Post-Translational Control of Endothelial Nitric Oxide Synthase: Why Isn’t Calcium/Calmodulin Enough?
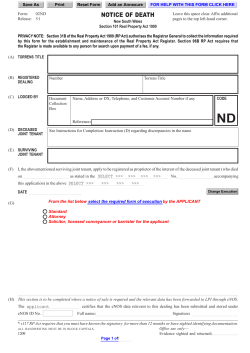
0022-3565/01/2993-818 –824$3.00 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS Copyright © 2001 by The American Society for Pharmacology and Experimental Therapeutics JPET 299:818–824, 2001 Vol. 299, No. 3 900046/942728 Printed in U.S.A. Perspectives in Pharmacology Post-Translational Control of Endothelial Nitric Oxide Synthase: Why Isn’t Calcium/Calmodulin Enough? DAVID FULTON, JEAN-PHILIPPE GRATTON, AND WILLIAM C. SESSA Department of Pharmacology and Molecular Cardiobiology Program, Boyer Center for Molecular Medicine, Yale University School of Medicine, New Haven, Connecticut Received February 2, 2001; accepted May 25, 2001 This paper is available online at http://jpet.aspetjournals.org ABSTRACT Endothelial nitric oxide synthase (eNOS) is important for cardiovascular homeostasis, vessel remodeling, and angiogenesis. Given the impact of endothelium- derived nitric oxide (NO) in vascular biology, much work in the past several years has focused on the control of NO synthesis by regulatory proteins that influence its function. Indeed calcium-activated calmodulin Endothelium-derived nitric oxide (NO), the classic relaxing factor discovered by Furchgott in 1980, is produced by the enzyme endothelial nitric oxide synthase (eNOS). Early observations by pharmacologists studying endothelium-dependent relaxations of blood vessels and the release of relaxing factor by cultured endothelial cells demonstrated that removal of extracellular calcium from media solutions blocked agonist-induced release of NO, suggesting that calcium was important for the release of endothelium-derived NO (Singer and Peach, 1982; Forstermann et al., 1991). Additional studies using broken cell systems documented that calcium removal or antagonism of calmodulin (CaM) with inhibitors blocked the generation of NO and NOS activity, suggesting that eNOS was a calcium-calmodulin-requiring enzyme (Busse and Mulsch, 1990; Forstermann et al., 1991). The requirement for calcium-calmodulin was proven upon purification of eNOS to homogeneity (Pollock et al., 1991) and rationalized by the This work is supported by grants from the National Institutes of Health (RO1 HL57665, HL61371, and HL64793 to W.C.S.; T32HL10183 to D.F.) and a Grant-in-Aid from the American Heart Association (National Grant to W.C.S.). J.P.G. is the recipient of a fellowship from the Canadian Institutes of Health Research. W.C.S. is an Established Investigator of the American Heart Association. is important for regulation of NOS activity. Herein we discuss why other proteins, in addition to calmodulin, are necessary for eNOS regulation and summarize the biology of negative and positive regulators of eNOS function in vitro, in cells, and in blood vessels. presence of a calmodulin binding motif in the deduced amino acid sequence of the cloned eNOS cDNA. In the past fours years many laboratories have described proteins other than CaM that may negatively or positively impact eNOS function. Insights into the need for additional regulatory proteins important for NO production from endothelial cells stemmed from observations that eNOS was an N-myristoyl protein (Pollock et al., 1992).N-Myristoylation is important for the subcellular targeting of discrete microdomains of cells, and mutations that block N-myristoylation impede proper subcellular targeting and various aspects of signal transduction. Indeed, expression of a nonacylated form of eNOS did not affect enzymatic activity in broken cell lysates but prevented calcium ionophore-stimulated NO release, arguing that additional mechanisms other than CaM, per se, were important for the fidelity of signal transduction coupling to eNOS (Sakoda et al., 1995; Sessa et al., 1995). In addition, the hypothesis that eNOS had to be localized to proper intracellular membranes to be near to other regulatory proteins (scaffolds, chaperones, kinases) provided the rationale for the discovery of additional protein regulators of eNOS function. Described below are putative regulators of eNOS function that have been shown to inhibit or enhance eNOS activity and NO release (Table 1). ABBREVIATIONS: NO, nitric oxide; eNOS, endothelial NO synthase; ACh, acetylcholine; B2, bradykinin 2; CaM, calmodulin; Erk, extracellular signal-related kinase; GA, geldanamycin; GST, glutathione S-transferase; hsp90, heat shock protein 90; ID4, intracellular domain 4; IGF, insulin-like growth factor; NOSIP, nitric oxide synthase interacting protein; PI-3K, phosphatidylinositol 3-kinase; VEGF, vascular endothelial growth factor. 818 Protein-Protein Modulation of NO Release Negative Regulatory Proteins Caveolin. Caveolin, being the major coat protein of caveolae, has several faces that may influence the biology of proteins that localize to cholesterol-rich plasmalemma caveolae. Indeed caveolin-1 is necessary for the biogenesis of caveolae through an unknown mechanism (Smart et al., 1999). In addition, caveolin-1 can serve as a cholesterol binding protein and traffic cholesterol from the endoplasmic reticulum through the Golgi to the plasma membrane. Finally, caveolin has the capacity to directly interact with other intracellular proteins such as c-Src and H-Ras through amino acids 82– 101, the putative scaffolding domain (Smart et al., 1999). Indeed, three groups independently demonstrated that eNOS could directly interact with caveolin-1 or caveolin-3 (Feron et al., 1996; Garcı´a-Carden˜a et al., 1996; Ju et al., 1997). The primary binding region of caveolin-1 for eNOS is within amino acids 60 –101 and, to a lesser extent, amino acids 135–178 (Garcia-Cardena et al., 1997; Ju et al., 1997). Furthermore, the caveolin-eNOS immunocomplex is disrupted in the presence of caveolin scaffolding peptides (amino acids 82–101) (Michel et al., 1997b). eNOS contains a consensus caveolin binding motif (Smart et al., 1999) located within amino acids 350 –358. The importance of the caveolin interaction with eNOS has been most reproducibly demonstrated by the effects of caveolin scaffolding peptides and GST-caveolin on NOS activity. Incubation of pure eNOS with peptides derived from the scaffolding domains of caveolin-1 and -3 result in inhibition of eNOS activity (Garcia-Cardena et al., 1997). In cotransfection experiments, caveolin over-expression in COS-7 cells resulted in a reduction of eNOS activity (Michel et al., 1997b), and a reduction in NO release was also observed (Garcia-Cardena et al., 1997). Furthermore, mutagenesis of the predicted caveolin binding motif within eNOS blocked the ability of caveolin to suppress NO release in these latter experiments (GarciaCardena et al., 1997). The reduction of eNOS activity by caveolin peptides, or over-expressed caveolin, is reversed by exogenous addition of calmodulin, suggesting a reciprocal regulation of eNOS by calmodulin, an activator, and caveolin, an inhibitor (Michel et al., 1997a). Collectively, these overall results suggest that NO production is negatively regulated by interactions with caveolin and that for NO release to occur, the inhibitory clamp by caveolin must be overcome. CaM has been proposed to be solely responsible for the dissociation of eNOS from caveolin (Michel et al., 1997a). However, the relationship between caveolin as an inhibitor of eNOS and CaM as its allosteric modulator has not been examined in light of new findings demonstrating a role for other positive and negative regulators of eNOS activation. Another important issue is that there are no direct data showing more NO release from cells that do not express caveolins or that disruption of the eNOS-caveolin complex can lead to increased or prolonged NO release from cells, fundamental experiments if caveolin-1 truly negatively regulates eNOS and NO release. In Vivo Evidence Supporting the eNOS-Caveolin Interaction. To date, caveolin knockout mice are not available; therefore, examining endothelial function in these mice is not yet feasible. However, recent work using the caveolin scaffolding domain as a surrogate for caveolin has demonstrated that eNOS can be regulated in situ. Exposure of permeabil- 819 ized cardiac myocytes to the caveolin-3 scaffolding domain peptide (amino acids 55–74), but not a scrambled version, antagonized the negative chronotropic actions of carbachol (Feron et al., 1998). Our group recently used a membranepermeable form of the caveolin-1 scaffolding domain (amino acids 82–101) by fusing it to a cell-permeable leader sequence (Bucci et al., 2000a). Exposure of the peptide to blood vessels resulted in uptake into the endothelium and adventitia and blockade of ACh-induced relaxations, with no effect on relaxant responses to sodium nitroprusside or the release of prostacyclin, showing that in an intact blood vessel, the caveolin peptide is a potent inhibitor of eNOS. In addition, the peptide also blocked inflammation in two different models by influencing vascular permeability, suggesting that peptidomimetics may be useful therapeutically. With respect to disease mechanisms that may influence the caveolin/eNOS interaction, there is evidence that in a rat model of cirrhosis, caveolin-1 is over-expressed, more caveolin-1 interacts with eNOS, and the basal and stimulated production of NO is depressed (Shah et al., 1999a), suggesting that this interaction may increase portal pressures and contribute to the disease state. Intracellular Domains of G-Protein-Coupled Receptors. Work by Venema et al. (1996) has shown that the intracellular domain 4 (ID4) of the bradykinin 2 (B2) and the angiotensin II R1 receptors can negatively regulate eNOS activity in vitro (Ju et al., 1998). Indeed, eNOS coprecipitated with the B2 receptor and in vitro interacted with a GST fusion of ID4, and synthetic peptides from ID4 inhibited eNOS activity in a dose-dependent manner in vitro. Mechanistically, the ID4 peptide has been shown to affect NOS catalysis by interference with flavin to heme electron transfer (Golser et al., 2000). The concept that a receptor can directly interact with eNOS is extremely novel, suggesting that signaling, albeit negative signaling to eNOS, can occur in the absence of a G-protein intermediate. However, direct evidence supporting the physiological relevance of this interaction is presently unavailable. NOSIP. NOSIP is the newest protein to interact with eNOS (Dedio et al., 2001). NOSIP is a 34-kDa protein that was initially identified as an eNOS binding partner. The interaction between NOSIP and eNOS has been shown both in vitro and in vivo, and through deletion analysis, NOSIP was shown to bind eNOS between amino acids 366 and 486. Stimulation of cells with calcium ionophore does not change the association of NOSIP and eNOS; however, a peptide derived from the scaffolding domain of caveolin (82–101) is able to displace eNOS from NOSIP. NOSIP does not affect eNOS activity assays in vitro but, when coexpressed in cells, does reduce ionomycin-stimulated NO release. The ability of NOSIP to reduce NO release from intact cells is due to the redistribution of eNOS from the plasma membrane to intracellular compartments. The specificity of NOSIP to eNOS and the true function of NOSIP are not known. Positive Regulatory Proteins Calmodulin. The first protein shown to be involved in eNOS regulation was calmodulin (CaM). Early studies on neuronal NOS and eNOS (Bredt and Snyder, 1990; Forstermann et al., 1991), demonstrated that purified NOS utilized CaM as an activator of NO synthesis. Mechanistically, CaM binding to a canonical CaM binding motif can displace an 820 Fulton et al. TABLE 1 Potential eNOS interacting proteins Protein Agonist Association Effect of Bound Protein References Ju et al., 1997; Michel et al., 1997b Golser et al., 2000 Dedio et al., 2001 Caveolin A23187/bradykinin Decreased/increased Inhibitory B2 receptor NOSIP Calmodulin hsp90 Bradykinin, ionophore Ionomycin ?a VEGF, histamine, shear stress, estrogen Ionomycin Bradykinin Bradykinin Bradykinin Decreased No change ?b Increased Inhibitory Inhibitory Stimulatory Stimulatory Increased Decreased Decreased Decreased Stimulatory Inhibitory Inhibitory N.D. Dynamin-2 Erk 1/2 Raf-1 Akt Venema et al., 1996; GarciaCardena et al., 1998 Cao et al., 2000 Bernier et al., 2000 Bernier et al., 2000 Bernier et al., 2000 N.D., not determined. a It is presumed that more CaM is bound. adjacent autoinhibitory loop on eNOS and neuronal NOS, thus facilitating NADPH-dependent electron flux from the reductase domain of the protein through to the oxygenase domain. The terminal electron acceptor in the oxygenase domain is heme, which can bind oxygen for insertion into the NOS substrate, L-arginine. To date, there are no papers documenting that CaM can actually be recruited to eNOS in a stimulus-dependent manner and that the recruitment occurs contemporaneously with NO release. Pharmacological evidence using inhibitors of CaM or calcium-free buffers have indirectly shown the requirement for CaM. Recent work has shown that eNOS immunoprecipitated from human endothelial cells has immunoreactive CaM bound to it (Russell et al., 2000). Moreover, upon challenge of the cells with estrogen, the amount of CaM recovered in the eNOS immunocomplex does not change. This suggests that CaM may serve as a tightly bound prosthetic group, akin to CaM found in inducible NOS (Cho et al., 1992), and that regulation of the affinity of CaM interactions with NOS may occur through subtle changes in free calcium levels. Heat Shock Protein 90 (hsp90). The hsp90 family is a group of highly conserved stress proteins that are expressed in all eukaryotic cells (Pratt, 1997). Two genes encode hsp90, with the human gene products hsp90␣ and hsp90 having 86% sequence homology. The hsp90 is highly abundant in cells, accounting for 1 to 2% of cytosolic protein, and is localized to the cytoplasm, with a small amount found in the nucleus and cytoskeleton (Pratt, 1997). The main function of hsp90 has been its involvement in a multicomponent chaperone system that is responsible for the proper folding of proteins such as steroid receptors and cell cycle-dependent kinases (Pratt, 1997) However, the abundance of hsp90 associated with newly synthesized proteins suggests that this may not be its only function. There is increasing evidence that hsp90 may be an integral part of signal transduction in all cells. Indeed, hsp90 orthologs are important for tyrosine kinase signaling in Drosophila and receptor-G-protein signaling in yeast. Previously it had been shown that eNOS coprecipitated with a 90-kDa tyrosine-phosphorylated protein, later shown to be hsp90 (Venema et al., 1996; Garcia-Cardena et al., 1998). Indeed, hsp90 was associated with eNOS in resting endothelial cells; and treatment of cells with four distinct stimuli that cause NO release, vascular endothelial growth factor (VEGF), histamine, fluid shear stress, and estrogen, all enhanced the interaction between hsp90 and eNOS in a time frame consistent with NO release (Garcia-Cardena et al., 1998; Russell et al., 2000). The rapid stimulus-dependent formation of the hsp90-eNOS hetero-complexes suggests that it occurs simultaneously with other signaling events such as the mobilization of intracellular calcium and/or protein phosphorylation. The mechanism of how hsp90 regulates eNOS function is less clear. Previously we have shown that hsp90 can directly activate eNOS in vitro (Garcia-Cardena et al., 1998), and coexpression of eNOS with hsp90 in COS cells increased NOS activity in broken cell lysates. These results suggest that hsp90 may act as an allosteric modulator of eNOS by inducing a conformational change in the enzyme that results in increased activity or possibly stabilize the “activation” complex. A recent paper has shown that hsp90 increases CaM affinity for neuronal NOS (Song et al., 2001). Alternatively, hsp90 may act as a scaffold for the recruitment of other regulatory molecules including kinases and phosphatases that may influence eNOS function. Interactions Between Caveolin, CaM, and hsp90. As mentioned previously, CaM has been proposed to be exclusively responsible for the dissociation of eNOS from caveolin. Recently the relationship between caveolin as an inhibitor of eNOS and CaM as its allosteric modulator has been examined in light of hsp90 as an additional regulatory protein. Labeling of endothelial cells with [35S]methionine followed by immunoprecipitation of eNOS resulted in the appearance of several co-associated radiolabeled proteins interacting substoichiometrically with eNOS (Gratton et al., 2000). Western blotting of these immunoprecipitated proteins demonstrated the presence of eNOS, caveolin-1, and hsp90 in the same complex. Moreover, the addition of exogenous CaM weakly displaced caveolin from CaM. Reconstitution of the heterotrimeric complex in vitro showed the eNOS interaction with both hsp90 and caveolin, but the latter proteins did not interact with each other, demonstrating that eNOS was the bridge holding the complex together. Interestingly, the binding of caveolin to eNOS was displaced by the caveolin scaffolding domain peptide, but not by calcium-activated CaM, demonstrating that CaM cannot physically disrupt the eNOS-caveolin complex in vitro. However, hsp90, per se, did not influence the eNOS/caveolin interaction but facilitated the ability of CaM to displace caveolin from eNOS. These data are consistent with two potential models: 1) perhaps the “recruitment or activation” of hsp90 and CaM to eNOS results in weak physical displacement of eNOS from caveolin, Protein-Protein Modulation of NO Release but the complex remains in caveolae; or 2) hsp90 and calcium-activated CaM coexist with eNOS bound to caveolin, and a slight change in eNOS conformation, in the absence of bulk translocation away from caveolin, allows for efficient stimulus-response coupling. In Vivo Evidence Supporting the eNOS-hsp90 Interaction. To study the relationship between hsp90-mediated signaling and NO production, a specific inhibitor of hsp90, the ansamycin antibiotic geldanamycin (GA) was used. GA binds to the unique ATP site of hsp90 and a related protein, GRP94, and influences the conformational stability of hsp90 binding to its substrates (Pratt, 1997). GA attenuated histamine and VEGF-stimulated cGMP production in cultured endothelial cells and blocked ACh-induced vasorelaxation of rat aortic rings (Garcia-Cardena et al., 1998), middle cerebral artery (Khurana et al., 2000), and flow-induced dilation (Viswanathan et al., 1999), indicating that hsp90 signaling was crucial for NO release and endothelial function. Further support for the relevance of hsp90/eNOS interactions in vivo was demonstrated in a model of portal vein ligation in rats (Shah et al., 1999b) and in a model of inflammation (Bucci et al., 2000b). In the former study, the physical interaction of hsp90 with eNOS isolated from the mesenteric microcirculation was documented, and GA attenuated ACh-dependent vasodilatation to the same extent as conventional NOS inhibitors. In portal hypertensive rats, eNOS protein levels are not changed compared with control rats, but NOS activity is markedly enhanced in the mesenteric tissue of hypertensive rats. The enhanced activity correlated with hyporesponsiveness to the vasoconstrictor methoxamine, and GA potentiated the methoxamine-induced vasoconstriction after portal vein ligation, partially reversing the hyporeactivity to this agent, indicating that hsp90 can act as a signaling component leading to NO-dependent responses in the mesenteric microcirculation. In the latter study, GA inhibited inflammation in a dose-dependent manner, an effect as potent as a steroid. Because GA blocks NO release and NOS inhibitors reduce edema formation, it is possible that drugs that specifically inhibit hsp90 will be good anti-inflammatory drugs. Dynamin-2. Dynamin-2 belongs to the family of large GTPases and is believed to be involved in vesicle formation, receptor-mediated endocytosis, caveolae internalization and vesicle trafficking in and out of the Golgi. Dynamin-2 has been shown by confocal microscopy to colocalize with eNOS in the Golgi membranes of endothelial cells and to bind eNOS directly, both in vivo and in vitro (Cao et al., 2000). Previous work by others has documented dynamin-2 in the plasma membrane of endothelial cells, suggesting that, like eNOS, dynamin-2 exists in the plasma membrane and Golgi. Based on extensive in vitro studies, dynamin-2 has an affinity for eNOS in the nanomolar range. In cells, the association between eNOS and dynamin-2 is increased by calcium ionophore, and in in vitro activity assays, dynamin has been shown to directly augment NOS activity. The physiological role of this interaction has yet to be explored. Signaling Kinases: Akt, RAF, and Erk. Immunoprecipitation of eNOS from endothelial cells also results in the coprecipitation of kinases and related proteins including Akt, Erk, and RAF (Michell et al., 1999; Bernier et al., 2000). The interaction of these proteins with eNOS distinguishes them from other protein/protein interactions in that it is the effect of the kinase (phosphorylation) rather than the presence of 821 the protein that influences eNOS activity. The relevance of Akt binding is clear based on in vitro and in vivo evidence describing the phosphorylation site (see below), whereas the phosphorylation by Erk has not been characterized. However, the association of these proteins to eNOS following agonist activation is indicative of a dynamic multiprotein signaling complex influencing eNOS function (i.e., NOS-osome). Protein Phosphorylation. Another post-translational modification that can potentially regulate eNOS activity is through protein phosphorylation (Fig. 1; Table 2). eNOS is primarily phosphorylated on serine residues and to a lesser extent on tyrosine and threonine residues (Michel et al., 1993; Corson et al., 1996; Garcı´a-Carden˜ a et al., 1996). The ability of pharmacological inhibitors of phosphatidylinositol 3-kinase (PI-3K; i.e., wortmannin and LY298004) to reduce insulin- and VEGF-stimulated NO release provided the first evidence that a downstream effector of PI-3K could modulate eNOS activity (Zeng and Quon, 1996; Papapetropoulos et al., 1997). The protein kinase Akt is activated by the 3-phosphorylated inositol lipids generated by PI-3K, and is known to phosphorylate a limited number of cellular substrates according to a distinct substrate motif that is found in eNOS (RXRXXXS/T). Akt can directly phosphorylate recombinant eNOS or eNOS in situ, at serine 1177 (human)/1179 (bovine) (Dimmeler et al., 1999; Fulton et al., 1999; Gallis et al., 1999; Michell et al., 1999). Due to the promiscuous nature of kinase cascades, it is much more difficult to demonstrate that eNOS is a direct Akt substrate in vivo; however, several lines of evidence support this idea. Cotransfection of wild-type Akt and eNOS in COS cells increases eNOS phosphorylation in a wortmannin-sensitive manner and is inhibited by mutation of serine 1177/1179 to alanine (Dimmeler et al., 1999; Fulton et al., 1999). Stimulation of endothelial cells with VEGF and shear stress phosphorylates and activates Akt, and within a similar time frame, eNOS is phosphorylated on serine 1179 in a PI-3K-dependent manner (Dimmeler et al., 1999; Fulton et al., 1999; Gallis et al., 1999; Michell et al., 1999). Aktphosphorylated eNOS is 15- to 20-fold more active than unphosphorylated eNOS (Gallis et al., 1999) or more active at lower levels of calcium or calmodulin (Fulton et al., 1999; Michell et al., 1999). Mutation of serine 1177 to aspartate (S1177D), which mimics the negative charge afforded by phosphorylation, results in an enzyme that is constitutively active at low levels (10 nM) of calcium (Dimmeler et al., 1999), whereas mutation of serine 1177/1179 to an alanine prevents Akt-dependent NO release (Fulton et al., 1999). Adenoviral-mediated gene transfer of constitutively active Akt to endothelial cells markedly increases basal NO release. Activated Akt potentiated and the activation-deficient Akt inhibited VEGF-stimulated NO release by approximately 50 to 70%, similar to levels after wortmannin treatment (Papapetropoulos et al., 1997; Fulton et al., 1999). As stated previously, the subcellular localization of eNOS is crucial for agonist-induced NO release; therefore, we tested whether Akt-dependent activation of eNOS was influenced by its distribution (Fulton et al., 1999). Transfection of cells with a mutant form of eNOS that cannot be acylated prevents the ability of Akt to stimulate NO release, suggesting that eNOS must be membrane-associated for this interaction to occur, and may explain in part the reduction in agonist-induced NO 822 Fulton et al. Fig. 1. Proposed model for eNOS post-translational activation. Top panel represents myristoylated and palmitoylated membrane-bound eNOS under basal condition (less active). eNOS is associated with caveolin-1 and the fourth intracellular domain of the bradykinin (BK) receptor. Also, under basal conditions, a population of eNOS is thought to be associated with heat shock protein 90 (hsp90). Mitogen-activated protein kinase and protein kinase C (PKC) have been proposed to phosphorylate eNOS, which renders it less active. Endothelial cell stimulation by various stimuli (bottom panel) activates eNOS catalysis [i.e., the conversion of L-arginine (L-Arg) to nitric oxide (NO)] through its association with calcium-activated calmodulin (CaM). Whether CaM is always bound and small changes in calcium determine calcium-CaM dependence, more CaM is recruited to eNOS by large fluxes in cytoplasmic calcium, or how phosphorylation influences the calcium/CaM requirements of the enzyme in situ is not known. However, the actions of CaM are thought to be facilitated by the recruitment of hsp90 to eNOS and from the dissociation of eNOS from caveolin. BK receptor activation promotes dissociation of eNOS from the receptor, thus lifting its inhibitory effect. Both calcium-dependent and -independent stimuli have been shown to induce phosphorylation of serine 1177/1179 eNOS. Phosphorylation of this residue by Akt, protein kinase A (PKA), or AMP-dependent kinase (AmpK) is associated with increased enzyme activity. Other proteins have been shown to be associated with increased eNOS activity or NO release such as dynamin (Dyn). The role of nitric oxide synthase-interacting protein (NOSIP) is less clear, but over-expression of this protein mislocalizes eNOS. release from cells where eNOS is mislocalized (Sessa et al., 1995; Liu et al., 1996). Wortmannin does not completely block agonist-induced phosphorylation of eNOS on serine 1177/1179, suggesting that there are other kinases capable of phosphorylating serine 1177/1179. Moreover, there appears to be a discrepancy in the ability of VEGF and IGF-1 to phosphorylate Akt and eNOS. IGF-1 induces greater phosphorylation of Akt relative to VEGF, yet is less effective at phosphorylating eNOS (Michell et al., 1999). Other kinases that phosphorylate serine 1177/1179 are the AMP-activated kinase, which phosphorylates serine 1177 in addition to threonine 495 (Chen et al., 1999), protein kinase A, and protein kinase G (Butt et al., 2000). Inhibition of calcium-calmodulin kinases with KN-62 does not affect serine 1179 phosphorylation and activation of cyclic GMP-dependent kinases with NO or cGMP did not induce phosphorylation of this site (Gallis et al., 1999). It is likely that other kinases capable of phosphorylating serine 1177/1179 remain to be identified. Serine 1177/1179 is not the only eNOS phosphorylation site. For example, shear stress induces the phosphorylation of another site on eNOS, serine 116 (Gallis et al., 1999). The region surrounding this site does not conform to the accepted Akt motif, thus the kinase and the functional significance are Protein-Protein Modulation of NO Release 823 TABLE 2 Potential kinases that phosphorylate eNOS Kinase Site Akt S1177/1179 AMPK PKC PKA PKG ? MAP kinase S1177,a T495 T495 S1177, S633 S1177, S633 S116 ? (not 1177) Agonists eNOS Activity References VEGF, IGF, shear stress, estrogen, simvastatin [AMP]i PMA Iloprost N.D. Shear stress Bradykinin 1 Dimmeler et al., 1999; Fulton et al., 1999; Gallis et al., 1999; Michell et al., 1999 Chen et al., 1999 Michell et al., 1999 Butt et al., 2000 Butt et al., 2000 Gallis et al., 1999 Bernier et al., 2000 1a 2 1 1 ? 2 N.D., not determined. a In the presence of CaM/Ca2⫹. not known. eNOS is also phosphorylated at threonine 495 (497) by AMP-activated kinase and by protein kinase C. Phosphorylation of eNOS at this site reduces eNOS catalytic activity (Chen et al., 1999). Tyrosine phosphorylation of eNOS results in an enzyme with less activity; however, the kinase responsible and the site(s) of phosphorylation are unknown (Garcı´a-Carden˜ a et al., 1996). Given the demonstrated importance of serine 1177/1179, there are still unresolved issues: in particular, the mechanism of why phosphorylation of serine 1179 increases eNOS activity and sensitivity to calcium/calmodulin in intact cells. It has been speculated that this may be due to a conformational change and displacement of an autoinhibitory carboxy tail. Comparison of recombinant wild-type eNOS to an S1179D mutant to mimic the activated state shows that S1179D eNOS is a much more efficient NOS due to enhanced electron flux from the reductase to the oxygenase domain. In addition, the dissociation of CaM is slower than that of wildtype enzyme. The idea that phosphorylation on the carboxy tail removes autoinhibition is supported by the increased activity of truncation mutants of eNOS, terminated at serine 1177 (Chen et al., 1999). It is also possible that phosphorylation influences the relationship between the carboxy tail and the calmodulin-autoinhibitory loop (Fulton et al., 1999). It is unlikely that phosphorylation-induced changes in eNOS activity can be entirely attributed to changes in eNOS-associated proteins because recombinant-phosphorylated eNOS and eNOS S1179D are more active than unphosphorylated eNOS (McCabe et al., 2000). In Vivo Evidence Supporting a Functional Role for eNOS Phosphorylation. A physiological role of endogenous Akt in vasomotor function has been identified in blood vessels. Akt activity in the endothelium of blood vessels was modified by adenoviruses encoding constitutively active Akt, myr-Akt, and a dominant negative Akt, Akt-AA (Luo et al., 2000). In femoral arteries infected with the myr-Akt virus, the resting diameter was significantly larger than control arteries, and the increase in diameter was reversed by Nnitro-L-arginine methyl ester, an inhibitor of nitric oxide synthesis. Also, myr-Akt-infected blood vessels displayed an increase in baseline blood flow. Although dominant negative Akt did not significantly affect resting diameter or blood flow, it did reduce the ability of ACh, but not nitroglycerin, to increase both diameter and blood flow. These data strongly indicate that the Akt-eNOS axis is important for blood flow control in conduit vessels. For several years, the hydroxymethylglutaryl-coenzyme A reductase inhibitors have been shown to provide beneficial cardiovascular actions that are not related to the ability of these drugs to reduce cholesterol. Although statins have been shown to influence eNOS mRNA and protein levels (Laufs and Liao, 1998), the improvement in endothelial function may not entirely be attributed to changes in gene expression (Kaesemeyer et al., 1999). Recently, it has been shown that simvastatin can activate endothelial Akt, leading to an increase in eNOS phosphorylation and NO release (Kureishi et al., 2000). Simvastatin treatment resulted in an increase in endothelial cell survival and angiogenesis in normocholesterolemic animals. Collectively, these results suggest that endogenous Akt can participate in the release of NO from the endothelium in response to agonist stimulation and that increasing Akt activity, either using adenoviruses or simvastatin, can stimulate NO release. Summary Given the fundamental importance of endothelial-derived NO in cardiovascular homeostasis and physiology, elucidation of the enzymatic control mechanisms by the aforementioned protein regulators will increase our understanding of how NO release is controlled in vivo. In addition, perhaps novel insights into the mechanisms of endothelial dysfunction, a manifestation of many cardiovascular diseases, may be attributable to impairments in upstream protein regulators of eNOS function. Note Added in Proof. Recently, two papers have demonstrated enhanced endothelium-dependent responses in mice lacking the gene for caveolin-1 consistent with the concept that caveolin-1 negatively regulates eNOS function (Drab et al., 2001; Razani et al., 2001). References Bernier SG, Haldar S, and Michel T (2000) Bradykinin-regulated interactions of the mitogen-activated protein kinase pathway with the endothelial nitric-oxide synthase. J Biol Chem 275:30707–30715. Bredt DS and Snyder SH (1990) Isolation of nitric oxide synthetase, a calmodulinrequiring enzyme. Proc Natl Acad Sci USA 87:682– 685. Bucci M, Gratton JP, Rudic RD, Acevedo L, Roviezzo F, Cirino G, and Sessa WC (2000a) In vivo delivery of the caveolin-1 scaffolding domain inhibits nitric oxide synthesis and reduces inflammation. Nat Med 6:1362–1367. Bucci M, Roviezzo F, Cicala C, Sessa WC, and Cirino G (2000b) Geldanamycin, an inhibitor of heat shock protein 90 (Hsp90) mediated signal transduction has anti-inflammatory effects and interacts with glucocorticoid receptor in vivo. Br J Pharmacol 131:13–16. Busse R and Mulsch A (1990) Calcium-dependent nitric oxide synthesis in endothelial cytosol is mediated by calmodulin. FEBS Lett 265:133–136. Butt E, Bernhardt M, Smolenski A, Kotsonis P, Frohlich LG, Sickmann A, Meyer HE, Lohmann SM, and Schmidt HH (2000) Endothelial nitric-oxide synthase (type III) is activated and becomes calcium independent upon phosphorylation by cyclic nucleotide-dependent protein kinases. J Biol Chem 275:5179 –5187. Cao S, Yao J, McCabe TJ, Yao Q, Katusic ZS, Sessa WC, and Shah V (2001) Direct interaction between endothelial nitric oxide synthase and dynamin-2: implications for nitric oxide synthase function. J Biol Chem 276:14249 –14256. 824 Fulton et al. Chen ZP, Mitchelhill KI, Michell BJ, Stapleton D, Rodriguez-Crespo I, Witters LA, Power DA, Ortiz de Montellano PR, and Kemp BE (1999) AMP-activated protein kinase phosphorylation of endothelial NO synthase. FEBS Lett 443:285–289. Cho HJ, Xie QW, Calaycay J, Mumford RA, Swiderek KM, Lee TD, and Nathan C (1992) Calmodulin is a subunit of nitric oxide synthase from macrophages. J Exp Med 176:599 – 604. Corson MA, James NL, Latta SE, Nerem RM, Berk BC, and Harrison DG (1996) Phosphorylation of endothelial nitric oxide synthase in response to fluid shear stress. Circ Res 79:984 –991. Dedio J, Konig P, Wohlfart P, Schroeder C, Kummer W, and Muller-Esterl W (2001) NOSIP, a novel modulator of endothelial nitric oxide synthase activity. FASEB J 15:79 – 89. Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, and Zeiher AM (1999) Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature (Lond) 399:601– 605. Drab M, Verkade P, Elger M, Kasper M, Lohn M, Lauterbach B, Menne J, Lindschau C, Mende F, Luft FC, Schedl A, Haller H, and Kurzchalia TV (2001) Loss of caveolae, vascular dysfunction, and pulmonary defects in caveolin-1 genedisrupted mice. Science (Wash DC) 293:2449 –2452. Feron O, Belhassen L, Kobzik L, Smith TW, Kelly RA, and Michel T (1996) Endothelial nitric oxide synthase targeting to caveolae. Specific interactions with caveolin isoforms in cardiac myocytes and endothelial cells. J Biol Chem 271:22810 – 22814. Feron O, Dessy C, Opel DJ, Arstall MA, Kelly RA, and Michel T (1998) Modulation of the endothelial nitric-oxide synthase-caveolin interaction in cardiac myocytes. Implications for the autonomic regulation of heart rate. J Biol Chem 273:30249 – 30254. Forstermann U, Pollock JS, Schmidt HH, Heller M, and Murad F (1991) Calmodulindependent endothelium-derived relaxing factor/nitric oxide synthase activity is present in the particulate and cytosolic fractions of bovine aortic endothelial cells. Proc Natl Acad Sci USA 88:1788 –1792. Fulton D, Gratton JP, McCabe TJ, Fontana J, Fujio Y, Walsh K, Franke TF, Papapetropoulos A, and Sessa WC (1999) Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature (Lond) 399:597– 601. Gallis B, Corthals GL, Goodlett DR, Ueba H, Kim F, Presnell SR, Figeys D, Harrison DG, Berk BC, Aebersold R, and Corson MA (1999) Identification of flow-dependent endothelial nitric-oxide synthase phosphorylation sites by mass spectrometry and regulation of phosphorylation and nitric oxide production by the phosphatidylinositol 3-kinase inhibitor LY294002. J Biol Chem 274:30101–30108. Garcia-Cardena G, Fan R, Shah V, Sorrentino R, Cirino G, Papapetropoulos A, and Sessa WC (1998) Dynamic activation of endothelial nitric oxide synthase by Hsp90. Nature (Lond) 392:821– 824. Garcı´a-Carden˜ a G, Fan R, Stern DF, Liu J, and Sessa WC (1996) Endothelial nitric oxide is regulated by tyrosine phosphorylation and interacts with caveolin-1. J Biol Chem 271:27237–27240. Garcia-Cardena G, Martasek P, Masters BS, Skidd PM, Couet J, Li S, Lisanti MP, and Sessa WC (1997) Dissecting the interaction between nitric oxide synthase (NOS) and caveolin. Functional significance of the nos caveolin binding domain in vivo. J Biol Chem 272:25437–25440. Golser R, Gorren AC, Leber A, Andrew P, Habisch HJ, Werner ER, Schmidt K, Venema RC, and Mayer B (2000) Interaction of endothelial and neuronal nitricoxide synthases with the bradykinin B2 receptor. Binding of an inhibitory peptide to the oxygenase domain blocks uncoupled NADPH oxidation [published erratum appears in J Biol Chem (2000) 275:16400]. J Biol Chem 275:5291–5296. Gratton JP, Fontana J, O’Connor DS, Garcia-Cardena G, McCabe TJ, and Sessa WC (2000) Reconstitution of an endothelial nitric-oxide synthase (eNOS), hsp90, and caveolin-1 complex in vitro. Evidence that hsp90 facilitates calmodulin-stimulated displacement of eNOS from caveolin-1. J Biol Chem 275:22268 –22272. Ju H, Venema VJ, Marrero MB, and Venema RC (1998) Inhibitory interactions of the bradykinin B2 receptor with endothelial nitric-oxide synthase. J Biol Chem 273: 24025–24029. Ju H, Zou R, Venema VJ, and Venema RC (1997) Direct interaction of endothelial nitric-oxide synthase and caveolin-1 inhibits synthase activity. J Biol Chem 272: 18522–18525. Kaesemeyer WH, Caldwell RB, Huang J, and Caldwell RW (1999) Pravastatin sodium activates endothelial nitric oxide synthase independent of its cholesterollowering actions. J Am Coll Cardiol 33:234 –241. Khurana VG, Feterik K, Springett MJ, Eguchi D, Shah V, and Katusic ZS (2000) Functional interdependence and colocalization of endothelial nitric oxide synthase and heat shock protein 90 in cerebral arteries [In Process Citation]. J Cereb Blood Flow Metab 20:1563–1570. Kureishi Y, Luo Z, Shiojima I, Bialik A, Fulton D, Lefer DJ, Sessa WC, and Walsh K (2000) The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals [see comments]. Nat Med 6:1004 –1010. Laufs U and Liao JK (1998) Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem 273:24266 –24271. Liu J, Garcia-Cardena G, and Sessa WC (1996) Palmitoylation of endothelial nitric oxide synthase is necessary for optimal stimulated release of nitric oxide: implications for caveolae localization. Biochemistry 35:13277–13281. Luo Z, Fujio Y, Kureishi Y, Rudic RD, Daumerie G, Fulton D, Sessa WC, and Walsh K (2000) Acute modulation of endothelial Akt/PKB activity alters nitric oxidedependent vasomotor activity in vivo. J Clin Invest 106:493– 499. McCabe TJ, Fulton D, Roman LJ, and Sessa WC (2000) Enhanced electron flux and reduced calmodulin dissociation may explain “calcium-independent” eNOS activation by phosphorylation. J Biol Chem 275:6123– 6128. Michel JB, Feron O, Sacks D, and Michel T (1997a) Reciprocal regulation of endothelial nitric-oxide synthase by Ca2⫹-calmodulin and caveolin. J Biol Chem 272: 15583–15586. Michel JB, Feron O, Sase K, Prabhakar P, and Michel T (1997b) Caveolin versus calmodulin. Counterbalancing allosteric modulators of endothelial nitric oxide synthase. J Biol Chem 272:25907–25912. Michel T, Li GK, and Busconi L (1993) Phosphorylation and subcellular translocation of endothelial nitric oxide synthase. Proc Natl Acad Sci USA 90:6252– 6256. Michell BJ, Griffiths JE, Mitchelhill KI, Rodriguez-Crespo I, Tiganis T, Bozinovski S, de Montellano PR, Kemp BE, and Pearson RB (1999) The Akt kinase signals directly to endothelial nitric oxide synthase. Curr Biol 9:845– 848. Papapetropoulos A, Garcia-Cardena G, Madri JA, and Sessa WC (1997) Nitric oxide production contributes to the angiogenic properties of vascular endothelial growth factor in human endothelial cells. J Clin Invest 100:3131–3139. Pollock JS, Forstermann U, Mitchell JA, Warner TD, Schmidt HH, Nakane M, and Murad F (1991) Purification and characterization of particulate endotheliumderived relaxing factor synthase from cultured and native bovine aortic endothelial cells. Proc Natl Acad Sci USA 88:10480 –10484. Pollock JS, Klinghofer V, Forstermann U, and Murad F (1992) Endothelial nitric oxide synthase is myristylated. FEBS Lett 309:402– 404. Pratt WB (1997) The role of the Hsp90-based chaperone system in signal transduction by nuclear receptors and receptors signaling via MAP kinase. Annu Rev Pharmacol Toxicol 37:297–326. Razani B, Engelman JA, Wang XB, Schubert W, Zhang XL, Marks CB, Macaluso F, Russell RG, Li M, Pestell RG, Di Vizio D, Hou H Jr, Kneitz B, Lagaud G, Christ GJ, Edelmann W, and Lisanti MP (2001) Caveolin-1 null mice are viable but show evidence of hyperproliferative and vascular abnormalities. J Biol Chem 276: 38121–38138. Russell KS, Haynes MP, Caulin-Glaser T, Rosneck J, Sessa WC, and Bender JR (2000) Estrogen stimulates heat shock protein 90 binding to endothelial nitric oxide synthase in human vascular endothelial cells. Effects on calcium sensitivity and NO release. J Biol Chem 275:5026 –5030. Sakoda T, Hirata K, Kuroda R, Miki N, Suematsu M, Kawashima S, and Yokoyama M (1995) Myristoylation of endothelial cell nitric oxide synthase is important for extracellular release of nitric oxide. Mol Cell Biochem 152:143–148. Sessa WC, Garcı´a-Carden˜ a G, Liu J, Keh A, Pollock JS, Bradley J, Thiru S, Braverman IM, and Desai KM (1995) The Golgi association of endothelial nitric oxide synthase is necessary for the efficient synthesis of nitric oxide. J Biol Chem 270:17641–17644. Shah V, Toruner M, Haddad F, Cadelina G, Papapetropoulos A, Choo K, Sessa WC, and Groszmann RJ (1999a) Impaired endothelial nitric oxide synthase activity associated with enhanced caveolin binding in experimental cirrhosis in the rat. Gastroenterology 117:1222–1228. Shah V, Wiest R, Garcia-Cardena G, Cadelina G, Groszmann RJ, and Sessa WC (1999b) Hsp90 regulation of endothelial nitric oxide synthase contributes to vascular control in portal hypertension. Am J Physiol 277:G463–G468. Singer HA and Peach MJ (1982) Calcium- and endothelial-mediated vascular smooth muscle relaxation in rabbit aorta. Hypertension 4:19 –25. Smart EJ, Graf GA, McNiven MA, Sessa WC, Engelman JA, Scherer PE, Okamoto T, and Lisanti MP (1999) Caveolins, liquid-ordered domains, and signal transduction. Mol Cell Biol 19:7289 –7304. Song Y, Zweier JL, and Xia Y (2001) Heat-shock protein 90 augments neuronal nitric oxide synthase activity by enhancing Ca2⫹/calmodulin binding. Biochem J 355: 357–360. Venema VJ, Marrero MB, and Venema RC (1996) Bradykinin-stimulated protein tyrosine phosphorylation promotes endothelial nitric oxide synthase translocation to the cytoskeleton. Biochem Biophys Res Commun 226:703–710. Viswanathan M, Rivera O, and Short BL (1999) Heat shock protein 90 is involved in pulsatile flow-induced dilation of rat middle cerebral artery. J Vasc Res 36:524 – 527. Zeng G and Quon MJ (1996) Insulin-stimulated production of nitric oxide is inhibited by wortmannin. Direct measurement in vascular endothelial cells. J Clin Invest 98:894 – 898. Address correspondence to: Dr. William C. Sessa, Yale University School of Medicine, Boyer Center for Molecular Medicine, Rm 436 D, New Haven, CT 06536. E-mail: william.sessa@yale.edu
© Copyright 2025