What Is the Minimal Pacing Rate that Prevents Permanent Pacemakers
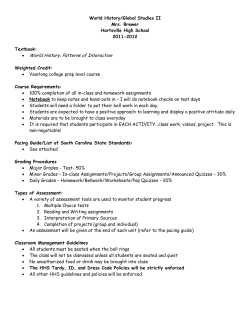
Reprinted with permission from JOURNAL OF PACING AND CLINICAL ELECTROPHYSIOLOGY, Volume 25, No. 11, November 2002 Copyright © 2002 by Futura Publishing Company, Inc., Armonk, NY 10504-0418. What Is the Minimal Pacing Rate that Prevents Torsades de Pointes? Insights from Patients with Permanent Pacemakers SERGIO L. PINSKI, LUIS E. EGUÍA, and RICHARD G. TROHMAN From the Section of Cardiology, Rush-Presbyterian-St. Luke’s Medical Center and Rush Medical College, Chicago, Illinois PINSKI, S.L., ET AL.: What is the Minimal Pacing Rate that Prevents Torsades de Pointes? Insights From Patients with Permanent Pacemakers. In the acquired long QT syndrome, torsades de pointes (TP) is invariably preceded by pauses or bradycardia. Thus, it has been proposed that out-of-hospital initiation of drugs that prolong repolarization should be safe in patients with permanent pacemakers. However, a minimal protective pacing rate has not been identified. The authors reviewed published reports of acquired TP in patients with permanent pacing. Those providing documentation of tachycardia onset and pacemaker programming were included in the analysis. Events occurring # 1 month after AV nodal ablation were excluded. Eighteen cases were identified (age 74 6 5; 10 women). QT prolonging drugs were present in 15 patients (quinidine 5, sotalol 3, disopyramide 3, amytriptiline, chloroquine, cisapride 1 haloperidol, and monopride 1 flecainide 1 each). Hypokalemia was present in eight patients. At the time of TP, the programmed lower rate was 63 6 13 beats/min. However, the effective pacing rate was lower (55 6 11 beats/min) due to invocation of pause-promoting features (hysteresis [4 patients]; 1 PVARP extension on PVC [1 patient]) or ventricular oversensing (2 patients). No patient developed TP with an effective pacing rate . 70 beats/min. TP is possible in the presence of a functional permanent pacemaker. Programmed lower rates # 70 beats/min are not protective. At programmed lower rates . 70 beats/min, TP may occur only when facilitated by programmable pause-promoting features or oversensing. It remains to be seen if rate smoothing algorithms can prevent TP when the baseline rate is programmed # 70 beats/min. (PACE 2002; 25:1612–1615) pacemaker, artificial, torsades de pointes, proarrhythmia, quinidine; disopyramide, sotalol Introduction Torsades de pointes (TP) ventricular tachycardia occurring in the setting of acquired long QT syndrome is almost invariably preceded by a pause followed by a markedly prolonged QT interval.1– 3 An early beat (most often a premature ventricular depolarization) arising from the prolonged T wave initiates torsades (i.e., the longshort sequence). Although the intimate electrophysiological mechanisms responsible for this pattern are a matter of debate,4–6 it is well documented that temporary pacing, by suppressing the pauses, can acutely prevent TP.7,8 Patients with permanent pacemakers, espe- Address for reprints: Sergio L. Pinski, M.D., Cleveland Clinic Florida, 2950 Cleveland Clinic Blvd., Weston, FL 33331. Fax: (954) 659-5292; e-mail: pinski@cef.org. Presented in part at the 22nd Annual Scientific Session of the North American Society of Pacing and Electrophysiology (NASPE), Boston, Massachusetts, May 2001. Received August 16, 2001; revised September 28, 2001; accepted October 17, 2001. 1612 cially those with sick sinus syndrome, often require antiarrhythmic drug therapy for suppression of concomitant atrial tachyarrhythmias. It has been hypothesized that the risk of TP should be low in patients with functional permanent pacemakers, making out-of-hospital initiation of antiarrhythmic drugs that prolong repolarization safe in this population.9 In a large series of patients undergoing in hospital initiation of sotalol for atrial tachyarrhythmias, the presence of a permanent pacemaker was the only variable that predicted freedom from proarrhythmic complications.10 To characterize the relation between pacing rate and risk of TP (and hopefully identify a pacing rate that would make this arrhythmia unlikely), the authors searched the literature for reports of acquired TP in patients with permanent pacemakers.9–21 Methods Several strategies were used to identify the relevant reports. Medline computerized searches were conducted using the search words “torsade” November 2002 PACE, Vol. 25, No. 11 MINIMAL PACING RATE TO PREVENT TP and “pacemaker” and their variants (e.g., “polymorphic ventricular tachycardia,” “pacing,” etc). Auxiliary searches were conducted using the words “quinidine” and “pacemaker,” “sotalol” and “pacemaker,” etc. Further searches included all papers indicated as “related articles” in PubMed for each relevant report. In addition, the authors manually searched the bibliography of all articles describing qualifying patients and of review articles on pharmacological proarrhythmia or TP. Cases with clearly documented acquired TP in the presence of a permanent pacemaker (or implantable defibrillator with pacing capabilities) were included if information on the programmed settings of the device plus a description of the intervals leading to arrhythmia initiation or electrocardiographic (ECG) documentation of its onset were available. Good quality copies of ECG recordings were magnified to allow measurement of the relevant intervals with hand held calipers. Cases were not included if the diagnosis of congenital long QT (Romano-Ward) syndrome could be made on the basis of available information.22 Because the relationship between pacing rate and QT duration is altered shortly after ablation of the AV junction,23 cases occurring within 1 month of this procedure were not included in the analysis.24 Results Eighteen patients (10 women, 8 men) were identified (Table I). Their age was 74 6 5 years (range 64–82). Fifteen patients were taking drugs known to prolong ventricular repolarization (quinidine 5, sotalol 3, disopyramide 3, amytriptiline, chloroquine, cisapride 1 haloperidol, and monopride 1 flecainide 1 each). Hypokalemia (# 3.5 mM/L) was present in at least eight patients (information on potassium level was not provided in six case reports). The mean programmed lower rate at time of TP was 63 6 13 beats/min (range 40–85). In 15 (88%) cases the pacemaker lower rate was set at # 70 beats/min. However, the effective pacing rate at time of TP was lower, 55 6 11 beats/min (range 40–70), due to the operation of pause-promoting algorithms (hysteresis in four patients; premature ventricular atrial refractory period [PVARP] 1 in premature ventricular contraction [PVC] in patient) or oversensing (myopotentials in 1 patient; T wave in 1 patient). In no instance did TP occur with an effective pacing rate . 70 beats/min. Figure 1 displays the distribution of programmed and effective pacing rates at the onset of TP. In all the patients reported, increasing the pacing rate or disabling the pause promoting algorithms when appropriate prevented arrhythmia recurrence. Table I. Clinical Characteristics and Pacemaker Programming First Author Age Sex Mode Medication Thompson (1976)11 Thompson (1976)11 Speca (1978)1 2 Iesaka (1982)13 79 77 70 64 M M M M VVI VVI VVI VVI Quinidine Quinidine None Quinidine Delia Bella (1990)14 Kimura (1994)1 5 Kimura (1994)1 5 Kimura (1994)1 5 Alt (1996)1 6 Kurita (1996)17 Chung (1998)10 Chung (1998)10 Goldman (1998)18 Pardo (1998)1 9 Pinski (1999)9 Pinski (1998)9 Ng (2000)2 0 Ohki (2000)2 1 75 71 77 69 82 74 78 74 71 81 75 70 81 68 M F F F F F F M F F F M F M VVI VVI VVI VVI VVI DDI DDD VVI DDD VVI DDD VVI VVI DDD Quinidine Disopyramide Disopyramide Disopyramide Chloroquine None Sotalol Sotalol None Amytriptiline Quinidine Sotalol Cisapride1haloperidol Mosapride1flecainide K (mM/L) LRL (bpm) Effective Rate (bpm) N/A N/A 3.2 N/A 70 70 72 85 60 60 60 30 Normal 3.2 2.6 2.9 3.5 3 3.4 Normal N/A 3.6 N/A N/A Normal 3.2 70 50 60 70 40 70 60 40 85 70 50 44 70 60 50 50 60 70 40 70 60 40 61 70 50 44 60 60 Pause-Promoting Feature Hysteresis (60 bpm) Hysteresis (60 bpm) Hysteresis (50 bpm) Oversending of myopotentials Hysteresis (50 bpm) PVARP 1 on PVC T wave overspending bpm 5 beats per minute; LRL 5 programmed lower rate limit; N/A 5 not available; PVARP 5 premature ventricular atrial refractory period; PVC 5 premature ventricular contraction. PACE, Vol. 25, No. 11 November 2002 1613 PINSKI, ET AL. Figure 1. Histogram showing distribution of programmed lower rates (LRL) and effective pacing rates at the time of torsades de pointes in 18 patients. Discussion From this review of published cases of acquired TP in the presence of permanent pacing it can be concluded that a pacemaker cannot provide reliable protection against this arrhythmia if the programmed lower rate is # 70 beats/min. A “protective” rate could not be identified, although the limited available evidence suggests that at programmed rates . 70 beats/min, TP may be possible only after activation of device algorithms that allow for the occurrence of pauses longer than the lower rate limit or in case of ventricular oversensing. These findings have implications for patient care. Initiation of antiarrhythmic drugs that prolong repolarization cannot be assumed absolutely safe solely on the basis of a functional pacemaker programmed at the usual lower rates of 60–70 beats/min. One can speculate regarding why a heart rate of $ 70 beats/min may be necessary to prevent TP. Most drugs that prolong the QT interval do so more at slow rates than at fast ones, a phenomenon termed reverse use-dependence and this phenomenon probably contributes to the bradycardia dependence of TP.25 There are few human studies assessing the effects of Class III drugs on ventricular repolarization over a wide range of cardiac rates. Visual inspection of the graph plotting QT interval versus RR interval in a study of sotalol suggests that the effect becomes more marked at rates , 80 beats/min.26 Other evidence also indicate that the protective pacing rate may be slightly . 70 beats/min. In a placebo-controlled trial of dofetilide in patients with ICDs, pause dependent polymorphic ventricular tachycardia (presumably TP) was seen in stored electrograms in 15 (17%) of 87 patients assigned to dofetilide.27 The pro1614 grammed pacing rate was , 70 beats/min in 14 patients, and 70 beats/min in 1 patient. No detail was provided regarding the effective pacing and initiating intervals. Among patients with congenital long QT syndrome treated with a permanent pacemaker, recurrent arrhythmic events with pacing rates , 75 beats/min are well documented.28 Several idiosyncratic or programmable functions can result in pacing at rates below the lower rate limit. Hysteresis is the most obvious, and it was operative in four of the patients in this study. Although some investigators have recommended hysteresis in patients with sinus node dysfunction and single chamber ventricular pacemakers to promote atrioventricular (AV) synchrony,29 it may not reduce pacemaker use or improve patient well-being.30 Circadian functions that automatically drop the stimulation rate during night hours or patient inactivity are also a frequent cause of lower rate limit overriding. Less known idiosyncratic features including, for example, atrial-based timing after a late-coupled ventricular premature beat, and the programmable “1 PVARP on PVC” feature in Pacesetter/St. Jude (Sylmar, CA, USA) pacemakers can result in pauses longer than the programmed lower rate limit. In general, all these algorithms should be avoided in patients with a history of TP or risk factors for its development, especially drugs that prolong repolarization. The risk of TP is higher after a sudden drop from persistently fast ventricular rates. Electrical remodeling due to potassium channel down-regulation has been implicated.31 TP during pacing at “usual” rates shortly after AV junction ablation in patients with supraventricular tachyarrhythmias is well documented, and faster pacing rates are recommended for the first few days thereafter. In addition, the authors have recently demonstrated a high risk of ventricular tachyarrhythmia immediately after pacemaker reprogramming to usual rates in patients “tracking” atrial tachyarrhythmias at rapid rates.32 The available clinical descriptions allowed them to rule out the role of a preexistent fast ventricular rate in promoting TP in most of the patients included in this analysis. A relatively high baseline pacing rate (i.e., . 80 beats/min) could be programmed to prevent TP in patients at risk. However, such fast rates can be detrimental to patient well-being and, if maintained for long periods, can provoke myocardial dysfunction.33 Alternatively, rate stabilization algorithms available in newer pacemakers and implantable defibrillators can eliminate post ectopic pauses without the need to program fast baseline rates.34 Early data suggest that they may be highly effective in preventing TP in patients with congenital long QT syndrome.35 Given the common November 2002 PACE, Vol. 25, No. 11 MINIMAL PACING RATE TO PREVENT TP mechanisms that underlie the congenital and acquired long QT syndromes (including similar molecular targets and frequent existence of mutations or polymorphisms in ion channel genes in patients with otherwise “acquired” long QT36,37 ) the algorithms could also be efficacious in pre- venting acquired TP. Prospective validation of this hypothesis would be highly desirable. It should be remembered that in some dual chamber pacemakers and defibrillators rate smoothing algorithms may become inactive during mode switching in response to atrial tachyarrhythmias.38 References 1. Kay GN, Plumb VJ, Arciniegas JG, et al. Torsades de pointes: The long-short initiating sequence and other clinical features: Observations in 32 patients. J Am Coll Cardiol 1983; 2:806–817. 2. Roden DM, Woosley RL, Promm RK. Incidence and clinical features of the quinidine-associated long QT syndrome: Implications for patient care. Am Heart J 1986; 11:1088–1093. 3. Gilmour RF Jr, Riccio ML, Locati EH, et al. Time- and rate-dependent alterations of the QT interval precede the onset of torsade de pointes in patients with acquired QT prolongation. J Am Coll Cardiol 1997; 30:209–217. 4. Brachmann J, Scherlag BJ, Rosenshtraukh LV. Bradycardia-dependent triggered activity: Relevance to drug-induced multiform ventricular tachycardia. Circulation 1983; 68:846–856. 5. El-Sherif N, Caref EB, Chinushi M, et al. Mechanism of arrhythmogenicity of the short-long cardiac sequence that precedes ventricular tachyarrhythmias in the long QT syndrome: Tridimensional mapping of activation and recovery patterns. J Am Coll Cardiol 1999; 33:1415–1423. 6. Roden DM, Anderson ME. The pause that refreshes, or does it? Mechanisms in torsades de pointes. Heart 2000; 84:235–237. 7. DiSegni E, Klein HO, David D, et al. Overdrive pacing in quinidine syncope and other long QT-interval syndromes. Arch Intern Med 1980; 140:1036–1040. 8. Sclarovsky S, Strasberg B, Lewin R, et al. Polymorphous ventricular tachycardia: Clinical features and treatment. Am J Cardiol 1979; 44:339–345. 9. Pinski SL, Helguera ME. Antiarrhythmic drug initiation in patients with atrial fibrillation. Prog Cardiovasc Dis 1999; 42:75–90. 10. Chung MK, Schweikert RA, Wilkoff BL, et al. Is hospital admission for initiation of antiarrhythmic therapy with sotalol for atrial arrhythmias required? Yield of in-hospital monitoring and prediction of risk for significant arrhythmia complications. J Am Coll Cardiol 1998; 32:169–176. 11. Thompson ME, Shaver JA. Undesirable cardiac arrhythmias associated with rate hysteresis pacemakers. Am J Cardiol 1976; 38:685–688. 12. Speca G, Di Sabatino P, Potena A. Episodi sincopali da tachiaritmie ventricolari con “torsade de pointe” in portatore di segnapassi artificiale. G Ital Cardiol 1978; 8(Suppl. 1):283–288. 13. Iesaka Y, Pinakatt T, Gosselin AJ, et al. Bradycardia dependent ventricular tachycardia facilitated by myopotential inhibition of a VVI pacemaker. PACE 1982; 5:23–29. 14. Della Bella P, Tondo C, et al. Polymorphous ventricular tachycardia as undesirable effect of the association of quinidine treatment with hysteresis ventricular inhibited pacing. Eur Heart J 1990; 11:1124–1126. 15. Kimura Y, Takayanagi K, Sakai Y, et al. Torsades de pointes in paced patients with sick sinus syndrome after disopyramide administration. Jpn Heart J 1994; 35:153–161. 16. Alt E, Coenen M, Baedeker W, et al. Ventricular tachycardia initiated solely by reduced pacing rate during routine pacemaker follow-up. Clin Cardiol 1996; 19:668–671. 17. Kurita T, Ohe T, Maeda K, et al. QRS alteration-induced torsade de pointes in a patient with an artificial pacemaker and hypokalemia. Jpn Circ J 1996; 60:189–191. 18. Goldman DS, Levine PA. Pacemaker-mediated polymorphic ventricular tachycardia. PACE 1998; 21:1993–1995. 19. Pardo J, Novoa O, Gonzalez R. Torsion de las puntas y marcapaso PACE, Vol. 25, No. 11 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. endocavitario ventricular de demanda. Rev Med Chil 1998; 126:1503–1506. Ng KS, Tham LS, Tan HH, et al. Cisapride and torsades de pointes in a pacemaker patient. PACE 2000; 23:130–132. Ohki R, Takahashi M, Mizuno O, et al. Torsades de pointes ventricular tachycardia induced by mosapride and flecainide in the presence of hypokalemia. PACE 2001; 24:119–121. Schwartz PJ, Moss AJ, Vincent GM, et al. Diagnostic criteria for the long QT syndrome: An update. Circulation 1993; 88:782–784. Cellarier G, Deharo JC, Chalvidan T, et al. Prolonged QT interval and altered QT/RR relation early after radiofrequency ablation of the atrioventricular junction. Am J Cardiol 1999; 83:1671–1674. Geelen P, Brugada J, Andries E, et al. Ventricular fibrillation and sudden death after radiofrequency catheter ablation of the atrioventricular junction. PACE 1997; 20:343–348. Dorian P, Newman D. Rate dependence of the effect of antiarrhythmic drugs delaying cardiac repolarization: An overview. Europace 2000; 2:277–285. Funck-Brentano C, Kibleur Y, Le Coz F, et al. Rate dependence of sotalol-induced prolongation of ventricular repolarization during exercise in humans. Circulation 1991; 83:536–545. Mazur A, Anderson ME, Bonney S, et al. Pause-dependent polymorphic ventricular tachycardia during long-term treatment with dofetilide. A placebo-controlled, implantable cardioverter-defibrillator-based evaluation. J Am Coll Cardiol 2001; 37:1100–1105. Moss AJ, Liu JE, Gottlieb S, et al. Efficacy of permanent pacing in the management of high-risk patients with long QT syndrome. Circulation 1991; 84:1524–1529. Stangl K, Wirtzfeld A, Sichart U, et al. The combined use of hysteresis and Holter functions improves diagnosis and therapy in patients with sick sinus syndrome. PACE 1988; 11:1698–1702. Rosenqvist M. Edhag OK, Lagergren H, et al. Choosing the stimulation rate in patients with intermittent bradycardia and a single lead pacemaker. PACE 1993; 16:702–707. Näbauer M, Kääb S. Potassium channel down-regulation in heart failure. Cardiovasc Res 1998; 37:324–334. Pinski SL, Murphy J, Haw J, et al. Lethal ventricular arrhythmias following one-step pacemaker reprogramming for rapid tracking of atrial tachyarrhythmias. Am J Cardiol 2001; 87:349–350. Shinbane J, Wood M, Jensen N, et al. Tachycardia-induced cardiomyopathy: A review of animal models and clinical studies. J Am Coll Cardiol 1997; 29:709–715. Fromer M, Wietholt D. Algorithm for the prevention of ventricular tachycardia onset: The Prevent study. Am J Cardiol 1999; 83:45D–47D. Viskin S, Glikson M, Fish R, et al. Rate smoothing with cardiac pacing for preventing torsade de pointes. Am J Cardiol 2000; 86(Suppl. 1):K111–K115. Donger C, Denjoy I, Berthet M, et al. KVLQT1 C-terminal missense mutation causes a forme fruste long-QT syndrome. Circulation 1997; 96:2778–2781. Sesti F, Abbott GW, Wei J, et al. A common polymorphism associated with antibiotic-induced cardiac arrhythmia. Proc Natl Acad Sci USA 2000; 97:10613–10618. Eguía LE, Pinski SL. Inactivation of a ventricular tachycardia preventive algorithm during automatic mode-switching for atrial tachyarrhythmia. PACE 2001; 24:252–253. November 2002 1615
© Copyright 2025