Dual-chamber defibrillators reduce clinically significant adverse events compared with single-chamber devices:
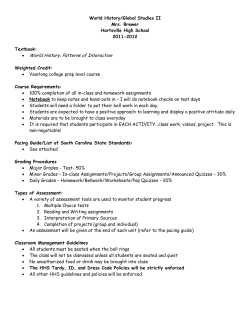
Europace (2008) 10, 528–535 doi:10.1093/europace/eun072 Dual-chamber defibrillators reduce clinically significant adverse events compared with single-chamber devices: results from the DATAS (Dual chamber and Atrial Tachyarrhythmias Adverse events Study) trial Jesus Almendral1*, Fernando Arribas2, Christian Wolpert3, Renato Ricci4, Pedro Adragao5, Erik Cobo6, Xavier Navarro7, and Aurelio Quesada8, the DATAS Steering Committee and Writing Committee on behalf of the DATAS Investigators 1 Received 8 December 2007; accepted after revision 22 February 2008; online publish-ahead-of-print 7 April 2008 KEYWORDS Defibrillation; Tachyarrhythmias; Pacing Aims This randomized trial evaluated clinically significant adverse events (CSAEs), in patients implanted with dual-chamber (DC) vs. single-chamber (SC) implantable cardioverter defibrillator (ICD). DC-ICD had atrial tachyarrhythmia (AT) therapy capabilities. Strict programming recommendations were reinforced. Methods and results Patients with conventional SC-ICD indication were randomized to DC-ICD, SC-ICD, or a DC-ICD programmed as an SC-ICD (SC-simulated) and followed for 16 months. Patients in the DC and SCsimulated groups crossed over after 8 months. The primary endpoint was a composite of CSAE: all-cause mortality; invasive intervention; hospitalization (.24 h) for cardiovascular causes; inappropriate shocks (two or more episodes); and sustained symptomatic AT lasting .48 h. The outcome variable was a prespecified score that corrected for clinical severity and follow-up duration. Three hundred and thirtyfour patients were analysed (DC-ICD, n ¼ 112; SC-ICD, n ¼ 111; SC-simulated, n ¼ 111). The mean left ventricular ejection fraction was 0.36 + 0.13, 69% were in functional class II. CSAE occurred in 65 DC-ICD, 82 SC-ICD, and 84 SC-simulated patients. The outcome variable was 33% lower in the DC-ICD group (OR 0.31; 95% CI 0.14–0.67; P ¼ 0.0028). Mortality was 4% in DC, 9% in SC, and 10% in SC-simulated. Conclusion In patients with a standard SC-ICD indication, DC-ICD was associated with less CSAE when compared with SC-ICD. Introduction The therapeutic benefits of implantable cardioverter defibrillators (ICDs) have been primarily studied in patients * Corresponding author: Servicio de Cardiologia (Planta 5), Hospital Gregorio Maran ˜on, Doctor Esquerdo, 46, 28007 Madrid, Spain. Tel: þ34 915868281; fax: þ34 915868018. E-mail address: almendral@secardiologia.es implanted with single-chamber (SC) devices. However, dualchamber (DC)-ICDs provide atrial pacing, atrioventricular (AV) synchrony, information about the atrial rhythm during tachycardia, and (some DC-ICD) electrical therapy for atrial tachyarrhythmias (ATs). On the other hand, DC-ICDs involve a more complex implant procedure and some of these features could even be harmful. Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2008. For permissions please email: journals.permissions@oxfordjournals.org. The online version of this article has been published under an open access model. Users are entitled to use, reproduce, disseminate, or display the open access version of this article for non-commercial purposes provided that the original authorship is properly and fully attributed; the Journal, Learned Society and Oxford University Press are attributed as the original place of publication with correct citation details given; if an article is subsequently reproduced or disseminated not in its entirety but only in part or as a derivative work this must be clearly indicated. For commercial re-use, please contact journals.permissions&oxfordjournals.org. Downloaded from by guest on October 15, 2014 Cardiology Department, Hospital General Universitario Gregorio Maranon, Madrid, Spain; 2Cardiology Department, Hospital Universitario 12 de Octubre, Madrid, Spain; 3Cardiology Department, University Hospital of Mannheim, Mannheim, Germany; 4 Heart Diseases Department, Hospital San Filippo Neri, Roma, Italy; 5Cardiology Department, Hospital Santa Cruz, Carnaxide, Portugal; 6Estadistica e Investigacion Operativa, Universitat Politecnica de Catalunya, Barcelona, Spain; 7 Scientific and Clinical Department, Medtronic Iberica, Barcelona, Spain; 8Cardiology Department, Hospital General Universitario de Valencia, Valencia, Spain Dual- vs. single-chamber ICD: the DATAS trial When the DATAS Trial started its inclusion phase, in year 2000,1 the information regarding DC-ICD was emerging.2 Two additional concerns were: (a) some laboratory findings, available at that time, suggested negative effects of right ventricular (RV) pacing;3 (b) clinical studies had suggested that the ICD electrode could itself be proarrhythmic, at least transiently after implantation,4 raising the concern for some proarrhythmic effect of the atrial electrode. The DATAS Trial was designed to compare DC-ICD (capable of electrical therapies for AT) and SC-ICD, the outcome being clinically significant adverse events (CSAEs). We hypothesized that both the potential for device-related complications and the potential to reduce or increase spontaneous deleterious effects of the primary disease process would translate into relatively simple and clinically measurable consequences, i.e. CSAE. In order to reduce the potentially negative effects of RV pacing and homogenize the population, strict programming recommendations were made to reduce RV pacing, with the tools available in the ICD at that time. Finally, in order to assess the potential for proarrhythmia (and for a better look at AT in SC devices), a ‘third arm’ of patients with a DC hardware but a SC programming was added to the usual parallel design. The main outcome of the trial is presented here. Study design, randomization, and data collection The design of the trial has been published.1 Briefly, DATAS was a prospective, multicentre, randomized study, with three arms: SC-ICD, DC-ICD, and a DC-ICD system but programmed as SC-ICD (‘SC-simulated arm’) (Figure 1). The DC-ICD and SC-simulated arms crossed over after 8 months (‘programmed crossover’). All other crossovers were considered ‘premature crossovers’ and had to be authorized by an independent Adverse Events Advisory Committee (AEAC). In addition, the AEAC analysed all events (masked as to the patient’s group assignments), classified all adverse events, and validated primary endpoints. The study complies with the Declaration of Helsinki. The study protocol was approved by the IRB at each centre, and informed consent of the subjects was obtained. The randomization procedure was centralized through a specifically designed web site. DATAS investigators are listed in the Appendix. Follow-up started immediately after randomization. A 1-month wash out period was implemented after programmed crossover. Primary endpoint and main outcome The primary endpoint was a composite of five pre-determined CSAE: (i) all-cause mortality, (ii) invasive intervention due to cardiovascular cause, (iii) hospitalization (longer than 24 h) or prolongation of hospitalization due to cardiovascular cause, (iv) inappropriate shocks: two or more episodes with inappropriate shocks, and (v) sustained symptomatic ATs that (a) require urgent termination or (b) lasted more than 48 h leading to therapeutic intervention. Since this composite endpoint was specifically designed to assess the global impact of clinically relevant events, a CSAE-score was created in order to rank clinical severity. Death was obviously the worst outcome; we assigned a high score to a premature crossover because it represented a basic failure of the assigned therapy. Point assignment was as follows: each CSAE: 1 point; death: maximum number of CSAE points in any individual patient in the entire study plus one; premature crossover: maximum number of CSAE points in any individual patient in that study period. Main outcome was defined as the CSAE-score over length of follow-up, i.e. CSAE-score rate. Patient eligibility criteria Patients were eligible for the study if they met a standard Class I indication for an SC-ICD according to the 1998 ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices. After November 2001, patients as those enrolled in the MUSTT study5 were also accepted for inclusion. Every patient eligible for ICD therapy was screened at each centre. Exclusion criteria were the following: (i) permanent AT; (ii) absence of structural heart disease; (iii) implantation criteria for DC pacing: symptomatic sinus node disease, second degree AV block (except asymptomatic Mobitz I), and complete AV block; (iv) a previously implanted pacemaker or ICD; (v) mechanical right heart valve; (vi) any medical condition that would preclude the testing required by the protocol; (vii) any medical condition that would limit study participation; (viii) the patient is unwilling or unable to cooperate or give written informed consent; (ix) legal guardians (of a minor) refuse to give informed consent; (x) inaccessibility for follow-up at the study centre; (xi) indication for cardiac resynchronization therapy; (xii) enrolment or planning to be enrolled in another clinical trial. Implantable cardioverter defibrillator devices and programming All devices were commercially available from Medtronic Inc. (Minneapolis, MN, USA). The DC devices had automatic atrial tiered antitachycardia therapies. There were strong programming recommendations as previously reported1 and summarized as follows: (i) for all devices, a zone with antitachycardia pacing for cycle length ,360 ms; (ii) for SC (or SC-simulated) devices: (a) stability criteria of 50 ms for arrhythmia discrimination; (b) lower pacing rate of 50 bpm or less; (iii) for DC devices: (a) arrhythmia discrimination via the ‘PR logic’ function; (b) lower pacing rate of 70 bpm, in the DDD mode; (c) paced AV of 230 ms, sensed AV of 200 ms, or even longer values to reduce RV pacing; (d) atrial tachycardia detection zone: atrial cycle length 320 ms; (e) atrial fibrillation detection: atrial cycle length ,150 ms; (f) tiered therapies for AT (antitachycardia pacing, 50 Hz, cardioversion). Statistical analysis Figure 1 Study design. Flow chart of the three arms of the study. It should be noted that: (a) the DC group included twice the number of patients since it pooled together patients from the two crossover arms (first period of DC/SC-simulated group and second period of Downloaded from by guest on October 15, 2014 Methods 529 530 SC-simulated/DC true group) and (b) every patient in the SC group would be followed for a longer period of time (17 months) than patients in DC (8 month); (c) in order to make groups as comparable as possible, a 1-month ‘window’ (absence of adverse events counting) was opened at the 9th month in the SC arm. We accounted for this disparity in follow-up duration by calculating a CSAE-score rate; defined as the CSAE-score value divided by months of follow-up. The intention-to-treat principle was used. Two statistical analyses were pre-planned before and during the inclusion phase in the absence of any information about allocated group. The protocol, as well as the sample size calculation, was based on the distribution free Mann–Whitney–Wilcoxon statistic. In order to obtain a more standard effect size measure, an additional primary analysis was changed to the odds ratio (OR) of CSAE-score between DC and SC obtained from SAS GENMOD procedure with the length of follow-up as an ‘offset’ variable and making the assumption of a negative binomial distribution in order to allow the over-dispersion introduced by the highest values imputed to deaths. Both statistics would be able to observe a combination of effects both in the reduction of the proportion of patients with tendency to develop a CSAE, as well as in the mean of CSAE over all patients. J. Almendral et al. Primary endpoint The absolute number of CSAEs was 65 in the DC group when compared with 82 in the SC and 84 in the SC-simulated groups (Figure 3A). The correspondent CSAE-score is depicted in Figure 3B. The rate of CSAE-score (Figure 3C) was 33% lower in the DC group, a difference that was statistically significant (P ¼ 0.0028; OR 0.31; 95% CI 0.14– 0.67). The proportion of patients performing better with DC was also statistically significant (P ¼ 0.030; OR 0.56; 95% CI 0.51–0.62). A secondary sensitivity analysis was performed, including also the 20 patients randomized but not included in the analysis, showing similar results. Although the study was not powered to make statistical comparisons for each of the components of the primary endpoint, these are shown in Table 4 and Figure 4. Of note, total mortality was similar in SC (9%) and SC-simulated (10%) groups, but tended to be lower in the DC group (4%). Discussion Main findings Sample size and power for the main analysis Results Study population Patients were enrolled between November 2000 and December 2003. Figure 2 depicts a flow diagram of patients entering the trial with a final number of 334 patients for analysis. Their relevant clinical data are provided in Table 1. Device implantation and follow-up Lead- and procedure-related complications are depicted in Table 2. There were no statistically significant differences among groups, with a non-significant trend towards a higher procedure-related complication rate in DC-ICD, even if considering DC and SC-simulated (identical hardware, see fourth column in Table 2) as a single group [14/ 223 (6.3%) vs. 3/111 (2.7%), P ¼ NS]. Of the 334 patients, 12 (3.6%) were lost to follow-up (Figure 2). The mean follow-up duration was 16 months in DC, 15.6 in SC, and 15.5 in SC-simulated. There were no significant differences among groups in the percentage of patients on each cardioactive medication at hospital discharge, and at 8- or 17-month follow-up, except for digoxin at the 8-month follow-up (12% in DC, 3% in SC-simulated, P ¼ 0.03). There were 20 premature crossovers during follow-up with only one of those being in the SC-ICD arm (Table 3, Figure 2). The percentage of ventricular pacing, obtained from the device counters at each follow-up visit, is shown in Table 3. Primary outcome Since efficacy for termination of ventricular tachyarrhythmias is expected to be identical in SC and DC devices, but common sense suggests that DC-ICD may have more complications but also some advantages and risks, we addressed the question of whether adverse events differ in these two types of ICD. Some DC-ICDs are also able to sense and treat AT,6,7 with the ability to potentially improve the clinical status of patients by reducing AT burden, an additional element of the study. Not all adverse events have the same clinical implications, and what finally matters is the likelihood of those that (whether produced or reduced by ICD) are clinically relevant, i.e. resulting in death, an invasive intervention, hospitalization, undesired shocks, or prolonged ATs (what we have considered as CSAE). For these reasons, our study focused on CSAE and a score was developed for further ‘tuning’ by assigning a ‘weight’ to each CSAE. Several studies have now been published comparing DC and SC-ICD,8–14 but to the best of our knowledge, this is the first study with a pooled CSAE as the primary endpoint. The results of the primary outcome of the DATAS study are, in this sense, unique, as they show that this outcome variable is better with a DC-ICD than with an SC-ICD device. Procedure/lead-related complications The overall incidence of lead- and device-related complications of 9% compares favourably with that of most recent ICD trials of SC- and DC-ICD that provided a detailed report of complications.8,10 Most of the complications resulted in a CSAE, indicating that the parameters selected for our composite CSAE were sensitive enough to pick up procedure- and lead-related complications. Downloaded from by guest on October 15, 2014 The assumed effect of the DC treatment was a reduction from 30 to 15% in the proportion of patients who develop a CSAE, as well as a 15% reduction in the mean of CSAE (from 6 to 5.1). The estimated sample size1 was 200 (DC true) vs. 100 (SC true) patients followed for 8 months, with a two-sided a ¼ 0.05 and a power of 88.8%. The sample size was set up to 360 patients (120 patients per arm), considering loses in follow-up. The main finding of this study is that in a setting where the excess hardware-related complications of DC devices are limited and the RV pacing effects are reduced by strict programming, the impact of CSAEs was lower in patients with a DC-ICD than in patients with an SC-ICD device. Dual- vs. single-chamber ICD: the DATAS trial 531 Table 1 Patient baseline characteristics Characteristic DCa (n ¼ 112) SC (n ¼ 111) SC-simulateda (n ¼ 111) Age in years, mean + SD Male, n (%) NYHA functional class 2, N/total (%) Clinical History, n (%) Hypertension, n/total (%) Diabetes, n (%) Coronary artery disease, n (%) Cardiomyopathy, n/total (%) Valvular heart disease, n/total (%) Indications for ICD therapy, n (%) VF or cardiac arrest Sustained VT Syncopal VT/syncope with inducible VT/VF Primary prevention Laboratory findings LVEF Bundle branch block, n (%) 66 + 9 92 (82) 77/110 (70) (n ¼ 112) 54 (48) 20 (18) 98 (87) 46 (41) 11 (10) 63 + 10 100 (90) 77/108 (71) (n ¼ 111) 55/109 (50) 32 (29) 99 (90) 56/110 (51) 11/110 (10) 62 + 11 90 (81) 70/109 (64) (n ¼ 110) 64 (58) 28 (25) 88 (80) 51 (46) 19 (17) 31 (28) 46 (41) 19 (17) 16 (14) 41 (37) 42 (38) 16 (14) 12 (11) 47 (42) 37 (33) 16 (14) 11 (10) 34 + 12 24 (21) 35 + 13 26 (23) 39 + 14 33 (30) DC, dual chamber; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; SC, single chamber; VF, ventricular fibrillation; VT, ventricular tachycardia. a Refers to original randomization assignment arm to which these patients belonged during the first 8-month follow-up study period. Ventricular pacing The issue of the negative effects of RV pacing on ventricular function facilitating heart failure has been of increasing interest,15 and this deleterious effect shown to be clinically relevant in DAVID.9 More recently, subanalyses from randomized clinical trials (RCTs) have described the effect of the proportion of paced beats on clinical outcome.16–18 In our study, this effect was not so obvious. The number of heart failure-related hospitalizations was higher in DAVID than in DATAS (13.3 and 22.6% in SC and DC, respectively, at 1 year in DAVID, 5 and 8% at 8 months in DATAS). DAVID selected patients with lower left ventricular ejection fraction (LVEF) (mean LVEF 27% in DAVID and 36% in DATAS) and had more ventricular pacing (60% in DAVID and 40% in DATAS). The recent INTRINSIC RV trial showed if ventricular pacing is minimized with an algorithm, DC-ICD is not inferior to SC-ICD.13 Our results, with an intermediate decrease in %RV pacing producing less deleterious effects, could be consistent with these findings. Downloaded from by guest on October 15, 2014 Figure 2 Summary of patient recruitment and follow-up. 532 J. Almendral et al. Table 2 Lead- and procedure-related complications Variable Lead-related complications Atrial lead dislodgement (%) Atrial lead reposition (%) Ventricular lead dislodgement and reposition (%) Total (%) Procedure-related complications Venous access problem (%) Pocket infections (%) Pocket haematoma (%) Pneumotorax (%) RV perforation (%) Total (%) DC (n ¼ 112) SC (n ¼ 111) SC-simulated (n ¼ 111) 1 (0.9) 0 1 (0.9) 2 (1.8) 0 0 4 (3.6) 4 (3.6) 3 1 3 7 (2.7) (0.9) (2.7) (6.3) 4 (1.8) 1 (0.4) 4 (1.8) 9 (4.0) 1 1 2 2 0 6 0 1 1 0 1 3 2 2 1 2 1 8 (1.8) (1.8) (0.9) (1.8) (0.9) (7.2) 3 (1.3) 3 (1.3) 3 (1.3) 4 (1.8) 1 (0.4) 14 (6.3) (0.9) (0.9) (1.8) (1.8) (5.4) (0.9) (0.9) (0.9) (2.7) DC þ SC-simulated (n ¼ 223) DC, dual chamber; SC, single chamber; RV, right ventricular. Atrial tachyarrhythmias Table 3 Follow-up: premature crossover, proportion of ventricular pacing DC (n ¼ 112) SC (n ¼ 111) SC-simulated (n ¼ 111) Premature crossover Due to symptoms Due to venous access Due to atrial lead problems Unclear reason Total Ventricular pacing Mean % of paced beats Median no. of % paced beats P with .40% paced beats (%) DC!SCsim SC!DC SCsim!DC 1 1 9 3 0 0 4 0 0 1 9 0 1 2 11 40 + 35 3+9 6 + 13 30 0 1 42 (43) 2 (2) 1 (1) Total mortality DC, dual chamber; SC, single chamber; RV, right ventricular; P, patients. Inappropriate shocks The extent to which DC-ICD devices decrease inappropriate therapies has been controversial. Some studies found no benefit of DC devices.8,14 More recently, both in a population with slow VT10 and in a more general population,11 a modest reduction was found. Since frequent ICD shocks are detrimental for patient’s well-being, in our clinically focused approach, it was considered that two or more inappropriate shocks (first inappropriate shock could just mean a need for reprogramming, then preventing further inappropriate shocks) represented a significant problem. Our results point in a similar direction as these recent studies: it is infrequent to have two or more inappropriate shocks, but seems to be even more so in patients with DC-ICD. Two RCTs reported a non-significant trend towards a higher mortality in DC-ICD.9,12 A recent RCT,13 including only patients in whom a DC algorithm minimized ventricular pacing to ,20%, reported non-inferiority of DC-ICD with a favourable mortality trend. In DATAS, with a strict but relatively simple programming and no patient exclusion as to the amount of ventricular pacing, mortality trended similarly. Moreover, the mortality of the SC-simulated group (10%) was similar to that of the SC group, showing inherent consistency of our findings. It can be argued that the short follow-up in DATAS (before crossover) minimizes the deleterious effects of RV pacing. However, an increase in mortality was an early effect in DAVID.9 In contrast to the other reported RCT, our study included electrical therapy for AT. ATs in patients with decreased LVEF are associated with an increase in total mortality, and the composite of death or hospitalization.20 AT left untreated could promote ventricular tachyarrhythmias.21 Inappropriate recognition and therapy of AT could even lead to a vicious life-threatening cycle.22 Limitations The follow-up might have been too short to reveal differences in heart failure-related hospitalizations and related mortality, since by the crossover design of DATAS, each DC patient was not followed for .8 months. However, hospitalizations in the second 8-month period tended to decrease in all arms. Downloaded from by guest on October 15, 2014 Variable Several reports have substantiated the efficacy of some DC-ICD to detect and terminate AT.6,7 However, since most of these ATs lasted only minutes to hours19 and the symptomatic status was largely ignored (device retrieved arrhythmias), their clinical significance is unclear. In contrast, our study considered AT as part of the primary endpoint only if the episodes were symptomatic and/or long-lasting requiring therapeutic intervention, thus with undisputable clinical significance. As such, they were observed in a minority of patients, but mostly in patients with SC devices. Dual- vs. single-chamber ICD: the DATAS trial 533 Figure 3 Number, score, and rate of score of clinically significant adverse events. CSAE, clinically significant adverse effects. See text for details. Table 4 Clinically significant adverse effects: death, invasive interventions, hospitalizations, inappropriate shocks, long-duration AT, each further divided into first and second follow-up periods, and into individual components DC (n ¼ 112) SC (n ¼ 111) SC-simulated (n ¼ 111) Death (%) 1st period/2nd period Arrhythmic Heart failure Other Invasive interventions (%) 1st period/2nd period Hospitalizations (%) 1st period/2nd period Arrhythmia related (%) 1st period/2nd period CHF related (%) 1st period/2nd period Device/procedure related (%) Other (%) Inappropriate shocks (%) 1st period/2nd period Long-duration AT (%) 1st period/2nd period 4 (4) 3/1 10 (9) 7/3 11 (10) 8/3 0 2 2 10 (9) 3 5 2 11 (10) 1 4 6 12 (11) 9/1 6/5 9/3 47 (42) 31/16 42 (38) 31/11 51 (46) 42/9 18 (16) 18 (16) 17 (15) 13/5 16/2 12/5 14 (13) 8/6 6 (5) 5/1 19 (16) 16/3 4 (4) 3 (3) 5 (5) 11 (10) 3 (3) 15 (14) 13 (12) 10 (9) 7 (6) 3/0 13/0 7/0 1 (1) 1/0 6 (5) 4/2 3 (3) 3/0 AT, atrial tachyarrhythmias; CHF, congestive heart failure; DC, dual chamber; P, patients; SC, single chamber. It is possible that recently introduced sophisticated algorithms designed to minimize RV pacing could have further decreased RV pacing.13,23 However, they were introduced after the enrolment of patients in DATAS. Downloaded from by guest on October 15, 2014 Variable Figure 4 Odds ratio for each individual clinically significant adverse effect. Premature crossovers are a limitation of RCT. Despite the need for AEAC authorization, 10% of the patients implanted with a DC-ICD hardware crossed over as opposed to 1% in the SC-ICD. This was likely to have reflected the ease for ‘software crossover’ once the DC hardware is in place (in the DC and SC-simulated arms) when compared with a ‘hardware upgrade’ (in the SC-ICD arm). However, our scoring system severely penalized the premature crossover, thus correcting for this difference. Clinical implications The characteristics of our patient population seem to be similar to those of other recently published ICD series in which patients were not selected based on LV function10–12 534 and thus represents an unselected ICD population, with mean LVEF over 0.30. To this extent, DATAS can be considered representative of the daily clinical ICD practice in typical European countries. In this context, the DATAS study demonstrates a reduction in pooled CSAE with the use of DC-ICD. The study’s conclusions could lead to the development of trials to explore if CSAE can be reduced even further with algorithms intended to minimize RV pacing. Funding This study was funded in full by Medtronic. Acknowledgements This study would not have been possible without Mercedes Ortiz, from Hospital Gregorio Maran ˜on (Madrid, Spain), our study data coordinator. Author contributions: original idea and launching of the study: Aurelio Quesada. Members of the Steering Committee: Aurelio Quesada, Jesus Almendral, Fernando Arribas, Christian Wolpert, Renato Ricci, Pedro Adragao, Xavier Navarro. Statistical design and analysis: Erik Cobo. Funding to pay the Open Access publication charges for this article was provided by Medtronic. www.clinicaltrials.gov Identifier: NCT00157820. Appendix DATAS Investigators and study centres: B. Lu ¨deritz, J. Schwab, T. Lewalter, R. Schimpf, University Hospital, Bonn, Germany; M. Santini, R. Ricci, C. Pignalberi, M. Russo, San Filippo Neri, Rome, Italy; P. Hanrath, Ch. Stellbrink, K. Mischke, R. Koos, University Hospital RWTH, Aachen, Germany; J. Brugada, L. Mont, M. Matas, H. Clinic i Provincial, Barcelona, Spain; J. Gill, R. Simon, A. Rinaldi, N. Gall, St Thomas’ Hospital, London, UK; M. Glikson, Sheba Medical Center, Tel-Hashomer, Israel; J. Roda, S. Villalba, V. Palanca, J. Belchi, H. General Universitario, Valencia, Spain; C. Muto, M. Canciello, G. Carreras, B. Tuccillo, Loreto Mare Hospital, Naples, Italy; A. Arenal, E. Gonzalez-Torrecillas, F. Atienza, H. Gregorio Maran ˜on, Madrid, Spain; M. Borggrefe, S. Spehl, 1st Department of Medicine Cardiology, University Hospital Mannheim, Mannheim, Germany; J.L. Merino, R. Peinado, H. La Paz, Madrid, Spain; J.C. Rodriguez, O. Medina, J. Garcı´a, H. Insular de Gran Canaria, Las Palmas, Spain; F. Morgado, Santa Cruz, Lisbon, Portugal; I. Lozano, J. Toquero, R. Arroyo, H. Puerta de Hierro, Madrid, Spain; J.M. Ormaetxe, M. Arkotxa, H. de Basurto, Bilbao, Spain; G. Steinbeck, E. Hoffman, S. Janko, U. Dorwarth, Ludwig-Maximilian-University Hospital, Mu ¨nchen, Germany; M. Geist, V. Turkisher, Wolfson Medical Center, Holon, Israel; P. Della Bella, G. Fassini, C. Carbucicchio, F. Giraldi, Centro Cardiologico Monzino, Milano, Italy; P. Golino, M. Viscusi, F. Mascia, Hospedale Civile, Caserta, Italy; L. Tercedor, M. Alvarez, H. Virgen de las Nieves, Granada, Spain; J.G. Martinez, A. Iban ˜ez, H. General Universitario, Alicante, Spain; A. Moya, E. Rodriguez, C. Alonso, H. Valle Hebron, Barcelona, Spain; M. Lopez Gil, J. Sanz, H. 12 Octubre, Madrid, Spain; R. Garcia-Civera, R.Ruiz, S. Morell, R. SanJuan, H. Clinico Universitario, Valencia, Spain; A. Garcı´a-Alberola, J. Martinez, J.J. Sanchez, H. Virgen de la Arrixaca, Murcia, Spain; M. Manz, D.Burkhardt, A. Markewitz, Krankenhaus Marienhof, Koblenz, Germany; E. Castellanos, L. Rodriguez-Padial, H. Virgen de la Salud, Toledo, Spain; M. Sassara, A. Achilli, E. Scabbia, Civile Hospital, Viterbo, Italy; J. Olagu ¨e, J.E. Pareja, M.J. Sancho-Tello, H. La Fe, Valencia, Spain; S. Hohnloser, G. Gro ¨nefeld, Johann Wolfgang Goethe University, Frankfurt, Germany; T Fuchs, Assaf Harofe Medical Center, Tzerifin, Israel; W. Jung, N. Schwick, B. Roggenbuck-Schwilk, Klinikum Villingen-Schwenningen, Villingen, Germany; B. Lemke, T. Lawo, T. Deneke, S. Holt, BG Kliniken Bergmannsheil, Bochum, Germany; G.Baumann, H. Bondke, M. Claus, Campus Charite Mitte, Berlin, Germany; A. Maresta, S. Silvani, D. Cornacchia, E. Tampieri, Civile Hospital, Ravenna, Italy; J.J. Manzano, A. Medina, E. Caballero, F. Wangu ¨emert, H. General Dr Negrı´n, Las Palmas, Spain. References 1. Quesada A, Almendral J, Arribas F, Ricci R, Wolpert C, Adragao P et al. The DATAS rationale and design: a controlled, randomized trial to assess the clinical benefit of dual chamber (DDED) defibrillator. Europace 2004;6:142–50. 2. Trappe HJ, Achtelik M, Pfitzner P, Voigt B, Weismuller P. Single-chamber versus dual-chamber implantable cardioverter defibrillators: indications and clinical results. Am J Cardiol 1999;83:8–16D. 3. Tse HF, Lau CP. Long-term effect of right ventricular pacing on myocardial perfusion and function. J Am Coll Cardiol 1997;29:744–9. 4. Kim SG, Ling J, Fisher JD, Wang G, Rameneni A, Roth JA et al. Comparison and frequency of ventricular arrhythmias after defibrillator implantation by thoracotomy versus nonthoracotomy approaches. Am J Cardiol 1994; 74:1245–8. 5. Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med 1999;341:1882–90. 6. Ricci R, Pignalberi C, Disertori M, Capucci A, Padeletti L, Botto G et al. Efficacy of a dual chamber defibrillator with atrial antitachycardia functions in treating spontaneous atrial tachyarrhythmias in patients with lifethreatening ventricular tachyarrhythmias. Eur Heart J 2002;23:1471–9. 7. Adler SW, Wolpert C, Warman EN, Musley SK, Koehler JL, Euler DE et al. Efficacy of pacing therapies for treating atrial tachyarrhythmias in patients with ventricular arrhythmias receiving a dual-chamber implantable cardioverter defibrillator. Circulation 2001;104:887–92. 8. Deisenhofer I, Kolb C, Ndrepepa G, Schreieck J, Karch M, Schmeider S et al. Do current dual chamber cardioverter defibrillators have advantages over conventional single chamber cardioverter defibrillators in reducing inappropriate therapies? A randomized, prospective study. J Cardiovasc Electrophysiol 2001;12:134–42. 9. The DAVID Trial Investigators. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) trial. JAMA 2002;288:3115–23. 10. Bansch D, Steffgen F, Gronefeld G, Wolpert C, Bocker D, Mletzko RU et al. The 1þ1 trial: a prospective trial of a dual- versus a single-chamber implantable defibrillator in patients with slow ventricular tachycardias. Circulation 2004;110:1022–9. 11. Friedman PA, McClelland RL, Bamlet WR, Acosta H, Kessler D, Munger TM et al. Dual-chamber versus single-chamber detection enhancements for implantable defibrillator rhythm diagnosis. The Detect Supraventricular Tachycardia Study. Circulation 2006;113:2871–9. 12. Kolb C, Deisenhofer I, Schmieder S, Barthel P, Zrenner B, Karch MR et al. Long-term follow-up of patients supplied with single-chamber or dualchamber cardioverter defibrillators. Pacing Clin Electrophysiol 2006; 29:946–52. 13. Olshansky B, Day JD, Moore S, Gering L, Rosenbaum M, McGuire M et al. Is dual-chamber programming inferior to single-chamber programming in an implantable cardioverter-defibrillator? Results of the INTRINSIC RV (Inhibition of Unnecessary RV Pacing With AVSH in ICDs) Study. Circulation 2007;115:9–16. 14. Theuns DA, Klootwijk AP, Goedhart DM, Jordaens LJ. Prevention of inappropriate therapy in implantable cardioverter-defibrillators: results of a prospective, randomized study of tachyarrhythmia detection algorithms. J Am Coll Cardiol 2004;44:2362–7. Downloaded from by guest on October 15, 2014 Conflict of interest: J.A. has received honoraria from Medtronic, Guidant (now Boston Scientific), Johnson & Johnson and St Jude Medical for lectures, and has served as a consultant for Johnson & Johnson. C.W. has received honoraria from Medtronic and St Jude Medical for lectures. E.C. is a consultant for Ferrer International and Medtronic, and receives teaching grants from Instituto de Formacio ´n Novartis. X.N. is an employee of Medtronic. A.Q. is currently conducting research sponsored by Medtronic and has served as a paid consultant for Medtronic and Boston Scientific. J. Almendral et al. Dual- vs. single-chamber ICD: the DATAS trial 15. Sweeney MO, Prinzen FW. A new paradigm for physiologic ventricular pacing. J Am Coll Cardiol 2006;47:282–8. 16. Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 2003;107:2932–7. 17. Steinberg JS, Fischer A, Wang P, Schuger C, Daubert J, McNitt S et al. The clinical implications of cumulative right ventricular pacing in the Multicenter Automatic Defibrillator Trial II. J Cardiovasc Electrophysiol 2005;16:359–65. 18. Sharma AD, Rizo-Patron C, Hallstrom AP, O’Neill GP, Rothbart S, Martins JB et al. Percent right ventricular pacing predicts outcomes in the DAVID trial. Heart Rhythm 2005;8:830–4. 19. Darbar D, Warman EN, Hammill SC, Friedman PA, Worldwide Jewel AF Investigators. Recurrence of atrial tachyarrhythmias in implantable cardioverter-defibrillator recipients. Pacing Clin Electrophysiol 2005; 28:1047–51. 535 20. Dries DL, Exner DV, Gersh BJ, Domanski MJ, Waclawiw MA, Stevenson LW. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a retrospective analysis of the SOLVD trials. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol 1998;32: 695–703. 21. Stein KM, Euler DE, Mehra R, Seidl K, Slotwiner DJ, Mittal S et al. Do atrial tachyarrhythmias beget ventricular tachyarrhythmias in defibrillator recipients? J Am Coll Cardiol 2002;40:335–40. 22. Birgersdotter-Green U, Rosenqvist M, Lindemans FW, Ryden L, Radegran K. Holter documented sudden death in a patient with an implanted defibrillator. Pacing Clin Electrophysiol 1992;15:1008–14. 23. Sweeney MO, Shea JB, Fox V, Adler S, Nelson L, Mullen TJ et al. Randomized pilot study of a new atrial-based minimal ventricular pacing mode in dual-chamber implantable cardioverter-defibrillators. Heart Rhythm 2004;1:160–7. Downloaded from by guest on October 15, 2014
© Copyright 2025