North East - Health Sciences North
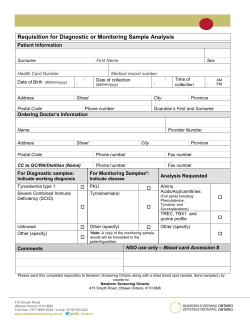
NEW RESOURCES CCO Aboriginal Cancer Control Unit Dr. Annelind Wakegijig, Regional Aboriginal Cancer Lead, Northeast Cancer Centre Cancer Screening Fact Sheets Cancer Care Ontario’s (CCO) Aboriginal Cancer Control Unit (ACCU) has recently released a new patient resource: First Nation, Inuit and Métis Cancer Screening Fact Sheets for breast, cervical and colorectal cancer screening (see insert). The fact sheets were developed in consultation with internal and external stakeholders, and to ensure the information was culturally relevant and welcoming, three sets of fact sheets for each of the cancer screening programs specifically for First Nations, Inuit or Métis people (nine fact sheets in total) were created. Plain language principles were used in the design and the sheets incorporate a variety of visuals, tables, relevant screening statistics, as well as preventative messaging in a clear and concise format. The fact sheets are currently available in English, with additional versions being produced in Inuktitut, Oji-Cree and Ojibway within the next year. CCO has disseminated the fact sheets to all Aboriginal Health Access Centres and regional cancer centres; additionally they will be available on the CCO website (www.cancercare.on.ca) for download in the coming weeks. Requests for hard copies can be made to the Northeast Cancer Centre (NECC) via the North East Oncology News mailbox at neoncologynews@hsnsudbury.ca. Any questions or comments on the new fact sheets can be directed to CCO’s ACCU at accu@cancercare.on.ca. Palliative Care Toolkit ‘Tools for the Journey’ Also recently released from CCO’s ACCU is a new palliative care toolkit - a resource developed for both patients and providers. The kit, entitled ‘Tools for the Journey’, is designed to support the needs of First Nation, Inuit and Métis (FNIM) patients and caregivers experiencing the palliative stage of the cancer journey. The Palliative Care Toolkit content was developed and informed through direct engagement with both FNIM community members and health care providers serving FNIM people in palliative care and features original artwork by an Ojibway artist, created specifically for the project. The Palliative Care Toolkit contains 6 brochures in a pocket folder, with topics including: • • • Understanding the Diagnosis for Patients and Caregivers Taking Care of Your Loved One Guidelines for Working Together • • • What to Expect: Making Decisions and Plans Teachings to Support Grief and Loss (insert) Who to Talk to for Support The ACCU has also developed a complementary resource binder for health care providers. The binder mirrors the brochures, with expanded information on topics including: avoiding caregiver burnout and how to write a will, among others. CCO, through various partnerships, is working on hard copy distribution of the toolkits to Aboriginal Health Access Centres, First Nation Community Health Centres, Métis Community Councils and regional cancer programs. An Oji-Cree translation of the toolkit brochures is planned for next year. The Palliative Care Toolkit will be available for download from the CCO website (www.cancercare.on.ca) in the coming weeks, however if you are interested in a hard copy please contact the NECC Aboriginal Navigator Sherri Baker at: sbaker@hsnsudbury.ca or 705-522-6237 ext. 2175. Any questions or comments on the Palliative Care Toolkit can be directed to CCO’s ACCU at accu@cancercare.on.ca. Palliative Care in First Nations, Inuit and Métis Communities Tools for the Journey North East Oncology News is produced by the Editorial Advisory Board of the Northeast Cancer Centre Editor: Mark Hartman Assistant Editor: Dr. Amanda Hey Advisory Board Members: Dr. M. Bonin, Dr. A. Caycedo, Dr. P. Critchley, Dr. J. Grynspan, Dr. A. Khomani, Dr. A. Knight, C. Mayer, Ph.D, Dr. E. Roberts, Dr. S. Shehata, Dr. S. Shulman, Dr. S. Spadafora & Dr. A. Wakegijig Production Coordinator: Merci Miron-Black Production Assistant: Kyla Young Questions or Comments? Want to join our electronic distribution list? Contact us at neoncologynews@hsnsudbury.ca 41 Ramsey Lake Road - Sudbury, ON - P3E 5J1 Phone: 705.522.6237 - Fax: 705.671.5496 printed on 100% recycled paper visit Cancer Care Ontario on the web at www.cancercare.on.ca visit Health Sciences North|Horizon Santé-Nord on the web at www.hsnsudbury.ca Available online at www.hsnsudbury.ca/NECCprimarycareresources North East Oncology News S trengthening C ommunications As health care knowledge and delivery systems become more complex, it becomes ever more important to have effective, efficient and integrated communication methods amongst health care partners. It is also critical that patients are provided with health care information in a form that is relevant to them and invites them to seek further care if needed. Inside this newsletter you will find examples of how clear documentation on a lab sample can reduce rejection rates and how adoption of a standardized reporting system for mammogram results can clarify clinical management. You’ll also read about how a Northeast Cancer Centre Multidisciplinary Cancer Conference in palliative care, delivered through Ontario Telemedicine Network, allows a community of practice for palliative health care providers to share challenging cases and best practices. You’ll also read about how Cancer Care Ontario’s Aboriginal Cancer Control Unit, following extensive community consultation, has launched public communications regarding cancer screening and palliative care. By continuing to strengthen health care communications, both health care providers and the population they serve will benefit. Mark Hartman Regional Vice President, Northeast Cancer Centre NEW Regional Surgical Oncology Lead I am pleased to have been appointed to the role of Regional Surgical Oncology Lead in North East Ontario, a role that provides leadership to build, foster and maintain a regional surgical oncology program throughout the North East. This role involves working across the region with cancer surgeons, other cancer care providers, hospitals and organizations as well as with the Cancer Care Ontario’s (CCO) Surgical Oncology Program to implement cancer surgery initiatives (guidelines, standards, staging, etc.) and to enhance the cohesion and organization of surgical oncology services across the region. I truly believe that in the North East we have health care professionals, facilities and programs that provide world class surgical oncology care to our population, and I look forward to meeting and working with regional health care colleagues and organizations as we further advance surgical oncology services. I am originally from Colombia, where I attended medical school and trained in general surgery. After practicing for 20 months, I came to Canada to retrain and repeated general surgery at the University of Ottawa and then went to London (Ontario) where I did a clinical fellowship in colorectal surgery. Currently, I am doing a Masters in Clinical Research through the University of Liverpool. I have a strong interest in colorectal and minimally invasive surgery, as well as medical education. Dr. Antonio Caycedo Regional Surgical Oncology Lead, Northeast Cancer Centre Volume 4 Issue 3 Fall 2014 Focus on: Communications INSIDE THIS ISSUE: Strengthening Communications. ...............1 New Regional Surgical Oncology Lead ...................1 Improving the Performance of CCC FOBT Kits...............2 Improving the Communication of Test Results................................3 Multidisciplinary Cancer Conferences: Palliative Care....................................3 New Resources: Aboriginal Cancer Control Unit.............4 Inserts: BI-RADS® Quick Reference Guide Palliative Care MCC Poster Cancer Screening Fact Sheet Teachings to Support Grief and Loss Cancer Screening App North East Oncology News is a triannual publication from the Northeast Cancer Centre providing evidence based guidance, and clinical and operational updates of interest with a focus on Primary Care in North East Ontario. **References used for this issue of North East Oncology News are available upon request from the editor. Articles may be reprinted without permission, provided the source is acknowledged.** IMPROVING the Performance of CCC FOBT Kits IMPROVING the Communication of Test Results Dr. Amanda Hey Regional Primary Care Lead, Northeast Cancer Centre Dr. Evan Roberts Regional Breast Imaging Lead, Northeast Cancer Centre The Guaiac Fecal Occult Blood Test (gFOBT) is the colorectal cancer screening test currently recommended for average risk individuals by ColonCancerCheck (CCC), a joint program of Cancer Care Ontario and the Ministry of Health and Long Term Care, with colonoscopy being recommended for increased risk individuals. The following reviews some gFOBT kit use characteristics in the North East LHIN. North East Characteristic Ontario 2010-11 2013-14 2010-11 2013-14 Use of Non-CCC FOBT kit 22% 11% 15% 9% CCC FOBT kit Rejection Rate 5% 6% 5% 6% Reason for CCC FOBT kit Rejection (% of rejected kits) Not labelled 72% 67% 55% 59% Card expired 3% 15% 2% 11% Specimen expired 16% 9% 18% 10% Data Source: Cancer Care Ontario. (2014). ICS CCC Regional Monthly 2014_09 Report [Unpublished]. Toronto, ON: Evaluation and Reporting, Cancer Screening. CCC FOBT KIT REJECTION RATES There has been a slight increase in the rate of rejection of kits, representing 1216 kits rejected in the North East in 2013-14! The following provides some tips for improving CCC FOBT kit use to optimize quality and reduce rejection of kits. KIT NOT LABELLED, representing 820 kits in the North East in 2013-14. The CCC FOBT card requires labelling with the patient’s name and date of birth. Try ‘point of care’ labelling by health care providers when dispensing the kits AND a clear message to the patient to follow the instructions included in the CCC FOBT kit. CARD EXPIRED, representing 183 kits in the North East in 2013-14. Check your current inventory of CCC FOBT kits to ensure that they are not expired or about to expire. Provide at least 3 months to allow time for the kit to be completed and returned for testing. Advise the patient to complete and return the kit at least a month before it expires AND explain the kit will not be processed if it does expire. SPECIMEN EXPIRED, representing 115 kits in the North East in 2013-14. For lab quality reasons, CCC FOBT kits require lab processing within 21 days of specimen collection. Advise your patient to submit the kit by mail or to a commercial lab drop off box within 10 days of taking the first specimen. USE OF NON-CCC FOBT Kits The use of CCC FOBT kits is recommended to realize the full benefits of an organized program for both patients and primary care providers (PCP). CCC FOBT kits must be ordered through Medical Laboratory Web Address How to Order an affiliated community laboratory for Phlebotomy or dispensing by PCP offices. CCC FOBT LifeLabs www.lifelabs.com Non-phlebotomy Order Form kits are not available for patients to pick up at community or hospital laboratory Gamma Dynacare www.gamma-dynacare.ca CCC FOBT Order Form specimen collection centres. For more information on CCC eligibility please visit: www.cancercare.on.ca/cms/one.aspx?pageId=9921 American College of Radiology BI-RADS® The American College of Radiology (ACR) developed a comprehensive guide for standardized breast imaging terminology and a classification system for mammography, ultrasound and MRI called Breast Imaging Reporting and Data System or ACR BI-RADS®1. This allows results of breast imaging studies to be communicated to the ordering physician/ nurse practitioner (PCP) in a clear fashion with a final assessment that indicates a specific course of action. In North East Ontario, breast imaging radiologists have adopted ACR BI-RADS® for diagnostic mammography and will include an ACR BI-RADS® category at the end of mammography reports. The ACR-BIRADS® Quick Reference insert in this issue will assist ordering PCPs in interpreting the ACR BI-RADS® category. Of note, ACR BI-RADS® Category 3 is used when it is felt that the probability of malignancy is <2% and that a lesion is not expected to change in the suggested interval, but the radiologist would prefer to establish stability. Categories 4 and 5 should be referred for appropriate interventional work-up. The next step is usually a breast image-guided core biopsy (IGCB). Many North East (NE) Ontario mammography sites have arrangements that can facilitate and expedite the pathway to IGCB for the ordering PCP and patient. The Concordance Report When a patient undergoes an IGCB it is important that the radiologist reviews the pathology report and communicates to the ICGB ordering physician whether the results of the imaging exam are explained by the pathology result. This addendum report is often called a ‘concordance’ report. A concordance report will now be issued by NE Ontario radiologists after the pathology report of the IGCB specimen has been reviewed by the radiologist. A care path will be advised (e.g. repeat IGCB, refer for surgical biopsy, return to age appropriate screening). The arrangement for the next steps will depend on the care pathways that have been developed at each of the NE Ontario facilities performing IGCB. American College of Radiology BI-RADS® 4th Edition. ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas; BI-RADS. Reston VA. American College of Radiology, 2003. www.acr.org 1 Multidisciplinary Cancer Conferences: Palliative Care Dr. Andrew Knight, Regional Palliative Care Lead, Northeast Cancer Centre Dr. Patrick Critchley, Regional Primary Care Lead - Northern Districts, Northeast Cancer Centre Multidisciplinary Cancer Conferences (MCCs) were first introduced to the North East about four years ago. Over this time, they have become a very robust forum bringing together on a regular basis multiple specialists from multiple communities via Ontario Telemedicine Network (OTN) to discuss prospectively the optimal management and treatment of newly diagnosed cancer patients. Over the years, for those of us that have been involved in providing palliative care education across the North East, we have been continually challenged in developing a forum that would lend itself for ongoing education. It became obvious to us that the MCC format could provide a vehicle for Continuing Professional Development in palliative care for medical staff and other health professionals. MCC participants are invited to present challenging local palliative care cases for discussion. The format provides participants with an opportunity to review best practices with other primary care providers, local palliative care consultants and specialists. The goal is to help each other better manage challenging palliative cancer cases while building and supporting a palliative primary care provider community of practice. We embarked on our program in February of this year and by June, after three such conferences, had begun to shape a community of practice with regular attendance from health care providers in North Bay, Sault Ste. Marie, Timmins and Sudbury. Resuming in September after our summer break, we now have had our rounds accredited by the College of Family Physicians of Canada, eligible for Mainpro-M1 credits. Our current plan is to continue on a bi-monthly basis (Jan, Mar, May, Jun, Sep, Nov). Please refer to the insert for details of how to participate. If you would like to be added to our distribution list please contact Karen Teddy at kteddy@hsnsudbury.ca. Questions or Comments? Contact us at neoncologynews@hsnsudbury.ca IMPROVING the Performance of CCC FOBT Kits IMPROVING the Communication of Test Results Dr. Amanda Hey Regional Primary Care Lead, Northeast Cancer Centre Dr. Evan Roberts Regional Breast Imaging Lead, Northeast Cancer Centre The Guaiac Fecal Occult Blood Test (gFOBT) is the colorectal cancer screening test currently recommended for average risk individuals by ColonCancerCheck (CCC), a joint program of Cancer Care Ontario and the Ministry of Health and Long Term Care, with colonoscopy being recommended for increased risk individuals. The following reviews some gFOBT kit use characteristics in the North East LHIN. North East Characteristic Ontario 2010-11 2013-14 2010-11 2013-14 Use of Non-CCC FOBT kit 22% 11% 15% 9% CCC FOBT kit Rejection Rate 5% 6% 5% 6% Reason for CCC FOBT kit Rejection (% of rejected kits) Not labelled 72% 67% 55% 59% Card expired 3% 15% 2% 11% Specimen expired 16% 9% 18% 10% Data Source: Cancer Care Ontario. (2014). ICS CCC Regional Monthly 2014_09 Report [Unpublished]. Toronto, ON: Evaluation and Reporting, Cancer Screening. CCC FOBT KIT REJECTION RATES There has been a slight increase in the rate of rejection of kits, representing 1216 kits rejected in the North East in 2013-14! The following provides some tips for improving CCC FOBT kit use to optimize quality and reduce rejection of kits. KIT NOT LABELLED, representing 820 kits in the North East in 2013-14. The CCC FOBT card requires labelling with the patient’s name and date of birth. Try ‘point of care’ labelling by health care providers when dispensing the kits AND a clear message to the patient to follow the instructions included in the CCC FOBT kit. CARD EXPIRED, representing 183 kits in the North East in 2013-14. Check your current inventory of CCC FOBT kits to ensure that they are not expired or about to expire. Provide at least 3 months to allow time for the kit to be completed and returned for testing. Advise the patient to complete and return the kit at least a month before it expires AND explain the kit will not be processed if it does expire. SPECIMEN EXPIRED, representing 115 kits in the North East in 2013-14. For lab quality reasons, CCC FOBT kits require lab processing within 21 days of specimen collection. Advise your patient to submit the kit by mail or to a commercial lab drop off box within 10 days of taking the first specimen. USE OF NON-CCC FOBT Kits The use of CCC FOBT kits is recommended to realize the full benefits of an organized program for both patients and primary care providers (PCP). CCC FOBT kits must be ordered through Medical Laboratory Web Address How to Order an affiliated community laboratory for Phlebotomy or dispensing by PCP offices. CCC FOBT LifeLabs www.lifelabs.com Non-phlebotomy Order Form kits are not available for patients to pick up at community or hospital laboratory Gamma Dynacare www.gamma-dynacare.ca CCC FOBT Order Form specimen collection centres. For more information on CCC eligibility please visit: www.cancercare.on.ca/cms/one.aspx?pageId=9921 American College of Radiology BI-RADS® The American College of Radiology (ACR) developed a comprehensive guide for standardized breast imaging terminology and a classification system for mammography, ultrasound and MRI called Breast Imaging Reporting and Data System or ACR BI-RADS®1. This allows results of breast imaging studies to be communicated to the ordering physician/ nurse practitioner (PCP) in a clear fashion with a final assessment that indicates a specific course of action. In North East Ontario, breast imaging radiologists have adopted ACR BI-RADS® for diagnostic mammography and will include an ACR BI-RADS® category at the end of mammography reports. The ACR-BIRADS® Quick Reference insert in this issue will assist ordering PCPs in interpreting the ACR BI-RADS® category. Of note, ACR BI-RADS® Category 3 is used when it is felt that the probability of malignancy is <2% and that a lesion is not expected to change in the suggested interval, but the radiologist would prefer to establish stability. Categories 4 and 5 should be referred for appropriate interventional work-up. The next step is usually a breast image-guided core biopsy (IGCB). Many North East (NE) Ontario mammography sites have arrangements that can facilitate and expedite the pathway to IGCB for the ordering PCP and patient. The Concordance Report When a patient undergoes an IGCB it is important that the radiologist reviews the pathology report and communicates to the ICGB ordering physician whether the results of the imaging exam are explained by the pathology result. This addendum report is often called a ‘concordance’ report. A concordance report will now be issued by NE Ontario radiologists after the pathology report of the IGCB specimen has been reviewed by the radiologist. A care path will be advised (e.g. repeat IGCB, refer for surgical biopsy, return to age appropriate screening). The arrangement for the next steps will depend on the care pathways that have been developed at each of the NE Ontario facilities performing IGCB. American College of Radiology BI-RADS® 4th Edition. ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas; BI-RADS. Reston VA. American College of Radiology, 2003. www.acr.org 1 Multidisciplinary Cancer Conferences: Palliative Care Dr. Andrew Knight, Regional Palliative Care Lead, Northeast Cancer Centre Dr. Patrick Critchley, Regional Primary Care Lead - Northern Districts, Northeast Cancer Centre Multidisciplinary Cancer Conferences (MCCs) were first introduced to the North East about four years ago. Over this time, they have become a very robust forum bringing together on a regular basis multiple specialists from multiple communities via Ontario Telemedicine Network (OTN) to discuss prospectively the optimal management and treatment of newly diagnosed cancer patients. Over the years, for those of us that have been involved in providing palliative care education across the North East, we have been continually challenged in developing a forum that would lend itself for ongoing education. It became obvious to us that the MCC format could provide a vehicle for Continuing Professional Development in palliative care for medical staff and other health professionals. MCC participants are invited to present challenging local palliative care cases for discussion. The format provides participants with an opportunity to review best practices with other primary care providers, local palliative care consultants and specialists. The goal is to help each other better manage challenging palliative cancer cases while building and supporting a palliative primary care provider community of practice. We embarked on our program in February of this year and by June, after three such conferences, had begun to shape a community of practice with regular attendance from health care providers in North Bay, Sault Ste. Marie, Timmins and Sudbury. Resuming in September after our summer break, we now have had our rounds accredited by the College of Family Physicians of Canada, eligible for Mainpro-M1 credits. Our current plan is to continue on a bi-monthly basis (Jan, Mar, May, Jun, Sep, Nov). Please refer to the insert for details of how to participate. If you would like to be added to our distribution list please contact Karen Teddy at kteddy@hsnsudbury.ca. Questions or Comments? Contact us at neoncologynews@hsnsudbury.ca NEW RESOURCES CCO Aboriginal Cancer Control Unit Dr. Annelind Wakegijig, Regional Aboriginal Cancer Lead, Northeast Cancer Centre Cancer Screening Fact Sheets Cancer Care Ontario’s (CCO) Aboriginal Cancer Control Unit (ACCU) has recently released a new patient resource: First Nation, Inuit and Métis Cancer Screening Fact Sheets for breast, cervical and colorectal cancer screening (see insert). The fact sheets were developed in consultation with internal and external stakeholders, and to ensure the information was culturally relevant and welcoming, three sets of fact sheets for each of the cancer screening programs specifically for First Nations, Inuit or Métis people (nine fact sheets in total) were created. Plain language principles were used in the design and the sheets incorporate a variety of visuals, tables, relevant screening statistics, as well as preventative messaging in a clear and concise format. The fact sheets are currently available in English, with additional versions being produced in Inuktitut, Oji-Cree and Ojibway within the next year. CCO has disseminated the fact sheets to all Aboriginal Health Access Centres and regional cancer centres; additionally they will be available on the CCO website (www.cancercare.on.ca) for download in the coming weeks. Requests for hard copies can be made to the Northeast Cancer Centre (NECC) via the North East Oncology News mailbox at neoncologynews@hsnsudbury.ca. Any questions or comments on the new fact sheets can be directed to CCO’s ACCU at accu@cancercare.on.ca. Palliative Care Toolkit ‘Tools for the Journey’ Also recently released from CCO’s ACCU is a new palliative care toolkit - a resource developed for both patients and providers. The kit, entitled ‘Tools for the Journey’, is designed to support the needs of First Nation, Inuit and Métis (FNIM) patients and caregivers experiencing the palliative stage of the cancer journey. The Palliative Care Toolkit content was developed and informed through direct engagement with both FNIM community members and health care providers serving FNIM people in palliative care and features original artwork by an Ojibway artist, created specifically for the project. The Palliative Care Toolkit contains 6 brochures in a pocket folder, with topics including: • • • Understanding the Diagnosis for Patients and Caregivers Taking Care of Your Loved One Guidelines for Working Together • • • What to Expect: Making Decisions and Plans Teachings to Support Grief and Loss (insert) Who to Talk to for Support The ACCU has also developed a complementary resource binder for health care providers. The binder mirrors the brochures, with expanded information on topics including: avoiding caregiver burnout and how to write a will, among others. CCO, through various partnerships, is working on hard copy distribution of the toolkits to Aboriginal Health Access Centres, First Nation Community Health Centres, Métis Community Councils and regional cancer programs. An Oji-Cree translation of the toolkit brochures is planned for next year. The Palliative Care Toolkit will be available for download from the CCO website (www.cancercare.on.ca) in the coming weeks, however if you are interested in a hard copy please contact the NECC Aboriginal Navigator Sherri Baker at: sbaker@hsnsudbury.ca or 705-522-6237 ext. 2175. Any questions or comments on the Palliative Care Toolkit can be directed to CCO’s ACCU at accu@cancercare.on.ca. Palliative Care in First Nations, Inuit and Métis Communities Tools for the Journey North East Oncology News is produced by the Editorial Advisory Board of the Northeast Cancer Centre Editor: Mark Hartman Assistant Editor: Dr. Amanda Hey Advisory Board Members: Dr. M. Bonin, Dr. A. Caycedo, Dr. P. Critchley, Dr. J. Grynspan, Dr. A. Khomani, Dr. A. Knight, C. Mayer, Ph.D, Dr. E. Roberts, Dr. S. Shehata, Dr. S. Shulman, Dr. S. Spadafora & Dr. A. Wakegijig Production Coordinator: Merci Miron-Black Production Assistant: Kyla Young Questions or Comments? Want to join our electronic distribution list? Contact us at neoncologynews@hsnsudbury.ca 41 Ramsey Lake Road - Sudbury, ON - P3E 5J1 Phone: 705.522.6237 - Fax: 705.671.5496 printed on 100% recycled paper visit Cancer Care Ontario on the web at www.cancercare.on.ca visit Health Sciences North|Horizon Santé-Nord on the web at www.hsnsudbury.ca Available online at www.hsnsudbury.ca/NECCprimarycareresources North East Oncology News S trengthening C ommunications As health care knowledge and delivery systems become more complex, it becomes ever more important to have effective, efficient and integrated communication methods amongst health care partners. It is also critical that patients are provided with health care information in a form that is relevant to them and invites them to seek further care if needed. Inside this newsletter you will find examples of how clear documentation on a lab sample can reduce rejection rates and how adoption of a standardized reporting system for mammogram results can clarify clinical management. You’ll also read about how a Northeast Cancer Centre Multidisciplinary Cancer Conference in palliative care, delivered through Ontario Telemedicine Network, allows a community of practice for palliative health care providers to share challenging cases and best practices. You’ll also read about how Cancer Care Ontario’s Aboriginal Cancer Control Unit, following extensive community consultation, has launched public communications regarding cancer screening and palliative care. By continuing to strengthen health care communications, both health care providers and the population they serve will benefit. Mark Hartman Regional Vice President, Northeast Cancer Centre NEW Regional Surgical Oncology Lead I am pleased to have been appointed to the role of Regional Surgical Oncology Lead in North East Ontario, a role that provides leadership to build, foster and maintain a regional surgical oncology program throughout the North East. This role involves working across the region with cancer surgeons, other cancer care providers, hospitals and organizations as well as with the Cancer Care Ontario’s (CCO) Surgical Oncology Program to implement cancer surgery initiatives (guidelines, standards, staging, etc.) and to enhance the cohesion and organization of surgical oncology services across the region. I truly believe that in the North East we have health care professionals, facilities and programs that provide world class surgical oncology care to our population, and I look forward to meeting and working with regional health care colleagues and organizations as we further advance surgical oncology services. I am originally from Colombia, where I attended medical school and trained in general surgery. After practicing for 20 months, I came to Canada to retrain and repeated general surgery at the University of Ottawa and then went to London (Ontario) where I did a clinical fellowship in colorectal surgery. Currently, I am doing a Masters in Clinical Research through the University of Liverpool. I have a strong interest in colorectal and minimally invasive surgery, as well as medical education. Dr. Antonio Caycedo Regional Surgical Oncology Lead, Northeast Cancer Centre Volume 4 Issue 3 Fall 2014 Focus on: Communications INSIDE THIS ISSUE: Strengthening Communications. ...............1 New Regional Surgical Oncology Lead ...................1 Improving the Performance of CCC FOBT Kits...............2 Improving the Communication of Test Results................................2 Multidisciplinary Cancer Conferences: Palliative Care....................................3 New Resources: Aboriginal Cancer Control Unit.............4 Inserts: BI-RADS® Quick Reference Guide Palliative Care MCC Poster Cancer Screening Fact Sheet Teachings to Support Grief and Loss Cancer Screening App North East Oncology News is a triannual publication from the Northeast Cancer Centre providing evidence based guidance, and clinical and operational updates of interest with a focus on Primary Care in North East Ontario. **References used for this issue of North East Oncology News are available upon request from the editor. Articles may be reprinted without permission, provided the source is acknowledged.** PALLIATIVE Medicine Multidisciplinary Cancer Conference Rounds Frequency: 3rd Tuesday, every 2 months Upcoming Sessions: January 20, March 17, May 19, and June 16, 2015 Tuesday, January 20, 2015 NECC 4 BOARDROOM / OTN 5:00PM TO 6:00PM CHAIR KNIGHT, Andrew PARTICIPATION Come to NECC 4 BOARDROOM / OTN for 5:00PM or if outside of the NECC/HSN, please contact your Telehealth Coordinator for location details. CASE SUBMISSION If you would like to present a case at these rounds, please contact Dr. Andrew Knight (aknight@hsnsudbury.ca) DESCRIPTION AND OBJECTIVES This session will provide participants with an opportunity to review best practices with other primary care providers and local experts. The goal is to help each other better manage challenging palliative cancer cases in northeastern Ontario. AUDIENCE Family and Palliative Physicians, Nurse Practitioners. Other disciplines may be invited according to the case presented: Surgeons, Pathologists, Radiologists, Medical and Radiation Oncologists, Nurses and other Allied Healthcare Practitioners. HOW TO PARTICIPATE Please contact Karen Teddy to register your site. Please see the list below of current participating sites for this event. SUDBURY Location: NECC 4 BOARDROOM / OTN Contact: Karen Teddy Email: kteddy@hsnsudbury.ca NORTH BAY Contact: Deb Hunt Email: telemed@nrbrhc.on.ca SAULT STE. MARIE Contact: Telehealth Coordinators Email: TeleHealthCoord@sah.on.ca TIMMINS Location: System 05 Contact: Diane Veilleux Email: dveilleux@tadh.com PCVC (Personal Computer Video Conferencing) Contact: OTN Website: http://otn.ca/en/services/pcvc This program meets the accreditation criteria of The College of Family Physicians of Canada and has been accredited for up to 1.0 Mainpro‐M1 credits as approved by the Continuing Education and Professional Development Office at the Northern Ontario School fo Medicine PALLIATIVE MCCs are an accredited group learning activity as defined by the Maintenance of Certification Program of The Royal College of Physicians and Surgeons of Canada. Honouring the First Nations Path of Well-being WHAT IS CANCER SCREENING? Cancer screening means taking a test that can find cancer before you have any symptoms. Finding cancer early is one of the best ways we have of beating it. Getting screened regularly leads to healthier and happier lives for you, your family, and your community. WHAT IS THE COLONCANCERCHECK PROGRAM? There are different ways to screen for ColonCancerCheck is a screening program in Ontario colorectal cancer. The screening tests in that encourages men and women aged 50 to 74 to the ColonCancerCheck program are: test for colorectal cancer. When you are between the ages of 50 and 74, ColonCancerCheck will send you a letter 1. Fecal Occult Blood Test (FOBT) inviting you to be screened for colorectal cancer and gives you information on how to get screened. • This test is recommended for men and women aged 50 to 74 every 2 What is a Fecal Occult Blood Test (FOBT)? years if they have no symptoms or • The FOBT is a simple test that can be done at home. family history of colorectal cancer. • The test looks for blood in your stool (poop) that can be an indication of colorectal cancer. 2. Colonoscopy • Your health care provider will tell you how to complete the test. This test is recommended for people What happens after I complete my FOBT? with: • Both you and your health care provider will receive the • Symptoms of colorectal cancer results of the test. • A family history of colorectal • If your test is normal (negative) you will receive a cancer (parent, sibling, or child reminder letter from ColonCancerCheck to be screened who has been diagnosed) again in two years. • If your test is abnormal (positive) your health care • A positive (abnormal) FOBT provider will arrange for you to have a colonoscopy. Most people needing more testing will not have colorectal cancer. What is a colonoscopy? • A colonoscopy is procedure where a doctor inserts a long flexible tube into the anus and is extended along the length of the colon. • There is a small camera at the end of the tube to help the doctor see and remove any changes that might be visible. Colorectal Cancer Screening COMMUNITY LEARNING SERIES ➥ Signs and Symptoms What happens after my colonoscopy appointment? • You will be contacted by your primary care provider or specialist with the results of your colonoscopy. • Your primary care provider or specialist will let you know when you need to be screened for colorectal cancer again. In some regions, flexible sigmoidoscopy performed by a registered nurse is also a screening option. This test is similar to a colonoscopy, but the tube is shorter and does not look at your entire colon. It generally does not involve being put to sleep and the preparation before the test is simple. It is important to talk to your health care provider about what screening test is right for you. If you do not have a health care provider, you can still get screened! Call Telehealth Ontario at 1-866-828-9213 for more information. Changes in shape of your stool from firm to loose and narrow Urgent feeling to empty bowel Blood in your stool Changes in bowel movement – diarrhea WHAT IS COLORECTAL CANCER? DOES IT AFFECT US? Colorectal cancer is the second leading cause of cancer deaths in Ontario for both men and women. Colorectal cancer is a type cancer that develops in the colon and rectum (also known as the large intestine or large bowel). Most colorectal cancers Colon start as small growths (polyps). We Anus know that the number of First Nations Rectum men and women diagnosed with colorectal cancer has dramatically increased. However, if colorectal cancer is found and treated early, there is a 90% chance it can be cured. Screening is the best thing you can do to find colorectal cancer early. ARE YOU AT RISK? Changes in bowel movement – constipation Stomach discomfort ColonCancerCheck program encourages all men and women between the ages of 50 to 74 to be screened for colorectal cancer. Some men and women are at an increased risk of developing colorectal cancer. For example, people with a parent, sibling or child who has been diagnosed with colorectal cancer are at an increased risk. If this applies to you, you should be screened with a colonoscopy when you turn 50 or 10 years earlier than the age that your relative was diagnosed, whichever occurs first. THE PATH TO WELLNESS Constant tiredness and weakness Unexplained weight loss If you experience any of these symptoms, it is important to talk to your health care provider. You may not feel anything if you have colorectal cancer A healthy lifestyle may reduce your chance of getting colorectal cancer, as well as many other diseases. Here are some simple things you can do: • Be smoke free • Maintain a healthy body weight • Limit alcohol • Be physically active • Be sun safe • Eat a healthy diet It is easy to get screened! Talk to your health care provider about what screening test is right for you, or call INFOline at 1-866-410-5853. For more information, please visit: www.ontario.ca/screen forlife Pa l l iat iv e Ca r e in F irst N ations, I n ui t a nd M éti s Com m uni ties Support In Your Community • When we are grieving we might feel that we are to blame for our loved ones being sick, or that we are being punished. No-one knows why they became ill; it is not anyone’s fault For more information about palliative care, talk to your health care provider (e.g. doctor, specialist, or nurse) or community health worker (e.g. home support worker). • When we are grieving there are people who will help take care of things and who will be there for us with compassion and kindness, because grieving is hard work • At some point the grieving will get easier, but the grieving process is a difficult one • We are all on our own journey; we can depend on each other and use our spiritual beliefs as tools to help us Your health care provider or community health worker can also provide more resources with information and support, including information from Cancer Care Ontario and the Canadian Cancer Society. Palliative Care in First Nations, Inuit and Métis Communities Teachings to Support Grief and Loss Pa l l iat iv e Ca r e in F irs t N ations, Inui t a nd M éti s Com m uni ties We Are Not Alone Our Beliefs Respect “Palliative care” is not a common term in First Nations, Inuit and Métis communities. Palliative care is comfort care. It makes a person as comfortable as possible when they have an illness that is unlikely to be cured, and it can also support their family throughout this time. From a traditional Anishinaabe view, the Elders talk about how everything is interconnected; one symbol of this is the medicine wheel. They tell us that we are spiritual beings who come into this world. Our life begins in the eastern door and we journey to the west. As a person passes, they will walk through the western door and return to the spirit world. Dying is a sacred and natural part of life’s journey; it is the final stage of our life when our spirit returns to the Creator. For those who are terminally ill, or for their caregivers, it may be hard to cope with your feelings. It might help to know: For those who have been diagnosed with a terminal illness it might come as a shock to realize that nothing more can be done to cure the illness. People often react with disbelief and do not want to upset their families by telling them. Experiencing grief and loss is very painful. Some of our beliefs and perspectives as First Nations, Inuit and Métis might be helpful and comforting at this time. Many of us share a belief in the Creator or God, and we recognize the Creator in our prayers and ceremonies. We have a spiritual connection to the Creator and our Elders remind us that we are connected to the land and related to all of the living beings around us. Mushkegowuk people as original inhabitants of the land traditionally value harmony, and respect and honour the teachings our Elders and ancestors have shared. The Haudenosaunee traditionally believe in being of good mind and honouring the cycles of life represented by the circle, which is a symbol of unity and strength. When someone passes, their spirit leaves the body and rises to the sky world. There is a shared responsibility for comforting each other in times of loss as well as for celebrating life. The Inuit have a traditional practice where a newborn child is given the name of a relative or community member who has recently passed on, connecting the families. This practice helps the community healing process and the celebration of life. For the Métis, the land sustains the spirits and lives of the people. Death is seen as a spiritual rite of passage that respects the beliefs and values of the individual and their family. The Christian faith has a strong presence in many First Nations, Inuit and Métis communities and can be a source of comfort. • When someone is terminally ill they often want to spend their remaining time at home with family close by • It has been part of our culture as Aboriginal Peoples to look after our own throughout life, from birth to the time of dying. This can be done at home with the right support and equipment, or we can support our loved ones in the hospital or hospice • The person who is terminally ill may want to have time with an Elder, a healer, a priest or a minister, depending on their beliefs. Any of these people can offer spiritual support and ceremonies for the person and the family, depending on their wishes • For the person who is terminally ill, the love and support of those around them can help them to find healing and forgiveness in their life, and share final messages or make memories to leave behind • When the time comes for our loved ones to pass, we can remember that they are more than their physical body; their spirit will be free • When we lose someone we need time to let go of our loved one and to grieve on all levels. There is great support when we are surrounded by our family, our community and our beliefs and customs
© Copyright 2025