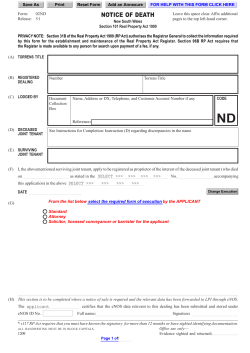
Na /H exchanger is required for hyperglycaemia
Cardiovascular Research (2008) 80, 255–262 doi:10.1093/cvr/cvn179 Na1/H1 exchanger is required for hyperglycaemia-induced endothelial dysfunction via calcium-dependent calpain Shuangxi Wang, Qisheng Peng†, Junhua Zhang‡, and Liying Liu* Department of Pharmacology, Pharmaceutical College, Central South University, 110 Xiang-Ya Road, Changsha, Hunan 410078, China Received 27 February 2008; revised 24 June 2008; accepted 26 June 2008; online publish-ahead-of-print 30 June 2008 Time for primary review: 34 days KEYWORDS Aims Recent studies have reported that the calcium-dependent protease calpain is involved in hyperglycaemia-induced endothelial dysfunction and that the Naþ/Hþ exchanger (NHE) is responsible for an increase in the intracellular calcium (Ca2þ i ) concentration in diabetes. We hypothesized that activation of NHE mediates hyperglycaemia-induced endothelial dysfunction via calcium-dependent calpain. Methods and results Exposure of human umbilical vein endothelial cells (HUVECs) to high glucose (HG, 30 mM D-glucose) time dependently increased both the Ca2þ concentration and calpain activity. i Chelation of free Ca2þ with 1,2-bis (2-aminophenoxy) ethane-N, N, N0 ,N0 -tetraacetic acid abolished the i HG-increased calpain activity. In addition, HG activated NHE in a time-dependent manner, but cariporide, an NHE inhibitor, blocked the HG-induced increase in NHE activity. Furthermore, cariporide or NHE siRNA (small interfering ribonucleic acid) attenuated the HG-induced increases of both Ca2þ i concentration and calpain activity. All of these HG-induced effects in HUVECs, including decreased endothelial nitric oxide synthase (eNOS) activity and NO (nitric oxide) production and increased dissociation of heat shock protein (hsp90) from eNOS, were NHE or calpain reversible. In vivo experiments showed that cariporide treatment via inhibition of NHE activity significantly attenuated the hyperglycaemia-induced impairment of acetylcholine-induced endothelium-dependent relaxation in streptozotocin-injected diabetic rats. Conclusion Activation of NHE via calcium-dependent calpain contributes to hyperglycaemia-induced endothelial dysfunction through dissociation of hsp90 from eNOS. 1. Introduction Diabetes is associated with a significantly increased risk of cardiovascular disease, including atherosclerosis,1 coronary artery disease,2 and microvascular complications.3 Hyperglycaemia is thought to play a key pathogenic role in the development of diabetic cardiovascular disease. High blood glucose concentration results in endothelial dysfunction that is associated with a loss of endothelium-derived nitric oxide (NO), increased vascular permeability, increased endothelial adhesiveness, and thickening of the basement membrane of blood vessels.4 However, the exact mechanism responsible for † Present address. College of Veterinary Medicine, Jilin University, Changchun 130062, China. ‡ Present address. Department of Anesthesiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing 100730, China. * Corresponding author. Tel: þ86 731 471 6249. E-mail address: liyingliu2004@yahoo.com.cn endothelial dysfunction in diabetes remains largely unknown, limiting effective therapeutic interventions. In endothelial cells, NO is produced from L-arginine in the catalysis of endothelial nitric oxide synthase (eNOS). Previous studies5,6 showed that the association of heat shock protein 90 (hsp90) with eNOS plays an important role in the generation of NO in endothelial cells. This process is controlled by calpain because hsp90 is a natural substrate for calpain.7,8 For example, exposure of pulmonary artery endothelial cells to hypoxia triggers calpain-mediated loss of hsp90 from the eNOS complex, resulting in decreased eNOS activity and NO release.9 Recent study by Stalker et al.10,11 has also reported that acute experimental hyperglycaemia up-regulated the endothelial-expressed m-calpain isoform in the microcirculation and induced endothelial dysfunction, however, the mechanism of calpain activation in hyperglycaemia is not fully understood. The Naþ/Hþ exchanger (NHE) is expressed ubiquitously in the plasma membrane of mammalian cells and exchanges Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2008. For permissions please email: journals.permissions@oxfordjournals.org. Downloaded from by guest on December 3, 2014 Naþ/Hþ exchanger; Diabetes; Endothelial function; Calpain; eNOS 256 intracellular Hþ for extracellular Naþ to regulate intracellular pH (pHi) value and the concentration of intracellular Naþ 12 (Naþ The activation of NHE increases Naþ i ). i that leads to Ca2þ overload through the Naþ/Ca2þ exchanger, which is assumed to be the crucial factor in diabetic injuries.13 Inhibition of NHE has been shown to have protective effects against diabetic nephropathy.14 Our previous study has demonstrated that cariporide, an NHE inhibitor, inhibited the high glucose (HG)-induced adhesion of monocytes to endothelial cells.15 These findings support the hypothesis that HG or hyperglycaemia-induced dissociation of hsp90 from eNOS via Ca2þ-dependent calpain is mediated by NHE. Accordingly, the aim of the current study is to investigate if hyperglycaemia-induced endothelial dysfunction is mediated by NHE and Ca2þ/calpain. Our results suggest that hyperglycaemia-induced endothelial dysfunction is due to the activation of NHE via dissociation of hsp90 from eNOS by Ca2þ-dependent calpain. 2. Methods 2.1 Animals 2.2 Materials The NHE inhibitor, cariporide, was kindly provided by Hoechst (Frankfurt, Germany). Calpain inhibitor, ZLLal (benzyloxycarbonyl-leucylleucinal) was from Biomol Research Laboratories, PA, USA. Calcium chelator [1,2-bis (2-aminophenoxy) ethane-N, N, N0 ,N0 -tetraacetic acid (BAPTA)] was obtained from Invitrogen Corporation, CA, USA. Fluorescent indicators, diaminofluorescein (DAF) and 2-carboxyethyl5(6)-carboxyfluorescein were purchased from Calbiochem (CA, USA). Both [3H]L-arginine and [32P]ATP were obtained from NEN (Boston, MA, USA). Streptozotocin (STZ), phenylephrine, acetylcholine (ACh), sodium nitroprusside (SNP), hydroxyethyl piperazine ethanesulphonic acid (HEPES), and other chemicals were purchased from Sigma Chemical Co, MO, USA. Primary antibodies (NHE, hsp90, eNOS, and b-actin), human NHE siRNA (small interfering ribonucleic acid), and control siRNA were obtained from Santa Cruz Biotechnology (CA, USA). All chemicals were of reagent grade. 2.3 Cell culture Human umbilical vein endothelial cells (HUVECs) purchased from the American Type Culture Collection were grown in endothelial basal medium (EBM) (Clonetics Inc., Walkersville, MD, USA) supplemented with 2% fetal bovine serum, 12.5 mg/mL ECGF, 1 mg/ mL hydrocortisone, 100 m/mL penicillin and 100 mg/mL streptomycin. The cells were cultured at 378C in a humidified atmosphere of 5% CO2 and 95% air. Culture medium was replaced twice a week, and cells were subcultured when 80% confluent. Cells at passage 4 were used for all experiments. 2.4 High-glucose treatment of human umbilical vein endothelial cells After reaching 80% confluence, HUVECs were exposed to normal glucose (NG; 5 mM D-glucose), HG (30 mM D-glucose), or hyperosmotic control (HO, 5 mM D-glucose plus 25 mM L-glucose) for different lengths of time with a daily change of culture media. 2.5 Transfection of small interfering ribonucleic acid into human umbilical vein endothelial cells Transient infection of siRNA into cells was carried out according to Santa Cruz’s protocol.16 Briefly, 100 mL transfection medium containing 6 mL siRNA (10 mM) stock solution was added to 100 mL transfection medium containing 6 mL transfection reagent (Lipofectamine 2000, Invitrogen, CA, USA) and mixed gently. After 30 min incubation at room temperature, 200 mL siRNA–lipid complex solution was added to each well (6-well plate) in 1.0 mL transfection medium. After incubation for 6 h at 378C, the medium was replaced with normal medium and cultured for 24–48 h. 2.6 Western blot After treatment, HUVECs were lysated in cell-lysis buffer (Cell Signaling Company, MA, USA). The protein content was assayed by bicinchoninic acid protein assay reagent (Pierce, IL, USA). Twenty microgram of protein was loaded to sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS–PAGE) and then transferred to membrane. Membrane was incubated with a 1:1000 dilution of primary antibody, followed by a 1:2000 dilution of horseradish peroxidase-conjugated secondary antibody. Protein bands were visualized by enhanced chemiluminescence (GE Healthcare, Chicago, IL, USA). The intensity (area density) of the individual bands on western blots was measured by densitometry (model GS-700, Imaging Densitometer; Bio-Rad, CA, USA). The background was subtracted from the calculated area. 2.7 Measurement of intracellular calcium concentration The intracellular calcium (Ca2þ i ) concentration was measured by using a Fluo-4 NW kit from Invitrogen following kit protocol. Briefly, HUVECs were treated as indicated, the cell culture medium was aspirated, washed with HEPES buffer (pH 7.4) once, and 1 mL of HEPES buffer with fluorescent dye was added to cultured cells. After 30 min incubation, fluorescence strength was measured in wavelength of excitation/emission of 485/520 nm. 2.8 Calpain activity The calpain activity was measured by using the fluorogenic peptide Suc-Leu-Leu-Val-Tyr-AMC as a substrate following the procedure described previously with slight modification.17 Shortly, cells were cultured in 24-well plates in EBM with different treatments. After being washed twice with phosphate buffered saline (PBS), fluorogenic peptide was added to a final concentration of 80 mM in PBS. Immediately after addition of fluorogenic peptide, fluorescence was recorded at 2 min intervals for 20 min at excitation 360 nm and emission 460 nm using a Synergy HT Multi-Detection Microplate Reader (BIO-TEK Instruments Inc., VT, USA). The initial rate of peptidyl-AMC hydrolysis was used as the velocity of enzyme activity. 2.9 Determination of Na1/H1 exchanger activity To evaluate NHE activity in HUVECs or rat aortas, the pHi, rate of recovery from an induced acidification, cellular buffer capacity of the HUVECs or rat aortas, and the calibration of the fluorescence to pH values were determined as described previously.14,15 2.10 Endothelial nitric oxide synthase activity assay eNOS activity was monitored by L-[3H]citrulline production from L-[3H]arginine as described previously.18 Briefly, protein samples were incubated in reaction buffer [1 mM L-arginine/100 mM NADPH/1 mM tetrahydrobiopterin/0.2 mCi of L-[3H] arginine Downloaded from by guest on December 3, 2014 Male Sprague–Dawley rats, 180 + 20 g, 6–8 weeks of age, were obtained from the Animal Department of Central South University (Changsha, China). Rats were housed in temperature-controlled cages with a 12 h light–dark cycle and given free access to water and normal feed. The animal protocol was reviewed and approved by the Central South University Institute Animal Care and Use Committee. The current investigation conforms to the Guide for the Care and Use of laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996). S. Wang et al. 257 Hyperglycaemia activates NHE (.66 Ci/mmol) per reaction] for 15 min at 378C, separated by Dowex-50W ion-exchange chromatography in 20 mM HEPES (pH 5.5), 2 mM ethylene-diamine-tetra-acetic acid, and 2 mM ethylene glycol tetra-acetic acid, and the flow-through was used for liquid scintillation counting. and STZ-injected rats were given cariporide (1 mg/kg body weight daily) in their drinking water for 28 days. 2.14 Organ chamber Immunoprecipitations were performed to study the association of eNOS and hsp90 in endothelial cells extracts.19 Cell lysates (500 mg protein) were incubated with anti-eNOS monoclonal antibody for 1 h followed by incubation with pre-washed Protein G-agarose for 2 h. The resulting pellet was washed three times, boiled in SDS sample buffer, and resolved by SDS–PAGE with immunoblot analysis by using primary antibodies against eNOS or hsp90. Organ chamber experiments were performed as described previously.22 Briefly, rings (3–5 mm in length) from rat aortas, free of fat and connective tissue, were mounted in organ bath in 5 mL Kreb’s solution at 378C, gassed with 95%O2 þ 5%CO2, under a tension of 2 g, for 1 h equilibration period. After the equilibration, rings were contracted with 60 mM KCl. After washing and another 30 min equilibration, contractile response was evoked by phenylephrine (1 mM) to elicit reproducible responses. At the plateau of contraction, accumulative ACh (0.003–3 mM) or SNP (0.001 to 1 mM) was added into the organ bath to induce the endotheliumdependent/independent relaxation. 2.12 Detection of nitric oxide 2.15 Apoptosis assay NO production in cultured cells was detected using the fluorescent probe DAF as described previously.20 In brief, before the end of treatment, 10 mM DAF was added to the medium and incubated for 30 min at 378C, then washed with PBS. The DAF fluorescent intensity was recorded by fluorescence spectrometry at the wavelength of excitation (485 nm) and emission (545 nm). After treatment, HUVECs were fixed with 4% paraformaldehyde in PBS. Apoptosis was assessed by terminal deoxynucleotidyl transferase-mediated dUTP nick end labelling (TUNEL) staining (TMR red) using a kit from Roche Applied Science and following the provided instruction manual. The percentage of apoptosis was calculated from the number of TUNEL positive cells divided by the total number of cells counted. 2.11 Association of endothelial nitric oxide synthase with heat shock protein 90 2.13 Streptozotocin-induced diabetes 2.16 Statistical analysis All values are expressed as means + SEM. Data were analysed using a one-way or two-way ANOVA followed by Newman-Student’s t-test. P , 0.05 was considered significant. Figure 1 High glucose (HG) increases intracellular calcium (Ca2þ i ) and calpain activity in human umbilical vein endothelial cells (HUVECs). Cultured HUVECs concentration was detected by Fluo-4 fluorescence. (B) Calpain activity was were incubated with HG (30 mM D-glucose) for 3, 6, 12, 24, and 48 h. (A) Ca2þ i assayed by fluorogenic peptide in situ. (C) HUVECs were incubated with normal glucose (NG, 5 mM D-glucose), HG, or hyperosmotic control (HO, 5 mM 2þ 0 0 D-glucose plus 25 mM L-glucose) for 24 h in presence or absence of BAPTA [1,2-bis (2-aminophenoxy) ethane-N, N, N ,N -tetraacetic acid] (0.5 mM), a Cai chelator, and then calpain activity was detected. Data are expressed by mean + SEM (n ¼ 5). *P , 0.05 vs. Control, #P , 0.05 vs. HG. Downloaded from by guest on December 3, 2014 For induction of diabetes, rats were anaesthetized with ketamine/ xylocaine and injected with a single dose of STZ (60 mg/kg bodyweight in 5 mM pH 4.5 citrate buffer, I.P.).21 Hyperglycaemia is defined as random blood glucose levels of .300 mg/dL. Control 258 3. Results 3.1 High glucose increases intracellular calcium and calpain activity in human umbilical vein endothelial cells Previous studies have demonstrated that calpain is activated by hyperglycaemia via calcium overload and causes endothelial dysfunction.10,11,23 To investigate whether HG alters the activity of calpain and Ca2þ level in HUVECs, both i concentration and calpain activity were determined Ca2þ i in HUVECs incubated with HG (30 mM) at different times. As shown in Figure 1A and B, HG significantly increased both Ca2þ concentration and calpain activity in a timei dependent manner. 3.2 High glucose-induced increase in calpain activity is calcium dependent 3.3 Inhibition of Na1/H1 exchanger abolishes high glucose-induced intracellular calcium and calpain activity Activation of NHE by some pathologic factors, such as ischaemia25 and hypoxia,26 leads to an increased Ca2þ level i and causes cellular damage in the vascular system. Next we determined if the HG-increased Ca2þ-dependent calpain activity is mediated by NHE. HUVECs were treated with HG in absence or presence of cariporide (10 mM) for 24 h. As shown in Figure 2A and B, in both NG and HO groups, inhibition of NHE by cariporide did not change basal calpain activity and Ca2þ level. However, cariporide blocked the i increase in calpain activity and Ca2þ level induced by HG. i In order to further investigate whether the inhibitory effect of cariporide on HG-increased calpain activity is specific to NHE, we used siRNA to silence NHE protein expression. In Figure 2C, specific siRNA of NHE reduced NHE protein expression to 20%, but control siRNA did not change NHE protein expression. In Figure 2D, control siRNA did not block the increase in calpain activity induced by HG, however, NHE siRNA inhibited the HG-increased calpain activity. 3.4 High glucose induces Na1/H1 exchanger activation Since inhibition of NHE by pharmacologic inhibitor or siRNA abolished HG-induced increase in calpain activity, we next Figure 2 Inhibition of Naþ/Hþ exchanger (NHE) by pharmacologic inhibitor or small interfering ribonucleic acid (siRNA) abolishes high glucose (HG)-induced increase in intracellular calcium (Ca2þ i ) level and calpain activity. Human umbilical vein endothelial cells (HUVECs) were incubated with NG (normal glucose), HG or HO (hyperosmotic control) for 24 h in presence or absence of cariporide (10 mM). Cells were subjected to detect (A) calpain activity and (B) concentration of Ca2þ i . Confluent HUVECs were transfected with control siRNA or NHE siRNA and then incubated with HG for 24 h. (C ) NHE siRNA silenced NHE protein expression by western blot. The blot is a representative of five blots obtained from five independent experiments. (D) NHE siRNA abolished HG-induced increase in calpain activity. Data are expressed by mean + SEM (n ¼ 5). *P , 0.05 vs. Control, #P , 0.05 vs. HG. Downloaded from by guest on December 3, 2014 Calpains are a family of Ca2þ-dependent cysteine proteases found in mammals and many lower organisms. In the preconcentration, calpain is actisence of an elevated Ca2þ i vated in endothelial cells.24 We next detected whether the HG-increased calpain activity is dependent on Ca2þ in i HUVECs. As shown in Figure 1C, in NG and HO groups, BAPTA, a Ca2þ remover, did not change basal calpain i activity. However, BAPTA inhibited the enhanced calpain activity induced by HG. S. Wang et al. Hyperglycaemia activates NHE investigated the effects of HG on NHE activity in HUVECs. In Figure 3A, HG increased NHE activity in a time-dependent manner. However, cariporide, a new NHE inhibitor, dosedependently inhibited NHE activity when HUVECs were treated with HG for 24 h (Figure 3B). 3.5 High glucose decreases endothelial nitric oxide synthase activity, association of endothelial nitric oxide synthase with heat shock protein 90 and nitric oxide production One of the main functions of endothelium is to produce NO, which is catalysed by eNOS. We next studied whether HG 259 affected NO production and eNOS activity in HUVECs. In Figure 4A, HG decreased NO release from endothelial cells in a time-dependent manner, associated with a decreased eNOS activity (Figure 4B). There is evidence that hsp90 plays an important role in positively regulating eNOS activity.16,27 We further investigated whether HG decreased eNOS activity by decreasing its association with hsp90. The interaction of hsp90 and eNOS was assayed using immunoprecipitation of eNOS or hsp90 with the specific antibodies. In Figure 4C, exposure of HUVECs to HG up to 30 mM for 24 h did not alter the expression of hsp90 and eNOS. Compared with NG, however, decreased amounts of eNOS were detected when Figure 4 High glucose (HG) decreases nitric oxide (NO) production, endothelial nitric oxide synthase (eNOS) activity, and association of eNOS with heat shock protein (hsp90). (A, B) Human umbilical vein endothelial cells (HUVECs) were incubated with HG (30 mM) for 3, 6, 12, 24, and 48 h. Cell lysates were subjected to detect NO production by DAF (diaminofluorescein) fluorescence and eNOS activity by L-[3H]citrulline production from L-[3H]arginine. Data are expressed by mean + SEM (n ¼ 5). *P , 0.05 vs. Control [or normal glucose (NG)]. (C ) HUVECs were incubated with NG, HO (hyperosmotic control) or HG for 24 h. After treatment, hsp90 or eNOS were first immunoprecipitated from the cell lysates and then detected in western blots with the specific antibody. The blot is a representative of five blots obtained from five independent experiments. Downloaded from by guest on December 3, 2014 Figure 3 High glucose (HG) increases cariporide-sensitive Naþ/Hþ exchanger (NHE) activity. (A) Human umbilical vein endothelial cells (HUVECs) were incubated with HG (30 mM) for 3, 6, 12, 24, and 48 h. (B) HUVECs were incubated with NG (normal glucose), and HG with or without cariporide (1, 10, 100 mM), a selective NHE inhibitor. Cells were subjected to detect NHE activity by NH4Cl pulse method. Data are expressed by mean + SEM (n ¼ 5). *P , 0.05 vs. Control, #P , 0.05 vs. HG. 260 S. Wang et al. hsp90 was immunoprecipitated from HG-treated HUVECs. These results were further corroborated by decreased detection of hsp90 when eNOS was immunoprecipitated from HG-treated cells. 3.6 Inhibition of Na1/H1 exchanger or calpain abolishes high glucose-induced reduction of endothelial nitric oxide synthase activity, association of endothelial nitric oxide synthase with heat shock protein 90, and nitric oxide production Activation of calpain caused hsp90 degradation from eNOS– hsp90 complex, leading to inactivation of eNOS.9 Thus, we further investigated whether NHE or calpain was involved in HG-reduced eNOS association with hsp90. As shown in Figure 5A, inhibition of either NHE with cariporide or calpain with ZLLa1 reversed HG-decreased eNOS activity. Although inhibition of either NHE with cariporide or calpain with ZLLa1 alone did not alter NO production in basal condition, it significantly increased the NO release from HG-treated HUVECs (Figure 5B). In addition, inhibition of either NHE with cariporide or calpain with ZLLa1 restored the association of eNOS with hsp90 (Figure 5C). 3.7 Inhibition of Na1/H1 exchanger with cariporide reverses streptozotocin-induced endothelial dysfunction via apoptosis-independent pathway We next investigated whether cariporide reversed diabetes mellitus-induced endothelial dysfunction in vivo. As shown in Figure 6A, cariporide alone did not change ACh-induced endothelium-dependent relaxation in control rats, however, STZ-induced hyperglycaemia impaired ACh-induced endothelium-dependent relaxation. Furthermore, administration of cariporide in diabetic rats abolished hyperglycaemiaimpaired endothelium-dependent relaxation but had no effects on NO donor-triggered endothelium-independent relaxation (Figure 6B). In order to confirm whether HG activates NHE in rat aorta endothelium, the activity of NHE was assayed in rat aortas. As shown in Figure 6C, STZ-induced hyperglycaemia activates NHE in rat aortas. Administration of cariporide attenuated the hyperglycaemia-increased NHE, but cariporide did not change the NHE activity in control rat aortas. It has been reported that HG-induced apoptosis contributes to endothelial dysfunction in diabetes. In order to study whether apoptosis is involved in the NHE-mediated endothelial dysfunction in diabetes, we detected the apoptosis of endothelial cells treated with HG. We used tumour necrosis factor, TNFa (20 ng/mL), a well-known positive control of apoptosis inducer, and HG to treat HUVECs for 24 h. As shown in Figure 6D, we did not see the increased apoptosis in HG-treated HUVECs. However, TNFa caused HUVECs apoptosis after 24 h incubation without altering NHE activity and the association of eNOS with hsp90 (data not shown). 4. Discussion The current study demonstrates that HG (or hyperglycaemia) via NHE induces vascular endothelial dysfunction by Downloaded from by guest on December 3, 2014 Figure 5 High glucose (HG)-induced reduction of endothelial nitric oxide synthase (eNOS) activity, association of eNOS with heat shock protein (hsp90) or nitric oxide (NO) production is both NHE (Naþ/Hþ exchanger) and calpain dependent. HUVECs (human umbilical vein endothelial cells) were incubated with NG (normal glucose) or HG for 24 h in presence or absence of cariporide (10 mM) or calpain inhibitor [ZLLa1 (benzyloxycarbonyl-leucyl-leucinal), 50 mM]. Cells were used to detect (A) eNOS activity by L-[3H]citrulline production from L-[3H]arginine and (B) NO production by DAF (diaminofluorescein) fluoresence. Data are expressed by mean + SEM (n ¼ 5). *P , 0.05 vs. HG. (C ) After treatment, hsp90 or eNOS were first immunoprecipitated from the cell lysates and detected in western blots with the specific antibody. The blot is a representative of five blots obtained from five independent experiments. Hyperglycaemia activates NHE 261 activating calpain-dependent dissociation of eNOS from hsp90. Not only did inhibition of NHE by a pharmacologic inhibitor, cariporide, reverse HG-induced increase in Ca2þ i concentration and calpain activity, but its actions were also mimicked by silencing of NHE with siRNA. In addition, inhibition of either NHE by cariporide or calpain by ZLLa1 blocked the decrease in eNOS activity and eNOS association with hsp90 caused by HG. Treatment of diabetic mice with cariporide restored endothelial function in vivo. These results strongly suggest that NHE is required for hyperglycaemia-induced endothelial dysfunction via calcium-dependent protease calpain. Recent studies have reported that calpain inhibition exerts anti-inflammatory effects in diabetes. Ruetten et al.28 showed that calpain inhibitors significantly improve leukocyte-endothelium interactions cardiovascular outcome and ameliorate multiple organ dysfunction during endotoxic shock. Similarly, Scalia R et al.29 reported that hyperglycaemia is a major determinant of albumin permeability in diabetic microcirculation via calpain. These studies imply that calpain plays a role in diabetes-induced endothelial dysfunction. Our data clearly indicated that inhibition of NHE by cariporide or siRNA blocked the increase in either calpain activity or Ca2þ concentration caused by i HG and improved endothelial function in diabetic rats. It strongly suggested to us that NHE is essential for hyperglycaemia-induced endothelial dysfunction. To our knowledge, this is the first study to report that inhibition of NHE prevents endothelial dysfunction in diabetes via Ca2þ/calpain-dependent pathway. Our data also clearly indicate that inhibition of NHE abolished HG-induced increase in calpain activity via Ca2þ. The calpains are a family of calcium-dependent proteases that cleave a number of cellular substrates, including kinases, phosphatases, transcription factors, and cytoskeletal proteins.30 In this study, we found that HG increased calpain activity in vascular endothelial cells as well as increased Ca2þ i . In addition, chelation of intracellular free-calcium by BAPTA inhibited the activation of calpain induced by HG. So we speculated that HG-induced calpain activation is calcium dependent because it has been reported that calpain is activated in response to large calcium fluxes.24 To determine whether or not the elevated glucose produced a cariporide-sensitive activation of NHE in endothelial cells, we measured NHE activity in vitro and in vivo. These results showed that HG produced a cariporide-sensitive activation of NHE in endothelial cells. A potential mechanism of glucose-induced increase in NHE activity is a phosphorylationdependent increase in the activity of existing exchangers or the activation of dormant membrane-associated exchangers. Indeed, Sardet et al.31 had demonstrated that the NHE is rapidly phosphorylated in response to various mitogens and concluded that this phosphorylation of the NHE is temporally correlated with its activation. Additional experiments32 support the hypothesis that protein kinase C is one of the kinases responsible for this phosphorylation. Downloaded from by guest on December 3, 2014 Figure 6 Hyperglycaemia-induced endothelial dysfunction via calpain-dependent but apoptosis-independent pathway. Hyperglycaemia was induced by streptozotocin (STZ) in male rats. Cariporide (1 mg/kg body weight daily) was given to rats in their drinking water. Twenty-eight days later, endothelium-dependent/ independent relaxation was detected by organ chamber. (A) Ach (acetylcholine)-induced endothelium-dependent relaxation. (B) SNP (sodium nitroprusside)-induced endothelium-independent relaxation. (C ) Naþ/Hþ exchanger (NHE) activity in rat aortas. (D) HUVECs (human umbilical vein endothelial cells) were incubated with high glucose (HG), and tumour necrosis factor, TNFa (20 ng/mL), for 24 h. Cell apoptosis was detected by TUNEL (terminal deoxynucleotidyl transferase-mediated dUTP nick end labelling) in situ. Data are expressed by mean + SEM (n ¼ 7). *P , 0.05 vs. Control or NG (normal glucose), # P , 0.05 vs. STZ. (E) Proposed scheme of HG-induced endothelial dysfunction mediated by NHE via calpain. 262 In summary, we have demonstrated that diabetic hyperglycaemia activates NHE and results in the increased Ca2þ and calpain activity, which degraded hsp90, a positive i regulator of eNOS activity, and subsequently impaired endothelium-dependent vessel relaxation (Figure 6E). These results are particularly relevant to hyperglycaemic conditions and endothelial dysfunction, both of which are prevalent in type 1 diabetes mellitus. Acknowledgement The authors acknowledge Mrs Vivian for reading proof. Conflict of interest: none declared. Funding This work was supported by National Natural Science Foundation of China (No. 30600248). References 14. Jandeleit-Dahm K, Hannan KM, Farrelly CA, Allen TJ, Rumble JR, Gilbert RE et al. Diabetes-induced vascular hypertrophy is accompanied by activation of Na(þ)-H(þ) exchange and prevented by Na(þ)-H(þ) exchange inhibition. Circ Res 2000;87:1133–1140. 15. Wang SX, Sun XY, Zhang XH, Chen SX, Liu YH, Liu LY. Cariporide inhibits high glucose-mediated adhesion of monocyte-endothelial cell and expression of intercellular adhesion molecule-1. Life Sci 2006;79: 1399–1404. 16. Cheng KK, Lam KS, Wang Y, Huang Y, Carling D, Wu D et al. Adiponectininduced endothelial nitric oxide synthase activation and nitric oxide production are mediated by APPL1 in endothelial cells. Diabetes 2007;56: 1387–1394. 17. Dong Y, Tan J, Cui MZ, Zhao G, Mao G, Singh N et al. Calpain inhibitor MDL28170 modulates Abeta formation by inhibiting the formation of intermediate Abeta46 and protecting Abeta from degradation. FASEB J 2006;20:331–333. 18. Davis BJ, Xie Z, Viollet B, Zou MH. Activation of the AMP-activated kinase by antidiabetes drug metformin stimulates nitric oxide synthesis in vivo by promoting the association of heat shock protein 90 and endothelial nitric oxide synthase. Diabetes 2006;55:496–505. 19. Xu H, Shi Y, Wang J, Jones D, Weilrauch D, Ying R et al. A heat shock protein 90 binding domain in endothelial nitric-oxide synthase influences enzyme function. J Biol Chem 2007;282:37567–37574. 20. Thomas S, Kotamraju S, Zielonka J, Harder DR, Kalyanaraman B. Hydrogen peroxide induces nitric oxide and proteosome activity in endothelial cells: a bell-shaped signaling response. Free Radic Biol Med 2007;42: 1049–1061. 21. Hurdag C, Uyaner I, Gurel E, Utkusavas A, Atukeren P, Demirci C. The effect of alpha-lipoic acid on NOS dispersion in the lung of streptozotocin-induced diabetic rats. J Diabetes Complications 2008;22:56–61. 22. Wang SX, Xiong XM, Song T, Liu LY. Protective effects of cariporide on endothelial dysfunction induced by high glucose. Acta Pharmacol Sin 2005;26:329–333. 23. Scalia R, Gong Y, Berzins B, Zhao LJ, Sharma K. Hyperglycemia is a major determinant of albumin permeability in diabetic microcirculation: the role of mu-calpain. Diabetes 2007;56:1842–1849. 24. Goll DE, Thompson VF, Li H, Wei W, Cong J. The calpain system. Physiol Rev 2003;83:731–801. 25. Toda T, Kadono T, Hoshiai M, Eguchi Y, Nakazawa S, Nakazawa H et al. Naþ/Hþ exchanger inhibitor cariporide attenuates the mitochondrial Ca2þ overload and PTP opening. Am J Physiol Heart Circ Physiol 2007; 293:H3517–H3523. 26. Peters SC, Piper HM. Reoxygenation-induced Ca2þ rise is mediated via Ca2þ influx and Ca2þ release from the endoplasmic reticulum in cardiac endothelial cells. Cardiovasc Res 2007;73:164–171. 27. Miao RQ, Fontana J, Fulton D, Lin MI, Harrison KD, Sessa WC. Dominantnegative Hsp90 reduces VEGF-stimulated nitric oxide release and migration in endothelial cells. Arterioscler Thromb Vasc Biol 2008;28: 105–111. 28. Ruetten H, Thiemermann C. Effect of calpain inhibitor I, an inhibitor of the proteolysis of I kappa B, on the circulatory failure and multiple organ dysfunction caused by endotoxin in the rat. Br J Pharmacol 1997; 121:695–704. 29. McDonald MC, Mota-Filipe H, Paul A, Cuzzocrea S, Abdelrahman M, Harwood S et al. Calpain inhibitor I reduces the activation of nuclear factor-kappa B and organ injury/dysfunction in hemorrhagic shock. FASEB J 2001;15:171–186. 30. Sorimachi H, Ishiura S, Suzuki K. Structure and physiological function of calpains. Biochem J 1997;328:721–732. 31. Sardet C, Counillon L, Franchi A, Pouyssegur J. Growth factors induce phosphorylation of the Naþ/Hþ antiporter, glycoprotein of 110 kD. Science 1990;247:723–726. 32. Williams B, Howard RL. Glucose-induced changes in Naþ/Hþ antiport activity and gene expression in cultured vascular smooth muscle cells. Role of protein kinase C. J Clin Invest 1994;93:2623–2631. Downloaded from by guest on December 3, 2014 1. Colette C, Monnier L. Acute glucose fluctuations and chronic sustained hyperglycemia as risk factors for cardiovascular diseases in patients with type 2 diabetes. Horm Metab Res 2007;39:683–686. 2. Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ. Screening for coronary artery disease in patients with diabetes. Diabetes Care 2007;30:2729–2736. 3. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 2002;287:2570–2581. 4. Stehouwer CD, Lambert J, Donker AJ, van Hinsbergh VW. Endothelial dysfunction and pathogenesis of diabetic angiopathy. Cardiovasc Res 1997; 34:55–68. 5. Garcia-Cardena G, Fan R, Shah V, Sorrentino R, Cirino G, Papapetropoulos A et al. Dynamic activation of endothelial nitric oxide synthase by Hsp90. Nature 1998;392:821–824. 6. Shah V, Wiest R, Garcia-Cardena G, Cadelina G, Groszmann RJ, Sessa WC. Hsp90 regulation of endothelial nitric oxide synthase contributes to vascular control in portal hypertension. Am J Physiol 1999;277:G463–G468. 7. Minami Y, Kimura Y, Kawasaki H, Suzuki K, Yahara I. The carboxy-terminal region of mammalian HSP90 is required for its dimerization and function in vivo. Mol Cell Biol 1994;14:1459–1464. 8. Bellocq A, Doublier S, Suberville S, Perez J, Escoubet B, Fouqueray B et al. Somatostatin increases glucocorticoid binding and signaling in macrophages by blocking the calpain-specific cleavage of Hsp 90. J Biol Chem 1999;274:36891–36896. 9. Su Y, Block ER. Role of calpain in hypoxic inhibition of nitric oxide synthase activity in pulmonary endothelial cells. Am J Physiol Lung Cell Mol Physiol 2000;278:L1204–L1212. 10. Stalker TJ, Gong Y, Scalia R. The calcium-dependent protease calpain causes endothelial dysfunction in type 2 diabetes. Diabetes 2005;54: 1132–1140. 11. Stalker TJ, Skvarka CB, Scalia R. A novel role for calpains in the endothelial dysfunction of hyperglycemia. FASEB J 2003;17:1511–1513. 12. Slepkov ER, Rainey JK, Sykes BD, Fliegel L. Structural and functional analysis of the Naþ/Hþ exchanger. Biochem J 2007;401:623–633. 13. Vial G, Dubouchaud H, Couturier K, Lanson M, Leverve X, Demaison L. Naþ/Hþ exchange inhibition with cariporide prevents alterations of coronary endothelial function in streptozotocin-induced diabetes. Mol Cell Biochem 2008;310:93–102. S. Wang et al.
© Copyright 2025