®, Eltroxin®, Ferinject®, Redipred® and Simdax®. For more information visit www.aspenpharma.co.nz CELGENE Stand 2 PO Box 3035 Wellington 6140 T: 0800 526 529 www.celgene.com Contact: Kirsty Vercoe Products on display: 1. Revlimid (lenalidomide) 2. Vidaza (azacitidine) Celgene is a leading biopharmaceutical company engaged in the discovery, development and delivery of innovative therapies such as VIDAZA, REVLIMID and THALOMID which are designed to significantly enhance the quality of life and improve the prospects for critically ill patients with cancer and other debilitating diseases worldwide. For further information visit our website www.celgene.com 38 Oncology & Haematology Conference 2015 GSK Stand 8 Private Bag 106600 AUCKLAND 1143 T: +64 9 367 2900 www.gsk.co.nz Contact: Sean Reeves Products on display: 1. Votrient 2. Revolade 3. Tyker6 JANSSEN Stand 4 PO Box 62185 Sylvia Park AUCKLAND 1644 T: +64 9 588 1300 F: +64 9 588 1398 Contact: Gretchen Hamilton Products on display: 1. Velcade 2. Zytiga At Janssen, we collaborate with the world for the health of everyone in it. What matters most to us is a healthy outcome for each patient. We’re committed to providing safe and effective medicines as well as the services and support that contribute to healthy outcomes. One of the fastest growing of the top 10 pharmaceutical companies globally, we’re focusing our unique model of innovation on some of the most devastating diseases and the most complex medical challenges of our time, across five therapeutic areas; Immunology, Oncology, Neuroscience, Cardiovascular Medicine, and Infectious Disease. Products include Velcade for myeloma and Zytiga for prostate cancer. Oncology & Haematology Conference 2015 39 LEUKAEMIA & BLOOD CANCER NEW ZEALAND Stand 5 PO Box 99182 Newmarket AUCKLAND 1149 T: 0800 151 015 F: +64 9 638 3557 E: supportservices@leukaemia.org.nz www.leukaemia.org.nz Contact: Meg Morgan Leukaemia & Blood Cancer New Zealand (LBC) is the only not-for-profit organisation in New Zealand dedicated solely to supporting patients and families living with leukaemia lymphoma, myeloma and blood conditions. In addition LBC supports and funds research, advocates on behalf of patients, provides information and education and raises awareness. NEW ZEALAND MEDICAL AND SCIENTIFIC LTD Stand 7 PO Box 132400 Sylvia Park AUCKLAND 1644 T: +64 9 259 4062 F: +64 9 259 4067 E: rhughes@nzms.co.nz www.nzms.co.nz Contact: Ruth Hughes Products on display: 1. Medcomp Power Injectable Ports and PICCS 2. Eusapharma Caphosol mouth rinse 3. Focal Biozorb – 3 dimensional tissue marker NZMS proudly distributes Medcomp leading edge vascular access devices for the delivery of chemotherapy via power injectable ports and PICCs. Medcomp, by continually improving on existing technology can offer a catheter to suit every medical requirement while also considering you patients comfort. Caphosol™ for the treatment of Oral Mucositis. A supersaturated solution of calcium and phosate mouth rinse to assist healing and improve oral health. Commence Cancer therapy commence Caphosol™. BioZorb – the 3 dimensional tissue marker used in breast care treatment. 40 Oncology & Haematology Conference 2015 NEW ZEALAND NURSES ORGANISATION Table T: 021 579 020 www.nzno.org.nz/groups/colleges/cancer_nurses_college Contact: Angela Knox, Chair: aknox@middlemore.co.nz Wendy Jar, Vice-Chair: Wendy.Jar@Cdhb.health.nz The Cancer Nurses College encompasses a wide ranging group of nurses with an interest in the care of the person with cancer. This area may include the disciplines of oncology, haematology, paediatrics, surgery, community and rural health, research, education, management and health promotion and palliative care. NOVARTIS ONCOLOGY Stand 1 109 Carlton Gore Road Newmarket AUCKLAND 1023 T: +64 9 532 8500 F: +64 9 473 1531 E: Hannaki.smalberger@novartis.com www.novartis.com Contact: Hannaki Smalberger Novartis is caring and curing. We are committed to the research, development and supply of medicines to prevent and cure disease, ease suffering and enhance quality of life. To find out more about who Novartis is, visit www.novartis.com. Oncology & Haematology Conference 2015 41 REM SYSTEMS Stand 6 PO Box 90147 Victoria Street West AUCKLAND 1142 T: +64 9 570 3322 F: +64 9 570 3321 E: bforder@remsystems.co.nz Contact: Brenda Forder / Lesley Powell Products on display: 1. CODAN CYTO® Safe preparation and administration of cytostatics 2. CODAN CHEMOPROTECT® Complete protection in the preparation and administration of cytotoxic drugs 3. EQUASHIELD® 2nd generation closed system transfer devices for hazardous drugs REM SYSTEMS invites delegates to view our closed systems and protective wear for administration and compounding of Cytotoxic / Hazardous Medications. REM SYSTEMS has the CODAN CYTO® Safe Preparation and Administration Systems, which are used by multiple Oncology and Haematology Units. REM SYSTEMS has recently launched EQUASHIELD® which is a 2nd Generation Closed System Transfer Device for Hazardous Medications. EQUASHIELD® Syringes have a unique sealed barrel which ensures syringe equalisation to prevent the escape of vapors and aerosols. REM SYSTEMS looks forward to supporting the 2015 conference. ROCHE NZ (LTD) Stand 3 PO Box 109113 Newmarket AUCKLAND 1149 T: +64 9 523 9400 F: +64 9 523 9465 E: nz.info@roche.com www.roche.co.nz Contact: Paul Schon Products on display: 1. GAZYVA® 2. MABTHERA® Roche ranks as the leading oncology pharmaceutical company in the world and is known internationally for its many innovative contributions to medicine. Globally, Roche is number one in diagnostics, covering all fields of medical testing. Roche NZ (Ltd) plays a significant role in improving cancer outcomes for New Zealanders with a portfolio consisting of the following innovative targeted therapies, Avastin®, GAZYVA®, Herceptin®, Kadcyla®, MabThera®, Neulastim®, Perjeta®, Tarceva®, Zelboraf®, and Erivedge®. In New Zealand, Roche invests heavily in clinical research with almost 38 on going trials active throughout the country. 42 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 43 NOTES 44 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 45 NOTES 46 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 47 NOTES 48 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 49 NOTES 50 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 51 NOTES 52 Oncology & Haematology Conference 2015 NOTES Oncology & Haematology Conference 2015 53 NOTES 54 Oncology & Haematology Conference 2015 QUESTIONS FOR SHELLEY DOLAN Oncology & Haematology Conference 2015 55 QUESTIONS FOR SHELLEY DOLAN KO AWATEA 1 2 3 4 11 12 13 14 107 5 6 7 9 106 10 105 103 102 Exhibition 104 Lecture Theatre 2 101 Technology help Rest Rooms Computer bank an k ute rb Co mp Reheat area Water Station Wishbone Café Area Ground Floor - Korotangi Exhibition Emergency Exit 8 Lecture Theatre 1 Main Entrance Support Building Innovation Centre Computer bank Knowledge Help Venue Floor Plan Ground Floor - Korotangi
© Copyright 2025