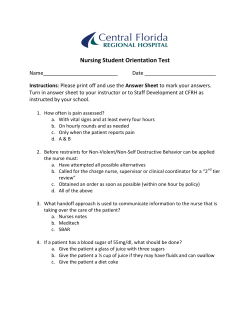
publication PDF - NursingALD.com
The official publication of the West Virginia Nurses Association Volume 18 • No. 1 February, March, April 2015 “Nurses working together for a healthy West Virginia” Quarterly publication direct mailed to approximately 38,000 RNs and LPNs in West Virginia. West Virginia Nurse Anesthetists Never Miss a Beat While Providing Anesthesia Future of Nursing WV Update Page 3 Page 8 President’s Message Aila Accad, MSN, RN WVNA President Dear WVNA Members and Future Members, The past two years as President of WVNA has been exciting and rewarding! I’ve grown personally and professiona lly wh ile making lifelong friends, teaming with the brightest and best nurse leaders in WV and nationally. If you are not a member, you are missing out on the most Aila Accad enriching mentoring and networking you will ever have in your career. While I am stepping down as President this month, I will remain active on the Board as Past President and enjoy my role as the “dancing” emcee for Unity Day 2015. I’ll also be actively involved in supporting our legislative action team to “Remove the Barriers to APRN practice” and help educate our incoming legislators on the essential role of nurses to improve the health of WV as a Nurse Policy Advocate. Nurse Policy Advocates Advocacy is a primary role for nurses and a pillar of our work at WVNA. We advocate for all nurses in order to facilitate their work to improve the health of West Virginians. To support this work, we recruit and train interested members to be Nurse Policy Advocates (NPAs) in each of West Virginia’s seventeen Senatorial Districts. These NPAs establish and maintain relationships as health information resources to the Senators and Delegates in their area. NPA online and conference call training will begin again in January. Beth Baldwin, our incoming Vice President and Past President of WVNA leads the training team which also includes our professional lobbyist, Nancy Tyler, and nurse lobbyists, Angy Nixon, a certified nurse midwife, and Lori Chaffin, staff nurse. If you want to make a significant difference in health policy, being a WVNA NPA is perfect for you. Just contact the office at centraloffice@ wvnurses.org to learn more and enroll for the next training session. Nurse Unity Day ~ This is the Year! We expect nearly one thousand nurses and students to don white lab coats and influence the legislative process this year for Nurses Unity Day at the Capitol. The newly elected President of ANA, Pam Cipriano, will kick the day off as our keynote speaker for the educational session at the Culture Center and lead the march to the Capitol. We will fill the galleries in the House and Senate where proclamations on the important work of WV nurses will be read. Then, we will meet, greet and lunch with legislators in the Capitol rotunda. Awards will be presented along with poster presentations by students and faculty on the past, present and future roles of nurses. WVNA 2nd Vice President, Brenda Keefer, a family nurse practitioner, is Chairperson for Unity Day. Kudos to Brenda and her dedicated team of volunteers who are working diligently to plan and execute this important event! If you want to be part of the most exciting nursing event of the year, I’m sure she would welcome more volunteers. Contact the office for more information. Partnering for Success Removing the Barriers to APRN Practice won the vote to become one of the top ten policy issues for the Healthy Kids and Families Coalition! All of the issues on the Our Children Our Future policy platform are vital to supporting the health and well-being of WV families. WVNA is proud to be a partner and encourage all nurses to get involved in Kids and Family Day at the legislature on January 14. Presort Standard US Postage PAID current resident or Permit #14 Princeton, MN 55371 Your Future “Patients deserve the right care by the right clinician, at the right time, in the right place.” I heard this comment at a conference recently and think it clearly captures the future of your career as a nurse. The Affordable Care Act’s focus on health promotion and wellness is a focus on nursing. Only 3% of the population is in a President’s Message continued on page 2 When Should You Offer Hospice Care? Page 14 Unity Day UNITY DAY 2015: February 25, 2015 Brenda Keefer, RN MSN, APRN, FNP 2nd Vice President WVNA WVNA is delighted to welcome all nurses and student nurses in West Virginia to Unity Day 2015. We will meet at the capitol in Charleston WV. All nursing schools are encouraged to bring student to the state capitol for this yearly event. Students will have poster presentations. Our theme is “Past to present, Evolving Nurses Role, This is the Year.” Your posters are informative to your legislators and the public. We begin Unity Day at the Cultural Center, followed by a unified march to the capitol building. This truly impacts our legislatures to see 500+ at one time, identified as the nursing profession. This certainly demonstrates our influence on health care to West Virginians. We will have opportunities to meet our legislatures, voicing our concerns to the decisions makers for health care in West Virginia. Nurses have a tremendous impact on legislature’s decision making related to health care policies. Lunch will be provided in lower rotunda, along with celebrating leaders in health care with awards for their contribution to nursing. WVNA is working toward creating a learning day for all participants, which you can use throughout your career. For more information contact centraloffice@ wvnurses.org; or call 304-342-1169 Page 2 West Virginia Nurse President’s Message continued from page 1 hospital or long term care facility. The other 97% are people who need nurses to help them get and stay well in the community. New roles for nurses are emerging now and nursing leadership is guiding this healthcare transformation. Our association of members is leading the profession toward a bright future at WVNA. Being a member of your professional association puts you in the right place at the right time to chart the future of your career as a nurse! Go to www.wvnurses.org and become a WVNA member today. Shape the Future … Join WVNA! Warm Regards, Aila Come Join Our Team!! Ever get tired of the fast pace of city life or need to make your child’s ballgame? Come join Webster County Memorial Hospital located in rural WV, within the beautiful mountain lakes region. Join our team at this 15-bed critical access non-profit facility where all employees are family and provide a teamwork approach to care. We offer competitive benefit packages including: student loan reimbursement, vision/dental insurance, discount healthcare for employee/family, flexible hours and salary that is commensurate to experience. ACLS /PALS are preferred. We currently have two registered nurse openings for: Full Time and Part Time. If interested please call Debbie Bragg or Shannon Sigley at 304-847-5682. Webster County Memorial Hospital Serving Webster County & Surrounding Areas Nursing Faculty in Med/Surg Tenure track position with experience teaching Medical-Surgical classes. Minimum Qualifications: Master of Science in Nursing required. Doctorate preferred as well as two years of experience in nursing. Teaching experience desired. How to Apply: Interested applicants may email their curriculum vitae with cover letter and the names and contact information of three references to HR@ab.edu or mail to: Alderson Broaddus University, ATTN: Human Resources-Nursing/Med-Surg Position, 101 College Hill Drive, Box 2004, Philippi, WV 26416 February, March, April 2015 Carefrontation Rose Morton, MSN, RN Nurses care for patients, families, significant others, their own families in a caring manner but often forget that it is important to treat coworkers in a like manner also. Nursing is a stressful profession and tensions can run high in the work environment. Conflict that arises needs to be identified and resolved in the early stage so that the nursing unit/organization can operate efficiently. Confronting someone that you work with on a daily basis is not an easy task. When conflict arises it is necessary to be able to communicate with your co-worker(s). The best practice is to have an openness and willingness. “Creative and successful people want to find balance in their working relationships without feeling angry and misunderstood (Goldsmith, 2009).” Carefrontation is a made-up word that combines caring with confrontation. Everyone working on the unit, in the organization, and within the work environment needs to be committed to being honest and addressing conflict in a caring manner. Carefrontation is not just a made-up word; it’s an attitude that is rooted in wanting “to be part of a successful working relationship that has a spirit of commitment (Goldsmith, 2009).” The spirit behind it and the commitment is that everyone wants their unit/organization/business to grow, to continue to improve, and to enjoy the work. Nurses need to identify conflict and address it in the early stage by confronting in a caring manner; carefrontation. By doing so, they can avoid feelings of anger and feeling misunderstood. Nurses should not use avoidance or competing when conflict occurs because the actual conflict will not be addressed. With carefrontation nurses must be willing to take a risk, share their feelings with their teammates, and begin to master the skill of carefrontation. It can be a valuable gift to share with co-workers (Goldsmith, 2009). Use carefrontation when you care about the other person and need to resolve conflict in a caring manner. Goldsmith, Barton. Office Solutions26.2 (Fall 2009): 42. WVNA Election Results Congratulations to our newly elected WVNA Board Members who will begin their terms in January 2015 President - Evelyn Martin Vice-President - Beth Baldwin Treasurer - Toni Dichiacchio Membership Assembly Representative Denise Campbell Alternates - Aila Accad, Mary Shamblin, Sherry McClalahan West Virginia Nurse Official Publication of the West Virginia Nurses Association 1007 Bigley Avenue, Suite 308 Charleston, WV 25302 Phone: 304.342.1169 or 800.400.1226 Fax: 304.414.3369 Email: centraloffice@wvnurses.org Webpage: www.wvnurses.org Published quarterly every February, May, August and November for the West Virginia Nurses Association, a constituent member of the American Nurses Association. The opinions contained herein are those of the individual authors and do not necessarily reflect the views of the Association. WV Nurse reserves the right to edit all materials to its style and space requirements and to clarify presentations. WVNA Mission Statement The mission of WVNA is to empower the diverse voice of nurses in all settings toward unified focus of nursing knowledge, skill and ability to promote the health & wellbeing of all West Virginians, through education, legislation and health policy. Executive Board Aila Accad, President: ailaspeaks@gmail.com Evelyn Martin, 1st Vice President: emmartin@hsc.wvu.edu Brenda Keefer, 2nd Vice President: bkeefer@aol.com Angy Nixon, Treasurer: anmidwife@netzero.com Susan Rash, Secretary: susierashrn@yahoo.com Beth Baldwin, Immediate Past President and APRN Congress Chair: elbrn6e21@msn.com Sherri Williams, Approver Chair: swilliams@bluefieldstate.edu Joyce Egnor, Approver Co-Chair: jegnor@newriver.edu Patty Hermosilla, District 5: phermosilla@hsc.wvu.edu Shelia Kyle, District 9: skyle@st-marys.org Sam Cotton, WVN-PAC Chair: scotton@hsc.wvu.org WVNA Staff Linda West, Interim Executive Director, centraloffice@wvnurses.org WV Nurse Staff Aila Accad, Managing Editor West Virginia Nurse Copy Submission Guidelines All WVNA members are encouraged to submit material for publication that is of interest to nurses (especially in the following sections: Nightingale Tribute and Members in the News). The material will be reviewed and may be edited for publication. There is no payment for articles published in the West Virginia Nurse. Article submission is preferred in Word Perfect or MS Word format. When sending pictures, please remember to label pictures clearly since the editors have no way of knowing who persons in the photos might be. Copy Submission via email: Only use MS Word for text submission. Please do not embed photos in Word files, send photos as separate jpg files. Approximately 1,600 words equal a full page in the paper. This does not account for headlines, photos, special graphics, pull quotes, etc. Submit material to: West Virginia Nurse PO Box 1946, Charleston, WV 25327 or Email: centraloffice@wvnurses.org For advertising rates and information, please contact Arthur L. Davis Publishing Agency, Inc., 517 Washington Street, PO Box 216, Cedar Falls, Iowa 50613, (800) 626-4081, sales@aldpub.com. WVNA and the Arthur L. Davis Publishing Agency, Inc. reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement. www.wvnurses.org O Published by: Arthur L. Davis Publishing Agency, Inc. Acceptance of advertising does not imply endorsement or approval by the West Virginia Nurses Association of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. WVNA and the Arthur L. Davis Publishing Agency, Inc. shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of WVNA or those of the national or local associations. February, March, April 2015 West Virginia Nurse Page 3 Future of Nursing WV Update Aila Accad, MSN, RN The Future of Nursing WV (FONWV) is now officially a 501c3 non-profit organization. As such the organization can directly accept tax deductible donations and grant funding. Individual and organizational memberships are now available. FONWV has three co-sponsoring organizations: WVNA, WV Organization of Nurse Executives and WV Hospital Association. There are also eight implementation teams which correspond to the key recommendations of the Institute of Medicine Report on the Future of Nursing (2010). Those recommendations focus in three areas, Education, Practice and Leadership. All teams are open for new members. Education The educational initiatives focus on increasing the number of BSN and doctoral prepared nurses along with life-long learning. Ron Moore, MSN, RN, Vice President of Professional Practice and Chief Nursing Officer Charleston Area Medical Center leads the Education Teams. The two largest hospital systems in the state are committed to implementing all BSN nursing staffing and have contracted with local universities to provide the continuing education to achieve this goal. The state Community College ADN programs collaborated on a core curriculum that will facilitate ADN graduates going on for their BSNs in WV. Practice Beth Baldwin, APRN, PNP, BC, a pediatric nurse practitioner in private practice, chairs the initiative to “Removing the Barriers to Nursing Practice.” This team educates the legislature and public about the importance of nurses being able to offer the full scope of their services without restriction. The lobbying required to change the statutes is conducted by WVNA. Mary Fanning, DNP, RN, NEA-BC, Director, Nursing Administration/ Magnet Program Director at WVU Healthcare System is leading a team that is researching, developing and implementing an online system for a successful Transition to Practice Program for graduate nurses in all settings. Leadership The leadership initiatives focus on developing leadership skills for management, board directorship and policy making roles. The teams are lead by Dottie Oakes, MSN, RN, NE-BC, Vice President and Chief Nursing Officer at WVU Healthcare System and Lora Duncan, MSN, RN, Nurse Manager at Charleston Area Medical Center. One of their top priorities is to increase the number of nurses serving on health related boards. To that end, the teams are developing online training modules to better prepare nurses for these leadership positions. Funding To date, FONWV has been an all volunteer organization. With funding we look forward to entering another stage of organizational development that can accelerate our progress. FONWV has received $100,000 in grants and memberships in the last quarter of 2014 and is awaiting a response from Robert Wood Johnson Foundation, which will provide funding for a full time Program Director. We are deeply grateful for all the current financial support for the online Transition to Practice and Leadership Project. That generous support is from: Benedum Foundation, Sisters of St Joseph, Logan Healthcare Foundation, WV Center for Nursing, Valley Health Systems, CAMC and WVU Hospitals. A future membership drive is also in the planning stages for both organizational and individual membership in the Coalition. Meetings & Presentations FONWV sponsored its second annual leadership meeting on October 31at the WV Hospital Association. Aila Accad & Dr. Lou Ann Hartley represent FONWV at Leadership Conference in National leaders met with Phoenix, AZ local team leaders and our newly installed Strategic Advisors for a stimulating day of presentations and planning for the future of nursing to meet the health needs of West Virginians. Co-sponsor representatives Aila Accad (WVNA) and Dr. Lou Ann Hartley (WVONE) presented the FONWV to enthusiastic participants at the WVONE Conference in Morgantown, WV on November 6. Several nursing leaders joined teams at that event. Aila also presented FONWV to the WVNA Board at their annual strategic planning retreat in August and will present the same slide presentation to faculty at WVU School of Nursing in Morgantown on November 18 on the request of the new Dean, Dr. Tara Hulsey. Aila and Lou Ann also attended the National Leadership Conference sponsored by RWJF and AARP in Phoenix AZ November 17-19. They brought back powerful information and networking contacts focused on creating a culture of health through nursing leadership. If you or are interested in becoming a member, learning more or joining a team or if your employer wants to become an organizational member, contact Aila Accad at ailaspeaks@gmail.com. Page 4 West Virginia Nurse February, March, April 2015 Legislative Update Beth Baldwin, APRN, PNP, BC The WV Legislature has been a rapidly moving target that the APRN Congress of WVNA has been diligently working to pin down. The current progression has taken WV APRNs through many legislative channels including testimony at three separate hearings, resulting in Government Organization Subcommittee negotiations. The negotiations focused on the feasibility of changes to the regulatory requirements of APRNs. This has resulted in a continued focus on the major barriers addressed in the original Sunrise/PERD application which are, in order of priority: 1. Removing the written collaborative agreement regulation. The West Virginia Nurses Association (WVNA) believes the regulation of APRNs must always remain under the WV Board of Nursing in its entirety for the many reasons of evidence based practice and to prevent restraint of trade restrictions. 2. Expanding medication prescribing, allowing APRNs to prescribe and monitor medications based on proper practice evidence. The current law is convoluted and cumbersome and does not allow best and timely prescribing of medication to patients as needed to provide the safest, high quality care. This would also allow close monitoring of medications by the health professional providing direct care. 3.Global signatures on documents related to the health care of patients include, but are not limited to DNR, death certificates, various handicapped accessible applications, and others documents paramount to timely and cost effective care delivery. WVNA/APRN Congress requested that the Government Organization subcommittee address legislation related to APRN expansion of scope of practice in view of WV code §30-1A-1: “Legislative findings. The Legislature finds that regulation should be imposed on an occupation or profession only when necessary for the protection of public health and safety. The Legislature further finds that establishing a procedure for reviewing the necessity of regulating an occupation or profession prior to enacting laws for such regulation will better enable it to evaluate the need for the regulation and to determine the least restrictive regulatory alternative consistent with public health and safety.” This is the introductory clause to WV legislative code for regulating professions. It is clearly of the utmost importance to allow freedom of choice to the public as long as professionals are safe within their respective practices. WVNA/APRN Congress has worked to negotiate a proposal on §30-3F-5. Certificate for limited prescriptive authority. This proposal would allow for medication prescribing autonomously after providing the board with evidence that new APRN has continuously held a certificate for prescriptive authority with a determined number of years as a type of “residency” requirement for prescribing medication. In addition, state reciprocity and grandfathering clauses must be present. WVNA would like to express thanks to the Government Organization Subcommittee legislators and legal staff, for taking on the negotiations of the study of the feasibility of changes to the regulatory requirements of APRNs. We further implore the entire new legislature to embrace the evidence presented and address this critical health care need for all West Virginians. To be successful in passing this legislation it is of utmost importance this year to have a large grassroots support of nurses and citizens supporting access to care and freedom of provider choices. WVNA/ APRN congress is moving to motivate support from the WV Future of Nursing (IOM), WV Healthy Kids and Families’ coalition and various nursing and community groups. We are also starting a CLEAR campaign for individual and groups to write to their legislators in support of clearing the way for citizens’ choices in health care. Please get involved, send a letter, and join our efforts now. We need everyone to pitch in for a successful campaign. See letter below as an example. For best impact use light blue envelope available through centraloffice@wvnurses.org. Elizabeth Baldwin, APRN, PNP, BC is the WVNA APRN Chair and association Past President Example of Letter to Legislators (use light blue envelope for best impact) Date________________ Honorable Legislative leaders, I am writing to you in support of retiring outdated barriers to health care in WV. I am a WV citizen and use an APRN as my chosen health care provider. As a citizen, I feel I have a right to clear transparent care. I want my chosen provider to be able to provide my complete care to the full scope and abilities of his/her training without unwarranted barriers. I am asking you to clear the way for her/ him to be able to provide my care to the full extent of their education and training by retiring the written collaborative requirement that blurs the lines of care and adds costly, unnecessary burdens. Next, I am asking that you expand the medication formulary so that WV is NOT the 48th most restrictive state and that my health care provider can clearly prescribe medication when necessary without added stress, timely visits, and travel to obtain recommended therapy. Finally, I request that my chosen care provider be able to clearly sign any documentation that may be required to obtain services I may request or need to promote my wishes, health, and wellness. The path for WV health care needs to be CLEAR and the outdated bureaucratic barriers to healthcare in WV need removed. Please make the CLEAR initiative your number one goal this year for WV health. CLEAR the path to allow access to care for myself and all WV citizens. Thanks for your time and attention to this concern Name____________________________________ Address__________________________________ _________________________________________ Phone___________________________________ Email___________________________________ February, March, April 2015 West Virginia Nurse Page 5 Legislative Update 2015 Health Policy and Legislative Position Statement The West Virginia Nurses Association (WVNA) goal is to support enactment and implementation of policy that will benefit the health and welfare of all citizens. The WVNA strives to provide information, advocacy, representation and protection for the state’s professional nurses. As part of the American Nurses Association (ANA), the organization establishes policies and goals for the profession that form the basis for nursing’s contribution to the advancement of health care policy. awareness and utilizing the full impact of the media; 2. Aggressively addresses leading health indicators including physical activity, obesity, tobacco use, substance abuse, responsible sexual behavior, mental health, injury and violence, environmental quality, immunization, and access to health care (Healthy People, 2020); 3. Provides interdisciplinary patient-centered care, employs evidence-based practice, applies quality improvement, and utilizes informatics (IOM, 2010); 4. Supports professional nurses practicing to the full extent of their education and training. Review existing and proposed state regulations concerning professional nurses to identify those that have anticompetitive effects without contributing to the health and safety of the public (IOM, 2010; FTC, 2012); 5.Supports patient safety though adequate staffing patterns with RN supervision and appropriate delegation of licensed and unlicensed assistive nursing personnel. WVNA supports public policies that: 1. Promote equal access to quality, comprehensive health care for all West Virginians; 2.Promote a commitment to the principle that all persons are entitled to affordable, readily accessible, high quality health care services (AHRQ, 2008; ACA, 2010); 3.Promote reimbursement parity for all health care services including, but not limited to medications, complementary care, reproductive services, and mental health services (ACA, 2010); Legislative Update continued on page 6 I. PROFESSIONAL ISSUES WVNA supports regulatory legislation that: 1. Assures the continued autonomy and full scope of authority of the West Virginia Board of Examiners for Registered Professional Nurses (WVRNB); 2. Supports the licensure, accreditation, certification, and education (LACE) consensus model for Advanced Practice Registered Nurses [(APRNs), Certified Registered Nurse Anesthetist, Certified Nurse Practitioner, Certified Nurse-Midwives and Clinical Nurse Specialist]; 3.Supports Future of Nursing WV Action Coalition in implementing the Institute of Medicine (IOM) recommendations. (IOM, 2010); 4.Promotes APRNs as licensed independent practitioners, promotes full compensation for APRNs, prevents professional liability carriers from limiting coverage that restricts the full APRN scope of practice, and prevents restraint of trade through collaborative requirements (ACNM, 2011; NCSBN, 2008); 5. Improves health care access through retiring restrictions on APRN prescriptive and signature authority. (AANP, 2013); 6.Recognizes the full scope of practice and autonomy of RNs as established by professional licensure and delineated by professional organizations; 7.Promotes the exclusive use of appropriate medically and scientifically correct terminology in proposed legislation; 8.Promote full practice authority for APRNs within their educational standards of practice, specific to the national credentialing standards (NCSBN, 2008). WVNA supports workplace initiatives that: 1. Uphold individual nurses’ right to make moralethical decisions (ANA Code of Ethics, 2010); 2. Recognize the RN as the coordinator for patient care; 3. Improve patient and staff safety with supplied devices to protect the patient and staff from injury; 4. Provide flexible work schedules that lessen the risk of fatigue-related errors; 5.Supports safe staffing initiatives determined by nurses, that take into account patient acuity and that maximize standard quality outcomes; 6. Prohibit forced overtime and fairly compensate RNs and other health care providers utilizing traditional payment scales for overtime hours (ANA Code of Ethics, 2010); 7. Standardize policies and procedures, equipment and medication delivery systems, including but not limited to information technology, to provide seamless care to rural populations; 8. Support unrestricted use of titles appropriate to educational degrees and credentials (e.g., Doctor of Nursing Practice, DNP). II. HEALTH CARE DELIVERY WVNA supports a health care delivery system that: 1. Encourages wellness through education, public Explore Your Career Opportunities at UHC BENEFITS United Hospital Center offers a comprehensive benefits program including a competitive salary, health and life insurance, retirement and TSA plans, vacation and ill time, tuition reimbursement, and a Clinical Ladder for advancement. Please apply online at www.uhcemployment.com Page 6 West Virginia Nurse Conferences and Meetings January 14, 2015 – Kids and Families Day at the Legislature January 22, 2015 – Rural Health Day at the Legislature February 24, 2015 – 4:00-6:00 WVNA Policy Advocate Training Update, Charleston Marriott. Contact centra lof f ice @ w v nu rses.org for information and registration February 24, 2015 – 6:00- 8:00 WVN-PAC Legislative Reception, Charleston Marriott Contact centra lof f ice @ w v nu rses.org for information and registration February 25, 2015 – 8:00-4:00 PM Nurses Unity Day, WV Culture Center and Capitol Register online at wvnurses.org March 5, 2015 – Women’s Day at the Legislature SAVE THE DATE: May 5-6, 2015 - Choosing Wisely Quality Conference, Edgewood Country Club, Charleston, WV The purpose of the conference is to bring together clinicians from across the state to learn about and discuss the Choosing Wisely and other quality improvement initiatives. To get your name on our email list and receive further information about the conference, contact Renate Pore at renatepore@gmail.com. Earn $150/hr! Any Nurse Can Get Certified as a Legal Nurse Consultant in only 2 Days. Register NOW! Atlanta Washington, DC Apr 11 & 12 Apr 18 & 19 Apr 25 & 26 May 30 & 31 .............................. ChattanoogaNashville jurexnurse.com or call (901) 496-5447 February, March, April 2015 Legislative Update Legislative Update continued from page 5 4. Assure that high quality, supportive/palliative, end-of-life care, including effective symptom control and psychosocial and spiritual support, is accessible to all people; 5. Maintain current West Virginia (WV) immunization mandates and ongoing immunization guideline modifications as outlined by the U.S. Centers for Disease Control (CDC, 2012); 6. Encourage senior West Virginians to maintain active, healthy, and independent lifestyles and when desired and needed, have access to quality long-term care; 7.Identify, prevent, and report elder abuse and neglect including physical, mental and financial abuse (WV State Auditor’s Office, 2012); 8.Decrease substance abuse, including drug diversion; 9.Support the safe regulated prescribing of medical marijuana by all prescribing providers as alternative to narcotics and deemed appropriate by the provider; 10.Promote seamless health care delivery through recognition of endorsement by an APRN any WV law or regulation requiring a signature, certification, stamp, verification, affidavit or endorsement by a physician; 11.Recognize the importance of understanding the impact of social media on professional practice and following secure guidelines for patient confidentiality (ANA, 2012). WVNA supports school health initiatives that: 1.Support the Certified School Nurse RN and other nursing healthcare providers in the school setting as the sole administrators of insulin to students with Insulin-Dependent Diabetes Mellitus (IDDM)(Reference WVASN and WV COSN Position Papers); 2.Promote the coordination and linkage of students to a health home including dental care through the Certified School Nurse RN; 3. Promote the role of RN in the enrollment of children and families in health and dental insurance programs; 4.Recognize the Certified School Nurse RN as the coordinator of health care intervention with the authority to make appropriate health care task delegations and assignments within the educational setting and the RN’s scope and ability; 5.Promote every school having a school nurse in collaboration with a school-based clinic to support health promotion and disease management, (Note: a distinct difference in roles exists with the daily educational health support services performed by a Certified School Nurse RN to cover all children in public schools, and performed in a SchoolBased Health Center that provides care to only enrolled patients); 6.Recognize the Certified School Nurse RN as the professional who ensures quality health care instruction for pre-K through 12th grade students, including comprehensive age-appropriate human sexuality education, asthma and diabetes (WVDE School Nurse Needs Assessment 2010); 7.Support Certified School Nurse RNs’ pay parity within educational funding formula for teachers; 8. Promote the community school concept coordinating programs and services to support healthy lifestyles for students, staff, parents and the community for which each school serves (Coalition for Community Schools/CDCCoordinated School Health Programs). III. PATIENT RIGHTS WVNA supports patients’ rights to: 1. Health care as a basic human right; 2. Safe, error-free health care environments; 3.Choice of sources, methods, services, and providers of health care; 4. Privacy and confidentiality; 5.Participation in informed decision making about personal health care, including end-of-life care and reproductive health choices; 6.Information about all treatment options, including the comparative risks and benefits of each presented at the appropriate literacy-level; 7.Transparent information regarding health institution nursing staffing and patient outcome benchmarks; 8.Designate APRNs as their primary licensed independent provider of healthcare. IV. NURSING RETENTION AND RECRUITMENT WVNA supports strategies for retention and recruitment including: 1. Practices that promote a safe, professional work environment; 2.Support strategies and organizations that promote nursing recruitment and retention; 3. Support efforts to secure sources and amounts of funding for: undergraduate and graduate nursing education, continued educational opportunities for promoting qualified faculty, nursing workforce redevelopment programs (ANA, 2010); 4. Initiatives to retain currently practicing nurses and recruit others into the profession; 5.Promote proposals that enhance and recruit nurse educators to attract and retain qualified nursing faculty such as tax incentives and educational loan repayment plans (ANA, 2010); 6.Promote parity of reimbursement for APRN services to encourage and establish health care services for all West Virginians; 7.Peer monitoring and counseling that is confidential and compassionate to protect the public and promote retention of recovering nurses in the workforce (ANA, 2010). V. SOCIAL ISSUES WVNA supports the following: 1.Professional and lay education focusing on social justice issues; 2. Hate crime legislation that addresses violence against vulnerable populations; 3.Legislation focused on prevention of violence and bullying, particularly the protection of vulnerable populations in all venues including social media; 4.Initiatives to screen, educate and reduce public health risks, including but not limited to unclean air and water, harmful health additives and toxins, drug and alcohol impairment, distracted driving, sexually transmitted infections, and ATV/motorcycle helmet use (ex. clean water); 5. Public disclosure and education of environmental health risks in home, work, school, and other public settings (ANA, 2010); 6. Adequate funding, including a tobacco excise tax, to provide smoking prevention, cessation, and educational programs to eliminate tobacco use and environmental tobacco smoke exposure; 7. A mother’s right to breastfeed as an important, basic act of nutrition and nurturing and a child’s right to be breastfed in any venue as a basic human need. Support the establishment of a state law that would protect a mother who breastfeeds her child in any location, public or private (WVBA, 2012); 8. Ongoing recognition and support of WV nurse veterans; 9. Programs developed to identify and treat the high incidence of post-traumatic stress disorder (PTSD) and post-concussive head injuries in the post-war veteran population (e.g., traumatic brain injury or TBI) (AANP, 2012); 10. Access to mental health services for all veterans with supportive opportunities for the highest quality of independent living (AANP, 2012); 11.Promotion of an “all hands inter-professional approach” to disaster planning and rapid response including anticipated readiness to support current communities and potential influx of populations; 12.Support a realistic living minimum wage. February, March, April 2015 West Virginia Nurse Page 7 Your Personal Conduct Outside of Work Can Lead to Discipline from the Nursing Boards Lisa L. Lilly, BSN, RN, JD Many nurses erroneously believe that their board of nursing is only concerned with their clinical abilities and the performance of their professional duties, specifically while on the job or in relation to the nurse-patient relationship. Unfortunately, such a belief is flatly wrong. Nursing boards can take action against a licensee for unprofessional behavior, including activities that are deemed to be in violation of the “morals” and “good-character” provisions of their rules and regulations. These provisions allow discipline for a variety of perceived offenses, even those based solely upon activities in a licensee’s private life or involving only their personal conduct. Nurses must remember that the primary function of a nursing board is not to advocate for their nurse licensees, but rather to protect the citizens of the state from the actions of their nurse licensees. It can be startling to learn of the full breadth and scope of a Board’s powers to not only investigate a nurse, but also to prosecute that nurse, for activities far beyond the four walls of a nurse’s employer and into virtually all areas of a nurse’s private life, seeking out activity in which the Board may find a nurse’s judgment or moral character to be questionable or that the nurse poses a threat to the health, safety and welfare of the public. Many nurses understand that certain behaviors in their personal lives, like using illegal drugs or habitual or excessive alcohol use, can cause problems which extend into their work lives. These problems can directly affect a nurse’s professional abilities, which ultimately results in discipline. However, many nurses do not appreciate that certain behaviors, which may initially appear to be wholly unrelated to patient care, the nurse-client relationship or their professional life can result in disciplinary action by the Board. The most common example and a cautionary tale, is that of off-duty “Nurse Nancy.” Nurse Nancy has an excellent work history, working in ICU at a local hospital for 12 years; she is well-liked and always gets high marks on her evaluations from both supervisors and patients. While attending a birthday dinner for a relative, Nurse Nancy consumed two (2) glasses of wine, but did not feel she was intoxicated. While driving home after dinner, a deer suddenly jumps in front of Nurse Nancy’s car. Nurse Nancy swerves off the road to avoid the deer and runs into a ditch. No one (including the deer) sustain any injuries. A tow truck is called and police respond to this single car accident. The police officer responding smells alcohol on Nurse Nancy’s breath. Nurse Nancy subsequently fails a roadside sobriety test and her blood alcohol level is found to be slightly higher than the legal limit for intoxication. Nurse Nancy is arrested and charged with driving under the influence (“DUI”). She later pleads guilty to a misdemeanor DUI, pays a fine and completes 1-day driving safety course. Nurse Nancy has never had any complaints or disciplinary action filed against her with the Board, but she reports this conviction on her annual nursing license renewal. What will happen to Nurse Nancy? In this scenario, at least at first blush, it doesn’t appear that the Nursing Board should have any reason to be interested in Nurse Nancy’s DUI arrest or subsequent plea, as all happened outside Nurse Nancy’s nursing practice and it did not involve her ability to provide clinical care to her patients. Although Nurse Nancy may have no prior disciplinary action and an excellent work history, without any issues regarding her nursing skills or the care she has rendered to her patients, she is nonetheless at risk for disciplinary action against her nursing license. What could possibly be the grounds for such action? The first and most obvious choice would be related to potential habitual alcohol or drug use by Nurse Nancy. WV Code §30-7-11, states that discipline can be taken against nurses that are “habitually intemperate” or who’s conduct is “derogatory to the morals” of the nursing profession. Professional misconduct is further defined as including being a chronic or persistent alcoholic (19 CSR §3.14.1.n). However, in this instance, Nurse Nancy was evaluated and found not to be addicted to alcohol or drugs and does not have any substance abuse issues. Even so, Nurse Nancy’s license is not in the clear. Nurse Nancy must be prepared to defend her license on the grounds that her behavior was “unprofessional,” in that she put the public in harm’s way by driving while under the influence of alcohol and that she failed to exercise “good professional character,” as required by 19 CSR §3.14.1.o. Moreover, poor Nurse Nancy may also be accused of “morality” violations, specifically that her conduct was “derogatory to the morals or standing” of the nursing profession. WV Code §30-7-11(f). Unprofessional Conduct is a very broad term, encompassing a wide variety of activities, including those in a nurse’s professional capacity, but also in a nurse’s personal life, far beyond employment activities. In Nurse Nancy’s case, even if the nursing board only investigates and then declines prosecution, the process takes many months, it can be expensive and Nurse Nancy will be understandably anxious until the investigation or prosecution is resolved. The best option for dealing with such licensure situations is simply to avoid them. If Nurse Nancy knew the potential career-ending implications of her impaired driving, she assures that she would never have driven after consuming any alcohol. Like alcohol consumption, many other criminal behaviors in a nurse’s personal life can also trigger licensure action. Any criminal conviction or no contest plea can trigger a board investigation, as such convictions can suggest that the nurse’s conduct is derogatory to the morals of the nursing profession, are unethical, dishonorable and that the nurse is likely to defraud, deceive or generally pose a danger to the public. In addition to the DUI discussed above, the types of criminal violations that can trigger an investigation include: public intoxication; failing to pay child support; domestic violence; child/elder abuse or neglect; harassment; stalking; violation of a restraining order; indecent exposure/lewd acts (including public urination and sex acts in public places); assault and battery (fighting); theft (including shoplifting, robbery and burglary); fraud; firearm charges; failure to file tax returns; and, the possession, sale or distribution of controlled substances without legitimate prescription/purpose. There are very specific requirements, outside of patient care, that the nursing board requires of its nurses. Any reported conduct that suggests that a nurse may have poor judgment or lapses in judgment can trigger a Board investigation. Failure to abide by any of the following is considered “professional misconduct.” It is misconduct to “knowingly falsify an application for employment,” including errors of omission, such as leaving out information from that employer who may would be a bad reference. Also dangerous are “exaggerations” or misleading entries of any sort, but particularly dangerous is puffery involving your licensure status, education, clinical experience or skill level. It is also misconduct to submit false information to the Board on any application or other document. This provision includes your yearly renewal documents, which should be answered fully and truthfully. The Board also considers misappropriating medications, supplies or personal items belonging to either a patient or an employer to be misconduct. Consider the risk to your license under this provision, before you are tempted to grab a box of Band-Aids or a handful of pens to take home. Another area of danger in relation to misconduct involves developing personal relationships with current or former patients, likewise for treating people with whom you have a preexisting personal relationship. While in some small communities, it can be difficult to avoid treating people that you know, but the best practice is to hand off responsibility for caring for this client to another nurse without any personal connections to the patient. While sexual relationships are typically what come to mind when “personal relationships” are at issue, violations in this area, more commonly occur when a nurse becomes over involved in a patient’s personal or family life. A nurse should strive to keep the nurse-client relationship in the therapeutic range, with neither too little nor too much involvement into the client’s “outside” life. Finally, an area of significant high risk for licensure action relates to the nurse’s use of social media. As nurses more frequently use social media, their risk for disciplinary action also increases. A frequent violation is the inadvertent disclosure of HIPAA protected patient health information. To avoid licensure, a nurse avoids mention of any specifics related to the job or client on their social media posts. Even if a nurse believes that she is not putting any patientspecific details on her post (example: “the postop hip”), unfortunately, the reference can still give enough info be traced to the nurse’s unit and frequently to the patient. Likewise, the best and only way to avoid inadvertent disclosure of patient photographs is to never take a patient photo with your own device. Even if you are granted permission from a patient, it is not a guarantee that any subsequent disclosure is also permitted. Beware that there is really no “privacy” settings on social media that provide protection from the media company accessing or using your “private” data. The TOS typically give the co-ownership rights to your information. Finally, first accept all posts remain in cyberspace forever. Even if you try to delete posts, they can still be recovered. Therefore, although it may seem like a great idea to post how awful your co-workers, patients or administration are behaving in the middle of your shift, such a post is a keg of dynamite, always stop and wait several hours or overnight before any negative post. For Nurses, the ability to maintain a state license in good standing is the key to being able to work to provide for your family and put food on the table. In order to protect your license, you must be proactive – know the laws that apply to your practice and the appropriate boundaries they require of you. Anytime your license is at stake, representation by a competent attorney with knowledge of the licensure process is critical. Lisa L. Lilly, B.S.N., R.N., J.D has over 23 years of experience as a civil defense litigator and focuses her practice in the areas of professional negligence, complex civil liability and litigation involving wrongful death or serious injury. A substantial portion of Ms. Lilly’s practice involves the defense of professionals, licensed by the State of West Virginia, with an emphasis in representing doctors, nurses, hospitals and other healthcare providers in professional negligence actions brought under the West Virginia Medical Professional Liability Act. She was employed as a Registered Nurse in critical care at Ruby Memorial Hospital in Morgantown, WV prior to becoming an attorney. We have full-time RN openings in Float Pool and OB. Tired of air pollution, traffic jams, crowds, and crime? Then Garrett County is for YOU. Garrett County Memorial Hospital is nestled in the scenic mountains of beautiful western Maryland. Live and work in a mountain playground with good schools, low crime and a stable economy. GCMH is located just minutes away from Deep Creek Lake, Wisp Ski Resort, and numerous state parks. Enjoy hunting, fishing, hiking, boating, skiing (water and snow), swimming, snowshoeing, mountain biking, etc. At Garrett County Memorial Hospital, our motto is “We’re Here for Each Other.” This exemplifies the atmosphere of caring, commitment, respect and professionalism that is felt throughout the hospital. Garrett County Memorial Hospital Human Resources Department 251 North Fourth St., Oakland, MD 21550 FAX: 301-533-4328 Visit our website at: www.gcmh.com to access an online application. EOE H/V/M/F Page 8 West Virginia Nurse Congratulations February, March, April 2015 West Virginia Nurse Anesthetists Never Miss a Beat While Providing Anesthesia Congratulations to Damia Hayman, APRN for receiving the 2015 State Award for Excellence from American Association of Nurse Practitioners. This prestigious award is given annually to a dedicated Nurse Practitioner in each state. Congratulations to Delegate Denise Campbell, RN, MA for receiving the 2015 Advocate State Award for Excellence from American Association of Nurse Practitioners. This prestigious award is given annually to a dedicated nurse practitioner advocate in each state who has made a significant contribution to increasing awareness and acceptance of the NP role. Congratulations to Dr. Lisa Anne McBride of Cardinal Pediatrics in Morgantown, WV on receiving the WV APRN Mentorship Award for her support and mentorship of the APRN profession. If you would like to congratulate a nurse for receiving an award please contact centraloffice@wvnurses.org with the information. More than 450 Certified Registered Nurse Anesthetists (CRNA) from West Virginia and thousands from across the country tell America We Never Miss a Beat as they celebrate the 16th annual National CRNA Week celebration, January 25 – 31, 2015. The catchphrase We Never Miss a Beat touts the quality of care that nurse anesthetists pride themselves on providing patients. To provide the safest anesthesia possible, nurse anesthetists remain by their patients’ side every moment of their procedure, monitoring their vital signs to help ensure a comfortable and safe anesthesia experience. “As anesthesia providers, it is important to be aware of every heartbeat, every breath, and be ready to quickly respond if necessary. Which is why CRNAs are so proud to belong to a profession that has maintained a sterling record of providing patient-safety for 150 years,” said Cassy Taylor, CRNA and WVNA member. Established by the American Association of Nurse Anesthetists (AANA), National CRNA Week was created to encourage CRNAs to take the opportunity to educate the public about anesthesia safety, questions to ask prior to undergoing surgery, and the benefits of receiving anesthesia care from nurse anesthetists. Nurse anesthetists are advanced practice nurses who administer more than 34 million anesthetics in the United States each year. Practicing in every setting where anesthesia is delivered, CRNAs are the primary anesthesia providers in rural hospitals, and have been the main provider of anesthesia care to U.S. service men and women on the front lines since World War I. “It is a privilege to be a part of a profession with a focal point that is dedicated to providing patient safety. Historically, CRNAs have played a considerable role in advancing trends related to monitoring technology, anesthetic drugs, and patient education. In fact, anesthesia today is nearly 50 times safer than it was just 20 years ago,” said Taylor. The West Virginia Association of Nurse Anesthetists (WVANA) represents West Virginia CRNAs, and maintains a working relationship with the West Virginia Nurses Association. Visit www. wvana.com for more information about WVANA. The American Association of Nurse Anesthetists (AANA) was founded in 1931, is located in Park Ridge, Ill., and is the professional organization representing more than 48,000 Certified Registered Nurse Anesthetists (CRNAs) and student registered nurse anesthetists. As advanced practice registered nurses, CRNAs safely administer more than 34 million anesthetics to patients in the United States each year. For more information, visit www.aana.com. February, March, April 2015 West Virginia Nurse Page 9 Our Children, Our Future 4. Drinking Water Protections. The chemical spill crisis disproportionately hurt low-income and working families, and their children. We must protect drinking water protections, especially SB 373. Contact Angie Rosser (arosser@wvrivers.org). WVNA is a Proud Partner in the Our Children, Our Future Campaign! Huge thanks to everyone who voted for Retiring Old Laws so Nurses can meet health needs for WV Families issue to be placed on the 2015 Legislative Platform for the Our Children, Our Future Campaign to End Child Poverty (OCOF). As a result our issue made it into the top ten at #7. You can see the entire OCOF platform below. This means that the whole grassroots effort of the Healthy Kids and Families Coalition will work to help us pass this important nursing legislation this year. Now, the work begins to educate our legislators on the importance of all of these issues to the health and well-being of our WV families. Join us at the legislature for Kids and Families Day on Wednesday, January 14. Register here: https://www.eventbrite.com/e/our-children-ourf utu re -k ids-a nd-fa m il ies- day-at -w v- capit oltickets-14781069577. 5. Defend Medicaid and CHIP, while Expanding Medicaid Access to Mental Health Therapy. Health bills are the leading cause of bankruptcy in America… and Medicaid Expansion and CHIP are proven to save money in the long run. We must defend and adequately fund these programs, while expanding Medicaid access to mental health therapy so that a struggling child or family doesn’t have to wait months to get help just because they have the ‘wrong’ insurance plan. Contact Sam Hickman (shickman@naswwv.org) or Renate Pore (renatepore@gmail.com). 6. Past Due! It’s time to choose: WV’s kids or Big Tobacco? Increasing the tax on tobacco saves lives, reduces health care costs and provides a revenue source. It’s proven as the best way to protect kids and pregnant women from this addition. Contact Christine Compton (Christine. compton@heart.org). 10. Providing Earned, Paid Sick Days for Workers & Schedules that Work. A paid sick time policy would make our families stronger, our workplaces healthier, and improve the wellbeing of children. Workers shouldn’t have to choose between their job and their family’s health. Contact Erin Snyder (esnyder@wvpolicy.org). The Our Children, Our Future Campaign is a non-partisan alliance of 177+ churches, community organizations, businesses, unions, schools, and advocates – devoted to ending child poverty in West Virginia. We have fought and won 12 policy victories in two years by engaging new voters and families in the political process; we will defend these victories in addition to the campaigns above. Over 3400 leading West Virginians participated in the creation of the above platform – attending a community meeting, participating in a policy workshop or Symposium, or casting a ballot. Contact Chris Kimes ckimeshkfc@gmail.com for more information. 7. Retiring Old Laws so Nurses (APRN’s) can meet health needs for WV Families. Let nurses nurse. Old laws bar Advance Practice Nurses from doing what they are trained to do; we need a change so communities get the care they need, while saving everyone money. Contact Aila Accad (ailaspeaks@gmail.com). 8. Stopping Meth Labs in WV. Over-thecounter pseudo-ephedrine now exists that can’t be turned into meth. Now is the time to require a prescription for pseudo-ephedrine that can be turned into meth. Supported by law enforcement, shown to reduce meth labs. Contact Judy Crabtree (judy.crabtree@camc.org). 9. Erin’s Law: Preventing Childhood Sexual Assualt. We must train educators and school personnel to spot the signs of child sexual abuse, and respond. Contact Brooke Drake (iambrookedrake@gmail.com). Nurse Policy Advocates in Morgantown host reception for newly elected Senators and Delegates at the home of Sam Cotton, WVN-PAC Chairperson. From left to right: Angy Nixon, Sam Cotton, Beth Baldwin, Senator Kent Leonhardt & Mrs Leonhardt. 2015 Legislative Platform Our Children, Our Future Campaign to End Child Poverty 1. Protect and Provide a Secure Funding Stream for Family Support Programs. Last year, the legislature heroically fought to protect vital state programs that give families a hand-up out of poverty; programs like the Family Resource Networks (that produce better than a 10:1 return on investment, by leveraging private, local and federal dollars) and Family Resource Centers (which are a hub for family services). We need a permanent funding solution so these programs are not always fighting for their lives. Contact April Miller (tuckerfrn@hotmail.com). 2. A Smart Start for WV—Invest in Early Childhood. The Governor’s Early Childhood Task Force offers a 10-year plan to make WV a national leader in early childhood, so our children grow up healthy, strong and ready to learn. Recommendations include expanding homevisiting, access for quality childcare, Birth to three, financing options, governance and program accountability. The legislature should adopt these recommendations and pass a plan to begin this expansion. $1 in = $7 in the long-run. Contact Jim McKay (jim@teamwv.org). 3. Juvenile Justice Reform. West Virginia is experiencing a crisis in the number of children referred to juvenile court as a result of missing school. We must amend the currant truancy law to extend the number of unexcused absences from five days to ten. Additionally, the truancy law should require schools to employ school-based and community interventions to improve attendance before referring a student to juvenile court. Contact Jen Meinig (jmeinig@acluwv.org). Alderson Broaddus University Earn your Bachelor of Nursing degree! We offer: •Traditional, on-campus, 4yr BSN •RN-BSN 100% online, flexible & works around your schedule •LPN-BSN, most work off-campus. One week end/month required to work directly with faculty, up to 4 days/mo. in clinicals. Apply Today! Philippi, West Virginia www.ab.edu 800-263-1549 Page 10 West Virginia Nurse February, March, April 2015 Unity Day Format For The Nightingale Tribute The Nightingale Tribute begins with a short synopsis of the nurse’s career. A creative reading follows the synopsis. A white rose is placed with the nurse after the reading, with the statement: “(Name), we honor you this day and give you a white rose to symbolize our honor and appreciation for being our nursing colleague.” This entire tribute takes only two minutes and can be placed anywhere in the service appropriate to the traditions and beliefs of the recipient’s faith. How do I arrange for this tribute for my loved one? • Visit with your funeral home director about this tribute. • Choose a nurse friend or colleague (active or retired) of the deceased to present the tribute. • Ask the nurse to visit with you. Provide them a brief synopsis of your loved one’s life as a nurse. • Use the words included with this brochure as a creative reading to follow the career synopsis. Adapt the reading to fit the recipient. • The Tribute will be scheduled in the service in collaboration with the family, funeral home and place of worship as appropriate. • Decide if you would like a white rose placed with your loved one in tribute and honor. If so, notify the nurse presenter and any other nurse friends to bring a white rose or make arrangements to have white roses available for the tribute and the colleagues. Nightingale Tribute We lose may people in our lives and nurses who have an impact on the nursing community have a special place in our hearts. If you have lost a nurse this year please let WVNA know so that we might honor these nurses at Unity Day February 25, 2015. Join West Virginia Nurses Association Today! Application on page 15 or join online at www.wvnurses.org THE NIGHTINGALE TRIBUTE READING Nursing is a calling, a lifestyle, a way of living. Nurses here today honor __________ and his/her life as a nurse. __________ is not remembered by his/her _____ years as a nurse, but by the difference he/she made during those years by stepping into people’s lives… by special moments: SHE WAS THERE When a calming, quiet presence was all that was needed, she was there. In the excitement and miracle of birth or in the mystery and loss of life, she was there. When a silent glance could uplift a patient, family member or friend, she was there. At those times when the unexplainable needed to be explained, she was there. When the situation demanded a swift foot and sharp mind, she was there. When a gentle touch, a firm push, or an encouraging word was needed, she was there. In choosing the best one from a family’s “Thank You” box of chocolates, she was there. To witness humanity—its beauty, in good times and bad, without judgment, she was there. To embrace the woes of the world, willingly, and offer hope, she was there. And now, that it is time to be at the Greater One’s side, she is there. NOTE: Pronoun can be changed. © 2004 by Duane Jaeger, RN, MSN __________________, we honor you this day and give you a white rose to symbolize our honor and appreciation for being our nursing colleague. February, March, April 2015 Unity Day West Virginia Nurse Page 11 A Tribute to Jay Rockefeller WV Nurses celebrate with Senator Jay Rockefeller. L-R Aila Accad, Angy Nixon, Beth Baldwin, Ruth Blevins, Sam Cotton WVNA leaders turned out enforce for the West Virginians for Affordable Healthcare Annual Meeting and tribute to retiring Senator, Jay Rockefeller. Senator Rockefeller has been a champion of healthcare, especially for children and coal miners. He was instrumental in shaping the Affordable Care Act to be more consumer friendly, protected the Children’s Health Insurance Program (CHIPs), and preserved health insurance benefits for retired coal miners and their widows. In his own words: “I have spent my entire career working to protect children and other vulnerable populations. I will never stop fighting to make sure they have all the safeguards they need and deserve. These are children—we should do all we can to shield them from harm. Period!” Senator Jay Rockefeller, October 2, 2009. Your license is your livelihood! Elizabeth S. Lawton, RN, BSN, JD Representing Nurses before the West Virginia Board of Nursing & in Medical Malpractice cases. CHARLESTON 304-345-1400 MORGANTOWN 304-291-2702 Page 12 West Virginia Nurse February, March, April 2015 Do You Know Someone who is the Victim of a Crime? Let’s Talk About Sex… and Relationships! Steve McElroy Carrie-Meghan Quick-Blanco The West Virginia Court of Claims, created by the West Virginia Legislature in 1967, was established to allow claims to be filed against the state which cannot be heard in the regular courts due to constitutional immunity. Awarded claims are considered by the West Virginia Legislature in a claims bill and are declared to be moral obligations of the state for payment. Crime victims can be awarded compensation. In 1981, the West Virginia Legislature passed the West Virginia Crime Victims Compensation Act, to be administered by the Court of Claims. The law established a Fund to assist innocent victims of violent crimes with their out-of-pockets losses, including medical care, counseling, lost income and funeral and burial expenses. We are surrounded by it. In movies, commercials, television shows, music, pop culture, magazines and stand-up routines. Sex is everywhere; yet, in America, talking about it still remains taboo. If only preparing children for sex and healthy relationships could be like learning how to drive a car: an important transition into adulthood that requires responsibility and trust. In fact, many people believe that we shouldn’t be talking about sex at all with young people. If we do, it will only encourage them to have sex. Unfortunately, that stance of “don’t ask, don’t tell” has contributed to the situation we face today: 2nd highest nation in the industrialized world for teen births with West Virginia touting the 5th highest rate in the United States. In fact, the costs of teen childbearing in America totaled $9.4 billion dollars in 2010! We also know that teenagers in West Virginia are sexually active and by the time they are seniors in high school, 2/3 of them will have had sexual intercourse. So while everyone isn’t doing it, everybody needs information about how to protect themselves against unintended pregnancies and STD’s (including HIV/AIDS). Estimates suggest that about 48% of STD cases in the United States are acquired by persons aged 15-24 years olds. Talking about the importance of being sexually healthy is not a hard sell for nurses and others in the health care community. Nurses often see firsthand diseases or issues that could have been prevented as a result of poor decisions or lack of education and resources. Because they are on the front line, nurses have a unique opportunity in educating and supporting teens and their families in a variety of settings and positively influencing further transmission of STD’s and unintended pregnancies. With statistics like this, it’s easy to see that we need to make a change and October is a great place to start at home with these two words: “Let’s Talk.” Let’s Talk Month is a national public education campaign celebrated each October sponsored by Advocates for Youth, an organization that champions young people to make informed and responsible decisions about their reproductive and sexual health. Let’s Talk Month provides an opportunity for community agencies, businesses, religious institutions, schools, media, health care providers and families to plan programs and activities that encourage family dialogue about sexuality and healthy relationships. Locally, WV FREE’s WISE Initiative (Working to Institutionalize Sex Education) is working with partners from across the state to encourage this dialogue. Research shows that good parent-child communication leads to better contraceptive use and lower sexual risk behaviors. Adolescents who feel open to discuss sexual health with their parents are more likely to delay sexual intercourse. Believe it or not, studies show that teens would rather talk at home than get information from the media, school, or even friends about sex. It’s OK not to know all the answers! What you know is less important than how you respond. If you can convey the message that no subject is off limits at home, you’ll be on the right track to setting your children up for success in adulthood! Follow the link below to check out “Let’s Talk Month” resources. http:// www.wvfree.org/reproductive-guide/ Interested in learning more about WISE in WV? Please visit the WISE Facebook or Twitter or become a member of WV FREE. Together we can create a brighter future for WV students and families! Steve McElroy is the Community Liaison Administrator for West Virginia Court of Claims, Crime Victims Compensation Steve.mcelroy@wvlegislature. gov 304.347.4850 LICENSED PRACTICAL NURSE The Emergency Department (ED) has FT, PT, or per diem positions available. Previous ED experience is preferred. Appliants must be licensed in the state of WV and possess the following certifications: CPR and PHTLS. Certification in NRP, PALS, and NCI are an asset. Apply to: Jason Ashley, Director of Human Resources 304.927.6370 • jwashley@rghwv.org Roane General Hospital Care you can trust...close to home www.roanegeneralhospital.com Nurse Manager - Intensive Care Unit (Full-Time) The Cabell Huntington Hospital Intensive Care Unit provides specialized care for adults with serious illnesses. We are searching for a top tier, experienced Nurse Manager to lead our ICU team. We are looking for a take charge candidate with a vision and an understanding of how to provide unparalleled and uncompromised patient care. We are entertaining candidates with a Bachelor’s Degree in Nursing and at least three years of Nurse Manager or ICU experience. Job Requirements : BSN degree required MSN, MHA or MHA degree preferred Three or more years experience in ICU or as a Nurse Manager Certification/Registration: Current RN license in the state of West Virginia Maintains required CEU’s for licensure OCN certification strongly preferred CPR Certification required For immediate consideration, please apply online at Carrie-Meghan Quick-Blanco is the WISE Program Manager at WV FREE. She also works as a DONA certified birth doula and a certified lactation counselor (CLC). www.chhjobs.com COMMITTED TO OUTSTANDING NURSE LEADERSHIP • Master of Science in Nursing – Family Nurse Practitioner • Masters of Science in Nursing/Masters in Business Administration Dual degree WVU Hospitals/University Health Associates is currently hiring Registered Nurses in all specialties and with all levels of experience. We have full-time, part-time, casual, and per diem positions available. • Post Masters Certificates available in Family Nurse Practitioner, Nursing Education, and Nursing Administration • Master of Science in Nursing from WVWC Post-Graduate Certificate in Nurse-Midwifery from Shenandoah University The MSN degrees combine online and hybrid course design with practicum experiences arranged in the student’s home community. Programs are flexible; students can plan their own schedules and choose the pace of study. The West Virginia Wesleyan Master of Science in Nursing program is fully accredited by the Accreditation Commission for Education in Nursing, Inc., (ACEN) (formerly NLNAC). Contact Graduate Admissions gradadmission@wvwc.edu l 304.473.8000 • Master of Science in Nursing from WVWC and a Post-Graduate Certificate for Psychiatric Mental Health NURSE PRACTITIONER from Shenandoah University • Master of Science in Nursing with a concentration in Nursing Education. • Master of Science in Nursing with a concentration in Nursing Administration  www.wvwc.edu/academics/gradprograms/MSN We offer a great benefits package that includes: • • • • Competitive Pay Medical/Dental/Vision Insurance Shift Differentials • • • • Tuition Assistance/Nursing Certifications RN CEUs Offered On-site Holiday Pay and Paid Days Off Retirement Savings Plan Human Resources Department Phone: 304-598-4075 or 1-800-453-5708 • Fax: 304-598-4264 wvuhjobs@wvuhealthcare.com WVU Hospitals is a 531-bed, progressive teaching hospital and Level 1 Trauma center located in Morgantown. WVUH is dedicated to providing the highest quality of patient care and creating a positive work environment. EEO M/F/V/D February, March, April 2015 West Virginia Nurse Debra Lopez-Bonasso, BA, MA In West Virginia, 1 in 6 women and 1 in 22 men will be victims of an attempted or completed forcible rape in their lifetime. According to the 2010 Census, there are nearly 750,000 women age 18 or older living in WV. This means that the estimated number of WV adult women who have ever been raped is about 125,250. This prevalence is higher than in many other states, including New York, Pennsylvania and Texas. Health care practitioners who respond to the needs of sexual assault victims, according to The National Protocol for Sexual Assault Medical Forensic Examinations, should strive to ensure that they receive special training and be clinically prepared to conduct the medical forensic examination. The West Virginia Foundation for Rape Information and Services (WVFRIS), the state sexual assault coalition, began to address this training need in 2000 by working to establish Sexual Assault Nurse Examiner (SANE) programs in West Virginia. Sexual Assault Nurse Examiners (SANEs) are registered nurses who are specially-trained to offer victims prompt, compassionate care and comprehensive forensic evidence. This kind of training can reduce the impact of the trauma experienced by victims and can ensure that prosecutors have quality evidence needed to obtain convictions. After years of work and much collaboration, WVFRIS is pleased to announce the development of the West Virginia Sexual Assault Nurse Examiner (SANE) training program. This 40 hour SANE training coursework is developed for physicians, advanced practice nurses, nurses and physician assistants. The SANE training provides medical personnel with the skills to assess, evaluate, treat and properly care for patients that have been sexually assaulted to ensure that victims of sexual assault receive quality patient care and comprehensive forensic evaluations. The 40 hour training includes information on how to: • obtain a relevant medical history from a sexual assault patient; • conduct a physical examination specific to the medical history; • document injury using photography, body diagrams and charting; • collect and preserve forensic samples; • use the West Virginia State Police Forensic Laboratory’s sexual assault evidence collection kit (SAECK); • provide the patient with prophylactic medications and/or emergency contraception for the prevention of sexually transmitted infections (STIs) and pregnancy; Page 13 • treat and/or refer the patient for medical treatment; and • work as part of a victim-centered, multidisciplinary response for the patient who is a victim of sexual assault. six (6) month time frame, but MUST be completed within one year following the SANE training. Details about the clinical requirements for the SANE can be found by viewing the: Since the training was launched at the end of June, 2014, 78 nurses have registered for the online course and 38 of those nurses have completed the two day SANE Classroom training. Nurses participating represent Charleston Area Medical Center, Logan Regional Medical Center, Minnie Hamilton Health Care, United Hospital Center, Webster Memorial, and Cabell County Health Department. The West Virginia Sexual Assault Examiner (SANE) Training for Adults and Adolescents has a three-part blended learning format. The training combines online and classroom educational methods. 1. 24 Hours of SANE Online Training - To better accommodate busy schedules, 24 hours of the SANE training can be taken online for free. It is a self-paced course comprised of twenty-three units. The entire online portion of the course takes approximately 24 hours to complete. All 24 hours of the online coursework must be completed before beginning the second phase of the training, which is the 16 hour (2 day) classroom training. 2. 16 Hours of SANE Classroom Training - This classroom training will provide practical application from the online course and will be facilitated by members of the West Virginia SANE faculty. The 16 hour (2 day) classroom training is a requirement for all nurses wishing to practice as a SANE. The registration cost for this part of the training is $150. Nurses will receive 40 contact hours of continuing education for completion of the online and the classroom training. The SANE classroom training will be offered regionally several times a year in West Virginia and must have at least 16 nurses registered for the training to take place as scheduled. Class size will be limited to 20 participants. 3. 25 Hours of Clinical Requirements - Demonstration of clinical competence is an essential part of the SANE training. SANEs must have 25 hours of clinical practice with qualified preceptors (physicians, advanced practice nurses, SANE-As or physician assistants) to adequately develop and demonstrate the competencies and skills required in conducting medical forensic exams and collecting forensic evidence. This work is done independently by the SANE following the completed 40 hour training once a preceptor is selected. It is recommended that these requirements be completed within a West Virginia Clinical Requirements for the Adult/Adolescent SANE Training PDF To register for the Sexual Assault Nurse Examiner (SANE) Online Training for Adults and Adolescents, go to www.wvsasta.org/moodle. Follow instructions for setting up an account in the Sexual Assault Services Training Academy (SASTA). Request access to the SANE course and finish the registration process by completing the “SANE Survey.” When you receive the email confirmation, activate your SASTA account by clicking on the link in the email. You will be able to begin the SANE training after you receive a second email (within 48 hours) confirming your access to the online SANE training. All healthcare providers have a unique opportunity to help tobacco users FREE WORKSHOP • FREE CMEs and CEUs Learn evidence-based practices to advise and counsel patients in tobacco cessation. Online registration is required. • Bridgeport – http://HCPBridgeport2015.doattend.com o Saturday, March 28, 2015 8:30 am – 12:15 pm @ Bridgeport Conference Center • Charleston – http://HCPCharleston2015.doattend.com o Saturday, May 9, 2015 8:30 am – 12:15 pm @ Holiday Inn and Suites, S. Charleston For additional information contact: Cinny Kittle at ckittle@wvha.org or 304-419-0899. Sponsored by: WVDHHR/Division of Tobacco Prevention, Joan C. Edwards School of Medicine and the WV Hospital Association. For questions and additional information, you may contact WVFRIS staff: Bonnie Fields, RN, BS, SANE-A, WV SANE Project Coordinator 304-685-3159 bfields54@verizon.net Debra Lopez-Bonasso, BA, MA, Education/SANE Coordinator 304 366-9508 dlbonasso@aol.com The West Virginia Online SANE Training and the Classroom SANE Training Curriculum were developed with funding provided by the Claude Worthington Benedum Foundation. Additional financial support was provided by the West Virginia Prosecuting Attorneys Institute (WVPAI) and the West Virginia Women’s Commission. Dynamic Career Opportunity Mildred Mitchell-Bateman Hospital is a 110-bed acute care mental health facility operated by the West Virginia Department of Health and Human Resources. We are seeking qualified staff to fill permanent and temporary positions. • RNs • LPNs • Health Service Workers (CNA) • Interpreters for the Deaf Some of the benefits you will enjoy: • Paid holidays with incentive for working Thanksgiving, Christmas, and New Year’s Day • Accrued sick leave • Accrued annual leave • Shift differential for evenings and night shifts • Education assistance (tuition reimbursement) • Annual increment pay after 3 years of service • Public Employees Retirement System • Comprehensive health insurance plans, including PEIA • Prescription drug plan and optional dental and vision coverage • Staff to acuity Temporary positions do not include benefits. Interested individuals should contact: Patricia G. Hamilton, RN BC Chief Nurse Executive dhhrmmbhhr@wv.gov 1530 Norway Avenue, Huntington, WV 25709 Phone: 304-525-7801 x 734 Fax: 304-529-6399 www.batemanhospital.org Mildred Mitchell-Bateman Hospital is a Drug Free Workplace. Minorities are encouraged to apply. Equal Opportunity Employer. Page 14 West Virginia Nurse February, March, April 2015 When Should you Offer Hospice Care? Chris Zinn, RN, MSc, CHPN Executive Director of the Hospice Council of West Virginia Hospice Services include: • Physician services • Registered Nurse visits and case management • 24-7 on call support and visits • Psychosocial Support • Spiritual support* • Hospice Aide Visits* • • • • • Trained volunteers* Physical Therapy* Dietary Counseling* Durable Medical Equipment Medications and supplies related to the terminal prognosis *when needed or requested Hospice care is a great resource for those who need palliative care, but when should this be offered? As the public’s most trusted professionals, nurses need to be able to talk about hospice to patients, family, friends, and neighbors and know when to refer. As patient advocates, they can support doctors with difficult conversations about end-of-life care. When offered at the appropriate time, hospice care can improve quality of life and help patients remain at home. According to a survey by the West Virginia Center for End of Life Care (WVCEOLC), 75% of West Virginians want to be cared for at home or in a hospice inpatient facility when they are dying. However, many West Virginians still die in a hospital unless they have hospice support. Less than 4% of the 10,000 West Virginia hospice patients died in a hospital in 2012. West Virginia’s hospice utilization is 37% of Medicare deaths, 42nd in the nation, despite an older population with higher morbidity. About 50% of Medicare deaths are now with hospice in Kanawha, Randolph and Lincoln counties, but half of all patients are referred less than 4 weeks before death. There is a great need for nurse advocacy to promote increased utilization and earlier referrals and to overcome cultural barriers. People need to know that hospice can take care of people in their own home or in other settings, such as assisted living, nursing home or hospice facilities. The care provided is personalized, coordinated and interdisciplinary. RELOCATION ASSISTANCE NOW AVAILABLE! Raleigh General Hospital is currently seeking full-time RNs. Areas of specialty include Med/Surg, Critical Care, Women’s Services, Emergency Care & Cardiac Cath Lab. We offer competitive salaries and benefits along with a patient centered family atmosphere. Located in Beckley, the largest city in Southern WV, which boasts major shopping centers, restaurants, museums and galleries. Beckley is also an outdoorsman’s paradise offering whitewater rafting, hunting, fishing, climbing, hiking, camping, horseback riding, mountain biking and photography. Apply on-line at www.raleighgeneral.com The whole family is the unit of care and receives support and education to help patients achieve their goals. Respite and inpatient care may be part of the plan of care. Medicare and Medicaid have special hospice benefits and most insurance covers hospice. Some private insurance companies have established advanced illness programs that cover earlier hospice support. However, most hospice benefits can only be accessed when a physician certifies that the patient has a prognosis of less than six months if the illness follows its expected course. The question ‘Would you be surprised if this patient died in six months?’ can help providers determine eligibility. When patients have cancer, determination of a terminal prognosis may be more predictable. Hospice should be offered when curative treatment is no longer beneficial. There are eligibility guidelines for many non-malignant diseases, such as Alzheimer’s disease, heart failure, COPD, ALS, cirrhosis and end-stage renal disease. Some of the general guidelines that may predict poor prognosis include uncontrolled symptoms, frequent hospitalizations, weight loss, nutritional problems and a decline in the ability to perform activities of daily living. Sometimes elderly patients have multiple co-morbidities that lead to a terminal prognosis. Prognostication is not an exact science. If patients remain terminally ill, they can continue to receive hospice care for as long as this is needed. A significant number of hospice patients are discharged because they have improved and are no longer considered to be terminally ill. They can be readmitted to a hospice program if their condition declines. When communicating with patients, it may be helpful to tell them that hospice does not make death come any sooner and that some patients do improve with attentive holistic care. Patients may live longer with improved quality of life and are less likely to be hospitalized. Hospice can also improve quality of life for the family and bereavement care is provided after the patient dies. Since the health of caregivers can be adversely affected by grief, this care and support is vital. Anyone can make a hospice referral and the hospice will then contact the attending physician to get approval. During the initial hospice assessment, eligibility is determined, informed consent is obtained and an initial care plan is established. The right time to refer may be different for everyone, but the important thing is to make sure people know they have a right to this support. Too many people write ‘I wish we had known about hospice sooner’ on satisfaction surveys. Honest information gives patients more control and choice and nurses must advocate for this. For a map of Hospice Council of West Virginia providers, contact information and other resources visit www.hospicecouncilofwv.org. Information for patients and families can also be found at the National Hospice and Palliative Care Organization’s new website www.momentsof life.org. Chris Zinn is a certified hospice & palliative care nurse (CHPN) with a Masters in Palliative care. She is a WVNA and HPNA member who worked with Kanawha Hospice Care, Inc as a hospice nurse for 30 years and was the first administrator of the Hubbard Hospice House. As director of the state hospice organization, she represents WV hospices on the Advisory Board of WVCEOLC and the National Hospice & Palliative Care Organization’s Council of States. February, March, April 2015 West Virginia Nurse Membership News Please complete and return to: West Virginia Nurses Association PO Box 1946 Charleston, West Virginia 25327 (f) 304-414-3369 Page 15 CHIP Running Out of Federal Funds WVNA/ANA Membership Application Contact Information Payment Plans Employed Full Time $288.00 Transfer* Employed Part Time $24.50 Renate Pore West Virginians for Affordable Health Care The highly popular West Virginia Children’s Health Insurance Program is in danger of losing its funding unless Congress acts before September 2015. CHIP provides coverage to uninsured children, whose families earn as much as 300 percent of the Federal Poverty Level. Since its enactment more than 185,000 West Virginia children have been covered by the program. This year, CHIP will cover about 25,000 children. The federal government has always provided generous funding for WVCHIP up to 82 percent of the total cost of the program. CHIPs funding, however, will end next September unless Congress acts to extend the program. More than 26 West Virginia organizations including the West Virginia Nurses Association have asked our Congressional delegation to do everything they can to extend CHIP funding. In the past, CHIP has had bipartisan support, and we hope that will be the case this time. While the Nurses Association has asked the West Virginia Congressional Delegation to support continued CHIP funding, our representatives need to hear from each one of us. I urge all West Virginia nurses to contact our current congressional delegation, and if nothing happens to repeat the contact in the next Congress. A simple post card or email through the congressional websites saying that “I want you to support refunding of the Children’s Health Insurance Program,” can make a big difference. Do it today. You can find the email message system on each representatives’ website. It’s especially important to contact Representatives Capito and McKinley and Senator Manchin. Your action can make a difference in the life of a child. PAYMENT DETAILS $288.00 (Full) $149.00 (State Only) Protecting Your Career Is Our Job We have a long history of representing professionals who are licensed by the state of West Virginia and experience a claim that could result in either a loss of license or professional discipline. Visit: www.mcqueendavis.com or Contact Us for a Consultation 304.522.1344 www.nursingALD.com RN’s who work or live in $151.00 Transfer* Your online resource for nursing jobs, research, and events. Find your dream job today! Page 16 West Virginia Nurse February, March, April 2015 Apply Now to the Online RN to BSN Program At Bluefield State College Applications accepted until April 15th ❖ Join the “Future of Nursing” & obtain your BSN ❖ Optional “Boot Camp” days with faculty to enhance learning ❖ Individual counseling/close contact with faculty ❖ Affordable 3 or 4 semester plan ❖ 120 hours for completion of BSN Degree Fully Accredited by: The Commission on Collegiate Nursing Education (CCNE) One Dupont Circle, NW, Suite 530, Washington, D.C. 20036 (202) 887-6791 For further information & to apply online: www.bluefieldstate.edu or email/call Director bpritchett@bluefieldstate.edu (304) 327-4139 www.bluefieldstate.edu
© Copyright 2025